Abstract
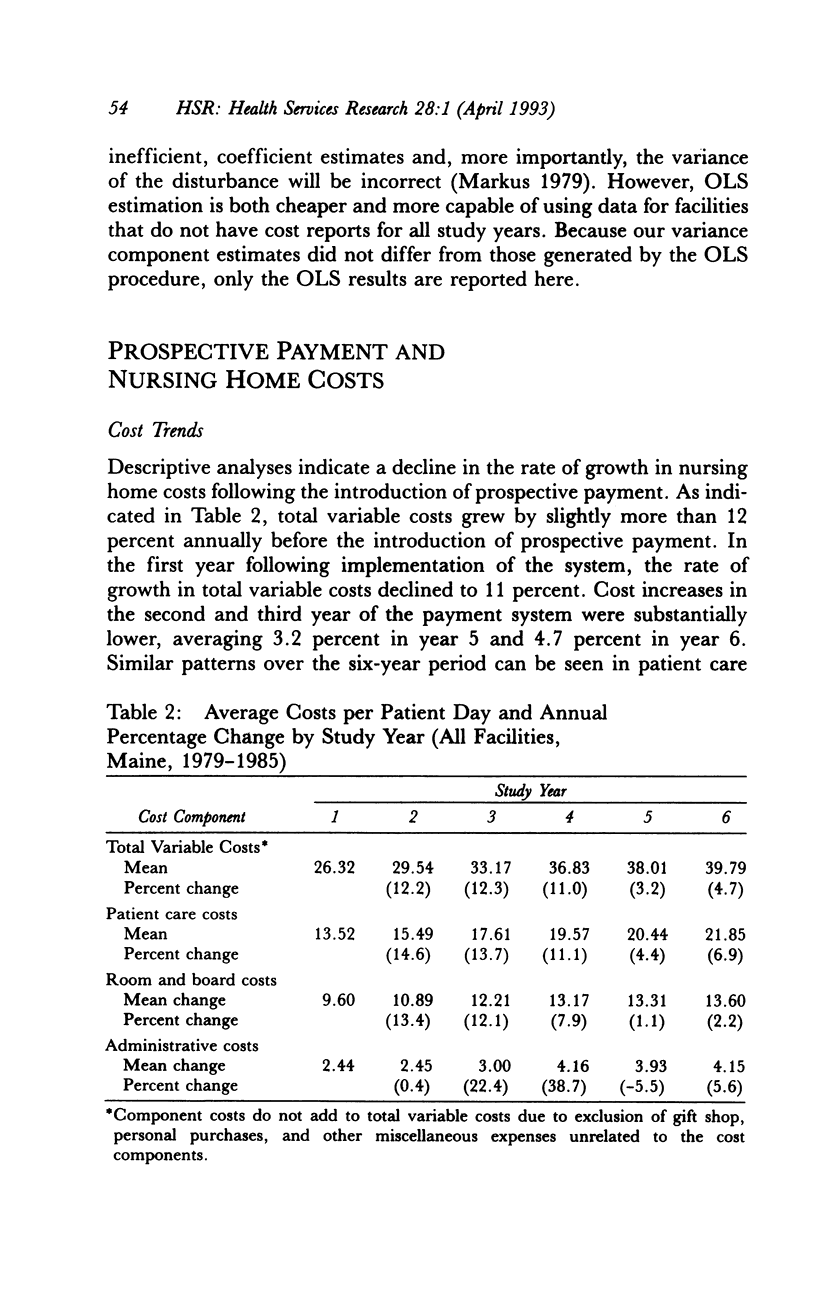
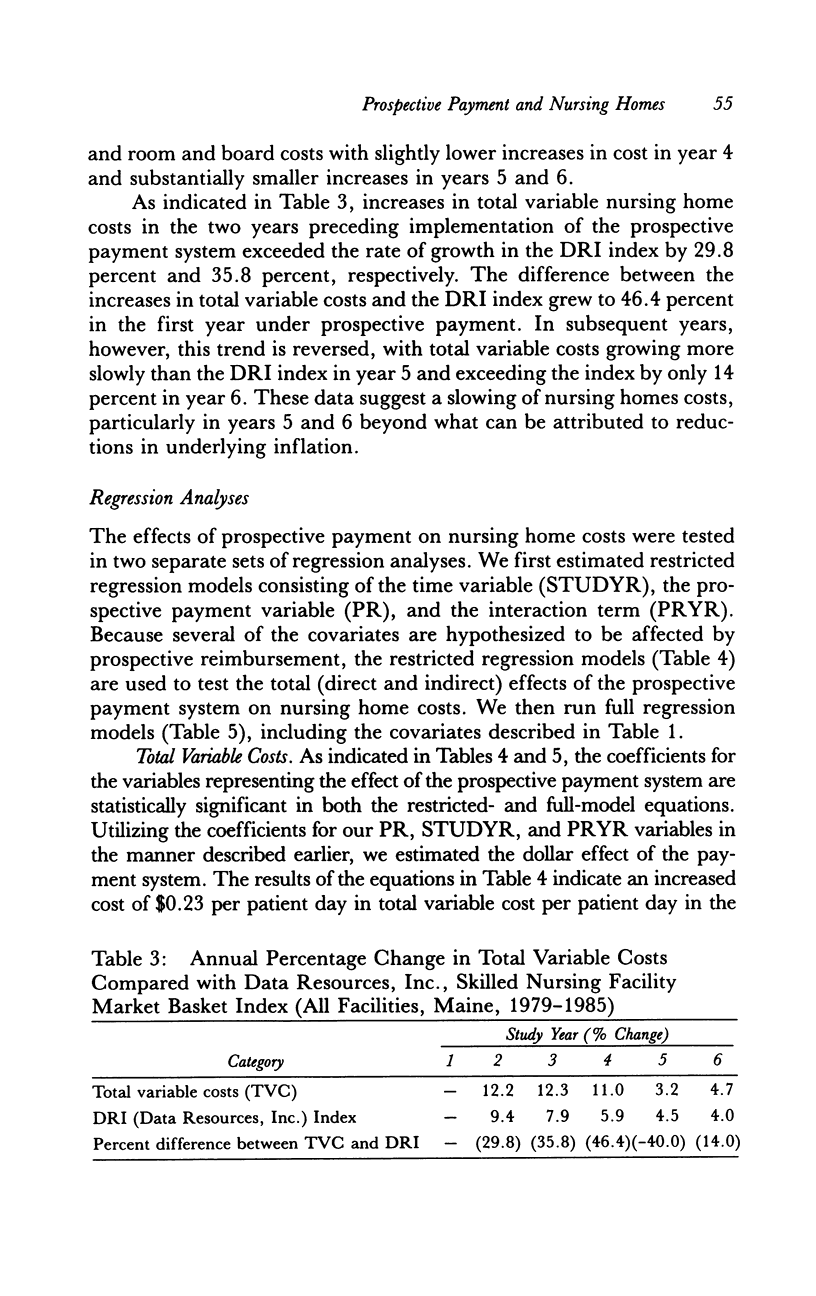
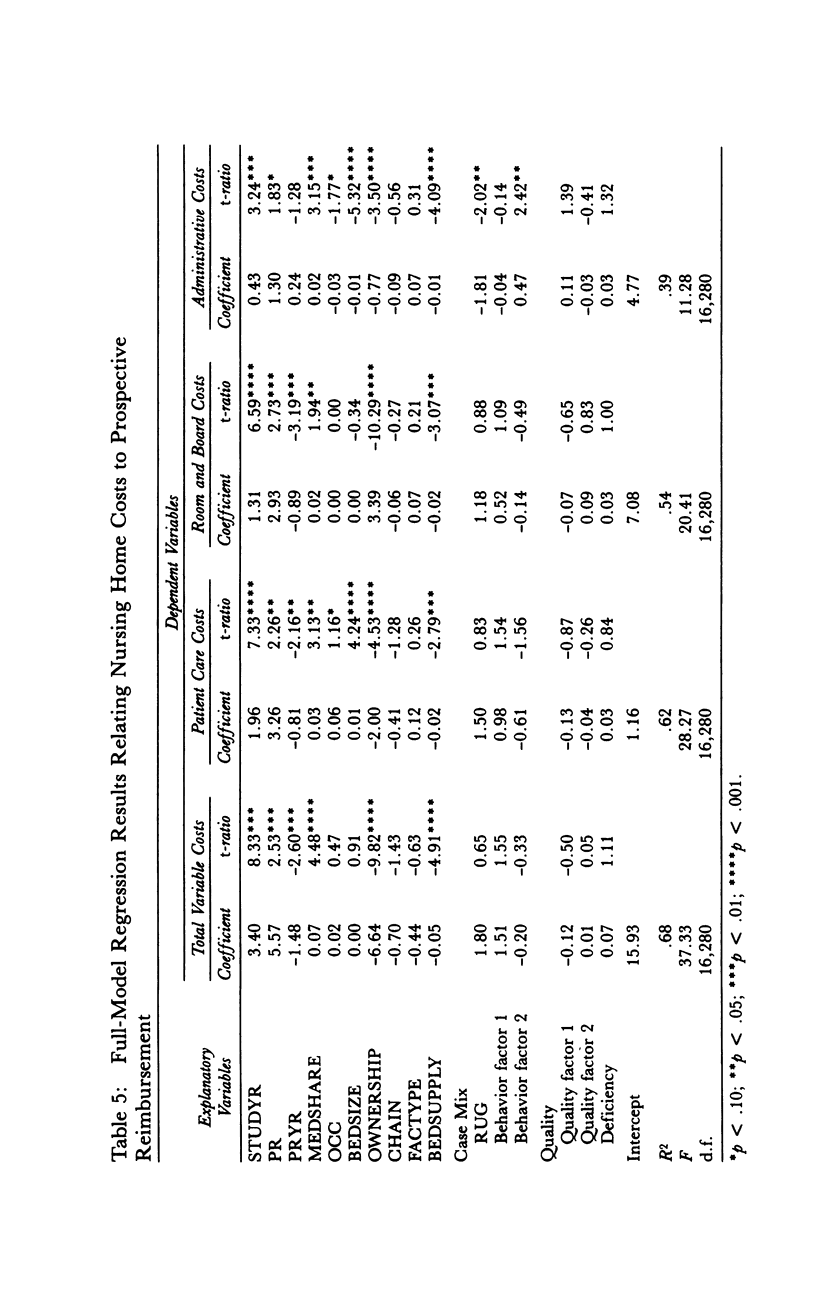
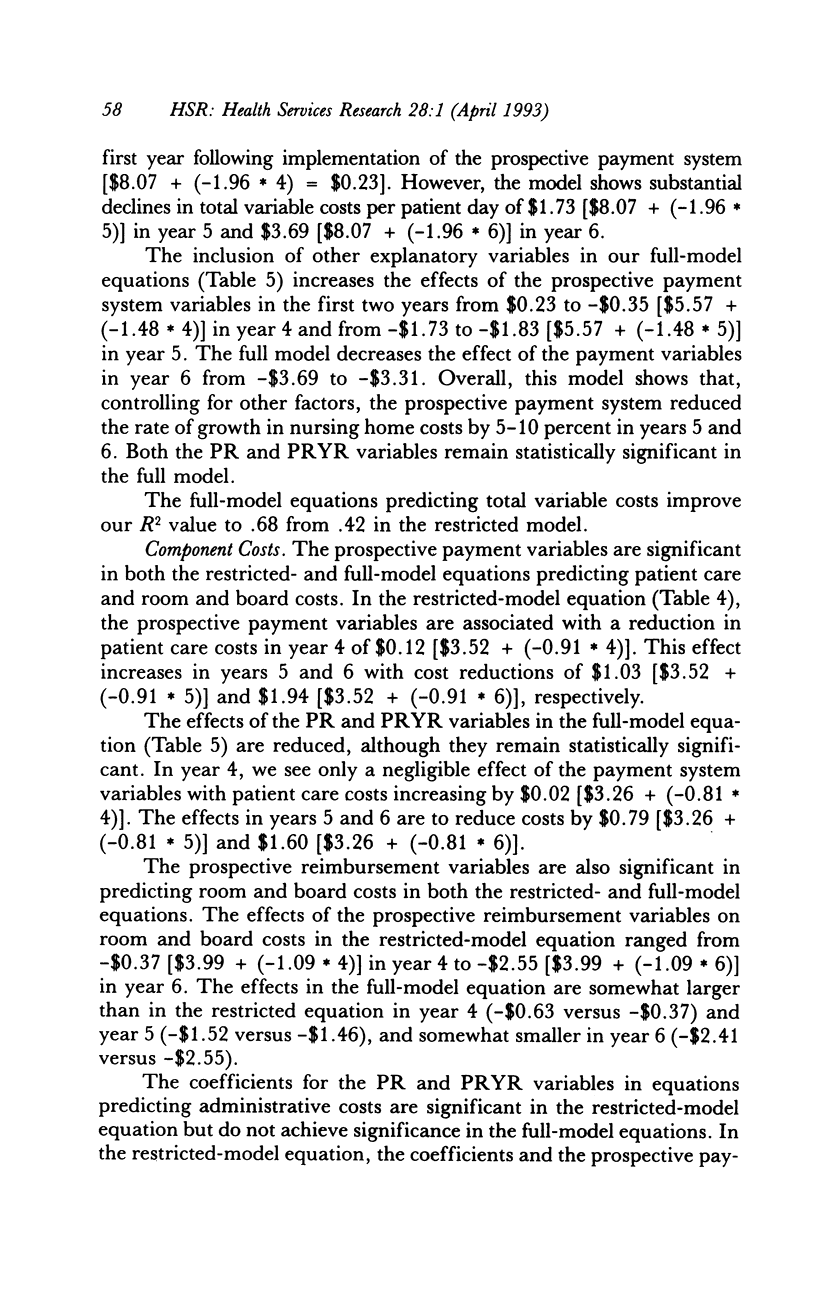
OBJECTIVE. This study evaluates the effect of Maine's Medicaid nursing home prospective payment system on nursing home costs and access to care for public patients. DATA SOURCES/STUDY SETTING. The implementation of a facility-specific prospective payment system for nursing homes provided the opportunity for longitudinal study of the effect of that system. Data sources included audited Medicaid nursing home cost reports, quality-of-care data from state facility survey and licensure files, and facility case-mix information from random, stratified samples of homes and residents. Data were obtained for six years (1979-1985) covering the three-year period before and