Abstract
Background
Higher social support protects people from developing mental disorders. Limited evidence is available on the mechanism through which social support plays this protective role.
Objective
To investigate the stress-buffering process of social support on depressive symptoms using a novel longitudinal dynamic symptom network approach.
Methods
A total of 4242 adult participants who completed the first two waves (from May to October 2020) of the International Covid Mental Health Survey were included in the study. Cross-lagged panel network modelling was used to estimate a longitudinal network of self-reported social support, loneliness and depressive symptoms. Standardised regression coefficients from regularised cross-lagged regressions were estimated as edge weights of the network.
Findings
The results support a unidirectional protective effect of social support on key depressive symptoms, partly mediated through loneliness: A higher number of close confidants and accessible practical help was associated with decreased anhedonia (weight=−0.033) and negative self-appraisal symptoms (weight=−0.038). Support from others was also negatively associated with loneliness, which in turn associated with decreased depressed mood (weight=0.086) and negative self-appraisal (weight=0.077). We identified a greater number of direct relationships from social support to depressive symptoms among men compared with women. Also, the edge weights from social support to depression were generally stronger in the men’s network.
Conclusions
Reductions in negative self-appraisal might function as a bridge between social support and other depressive symptoms, and, thus, it may have amplified the protective effect of social support. Men appear to benefit more from social support than women.
Clinical implications
Building community-based support networks to deliver practical support, and loneliness reduction components are critical for depression prevention interventions after stressful experiences.
Keywords: depression & mood disorders, adult psychiatry, COVID-19
WHAT IS ALREADY KNOWN ON THIS TOPIC
Multiple theories have been proposed to explain why social support from others is associated with lower mental disorder symptoms after stress. However, few of the theories have been adequately supported by empirical evidence, and previous studies also failed to address the heterogeneity of mental disorder symptoms.
WHAT THIS STUDY ADDS
Guided by the network theory of mental disorders, this empirical study provides strong evidence to the self-esteem theory of social support and insights into the impact of gender on social support and depression.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The study provides a new network perspective to investigate social determinants of depression. The findings on self-appraisal and loneliness suggest that these should be considered as key intervention elements in future depression prevention projects.
Introduction
Depression is a mood disorder associated with poorer health outcomes, reduced overall functioning and quality of life.1 Depressive disorders are the forth leading disease burden among 10–24-year olds, and sixth among 25–49-year olds.2 The role of psychological stress in the development and onset of depressive episodes is well established.3 Theoretical models of depression suggest that stressful life events induce psychological changes, resulting in depressive symptoms.4 This effect is heterogenous and most people do not develop major depressive disorder after stressful events, which suggests there are key psychosocial factors that enhance resilience to stress and prevent the development of depressive symptoms. Numerous epidemiological studies have explored protective factors and social support was a robust protective factor against depression.5
Usually, social support refers to psychosocial resource that is accessible in the context of interpersonal relationships within one’s social network.6 It is multidimensional: structural support refers to the size and type of social network, while functional support is related to the experience or expectancy of obtaining instrumental and emotional support from others. A meta-analysis of observational studies showed that the higher levels of social support people perceived, the less likely they endorsed psychiatric symptoms, including depression.5 Multiple social psychological processes have been proposed to explain the mechanisms through which social support prevents depressive symptoms. According to Thoits, support from significant or similar others work as stress buffers through various processes including emotional sustenance, active coping assistance and social influence.7 Evidence from empirical studies to support these processes are still lacking. Although studies are looking for mediators of the social support-depression association,8 recent psychopathology studies demonstrated that identifying the mediators alone does not precisely capture the stress-buffering process. Depression is a complex syndrome with high symptom heterogeneity: people who scored the same on a depressive symptom scale could have quite different symptom profiles. The relationships between social support and each single symptom could be uneven. Therefore, more nuanced approaches are, therefore, needed to capture associations with specific symptoms and social support processes.9 A network approach provides such opportunities as it (1) enables a test of the relationship between social support and depression on a symptom level; (2) takes the dynamics between different depressive symptoms into account.
The network theory of mental disorders provides a novel perspective to conceptualise mental disorders as a complex dynamic system formed by causal interactions between single symptoms.10 Unlike diagnosis-based or total score-based analyses, the model allows investigation of single symptoms within a disorder network. The symptoms in these networks are treated as nodes that are linked to other symptoms through edges. Nodes that also link to other external constructs (eg, social support or symptoms of another disorder) are considered bridge symptoms. The relationship between mental disorder symptoms and risk/protective psychosocial factors such as social support showed that perceived social support was a key factor that reduced mood disorder symptoms, buttressing the stress buffering role of social support.11
The vast majority of current network studies rely on cross-sectional data and were criticised as they fail to reflect how symptoms influence one another as described in the original network theory, therefore limiting the interpretation of cross-sectional network models.12 To reveal the relationship between depression symptomatology and related psychosocial factors over time, a longitudinal network approach is critically needed. The cross-lagged panel network (CLPN) model that combines the cross-lagged model and network model of mental disorders enables modelling of temporal effects between individual nodes within the network using panel data.13 The CLPN methodology has been applied in a few depression studies.14–16 Although there have recently been emerging longitudinal network studies of cognitive factors and depressive symptoms,17 18 to our knowledge, no similar study has been conducted to investigate the relationship between social support and depressive symptoms. Therefore, we found the CLPN a novel and appropriate tool to answer the research question of the mechanism underlying the protective effect of social support.
