Abstract
Background
Virtual reality (VR) is a computer simulation technique that has been increasingly applied in pain management over the past 2 decades.
Objective
In this study, we used bibliometrics to explore the literature on VR and pain control, with the aim of identifying research progress and predicting future research hot spots.
Methods
We extracted literature on VR and pain control published between 2000 and 2022 from the Web of Science Core Collections and conducted bibliometric analyses. We analyzed the publication and citation trends in the past 2 decades, as well as publication and citation analyses of different countries, institutions, journals, and authors. For references, we conducted cocitation and burst analyses. For keywords, we conducted co-occurrence, clustering, timeline view, and citation burst analyses.
Results
Based on 1176 publications, we found that there was a continuous increase in publication and citation volumes, especially in the last 5 years. The United States was the most representative country, and the University of Washington was the most representative institution, with both having the most publications and citations. The most popular journal in this field was Burns, and Hoffman HG was the most productive author, leading many studies on patients with burn pain. The reference with the most citation burst was a study on the verification of new hardware in pain control. The keywords with the highest citation bursts related to various situations of pain such as “burn pain,” “wound care,” “low back pain,” and “phantom limb.”
Conclusions
VR has been applied in various clinical situations for pain management, among which burns and pediatric surgery have achieved satisfactory results. We infer that VR will be extended to more clinical pain situations in the future, such as pain control in wound care, low back pain, and phantom limb pain. New research hot spots will include the development of software and hardware to improve the immersive experience of VR for pain control. However, our work was based solely on English literature from the Web of Science database. For future studies, we recommend that researchers explore literature from multiple databases to enhance the scope of their research.
Keywords: virtual reality, pain management, bibliometrics, research trends, CiteSpace, VOSviewer
Introduction
Pain is an unpleasant sensory and emotional experience that can affect patients’ quality of life. Any form of harmful irritation has the potential to cause pain, and various medical procedures, including venipuncture and wound care, can result in temporary discomfort for patients. Moreover, chronic pain can have an even more substantial impact on individuals. It has been reported to affect more than 30% of people worldwide, and epidemiological studies have estimated that the prevalence of chronic pain is between 18% and 34.5% [1-3]. To a certain extent, continuous pain can adversely affect the patients’ family relationships and become the cause of both heavy social burden and economic burden [4-7]. The main clinical treatment for pain is medication, including paracetamol, opioids, etc. In addition, there are other interventions to relieve pain such as psychological interventions, acupuncture, massage, and spinal cord stimulation [8]. Because of the strong influence of psychological factors on pain perception, psychological intervention has become an important means of adjuvant drug treatment [9].
Virtual reality (VR) is an emerging technology in the psychological intervention for pain, which immerses users in a virtual 3D environment through a wearable screen [10]. In recent years, research has demonstrated that VR can effectively control pain by shifting attention [11]. Some researchers believe that VR influences memory, emotion, and attention, which can help alleviate pain [12]. Functional magnetic resonance imaging has provided evidence that VR can effectively reduce the activity of brain regions associated with pain [13], similar to the effects of opioids [14]. Due to its action mechanism, VR has shown significant efficacy in controlling acute pain and has been used in the management of pain during procedures such as burn wound care and acupuncture [15,16]. Additionally, VR has been applied to chronic pain management, where it creates a sense of presence in a new environment, improves mood, and diverts attention, ultimately reducing pain levels [17]. Chronic conditions such as chronic low back pain [18], chronic cervical pain [19], fibromyalgia [20], complex regional pain syndrome [21], and chronic neuropathic pain have also been targeted with VR-based interventions [22,23].
Despite the growing scientific literature on the use of VR in pain management, there is still a lack of studies on its development trends and hot spots, which can provide scientific guidance for researchers in this area. Bibliometrics is an analytical method that can generate a comprehensive view or quantitative parametric analysis of an entire research field or a specific scientific application area [24-26]. This study aimed to analyze the application of VR in the field of pain management in the past 2 decades using bibliometrics, to provide researchers with an overall research development trend and to help guide future research directions.
Methods
Search Strategy
We searched publications from the Web of Science Core Collection (WoSCC) for analysis. The search strategy was “((TS= (virtual reality)) AND ((TS=(pain)) OR TS= (painful))).” The search was conducted in April 2022.
Included and Excluded Criteria
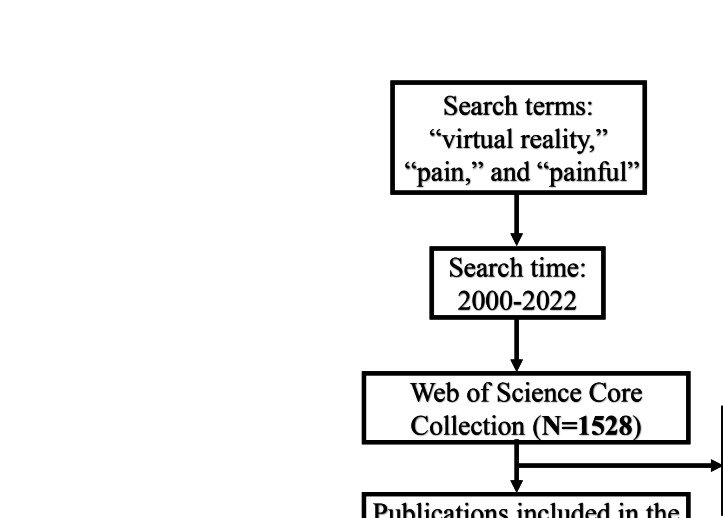
This study included articles and reviews that were published from 2000 to 2022. The following were excluded: (1) non-English literature and (2) publications that are books, book chapters, meeting abstracts, letters, conference proceedings, editorial materials, etc. The screening process is shown in Figure 1.
Figure 1.
The screening process of the selected literature in this study.
Data Export and Analysis
We obtained the information of these publications from the WoSCC through the above search strategy. CiteSpace (version 5.8.R3; Drexel University) and VOSviewer (version 1.6.11.0; Centre for Science and Technology Studies, Leiden University) were used for further data analysis. Quantitative and qualitative analyses were performed and presented in this study, including the following:
Annual trends of the publications and citations: these present the general trends in this field.
Publication and citation analyses of different countries and institutions: these aim to find the countries or institutions that have contributed more to this field and their partnerships. Researchers may choose to learn from or collaborate with them.
Publication and cocitation analyses of different journals: if a study published in journal A and another study published in journal B are both cited by a study published in journal C, then journal A and journal B are considered to have a cocitation relationship and the cocitation count is increased by 1. The definition also extends to the cocitation analysis of authors and references, which is described in further detail below. Journals with a higher number of publications and cocitations are considered as more important journals in the field. Researchers can pay attention to these journals to identify the research progress or publish their study in these journals in the future.
Publication and cocitation analyses of different authors: by identifying authors with a high volume of publications or cocitations, researchers can potentially connect with leading experts and stay informed about their research directions and progress.
Cocitation and citation burst analyses of references: references with a high number of cocitations can provide insights into the research hot spots of a field. These references are widely recognized and cited by authors in the field, indicating their relevance and significance within the research community. Researchers can use these references to identify key topics and focuses within the field. The citation burst analysis is an indication of the increase regarding researchers’ attention to a reference over a given period of time, which is a very important indicator for identifying research hot spot trends.
Keywords analysis (co-occurrence, clustering, timeline view, and citation burst): we presented the keywords in the field based on co-occurrence and obtained the research hot spots in the field through the keywords that appear more frequently. Subsequently, those keywords were divided into several clusters, with similar keywords in each cluster, to capture the main research topics. By tracking these keywords through a timeline perspective, we gained a better understanding of the development and evolution in this field over time. Finally, by the analysis of citation bursts, we identified the research hot spots and trends in the field.
