Abstract
Introduction
Automated cardiac arrest diagnosis offers the possibility to significantly shorten the interval between onset of out-of-hospital cardiac arrest (OHCA) and notification of EMS, providing the opportunity for earlier resuscitation and possibly increased survival.
Methods
Automated cardiac arrest diagnosis was one of six focus topics for the Wolf Creek XVII Conference held on June 14–17 2023 in Ann Arbor, Michigan, USA. Conference invitees included international thought leaders and scientists in the field of cardiac arrest resuscitation from academia and industry. Participants submitted via online survey knowledge gaps, barriers to translation and research priorities for each focus topic. Expert panels used the survey results and their own perspectives and insights to create and present a preliminary unranked list for each category that was debated, revised and ranked by all attendees to identify the top 5 for each category.
Results
Top knowledge gaps include the accuracy of automated OHCA detection technologies and the feasibility and reliability of automated EMS activation. The main barriers to translation are the risk of false positives potentially overburdening EMS, development and application costs of technology and the challenge of integrating new technology in EMS IT systems. The top research priorities are large-scale evaluation studies to measure real world performance and user research regarding the willingness to adopt these technologies.
Conclusion
Automated cardiac arrest diagnosis has the potential to significantly impact time to resuscitation and survival of OHCA because it could convert unwitnessed events into witnessed events. Validation and feasibility studies are needed. The specificity of the technology must be high not to overburden limited EMS resources. If adequate event classification is achieved, future research could shift toward event prediction, focusing on identifying potential digital biomarkers and signatures of imminent cardiac arrest. Implementation could be challenging due to high costs of development, regulatory considerations and instantiation logistics.
Keywords: Automated cardiac arrest diagnosis, Out-of-hospital cardiac arrest, Resuscitation, Health technology, Smart devices, Wearables
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of mortality in developed countries, with survival rates ranging from 4–25%.1, 2, 3 Efforts aimed to increase survival are often focused on optimization of a series of interconnected steps, termed the ‘chain of survival’.4 The first step in the chain of survival involves timely detection of the OHCA and alerting Emergency Medical Services (EMS). This step is crucial because it initiates the entire chain, yet it is also challenging because it requires a human to be present and to quickly recognize the event as a cardiac arrest. Delays commonly occur both in the recognition of cardiac arrest and in the alerting of EMS.5, 6 Moreover, 34–51% of OHCA are unwitnessed,1, 2 which translates to nearly 150,000 arrests annually in the United States alone,2 resulting in a substantial fraction of victims who have diminished chances of survival due to delayed or no resuscitation.
Automated cardiac arrest diagnosis offers the possibility to significantly shorten the interval between onset of OHCA and notification of EMS, transforming the opportunity for meaningful resuscitation and survival among a majority of OHCA victims. In this paper, we discuss the current state, potential future state, knowledge gaps, barriers to translation and research priorities regarding automated cardiac arrest diagnosis.
Methods
Since its inception in 1975, the Wolf Creek Conference has a well-established tradition of providing a unique forum for robust intellectual exchange between thought leaders and scientist from academia and industry that focuses on advancing the science and practice of cardiac arrest resuscitation.7 The Wolf Creek XVII Conference was hosted by the Max Harry Weil Institute for Critical Care Research and Innovation in Ann Arbor, Michigan, USA on June 15–17 2023.8 Automated cardiac arrest diagnosis was one of 6 focus topics for the conference. Meeting invitees included international academic and industry scientists as well as thought leaders in the field of cardiac arrest resuscitation. All participates were required to complete conflict of interest disclosures. Prior to the meeting, all participants were asked via online survey to list up to three knowledge gaps, barriers to translation and research priorities for each topic. Participants were instructed that the topic of automated cardiac arrest diagnosis would focus on wearable, audio, and video technologies (including from smartphone and other smart devices) capable of diagnosing cardiac arrest and activating the system-of-care.
Knowledge gaps were defined as areas where our understanding or knowledge is incomplete or limited. These gaps can arise due to various factors, such as lack of research, inadequate information, limited access to data or resources, or simply because the topic is new or complex. Barriers to translation were defined as obstacles that can prevent the successful transfer of knowledge or innovations from research or development settings to practical applications in the real world. Research priorities were defined as the areas of study that are considered most important or urgent by the scientific community or society as a whole. These priorities are often determined by a range of factors such as knowledge gaps, scientific breakthroughs, new challenges, societal needs or funding opportunities.
