Summary
Background
This study aims to evaluate primary care providers' adherence to the standard of measuring blood pressure for people aged 35 or above during their initial visit, as per Chinese guidelines, and to identify factors affecting their practices.
Methods
We developed 11 standardized patients (SP) cases as tracer conditions to evaluate primary care, and deployed trained SPs for unannounced visits to randomly selected providers in seven provinces of China. The SPs used a checklist based on guidelines to record whether and how blood pressure was measured. Data were analyzed descriptively and regression analysis was performed to examine the association between outcomes and factors such as provider, patient, facility, and clinical case characteristics.
Findings
The SPs conducted 1201 visits and found that less than one-third of USPs ≥35 had their blood pressure measured. Only 26.9% of migraine and 15.4% of diabetes cases received blood pressure measurements. Additionally, these measurements did not follow the proper guidelines and recommended steps. On average, 55.6% of the steps were followed with few providers considering influencing factors before measurement and only 6.0% of patients received both-arm measurements. The use of wrist sphygmomanometers was associated with poor blood pressure measurement.
Interpretation
In China, primary care hypertension screening practices fall short of guidelines, with infrequent initiation of blood pressure measurements and inadequate adherence to proper measurement steps. To address this, priority should be placed on adopting, implementing, and upholding guidelines for hypertension screening and measurement.
Funding
National Natural Science Foundation of China, Swiss Agency for Development and Cooperation, Doctoral Fund Project of Inner Mongolia Medical University, China Postdoctoral Science Foundation.
Keywords: Unannounced standardized patients, Hypertension screening, Blood pressure measurement
Research in context.
Evidence before this study
Prior to conducting this study, there was a lack of research on the quality of blood pressure screening and measurement practices among primary care providers in China. In March 2022, we conducted a comprehensive literature search using keywords such as “blood pressure measurement,” “blood pressure screen,” and “primary healthcare” in databases including PubMed, Google Scholar, and China National Knowledge Infrastructure. Our search yielded no studies specifically focused on blood pressure screening in primary care, and only a few studies indicated suboptimal blood pressure measurement practices among primary care providers.
Added value of this study
This study represents the first national effort to comprehensively understand blood pressure measurement practices in primary care settings using a large sample. To the best of our knowledge, it is also the first study to employ unannounced standardized patients for assessing primary care providers' adherence to blood pressure screening and measurement requirements. The findings revealed a lack of awareness among primary care providers regarding blood pressure screening and suboptimal adherence to proper measurement procedures. This deficiency may be attributed to limited knowledge or inconsistencies in knowledge and practice among primary care providers themselves. Furthermore, the utilization of wrist sphygmomanometers by primary care providers was associated with poorer performance.
Implications of all the available evidence
The findings of this study underscore the urgent need to enhance the capacity of primary care providers in China and other developing countries for hypertension prevention and management. Specifically, the study highlights the necessity of raising awareness among primary care providers regarding blood pressure screening and emphasizes the importance of systematically replacing blood pressure sphygmomanometers. These implications can inform interventions and policies aimed at improving the quality of blood pressure measurement in primary care settings.
Introduction
Hypertension is a significant global public health concern worldwide and is closely associated with a high burden of cardiovascular disease (CVD) and premature death.1 In 2015, systolic blood pressure (BP) levels of ≥110–115 mmHg and ≥140 mmHg were responsible for an estimated 10.7 million (19.2% of all deaths) and 7.8 million (14.0% of all deaths) deaths, respectively.2 Of note, China has a disproportionately high hospital admission rate for hypertension, with 490 admissions per 100,000 population, greatly exceeding the average rate of 95 per 100,000 population among countries in the Organization for Economic Co-operation and Development (OECD).3,4 Furthermore, the prevalence of hypertension in China is high and rapidly increasing.5 From 2012 to 2015, the crude prevalence of hypertension among Chinese residents aged 18 years and above was 27.9%, and nearly half of Chinese adults aged 35–75 years had hypertension in 2017.6
Accurate blood pressure measurement is crucial for the effective management of hypertension.7 Timely screening can aid in preventing and managing hypertension, as recommended by the US Preventive Services Task Force (USPSTF) for adults aged 18 years or older with office blood pressure measurement.8 In China, the Medium and Long-Term Plan for Prevention and Treatment of Chronic Diseases (2017–2025) requires BP measurements for people over 35 years at their initial health provider visits.9,10 BP measurement is also a standard procedure in various healthcare settings as a part of vital sign measurement and assessment. Thus, an accurate and reliable BP measurement is essential for the proper diagnosis and management of diseases and for identifying potential health problems.11 It also provides therapist with information regarding the patient's baseline cardiovascular status and response to exercise/activity and guides exercise prescription.12
However, inaccurate BP measurement procedures can result in overdiagnosis and unnecessary treatment or underdiagnosis and increased risk for CVD.13 Factors such as observer bias, faulty equipment, and lack of standardization in measurement techniques can contribute to inaccurate results.14 Guidelines have been established to improve the accuracy of BP measurements.15,16 In China, primary care is responsible for providing free hypertension management services. But there are challenges in understanding the BP measurement practices in primary care,17,18 including a lack of studies using nationally representative samples and the use of assessment tools with low validity. To address these challenges, this study This study used a sample of primary care from seven provinces in China with different socio-economic characteristics and unannounced standardized patients (USPs)—a tool with high validity and reliability to assess the BP measurement practices in China.
