Abstract
Background
The coronavirus disease 2019 (COVID‐19) pandemic has constrained opportunities in social, educational and professional domains, leading to developmental challenges for adolescents initiating their transition to adulthood. Meta‐analysis indicated that there was a small increase in psychological distress during the first year of the COVID‐19 pandemic. However, significant heterogeneity in the psychological response to the COVID‐19 pandemic was noted. Developmental antecedents as well as social processes may account for such heterogeneity. The goal of this study was to characterize trajectories of psychological distress in late adolescence during the COVID‐19 pandemic.
Methods
5014 late adolescents born between 2000 and 2002 from the UK Millennium Cohort Study completed online self‐reported assessments at three occasions during the first year of the COVID‐19 pandemic (May 2020, September/October 2020 and February/March 2021). These surveys assessed psychological distress, loneliness, social support, family conflict, as well as other pandemic stressors. Information on developmental antecedents were obtained when cohort members were 17 years of age.
Results
Four distinct trajectories class were identified. Normative class (52.13%) experienced low and decreasing levels of psychological distress, while moderately increasing class (31.84%) experienced a small, but significant increase in distress over time and increasing class (8.75%) exhibited a larger increase in distress after the first wave of the pandemic. Inverted U‐shaped class (7.29%) experienced elevated psychological distress during the first wave of the pandemic, followed by a decrease in distress in subsequent waves of the pandemic. Larger longitudinal increases in loneliness were noted among individuals in the elevated distress trajectory, compared to other trajectories. Pre‐pandemic psychopathology was associated with elevated distress early in the pandemic.
Conclusions
The largest trajectory showed low and declining psychological distress, highlighting the resilience of the majority of late adolescents. However, a subgroup of adolescents experienced large increases in psychological distress, identifying a group of individuals more vulnerable to pandemic‐related stress.
Keywords: adolescence, anxiety, COVID‐19, depression, loneliness, psychological distress, social support
Trajectories of psychological distress during the COVID‐19 pandemic.
Key points.
Prior work with adolescents highlights significant heterogeneity in change in psychological distress during the COVID‐19 pandemic.
Among late adolescents, increases in distress were small for about 30% of participants and large for about 9% of participants.
About 8% of participants experienced elevated distress during the first wave followed by a subsequent decrease in distress.
Individuals who experienced larger increase in psychological distress also reported concomitant increases in loneliness during the pandemic.
Longitudinal follow‐ups are required to characterize the evolution of psychological distress once pandemic stressors abate.
BACKGROUND
The public health and social measures (PHSMs) imposed during the coronavirus disease 2019 (COVID‐19) pandemic led to protracted disruptions in daily occupational, educational, and social activities, such as limited access to social and leisure activities, online schooling, unstable labor markets with recurrent closure of non‐essential businesses, and loss of career and educational opportunities (Lee et al., 2021; Sahu, 2020). Late adolescents and emerging adults (i.e., those aged 18–24 years) who are undergoing the transition to adulthood are negotiating novel developmental tasks including living independently, establishing their first romantic and sexual relationships, making educational and vocational choices, and beginning a working career (Arnett & Sugimura, 2014; Scales et al., 2016; Zarrett & Eccles, 2006). Pandemic‐related confinement measures may have constrained opportunities in social, romantic, sexual, educational, and vocational domains, creating unique challenges for late adolescents negotiating these various developmental tasks (Scales et al., 2016).
Several studies highlight that late adolescents reported higher levels of psychological distress during the first wave of the pandemic, compared to other age groups (Wetherall et al., 2022; World Health Organization, 2022). Specifically, it has been observed that late adolescents have experienced more depressive and anxiety symptoms than adults (30–59 years) and older adults (>60 years) (Sun et al., 2023; Wetherall et al., 2022). In addition, within this age group, an increase in psychological distress has been observed before and during the pandemic, particularly among girls (Madigan et al., 2023). Before the COVID‐19 pandemic it was estimated that 12.9% (Lu, 2019) and 11.6% (Tiirikainen et al., 2019) of young people had clinically significant symptoms of depression and anxiety, while during the pandemic these were rates of 25.2% and 20.4%, respectively (Racine et al., 2021). Similarly, in a longitudinal study of late adolescents with pre‐pandemic assessment in 2018, both depressive and anxious symptoms increased during the first 12 months of the COVID‐19 pandemic (Gouin et al., 2023). This contrasts with the typical decrease in psychological distress that have occurred among this age group in pre‐pandemic cohorts (Hangrove et al., 2020).
Meta‐analyses of longitudinal studies including pre‐pandemic data indicate small, but significant increases in psychological distress during the first few months of the pandemic, followed by a decline in distress toward the end of the first wave in the Spring 2020 (Kunzler et al., 2021; Madigan et al., 2023; Prati & Mancini, 2021; Robinson et al., 2022). Although most countries maintained some PHSMs during subsequent waves of the pandemic (Aknin et al., 2022), research examining the trajectories of psychological distress throughout the pandemic is limited. In longitudinal studies within the general population, fluctuations in psychological distress were observed during the first 15 months of the pandemic, largely in line with the waxing and waning indices of stringency of PHSMs and pandemic intensity (Aknin et al., 2022; Daly & Robinson, 2022; Ori et al., 2022). Several longitudinal studies of late adolescents reported a worsening of anxiety and depressive symptoms during the first 12 months of the COVID‐19 pandemic (Benatov et al., 2022; Hawke et al., 2021; Hu & Gutman, 2021; Patel et al., 2022; Rogowska et al., 2021; Stroud & Gutman, 2021). However, not all studies have observed protracted elevations in psychological distress among adolescents during this timeframe (Graupensperger et al., 2022; Rimfeld et al., 2021), highlighting the heterogeneity in psychological distress responses during the COVID‐19 pandemic.
Understanding variability in the psychological responses to the COVID‐19 pandemic and the related PHSM is important given the high risk for future pandemics (Marani et al., 2021). Characterizing trajectories of psychological distress and identifying their correlates will help us identify vulnerable individuals and potential mitigations strategies. Several risk and protective factors may explain differences in psychological distress during the COVID‐19 pandemic. In cross‐sectional and longitudinal studies, female adolescents reported on average more anxiety and depression than males (Del‐Valle et al., 2022; Stroud & Gutman, 2021). Ethnic and racial minority experienced more psychological distress than individuals from the majority group (Smith et al., 2020). Furthermore, financial stress exacerbated by the pandemic, that is, the worries about having enough money to meet their household's basic needs, have been associated with higher depression and anxiety among late adolescents over time (Ellwardt & Präg, 2021; Schoon & Henseke, 2022). Moreover, past studies indicate that pre‐pandemic mental health is a moderator of psychological distress during the pandemic. Individuals with severe anxiety and depressive symptoms pre‐pandemic displayed patterns of stable or decreasing symptoms during the first wave of the pandemic, whereas their counterparts with better pre‐pandemic mental health displayed patterns of increasing symptoms during the first wave of the pandemic (Bouter et al., 2022; De France et al., 2022; Hamza et al., 2021; Watkins‐Martin et al., 2021).
The quality of social relationships is also an important determinant of psychological distress across the lifespan. Late adolescence is usually associated with the expansion of social networks (Arnett & Sugimura, 2014; Miething et al., 2016). Pandemic‐related restrictions in in‐person interactions may have impacted distinct social processes that modulate risk for psychological distress (Foulkes & Blakemore, 2021). Loneliness is defined by the subjective and distressing perception of a discrepancy between the actual and desired quantity and quality of one's social relationships (Hawkley & Cacioppo, 2010). A meta‐analysis indicated that PHSMs were associated with increases in loneliness (Knox et al., 2022). Notably, late adolescents reported more loneliness than other age groups (Bu et al., 2020; Hu & Gutman, 2021; O’Connor et al., 2021; Varga et al., 2021). Outside of a pandemic context, loneliness is associated with elevated psychological distress (Beutel et al., 2017). Loneliness was also one of the strongest predictors of anxiety and depression during the first wave of the COVID‐19 pandemic (González‐Sanguino et al., 2020), including among late adolescents (Loades et al., 2020). Loneliness may thus be a key social process increasing risk for psychological distress among adolescents during the COVID‐19 pandemic.
Social support, the perception of the availability of close others to provide assistance in times of needs (Wethington & Kessler, 1986), is another social process that may modulate pandemic‐related psychological distress. Although loneliness and social support are conceptually related, empirical studies indicate that size of the correlation between the two constructs is small‐to‐moderate, indicating the unique contribution of each of these two social processes (Grey et al., 2020). Social support is an important protective factor against the development and worsening of mental health symptoms across the lifespan (Gariépy et al., 2016; Rueger et al., 2016), and especially during periods of transition or stress such as late adolescence (Pettit et al., 2011; Scardera et al., 2020). Social support may play a key role in supporting adaptive coping behaviors in response to various pandemic‐related stressors (Thoits, 1986). Higher social support was cross‐sectionally associated with decreased psychological distress during the COVID‐19 (Szkody et al., 2021). More social support was associated with faster decreases in psychological distress during the first wave of the pandemic (Amendola et al., 2021; Fluharty et al., 2021; Zhou et al., 2020), as well as lower depressive and anxiety symptoms, during the first year of the pandemic (Laham et al., 2021; Li et al., 2021). Within the general population, some studies suggest that social support is more stable than loneliness in the context of changing PHSMs (Laham et al., 2021; Xu et al., 2020), while other studies indicate that social support have increased during the pandemic (Luchetti et al., 2020). Given that the transition to adulthood is a key period for the expansion of social network, late adolescents may experience greater difficulties building or maintaining close social relationships than other age groups during periods of pandemic‐related restrictions in social activities, leading to cumulative negative impact on adolescents' mental health over time.
Finally, interpersonal stress may contribute to aggravate psychological distress under stressful conditions (Hammen, 2016). In particular, studies have provided some evidence of increased family conflict during lockdowns (Guo et al., 2020; Morgül, Kallitsoglou, Essau, Castro‐kemp, & Mateo, 2022). These family conflict, resulting from a wide range of stressors affecting family members, such as work from home/teleworking, loss of income, home‐schooling, and movement restrictions for young people to meet up with their friends, could increase risk for adolescents' psychological distress.
