Abstract
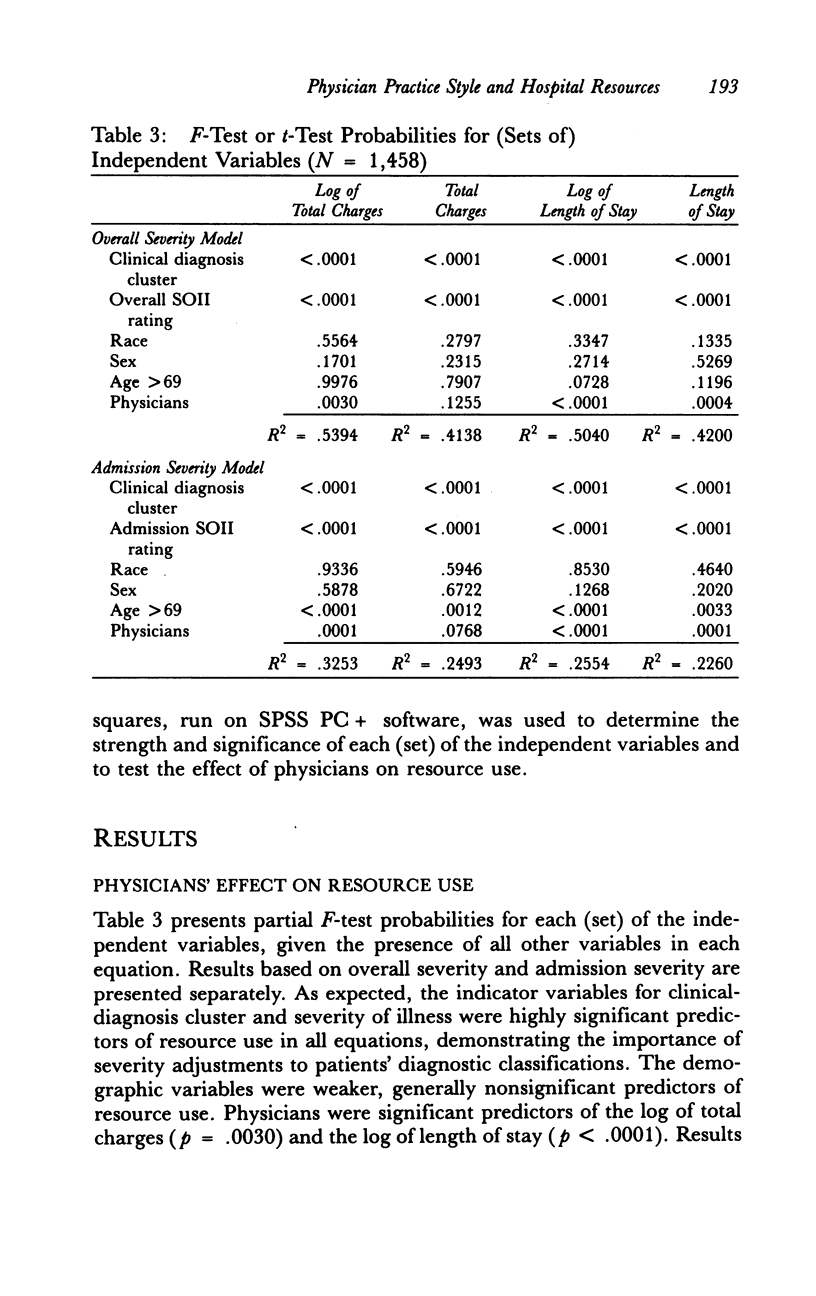
Several specifications of a statistical model were used to measure the effect that internal medicine attending physicians had on inpatient charges and length of stay at a large urban teaching hospital. The study was based on a sample of 1,458 patients discharged during 1985-1987 with 12 common principal diagnosis clusters. The relationship between 31 physicians' clinical decisions and hospital charges and length of stay was analyzed controlling for patients' health status, as measured by demographic characteristics, diagnostic group, and ratings for the Severity of Illness Index (SOII). Results indicated that attending physicians were statistically significant predictors of the log of total charges (p = .0030) and the log of length of stay (p less than .0001), and not as significant predictors of untransformed total charges (p = .1255). Equivalent results were obtained when overall SOII ratings were replaced by SOII subscale ratings for the presenting stage of the principal diagnosis on admission. Examination of individual physician regression coefficients revealed that physicians varied within a 40 percent range of generated per patient charges. No significant differences in mortality, early readmissions or residual impairment on discharge were found between the ten highest and ten lowest resource use physicians. The conservatively estimated range of attending physician practice variations observed in this study has serious financial implications for hospitals operating under incentives to minimize operating costs, particularly for teaching hospitals facing reductions in subsidies for graduate medical education.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bernard A. M., Shapiro L. R., McMahon L. F., Jr The influence of attending physician subspecialization on hospital length of stay. Med Care. 1990 Feb;28(2):170–174. doi: 10.1097/00005650-199002000-00007. [DOI] [PubMed] [Google Scholar]
- Cameron J. M. The indirect costs of graduate medical education. N Engl J Med. 1985 May 9;312(19):1233–1238. doi: 10.1056/NEJM198505093121906. [DOI] [PubMed] [Google Scholar]
- Cherkin D. C., Rosenblatt R. A., Hart L. G., Schneeweiss R., LoGerfo J. The use of medical resources by residency-trained family physicians and general internists. Is there a difference? Med Care. 1987 Jun;25(6):455–469. doi: 10.1097/00005650-198706000-00001. [DOI] [PubMed] [Google Scholar]
- Franks P., Dickinson J. C. Comparisons of family physicians and internists. Process and outcome in adult patients at a community hospital. Med Care. 1986 Oct;24(10):941–948. doi: 10.1097/00005650-198610000-00007. [DOI] [PubMed] [Google Scholar]
