Abstract
The COVID-19 pandemic has had a profound impact on women's health, particularly on their menstrual cycles. The menstrual cycle serves as a crucial indicator of fertility and reproduction.
Objectives
This study aimed to examine the impact of COVID-19 infection and vaccination on menstrual regularity in Saudi women of childbearing age. Additionally, it sought to explore the potential effects of COVID-19 vaccination on serum hormonal levels during the follicular phase of the menstrual cycle, along with their relationship with Vit.D.
Methods
This case‒control study investigated the impact of COVID-19 infection and vaccination on menstrual regularity and hormonal function in Saudi women of reproductive age. Data were collected from 79 women who attended the Outpatient Department of Obstetrics and Gynaecology at King Faisal Medical Complex in Taif, Saudi Arabia. All participants had received COVID-19 vaccines. The data collection process was comprehensive, encompassing various participant characteristics, such as demographic information, history of COVID-19 infection, and details about menstrual patterns before and after infection and vaccination. Furthermore, hormonal measurements, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), oestradiol, prolactin, thyroid-stimulating hormone (TSH), and vitamin D (Vit.D) levels, were extracted from the participants' medical records.
Results
Among the participants, 39.24 % had a history of COVID-19 infection, and following the infection, there was a significant increase in the proportion of women experiencing irregular menstruation. After receiving the COVID-19 vaccine, 72.15 % of the participants continued to have irregular menstrual cycles. The study found that a considerable number of participants had menstrual cycles outside the normal range, with 43.80 % having cycles shorter than 21 days and 35.10 % having cycles longer than 35 days. Comparing participants with regular and irregular cycles after COVID-19 vaccination, no significant changes were observed in most hormonal levels. However, the prolactin hormone showed a significant increase in participants with irregular cycles, while Vit.D levels were significantly decreased in this group.
Conclusion
The study findings indicate a higher prevalence of irregular menstruation among participants, particularly after vaccination. Notably, irregular menstrual cycles were found to be associated with elevated levels of prolactin hormone and decreased levels of Vit.D.
Keywords: COVID-19 infection, COVID-19 vaccination, Menstrual cycle. FSH, LH, Prolactin, Vit.D
1. Introduction
The menstrual cycle is a biological process that occurs in the female reproductive system. It comprises monthly discharge of an ovum from the ovaries, which is transferred to the fallopian tube and into the uterus. If the ovum is not fertilized by sperm, it sheds along with the lining of the uterus, resulting in menstruation. Therefore, the menstrual cycle involves changes in the ovary and uterus. It on average lasts 28 days but can range from 21 to 35 days [1]. The ovarian cycle is controlled by hormones such as follicular stimulating hormone (FSH) and luteinizing hormone (LH): FSH is produced by the pituitary gland and stimulates the growth and development of follicles in the ovaries. LH is also produced by the pituitary gland and activates ovulation, which is the discharge of an ovum from the ovary. The production of FSH and LH is controlled by gonadotropic releasing hormone (GnRH) from the hypothalamus [2].
The uterine cycle is regulated by oestrogen, which is generated by the developing follicles in the ovaries and helps to thicken the lining of the uterus in preparation for a fertilized egg, and progesterone hormone, which is formed by the corpus luteum, which develops after ovulation and helps to maintain the thickened uterine lining in cases of pregnancy [3,4].
Another hormone that has an indirect effect on the menstrual cycle is prolactin: it is mainly responsible for stimulating milk production in the breasts after childbirth [5]. However, high concentrations of prolactin can interfere with ovulation and cause irregular periods or even complete menstruation cessation [6]. This disorder is identified as hyperprolactinemia and can be caused by some medications, tumours, or other medical conditions [7]. Prolactin constrains ovulation by suppressing the secretion of GnRH from the hypothalamus. GnRH is accountable for promoting the release of FSH and LH from the pituitary gland. When prolactin levels are high, it affects the normal pulsatile release of GnRH, leading to a decrease in FSH and LH secretion and eventually inhibiting ovulation. Therefore, lactation can act as a natural form of contraceptives in some women, as breast feeding enhances prolactin production and can suppress ovulation [8].
The ovarian cycle can be divided into three phases: follicular phase, ovulation, and luteal phase. In a female with a regular cycle (28 days), the follicular phase begins on the first day of menstruation and persists for approximately 14 days. Through this time, an ovum matures in one of the ovaries. Ovulation occurs when the mature ovum is liberated from the ovary and travels down the fallopian tube heading towards the uterus.
The uterine cycle can be split into three phases: menstruation, proliferation and secretion. Menstruation occurs when the endometrial layer of the uterus sheds and lasts for 3–7 days. The luteal phase begins after ovulation and lasts for approximately 14 days. Meanwhile, if fertilization does not occur, oestrogen and progesterone levels drop, and menstruation starts again [9]. The menstrual cycle plays a principal role in fertility and reproductive health. Variations in menstrual patterns or symptoms may suggest underlying health issues that should be addressed by a health care provider.
Coronavirus disease (COVID-19) is a highly contagious respiratory disease caused by the SARS-CoV-2 virus. The first incident of COVID-19 was detected in Wuhan, China, in December 2019. Then, it spread worldwide, causing a pandemic [10]. The most familiar symptoms of COVID-19 are fever, cough, fatigue, body aches, loss of taste or smell, and problems in breathing. The virus disseminates through respiratory droplets when a sick person coughs, sneezes or speaks [11]. To reduce the spread of COVID-19, it was advised to wear masks in public places, practice social distancing and regularly wash hands with soap and water [12]. Vaccines have been developed to protect against COVID-19 and are being distributed worldwide.