after implementation of the prospective payment system. STUDY DESIGN. This study used a pre-post, longitudinal analytical design in which interrupted, time-series regression models were estimated to test the effects of prospective payment and other factors, e.g., facility characteristics, nursing home market factors, facility case mix, and quality of care, on nursing home costs. PRINCIPAL FINDINGS. Prospective payment contributed to an estimated $3.03 decrease in total variable costs in the third year from what would have been expected under the previous retrospective cost-based payment system. Responsiveness to payment system efficiency incentives declined over the study period, however, indicating a growing problem in achieving further cost reductions. Some evidence suggested that cost reductions might have reduced access for public patients. CONCLUSIONS. Study findings are consistent with the results of other studies that have demonstrated the effectiveness of prospective payment systems in restraining nursing home costs. Potential policy trade-offs among cost containment, access, and quality assurance deserve further consideration, particularly by researchers and policymakers designing the new generation of case mix-based and other nursing home payment systems.
Full text
PDF










Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Coelen C., Sullivan D. An analysis of the effects of prospective reimbursement programs on hospital expenditures. Health Care Financ Rev. 1981 Winter;2(3):1–40. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. W., Dubay L. C. The effects of Medicaid reimbursement method and ownership on nursing home costs, case mix, and staffing. Inquiry. 1990 Summer;27(2):183–200. [PubMed] [Google Scholar]
- Holahan J., Cohen J. Nursing home reimbursement: implications for cost containment, access, and quality. Milbank Q. 1987;65(1):112–147. [PubMed] [Google Scholar]
- Meiners M. R. An econometric analysis of the major determinants of nursing home costs in the United States. Soc Sci Med. 1982;16(8):887–898. doi: 10.1016/0277-9536(82)90208-8. [DOI] [PubMed] [Google Scholar]
- Schlenker R. E. Nursing home costs, Medicaid rates, and profits under alternative Medicaid payment systems. Health Serv Res. 1991 Dec;26(5):623–649. [PMC free article] [PubMed] [Google Scholar]
- Schlenker R. E., Shaughessy P. W. Case mix, quality, and cost relationships in Colorado nursing homes. Health Care Financ Rev. 1984 Winter;6(2):61–71. [PMC free article] [PubMed] [Google Scholar]