Results
Publication and Citation Trends
A total of 1528 publications were retrieved from the WoSCC. In all, 1176 publications were used for further analysis after excluding 41 non-English publications and 311 other publication types. Time trend analysis showed that from 2000 to 2021, the number of published papers increased from 3 to 234, which was statistically significant (2-tailed t22=4.061, P=.001; Figure 2). The annual citation frequency had also increased from 3 times in 2000 to 5613 times in 2021, which indicated a similarly significant growth (2-tailed t22=3.565, P=.002). In addition, publications and citations in the past 5 years showed a particularly rapidly growth, with an average annual increase of 42.75 papers and 1005.75 citations.
Figure 2.
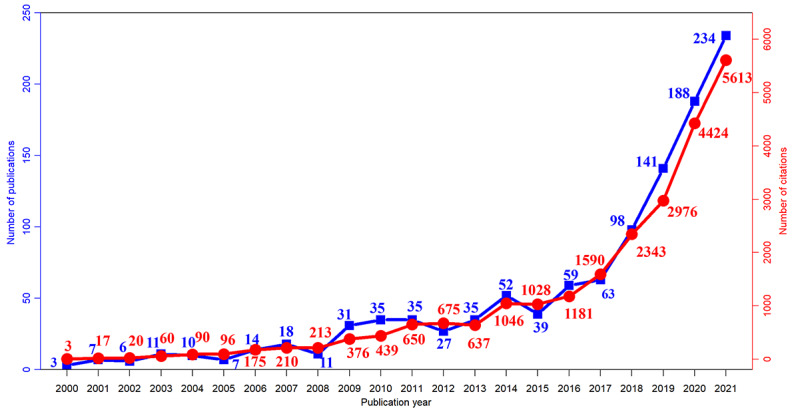
Annual trends of publications and citations.
Distribution of Countries and Institutions
In this study, all the included publications came from 69 countries. The top 11 countries with the most publications are showed in Figure 3A (each node in the figure represents a country). Of these countries, the United States (n=382) had the most publications, followed by England (n=97), Australia (n=89), Canada (n=86), and Spain (n=81). Furthermore, the country citation analysis is shown in Figure 3B. The lines between countries represent the mutual citation relationship between them (Figure 3B); more frequent citations are represented by thicker lines. A total of 1674 institutions participated in this research area, as shown in Figure 3C. In this figure, the institution that generated the most publications was the University of Washington (n=70), followed by the University of Barcelona (n=19), University of Queensland (n=18), University of Haifa (n=14), and University of Sydney (n=14). Similarly, we also analyzed the citation of institutions (Figure 3D). The top 5 countries and institutions with the most citations are summarized in Table S1 in Multimedia Appendix 1. Moreover, clustering analyses of countries and institutions are summarized in Tables S2 and S3 in Multimedia Appendix 1. A total of 5 and 12 clusters were found for countries and institutions, respectively. The top 5 countries and institutions in each cluster are shown in Tables S2 and S3 in Multimedia Appendix 1.
Figure 3.
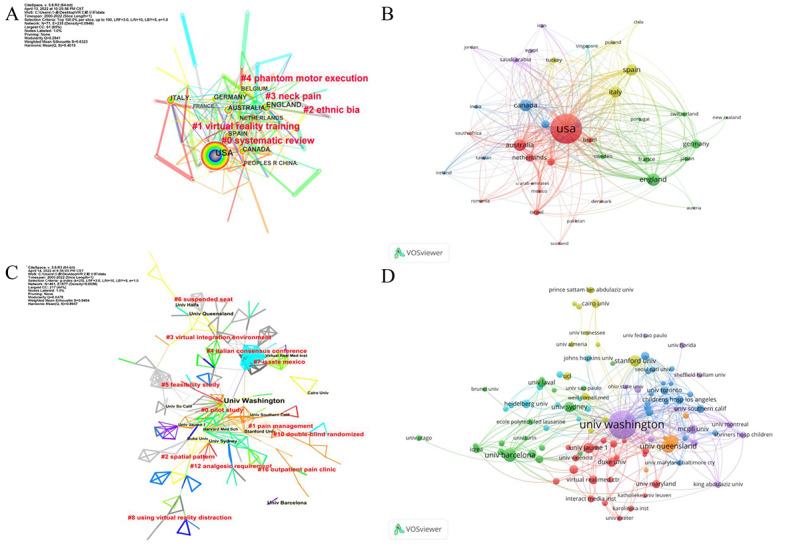
Distribution of countries and institutions. (A) Cooperation mapping of different countries. (B) Citation mapping of different countries. (C) Cooperation mapping of different institutions. (D) Citation mapping of different institutions.
Distribution of Journals
The included 1176 publications on pain and VR research came from 720 academic journals, of which the top 10 journals with the most publications accounted for 15.31% (180/1176) of the total publications, which can be considered as authoritative journals or mainstream journals in this field. Figure 4A shows the visualization results of the publications by different journals. Each node represents a journal, and a larger node indicates greater volume of publications. The cocitation relationship between journals is shown in Figure 4B. The line connecting the nodes indicates that there was a cocitation relationship between the 2 nodes. The top 10 journals with the most publications and cocitations are summarized in Table 1. Among the top 10 journals, 60% (n=6) were from the Q1 quartile and 30% (n=3) were from the Q2 quartile.
Figure 4.
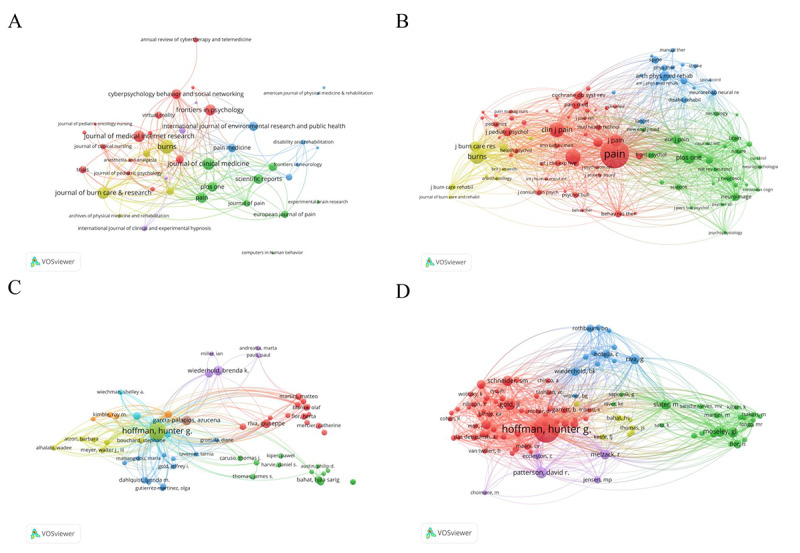
Distribution of journals and authors. (A) Publication mapping of different journals. (B) Cocitation mapping of different journals. (C) Cooperation mapping of different authors. (D) Cocitation mapping of different authors.
Table 1.