Panels made up of experts in each topic used the survey results and their own perspectives and insights to create an initial unranked list of up to ten items for each category. During the conference, expert panelists provided an overview of the current state and potential future state of the field lay the groundwork for an informed debate. This was followed by presentation and initial ranking of the knowledge gaps, barriers to translation, and research priorities by all attendees using electronic voting, discussion and revision by the panel and attendees, and then re-ranking (Supplemental figure). The top 5 items in each category underwent final review on the last day of the conference. An overview of the current and potential future state of the field and prioritized results for automated cardiac arrest diagnosis are presented and discussed in this manuscript.
Current state
More than half of the global population uses the Internet and there are more than 8 billion mobile phone subscriptions globally. More than 80% of the global population is in range of a 4G mobile network.9 The newest communication technologies are wearable electronics such as smartwatches and smart rings. Ownership of wearable devices has increased substantially over the past decade10 with more than 500 million units shipped in 2021.11 The ubiquity of mobile phones12 and wearables offers the opportunity for continuous, mostly passive monitoring, an approach already established across an array of medical domains, including cardiovascular health, metabolic diseases, mental health, movement disorders etc.13, 14
Wearable technologies could theoretically use photoplethysmography (PPG), ECG, temperature and accelerometer sensors to detect cardiac arrest events and the cessation of circulation.15 The audio sensors (i.e., speakers and microphones) of smart devices have been shown capable of detecting agonal breathing, a respiratory manifestation of cardiac arrest16 as well as dangerous breathing patterns (e.g., apnea, hypopnea) using sonar.17 Research to date shows promising results, with some technologies showing a sensitivity and specificity greater than 99%18, 19 in controlled settings. However, the studies conducted have small sample sizes and limited or no real-world data. Currently, many research groups are developing technologies to automatically diagnose cardiac arrest.20, 21, 22
Potential future state
We envision a future where there are no unwitnessed cardiac arrests. By using continuous monitoring to automatically detect every OHCA, every unwitnessed arrest can become a witnessed arrest, transforming OHCA victims’ chance of meaningful resuscitation and significantly increasing survival rates. Using the United States population from the CARES registry2 as an example; the incidence of EMS-treated non-traumatic OHCA is approximately 88.8 per 100,000 population, and 51.2% of the EMS-treated OHCA was unwitnessed. The survival rate of witnessed OHCA with resuscitation was 14.2%. The survival rate of an unwitnessed arrest treated by EMS was 4.1%. If every unwitnessed event was witnessed, potentially more than 15,000 lives could be saved in the United States annually. While this estimation might be optimistic and confined to one country, the potential benefit of immediate detection of cardiac arrest is considerable.23
Beyond the potential to make unwitnessed arrests witnessed, automated detection could in theory significantly reduce the delay in recognizing cardiac arrest and alerting the EMS when the event is witnessed. In settings where an arrest is witnessed, it can take, on average, 4 minutes to call EMS.6 If cardiac arrest can be automatically detected and an alert can be sent to EMS with minimal delay, this represents an expanded opportunity to improve survival, as more rapid contact with EMS following collapse has been shown to increase survival.24, 25
Knowledge gaps
The following top 5 knowledge gaps were identified by conference participants and discussed during the Automated Cardiac Arrest Diagnosis Panel (Fig. 1).
-
1.
Sensitivity and specificity of automatic diagnosis of cardiac arrest in wearable devices.
Fig. 1.
Automated cardiac arrest diagnosis: Top 5 knowledge gaps as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI, USA.
Sensitivity and specificity of automated cardiac arrest detection systems are critical and require a thoughtful approach contextualized to the problem these systems look to solve. Currently, unwitnessed OHCA victims experience materially worse survival, with people regularly found too late having no chance for meaningful resuscitation. Thus, any sensitivity above zero has the potential to translate into saved lives. Conversely, emergency medical services are a limited and important societal resource. Unnecessary notifications due to false positives could prevent the system from being widely deployed. Acknowledging this tradeoff is key in any automated OHCA detection design and approach. Current research in automated cardiac arrest detection mostly involves feasibility studies, whose primary focus is sensitivity, with small populations or retrospective studies using data to create a model to diagnose cardiac arrest.15 Prospective studies with larger populations and real-world data from patients in the preclinical setting are important to measure real-world performance of these systems with respect to sensitivity and specificity. There are several barriers to conducting this research, for example false positive rates, which we will discuss in the section on barriers to translation.
-
2.
Feasibility and reliability of automatic EMS system activation
If it is possible to automatically detect OHCA, it is imperative to implement these systems into existing ‘chain of survival’ and EMS infrastructures. Based on what we know about time to resuscitation and improved survival, automatic activation of EMS can potentially reduce time to resuscitation and improve survival. The feasibility and reliability of automatic EMS activation depends on the availability and compatibility of the technology with the local EMS. In order for these systems to be effective, EMS infrastructure must be able and willing to adopt this new technology. Adoption by EMS would be directly related to classification performance, which depends on the accuracy with which the technology can detect OHCA. False-positive classifications, leading to unnecessary dispatches, has the potential to strain the already limited resources available to EMS and erode trust. While false positive dispatches, including for suspected OHCA, have always been part of EMS operations, the ease and scale with which commodity devices can contact 911 make this a key consideration, which could result in longer response times to other medical emergencies. This is a particular concern with this type of system given that OHCA is a critical medical emergency and often takes priority over most other EMS calls. Comprehensive testing and validation is thus needed for stakeholders to make informed decisions on implementation of these technologies.