Taken together, prior studies indicate that, on average, a small increase in psychological distress was observed among late adolescents during the COVID‐19. However, significant heterogeneity in the psychological response to the pandemic were noted. Given key pivotal changes in social networks during this developmental period, changes in social support, loneliness, and family conflict may be key social processes underlying changes in distress among late adolescents during the COVID‐19 pandemic. Within the Millennium Cohort Study, significant increases in psychological distress were noted 12 months into the COVID‐19 pandemic, compared to the pre‐pandemic period (Patel et al., 2022). However, no study has examined heterogeneity in the change in psychological distress over time. Capitalizing on this longitudinal cohort design provides a unique opportunity to examine how previous psychopathology and current social functioning influences changes in psychological distress during the pandemic. The goals of the current study were thus to (a) examine the heterogeneity of change in psychological distress among late adolescents at 3 time points during the COVID‐19 pandemic, (b) examine change in social support and loneliness during the pandemic, and (c) to examine the contributions of pre‐pandemic psychopathology and other COVID‐19 and PHSMs‐related stressors to changes in psychological distress during the pandemic.
METHOD
Sample and data in analysis
Data from the Millennium Cohort Study (MCS) (Connelly & Platt, 2014) were used in this study. The MCS is a nationally‐representative birth cohort study aiming at depicting the developmental course of physical and mental health outcomes of British people born between 2000 and 2002 (i.e., the so‐called Generation Z). In terms of sampling, a stratified clustering strategy was followed to ensure adequate representation of ethnic minorities at the baseline assessment (i.e. 82% of participants were White, 2.5% were Indian, 4.8% were Pakistani, 2% were Bangladeshi, 1.3% were Black Caribbean, 2% were Black African, and 3% of cohort members had mixed ethnicity) (MCS; Connelly & Platt, 2014). The MCS comprises seven sweeps following cohort members from 9 months of age to age 17. In addition, data during the COVID‐19 pandemic were collected at three occasions (May 2020, September/October 2020 and February/March 2021). The first COVID‐19 survey took place in May 2020, representing 38 days of home confinement with universities, entertainment venues, hotels and any type of indoor leisure facilities had been closed by the UK government. The second COVID‐19 survey was conducted between September‐October 2020 while restaurants, pubs and other entertainment venues had been open since July 4, but opening hours were restricted and there were still social distancing measures such as the “rule of six” (The Health Foundation, 2023). The third assessment was between February‐March 2021. A new home confinement of the population had been decreed January 6th but lifted on March 8th. Citizens were encouraged to stay in their locality. Outdoor recreation in public spaces between two people and outdoor gatherings of six people or two households were permitted (The Health Foundation, 2023). Further details on the COVID‐19 surveys can be consulted on the MCS webpage (https://cls.ucl.ac.uk/covid‐19‐survey/). All MCS protocols were approved by an ethical committee for human research (Shepherd & Gilbert, 2019).
The sample included in this study comprised 5014 late adolescents aged 19–21 years (60.59% female, mean age = 19.27, SD = 0.46) who responded to the psychological distress scale (i.e., the K6 scale below) at least once across the COVID‐19 survey waves. In terms of COVID‐19 survey response rate, 44.22% of the study sample responded to the first COVID‐19 survey; 56.42% of participants responded to the second survey and the response rate to the third survey was 81.27%.
Measures
Sociodemographic (i.e., sex at birth, age, and ethnic group), pre‐COVID‐19 psychopathology and COVID‐19‐related (proximal factors) data were used in this study.
Demographic variables
Demographic variables assessed for all participants were sex at birth, age and ethnic group (subjects were classified as: white Caucasian or non‐white Caucasian) and country (i.e. England, Wales, Scotland and Ireland).
Psychopathology
Previous psychopathology factors were taken from the MCS 2018 sweep when cohort members were 17 years old. Specifically, the Strength and Difficulties Questionnaire (SDQ), self‐reported version (SDQ; Goodman et al., 1998) assessed internalizing and externalizing symptoms (i.e., the Difficulties scores) as well as prosocial behaviors. The SDQ is a 25‐item scale covering psychopathology symptoms from four dimensions (i.e., emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems) and prosocial behaviors. Each item can be responded using a 3‐point Likert scale. The SDQ showed acceptable levels of reliability in adolescents in a study previously conducted in five European countries (Cronbach's α = 0.71 for the Total Difficulties scale; and Cronbach's α = 0.71 for the Prosocial Behaviors scale) (Essau et al., 2012).
Moreover, self‐harm behavior at age 17 was considered. Self‐harm was measured by a single item (item: whether the cohort member had self‐hurt in the last year at least in one of these ways: bruising or pinching; burning, cutting or stabbing, taking an overdose of tablets, pulling out hair).
COVID‐related factors
Most of the COVID‐19‐related factors studied were measured by single items: whether the participant was infected by the SARS‐CoV‐2 virus during the study period (yes/no), whether the participant experienced more family conflict during the pandemic, compared to the pre‐pandemic, whether the participant experienced more financial difficulties during the first national lockdown (first COVID‐19 survey wave) in comparison to the pre‐pandemic period.
Furthermore, two time‐variant social processes were considered. First, perceived loneliness was measured across the three COVID‐19 surveys with the 3‐item University of California, Los Angeles (UCLA) Loneliness Scale (Russell, 1996). Items were rated on a 3‐point Likert scale. The 3‐item Social Provisions Scale (SPS) (Cutrona & Russell, 1983) measured the availability of social support across the COVID‐19 surveys. Reliability indexes of the 3‐item SPS in our sample ranged from Cronbach's α between 0.65 and 0.79 across the survey waves.
Finally, psychological distress across the COVID‐19 surveys was measured by the Kessler Distress Scale‐6 (Kessler et al., 2003). The K6 is made up of six items on a 5‐point Likert scale assessing anxiety and depressive symptoms in the past 30 days. The psychometric properties of the K6 were adequate in previous studies with adolescent and young adults populations (α = 0.84; Mewton et al., 2016).
Data analysis
The overall course of psychological distress and time‐variant factors (i.e., loneliness and social support) was evaluated using repeated‐measure analysis of variance. To prevent inflated type I error due to large sample size (Lin et al., 2013), only differences with at least a medium effect size (I.E., η 2 ≥ 0.06) would be considered to be meaningful differences.
The heterogeneous trajectories of psychological distress throughout the first COVID‐19 pandemic year were identified using growth mixture modeling (GMM) (Proust‐lima & Liquet, 2017; Ram & Grimm, 2009). The K6 score across the MCS COVID‐19 surveys was used as an observed variable capturing the psychological distress latent process. Growth mixture modeling, as a person‐centered approach, allows relaxing of the assumption of a unitary course of development. Subject‐specific variability may be well captured by clustering individuals with a similar trajectory into the same group (class). For parameter estimation, robust maximum likelihood and full information methods were used, enabling the estimation of individual‐specific trajectories even when intermittent missing data were present. Days from the WHO's pandemic declaration (11 March 2022) was used to estimate the linear and quadratic time effects. Unconstrained GMM solutions were estimated to decrease the probability of class overestimation due to covariates (Hu et al., 2017; Vermunt, 2010). Growth mixture modeling solutions with an increasing number of trajectory classes were compared. The model with an optimal class enumeration was selected according to the following criteria: low sample‐adjusted Bayesian information criterion (SABIC) and Akaike information criterion (AIC), mean of posterior probabilities to belong to each identified class higher than 0.70; and meaningful proportion of participants within each class (5%) (Nylund‐Gibson et al., 2023; Spiegelhalter et al., 2002).
Multinomial logistic regression was used to study the associations between distress trajectory membership and sociodemographic (i.e., sex at birth and ethnic group), pre‐COVID‐19 psychopathology factors (i.e., SDQ total difficulties, SDQ prosocial score and self‐harm on the MCS 2018 sweep) and COVID‐related cross‐sectional predictors (i.e., SARS‐CoV‐2 virus infection, family conflict level, and financial difficulties in comparison to the pre‐pandemic period), entered simultaneously in the model. Finally, multilevel linear regression was used to study the relationship between distress trajectory class membership and the course of loneliness and social support during the first year of the pandemic, controlling for the above‐mentioned covariates. Note that small correlations were observed between the loneliness and social support scores across COVID‐19 survey waves (r = −0.23 in the first wave, r = −0.25 in the second wave and r = −0.17 in the third wave). The repeated measure factor was used as a multilevel factor. Linear and quadratic effects of time, as well as sociodemographic, pre‐COVID‐19 psychopathology, trajectory class membership factors and cross‐sectional predictors COVID‐19‐related factors were included in the model. In addition, time*trajectory class interaction effects were tested.
Regarding model fit for both multinomial logistic and multilevel linear regression, the AIC was estimated to assess whether the model with covariates fitted better than an unconstrained model. The relative risk ratio (RRR) for multinomial logistic regression and the B coefficient, for the multilevel linear regression, were used as covariate loading estimates. All analyses were conducted using R x64 3.0.1 (lcmm, mice, lmer4 and psych packages) and STATA 15.
RESULTS
The Table 1 displays the descriptive statistics of sample. In total, a sample of 5014 participants was analyzed. Most participants were born in England (65.61%) and were White Caucasian (87.47%). Adolescent psychopathology at age 17 (MCS 2018 sweep X̄ = 11.31, sd = 5.56) was over the mean levels observed in other normative samples (i.e. German sample: X̄ = 10.93, sd = 4.9, Cypus sample: X̄ = 9.87, sd = 3.8, UK sample: X̄ = 10.87, sd = 2.9¸ Sweden sample: X̄ = 8.99, sd = 2.3 and Italy sample: X̄ = 10.26, sd = 2.3) (Essau et al., 2012). Moreover, more than one in four cohort members engaged in self‐harm behavior at age 17. Regarding psychological distress, there was a slightly increasing trend in K6 scores across the COVID‐19 survey waves, with a small effect size, F (1.97, 2537.12) = 16.47, p < 0.01, η 2 = 0.003. A slightly increasing levels of loneliness across waves was also observed, with a small effect size, F (1.94, 2546.98) = 18.25, p < 0.01, η 2 = 0.004. The repeated‐measure analysis of variance revealed the absence of change over time in perceived social support across the COVID‐19 survey waves, F (2, 2478) = 0.01, p = 0.99, η 2 < 0.001.
TABLE 1.
