PREFACE
The American College of Cardiology (ACC) has a long history of developing documents (eg, decision pathways, health policy statements, appropriate use criteria) to provide members with guidance on both clinical and nonclinical topics relevant to cardiovascular care. In most circumstances, these documents have been created to complement clinical practice guidelines and to inform clinicians about areas where evidence is new and evolving or where sufficient data is more limited. Despite this, numerous gaps persist, highlighting the need for more streamlined and efficient processes to implement best practices in patient care.
Central to the ACC’s strategic plan is the generation of actionable knowledge—a concept that places emphasis on making clinical information easier to consume, share, integrate, and update. To this end, the ACC has shifted from developing isolated documents to creating integrated “solution sets.” These are groups of closely related activities, policy, mobile applications, decision-support tools, and other resources necessary to transform care and/or improve heart health. Solution sets address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care. They use both established and emerging methods to disseminate information for cardiovascular conditions and their related management. The success of solution sets rests firmly on their ability to have a measurable impact on the delivery of care. Because solution sets reflect current evidence and ongoing gaps in care, the associated tools will be refined over time to match changing evidence and member needs.
Expert Consensus Decision Pathways represent a key component of solution sets. Standard methodology for developing an Expert Consensus Decision Pathway is as follows: for a high-value topic that has been selected by the Science and Quality Committee and prioritized by the Solution Set Oversight Committee, a group of clinical experts is assembled to develop content that addresses key questions facing our members.1 This content is used to inform the development of various tools that accelerate real-time use of clinical policy at the point of care. Expert Consensus Decision Pathways are not intended to provide single correct answers to clinical questions; rather, they encourage clinicians to consider a range of important factors as they define treatment plans for their patients. Whenever appropriate, Expert Consensus Decision Pathways seek to provide unified articulation of clinical practice guidelines, appropriate use criteria, and other related ACC clinical policy. In some cases, covered topics will be addressed in subsequent clinical practice guidelines as the evidence base evolves. In other cases, these will serve as stand-alone policy.
Nicole M. Bhave, MD, FACC
Chair, ACC Solution Set Oversight Committee
1. INTRODUCTION
Chest pain is one of the most common reasons for emergency department (ED) visits, accounting for over 7 million ED visits annually.2 It is one of the most challenging conditions to evaluate, which contributes to ED overcrowding, inefficient use of resources, and delays to diagnosis. A major challenge is to rapidly identify the small number of patients who have acute coronary syndrome (ACS) or other life-threatening conditions among the large number who have more benign conditions, many of which are noncardiac.3,4
Over the last 40 years, considerable efforts have been made to streamline and improve the chest pain evaluation process. Successive iterations of evaluation and management strategies have reduced both the number of patients who require admission as well as ED length of stay. The objectives of this Expert Consensus Decision Pathway are to provide structure around the evaluation of chest pain in the ED and to facilitate rapid disposition and limit unnecessary testing among patients with chest pain who are at low risk and who do not have ACS. The document also aims to provide critical appraisal of the options for clinical decision pathways (CDPs) that hospitals may choose from to achieve these aims. Implementation of accelerated CDPs has the potential to further reduce ED length of stay and increase the proportion of patients who are eligible for rapid ED discharge and do not routinely require additional diagnostic testing, without compromising patient safety.
2. METHODS
2.1. Background
On February 26, 2020, the ACC Heart House Roundtable “Emergency Department Evaluation of Patients with Possible Acute Coronary Syndrome” was convened to bring together multidisciplinary stakeholders in an effort to include the multiple perspectives involved in the care of patients with acute chest pain. Participants included representatives from medical specialties, including emergency medicine, cardiology, nursing, laboratory medicine, hospital medicine, internal medicine, family medicine, radiology, health systems administrators, insurance company representatives, industry representatives, and government regulators. Clinicians included physicians, nurses, and advanced practice providers (APPs). The purpose of the meeting was to discuss optimal approaches to the evaluation and management of acute chest pain in the ED, with a specific focus on the implementation of protocols using high-sensitivity cardiac troponin (hs-cTn). Participants in this ACC Heart House Roundtable agreed that practical guidance was needed for practitioners, administrators, and health systems as they seek to apply the 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain (denoted as the 2021 American Heart Association [AHA]/ACC/multisociety chest pain guideline in this document) into practice for patients with acute chest pain in the ED.
2.2. Process
The guidance that follows in this Expert Consensus Decision Pathway was informed by the scientific evidence presented and expert opinions considered during the Heart House Roundtable, by subsequent review and deliberation on available evidence by this Expert Consensus Decision Pathway writing committee, and review of the 2021 AHA/ACC/multisociety chest pain guideline5 and other relevant international guidelines.6 Although the Heart House Roundtable provided valuable insight into the practical issues and gaps in care, this document is a separate and independent endeavor aimed specifically at addressing the questions raised during the meeting, as well as other practical questions related to the clinical application of the 2021 AHA/ACC/multisociety chest pain guideline.
The writing committee included representatives from emergency medicine, hospital medicine, cardiology, and nursing. The work of the writing committee was supported exclusively by the ACC without commercial support, as committee members volunteered their time to this effort. Video conference calls of the writing committee were confidential and attended only by committee members and ACC staff. A formal peer review process was completed, consistent with ACC policy, by expert reviewers nominated by the ACC. A public comment period was also held to obtain additional feedback. Following reconciliation of all comments, this document was approved for publication by the ACC Clinical Policy Approval Committee.
The ACC and the Solution Set Oversight Committee recognize the importance of avoiding real or perceived relationships with industry (RWI) or other entities that may affect clinical policy. The ACC maintains a database that tracks all relevant relationships for ACC members and persons who participate in ACC activities, including those involved in the development of Expert Consensus Decision Pathways. Expert Consensus Decision Pathways follow ACC RWI Policy in determining what constitutes a relevant relationship, with additional vetting by the Solution Set Oversight Committee.
Expert Consensus Decision Pathway writing groups must be chaired or co-chaired by an individual with no relevant RWI. Although vice chairs and writing group members may have relevant RWI, they must constitute less than 50% of the writing group. Relevant disclosures for the writing group and comprehensive disclosures for external peer reviewers can be found in Appendixes 1 and 2. To ensure complete transparency, a comprehensive list of disclosure information for the writing group, including relationships not pertinent to this document, is available in a Supplemental Appendix. Writing committee members are discouraged from acquiring relevant RWI throughout the writing process and required to disclose any new relationships.
3. DEFINITIONS AND ASSUMPTIONS
To limit inconsistencies in interpretation and to develop guidance that is complementary to current evidence-based guidelines for the management of chest pain in the ED, specific definitions and assumptions were considered by the writing committee in the development of the consensus recommendations.
3.1. Definitions
hs-cTn assays: Assays for cardiac troponin (cTn) T or I that meet the following criteria: assay imprecision (ie, coefficient of variation [CV]) at the 99th percentile value ≤10%; and at least 50% of apparently healthy men and women have cTn concentrations above the assay’s limit of detection (LoD).7 However, not all assays designated as hs-cTn by the United States Food and Drug Administration (FDA) meet these measurement criteria, particularly in women.8
CDPs: These are structured protocols for evaluation of patients with suspected ACS using hs-cTn assays. They include serial measurements of hs-cTn at specific timepoints and are designed to allow safe disposition of low-risk patients with chest pain in an expedited and efficient manner.
Efficacy: In studies evaluating performance of CDPs, efficacy is defined as the proportion of individuals meeting “rule-out” criteria based on the CDP algorithm.
Limit of blank (LoB): This is the highest apparent cTn concentration found with a given assay when testing replicates of a sample known to contain no cTn (ie, blank sample).
LoD: This is the lowest cTn concentration that can be reliably distinguished from the LoB when testing replicates of samples known to contain cTn.
Limit of quantification (LoQ): This is the lowest cTn concentration that can be reported reliably as a number, based on a CV ≤20%, as per FDA regulations.
Minimally elevated hs-cTn or minor elevations in hs-cTn: hs-cTn values above the LoQ but below the 99th percentile upper reference limit (URL).
Elevated hs-cTn: hs-cTn values above the 99th percentile.
Relative change (Δ) in hs-cTn: the percentage change in hs-cTn across serial measurements. Relative changes ≥20% are considered significant and indicative of acute myocardial injury. However, at low troponin concentrations near the 99th percentile URL, absolute (rather than relative) change values provide greater specificity for acute myocardial injury.
Absolute change (Δ) in hs-cTn: The change in hs-cTn across serial measurements, reported as an absolute value in ng/L. At low hs-cTn concentrations near the 99th percentile URL, absolute rather than relative Δ should be used. Values are assay dependent. Recommended CDPs use absolute rather than relative Δ values.
Nonischemic electrocardiogram (ECG): ECGs that are normal, have nonspecific findings, left ventricular hypertrophy with or without repolarization abnormalities, left or right bundle branch block, or paced rhythm (not meeting Sgarbossa9 or Modified Sgarbossa10,11 criteria for myocardial infarction [MI]).
3.2. General Clinical Assumptions
The content of this Expert Consensus Decision Pathway applies only to patients presenting to the ED with chest pain or other symptoms suggestive of myocardial ischemia undergoing evaluation for possible ACS. The Expert Consensus Decision Pathway does not apply to patients with stable angina or those evaluated in settings other than the ED. For these other patient groups, the 2021 AHA/ACC/multisociety chest pain guideline provides comprehensive recommendations on chest pain evaluation and management not limited to the ED setting.5 This Expert Consensus Decision Pathway is not applicable to patients with hemodynamic instability, significant heart failure, or other conditions that would mandate hospital admission.
The document is focused on the rapid evaluation and disposition of patients with possible ACS in the ED. It does not address the evaluation and management of patients with definite ACS or to serve as a guide for the diagnosis or management of MI. Readers are referred to the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction (STEMI),12 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes (NSTE-ACS),13 and the Fourth Universal Definition of MI14 for comprehensive recommendations on these topics.
This Expert Consensus Decision Pathway is focused on CDPs using high-sensitivity cardiac troponin I (hs-cTnI) assays. The pathways are not appropriate for use with older-generation, less-sensitive assays. An important secondary objective of this document is to support the transition to hs-cTn assays, which offer important advantages for the rapid evaluation and disposition of chest pain in the ED and are recommended by the 2021 AHA/ACC/multisociety chest pain guideline.5 It is recommended that U.S. centers transition to hs-cTn assays for optimal patient care.
Recommendations regarding noninvasive testing should be considered in the context of availability of institutional testing and local expertise. However, coronary computed tomography angiography (CTA) is an important tool for evaluation of intermediate-risk patients in the ED, and thus, broader application across centers and greater availability within centers is recommended.
CDPs for rapid evaluation of chest pain should be interpreted within the context of all available clinical information. The provider’s clinical judgment at the bedside remains an indispensable tool that may lead to different triage decisions than those suggested by the CDP.
The rule-out cutpoints for high-sensitivity cardiac troponin T (hs-cTnT) and hs-cTnI assays recommended in this document may differ slightly from those reported in studies evaluating accelerated CDPs, because we have synthesized data across multiple studies and used concentration cutoffs permitted for reporting in the United States by the FDA. The CDPs included in this document use the LoQ (see definition in the previous text) permitted by the FDA for the 0-hour rule-out criterion.
The recommendations in this document are based on available data, much of which is observational rather than from randomized controlled trials. As new, relevant, and sound data become available, modifications to CDPs may be necessary.
Successful implementation of the CDPs outlined in this document requires engagement of a multidisciplinary team with collaboration among emergency medicine, laboratory medicine, cardiology, and hospital medicine specialties. Clinicians caring for patients in whom hs-cTn assays are used need to be aware of the clinical decision thresholds as well as the strengths and limitations of the CDP. Specific recommendations for transitioning to hs-cTn assays have been outlined previously.15
4. SUMMARY GRAPHIC
This Expert Consensus Decision Pathway is designed to parallel the usual course of evaluation of patients in the ED with symptoms requiring evaluation for possible ACS (see Figure 1). The first step is careful evaluation of the ECG (see Section 5.2). Patients with a nonischemic ECG can enter an accelerated CDP designed to provide rapid risk assessment and exclusion of ACS (see Section 5.4). Patients classified as low risk (rule out) using hs-cTn–based CDPs supported by this document can generally be discharged directly from the ED without additional testing, although outpatient testing may be considered in selected cases. In contrast, patients with substantially elevated initial hs-cTn values or those who have significant dynamic changes over 1 to 3 hours are assigned to the abnormal/high-risk category and should be further classified according to the Universal Definition of MI into type 1 or 2 MI or acute or chronic nonischemic cardiac injury (see Section 5.7). High-risk patients should usually be admitted to an inpatient setting for further evaluation and treatment. Patients determined to be intermediate risk with the CDP should undergo additional observation with repeat hs-cTn measurements at 3 to 6 hours and risk assessment using either the modified History, ECG, Age, Risk Factors, and Troponin (HEART) score or the ED Assessment of Chest Pain Score (EDACS) (see Section 5.5). Noninvasive testing should be considered for the intermediate-risk group unless low-risk features are identified using risk scores or noninvasive testing has been performed recently with normal or low-risk findings. Details of the assessment steps are provided in Section 5.
FIGURE 1. Pathway Summary Graphic.
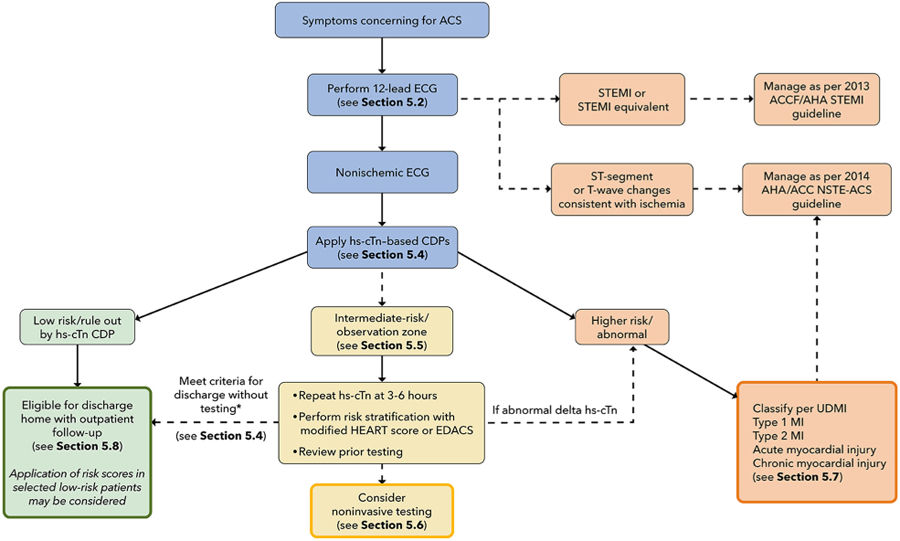
*Unchanged high-sensitivity troponin concentration (ie, no or minimal change over serial measurements) with 1) recent normal testing (ie, invasive or CT coronary angiogram <2 years ago or stress test <1 year ago); 2) symptoms inconsistent with possible ACS; 3) chronic elevations in hs-cTn that are unchanged compared with levels measured previously; or 4) a modified HEART score ≤3 or EDACS <16.
ACC = American College Cardiology; ACS = acute coronary syndrome; AHA = American Heart Association; CDP = clinical decision pathway; ECG = electrocardiogram; EDACS = Emergency Department Assessment of Chest Pain Score; HEART = History, ECG, Age, Risk Factors, and Troponin; hs-cTn = high-sensitivity cardiac troponin; MI = myocardial infarction; NSTE-ACS = non-ST-segment elevation acute coronary syndrome; STEMI = ST-segment elevation myocardial infarction; UDMI = Universal Definition of MI.
5. DESCRIPTION AND RATIONALE
5.1. Initial Evaluation
The initial clinical evaluation of a patient with acute chest pain should focus on rapid identification and treatment of patients with life-threatening conditions such as ACS, aortic dissection, and pulmonary embolism. Patients who are hemodynamically unstable, have significant arrhythmias, or have evidence of significant heart failure should be evaluated and treated appropriately and are not candidates for an accelerated CDP.
Although the term chest discomfort is more accurate, the term chest pain is embedded in clinical use and will be used throughout this document to describe potential ischemic chest symptoms. Symptoms described as a pressure, tightness, squeezing, heaviness, or burning should be considered consistent with ACS. Pain locations other than the chest can also occur and include the shoulder, arm, neck, back, upper abdomen, or jaw. Other associated symptoms include shortness of breath, nausea, vomiting, diaphoresis, fatigue, and mental status changes, which, in some cases, may be the predominant symptom. In contrast, symptoms described as sharp, fleeting, related to inspiration (pleuritic) or position, or localized to a single point are unlikely to represent myocardial ischemia.
Chest pain has been traditionally classified as “typical” or “atypical.” The 2021 AHA/ACC/multisociety chest pain guideline discourages the use of the term atypical chest pain and instead emphasizes focusing on specific aspects that suggest whether the pain is likely related to ischemia. The guideline also recommends using cardiac, possible cardiac, and noncardiac to describe the suspected cause of chest pain.5 Chest pain should be considered stable when symptoms are chronic and associated with precipitants such as exertion or emotional stress.
Clinical assessment should include the chest pain description and associated symptoms, onset, duration, location, radiation, and precipitating and relieving factors. In addition, a detailed assessment of cardiovascular risk factors and medical, family, and social history should complement the assessment of presenting symptoms. The results of prior testing for coronary artery disease (CAD) as well as prior computed tomography (CT) imaging of the chest that delineates the presence and severity of coronary calcification should be reviewed, as it may inform subsequent diagnostic testing strategies.
There are no physical examination findings specific for coronary ischemia; thus, the examination should be targeted to identify findings associated with high risk for morbidity and mortality in ACS, or to the presence of potential alternative diagnoses. High-risk examination findings include signs of low cardiac output (tachycardia, hypotension, cool extremities, low urine output, and altered mental status), heart failure (pulmonary edema, elevated jugular venous pressure, and peripheral edema), and a new systolic murmur concerning for acute mitral regurgitation or a ventricular septal defect. Clues to non-ACS causes for the patient’s symptoms include fever (endocarditis, pneumonia), pulse differential (aortic dissection), abnormal lung findings (pneumonia, pneumothorax), and abnormal cardiac findings such as a pericardial friction rub (pericarditis) or other murmurs (aortic stenosis, outflow tract obstruction, endocarditis).
As part of the initial assessment, a chest X-ray should be performed in almost all patients with possible ACS, given the potential to identify high-risk findings such as pulmonary edema, as well as to identify potential noncardiac causes for the patient’s symptoms. Performance of a chest X-ray should not delay emergent interventions such as primary percutaneous coronary intervention for those with a definitive STEMI.
5.2. Initial Evaluation: Focus on ECG
5.2.1. Initial ECG Interpretation
The ECG is critical for the initial assessment and management of patients with potential ACS and therefore should be performed and interpreted within 10 minutes of arrival at the ED.5,12,13 In patients who arrive via emergency medical service transport, the pre-hospital ECG should be reviewed, because ischemic changes may have resolved before ED arrival. In the ED, the initial ECG should be examined for signs of ischemia (see Figure 2), particularly for STEMI or a STEMI equivalent (see Table 1), as this identifies patients who should undergo immediate reperfusion therapy and be managed in accordance with the 2013 STEMI guideline.12 Automated ECG algorithms provide an immediate interpretation and diagnostic assistance, particularly for the inexperienced ECG reader, and may identify subtle ECG changes that just meet STEMI criteria, particularly with inferior ST-segment elevation. However, interpretation accuracy varies among different algorithms, with up to a 2-fold variation in identification of ECGs concerning for ACS.16 Unfortunately, physician accuracy for determining ischemic ECG changes is also variable, with lower sensitivity for smaller degrees of ST-segment elevation.17
FIGURE 2. Initial ECG Assessment.