The USP method is a gold standard for measuring quality of care and has been increasingly used in low and middle income countries.19,20 This method involves training healthy individuals to consistently simulate the medical history, physical symptoms, and emotional characteristics of real patients, and then observing how healthcare providers interact with these “standardized patients” without informing the providers that they are being observed.21 This approach reduces the “Hawthorne effect”, where providers may act differently when they know they are being watched, and minimizes issues such as falsification or loss of records, and patient recall bias. Additionally, this method controls for case mix and allows for comparison between different providers.22,23
In summary, our study aims to use USPs to assess primary care providers' adherence to the best blood pressure screening and measurement practices and to explore the influencing factors to strengthen the primary care practice in BP measurement.
Method
Study design
This cross-sectional study was conducted in China between March 2021 and December 2022, is part of the Primary heAlth Care quAlity Cohort In chinA (ACACIA study/https://www.researchgate.net/project/ACACIA Study),24,25 which aims to assess the quality of primary care every five years. This study used the current and the first assessment of ACACIA.
Study setting and participants
The sample included primary care institutions that meet our inclusion criteria of (1) outpatient clinics of the level I and level II hospitals (which are responsible for a large number of primary health services in China) and (2) community health centers, community health stations, urban clinics, township health centers, and village clinics in the rural settings. The research participants only include licensed physicians, assistant licensed physicians, and village doctors working in the selected institutions. Furthermore, the included clinicians must practice in general practice, internal medicine, surgery, obstetrics, gynecology, or pediatrics (please see the previously published study protocol for details).21,24 ACACIA study developed, validated, and used 11 USP cases as tracers for common primary health care conditions, including migraine, postpartum depression, infantile diarrhea, lower back pain, gastritis, stress urinary incontinence, hypertension, diabetes, angina, asthma, and common cold.
Sample size
The sample size was determined using the formula n = z1ˆ2-α/2p (1-p)/dˆ2, with a type I error (both sides) of 0.05, an assumed complete rate with BP measurement practice of 65% (based on previous studies and suggestions from primary care physicians),26 and a tolerable error was 0.2. As a result, the sample for the study should consist of 220 USP–clinician encounters.
Sampling method
Our sampling method intends to create a representative sample of primary care in China, and we reported the sampling details in our protocol.21 In summary, the sampling process includes two stages. In stage I, we purposely selected seven provinces across China from north to south to represent the different socioeconomic development statuses, including Inner Mongolia, Shaanxi, Gansu, Hunan, Guizhou, Sichuan, and Guangdong (Supplementary Figure S1). In stage II, we randomly selected primary care institutions from each province for the USP-clinician encounter. As primary care institutions varied in clinician numbers, several institutions were packaged into pseudo-groups of similar size for random selection. The final sample comprised 2200 expected USP-clinician visits across 1226 primary care institutions in the seven selected provinces (Supplementary Figure S2).
Outcomes
We selected three groups of outcomes in this study. The first two outcomes evaluate whether primary care providers adhere to the BP measurement requirements mandated by national policies and guidelines. The third outcome evaluates the extent to which primary care providers follow the best measurement practices. We provide details below.
Initial BP measurement in individuals ≥35 years of age
The first outcome was the incidence of measuring BP at the initial visit for people ≥35 years old. China's national health policies mandate this BP measurement to promote the screening and treatment of chronic diseases.9,10
BP measurement in migraine, diabetes, and hypertension
Our second outcome was a binary variable that assessed whether primary care providers check BP in individuals with migraine, hypertension, and diabetes. These three cases were chosen because clinical practice guidelines explicitly recommend measuring BP for those conditions.16,27, 28, 29
Completed rate of BP measurement practice
We must follow proper procedures to measure BP to obtain a valid reading. This outcome was a continuous variable and was operationalized as a percentage of procedural items completed in BP measurement, following the nine items of the Chinese Guideline for the Management of Primary Hypertension.16 These items include:
-
1)
Asking patients to avoid caffeine, exercise, and smoking before measurement and ensuring they have emptied their bladder;
-
2)
Arranging the patient to relax in a chair (feet on the floor, back supported) for more than 5 min;
-
3)
Not allowing the patient or observer to talk during the rest period or the measurement;
-
4)
Reminding the patients to keep their legs uncrossed and their feet flat on the floor;
-
5)
Measuring the patient's blood pressure in a sitting position;
-
6)
Positioning the middle of the cuff on the patient's upper arm at the level of the right atrium (midpoint of the sternum);
-
7)
Using the correct cuff size;
-
8)
Placing the cuff 2–3 cm above the antecubital fossa (wrist blood pressure monitor is not applicable);
-
9)
Recording BP for both arms for the first visit.
Immediately after each USP visit, the USPs recorded whether each step in measuring BP was performed and calculated the proportion of completed steps (i.e., the number of completed steps divided by the total number of applicable steps) as a measure of adherence to proper BP measurement practices.
Other variables
In addition to the study outcome variables, we also collected information on factors that may predict adherence to best practices for measuring BP. This including the location of the USP visit, sociodemographic information of USPs and physicians, and characteristics of the healthcare facilities such as facility management category, facility type, and rural/urban attributes). We extracted institutional information from the government health institution database, while information on the clinicians was collected on-site by the USPs.
Data collection
To ensure the quality of data collected, the USPs were trained and validated before conducting their visit. The details of the training and validation were reported earlier.25 In summary, each USP received online-offline hybrid training focused on the accurate and reliable rendition of their roles and completing the quality checklists. The USPs were, in particular, trained to identify different BP measurement tools and the proper steps for measurement. The USPs visited clinicians without prior announcement (primary care in China generally does not require appointments) and followed regular care procedures. After each encounter with the clinician, the USPs completed a pre-defined quality checklist. The checklist included evidence-based and explicit quality criteria for consultation, physical examination, lab tests, diagnosis, and treatment, as well as BP-measurement-related items.
