Abstract
Fibromyalgia is a complex chronic pain disorder that significantly impacts the quality of life of affected individuals. The etiology of fibromyalgia remains elusive, necessitating effective treatment options. This review aims to provide an overview of current treatment options for fibromyalgia and highlight recent updates in managing the condition.
The methodology employed in this systematic review comprised the following key steps. We conducted a comprehensive search across various databases to identify pertinent studies published between 2000 and 2023. Inclusion criteria were defined to specifically target studies involving adult individuals diagnosed with fibromyalgia, with a focus on both pharmacological and non-pharmacological interventions for managing the condition. The review encompassed a range of study types, including randomized controlled trials, observational studies, and systematic reviews. To ensure the quality of the selected studies, we employed appropriate assessment tools, and data extraction and synthesis adhered to established guidelines. This rigorous approach allowed for a robust analysis of the literature on fibromyalgia management.
In the course of our review, it became evident that a spectrum of treatment approaches holds significant promise in the management of fibromyalgia. Specifically, pharmacological interventions, including selective serotonin-norepinephrine reuptake inhibitors, anticonvulsants, cannabinoids, tropisetron, and sodium oxybate, have exhibited substantial potential in alleviating fibromyalgia symptoms. Concurrently, non-pharmacological strategies, such as cognitive-behavioral therapy, exercise regimens, and complementary and alternative therapies, have yielded positive outcomes in improving the condition's management. Recent developments in the field have introduced innovative pharmacological agents like milnacipran and pregabalin, in addition to non-pharmacological interventions like mindfulness-based stress reduction and aquatic exercise, expanding the array of options available to enhance fibromyalgia care and alleviating patient symptoms.
Fibromyalgia necessitates a multidisciplinary approach to treatment, encompassing both pharmacological and non-pharmacological interventions. Recent updates in fibromyalgia management offer additional options to alleviate symptoms and improve the quality of life for individuals with fibromyalgia. Healthcare professionals should remain informed about these advancements to provide evidence-based care, addressing the complex symptoms associated with fibromyalgia and enhancing patient outcomes.
Keywords: quality of life (qol), complementary therapy, cognitive-behavioral therapy, chronic pain disorder, fibromyalgia
Introduction and background
Fibromyalgia, a debilitating chronic pain disorder that predominantly affects women, is a complex condition characterized by widespread pain, tenderness, and chronic fatigue [1,2]. Despite extensive research, its etiology remains enigmatic, and there is no known cure [3]. The profound impact of fibromyalgia on patients' quality of life underscores the need for effective treatment options.
Fortunately, recent advancements in pharmacological and non-pharmacological approaches have emerged as viable alternatives for managing fibromyalgia [4]. Pharmacological options, such as antidepressants, anticonvulsants, and muscle relaxants, have shown promise in providing pain relief and improving patients' well-being [5]. However, the limitations of these drugs, such as potential side effects, have resulted in alternative treatments being developed [6]. Non-pharmacological interventions, such as cognitive-behavioral therapy and exercise, and alternative therapies, such as acupuncture and massage therapy, have shown encouraging results in reducing pain and fatigue and enhancing overall quality of life [7,8]. Lifestyle changes, such as improving sleep hygiene and stress reduction, also play an integral role in managing the symptoms of fibromyalgia [9].
As research in fibromyalgia treatment progresses, recent updates in the management of this condition have emerged. Novel pharmacological agents, such as milnacipran and pregabalin, and non-pharmacological interventions, such as mindfulness-based stress reduction and aquatic exercise, have demonstrated promise in alleviating symptoms and improving patients' quality of life [7,10,11]. Healthcare professionals must remain informed of these recent updates in fibromyalgia treatment to offer comprehensive and evidence-based care to their patients. By staying informed, healthcare providers can make informed decisions that address the complex symptoms of fibromyalgia. This review provides an overview of current treatment options for fibromyalgia and summarizes recent updates in managing the condition. We evaluate the strength of the evidence supporting these updates and discuss their clinical implications. We aim to enhance healthcare professionals' knowledge and facilitate informed decision-making in managing fibromyalgia to offer optimal care for patients suffering from this debilitating condition.
Review
Methods
The databases, including PubMed, MEDLINE, Scopus, Web of Science, and Embase, were searched for relevant studies published between 2000 and 2023. The following search terms were used in combination with Boolean operators: fibromyalgia, treatment, therapy, intervention, pharmacological, non-pharmacological, complementary, alternative, latest, advancements, developments, novel, and innovative. The search was limited to articles published in the English language from the year 2000 to the present.
Inclusion Criteria
We followed the PICOSTL (population, intervention, comparison, outcomes, study design, timeframe, and language) criteria.
Population: Adult individuals (18 years and older) diagnosed with fibromyalgia syndrome (FMS).
Intervention: Pharmacological and non-pharmacological interventions for FMS management, including dosage, frequency, duration, and mode of delivery.
Comparison: Studies with a clearly defined control group, if applicable.
Outcomes: (a) Primary or secondary outcomes relevant to FMS management, such as pain, physical function, quality of life, or other FMS-related symptoms. (b) Adverse events associated with the intervention(s) used.
Study design: Randomized controlled trials, observational studies, and systematic reviews.
Timeframe: Studies published between 2000 and 2023.
Language: Only studies published in English were included.
Exclusion Criteria
Studies with a small sample size may limit generalizability or statistical power, studies that lack a clear description of the intervention(s) used or have poorly defined intervention(s), studies that do not report on relevant outcomes or adverse events, studies that do not report on the statistical significance of the results or effect sizes, and study designs such as case reports and case series were excluded.
Data Extraction
Two reviewers independently extracted data from eligible studies using a standardized data extraction form. The data extraction form included information on study design, participant characteristics, intervention type, outcome measures, and results.
Quality Assessment
The quality of eligible studies was assessed using appropriate tools, such as the Cochrane risk of bias tool and the Joanna Briggs Institute critical appraisal tool, by two independent reviewers. Any discrepancies were resolved through discussion or consultation with a third reviewer.
By registering the systematic review in the International Prospective Register of Systematic Reviews (PROSPERO; ID-CRD42023421154) and following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, the review process was transparent, reproducible, and of high quality, which enhanced the credibility and validity of the systematic review.
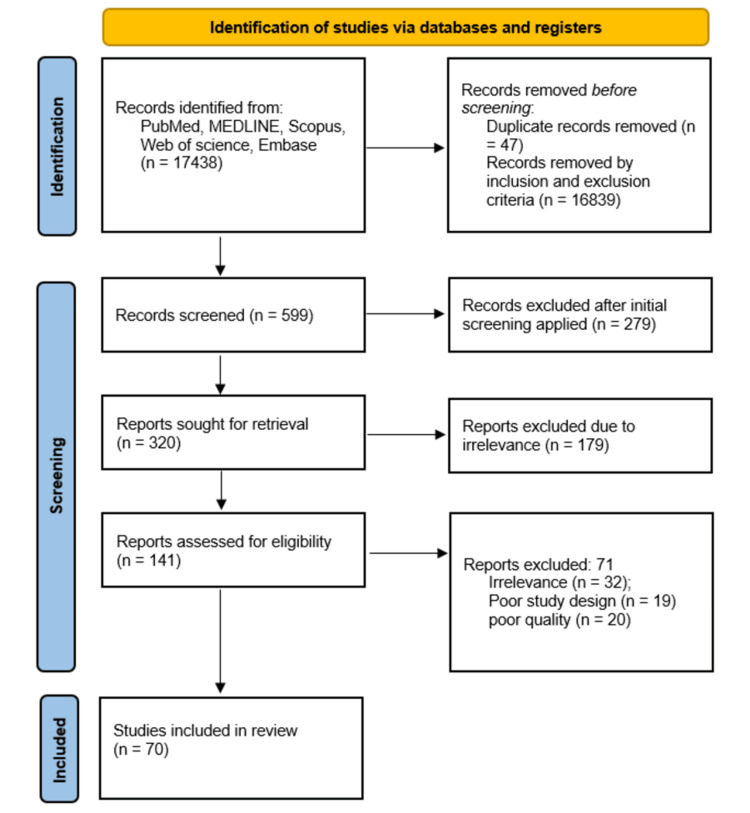
To eliminate bias and ensure quality control in the systematic review, the following steps were taken as depicted in Figure 1.