-
3.
Sensitivity and specificity of automatic diagnosis of cardiac arrest using surveillance devises in high-risk areas (e.g. video/sound/etc).
Approximately 70% of OHCA occurs in the home.1, 2 Leveraging detection systems people already have in their homes, such as smart phones, smart speakers or cameras could enhance rapid detection and in turn improve survival. One system researchers are developing is a smartphone or smart speaker-based system to identify a sensitive and specific sign present in cardiac arrest, agonal breathing, through passive audio classification.16 This is an example of technology that is well suited for home monitoring, as most people have smartphones and increasingly many have smart speakers at home. The technology looks promising as a widely scalable proof of principle, though further validation in real world contexts is necessary. In addition, other sensing modalities such as radar and computer vision have the potential to detect cardiac arrest. Video monitoring employing computer vision is currently used for a variety of applications, including motion detection and human behavior detection.26 It may be worth exploring whether this approach could also be used to detect signs of cardiac arrest such as syncopal collapse, profound hypoxia or even a bystander performing cardiopulmonary resuscitation (CPR). In some countries, widespread community camera monitoring is already being used to view public spaces.
-
4.
Understanding underlying mechanisms of cardiac arrest to detect prodromal signs.
Cardiac arrest is defined as a cessation of cardiac activity resulting in an absence of circulation with hemodynamic collapse. There are numerous causes that can lead to cardiac arrest,27, 28 which can broadly be classified into 4 groups: ischemic heart disease, non-ischemic/structural heart disease, no structural heart disease and non-cardiac diseases.29, 30 Approximately 50% of patients have warning symptoms before cardiac arrest, and of these patients, 70% have symptoms within 24 hours of arrest, but only 19% call EMS when they have these initial symptoms.31
Currently, the precise mechanism leading to collapse is often unknown because cardiac arrests are rarely monitored. The underlying mechanism can only be inferred based on information obtained after the process of resuscitation has been initiated. Continuous, passive monitoring, particularly using a wearable device, could in theory provide insight into these prodromal signs of arrest. Such insight would be useful from a research and prediction standpoint and could provide new approaches to intervention if an OHCA was detected to be imminent or a sudden spike in near-term risk were identified.
-
5.
Acceptability of use + impact on equity.
When implementing a new health technology it is important to understand if the technology will meet the needs, values and preferences of end-users. Cultural values, social influences and local health systems affect people’s willingness to adopt a technology.32 Involving the target population, including EMS stakeholders, throughout the implementation process improves acceptability.33 In addition, a new technology’s impact on equity must be evaluated to minimize potential disparities and unintended consequences. Health equity requires that those with equal needs have the same opportunities to access health care.34 There are many reasons that can lead to health disparities when a new technology is introduced, including income, geographic location and ethnicity.34 For a system such as this, where the condition of interest affects disproportionally traditionally underserved communities,35 extra care must be taken to ensure these systems do not exacerbate existing disparities.
Barriers to translation
The following top 5 barriers to translation were identified by conference participants and discussed during the Automated Cardiac Arrest Diagnosis Panel (Fig. 2).
-
1.
Risk of automatic cardiac arrest diagnosis increasing the burden on system of care due to large numbers of false positives.
Fig. 2.
Automated cardiac arrest diagnosis: Top 5 barriers to translation as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI, USA.
A significant barrier to real-time predictive models and continuous monitoring centers on concerns around false positives and generally misclassifications that lead to unnecessary communication with emergency medical services. False positives are a major barrier due to 2 problems. First, data is needed to train algorithms and to optimize performance, and accurate (sensor) data of cardiac arrest are scarce. Although there are machine learning techniques to optimize the use of available data, in general, performance grows as data from true events expands.36 Secondly, due to the nature of continuous monitoring with many points of measurement, even tests with very high specificity will have false positives. In addition, a technology may have a high sensitivity and specificity in preclinical studies, but this may not be the case when the technology is tested in a real-world setting at scale. It is imperative that the current EMS is not overwhelmed with false alarms, which could increase the burden on EMS systems, lead to alarm fatigue37 and foster distrust of these technologies. Research focused on determining what false positive rate is acceptable to communities and EMS systems, that acknowledges the opportunity to save more lives, could be beneficial. In addition, proof-of-concept studies are needed to demonstrate clinical and technical feasibility, including communication to EMS to help understand the incidence of false positives38 that lead to escalations to dispatchers.