Data were collected and managed using the cloud-based Research Electronic Data Capture (REDCap) system.30 To minimize missing data, the electronic questionnaire was designed with a “must-enter” format for all items related to BP measurement.
Statistical methods
Covariates in our analysis were patient age and sex. We performed descriptive analyses to characterize BP measurements and used generalized linear model analyses to investigate influencing factors. SPSS v26.0 was used for data analyses. Categorical variables were presented as frequency (percentage), and continuous variables were expressed as mean (standard deviation). We used appropriate statistical tests, such as chi-squared test, Fisher exact, t-test, and ANOVA, to compare differences between groups. Compared to the odds ratio (OR), the risk ratio (RR) offers a more intuitive representation of the impact of various factors on the outcome.31 And when the incidence of the outcome event is relatively common (>10%), the or tends to significantly overestimate or underestimate the true rr. Therefore, we utilized a modified Poisson regression, utilizing a procedure known as ‘sandwich estimation,’ to estimate robust standard errors and address model misspecification due to the binary outcome not adhering to a Poisson distribution.32, 33, 34 This approach allowed us to estimate the risk ratio and its 95% confidence interval (CI) to explore the association between independent variables and primary care physician guideline adherence (binary outcome). Additionally, a generalized linear model with normal distribution and identity link was employed to explore potential independent factors influencing physicians' completed rate of BP measurement practice (continuous outcome). Baseline variables that were clinically relevant or statistically significant in univariate analyses (p < 0.2) were included in multivariate analyses, with a two-tailed significance level of p < 0.05. Due to the presence of missing values in less than 1% of visits, with only two instances where institutional management type, doctor's age and gender exhibited missing data, we excluded these visits from the multivariate model. For the first outcome, initial measurement in individuals ≥35 years of age, given the potential correlation or multicollinearity between variables related to blood pressure measurement and the variable representing different clinical cases, we made the deliberate choice to include only the “cases” in the multivariate analysis. Although both variables exhibited statistical significance in the univariate analyses.
Ethical reviews
Ethical approvals were obtained from Sun Yat-sen University (2017–011 and 2019–024), Xi'an Jiaotong University (2020–1288), Guizhou Medical University (2020–201) and Lanzhou University (2020–0901). All review boards granted a waiver for consent from the clinicians involved in the USP visits. The waiver is necessary to eliminate sample bias due to possible clinician self-selection into the program. All data were fully de-identified and reported as aggregated results only.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
The USPs completed 2023 out of the 2200 planned visits. In our study, we employed standardized patients (USPs) for assessments instead of real patients. The sociodemographic characteristics of USPs were designed according to clinical guidelines and primary care physician case records. Therefore, apart from age and sex, all other “patient” characteristics were simulated, including education and occupation.
A total of 40 USPs were involved in the visits we included. To address the shortage of personnel due to the impact of the COVID-19 pandemic and to ensure visit quality, 27 USPs portrayed two different cases each, while 13 USPs portrayed a single case. 57.5% of usps aged over 35 years, and 28 were female (Supplementary Table S1).
Screening blood pressure in individuals ≥35 years of age
We analyzed a total of 1201 visits while excluding 822 visits from the analysis. Among the excluded visits, 646 were related to usps under the age of 35, and an additional 176 visits pertained to cases of infantile diarrhea which did not involve actual pediatric patients. Meanwhile, The substantial number of visits involving individuals under the age of 35 is attributed to our case design. We have selected 11 common case types found in primary healthcare settings. Additionally, to align with the real world, we have pre-defined the sociodemographic characteristics of standardized patients. Subsequent recruitment was conducted based on age distribution, with standardized patients over 35 years old specifically assigned to cases involving asthma, lower back pain, angina, hypertension, diabetes, and stress urinary incontinence, while patients under 35 years old were assigned to migraine cases. For the remaining cases, the age range was more diverse, encompassing standardized patients both above and below 35 years old. Each case required 200 visits, resulting in a relatively higher proportion of visits from patients under 35 years old. However, upon comparing the included and excluded visits, we did not identify any significant differences. Furthermore, our comparison between the included and excluded visits did not reveal any significant differences (Supplementary Table S2).
Our results showed that BP was measured in only 340 (28.3%) visits by USPs over 35 years of age. The ratio of BP screening did not vary significantly between provinces. The highest ratio of BP measurement was observed in hypertension cases (148 out of 185, 80.0%), while fewer than 10% of visits for stress urinary incontinence and gastritis received BP measurements (Table 1). Our analysis also showed that standardized patients with hypertension were more likely to receive a blood pressure measurements compared to other cases. However, other institutional and clinician characteristics were not found to be associated with BP measurement (Table 2).
Table 1.
Univariate analysis of primary care physician adherence to initial BPM in individuals above 35 years old.