Figure 1. PRISMA flowchart for the studies included in the review.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
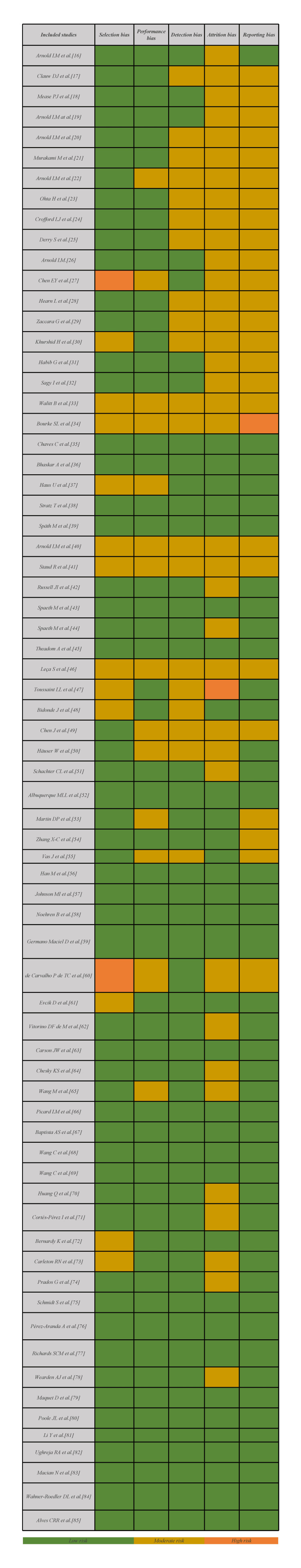
The heterogeneity of the included manuscripts is reported in Figure 2.
Figure 2. Heterogeneity of the studies included in the manuscript.
Results
Overview of Fibromyalgia Treatment Options
Pharmacological treatments: Pharmacological treatments for fibromyalgia include analgesics, antidepressants, anticonvulsants, muscle relaxants, and opioids. Analgesics can provide short-term relief for fibromyalgia pain but are generally not recommended for long-term use due to potential side effects. Antidepressants, including selective serotonin reuptake inhibitors (SSRIs), selective serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs), are often prescribed to regulate levels of neurotransmitters involved in pain perception [12,13]. Anticonvulsants, such as pregabalin and gabapentin, work by reducing nerve activity involved in pain signaling [14]. Muscle relaxants, including cyclobenzaprine and tizanidine, reduce muscle spasms and promote relaxation [15]. Opioids may be used for severe fibromyalgia pain, but they are not recommended for long-term use due to the risk of dependence and worsening symptoms over time.
Non-pharmacological treatments: In addition to pharmacological treatments, non-pharmacological treatments include cognitive behavioral therapy (CBT), exercise, sleep hygiene, occupational therapy, hydrotherapy, transcutaneous electrical nerve stimulation (TENS), graded exercise therapy, psychological therapies, and complementary and alternative therapies such as acupuncture, massage therapy, mind-body therapies, and dietary supplements [9-11]. Individuals with fibromyalgia need to work with healthcare providers to develop a comprehensive treatment plan that is tailored to their individual needs and abilities. The overview of fibromyalgia treatment options is tabulated in Table 1.
Table 1. Overview of fibromyalgia treatment options.
| Treatment options | Principles | Significance | References | |
| Pharmacological treatments | ||||
| Selective serotonin-norepinephrine reuptake inhibitors (SNRIs) | Alleviate pain, fatigue, and sleep disturbances associated with fibromyalgia | Demonstrated effectiveness in reducing pain and fatigue and improving quality of life. Well-tolerated and effective for managing multiple symptoms. | Arnold LM et al. (2008) [16]; Clauw DJ et al. (2008) [17]; Mease PJ et al. (2009) [18]; Arnold LM et al. (2005) [19]; Arnold LM et al. (2010) [20]; Murakami M et al. (2015) [21]; Arnold LM et al. (2009) [22] | |
| Anticonvulsants | Pregabalin | Reduce pain, sleep disturbances, and anxiety associated with fibromyalgia | Demonstrated effectiveness in reducing pain, improving sleep patterns, and reducing fatigue. Adverse effects include dizziness and somnolence. | Ohta H et al. (2012) [23]; Crofford LJ et al. (2005) [24]; Derry S et al. (2016) [25] |
| Mirogabalin | Potential treatment for fibromyalgia | Effective in reducing pain and improving sleep quality. Associated with central nervous system side effects. | Arnold LM et al. (2019) [26]; Chen EY et al. (2021) [27] | |
| Lacosamide | Potential analgesic effects | More effective than the placebo in reducing pain and improving sleep quality. Adverse effects include dizziness, nausea, and tremor. | Hearn L et al. (2012) [28]; Zaccara G et al. (2013) [29] | |
| Cannabidiol (CBD) and tetrahydrocannabinol (THC) | Interact with the endocannabinoid system to regulate pain, mood, and sleep | Effective in reducing pain, improving sleep quality, and reducing anxiety and depression. Potential side effects include dizziness and dry mouth. | Khurshid H et al. (2021) [30]; Habib G, Artul S (2018) [31]; Sagy I et al. (2019) [32]; Walitt B et al. (2016) [33]; Bourke SL et al. (2022) [34]; Chaves et al. (2020) [35] Bhaskar A et al. (2021) [36] | |
| Tropisetron | 5-HT3 receptor antagonist | More effective than placebo in reducing pain and fatigue, and improving sleep quality. | Haus U et al. (2000) [37]; Stratz T et al. (2001) [38]; Späth M et al. (2004) [39]; Arnold LM (2006) [40] | |
| Sodium oxybate | Central nervous system depressant | Effective in reducing pain, fatigue, and sleep disturbance. Common side effects include nausea, dizziness, and vomiting. | Staud R (2011) [41]; Russell JI et al. (2011) [42]; Spaeth M et al. (2012) [43]; Spaeth M et al. (2013) [44] | |
| Non-pharmacological treatments | ||||
| Mind-body interventions | Target stress, anxiety, and depression | Effective in reducing pain and fatigue, and improving quality of life. | Theadom A et al. (2015) [45]; Leça S and Tavares I (2022) [46]; Toussaint LL (2012) [47] | |
| Exercise therapy | Improve physical function and reduce pain and fatigue | Effective in reducing pain and fatigue, and improving quality of life. | Bidonde J et al. (2017) [48]; Chen J et al. (2022) [49]; Häuser W et al. (2010) [50]; Schachter CL et al. (2003) [51]; Albuquerque MLL et al. (2023) [52] | |
| Acupuncture | Traditional Chinese medicine technique | Effective in reducing pain and improving quality of life. | Martin DP et al. (2006) [53]; Zhang X-C et al. (2019) [54]; Vas J et al. (2016) [55]; Han M et al. (2020) [56] | |
| Transcutaneous electrical nerve stimulation (TENS) | Modulate pain signals in nerves | Effective in reducing pain and fatigue, and improving physical function. | Johnson MI et al. (2017) [57]; Noehren B et al. (2015) [58] | |
| Low-level laser therapy | Modulate cellular function and reduce inflammation | Effective in reducing pain and fatigue, and improving quality of life. | Germano Maciel D et al. (2018) [59]; De Carvalho P de TC et al. (2012) [60] | |
| Hydrotherapy | Use of water for therapeutic purposes | Effective in reducing pain and fatigue, and improving physical function. | Evcik D et al. (2008) [61]; Vitorino DF de M et al. (2006) [62] | |
| Yoga therapy | Practice of physical postures, breathing techniques, and meditation | Effective in reducing pain, anxiety, and depression, and improving physical function. | Carson JW et al. (2010) [63] | |
| Music therapy | Use of music for therapeutic purposes | Effective in reducing pain, anxiety, and depression. | Chesky KS et al. (1997) [64]; Wang M et al. (2020) [65]; Picard LM et al. (2014) [66] | |
| Mindfulness-based art therapy (MBAT) | Use of art-making and mindfulness-based practices | Effective in reducing pain, anxiety, and depression, and improving quality of life. | Leça S, Tavares I (2022) [46]; Baptista AS et al. (2013) [67] | |
| Tai chi | Chinese martial art involving slow movements and meditation | Effective in reducing pain and fatigue, and improving physical function. | Wang C et al. (2010) [68]; Wang C et al. (2018) [69] | |
