Abstract
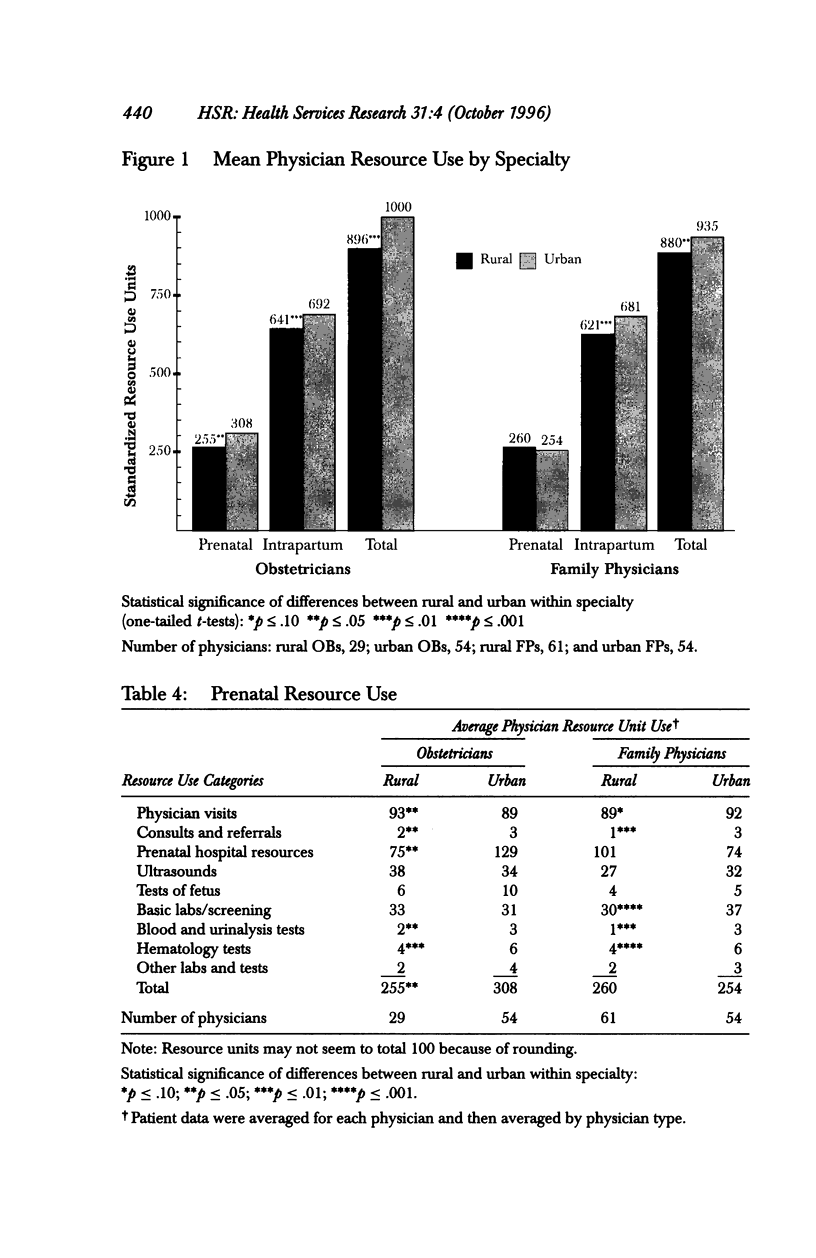
