Abstract
Introduction
The aim of this study was to assess the effectiveness of low-power thulium (30 W) and the duration necessary to eliminate adenomas at the level of the surgical capsule, as well as its impact on postoperative urinary and sexual function.
Material and methods
Patients with symptomatic benign prostatic hyperplasia (BPH), who had ThuLEP between December 2019 and March 2022 and had a prostate size >80 mL and had not responded to the medication therapy, were included. The prostate size, prostate-specific antigen (PSA), enucleation and morcellation times, postoperative International Prostate Symptom Score (IPSS), and International Index of Erectile Function-5 (IEFF-5) records at 1, 3, 6, and 12 months were among the information gathered.
Results
The average age of the 80 patients who received ThuLEP was 66.7 ±6.4 years, with a mean prostate volume of 112.65 ±19.3 mL. The mean duration for enucleation was 71 ±11 min. At the initial follow-up after one month, the mean IPSS was 8.012 ±1.78 mL and the mean Qmax enhancement was 30.16 ±4 mL s-1. In contrast to baseline, our findings demonstrated a substantial improvement in postoperative urgency and urgency urinary incontinence (UUI) (p = 0.005) but no meaningful variation in IIEF-5 score at the 12-month follow-up.
Conclusions
Low-power ThuLEP is worthwhile for therapeutic use because it effectively treats patients with large prostates with satisfactory urinary and sexual effects.
Clinical trials .gov ID: NCT05494944
Keywords: benign prostatic hyperplasia, enucleation, low power, ThuLEP
INTRODUCTION
Benign prostatic hyperplasia (BPH) is a medical disorder that often affects older men and has been linked to the natural aging process. Around 40% of 70-year-old men have this condition [1, 2].
Laser prostate enucleation (HoLEP) has been shown to be a safe procedure with a reduced risk of bleeding [3], shorter hospital stays [4], and a quicker features time [5] when compared to other BPH treatment options, i.e. open prostatectomy and transurethral resection of the prostate (TURP), which have some minimal and key adverse impacts such as dysuria, urinary frequency, sexual dysfunction, and sepsis [6]. ThuLEP is rapidly becoming recognized as a safe and efficient method for treating BPH [7]. Most previous research assessed the effectiveness and viability of using high-power ThuLEP (120–200 W) for large prostates [8, 9, 10].
In 2021 Omar et al. [11] published a study that evaluated the utilization of low-power ThuLEP. They successfully performed prostate enucleation using a 30-W thulium laser.
The premise behind adopting low-power laser enucleation is to give less energy to the surrounding structures but with similar outcomes to high-power ThuLEP and a lower incidence of postoperative dysuria, decreased storage LUTs, and improved erectile function.
Our study aimed to assess the feasibility and effectiveness of using low-power ThuLEP to effectively eliminate the adenoma at the level of the surgical capsule within the appropriate time, as well as to assess the urine and sexual result over the course of a one-year follow-up.
MATERIAL AND METHODS
This prospective observational study was performed in Cairo University Hospitals, Department of Urology, Egypt. Our study comprised patients with a symptomatic BPH and a prostate size greater than 80 mL, failed medical therapy for their BPH, or BPH-related comorbidities. Omitted from the study were patients with a history of bleeding, neurogenic bladder, urethral strictures, failed transurethral prostate surgery, or prostate cancer.
Our research plan received approval from the Local Ethics Committee (Faculty of Medicine, Kasr Al Aini, Cairo University, with ethical IRB number: MD – 189 – 2020), and we obtained signed informed consent from each eligible patient who visited our prostate unit. Each patient completed an informed consent form prior to surgery after taking the time they needed to consider whether to participate. The history, digital rectal exam, international prostate symptom score (IPSS), urine analysis and culture, haemoglobin concentration (Hb), serum prostate-specific antigen (PSA) (preoperative and at 6 months), transrectal ultrasonography (TRUS), Uroflow, and post-void residual urine PVR were all performed on eligible individuals (after voiding residual urine). The International Index of Erectile Function (IIEF-5) score was used to determine preoperative erectile function (EF).
