Abstract
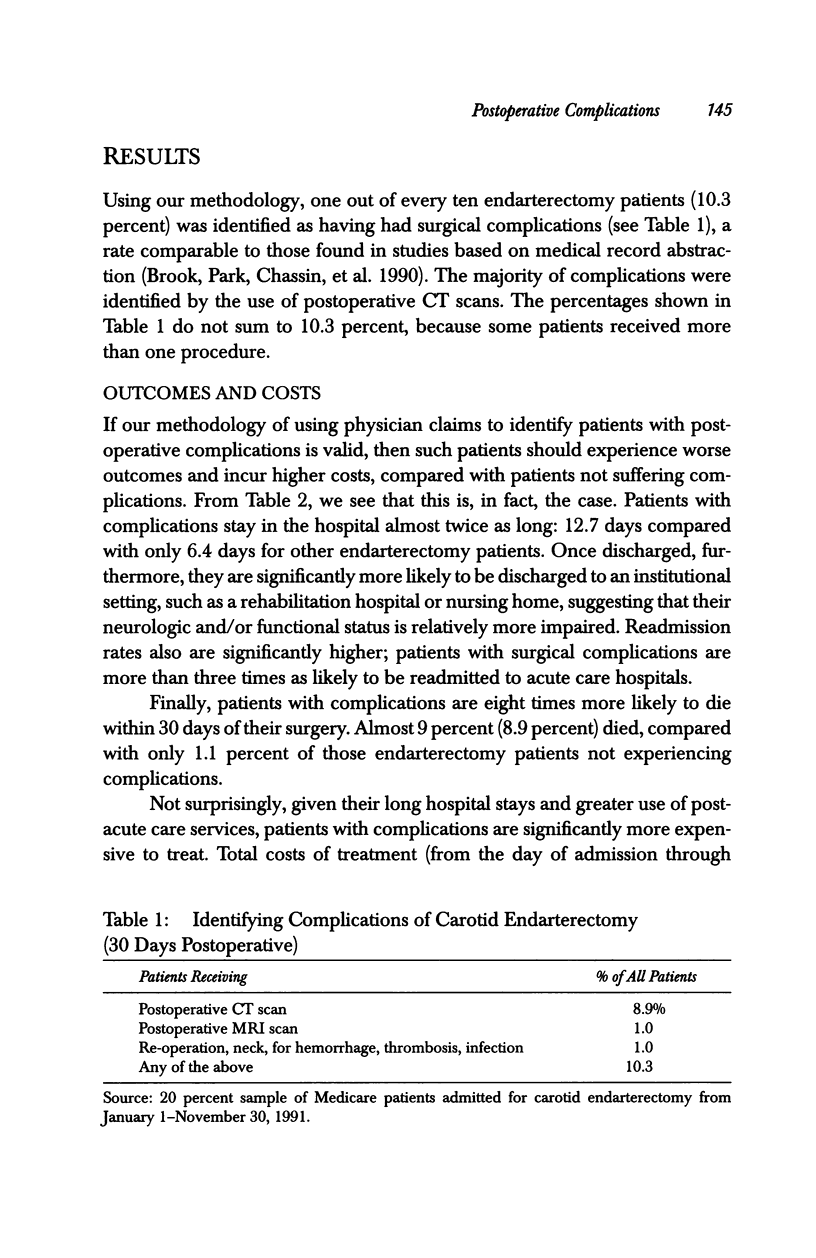
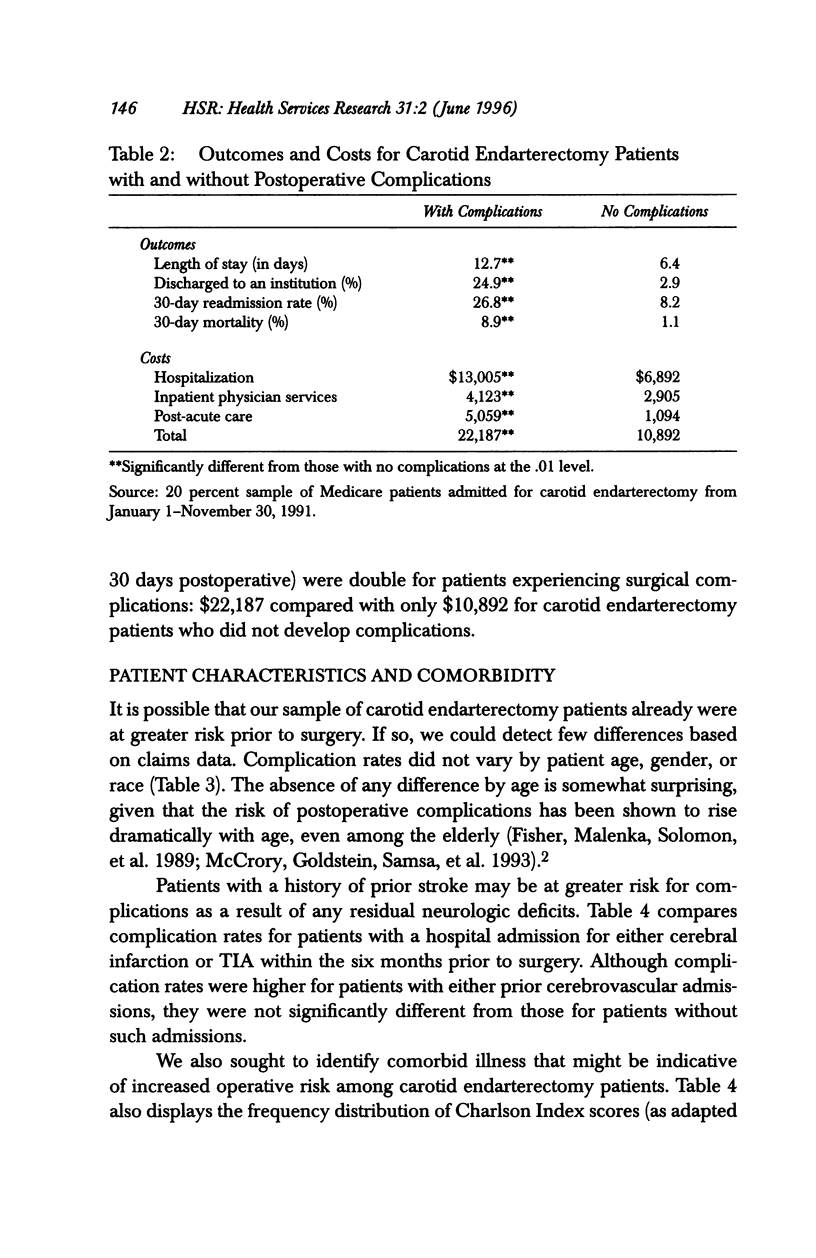
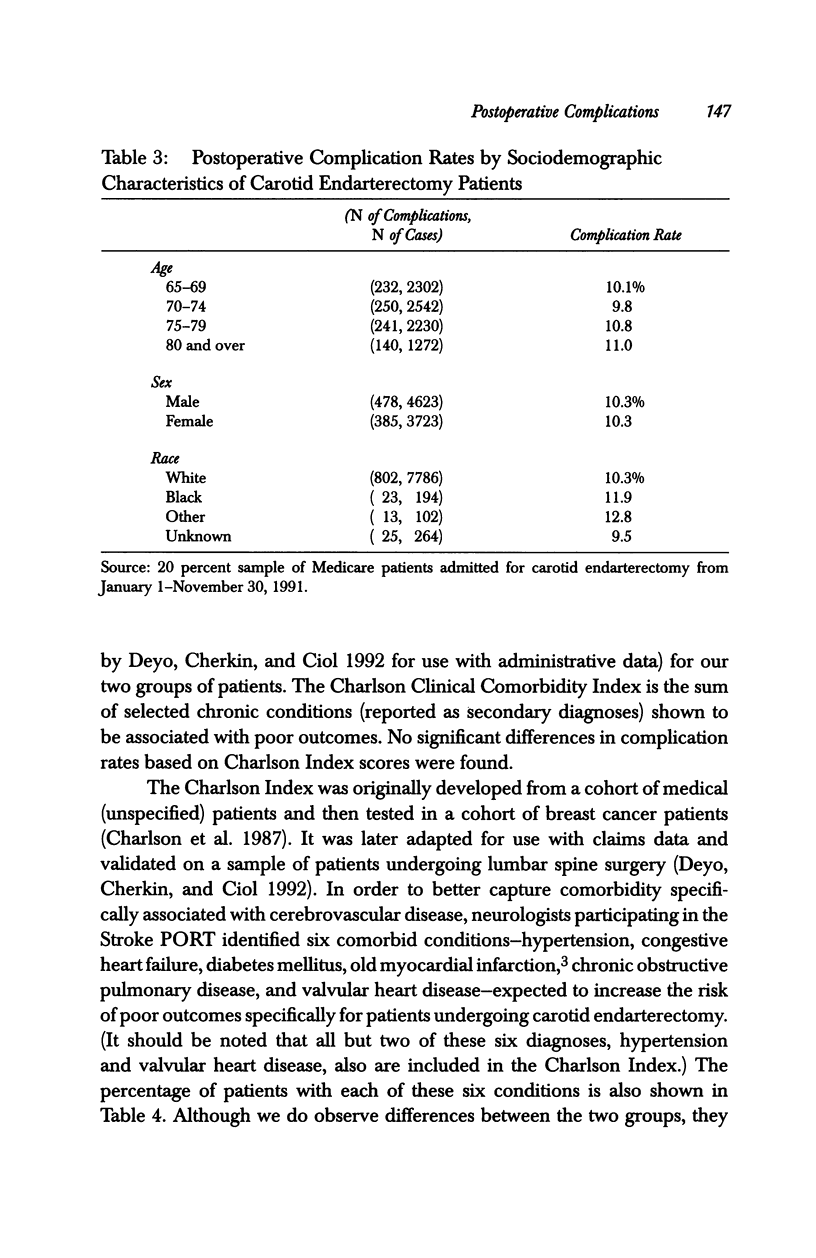
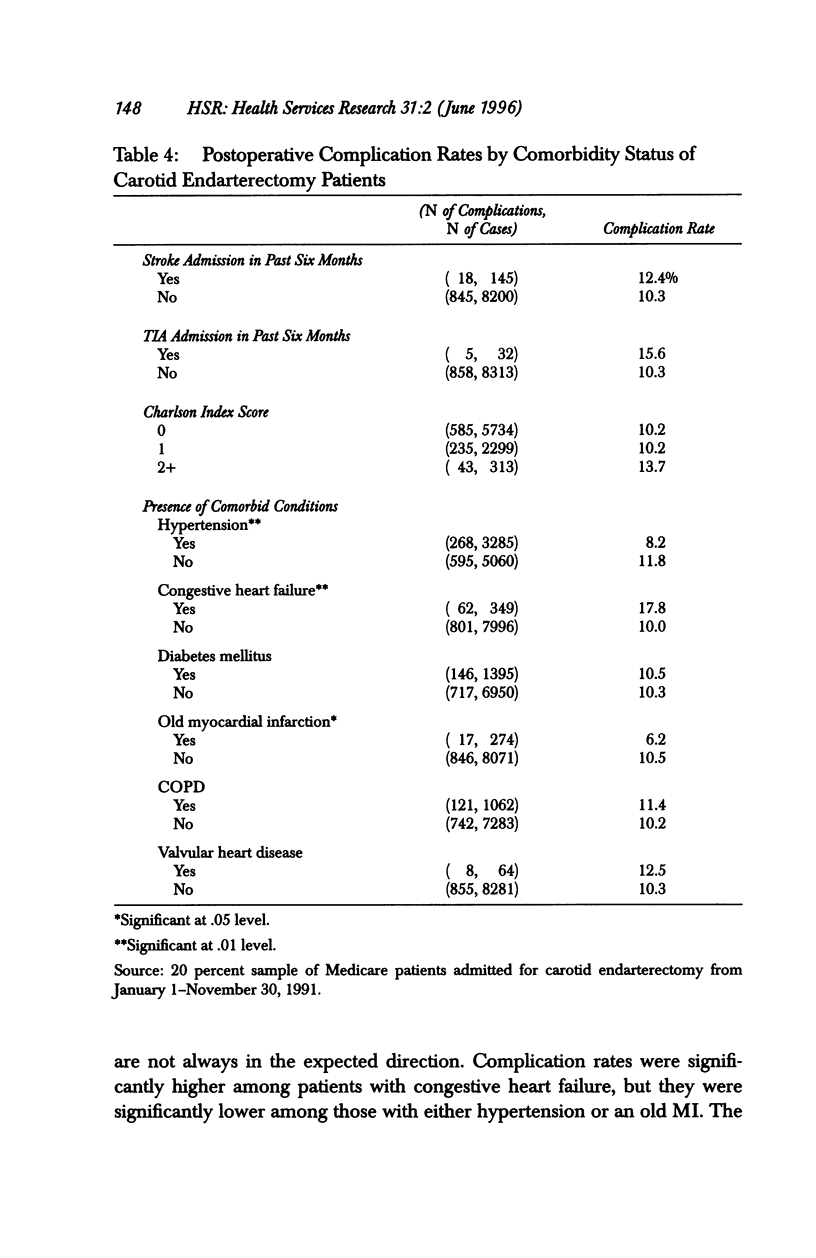
OBJECTIVE. This study develops a methodology for identifying complications following carotid endarterectomy, using physician claims data. DATA SOURCES/STUDY SETTING. We selected a random 20 percent sample of Medicare patients undergoing carotid endarterectomy in 1991 (n = 8,345) and extracted all of their claims. STUDY DESIGN. Project neurologists identified the following services as indicative of complications following carotid endarterectomy if they were provided within 30 days of surgery: head CT, head MRI, and surgical exploration of the neck for hemorrhage, thrombosis, or infection. DATA COLLECTION/EXTRACTION METHODS. Total costs were calculated from all claims associated with the hospitalization and the 30-day postoperative period. Outcomes included mortality (obtained from Medicare eligibility files), length of stay, discharge to an institution, and readmission to an acute care hospital (the latter obtained from claims