Sociodemographic and psychopathological features of sample.
| Variable | Statistic |
|---|---|
| Sex (%male) | 39.41 |
| Age at first COVID‐19 sweep | 19.27 (0.46) |
| Ethnic group (%non‐white) | 12.53 |
| Country | |
| England | 65.61 |
| Wales | 13.82 |
| Scotland | 11.88 |
| Ireland | 8.7 |
| Pre‐COVID (mid‐adolescence) psychopathology | |
| Total difficulties a | 11.31 (5.56) |
| Prosocial behavior a | 8.04 (1.67) |
| Self‐harm at age 17 (%yes) | 25.62 |
| COVID‐19 factors | |
| SARS‐Cov‐2 infection (%yes) | 12.93 |
| Family conflict (%more conflict during the pandemic) | 5.92 |
| Financial management (%worse off management during the pandemic) | 25.99 |
| Psychological distress b | |
| COVID‐19 wave 1 | 8.40 (5.12) |
| COVID‐19 wave 2 | 8.44 (5.37) |
| COVID‐19 wave 3 | 8.61 (5.58) |
| Perceived loneliness c | |
| COVID‐19 wave 1 | 5.16 (1.70) |
| COVID‐19 wave 2 | 5.21 (1.77) |
| COVID‐19 wave 3 | 5.28 (1.80) |
| Social support d | |
| COVID‐19 wave 1 | 6.79 (0.65) |
| COVID‐19 wave 2 | 6.79 (0.68) |
| COVID‐19 wave 3 | 6.80 (0.70) |
Note: Percentage of cases are displayed for dichotomous and categorical variables. Mean and standard deviation (between brackets) are displayed for continuous variables. The pre‐COVID data were collected in 2018, when cohort members were 17 years old. The COVID‐19 data were collected across three waves: COVID‐19 wave 1 (May 2020), COVID‐19 wave 2 (September/October 2020) and COVID‐19 wave 3 (February/March 2021).
Derived from the SDQ.
Coming from the Kessler K6 Scale (K6).
Derived from the 3‐item UCLA Loneliness Scale.
Derived from the 3‐item Social Provisions Scale.
Trajectories of psychological distress
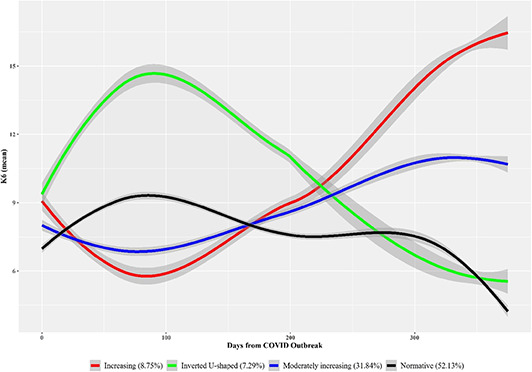
Psychological distress trajectory analysis revealed a better fit for the 4‐class model depicting a linear effect of time (SABIC = 186,115.48, AIC = 186,072.05; mean of posterior probabilities for each class = 0.70–0.90). The Table S1 displays the fit indexes derived from all the estimated GMM models (see Supplementary materials). The heterogeneous trajectories of psychological distress across the COVID‐19 measurement occasions are displayed in Figure 1. The first identified class (increasing class; 8.75% of participants) was characterized by an increasing distress trend (b coming from a peak of minimal distress over then first assessment wave, on May 2020) following the first COVID‐19 survey (intercept, B = −1.32, Z = −20.12, p < 0.01; time effect, B = 0.02, Z = 91.61, p < 0.01). The second identified class (inverted U‐shaped class) comprised 7.29% of participants and was characterized by an elevation in distress (reaching in maximum level over 90 days after the pandemic declaration) during the first wave of the pandemic, followed by a decreasing course of distress thereafter (intercept in comparison with the first class intercept, B = 7.46, Z = 25.66, p < 0.01; time effect, B = −0.02, Z = −74.06, p < 0.01). The third class (so‐called moderately increasing class; 31.84% of sample) was characterized by a smooth rise in distress over time after the first COVID‐19 survey (intercept in comparison with the first class intercept, B = 1.32, Z = 5.37, p < 0.01; time effect, B = 0.01, Z = 54.03, p < 0.01). Finally, the fourth class (normative class; 52.13% of participants) showed a slight increase in distress during the first COVID‐19 survey (on May 2020 approximately) and a decreasing trend onwards (intercept in comparison with the first class intercept, B = 2.70, Z = 11.84, p < 0.01; time effect, B = −0.01, Z = −34.45, p < 0.01).
FIGURE 1.
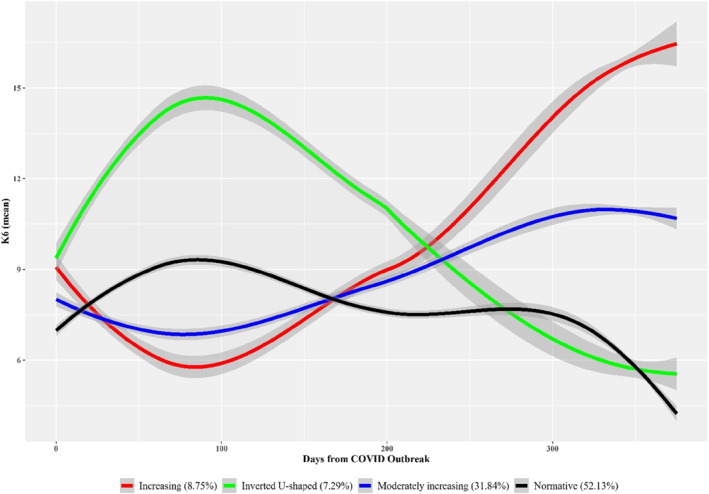
Psychopathology distress trajectories during the first coronavirus disease 2019 (COVID‐19) pandemic year. Trajectories were estimated on the Kessler K6 Scale (K6) scores across the three COVID‐19 survey occasions. Shaded area represents the 95% confidence interval of mean.
Multinomial logistic regression and multilevel linear regression
Regarding multinomial logistic regression and multilevel linear regression analysis to characterize trajectory class membership, sample size was different across analyses due to the amount of missing data for each outcome. A sample of 1355 subjects was used for these analyses. Attrition statistics for each regression analysis are displayed in Table S2 (see the Supplementary analysis). Significant differences were found across several factors, but they were not meaningful (i.e., with at least medium effect size: Cohen's d ≥ 0.50, Cramer's V ≥ 0.30, η 2 ≥ 0.06), except for sex. In this case, a higher number of men had missing data, in comparison to women. For that reason, a smaller number of men were included in the regression analyses.
Associations between distress trajectory membership and sociodemographic pre‐COVID‐19 and COVID‐19‐related factors
Multinomial logistic regression was used to study the relationship between the cross‐sectional predictors and psychological distress class membership. The model with covariates (AIC = 3033.03) fitted significantly better to data than the unconstrained model (AIC = 3168.71). Thus, the explanatory power of the model increases with the inclusion of covariates. Covariate coefficients are displayed in Table 2. The inverted U‐shaped class membership (in comparison to the normative class membership) was associated with higher adolescent psychopathology measured with the SDQ (RRR = 1.08, p < 0.01) and lower risk of self‐harm at age 17 (RRR = 0.50, p < 0.05), as well as higher risk of financial difficulties during the pandemic lockdown (RRR = 1.62, p < 0.05). The minimally increasing class membership was associated with higher risk of family conflict during the first year of the pandemic (RRR = 1.44, p < 0.05), in comparison to normative class membership. Finally, no cross‐sectional predictors were associated with increasing trajectory class membership (in comparison to normative class).
TABLE 2.
Multinomial logistic regression to explain psychopathology trajectory class membership.
| Inverted U‐shaped | Minimally increasing | Increasing | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RRR | CI95 | Z | RRR | CI95 | Z | RRR | CI95 | Z | |
| (Intercept) | 0.07 | (0.02, 0.25) | −4.01** | 0.38 | (0.18, 0.79) | −2.57* | 0.18 | (0.06, 0.55) | −2.98** |
| Sex (ref.: Male) | 0.75 | (0.45, 1.22) | −1.16 | 1.07 | (0.82, 1.40) | 0.49 | 0.94 | (0.62, 1.42) | −0.31 |
| Ethnicity (ref.: White Caucasian) | 0.78 | (0.36, 1.69) | −0.63 | 1.24 | (0.87, 1.78) | 1.2 | 1.06 | (0.60, 1.89) | 0.2 |
| Pre‐COVID (mid‐adolescence) psychopathology | |||||||||
| SDQ (total difficulties) | 1.08 | (1.03, 1.13) | 3.17** | 1.02 | (0.99, 1.04) | 1.2 | 1.00 | (0.96, 1.04) | 0 |
| SDQ (prosocial scale) | 0.98 | (0.86, 1.13) | −0.22 | 1.02 | (0.94, 1.10) | 0.39 | 0.99 | (0.88, 1.12) | −0.11 |
| Self‐harm behavior | 0.50 | (0.28, 0.92) | −2.22* | 0.88 | (0.65, 1.20) | −0.8 | 1.14 | (0.72, 1.82) | 0.56 |
| COVID‐related factors | |||||||||
| Being infected by COVID‐19 (ref.: no) | 0.80 | (0.37, 1.73) | −0.56 | 0.84 | (0.56, 1.25) | −0.87 | 0.79 | (0.42, 1.51) | −0.71 |
| Family conflict (ref.: no more conflict) | |||||||||
| More conflict during the pandemic | 1.17 | (0.66, 2.08) | 0.54 | 1.44 | (1.07, 1.94) | 2.37* | 1.12 | (0.69, 1.83) | 0.47 |
| Financial management (ref.: About the same or better off in comparison to the pre‐pandemic) | |||||||||
| Worse off management during the pandemic | 1.62 | (1.00, 2.61) | 1.97* | 1.16 | (0.88, 1.53) | 1.08 | 1.24 | (0.81, 1.88) | 0.99 |
Note: The normative distress trajectory membership was the reference category.
Abbreviations: CI95, 95% confidence interval of the RR; RRR, Relative ratio; SDQ, Strengths and Difficulties Questionnaire; Z, Wald's z‐based statistic to test whether loading is significantly different from one.
*p < 0.05; **p < 0.01.
Relationship between distress trajectory class membership and the course of loneliness and social support during the first year of the pandemic
In terms of the associations between the distress trajectory class membership and time‐variant social processes (i.e., loneliness and social support), the multilevel linear regression model with covariates, quadratic time term and time*class interaction effects fitted better to data (see Table 3). A sample of 1033 and 1030 participants was used to study the relationship between distress trajectory class membership and the course of loneliness and social support during the first year of the pandemic, respectively.
TABLE 3.