Under local anaesthesia, ThuLEP was conducted by 2 surgeons with experience in BPH endoscopic surgery (TURP) and more than 50 operations with ThuLEP and HoLEP. For both cutting and coagulation, we employed the Revolix DUO® Thulium laser unit (LISA laser, Katlenburg-Lindau, Germany) with an energy setting of 30 W. The laser fibre was a 26 Fr constant-flow resectoscope with a 550 µm RigiFib from LISA Laser in Katlenburg-Lindau, Germany. In all cases, we underwent two-lobe enucleation. A Storz morcellator was used to perform the mutilation (Karl Storz GmbH & Co., Tuttlingen, Germany). Saline solution utilized physiologically was used for irrigation.
The haemoglobin concentration, operative time, enucleation and morcellation time, need for blood transfusion, presence and type of complications (intra- and immediate postoperatively), hospital stay, and catheter removal comprised the perioperative data. After smooth surgical operations, catheter removal was routinely done within 24 h, and patients were released after they were catheter-free and had no clinically substantial voiding symptoms.
Functional follow-up data at 1, 3, 6, and 12 months, such as the existence of dysuria and urgency with or without urge urinary incontinence, stress urinary incontinence, IPSS score, IIEF-5 score, post-void residual urine (PVR), and Qmax, were also recorded. Treatment failure was described as the prerequisite for a second operation or the presence of patients with poor functional outcomes as shown by persistent obstructive symptoms (IPSS), severe PVR, or recurrent urine retaining.
Our main aim was to estimate the efficacy of using low-power thulium (30 W) to effectively eliminate the adenoma from the surgical capsule’s level and the time needed to complete the procedure. Meanwhile, our secondary target was to assess the postoperative urinary and sexual outcomes.
Statistical analysis
Data were statistically characterized using the mean, standard deviation (SD), and range or, when appropriate, frequencies (number of occurrences) and percentages. The paired t test was utilized to match the numerical data because the sample size was large enough, and the McNemar test was used to compare the categorical data. Through the study of the General Linear Model, Repeated Measure ANOVA was used for all comparisons of 2 variables over time among more than 3 time points. Statistics were regarded as significant when two-sided p-values were <0.05. IBM SPSS (Statistical Package for the Social Science; IBM Corp., Armonk, NY, USA) version 22 for Microsoft Windows was utilized to perform all statistical computations.
RESULTS
Between December 2019 and March 2022, 80 patients with characteristic BPH with failed medicinal therapy or BPH-related problems and a prostate size greater than 80 mL underwent ThuLEP; their mean age was 66.7 ±6.4 years. With a mean IPPS score of 26 ±1.96, surgical intervention was primarily indicated in 60% of patients after unsuccessful medicinal therapy. The haematuria rate was 15%, and refractory retention was 25%. The mean Qmax was 7 ±2.05 mL sec-1, and the mean prostate volume was 112.65 ±19.3 mL. The mean preoperative Hb was 13.305 ±1.33 and the mean preoperative PSA amount was 4.4 ±1.4. Post-voiding residual urine was 127 ±18.95. The median IIEF-5 score prior to surgery was 15.8 ±1.977. Urinary bladder stones co-existed in 4 cases. Table 1 compares the features of the preoperative patients to the postoperative results at 1-, 3-, 6-, and 12-month intervals.
Table 1.