| Virtual reality distraction therapy (VRDT) | Use of virtual reality technology to distract from pain | Effective in reducing pain and improving quality of life. | Huang Q et al. (2022) [70]; Cortés-Pérez I et al. (2021) [71] | |
| Cognitive behavioral therapy (CBT) | Focus on changing negative thoughts and behaviors | Effective in reducing pain, anxiety, and depression, and improving quality of life. | Bernardy K et al. (2013) [72]; Carleton RN et al. (2011) [73]; Prados G et al. (2020) [74] | |
| Mindfulness-based stress reduction (MBSR) | Practice of mindfulness meditation and yoga | Effective in reducing pain and fatigue, and improving quality of life. | Schmidt S et al. (2011) [75]; Pérez-Aranda A et al. (2019) [76] | |
| Graded exercise therapy (GET) | Gradual increase in physical activity levels | Effective in improving physical function, but may cause increased pain in some patients. | Richards SCM et al. (2002) [77]; Wearden AJ et al. (1998) [78]; Maquet D et al. (2007) [79] | |
| Occupational therapy | Strategies for managing symptoms and maintaining daily activities | Effective in helping patients manage symptoms and improve daily functioning. | Poole JL and Siegel P (2017) [80] | |
| Massage therapy | Manipulation of soft tissues in the body | Effective in reducing pain, stiffness, and fatigue. | Li Y et al. (2014) [81]; Ughreja RA et al. (2021) [82] | |
| Dietary supplements | Manage symptoms and potentially alleviate deficiencies | Some dietary supplements have been studied for their potential benefits in managing fibromyalgia symptoms. | Macian N et al. (2022) [83]; Wahner-Roedler DL et al. (2011) [84]; Alves CRR et al. (2013) [85] | |
Recent updates in fibromyalgia treatment
Pharmacological Treatments
In recent years, there have been updates in the pharmacological treatments for fibromyalgia, including the introduction of new drugs and studies examining the effectiveness of existing and new drugs.
Selective serotonin-norepinephrine reuptake inhibitors (SNRIs): SNRIs used for treating fibromyalgia include milnacipran and duloxetine.
Milnacipran: Milnacipran is an FDA-approved SNRI used for treating fibromyalgia. It has been found to effectively reduce pain, fatigue, and sleep disturbances associated with this condition. In a clinical trial, milnacipran demonstrated a significant reduction in pain scores compared to a placebo [16]. Furthermore, a study by Clauw et al. showed that both doses of milnacipran (100 and 200 mg/day) resulted in notable improvements in pain and other symptoms [17]. Milnacipran not only improves function and quality of life but also exhibits a favorable safety profile, being well-tolerated and effective for managing multiple symptoms of fibromyalgia [18]. Adverse effects such as nausea and headache were rarely reported and were the most commonly observed [18].
Duloxetine: Duloxetine, an FDA-approved SNRI, is utilized for treating fibromyalgia. It has demonstrated effectiveness in reducing pain, fatigue, and depression associated with this condition. In a clinical trial, duloxetine exhibited a significant decrease in pain scores when compared to a placebo [19]. Treatment with duloxetine at doses of 60, 90, and 120 mg/day resulted in substantial improvements, including a sense of well-being, pain reduction, decreased sleep difficulties, and enhancements in mood, stiffness, fatigue, and functioning [20]. Duloxetine treatment was found to be safe and well-tolerated [21]. Additionally, duloxetine has been shown to enhance function and improve the quality of life for patients with fibromyalgia [22].
Anticonvulsants: Anticonvulsants used for treating fibromyalgia include pregabalin, mirogabalin, and lacosamide.
Pregabalin: Pregabalin, an anticonvulsant drug, has received FDA approval for the treatment of fibromyalgia. It has demonstrated effectiveness in reducing pain, sleep disturbances, and anxiety associated with this condition. In a clinical trial, pregabalin exhibited a significant decrease in pain scores when compared to a placebo [23]. A dosage of 450 mg/day of pregabalin proved to be effective in treating fibromyalgia, resulting in the reduction of pain, improved sleep patterns, and reduced fatigue compared to the placebo group [24]. The most commonly reported adverse events related to pregabalin were dizziness and somnolence, with their occurrence typically dependent on the dosage administered [16]. Furthermore, pregabalin has been shown to enhance function and improve the quality of life for patients with fibromyalgia [25].
Mirogabalin: Mirogabalin, a novel gabapentinoid, has been under investigation for its potential as a treatment for fibromyalgia. A study conducted in 2019 utilized a randomized, double-blind, placebo-controlled design to assess the effects of mirogabalin on pain, fatigue, and sleep in fibromyalgia patients [26]. The results indicated that mirogabalin was effective in reducing pain and improving sleep quality. However, it is important to note that mirogabalin is primarily associated with the central nervous system (CNS) side effects, with somnolence, dizziness, and headache being the most commonly reported [27]. These side effects appear to increase in incidence with higher doses of mirogabalin, although their severity remains relatively constant. Other reported side effects include constipation, nausea, diarrhea, edema, weight gain, and fatigue.
Lacosamide: Lacosamide, an anticonvulsant medication, has demonstrated analgesic effects in animal models. In a randomized, double-blind, placebo-controlled trial conducted in 2012, the effects of lacosamide on pain and sleep in fibromyalgia patients were evaluated and concluded that lacosamide was more effective than a placebo in reducing pain and improving sleep quality, with a statistically significant reduction in pain scores [28]. Adverse effects of lacosamide include dizziness, vertigo, ataxia, balance disorder, diplopia, fatigue, nausea, vomiting, and tremor. It is important to note that these adverse effects are dose-dependent [29]. However, further studies are needed to explore the potential of lacosamide for fibromyalgia treatment.
Cannabinoids: Cannabidiol (CBD) and tetrahydrocannabinol (THC) have garnered attention in the medical community as potential treatments for fibromyalgia. These compounds interact with the endocannabinoid system, which regulates pain, mood, and sleep [30]. Habib et al. investigated the effects of a THC/CBD spray on pain and sleep in fibromyalgia patients. The study demonstrated that the THC/CBD spray was more effective than a placebo in reducing pain and improving sleep quality, with a significant decrease in pain scores [31]. Sagy et al. assessed the effects of a CBD-rich cannabis extract on pain, anxiety, and depression in individuals with fibromyalgia. The findings revealed that the CBD-rich cannabis extract effectively reduced pain, anxiety, and depression, with a significant reduction in pain scores [32].