-
2.
Cost as barrier to both development and widespread application of new technology for automated cardiac arrest diagnosis.
To develop a new technology is very expensive. First, funding is needed for research and development of a novel system, and securing funding for high-risk, high reward projects remains a perennial challenge.39 The availability of regional or national funding varies greatly across regions and countries. Beyond research, instantiation of research systems into usable products is a complicated and expensive process. Furthermore, if a system is eventually made widely available, continuous maintenance is necessary for its continued optimal performance and safety, particularly if these systems rely on machine intelligence.40 To reduce development costs, one possible solution is using pre-existing devices (smartwatch, smartphone, smart speaker etc.) used by the general population. Furthermore, using pre-existing devices may simplify distribution and facilitate easier integration, though this is not guaranteed.
-
3.
Integrating new technology with current EMS or health care services IT systems has historically been challenging.
Introducing new technologies into existing healthcare environments presents various challenges. First, strict regulations must be followed to ensure patient safety and data protection. Historically, a common experience within the healthcare systems is that the various clinical IT components are poorly integrated even within the same healthcare system, and communication and data transfer between systems can be notoriously challenging. This is true of EMS systems as well which do not have shared and uniform IT systems. Several large investments made into new IT systems for healthcare systems have been controversial with high development costs, substantial need for troubleshooting and concerns over patient safety. Concerns and uncertainties were raised concerning healthcare professionals, healthcare administrators and tech industry appetite for research and development into the integration of new cardiac arrest detection technologies with current EMS and healthcare IT systems. Resources are scarce and policymakers must make decisions about the use and acquisition of any technology. A comprehensive evaluation of the technology, as stated previously, helps to make an informed decision about whether or not to implement the technology.41 Finally, the introduction of new technology to EMS may be challenged by regional differences in IT infrastructure and other technologies in use. When implementing an automated OHCA technology, the EMS IT infrastructure must be compatible and able to accommodate the new technology.
-
4.
Lack of commercial interest and collaboration with industry. There needs to be a strong business case to make this work.
This touches on the second barrier; cost as barrier to development and application. Since the development cost of creating a new technology is high, it may be preferable to collaborate with industry to create a device or technology that can detect OHCA. Historically business incentives have played a key role in facilitating new research and change.40 An example of this is the introduction of the implantable defibrillator which would not have been possible without close collaboration with industry. Over the last decade we have seen an exponential growth in the health Artificial Intelligence (AI) market, from around 717 million dollars in 2016 to over 6 billion dollars in 2021 in the United States alone.42 This shows that companies are interested in investing in AI in health and that business cases surrounding health AI are feasible. However, the question whether AI-based technologies improve outcomes and add value to healthcare has yet to be proven,40 so a strong business case is needed.
-
5.
Regulatory barriers with respect to data privacy and data security.
Building and improving AI algorithms require a continuous supply of patient data. This will include sensor data, but also personal data will be collected.
Governments and regulatory entities are developing guidelines and new regulatory frameworks for technologies and medical devices that use AI to ensure the patient safety. The Federal Drug Administration (FDA), along with the International Medical Device Regulatory Forum (IMDRF), has defined the category Software as Medical Device (SaMD). In 2013, the IMDRF created a working group to provide guidance on quality management, clinical evaluation and a risk categorization framework.43, 44, 45 Several other regions have established guidelines. For instance, in 2017, the China State Council developed an AI which includes a plan promoting AI in healthcare. Moreover, in the same year, the European Parliament adopted a set of comprehensive set of regulations from the General Data Protection and Regulation (GDPR), this includes use of personal data, data collection and storage.46 These comprehensive guidelines will provide safety and security for patients, but also a high administrative burden for researchers.47
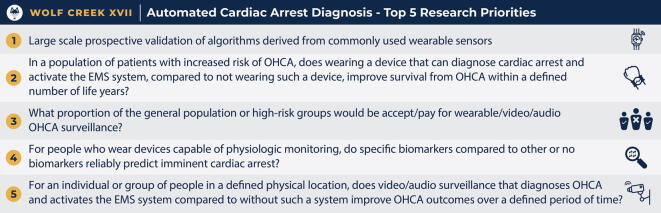
Research priorities
The following top 5 research priorities were identified by conference participants and discussed during the Automated Cardiac Arrest Diagnosis Panel (Fig. 3).
-
1.
Large scale prospective validation of algorithms derived from commonly used wearables.
Fig. 3.