Preoperative and postoperative urinary and sexual outcomes
| Pre-operative | 1 month | 3 months | 6 months | 12 months | P value | |
|---|---|---|---|---|---|---|
| Age (years) | 66.7 ±6.4 | – | – | – | – | – |
| IPSS | 25.6 ±2.2 | 8.012 ±1.78 | 6.6 ±2.0 | 5.1 ±1.3 | 4.2 ±1.0 | <0.001 |
| Qmax | 6.9 ±2.2 | 30.16 ±4 | 30.2 ±4.1 | 32.6 ±5.2 | 35.0 ±4.9 | <0.001 |
| PSA | 4.4 ±1.4 | – | – | 1.06 ±0.3 | – | <0.001 |
| PVR | 127.0 ±19.0 | 37.8 ±9.7 | 22.8 ±5.4 | 15.5 ±4.6 | 11.7 ±3.4 | <0.001 |
| IIEF-5 | 15.1 ±2.0 | 14.5 ±1.6 | 15.0 ±1.7 | 0.009 |
IPSS – International Prostate Symptom Score; PSA – prostate-specific antigen; PVR – post-void residual urine; IIEF-5 – International Index of Erectile Function
The average length of the operation was 94.2 ±16.5 min, with the average enucleation taking 71 ±11 min, and the average morcellation taking 25.21 ±6.25 min. The average amount of laser energy was 86.3 ±17.16. After 6 months, the average PSA level dropped by 3.38 ±1.1 and the average haemoglobin level dropped by 1.81 ±0.63 mg dL-1. One patient required blood transfusions owing to substantial bleeding, and the other 4 were recommended by the anaesthesia team because of their age and borderline preoperative Hb concentrations (between 10 and 12 gm dL-1). The average length of stay in the hospital was 1.19 d, and 80% of patients had their catheters removed on the first day. As regards intraoperative complications, 6 patients had a capsular perforation, with 2 converted to bipolar TURP, 4 patients had mild sub-trigonal dissection, 2 patients had minor bladder mucosal injury with morcellation, and 2 patients had significant bleeding controlled by bipolar coagulation. In complicated patients, urinary catheters stayed in for longer periods of time (Table 2).
Table 2.
Operative outcomes and intra-operative complications
| Result | |
|---|---|
| Operative time (minutes)* | 94.2 ±16.5 |
| Enucleation time (minutes)* | 71 ±11 |
| Morcellation time (minutes)* | 25.21 ±6.25 |
| Laser energy used (kilojoules)* | 86.3 ±17.16 |
| Resected prostate weight (grams)* | 69.25 ±13.2 |
| Hb drop (g/dL) * | 1.81 ±0.63 |
| Hospital stay (days)* | 1.2 ±0.4 |
| Catheter Duration (days)* | 1.5 ±1.0 |
| Patient readmission** | 2 (2.5%) |
| Capsular perforation** | 6 (7.5%) |
| Subtrigonal dissection** | 4 (4.8%) |
| Conversion to TUR** | 2 (2.5%) |
| Minor bladder injury from morcellator** | 2 (2.5%) |
| Significant IO bleeding** | 2 (2.5%) |
Hb – haemoglobin concentration
data were described in mean ±SD;
data were described using the number of cases (%)
Two patients with post-operative haematuria were treated with anti-bleeding medications (Clavien grade II), 2 patients with clot retention required readmission but were treated with a 3-way catheter and irrigation and discharged within 3 d (Clavien grade II), and no blood transfusion was required. These events occurred during the first 2 weeks. There are no reported cases of postoperative epididymitis or epididymo-orchitis (Table 3).
Table 3.
Post-operative complications
| Number of patients (%) | Management | |
|---|---|---|
| At 1 week post-operative | ||
| Haematuria | 2 (2.5%) | Antibleeding measures and antibiotics |
| Clot retention | 2 (2.5%) | 3-way catheter fixation and bladder irrigation |
| Febrile UTI | 6 (7.5%) | IV antibiotics |
| At 1 month post-operative | ||
| Urge | 4 (5.4%) | Anticholinergics and reassurance |
| SUI | 10 (12.5%) | Reassurance and Kegel exercises |
| At 3 months post-operative | ||
| Urge | 0 | |
| SUI | 4 (5%) | |
| At 6 months post-operative | ||
| SUI | 0 | |
UTI – urinary tract infections; SUI – stress urinary incontinence
The initial visit was at one month, and we noticed significant mean IPSS score enhancement with a value of 8.012 ±1.78, Qmax progress of 30.16 ±4 mL sec-1, and post-void residual value of 37.78 ±9.6 mL.
