Abstract
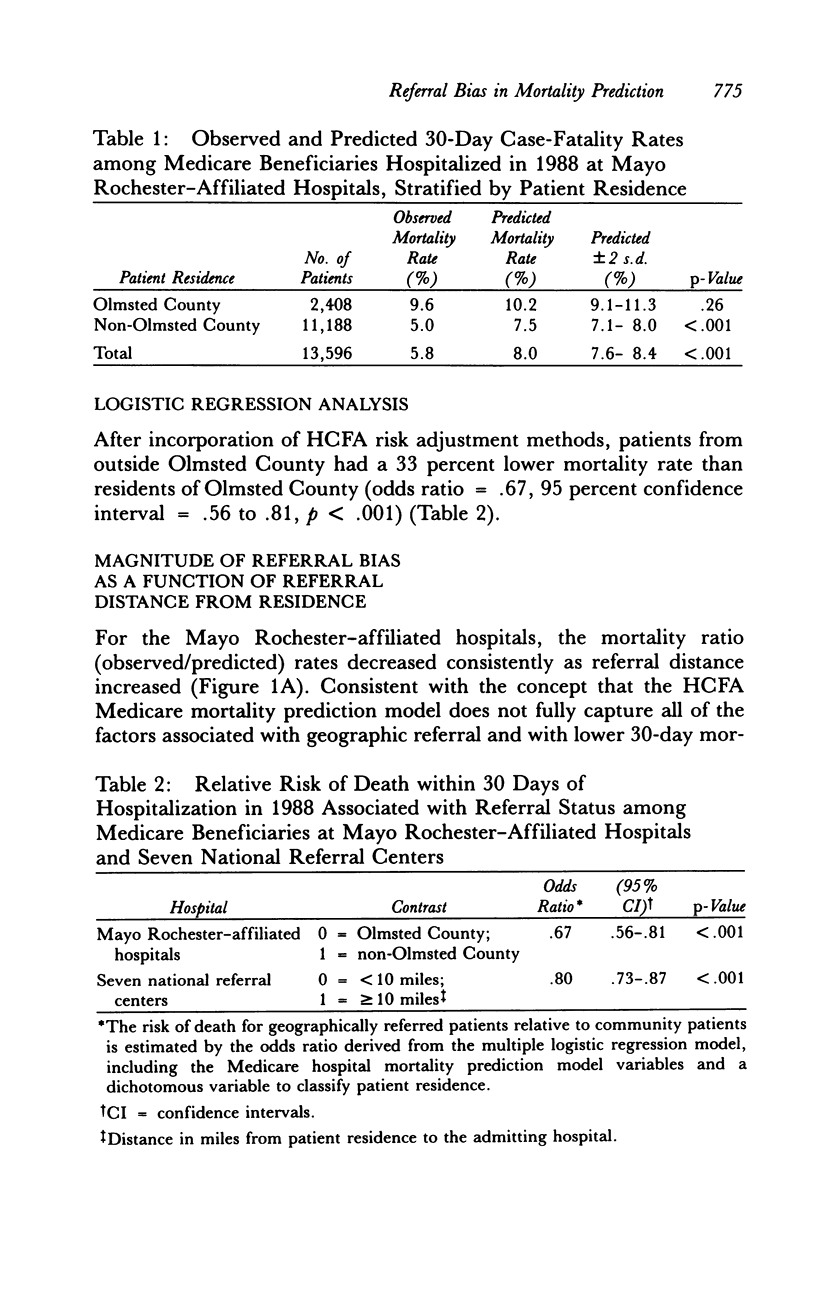
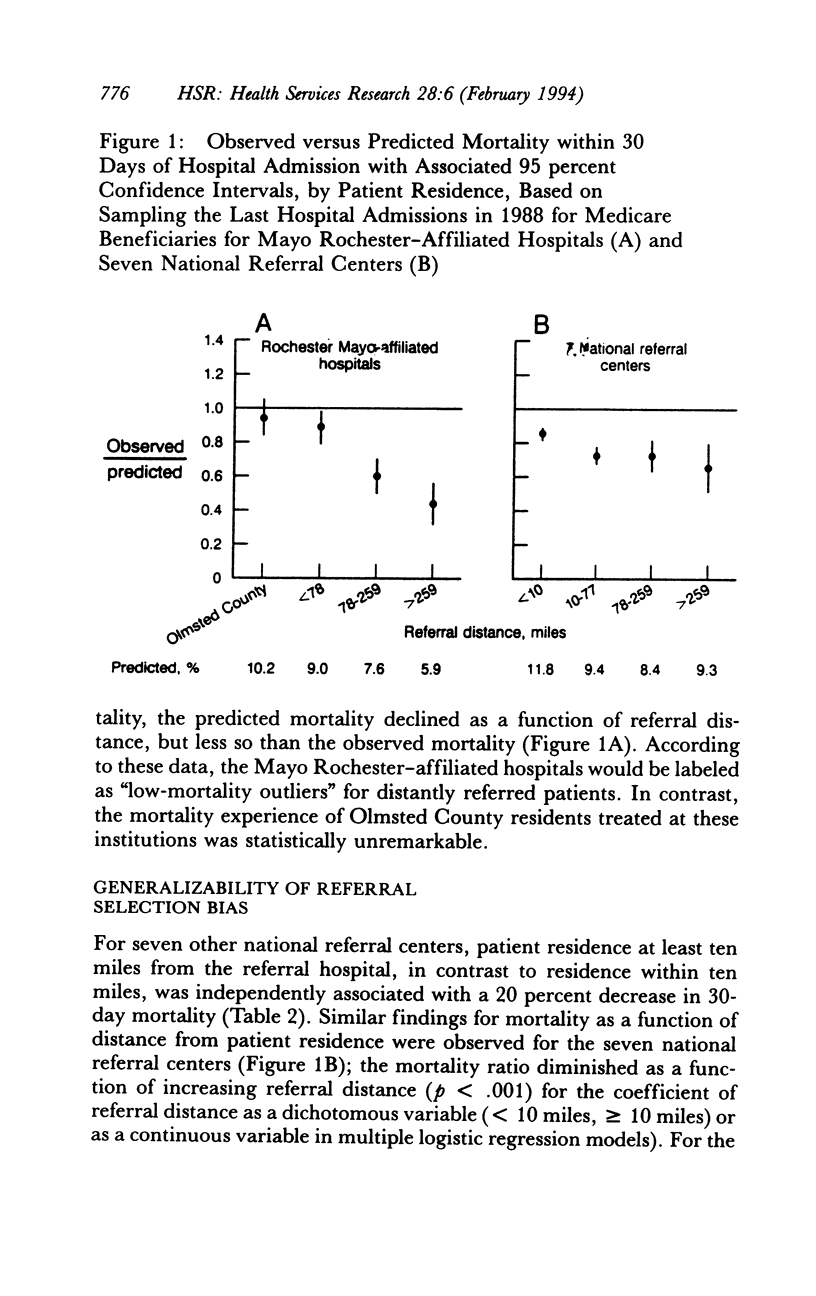
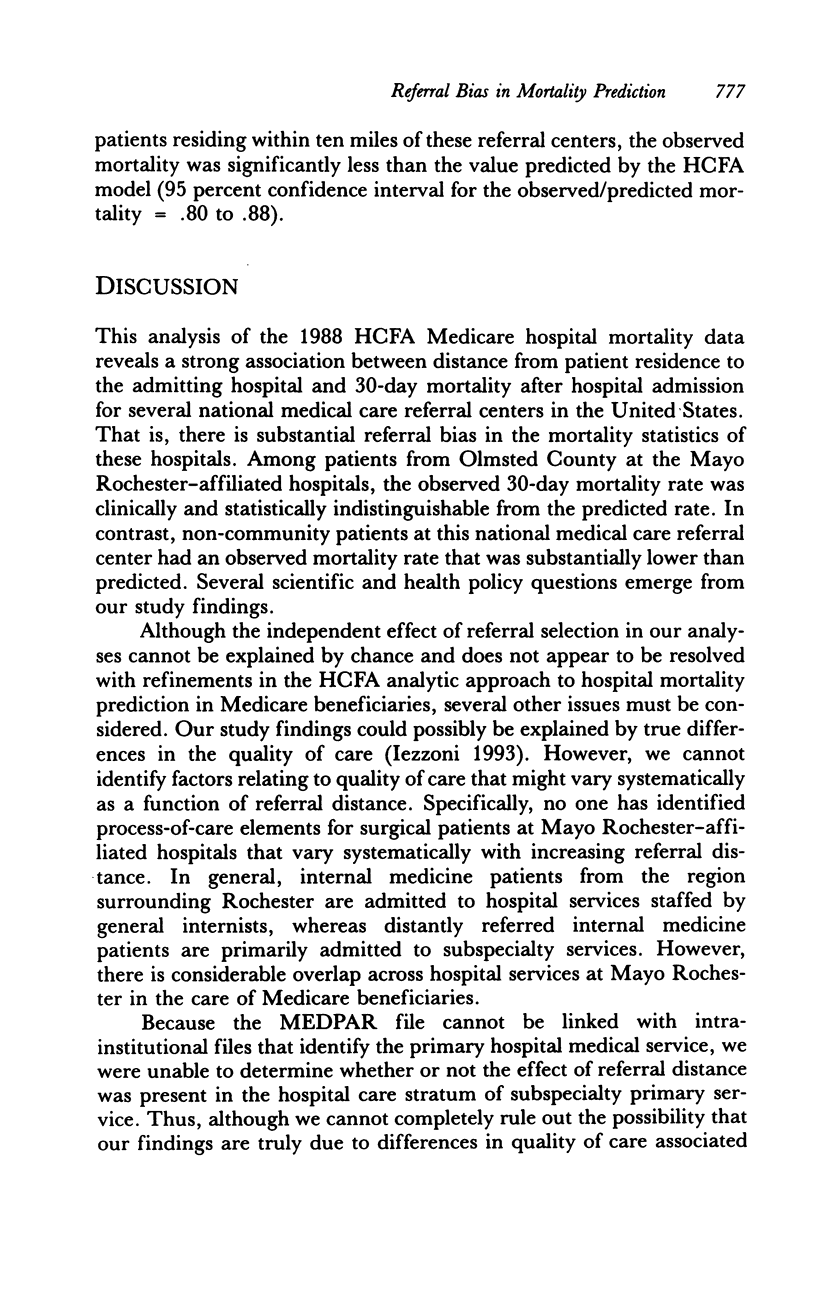
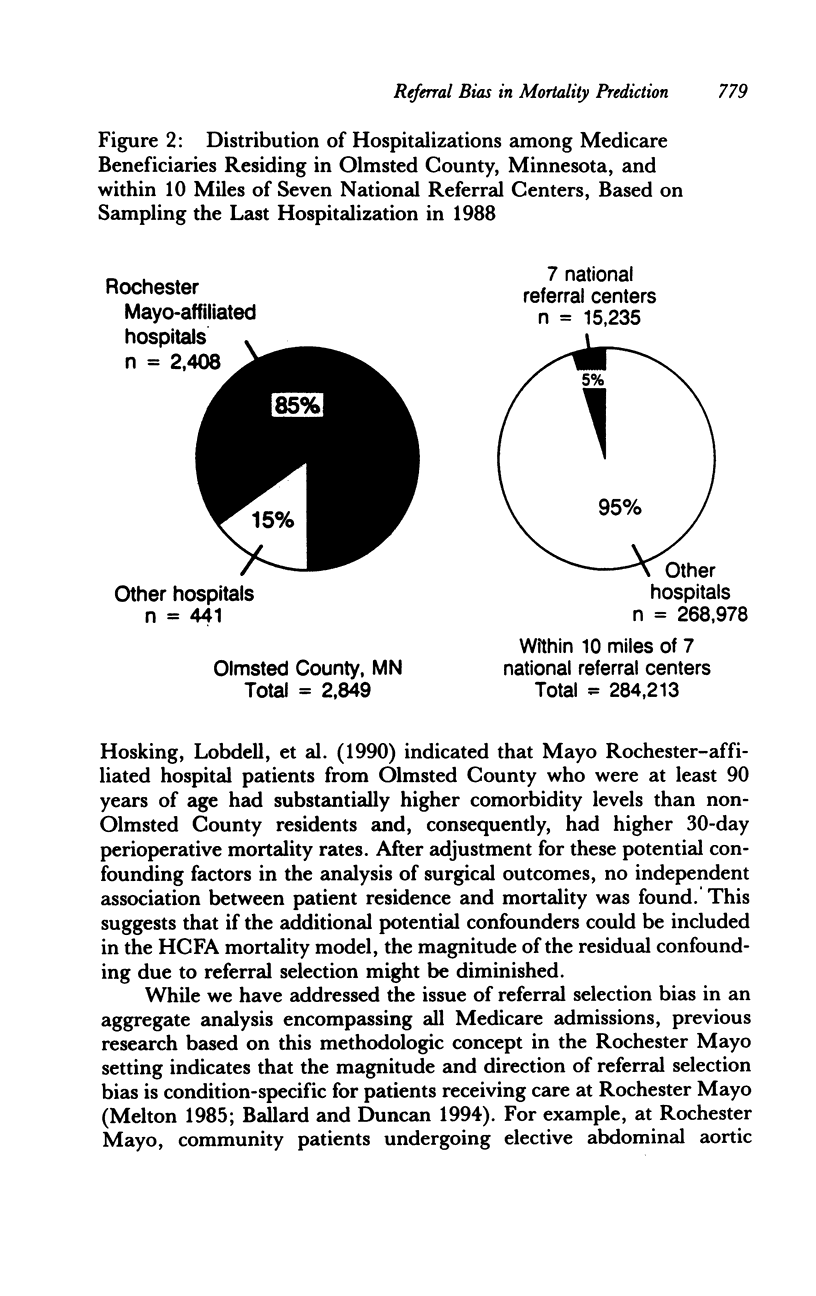
OBJECTIVE. Although the Health Care Financing Administration (HCFA) uses Medicare hospital mortality data as a measure of hospital quality of care, concerns have been raised regarding the validity of this concept. A problem that has not been fully evaluated in these data is the potential confounding effect of illness severity factors associated with referral selection and hospital mortality on comparisons of risk-adjusted hospital mortality. We address this issue. DATA SOURCES AND STUDY SETTING. We analyzed the 1988 Medicare hospitalization data file (MEDPAR). We selected data on patients treated at the two Mayo Clinic-associated hospitals in Rochester, Minnesota, and a group of seven other hospitals that treat many patients from large geographic areas. These hospitals have had observed mortality rates substantially lower than those predicted by the HCFA model for the period 1987-1990. STUDY DESIGN. Using the multiple logistic regression model applied by HCFA to the 1988 data, we evaluated the relationship between distance from patient residence to the admitting hospital and risk-adjusted hospital mortality. PRINCIPAL FINDINGS. Among patients admitted to Mayo Rochester-affiliated hospitals, residence outside Olmsted County, Minnesota was independently associated