Automated cardiac arrest diagnosis: Top 5 research priorities as ranked by attendees at Wolf Creek XVII, June 15-17, 2023, Ann Arbor, MI, USA.
There are currently no prospective studies to validate cardiac arrest detection algorithms in real-world settings using commodity smart devices. Real-world evaluation presents a wide range of complexities and unexpected variables that cannot be replicated in a generally controlled laboratory setting. Given the rarity of the event of interest, designing prospective randomized studies adequately powered to capture cardiac arrest events, would require following at-risk participants over years, represents a challenge from a resource perspective. In addition, product development can also be an iterative process with prospective evaluation at scale following a release (e.g., release of and iteration of fall detection and atrial fibrillation systems on commodity wearables), where potential system performance challenges can be unearthed and fixed. If done thoughtfully (i.e, system release is done only after comprehensive testing and validation), these large scale, real-world evaluations can lead to feedback that help improve performance and increase acceptability and reliability.
-
2.
In a population of patients with increased risk of OHCA, does wearing a device that can diagnose cardiac arrest and activate the EMS system, compared to not wearing such a device, improve survival from the OHCA within the defined number of life years?
The introduction of any technology that can automatically detect cardiac arrest must demonstrate that it improves the outcome of the arrest to be widely accepted and implemented. Identifying the appropriate population level of risk for cardiac arrest as well as the acceptable diagnostic sensitivity and specificity levels would inform a study designed to evaluate the effectiveness of an automated cardiac arrest detection device. While acknowledging that a significant proportion of cardiac arrest victims cannot currently be identified as “at risk” prior to their arrest, focusing studies on patients with known risk factors might be preferable for feasibility purposes, due to the rarity of an arrest event and the scale of the study needed to assess the effectiveness of the technology.
-
3.
What proportion of the general population or high-risk groups would accept/pay for wearable/video/audio surveillance?
There are large variations in the general public’s willingness to have biometric data captured, processed, stored and shared. This key consideration arises when trying to understand people’s willingness to use these systems to detect arrest events. A large part of the population is already accustomed to sharing personal and biometric data, for example heart rate to detect arrhythmia’s or sleep pattern recognition. It may stand to reason that a large percentage of this population would also be willing to use their heart rate data to detect a cardiac arrest, but this may not always be the case. For example, there could be fears about having a system that can automatically call 911. This is one example but points to the larger issue of the research community having an incomplete understanding of peoples’ desire for this functionality and how it might conform to their needs, values and preferences. In the absence of such data, the implementation of this technology could inadvertently lead to or exacerbate existing health disparities. While it seems plausible and even likely that people would desire a potentially life-saving system, empiric evaluation of these questions would be important for long term and sustained success of these systems.
-
4.
For people who wear devices capable of physiologic monitoring, do specific biomarkers compared to other or no biomarkers reliably predict imminent cardiac arrest?
Research to identify specific biomarkers to detect imminent cardiac arrest is a tantalizing and important research area. As an increasing number of people use devices capable of physiologic monitoring, the potential for leveraging continuously collected data for early detection and possibly prediction increases. Identification of biomarkers that could predict cardiac arrest with high accuracy, could potentially improve patient outcomes. This research question also relates to knowledge gap 4: understanding the underlying mechanisms of cardiac arrest to identify prodromal signs. Supporting this area of research is data indicating that approximately 50% of patients have warning symptoms before their cardiac arrest, and of these, 70% have symptoms within 24 hours of arrest, but only 19% call EMS when they experience symptoms.31 Gaining insight into the digital signatures that may accompany these prodromal symptoms is important to understand if they can serve as potential biomarkers for imminent onset of arrest. These digital signatures may also provide more information about cardiac arrest etiology, if it is possible to identify or differentiate between etiologies, such as aortic rupture or myocardial ischemia due to thromboembolism, it may offer the possibility to adjust interventions accordingly. If validated, biomarkers could in theory be used to accurately detect imminent cardiac arrest and potentially prevent cardiac arrest.
-
5.
For individual or group of people in a defined physical location, does video/audio surveillance that diagnoses OHCA and activates EMS compared to without such a system improve OHCA outcomes over a defined period of time?
People in a defined physical location represents another potential population where the efficacy and effectiveness of automated cardiac arrest detection may be evaluated. Computer vision, whereby a machine can make inferences based on dynamic images, has been shown capable of detecting falls and measuring heart rate and respiratory rate, all of which are relevant in cardiac arrest.48, 49, 50 Research is needed to confirm that automated diagnosis using passive, audio-visual inputs is feasible and to identify locations where evaluation is possible. Conducting comparative analyses over a defined period of time could provide useful insights on the potential benefits and implications of implementing these kinds of surveillance-based classification systems. Because many of these systems are already in place (e.g., CCTV), these investigations could be undertaken in theory with relatively fewer resources (vs. standing up this infrastructure from scratch).