| Variable | Total (n/%) | Initial BPM in individuals above 35 years old |
p-value | |
|---|---|---|---|---|
| No | Yes | |||
| Total | 1201 (100.0) | 861 (71.7) | 340 (28.3) | |
| Province | 0.93 | |||
| Inner Mongolia | 79 (6.6) | 58 (73.4) | 21 (26.6) | |
| Hunan | 173 (14.4) | 122 (70.5) | 51 (29.5) | |
| Guangdong | 323 (26.9) | 227 (70.3) | 96 (29.7) | |
| Sichuan | 296 (24.6) | 211 (71.3) | 85 (28.7) | |
| Guizhou | 104 (8.7) | 77 (74.0) | 27 (26.0) | |
| Shaanxi | 144 (12.0) | 103 (71.5) | 41 (28.5) | |
| Gansu | 82 (6.8) | 63 (76.8) | 19 (23.2) | |
| Case | <0.0001 | |||
| Migraine | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Postpartum depression | 12 (1.6) | 11 (91.7) | 1 (8.3) | |
| Gastritis | 67 (5.6) | 63 (94.0) | 4 (6.0) | |
| Asthma | 185 (14.2) | 140 (75.7) | 45 (24.3) | |
| Angina | 186 (15.5) | 111 (59.7) | 75 (40.3) | |
| Lower back pain | 191 (15.9) | 171 (89.5) | 20 (10.5) | |
| Stress urinary incontinence | 187 (15.6) | 169 (90.4) | 18 (9.6) | |
| Hypertension | 185 (15.4) | 37 (20.0) | 148 (80.0) | |
| T2 Diabetes | 188 (15.7) | 159 (84.6) | 29 (15.4) | |
| Management type | 0.79 | |||
| Not-for-profit | 1029 (85.7) | 741 (72.0) | 288 (28.0) | |
| For-profit | 168 (14.0) | 117 (69.6) | 51 (30.4) | |
| Others | 3 (0.2) | 2 (100.0) | 1 (0.0) | |
| Institution type | 0.38 | |||
| Hospital | 372 (31.0) | 272 (73.1) | 100 (26.9) | |
| Community Health Service Center/Station | 62 (5.2) | 39 (62.9) | 23 (37.1) | |
| Township Health Centers | 238 (19.8) | 164 (68.9) | 74 (31.1) | |
| Clinics | 98 (8.2) | 70 (71.4) | 28 (28.6) | |
| Village clinics | 431 (35.9) | 316 (73.3) | 115 (26.7) | |
| Ownership type | 0.34 | |||
| Public | 854 (71.3) | 619 (72.5) | 235 (27.5) | |
| Private | 347 (28.7) | 242 (69.7) | 105 (30.3) | |
| Place of facility | 0.96 | |||
| Urban | 532 (44.3) | 381 (71.6) | 151 (28.4) | |
| Rural | 669 (55.7) | 480 (71.7) | 189 (28.3) | |
| Physician gender | 0.033 | |||
| Male | 861 (71.8) | 632 (73.4) | 229 (26.6) | |
| Female | 339 (28.2) | 228 (67.3) | 111 (33.7) | |
BPM, blood pressure measurement.
Table 2.
Modified poisson regression of adherence to blood pressure measurement at the first visit at age ≥35 years.
| Variables | p-value | RR (95% CI) |
|---|---|---|
| Case | ||
| Hypertension | reference | |
| Postpartum depression | 0.023 | 0.10 (0.014,0.74) |
| Gastritis | <0.0001 | 0.076 (0.028,0.21) |
| Asthma | <0.0001 | 0.27 (0.17,0.42) |
| Angina | <0.0001 | 0.45 (0.30,0.68) |
| Lower back pain | <0.0001 | 0.14 (0.086,0.22) |
| Stress urinary incontinence | <0.0001 | 0.12 (0.076,0.20) |
| T2 Diabetes | <0.0001 | 0.20 (0.13,0.29) |
RR, risk ratio; CI, confidence interval.
BP measurement for migraine, hypertension, and diabetes
There was a total of 566 visits for BP measurement in these three cases, with 26.9% for migraine, 80.0% for hypertension, and 15.4% for diabetes (Supplementary Table S4). The regression also showed that visits for hypertension were more likely to receive a BP measurement compared to migraine (RR = 0.34, 95% CI (0.28, 0.47), p < 0.0001) and diabetes (RR = 0.19, 95% CI (0.13, 0.29), p < 0.0001 respectively). In addition, providers at higher levels of institutions were associated with better performance in checking BP (Table 3).
Table 3.
Modified poisson regression of clinical guidelines adherence.
| Variable | p-value | RR (95% CI) |
|---|---|---|
| Case | ||
| Hypertension | (Reference) | |
| Migraine | <0.0001 | 0.34 (0.25, 0.47) |
| T2 Diabetes | <0.0001 | 0.19 (0.13, 0.29) |
| Institution type | ||
| Hospital | (Reference) | |
| Village Clinic | 0.033 | 0.69 (0.49, 0.97) |
| Community Health Service Center/Station | 0.60 | 1.04 (0.58, 1.84) |
| Township Health Centers | 0.51 | 0.89 (0.62, 1.27) |
| Clinics | 0.91 | 0.88 (0.56, 1.40) |
RR, risk ratio; CI, confidence interval.
Best practice in BP measurement
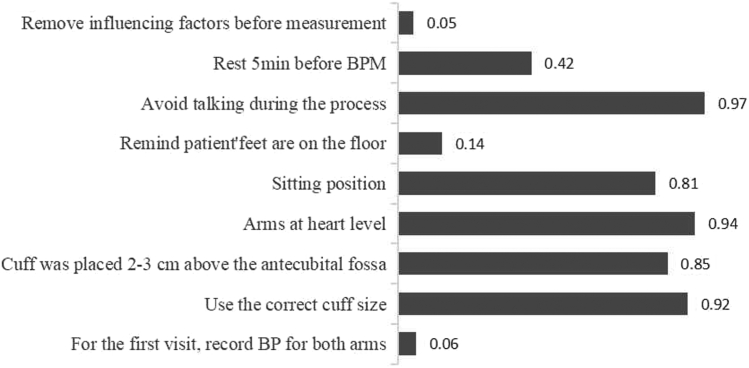
The primary care providers, on average, followed approximately half of the steps required in BP measurement (Supplementary Table S5). They tended to perform well with steps involving direct operation such as correctly placing cuffs, but did not do as well with steps requiring inquiry of patients such as excluding influencing factors before measurement (Fig. 1). Most clinicians used mercury (48.7%) or upper arm sphygmomanometers (31.1%) (Supplementary Table S5). Primary care providers in economically developed provinces tend to have better adherence to measurement requirements (Supplementary Tables S7, S8 and S9). Village doctors had the worst adherence compared with those working in other settings (Table 4, Supplementary Table S6). Meanwhile, the use of a wrist sphygmomanometer was associated with poorer adherence than using the guideline-recommended upper-arm sphygmomanometer (mean difference = −0.13 (−0.16, −0.087), p < 0.0001), particularly for items closely related to the proper usage of the sphygmomanometer itself (Supplementary Tables S10, S11 and S12). No statistically significant association was found between adherence and sociodemographic characteristics of the providers (Table 4).