However, it is important to consider potential side effects associated with cannabinoids, such as dizziness, dry mouth, and cognitive impairment. Therefore, close monitoring by a healthcare provider is necessary to identify any potential side effects and determine the appropriate dosage and frequency of cannabinoid therapy [33]. While cannabinoids may offer a cost-effective and well-tolerated option for alleviating symptoms and improving the quality of life in fibromyalgia patients [34,35], further research is required to fully understand their long-term safety and effectiveness. Moreover, it should be noted that the use of cannabinoids for fibromyalgia is not legal in all jurisdictions, and patients should consult with a healthcare provider to ascertain the legal status and evaluate the potential risks and benefits of cannabinoid therapy for fibromyalgia [36].
Tropisetron: Tropisetron, which is a 5-HT3 receptor antagonist, has been investigated as a potential treatment for fibromyalgia [37]. Stratz et al. demonstrated that tropisetron was more effective than a placebo in reducing pain and fatigue, and also in improving sleep quality [38]. Furthermore, another study showed a statistically significant reduction in pain scores with tropisetron treatment [39]. Moreover, Arnold found that administering a daily dose of 2 mg of tropisetron for five days provided pain relief that lasted for two weeks to two months [40].
Sodium oxybate: Sodium oxybate, a central nervous system depressant, has been investigated as a potential treatment for fibromyalgia [41]. In a randomized, double-blind, placebo-controlled trial conducted in 2011, the effects of sodium oxybate on pain, sleep, and fatigue in fibromyalgia patients were evaluated [42]. Spaeth et al. found that sodium oxybate was effective in reducing pain, fatigue, and sleep disturbance [43]. Common side effects reported included nausea, dizziness, vomiting, and anxiety [44]. However, further long-term studies are needed to better understand the safety and effectiveness of sodium oxybate as a treatment option for fibromyalgia.
Non-pharmacological Treatments
Non-pharmacological treatments include the following.
Mind-body interventions: Mind-body interventions, such as mindfulness-based stress reduction (MBSR), have demonstrated efficacy in improving symptoms of fibromyalgia by targeting stress, anxiety, and depression [45]. A recent study published in 2022 investigated the effectiveness of MBSR in fibromyalgia patients and reported positive outcomes, including reductions in pain and fatigue, as well as improvements in quality of life [46]. Similarly, a study published in 2012 examined the effectiveness of CBT in fibromyalgia patients and found that it effectively reduced pain, anxiety, and depression, while enhancing physical function [47]. However, further research is necessary to explore the long-term sustainability of these intervention outcomes.
Exercise therapy: Exercise therapy, such as aerobic exercise and resistance training, has been shown to improve symptoms of fibromyalgia by reducing pain and fatigue and improving physical function [48]. A recent study published in 2022 evaluated the effectiveness of a combined aerobic and resistance training program on fibromyalgia (FM) patients and found that it was effective in reducing pain and fatigue and improving quality of life [49]. Exercise is an important component of fibromyalgia treatment, as it can help to improve pain, sleep, and overall quality of life [50]. Low-impact aerobic exercises, such as walking, swimming, and cycling, are effective in managing fibromyalgia symptoms [51]. Strength training and stretching exercises can also be beneficial in improving muscle strength and flexibility [52].
Acupuncture: Acupuncture is a traditional Chinese medicine technique that involves the insertion of thin needles into specific points of the body [53]. Few studies reported the effectiveness of acupuncture on FM patients and found that it was effective in reducing pain and improving quality of life [54-56]. However, further research is needed to determine the optimal acupuncture points and duration of treatment for FM management.
Transcutaneous electrical nerve stimulation (TENS): TENS is a non-invasive technique that uses electrical impulses to modulate pain signals in the nerves [57]. In 2015, Noehren et al. evaluated the effectiveness of TENS on FM patients and found that it was effective in reducing pain and fatigue and improving physical function [58].
Low-level laser therapy (LLLT): LLLT is a non-invasive technique that uses low-level laser light to modulate cellular function and reduce inflammation [59]. de Carvalho et al. evaluated the effectiveness of LLLT on FM patients and found that it was effective in reducing pain and fatigue and improving quality of life [60].
Hydrotherapy: Hydrotherapy involves the use of water for therapeutic purposes, such as warm water immersion or aquatic exercise [61]. A recent study published in 2006 evaluated the effectiveness of hydrotherapy on FM patients and found that it was effective in reducing pain and fatigue and improving physical function [62].
Yoga therapy: Yoga therapy involves the practice of physical postures, breathing techniques, and meditation to improve physical and mental health. A recent study published in 2010 evaluated the effectiveness of yoga therapy on FM patients and found that it was effective in reducing pain, anxiety, and depression, and improving physical function [63].
Music therapy: Music therapy involves the use of music for therapeutic purposes, such as relaxation and pain management [64]. Few studies evaluated the effectiveness of music therapy on FM patients and found that it was effective in reducing pain, anxiety, and depression [65,66]. Further research is needed to fully understand its benefits.
Mindfulness-based art therapy (MBAT): MBAT involves the use of art-making and mindfulness-based practices to improve physical and mental health [46]. It involves the use of creative expression to promote healing and improve mental health. A recent study published in 2014 evaluated the effectiveness of MBAT on FM patients and found that it was effective in reducing pain, anxiety, and depression, and improving quality of life [67].
Tai chi: Tai chi is a Chinese martial art that involves slow, controlled movements and meditation [68]. Wang et al. evaluated the effectiveness of tai chi on FM patients and found that it was effective in reducing pain and fatigue and improving physical function [69].
Virtual reality distraction therapy (VRDT): VRDT involves the use of virtual reality technology to distract patients from pain and provide a relaxing experience and is effective in reducing pain and improving quality of life [70]. VRDT is effective in reducing the impact of FMS, pain, fatigue, anxiety, and depression and increases dynamic balance, aerobic capacity, and quality of life [71].
Cognitive behavioral therapy (CBT): CBT is a type of talk therapy that focuses on changing negative thoughts and behaviors to improve mental health [72]. It involves teaching patients coping skills and relaxation techniques, as well as helping them to identify and challenge negative thoughts that may be contributing to their symptoms [73]. Prados et al. evaluated the effectiveness of CBT on FM patients and found that it was effective in reducing pain, anxiety, and depression, and improving quality of life [74].
Mindfulness-based stress reduction (MBSR): MBSR involves the practice of mindfulness meditation and yoga to reduce stress and improve mental and physical health [75]. Perez-Aranda et al. evaluated the effectiveness of MBSR on FM patients and found that it was effective in reducing pain and fatigue and improving quality of life [76].
Graded exercise therapy (GET): GET involves gradually increasing physical activity levels to improve physical function and reduce pain and it was effective in improving physical function but may cause increased pain in some patients [77]. GET is a structured exercise program that gradually increases physical activity levels over time [78]. It is effective in improving symptoms and quality of life in people with fibromyalgia [79].
Occupational therapy: Occupational therapy can help individuals with fibromyalgia to manage their symptoms and maintain their daily activities. Occupational therapists can work with patients to develop strategies for conserving energy, improving work or home environments, and adapting activities to reduce pain and fatigue [80].
Massage therapy: Massage therapy involves the manipulation of soft tissues in the body, which is effective in reducing pain, stiffness, and fatigue in people with fibromyalgia [81,82].
Dietary supplements: Some dietary supplements such as magnesium, soy supplements, and creatine have been studied for their potential benefits in managing fibromyalgia symptoms [83-85].