Regarding the postoperative urgency, in dysuria urgency urinary incontinence follow-up at 1, 3, and 6 months, there was a noticeable improvement at the first month with only 4 (5.4%) patients having dysuria and urge incontinence treated by reassurance and antimuscarinics and resolved completely in all patients by the 3-month follow-up.
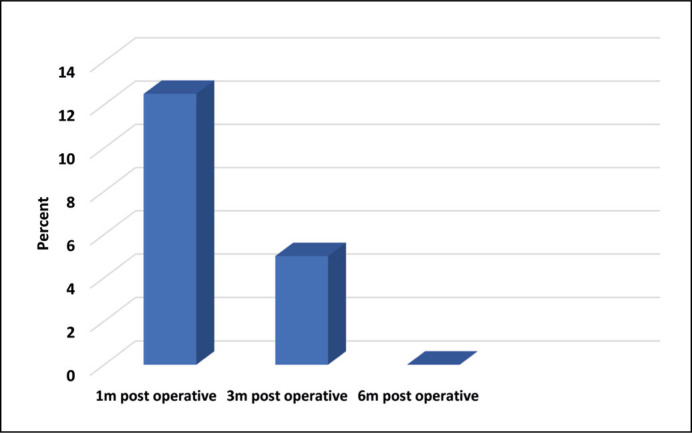
Regarding stress urinary incontinence (SUI), 10 (12.5%) patients were reassured and given instructions to conduct pelvic floor exercises during the one-month follow-up, but at the 3-month mark, only 4 (5%) patients showed improvement. Most incontinence cases had improved by 6 months after surgery (Table 3, Figure 1).
Figure 1.
Occurrence of stress urinary incontinence during follow-up.
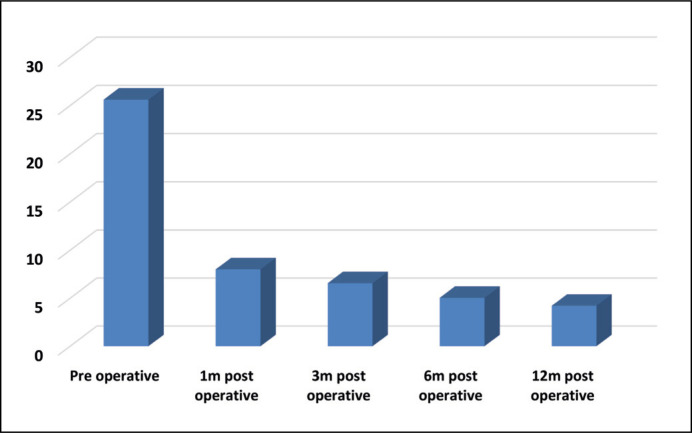
There was a statistically significant decrease in IPSS (p <0.001), PSA (p <0.001), and PVR (p <0.001) throughout follow-up at 1, 3, and 6 months, but a statistically significant (p <0.001) rise in Qmax (Figure 2).
Figure 2.
Mean values of International Prostate Symptom Score during follow-up.