Vaccines work by motivating the immune system to generate antibodies against the virus, which can help stop infection or diminish the severity of symptoms if a person becomes infected [13,14]. There are currently numerous COVID-19 vaccines available, including those established by Pfizer-BioNTech, Moderna, Johnson & Johnson and AstraZeneca [15]. These vaccines have undergone precise testing and have been proven to be secure and effective in clinical experiments [16]. Many countries around the world have started vaccination campaigns to protect their residents from COVID-19. Governments and health organizations are persuading people to get vaccinated as soon as possible to help slow the spread of the virus and to end the pandemic [17].
It is worth noting that while COVID-19 vaccinations are very effective at stopping severe illness and hospitalization, they do not offer 100 % protection against infection [18]. It is still likely that vaccinated individuals will catch and spread the virus, so it is essential to continue practising other protective methods, such as wearing masks and social distancing. The vaccine does not include any hormones or other ingredients that could influence hormone levels or the menstrual cycle [19]. However, there are some publications suggesting that COVID-19 vaccines influence female menstrual cycle regularity [20,21].
The COVID-19 pandemic has had an extreme effect on the lives of people worldwide, and females of childbearing age have been influenced by the pandemic due to its consequences on their physical and mental health [22]. This study aims to answer the following questions:
-
•
What are the effects of COVID-19 infection/vaccination on menstrual regularity in women of childbearing age?
-
•
Are there any differences in menstrual regularity between those who have been infected with COVID-19 and those who have received the vaccine?
-
•
What are the potential implications of COVID-19 vaccination on serum levels of FSH, LH, oestradiol, prolactin, thyroid stimulating hormone (TSH), free T3, free T4 and vitamin D (Vit.D) during the follicular phase of the menstrual cycle?
This study investigates for the first time the effect of COVID-19 vaccination on serum levels of FSH, LH, oestradiol, prolactin, thyroid stimulating hormone (TSH), free T3, free T4 and Vit.D during the follicular phase of the menstrual cycle.
2. Material and methods
The study is a case‒control study in which data were collected randomly from every three women attending the blood collection room in the Outpatient Department of Obstetrics and Gynaecology at King Faisal Medical Complex (KFMC) in Taif City, Saudi Arabia. The total number of participants was 79 women. All participants received the COVID-19 vaccines. The data were collected using a data collection form designed for this study. The data include the participants’ characteristics, such as age, history of COVID-19 infection, menstruation pattern before and after COVID-19 infection, types of received doses of COVID-19 vaccine and menstruation pattern before and after the COVID-19 vaccine. In addition, their hormonal measurements were collected from their medical records. The data include serum levels of FSH, LH, oestradiol, prolactin, thyroid stimulating hormone (TSH), free T3, free T4 and Vit.D during the follicular phase of the menstrual cycle (samples were collected on day two or day three of the menstrual cycle). All these hormones were tested in the core lab at King Faisal Medical Complex by Cobas 6000 (e601) electrochemiluminescence (ECL) technology (Fig. 1). Sample inclusion criteria: nonlactating women of childbearing age (18–45 years) without known gynaecological conditions who regularly monitor their menstruation through an electronic calendar. Not receiving any hormonal contraceptives.
Fig. 1.
A diagram showing the overall organization of the developed methodology.
3. Statistical analysis
Graph Pad Prism version 8 was used to analyse the current data. Student's t-test analysis was utilized to compare various factors between the groups under study. To evaluate the relationship between Vit.D and other analysed hormones in the studied groups, Pearson's correlation coefficient was utilized. To investigate the association between two qualitative variables, the chi-square (X2) test was performed. P was deemed significant if it was less than 0.05 at the 95 % confidence level.
4. Results
A total of 79 participants who received the COVID-19 vaccine were included in this study. Table 1 shows the characteristics of the participants, such as age, history of COVID-19 infection, menstruation pattern before and after COVID-19 infection, types of received doses of COVID-19 vaccine and menstruation pattern before and after COVID-19 vaccination. The results demonstrated that the age groups of the study participants were between 18 and 45 years. The mean age was 33.92 ± 7.3 years; 31 (39.24 %) of them were infected with COVID-19. Before COVID-19 infection, 26 (83.87 %) of them had regular menstruation, and 5 (16.13 %) had irregular menstruation. After COVID-19 infection, irregularity of the menstrual cycle was found in 23 (74.19 %) patients. It was found that most of the study participants received the Pfizer vaccine as the first (78.48 %), second (92.11 %), and third (93.88 %) doses. Before the COVID-19 vaccine, 66 (83.54 %) of the participants were regularly menstruating, and 13 (16.46 %) were irregularly menstruating. After the COVID-19 vaccine, irregular cycles were found in 57 (72.15 %) of the participants.
Table 1.