Objective
The current study used a longitudinal network model to (1) investigate the mechanism by which social support protects individuals from developing a high severity of depression under a stressful situation. We performed the CLPN analysis on data obtained from the Covid Mental Health Survey (COMET) cohort. According to the network theory, the (de)activation of a highly central symptom will spread through the network and (de)activate a greater number of other symptoms.10 By estimating and comparing the centrality indices of depressive symptoms in the networks, we were able to identify which specific symptoms were playing key roles in the protective effect of social support on depression.
Loneliness was a frequent consequence of the COVID-19 pandemic due to public health interventions that promoted social isolation and has a moderately significant effect on depression.19 Social support also decreased loneliness during the COVID-19 pandemic.20 Therefore, we evaluated (2) whether loneliness bridged the protective effect of social support on depression. This research question can be answered by evaluating the position of loneliness in the combined network, as well as its bridge centrality.
Additionally, gender differences in depression symptomology are notable.21 Previous studies suggested gender differences in the relationship between depression and social support.22 A small social network predicted depression in men but not in women. Given the lack of consensus of the reasons underlying these gender differences, the final aim was (3) to compare the stress buffering function of social support separately for men and women participants through the network approach. By comparing the structures of social support-depression networks (eg, the density and weight of edges) among men and women, we investigated how gender moderates the relationship between social support and depression.
Methods
Study design and data source
The data for this study were from a large international cohort study—the COMET Survey, started in May 2020–during the early world-wide outbreak of COVID-19. More details of the survey are available online (https://osf.io/bgtsf/). In brief, the survey was conducted simultaneously via an online tool (Survalyzer) in 13 countries affected by the pandemic. Sampling was conducted by sharing links to the survey via social media, instant messaging platforms and emails. Only adults (over 18 years old) who consented to participate were eligible. Participation was voluntary and participants were free to skip questions or withdraw from the study at any time. Participants included in the baseline were invited for future study waves via email invitations. Participants who completed the full survey entered a survey lottery as compensation for their participation. The study protocol was approved from relevant ethical review boards from lead centres/institutions involved in the COMET study (see online supplemental material).
bmjment-2023-300802supp001.pdf (570.9KB, pdf)
Baseline data were collected from 8013 participants. Our study focused on the time window between wave 1 (May–July 2020) and wave 2 (September—October 2020), the early stage of pandemic when most people perceive COVID as stressful. For the longitudinal analysis, a subsample of 4500 individuals who completed the follow-up survey was initially included. For the analysis, a listwise deletion procedure was conducted to address missing data among main outcomes, resulting in a final sample of 4242 participants in the analysis.
Measurement
Socio-demographic information of the participants was obtained by a self-report questionnaire.
Depressive symptoms were measured by the Patient Health Questionnaire (PHQ-9) scale.23 PHQ-9 is a nine-item self-report questionnaire measuring The diagnostic and statistical munual of mental disorders (DSM)-defined depression symptoms in the last 2 weeks and is one of the most used scales in large-scale epidemiology studies of depression. It is a four-point Likert scale, and each item was rated from 0 (not at all) to 3 (nearly every day). The scale has been translated and validated in different language versions used in the current survey.
Social support was measured by the Oslo Social Support Scale (OSSS-3), a brief scale to assess social support in large-scale surveys. It contains three items asking questions about the number of close confidants, the sense of concern from others and the accessible practical help from neighbours, covering structural, instrumental and emotional support. Psychometric characters of the OSSS-3 were previously validated.6
One item asking frequency of feeling lonely on a 5-point Likert scale (from Never to Frequently) was used to measure loneliness.
Statistical analysis
All analyses were performed using R (V.4.1.3). Two-tailed t-test was used to compare the demographics, baseline depression and social support between the excluded and the retained participants. The CLPN model was estimated by performing a series of regularised regressions (lasso) to test the cross-lagged effects of each item using the glmnet package.13 For each item of the PHQ, OSSS and loneliness at wave 2, a multivariate regression model with all the items at baseline as predictors was estimated. The standardised regression coefficients (from baseline to follow-up) were used as edge weights to visualise the network using the qgraph package.24 Network layout was created using the Fruchterman-Reingold algorithm: arrows indicate direction of the influence. The colour and thickness of the edges reflect regression coefficient values (ie, edge weight): red indicated negative values and positive values are in blue, thicker edges indicate higher absolute weight values. For the gender comparison, the same procedure was then used to separately create networks for men and women. To visualise changes and network comparisons, the same layout from the first network in whole sample was used for other networks.