with a 33 percent lower 30-day mortality rate (p < .001) than that associated with residence in Olmsted County. When patients at Mayo hospitals were stratified by residence (Olmsted County versus non-Olmsted County), the observed mortality was similar to that predicted for community patients (9.6 percent versus 10.2 percent, p = .26), whereas hospital mortality for referral patients was substantially lower than predicted (5.0 percent versus 7.5 percent, p = < .001). After incorporation of the HCFA risk adjustment methods, distance from patient residence to the hospitals was also independently associated with mortality among the Mayo Rochester-affiliated hospitals and seven other referral center hospitals. CONCLUSIONS. The HCFA Medicare hospital mortality model should be used with extreme caution to evaluate hospital quality of care for national referral centers because of residual confounding due to severity of illness factors associated with geographic referral that are inadequately captured in the extant prediction model.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berwick D. M., Wald D. L. Hospital leaders' opinions of the HCFA mortality data. JAMA. 1990 Jan 12;263(2):247–249. [PubMed] [Google Scholar]
- Blumberg M. S. Comments on HCFA hospital death rate statistical outliers. Health Care Financing Administration. Health Serv Res. 1987 Feb;21(6):715–739. [PMC free article] [PubMed] [Google Scholar]
- Dubois R. W., Rogers W. H., Moxley J. H., 3rd, Draper D., Brook R. H. Hospital inpatient mortality. Is it a predictor of quality? N Engl J Med. 1987 Dec 24;317(26):1674–1680. doi: 10.1056/NEJM198712243172626. [DOI] [PubMed] [Google Scholar]
- Fink A., Yano E. M., Brook R. H. The condition of the literature on differences in hospital mortality. Med Care. 1989 Apr;27(4):315–336. doi: 10.1097/00005650-198904000-00001. [DOI] [PubMed] [Google Scholar]
- Fuster V., Gersh B. J., Giuliani E. R., Tajik A. J., Brandenburg R. O., Frye R. L. The natural history of idiopathic dilated cardiomyopathy. Am J Cardiol. 1981 Mar;47(3):525–531. doi: 10.1016/0002-9149(81)90534-8. [DOI] [PubMed] [Google Scholar]
- Green J., Passman L. J., Wintfeld N. Analyzing hospital mortality. The consequences of diversity in patient mix. JAMA. 1991 Apr 10;265(14):1849–1853. doi: 10.1001/jama.265.14.1849. [DOI] [PubMed] [Google Scholar]
- Green J., Wintfeld N., Sharkey P., Passman L. J. The importance of severity of illness in assessing hospital mortality. JAMA. 1990 Jan 12;263(2):241–246. [PubMed] [Google Scholar]
- Hollier L. H., Reigel M. M., Kazmier F. J., Pairolero P. C., Cherry K. J., Hallett J. W., Jr Conventional repair of abdominal aortic aneurysm in the high-risk patient: a plea for abandonment of nonresective treatment. J Vasc Surg. 1986 May;3(5):712–717. [PubMed] [Google Scholar]