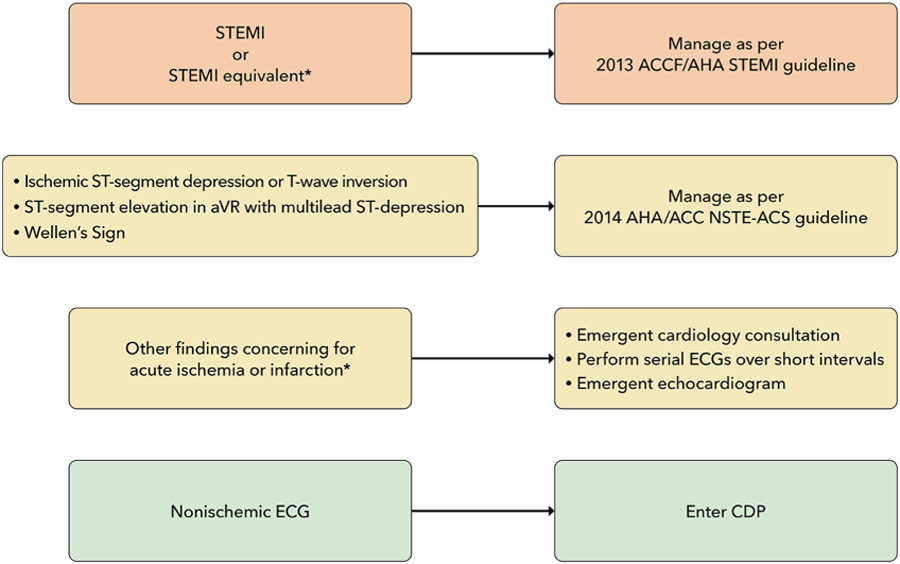
*See Table 1 for ECG findings of STEMI equivalent and findings consistent with ischemia or infarction.
ACC = American College of Cardiology; AHA = American Heart Association; aVR = augmented vector right; CDP = clinical decision pathway; ECG = electrocardiogram; NSTE-ACS = non–ST-segment elevation acute coronary syndrome; STEMI = ST-segment elevation myocardial infarction.
TABLE 1.
Electrocardiogram Findings Suggestive of Ischemia
| FINDING | CRITERIA |
|---|---|
| STEMI equivalents | |
| Posterior STEMI |
Criteria:
|
| Left bundle branch block or ventricular paced rhythm with Sgarbossa Criteria | A total score ≥3 points is required:
|
| Left bundle branch block or ventricular paced rhythm with Smith-modified Sgarbossa Criteria | Positive if any of the following are present:
|
| De Winter Sign |
|
| Hyperacute T waves | Broad, asymmetric, peaked T waves may be seen early in STEMI Serial ECGs over very short intervals are useful to assess for progression to STEMI |
| ECG findings consistent with acute/subacute myocardial ischemia | |
| aVR ST-segment elevation | Most often caused by diffuse subendocardial ischemia and usually occurs in the setting of significant left main coronary artery or multivessel coronary artery disease
|
| ST-segment depression | Horizontal or downsloping ST-segment depression ≥0.5 mm at the J-point in 2 or more contiguous leads is suggestive of myocardial ischemia |
| Wellen’s syndrome | Clinical syndrome characterized by:
|
| Inverted T waves | May be seen in ischemia (subacute) or infarction (may be fixed and associated with Q waves) in continuous leads |
V7 placed at left posterior axillary line in same plane as V6; V8 placed at the tip of the left scapula; V9 placed in the left paraspinal region in the same plane as V6. aVR = augmented vector right; ECG = electrocardiogram; STEMI = ST-elevation myocardial infarction.
In the absence of ischemic ST-segment elevation, the ECG should be examined for other changes that have been associated with coronary artery occlusion (see Table 1)18–21; when present, these should prompt evaluation for emergent coronary angiography.
For patients suspected of ACS who have ST-segment or T-wave changes suggestive of ischemia, comparison with previous ECGs can be helpful.22 Emergent consultation for expert over-read should be obtained for ECGs concerning for ACS that lack clear diagnostic criteria. Serial ECGs performed over short time intervals in those with a high suspicion for ACS may detect dynamic ischemic changes.23,24 ECGs performed later, even the next day, may show evolution of findings that confirm the diagnosis, such as Q waves or new T-wave inversions. A posterior ECG should be performed if the initial ECG is nondiagnostic but suspicion for a posterior MI is high (see Section 5.2.2 and Table 1). Emergent transthoracic echocardiography (TTE) for assessment of wall motion should be considered in patients with ECGs concerning for but not diagnostic of ischemia and infarction, particularly when borderline ST-segment elevation or left bundle branch block (LBBB) or equivocal signs of posterior MI are present. Because accurate assessment of wall motion is difficult, the TTE should be performed and reviewed by a clinician qualified in echocardiography (see Section 5.6).
Finally, the ECG should be reviewed for other findings suggesting alternative causes for the patient’s symptoms, such as pericarditis or pulmonary embolism. The absence of ischemic ECG changes identifies patients at relatively lower (although not necessarily low) risk for MI and ischemic complications but is not sufficient for excluding ACS25,26; therefore, these patients are appropriate for evaluating using a CDP.
All CDPs (see Section 5.4) exclude patients with ischemic ST-segment elevation; however, many do not specifically exclude those with other ECG findings potentially associated with ischemia.27 We recommend that patients with new ischemic ECG changes should be considered high risk and undergo evaluation and treatment according to current NSTE-ACS guidelines13 and not be entered into an accelerated CDP. For the purposes of this document, ECGs are classified into 3 groups: 1) STEMI or equivalent; 2) ischemic ST-segment or T-wave abnormalities; and 3) nonischemic, which includes ECGs interpreted as normal, having nonspecific findings, left ventricular hypertrophy with or without repolarization ST-T wave changes, and left or right bundle branch block or paced rhythm (not meeting Sgarbossa9 or modified Sgarbossa10,11 criteria for MI).
5.2.2. Additional ECG Findings Consistent With Acute Coronary Artery Occlusion
The application of STEMI ECG criteria on a standard 12-lead ECG alone will miss a significant minority of patients who have acute coronary occlusion.21 Therefore, the ECG should be closely examined for subtle changes that may represent initial ECG signs of vessel occlusion, such as hyperacute T waves (in the absence of electrolyte imbalances or significant left ventricular hypertrophy) or ST-segment elevation <1 mm, particularly when combined with reciprocal ST-segment depression, as this may represent abnormal coronary blood flow and/or vessel occlusion.21 Concomitant reciprocal ST-segment depression may be visually more evident than the minor ST-segment elevation in such patients.28 If present, these patients should be evaluated for emergent coronary angiography as their outcomes are similar to those with more extensive ST-segment elevation.29
Other ECG findings may also indicate acute coronary artery occlusion. Anterior ST-segment depression (eg, leads V1-V3) may represent acute posterior transmural MI.19 Acute posterior MI can be confirmed by evaluating for the presence of ST-segment elevation on posterior leads19 or emergent echocardiography demonstrating wall motion abnormalities in the posterior and/or inferior territories. Emergent coronary angiography should be performed when there is a high suspicion for acute posterior MI, because delay in reperfusion has been associated with worse outcomes.30 Similarly, de Winter’s sign, suggested by tall, prominent, symmetrical T waves arising from upsloping ST-segment depressions >1 mm in the precordial leads, can be seen in proximal left anterior descending artery occlusion and therefore warrants immediate angiography.18
The identification of acute coronary occlusion among patients with LBBB or ventricular pacing poses particular challenges. The presence of a new LBBB is no longer considered a STEMI equivalent,12 although it is associated with higher risk because most patients with LBBB have underlying cardiac disease, typically CAD or a cardiomyopathy.31 The Sgarbossa criteria (see Table 1) are specific, although not sensitive for acute coronary artery occlusion.9 In a study that included patients with acute left anterior descending artery occlusion, a modification that used an ST/T-wave ratio improved sensitivity from 52% to 91% with similar specificity to the original criteria.10,11 For those meeting the Sgarbossa or modified Sgarbossa criteria, treatment should be similar to those with STEMI. Emergent echocardiography can be performed in cases in which there is an LBBB and suspicion for ischemia/infarction with the caveat that the frequent coexistent cardiomyopathy may make differentiation difficult. Although less well studied, patients with ventricular paced rhythms who have ECG findings that meet Sgarbossa criteria should also be considered high risk and undergo emergent coronary angiography.9,32
5.2.3. ECG Findings Consistent With Ischemia
Wellen’s syndrome is characterized by biphasic or inverted T-wave inversions in the anterior precordial leads in patients whose ischemia has resolved.33 Its presence is associated with proximal left anterior descending artery stenosis and is associated with high rate of subsequent transmural MI.
In patients with ischemic symptoms, ST-segment elevation in lead augmented vector right (with or without elevation in V1) combined with multilead ST-segment depression represents a high-risk ECG finding that is associated with high morbidity and mortality.34 In patients with ischemic symptoms, this often represents diffuse ischemia due to significant stenosis involving the left main and/or 3-vessel disease,35,36 although it can be seen in other non-ACS conditions causing a demand/supply mismatch.37 In approximately 10% of cases, acute coronary occlusion is present.35 Accordingly, management of patients with this ECG pattern must be nuanced. Precipitants of supply/demand mismatch (if present) should be treated. Emergent coronary angiography should be considered in patients with persistent ischemic symptoms or ECG changes after treatment or if there is hemodynamic instability.35
Ischemic ST-segment depression is present in a minority of ACS patients, representing a specific, but not sensitive finding for ACS. In the setting of ischemic symptoms, it should prompt treatment consistent with the 2014 NSTE-ACS guidelines,13 as the majority of patients with ischemic ST-segment depression will be diagnosed with MI.38 T-wave inversion is a less-specific marker of subendocardial ischemia because it can be present in non-ACS conditions. Rather than being indicative of acute ischemia, T-wave inversion can become evident after clinical ischemia resolves. Ischemic T-wave inversion tends to be deeper and new when compared with prior ECGs.
5.2.4. Summary
The ECG is a critical component of the initial assessment and management of ED patients with possible ACS. The ECG should be rapidly assessed for evidence of acute infarction or ischemia, and if present, subsequent care should follow current guidelines for management of acute STEMI12 and NSTE-ACS.13 The ECG should also be examined for subtle changes that are also consistent with ACS as well as for other findings that could suggest a non-ACS cause for their symptoms. Patients who have a nonischemic ECG (as defined previously) are eligible for entering a CDP, and further clinical evaluation should take place as outlined later.
5.3. Hs-cTn Assays
Measurement of cardiac troponin T (cTnT) or cardiac troponin I (cTnI), the gold-standard biomarkers of myocardial injury, is critical for the evaluation of possible ACS in the ED. In the United States, hs-cTn assays are being increasingly adopted because of their ability to detect lower cTn concentrations with improved analytical performance (ie, greater sensitivity and precision) compared with older-generation assays.15 “High sensitivity” in this context refers to assay characteristics; the analytes being measured (cTnT and cTnI) are the same as for older-generation, conventional assays. Accordingly, hs-cTn assays are preferred to conventional assays for the evaluation of acute chest pain.5,6 The “high-sensitivity” designation was initially adopted by cTn assay manufacturers in the absence of clear analytical criteria defining high sensitivity. The International Federation of Clinical Chemistry and Laboratory Medicine Task Force on Clinical Applications of Cardiac Biomarkers lists 2 criteria to define “true” hs-cTn assays: first, the assay imprecision (ie, CV) at the 99th percentile value for that assay should be ≤10%; and second, at least 50% of apparently healthy men and women7 should have cTn concentrations above the assay’s LoD.39 Most manufacturers now voluntarily report assay characteristics according to these criteria (see Table A in the Supplemental Appendix). Of note, point-of-care cTn assays must also meet these criteria to be considered high-sensitivity assays.
When considering assay characteristics, it is important to understand the terminology commonly used both in product inserts and in the literature. The LoB is the highest apparent cTn concentration found with a given assay when testing replicates of a sample known to contain no cTn (ie, blank sample). The LoD is the lowest cTn concentration that can be reliably distinguished from the LoB when testing replicates of samples known to contain cTn. In research settings, the term undetectable troponin is typically used for cTn concentrations that are below the LoD of the assay. The LoQ is the lowest cTn concentration that can be reported reliably as a number, either with a CV ≤20% (as per FDA regulations), or with a more stringent CV ≤10%. Analytical definitions are summarized in Figure A of the Supplemental Appendix.15 In clinical settings, the FDA only allows cTn concentrations to be reported numerically if they are equal to or above the LoQ; therefore, cTn concentrations above the LoD but below the LoQ are not reported in U.S. clinical settings. This has implications for algorithms that use a single hs-cTn measurement at ED arrival to exclude MI. For example, for hs-cTnT, the lowest value that the FDA allows to be reported is 6 ng/L, although the LoD is 3 to 5 ng/L depending on the specific analyzer used. It is therefore important to interpret the term undetectable troponin in context for each hs-cTn assay and for each usage scenario.
Concentrations of hs-cTn should be reported in whole numbers without decimal places as nanograms per liter (ng/L), as recommended by the International Federation of Clinical Chemistry and Laboratory Medicine, endorsed in the Fourth Universal Definition of MI,14,39 and adhered to by assay manufacturers. Reporting in ng/L avoids potential confusion related to the use of 3 decimal places and multiple zeroes (for instance, 14 ng/L is preferred over 0.014 ng/mL).
5.3.1. Defining Abnormal Hs-cTn Values
Key questions for the management of patients with possible ACS in the ED are what constitutes an “abnormal” or an “elevated” hs-cTn value and how to rapidly and reliably differentiate between ACS and the multitude of other potential causes for cTn elevation (see Section 5.7).40 In the absence of an objective cTn threshold, the 99th percentile URL cTn value derived from a “normal reference population” has been endorsed by expert consensus as a cutpoint for the diagnosis of MI for more than 20 years.41 However, studies in large population-based cohorts have shown that hs-cTn represents a continuum of risk, such that minor cTn elevations (detectable but below the 99th percentile URL) are associated with structural heart disease, worse cardiovascular outcomes, and increased mortality.42–44 Similar to population-based studies, minor hs-cTn elevations are also associated with worse outcomes in ED patients who are ruled out for MI.27,45 Based on these findings, no detectable cTn level can be considered entirely “normal.” The higher the cTn value, the more likely it is related to ACS,46–48 although there is significant overlap among cTn values for type 1 and 2 MI and acute myocardial injury. As a result, hs-cTn values still require interpretation based on the appropriate clinical context. Serial hs-cTn measurements should be performed to confirm the MI diagnosis, and peak values can be used to estimate MI size.49
False-positive and -negative hs-cTn assay results are rare but can occur. False-positive values may be secondary to sample preparation and handling, instrument malfunction, assay interference, and macro troponin complexes.50,51 Although rare, clinicians should be aware that false-negative values can occur as a result of assay interference from ingested substances such as biotin.50 Close collaboration between laboratory medicine professionals and clinicians is necessary to troubleshoot suspected false-positive or -negative values.
5.3.2. 99th Percentile Thresholds
The 2018 Fourth Universal Definition of MI defined biomarker evidence of acute myocardial injury as an acute rise and/or fall in cTn values (≥20% change between serial measurements), with at least 1 cTn value above the assay’s 99th percentile URL.14 Although this definition has undeniable merits, it also has important limitations when applied to the acute evaluation of ED patients with possible MI. First, the ≥20% change criterion is based on expert consensus. Using absolute rather than relative changes in cTn results in better diagnostic performance among patients with smaller cTn elevations near the 99th percentile value (in whom the diagnosis of MI is often most difficult). In contrast, relative cTn changes may be more useful for patients with higher cTn levels.14,52 Second, 99th percentile URLs for hs-cTn assays are derived by manufacturers from “normal reference populations.” However, the methodology used to select reference populations varies across studies, and the 99th percentile URLs for some hs-cTn assays may change significantly with only slight modifications in the reference population (such as removal of 1 or 2 subjects with high cTn levels).53 Third, hs-cTn levels vary significantly with sex and age, even among healthy individuals, in addition to increasing with the presence of comorbidities.8,54,55 Troponin levels are higher in men than in women and increase with age in both sexes, even after excluding individuals with subclinical structural heart disease using a combination of ECGs, imaging tests, and established biomarkers.54
This latter limitation has spurred active debate about the appropriateness of uniform 99th percentile URLs for hs-cTn assays, with endorsement of sex-specific 99th percentile cutoffs in the 2018 Fourth Universal Definition of MI14 and the 2021 AHA/ACC/multisociety chest pain guideline,5 but notably absent from the 2020 European Society of Cardiology (ESC) guidelines.6 Use of uniform 99th percentile URLs results in decreased sensitivity and negative predictive value (NPV) in women, contributing to the existing sex bias in the diagnosis and treatment of women with possible ACS.56,57 Use of sex-specific cutoffs can decrease the problem of MI underdiagnosis in women.58,59
Using sex-specific 99th percentile thresholds only addresses a single determinant of cTn variation in the population and does not account for other important factors that influence the 99th percentile threshold, such as age and renal function.60 Moreover, a focus on the 99th percentile threshold does not capitalize on analytical advances with hs-cTn assays that allow the use of very low values for risk stratification. Newer MI rule-out algorithms have been developed that either de-emphasize or avoid altogether the use of 99th percentile URLs (see Section 5.4).
5.3.3. Summary
Hs-cTnT and hs-cTnI are the preferred biomarkers for the evaluation of patients with possible ACS. In U.S. clinical settings, concentrations are reported when at or above the LoQ; concentrations should be reported as whole numbers in nanograms per liter (ng/L). Detectable values represent a continuum of risk for adverse events; thus, no detectable cTn level can be considered “normal.” Sex-specific 99th percentile cutoffs are endorsed to increase sensitivity for diagnosis of MI among women and specificity among men.
5.4. CDPs Using Hs-cTn Assays
Hs-cTn assays have several intrinsic advantages that have facilitated the development of novel accelerated CDPs designed to shorten the time to exclude (“rule out”) MI. Compared with older-generation assays, hs-cTn assays are both more sensitive and more precise. Increased sensitivity allows exclusion of even minor cTn elevations, permitting rule out of MI with a single blood draw when the hs-cTn value is very low and symptoms have been present for 3 hours or more. Assay precision is particularly important when assessing change over serial measurements at low values. Augmented precision of the hs-cTn assays allows biological changes to be distinguished from assay imprecision (ie, noise). This feature has been capitalized on by algorithms that use the absence of small changes in hs-cTn over 1 to 2 hours to exclude (“rule out”) MI.
