Abstract
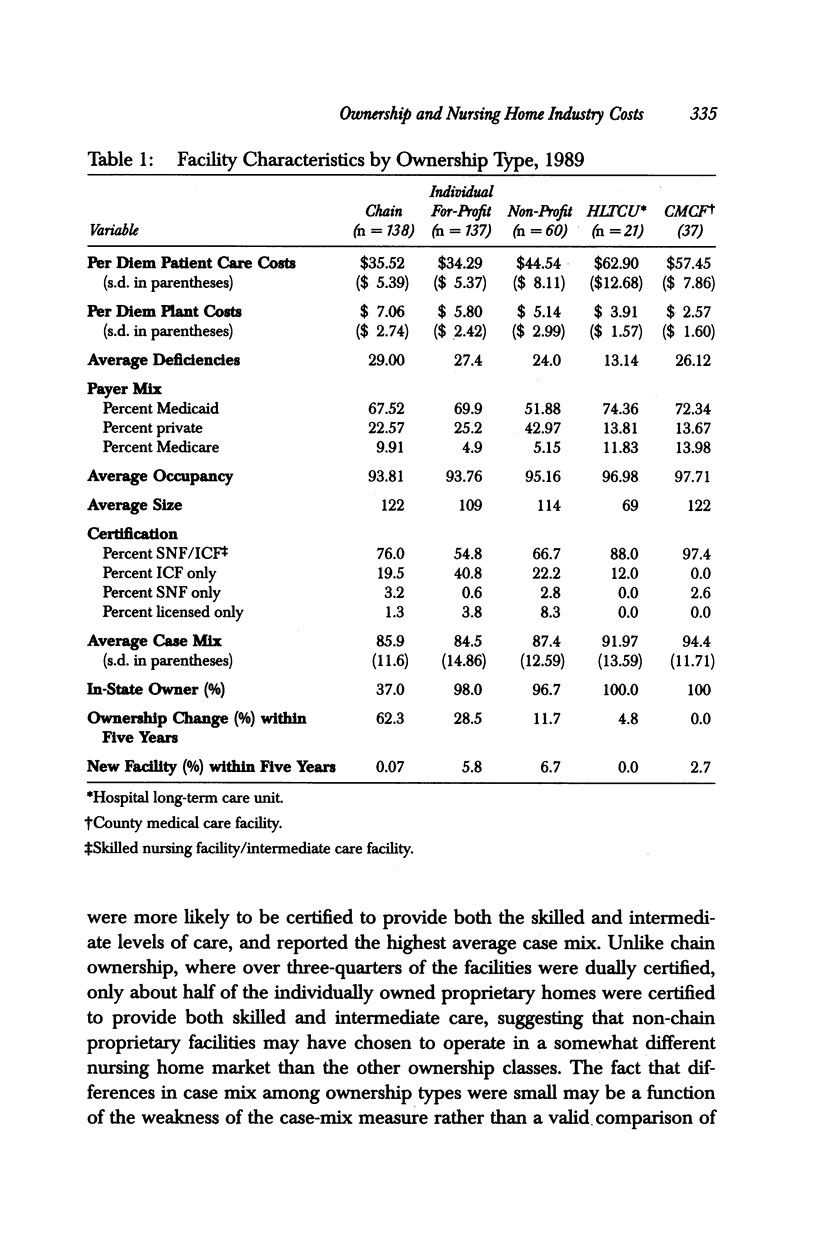
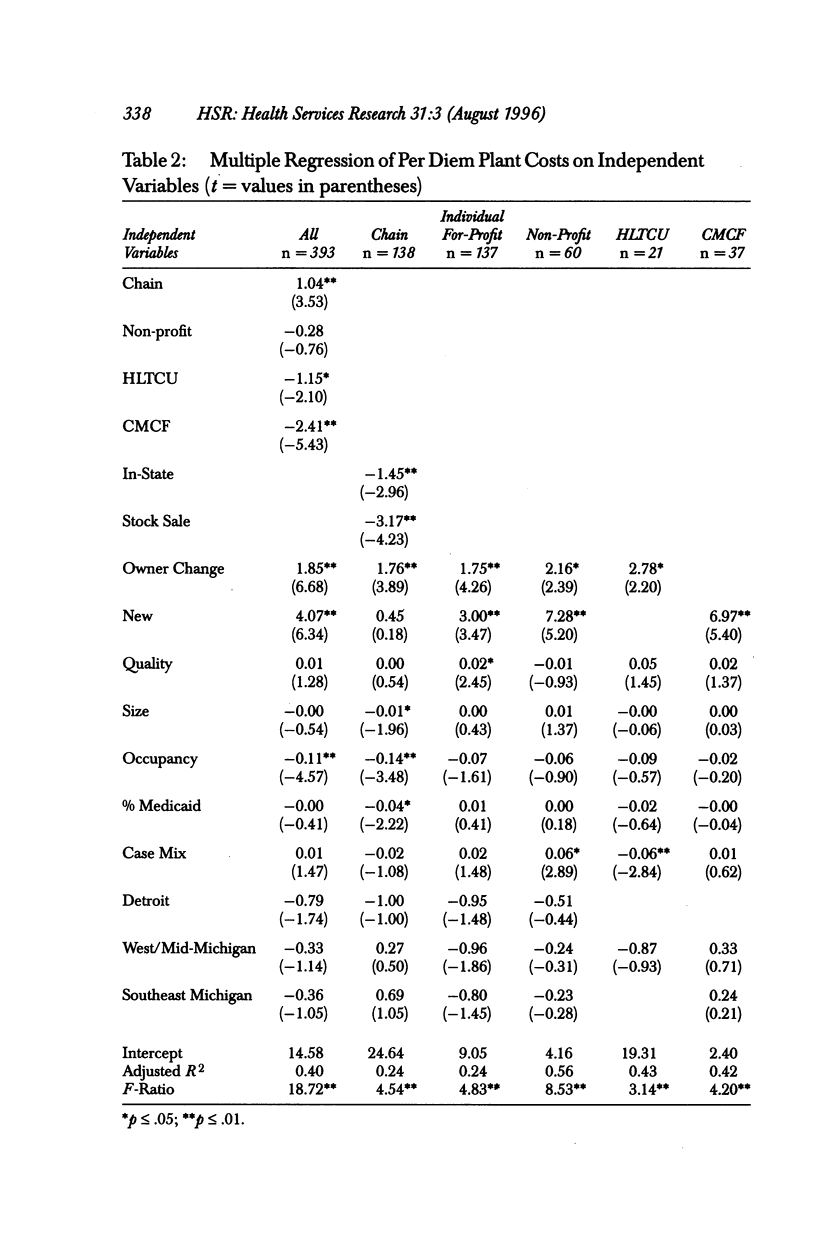
OBJECTIVE. This study examines the effects of ownership type and ownership change on nursing home cost structures, differentiating patient care costs from plant costs. DATA SOURCES. Administrative data from the Michigan Department of Social Services, Medical Services Administration (Medicaid), and the Michigan Department of Public Health are used. Cost data are based on audited cost reports for 393 nursing care facilities in Michigan in 1989. Other facility characteristics are based on data from the 1989 annual licensing and certification survey conducted by the Michigan Department of Public Health. STUDY DESIGN. A series of ordinary least squares regressions is estimated, in which the dependent variable is either per diem patient costs or per diem plant costs. Ownership types are defined as chain, proprietary non-chain, freestanding non-profit, government-owned, and hospital-based facilities. Pooled estimation techniques, as well as separate regressions by ownership type, are presented to test for interaction effects. Key variables include whether a facility changed ownership in the preceding five years and whether chain facilities are in-state- or out-of-state-owned, in addition to size, payer mix, and case mix. PRINCIPAL FINDINGS. Behavioral differences among nursing home ownership types in respect to patient care costs tended to distinguish government-owned and hospital-based facilities from the freestanding homes rather than the usual distinction between for-profit and not-for-profit classes. Variables traditionally included in nursing home cost studies, such as size, occupancy, payer mix and case mix, were found to have similar effects on per diem patient care costs for freestanding non-profit homes as well as for chain proprietary facilities. With regard to the effects of ownership change on per diem plant and per diem patient costs, however, there are few differences among ownership types. Chain and non-chain for-profit facilities, non-profit homes, and hospital long-term care units that had changed