Characteristics of the study participants (total number = 79).
| Variable | Number (No) | Percent (%) |
|---|---|---|
| Age (Years) | ||
| 18–24 | 9 | 11.39 % |
| 25–29 | 15 | 18.98 % |
| 30–34 | 18 | 22.78 % |
| 35–39 | 13 | 16.45 % |
| 40–45 | 24 | 30.37 % |
| History of COVID-19 infection | ||
| Yes | 31 | 39.24 % |
| No | 48 | 60.76 % |
| Menstruation pattern before COVID-19 infection: | ||
| Regular cycle | 26 | 83.87 % |
| Irregular cycle | 5 | 16.13 % |
| Menstruation pattern after COVID-19 infection: | ||
| Regular cycle | 8 | 25.81 % |
| Irregular cycle | 23 | 74.19 % |
| Types of received doses of COVID-19 vaccine: | ||
| First dose: | ||
| Pfizer | 62 | 78.48 % |
| AstraZeneca | 9 | 11.39 % |
| Moderna | 8 | 10.12 % |
| Second dose: | ||
| Pfizer | 70 | 92.11 % |
| AstraZeneca | 3 | 3.94 % |
| Moderna | 3 | 3.94 % |
| Third dose: | ||
| Pfizer | 46 | 93.88 % |
| AstraZeneca | 0 | 0 % |
| Moderna | 3 | 6.12 % |
| Menstruation pattern before COVID-19 vaccine: | ||
| Regular cycle | 66 | 83.54 % |
| Irregular cycle | 13 | 16.46 % |
| Menstruation pattern after COVID-19 vaccine: | ||
| Regular cycle | 22 | 27.85 % |
| Irregular cycle | 57 | 72.15 % |
Table 2 demonstrates the associated changes in the pattern of the menstrual cycle in participants with irregular cycles after COVID-19 vaccination. Regarding the menstrual cycle length, 25 (43.80 %) participants had their menstrual cycle for less than 21 days, 20 (35.10 %) for more than 35 days and 12 (21.10 %) for 21–35 days. The menstrual period lasted for less than five days in 10 (17.54 %) participants, for more than seven days in 24 (42.11 %) participants and for five to seven days in 23 (40.35 %) participants. After receiving the COVID-19 vaccine, the timing of the next period was earlier than usual in 29 (50.88 %), later than usual in 17 (29.82 %) and on time in 11 (19.29 %) of the participants. The flow of the period was lighter than usual in 13 (22.81 %), heavier than usual in 30 (52.63 %) and the same as usual in 14 (24.56 %) of the participants. Associated pain or cramps were less than usual in 9 (15.78 %), more than usual in 27 (47.36 %) and the same as usual in 21 (36.84 %) of the participants.
Table 2.
Associated changes in the pattern of the menstrual cycle in participants with irregular cycles after COVID-19 vaccination (number = 57).
| Variable | Number (No) | Percent (%) |
|---|---|---|
| How long is length of your menstrual cycle (in days)? | ||
| 21–35 days | 12 | 21.10 % |
| Less than 21 days | 25 | 43.80 % |
| More than 35 days | 20 | 35.10 % |
| How long does your menstrual period last (in days)? | ||
| 5–7 days | 23 | 40.35 % |
| Less than 5 days | 10 | 17.54 % |
| More than 7 days | 24 | 42.11 % |
| After receiving COVID-19 vaccine, the timing of next period is | ||
| On time | 11 | 19.29 % |
| Earlier than usual | 29 | 50.88 % |
| Later than usual | 17 | 29.82 % |
| After receiving COVID-19 vaccine, the flow of the period is | ||
| The same as usual | 14 | 24.56 % |
| Lighter than usual | 13 | 22.81 % |
| Heavier than usual | 30 | 52.63 % |
| Associated pain or cramps | ||
| The same as usual | 21 | 36.84 % |
| Less than usual | 9 | 15.78 % |
| More than usual | 27 | 47.36 % |
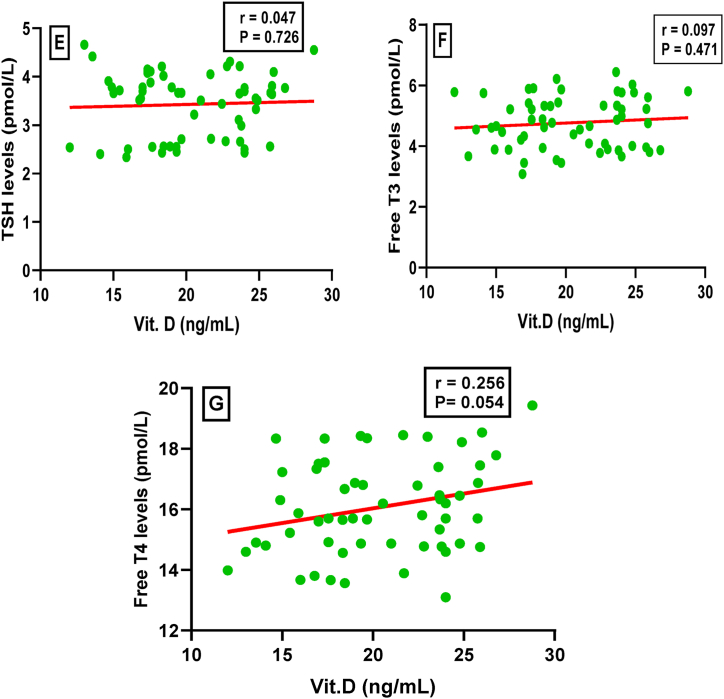
Fig. 2 (A-H) shows the associated hormonal changes during the follicular phase of the menstrual cycle in participants with irregular menstrual cycles in comparison with those with regular menstrual cycles after COVID-19 vaccination. Serum levels of follicle stimulating hormone (FSH), luteinizing hormone (LH), oestradiol, thyroid stimulating hormone (TSH), free T3, and free T4 were not significantly varied in either group. Serum levels of prolactin hormone were significantly (P < 0.001) increased, whereas serum Vit.D levels were significantly (P < 0.001) decreased in participants with irregular cycles compared to those with regular cycles.