The top 10 journals with the most publications and cocitations.
| Ranking | Journal | JCRa category | Category rank in 2020 | Category quartile in 2020 | IFb in 2020 | Publications or cocitations, n | |
| Publications | |||||||
| 1 | Burns |
|
|
|
2.744 | 23 | |
| 2 | Journal of Burn Care and Research |
|
|
|
1.845 | 20 | |
| 3 | Journal of Clinical Medicine |
|
|
|
4.242 | 20 | |
| 4 | Journal of Medical Internet Research |
|
|
|
5.428 | 19 | |
| 5 | Frontiers in Psychology |
|
|
|
2.988 | 18 | |
| 6 | Pain |
|
|
|
6.961 | 17 | |
| 7 | Cyberpsychology Behavior and Social Networking |
|
|
|
4.157 | 16 | |
| 8 | PLoS One |
|
|
|
3.24 | 16 | |
| 9 | Scientific Reports |
|
|
|
4.38 | 16 | |
| 10 | International Journal of Environment Research and Public Health |
|
|
|
3.39 | 15 | |
| Cocitations | |||||||
| 1 | Pain |
|
|
|
6.961 | 2341 | |
| 2 | Cyberpsychology & Behavior |
|
|
|
2.71 | 946 | |
| 3 | Clinical Journal of Pain |
|
|
|
3.442 | 930 | |
| 4 | Burns |
|
|
|
2.744 | 914 | |
| 5 | PLoS One |
|
|
|
3.24 | 728 | |
| 6 | Journal of Pain |
|
|
|
5.828 | 688 | |
| 7 | Journal of Burn Care & Research |
|
|
|
1.845 | 558 | |
| 8 | Archives of Physical Medicine and Rehabilitation |
|
|
|
3.966 | 528 | |
| 9 | Cyberpsychology Behavior and Social Networking |
|
|
|
4.157 | 472 | |
| 10 | European Journal of Pain |
|
|
|
3.934 | 467 | |
aJCR: Journal Citation Reports.
bIF: impact factor.
cSCIE: Science Citation Index Expanded.
dSCCI: Social Sciences Citation Index.
Distribution of Authors
The relationships between author and citation are showed in Figure 4C. Each node represents an author and the size of the node indicates the publication counts of the author. The lines between the nodes represent the citation relationship between authors: the thicker the line, the more citations there are between the 2 authors. Table 2 showed the top 10 authors with the most publications and their cocitations. For better visualization, we only included authors with more than 30 cocitations, and a total of 153 authors were included (Figure 4D). The top 10 authors with the most publications came from 4 countries (the United States, Spain, Italy, and Israel), and 7 (70%) out of 10 are American authors.
Table 2.
The top 10 authors with the most publications and cocitations.
| Ranking | Author | Publications or cocitations, n | Country | |
| Publications | ||||
| 1 | Hoffman HG | 47 | United States | |
| 2 | Patterson DR | 32 | United States | |
| 3 | Sharar SR | 28 | United States | |
| 4 | Wiederhold BK | 17 | United States | |
| 5 | Garcia-Palacios A | 16 | Spain | |
| 6 | Riva G | 14 | Italy | |
| 7 | Wiederhold MD | 13 | United States | |
| 8 | Jensen MP | 11 | United States | |
| 9 | Bahat HS | 11 | Israel | |
| 10 | Carrougher GJ | 10 | United States | |
| Cocitations | ||||
| 1 | Hoffman HG | 1561 | United States | |
| 2 | Gold JI | 275 | United States | |
| 3 | Patterson DR | 270 | United States | |
| 4 | Moseley GL | 253 | Australia | |
| 5 | Riva G | 236 | Italy | |
| 6 | Ramachandran VS | 227 | India | |
| 7 | Schneider SM | 225 | United States | |
| 8 | Slater M | 222 | Spain | |
| 9 | Melzack R | 208 | Canada | |
| 10 | Dahlquist L | 168 | United States | |
Distribution of References
We analyzed a total of 36,224 references from 1176 papers. The most frequently cited and cocited papers are summarized in Table 3. The cocitation relationships are visualized in Figure 5A. It is worth noting that the top 10 cocited references were all from the United States, and 6 of them were from Hoffman HG. We found that all the papers that were cocited the most were about pain control using VR technology.
Table 3.
The top 10 papers with the most citations and cocitations.
| Ranking | Citations or cocitations, n | Title | Authors and year | Journal | Country | |
| Citations | ||||||
| 1 | 435 | Virtual Reality in Neuroscience Research and Therapy | Bohil et al [27], 2011 | Nature Reviews Neuroscience | United States | |
| 2 | 304 | Don’t Fear ‘Fear Conditioning’: Methodological Considerations for the Design and Analysis of Studies on Human Fear Acquisition, Extinction, and Return of Fear | Lonsdorf et al [28], 2017 | Neuroscience and Biobehavioral Reviews | Germany | |
| 3 | 274 | Virtual Reality as an Adjunctive Pain Control During Burn Wound Care in Adolescent Patients | Hoffman et al [29], 2000 | Pain | United States | |
| 4 | 254 | Biofeedback in Rehabilitation | Giggins et al [30], 2013 | Journal of Neuroengineering and Rehabilitation | Ireland | |
| 5 | 253 | The Effectiveness of Virtual Reality Distraction for Pain Reduction: A Systematic Review | Malloy and Milling [31], 2010 | Clinical Psychology Review | United States | |
| 6 | 242 | Keeping Pain in Mind: A Motivational Account of Attention to Pain | van Damme et al [32], 2010 | Neuroscience and Biobehavioral Reviews | Belgium | |
| 7 | 239 | Transcontinental Robot-Assisted Remote Telesurgery: Feasibility and Potential Applications | Marescaux et al [33], 2002 | Annals of Surgery | France | |
| 8 | 220 | Use of Virtual Reality for Adjunctive Treatment of Adult Burn Pain During Physical Therapy: A Controlled Study | Hoffman et al [9], 2000 | Clinical Journal of Pain | United States | |
| 9 | 200 | Effectiveness of Virtual Reality-Based Pain Control With Multiple Treatments | Hoffman et al [34], 2001 | Clinical Journal of Pain | United States | |
| 10 | 199 | Virtual Reality as an Adjunctive Non-Pharmacologic Analgesic for Acute Burn Pain During Medical Procedures | Hoffman et al [35], 2011 | Annals of Behavioral Medicine | United States | |
| Cocitations | ||||||
| 1 | 192 | Virtual Reality as an Adjunctive Pain Control During Burn Wound Care in Adolescent Patients | Hoffman et al [29], 2000 | Pain | United States | |
| 2 | 149 | The Effectiveness of Virtual Reality Distraction for Pain Reduction: A Systematic Review | Malloy and Milling [31], 2010 | Clinical Psychology Review | United States | |
| 3 | 142 | Effectiveness of Virtual Reality-Based Pain Control With Multiple Treatments | Hoffman et al [34], 2001 | Clinical Journal of Pain | United States | |
| 4 | 135 | Use of Virtual Reality for Adjunctive Treatment of Adult Burn Pain During Physical Therapy: A Controlled Study | Hoffman et al [9], 2000 | Clinical Journal of Pain | United States | |
| 5 | 116 | Virtual Reality as an Adjunctive Non-Pharmacologic Analgesic for Acute Burn Pain During Medical Procedures | Hoffman et al [35], 2011 | Annals of Behavioral Medicine | United States | |
| 6 | 114 | Effectiveness of Virtual Reality for Pediatric Pain Distraction During IV Placement | Gold et al [36], 2006 | Cyberpsychology & Behavior | United States | |
| 7 | 112 | Virtual Reality and Pain Management: Current Trends and Future Directions | Li et al [37], 2011 | Pain Management | United States | |
| 8 | 104 | A Pilot and Feasibility Study of Virtual Reality as a Distraction for Children With Cancer | Gershon et al [38], 2004 | Journal of the American Academy of Child and Adolescent Psychiatry | United States | |
| 9 | 102 | Modulation of Thermal Pain-Related Brain Activity With Virtual Reality: Evidence From fMRI | Hoffman et al [13], 2004 | Neuroreport | United States | |
| 10 | 102 | Virtual Reality Pain Control During Burn Wound Debridement in the Hydrotank | Hoffman et al [39], 2008 | Clinical Journal of Pain | United States | |
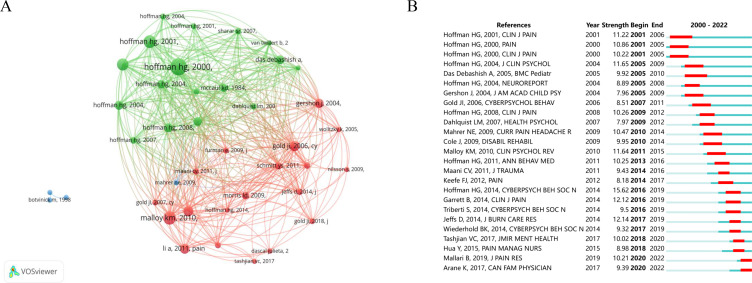
Figure 5.