Multilevel linear regression for loneliness and social support course.
| Loneliness course | Social support course | |||||
|---|---|---|---|---|---|---|
| B | SE | t | B | SE | t | |
| (Intercept) | 5.02 | 0.06 | 93.91** | 6.83 | 0.03 | 266.71** |
| Time effect a | ||||||
| Linear | 2.91 | 1.74 | 1.68 | 0.24 | 1.18 | 0.21 |
| Quadratic | 1.72 | 1.74 | 0.99 | −0.1 | 1.1 | −0.09 |
| Distress trajectory class (ref.: normative) | ||||||
| Inverted U‐shaped | −0.01 | 0.14 | −0.1 | −0.01 | 0.07 | −0.11 |
| Minimally increasing | −0.05 | 0.08 | −0.71 | 0.01 | 0.03 | 0.31 |
| Increasing | 0.15 | 0.12 | 1.27 | 0.01 | 0.06 | 0.06 |
| Pre‐COVID (mid‐adolescence) psychopathology | ||||||
| SDQ (total difficulties) | 0.58 | 0.03 | 16.48** | −0.09 | 0.02 | −5.54** |
| SDQ (prosocial) | −0.05 | 0.03 | −1.59 | 0.05 | 0.02 | 3.07** |
| COVID‐related factors | ||||||
| Being infected by COVID‐19 (ref.: no) | −0.15 | 0.11 | −1.44 | 0.04 | 0.05 | 0,74 |
| Family conflict (ref.: no more conflict) | ||||||
| More conflict | 0.29 | 0.08 | 3.37** | −0.04 | 0.03 | −1.11 |
| Financial management (ref.: Same or better off) | ||||||
| Worse | 0.23 | 0.07 | 3.04** | −0.09 | 0.03 | −2.61** |
| Interaction effects b | ||||||
| Linear time effect*Inverted U‐shaped class | −0.06 | 5.25 | −0.01 | −4.35 | 3.85 | −1.13 |
| Quadratic time effect*Inverted U‐shaped class | 2.56 | 5.25 | 0.49 | 1.75 | 3.68 | 0.47 |
| Linear time effect*Minimally increasing class | 4.25 | 2.86 | 1.48 | 1.31 | 1.89 | 0.69 |
| Quadratic time effect*Minimally increasing class | −1.2 | 2.86 | −0.42 | 0.65 | 1.78 | 0.37 |
| Linear time effect*Increasing class | 11.5 | 4.49 | 2.56* | −1.59 | 3.08 | −0.51 |
| Quadratic time effect*Increasing class | 5.91 | 4.49 | 1.31 | −0.1 | 2.9 | −0.03 |
| Random‐effects SD | 1.04 | 0.31 | ||||
| AIC | ||||||
| Unconstrained | 16,231.69 | 4246.53 | ||||
| Linear model | 15,941.12 | 4246.92 | ||||
| Quadratic | 15,930.19 | 4239.48 | ||||
| Model with interaction term (linear) | 15,949.55 | 4262.65 | ||||
| Model with interaction term (quadratic) | 15,904.39 | 4225.69 | ||||
Time effects accounts for the outcomes across the three COVID‐19 waves.
Effects derived from the interaction between the time (wave) effects and the distress trajectory class (in comparison to the reference category = normative trajectory class).
Abbreviations: AIC, Akaike information criterion; B, Loading coefficient; SD, Standard deviation; SE, Standard error; SDQ, Strengths and Difficulties Questionnaire.
*p < 0.05; **p < 0.01.
Several factors were significantly associated with both the loneliness course (i.e., greater loneliness was related to mental health difficulties at age 17, more family conflict and financial difficulties during the first COVID‐19 years) and social support course (i.e., less social support was related to mental health difficulties at age 17 and poorer prosocial behavior, and financial difficulties during the first COVID‐19 years), but no time main effects were observed for both processes. However, an interaction effect was found between the linear time effect of perceived loneliness and the increasing class membership (B = 11.5, p < 0.05). Figure 2 displays the course of loneliness according to distress trajectory class membership. Participants from the increasing distress trajectory class showed a sharp increase in loneliness starting at the second COVID‐19 wave, in comparison to the rest of participants. No other class membership effect or interaction effects was found for the loneliness and social support models.
FIGURE 2.
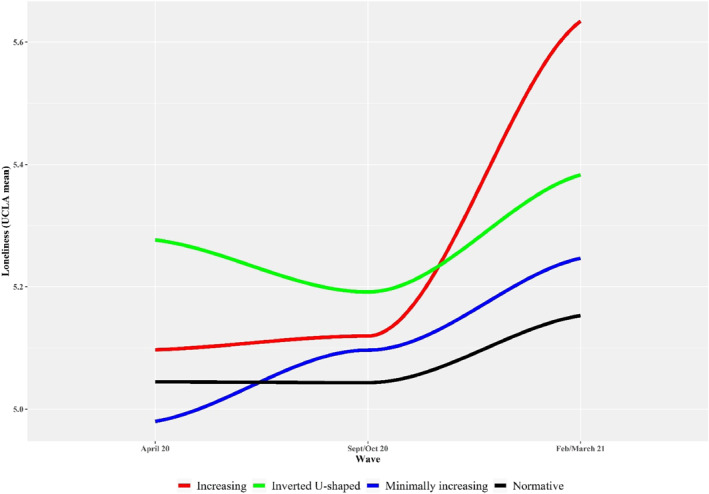
Course of loneliness according to psychopathology distress trajectory class.
DISCUSSION
Using a large longitudinal cohort of late adolescents, the UK Millennium Cohort Study, this study examined heterogeneity in the changes in psychological distress at 3 time points during the first year of the COVID‐19 pandemic (May 2020, September/October 2020 and February/March 2021). Four distinct trajectories of psychological distress were identified. Furthermore, although perceived social support was stable throughout the assessment period, there was an increase in loneliness during the first year of the pandemic. Larger longitudinal increases in loneliness during the pandemic period were noted among individuals belonging to the elevated distress class, compared to those who experienced less psychological distress. Pre‐pandemic psychopathology was higher among participants who exhibited elevated distress during the first wave of the pandemic. These findings highlight that although the normative group exhibited low and even decreasing distress, a subset of adolescents experienced prolonged and increasing distress in the context of prolonged pandemic‐related PHSM.
Results indicated that there was an overall slight increase in psychological distress across the first year of the COVID‐19 pandemic among UK late adolescents. However, there was significant heterogeneity in the patterns of change over time. Growth mixture modeling identified four latent trajectory classes. On one hand, we observed that half of the participants experienced low and decreasing levels of psychological distress during the pandemic, highlighting the resilience of the majority of late adolescents during the pandemic. This result is consistent with findings from other cohorts (Foster et al., 2023; Manchia et al., 2022). This adaptation could reflect the decreased COVID‐19 related uncertainty over time (Killgore et al., 2020), the progressive adaptation to the crisis situation and the development of alternative socialization strategies in the face of restrictions for in‐person social interactions (Manchia et al., 2022). On the other hand, about 31.1% experienced a small, but significant increase in distress over time and about 8.75% exhibited a larger increase in distress after the first wave of the pandemic. Another 7.29% of participants experienced elevated psychological distress during the first wave of the pandemic, followed by a decrease in distress in subsequent waves of the pandemic. This heterogeneity is in line with other studies who identified distinct psychological distress trajectories during the COVID‐19 pandemic (Pierce et al., 2021; Saunders et al., 2021).
The transition to adulthood is characterized by developmental changes in different life domains and roles, including education, employment, social network, marriage, cohabitation, and parenthood (Scales et al., 2016). Pandemic‐related restrictions led to constrained opportunities in several of these key life domains, highlighting the unique developmental challenges experienced by late adolescents during the COVID‐19 pandemic. Specifically, confinement‐related and physical distancing measures may have constrained opportunities for expansion of social, romantic, and sexual relationships. In the present study, there was a significant increase in loneliness over time. This is consistent with other studies indicating that late adolescents and young adults experienced largest increases in loneliness compared to other age groups (Varga et al., 2021). In contrast, but consistent with other work (Hamza et al., 2021; Laham et al., 2021), there was no change in perceived social support in the present study. This may be because one's perception of the availability of social support may be less dependent on in‐person social interactions, but more strongly related to core attachment‐related beliefs about the availability and responsiveness of close others (Green et al., 2011).
Adolescents experiencing larger increase in psychological distress over time also reported larger increases in loneliness during the pandemic period. This is in line with other studies that observed that loneliness was one of the most robust predictors of psychological distress during the COVID‐19 pandemic (Laham et al., 2021). Although increases in psychological distress and loneliness co‐occurred in the present study, cross‐lagged analysis in a prior longitudinal study indicated that loneliness predicted future depressive symptoms, but not vice‐versa (Cacioppo et al., 2010; Erzen & Çikrikci, 2018; Kraav et al., 2021; Martín‐María et al., 2021). Depression often also leads to a decrease in social relations linked to anhedonia (Brohan et al., 2011; Fernández‐Theoduloz et al., 2019; Hauenstein; 2003; Hopko et al., 2008; Lynch et al., 2021) in addition to the acquisition of a more sedentary lifestyle habits that result in a decrease in social interaction, leading to vicious circle between depression and loneliness (De Moor et al., 2006; Vancampfort et al., 2015).
Conceptual models of loneliness suggest that prolonged loneliness may foster biased social cognition associated with hypervigilance to social threat (Cacioppo & Hawkley, 2009). This biased social information processing may in turn result in more negative social experiences that increase interpersonal stress and risk for psychological distress (Spithoven et al., 2017). In line with this model, prior psychopathology (i.e. elevated SDQ score at age 17) and the presence of family conflict were associated with higher loneliness in the present study. Furthermore, in line with other work (Loibl et al., 2021; Refaeli & Achdut, 2021), greater financial stress was also related to higher loneliness during the COVID‐19 pandemic. Elevated internalizing and externalizing symptoms assessed using the SDQ Difficulties score at age 17 was associated with the inverted U‐shaped trajectory, compared to the other trajectory groups. Individuals in this group experienced the highest levels of psychological distress during the first wave of the pandemic. However, they experienced a gradual decrease in psychological distress during the latter part of the year, suggesting a habituation process, whereby individuals become less reactive or impacted by pandemic‐related stressors over time. Habituation is defined as a decrease in response to repeated stimulation (Thompson, 2010). In prior work, the presence of elevated psychological distress prior to the pandemic moderated changes in distress over time. Although individuals with prior anxiety and depression had overall higher levels of distress, they experienced a smaller increase, and even a decrease in distress in some studies, during the pandemic (Bouter et al., 2022; Hamza et al., 2021; Watkins‐Martin et al., 2021). The PHSMs may have constrained opportunities for in‐person social interactions. However, they may also have reduced exposure to a number of social stressors. This context may have promoted less psychological distress among those who typically display emotion regulation difficulties in response to social stressors. Intriguingly, the presence of a history of non‐suicidal self‐harm was associated with a lower probability of belonging to the inverted U‐shaped trajectory. The negative urgency associated with self‐injury behavior may be associated with distinct emotion regulation strategies (e.g., increased use of alcohol and tobacco) during the pandemic (Essau & de la Torre‐Luque, 2021; Hamza et al., 2015; King et al., 2018). Prior work indicate that higher loneliness during the COVID‐19 pandemic was associated with a decrease in self‐harm among those with high pre‐pandemic self‐harm, suggesting a distinct distress trajectory among this group (Schwartz‐Mette et al., 2022).