Implications for practice
Consider prescribing medications such as duloxetine, pregabalin, and milnacipran to people with fibromyalgia who are experiencing pain. Consider exercise therapy, such as aerobic and resistance training, as part of the treatment plan. CBT can be effective in reducing pain, improving the quality of life, and decreasing depression and anxiety. Mind-body therapies, such as yoga and tai chi, can be effective in reducing pain and improving physical function. Provide patients education about fibromyalgia and its management to improve patient outcomes. Use a multi-modal approach to fibromyalgia treatment that combines different treatments for optimal outcomes. Tailor treatment plans to individual patient needs for optimal outcomes [83-85]. Involve patients in the treatment decision-making process to improve treatment outcomes. Early intervention and regular monitoring of symptoms and treatment outcomes are important for optimal outcomes.
Strengths of the study
Inclusion Criteria
The review had clear inclusion criteria, which helped to ensure that the studies included in the review were relevant to the research question.
Clinical Implications
The review provided important information on the effectiveness and safety of different fibromyalgia treatments, which can inform clinical practice and improve patient outcomes.
Transparency
The review provided detailed information on the methods used to select and analyze studies, which increased the transparency and reliability of the findings.
Comprehensive Search Strategy
The review included a thorough search of multiple electronic databases, including PubMed, Embase, and Cochrane Library, as well as a manual search of reference lists, which increases the likelihood of capturing all relevant studies.
Critical Appraisal
The quality of the studies included in the review was assessed using the Cochrane risk of bias tool and the GRADE approach, which provides a rigorous evaluation of the strength of the evidence.
Generalizability
The review included studies from different countries and settings, which increases the generalizability of the findings to different populations.
Use of PRISMA and PROSPERO
The review was conducted using the PRISMA guidelines, which provide a standardized method for reporting systematic reviews. Additionally, the review was registered with PROSPERO, which increases the transparency and rigor of the review process.
Limitations of the study
Language Bias
The review only included studies that were published in English, which may have excluded relevant studies that were published in other languages.
Outcome Measures
The studies included in the review used different outcome measures, which may limit the ability to compare the effectiveness of different treatments.
Small Sample Sizes
Some of the studies included in the review had small sample sizes, which may limit the generalizability of the findings to larger populations.
Publication Bias
The review may be subject to publication bias, as only studies that were published in English and peer-reviewed journals were included, which may have excluded relevant studies that were not published or were published in other languages.
Heterogeneity
The studies included in the review varied in terms of study design, sample size, and intervention type, which may limit the ability to draw firm conclusions.
Future research directives
Given the demonstrated analgesic effects of tianeptine in animal models, future research could investigate the potential of tianeptine as a treatment option for fibromyalgia patients [86]. Pramipexole, a dopamine agonist previously studied for fibromyalgia, could be further investigated in clinical trials as a potential treatment option for fibromyalgia patients, particularly in terms of its effects on pain, fatigue, and sleep [87].
Agomelatine, a melatonin receptor agonist and serotonin receptor antagonist, may hold promise as a therapeutic agent for fibromyalgia, particularly in improving sleep quality and reducing pain and fatigue. Future research could explore the efficacy and safety of agomelatine in fibromyalgia patients [88].
Sleep hygiene interventions, such as cognitive behavioral therapy for insomnia (CBT-I) and sleep hygiene education, have shown promise in improving sleep quality and reducing fibromyalgia symptoms [89,90]. Future research could investigate the effectiveness of these interventions in larger and more diverse populations, and explore their potential long-term benefits.
Biofeedback therapy has shown potential in reducing pain and improving physical function in fibromyalgia patients [91,92]. Future research could investigate the optimal parameters of biofeedback therapy, such as the type and duration of treatment, and the patient characteristics that may influence its effectiveness.
Balneotherapy, a form of hydrotherapy that involves immersion in mineral-rich water, has been studied for its potential benefits in fibromyalgia patients [93]. Future research could further explore the effects of balneotherapy on fibromyalgia symptoms and identify the optimal treatment protocols.
Transcranial magnetic stimulation (TMS) has shown promise in reducing pain and improving physical function in fibromyalgia patients [94-96]. Future research could investigate the optimal parameters of TMS, such as the frequency, intensity, and duration of treatment, and explore the potential mechanisms underlying its effects.
Conclusions
Fibromyalgia, a chronic pain disorder, affects millions worldwide, with a complex etiology involving genetic, environmental, and psychological factors. Diagnosis relies on symptom assessment and the exclusion of other conditions. Despite its impact on quality of life, appropriate management with a multidisciplinary approach enables individuals with fibromyalgia to lead fulfilling lives. Hence, staying up to date with the latest treatment strategies is crucial in effectively managing fibromyalgia and providing optimal care to patients.
The authors have declared that no competing interests exist.
References
- 1.Bhargava J, Hurley JA. Treasure Island, FL: StatPearls Publishing; 2023. Fibromyalgia. [Google Scholar]
- 2.Branch NSC and O: Fibromyalgia. Fibromyalgia. [ Jun; 2023 ]. 2023. https://www.niams.nih.gov/health-topics/fibromyalgia https://www.niams.nih.gov/health-topics/fibromyalgia
- 3.Treatment of fibromyalgia. Kwiatek R. Aust Prescr. 2017;40:179–183. doi: 10.18773/austprescr.2017.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.EULAR revised recommendations for the management of fibromyalgia. Macfarlane GJ, Kronisch C, Dean LE, et al. Ann Rheum Dis. 2017;76:318–328. doi: 10.1136/annrheumdis-2016-209724. [DOI] [PubMed] [Google Scholar]
- 5.Pharmacological management of fibromyalgia: a Bayesian network meta-analysis. Migliorini F, Maffulli N, Eschweiler J, Knobe M, Tingart M, Colarossi G. Expert Rev Clin Pharmacol. 2022;15:205–214. doi: 10.1080/17512433.2022.2044792. [DOI] [PubMed] [Google Scholar]