Multiple diagnostic algorithms incorporating hs-cTn have been investigated and implemented. Strengths and weaknesses of several of these approaches are shown in Table 2. The simplest algorithm is conceptually very similar to approaches used in many hospitals with older-generation assays, ruling out patients with an hs-cTn level below the 99th percentile value at 0 and 3 hours, with or without sex-specific 99th percentile URL cutpoints.62 Although this 0/3-hour approach has the advantage of ease of implementation, it fails to capitalize on the advantages of the hs-cTn assays and suffers from all of the limitations of emphasizing the 99th percentile URL value discussed in Section 5.3. More importantly, comparison studies and a recent meta-analysis63 (discussed later) demonstrate that the 0/3-hour approach is inferior to the more innovative 0/1, 0/2, and High-Sensitivity Troponin in the Evaluation of Patients with Acute Coronary Syndrome (High-STEACS) approaches, ruling out a smaller proportion of patients and suffering from higher false-positive diagnosis rates. For this reason, the 0/3-hour approach is not recommended.
TABLE 2.
Clinical Decision Pathways With Hs-cTn
| Approach | Criteria for Rule Out | Advantages | Disadvantages |
|---|---|---|---|
| 0/3 h | Single hs-cTn <99th percentile URL if symptoms >6 h and now pain free OR If <6 h of symptoms, 0- and 3-h troponin less than the 99th percentile URL |
|
|
| 0-h (single draw) | 0-h rule out for cTn below LoQ or an optimized cutoff (eg, hs-cTnI <5 ng/L) |
|
|
| 0/1-h rule out | Use baseline (0-h) and delta values at 1 h to assign patients to the rule-out, observation, or abnormal groups |
|
|
| 0/2-h rule out | Identical approach to 0/1-h rule out except delta assessed at 2 h |
|
|
| High-STEACS | MI is ruled out if initial hs-cTnI <5 ng/L or hs-cTnT <6 ng/L (if >3 h from symptom onset) or if change from initial to 3-h hs-cTn is <3 ng/L and remains below sex-specific 99th percentile URL |
|
|
ED = emergency department; High-STEACS = High-Sensitivity Troponin in the Evaluation of Patients with Acute Coronary Syndrome; hs-cTn = high-sensitivity cardiac troponin; hs-cTnI = high-sensitivity cardiac troponin I; hs-cTnT = high-sensitivity cardiac troponin T; LoQ = limit of quantification; MI = myocardial infarction; NPV = negative predictive value; RCT = randomized controlled trial; URL = upper reference limit.
5.4.1. Ruling Out MI With a Single Blood Draw at the Time of Presentation (0-Hour Rule Out)
Immediate disposition of approximately 25% to 50% of chest pain patients is possible in those who have a single undetectable or very low hs-cTn value, provided symptoms started ≥3 hours before the hs-cTn measurement (“0-hour rule out”). This approach is not suitable for early presenters who have symptom onset <3 hours before presentation. Extensive observational data support the safety of this approach, with a high NPV and sensitivity for excluding index MI, and a <1% risk for death or MI through 30 days observed with both hs-cTnT and hs-cTnI.27,64–67 In addition, randomized clinical trials in which this strategy has been used to guide actual patient care support the safety of this approach.61,68
The threshold value used to define the very low hs-cTn cutpoint has varied. Initial studies examined the use of the LoD as a cutoff for single hs-cTn rule out. However, because the FDA does not allow reporting to the LoD unless it is the same as the LoQ (which is not the case for most FDA-approved hs-cTn assays), alternative cutoffs for single hs-cTn rule-out strategies have been investigated.67 These include using the LoQ or an optimized cutoff above the LoQ. For hs-cTnI, a threshold of <5 ng/L has been validated in a randomized controlled trial and performed well across multiple different hs-cTnI assays in observational studies.61,69–71 In a meta-analysis of 22,457 patients from 19 studies, hs-cTnI <5 ng/L at presentation (which was present in 49% of patients) had 99.5% (95% CI: 99.3%–99.6%) NPV for 30-day death or MI.27 For hs-cTnT, several observational studies using the LoQ (6 ng/L) have demonstrated excellent sensitivity and NPV, supporting use of the 6-ng/L hs-cTnT threshold for U.S. centers.72,73 Thus, a 0-hour rule-out threshold of <6 ng/L for hs-cTnT and either <LoQ or <5 ng/L for hs-cTnI is reasonable in patients with a nonischemic ECG and onset of symptoms ≥3 hours before cTn measurement.
5.4.1.1. Criterion for Duration of Chest Pain for 0-Hour Rule-Out
Although some studies have used a 2-hour cutoff for chest pain onset before initial blood sampling for a single hs-cTn rule out,74,75 others have required a minimum of at least 3 hours.64,76–80 We recommend the more conservative 3-hour criterion. Determination of the exact time of symptom onset is frequently difficult. In addition, studies performed to date have commonly used time of chest pain onset to ED presentation, which is often shorter than the time from chest pain onset to the initial cTn sample. Finally, the 3-hour timepoint is in alignment with the 2021 AHA/ACC/multisociety chest pain guideline.5
5.4.1.2. Criterion for ECG Findings to Allow Entry Into CDP
For inclusion in a CDP, we recommend that the patient have a nonischemic 12-lead ECG. Although not all studies have explicitly required this, in a metanalysis of studies using a single hs-cTn at the time of ED arrival to exclude MI, the NPV was lower at 98.2% in patients who had ischemic findings on the initial ECG, compared with 99.7% in those without ECG abnormalities.27
5.4.2. 0/1- and 0/2-Hour Algorithms
Reichlin et al77 developed an algorithm incorporating both baseline hs-cTnT values and changes in hs-cTnT between 0 and 1 hour to assign patients to rule out, rule in, or observation zones. This approach has been replicated with multiple hs-cTnI assays and externally validated.76,78–80 This algorithm has been combined with the 0-hour rule out described previously, such that patients may be ruled out either by having a very low hs-cTn at baseline (if chest pain onset is ≥3 hours) or by having values below a specified threshold and no more than a very small change (”delta”) between the serial measurements (see Figure 3). This combined 0- and 0/1-hour pathway has been labeled the “ESC 0/1 algorithm.” Options are also available for 0/2-hour algorithms that are conceptually identical but may be logistically easier to implement in EDs that cannot consistently capture a second hs-cTn value 60 minutes after the first measurement (see Figure B in the Supplemental Appendix for 0/2-hour CDPs for ruling out MI). Because the change thresholds for the 0/1 and 0/2 algorithms are time-dependent, it is critical that the blood specimens are collected within the specified windows, and accurate timing of specimen collection should be a performance metric that is tracked by health care systems using CDPs. Specimens collected outside of the specific time window should be interpreted with consideration of the actual time the specimen was collected. Importantly, thresholds tested are assay-specific (see Figure 3 and Figure B in the Supplemental Appendix). Although the vast majority of studies evaluating the 0/1- and 0/2-hour protocols have been observational, several prospective studies and randomized trials where the 0/1-hour protocol has been used for patient care have found a 30-day death/MI rate of <1%.68,86,87
FIGURE 3. Modified European Society of Cardiology 0/1-Hour CDP for Ruling Out MI.
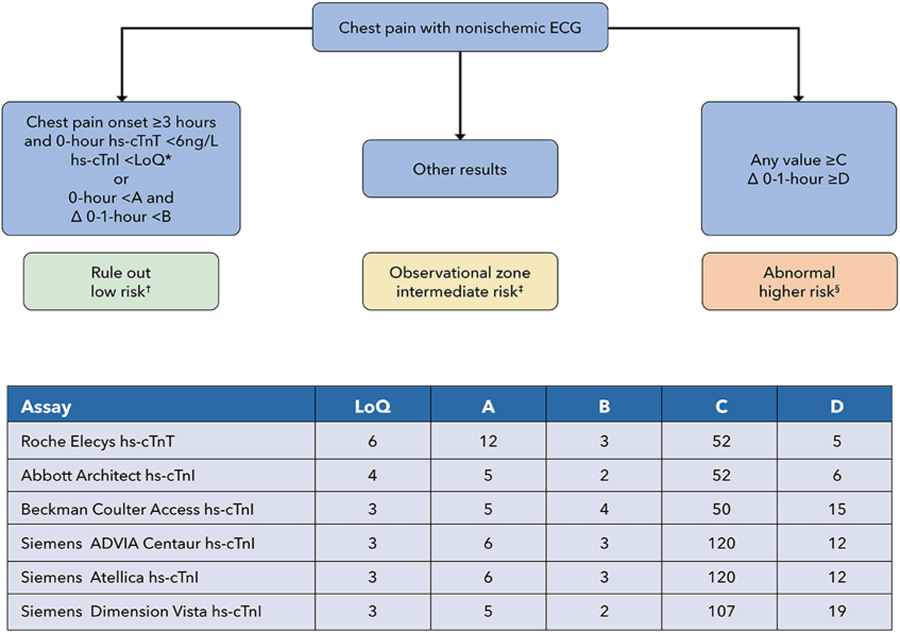
Sources for this Figure: 65,71,77–79,81–85
Note that variations of these rapid CDPs have been implemented in different centers, and modification of the algorithms shown may be considered based on local considerations. All values in the chart in are ng/L. *The LoQ may differ slightly from the 0-hour rule-out threshold tested in individual studies. Using a cutoff of <5 ng/L can also be considered instead of the LoQ for the 0-hour rule-out threshold for hs-cTnI assays. †See Sections 5.6 and 5.8 for recommendations on follow-up and testing. ‡See Section 5.5.3. Additional evaluation should include at least one additional observation with hs-cTn measurement at 3–6 hours, with classification of myocardial injury, as described in Section 5.7, into chronic myocardial injury, acute myocardial injury, type 1 MI, and type 2 MI, as per the Universal Definition of Myocardial Infarction. §Patients with acute MI should be managed according to standard practice guidelines.
CDP = clinical decision pathway; ECG = electrocardiogram; hs-cTnI= high-sensitivity cardiac troponin I; hs-cTnT = high-sensitivity cardiac troponin T; LoQ = limit of quantification; MI = myocardial infarction.
Efficacy with these algorithms is typically defined as the proportion of patients ruled out for MI, with safety defined by sensitivity and NPV for MI diagnosis at the index presentation and freedom from death/MI at 30 days. Efficacy with the 0/1- and 0/2-hour algorithms is approximately 60%, with some variation due to different assay thresholds and populations tested. Safety is high, with sensitivities of ~99% and NPVs >99.5% for MI at the index admission demonstrated in a meta-analysis.88 These protocols rule out approximately 60% to 65% of individuals, “rule in” ~15% of individuals, and assign ~25% to 30% to an intermediate-risk/observation zone (see Section 5.5). Direct comparisons with the 0/3-hour hs-cTn protocol demonstrate that the 0/1-hour protocol rules out more patients (64% vs 49%; P < 0.001) with a similar safety profile.89 In a randomized controlled trial using hs-cTnT, an ESC 0/1-hour algorithm resulted in more frequent discharge from the ED (45% vs 32%; P < 0.001) and a 1-hour shorter ED length of stay (P < 0.001), with similar clinical outcomes at 30 days (P = 0.001 for noninferiority) compared with a modified usual care approach using 0/3-hour cTn measurements with an hs-cTnT threshold of ≥30 ng/L.68
In initial studies, the positive predictive value (PPV) for those assigned to the rule-in group was approximately 75%,77 higher than the 50% PPV seen when the 99th percentile threshold was used for rule-in.90 However, the rate of MI in the European cohorts where the algorithms were developed was high (>15%). When similar approaches have been applied to U.S. populations where cTn testing is used more liberally, the proportion with adjudicated MI is much smaller (in some centers <5%), and thus the PPV of these algorithms has been considerably lower, ranging from 20% to 50% in less-selected populations of ED patients. In contrast, the PPV was approximately 70% in a U.S. study that enrolled patients more carefully selected based on a higher probability of ACS, and also incorporated a higher “rule-in” cTn threshold of 120 ng/L.85
Given the low PPV for MI when these CDPs are used broadly (as is typical for U.S. EDs), we recommend avoiding the term rule in for these algorithms and instead classifying this group as “abnormal.” The term rule in should be reserved for the subset of patients in the abnormal group meeting Universal Definition of MI criteria for MI (see Section 5.7).14
The ESC 0/1- or 0/2-hour algorithms take advantage of the better sensitivity and precision of the assay to safely rule out a majority of patients presenting with possible ACS and avoid the issues inherent with differing 99th percentile thresholds, including sex and age influences. Although efficacy (the proportion of patients ruled out) differs across multiple subgroups, with lower proportions of men, the elderly, and those with diabetes or chronic kidney disease ruled out, safety remains high in all subgroups.91–93
Disadvantages of these protocols include algorithm complexity, sensitivity to timing of blood draws, and the relegation of approximately one-quarter of patients to an observation zone in which there is limited evidence available to guide subsequent evaluation and treatment (see Section 5.5.3 and Table 3). A modification of the 0/1-hour protocol has been proposed, adding a 3-hour measurement of hs-cTn for those in the observation zone and classifying all patients at 3 hours into rule out or abnormal based on hs-cTn changes through 3 hours,94,95 although a recent study has questioned whether this provides a sufficiently high NPV.96
TABLE 3.
Modified HEART Scores and EDACS Data Components
| HEART Score Components Low risk: 0–3 points; non–low risk: ≥4 points |
EDACS Components Low risk: 0–15 points; non–low risk: ≥16 points |
||
|---|---|---|---|
| History | Age, y | ||
| High suspicion | 2 | 18–45 | 2 |
| Moderate suspicion | 1 | 46–50 | 4 |
| Low suspicion | 0 | 51–55 | 6 |
| Electrocardiogram | 56–60 | 8 | |
| ST-segment deviation | 2 | 61–65 | 10 |
| Paced, LBBB, RBBB, or LVH | 1 | 66–70 | 12 |
| Normal or nonspecific changes | 0 | 71–75 | 14 |
| Age, y | 76–80 | 16 | |
| >65 | 2 | 81–85 | 18 |
| 45–65 | 1 | 86+ | 20 |
| <45 | 0 | Male sex | 6 |
| Cardiac risk factors | Age 18–15 and either ≥3 cardiac | 4 | |
| ≥3 or known CAD | 2 | Diaphoresis | 3 |
| 1–2 | 1 | Pain radiating to arm or shoulder | 5 |
| 0 | 0 | Pain worsened with inspiration | −4 |
| Pain reproduced by palpation | −6 | ||
CAD = coronary artery disease; EDACS = Emergency Department Assessment of Chest Pain; HEART = History, ECG, Age, Risk Factors, and Troponin; LBBB = left bundle branch block; LVH = left ventricular hypertrophy; RBBB = right bundle branch block.
An additional limitation of these algorithms is that they may be susceptible to missing MI among late presenters who are on a flat portion of a descending cTn trend, where little or no change may be evident over 1 to 2 hours.97 Identification of these patients requires correlation of the clinical presentation with hs-cTn results and consideration for additional serial hs-cTn measurements.
5.4.3. High-STEACS 0/3-Hour Algorithm
The High-STEACS algorithm (see Figure 4) is another validated implementation approach for hs-cTn. With this algorithm, MI is ruled out if the initial hs-cTnI is <5 ng/L; if hs-cTnI is ≥5 ng/L (or the patient is an early presenter) but hs-cTnI is less than the sex-specific 99th percentile URL, a second hs-cTnI measurement is performed 3 hours from the time of presentation. If the change from the first measurement is <3 ng/L and the value remains below the sex-specific 99th percentile URL, MI is ruled out. Although early presenters may be defined as those presenting within 2 hours of chest pain onset, we recommend using the more conservative 3-hour criterion for the time from chest pain onset, as described earlier. The High-STEACS algorithm was studied in a stepped-wedge randomized implementation trial in the EDs of 7 hospitals in Scotland (N = 31,492 individuals).61 Implementation of the pathway was associated with a reduction in length of stay from 10.1 ± 4.1 to 6.8 ± 3.9 hours (P < 0.001) and an increase in the proportion of patients discharged from the ED from 50% to 71%, with similar 30-day safety outcomes preimplementation and postimplementation. It is important to note that in the preimplementation period, the usual care protocol performed measurements of hs-cTnI at 0 and 6 to 12 hours, which is more conservative than “usual care” in most U.S. hospitals and may exaggerate benefits on length of stay vs what would be expected with implementation in the United States. Nevertheless, the High-STEACS pathway represents a validated approach for rule out that capitalizes on hs-cTn assay strengths. Observational data from the United States have demonstrated a similar safety profile with 100% sensitivity and 100% NPV for 30-day death or MI when combined with a normal ECG.62 In a subsequent analysis of the High-STEACS trial, the investigators demonstrated that the algorithm also performed well with the Roche fifth-generation hs-cTnT assay using the LoQ cutoff of 6 ng/L.75
FIGURE 4. High-STEACS Early Rule-Out CDP.
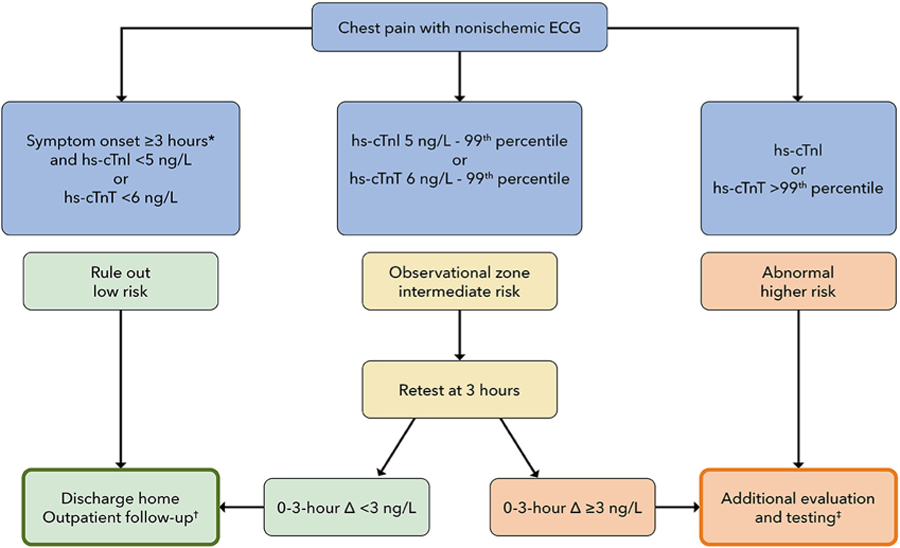
Sources for this Figure: 74,75
*Although clinical trials with the HIGH-STEACS pathway have required chest pain onset ≥2 hours before presentation, we recommend requiring a ≥3-hour period between chest pain onset and the first troponin measurement in order to qualify for rule out at time 0. †See Sections 5.6 and 5.8 for recommendations on outpatient follow-up and testing. ‡Additional evaluation is recommended, with consideration of hospital observation or admission, and noninvasive anatomical or functional testing as described in Section 5.6. Myocardial injury should be classified as described in Section 5.7 into chronic myocardial injury, acute myocardial injury, type 1 MI, and type 2 MI, as per the Universal Definition of Myocardial Infarction. Patients with acute MI should be managed according to standard practice guidelines. Patients with chronic myocardial injury may be appropriate for discharge and management in an outpatient setting (see Sections 5.7 and 5.8).
ACS = acute coronary syndrome; ECG = electrocardiogram; High-STEACS = High-Sensitivity Troponin in the Evaluation of Patients With Acute Coronary Syndrome; hs-cTnI = high-sensitivity cardiac troponin I; hs-cTnT = high-sensitivity cardiac troponin T; MI = myocardial infarction.