Distribution of references. (A) Cocitation mapping of different references. (B) Top 25 references with the strongest citation bursts.
Figure 5B [9,11,13,29,31,34-36,38-54] shows the top 25 strongest citation bursted between 2000 and 200enting more citations and green ones representing fewer citations. A burst of reference means that this paper has been cited more frequently by other papers during this period. From the burst analysis of the references, we found that new directions and new hot spots in this field were constantly emerging and research interest in VR and pain had grown substantially. The burst of reference citations first started from 3 papers written by Hoffman HG in 2001, of which 2 were published in the Clinical Journal of Pain and the other in Pain. After a lapse of 14 years, the article published by Hoffman HG in Cyberpsychology Behavior and Social Networking in 2014 became the most persuasive one. These 3 journals were also among the top 10 journals in the field of VR and pain. Moreover, 8 of the top 25 strongest citation reference were published by Hoffman HG, which was sufficient to justify that Hoffman HG was a pioneer and leader in this field. The latest emerging authors were Mallari B and Arane K, who had published articles in the Journal of Pain Research and Canadian Family Physician, and these articles had received high citations recently.
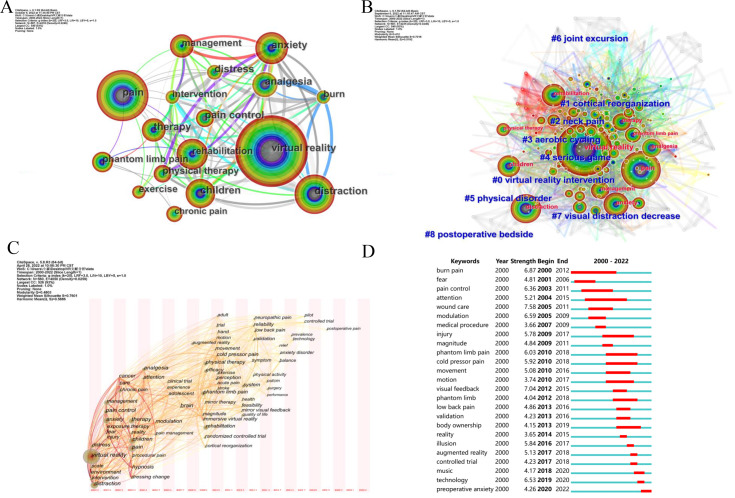
Keyword Analysis
The keyword co-occurrence analysis is shown in Figure 6A. The top 10 keywords and their centrality are summarized in Table S4 in Multimedia Appendix 1. The keyword with the highest number of occurrences was “virtual reality” with the highest centrality of 0.09, followed by “pain” with 348 occurrences and a centrality of 0.07.
Figure 6.
Keyword analyses. (A) Co-occurrence mapping of different keywords. (B) Clustering mapping of different keywords. (C) Timeline view mapping of different keywords. (D) Top 25 keywords with the strongest citation bursts.
A total of 9 clusters were identified in the clustering analysis, and they are shown in Figure 6B. The Q value is 0.412>0.3, and the S value is 0.7018>0.7, indicating that the clusters were credible. The top 10 keywords in each cluster are shown in Table S5 in Multimedia Appendix 1. In the cluster, labels were derived from the keywords; a smaller cluster number indicates that the cluster contains more keywords.
The timeline view analysis is shown in Figure 6C. For better visualization, we only showed keywords with more than 18 occurrences. Each node represents a keyword, and only the year that the keyword first appeared was counted. The size of the nodes indicates the frequency of the occurrence. The lines between nodes refer to 2 keywords appearing in the same paper or several papers. For examples, “virtual reality” first appeared in 2000, and the node is the largest, indicating that “virtual reality” had the most occurrences from 2000 to 2022. “Pain” first appeared in 2003, and there is a connection between “virtual reality” and “pain,” indicating that these 2 keywords appeared in 1 or several papers in 2003 at the same time.
The citation burst analysis of the keywords is shown in Figure 6D. The most cited keyword was “wound care,” followed by “visual feedback,” “burn pain,” and “modulation,” indicating that the research on pain relief using VR technology was very popular in the field of burn pain. The latest hot keyword was “preoperative anxiety.”
Discussion
Overview
With high incidence and prevalence, chronic pain has become the cause of both heavy social burden and economic burden. VR is a computer simulation technique that has been shown to help patients manage their pain, reducing unnecessary medication use and the numerous side effects. In this study, we analyzed the development process of VR in the field of pain management, as well as research hot spots and future trends. Our results showed that publications in this field grew rapidly, and the United States is now leading in this field. According to our research, the hot spot in this field was burn-related pain, and the representative keywords were “virtual reality,” “burn,” “surgery” and “pain control.” This study provides systematic guidance and potential research directions for researchers in this area.
Principal Findings
VR was first popularized for pain control by Hoffman HG in 2000 [29,55]. Subsequently, publications in this field increased slowly from 2000 to 2017. After 2017, the publications increased rapidly from 63 in 2017 to 234 in 2021, with an average annual increase of 42.75 papers. We infer that there may be 2 reasons for this. First, according to the hype cycle of emerging technologies produced by the Gartner Group in 2015 [56], VR just ended the trough of disillusionment period in 2015 and was in the slope of enlightenment period. At that time, more and more organizations carried out in-depth research on VR technology [57]. The second reason is that as many technology companies such as Facebook, Sony, and other companies made huge investments in the VR field around 2016, VR technology has continued to improve. Additionally, there have been more ways for researchers to obtain VR technology while the cost has also become much lower [58]. In the future, with the continuous innovation of VR technology, we believe that the research on VR technology in medical treatment, including pain control, will become more and more popular. In terms of the global publications, the United States had published a total of 382 articles, accounting for about 32.5% of the 1176 selected articles, which indicates that the United States is the absolute leader in this field. In terms of the number of citations, US researchers topped the list with 12,454 citations, indicating that literature published from the United States are authoritatively reliable in the field of VR pain management, which is inseparable from the leading level of VR technology research. Other countries still have great potential for research in this field on the basis of this citation analysis.
The quality of articles published in this field was also high. Overall, 60% of the top 10 journals were from the Q1 quartile. The top 5 journals with the highest number of publications were Burns, Journal of Burn Care & Research, Journal of Clinical Medicine, Journal of Medical Internet Research, and Frontiers in Psychology. To sum up, papers in these journals were mostly about burn pain, which is the first application area of VR in pain control [9,29]. Hoffman et al [59,60] have done a lot on the application of VR in burns, and they have confirmed that VR is effective and feasible in pain control of patients with burn pain. However, the mechanism of VR analgesia has not yet been fully elucidated. Whether the analgesic effect can be improved through interaction in the field of burns is a research trend, and there is still a lot of research space in the field of burns [60].