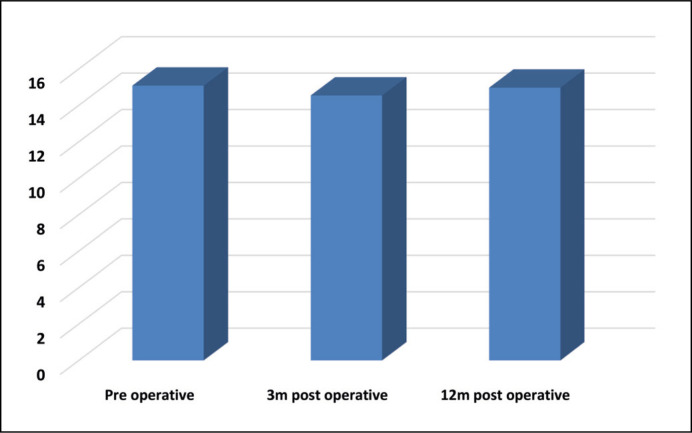
In terms of IIEF score, there was a statistically significant decrease at 3 months after surgery (p = 0.027), but there was no statistically significant change between the IIEF score before surgery and at 12 months after surgery (p = 0.554) (Figure 3).
Figure 3.
Mean values of International Index of Erectile Function score during follow-up.
At the 12-month follow-up, there were no re-interventions for reoccurring obstructive symptoms. There have not been any occurrences of urethral stricture or bladder neck contracture recorded.
DISCUSSION
The gold standard for treating BPH is transurethral resection of the prostate (TURP), which causes less trauma and has a quicker healing time than open surgery [12, 13]. With good and secure outcomes for a prostate of average size, bipolar TURP altered the paradigm of a minimally invasive prostatectomy [14]. Prior to the invention of laser prostate enucleation, larger prostates (>80 g) typically required more invasive procedures like open or robotic prostatectomy.
Both American Urological Association (AUA) and European Association of Urologists (EAU) suggestions for BPH treatment have recommended holmium laser enucleation of the prostate (HoLEP) [15, 16]. The high initial costs and the challenging learning curve of this approach were the 2 primary drawbacks that prevented its widespread implementation in the urological community.
The thulium laser, which was introduced for clinical use in 2005, is now the most innovative and widely used laser in urology [17]. It has enhanced vaporization and haemostasis advantages in comparison to all other lasers [18]. Thulium use started with the resection of the prostate (vaporesection), followed by the introduction of enucleation techniques. Most thulium-based enucleations in the literature have been performed with power settings ranging from 120 [7] to 60 W [19], with the power setting for the coagulation limited to 40–60 W [20]. The main drawback of using high-power thulium is its black escharing effect on the incised tissues due to its physical properties, which could mask the enucleation planes and affect the learning curve.
Two HoLEP-inexperienced surgeons performed 105 HoLEPs over the course of 14 months in 2015 utilizing a 50 W Holmium laser, and they reported positive patient results [21].
Elshal et al. (2018) examined low-power and high-power holmium in 121 patients and found that regardless of the amount of surgeon expertise, low-power HoLEP (50 W) is similar to high-power HoLEP (100 W) in terms of all operating efficacy measures [22].
Low-power THuLEP has been shown to increase the clinical effectiveness in BPH patients; however, there is currently very little study of this topic. Our hypothesis is based on the idea that we can perform laser-assisted enucleation of the prostate at a comparable rate utilizing a low-power thulium laser (30 W), while retaining the same efficacy factors as high-power lasers. This will help to reduce the postoperative dysuria, storage urinary symptoms, and possible adverse effects on erectile function.
In this work, we attempted to reduce the amount of energy used during enucleation by favouring mechanical enucleation. Because it is better for haemostasis, we simply utilized a low-power ThuLEP to separate the capsule and the gland at their places of attachment and to halt bleeding there. We reasoned that utilizing a lower power level would make tissue cutting safer and less complicated, while also reducing the risk of harm to adjacent healthy tissues. Our investigation also shows that employing low-power ThuLEP has the benefit of making it simple to identify the planes and the capsule anatomically while having no adverse effects on the length of the operation.
Our data showed that there was a marked improvement in the postoperative dysuria and storage symptoms in one month of follow-up, which resolved completely after 3 months. Furthermore, our data noted no statistically significant alteration between the IIEF score preoperatively and at 12 months postoperative. No re-interventions were recorded for recurrence at 12 months of follow-up.