Conclusions
This paper provides an overview of the Automated Cardiac Arrest Diagnosis expert panel session during the 2023 Wolf Creek XVII Conference, including the top 5 knowledge gaps, barriers to translation and research priorities.
Automated cardiac arrest diagnosis, using smart devices such as wearables and phones, is a new and innovative field of research. With these devices’ capability to communicate and summon emergency medical services, they hold the capability to convert unwitnessed cardiac events to effectively witnessed events, which have a higher association with survival – in some locations up to 5x. Currently, several research teams are attempting to develop technologies that can accurately detect OHCA. To date these studies have primarily been feasibility studies with smaller populations or they have relied on retrospective data given the inherent difficulty of capturing these individually rare events. There are also several barriers that need to be overcome before this technology can be responsibly introduced. One of the main barriers is false positives. The specificity of the technology must be acceptably high to avoid overburdening limited emergency medical services resources. Integrating the technology successfully with local EMS and IT infrastructures is complex as is adhering to regulations regarding privacy and data protection. Despite these challenges, the opportunity to impact OHCA survival, particularly in unwitnessed circumstances, is potentially transformative. The focus of future research should be to validate that these systems can both automatically detect cardiac arrests and have acceptable false positive performance at scale, ideally with prospective research done in real-world settings. Further research is also needed to determine the acceptability of this technology to end-users, both patients and EMS systems, and its potential to exacerbate health disparities. Once feasibility of these systems can be established, interesting follow-on research questions immediately emerge, such as can these systems be used to understand the underlying mechanisms of arrest events and are there potential digital biomarkers of imminent cardiac arrest. Given the critical role of recognition in the chain of survival, automated cardiac arrest detection represents an important and new frontier in resuscitation science with considerable potential to improve cardiac arrest outcomes.
CRediT authorship contribution statement
Wisse M.F. van den Beuken: Conceptualization, Investigation, Writing – original draft. Michael R. Sayre: Conceptualization, Writing – review & editing. Theresa M. Olasveengen: Conceptualization, Writing – review & editing. Jacob E. Sunshine: Supervision, Conceptualization, Writing – review & editing.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: [Lisa Coon coordinated the conflict of interest statements].
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100499.
Contributor Information
Wisse M.F. van den Beuken, Email: w.m.f.vandenbeuken@amsterdamumc.nl.
Jacob E. Sunshine, Email: jesun@uw.edu.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Gräsner J.T., Wnent J., Herlitz J., et al. Survival after out-of-hospital cardiac arrest in Europe - Results of the EuReCa TWO study. Resuscitation. 2020;148:218–226. doi: 10.1016/j.resuscitation.2019.12.042. [DOI] [PubMed] [Google Scholar]
- 2.The CARES Group. CARES 2022 Annual Report 2022:51. https://mycares.net/sitepages/uploads/2023/2022_flipbook/index.html?page=1.
- 3.Kiguchi T., Okubo M., Nishiyama C., et al. Out-of-hospital cardiac arrest across the World: first report from the International Liaison Committee on Resuscitation (ILCOR) Resuscitation. 2020;152:39–49. doi: 10.1016/j.resuscitation.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 4.Cummins R.O., Ornato J.P., Thies W.H., Pepe P.E. Improving survival from sudden cardiac arrest: the “chain of survival” concept. a statement for health professionals from the advanced cardiac life support subcommittee and the emergency cardiac care committee, american heart association. Circulation. 1991;83:1832–1847. doi: 10.1161/01.cir.83.5.1832. [DOI] [PubMed] [Google Scholar]
- 5.Dami F., Heymann E., Pasquier M., Fuchs V., Carron P.N., Hugli O. Time to identify cardiac arrest and provide dispatch-assisted cardio-pulmonary resuscitation in a criteria-based dispatch system. Resuscitation. 2015;97:27–33. doi: 10.1016/j.resuscitation.2015.09.390. [DOI] [PubMed] [Google Scholar]
- 6.Herlitz J., Engdahl J., Svensson L., Young M., Angquist K.A., Holmberg S. A short delay from out of hospital cardiac arrest to call for ambulance increases survival. Eur Heart J. 2003;24:1750–1755. doi: 10.1016/s0195-668x(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 7.Neumar R.W., Tang W. Wolf Creek XVII Part 2: The Origin, Evolution, and Impact of the Wolf Creek Conference. Resuscitation Plus. 2023 doi: 10.1016/j.resplu.2023.100505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Neumar R.W. Wolf Creek XVII Part 1: The Future of Cardiac Arrest Resuscitation. Resuscitation Plus. 2023 doi: 10.1016/j.resplu.2023.100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Max Roser, Hannah Ritchie, Edouard Mathieu. Technological Change. Our World in Data. 2023.