- Iezzoni L. I., Ash A. S., Coffman G. A., Moskowitz M. A. Predicting in-hospital mortality. A comparison of severity measurement approaches. Med Care. 1992 Apr;30(4):347–359. doi: 10.1097/00005650-199204000-00005. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I. Monitoring quality of care: what do we need to know? Inquiry. 1993 Summer;30(2):112–114. [PubMed] [Google Scholar]
- Jencks S. F., Wilensky G. R. The health care quality improvement initiative. A new approach to quality assurance in Medicare. JAMA. 1992 Aug 19;268(7):900–903. [PubMed] [Google Scholar]
- Krakauer H., Bailey R. C., Skellan K. J., Stewart J. D., Hartz A. J., Kuhn E. M., Rimm A. A. Evaluation of the HCFA model for the analysis of mortality following hospitalization. Health Serv Res. 1992 Aug;27(3):317–335. [PMC free article] [PubMed] [Google Scholar]
- Melton L. J., 3rd Selection bias in the referral of patients and the natural history of surgical conditions. Mayo Clin Proc. 1985 Dec;60(12):880–885. doi: 10.1016/s0025-6196(12)64794-6. [DOI] [PubMed] [Google Scholar]
- Nash D. B. Is the quality cart before the horse? JAMA. 1992 Aug 19;268(7):917–918. [PubMed] [Google Scholar]
- Park R. E., Brook R. H., Kosecoff J., Keesey J., Rubenstein L., Keeler E., Kahn K. L., Rogers W. H., Chassin M. R. Explaining variations in hospital death rates. Randomness, severity of illness, quality of care. JAMA. 1990 Jul 25;264(4):484–490. [PubMed] [Google Scholar]