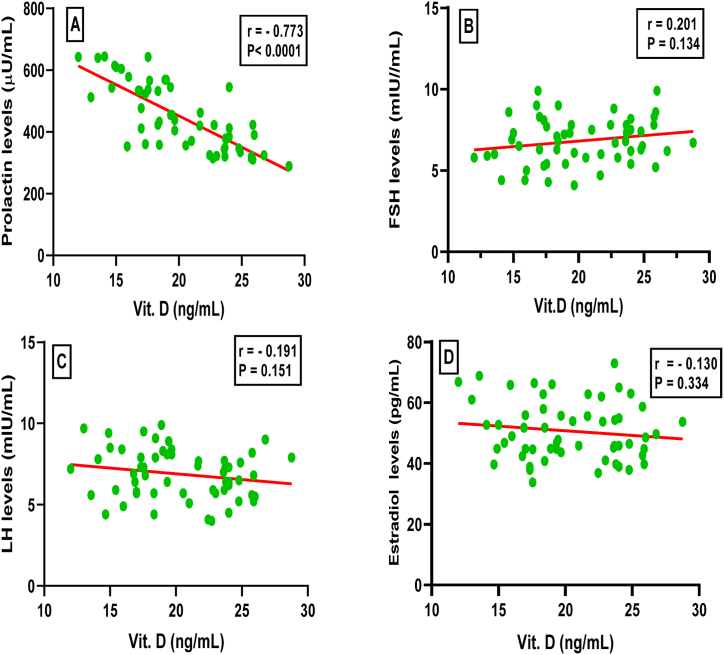
Fig. 3.
(A–G) demonstrates the correlation coefficient analysis between serum levels of Vit.D and each of prolactin, FSH, LH, oestradiol, TSH, free T3 and free T4 during the follicular phase of the menstrual cycle in participants with irregular cycles. There was a significant negative correlation between serum levels of Vit.D and prolactin hormone (r = - 0.773, P < 0.0001), whereas the correlations were not significant for other hormonal levels.
Fig. 3(A–G): Correlation coefficient analysis between serum levels of Vit.D and each of prolactin (A), FSH (B), LH (C), oestradiol (D), TSH (E), free T3 (F) and free T4 (G) during the follicular phase of the menstrual cycle in participants with irregular cycles.
Fig. 2.
(A–H): Serum levels (means ± SDs) of follicle stimulating hormone (FSH), luteinizing hormone (LH), oestradiol, prolactin, thyroid stimulating hormone (TSH), free T3, free T4 and Vit.D during the follicular phase of the menstrual cycle in participants with irregular menstrual cycles in comparison with those with regular cycles. ***: P < 0.001, NS: not significant.
5. Discussion
Like COVID-19, Zika virus (ZIKV) causes infection, which is primarily spread by the bite of infected Aedes mosquitoes. It was discovered for the first time in Uganda in 1947 and has since spread to several locations throughout the globe [23]. COVID-19 and ZIKV infection share several similarities concerning the complications of pregnant women who contracted the infection. Both viral infections have been demonstrated to raise the chance of premature birth [23,24]. Additionally, although the underlying mechanisms may vary, infection with the COVID-19 and ZIKV have both been linked to an increased risk of preeclampsia. Among pregnant women, especially those who develop COVID-19 pneumonia, there is an increased risk of preeclampsia and preterm delivery due to fever and hypoxemia [24]. ZIKV can cross the placental barrier and cause damage to the placenta, leading to inflammation and metabolic alterations. Once the virus reaches the foetal bloodstream, it primarily affects neuronal cells, potentially causing microcephaly [23]. It has been suggested that increased secretion of proinflammatory cytokines may play a role in triggering preterm delivery [25]. There is no specific medicine or vaccine for ZIKV. On the other hand, COVID-19 vaccination has been developed to save people from COVID-19.
Undergoing radiological diagnostic examinations and vaccinations has been significant for mothers during the COVID-19 pandemic. Regarding radiation and contrast media toxicity, studies suggest that the critical dose for foetal health is higher than that of a single radiological examination, and if clinically necessary, these examinations can be safely performed during pregnancy [26]. There was low acceptance of anti-SAR-CoV-2 vaccines among pregnant women, primarily due to limited knowledge about the disease and a lack of recommendations from health care providers [27].
Moreover, public concern has been raised due to the possibility that receiving a COVID-19 immunization may affect menstrual cycles [28]. An increasing quantity of research indicates that COVID-19 infection and immunization may have an impact on some women's menstrual cycles. The menstrual cycle changes may be alterations in menstrual flow, irregular periods, and spotting. This might be a result of both the body's immune reaction to the virus and the stress and inflammation brought on by the disease [29]. The menstrual cycle involves numerous signalling pathways that can be affected by both internal and external factors. Stress, whether it is caused by physical, psychological, or social factors, can disrupt these pathways and have a profound impact on a woman's well-being. Consequently, it is essential to consider the potential devastating effects of stress on the menstrual cycle [30]. The results of the current research revealed that before COVID-19 infection, 26 of the 31 infected participants had regular menstruation, and 5 irregularly menstruated. After COVID-19 infection, irregularity of the menstrual cycle was found in 23 of them. In addition, before the COVID-19 vaccine, 66 of the 79 participants were regularly menstruating, and 13 were irregularly menstruating. After the COVID-19 vaccine, irregular cycles were found in 57 of the participants. Many studies support the presence of menstrual irregularities after COVID-19 infection and vaccination. A cross-sectional survey-based study found that women between the ages of 21 and 42 may experience effects on their menstrual cycles because of COVID-19 infection [31]. The study of Qashqari et al. [32] discovered a possible link between the COVID-19 vaccine and irregular menstrual cycles, which may influence women's quality of life.