For the minimally increasing distress, the presence of family conflict was the only predictor of membership to this trajectory. Some studies have reported increases in family conflict during lockdown periods (Morgül, Kallitsoglou, Essau, & Castro‐Kemp, 2022; Orgilés et al., 2020; Stassart et al., 2021). In a longitudinal study with adolescents, family conflict was associated with larger increases in distress over time (Magson et al., 2021). During the COVID‐19 pandemic, adolescents had less opportunities to interact in person with friends, classmates or colleagues, but spent more time with other household members. The presence of social conflict in the proximal social environment may thus have impeded adjustment to pandemic‐related stressors.
A key strength of the present study is the longitudinal study design with repeated measurements before and during the pandemic, allowing us to examine the influence of developmental antecedents as well as changing social processes during the pandemic. Moreover, a robust analytical strategy was followed. Limitations include the use of non‐validated measures to assess social support and family conflict. In addition, although previous studies have taken into account this type of intentional acts of harming oneself using as a measure the performance of self‐harming behaviors (Hartas, 2023; Uh et al., 2021) this is a non‐validated measure of self‐harm. Similarly, the Kessler Psychological Distress Scale (K6) is a brief scale that does not allow for distinctions between anxiety and depressive symptoms. Furthermore, although the sample was representative at the study outset, differential attrition may have reduced its representativeness. Furthermore, although many participants completed at least one assessment during the COVID‐19 pandemic, only a smaller percentage completed all 3 pandemic assessments. Moreover, late adolescence is a developmental period associated with the onset and a high incidence of anxiety and depressive disorders (Solmi et al., 2022). As such, it is difficult to disentangle the contribution of developmental changes, pandemic‐related stress, or other cohort effects to the change in psychological distress over time.
CONCLUSION
In conclusion, about 8.75% of late adolescents exhibited a pattern of increasing distress over time, which was associated with concomitant increases in loneliness. Whether adolescents within the increasing distress trajectory will experience a decrease in symptoms once pandemic‐related stressors abate is unclear. Longitudinal follow‐ups will be required to characterize the longer‐term trajectories of psychological distress among these individuals in the post‐pandemic period.
On the other hand, it is also important to note that about 51.2% of late adolescents experienced low levels of psychological distress throughout the first year of the COVID‐19 pandemic. The fact that the majority were resilient in the face of the various pandemic stressors is important. The risk for future pandemics is high (Marani et al., 2021). Furthermore, climate change leading to more frequent extreme weather events may prompt the use of confinement measures restricting in‐person interactions in the future (Longman et al., 2023). Exploring the different trajectories of distress in times of crisis can help confront possible future threats and identify vulnerable populations. In addition, knowing the factors associated with psychological distress will allow us to develop interventions protocols for action in different contexts (e.g., educational, health and family), and to propose specific interventions to target risk factors such as loneliness (Cooper et al., 2021; Loades et al., 2020).
AUTHOR CONTRIBUTIONS
Jean‐Philippe Gouin: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Alejandro de la Torre‐Luque: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Yolanda Sanchez‐Carro: Writing – review & editing. Marie‐Claude Geoffroy: Conceptualization, Writing – review & editing. Cecilia Essau: Conceptualization, Writing – review & editing.
CONFLICT OF INTEREST STATEMENT
The authors have declared that they have no competing or potential conflicts of interest.
Ethical considerations
For this study, we used MCS data, registered with the UK data service upon an End User Licence agreement. Existing data use does not require independent ethics committee application. MCS survey participants provided a written consent to participate. Ethical approval for the MCS was obtained from the relevant committees and from the University College London Institute of Education Research Ethics Committee (REC1334).
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors are grateful to the Center for Longitudinal Studies (CLS), UCL Social Research Institute, for the use of the MCS data and to the UK Data Service for making them available. However, neither CLS nor the UK Data Service bear any responsibility for the analysis or interpretation of these data.
Gouin, J.‐P. , de la Torre‐Luque, A. , Sánchez‐Carro, Y. , Geoffroy, M.‐C. , & Essau, C. (2023). Heterogeneity in the trajectories of psychological distress among late adolescents during the COVID‐19 pandemic. JCPP Advances, 3(4), e12195. 10.1002/jcv2.12195
DATA AVAILABILITY STATEMENT
Data from the MCS are public and can be accessed online.
REFERENCES
- Aknin, L. B. , Andretti, B. , Goldszmidt, R. , Helliwell, J. F. , Petherick, A. , De Neve, J.‐E. , Dunn, E. W. , Fancourt, D. , Goldberg, E. , Jones, S. P. , Karadag, O. , Karam, E. , Layard, R. , Saxena, S. , Thornton, E. , Whillans, A. , & Zaki, J. (2022). Policy stringency and mental health during the COVID‐19 pandemic: A longitudinal analysis of data from 15 countries. The Lancet Public Health, 7(5), e417–e426. 10.1016/S2468-2667(22)00060-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amendola, S. , von Wyl, A. , Volken, T. , Zysset, A. , Huber, M. , & Dratva, J. (2021). A longitudinal study on generalized anxiety among university students during the first wave of the COVID‐19 pandemic in Switzerland. Frontiers in Psychology, 12, 643171. 10.3389/fpsyg.2021.643171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett, J. J. , Žukauskienė, R. , & Sugimura, K. (2014). The new life stage of emerging adulthood at ages 18‐29 years: Implications for mental health. The Lancet Psychiatry, 1(7), 569–576. 10.1016/S2215-0366(14)00080-7 [DOI] [PubMed] [Google Scholar]
- Benatov, J. , Ochnik, D. , Rogowska, A. M. , Arzenšek, A. , & Mars Bitenc, U. (2022). Prevalence and sociodemographic predictors of mental health in a representative sample of young adults from Germany, Israel, Poland, and Slovenia: A longitudinal study during the COVID‐19 pandemic. International Journal of Environmental Research and Public Health, 19(3), 1334. 10.3390/ijerph19031334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beutel, M. E. , Klein, E. M. , Brähler, E. , Reiner, I. , Jünger, C. , Michal, M. , Wiltink, J. , Wild, P. S. , Münzel, T. , Lackner, K. J. , & Tibubos, A. N. (2017). Loneliness in the general population: Prevalence, determinants and relations to mental health. BMC Psychiatry, 17(1), 7. 10.1186/s12888-017-1262-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouter, D. C. , Zarchev, M. , de Neve‐Enthoven, N. G. M. , Ravensbergen, S. J. , Kamperman, A. M. , Hoogendijk, W. J. G. , & Grootendorst‐van Mil, N. H. (2022). A longitudinal study of mental health in at‐risk adolescents before and during the COVID‐19 pandemic. European Child & Adolescent Psychiatry, 1–9. 10.1007/s00787-021-01935-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brohan, E. , Gauci, D. , Sartorius, N. , & Thornicroft, G. , & GAMIAN‐Europe Study Group . (2011). Self‐stigma, empowerment and perceived discrimination among people with bipolar disorder or depression in 13 European countries: The GAMIAN‐europe study. Journal of Affective Disorders, 129(1–3), 56–63. 10.1016/j.jad.2010.09.001 [DOI] [PubMed] [Google Scholar]
- Bu, F. , Steptoe, A. , & Fancourt, D. (2020). Loneliness during a strict lockdown: Trajectories and predictors during the COVID‐19 pandemic in 38,217 United Kingdom adults. Social Science & Medicine, 265(1982), 265, 113521. 10.1016/j.socscimed.2020.113521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, J. T. , & Hawkley, L. C. (2009). Perceived social isolation and cognition. Trends in Cognitive Sciences, 13(10), 447–454. 10.1016/j.tics.2009.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo, J. T. , Hawkley, L. C. , & Thisted, R. A. (2010). Perceived social isolation makes me sad: 5‐year cross‐lagged analyses of loneliness and depressive symptomatology in the Chicago health, aging, and social relations study. Psychology and Aging, 25(2), 453–463. 10.1037/a0017216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connelly, R. , & Platt, L. (2014). Cohort profile: UK Millennium cohort study (mcs). International Journal of Epidemiology, 43(6), 1719–1725. 10.1093/ije/dyu001 [DOI] [PubMed] [Google Scholar]
- Cooper, K. , Hards, E. , Moltrecht, B. , Reynolds, S. , Shum, A. , McElroy, E. , & Loades, M. (2021). Loneliness, social relationships, and mental health in adolescents during the COVID‐19 pandemic. Journal of Affective Disorders, 289, 98–104. 10.1016/j.jad.2021.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutrona, C. E. , & Russell, D. W. (1983). The Provisions of social relationships and adaptation to stress. In Jones W. H. & Perlman D. (Eds.), Advances in personal relationships (pp. 37–67). Jessica Kingsley Publishers. [Google Scholar]
- Daly, M. , & Robinson, E. (2022). Psychological distress associated with the second COVID‐19 wave: Prospective evidence from the UK Household Longitudinal Study. Journal of Affective Disorders, 310, 274–278. 10.1016/j.jad.2022.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De France, K. , Hancock, G. R. , Stack, D. M. , Serbin, L. A. , & Hollenstein, T. (2022). The mental health implications of COVID‐19 for adolescents: Follow‐up of a four‐wave longitudinal study during the pandemic. American Psychologist, 77(1), 85–99. 10.1037/amp0000838 [DOI] [PubMed] [Google Scholar]