ownership reported significantly higher per diem plant costs than facilities without a change of ownership, but did not spend more on patient-related costs. Michigan Medicaid plant reimbursement system policy changes instituted in 1985 to promote continued ownership of facilities were not entirely successful. CONCLUSIONS. Non-profit homes look increasingly like their for-profit counterparts with respect to spending on patient care costs. Increased competition for the more lucrative private-pay patients, coupled with declining state Medicaid reimbursement to nursing homes, may have blurred the historical distinctions between the non-profit and for-profit sectors in the nursing home industry. An exception to increasing homogeneity within the nursing home industry is the tendency of proprietary homes to experience more frequent changes of ownership, which results in higher capital costs passed on to state Medicaid programs. Findings from this study indicate that while facility sales increase per diem plant costs, they do not result in increased spending for direct patient care, suggesting that state Medicaid programs may be indirectly subsidizing facility sales with no accompanying increase in expenditures for patient care. To discourage frequent facility sales, state Medicaid programs may need to consider alternative methods of reimbursing nursing home owners for capital costs.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arling G., Nordquist R. H., Capitman J. A. Nursing home cost and ownership type: evidence of interaction effects. Health Serv Res. 1987 Jun;22(2):255–269. [PMC free article] [PubMed] [Google Scholar]
- Baldwin C. Y., Bishop C. E. Return to nursing home investment: issues for public policy. Health Care Financ Rev. 1984 Summer;5(4):43–52. [PMC free article] [PubMed] [Google Scholar]
- Birnbaum H., Bishop C., Lee A. J., Jensen G. Why do nursing home costs vary? The determinants of nursing home costs. Med Care. 1981 Nov;19(11):1095–1107. doi: 10.1097/00005650-198111000-00004. [DOI] [PubMed] [Google Scholar]