Centrality was evaluated using the expected influence (EI), the sum of all absolute values of edge weights of a node.25 Out-EI (all edges coming from the node) and in-EI (all edges pointing to the node) were calculated to show how much influence a node has towards and from all other nodes. To focus on connections between constructs, we also calculated the bridge-EIs, which reflects how strong a node affects nodes in other constructs (bridge out-EI) and is affected by nodes from other constructs (bridge in-EI).26 Autoregressive effects were removed when calculating centrality.
The stability of the network was evaluated following standard guidelines for psychological network analyses,24 using a two-step bootstrapping approach for CLPN developed by Funkhouser et al.27 More details of the bootstrap function are available on https://osf.io/paqj8. Correlation stability (CS) coefficients of centrality indices were also calculated: over 0.25 means acceptable stability and over 0.5 means strong stability. To test replicability, we reran the CLPN with gender, age, education level and marital status as covariates into the regularised regressions.
In addition to evaluating the effect on symptom severity, we also investigated the relationship between presence of support and endorsement of depressive symptoms. Therefore, a sensitivity analysis was performed by estimation of a network after dichotomisation of each item. The same procedure with the primary analysis was used to generate the dichotomised network. For the dichotomised network, regularised logistic regressions were used to estimate the CLPN model.15 For both 4-point and 5-point Likert-scaled items, the first two options were coded as ‘0’ and remaining options were coded as ‘1’. The similarities between the original network and the dichotomised network were evaluated by calculation of correlations of edge weights and centrality indices.27
Findings
Demographics and clinical outcomes of participants
The excluded participants by listwise deletion were significantly older than those retained (DIM=5.3, 95% CI 3.4 to 7.3) but there was no significant difference in baseline PHQ-9 total score (DIM=0.1, 95% CI −0.9 to 1.1), OSSS-3 total score (DIM = −0.2, 95% CI −0.5 to 0.1) or loneliness (DIM<0.1, 95% CI −0.1 to 0.1). Demographic information, overall depressive symptom severity, level of social support and self-reported loneliness at each time point are summarised in table 1. Most participants had high education level and were women. The mean scores for PHQ-9 decreased from wave 1 (M=7.46, SD=6.15) to wave 2 (M=6.69, SD=5.95). Loneliness decreased from wave 1 (M=2.67, SD=1.13) to wave 2 (M=2.61, SD=1.11). There was little change in OSSS-3, from mean score of 9.46 (SD=2.31) at wave 1 to 9.47 at wave 2 (SD=2.30).
Table 1.
Demographic and clinical characteristics of the sample
| Characteristics | Wave 1 (included N=4242) | Wave 1 (excluded N=258) |
| Age (M, SD) | 40.4 (15.5) | 45.8 (17.1) |
| Gender (N, %) | ||
| Man | 856 (20.2%) | 72 (27.9%) |
| Woman | 3339 (78.7%) | 180 (69.8%) |
| Others | 35 (0.8%) | 5 (2.0%) |
| Education level (N, %) | ||
| High school or lower | 876 (20.7%) | 66 (25.6%) |
| University degree | 3362 (79.3%) | 190 (73.6%) |
| Marital status (N, %) | ||
| Single | 1257 (29.6%) | 68 (26.4%) |
| Married or steady relationship | 2660 (62.7%) | 163 (63.2%) |
| Divorced/widowed | 273 (6.4%) | 24 (9.3%) |