Fig. 1.
Completed rate of each item of blood pressure measurement practice.
Table 4.
Generalized linear model analysis of factors influencing adherence to best practice in BPM (complete rate).
| Variable | p-value | Mean difference (95% CI) |
|---|---|---|
| Province | ||
| Guangdong | (Reference) | |
| Inner Mongolia | 0.65 | −0.012 (−0.061, 0.038) |
| Hunan | <0.0001 | −0.094 (−0.13, −0.059) |
| Sichuan | 0.004 | −0.047 (−0.079, −0.015) |
| Guizhou | 0.30 | −0.024 (−0.070, 0.021) |
| Shaanxi | 0.46 | 0.014 (−0.023, 0.051) |
| Gansu | 0.001 | −0.090 (−0.14, −0.039) |
| Institution type | ||
| Hospital | (Reference) | |
| Village Clinic | 0.002 | −0.046 (−0.075, −0.018) |
| Community Health Service Center/Station | 0.002 | −0.072 (−0.12, −0.026) |
| Township Health Centers | 0.70 | 0.006 (−0.025, 0.038) |
| Clinics | 0.019 | −0.051 (−0.078, −0.021) |
| Sphygmomanometer type | ||
| Upper arm sphygmomanometer | (Reference) | |
| Mercury sphygmomanometer | 0.67 | −0.006 (−0.032, 0.021) |
| Arm cylinder sphygmomanometer | 0.30 | −0.023 (−0.067, 0.021) |
| Wrist sphygmomanometer | <0.0001 | −0.13 (−0.16, −0.087) |
| Physician gender | ||
| Male | (Reference) | |
| Female | 0.014 | 0.030 (0.006, 0.055) |
CI, confidence interval.
Sensitivity analysis
We conducted a sensitivity analysis to compare the results of the original analysis with those obtained after applying mode imputation for missing data. The findings were robust to the choice of method, aligning with the original results.
Discussion
In this study, we assessed blood pressure screening and measurement in primary care clinics in seven Chinese provinces using a random sample of visits by unannounced standardized patients. We found that primary care providers screened for BP in only one-third of the first-visits in individuals aged ≥35 years, and they followed, on average, only 55.6% of the recommended steps for BP measurement. Adherence to best practices in BP measurement varied based on factors such as provider gender, facility type, clinical cases involved, and the type of sphygmomanometer used.
The failure to adhere to blood pressure screening and measurement standards is a cause for concern. Screening BP for adults is a standard of care in many countries, including China.8, 9, 10,35 Research suggests that regular blood pressure screening can substantially reduce the risk associated with hypertension and lower blood pressure levels within the population. A large randomized trial in Canada found that BP screening reduced hospitalizations for heart-related conditions such as acute myocardial infarction, congestive heart failure, and stroke.36 China's Longitudinal Healthy Longevity Surveys also suggested that regular community-based blood pressure screening can effectively manage blood pressure and significantly reduce population blood pressure levels.37 However, in this study, less than one-third of USPs ≥35 years received BP measurements during their visits, and those measurements were focused on suspected cases of hypertension, suggesting that BP measurements were likely to be performed for diagnostic rather than screening purposes. Even for the migraine and diabetes cases, where clinical practice guidelines explicitly require BP measurement, BP was measured in only 26.9% and 15.4% of our USP visits for the two cases, respectively. In the UK, 60.0% of non-diabetic patients self-reported having undergone hypertension screening at primary care offices,38 while chart audits in Indiana rural counties in the US revealed a rate of 71.0%.39 The low rate of BP screening in China is compounded by a lack of adherence to proper measurement techniques. Accurate measurement is crucial for enhancing the effectiveness of BP screening.14 However, primary care providers in China, in particular, often neglect important steps such as properly preparing patients for BP measurement and taking blood pressure in both arms during initial visits. It is concerning that primary care providers in our study only followed only 55.6% of the recommended procedures for BP measurement, which is lower than many other developing countries such as Maldonado (69.0%) and Brazil (65.0%), where adherence was assessed using clinical vignettes and direct observation, respectively.26,40 However, it's important to note that medical records in primary care are often unavailable or incomplete, and charts only record that a BP measurement was made, not how it was done. Patient surveys are prone to recall bias and can be influenced by the information asymmetry between doctors and patients. While clinical vignettes provide a more standardized measurement, they test a clinician's competency rather than their actual practice. And direct observation leads to the “Hawthorne effect”, where clinicians modify their behavior when aware of being observed.23,41 These methods rely on indirect information that may not faithfully or comprehensively represent the intricacies of actual clinical practice. Comparatively, the use of Usp comes closer to real clinical practice, allowing for a more systematic measurement of healthcare quality.42