- Frick A. P., Martin S. G., Shwartz M. Case-mix and cost differences between teaching and nonteaching hospitals. Med Care. 1985 Apr;23(4):283–295. doi: 10.1097/00005650-198504000-00001. [DOI] [PubMed] [Google Scholar]
- Garber A. M., Fuchs V. R., Silverman J. F. Case mix, costs, and outcomes. Differences between faculty and community services in a university hospital. N Engl J Med. 1984 May 10;310(19):1231–1237. doi: 10.1056/NEJM198405103101906. [DOI] [PubMed] [Google Scholar]
- Garg M. L., Mulligan J. L., Gliebe W. A., Parekh R. R. Physician specialty, quality and cost of inpatient care. Soc Sci Med. 1979 Oct;13C(3):187–190. doi: 10.1016/0160-7995(79)90043-1. [DOI] [PubMed] [Google Scholar]
- Glandon G. L., Morrisey M. A. Redefining the hospital-physician relationship under prospective payment. Inquiry. 1986 Summer;23(2):166–175. [PubMed] [Google Scholar]
- Horn S. D., Horn R. A., Moses H. Profiles of physician practice and patient severity of illness. Am J Public Health. 1986 May;76(5):532–535. doi: 10.2105/ajph.76.5.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn S. D., Horn R. A. Reliability and validity of the Severity of Illness Index. Med Care. 1986 Feb;24(2):159–178. doi: 10.1097/00005650-198602000-00007. [DOI] [PubMed] [Google Scholar]
- Horn S. D., Horn R. A., Sharkey P. D., Chambers A. F. Severity of illness within DRGs. Homogeneity study. Med Care. 1986 Mar;24(3):225–235. doi: 10.1097/00005650-198603000-00005. [DOI] [PubMed] [Google Scholar]
- Horn S. D., Horn R. A., Sharkey P. D. The Severity of Illness Index as a severity adjustment to diagnosis-related groups. Health Care Financ Rev. 1984;Suppl:33–45. [PMC free article] [PubMed] [Google Scholar]
- Hsiao W. C., Sapolsky H. M., Dunn D. L., Weiner S. L. Lessons of the New Jersey DRG payment system. Health Aff (Millwood) 1986 Summer;5(2):32–45. doi: 10.1377/hlthaff.5.2.32. [DOI] [PubMed] [Google Scholar]
- Jones K. R. The influence of the attending physician on indirect graduate medical education costs. J Med Educ. 1984 Oct;59(10):789–798. doi: 10.1097/00001888-198410000-00003. [DOI] [PubMed] [Google Scholar]
- Kralewski J. E., Dowd B., Feldman R., Shapiro J. The changing climate of medical practice. The physician rebellion. N Engl J Med. 1987 Feb 5;316(6):339–342. doi: 10.1056/NEJM198702053160612. [DOI] [PubMed] [Google Scholar]
- Linn L. S., Yager J., Leake B. D., Gastaldo G., Palkowski C. Differences in the numbers and costs of tests ordered by internists, family physicians, and psychiatrists. Inquiry. 1984 Fall;21(3):266–275. [PubMed] [Google Scholar]