There were different changes in menstrual cycle patterns (length, period, flow, and pain) in our participants with menstrual irregularities after receiving the COVID-19 vaccine. It was found that most of the study participants received the Pfizer vaccine as the first (78.48 %), second (92.11 %), and third (93.88 %) doses. Filfilan et al. [33] reported that after receiving the COVID-19 immunization, females frequently experience irregular menstrual cycles. The inconsistent length of the cycle following two doses of the COVID-19 vaccine is the most common aberration. According to the Qashqari et al. [32] study, women who have received the COVID-19 vaccine may experience abnormal menstrual cycles, including longer menstrual periods. Furthermore, the type of COVID-19 vaccine and its effect on the menstrual cycle were not significantly correlated, either for the first or the second dose. Alvergne et al. [34] found that the menstrual cycle can be lengthened by the COVID-19 vaccine, and this effect can be mediated via ovarian hormones.
However, there are other theories that explain how COVID-19 immunization alters the menstrual cycle. According to Emma et al. [35], one potential explanation is that the uterine lining has the same chemical messengers, called cytokines, that control inflammation. If these are impacted by immunization, some women may experience alterations in their bleeding patterns. Another factor that may also have a slight impact on the timing of menstruation was that some women may have taken nonsteroidal inflammatory drugs to treat the side effects of vaccinations, such as fever or aches and pains. Therefore, the impact of COVID-19 immunization may be related to the immune system's impact on the hormones that control the menstrual cycle. When compared to individuals who had not received the COVID-19 vaccine, Edelman et al. [36] discovered that the length of the menstrual cycle (the interval between periods) temporarily lengthened by an average of less than one day in those who had. The number of days of bleeding was not altered because of the vaccine. However, researchers have discovered a variety of menstrual alterations among COVID-19-infected women, including menstrual volume changes (25 %), menstrual cycle variations (28 %) and protracted cycles (19 %) [37]. The results of the current study found that there was no significant difference in serum levels of FSH, LH, TSH, T3, and T4 between female participants with irregular menstrual cycles and those with regular cycles after COVID-19 vaccination. On the other hand, serum levels of prolactin hormone were significantly increased, whereas serum Vit.D levels were significantly decreased in this comparison. Many studies have demonstrated that there is no significant difference between COVID-19 and control patients, between mild and severe patients, or even between patients with menstrual changes and those without menstrual changes in the usual levels of sex hormones (FSH, LH, oestradiol, progesterone, testosterone, and anti-Mullerian hormone). This finding indicates that the menstrual alterations brought on by COVID-19 infection are presumed to be temporary and have no known long-term effects. The transient alterations in the menstrual cycle could mostly be attributed to stress that is mediated by an immune response. The relationship between the hypothalamic pituitary adrenal (HPA) axis and hypothalamic pituitary gonadal (HPG) axis makes this possible [37,38].
People have experienced tremendous psychological stress because of the COVID-19 pandemic, and one strategy for coping with this stress has been to get vaccinated against the SARS-CoV-2 virus [30]. The HPA axis is a term used to describe the connection between the hypothalamus, pituitary, and adrenal glands; it plays a significant role in the body's response to stress [39]. There is a substantial relationship and interaction between the HPA axis and SARS-CoV-2 infection in COVID-19, since proinflammatory cytokines and stress stimulate the HPA axis, which also regulates the response to inflammatory cytokines [40]. Al-Kuraishy et al. [41] revealed that the dysfunction of the HPA axis caused by SARS-CoV-2 infection may increase prolactin secretion from the anterior pituitary in COVID-19. It is believed that elevated levels of IL-6 in COVID-19 may act as a strong stimulus for prolactin secretion from the anterior pituitary gland, indicating that the presence of an inflammatory environment in COVID-19 may contribute to increased blood prolactin levels [42,43]. In addition, Song et al. revealed that elevated levels of prolactin hormone in individuals with COVID-19 infection are thought to be influenced by factors such as stress, oxidative stress, and immune system dysregulation [44]. There is evidence to suggest that hormonal changes during COVID-19 infection may be associated with a lack of Vit.D. It has been suggested that a deficiency in Vit.D may increase the risk and severity of COVID-19 infection, as Vit.D plays a crucial role in regulating the immune system and maintaining overall health [45]. Prolactin levels have been linked in some studies to Vit.D deficiency [46]. Vit.D deficiency may contribute to elevated prolactin levels through its effects on the hypothalamus-pituitary axis. The hypothalamus and pituitary, which are crucial regulators of prolactin release, both have Vit.D receptors (VDRs) [47,48]. A lack of Vit.D can cause these receptors to stop functioning normally, which can cause prolactin production to become dysregulated. Inflammation and impaired immunological function have also been linked to Vit.D deficiency [49]. Inflammatory processes can stimulate the secretion of prolactin from immune cells, which boosts its levels. A lack of Vit.D may cause chronic inflammation and an increase in prolactin since Vit.D is essential for controlling immunological responses. Whereas there is evidence suggesting a connection between low Vit.D levels and elevated prolactin levels, more investigation is necessary to fully understand the underlying mechanisms and establish a clear causal association.