5.4.4. Patients With Chronic Kidney Disease
Evaluating patients with kidney dysfunction who present with chest pain is a particular challenge because elevations in hs-cTn above the 99th percentile URL are very common.98 Data in this group are limited, as most studies have specifically excluded patients with end-stage kidney disease. In the High-STEACS trial, the proportion of patients with elevated hs-cTnI above the 99th percentile URL increased from 10% for those with an estimated glomerular filtration rate (eGFR) ≥90 mL/min/1.73 m2) to 66% among those with an eGFR <30 mL/min/1.73 m2.99 Concomitant with this, the proportion of patients diagnosed with acute myocardial injury and type 2 MI also increased.
Studies examining hs-cTn CDPs among this population have suggested similar safety compared with those without kidney dysfunction; however, efficacy and PPV of the pathways are reduced. Twerenbold et al93 demonstrated that the ESC 0/1-hour algorithm had a sensitivity of 100% and NPV of 100% for MI when applied to patients with renal dysfunction (eGFR <60 mL/min/1.73 m2) using hs-cTnT, and a sensitivity of 98.6% and NPV of 97.4% when using an hs-cTnI assay. However, only approximately were 18% ruled out with the pathway, and almost one-half of patients were triaged to the intermediate-risk/observation group. Similarly, the High-STEACS investigators demonstrated that an hs-cTnI of <5 ng/L at presentation had a sensitivity of 98.9% and NPV of 98.4% for 30-day death and MI in patients with chronic kidney disease; however, only 17% of patients were ruled out with the baseline hs-cTnI measurement, a proportion that was further reduced in those with an eGFR of <30–60 mL/min/1.73 m2. 100,101 One analysis proposed using an eGFR-adjusted baseline rule-in threshold to improve specificity without affecting sensitivity101; however, another study found that threshold adjustments improved efficacy, but at the cost of reduced safety.93
It should be anticipated that a large proportion of patients with renal dysfunction will fall into an intermediate-risk category and may require further diagnostic testing. The noninvasive test of choice will depend on the degree of renal dysfunction and other clinical factors, as outlined in Section 5.6. Further research is needed to develop more efficient pathways for evaluating this challenging patient population.
5.4.5. Summary
In aggregate, studies performed to date (including real-world implementation studies)95,102,103 demonstrate that the ESC 0/1-hour, 0/2-hour, and High-STEACS CDPs reduce ED length of stay and increase the proportion ruled out and dispositioned home compared with traditional approaches using less-sensitive cTn assays and with the ESC 0/3-hour algorithm using hs-cTn. Implementation of these CDPs is associated with similar clinical outcomes compared with the more traditional approaches that require longer times to rule out MI. With the transition to hs-cTn from older-generation assays, the rate of type 1 MI diagnosis is slightly increased, with greater increases in type 2 MI diagnosis and marked increases in the diagnosis of cardiac injury.68,104 The impact on cardiac testing and coronary angiography has varied slightly between studies, but overall rates do not appear increased102,105,106; however, most have been performed outside of the United States where testing thresholds are different. Importantly, the available data from U.S. studies also showed no significant increase in downstream resource use102,103,105,106, but further data is needed. The absence of improvement in clinical outcomes with implementation of a CDP is expected given their low overall risk.
The ESC 0/1 (or 0/2) and High-STEACS approaches are recommended over simply using the 99th percentile URL value at 0 and 3 hours to rule out MI because direct comparisons demonstrate both greater efficacy (more patients ruled out) and greater safety (fewer missed MIs). Thus, hs-cTn should be implemented in the context of a CDP to achieve maximal performance. Setting objectives and expectations is crucial for successful implementation. The hs-cTn assays diagnose a larger number of patients with type 2 MI and acute and chronic cardiac injury than do approaches using standard assays. Successful implementation of hs-cTn CDPs requires consideration of triage of these patients in ED workflows. The term rule in should be reserved for those in the abnormal group who meet Universal Definition of MI criteria for MI. Careful education is necessary to mitigate untoward consequences, including unnecessary testing and hospitalization for patients without MI (see Section 5.8). The dominant value of the hs-cTn assays is to accelerate chest pain evaluation in the ED, with more patients ruled out faster, allowing more rapid ED discharge, and thus decreasing ED crowding and limiting unnecessary use of resources.
5.5. Additional Risk Stratification Beyond Troponin Measurement
5.5.1. Patients Classified as “Rule Out” by Conventional Cardiac Troponin
Risk stratification is an important component of the evaluation of patients with possible ACS. For institutions using conventional cTn assays (ie, non–hs-cTn assays) or those using hs-cTn but not reporting below the 99th percentile URL, the 2021 AHA/ACC/multisociety chest pain guideline recommends the incorporation of clinical risk scores in the evaluation of patients with concern for ACS due to the insufficient sensitivity and NPV of these assays alone for ruling out MI.5
There are several risk scores that have been used for ED chest pain evaluation. One of the most commonly used scores is the HEART score, which uses readily-available clinical data and the clinician’s interpretation of the history to risk-stratify patients (see Table 3). A common modification of this risk score omits cTn or hs-cTn. This “modified HEART score” or “HEAR” score is used for risk stratification among patients who have been ruled out for MI based on cTn criteria. In a randomized clinical trial, a comparison of the HEART pathway with standard of care among 282 patients with possible ACS, with a primary endpoint of objective cardiac testing,107 found a 12% reduction in objective cardiac testing at 30 days (P = 0.048). A U.S. implementation study of the HEART pathway found that a HEART score ≤3 combined with a nonischemic ECG and 0- and 3-hour cTn <99th percentile identified 30.7% of patients as low risk and eligible for early discharge, with a 30-day rate of death from MI of only 0.4%.108
A second commonly used risk score is EDACS, which also uses readily available clinical information.109 This scoring system requires that the patient have a nonischemic ECG and serial conventional cTn values ≤99th percentile over 2 hours. Validation studies in the United States have demonstrated that those classified as low risk by the EDACS pathway have a 30-day major adverse cardiac event rate of ≤1%.110,111 The Global Registry of Acute Coronary Events and Thrombolysis in MI scores were initially developed for risk stratification for managing NSTE-ACS, but have also been studied for evaluating patients with acute chest pain. However, they have inferior sensitivity and NPV to the HEART score and EDACS.112 The 2-Hour Accelerated Diagnostic Protocol to Assess Patients With Chest Pain Symptoms Using Contemporary Troponins as the Only Biomarker (ADAPT) pathway combines a Thrombolysis In Myocardial Infarction score of 0, a nonischemic ECG, and 0- and 2- hour cTn concentrations <99th percentile to identify patients at low risk (30-day major adverse cardiac event risk <1%), but does so with less efficacy than the HEART and EDACS pathways.113,114
In summary, for patients presenting with symptoms of possible ACS with serial conventional (ie, non–hs-cTn) cTn values less than the 99th percentile URL and nonischemic ECGs, a low modified HEART score (≤3) or EDACS (<16) can identify patients eligible for discharge without a requirement for further diagnostic testing. Patients with intermediate- or high-risk scores, elevated cTn concentrations, ischemic ECGs, or high suspicion for unstable angina should undergo further diagnostic testing. EDACS and the modified HEART score are the best validated strategies and identify the largest number of patients as low risk using conventional cTn assays.
5.5.2. Patients Classified as “Rule Out” by Hs-cTn Pathways
The 2021 AHA/ACC/multisociety chest pain guideline advises that patients who are ruled out by an hs-cTn CDP and have a nonischemic initial ECG may be discharged without further testing and do not require the application of risk scores.5 Indeed, randomized clinical trials that demonstrated safety and efficacy of the ESC 0/1-hour algorithm,68 the HIGH-STEACS algorithm,74 and single baseline hs-cTn rule-out pathways61,115 did not mandate the use of risk scores to identify patients at low risk.
Observational studies have evaluated the incremental value of risk scores when combined with hs-cTn CDPs with mixed results. Among 1,935 patients with suspected ACS, Chapman et al116 found that the addition of risk scores did not further improve the safety of the ESC 0/1-hour and High-STEACS pathways but decreased the number of patients identified as low risk. In contrast, a multicenter U.S. study of 1,462 patients presenting with symptoms of possible ACS suggested that a single hs-cTnT < LoQ combined with a nonischemic ECG may not be sufficient to define low-risk when used without a risk score (sensitivity of 97.4% and NPV of 98.9% for 30-day MI or cardiovascular death).117 Requiring a modified HEART score of ≤3 increased the sensitivity to 99.5% and NPV to 99.7% but reduced the efficacy from 31.9% to 20.1%. Others have also found higher event rates in patients who had an hs-TnI <5 ng/L.118 Differences between the studies include variation in populations studied and choice of endpoints, with lower NPV found when revascularization or readmission are included in composite study endpoints.
In summary, patients identified as low-risk by hs-cTn–based pathways endorsed by this document (ESC 0/1-hour, ESC 0/2-hour, and High-STEACS pathways) combined with a nonischemic ECG are eligible for early discharge without further inpatient diagnostic testing. Although routine application of risk scores for patients identified as low risk by these pathways is not recommended, the modified HEART score or EDACS may be considered for selective application especially in cases where the physician believes the patient may be higher risk based on their clinical history or symptoms at presentation. For hospitals that wish to take a more conservative approach to ED discharge of low-risk chest pain patients, applying risk scores to low-risk groups can be considered, recognizing that the improvement in safety will be small and fewer patients will be discharged home. Among patients who do undergo risk score application, patients with an intermediate or high risk score (ie, modified HEART score ≥4 or EDACS ≥16) may be considered for additional noninvasive testing, early outpatient follow-up, or prompt outpatient noninvasive testing following discharge. Ultimately, the decision for discharge from the ED should not rely on the CDP algorithm alone, but should always include the clinical assessment and judgment of the ED provider.
5.5.3. Patients Classified as “Intermediate Risk” by Hs-cTn Pathways
For hospitals using hs-cTn assays, chest pain algorithms stratify patients into rule-out (ie, low-risk) or abnormal/rule-in (ie, high risk) categories (2-tiered approach), with some algorithms including an intermediate-risk or observation-zone group (3-tiered approach). Examples of the 2-tier risk stratification approach include the ESC 0/3-hour and High-STEACS pathway (see Section 5.4). In contrast, the ESC 0/1- and 0/2-hour algorithms generally have 3 tiers of risk, although some algorithm modifications reclassify patients defined as intermediate risk at 1-hour into rule out or abnormal at 3 hours based on hs-cTn change through 3 hours.94,95 Patients classified as intermediate risk by the ESC 0/1- and ESC 0/2-hour algorithms have minimally elevated hs-cTn (between the LoQ and the 99th percentile URL) or hs-cTn above the 99th percentile URL but below the abnormal/high risk threshold, with no or only minor changes in the cTn concentration over the serial measurements. Approximately 1 in 4 patients presenting with possible ACS will be assigned to the intermediate-risk group by the ESC 0/1-hour algorithm.83,86,117 These patients are higher risk than those traditionally admitted to observation units as they frequently have concomitant pre-existing cardiovascular disease, other cardiovascular risk factors, and medical comorbidities. Some will ultimately be diagnosed with a non-STEMI during their index presentation, and accordingly, serial cTn measurements are warranted to assess for dynamic changes that would meet the Universal Definition for MI in the setting of symptoms of ischemia.14 Notably, the observation group has a 30-day rate of death or MI ranging from 5% to 22%.76,84,86
Given the increased risk for an index MI diagnosis and 30-day major adverse cardiac events in the intermediate-risk group, further monitoring is recommended, and diagnostic testing may be needed (see Figure 5). When considering the disposition of these patients, the physician must first take into consideration the patient’s presenting symptoms and consider alternative causes to ACS for the cTn elevation. All intermediate-risk patients should undergo repeat hs-cTn testing at 3 to 6 hours to assess for dynamic cTn changes. Those with a significant rise in cTn will be diagnosed with acute myocardial injury or MI. For patients without a significant change in hs-cTn concentration not meeting the criteria for abnormal/high risk after serial measurements, there is limited guidance from observational or clinical trials to best inform patient selection for additional noninvasive testing. Test selection should therefore take into account the suspicion for ACS, as well as results from recent prior testing. In hospital systems that have adequate resources to perform cardiac diagnostic testing within an observation unit setting, this may be preferable. For patients with no or minimal additional cTn change from the prior measurement and 1) recent normal noninvasive testing (ie, invasive or CT coronary angiogram <2 years or stress test <1 year); or 2) chronic elevations in hs-cTn that are unchanged compared with levels measured previously; and 3) a modified HEART score of ≤3 or EDACS <16, discharge without further testing is reasonable, provided access to rapid follow-up is available. For those not meeting these criteria, noninvasive diagnostic testing should be considered for additional risk stratification, generally before discharge. The diagnostic test of choice will depend on the patient’s characteristics and prior testing (outlined in Section 5.6). For those with obstructive CAD (≥50% stenosis) identified on CT coronary angiography or moderate to severe ischemia identified on functional testing, invasive cardiac catheterization is recommended in those with symptoms consistent with ACS.5
FIGURE 5. Algorithm for Intermediate-Risk Patients.
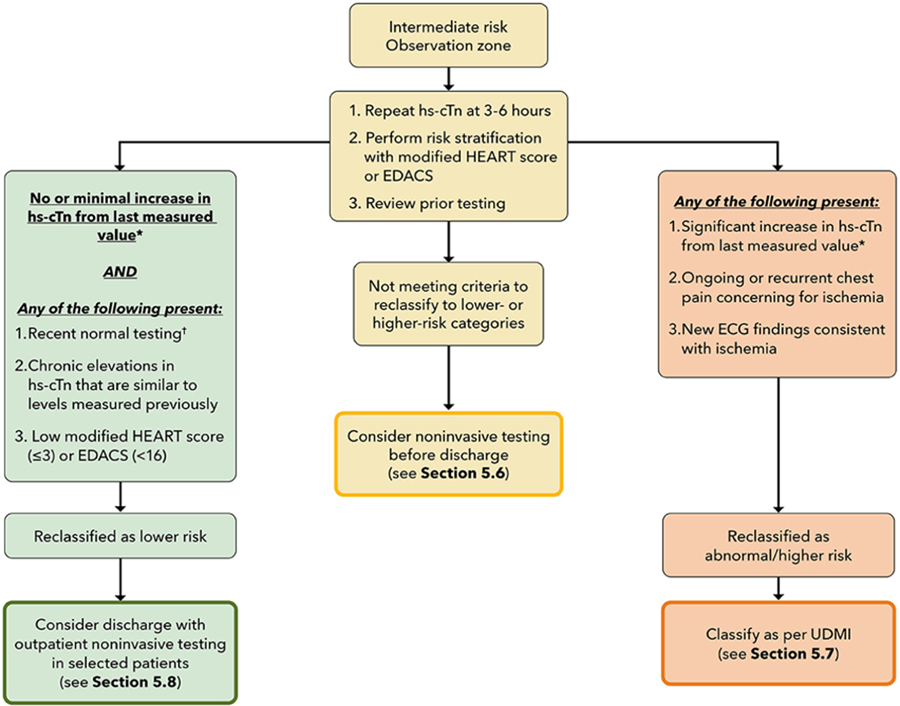
*Evidence-based criteria do not exist to define change thresholds for hs-cTn at the 3- to 6-hour timepoint. As reviewed in Section 5.2, although a 20% relative change from the baseline measurement has been proposed to define significant change, this threshold lacks specificity at low hs-cTn values in part due to assay imprecision. Thus, at lower hs-cTn values near the sex-specific 99th percentile URL values, absolute changes should be used to define clinically-significant change, whereas at higher troponin values, a 20% relative change in values may be a more reasonable threshold. Clinical judgment is needed to interpret small fluctuations in hs-cTn values over serial measurements, as these small changes may reflect assay imprecision rather than acute cardiac injury. †Recent normal testing is considered an invasive or CT coronary angiogram <2 years without evidence of coronary plaque or a stress test <1 year without ischemia.
ECG = electrocardiogram; EDACS = Emergency Department Assessment of Chest Pain Score; HEART = History, ECG, Age, Risk Factors, and Troponin; hs-cTn = high-sensitivity cardiac troponin; UDMI = Universal Definition of Myocardial Infarction.
5.5.4. Summary
Approximately one-quarter of patients will be categorized as at intermediate risk when applying a “3-tiered” hs-cTn pathway (ESC 0/1-hour algorithm or ESC 0/2-hour algorithm). Serial hs-cTn measurements over 3 to 6 hours are required for this population, with a significant rise identifying those with acute myocardial injury and possibly MI. For those with unchanged hs-cTn, patient selection for additional noninvasive testing should factor in prior testing, the likelihood that symptoms represent ACS, historical hs-cTn concentrations, risk scores, and access to rapid follow-up. For patients discharged without additional testing, early follow-up is recommended (see Section 5.8).
5.6. Subsequent Evaluation: Noninvasive Cardiovascular Diagnostic Testing
5.6.1. Objectives of Secondary Testing: Focus on “Intermediate-Risk” Patients
One of the primary goals of the initial ED diagnostic evaluation of patients with acute chest pain is the accurate risk classification into low-, intermediate-, or high-risk cohorts to allow for appropriate guideline-directed diagnostic and therapeutic treatments.5 As discussed in prior sections, low-risk patients have a very low event rate and can usually be discharged directly from the ED without additional in-hospital testing, whereas high-risk patients should usually be admitted, classified as myocardial injury or MI, and initiated on guideline-based NSTE-ACS therapies if considered a type 1 MI. Thus, the primary role of subsequent noninvasive cardiac testing is for the evaluation of patients classified as at intermediate risk according to the initial CDP evaluation. The goals of noninvasive testing are for the accurate diagnosis or exclusion of clinically significant CAD or other cardiovascular conditions that may be the cause of the patient’s symptoms and require specific treatments or further evaluation, as well as to risk-stratify patients who require immediate treatment and those for which it can be delayed or deferred. Importantly, diagnostic testing often identifies cardiac abnormalities, such as nonobstructive coronary atherosclerosis or left ventricular hypertrophy, that require follow-up and treatment to reduce future cardiovascular risk, highlighting the importance of consistent post-test reporting to better inform subsequent management.