- 10.Henriksen A., Haugen Mikalsen M., Woldaregay A.Z., et al. Using fitness trackers and smartwatches to measure physical activity in research: analysis of consumer wrist-worn wearables. J Med Internet Res. 2018;20:e110. doi: 10.2196/jmir.9157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laricchia F. Total wearable device unit shipments worldwide 2014–2022. Statistica. 2023 [Google Scholar]
- 12.Pew research center. mobile fact sheet pew research center webpage 2021 [Access date: Juli 11, 2023] Available from: https://www.pewresearch.org/internet/fact-sheet/mobile/#:∼:text=Mobile%20phone%20ownership%20over%20time,smartphone%20ownership%20conducted%20in%202011.
- 13.Dunn J., Runge R., Snyder M. Wearables and the medical revolution. Per Med. 2018;15:429–448. doi: 10.2217/pme-2018-0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu L., Zhang J., Xie Y., et al. Wearable health devices in health care: narrative systematic review. JMIR mHealth and uHealth. 2020;8 doi: 10.2196/18907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutton J., Lingawi S., Puyat J.H., et al. Sensor technologies to detect out-of-hospital cardiac arrest: a systematic review of diagnostic test performance. Resusc Plus. 2022;11 doi: 10.1016/j.resplu.2022.100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan J., Rea T., Gollakota S., Sunshine J.E. Contactless cardiac arrest detection using smart devices. NPJ Digit Med. 2019;2:52. doi: 10.1038/s41746-019-0128-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nandakumar R., Gollakota S., Sunshine J.E. Opioid overdose detection using smartphones. Sci Transl Med. 2019;11 doi: 10.1126/scitranslmed.aau8914. [DOI] [PubMed] [Google Scholar]
- 18.Sugano H., Hara S., Tsujioka T., et al. Development of a triage engine enabling behavior recognition and lethal arrhythmia detection for remote health care system. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:2160–2163. doi: 10.1109/iembs.2011.6090405. [DOI] [PubMed] [Google Scholar]
- 19.Gaibazzi N., Siniscalchi C., Reverberi C. The Heart Sentinel™ app for detection and automatic alerting in cardiac arrest during outdoor sports: Field tests and ventricular fibrillation simulation results. Int J Cardiol. 2018;269:133–138. doi: 10.1016/j.ijcard.2018.07.062. [DOI] [PubMed] [Google Scholar]
- 20.Hartstichting. Automatische signalering en alarmering bij een hartstilstand Hartstichting 2021 [Access date: July 11, 2023] Available from: https://professionals.hartstichting.nl/actualiteiten/automatische-signalering-en-alarmering-bij-een-hartstilstand.
- 21.Sinden S. How wearable devices to detect cardiac arrest could save thousands of lives each year CHÉOS (Centre for Health Evaluation & Outcome Sciences) 2023 [updated May 16, 2023. Access date: July 11, 2023] Available from: https://www.cheos.ubc.ca/research-in-action/how-wearable-devices-to-detect-could-save-thousands-of-lives-each-year/.
- 22.Schober P., van den Beuken W.M.F., Nideröst B., et al. Smartwatch based automatic detection of out-of-hospital cardiac arrest: study rationale and protocol of the HEART-SAFE project. Resusc Plus. 2022;12 doi: 10.1016/j.resplu.2022.100324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Deakin C.D. The chain of survival: not all links are equal. Resuscitation. 2018;126:80–82. doi: 10.1016/j.resuscitation.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 24.Bürger A., Wnent J., Bohn A., et al. The effect of ambulance response time on survival following out-of-hospital cardiac arrest. Dtsch Arztebl Int. 2018;115:541–548. doi: 10.3238/arztebl.2018.0541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Larsen M.P., Eisenberg M.S., Cummins R.O., Hallstrom A.P. Predicting survival from out-of-hospital cardiac arrest: a graphic model. Ann Emerg Med. 1993;22:1652–1658. doi: 10.1016/s0196-0644(05)81302-2. [DOI] [PubMed] [Google Scholar]
- 26.Elharrouss O., Almaadeed N., Al-Maadeed S. A review of video surveillance systems. J Vis Commun Image Representation. 2021;77 [Google Scholar]
- 27.Myat A., Song K.J., Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391:970–979. doi: 10.1016/s0140-6736(18)30472-0. [DOI] [PubMed] [Google Scholar]
- 28.Chen N., Callaway C.W., Guyette F.X., et al. Arrest etiology among patients resuscitated from cardiac arrest. Resuscitation. 2018;130:33–40. doi: 10.1016/j.resuscitation.2018.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Philip J, Podrid M, FACC. Overview of sudden cardiac arrest and sudden cardiac death. UpToDate. 2023.