Research Hot Spots
Combined with literature cocitation analysis and keyword co-occurrence analysis, the current research focus in the field revolves around 2 main areas: the control of burn-related pain and pain control during medical operations in children. Two important studies conducted by Hoffman et al [9,29] in 2000 demonstrated that VR can reduce pain perception in patients with burn pain during physical therapy and alleviate pain during burn wound care. Subsequent clinical experiments have consistently confirmed the pain-reducing effects of VR in procedures such as excision and hydrotherapy debridement for patients with burn pain [39,61-63]. Furthermore, Hoffman et al [64] provided additional evidence for VR’s pain control capabilities in patients with burn pain by using functional magnetic resonance imaging to demonstrate a reduction in pain-related brain activity while using VR devices. Lee et al [65] used functional near infrared spectroscopy to analyze cerebral blood flow in patients with burn pain during VR experiences. They discovered a significant increase in oxygenated hemoglobin in the prefrontal lobe, suggesting that VR activates the prefrontal lobe to inhibit pain sensations.
Researchers have also been interested in understanding the factors that influence VR’s pain control in patients with burn pain. Sharar et al [66] found that VR’s analgesic effect remains consistent regardless of factors such as age, gender, race, burn wound size, or duration of treatment. However, a comparison study by Hoffman et al [67] showed that VR headsets with wider viewing angles result in a more immersive experience and better pain control compared to headsets with narrower viewing angles. In summary, the pain-relieving benefits of VR for patients with burn pain have been consistently validated, and future efforts should focus on optimizing the VR experience to further enhance pain control efficacy.
Moreover, VR has shown promising results in pain relief during medical procedures for pediatric patients. Beyond its application in burn-related scenarios, VR has been used for venipuncture, intravenous catheterization [68], lumbar punctures [69], and even preoperative procedures [70] to alleviate anxiety and minimize procedure-related pain in children. Compared to adults, VR is particularly effective in capturing the attention of children and can be applied in various clinical scenarios. Recent research has explored the use of VR for preoperative anxiety relief, postoperative pain management [71], pain control during vaccinations [72], anesthesia and tooth extraction [73], as well as pain management during emergency sutures [73,74]. In the future, VR is poised to play an important role in various pediatric medical operations.
Research Trends and Directions
The role of VR in pain control has been proven, and future research in this field aims to promote the application scenarios of VR pain control and enhance the user experience for patients to improve the analgesic effect. At present, in addition to the application of treating patients with acute burn pain, the analgesic effect of VR has been applied in the first stage of labor analgesia [75], wound care [76], cystoscopy [77], oral surgery [78], and postoperative pain management [79]. However, further studies are needed to confirm its effectiveness in different clinical scenarios such as gastroenteroscopy and puncture surgery. Patients with chronic pain, including chronic cancer pain, chronic neuropathic pain, and chronic low back pain, can also benefit from VR devices, which can provide pain relief and improve mood [80-83]. To manage chronic pain effectively, there is a need to develop more diverse VR software that caters to the needs of patients.
Improving the patient experience will also be a key focus for future research. As an immersive device, VR presents certain challenges. First, hardware equipment needs to be enhanced to provide a more interactive VR experience, as suggested by Yeo et al [84]. Second, the development of high-quality VR software specific to different pain types is crucial for enhancing the patient experience. Additionally, creating appropriate VR scenarios and games tailored to patients’ needs will contribute to a better patient experience.
In conclusion, this study conducted a 2-decade bibliometric analysis of research on VR interventions in pain management. Currently, the research of VR in the field of pain has received extensive attention, and satisfactory results have been achieved in a series of fields such as burn pain and pediatrics medical procedure–related pain. It is remarkable that burn pain control is still a research hot spot in this field. The emerging trends include the application of VR in other departments related to pain and improving VR technology to enhance the patient experience. However, the mechanism of pain control with VR is not yet understood, and researchers are constantly working in this field, which will guide the development of more effective VR pain management technology.
Strengths and Limitations
This is the first bibliometric analysis of VR research in the field of pain. We provided scientific information in this field and predicted research hot spots and research trends to summarize the research status in this field and further promote the development of this field.
However, there are multiple limitations in our research. First, we only analyzed publications in the WoSCC and failed to exhaust all the publications on VR and pain control. Second, due to limitations of the analysis tools, we only analyzed the papers published in English and discarded other valuable books as well as non–article and review literature such as conference papers. Last but not least, our retrieval methods also have shortcomings, but they simplified the literature so that it is more in line with our theme, and simplicity was conducive to the development of our analysis and research. However, we still hope that future researchers can use more search terms to include some fringe literature in the analysis scope, which may be a useful recommendation for future treatment in this field.
Conclusions
Through bibliometric analysis and visualization, we provided an overview analysis of the field of VR for pain control. There were more than 60 countries participating in this field, and the relative research had been growing rapidly in recent years. The United States and the University of Washington were the representative country and institution, and Hoffman HG was the pioneer in this field. Through the analysis, we identified the hot spots in this research field, which included burn pain and pediatric surgery pain. More attention will be paid to the application of VR in various pain situations in the future, and more diversified software and hardware will be developed to improve the immersive experience of patients, making VR more distracting and more effective at reducing pain.
Acknowledgments
This study was funded by the Shanghai Key Laboratory of Peripheral Nerve and Microsurgery, National Health Commission Key Laboratory of Hand Reconstruction (Fudan University; grant 20DZ2270200), granted to XY; the National Natural Science Foundation of China (grant 82102640), the Medical Scientific Research Foundation of Guangdong Province of China (grant A2023195), the Nanshan District Health Science and Technology project (grant NS2023044), and the Nanshan District Health Science and Technology Major project (grant NSZD2023023), granted to GF; and the Science and Technology Commission of Shanghai Municipality (grant 22S31900100) and Yunnan Academician Expert Workstation (grant 202205AF150058), granted to SH. The funders had no role in study design, data collection, data analysis, interpretation, writing of this report, and in the decision to submit the paper for publication.
Abbreviations
- VR
virtual reality
- WoSCC
Web of Science Core Collection
The top 5 countries and institutions with the most citations, the top 5 countries in each country cluster, the top 5 institutions in each institution cluster, the top 10 co-occurrence keywords and the centrality, and the top 10 keywords in each keyword cluster.
Data Availability
The data sets generated during this study are available from the corresponding author on reasonable request.
Footnotes
XY contributed to project administration, writing–original draft, and writing–reviewing and editing. XY, SZ, and SY share first authorship for their equal contributions to this manuscript. SZ was involved in methodology, software, and writing–reviewing and editing. SY was involved in data curation, investigation, and writing–reviewing and editing. MH and XX contributed to writing–original draft and writing–reviewing and editing. SH, GF, and LL contributed to conceptualization, supervision, and writing–reviewing and editing. SH (tjhss7418@tongji.edu.cn) and GF (fan06309@163.com) are co-corresponding authors.
None declared.