5.6.2. Pre-Test Patient Assessment
Providers should identify patients with previously known CAD, defined as a prior MI, coronary revascularization procedure(s), or obstructive or nonobstructive CAD on previous invasive coronary angiography or coronary CTA.5 Additionally, the results of prior tests for CAD should influence subsequent test selection and refine the initial risk assessment. When available, prior nongated chest CT imaging should be reviewed for the presence and severity (mild, moderate, severe) of coronary calcification. Similarly, the results of prior anatomical coronary imaging (coronary artery calcium [CAC] scoring, coronary CTA, or invasive coronary angiography) and ischemia testing should be reviewed for CAD burden (stenosis severity, extent of disease) and the presence and severity of ischemia, respectively, as well as for the presence and severity of artifacts. A completely normal (no plaque or stenosis) invasive coronary angiogram or coronary CTA performed within 2 years or a normal functional test performed within 1 year of presentation makes the presence of ACS and significant CAD unlikely, with the absence of coronary atherosclerosis on coronary CTA providing the highest NPV for future ACS and adverse events.5
5.6.3. Test Description
5.6.3.1. Role of Rest Transthoracic Echocardiography
Bedside TTE can aid in the diagnostic evaluation of patients with acute chest pain by assessing left and right ventricular function, regional wall motion, valvular abnormalities, and pericardial effusion, among other findings. The proliferation of point-of-care ultrasound has increased its availability in the ED.119 High-risk patients, including those with elevated hs-cTn, should undergo a comprehensive TTE as part of their overall clinical assessment if no recent TTE has been performed.13 Before performing a comprehensive TTE, a more limited and focused urgent bedside ultrasound to assess for regional wall motion abnormalities, ventricular dysfunction, valvular dysfunction, and pericardial effusion can provide valuable triage information in intermediate-risk patients or those with ECG changes suggestive, but not diagnostic of ischemia.5 Although evaluation of ventricular function and pericardial effusion can be accomplished by most practitioners, assessment of regional wall motion abnormalities should be interpreted by those who have appropriate training and expertise.119
5.6.3.2. Coronary CTA
Coronary CTA is an accurate, noninvasive method for the diagnosis of CAD.120 The use of coronary CTA in patients presenting with acute chest pain is supported by numerous randomized clinical trials that enrolled predominately non–high-risk patients without previously known CAD.121 Coronary CTA is also effective as a “gate-keeper” to invasive coronary angiography in patients with inconclusive ischemia tests.122 Coronary CTA, compared with functional testing modalities, may be more rapidly available to patients undergoing evaluation in the ED, making it an attractive test to provide a timely evaluation of the presence and severity of CAD in intermediate-risk patients so that decisions regarding disposition and management can be expedited. Clinical trials conducted before the routine use of hs-cTn was implemented demonstrated that coronary CTA significantly reduced the time to diagnosis (ACS vs no ACS) as compared with traditional evaluation pathways in patients at low to intermediate risk for ACS123; limited data on the utility in intermediate-risk patients identified by hsTn has found less benefit.124,125 Coronary CTA also frequently identifies nonobstructive CAD that may be unrelated to the patient’s presentation but carries important long-term prognostic and preventive treatment implications, identifying patients with unsuspected atherosclerosis who would benefit from aggressive risk factor modification and treatment.126,127 Noncontrast chest CT for CAC scanning is not currently recommended for routine use as a stand-alone test (without coronary CTA) in patients with acute chest pain due to its inability to assess coronary artery stenosis, noncalcified plaque, and high-risk plaque features.128
When available, coronary CTA should be considered the preferred noninvasive test for patients presenting to the ED with possible ACS who do not have known CAD. Patient characteristics favoring coronary CTA, as compared with functional ischemia tests, are shown in Figure 6. Patients who undergo CTA who have no or nonobstructive (<50%) CAD may be safely discharged from the ED.5 Patients with obstructive coronary disease (≥50%) on CTA should generally be admitted, treated with therapies for ACS, and undergo invasive coronary angiography unless the location of stenosis or other clinical factors result in the shared decision for guideline-directed medical therapy alone.5 Protocols should be in place for a consistent process for follow-up of patients with nonobstructive CAD who require additional preventive treatments and lifestyle modifications, as well any incidental findings noted on coronary CTA.
FIGURE 6. Guideline-Directed Approach to Subsequent Diagnostic Testing in Patients With Suspected ACS at Intermediate Clinical Risk.
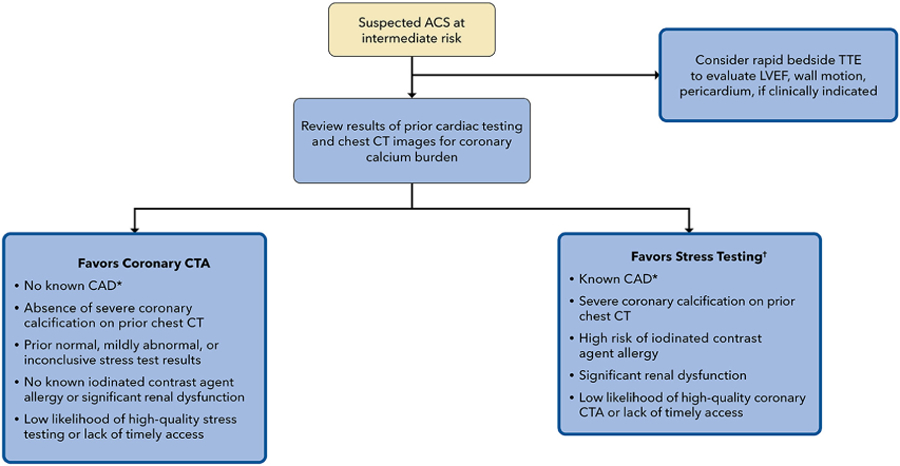
*Prior myocardial infarction, coronary revascularization, or stenosis >50% or extensive nonobstructive CAD on prior ICA/CTA. †Exercise ECG, stress CMR, stress echocardiography, stress perfusion imaging.
ACS = acute coronary syndrome; CAD = coronary artery disease; CT = computed tomography; CTA = computed tomography angiography; ICA = internal carotid artery; LVEF = left ventricle ejection fraction; TTE = transthoracic echocardiogram.
5.6.3.3. Ischemia Testing
There are numerous tests that assess for myocardial ischemia as a marker of clinically relevant CAD. These tests include exercise ECG testing without imaging and exercise or pharmacologic rest/stress ECG combined with imaging, using echocardiography, single-photon emission computed tomography, positron emission tomography, or cardiac magnetic resonance imaging (see Table 4). Most patients with acute chest pain at intermediate risk are likely to require stress testing with imaging, given the high frequency of known coronary disease, heart failure, and other comorbidities that limit the diagnostic utility of exercise ECG alone. Patient characteristics that favor ischemia testing using stress imaging rather than anatomical imaging with coronary CTA are shown in Figure 6.
TABLE 4.
Clinical Considerations for the Use of Noninvasive Testing for Coronary Artery Disease
| Ischemia Test Modality | Strengths | Limitations | Patient Considerations Favoring Its Use |
|---|---|---|---|
| Exercise stress ECG |
|
|
|
| Stress echocardiography |
|
|
|
| Stress/rest SPECT |
|
|
|
| Stress/rest PET |
|
|
|
| Stress CMR |
|
|
|
| CTA |
|
|
|
ACS = acute coronary syndrome CAC = coronary artery calcium; CAD = coronary artery disease; CMR = cardiovascular magnetic resonance; CT = computed tomography; CTA = computed tomography angiography; ECG = electrocardiogram; ICD = implantable cardioverter defibrillator; PET = positron emission tomography; SPECT = single-photon emission computed tomography.
The 2021 AHA/ACC/multisociety chest pain guideline recommends that an assessment of CAC burden using the Agatston calcium score or visual description (none, mild, moderate, severe), as appropriate, be included in nuclear stress test reports (single-photon emission computed tomography, positron emission tomography) if CT attenuation testing or dedicated CAC scoring is routinely performed by nuclear testing laboratories.5 Such information may assist in risk stratification, decision-making in the case of equivocal stress test findings or artifacts, and post-testing use of preventive therapies.
5.6.4. Diagnostic Algorithm for Choosing Appropriate Imaging Tests
The suggested diagnostic approach for subsequent testing in patients at intermediate risk of 30-day major adverse cardiac events is summarized in Figure 6.
5.6.5. Summary
It is important that providers understand the unique features of each of the noninvasive testing modalities to enable selection of the optimal diagnostic test based on patient characteristics and guideline recommendations (see Table 5). Decisions on the specific choice of test should include patient factors (see Figure 6), test availability and timeliness of test reporting, and institutional expertise. Additionally, patients previously having nondiagnostic test results using a particular modality should be considered for testing using an alternative test for CAD where high diagnostic accuracy is likely.
TABLE 5.
Myocardial Injury Differential
| Myocardial Injury: Defined as at Least 1 ng/L Above the 99th Percentile URL | |||
|---|---|---|---|
| Acute Myocardial Injury (Rising and/or Falling Cardiac Troponin) |
Chronic Myocardial Injury (Stable Elevation in Cardiac Troponin) |
||
| Cardiovascular Causes | Noncardiovascular Causes | Cardiovascular Causes | Noncardiovascular Causes |
| Acute myocardial infarction (type 1–5 MI) | Sepsis | Stable coronary artery disease | Chronic renal failure |
| Hypertensive emergency/urgency | Acute renal failure | Chronic heart failure | Skeletal myopathies |
| Acute heart failure | Noncardiac surgery | Uncontrolled arrhythmias | Cardiotoxic medications |
| Pulmonary embolism | Critical illness | Hypertension | |
| Acute aortic syndrome | Rhabdomyolysis | Valvular heart disease | |
| Cardiac surgery | Cardiotoxic medications | Cardiomyopathies | |
| Cardiac intervention, including PCI, ablations, valve replacements, cardioversion/defibrillation, endomyocardial biopsy | Stroke | Pulmonary hypertension | |
| Acute valvular heart disease | Extreme exercise | Left ventricular hypertrophy | |
| Stress cardiomyopathy | False-positive result | ||
| Cardiac contusion | |||
| Myocarditis/myopericarditis/endocarditis | |||
| Arrythmias | |||
PCI = percutaneous coronary intervention; URL = upper reference limit
5.7. Classification, Evaluation, and Management of Myocardial Injury
Increased implementation of hs-cTn assays will lead to more frequent detection of elevated cTn concentrations among patients presenting with possible ACS, with many elevations unrelated to MI.103,105 Appreciating this, the latest iteration of the Universal Definition of MI introduced the term myocardial injury to reflect the detection of any cTn concentration above the 99th percentile URL.14 Myocardial injury is considered acute if there is a dynamic rise and/or fall of cTn concentrations exceeding the analytical variation of the assay (>20% relative change), with at least 1 value above the 99th percentile, and chronic if the cTn level remains elevated but stable over serial measurements.14
When evaluating patients using cTn, the first step is to determine if the cTn elevation is acute or chronic. This is based on serial changes in cTn concentration over time, typically over a few hours (see Figure 7). Repeat sampling over a more prolonged time period should be considered in those with minimal change in concentrations to better discriminate acute from chronic injury. In addition, patients presenting late after MI onset may have minimal change in cTn concentrations when assessed over short time periods,97 such that clinical presentation is important for interpreting cTn values. A significant change has been variably defined, but for lower cTn concentrations, an absolute rather than a relative change should be used.52
FIGURE 7. Classification of Myocardial Injury.
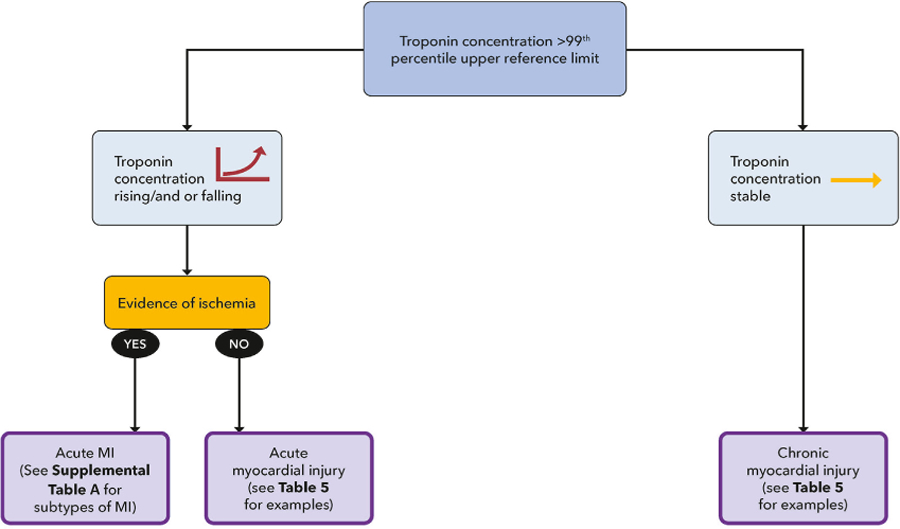
MI = myocardial infarction.
If acute myocardial injury is present, the next step is to determine if the cTn elevation reflects MI. According to the Universal Definition of MI, diagnosis requires both acute myocardial injury and the presence of myocardial ischemia based on the occurrence of one of the following: 1) symptoms suggestive of myocardial ischemia; 2) new ischemic changes on the ECG; 3) new pathological Q waves; 4) new ischemic regional wall motion abnormalities on cardiac imaging; or 5) acute coronary thrombus/erosion on invasive coronary angiography.14 Unfortunately, clinical evidence of ischemia is frequently ambiguous, and an accurate diagnosis may not be immediately evident; thus, additional testing may be needed.
Five distinct clinical subtypes of MI have been introduced. MI subtypes are summarized in Table B of the Supplemental Appendix.14 Type 1 MI occurs due to acute plaque disruption (from rupture or erosion). In the context of patients presenting to the ED with symptoms concerning for ischemia, and in the absence of any additional medical condition triggering their symptoms, patients should be managed for type 1 MI according to the latest ACC/AHA NSTE-ACS guidelines.12,13,129 A type 2 MI is myocardial necrosis precipitated by a mismatch in myocardial oxygen supply-demand in the absence of atherothrombosis. It may occur in the setting of an acute medical or surgical condition and often is associated with fixed atherosclerotic CAD, but this is not required. Similar to type 1 MI, type 2 MI requires symptoms, ECG changes, new wall motion abnormalities, or coronary angiographic findings to be considered an MI. The differentiation of type 2 MI from nonischemic acute myocardial injury can be challenging, as they can have overlapping precipitants (eg, heart failure).130 Even when given specific criteria, cardiologists have only a modest rate of agreement for differentiating between the two.131
5.7.1. Importance of Differentiating Subtypes of MI
The differentiation of type 1 MI from the remaining subtypes of MI and nonischemic myocardial injury is important for several reasons. Treatment strategies for type 1 MI are defined by evidence from large randomized controlled trials and outlined in clinical guidelines.12,13,129
In contrast, there are limited data on the appropriate management of patients with type 2 MI, and even less for patients with nonischemic myocardial injury. Accurate differentiation and coding of the subtypes of MI is important because patients with type 1 MI (unlike type 2 MI and myocardial injury) are included in value-based programs and have ACC/AHA Clinical Performance and Quality Measures to guide their care.105,132–134
5.7.2. Type 2 MI
Patients with type 2 MI are frequently encountered in clinical practice. Data from a U.S. national registry database in 2017 found type 2 MI represented at least 15% of total MI cases.135 However, the incidence appears higher in the ED (ranging from 26% to 58%) when causes of cTn elevation are adjudicated.130
When compared with patients with type 1 MI, those with type 2 MI are usually older, have more noncardiovascular comorbidities, and have less prevalent traditional atherosclerotic risk factors.135 Because type 2 MI patients have not been specifically evaluated in clinical trials, management of this population in practice has been heterogenous and divergent from patients with type 1 MI. Patients with type 2 MI are less likely than patients with type 1 MI to be discharged on secondary preventive therapies or to undergo invasive angiography and revascularization.135–138 However, CAD is common among patients with type 2 MI when imaging is systematically applied; approximately two-thirds have CAD and one-third have obstructive disease.139 Furthermore, one-third have left ventricular dysfunction detected on imaging.139 Following discharge, major adverse cardiovascular events are higher when compared with type 1 MI136 due to a greater comorbidity burden and risk of noncardiovascular mortality.136
Given the high burden of atherosclerotic disease and the substantial recurrent cardiovascular event rate, the following framework for managing patients with type 2 MI seems reasonable, although firm guidance is limited due to an absence of randomized clinical trials in this population (see Figure 8). If there is uncertainty regarding whether the diagnosis is a type 1 or 2 MI, clinicians should generally manage the patient as presumed type 1 MI. Once the diagnosis of type 2 MI is made, clinicians should first identify and treat the precipitant of acute supply/demand mismatch. A structural evaluation of the heart with TTE should be performed to assess for regional wall motion abnormalities, valvular heart disease, and systolic dysfunction. Among patients with no recent evaluation for CAD, an anatomical or functional evaluation for CAD should be considered, as undiagnosed CAD is frequently present, and obstructive CAD is associated with a higher rate of recurrent events.136,139–141 For patients who are clinically stable and without ongoing ischemic symptoms, this can be deferred to the outpatient setting following discharge.
FIGURE 8. Management of Type 2 MI.
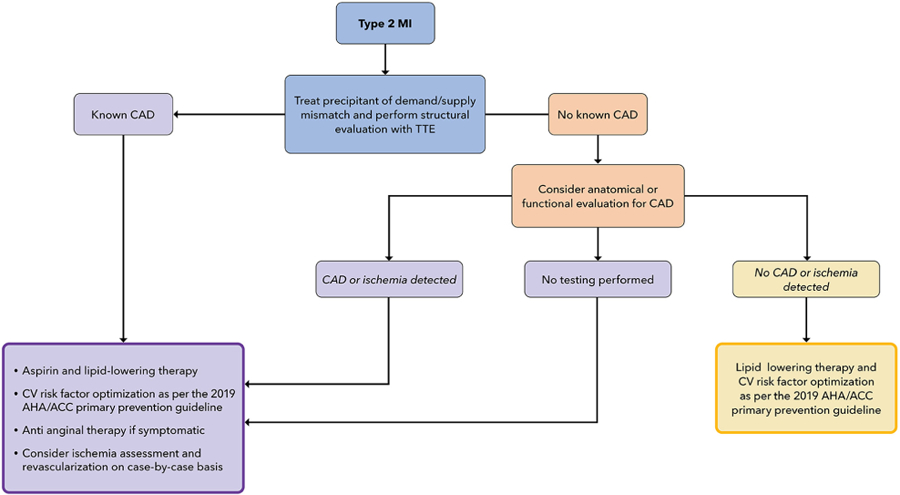
ACC = American College of Cardiology; AHA = American Heart Association; CAD = coronary artery disease; CV = cardiovascular; MI = myocardial infarction; TTE = transthoracic echocardiogram.
Among patients with known or newly diagnosed CAD or ischemia, secondary prevention therapies, including aspirin and lipid-lowering therapy, should be initiated or optimized.130,142,143 Beta-blockers may be beneficial, particularly among patients with angina, tachyarrhythmias, and confirmed CAD. Among patients with ischemic symptoms, antianginal medications should be adjusted. Treatments for cardiovascular comorbidities, including diabetes, chronic kidney disease, and hypertension, should also be optimized according to prevention guidelines. Among patients with obstructive CAD, revascularization may be considered on a case-by-case basis, considering the precipitant of the type 2 MI and likelihood of recurrence, burden of anginal symptoms and current antianginal therapy, severity and complexity of CAD, presence or absence of left ventricular dysfunction, comorbidities, and life expectancy. Clinical trials are needed to inform the role of routine revascularization in this population. For patients who have had CAD or ischemia excluded, aspirin and lipid-lowering therapy should be implemented in those who meet treatment indications based on the patient’s cardiovascular disease risk.144 Similarly, cardiovascular risk factors, including hypertension, diabetes, hypertriglyceridemia, and tobacco use, should be addressed and optimized.144,145
5.7.3. Myocardial Injury
Accumulating data indicate that the majority of patients with elevated cTn concentrations in the ED will not have type 1 MI but rather will have type 2 MI or myocardial injury, particularly among centers that have transitioned to hs-cTn assays.103,105,146,147 Although implementation of hs-cTn assays is associated with increased detection of type 1 MI, it is also associated with a greater increase in identification of type 2 MI and myocardial injury.104 The frequency of elevations will increase if sampling is performed in more heterogeneous patients where the diagnostic suspicion for ACS is lower. In one recent U.S. study, almost one-half (47%) of patients who had hs-cTnT sampling had values above the 99th percentile URL.105
Troponin may be elevated due to several mechanisms beyond ischemia, including inflammation, cell turnover, exocytosis, apoptosis, and decreased clearance.148 For that reason, the differential diagnosis for acute and chronic myocardial injury is broad (see Table 4). As left ventricular hypertrophy and heart failure are strongly correlated with myocardial injury, a structural evaluation of the heart with TTE should be performed if not recently undertaken.149 Cardiac magnetic resonance imaging can be useful in selected cases to better delineate the etiology of acute myocardial injury (eg, myocarditis or an infiltrative cardiomyopathy). As symptoms of ischemia can be challenging to differentiate from other pathologies (eg, heart failure), ischemic or anatomical testing may be required for clarification in some patients.