- 6.Progress towards improved non-pharmacological management of fibromyalgia. Pinto AM, Geenen R, Castilho P, da Silva JA. Joint Bone Spine. 2020;87:377–379. doi: 10.1016/j.jbspin.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Systematic review of randomized controlled trials of nonpharmacological interventions for fibromyalgia. Sim J, Adams N. Clin J Pain. 2002;18:324–336. doi: 10.1097/00002508-200209000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Effects of lifestyle physical activity in adults with fibromyalgia: results at follow-up. Fontaine KR, Conn L, Clauw DJ. J Clin Rheumatol. 2011;17:64–68. doi: 10.1097/RHU.0b013e31820e7ea7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lifestyle-oriented non-pharmacological treatments for fibromyalgia: a clinical overview and applications with home-based technologies. Friedberg F, Williams DA, Collinge W. J Pain Res. 2012;5:425–435. doi: 10.2147/JPR.S35199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.International, multidisciplinary Delphi consensus recommendations on non-pharmacological interventions for fibromyalgia. Kundakci B, Hall M, Atzeni F, et al. Semin Arthritis Rheum. 2022;57:152101. doi: 10.1016/j.semarthrit.2022.152101. [DOI] [PubMed] [Google Scholar]
- 11.Evidence-based non-pharmacological therapies for fibromyalgia. Aman MM, Jason Yong R, Kaye AD, Urman RD. Curr Pain Headache Rep. 2018;22:33. doi: 10.1007/s11916-018-0688-2. [DOI] [PubMed] [Google Scholar]
- 12.Patients' perspective of the effectiveness and acceptability of pharmacological and non-pharmacological treatments of fibromyalgia. Taylor SJ, Steer M, Ashe SC, Furness PJ, Haywood-Small S, Lawson K. Scand J Pain. 2019;19:167–181. doi: 10.1515/sjpain-2018-0116. [DOI] [PubMed] [Google Scholar]
- 13.Management of fibromyalgia syndrome in 2016. Okifuji A, Gao J, Bokat C, Hare BD. Pain Manag. 2016;6:383–400. doi: 10.2217/pmt-2016-0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pharmacological treatment options for fibromyalgia. Northcott MJ, Guymer EK, Littlejohn GO. Clin Pharm. 2017;9 [Google Scholar]
- 15.Fibromyalgia: presentation and management with a focus on pharmacological treatment. Sumpton JE, Moulin DE. Pain Res Manag. 2008;13:477–483. doi: 10.1155/2008/959036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. Arnold LM, Russell IJ, Diri EW, et al. J Pain. 2008;9:792–805. doi: 10.1016/j.jpain.2008.03.013. [DOI] [PubMed] [Google Scholar]
- 17.Milnacipran for the treatment of fibromyalgia in adults: a 15-week, multicenter, randomized, double-blind, placebo-controlled, multiple-dose clinical trial. Clauw DJ, Mease P, Palmer RH, Gendreau RM, Wang Y. Clin Ther. 2008;30:1988–2004. doi: 10.1016/j.clinthera.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 18.The efficacy and safety of milnacipran for treatment of fibromyalgia. a randomized, double-blind, placebo-controlled trial. Mease PJ, Clauw DJ, Gendreau RM, Rao SG, Kranzler J, Chen W, Palmer RH. J Rheumatol. 2009;36:398–409. doi: 10.3899/jrheum.080734. [DOI] [PubMed] [Google Scholar]
- 19.A randomized, double-blind, placebo-controlled trial of duloxetine in the treatment of women with fibromyalgia with or without major depressive disorder. Arnold LM, Rosen A, Pritchett YL, D'Souza DN, Goldstein DJ, Iyengar S, Wernicke JF. Pain. 2005;119:5–15. doi: 10.1016/j.pain.2005.06.031. [DOI] [PubMed] [Google Scholar]
- 20.Flexible dosed duloxetine in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled trial. Arnold LM, Clauw D, Wang F, Ahl J, Gaynor PJ, Wohlreich MM. J Rheumatol. 2010;37:2578–2586. doi: 10.3899/jrheum.100365. [DOI] [PubMed] [Google Scholar]
- 21.A randomized, double-blind, placebo-controlled phase III trial of duloxetine in Japanese fibromyalgia patients. Murakami M, Osada K, Mizuno H, Ochiai T, Alev L, Nishioka K. Arthritis Res Ther. 2015;17:224. doi: 10.1186/s13075-015-0718-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Efficacy of duloxetine in patients with fibromyalgia: pooled analysis of 4 placebo-controlled clinical trials. Arnold LM, Clauw DJ, Wohlreich MM, Wang F, Ahl J, Gaynor PJ, Chappell AS. Prim Care Companion J Clin Psychiatry. 2009;11:237–244. doi: 10.4088/PCC.08m00680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.A randomized, double-blind, multicenter, placebo-controlled phase III trial to evaluate the efficacy and safety of pregabalin in Japanese patients with fibromyalgia. Ohta H, Oka H, Usui C, Ohkura M, Suzuki M, Nishioka K. Arthritis Res Ther. 2012;14:0. doi: 10.1186/ar4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pregabalin for the treatment of fibromyalgia syndrome: results of a randomized, double-blind, placebo-controlled trial. Crofford LJ, Rowbotham MC, Mease PJ, et al. Arthritis Rheum. 2005;52:1264–1273. doi: 10.1002/art.20983. [DOI] [PubMed] [Google Scholar]
- 25.Pregabalin for pain in fibromyalgia in adults. Derry S, Cording M, Wiffen PJ, Law S, Phillips T, Moore RA. Cochrane Database Syst Rev. 2016;9:0. doi: 10.1002/14651858.CD011790.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Efficacy and safety of mirogabalin for the treatment of fibromyalgia: results from three 13-week randomized, double-blind, placebo- and active-controlled, parallel-group studies and a 52-week open-label extension study. Arnold LM, Whitaker S, Hsu C, Jacobs D, Merante D. Curr Med Res Opin. 2019;35:1825–1835. doi: 10.1080/03007995.2019.1629757. [DOI] [PubMed] [Google Scholar]
- 27.Mirogabalin as a novel gabapentinoid for the treatment of chronic pain conditions: an analysis of current evidence. Chen EY, Beutler SS, Kaye AD, et al. Anesth Pain Med. 2021;11:0. doi: 10.5812/aapm.121402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lacosamide for neuropathic pain and fibromyalgia in adults. Hearn L, Derry S, Moore RA. Cochrane Database Syst Rev. 2012;2012:0. doi: 10.1002/14651858.CD009318.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The adverse event profile of lacosamide: a systematic review and meta-analysis of randomized controlled trials. Zaccara G, Perucca P, Loiacono G, Giovannelli F, Verrotti A. Epilepsia. 2013;54:66–74. doi: 10.1111/j.1528-1167.2012.03589.x. [DOI] [PubMed] [Google Scholar]
- 30.A systematic review of fibromyalgia and recent advancements in treatment: is medicinal cannabis a new hope? Khurshid H, Qureshi IA, Jahan N, Went TR, Sultan W, Sapkota A, Alfonso M. Cureus. 2021;13:0. doi: 10.7759/cureus.17332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Medical cannabis for the treatment of fibromyalgia. Habib G, Artul S. J Clin Rheumatol. 2018;24:255–258. doi: 10.1097/RHU.0000000000000702. [DOI] [PubMed] [Google Scholar]
- 32.Safety and efficacy of medical cannabis in fibromyalgia. Sagy I, Bar-Lev Schleider L, Abu-Shakra M, Novack V. J Clin Med. 2019;8:807. doi: 10.3390/jcm8060807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cannabinoids for fibromyalgia. Walitt B, Klose P, Fitzcharles MA, Phillips T, Häuser W. Cochrane Database Syst Rev. 2016;7:0. doi: 10.1002/14651858.CD011694.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cannabinoids and the endocannabinoid system in fibromyalgia: a review of preclinical and clinical research. Bourke SL, Schlag AK, O'Sullivan SE, Nutt DJ, Finn DP. Pharmacol Ther. 2022;240:108216. doi: 10.1016/j.pharmthera.2022.108216. [DOI] [PubMed] [Google Scholar]
- 35.Ingestion of a THC-rich cannabis oil in people with fibromyalgia: a randomized, double-blind, placebo-controlled clinical trial. Chaves C, Bittencourt PC, Pelegrini A. Pain Med. 2020;21:2212–2218. doi: 10.1093/pm/pnaa303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Consensus recommendations on dosing and administration of medical cannabis to treat chronic pain: results of a modified Delphi process. Bhaskar A, Bell A, Boivin M, et al. J Cannabis Res. 2021;3:22. doi: 10.1186/s42238-021-00073-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oral treatment of fibromyalgia with tropisetron given over 28 days: influence on functional and vegetative symptoms, psychometric parameters and pain. Haus U, Varga B, Stratz T, Späth M, Müller W. Scand J Rheumatol Suppl. 2000;113:55–58. doi: 10.1080/030097400446652. [DOI] [PubMed] [Google Scholar]