Omar et al. [11] also reported no significant fluctuation in IIEF-5 score at 12-month follow-up, equated with the baseline using low-power ThuLEP, but without reporting any data about postoperative storage symptoms or dysuria. Furthermore, the mean enucleation time in our study was 70 ±10 min, which is comparable to their study despite our larger mean prostate size (Table 4).
Table 4.
Comparison between our study and other studies
| Study | No of patients | Prostate size (ml) | Type of study | Laser power (W) | Enucleation time (min) | One year follow-up results (IPSS/IIEF/dysuria) |
|---|---|---|---|---|---|---|
| Our study | 80 | Mean 111 ±20 |
Prospective | 30 | 69.8 ±10.7 | IPSS 4.2 ±1.0 IIEF 15.0 ±1.7 Postoperative dysuria resolved completely by 3 months |
|
| ||||||
| Omar et al. 2021 [11] | 60 | 102 ±25 | Prospective | 30 | 80 ±12 | IPSS 4 ±3 IIEF 15.3 ±3.8 Postoperative dysuria not assessed |
IPSS – International Prostate Symptom Score; IIEF-5 – International Index of Erectile Function
In places with limited resources, the use of a low-power machine may result in reduction of the initial cost of the ThuLEP operation, not only because of the low cost of the machine. However, employing low-power equipment eliminates the requirement for multiphase connectors, which are usually not available in operation rooms.
To date, very few studies have evaluated the efficacy and safety of using low-power ThuLEP in removing prostate adenomas greater than 80 g at the level of the surgical capsule within the appropriate time with satisfactory urinary and sexual outcomes. Further studies are needed on a large scale; one of the restrictions of our study was its small sample size owing to the COVID pandemic. In addition, further randomized studies are needed to compare low-power versus high-power ThuLEP and confirm the non-inferiority of low-power ThuLEP as a minimally invasive surgery with lower costs and reduced postoperative urinary and sexual negative impact.
CONCLUSIONS
Low-power ThuLEP is worthwhile for therapeutic use because it effectively treats patients with large prostates with satisfactory urinary and sexual effects.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
ETHICAL CONSIDERATION
Approval of the research protocol by an Institutional Review Board
The study was authorized by the Ethics Committee at the Faculty of Medicine, Kasr Al Aini, Cairo University with ethical IRB number: MD – 189 - 2020.
Registry and Registration No. of the study: Clinicaltrials.gov ID: NCT05494944
Informed consent: Written informed consent was obtained from all participants.
References
- 1.Chute CG, Panser LA, Girman CJ, et al. The prevalence of prostatism: a population-based survey of urinary symptoms. J Urol. 1993; 150: 85-89. [DOI] [PubMed] [Google Scholar]
- 2.Bahia LR, Araújo DV, Pepe C, Trindade M, Camargo CM, Javaroni V. Cost-effectiveness analysis of medical treatment of benign prostatic hyperplasia in the Brazilian public health system. Int Braz J Urol. 2012; 38: 595-605. [DOI] [PubMed] [Google Scholar]
- 3.Marien T, Kadihasanoglu M, Miller NL. Holmium laser enucleation of the prostate: patient selection and perspectives. Res Rep Urol. 2016; 8: 181-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilson LC, Gilling PJ, Fraundorfer MR, et al. A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol. 2006; 50: 569-573. [DOI] [PubMed] [Google Scholar]
- 5.Montorsi F, Naspro R, Salonia A, et al. Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center prospective randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol. 2008; 179: S87-S90. [DOI] [PubMed] [Google Scholar]