Few studies have explicitly discussed why primary care in China performs poorly in BP measurement. Studies have shown that primary care providers in China do not follow guideline recommendations well, with adherence rates ranging from 9.6% to 23.4%.25 One of the contributing factors is insufficient knowledge and know-do gaps.43 Consistent with previous study,44 we found primary care providers in economically developed provinces or higher-tier health institutions were more likely to comply with BP screening and measurement requirements, likely due to varying degrees of their knowledge gaps. Meanwhile, the gap between knowledge and practice among primary care providers is a widely recognized issue. Studies, such as one conducted by Mohan and colleagues, have found that there was often no correlation between a clinician's knowledge and their practice of measuring BP.45 Moreover, the prevalent issue of burnout among healthcare workers could significantly compromise the quality of care, especially during the COVID-19 pandemic. Primary care providers have grappled with substantial challenges linked to heightened burnout levels during this period.46,47 Lastly, it's worth noting that both financial and non-financial incentives might not adequately acknowledge high-quality work.48 Drawing from our findings, several key directions for future endeavors emerge: 1) Incorporating optimal practices into the daily routines of primary healthcare providers through systematic approaches49; 2) Providing feedback and mechanisms for improvement: offering primary healthcare personnel feedback on their actual behaviors and aiding them in recognizing gaps between knowledge and action to enhance quality50; 3) Ensuring that social health insurance programs provide payments to healthcare service providers to reward commendable performance and outcomes.3
Our study showed that nearly half of the primary care providers were still using mercury sphygmomanometers instead of the guideline-recommended upper arm sphygmomanometers. The type of sphygmomanometer used was correlated with the providers' BP measurement practices. Mercury sphygmomanometers require specialized clinical knowledge, manual dexterity, and good hearing and vision, and are being phased out due to concerns about mercury toxicity.51 Automatic and semi-automatic devices are easier to use and provide objective BP measurement, independent of the person performing the measurement, and guidelines recommend the use of upper-arm sphygmomanometers.52 The continued use of mercury sphygmomanometers is likely due to their long history of availability. There are no reports of systematic replacement of mercury sphygmomanometers. Cost-effectiveness studies of the system-level sphygmomanometer replacement may be necessary to support future policy decisions.
Strengths and limitations
To the best of our knowledge, this study is the first to use unannounced standardized patients to assess primary care providers' adherence to BP screening and measurement requirements. Compared to previous studies that relied on methods like medical chart reviews, patient surveys, and clinical vignettes to evaluate clinician performance in blood pressure (BP) measurements, the utilization of usp has significantly enhanced the measurement validity, reliability, and comparability.23,41 Additionally, the use of multiple tracer conditions allows for a more comprehensive understanding of primary care quality. Notably, there have been no previous efforts to assess BP screening and measurement practices in China at the national level.
This study has several limitations. Firstly, in order to minimize potential detection of the USP, SPs were only able to collect a limited amount of clinician information, which restricted our ability to analyze factors that may influence BP measurement practice. For example, there was no information on clinician training and incentives. Secondly, given the limitations of resources in this study, we chose purposive sampling to ensure the inclusion of provinces with varying levels of socioeconomic development. Our provincial sample underrepresents those with high GDP per capita and high life expectancy. Therefore, while our results can accurately capture the quality of care in the selected seven provinces, they may underestimate the national quality. However, it's important to note that our analysis shows the quality in Guangdong (which belongs to the category of highest GDP per capita and life expectancy) does not significantly differ from the other provinces. Additionally, due to resource constraints, we did not interview or survey clinicians after USP visits to better understand their practice behaviors. Finally, we did not assign weights to each BP measurement step to gain a more precise understanding. However, there is a lack of evidence to determine the appropriate weights for each step.
Conclusion
In conclusion, screening and measuring hypertension in China's primary care are inadequate and not standardized. Research and policy priorities should be given to adopting, implementing, and maintaining guide-recommended screening and measurement requirements for hypertension.
Contributors
LPZ and HJL contributed equally to this paper. They collaborated on data analysis and manuscript drafting. HYL, WJH, and SYL assisted in checking and determining the statistical methods used for the data. YYC and YCF managed the survey work, while WXH handled case development. QZ, DMZ, JQL, SSL, YYX, and CPL collected data. NZ was in charge of the survey design and implementation. DX conceived the study. Professors DX and NZ served as co-corresponding authors. All authors were responsible for the interpretation of the data, and revised, and gave final approval of the manuscript.
Data sharing statement
After completing the visit with standardized patients, we will consider making the data publicly available.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors declare that there are no conflicts of interest.
Acknowledgements
We extend our thanks to all members of ACACIA Labs and express our gratitude to the USP and investigators for their contributions to the completion of visits.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100973.
Contributor Information
Nan Zhang, Email: skyzn@126.com.
Dong (Roman) Xu, Email: romanxu@i.smu.edu.cn.