- Boerstler H., Carlough T., Schlenker R. E. Administrative and policy issues in reimbursement for nursing home capital investment. J Health Polit Policy Law. 1991 Fall;16(3):553–572. doi: 10.1215/03616878-16-3-553. [DOI] [PubMed] [Google Scholar]
- Burner S. T., Waldo D. R., McKusick D. R. National health expenditures projections through 2030. Health Care Financ Rev. 1992 Fall;14(1):1–29. [PMC free article] [PubMed] [Google Scholar]
- Cohen J. W., Dubay L. C. The effects of Medicaid reimbursement method and ownership on nursing home costs, case mix, and staffing. Inquiry. 1990 Summer;27(2):183–200. [PubMed] [Google Scholar]
- Cohen J., Holahan J. An evaluation of current approaches to nursing home capital reimbursement. Inquiry. 1986 Spring;23(1):23–39. [PubMed] [Google Scholar]
- Fottler M. D., Smith H. L., James W. L. Profits and patient care quality in nursing homes: are they compatible? Gerontologist. 1981 Oct;21(5):532–538. doi: 10.1093/geront/21.5.532. [DOI] [PubMed] [Google Scholar]
- Holahan J., Cohen J. Nursing home reimbursement: implications for cost containment, access, and quality. Milbank Q. 1987;65(1):112–147. [PubMed] [Google Scholar]
- Lee A. J., Birnbaum H., Bishop C. How nursing homes behave: a multi-equation model of nursing home behavior. Soc Sci Med. 1983;17(23):1897–1906. doi: 10.1016/0277-9536(83)90167-3. [DOI] [PubMed] [Google Scholar]
- McKay N. L. The effect of chain ownership on nursing home costs. Health Serv Res. 1991 Apr;26(1):109–124. [PMC free article] [PubMed] [Google Scholar]
- Meiners M. R. An econometric analysis of the major determinants of nursing home costs in the United States. Soc Sci Med. 1982;16(8):887–898. doi: 10.1016/0277-9536(82)90208-8. [DOI] [PubMed] [Google Scholar]
- Scanlon W. J. A theory of the nursing home market. Inquiry. 1980 Spring;17(1):25–41. [PubMed] [Google Scholar]
- Schlenker R. E., Shaughessy P. W. Case mix, quality, and cost relationships in Colorado nursing homes. Health Care Financ Rev. 1984 Winter;6(2):61–71. [PMC free article] [PubMed] [Google Scholar]
- Wagner L. Flat earnings spur nursing home chains to bolster balance sheets. Mod Healthc. 1987 Mar 13;17(6):146–149. [PubMed] [Google Scholar]