| Others | 43 (1.0%) | 1 (0.4%) |
| Wave 1 (included N=4242) | Wave2 (included N=4242) | |
| PHQ-9 Score (N, %) | ||
| < 10 (none to mild depression) | 3003 (70.8%) | 3217 (75.8%) |
| ≥ 10 (moderate and higher depression) | 1239 (29.2%) | 1025 (24.2%) |
| OSSS-3 Score (N, %) | ||
| 3–8 (low support) | 1423 (33.5%) | 1384 (32.6%) |
| 9–11 (moderate support) | 2008 (47.3%) | 2035 (48.0%) |
| 12–14 (strong support) | 811 (19.1%) | 823 (19.4%) |
| Loneliness (N, %) | ||
| Never or rarely | 1846 (43.5%) | 1924 (45.4%) |
| Sometimes | 1521 (35.9%) | 1512 (35.6%) |
| Often or frequently | 875 (20.6%) | 806 (19.0%) |
Longitudinal network of social support, loneliness and depression
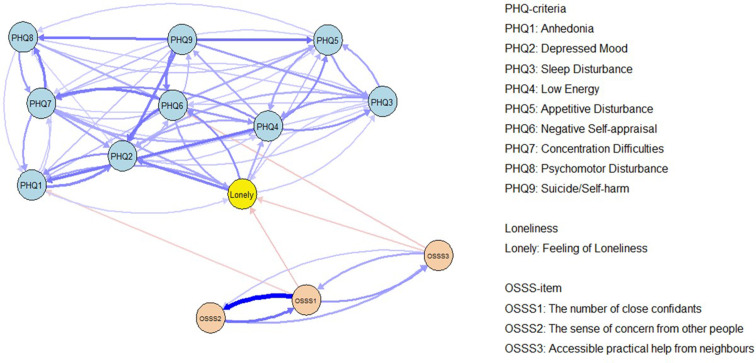
The CLPN plots three constructs, visualising the relationships among depressive symptoms, social support and loneliness (see figure 1). The matrix used to plot the network is shown in online supplemental table 1. Overall, edges within constructs had higher weight than those between constructs. Significant edges appeared between social support and depressive symptoms. Unidirectional pathways from OSSS1 (number of close confidants) to PHQ1 (anhedonia, weight=−0.033) and from OSSS3 (accessible practical help from neighbours) to PHQ6 (negative self-appraisal, weight=−0.038) were identified. In addition, OSSS1 and OSSS3 both showed effects on loneliness (weights=−0.043 and −0.036), which further affected multiple depressive symptoms mainly including PHQ2 (depressed mood, weight=0.086), PHQ6 (negative self appraisal, weight=0.077), PHQ1 (anhedonia, weight=0.064).
Figure 1.
A longitudinal network of social support, loneliness and depressive symptoms (N=4242). Arrows represent longitudinal association between different nodes. Elements for different constructs are in different colours. Nodes with higher connections are automatically clustered together by the Fruchterman-Reingold algorithm. Autoregressive edges and weaker edges with weights lower than 0.03 were excluded to ease visual interpretation as suggested by previous studies. OSSS, Oslo Social Support Scale; PHQ, Patient Health Questionnaire.
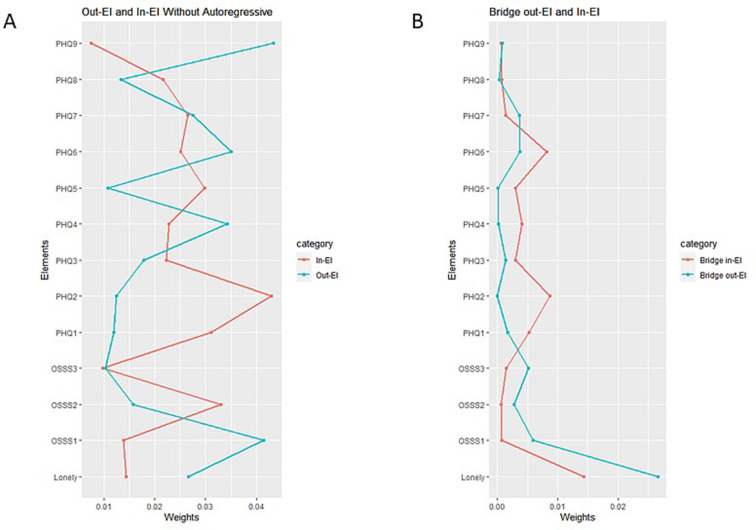
Centrality estimates of the nodes are plotted in figure 2. As edges within constructs were denser and higher weighted than those between constructs, the out-EI and in-EI mainly reflect centrality within constructs. PHQ9 (suicide/self-harm, 0.043), PHQ6 (negative self-appraisal, 0.035) and PHQ4 (low energy, 0.034) had relatively high out-EI compared with other symptoms, without being significantly different from each other. PHQ2 had the highest in-EI (0.043) while PHQ9 has the lowest in-EI (0.007). Regarding centrality between constructs, bridge centrality estimates were compared. For social support, OSSS1 and OSSS3 had higher bridge out-EIs than OSSS2 (concerns from others). For depressive symptoms, PHQ2 and PHQ6 had highest bridge in-EIs (0.009 and 0.008) among all symptoms. Loneliness demonstrated highest bridge in-EI and out-EI, implying a mediator role.
Figure 2.
Centrality (A) and bridge centrality (B) indices for elements of social support, loneliness and depressive symptoms in the network. Bridge EIs that focus on cross-construction edges. Autoregressive effects are removed when calculating the indices. EI, expected influence; OSSS, Oslo Social Support Scale; PHQ, Patient Health Questionnaire.