- 38.Fibromyalgia treatment with intravenous tropisetron administration. Stratz T, Färber L, Varga B, Baumgartner C, Haus U, Müller W. https://pubmed.ncbi.nlm.nih.gov/11447769/ Drugs Exp Clin Res. 2001;27:113–118. [PubMed] [Google Scholar]
- 39.Efficacy and tolerability of intravenous tropisetron in the treatment of fibromyalgia. Späth M, Stratz T, Neeck G, et al. Scand J Rheumatol. 2004;33:267–270. doi: 10.1080/03009740410005818. [DOI] [PubMed] [Google Scholar]
- 40.Biology and therapy of fibromyalgia. New therapies in fibromyalgia. Arnold LM. Arthritis Res Ther. 2006;8:212. doi: 10.1186/ar1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sodium oxybate for the treatment of fibromyalgia. Staud R. Expert Opin Pharmacother. 2011;12:1789–1798. doi: 10.1517/14656566.2011.589836. [DOI] [PubMed] [Google Scholar]
- 42.Sodium oxybate reduces pain, fatigue, and sleep disturbance and improves functionality in fibromyalgia: results from a 14-week, randomized, double-blind, placebo-controlled study. Russell JI, Holman AJ, Swick TJ, Alvarez-Horine S, Wang GY, Guinta D. Pain. 2011;152:1007–1017. doi: 10.1016/j.pain.2010.12.022. [DOI] [PubMed] [Google Scholar]
- 43.Sodium oxybate therapy provides multidimensional improvement in fibromyalgia: results of an international phase 3 trial. Spaeth M, Bennett RM, Benson BA, Wang YG, Lai C, Choy EH. Ann Rheum Dis. 2012;71:935–942. doi: 10.1136/annrheumdis-2011-200418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Long-term tolerability and maintenance of therapeutic response to sodium oxybate in an open-label extension study in patients with fibromyalgia. Spaeth M, Alegre C, Perrot S, Wang Y, Guinta DR, Alvarez-Horine S, Russell I. Arthritis Res Ther. 2013;15:0. doi: 10.1186/ar4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Mind and body therapy for fibromyalgia. Theadom A, Cropley M, Smith HE, Feigin VL, McPherson K. Cochrane Database Syst Rev. 2015;2015:0. doi: 10.1002/14651858.CD001980.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Research in mindfulness interventions for patients with fibromyalgia: a critical review. Leça S, Tavares I. Front Integr Neurosci. 2022;16:920271. doi: 10.3389/fnint.2022.920271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.A mind-body technique for symptoms related to fibromyalgia and chronic fatigue. Toussaint LL, Whipple MO, Abboud LL, Vincent A, Wahner-Roedler DL. Explore (NY) 2012;8:92–98. doi: 10.1016/j.explore.2011.12.003. [DOI] [PubMed] [Google Scholar]
- 48.Aerobic exercise training for adults with fibromyalgia. Bidonde J, Busch AJ, Schachter CL, et al. Cochrane Database Syst Rev. 2017;6:0. doi: 10.1002/14651858.CD012700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.On the superiority of a combination of aerobic and resistance exercise for fibromyalgia syndrome: a network meta-analysis. Chen J, Han B, Wu C. Front Psychol. 2022;13:949256. doi: 10.3389/fpsyg.2022.949256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Häuser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, Busch A. Arthritis Res Ther. 2010;12:0. doi: 10.1186/ar3002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Effects of short versus long bouts of aerobic exercise in sedentary women with fibromyalgia: a randomized controlled trial. Schachter CL, Busch AJ, Peloso PM, Sheppard MS. Phys Ther. 2003;83:340–358. [PubMed] [Google Scholar]
- 52.Effects of strength training in fibromyalgia on balance, neuromuscular performance, and symptomatic analysis: a 12-week study protocol. Albuquerque ML, Monteiro D, Alvarez MC, Vilarino GT, Andrade A, Neiva HP. Front Neurol. 2023;14:1149268. doi: 10.3389/fneur.2023.1149268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Improvement in fibromyalgia symptoms with acupuncture: results of a randomized controlled trial. Martin DP, Sletten CD, Williams BA, Berger IH. Mayo Clin Proc. 2006;81:749–757. doi: 10.4065/81.6.749. [DOI] [PubMed] [Google Scholar]
- 54.Acupuncture therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. Zhang XC, Chen H, Xu WT, Song YY, Gu YH, Ni GX. J Pain Res. 2019;12:527–542. doi: 10.2147/JPR.S186227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Acupuncture for fibromyalgia in primary care: a randomised controlled trial. Vas J, Santos-Rey K, Navarro-Pablo R, et al. Acupunct Med. 2016;34:257–266. doi: 10.1136/acupmed-2015-010950. [DOI] [PubMed] [Google Scholar]
- 56.Acupuncture for primary fibromyalgia: study protocol of a randomized controlled trial. Han M, Cui J, Xiao Y, et al. Trials. 2020;21:538. doi: 10.1186/s13063-020-04317-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Transcutaneous electrical nerve stimulation (TENS) for fibromyalgia in adults. Johnson MI, Claydon LS, Herbison GP, Jones G, Paley CA. Cochrane Database Syst Rev. 2017;10:0. doi: 10.1002/14651858.CD012172.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Effect of transcutaneous electrical nerve stimulation on pain, function, and quality of life in fibromyalgia: a double-blind randomized clinical trial. Noehren B, Dailey DL, Rakel BA, Vance CG, Zimmerman MB, Crofford LJ, Sluka KA. Phys Ther. 2015;95:129–140. doi: 10.2522/ptj.20140218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Low-level laser therapy combined to functional exercise on treatment of fibromyalgia: a double-blind randomized clinical trial. Germano Maciel D, Trajano da Silva M, Rodrigues JA, et al. Lasers Med Sci. 2018;33:1949–1959. doi: 10.1007/s10103-018-2561-2. [DOI] [PubMed] [Google Scholar]
- 60.Effect of low-level laser therapy on pain, quality of life and sleep in patients with fibromyalgia: study protocol for a double-blinded randomized controlled trial. de Carvalho Pde T, Leal-Junior EC, Alves AC, et al. Trials. 2012;13:221. doi: 10.1186/1745-6215-13-221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Effectiveness of aquatic therapy in the treatment of fibromyalgia syndrome: a randomized controlled open study. Evcik D, Yigit I, Pusak H, Kavuncu V. Rheumatol Int. 2008;28:885–890. doi: 10.1007/s00296-008-0538-3. [DOI] [PubMed] [Google Scholar]
- 62.Hydrotherapy and conventional physiotherapy improve total sleep time and quality of life of fibromyalgia patients: randomized clinical trial. Vitorino DF, Carvalho LB, Prado GF. Sleep Med. 2006;7:293–296. doi: 10.1016/j.sleep.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 63.A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. Pain. 2010;151:530–539. doi: 10.1016/j.pain.2010.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fibromyalgia tender point pain: a double-blind, placebo-controlled pilot study of music vibration using the music vibration table. Chesky KS, Russell IJ, Lopez Y, Kondraske GV. J Musculoskelet Pain. 1997;5:33–52. [Google Scholar]
- 65.Music-based interventions to improve fibromyalgia syndrome: a meta-analysis. Wang M, Yi G, Gao H, Wu B, Zhou Y. Explore (NY) 2020;16:357–362. doi: 10.1016/j.explore.2020.05.012. [DOI] [PubMed] [Google Scholar]
- 66.Music as a sleep aid in fibromyalgia. Picard LM, Bartel LR, Gordon AS, Cepo D, Wu Q, Pink LR. Pain Res Manag. 2014;19:97–101. doi: 10.1155/2014/272108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.THU0341 assessment of art therapy program for women with fibromyalgia: randomized, controlled, blinded study. Baptista AS, Jones A, Cardoso FP, Schaffir B, Coelho ERW, Orlandi A, Natour J. Ann Rheum Dis. 2013;71:271. [Google Scholar]