Scientific studies have demonstrated that Vit.D can boost the antimicrobial activity of monocytes and macrophages, which are vital parts of the immune system [50]. Furthermore, Vit.D has been shown to possess anti-inflammatory properties by facilitating the development of T regulatory cells and limiting the activity of T helper-17 cells, which play a role in promoting inflammation. Additionally, Vit.D can reduce the production of proinflammatory cytokines that may contribute to inflammation in the body [51].
6. Conclusion
This study investigates for the first time the effect of COVID-19 vaccination on serum levels of FSH, LH, oestradiol, prolactin, thyroid stimulating hormone (TSH), free T3, free T4 and Vit.D during the follicular phase of the menstrual cycle. Our findings revealed a greater occurrence of irregular menstruation among participants, especially following vaccination. It is noteworthy that irregular menstrual cycles were linked to higher levels of the prolactin hormone and lower levels of Vit.D. To mitigate the side effects of vaccination and support the immune system, we suggest that females with Vit.D deficiency consider taking Vit.D supplements. Further research is needed to understand the mechanisms underlying these changes in prolactin hormone and Vit.D by assessing stress hormones such as cortisol hormone, epinephrine and norepinephrine.
Ethics declarations
-
•
This study was reviewed and approved by the Scientific Research Ethics Committee at King Faisal Medical Complex in Taif, with the approval number [2023-B-17].
-
•
All participants/patients provided informed consent to participate in the study.
Data availability statement
-
-
Data associated with our study have not been deposited into a publicly available repository.
-
-
Data will be made available on request.
CRediT authorship contribution statement
Fouzeyyah Ali Alsaeedi: Writing – review & editing, Writing – original draft, Supervision, Methodology. Amal F. Gharib: Writing – original draft. Asmaa F. Hassan: Writing – original draft, Formal analysis. Amani A. Alrehaili: Writing – review & editing. Rahma Megli Althubiti: Data curation. Fatima Mastour Alharthi: Data curation. Sarah Suleiman Alotaibi: Data curation. Ayla Mohammed Al Thomali: Data curation. Maha M. Bakhuraysah: Writing – review & editing. Ohud Alsalmi: Methodology. Alaa Ismail: Resources.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The researchers would be like to acknowledge Deanship of Scientific Research. Taif University for funding the work.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e22291.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Reed B., Carr B. 2015. The Normal Menstrual Cycle and the Control of Ovulation.https://europepmc.org/article/nbk/nbk279054 [Online]. Available. [Google Scholar]
- 2.Thiyagarajan D.K., Basit H., Jeanmonod R. StatPearls; Oct. 2022. Physiology, Menstrual Cycle.https://www.ncbi.nlm.nih.gov/books/NBK500020/ [Online]. Available. [Google Scholar]
- 3.J. L.-K. and N. physiology of reproduction and undefined . cir.nii.ac.jp; 2015. Neuroendocrine Control of the Ovarian Cycle of the Rat.https://cir.nii.ac.jp/crid/1362262943770133632 [Google Scholar]
- 4.Richards J.A.S. The ovarian cycle. Vitam. Horm. 2018;107:1–25. doi: 10.1016/BS.VH.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Saleem M., Martin H., Coates P. Prolactin biology and laboratory measurement: an update on physiology and current analytical issues. Clin. Biochem. Rev. 2018;3(1) [PMC free article] [PubMed] [Google Scholar]
- 6.Grattan D.R. 60 years of neuroendocrinology: the hypothalamo-prolactin axis. J. Endocrinol. Aug. 2015;226(2):T101–T122. doi: 10.1530/JOE-15-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Samperi I., Lithgow K., Karavitaki N. Hyperprolactinaemia. J. Clin. Med. Dec. 2019;8(12) doi: 10.3390/JCM8122203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Auriemma R.S., et al. Vol. 11. 2020. p. 1. (The Interplay between Prolactin and Reproductive System: Focus on Uterine Pathophysiology). Article. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salamonsen L.A. Vol. 158. 2019. Women In Reproductive Science: My WOMBan's Life: Understanding Human Endometrial Function, Reproduction; pp. F55–F67. 6. [DOI] [PubMed] [Google Scholar]
- 10.Joint W. 2021. WHO-Convened Global Study of Origins of SARS-CoV-2: China Part.https://apps.who.int/gb/COVID-19/pdf_files/2021/28_03/20210328-%20Full%20report.pdf [Online]. Available. [Google Scholar]
- 11.Alimohamadi Y., Sepandi M., Taghdir M., Hosamirudsari H. Determine the most common clinical symptoms in COVID-19 patients: a systematic review and meta-analysis. J Prev Med Hyg. Oct. 2020;61(3):E304–E312. doi: 10.15167/2421-4248/JPMH2020.61.3.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mendez-Brito A., El Bcheraoui C., Pozo-Martin F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J. Infect. Sep. 2021;83(3):281–293. doi: 10.1016/J.JINF.2021.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeyanathan M., Afkhami S., Smaill F., M. M.-N. R., and undefined . nature.com; 2020. Immunological Considerations for COVID-19 Vaccine Strategies. [Online]. Available https://www.nature.com/articles/s41577-020-00434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.He Q., et al. COVID-19 vaccines: current understanding on immunogenicity, safety, and further considerations. Front. Immunol. Apr. 2021;12 doi: 10.3389/FIMMU.2021.669339/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marcec R., R. L.-P. M. Journal, and undefined Using Twitter for Sentiment Analysis towards AstraZeneca/Oxford, Pfizer/BioNTech and Moderna COVID-19 Vaccines. 2022. https://academic.oup.com/pmj/article-abstract/98/1161/544/6958962 academic.oup.com, Accessed: June. 19, 2023. [Online]. Available. [DOI] [PubMed]