Robustness of the network
CIs of the edge weights were examined (see online supplemental figure 1). Edge weight difference tests and centrality difference tests are presented in online supplemental figures 2 and 3. The estimations of out-EI, in-EI and bridge-EI showed strong stability in case-drop bootstrapping (see online supplemental figure 4). The CS coefficients for the parameters were 0.60, 0.75 and 0.67. Most edges between social support, loneliness and depression were replicated in the network when covariates were controlled, except for the edge from OSSS3 to PHQ6, which switched to OSSS1 to PHQ6 (see online supplemental figure 5).
For sensitivity analysis, the dichotomised network replicated most of the main findings except for the edge from OSSS1 to loneliness (see online supplemental figure 6). Of 94.3% of the edges in the main network were replicated in the dichotomised network. The edge weights of the main and dichotomised network were strongly correlated: r=0.93 (95% CI 0.91 to 0.95). Regarding centrality measures, all the parameters are highly correlated (rs from 0.75 to 0.97) between the two networks.
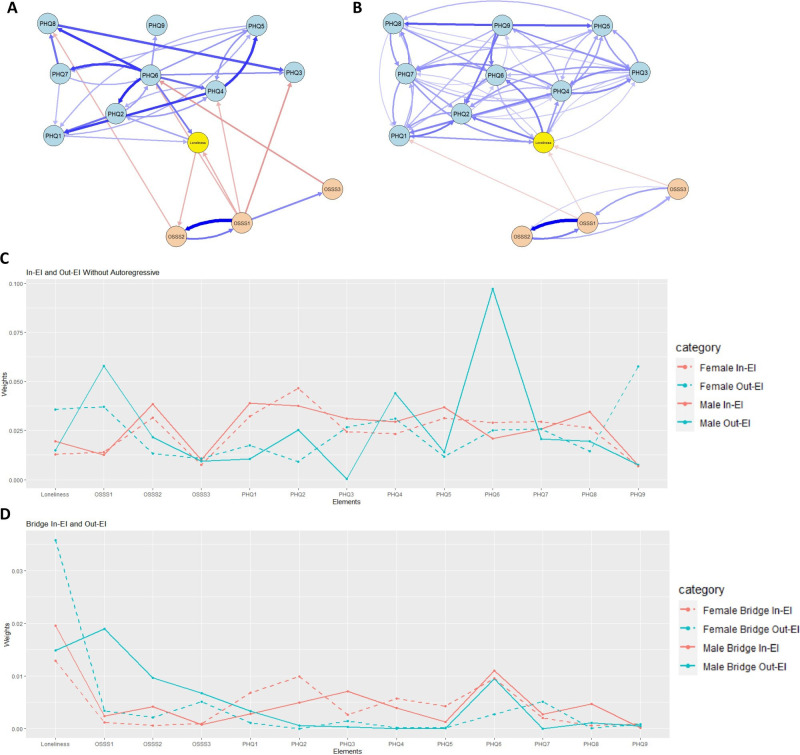
Gender difference tests
The CLPN model was estimated among men and women participants separately (figure 3A for men, figure 3B for women). The original edge weights are shown in online supplemental tables 2 and 3. In the men’s network, there are more edges with higher weights from social support to depressive symptoms, in addition those identified in the total sample: from OSSS1 to PHQ6 (weight=−0.055), PHQ3 (sleep disturbance, weight=−0.073) and PHQ4 (weight=−0.053) and from OSSS2 to PHQ8 (psychomotor disturbance, weight=−0.052). For women, there were no additional edges between social support and depression when compared with the full sample, and the effect from OSSS3 to PHQ6 was no longer adequately strong to be plotted (weight=−0.027).
Figure 3.
Comparison between the men’s and women’s networks. (A) Men’s network of social support, loneliness, and depressive symptoms; (B) women’s network of social support, loneliness, and depressive symptoms. To facilitate visual comparison, the same layout with the network in full sample was used to plot the networks and a higher threshold for weak edges (0.05) was used for men’s network. (C) Comparison of centrality indices for the nodes; (D) comparison of bridge centrality indices for the nodes. PHQ1: anhedonia; PHQ2: depressed mood; PHQ3: sleep disturbance; PHQ4: low energy; PHQ5: appetitive disturbance; PHQ6: negative self-appraisal; PHQ7: concentration difficulties; PHQ8: psychomotor disturbance; PHQ9: suicide/self-harm; OSSS1: number of close confidants; OSSS2: number of close confidants: concern from others; OSSS3: accessible practical help from neighbours. EI, expected influence; OSSS, Oslo Social Support Scale; PHQ, Patient Health Questionnaire.
Regarding nodes’ centrality (see figure 3C,D), both networks demonstrated moderate to good stability. CS coefficients for out-EI, in-EI and bridge EI were 0.44, 0.52 and 0.36 among men, and 0.44, 0.75 and 0.67 among women (see online supplemental figures 7 and 8). PHQ6 had highest out-EI (0.097) of all depressive symptoms of men, while PHQ9 was the highest (0.058) for women. The bridge out-EI for social support nodes was higher among men. PHQ6 had high bridge in-EI (approaching 0.01) in both men and women, while in the women’s network PHQ2 also had high bridge in-EI (0.099).