References
- 1.Dahlhamer J, Lucas J, Zelaya C, Nahin R, Mackey S, DeBar L, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018 Sep 14;67(36):1001–1006. doi: 10.15585/mmwr.mm6736a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johannes CB, Le TK, Zhou X, Johnston JA, Dworkin RH. The prevalence of chronic pain in United States adults: results of an internet-based survey. J Pain. 2010 Nov;11(11):1230–1239. doi: 10.1016/j.jpain.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Pitcher MH, von Korff M, Bushnell MC, Porter L. Prevalence and profile of high-impact chronic pain in the United States. J Pain. 2019 Feb;20(2):146–160. doi: 10.1016/j.jpain.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain. 2020 Sep 1;161(9):1976–1982. doi: 10.1097/j.pain.0000000000001939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.West C, Usher K, Foster K, Stewart L. Chronic pain and the family: the experience of the partners of people living with chronic pain. J Clin Nurs. 2012 Dec;21(23-24):3352–3360. doi: 10.1111/j.1365-2702.2012.04215.x. [DOI] [PubMed] [Google Scholar]
- 6.Breivik H, Eisenberg E, O’Brien T, OPENMinds The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health. 2013 Dec 24;13:1229. doi: 10.1186/1471-2458-13-1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain. 2012 Aug;13(8):715–724. doi: 10.1016/j.jpain.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 8.Abdulla A, Adams N, Bone M, Elliott AM, Gaffin J, Jones D, et al. Guidance on the management of pain in older people. Age Ageing. 2013 Mar;42(Suppl 1):i1–i57. doi: 10.1093/ageing/afs200. [DOI] [PubMed] [Google Scholar]
- 9.Hoffman HG, Patterson DR, Carrougher GJ. Use of virtual reality for adjunctive treatment of adult burn pain during physical therapy: a controlled study. Clin J Pain. 2000 Sep;16(3):244–250. doi: 10.1097/00002508-200009000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Liu Z, Ren L, Xiao C, Zhang K, Demian P. Virtual reality aided therapy towards Health 4.0: a two-decade bibliometric analysis. Int J Environ Res Public Health. 2022 Jan 28;19(3):1525. doi: 10.3390/ijerph19031525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arane K, Behboudi A, Goldman RD. Virtual reality for pain and anxiety management in children. Can Fam Physician. 2017 Dec;63(12):932–934. [PMC free article] [PubMed] [Google Scholar]
- 12.Gold JI, Belmont KA, Thomas DA. The neurobiology of virtual reality pain attenuation. Cyberpsychol Behav. 2007 Aug;10(4):536–544. doi: 10.1089/cpb.2007.9993. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, et al. Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport. 2004 Jun 7;15(8):1245–1248. doi: 10.1097/01.wnr.0000127826.73576.91. [DOI] [PubMed] [Google Scholar]
- 14.Hoffman HG, Richards TL, van Oostrom T, Coda BA, Jensen MP, Blough DK, et al. The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesth Analg. 2007 Dec;105(6):1776–1783. doi: 10.1213/01.ane.0000270205.45146.db. [DOI] [PubMed] [Google Scholar]
- 15.Schmitt YS, Hoffman HG, Blough DK, Patterson DR, Jensen MP, Soltani M, et al. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns. 2011 Feb;37(1):61–68. doi: 10.1016/j.burns.2010.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atzori B, Hoffman HG, Vagnoli L, Patterson DR, Alhalabi W, Messeri A, et al. Virtual reality analgesia during venipuncture in pediatric patients with onco-hematological diseases. Front Psychol. 2018 Dec 20;9:2508. doi: 10.3389/fpsyg.2018.02508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Garrett BM, Tao G, Taverner T, Cordingley E, Sun C. Patients perceptions of virtual reality therapy in the management of chronic cancer pain. Heliyon. 2020 May;6(5):e03916. doi: 10.1016/j.heliyon.2020.e03916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nambi G, Abdelbasset WK, Elsayed SH, Alrawaili SM, Abodonya AM, Saleh AK, et al. Comparative effects of isokinetic training and virtual reality training on sports performances in university football players with chronic low back pain-randomized controlled study. Evid Based Complement Alternat Med. 2020 Jun 16;2020:2981273. doi: 10.1155/2020/2981273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harvie DS, Smith RT, Moseley GL, Meulders A, Michiels B, Sterling M. Illusion-enhanced virtual reality exercise for neck pain: a replicated single case series. Clin J Pain. 2020 Feb;36(2):101–109. doi: 10.1097/AJP.0000000000000780. [DOI] [PubMed] [Google Scholar]
- 20.Gulsen C, Soke F, Eldemir K, Apaydin Y, Ozkul C, Guclu-Gunduz A, et al. Effect of fully immersive virtual reality treatment combined with exercise in fibromyalgia patients: a randomized controlled trial. Assist Technol. 2022 May 4;34(3):256–263. doi: 10.1080/10400435.2020.1772900. [DOI] [PubMed] [Google Scholar]
- 21.Sato K, Fukumori S, Matsusaki T, Maruo T, Ishikawa S, Nishie H, et al. Nonimmersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: an open-label pilot study. Pain Med. 2010 Apr;11(4):622–629. doi: 10.1111/j.1526-4637.2010.00819.x. [DOI] [PubMed] [Google Scholar]
- 22.Kumru H, Soler D, Vidal J, Navarro X, Tormos JM, Pascual-Leone A, et al. The effects of transcranial direct current stimulation with visual illusion in neuropathic pain due to spinal cord injury: an evoked potentials and quantitative thermal testing study. Eur J Pain. 2013 Jan;17(1):55–66. doi: 10.1002/j.1532-2149.2012.00167.x. [DOI] [PubMed] [Google Scholar]
- 23.Ortiz-Catalan M, Guðmundsdóttir RA, Kristoffersen MB, Zepeda-Echavarria A, Caine-Winterberger K, Kulbacka-Ortiz K, et al. Phantom motor execution facilitated by machine learning and augmented reality as treatment for phantom limb pain: a single group, clinical trial in patients with chronic intractable phantom limb pain. Lancet. 2016 Dec 10;388(10062):2885–2894. doi: 10.1016/S0140-6736(16)31598-7. [DOI] [PubMed] [Google Scholar]
- 24.Yeung AWK, Souto EB, Durazzo A, Lucarini M, Novellino E, Tewari D, et al. Big impact of nanoparticles: analysis of the most cited nanopharmaceuticals and nanonutraceuticals research. Curr Res Biotechnol. 2020 Nov;2:53–63. doi: 10.1016/j.crbiot.2020.04.002. [DOI] [Google Scholar]
- 25.Yeung AWK, Tzvetkov NT, Georgieva MG, Ognyanov IV, Kordos K, Jóźwik A, et al. Reactive oxygen species and their impact in neurodegenerative diseases: literature landscape analysis. Antioxid Redox Signal. 2021 Feb 10;34(5):402–420. doi: 10.1089/ars.2019.7952. [DOI] [PubMed] [Google Scholar]
- 26.Yeung AWK, Tzvetkov NT, Jóźwik A, Horbanczuk OK, Polgar T, Pieczynska MD, et al. Food toxicology: quantitative analysis of the research field literature. Int J Food Sci Nutr. 2020 Feb;71(1):13–21. doi: 10.1080/09637486.2019.1620184. [DOI] [PubMed] [Google Scholar]
- 27.Bohil CJ, Alicea B, Biocca FA. Virtual reality in Neuroscience research and therapy. Nat Rev Neurosci. 2011 Nov 3;12(12):752–762. doi: 10.1038/nrn3122. [DOI] [PubMed] [Google Scholar]