- 16.He Q., et al. COVID-19 vaccines: current understanding on immunogenicity, safety, and further considerations. Front. Immunol. Apr. 2021;12 doi: 10.3389/FIMMU.2021.669339/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.DeRoo S., Pudalov N., L. F.- Jama, and undefined Planning for a COVID-19 vaccination program. jamanetwork.com. 2020 doi: 10.1001/jama.2020.8711. https://jamanetwork.com/journals/jama/article-abstract/2766370 [DOI] [PubMed] [Google Scholar]
- 18.Thomas S.J., et al. Safety and efficacy of the BNT162b2 mRNA covid-19 vaccine through 6 months. N. Engl. J. Med. Nov. 2021;385(19):1761–1773. doi: 10.1056/NEJMOA2110345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Soto J., F. Dss.-J. of M. and C. Sciences, and undefined . Evaluation of the Moderna, Pfizer/biotech, Astrazeneca/Oxford and Sputnik V Vaccines for Covid-19. 2021 https://www.academia.edu/download/65566294/Joseph_Angel_de_Soto_MD_6.pdf academia.edu, Accessed: June. 19, 2023. [Online]. Available. [Google Scholar]
- 20.Wang S., et al. A prospective study of the association between SARS-CoV-2 infection and COVID-19 vaccination with changes in usual menstrual cycle characteristics. Am. J. Obstet. Gynecol. Nov. 2022;227(5):739.e1–739.e11. doi: 10.1016/J.AJOG.2022.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abdel-Moneim Y.A.S., et al. Menstrual cycle changes: a cross-sectional study of Saudi females following SARS-CoV-2 infection. PLoS One. 2022;17(12 December) doi: 10.1371/JOURNAL.PONE.0279408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menstruation: Science and Society. 2023 doi: 10.1016/j.ajog.2020.06.004. https://www.sciencedirect.com/science/article/pii/S0002937820306190 Elsevier[Online]. Available. 24, 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gullo G., et al. Congenital Zika syndrome: genetic avenues for diagnosis and therapy, possible management and long-term outcomes. J. Clin. Med. Mar. 2022;11(5) doi: 10.3390/JCM11051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maranto M., et al. Symptomatic COVID-19 in pregnancy: hospital cohort data between may 2020 and april 2021, risk factors and medicolegal implications. Diagnostics. Mar. 2023;13(6) doi: 10.3390/DIAGNOSTICS13061009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Te Lin L., et al. Correlation between maternal gingivitis/periodontitis and preterm delivery: fact or fancy? Italian Journal of Gynaecology and Obstetrics. 2018;30(4):7–12. doi: 10.14660/2385-0868-96. [DOI] [Google Scholar]
- 26.Perelli F., et al. Contrast agents during pregnancy: pros and cons when really needed. Int. J. Environ. Res. Publ. Health. Dec. 2022;19(24) doi: 10.3390/IJERPH192416699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Maranto M., Gullo G., Bruno A., Minutolo G. In: Factors Associated with Anti-SARS-CoV-2 Vaccine Acceptance Among Pregnant Women: Data from Outpatient Women Experiencing High-Risk Pregnancy. Maranto M., Gullo G., Bruno A., Minutolo G., Cucinella G., Maiorana A., Casuccio A., RestivoVaccines V., editors. mdpi.com; 2023. G. C.- Vaccines, and undefined.https://www.mdpi.com/2076-393X/11/2/454 2023•mdpi.com, Accessed: Sep. 09, 2023. [Online]. Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alvergne A., Kountourides G., Austin M., Sharp G.C., Maybin J.A. A retrospective case-control study on menstrual cycle changes following COVID-19 vaccination and disease. cell.com. 2023 doi: 10.1016/j.isci.2023.106401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yinon Y., Lebar V., Laganà A.S., Chiantera V., Kunič T., Lukanović D.L. The Effect of COVID-19 on the Menstrual Cycle: a Systematic Review. Mdpi.Com. 2022;2022:3800. doi: 10.3390/jcm11133800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Minakshi R., Rahman S., Ayaggari A., Dutta D., Shankar A. Understanding the trauma of menstrual irregularity after covid vaccination: a bird’s-eye view of female immunology. Front. Immunol. Jun. 2022;13 doi: 10.3389/FIMMU.2022.906091/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Najjar M.A.A., Al-Alwany R.R., Al-Rshoud F.M., Abu-Farha R.K., Zawiah M. Menstrual changes following COVID-19 infection: a cross-sectional study from Jordan and Iraq. PLoS One. Jun. 2022;17(6 June) doi: 10.1371/JOURNAL.PONE.0270537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Qashqari F.S.I., et al. Effect of the COVID-19 Vaccine on the Menstrual Cycle Among Females in Saudi Arabia. Ajol.Info. 2022 doi: 10.4314/ejhs.v32i6.