- McMahon L. F., Jr, Newbold R. Variation in resource use within diagnosis-related groups. The effect of severity of illness and physician practice. Med Care. 1986 May;24(5):388–397. doi: 10.1097/00005650-198605000-00002. [DOI] [PubMed] [Google Scholar]
- Pauker S. G., Kassirer J. P. The threshold approach to clinical decision making. N Engl J Med. 1980 May 15;302(20):1109–1117. doi: 10.1056/NEJM198005153022003. [DOI] [PubMed] [Google Scholar]
- Paul-Shaheen P., Clark J. D., Williams D. Small area analysis: a review and analysis of the North American literature. J Health Polit Policy Law. 1987 Winter;12(4):741–809. doi: 10.1215/03616878-12-4-741. [DOI] [PubMed] [Google Scholar]
- Payne S. M. Identifying and managing inappropriate hospital utilization: a policy synthesis. Health Serv Res. 1987 Dec;22(5):709–769. [PMC free article] [PubMed] [Google Scholar]
- Roos N. P., Flowerdew G., Wajda A., Tate R. B. Variations in physicians' hospitalization practices: a population-based study in Manitoba, Canada. Am J Public Health. 1986 Jan;76(1):45–51. doi: 10.2105/ajph.76.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider E. L., Brody J. A. Aging, natural death, and the compression of morbidity: another view. N Engl J Med. 1983 Oct 6;309(14):854–856. doi: 10.1056/NEJM198310063091411. [DOI] [PubMed] [Google Scholar]
- Schumacher D. N., Parker B., Kofie V., Munns J. M. Severity of Illness Index and the Adverse Patient Occurrence Index. A reliability study and policy implications. Med Care. 1987 Aug;25(8):695–704. doi: 10.1097/00005650-198708000-00003. [DOI] [PubMed] [Google Scholar]
- Stano M. A further analysis of the "variations in practice style" phenomenon. Inquiry. 1986 Summer;23(2):176–182. [PubMed] [Google Scholar]
- Stano M., Folland S. Variations in the use of physician services by Medicare beneficiaries. Health Care Financ Rev. 1988 Spring;9(3):51–58. [PMC free article] [PubMed] [Google Scholar]
- Strauss M. J., Conrad D., LoGerfo J. P., Hudson L. D., Bergner M. Cost and outcome of care for patients with chronic obstructive lung disease. Analysis by physician specialty. Med Care. 1986 Oct;24(10):915–924. doi: 10.1097/00005650-198610000-00005. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E. Dealing with medical practice variations: a proposal for action. Health Aff (Millwood) 1984 Summer;3(2):6–32. doi: 10.1377/hlthaff.3.2.6. [DOI] [PubMed] [Google Scholar]
- White R. E., Skipper B. J., Applegate W. B., Bennett M. D., Chilton L. A. Ordering decision and clinic cost variation among resident physicians. West J Med. 1984 Jul;141(1):117–122. [PMC free article] [PubMed] [Google Scholar]