Initial management should focus on identification and treatment of the underlying cause of myocardial injury (see Figure 9). Notably, patients with acute myocardial injury have a high rate of subsequent cardiovascular events,136,150 with approximately 15% experiencing an MI or cardiovascular death at 1 year.104 A higher risk of heart failure is also observed with increasing concentrations of cTn.150 The risk is higher among patients with acute rather than chronic myocardial injury.104 Similar to type 2 MI, there are limited data to inform management of myocardial injury. Most available data are observational and focus on chronic rather than acute myocardial injury. Observational data suggest that chronic myocardial injury may identify patients who derive greater absolute benefit from atherosclerotic and heart failure preventive therapies. In addition, data from primary prevention trials have found that patients with myocardial injury have a greater absolute benefit from statin therapy.151 Until further data emerge, for individuals not already on lipid-lowering therapy, the presence of myocardial injury should be considered as a risk enhancer in the application of the ACC/AHA guidelines for determining statin eligibility. This would result in a lower threshold for statin initiation in patients with cardiac injury.
FIGURE 9. Management of Myocardial Injury.
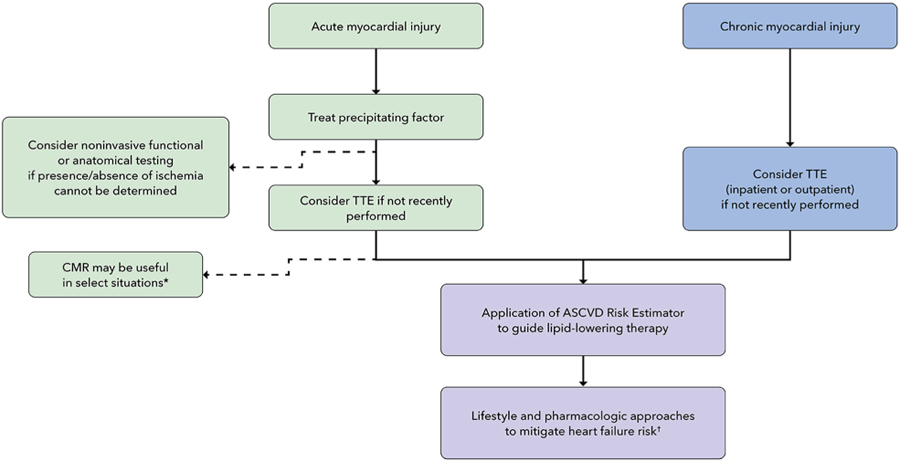
* Concern for myocarditis, hypertrophic cardiomyopathy, infiltrative cardiomyopathies. † Ensure blood pressure and diabetes are optimized; encourage increased physical activity and weight loss in overweight and obese individuals.
ACC = American College of Cardiology; AHA = American Heart Association; ASCVD = atherosclerotic cardiovascular disease; CMR = cardiac magnetic resonance imaging; TTE = transthoracic echocardiogram.
Among patients with hypertension, a post hoc analysis of the SPRINT (Systolic Blood Pressure Intervention Trial) found that intensive blood pressure control resulted in substantially larger absolute reductions in risk for heart failure and death among patients with chronic myocardial injury vs those with normal hs-cTnT levels.152 Additionally, modeling studies suggest that in the general population, chronic myocardial injury identifies individuals with elevated blood pressure or hypertension not currently recommended for antihypertensive medications who are at high risk for cardiovascular events153 and would be expected to benefit from pharmacologic treatment for hypertension. Accordingly, blood pressure should be optimized (<130/80 mm Hg) for all patients with myocardial injury. However, blood pressure optimization can be deferred to the outpatient setting for most patients unless blood pressure is markedly elevated. In addition to those with hypertension, patients with chronic myocardial injury may also derive greater benefit from newer glycemic agents. Post hoc analyses from 2 recent sodium-glucose cotransporter 2 inhibitor (SGLT2i) trials found that patients with myocardial injury derived greater absolute major adverse cardiac event reduction from SGLT2i treatment.154,155 Therefore, among individuals with type 2 diabetes and myocardial injury, addition of an SGLT2i may reduce subsequent risk for heart failure.
5.8. Disposition, Follow-up, and Treatment
Safe and efficient management of chest pain in the ED requires appropriate follow-up after discharge from the ED or hospital. Timing of follow-up and referral for outpatient noninvasive testing should be influenced by patient risk and results of cardiac testing.
Implementation of CDPs (see Section 5.4) results in important changes to hospital workflow for patients with chest pain, as many more patients are ruled out for MI while still in the ED rather than from observation or the hospital units, shifting the burden of ensuring safe discharge and transition to the ED. Thus, a major priority for all health systems considering implementation of accelerated CDPs is to ensure that adequate follow-up is available for all patients discharged from the ED, including those who are uninsured or underinsured or lack primary care physicians (PCPs).
5.8.1. Rule Out by CDP Algorithm
As discussed earlier in Sections 5.4 and 5.5, patients ruled out using an hs-cTn CDP are eligible for discharge from the ED without further noninvasive cardiac testing due to their low likelihood of 30-day death and MI. Given that most patients will have a noncardiac etiology for their chest pain, evaluation for alternative, non–ACS-related cardiac and noncardiac conditions should be performed as clinically appropriate. Following discharge, low-risk patients ruled out for MI by one of the CDPs should be referred for outpatient follow-up within 30 days and, if feasible, within 14 days. Whenever possible, patients with established PCPs (physician or advanced practice provider) or cardiologists should be instructed to follow up with their established clinician to maintain continuity of care. If possible, the patient’s PCP and/or cardiologist should be notified at the time the patient is discharged from the ED to facilitate outpatient follow-up.
5.8.2. Intermediate-Risk Patients
For hospitals using variations of the ESC 0/1-hour or ESC 0/2-hour algorithms, approximately 25% of patients will be classified as at intermediate risk83,86,117 and require additional observation and hs-cTn measurement 3 to 6 hours later. A substantial proportion of these patients will undergo predischarge noninvasive testing, based on results of serial hs-cTn, modified HEART score or EDACS, and prior cardiac testing (see Sections 5.5 and 5.6), However, a subset of patients in the intermediate-risk group may be determined to be sufficiently low risk to consider discharge without inpatient noninvasive testing (see Section 5.5.3). It is important to recognize that “intermediate-risk” patients are at higher risk than “rule-out” patients, as they frequently have concomitant pre-existing cardiovascular disease, other cardiovascular risk factors, and medical comorbidities, and thus close follow-up is recommended, preferably within 7 days. For patients who undergo predischarge noninvasive testing with normal or low-risk findings, a longer time window for follow-up is reasonable. Whenever possible, patients should follow-up with their established cardiologist or PCP, which can be particularly helpful given the complexity of this group of patients. In hospital systems in which PCP follow-up is not routinely available, development of an acute care follow-up clinic to address these issues should be strongly considered. Standardized follow-up can be useful for implementing risk factor modification and treatment, evaluating noncardiac causes for the patient’s chest pain, and identifying a need for further follow-up.
For patients undergoing noninvasive cardiac testing before discharge, admission to an observation unit is recommended as an alternative to inpatient admission. Patients with symptoms consistent with ACS with reduced left ventricular systolic function should be considered for coronary angiography.13 Patients with moderate or severe ischemia identified on stress testing or obstructive CAD detected on computed tomography coronary angiography should be admitted for further evaluation, with a strong consideration for coronary angiography. For patients with borderline obstructive CAD (≥0%–70% stenosis) identified on computed tomography coronary angiography not classified as high risk, fractional flow reserve-computed tomography or stress testing may be considered before proceeding with invasive coronary angiography.5
Patients with no or mild ischemia on stress testing, nonobstructive CAD, or obstructive CAD with fractional flow reserve-computed tomography >0.8 should be considered for discharge. Addition of preventive medical therapy should be implemented, as outlined in Section 5.8.4. Early follow-up with a PCP and/or established cardiologist is recommended after discharge to ensure appropriate implementation of risk factor modification therapies.
5.8.3. High-Risk or Abnormal Classification by CDP
The majority of patients who are classified as abnormal or high risk by hs-cTn–based CDPs will require hospital admission and/or cardiology consultation before discharge. Patients should be classified according to the Universal Definition of MI (see Section 5.7) as having type 1 or 2 MI or acute or chronic myocardial injury. Patients diagnosed with type 1 MI should be admitted and managed according to the ACC/AHA STEMI and NSTE-ACS guidelines.12,13,129 Close outpatient cardiology follow-up and referral to cardiac rehabilitation are recommended on discharge.
Patients diagnosed with type 2 MI or acute myocardial injury should be admitted by the most appropriate hospital team (medicine, surgery, or cardiology) for treatment of the underlying precipitant for their MI or injury. Management recommendations for patients with type 2 MI and acute myocardial injury, including considerations for cardiac testing and preventive therapy initiation, are outlined in Section 5.7. Importantly, because patients with type 2 MI and myocardial injury are at high risk for subsequent adverse cardiac events,136 outpatient follow-up with cardiology is recommended, as it has been associated with greater initiation of secondary prevention recommendations156 and may be associated with improved outcomes.157 Disposition of patients with chronic myocardial injury (elevated hs-cTn without significant change over serial sampling) should be individualized. These patients do not routinely require admission or cardiology consultation unless there is an indication for admission other than an elevated hs-cTn level. Because of the association of chronic myocardial injury with underlying structural and functional cardiovascular abnormalities, additional imaging with TTE as an outpatient with subsequent cardiology follow-up is recommended for those who have not had a TTE recently. Recommendations on cardiovascular disease prevention approaches for chronic myocardial injury are discussed in Section 5.7.3.
5.8.4. Abnormal Findings Detected on Noninvasive Cardiac Testing
5.8.4.1. Incidental Findings
Incidental nonurgent/emergent findings detected on CTA are not uncommon158 and therefore should be clearly documented in discharge information, which should be sent to the PCP. Arrangements for subsequent imaging (either surveillance or additional dedicated testing), if required, should be coordinated by the PCP following discharge. If the patient does not have an identified provider, referral to one or to a dedicated ED acute-care follow-up clinic should be performed.
5.8.4.2. Nonobstructive Coronary Artery Disease
It is now recognized that a large number of MIs arise from nonobstructive coronary lesions. Intensification of preventive therapies among patients with obstructive and nonobstructive CAD can reduce progression of CAD and may prevent subsequent cardiac events. However, approximately one-half of patients identified as having nonobstructive CAD on computed tomography coronary angiography in the ED are not discharged on lipid-lowering therapy or aspirin.159 This likely reflects, in part, an absence of dedicated clinical trials of preventive therapies for nonobstructive CAD, including those performed in patients presenting with acute chest pain, and an ED focus on the disposition and acute rather than long-term management of these patients. Observational studies have indicated that statins are associated with lower risk of all-cause mortality and cardiovascular events among patients with nonobstructive CAD.160 Similarly, aspirin has been associated with a lower risk of cardiovascular events in high-risk individuals.161
Until further data from clinical trials emerge, we advise that statin therapy should be initiated for patients diagnosed with nonobstructive CAD or those with CAC ≥100 from the ED. Initiation of aspirin may also be reasonable for patients with nonobstructive CAD or those with CAC ≥100 who have a low bleeding risk.162
6. CONCLUSIONS AND IMPLICATIONS
A systematic approach—both at the level of the institution and the individual patient—is essential to achieve optimal outcomes for patients presenting with chest pain to the ED. At the institution level, this Expert Consensus Decision Pathway recommends implementation of hs-cTn assays in conjunction with a CDP to reduce ED “dwell” times and increase the proportion of patients with chest pain who can safely be discharged without additional testing. Successful implementation will decrease ED crowding and limit unnecessary testing. At the individual patient level, this document aims to provide structure for the ED evaluation of chest pain, accelerating the evaluation process and matching the intensity of testing and treatment to patient risk. This evaluation includes careful ECG review and, for appropriate patients, entry into a CDP that combines hs-cTn measurements with risk assessment and selective use of noninvasive testing. The CDP is used to help to guide triage, treatment, and disposition decisions. The CDP should be viewed as a tool to augment rather than replace the clinical judgment of the care team.
Supplementary Material
Appendix
APPENDIX 1.
AUTHOR RELATIONSHIPS WITH INDUSTRY AND OTHER ENTITIES (RELEVANT)—2022 ACC EXPERT CONSENSUS DECISION PATHWAY ON THE EVALUATION AND DISPOSITION OF ACUTE CHEST PAIN IN THE EMERGENCY DEPARTMENT
| Committee Member | Employment | Consultant | Speakers Bureau |
Ownership/ Partnership/ Principal |
Personal Research | Institutional, Organizational, or Other Financial Benefit | Expert Witness |
|---|---|---|---|---|---|---|---|
| Michael C. Kontos (Chair) |
Virginia Commonwealth University Department of Internal Medicine Division of Cardiology—Professor, Medical Director, Coronary Intensive Care Unit; Co-Director, Chest Pain Center | None | None | None | None | None | None |
| James A. de Lemos (Vice Chair) | UT Southwestern Medical School—Professor of Medicine; Kern Wildenthal MD, PhD Distinguished Chair in Cardiology |
|
None | None | None | None | |
| Steven B. Deitelzweig | Ochsner Health System—Chairman for Hospital Medicine | Pfizer* | None | None |
|
None | None |
| Deborah B. Diercks | UT Southwestern Medical School—Professor and Chair of Emergency Medicine | ETHealthcare | None | None | None | None | |
| M. Odette Gore | Department of Medicine, Division of Cardiology, the University of Colorado Anschutz Medical Campus and Denver Health and Hospital Authority—Assistant Professor of Medicine | None | None | None | None | None | None |
| Erik P. Hess | Vanderbilt University Medical Center—Professor and Chair, Department of Emergency Medicine | None | None | None | None | None | None |
| Cian P. McCarthy | Massachusetts General Hospital—Cardiology Fellow | None | None | None | None | None | None |
| James K. McCord | Henry Ford Hospital Heart and Vascular Institute—Associate Professor of Medicine | None | None | None | |||
| Paul I. Musey Jr | Indiana University School of Medicine—Associate Professor of Emergency Medicine | None | None | None | None | None | None |
| Todd C. Villines | University of Virginia—Julian Ruffin Beckwith Distinguished Professor of Medicine, Division of Cardiovascular Medicine | None | None | None | None | None | None |
| Leesa J. Wright | Methodist University Hospital—Cardiovascular Institute Outreach Coordinator | None | None | None | None | None | None |
This table represents all relationships of committee members with industry and other entities that were reported by authors, including those not deemed to be relevant to this document, at the time this document was under development. The table does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$5,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person’s gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted. Please refer to http://www.acc.org/guidelines/about-guidelines-and-clinical-documents/relationships-with-industry-policy for definitions of disclosure categories or additional information about the ACC/AHA Disclosure Policy for Writing Committees.
Significant relationship.
No financial benefit.
ACC = American College of Cardiology; CTSN = Cardiothoracic Surgical Trials Network; DSMB = Data Management Safety Board; JAMA = Journal of the American Medical Association; NHLBI = National Heart, Lung, and Blood Institute; NIH = National Institutes of Health; SAEM = Society of Academic Emergency Medicine; VCSQI = Virginia Cardiac Services Quality Initiative; VHAC = Veterans’ Health Advisory Council.
APPENDIX 2.
PEER REVIEWER RELATIONSHIPS WITH INDUSTRY AND OTHER ENTITIES (COMPREHENSIVE)—2022 ACC EXPERT CONSENSUS DECISION PATHWAY ON THE EVALUATION AND DISPOSITION OF ACUTE CHEST PAIN IN THE EMERGENCY DEPARTMENT
| Reviewer | Representation | Employment | Consultant | Speakers Bureau | Ownership/Partnership/Principal | Research/Research Grants | Institutional, Organizational, or Other Financial Benefit | Expert Witness |
|---|---|---|---|---|---|---|---|---|
| H. Vernon Anderson | Official Reviewer—ACC/AHA Chest Pain and Acute MI Data Standards | McGovern Medical School, University of Texas Health Science Center at Houston—Professor | None | None | None | None |
|
None |
| Robert H. Christenson | Content Reviewer—Roundtable attendee | University of Maryland School of Medicine—Professor of Pathology and Professor of Medical and Research Technology |
|
None | None | None | None | |
| Steven M. Hollenberg | Content Reviewer—Roundtable attendee | Emory University School of Medicine—Professor | None | None | None | None | None | None |
| Seth Gemme | Content Reviewer—Roundtable attendee | Baystate Medical Center—Chief, Department of Emergency Medicine | None | None | None | None | None | None |
| Martha Gulati | Official Reviewer—2021 AHA/ACC Multisociety Chest Pain Guideline | The University of Arizona Phoenix—Professor of Medicine & Chief of Cardiology | None | None | None | None | None | None |
| Hani Jneid | Content Reviewer—Roundtable attendee | Baylor College of Medicine—Associate Professor of Medicine | None | None | None | None | None | None |
| Chayakrit Krittanawong | Official Reviewer—Solution Set Oversight Committee | Baylor College of Medicine—Clinical Fellow | None | None | None | None | None | None |
| L. Kristin Newby | Content Reviewer—Roundtable attendee | Duke University Medical Center—Professor of Medicine |
|
None | None | None | ||
| Rebecca Vigen | Content Reviewer—Roundtable attendee | University of Texas Southwestern Medical Center—Assistant Professor of Medicine | None | None | None | RCE Technologies* | None | None |
| David E. Winchester | Content Reviewer—Roundtable attendee | University of Florida–Associate Professor of Medicine and Radiology | None | None | None | None | Alachua County Medical Society Board of Directors† |
This table represents all relationships of reviewers with industry and other entities that were reported by authors, including those not deemed to be relevant to this document, at the time this document was under development. The table does not necessarily reflect relationships with industry at the time of publication. A person is deemed to have a significant interest in a business if the interest represents ownership of ≥5% of the voting stock or share of the business entity, or ownership of ≥$5,000 of the fair market value of the business entity; or if funds received by the person from the business entity exceed 5% of the person’s gross income for the previous year. Relationships that exist with no financial benefit are also included for the purpose of transparency. Relationships in this table are modest unless otherwise noted. Please refer to http://www.acc.org/guidelines/about-guidelines-and-clinicaldocuments/relationships-with-industry-policy for definitions of disclosure categories or additional information about the ACC/AHA Disclosure Policy for Writing Committees.
No financial benefit.
Significant relationship.