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Filfilan N.N., et al. Effects of Different Types of COVID-19 Vaccines on Menstrual Cycles of Females of Reproductive Age Group (15-49): A Multinational Cross-Sectional Study. Cureus.Com. 2023 doi: 10.7759/cureus.39640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alvergne A., Von Woon E., Male V. Effect of COVID-19 vaccination on the timing and flow of menstrual periods in two cohorts. Frontiers in Reproductive Health. Jul. 2022;4 doi: 10.3389/FRPH.2022.952976/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pritchard E., Matthews P., Stoesser N., D. E.-N. medicine, and undefined Impact of Vaccination on New SARS-CoV-2 Infections in the United Kingdom. Nature.com. 2021 doi: 10.1038/s41591-021-01410-w. https://www.nature.com/articles/s41591-021-01410-w [Online]. Available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edelman A., et al. Association between menstrual cycle length and coronavirus disease 2019 (COVID-19) vaccination: a U.S. Cohort. Obstet. Gynecol. Apr. 2022;139(4):481. doi: 10.1097/AOG.0000000000004695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.K. Li et al., Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age, Elsevier, Accessed: June. 23, 2023. [Online]. Available: https://www.sciencedirect.com/science/article/pii/S1472648320305253. [DOI] [PMC free article] [PubMed]
- 38.Ding T., et al. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in wuhan, China: an observational study. Front. Med. Mar. 2021;8 doi: 10.3389/FMED.2021.635255/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Amabebe E., Anumba D.O.C. Psychosocial stress, cortisol levels, and maintenance of vaginal health. Front. Endocrinol. Sep. 2018;9(SEP) doi: 10.3389/FENDO.2018.00568/FULL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Saadedine M., El Sabeh M., M. B.-B. of, and undefined The Influence of COVID-19 Infection-Associated Immune Response on the Female Reproductive System. academic.oup.com.. 2023 doi: 10.1093/biolre/ioac187. https://academic.oup.com/biolreprod/article-abstract/108/2/172/6731296 [Online]. Available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Al-Kuraishy H.M., Al-Gareeb A.I., Butnariu M., Batiha G.E.S. The crucial role of prolactin-lactogenic hormone in Covid-19. Mol. Cell. Biochem. May 2022;477(5):1381–1392. doi: 10.1007/S11010-022-04381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tomaszewska-Zaremba D., K. H.-M. of, and undefined Inflammation and LPS-Binding Protein Enable the Stimulatory Effect of Endotoxin on Prolactin Secretion in the Ovine Anterior Pituitary: Ex Vivo Study. 2018. https://www.hindawi.com/journals/mi/2018/5427089/ hindawi.com, Accessed: June. 23, 2023. [Online]. Available. [DOI] [PMC free article] [PubMed]
- 43.Sanli D., Altundag A., S. K.-A. journal of, and undefined . Relationship between Disease Severity and Serum IL-6 Levels in COVID-19 Anosmia. 2021 doi: 10.1016/j.amjoto.2020.102796. https://www.sciencedirect.com/science/article/pii/S0196070920304907 Accessed: June. 23, 2023. Elsevier[Online]. Available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Song E., et al. Divergent and self-reactive immune responses in the CNS of COVID-19 patients with neurological symptoms. Cell Rep Med. May 2021;2(5) doi: 10.1016/J.XCRM.2021.100288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Radujkovic A., Hippchen T., Tiwari-Heckler S., S. D.- Nutrients, and undefined Vitamin D Deficiency and Outcome of COVID-19 Patients. 2020 doi: 10.3390/nu12092757. https://www.mdpi.com/2072-6643/12/9/2757?type=check_update&version=1&utm_source=TrendMD&utm_medium=cpc&utm_campaign=Nutrients_TrendMD_0 mdpi.com, Accessed: June. 23, 2023. [Online]. Available. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aboelnaga M.M., Abdullah N., El Shaer M. 25-hydroxyvitamin D correlation with prolactin levels and adenoma size in female patients with newly diagnosed prolactin secreting adenoma. Endocr., Metab. Immune Disord.: Drug Targets. Oct. 2017;17(3) doi: 10.2174/1871530317666170609103332. [DOI] [PubMed] [Google Scholar]
- 47.Liu H., et al. 2020. Defining Vitamin D Receptor Expression in the Brain Using a Novel VDR Cre Mouse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang Y., Zhu J., DeLuca H.F. Where is the vitamin D receptor? Arch. Biochem. Biophys. Jul. 2012;523(1):123–133. doi: 10.1016/J.ABB.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 49.Ismailova A., White J.H. Vitamin D, infections and immunity. Rev. Endocr. Metab. Disord. Apr. 2022;23(2):265–277. doi: 10.1007/S11154-021-09679-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Guevara M.A., et al. Vitamin D and streptococci: the interface of nutrition, host immune response, and antimicrobial activity in response to infection. ACS Infect. Dis. Dec. 2020;6(12):3131–3140. doi: 10.1021/ACSINFECDIS.0C00666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bishop E.L., Ismailova A., Dimeloe S., Hewison M., White J.H. Vitamin D and immune regulation: antibacterial, antiviral, anti‐inflammatory. Wiley Online Library. Jan. 2020;5(1) doi: 10.1002/jbm4.10405. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
-
-
Data associated with our study have not been deposited into a publicly available repository.
-
-
Data will be made available on request.