- 68.A randomized trial of tai chi for fibromyalgia. Wang C, Schmid CH, Rones R, et al. N Engl J Med. 2010;363:743–754. doi: 10.1056/NEJMoa0912611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. Wang C, Schmid CH, Fielding RA, et al. BMJ. 2018;360:0. doi: 10.1136/bmj.k851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Using virtual reality exposure therapy in pain management: a systematic review and meta-analysis of randomized controlled trials. Huang Q, Lin J, Han R, Peng C, Huang A. Value Health. 2022;25:288–301. doi: 10.1016/j.jval.2021.04.1285. [DOI] [PubMed] [Google Scholar]
- 71.Virtual reality-based therapy reduces the disabling impact of fibromyalgia syndrome in women: systematic review with meta-analysis of randomized controlled trials. Cortés-Pérez I, Zagalaz-Anula N, Ibancos-Losada MD, Nieto-Escámez FA, Obrero-Gaitán E, Osuna-Pérez MC. J Pers Med. 2021;11:1167. doi: 10.3390/jpm11111167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Cognitive behavioural therapies for fibromyalgia. Bernardy K, Klose P, Busch AJ, Choy EH, Häuser W. Cochrane Database Syst Rev. 2013;2013:0. doi: 10.1002/14651858.CD009796.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Attention modification in persons with fibromyalgia: a double blind, randomized clinical trial. Carleton RN, Richter AA, Asmundson GJ. Cogn Behav Ther. 2011;40:279–290. doi: 10.1080/16506073.2011.616218. [DOI] [PubMed] [Google Scholar]
- 74.Combined cognitive-behavioral therapy for fibromyalgia: effects on polysomnographic parameters and perceived sleep quality. Prados G, Miró E, Martínez MP, Sánchez AI, Lami MJ, Cáliz R. Int J Clin Health Psychol. 2020;20:232–242. doi: 10.1016/j.ijchp.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Pain. 2011;152:361–369. doi: 10.1016/j.pain.2010.10.043. [DOI] [PubMed] [Google Scholar]
- 76.A randomized controlled efficacy trial of mindfulness-based stress reduction compared with an active control group and usual care for fibromyalgia: the EUDAIMON study. Pérez-Aranda A, Feliu-Soler A, Montero-Marín J, et al. Pain. 2019;160:2508–2523. doi: 10.1097/j.pain.0000000000001655. [DOI] [PubMed] [Google Scholar]
- 77.Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. Richards SC, Scott DL. BMJ. 2002;325:185. doi: 10.1136/bmj.325.7357.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Randomised, double-blind, placebo-controlled treatment trial of fluoxetine and graded exercise for chronic fatigue syndrome. Wearden AJ, Morriss RK, Mullis R, et al. Br J Psychiatry. 1998;172:485–490. doi: 10.1192/bjp.172.6.485. [DOI] [PubMed] [Google Scholar]
- 79.Benefits of physical training in fibromyalgia and related syndromes. Maquet D, Demoulin C, Croisier JL, Crielaard JM. Ann Readapt Med Phys. 2007;50:363–368. doi: 10.1016/j.annrmp.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 80.Effectiveness of occupational therapy interventions for adults with fibromyalgia: a systematic review. Poole JL, Siegel P. Am J Occup Ther. 2017;71 doi: 10.5014/ajot.2017.023192. [DOI] [PubMed] [Google Scholar]
- 81.Massage therapy for fibromyalgia: a systematic review and meta-analysis of randomized controlled trials. Li YH, Wang FY, Feng CQ, Yang XF, Sun YH. PLoS One. 2014;9:0. doi: 10.1371/journal.pone.0089304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Effectiveness of myofascial release on pain, sleep, and quality of life in patients with fibromyalgia syndrome: a systematic review. Ughreja RA, Venkatesan P, Balebail Gopalakrishna D, Singh YP. Complement Ther Clin Pract. 2021;45:101477. doi: 10.1016/j.ctcp.2021.101477. [DOI] [PubMed] [Google Scholar]
- 83.Short-term magnesium therapy alleviates moderate stress in patients with fibromyalgia: a randomized double-blind clinical trial. Macian N, Dualé C, Voute M, et al. Nutrients. 2022;14:2088. doi: 10.3390/nu14102088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Dietary soy supplement on fibromyalgia symptoms: a randomized, double-blind, placebo-controlled, early phase trial. Wahner-Roedler DL, Thompson JM, Luedtke CA, et al. Evid Based Complement Alternat Med. 2011;2011:350697. doi: 10.1093/ecam/nen069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Creatine supplementation in fibromyalgia: a randomized, double-blind, placebo-controlled trial. Alves CR, Santiago BM, Lima FR, et al. Arthritis Care Res (Hoboken) 2013;65:1449–1459. doi: 10.1002/acr.22020. [DOI] [PubMed] [Google Scholar]
- 86.Effects of tianeptine on symptoms of fibromyalgia via BDNF signaling in a fibromyalgia animal model. Lee H, Im J, Won H, et al. Korean J Physiol Pharmacol. 2017;21:361–370. doi: 10.4196/kjpp.2017.21.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Pramipexole, a dopamine D3/D2 receptor-preferring agonist, attenuates reserpine-induced fibromyalgia-like model in mice. Martins CP, Paes RS, Baldasso GM, et al. Neural Regen Res. 2022;17:450–458. doi: 10.4103/1673-5374.317984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Agomelatine for the treatment of patients with fibromyalgia and depressive symptomatology: an uncontrolled, 12-week, pilot study. Calandre EP, Slim M, Garcia-Leiva JM, Rodriguez-Lopez CM, Torres P, Rico-Villademoros F. Pharmacopsychiatry. 2014;47:67–72. doi: 10.1055/s-0033-1363659. [DOI] [PubMed] [Google Scholar]
- 89.Cognitive behavioral therapy for fibromyalgia. Bennett R, Nelson D. Nat Clin Pract Rheumatol. 2006;2:416–424. doi: 10.1038/ncprheum0245. [DOI] [PubMed] [Google Scholar]
- 90.Role of cognitive behavioral therapy in fibromyalgia: a systematic review. Heller HL, Borges AR, Franco LOA, et al. Open J Rheumatol Autoimmune Dis. 2021;11:169–187. [Google Scholar]
- 91.Efficacy of EMG- and EEG-biofeedback in fibromyalgia syndrome: a meta-analysis and a systematic review of randomized controlled trials. Glombiewski JA, Bernardy K, Häuser W. Evid Based Complement Alternat Med. 2013;2013:962741. doi: 10.1155/2013/962741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gonen T, Amital H. Fibromyalgia Syndrome. Cham, Switzerland: Springer International Publishing; 2021. Neuromodulation and biofeedback in the treatment of fibromyalgia; pp. 73–81. [Google Scholar]
- 93.Balneotherapy for fibromyalgia syndrome: a systematic review and meta-analysis. Cao CF, Ma KL, Li QL, et al. J Clin Med. 2021;10:1493. doi: 10.3390/jcm10071493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Effectiveness of repetitive transcranial magnetic stimulation on fibromyalgia patients responding to a first repetitive transcranial magnetic stimulation induction course after six months of maintenance treatment: a randomized pilot-controlled study. Lacroix A, Vergne-Salle P, Dumont JC, Labrunie A, Balestrat P, Calvet B, Girard M. Neuromodulation. 2022;25:624–632. doi: 10.1016/j.neurom.2021.12.015. [DOI] [PubMed] [Google Scholar]
- 95.Repetitive transcranial magnetic stimulation for patients with fibromyalgia: a systematic review with meta-analysis. Sun P, Fang L, Zhang J, Liu Y, Wang G, Qi R. Pain Med. 2022;23:499–514. doi: 10.1093/pm/pnab276. [DOI] [PubMed] [Google Scholar]
- 96.Repetitive transcranial magnetic stimulation of the prefrontal cortex for fibromyalgia syndrome: a randomised controlled trial with 6-months follow up. Tanwar S, Mattoo B, Kumar U, Bhatia R. Adv Rheumatol. 2020;60:34. doi: 10.1186/s42358-020-00135-7. [DOI] [PubMed] [Google Scholar]