- 28.Lonsdorf TB, Menz MM, Andreatta M, Fullana MA, Golkar A, Haaker J, et al. “Don't fear 'fear conditioning': methodological considerations for the design and analysis of studies on human fear acquisition, extinction, and return of fear”. Neurosci Biobehav Rev. 2017 Jun;77:247–285. doi: 10.1016/j.neubiorev.2017.02.026. S0149-7634(16)30846-6. [DOI] [PubMed] [Google Scholar]
- 29.Hoffman HG, Doctor JN, Patterson DR, Carrougher GJ, Furness TA. Virtual reality as an adjunctive pain control during burn wound care in adolescent patients. Pain. 2000 Mar;85(1-2):305–309. doi: 10.1016/s0304-3959(99)00275-4. [DOI] [PubMed] [Google Scholar]
- 30.Giggins OM, Persson UM, Caulfield B. Biofeedback in rehabilitation. J Neuroeng Rehabil. 2013 Jun 18;10:60. doi: 10.1186/1743-0003-10-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. 2010 Dec;30(8):1011–1018. doi: 10.1016/j.cpr.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 32.van Damme S, Legrain V, Vogt J, Crombez G. Keeping pain in mind: a motivational account of attention to pain. Neurosci Biobehav Rev. 2010 Feb;34(2):204–213. doi: 10.1016/j.neubiorev.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 33.Marescaux J, Leroy J, Rubino F, Smith M, Vix M, Simone M, et al. Transcontinental robot-assisted remote telesurgery: feasibility and potential applications. Ann Surg. 2002 Apr;235(4):487–492. doi: 10.1097/00000658-200204000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hoffman HG, Patterson DR, Carrougher GJ, Sharar SR. Effectiveness of virtual reality-based pain control with multiple treatments. Clin J Pain. 2001 Sep;17(3):229–235. doi: 10.1097/00002508-200109000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Hoffman HG, Chambers GT, Meyer WJ, Arceneaux LL, Russell WJ, Seibel EJ, et al. Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Ann Behav Med. 2011 Apr;41(2):183–191. doi: 10.1007/s12160-010-9248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS. Effectiveness of virtual reality for pediatric pain distraction during I.V. placement. Cyberpsychol Behav. 2006 Apr;9(2):207–212. doi: 10.1089/cpb.2006.9.207. [DOI] [PubMed] [Google Scholar]
- 37.Li A, Montaño Z, Chen VJ, Gold JI. Virtual reality and pain management: current trends and future directions. Pain Manag. 2011 Mar;1(2):147–157. doi: 10.2217/pmt.10.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gershon J, Zimand E, Pickering M, Rothbaum BO, Hodges L. A pilot and feasibility study of virtual reality as a distraction for children with cancer. J Am Acad Child Adolesc Psychiatry. 2004 Oct;43(10):1243–1249. doi: 10.1097/01.chi.0000135621.23145.05. [DOI] [PubMed] [Google Scholar]
- 39.Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008 May;24(4):299–304. doi: 10.1097/AJP.0b013e318164d2cc. [DOI] [PubMed] [Google Scholar]
- 40.Hoffman HG, Patterson DR, Magula J, Carrougher GJ, Zeltzer K, Dagadakis S, et al. Water-friendly virtual reality pain control during wound care. J Clin Psychol. 2004 Feb;60(2):189–195. doi: 10.1002/jclp.10244. [DOI] [PubMed] [Google Scholar]
- 41.Das DA, Grimmer KA, Sparnon AL, McRae SE, Thomas BH. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556] BMC Pediatr. 2005 Mar 3;5(1):1. doi: 10.1186/1471-2431-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dahlquist LM, McKenna KD, Jones KK, Dillinger L, Weiss KE, Ackerman CS. Active and passive distraction using a head-mounted display helmet: effects on cold pressor pain in children. Health Psychol. 2007 Nov;26(6):794–801. doi: 10.1037/0278-6133.26.6.794. [DOI] [PubMed] [Google Scholar]
- 43.Mahrer NE, Gold JI. The use of virtual reality for pain control: a review. Curr Pain Headache Rep. 2009 Apr;13(2):100–109. doi: 10.1007/s11916-009-0019-8. [DOI] [PubMed] [Google Scholar]
- 44.Cole J, Crowle S, Austwick G, Slater DH. Exploratory findings with virtual reality for phantom limb pain; from stump motion to agency and analgesia. Disabil Rehabil. 2009;31(10):846–854. doi: 10.1080/09638280802355197. [DOI] [PubMed] [Google Scholar]
- 45.Maani CV, Hoffman HG, Morrow M, Maiers A, Gaylord K, McGhee LL, et al. Virtual reality pain control during burn wound debridement of combat-related burn injuries using robot-like arm mounted VR goggles. J Trauma. 2011 Jul;71(1 Suppl):S125–30. doi: 10.1097/TA.0b013e31822192e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Keefe FJ, Huling DA, Coggins MJ, Keefe DF, Rosenthal ZM, Herr NR, et al. Virtual reality for persistent pain: a new direction for behavioral pain management. Pain. 2012 Nov;153(11):2163–2166. doi: 10.1016/j.pain.2012.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoffman HG, Meyer WJ, Ramirez M, Roberts L, Seibel EJ, Atzori B, et al. Feasibility of articulated arm mounted Oculus Rift virtual reality goggles for adjunctive pain control during occupational therapy in pediatric burn patients. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):397–401. doi: 10.1089/cyber.2014.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014 Dec;30(12):1089–1098. doi: 10.1097/AJP.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 49.Triberti S, Repetto C, Riva G. Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):335–345. doi: 10.1089/cyber.2014.0054. [DOI] [PubMed] [Google Scholar]
- 50.Jeffs D, Dorman D, Brown S, Files A, Graves T, Kirk E, et al. Effect of virtual reality on adolescent pain during burn wound care. J Burn Care Res. 2014;35(5):395–408. doi: 10.1097/BCR.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 51.Wiederhold BK, Gao K, Sulea C, Wiederhold MD. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):346–352. doi: 10.1089/cyber.2014.0207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tashjian VC, Mosadeghi S, Howard AR, Lopez M, Dupuy T, Reid M, et al. Virtual reality for management of pain in hospitalized patients: results of a controlled trial. JMIR Ment Health. 2017 Mar 29;4(1):e9. doi: 10.2196/mental.7387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hua Y, Qiu R, Yao WY, Zhang Q, Chen XL. The effect of virtual reality distraction on pain relief during dressing changes in children with chronic wounds on lower limbs. Pain Manag Nurs. 2015 Oct;16(5):685–691. doi: 10.1016/j.pmn.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 54.Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019 Jul 3;12:2053–2085. doi: 10.2147/JPR.S200498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ahmadpour N, Randall H, Choksi H, Gao A, Vaughan C, Poronnik P. Virtual reality interventions for acute and chronic pain management. Int J Biochem Cell Biol. 2019 Sep;114:105568. doi: 10.1016/j.biocel.2019.105568. [DOI] [PubMed] [Google Scholar]
- 56.Rivera J. Gartner's 2015 hype cycle for emerging technologies identifies the computing innovations that organizations should monitor. Gartner. 2015. Aug 18, [2023-10-20]. www.gartner.com/en/newsroom/press-releases/2015-08-18-gartners-2015-hype-cycle-for-emerging-technologies-identifies-the-computing-innovations-that-organizations-should-monitor .