- Del‐Valle, M. V. , López‐Morales, H. , Gelpi‐Trudo, R. , Poó, F. M. , García, M. J. , Yerro‐Avincetto, M. , Andrés, M. L. , Canet‐Juric, L. , & Urquijo, S. (2022). More than a year of pandemic: Longitudinal assessment of anxiety and depressive symptoms in the argentine general population during the COVID‐19 outbreak. Stress and Health : Journal of the International Society for the Investigation of Stress, 38(5), 1070–1079. 10.1002/smi.3163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Moor, M. H. , Beem, A. L. , Stubbe, J. H. , Boomsma, D. I. , & De Geus, E. J. (2006). Regular exercise, anxiety, depression and personality: A population‐based study. Preventive Medicine, 42(4), 273–279. 10.1016/j.ypmed.2005.12.002 [DOI] [PubMed] [Google Scholar]
- Ellwardt, L. , & Präg, P. (2021). Heterogeneous mental health development during the COVID‐19 pandemic in the United Kingdom. Scientific Reports, 11(1), 15958. 10.1038/s41598-021-95490-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erzen, E. , & Çikrikci, Ö. (2018). The effect of loneliness on depression: A meta‐analysis. International Journal of Social Psychiatry, 64(5), 427–435. 10.1177/0020764018776349 [DOI] [PubMed] [Google Scholar]
- Essau, C. A. , & de la Torre‐Luque, A. (2021). Adolescent psychopathological profiles and the outcome of the COVID‐19 pandemic: Longitudinal findings from the UK Millennium Cohort Study. Progress in Neuro‐Psychopharmacology and Biological Psychiatry, 110, 110330. 10.1016/j.pnpbp.2021.110330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Essau, C. A. , Olaya, B. , Anastassiou‐Hadjicharalambous, X. , Pauli, G. , Gilvarry, C. , Bray, D. , O’Callaghan, J. , & Ollendick, T. H. (2012). Psychometric properties of the strength and difficulties questionnaire from five European countries. International Journal of Methods in Psychiatric Research, 21(3), 232–245. 10.1002/mpr.1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández‐Theoduloz, G. , Paz, V. , Nicolaisen‐Sobesky, E. , Pérez, A. , Buunk, A. P. , Cabana, Á. , & Gradin, V. B. (2019). Social avoidance in depression: A study using a social decision‐making task. Journal of Abnormal Psychology, 128(3), 234–244. 10.1037/abn0000415 [DOI] [PubMed] [Google Scholar]
- Fluharty, M. , Bu, F. , Steptoe, A. , & Fancourt, D. (2021). Coping strategies and mental health trajectories during the first 21 weeks of COVID‐19 lockdown in the United Kingdom. Social Science & Medicine, 279(1982), 279, 113958. 10.1016/j.socscimed.2021.113958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster, S. , Estévez‐Lamorte, N. , Walitza, S. , & Mohler‐Kuo, M. (2023). The impact of the COVID‐19 pandemic on young adults' mental health in Switzerland: A longitudinal cohort study from 2018 to 2021. International Journal of Environmental Research and Public Health, 20(3), 2598. 10.3390/ijerph20032598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foulkes, L. , & Blakemore, S.‐J. (2021). Individual differences in adolescent mental health during COVID‐19: The importance of peer relationship quality. Neuron, 109(20), 3203–3205. 10.1016/j.neuron.2021.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariépy, G. , Honkaniemi, H. , & Quesnel‐Vallée, A. (2016). Social support and protection from depression: Systematic review of current findings in Western countries. The British Journal of Psychiatry : Journal of Mental Science, 209(4), 284–293. 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- González‐Sanguino, C. , Ausín, B. , Castellanos, M. Á. , Saiz, J. , López‐Gómez, A. , Ugidos, C. , & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID‐19) in Spain. Brain, Behavior, and Immunity, 87, 172–176. 10.1016/j.bbi.2020.05.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman, R. , Meltzer, H. , & Bailey, V. (1998). The strengths and difficulties questionnaire: A pilot study on the validity of the self‐report version. European Child & Adolescent Psychiatry, 7(3), 125–130. 10.1007/s007870050057 [DOI] [PubMed] [Google Scholar]
- Gouin, J. P. , MacNeil, S. , de la Torre‐Luque, A. , Chartrand, E. , Chadi, N. , Rouquette, A. , Boivin, M. , Côté, S. , & Geoffroy, M. C. (2023). Depression, anxiety, and suicidal ideation in a population‐based cohort of young adults before and during the first 12 months of the COVID‐19 pandemic in Canada. Canadian journal of public health = Revue canadienne de sante publique, 114(3), 368–377. 10.17269/s41997-023-00772-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger, S. , Calhoun, B. H. , Fleming, C. , Rhew, I. C. , & Lee, C. M. (2022). Mental health and well‐being trends through the first year‐and‐a‐half of the COVID‐19 pandemic: Results from a longitudinal study of young adults in the USA. Prevention Science : The Official Journal of the Society for Prevention Research, 23(6), 1–12. 10.1007/s11121-022-01382-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green, B. L. , Furrer, C. J. , & McAllister, C. L. (2011). Does attachment style influence social support or the other way around? A longitudinal study of early head start mothers. Attachment & Human Development, 13(1), 27–47. 10.1080/14616734.2010.488121 [DOI] [PubMed] [Google Scholar]
- Grey, I. , Arora, T. , Thomas, J. , Saneh, A. , Tohme, P. , & Abi‐Habib, R. (2020). The role of perceived social support on depression and sleep during the COVID‐19 pandemic. Psychiatry Research, 293, 113452. 10.1016/j.psychres.2020.113452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo, Y. , Cheng, C. , Zeng, Y. , Li, Y. , Zhu, M. , Yang, W. , Xu, H. , Li, X. , Leng, J. , Monroe‐Wise, A. , & Wu, S. (2020). Mental health disorders and associated risk factors in quarantined adults during the COVID‐19 outbreak in China: Cross‐sectional study. Journal of Medical Internet Research, 22(8), e20328. 10.2196/20328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen, C. (2016). Depression and stressful environments: Identifying gaps in conceptualization and measurement. Anxiety, Stress & Coping, 29(4), 335–351. 10.1080/10615806.2015.1134788 [DOI] [PubMed] [Google Scholar]
- Hamza, C. A. , Ewing, L. , Heath, N. L. , & Goldstein, A. L. (2021). When social isolation is nothing new: A longitudinal study on psychological distress during COVID‐19 among university students with and without preexisting mental health concerns. Canadian Psychology/Psychologie Canadienne, 62(1), 20–30. 10.1037/cap0000255 [DOI] [Google Scholar]
- Hamza, C. A. , Willoughby, T. , & Heffer, T. (2015). Impulsivity and nonsuicidal self‐injury: A review and meta‐analysis. Clinical Psychology Review, 38, 13–24. 10.1016/j.cpr.2015.02.010 [DOI] [PubMed] [Google Scholar]
- Hargrove, T. W. , Halpern, C. T. , Gaydosh, L. , Hussey, J. M. , Whitsel, E. A. , Dole, N. , Hummer, R. A. , & Harris, K. M. (2020). Race/ethnicity, gender, and trajectories of depressive symptoms across early‐ and mid‐life among the Add health cohort. Journal of racial and ethnic health disparities, 7(4), 619–629. 10.1007/s40615-019-00692-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartas, D. (2023). Wellbeing, psychological distress and self‐harm in late adolescence in the UK: The role of gender and personality traits. European Journal of Special Needs Education, 1–18. 10.1080/08856257.2023.2200107 [DOI] [Google Scholar]
- Hawke, L. D. , Szatmari, P. , Cleverley, K. , Courtney, D. , Cheung, A. , Voineskos, A. N. , & Henderson, J. (2021). Youth in a pandemic: A longitudinal examination of youth mental health and substance use concerns during COVID‐19. BMJ Open, 11(10), e049209. 10.1136/bmjopen-2021-049209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley, L. C. , & Cacioppo, J. T. (2010). Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine, 40(2), 218–227. 10.1007/s12160-010-9210-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopko, D. R. , & Mullane, C. M. (2008). Exploring the relation of depression and overt behavior with daily diaries. Behaviour Research and Therapy, 46(9), 1085–1089. 10.1016/j.brat.2008.05.002 [DOI] [PubMed] [Google Scholar]
- Hu, J. , Leite, W. L. , & Gao, M. (2017). An evaluation of the use of covariates to assist in class enumeration in linear growth mixture modeling. Behavior Research Methods, 49(3), 1179–1190. 10.3758/s13428-016-0778-1 [DOI] [PubMed] [Google Scholar]
- Hu, Y. , & Gutman, L. M. (2021). The trajectory of loneliness in UK young adults during the summer to winter months of COVID‐19. Psychiatry Research, 303, 114064. 10.1016/j.psychres.2021.114064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Barker, P. R. , Colpe, L. J. , Epstein, J. F. , Gfroerer, J. C. , Hiripi, E. , Howes, M. J. , Normand, S. L. T. , Manderscheid, R. W. , Walters, E. E. , & Zaslavsky, A. M. (2003). Screening for serious mental illness in the general population. Archives of General Psychiatry, 60(2), 184. 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- Killgore, W. D. S. , Taylor, E. C. , Cloonan, S. A. , & Dailey, N. S. (2020). Psychological resilience during the COVID‐19 lockdown. Psychiatry Research, 291, 113216. 10.1016/j.psychres.2020.113216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King, K. M. , Feil, M. C. , & Halvorson, M. A. (2018). Negative urgency is correlated with the use of reflexive and disengagement emotion regulation strategies. Clinical Psychological Science, 6(6), 822–834. 10.1177/2167702618785619 [DOI] [Google Scholar]
- Knox, L. , Karantzas, G. C. , Romano, D. , Feeney, J. A. , & Simpson, J. A. (2022). One year on: What we have learned about the psychological effects of COVID‐19 social restrictions: A meta‐analysis. Current Opinion in Psychology, 46, 101315. 10.1016/j.copsyc.2022.101315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraav, S. L. , Lehto, S. M. , Junttila, N. , Ruusunen, A. , Kauhanen, J. , Hantunen, S. , & Tolmunen, T. (2021). Depression and loneliness may have a direct connection without mediating factors. Nordic Journal of Psychiatry, 75(7), 553–557. 10.1080/08039488.2021.1894231 [DOI] [PubMed] [Google Scholar]