Appendix A. Supplementary data
References
- 1.Kearney P.M., Whelton M., Reynolds K., Muntner P., Whelton P.K., He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217–223. doi: 10.1016/S0140-6736(05)17741-1. [DOI] [PubMed] [Google Scholar]
- 2.Forouzanfar M.H., Liu P., Roth G.A., et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317(2):165–182. doi: 10.1001/jama.2016.19043. [DOI] [PubMed] [Google Scholar]
- 3.Li X., Krumholz H.M., Yip W., et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi: 10.1016/S0140-6736(20)30122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang Z., Chen Z., Zhang L., et al. China hypertension survey investigators. Status of hypertension in China: results from the China hypertension survey, 2012-2015. Circulation. 2018;137(22):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 5.Ye X., Yi Q., Shao J., et al. Trends in prevalence of hypertension and hypertension phenotypes among Chinese children and adolescents over two decades (1991-2015) Front Cardiovasc Med. 2021;8 doi: 10.3389/fcvm.2021.627741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lu J., Lu Y., Wang X., et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project) Lancet. 2017;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 7.Muntner P., Shimbo D., Carey R.M., et al. Measurement of blood pressure in humans: a scientific statement from the American heart association. Hypertension. 2019;73(5):e35–e66. doi: 10.1161/HYP.0000000000000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Preventive Services Task Force US. Krist A.H., Davidson K.W., et al. Screening for hypertension in adults: US preventive services task force reaffirmation recommendation statement. JAMA. 2021;325(16):1650–1656. doi: 10.1001/jama.2021.4987. [DOI] [PubMed] [Google Scholar]
- 9.The State Council Office issued a notice on the medium and long-term plan for the prevention and control of chronic diseases in China (2017-2025) EB/OL. 2022. http://www.gov.cn/gongbao/content/2017/content_5174509.htm
- 10.The state council's opinions on implementing the healthy China action (State Council Decree No. 2019 13) EB/OL. 2022. http://www.gov.cn/zhengce/content/2019-07/15/content_5409492.htm
- 11.Pickering T.G., Hall J.E., Appel L.J., et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the subcommittee of professional and public education of the American heart association council on high blood pressure research. Circulation. 2005;111(5):697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 12.Frese E.M., Fick A., Sadowsky H.S. Blood pressure measurement guidelines for physical therapists. Cardiopulm Phys Ther J. 2011;22(2):5–12. [PMC free article] [PubMed] [Google Scholar]
- 13.Stergiou G.S., Palatini P., Parati G., et al. European society of hypertension council and the European society of hypertension working group on blood pressure monitoring and cardiovascular variability. 2021 European society of hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39(7):1293–1302. doi: 10.1097/HJH.0000000000002843. [DOI] [PubMed] [Google Scholar]
- 14.Kallioinen N., Hill A., Horswill M.S., Ward H.E., Watson M.O. Sources of inaccuracy in the measurement of adult patients' resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35(3):421–441. doi: 10.1097/HJH.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Menon S.D., Ganapathi S. How to measure blood pressure accurately. Med J Aust. 2020;213(4):163–165.e1. doi: 10.5694/mja2.50701. [DOI] [PubMed] [Google Scholar]
- 16.National Center for Cardiovascular Diseases National primary care hypertension prevention and control management guidelines 2020 edition. Chin Circ J. 2021;36(3):209–220. [Google Scholar]
- 17.Drawz P. Clinical implications of different blood pressure measurement techniques. Curr Hypertens Rep. 2017;19(7):54. doi: 10.1007/s11906-017-0751-0. [DOI] [PubMed] [Google Scholar]
- 18.Todkar S., Padwal R., Michaud A., Cloutier L. Knowledge, perception and practice of health professionals regarding blood pressure measurement methods: a scoping review. J Hypertens. 2021;39(3):391–399. doi: 10.1097/HJH.0000000000002663. [DOI] [PubMed] [Google Scholar]
- 19.Rethans J.J., Gorter S., Bokken L., Morrison L. Unannounced standardised patients in real practice: a systematic literature review. Med Educ. 2007;41(6):537–549. doi: 10.1111/j.1365-2929.2006.02689. [DOI] [PubMed] [Google Scholar]
- 20.Swanson D.B., van der Vleuten C.P. Assessment of clinical skills with standardized patients: state of the art revisited. Teach Learn Med. 2013;25(Suppl 1):S17–S25. doi: 10.1080/10401334.2013.842916. [DOI] [PubMed] [Google Scholar]
- 21.Xu D., Pan J., Dai X., et al. Comparing quality of primary healthcare between public and private providers in China: study protocol of a cross-sectional study using unannounced standardised patients in seven provinces of China. BMJ Open. 2021;11(1) doi: 10.1136/bmjopen-2020-040792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Akachi Y., Kruk M.E. Quality of care: measuring a neglected driver of improved health. Bull World Health Organ. 2017;95(6):465–472. doi: 10.2471/BLT.16.180190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Aujla N., Chen Y.F., Samarakoon Y., et al. Comparing the use of direct observation, standardized patients and exit interviews in low- and middle-income countries: a systematic review of methods of assessing quality of primary care. Health Policy Plan. 2021;36(3):341–356. doi: 10.1093/heapol/czaa152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu D.R., Hu M., He W., et al. Assessing the quality of primary healthcare in seven Chinese provinces with unannounced standardised patients: protocol of a cross-sectional survey. BMJ Open. 2019;9(2) doi: 10.1136/bmjopen-2018-023997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu D.R., Cai Y., Wang X., et al. Improving data surveillance resilience beyond COVID-19: experiences of primary heAlth care quAlity cohort in China (ACACIA) using unannounced standardized patients. Am J Public Health. 2022;112(6):913–922. doi: 10.2105/AJPH.2022.306779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Machado J.P., Veiga E.V., Ferreira P.A., et al. Theoretical and practical knowledge of nursing professionals on indirect blood pressure measurement at a coronary care unit. Einstein (Sao Paulo) 2014;12(3):330–335. doi: 10.1590/s1679-45082014ao2984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chinese Medical Association Pain Branch Headache Group Chinese guidelines for the diagnosis and treatment of migraine. Chin J Pain Med. 2011;17(2):65–86. [Google Scholar]