ACC = American College of Cardiology; AHA = American Heart Association; CAD = coronary artery disease; DHHS = Department of Health & Human Services; JACC = Journal of the American College of Cardiology; MI = myocardial infarction; MURDOCK = Measurement to Understand Reclassification of Disease of Cabbarrus and Kannapolis; NHLBI = National Heart, Lung, and Blood Institute; NIH = National Institutes of Health
APPENDIX 3. ABBREVIATIONS
- ACC
American College of Cardiology
- ACS
acute coronary syndrome
- AHA
American Heart Association
- CAC
coronary artery calcium
- CAD
coronary artery disease
- CDP
clinical decision pathway
- cTn
cardiac troponin
- CTA
computed tomography angiography
- ECG
electrocardiogram
- ED
emergency department
- EDACS
Emergency Department Assessment of Chest Pain Score
- eGFR
estimated glomerular filtration rate
- ESC
European Society of Cardiology
- FDA
U.S. Food and Drug Administration
- HEART
History, ECG, Age, Risk Factors, and Troponin
- High-STEACS
High-Sensitivity Troponin in the Evaluation of Patients with Acute Coronary Syndrome
- hs-cTn
high-sensitivity cardiac troponin
- hs-cTnI
high-sensitivity cardiac troponin I
- hs-cTnT
high-sensitivity cardiac troponin T
- LBBB
left bundle branch block
- LoD
limit of detection
- LoQ
limit of quantification
- MI
myocardial infarction
- NPV
negative predictive value
- PCP
primary care physician
- PPV
positive predictive value
- NSTE-ACS
non–ST-segment elevation acute coronary syndrome
- STEMI
ST-segment elevation myocardial infarction
- TTE
transthoracic echocardiography
- URL
upper reference limit
Footnotes
This document was approved by the American College of Cardiology Clinical Policy Approval Committee in September 2022.
Copies: This document is available on the website of the American College of Cardiology (www.acc.org).
PRESIDENT AND STAFF
Edward T.A. Fry, MD, FACC, President
Cathleen C. Gates, Chief Executive Officer
Richard J. Kovacs, MD, MACC, Chief Medical Officer
Brendan Mullen Sr. Executive Vice President, Science & Quality
Joseph M. Allen, MA, Team Lead, Clinical Standards and Solution Sets
Amy Dearborn, Team Lead, Clinical Policy Content Development
Ashleigh M. Covington, MA, Team Lead, Clinical Pathways and Heart House Roundtables
Amanda B. Ladden-Stirling, MPP, Clinical Pathways and Heart House Roundtables
Grace D. Ronan, Team Lead, Clinical Policy Publications
REFERENCES
- 1.Januzzi JL Jr, Ahmad T, Binder LG, et al. 2019 methodology for creating expert consensus decision pathways: a report of the American College of Cardiology. J Am Coll Cardiol 2019;74:1138–1150. [DOI] [PubMed] [Google Scholar]
- 2.Cairns C, Kang K, Santoc L. National Hospital Ambulatory Medical Care Survey: 2018 emergency department summary tables U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 3.Lindsell CJ, Anantharaman V, Diercks D, et al. The Internet Tracking Registry of Acute Coronary Syndromes (i*trACS): a multicenter registry of patients with suspicion of acute coronary syndromes reported using the standardized reporting guidelines for emergency department chest pain studies. Ann Emerg Med 2006;48:666–677, 677.e661–669. [DOI] [PubMed] [Google Scholar]
- 4.Hsia RY, Hale Z, Tabas JA. A national study of the prevalence of life-threatening diagnoses in patients with chest pain. JAMA Intern Med 2016;176:1029–1032. [DOI] [PubMed] [Google Scholar]
- 5.Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the evaluation and diagnosis of chest pain: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2021;78:e187–e285. [DOI] [PubMed] [Google Scholar]
- 6.Collet JP, Thiele H, Barbato E, et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–1367. [DOI] [PubMed] [Google Scholar]
- 7.Wu AHB, Christenson RH, Greene DN, et al. Clinical laboratory practice recommendations for the use of cardiac troponin in acute coronary syndrome: expert opinion from the Academy of the American Association for Clinical Chemistry and the Task Force on Clinical Applications of Cardiac Bio-Markers of the International Federation of Clinical Chemistry and Laboratory Medicine. Clin Chem 2018;64:645–655. [DOI] [PubMed] [Google Scholar]
- 8.Apple FS, Wu AHB, Sandoval Y, et al. Sex-Specific 99th percentile upper reference limits for high sensitivity cardiac troponin assays derived using a universal sample bank. Clin Chem 2020;66:434–444. [DOI] [PubMed] [Google Scholar]
- 9.Sgarbossa EB, Pinski SL, Barbagelata A, et al. , for the GUSTO-1 (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) Investigators. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med 1996;334:481–487. [DOI] [PubMed] [Google Scholar]
- 10.Smith SW, Dodd KW, Henry TD, et al. Diagnosis of ST-elevation myocardial infarction in the presence of left bundle branch block with the ST-elevation to S-wave ratio in a modified Sgarbossa rule. Ann Emerg Med 2012;60:766–776. [DOI] [PubMed] [Google Scholar]
- 11.Meyers HP, Limkakeng AT Jr, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: a retrospective case-control study. Am Heart J 2015;170:1255–1264. [DOI] [PubMed] [Google Scholar]
- 12.O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78–e140. [DOI] [PubMed] [Google Scholar]
- 13.Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139–e228. [DOI] [PubMed] [Google Scholar]
- 14.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol 2018;72:2231–2264. [DOI] [PubMed] [Google Scholar]
- 15.Januzzi JL Jr, Mahler SA, Christenson RH, et al. Recommendations for institutions transitioning to high-sensitivity troponin testing: JACC Scientific Expert Panel. J Am Coll Cardiol 2019;73:1059–1077. [DOI] [PubMed] [Google Scholar]
- 16.De Bie J, Martignani C, Massaro G, et al. Performance of seven ECG interpretation programs in identifying arrhythmia and acute cardiovascular syndrome. J Electrocardiol 2020;58:143–149. [DOI] [PubMed] [Google Scholar]
- 17.McCabe JM, Armstrong EJ, Ku I, et al. Physician accuracy in interpreting potential ST-segment elevation myocardial infarction electrocardiograms. J Am Heart Assoc 2013;2:e000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion. N Engl J Med 2008;359:2071–2073. [DOI] [PubMed] [Google Scholar]
- 19.Wagner GS, Macfarlane P, Wellens H, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part VI: acute ischemia/infarction: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. J Am Coll Cardiol 2009;53:1003–1011. [DOI] [PubMed] [Google Scholar]
- 20.Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac cath lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction. Am Heart J 2010;160:995–1003, 1003.e1001–1008. [DOI] [PubMed] [Google Scholar]
- 21.Meyers HP, Bracey A, Lee D, et al. Comparison of the ST-elevation myocardial infarction (STEMI) vs. NSTEMI and occlusion MI (OMI) vs. NOMI paradigms of acute MI. J Emerg Med 2021;60:273–284. [DOI] [PubMed] [Google Scholar]
- 22.Ohlsson M, Ohlin H, Wallerstedt SM, et al. Usefulness of serial electrocardiograms for diagnosis of acute myocardial infarction. Am J Cardiol 2001;88: 478–481. [DOI] [PubMed] [Google Scholar]
- 23.Fesmire FM. Which chest pain patients potentially benefit from continuous 12-lead ST-segment monitoring with automated serial ECG? Am J Emerg Med 2000;18:773–778. [DOI] [PubMed] [Google Scholar]
- 24.Fesmire FM, Percy RF, Bardoner JB, et al. Usefulness of automated serial 12-lead ECG monitoring during the initial emergency department evaluation of patients with chest pain. Ann Emerg Med 1998;31:3–11. [DOI] [PubMed] [Google Scholar]
- 25.Chase M, Brown AM, Robey JL, et al. Prognostic value of symptoms during a normal or nonspecific electrocardiogram in emergency department patients with potential acute coronary syndrome. Acad Emerg Med 2006;13:1034–1039. [DOI] [PubMed] [Google Scholar]
- 26.Turnipseed SD, Trythall WS, Diercks DB, et al. Frequency of acute coronary syndrome in patients with normal electrocardiogram performed during presence or absence of chest pain. Acad Emerg Med 2009;16: 495–499. [DOI] [PubMed] [Google Scholar]
- 27.Chapman AR, Lee KK, McAllister DA, et al. Association of high-sensitivity cardiac troponin I concentration with cardiac outcomes in patients with suspected acute coronary syndrome. JAMA 2017;318:1913–1924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martí D, Salido L, Mestre JL, et al. Usefulness of reciprocal changes in the diagnosis of myocardial infarction with minimal ST-segment elevation. Rev Esp Cardiol (Engl Ed) 2016;69:706–707. [DOI] [PubMed] [Google Scholar]
- 29.Martí D, Mestre JL, Salido L, et al. Incidence, angiographic features and outcomes of patients presenting with subtle ST-elevation myocardial infarction. Am Heart J 2014;168:884–890. [DOI] [PubMed] [Google Scholar]
- 30.Pride YB, Tung P, Mohanavelu S, et al. Angiographic and clinical outcomes among patients with acute coronary syndromes presenting with isolated anterior ST-segment depression: a TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis In Myocardial Infarction 38) substudy. J Am Coll Cardiol Intv 2010;3:806–811. [DOI] [PubMed] [Google Scholar]
- 31.Neeland IJ, Kontos MC, de Lemos JA. Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. J Am Coll Cardiol 2012;60:96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dodd KW, Zvosec DL, Hart MA, et al. Electrocardiographic diagnosis of acute coronary occlusion myocardial infarction in ventricular paced rhythm using the modified Sgarbossa criteria. Ann Emerg Med 2021;78:517–529. [DOI] [PubMed] [Google Scholar]
- 33.de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J 1982;103:730–736. [DOI] [PubMed] [Google Scholar]
- 34.Yan AT, Yan RT, Kennelly BM, et al. Relationship of ST elevation in lead aVR with angiographic findings and outcome in non-ST elevation acute coronary syndromes. Am Heart J 2007;154:71–78. [DOI] [PubMed] [Google Scholar]
- 35.Harhash AA, Huang JJ, Reddy S, et al. aVR ST segment elevation: acute STEMI or not? Incidence of an acute coronary occlusion. Am J Med 2019;132:622–630. [DOI] [PubMed] [Google Scholar]
- 36.Gibbs MA, Leedekerken JB, Littmann L. Evolution of our understanding of the aVR sign. J Electrocardiol 2019;56:121–124. [DOI] [PubMed] [Google Scholar]
- 37.Knotts RJ, Wilson JM, Kim E, et al. Diffuse ST depression with ST elevation in aVR: Is this pattern specific for global ischemia due to left main coronary artery disease? J Electrocardiol 2013;46:240–248. [DOI] [PubMed] [Google Scholar]
- 38.Kaul P, Fu Y, Chang WC, et al. , for the PARAGON-A and GUSTO-IIb Investigators. Prognostic value of ST segment depression in acute coronary syndromes: insights from PARAGON-A applied to GUSTO-IIb. J Am Coll Cardiol 2001;38:64–71. [DOI] [PubMed] [Google Scholar]
- 39.Apple FS, Jaffe AS, Collinson P, et al. IFCC educational materials on selected analytical and clinical applications of high sensitivity cardiac troponin assays. Clin Biochem 2015;48:201–203. [DOI] [PubMed] [Google Scholar]
- 40.Agewall S, Giannitsis E, Jernberg T, et al. Troponin elevation in coronary vs. non-coronary disease. Eur Heart J 2011;32:404–411. [DOI] [PubMed] [Google Scholar]
- 41.Alpert JS, Thygesen K, Antman E, et al. Myocardial infarction redefined—a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol 2000;36:959–969. [DOI] [PubMed] [Google Scholar]
- 42.de Lemos JA, Drazner MH, Omland T, et al. Association of troponin T detected with a highly sensitive assay and cardiac structure and mortality risk in the general population. JAMA 2010;304: 2503–2512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saunders JT, Nambi V, de Lemos JA, et al. Cardiac troponin T measured by a highly sensitive assay predicts coronary heart disease, heart failure, and mortality in the Atherosclerosis Risk in Communities Study. Circulation 2011;123:1367–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jia X, Sun W, Hoogeveen RC, et al. High-sensitivity troponin I and incident coronary events, stroke, heart failure hospitalization, and mortality in the ARIC study. Circulation 2019;139:2642–2653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McCarthy CP, Raber I, Chapman AR, et al. Myocardial injury in the era of high-sensitivity cardiac troponin assays: A practical approach for clinicians. JAMA Cardiol 2019;4:1034–1042. [DOI] [PubMed] [Google Scholar]
- 46.Wereski R, Kimenai DM, Taggart C, et al. Cardiac troponin thresholds and kinetics to differentiate myocardial injury and myocardial infarction. Circulation 2021;144:528–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mueller-Hennessen M, Mueller C, Giannitsis E, et al. Serial sampling of high-sensitivity cardiac troponin T may not be required for prediction of acute myocardial infarction diagnosis in chest pain patients with highly abnormal concentrations at presentation. Clin Chem 2017;63:542–551. [DOI] [PubMed] [Google Scholar]
- 48.Boeddinghaus J, Nestelberger T, Badertscher P, et al. Predicting acute myocardial infarction with a single blood draw. Clin Chem 2019;65:437–450. [DOI] [PubMed] [Google Scholar]
- 49.Arruda-Olson AM, Roger VL, Jaffe AS, et al. Troponin T levels and infarct size by SPECT myocardial perfusion imaging. J Am Coll Cardiol Img 2011;4:523–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Januzzi JL Jr, McCarthy CP. Cardiac troponin and the true false positive. J Am Coll Cardiol Case Rep 2020;2:461–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Akhtar Z, Dargan J, Gaze D, et al. False-positive troponin elevation due to an immunoglobulin-G-cardiac troponin T complex: a case report. Eur Heart J Case Rep 2020;4:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reichlin T, Irfan A, Twerenbold R, et al. Utility of absolute and relative changes in cardiac troponin concentrations in the early diagnosis of acute myocardial infarction. Circulation 2011;124:136–145. [DOI] [PubMed] [Google Scholar]
- 53.McCord J, Newby LK, deFilippi CR. Designing a better mousetrap: reflections on the November 28, 2017, US Food and Drug Administration meeting on next-generation “high-sensitivity” cardiac troponin assays to diagnose myocardial infarction. Circulation 2018;138:316–318. [DOI] [PubMed] [Google Scholar]
- 54.Gore MO, Seliger SL, Defilippi CR, et al. Age- and sex-dependent upper reference limits for the high-sensitivity cardiac troponin T assay. J Am Coll Cardiol 2014;63:1441–1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hackler E 3rd, Lew J, Gore MO, et al. Racial differences in cardiovascular biomarkers in the general population. J Am Heart Assoc 2019;8:e012729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wenger NK. Women and coronary heart disease: a century after Herrick: understudied, underdiagnosed, and undertreated. Circulation 2012;126: 604–611. [DOI] [PubMed] [Google Scholar]
- 57.Mnatzaganian G, Hiller JE, Braitberg G, et al. Sex disparities in the assessment and outcomes of chest pain presentations in emergency departments. Heart 2020;106:111–118. [DOI] [PubMed] [Google Scholar]
- 58.Shah AS, Griffiths M, Lee KK, et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ 2015;350:g7873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee KK, Ferry AV, Anand A, et al. Sex-specific thresholds of high-sensitivity troponin in patients with suspected acute coronary syndrome. J Am Coll Cardiol 2019;74:2032–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Forman DE, de Lemos JA, Shaw LJ, et al. Cardiovascular biomarkers and imaging in older adults: JACC council perspectives. J Am Coll Cardiol 2020;76:1577–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Anand A, Lee KK, Chapman AR, et al. High-sensitivity cardiac troponin on presentation to rule out myocardial infarction: a stepped-wedge cluster randomized controlled trial. Circulation 2021;143:2214–2224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sandoval Y, Smith SW, Schulz K, et al. Comparison of 0/3-hour rapid rule-out strategies using high-sensitivity cardiac troponin I in a US emergency department. Circ Cardiovasc Qual Outcomes 2020;13: e006565. [DOI] [PubMed] [Google Scholar]
- 63.Chiang CH, Chiang CH, Pickering JW, et al. Performance of the European Society of Cardiology 0/1-hour, 0/2-hour, and 0/3-hour algorithms for rapid triage of acute myocardial infarction : An international collaborative meta-analysis. Ann Intern Med 2022;175: 101–113. [DOI] [PubMed] [Google Scholar]
- 64.Body R, Carley S, McDowell G, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol 2011;58:1332–1339. [DOI] [PubMed] [Google Scholar]
- 65.Shah AS, Anand A, Sandoval Y, et al. High-sensitivity cardiac troponin I at presentation in patients with suspected acute coronary syndrome: a cohort study. Lancet 2015;386:2481–2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Body R, Mueller C, Giannitsis E, et al. The use of very low concentrations of high-sensitivity troponin T to rule out acute myocardial infarction using a single blood test. Acad Emerg Med 2016;23:1004–1013. [DOI] [PubMed] [Google Scholar]
- 67.Pickering JW, Than MP, Cullen L, et al. Rapid rule-out of acute myocardial infarction with a single high-sensitivity cardiac troponin T measurement below the limit of detection: A collaborative meta-analysis. Ann Intern Med 2017;166:715–724. [DOI] [PubMed] [Google Scholar]
- 68.Chew DP, Lambrakis K, Blyth A, et al. A randomized trial of a 1-Hour troponin T protocol in suspected acute coronary syndromes: The rapid assessment of possible acute coronary syndrome in the emergency department with high-sensitivity troponin T study (RAPID-TnT). Circulation 2019; 140:1543–1556. [DOI] [PubMed] [Google Scholar]
- 69.Bularga A, Lee KK, Stewart S, et al. High-sensitivity troponin and the application of risk stratification thresholds in patients with suspected acute coronary syndrome. Circulation 2019;140:1557–1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chapman AR, Fujisawa T, Lee KK, et al. Novel high-sensitivity cardiac troponin I assay in patients with suspected acute coronary syndrome. Heart 2019;105: 616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sandoval Y, Nowak R, deFilippi CR, et al. Myocardial infarction risk stratification with a single measurement of high-sensitivity troponin I. J Am Coll Cardiol 2019;74:271–282. [DOI] [PubMed] [Google Scholar]
- 72.McRae AD, Innes G, Graham M, et al. Undetectable concentrations of a Food and Drug Administration-approved high-sensitivity cardiac troponin T assay to rule out acute myocardial infarction at emergency department arrival. Acad Emerg Med 2017;24:1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Peacock WF, Baumann BM, Bruton D, et al. Efficacy of high-sensitivity troponin T in identifying very-low-risk patients with possible acute coronary syndrome. JAMA Cardiol 2018;3:104–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet 2018;392: 919–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chapman AR, Sandeman D, Ferry AV, et al. Risk stratification using high-sensitivity cardiac troponin T in patients with suspected acute coronary syndrome. J Am Coll Cardiol 2020;75:985–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mueller C, Giannitsis E, Christ M, et al. Multicenter evaluation of a 0-Hour/1-Hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin T. Ann Emerg Med 2016;68:76–87. e74. [DOI] [PubMed] [Google Scholar]
- 77.Reichlin T, Schindler C, Drexler B, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012;172:1211–1218. [DOI] [PubMed] [Google Scholar]
- 78.Boeddinghaus J, Twerenbold R, Nestelberger T, et al. Clinical validation of a novel high-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin Chem 2018;64:1347–1360. [DOI] [PubMed] [Google Scholar]