- Kunzler, A. M. , Röthke, N. , Günthner, L. , Stoffers‐Winterling, J. , Tüscher, O. , Coenen, M. , Rehfuess, E. , Schwarzer, G. , Binder, H. , Schmucker, C. , Meerpohl, J. J. , & Lieb, K. (2021). Mental burden and its risk and protective factors during the early phase of the SARS‐CoV‐2 pandemic: Systematic review and meta‐analyses. Globalization and Health, 17(1), 34. 10.1186/s12992-021-00670-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laham, S. , Bertuzzi, L. , Deguen, S. , Hecker, I. , Melchior, M. , Patanè, M. , Pinucci, I. , Sijbrandij, M. , & van der Waerden, J. (2021). Impact of longitudinal social support and loneliness trajectories on mental health during the COVID‐19 pandemic in France. International Journal of Environmental Research and Public Health, 18(23), 12677. 10.3390/ijerph182312677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J. O. , Kapteyn, A. , Clomax, A. , & Jin, H. (2021). Estimating influences of unemployment and underemployment on mental health during the COVID‐19 pandemic: Who suffers the most? Public Health, 201, 48–54. 10.1016/j.puhe.2021.09.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Zhao, J. , Ma, Z. , McReynolds, L. S. , Lin, D. , Chen, Z. , Wang, T. , Wang, D. , Zhang, Y. , Zhang, J. , Fan, F. , & Liu, X. (2021). Mental health among College students during the COVID‐19 pandemic in China: A 2‐wave longitudinal survey. Journal of Affective Disorders, 281, 597–604. 10.1016/j.jad.2020.11.109 [DOI] [PubMed] [Google Scholar]
- Lin, M. , Henry, C. Lucas , Shmueli, G. , & Lin, M. (2013). Too big to fail: Large samples and the p ‐value problem. Information Systems Research, 7047(June 2014), 1–12. 10.1287/isre.2013.0480 [DOI] [Google Scholar]
- Loades, M. E. , Chatburn, E. , Higson‐Sweeney, N. , Reynolds, S. , Shafran, R. , Brigden, A. , Linney, C. , McManus, M. N. , Borwick, C. , & Crawley, E. (2020). Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. Journal of the American Academy of Child & Adolescent Psychiatry, 59(11), 1218–1239.e3. 10.1016/j.jaac.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loibl, C. , Drost, M. A. , Huisman, M. , Suanet, B. , Bruine de Bruin, W. , McNair, S. , & Summers, B. (2021). Worry about debt is related to social loneliness in older adults in The Netherlands. Ageing and Society, 42(12), 1–23. 10.1017/S0144686X21000325 [DOI] [Google Scholar]
- Longman, J. , Patrick, R. , Bernays, S. , & Charlson, F. (2023). Three reasons Why expecting 'recovery' in the context of the mental health impacts of climate change is problematic. International Journal of Environmental Research and Public Health, 20(10), 5882. 10.3390/ijerph20105882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, W. (2019). Adolescent depression: National trends, risk factors, and Healthcare disparities. American Journal of Health Behavior, 43(1), 181–194. 10.5993/AJHB.43.1.15 [DOI] [PubMed] [Google Scholar]
- Luchetti, M. , Lee, J. H. , Aschwanden, D. , Sesker, A. , Strickhouser, J. E. , Terracciano, A. , & Sutin, A. R. (2020). The trajectory of loneliness in response to COVID‐19. American Psychologist, 75(7), 897–908. 10.1037/amp0000690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch, H. , McDonagh, C. , & Hennessy, E. (2021). Social anxiety and depression stigma among adolescents. Journal of Affective Disorders, 281, 744–750. 10.1016/j.jad.2020.11.073 [DOI] [PubMed] [Google Scholar]
- Madigan, S. , Racine, N. , Vaillancourt, T. , Korczak, D. J. , Hewitt, J. M. A. , Pador, P. , Park, J. L. , McArthur, B. A. , Holy, C. , & Neville, R. D. (2023). Changes in depression and anxiety among children and adolescents from before to during the COVID‐19 pandemic: A systematic review and meta‐analysis. JAMA Pediatrics, 177(6), 567–581. 10.1001/jamapediatrics.2023.0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magson, N. R. , Freeman, J. Y. A. , Rapee, R. M. , Richardson, C. E. , Oar, E. L. , & Fardouly, J. (2021). Risk and protective factors for prospective changes in adolescent mental health during the COVID‐19 pandemic. Journal of Youth and Adolescence, 50(1), 44–57. 10.1007/s10964-020-01332-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manchia, M. , Gathier, A. W. , Yapici‐Eser, H. , Schmidt, M. V. , de Quervain, D. , van Amelsvoort, T. , Bisson, J. I. , Cryan, J. F. , Howes, O. D. , Pinto, L. , van der Wee, N. J. , Domschke, K. , Branchi, I. , & Vinkers, C. H. (2022). The impact of the prolonged COVID‐19 pandemic on stress resilience and mental health: A critical review across waves. European Neuropsychopharmacology : The Journal of the European College of Neuropsychopharmacology, 55, 22–83. 10.1016/j.euroneuro.2021.10.864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marani, M. , Katul, G. G. , Pan, W. K. , & Parolari, A. J. (2021). Intensity and frequency of extreme novel epidemics. Proceedings of the National Academy of Sciences of the United States of America, 118(35), e2105482118. 10.1073/pnas.2105482118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martín‐María, N. , Caballero, F. F. , Lara, E. , Domènech‐Abella, J. , Haro, J. M. , Olaya, B. , Ayuso‐Mateos, J. L. , & Miret, M. (2021). Effects of transient and chronic loneliness on major depression in older adults: A longitudinal study. International Journal of Geriatric Psychiatry, 36(1), 76–85. 10.1002/gps.5397 [DOI] [PubMed] [Google Scholar]
- Mewton, L. , Kessler, R. C. , Slade, T. , Hobbs, M. J. , Brownhill, L. , Birrell, L. , Tonks, Z. , Teesson, M. , Newton, N. , Chapman, C. , Allsop, S. , Hides, L. , McBride, N. , & Andrews, G. (2016). The psychometric properties of the Kessler Psychological Distress Scale (K6) in a general population sample of adolescents. Psychological Assessment, 28(10), 1232–1242. 10.1037/pas0000239 [DOI] [PubMed] [Google Scholar]
- Miething, A. , Almquist, Y. B. , Östberg, V. , Rostila, M. , Edling, C. , & Rydgren, J. (2016). Friendship networks and psychological well‐being from late adolescence to young adulthood: A gender‐specific structural equation modeling approach. BMC Psychology, 4(1), 34. 10.1186/s40359-016-0143-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgül, E. , Kallitsoglou, A. , Essau, C. A. , & Castro‐Kemp, S. (2022). Caregiver‐reported changes in the socioemotional wellbeing and daily habits of children with special educational needs during the first COVID‐19 national lockdown in the United Kingdom. Frontiers in Education, 7, 838938. 10.3389/feduc.2022.838938 [DOI] [Google Scholar]
- Morgül, E. , Kallitsoglou, A. , Essau, C. A. , Castro‐kemp, S. , & Mateo, E. A. (2022). Caregiver‐reported changes in the socioemotional wellbeing and daily habits of children with special educational needs during the first COVID‐19 national lockdown in the United Kingdom. Frontiers in Education, 7(February), 1–12. 10.3389/feduc.2022.838938 [DOI] [Google Scholar]
- Nylund‐Gibson, K. , Garber, A. C. , Carter, D. B. , Chan, M. , Arch, D. A. N. , Simon, O. , Whaling, K. , Tartt, E. , & Lawrie, S. I. (2023). Ten frequently asked questions about latent transition analysis. Psychological Methods, 28(2), 284–300. 10.1037/met0000486 [DOI] [PubMed] [Google Scholar]
- O’Connor, R. C. , Wetherall, K. , Cleare, S. , McClelland, H. , Melson, A. J. , Niedzwiedz, C. L. , O’Carroll, R. E. , O’Connor, D. B. , Platt, S. , Scowcroft, E. , Watson, B. , Zortea, T. , Ferguson, E. , & Robb, K. A. (2021). Mental health and well‐being during the COVID‐19 pandemic: Longitudinal analyses of adults in the UK COVID‐19 Mental Health & Wellbeing study. The British Journal of Psychiatry: Journal of Mental Science, 218(6), 326–333. 10.1192/bjp.2020.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orgilés, M. , Morales, A. , Delvecchio, E. , Mazzeschi, C. , & Espada, J. P. (2020). Immediate psychological effects of the COVID‐19 quarantine in youth from Italy and Spain. Frontiers in Psychology, 11, 579038. 10.3389/fpsyg.2020.579038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ori, A. P. S. , Wieling, M. , & Corona, L. (2022). Longitudinal analyses of depression and anxiety highlight greater prevalence during COVID‐19 lockdowns in the Dutch general population and a continuing increase in suicidal ideation in young adults.
- Patel, K. , Robertson, E. , Kwong, A. S. F. , Griffith, G. J. , Willan, K. , Green, M. J. , Di Gessa, G. , Huggins, C. F. , McElroy, E. , Thompson, E. J. , Maddock, J. , Niedzwiedz, C. L. , Henderson, M. , Richards, M. , Steptoe, A. , Ploubidis, G. B. , Moltrecht, B. , Booth, C. , Fitzsimons, E. , & Katikireddi, S. V. (2022). Psychological distress before and during the COVID‐19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Network Open, 5(4), e227629. 10.1001/jamanetworkopen.2022.7629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettit, J. W. , Roberts, R. E. , Lewinsohn, P. M. , Seeley, J. R. , & Yaroslavsky, I. (2011). Developmental relations between perceived social support and depressive symptoms through emerging adulthood: Blood is thicker than water. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43), 25(1), 127–136. 10.1037/a0022320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, M. , McManus, S. , Hope, H. , Hotopf, M. , Ford, T. , Hatch, S. L. , John, A. , Kontopantelis, E. , Webb, R. T. , Wessely, S. , & Abel, K. M. (2021). Mental health responses to the COVID‐19 pandemic: A latent class trajectory analysis using longitudinal UK data. The Lancet Psychiatry, 8(7), 610–619. 10.1016/S2215-0366(21)00151-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati, G. , & Mancini, A. D. (2021). The psychological impact of COVID‐19 pandemic lockdowns: A review and meta‐analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proust‐lima, C. , & Liquet, B. (2017). Estimation of extended mixed models using latent classes and latent processes: The R package lcmm.