- Roger V. L., Ballard D. J., Hallett J. W., Jr, Osmundson P. J., Puetz P. A., Gersh B. J. Influence of coronary artery disease on morbidity and mortality after abdominal aortic aneurysmectomy: a population-based study, 1971-1987. J Am Coll Cardiol. 1989 Nov 1;14(5):1245–1252. doi: 10.1016/0735-1097(89)90423-3. [DOI] [PubMed] [Google Scholar]
- Shapiro M. F., Park R. E., Keesey J., Brook R. H. Mortality differences between New York City municipal and voluntary hospitals, for selected conditions. Am J Public Health. 1993 Jul;83(7):1024–1026. doi: 10.2105/ajph.83.7.1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith D. W., Pine M., Bailey R. C., Jones B., Brewster A., Krakauer H. Using clinical variables to estimate the risk of patient mortality. Med Care. 1991 Nov;29(11):1108–1129. doi: 10.1097/00005650-199111000-00004. [DOI] [PubMed] [Google Scholar]
- Thomas J. W., Holloway J. J., Guire K. E. Validating risk-adjusted mortality as an indicator for quality of care. Inquiry. 1993 Spring;30(1):6–22. [PubMed] [Google Scholar]
- Warner M. A., Hosking M. P., Lobdell C. M., Offord K. P., Melton L. J., 3rd Effects of referral bias on surgical outcomes: a population-based study of surgical patients 90 years of age or older. Mayo Clin Proc. 1990 Sep;65(9):1185–1191. doi: 10.1016/s0025-6196(12)62742-6. [DOI] [PubMed] [Google Scholar]
- Wennberg J. E., Freeman J. L., Shelton R. M., Bubolz T. A. Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989 Oct 26;321(17):1168–1173. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]