- 79.Boeddinghaus J, Nestelberger T, Twerenbold R, et al. High-sensitivity cardiac troponin I assay for early diagnosis of acute myocardial infarction. Clin Chem 2019;65:893–904. [DOI] [PubMed] [Google Scholar]
- 80.Neumann JT, Twerenbold R, Ojeda F, et al. Application of high-sensitivity troponin in suspected myocardial infarction. N Engl J Med 2019;380:2529–2540. [DOI] [PubMed] [Google Scholar]
- 81.Twerenbold R, Costabel JP, Nestelberger T, et al. Outcome of applying the ESC 0/1-hour algorithm in patients with suspected myocardial infarction. J Am Coll Cardiol 2019;74:483–494. [DOI] [PubMed] [Google Scholar]
- 82.Nestelberger T, Boeddinghaus J, Wussler D, et al. Predicting major adverse events in patients with acute myocardial infarction. J Am Coll Cardiol 2019;74:842–854. [DOI] [PubMed] [Google Scholar]
- 83.Twerenbold R, Badertscher P, Boeddinghaus J, et al. Effect of the FDA regulatory approach on the 0/1-h algorithm for rapid diagnosis of MI. J Am Coll Cardiol 2017;70:1532–1534. [DOI] [PubMed] [Google Scholar]
- 84.Peacock WF, Christenson R, Diercks DB, et al. Myocardial infarction can be safely excluded by high-sensitivity troponin I testing 3 hours after emergency department presentation. Acad Emerg Med 2020;27: 671–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pickering JW, Greenslade JH, Cullen L, et al. Assessment of the European Society of Cardiology 0-Hour/1-Hour algorithm to rule-out and rule-in acute myocardial infarction. Circulation 2016;134:1532–1541. [DOI] [PubMed] [Google Scholar]
- 86.Twerenbold R, Neumann JT, Sörensen NA, et al. Prospective validation of the 0/1-h algorithm for early diagnosis of myocardial infarction. J Am Coll Cardiol 2018;72:620–632. [DOI] [PubMed] [Google Scholar]
- 87.Nowak RM, Christenson RH, Jacobsen G, et al. Performance of novel high-sensitivity cardiac troponin I assays for 0/1-hour and 0/2- to 3-hour evaluations for acute myocardial infarction: results from the HIGH-US study. Ann Emerg Med 2020;76:1–13. [DOI] [PubMed] [Google Scholar]
- 88.Burgos LM, Trivi M, Costabel JP. Performance of the European Society of Cardiology 0/1-hour algorithm in the diagnosis of myocardial infarction with high-sensitivity cardiac troponin: Systematic review and meta-analysis. Eur Heart J Acute Cardiovasc Care 2020:2048872620935399. [DOI] [PubMed] [Google Scholar]
- 89.Badertscher P, Boeddinghaus J, Twerenbold R, et al. Direct comparison of the 0/1h and 0/3h algorithms for early rule-out of acute myocardial infarction. Circulation 2018;137:2536–2538. [DOI] [PubMed] [Google Scholar]
- 90.Reichlin T, Hochholzer W, Bassetti S, et al. Early diagnosis of myocardial infarction with sensitive cardiac troponin assays. N Engl J Med 2009;361:858–867. [DOI] [PubMed] [Google Scholar]
- 91.Haller PM, Boeddinghaus J, Neumann JT, et al. Performance of the ESC 0/1-h and 0/3-h algorithm for the rapid identification of myocardial infarction without ST-elevation in patients with diabetes. Diabetes Care 2020;43:460–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Boeddinghaus J, Nestelberger T, Twerenbold R, et al. Impact of age on the performance of the ESC 0/1h-algorithms for early diagnosis of myocardial infarction. Eur Heart J 2018;39:3780–3794. [DOI] [PubMed] [Google Scholar]
- 93.Twerenbold R, Badertscher P, Boeddinghaus J, et al. 0/1-hour triage algorithm for myocardial infarction in patients with renal dysfunction. Circulation 2018;137:436–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Vigen R, Kutscher P, Fernandez F, et al. Evaluation of a novel rule-out myocardial infarction protocol incorporating high-sensitivity troponin T in a US hospital. Circulation 2018;138:2061–2063. [DOI] [PubMed] [Google Scholar]
- 95.Vigen R, Diercks DB, Hashim IA, et al. Association of a novel protocol for rapid exclusion of myocardial infarction with resource use in a US safety net hospital. JAMA Netw Open 2020;3:e203359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lopez-Ayala P, Nestelberger T, Boeddinghaus J, et al. Novel criteria for the observe-zone of the ESC 0/1h-hs-cTnT algorithm. Circulation 2021;144:773–787. [DOI] [PubMed] [Google Scholar]
- 97.Bjurman C, Larsson M, Johanson P, et al. Small changes in troponin T levels are common in patients with non-ST-segment elevation myocardial infarction and are linked to higher mortality. J Am Coll Cardiol 2013;62:1231–1238. [DOI] [PubMed] [Google Scholar]
- 98.deFilippi C, Seliger SL, Kelley W, et al. Interpreting cardiac troponin results from high-sensitivity assays in chronic kidney disease without acute coronary syndrome. Clin Chem 2012;58:1342–1351. [DOI] [PubMed] [Google Scholar]
- 99.Gallacher PJ, Miller-Hodges E, Shah ASV, et al. Use of high-sensitivity cardiac troponin in patients with kidney impairment: a randomized clinical trial. JAMA Intern Med 2021;181:1237–1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Miller-Hodges E, Anand A, Shah ASV, et al. High-sensitivity cardiac troponin and the risk stratification of patients with renal impairment presenting with suspected acute coronary syndrome. Circulation 2018;137:425–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Limkakeng AT Jr, Hertz J, Lerebours R, et al. Ideal high sensitivity troponin baseline cutoff for patients with renal dysfunction. Am J Emerg Med 2021;46:170–175. [DOI] [PubMed] [Google Scholar]
- 102.Ganguli I, Cui J, Thakore N, et al. Downstream cascades of care following high-sensitivity troponin test implementation. J Am Coll Cardiol 2021;77:3171–3179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sandoval Y, Askew JW 3rd, Newman JS, et al. Implementing high-sensitivity cardiac troponin T in a US regional healthcare system. Circulation 2020;141: 1937–1939. [DOI] [PubMed] [Google Scholar]
- 104.Chapman AR, Adamson PD, Shah ASV, et al. High-sensitivity cardiac troponin and the universal definition of myocardial infarction. Circulation 2020;141:161–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Ola O, Akula A, De Michieli L, et al. Clinical impact of high-sensitivity cardiac troponin T implementation in the community. J Am Coll Cardiol 2021;77:3160–3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ford JS, Chaco E, Tancredi DJ, et al. Impact of high-sensitivity cardiac troponin implementation on emergency department length of stay, testing, admissions, and diagnoses. Am J Emerg Med 2021;45:54–60. [DOI] [PubMed] [Google Scholar]
- 107.Mahler SA, Riley RF, Hiestand BC, et al. The HEART Pathway randomized trial: identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes 2015;8:195–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Mahler SA, Lenoir KM, Wells BJ, et al. Safely identifying emergency department patients with acute chest pain for early discharge. Circulation 2018;138: 2456–2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Than M, Flaws D, Sanders S, et al. Development and validation of the emergency department assessment of chest pain score and 2 h accelerated diagnostic protocol. Emerg Med Australas 2014;26:34–44. [DOI] [PubMed] [Google Scholar]
- 110.Stopyra J, Snavely AC, Hiestand B, et al. Comparison of accelerated diagnostic pathways for acute chest pain risk stratification. Heart 2020;106:977–984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mark DG, Huang J, Chettipally U, et al. Performance of coronary risk scores among patients with chest pain in the emergency department. J Am Coll Cardiol 2018;71:606–616. [DOI] [PubMed] [Google Scholar]
- 112.Reaney PDW, Elliott HI, Noman A, et al. Risk stratifying chest pain patients in the emergency department using HEART, GRACE and TIMI scores, with a single contemporary troponin result, to predict major adverse cardiac events. Emerg Med J 2018;35:420–427. [DOI] [PubMed] [Google Scholar]
- 113.Than M, Cullen L, Aldous S, et al. 2-hour accelerated diagnostic protocol to assess patients with chest pain symptoms using contemporary troponins as the only biomarker: the ADAPT trial. J Am Coll Cardiol 2012;59:2091–2098. [DOI] [PubMed] [Google Scholar]
- 114.Than MP, Pickering JW, Aldous SJ, et al. Effectiveness of EDACS versus ADAPT accelerated diagnostic pathways for chest pain: a pragmatic randomized controlled trial embedded within practice. Ann Emerg Med 2016;68:93–102. e101. [DOI] [PubMed] [Google Scholar]
- 115.Carlton EW, Ingram J, Taylor H, et al. Limit of detection of troponin discharge strategy versus usual care: randomised controlled trial. Heart 2020;106: 1586–1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chapman AR, Hesse K, Andrews J, et al. High-sensitivity cardiac troponin I and clinical risk scores in patients with suspected acute coronary syndrome. Circulation 2018;138:1654–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Allen BR, Christenson RH, Cohen SA, et al. Diagnostic performance of high-sensitivity cardiac troponin T strategies and clinical variables in a multisite US cohort. Circulation 2021;143:1659–1672. [DOI] [PubMed] [Google Scholar]
- 118.Marcusohn E, Epstein D, Roguin A, et al. Rapid rule out for suspected myocardial infarction: is the algorithm appropriate for all? Eur Heart J Qual Care Clin Outcomes 2020;6:193–198. [DOI] [PubMed] [Google Scholar]
- 119.Kirkpatrick JN, Grimm R, Johri AM, et al. Recommendations for Echocardiography Laboratories Participating in Cardiac Point of Care Cardiac Ultrasound (POCUS) and Critical Care Echocardiography Training: Report from the American Society of Echocardiography. J Am Soc Echocardiogr 2020;33:409–422.e404. [DOI] [PubMed] [Google Scholar]
- 120.Knuuti J, Ballo H, Juarez-Orozco LE, et al. The performance of non-invasive tests to rule-in and rule-out significant coronary artery stenosis in patients with stable angina: a meta-analysis focused on post-test disease probability. Eur Heart J 2018;39:3322–3330. [DOI] [PubMed] [Google Scholar]
- 121.Hulten E, Pickett C, Bittencourt MS, et al. Meta-analysis of coronary CT angiography in the emergency department. Eur Heart J Cardiovasc Imaging 2013;14: 607. [DOI] [PubMed] [Google Scholar]
- 122.Chang HJ, Lin FY, Gebow D, et al. Selective referral using CCTA versus direct referral for individuals referred to invasive coronary angiography for suspected CAD: A randomized, controlled, open-label trial. J Am Coll Cardiol Img 2019;12:1303–1312. [DOI] [PubMed] [Google Scholar]
- 123.Hulten E, Pickett C, Bittencourt MS, et al. Outcomes after coronary computed tomography angiography in the emergency department: a systematic review and meta-analysis of randomized, controlled trials. J Am Coll Cardiol 2013;61:880–892. [DOI] [PubMed] [Google Scholar]
- 124.Gray AJ, Roobottom C, Smith JE, et al. Early computed tomography coronary angiography in patients with suspected acute coronary syndrome: randomised controlled trial. BMJ 2021;374:n2106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nestelberger T, Wildi K, Boeddinghaus J, et al. Characterization of the observe zone of the ESC 2015 high-sensitivity cardiac troponin 0h/1h-algorithm for the early diagnosis of acute myocardial infarction. Int J Cardiol 2016;207:238–245. [DOI] [PubMed] [Google Scholar]
- 126.Dedic A, Kurata A, Lubbers M, et al. Prognostic implications of non-culprit plaques in acute coronary syndrome: non-invasive assessment with coronary CT angiography. Eur Heart J Cardiovasc Imaging 2014;15: 1231–1237. [DOI] [PubMed] [Google Scholar]
- 127.Pursnani A, Schlett CL, Mayrhofer T, et al. Potential for coronary CT angiography to tailor medical therapy beyond preventive guideline-based recommendations: insights from the ROMICAT I trial. J Cardiovasc Comput Tomogr 2015;9:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pursnani A, Chou ET, Zakroysky P, et al. Use of coronary artery calcium scanning beyond coronary computed tomographic angiography in the emergency department evaluation for acute chest pain: the ROMICAT II trial. Circ Cardiovasc Imaging 2015;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction. J Am Coll Cardiol 2016;67:1235–1250. [DOI] [PubMed] [Google Scholar]
- 130.DeFilippis AP, Chapman AR, Mills NL, et al. Assessment and treatment of patients with Type 2 myocardial infarction and acute nonischemic myocardial injury. Circulation 2019;140:1661–1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gard A, Lindahl B, Batra G, et al. Interphysician agreement on subclassification of myocardial infarction. Heart 2018;104:1284–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Jneid H, Addison D, Bhatt DL, et al. 2017 AHA/ACC clinical performance and quality measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol 2017;70:2048–2090. [DOI] [PubMed] [Google Scholar]
- 133.Centers for Medicare & Medicaid Services. Hospital readmissions reduction program (HRRP) Accessed January 21, 2022. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program
- 134.Centers for Medicare & Medicaid Services. The hospital value-based purchasing (VBP) program Accessed January 21, 2022. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HVBP/Hospital-Value-Based-Purchasing
- 135.McCarthy CP, Kolte D, Kennedy KF, et al. Patient characteristics and clinical outcomes of type 1 versus type 2 myocardial infarction. J Am Coll Cardiol 2021;77:848–857. [DOI] [PubMed] [Google Scholar]
- 136.Chapman AR, Shah ASV, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation 2018;137:1236–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Smilowitz NR, Subramanyam P, Gianos E, et al. Treatment and outcomes of type 2 myocardial infarction and myocardial injury compared with type 1 myocardial infarction. Coron Artery Dis 2018;29:46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.McCarthy CP, Murphy S, Cohen JA, et al. Underutilization of cardiac rehabilitation for type 2 myocardial infarction. J Am Coll Cardiol 2019;73:2005–2007. [DOI] [PubMed] [Google Scholar]
- 139.Bularga A, Hung J, Daghem M, et al. Coronary artery and cardiac disease in patients with type 2 myocardial infarction: a prospective cohort study. Circulation 2022;145:1188–1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Baron T, Hambraeus K, Sundström J, et al. Impact on long-term mortality of presence of obstructive coronary artery disease and classification of myocardial infarction. Am J Med 2016;129:398–406. [DOI] [PubMed] [Google Scholar]
- 141.Nestelberger T, Boeddinghaus J, Badertscher P, et al. Effect of definition on incidence and prognosis of type 2 myocardial infarction. J Am Coll Cardiol 2017;70:1558–1568. [DOI] [PubMed] [Google Scholar]
- 142.Lindahl B, Baron T, Erlinge D, et al. Medical therapy for secondary prevention and long-term outcome in patients with myocardial infarction with nonobstructive coronary artery disease. Circulation 2017;135:1481–1489. [DOI] [PubMed] [Google Scholar]
- 143.Fihn SD, Gardin JM, Abrams J, et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol 2012;60:e44–e164. [DOI] [PubMed] [Google Scholar]
- 144.Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:e177–e232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Virani SS, Morris PB, Agarwala A, et al. 2021 ACC expert consensus decision pathway on the management of ASCVD risk reduction in patients with persistent hypertriglyceridemia: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2021;78:960–993. [DOI] [PubMed] [Google Scholar]
- 146.Sandoval Y, Smith SW, Sexter A, et al. Type 1 and 2 myocardial infarction and myocardial injury: clinical transition to high-sensitivity cardiac troponin I. Am J Med 2017;130:1431–1439.e1434. [DOI] [PubMed] [Google Scholar]
- 147.McFalls EO, Larsen G, Johnson GR, et al. Outcomes of hospitalized patients with non-acute coronary syndrome and elevated cardiac troponin level. Am J Med 2011;124:630–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Raber I, McCarthy CP, Januzzi JL Jr. A test in context: interpretation of high-sensitivity cardiac troponin assays in different clinical settings. J Am Coll Cardiol 2021;77:1357–1367. [DOI] [PubMed] [Google Scholar]
- 149.Wallace TW, Abdullah SM, Drazner MH, et al. Prevalence and determinants of troponin T elevation in the general population. Circulation 2006;113:1958–1965. [DOI] [PubMed] [Google Scholar]
- 150.Eggers KM, Jernberg T, Lindahl B. Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol 2019;73:1–9. [DOI] [PubMed] [Google Scholar]
- 151.Everett BM, Zeller T, Glynn RJ, et al. High-sensitivity cardiac troponin I and B-type natriuretic peptide as predictors of vascular events in primary prevention: impact of statin therapy. Circulation 2015;131:1851–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Berry JD, Nambi V, Ambrosius WT, et al. Associations of high-sensitivity troponin and natriuretic peptide levels with outcomes after intensive blood pressure lowering: findings from the SPRINT randomized clinical trial. JAMA Cardiol 2021;6:1397–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Pandey A, Patel KV, Vongpatanasin W, et al. Incorporation of biomarkers into risk assessment for allocation of antihypertensive medication according to the 2017 ACC/AHA high blood pressure guideline: a pooled cohort analysis. Circulation 2019;140:2076–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Vaduganathan M, Sattar N, Xu J, et al. Stress cardiac biomarkers, cardiovascular and renal outcomes, and response to canagliflozin. J Am Coll Cardiol 2022;79:432–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Zelniker TA, Morrow DA, Mosenzon O, et al. Relationship between baseline cardiac biomarkers and cardiovascular death or hospitalization for heart failure with and without sodium-glucose co-transporter 2 inhibitor therapy in DECLARE-TIMI 58. Eur J Heart Fail 2021;23:1026–1036. [DOI] [PubMed] [Google Scholar]
- 156.McCarthy CP, Olshan DS, Rehman S, et al. Cardiologist evaluation of patients with type 2 myocardial infarction. Circ Cardiovasc Qual Outcomes 2021;14: e007440. [DOI] [PubMed] [Google Scholar]
- 157.Park J, Oh AR, Kwon JH, et al. Association between cardiologist evaluation and mortality in myocardial injury after non-cardiac surgery. Heart 2022;108:695–702. [DOI] [PubMed] [Google Scholar]
- 158.Williams MC, Hunter A, Shah ASV, et al. Impact of noncardiac findings in patients undergoing CT coronary angiography: a substudy of the Scottish Computed Tomography of the Heart (SCOT-HEART) trial. Eur Radiol 2018;28:2639–2646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Honigberg MC, Lander BS, Baliyan V, et al. Preventive management of nonobstructive CAD after coronary CT angiography in the emergency department. J Am Coll Cardiol Img 2020;13:437–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Øvrehus KA, Diederichsen A, Grove EL, et al. Reduction of myocardial infarction and all-cause mortality associated to statins in patients without obstructive CAD. J Am Coll Cardiol Img 2021;14:2400–2410. [DOI] [PubMed] [Google Scholar]
- 161.Hwang IC, Jeon JY, Kim Y, et al. Association between aspirin therapy and clinical outcomes in patients with non-obstructive coronary artery disease: a cohort study. PLoS One 2015;10:e0129584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cainzos-Achirica M, Miedema MD, McEvoy JW, et al. Coronary artery calcium for personalized allocation of aspirin in primary prevention of cardiovascular disease in 2019: The MESA study (Multi-Ethnic Study of Atherosclerosis). Circulation 2020;141:1541–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