- Racine, N. , McArthur, B. A. , Cooke, J. E. , Eirich, R. , Zhu, J. , & Madigan, S. (2021). Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID‐19: A meta‐analysis. JAMA Pediatrics, 175(11), 1142–1150. 10.1001/jamapediatrics.2021.2482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ram, N. , & Grimm, K. J. (2009). Growth mixture modeling: A method for identifying differences in longitudinal change among unobserved groups. International Journal of Behavioral Development, 33(6), 565–576. 10.1177/0165025409343765.Growth [DOI] [PMC free article] [PubMed] [Google Scholar]
- Refaeli, T. , & Achdut, N. (2021). Financial strain and loneliness among young adults during the COVID‐19 pandemic: The role of psychosocial resources. Sustainability, 13(12), 6942. 10.3390/su13126942 [DOI] [Google Scholar]
- Rimfeld, K. , Malanchini, M. , Arathimos, R. , Gidziela, A. , Pain, O. , McMillan, A. , Ogden, R. , Webster, L. , Packer, A. E. , Shakeshaft, N. G. , Schofield, K. L. , Pingault, J.‐B. , Allegrini, A. G. , Stringaris, A. , von Stumm, S. , Lewis, C. M. , & Plomin, R. (2021). The consequences of a year of the COVID‐19 pandemic for the mental health of young adult twins in England and Wales. In MedRxiv: The preprint server for health sciences. 10.1101/2021.10.07.21264655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, E. , Sutin, A. R. , Daly, M. , & Jones, A. (2022). A systematic review and meta‐analysis of longitudinal cohort studies comparing mental health before versus during the COVID‐19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowska, A. M. , Ochnik, D. , Kuśnierz, C. , Chilicka, K. , Jakubiak, M. , Paradowska, M. , Głazowska, L. , Bojarski, D. , Fijołek, J. , Podolak, M. , Tomasiewicz, M. , Nowicka, D. , Kawka, M. , Grabarczyk, M. , & Babińska, Z. (2021). Changes in mental health during three waves of the COVID‐19 pandemic: A repeated cross‐sectional study among polish university students. BMC Psychiatry, 21(1), 627. 10.1186/s12888-021-03615-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rueger, S. Y. , Malecki, C. K. , Pyun, Y. , Aycock, C. , & Coyle, S. (2016). A meta‐analytic review of the association between perceived social support and depression in childhood and adolescence. Psychological Bulletin, 142(10), 1017–1067. 10.1037/bul0000058 [DOI] [PubMed] [Google Scholar]
- Russell, D. W. (1996). UCLA loneliness scale (version 3): Reliability, validity, and factor structure. Journal of Personality Assessment, 66(1), 20–40. 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Sahu, P. (2020). Closure of universities due to coronavirus disease 2019 (COVID‐19): Impact on education and mental health of students and academic Staff. Cureus. 10.7759/cureus.7541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders, R. , Buckman, J. E. J. , Fonagy, P. , & Fancourt, D. (2021). Understanding different trajectories of mental health across the general population during the COVID‐19 pandemic. Psychological Medicine, 52(16), 1–9. 10.1017/S0033291721000957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scales, P. C. , Benson, P. L. , Oesterle, S. , Hill, K. G. , Hawkins, J. D. , & Pashak, T. J. (2016). The dimensions of successful young adult development: A conceptual and measurement framework. Applied Developmental Science, 20(3), 150–174. 10.1080/10888691.2015.1082429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scardera, S. , Perret, L. C. , Ouellet‐Morin, I. , Gariépy, G. , Juster, R.‐P. , Boivin, M. , Turecki, G. , Tremblay, R. E. , Côté, S. , & Geoffroy, M.‐C. (2020). Association of social support during adolescence with depression, anxiety, and suicidal ideation in young adults. JAMA Network Open, 3(12), e2027491. 10.1001/jamanetworkopen.2020.27491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoon, I. , & Henseke, G. (2022). Social inequalities in young people’s mental distress during the COVID‐19 pandemic: Do psychosocial resource factors matter? Frontiers in Public Health, 10, 820270. 10.3389/fpubh.2022.820270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz‐Mette, R. A. , Duell, N. , Lawrence, H. R. , & Balkind, E. G. (2022). COVID‐19 distress impacts adolescents’ depressive symptoms, NSSI, and suicide risk in the rural, northeast US. Journal of Clinical Child and Adolescent Psychology, 1–14. 10.1080/15374416.2022.2042697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd, P. , & Gilbert, E. (2019). Millennium cohort study. Ethical review and consent (Issue November).
- Smith, K. , Bhui, K. , & Cipriani, A. (2020). COVID‐19, mental health and ethnic minorities. Evidence‐Based Mental Health, 23(3), 89–90. 10.1136/ebmental-2020-300174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solmi, M. , Radua, J. , Olivola, M. , Croce, E. , Soardo, L. , Salazar de Pablo, G. , Il Shin, J. , Kirkbride, J. B. , Jones, P. , Kim, J. H. , Kim, J. Y. , Carvalho, A. F. , Seeman, M. V. , Correll, C. U. , & Fusar‐Poli, P. (2022). Age at onset of mental disorders worldwide: Large‐scale meta‐analysis of 192 epidemiological studies. Molecular Psychiatry, 27(1), 281–295. 10.1038/s41380-021-01161-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegelhalter, D. J. , Best, N. G. , Carlin, B. P. , & Van der Linde, A. (2002). Bayesian measures of model complexity and fit (with discussion). Journal of the Royal Statistical Society: Series B, 64(4), 583–616. 10.1111/1467-9868.00353 [DOI] [Google Scholar]
- Spithoven, A. W. M. , Bijttebier, P. , & Goossens, L. (2017). It is all in their mind: A review on information processing bias in lonely individuals. Clinical Psychology Review, 58, 97–114. 10.1016/j.cpr.2017.10.003 [DOI] [PubMed] [Google Scholar]
- Stassart, C. , Wagener, A. , & Etienne, A.‐M. (2021). Parents’ perceived impact of the societal lockdown of COVID‐19 on family well‐being and on the emotional and behavioral state of Walloon Belgian children aged 4 to 13 Years: An exploratory study. Psychologica Belgica, 61(1), 186. 10.5334/pb.1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud, I. , & Gutman, L. M. (2021). Longitudinal changes in the mental health of UK young male and female adults during the COVID‐19 pandemic. Psychiatry Research, 303, 114074. 10.1016/j.psychres.2021.114074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun, Y. , Wu, Y. , Fan, S. , Dal Santo, T. , Li, L. , Jiang, X. , Li, K. , Wang, Y. , Tasleem, A. , Krishnan, A. , Bonardi, O. , Boruff, J. T. , Rice, D. B. , Markham, S. , Levis, B. , Azar, M. , Thombs‐Vite, I. , Neupane, D. , & Thombs, B. D. (2023). Comparison of mental health symptoms before and during the covid‐19 pandemic: Evidence from a systematic review and meta‐analysis of 134 cohorts. BMJ, 380. 10.1136/bmj-2022-074224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkody, E. , Stearns, M. , Stanhope, L. , & McKinney, C. (2021). Stress‐buffering role of social support during COVID‐19. Family Process, 60(3), 1002–1015. 10.1111/famp.12618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Health Foundation . (2023). Retrieved from https://www.health.org.uk/news‐and‐comment/charts‐and‐infographics/covid‐19‐policy‐tracker
- Thoits, P. A. (1986). Social support as coping assistance. Journal of Consulting and Clinical Psychology, 54(4), 416–423. 10.1037//0022-006x.54.4.416 [DOI] [PubMed] [Google Scholar]
- Thompson, R. F. (2010). Habituation. Encyclopedia of Behavioral Neuroscience, 1–5. ISBN 9780080453965. 10.1016/B978-0-08-045396-5.00138-X [DOI] [Google Scholar]
- Tiirikainen, K. , Haravuori, H. , Ranta, K. , Kaltiala‐Heino, R. , & Marttunen, M. (2019). Psychometric properties of the 7‐item Generalized Anxiety Disorder Scale (GAD‐7) in a large representative sample of Finnish adolescents. Psychiatry Research, 272, 30–35. 10.1016/j.psychres.2018.12.004 [DOI] [PubMed] [Google Scholar]
- Uh, S. , Dalmaijer, E. S. , Siugzdaite, R. , Ford, T. J. , & Astle, D. E. (2021). Two pathways to self‐harm in adolescence. Journal of the American Academy of Child & Adolescent Psychiatry, 60(12), 1491–1500. 10.1016/j.jaac.2021.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vancampfort, D. , Stubbs, B. , Sienaert, P. , Wyckaert, S. , De Hert, M. , Rosenbaum, S. , & Probst, M. (2015). What are the factors that influence physical activity participation in individuals with depression? A review of physical activity correlates from 59 studies. Psychiatria Danubina, 27(3), 210–224. [PubMed] [Google Scholar]
- Varga, T. V. , Bu, F. , Dissing, A. S. , Elsenburg, L. K. , Bustamante, J. J. H. , Matta, J. , van Zon, S. K. R. , Brouwer, S. , Bültmann, U. , Fancourt, D. , Hoeyer, K. , Goldberg, M. , Melchior, M. , Strandberg‐Larsen, K. , Zins, M. , Clotworthy, A. , & Rod, N. H. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID‐19 pandemic: A longitudinal analysis of 200,000 western and northern Europeans. The Lancet Regional Health ‐ Europe, 2, 100020. 10.1016/j.lanepe.2020.100020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt, J. K. (2010). Latent class modeling with covariates: Two improved three‐step approaches. Political Analysis, 18(4), 450–469. 10.1093/pan/mpq025 [DOI] [Google Scholar]
- Watkins‐Martin, K. , Orri, M. , Pennestri, M.‐H. , Castellanos‐Ryan, N. , Larose, S. , Gouin, J.‐P. , Ouellet‐Morin, I. , Chadi, N. , Philippe, F. , Boivin, M. , Tremblay, R. E. , Côté, S. , & Geoffroy, M.‐C. (2021). Depression and anxiety symptoms in young adults before and during the COVID‐19 pandemic: Evidence from a Canadian population‐based cohort. Annals of General Psychiatry, 20(1), 42. 10.1186/s12991-021-00362-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherall, K. , Cleare, S. , McClelland, H. , Melson, A. J. , Niedzwiedz, C. L. , O’Carroll, R. E. , O’Connor, D. B. , Platt, S. , Scowcroft, E. , Watson, B. , Zortea, T. , Ferguson, E. , Robb, K. A. , & O’Connor, R. C. (2022). Mental health and well‐being during the second wave of COVID‐19: Longitudinal analyses of the UK COVID‐19 Mental Health and Wellbeing study (UK COVID‐MH). BJPsych Open, 8(4), e103. 10.1192/bjo.2022.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wethington, E. , & Kessler, R. C. (1986). Perceived support, received support, and adjustment to stressful life events. Journal of Health and Social Behavior 27(1), 78–89. American Sociological Assn. 10.2307/2136504 [DOI] [PubMed] [Google Scholar]
- World Health Organization (2022). Mental health and COVID‐19: Early evidence of the pandemic’s impact: Scientific brief, 2 March 2022. Geneva (pp. 1–11).
- Xu, J. , Ou, J. , Luo, S. , Wang, Z. , Chang, E. , Novak, C. , Shen, J. , Zheng, S. , & Wang, Y. (2020). Perceived social support protects lonely people against COVID‐19 anxiety: A three‐wave longitudinal study in China. Frontiers in Psychology, 11, 566965. 10.3389/fpsyg.2020.566965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarrett, N. , & Eccles, J. (2006). The passage to adulthood: Challenges of late adolescence. New Directions for Youth Development, 2006(111), 13–17. 10.1002/yd.179 [DOI] [PubMed] [Google Scholar]
- Zhou, Y. , MacGeorge, E. L. , & Myrick, J. G. (2020). Mental health and its predictors during the early months of the COVID‐19 pandemic experience in the United States. International Journal of Environmental Research and Public Health, 17(17), 6315. 10.3390/ijerph17176315 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Data Availability Statement
Data from the MCS are public and can be accessed online.