data). PRINCIPAL FINDINGS. Surgical complications were identified in one out of every ten endarterectomy patients (10.3 percent). Patients with complications were significantly more likely to die within 30 days of surgery (8.9 percent, compared with 1.1 percent of those not experiencing complications). They also were significantly more likely to be discharged to an institutional setting (24.9 percent versus 2.9 percent), and more likely to be readmitted to acute care hospitals (26.8 percent versus 8.2 percent). Patients with postoperative complications also were significantly more expensive: $22,187 versus $10,892. CONCLUSION. Our findings suggest that physician claims could be used by PROs or similar entities as a screening tool to identify potential problem hospitals or problem surgeons. First, however, the methodology would need to be clinically validated.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Beebe H. G., Clagett G. P., DeWeese J. A., Moore W. S., Robertson J. T., Sandok B., Wolf P. A. Assessing risk associated with carotid endarterectomy. A statement for health professionals by an Ad Hoc Committee on Carotid Surgery Standards of the Stroke Council, American Heart Association. Circulation. 1989 Feb;79(2):472–473. doi: 10.1161/01.cir.79.2.472. [DOI] [PubMed] [Google Scholar]
- Brook R. H., Park R. E., Chassin M. R., Kosecoff J., Keesey J., Solomon D. H. Carotid endarterectomy for elderly patients: predicting complications. Ann Intern Med. 1990 Nov 15;113(10):747–753. doi: 10.7326/0003-4819-113-10-747. [DOI] [PubMed] [Google Scholar]
- Charlson M. E., Pompei P., Ales K. L., MacKenzie C. R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Deyo R. A., Cherkin D. C., Ciol M. A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992 Jun;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Fisher E. S., Malenka D. J., Solomon N. A., Bubolz T. A., Whaley F. S., Wennberg J. E. Risk of carotid endarterectomy in the elderly. Am J Public Health. 1989 Dec;79(12):1617–1620. doi: 10.2105/ajph.79.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni L. I., Foley S. M., Daley J., Hughes J., Fisher E. S., Heeren T. Comorbidities, complications, and coding bias. Does the number of diagnosis codes matter in predicting in-hospital mortality? JAMA. 1992 Apr 22;267(16):2197–2203. doi: 10.1001/jama.267.16.2197. [DOI] [PubMed] [Google Scholar]
- Jencks S. F., Williams D. K., Kay T. L. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. JAMA. 1988 Oct 21;260(15):2240–2246. [PubMed] [Google Scholar]
- Matchar D. B., Pauker S. G. Endarterectomy in carotid artery disease. A decision analysis. JAMA. 1987 Aug 14;258(6):793–798. [PubMed] [Google Scholar]
- McCrory D. C., Goldstein L. B., Samsa G. P., Oddone E. Z., Landsman P. B., Moore W. S., Matchar D. B. Predicting complications of carotid endarterectomy. Stroke. 1993 Sep;24(9):1285–1291. doi: 10.1161/01.str.24.9.1285. [DOI] [PubMed] [Google Scholar]
- Mitchell J. B., Bubolz T., Paul J. E., Pashos C. L., Escarce J. J., Muhlbaier L. H., Wiesman J. M., Young W. W., Epstein R. S., Javitt J. C. Using Medicare claims for outcomes research. Med Care. 1994 Jul;32(7 Suppl):JS38–JS51. [PubMed] [Google Scholar]
- Mitchell J. B. Physician DRGs. N Engl J Med. 1985 Sep 12;313(11):670–675. doi: 10.1056/NEJM198509123131106. [DOI] [PubMed] [Google Scholar]