- 30.Marijon E., Uy-Evanado A., Dumas F., et al. Warning symptoms are associated with survival from sudden cardiac arrest. Ann Intern Med. 2016;164:23–29. doi: 10.7326/m14-2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang Meier D., Barthelmess P., Sun W., Liberatore F. Wearable technology acceptance in health care based on national culture differences: cross-country analysis between Chinese and Swiss consumers. J Med Internet Res. 2020;22:e18801. doi: 10.2196/18801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jacobs J.V., Hettinger L.J., Huang Y.-H., et al. Employee acceptance of wearable technology in the workplace. Appl Ergon. 2019;78:148–156. doi: 10.1016/j.apergo.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 33.Oliver A., Mossialos E. Equity of access to health care: outlining the foundations for action. J Epidemiol Community Health. 2004;58:655–658. doi: 10.1136/jech.2003.017731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reinier K., Stecker E.C., Vickers C., Gunson K., Jui J., Chugh S.S. Incidence of sudden cardiac arrest is higher in areas of low socioeconomic status: a prospective two year study in a large United States community. Resuscitation. 2006;70:186–192. doi: 10.1016/j.resuscitation.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 35.Adadi A. A survey on data-efficient algorithms in big data era. J Big Data. 2021;8:24. [Google Scholar]
- 36.Kristinsson Æ., Gu Y., Rasmussen S.M., et al. Prediction of serious outcomes based on continuous vital sign monitoring of high-risk patients. Comput Biol Med. 2022;147 doi: 10.1016/j.compbiomed.2022.105559. [DOI] [PubMed] [Google Scholar]
- 37.Wellens H.J., Lindemans F.W., Houben R.P., et al. Improving survival after out-of-hospital cardiac arrest requires new tools. Eur Heart J. 2016;37:1499–1503. doi: 10.1093/eurheartj/ehv485. [DOI] [PubMed] [Google Scholar]
- 38.Stafinski T., McCabe C.J., Menon D. Funding the unfundable: mechanisms for managing uncertainty in decisions on the introduction of new and innovative technologies into healthcare systems. Pharmacoeconomics. 2010;28:113–142. doi: 10.2165/11530820-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 39.He J., Baxter S.L., Xu J., Xu J., Zhou X., Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30–36. doi: 10.1038/s41591-018-0307-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mytton O.T., Velazquez A., Banken R., et al. Introducing new technology safely. Qual Saf Health Care. 2010;19:i9–i14. doi: 10.1136/qshc.2009.038554. [DOI] [PubMed] [Google Scholar]
- 41.Saxena R. Artificial Intelligence in Healthcare market analysis, 2016 – 2030. Grant View Research. 2021.
- 42.Software as a Medical Device Working Group. Software as a Medical Device (SAMD): Clinical Evaluation. IMDRF International Medical Device Regulators Forum. 2017:30.
- 43.Software as a Medical Device Working Group. “Software as a Medical Device”: Possible Framework for Risk Categorization and Corresponding Considerations. IMDRF International Medical Device Regulators Forum. 2014:30.
- 44.Software as a Medical Device Working Group. Software as a Medical Device (SaMD): Application of Quality.
- 45.Management System. IMDRF International Medical Device Regulators Forum. 2015:34.
- 46.Goodman B., Flaxman S. European Union regulations on algorithmic decision-making and a “right to explanation”. AI Mag. 2017;38:50–57. [Google Scholar]
- 47.Wierda E., Eindhoven D.C., Schalij M.J., et al. Privacy of patient data in quality-of-care registries in cardiology and cardiothoracic surgery: the impact of the new general data protection regulation EU-law. Eur Heart J Qual Care Clin Outcomes. 2018;4:239–245. doi: 10.1093/ehjqcco/qcy034. [DOI] [PubMed] [Google Scholar]
- 48.Anderson D., Keller J.M., Skubic M., Chen X., He Z. Recognizing falls from silhouettes. Conf Proc IEEE Eng Med Biol Soc. 2006;2006:6388–6391. doi: 10.1109/iembs.2006.259594. [DOI] [PubMed] [Google Scholar]
- 49.Chatterjee A., Prathosh A.P., Praveena P. Real-time respiration rate measurement from thoracoabdominal movement with a consumer grade camera. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:2708–2711. doi: 10.1109/embc.2016.7591289. [DOI] [PubMed] [Google Scholar]
- 50.Yan B.P., Lai W.H.S., Chan C.K.Y., et al. High-Throughput, contact-free detection of atrial fibrillation from video with deep learning. JAMA Cardiol. 2020;5:105–107. doi: 10.1001/jamacardio.2019.4004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.