- 6.Abedi A, Razzaghi MR, Rahavian A, et al. Is Holmium Laser Enucleation of the Prostate a Good Surgical Alternative in Benign Prostatic Hyperplasia Management? A Review Article. J Lasers Med Sci. 2020; 11: 197-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ketan PV, Prashant HS. Thulium laser enucleation of the prostate is a safe and a highly effective modality for the treatment of benign prostatic hyperplasia - Our experience of 236 patients. Urol Ann. 2016; 8: 76-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iacono F, Prezioso D, Di Lauro G, et al. Efficacy, and safety profile of a novel technique, ThuLEP (Thulium laser enucleation of the prostate) for the treatment of benign prostate hypertrophy. Our experience on 148 patients. BMC Surg. 2012; 12 Suppl 1: S21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang CH, Lin TP, Chang YH, Huang WJ, Lin AT, Chen KK. Vapoenucleation of the prostate using a high-power thulium laser: a one-year follow-up study. BMC Urol. 2015; 15: 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chang CH, Lin TP, Huang JY. Safety and effectiveness of high-power thulium laser enucleation of the prostate in patients with glands larger than 80 mL. BMC Urol. 2019; 19: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Omar M, Hodhod A, Moustafa A, et al. Combined top-down approach with low-power thulium laser enucleation of prostate: evaluation of one-year functional outcomes. World J Urol. 2021; 39: 3013-3017. [DOI] [PubMed] [Google Scholar]
- 12.Hu H, Zhang W, Liu X, et al. Nerve growth factor levels are associated with overactive bladder symptoms and long-term treatment outcome after transurethral resection of the prostate in patients with benign prostatic hyperplasia. J Urol. 2018; 200: 620-625. [DOI] [PubMed] [Google Scholar]
- 13.Gilling P, Barber N, Bidair M, et al. WATER: a double-blind, randomized, controlled trial of Aquablation® vs transurethral resection of the prostate in benign prostatic hyperplasia. J Urol. 2018; 199: 1252-1261. [DOI] [PubMed] [Google Scholar]
- 14.Alexander CE, Scullion MM, Omar MI, et al. Bipolar versus monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction. Cochrane Database Syst Rev. 2019; 12: CD009629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McVary KT, Roehrborn CG, Avins AL, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011; 185:1793. [DOI] [PubMed] [Google Scholar]
- 16.Oelke M, Bachmann A, Descazeaud A, et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol. 2013; 64: 118-140. [DOI] [PubMed] [Google Scholar]
- 17.Fried NM, Murray KE. High-power thulium fiber laser ablation of urinary tissues at 1.94 microm. J Endourol. 2005; 19: 25-31. [DOI] [PubMed] [Google Scholar]
- 18.Bach T, Huck N, Wezel F, Häcker A, Gross AJ, Michel MS. 70 vs 120 W thulium:yttrium-aluminium-garnet 2 microm continuous-wave laser for the treatment of benign prostatic hyperplasia: a systematic ex-vivo evaluation. BJU Int. 2010; 106: 368-372. [DOI] [PubMed] [Google Scholar]
- 19.Saredi G, Pirola GM, Pacchetti Aet al. . (2015) Evaluation of the learning curve for thulium laser enucleation of the prostate with the aid of a simulator tool but without tutoring: comparison of two surgeons with different levels of endoscopic experience. BMC Urol. 2015; 15: 49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Junjie Zhang, Zhenyu Ou, Xiaobo Zhang, et al. Holmium laser enucleation of the prostate versus thulium laser enucleation of the prostate for the treatment of large-volume prostates >80 ml: 18-month follow-up results. World J Urol. 2020; 38: 1555-1562. [DOI] [PubMed] [Google Scholar]
- 21.Khan F, Saleemi MA, Taneja S, et al. MP13-04 Is power everything in Holmium laser enucleation of the prostate surgery? The first reported 50-watt Holmium laser enucleation of the prostate surgery. The Journal of Urology. 2015; 193: e137-e137. [Google Scholar]
- 22.Elshal AM, El-Nahas AR, Ghazy M, et al. Low-power vs high-power holmium laser enucleation of the prostate: critical assessment through randomized trial. Urology. 2018; 121: 58-65. [DOI] [PubMed] [Google Scholar]