Discussion
The current study revealed the potential mechanism through which social support improves depression symptomatology early in the COVID-19 pandemic using a longitudinal network perspective. This study comes to two main findings: (1) a unidirectional protective effect of social support mainly on particular depressive symptoms, partly mediated through decreased loneliness; (2) significant gender differences in the strength and pattern of associations observed between social support and depression, with men showing stronger overall associations.
We found direct negative edges from social support nodes to depressive symptoms, which suggests that lower social support was associated with increased depressive symptom severity. Social support also negatively predicted loneliness, which further associated with depressive symptoms such as depressed mood and negative self-appraisal. This finding is in line with previous studies28 and supports the bridge role of loneliness: those with lower social support under stressful situations experience feelings of loneliness, which in turn exacerbate depressive symptoms.19 It was previously argued that pre-existing mental health problems might affect individual’s possession of social ties and perceived or received support.7 Social support could be the outcome rather than a cause of psychiatric disorders.29 By applying a longitudinal data-driven methodology, our study provided evidence against this argument as no significant edges from the depressive symptoms to social support were identified in the network.
Some of the depressive symptoms were playing a more important roles than others in the combined social support-depression network. Negative self-appraisal and depressed mood are depressive symptoms with highest bridge in-EI, suggest both symptoms are more likely to be affected by social support and loneliness when compared with other symptoms. The network shows that social support is directly associated with reductions in negative self-appraisal symptoms (ie, self-failure and letting others down), and also indirectly through loneliness. One’s view of oneself is shaped by the appraisal from surrounding people.7 Individuals receiving more support may gain more positive appraisal from people that facilitate reappraisal of the stressor and themselves, prevent self-criticism and create positive self-evaluation under stressful situations. Support from others creates a feeling that one deserves to be helped, which challenges negative self-cognitions that they have let others down. This pathway supports the self-esteem theory of social support.7 Positive self-evaluation helps build higher self-esteem (ie, internal beliefs regarding how good a person is in general), which further associated with lower depression.30 In our study, we noticed high out-EI of negative self-appraisal, suggesting the strong influence of the symptom on other depressive symptoms. The protective effect of social support could be spread and amplified to the whole depression dynamic network through decreased negative self-appraisal. In addition, this finding helps explain the role of social support in preventing other mental disorders related to negative self-appraisal after stressful events such as posttraumatic stress disorder.31 Changes in depressed mood are also predicted by social support, through bridge of loneliness. Connecting to other people creates a feeling of companionship, which reduces loneliness and subsequent negative effect.32 However, the depressed mood sysmptom has high in-EI and low out-EI, which suggests this symptom was more often predicted by other depressive symptoms than it predicted increases in other symptoms. Therefore, decreased depressed mood might constitute a common end point of social support’s protective effect.
Additionally, our study provides a novel perspective on gender differences in the relationship between social support and depression psychopathology. As discussed before, decreased negative self-appraisal and improved self-esteem are critical mechanisms through which social support has an impact on the depressive symptom network. In men, negative self-appraisal appeared to be dominant over other depressive symptoms, indicated by its highest out-EI in the network. Improvement in this symptom is related to overall depression improvement. The symptom with highest out-EI in the women’s network is suicide/self-harm, which cannot be addressed by increased social support (indicated by lowest bridge in-EI of the symptom). Negative self-appraisal does not have equivalent impact on other depressive symptoms as was found among men. This pattern of gender differences was consistent with a previous study showing that initial higher levels of self-esteem predicted fewer subsequent depressive symptoms among men, but not in their women partners.33 Furthermore, there were more direct edges from social support to depression for men with higher weights, which suggests men benefit more easily from support from their social network than women–increased social support can directly improve depressive symptoms, including sleep disturbance, negative self-appraisal and fatigue.
We included different domains of social support in this study. Both structural (OSSS1) and instrumental support (OSSS3) are associated with significant reductions in depressive symptoms, but there was a smaller effect from emotional support (OSSS2) to depression or loneliness. The results were consistent with one previous study reporting associations between depression remission and social network size, practical support and loneliness severity, but not with emotional support.34 Our findings suggest providing instrumental support such as financial support or practical help could be more beneficial than strategies focused on emotional support after stressful events.
There are several limitations of the current study. First, the data were obtained from an online survey using convenience sampling and this likely introduced sampling bias. Most of the participants were women with reliable access to the internet. The overall educational level of the sample is higher than what was reported in other online convenience samples. Second, population heterogeneity was not addressed in our current analyses. The time window of this study focused on the earlier stage of a stressful event, and the exposure to stress associated with the pandemic likely varied among populations limiting generalisability. The relationship between social support and depression might also differ in various cultural contexts. Last, we used listwise deletion to handle missing data, which might introduce bias and decreased statistical power. Finally, it is unclear how the time lag between wave 1 and wave 2 affects our results. Data that estimates the associations under study utilising varying time lags are needed to understand whether there are temporal effects underlying the mechanisms we evaluated.