- 57.Verbeek D. Virtual reality in education?!. 8th International Conference on Education and New Learning Technologies; Jul 4-6, 2016; Barcelona, Spain. pp. 6615–6622. [DOI] [Google Scholar]
- 58.Castelvecchi D. Low-cost headsets boost virtual reality’s lab appeal. Nature. 2016 May 12;533(7602):153–154. doi: 10.1038/533153a. [DOI] [PubMed] [Google Scholar]
- 59.Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Front Hum Neurosci. 2019 Aug 8;13:262. doi: 10.3389/fnhum.2019.00262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Al-Ghamdi NA, Meyer WJ, Atzori B, Alhalabi W, Seibel CC, Ullman D, et al. Virtual reality analgesia with interactive eye tracking during brief thermal pain stimuli: a randomized controlled trial (crossover design) Front Hum Neurosci. 2019 Jan 23;13:467. doi: 10.3389/fnhum.2019.00467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Markus LA, Willems KE, Maruna CC, Schmitz CL, Pellino TA, Wish JR, et al. Virtual reality: feasibility of implementation in a regional burn center. Burns. 2009 Nov;35(7):967–969. doi: 10.1016/j.burns.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 62.van Twillert B, Bremer M, Faber AW. Computer-generated virtual reality to control pain and anxiety in pediatric and adult burn patients during wound dressing changes. J Burn Care Res. 2007;28(5):694–702. doi: 10.1097/BCR.0B013E318148C96F. [DOI] [PubMed] [Google Scholar]
- 63.Chan EA, Chung JWY, Wong TKS, Lien ASY, Yang JY. Application of a virtual reality prototype for pain relief of pediatric burn in Taiwan. J Clin Nurs. 2007 Apr;16(4):786–793. doi: 10.1111/j.1365-2702.2006.01719.x. [DOI] [PubMed] [Google Scholar]
- 64.Hoffman HG, Richards TL, Bills AR, Van Oostrom T, Magula J, Seibel EJ, et al. Using fMRI to study the neural correlates of virtual reality analgesia. CNS Spectr. 2006 Jan;11(1):45–51. doi: 10.1017/s1092852900024202. [DOI] [PubMed] [Google Scholar]
- 65.Lee SY, Cha JY, Yoo JW, Nazareno M, Cho YS, Joo SY, et al. Effect of the application of virtual reality on pain reduction and cerebral blood flow in robot-assisted gait training in burn patients. J Clin Med. 2022 Jun 29;11(13):3762. doi: 10.3390/jcm11133762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sharar SR, Carrougher GJ, Nakamura D, Hoffman HG, Blough DK, Patterson DR. Factors influencing the efficacy of virtual reality distraction analgesia during postburn physical therapy: preliminary results from 3 ongoing studies. Arch Phys Med Rehabil. 2007 Dec;88(12 Suppl 2):S43–S49. doi: 10.1016/j.apmr.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 67.Hoffman HG, Seibel EJ, Richards TL, Furness TA, Patterson DR, Sharar SR. Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. J Pain. 2006 Nov;7(11):843–850. doi: 10.1016/j.jpain.2006.04.006. [DOI] [PubMed] [Google Scholar]
- 68.Chan E, Hovenden M, Ramage E, Ling N, Pham JH, Rahim A, et al. Virtual reality for pediatric needle procedural pain: two randomized clinical trials. J Pediatr. 2019 Jun;209:160–167. doi: 10.1016/j.jpeds.2019.02.034. [DOI] [PubMed] [Google Scholar]
- 69.Thomas JJ, Albietz J, Polaner D. Virtual reality for lumbar puncture in a morbidly obese patient with leukemia. Paediatr Anaesth. 2018 Nov;28(11):1059–1060. doi: 10.1111/pan.13505. [DOI] [PubMed] [Google Scholar]
- 70.Eijlers R, Dierckx B, Staals LM, Berghmans JM, van der Schroeff MP, Strabbing EM, et al. Virtual reality exposure before elective day care surgery to reduce anxiety and pain in children: a randomised controlled trial. Eur J Anaesthesiol. 2019 Oct;36(10):728–737. doi: 10.1097/EJA.0000000000001059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Esposito C, Autorino G, Iervolino A, Vozzella EA, Cerulo M, Esposito G, et al. Efficacy of a virtual reality program in pediatric surgery to reduce anxiety and distress symptoms in the preoperative phase: a prospective randomized clinical trial. J Laparoendosc Adv Surg Tech A. 2022 Feb;32(2):197–203. doi: 10.1089/lap.2021.0566. [DOI] [PubMed] [Google Scholar]
- 72.Chang ZY, Kang G-Y, Koh EYL, Fong RJK, Tang J, Goh CK, et al. Immersive virtual reality in alleviating pain and anxiety in children during immunization in primary care: a pilot randomized controlled trial. Front Pediatr. 2022;10:847257. doi: 10.3389/fped.2022.847257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pathak PD, Lakade LS, Patil KV, Shah PP, Patel AR, Davalbhakta RN. Clinical evaluation of feasibility and effectiveness using a virtual reality device during local anesthesia and extractions in pediatric patients. Eur Arch Paediatr Dent. 2023 Jun;24(3):379–386. doi: 10.1007/s40368-023-00801-6. [DOI] [PubMed] [Google Scholar]
- 74.Kavlakci M, Ogce F, Yavan T. The effects of playing digital games on children’s pain, fear, and anxiety levels during suturing: a randomized controlled study. Turk J Emerg Med. 2023 Jun 26;23(3):162–168. doi: 10.4103/tjem.tjem_8_23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Frey DP, Bauer ME, Bell CL, Low LK, Hassett AL, Cassidy RB, et al. Virtual reality analgesia in labor: the VRAIL pilot study-a preliminary randomized controlled trial suggesting benefit of immersive virtual reality analgesia in unmedicated laboring women. Anesth Analg. 2019 Jun;128(6):e93–e96. doi: 10.1213/ANE.0000000000003649. [DOI] [PubMed] [Google Scholar]
- 76.Guo C, Deng H, Yang J. Effect of virtual reality distraction on pain among patients with hand injury undergoing dressing change. J Clin Nurs. 2015 Jan;24(1-2):115–120. doi: 10.1111/jocn.12626. [DOI] [PubMed] [Google Scholar]
- 77.Walker MR, Kallingal GJS, Musser JE, Folen R, Stetz MC, Clark JY. Treatment efficacy of virtual reality distraction in the reduction of pain and anxiety during cystoscopy. Mil Med. 2014 Aug;179(8):891–896. doi: 10.7205/MILMED-D-13-00343. [DOI] [PubMed] [Google Scholar]
- 78.Furman E, Jasinevicius TR, Bissada NF, Victoroff KZ, Skillicorn R, Buchner M. Virtual reality distraction for pain control during periodontal scaling and root planing procedures. J Am Dent Assoc. 2009 Dec;140(12):1508–1516. doi: 10.14219/jada.archive.2009.0102. [DOI] [PubMed] [Google Scholar]
- 79.Mosso-Vázquez JL, Gao K, Wiederhold BK, Wiederhold MD. Virtual reality for pain management in cardiac surgery. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):371–378. doi: 10.1089/cyber.2014.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ahern MM, Dean LV, Stoddard CC, Agrawal A, Kim K, Cook CE, et al. The effectiveness of virtual reality in patients with spinal pain: a systematic review and meta-analysis. Pain Pract. 2020 Jul;20(6):656–675. doi: 10.1111/papr.12885. [DOI] [PubMed] [Google Scholar]
- 81.Castelnuovo G, Giusti EM, Manzoni GM, Saviola D, Gatti A, Gabrielli S, et al. Psychological considerations in the assessment and treatment of pain in neurorehabilitation and psychological factors predictive of therapeutic response: evidence and recommendations from the Italian consensus conference on pain in neurorehabilitation. Front Psychol. 2016 Apr 19;7:468. doi: 10.3389/fpsyg.2016.00468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bani Mohammad E, Ahmad M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: a randomized control trial. Palliat Support Care. 2019 Feb;17(1):29–34. doi: 10.1017/S1478951518000639. [DOI] [PubMed] [Google Scholar]
- 83.Chuan A, Zhou JJ, Hou RM, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021 May;76(5):695–704. doi: 10.1111/anae.15202. [DOI] [PubMed] [Google Scholar]
- 84.Yeo NL, White MP, Alcock I, Garside R, Dean SG, Smalley AJ, et al. What is the best way of delivering virtual nature for improving mood? an experimental comparison of high definition TV, 360° video, and computer generated virtual reality. J Environ Psychol. 2020 Dec;72:101500. doi: 10.1016/j.jenvp.2020.101500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The top 5 countries and institutions with the most citations, the top 5 countries in each country cluster, the top 5 institutions in each institution cluster, the top 10 co-occurrence keywords and the centrality, and the top 10 keywords in each keyword cluster.
Data Availability Statement
The data sets generated during this study are available from the corresponding author on reasonable request.