- 28.Chinese Hypertension Prevention and Control Guidelines Revision Committee Chinese hypertension prevention and control guidelines 2018 revised edition. Chin J Cardiovasc Med. 2019;24(1):24–56. [Google Scholar]
- 29.American Diabetes Association Standards of medical care in diabetes-2019 abridged for primary care providers. Clin Diabetes. 2019;37(1):11–34. doi: 10.2337/cd18-0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Van Bulck L., Wampers M., Moons P. Research Electronic Data Capture (REDCap): tackling data collection, management, storage, and privacy challenges. Eur J Cardiovasc Nurs. 2022;21(1):85–91. doi: 10.1093/eurjcn/zvab104. [DOI] [PubMed] [Google Scholar]
- 31.Schmidt C.O., Kohlmann T. When to use the odds ratio or the relative risk? Int J Public Health. 2008;53:165–167. doi: 10.1007/s00038-008-7068-3. [DOI] [PubMed] [Google Scholar]
- 32.Holmberg M.J., Andersen L.W. Estimating risk ratios and risk differences: alternatives to odds ratios. JAMA. 2020;324(11):1098–1099. doi: 10.1001/jama.2020.12698. [DOI] [PubMed] [Google Scholar]
- 33.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 34.Knol M.J., Le Cessie S., Algra A., Vandenbroucke J.P., Groenwold R.H. Overestimation of risk ratios by odds ratios in trials and cohort studies: alternatives to logistic regression. CMAJ. 2012;184(8):895–899. doi: 10.1503/cmaj.101715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Health Organization, Regional office for the eastern mediterranean . 2005. Clinical guidelines for the management of hypertension.https://apps.who.int/iris/handle/10665/119738 [Google Scholar]
- 36.Kaczorowski J., Chambers L.W., Dolovich L., et al. Improving cardiovascular health at population level: 39 community cluster randomised trial of Cardiovascular Health Awareness Program (CHAP) BMJ. 2011;342:d442. doi: 10.1136/bmj.d442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chen S., Sudharsanan N., Huang F., Liu Y., Geldsetzer P., Bärnighausen T. Impact of community based screening for hypertension on blood pressure after two years: regression discontinuity analysis in a national cohort of older adults in China. BMJ. 2019;366:l4064. doi: 10.1136/bmj.l4064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stevens S.L., McManus R.J., Stevens R.J. Current practice of usual clinic blood pressure measurement in people with and without diabetes: a survey and prospective 'mystery shopper' study in UK primary care. BMJ Open. 2018;8(4) doi: 10.1136/bmjopen-2017-020589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kirkman M.S., Williams S.R., Caffrey H.H., Marrero D.G. Impact of a program to improve adherence to diabetes guidelines by primary care physicians. Diabetes Care. 2002;25(11):1946–1951. doi: 10.2337/diacare.25.11.1946. [DOI] [PubMed] [Google Scholar]
- 40.Sandoya-Olivera E., Ferreira-Umpiérrez A., Machado-González F. Quality of blood pressure measurement in community health centres. Enferm Clin. 2017;27(5):294–302. doi: 10.1016/j.enfcli.2017.02.001. English, Spanish. [DOI] [PubMed] [Google Scholar]
- 41.Kwan A., Daniels B., Bergkvist S., Das V., Pai M., Das J. Use of standardised patients for healthcare quality research in low- and middle-income countries. BMJ Glob Health. 2019;4(5) doi: 10.1136/bmjgh-2019-001669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Weiner S.J., Schwartz A. Directly observed care: can unannounced standardized patients address a gap in performance measurement? J Gen Intern Med. 2014;29(8):1183–1187. doi: 10.1007/s11606-014-2860-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hwang K.O., Aigbe A., Ju H.H., Jackson V.C., Sedlock E.W. Barriers to accurate blood pressure measurement in the medical office. J Prim Care Community Health. 2018;9 doi: 10.1177/2150132718816929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Taweel D.M., Awad A.I., Johnson B.J. Evaluation of adherence to international guidelines for treating patients with type 2 diabetes mellitus in Kuwait. Int J Clin Pharm. 2013;35(2):244–250. doi: 10.1007/s11096-012-9738-8. [DOI] [PubMed] [Google Scholar]
- 45.Mohan B., Aslam N., Ralhan U., et al. Office blood pressure measurement practices among community health providers (medical and paramedical) in northern district of India. Indian Heart J. 2014;66(4):401–407. doi: 10.1016/j.ihj.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Asante J.O., Li M.J., Liao J., Huang Y.X., Hao Y.T. The relationship between psychosocial risk factors, burnout and quality of life among primary healthcare workers in rural Guangdong province: a cross-sectional study. BMC Health Serv Res. 2019;19:447. doi: 10.1186/s12913-019-4278-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jalili M., Niroomand M., Hadavand F., Zeinali K., Fotouhi A. Burnout among healthcare professionals during COVID-19 pandemic: a cross-sectional study. Int Arch Occup Environ Health. 2021;94(6):1345–1352. doi: 10.1007/s00420-021-01695-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li X., Lu J., Hu S., et al. The primary health-care system in China. Lancet. 2017;390(10112):2584–2594. doi: 10.1016/S0140-6736(17)33109-4. [DOI] [PubMed] [Google Scholar]
- 49.Bauer M.S., Kirchner J. Implementation science: what is it and why should I care? Psychiatry Res. 2020;283 doi: 10.1016/j.psychres.2019.04.025. [DOI] [PubMed] [Google Scholar]
- 50.Van Den Bulck S., Spitaels D., Vaes B., Goderis G., Hermens R., Vankrunkelsven P. The effect of electronic audits and feedback in primary care and factors that contribute to their effectiveness: a systematic review. Int J Qual Health Care. 2020;32(10):708–720. doi: 10.1093/intqhc/mzaa128. [DOI] [PubMed] [Google Scholar]
- 51.Brady T.M., Padwal R., Blakeman D.E., et al. Blood pressure measurement device selection in low-resource settings: challenges, compromises, and routes to progress. J Clin Hypertens. 2020;22(5):792–801. doi: 10.1111/jch.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.John O., Campbell N.R.C., Brady T.M., et al. The 2020 "WHO technical specifications for automated non-invasive blood pressure measuring devices with cuff". Hypertension. 2021;77(3):806–812. doi: 10.1161/HYPERTENSIONAHA.120.16625. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.