Overall, this study reinvestigated the psychosocial correlates of depressive symptoms among adults. By applying the longitudinal network methodology, this is the first time that the directed associations between mental disorder and social support were modelled to identify key elements through a quantitative evaluation of symptom centrality. Our study provides a new perspective to understand the social determinants of mental disorders: modified self-appraisal may be a key bridge to connect social support with improved depression. Additionally, a key gender difference in the social support-mental health association was revealed in this study.
Clinical implications
First, building community-based support networks to deliver practical support could be more effective than emotional support alone, especially for men. Second, suicidal ideation was largely unaffected by social support. Suicide prevention services are still necessary even when social support-based interventions are implemented to the target population under stress. Last, for women, subjective loneliness-reduction interventions would be a more straightforward strategy to help treat depressive symptoms than providing community network support.
Footnotes
Contributors: GL: conceptualisation, methodology, writing—original draft preparation; YL: methodology, software, writing—reviewing and editing; BJH: conceptualisation, data collection, supervision, writing—reviewing and editing; MS and MP: development of the international project concept, data collection; writing—reviewing and editing; TS: methodology, writing—reviewing and editing; all other co-authors involved in the data collection and writing—reviewing and editing. BJH is the guarantor of this paper.
Funding: Funding support is provided by the Center for Global Health Equity, NYU Shanghai, and the Freie Universität Berlin.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The research data are available upon reasonable request.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
Ethics approval
The COMET study was approved by the ethical review board of the Faculty of Behavioral and Movement Sciences of the Vrije Universiteit Amsterdam (VCWE-2020-077), by the Ethics Committee of the Department of Human Neurosciences—Sapienza University of Rome, Italy (approval n° 02/2020), the ethical review board of the University of Verona (UNIVR n8/2020), by the ethical review board in Sweden (Dnr 2020-02157), the Research Ethics Committee Universitas Padjadjaran Bandung (431/UN6.KEP/EC/2020) the ethical review board of the Koc University, Turkey (2020.134.IRB3.072), the Health Research Ethics Committee of Stellenbosch University (Ethics Reference No: N20/05/016_COVID-19), the Research Ethics Committee Universitas Padjadjaran Bandung (431/UN6.KEP/EC/2020), and by the ethical review board of Freie Universität Berlin, Germany (023/0000). The French contribution to the COMET consortium is in accordance with French regulations concerning the Comité de Protection des Personnes (CCP), the Règlement Général sur la Protection des Données (RGPD) and the Informatique et Libertés law. Participants gave informed consent to participate in the study before taking part.
References
- 1. Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal Ideation. Annu Rev Clin Psychol 2016;12:307–30. 10.1146/annurev-clinpsy-021815-093204 [DOI] [PubMed] [Google Scholar]
- 2. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yang L, Zhao Y, Wang Y, et al. The effects of psychological stress on depression. Curr Neuropharmacol 2015;13:494–504. 10.2174/1570159x1304150831150507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pryce CR, Azzinnari D, Spinelli S, et al. Helplessness: a systematic translational review of theory and evidence for its relevance to understanding and treating depression. Pharmacol Ther 2011;132:242–67. 10.1016/j.pharmthera.2011.06.006 [DOI] [PubMed] [Google Scholar]
- 5. Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry 2016;209:284–93. 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- 6. Kocalevent R-D, Berg L, Beutel ME, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol 2018;6:31. 10.1186/s40359-018-0249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav 2011;52:145–61. 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- 8. Lin J, Su Y, Lv X, et al. Perceived Stressfulness mediates the effects of subjective social support and negative coping style on suicide risk in Chinese patients with major depressive disorder. J Affect Disord 2020;265:32–8. 10.1016/j.jad.2020.01.026 [DOI] [PubMed] [Google Scholar]
- 9. Buch AM, Liston C. Dissecting diagnostic heterogeneity in depression by integrating neuroimaging and Genetics. Neuropsychopharmacology 2021;46:156–75. 10.1038/s41386-020-00789-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Borsboom D. A network theory of mental disorders. World Psychiatry 2017;16:5–13. 10.1002/wps.20375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Campbell S, Osborn TL. Adolescent psychopathology and psychological wellbeing: a network analysis approach. BMC Psychiatry 2021;21:333. 10.1186/s12888-021-03331-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bos FM, Snippe E, de Vos S, et al. Can we jump from cross-sectional to dynamic interpretations of networks? implications for the network perspective in psychiatry. Psychother Psychosom 2017;86:175–7. 10.1159/000453583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rhemtulla M, van Bork R, Cramer AOJ. Cross-lagged network models. Multivariate Behav Res 2022. [Google Scholar]
- 14. Zainal NH, Newman MG. Prospective network analysis of proinflammatory proteins, lipid markers, and depression components in Midlife community women. Psychol Med 2023;53:5267–78. 10.1017/S003329172200232X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chavez-Baldini U, Verweij K, de Beurs D, et al. The interplay between psychopathological symptoms: transdiagnostic cross-lagged panel network model. BJPsych Open 2022;8:e116. 10.1192/bjo.2022.516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rubin M, Bicki A, Papini S, et al. Distinct trajectories of depression symptoms in early and middle adolescence: preliminary evidence from longitudinal network analysis. J Psychiatr Res 2021;142:198–203. 10.1016/j.jpsychires.2021.07.053 [DOI] [PubMed] [Google Scholar]
- 17. Hoorelbeke K, Van den Bergh N, Wichers M, et al. Between vulnerability and resilience: a network analysis of fluctuations in cognitive risk and protective factors following remission from depression. Behav Res Ther 2019;116:1–9. 10.1016/j.brat.2019.01.007 [DOI] [PubMed] [Google Scholar]
- 18. Kraft B, Bø R, Hoorelbeke K, et al. Examining attentional functioning in depression using a personalized network approach: a proof-of-principle study. Psychiatry Research Communications 2023;3:100137. 10.1016/j.psycom.2023.100137 [DOI] [Google Scholar]
- 19. Erzen E, Çikrikci Ö. The effect of loneliness on depression: a meta-analysis. Int J Soc Psychiatry 2018;64:427–35. 10.1177/0020764018776349 [DOI] [PubMed] [Google Scholar]
- 20. Labrague LJ, De Los Santos JAA, Falguera CC. Social and emotional loneliness among college students during the COVID-19 pandemic: the predictive role of coping behaviors, social support, and personal resilience. Perspect Psychiatr Care 2021;57:1578–84. 10.1111/ppc.12721 [DOI] [PubMed] [Google Scholar]
- 21. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta-analyses of diagnoses and symptoms. Psychol Bull 2017;143:783–822. 10.1037/bul0000102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sonnenberg CM, Deeg DJH, van Tilburg TG, et al. Gender differences in the relation between depression and social support in later life. Int Psychogeriatr 2013;25:61–70. 10.1017/S1041610212001202 [DOI] [PubMed] [Google Scholar]
- 23. Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. primary care evaluation of mental disorders. Patient health questionnaire. JAMA 1999;282:1737–44. 10.1001/jama.282.18.1737 [DOI] [PubMed] [Google Scholar]
- 24. Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 2018;50:195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Robinaugh DJ, Millner AJ, McNally RJ. Identifying highly influential nodes in the complicated grief network. J Abnorm Psychol 2016;125:747–57. 10.1037/abn0000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jones PJ, Ma R, McNally RJ. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res 2021;56:353–67. 10.1080/00273171.2019.1614898 [DOI] [PubMed] [Google Scholar]
- 27. Funkhouser CJ, Chacko AA, Correa KA, et al. Unique longitudinal relationships between symptoms of psychopathology in youth: a cross-lagged panel network analysis in the ABCD study. J Child Psychol Psychiatry 2021;62:184–94. 10.1111/jcpp.13256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. von Känel R, Weilenmann S, Spiller TR. Loneliness is associated with depressive affect, but not with most other symptoms of depression in community-dwelling individuals: a network analysis. IJERPH 2021;18:2408. 10.3390/ijerph18052408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hall BJ, Bonanno GA, Bolton PA, et al. A longitudinal investigation of changes to social resources associated with psychological distress among Kurdish torture survivors living in northern Iraq. J Trauma Stress 2014;27:446–53. 10.1002/jts.21930 [DOI] [PubMed] [Google Scholar]
- 30. Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu Rev Clin Psychol 2007;3:377–401. 10.1146/annurev.clinpsy.3.022806.091520 [DOI] [PubMed] [Google Scholar]
- 31. Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther 2000;38:319–45. 10.1016/s0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- 32. Eaker ED. Social support and physical health: understanding the health consequences of relationships. American Journal of Epidemiology 2005;161:297–8. 10.1093/aje/kwi036 [DOI] [Google Scholar]
- 33. Johnson MD, Galambos NL, Finn C, et al. Pathways between self-esteem and depression in couples. Dev Psychol 2017;53:787–99. 10.1037/dev0000276 [DOI] [PubMed] [Google Scholar]
- 34. van den Brink RHS, Schutter N, Hanssen DJC, et al. Prognostic significance of social network, social support and loneliness for course of major depressive disorder in adulthood and old age. Epidemiol Psychiatr Sci 2018;27:266–77. 10.1017/S2045796017000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjment-2023-300802supp001.pdf (570.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The research data are available upon reasonable request.