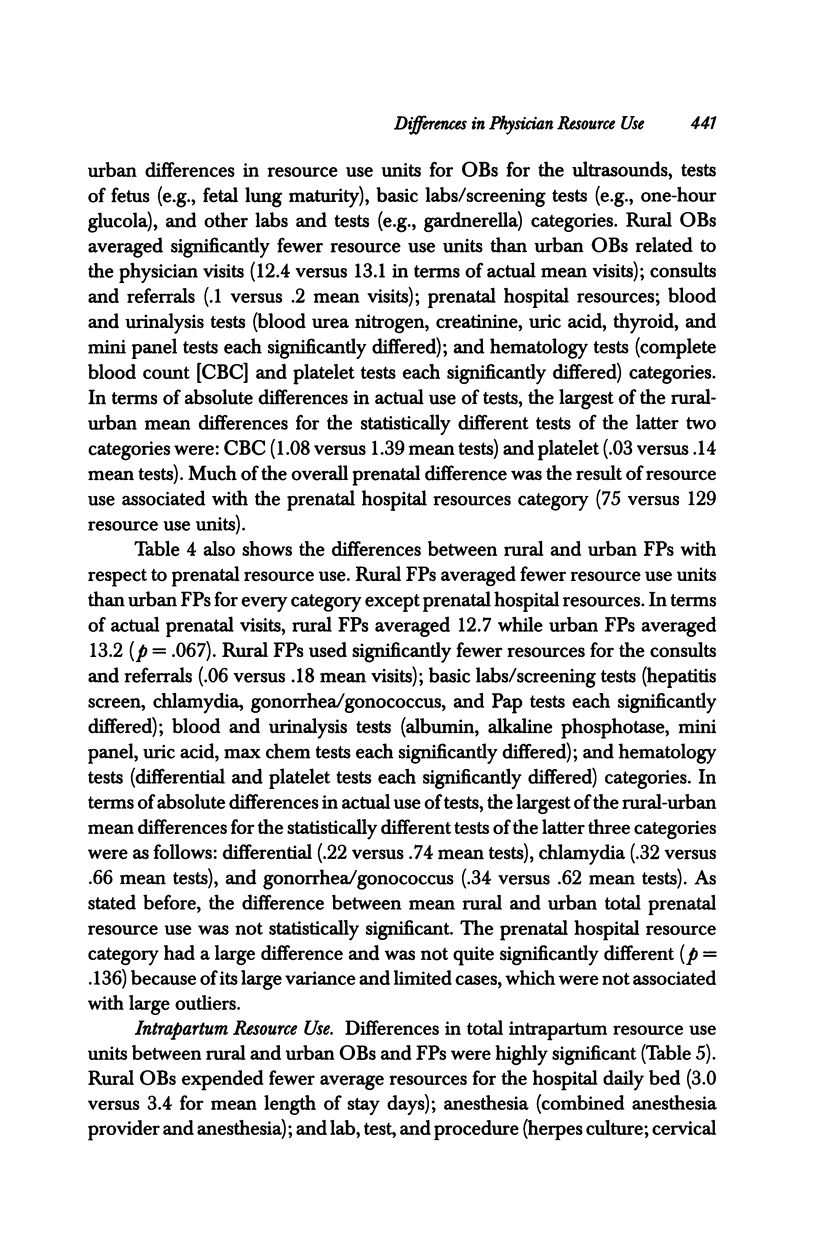
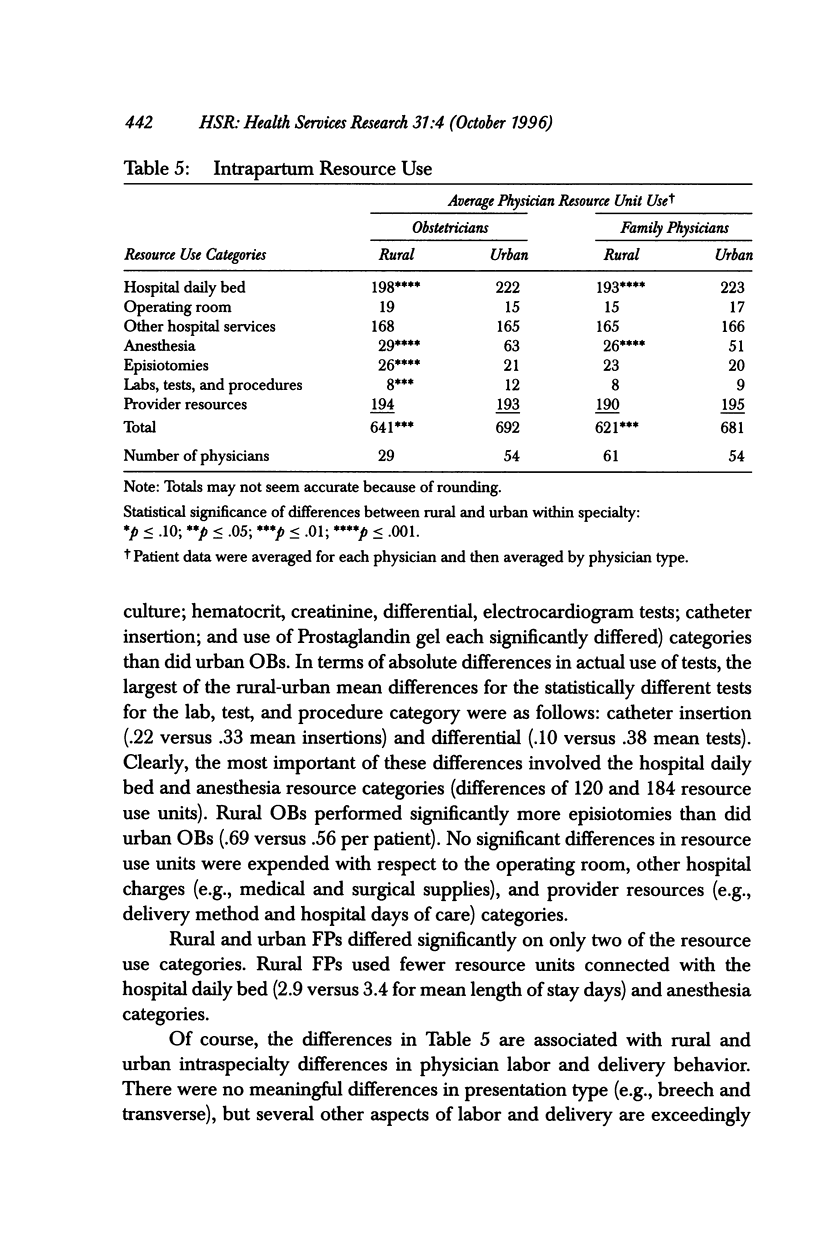
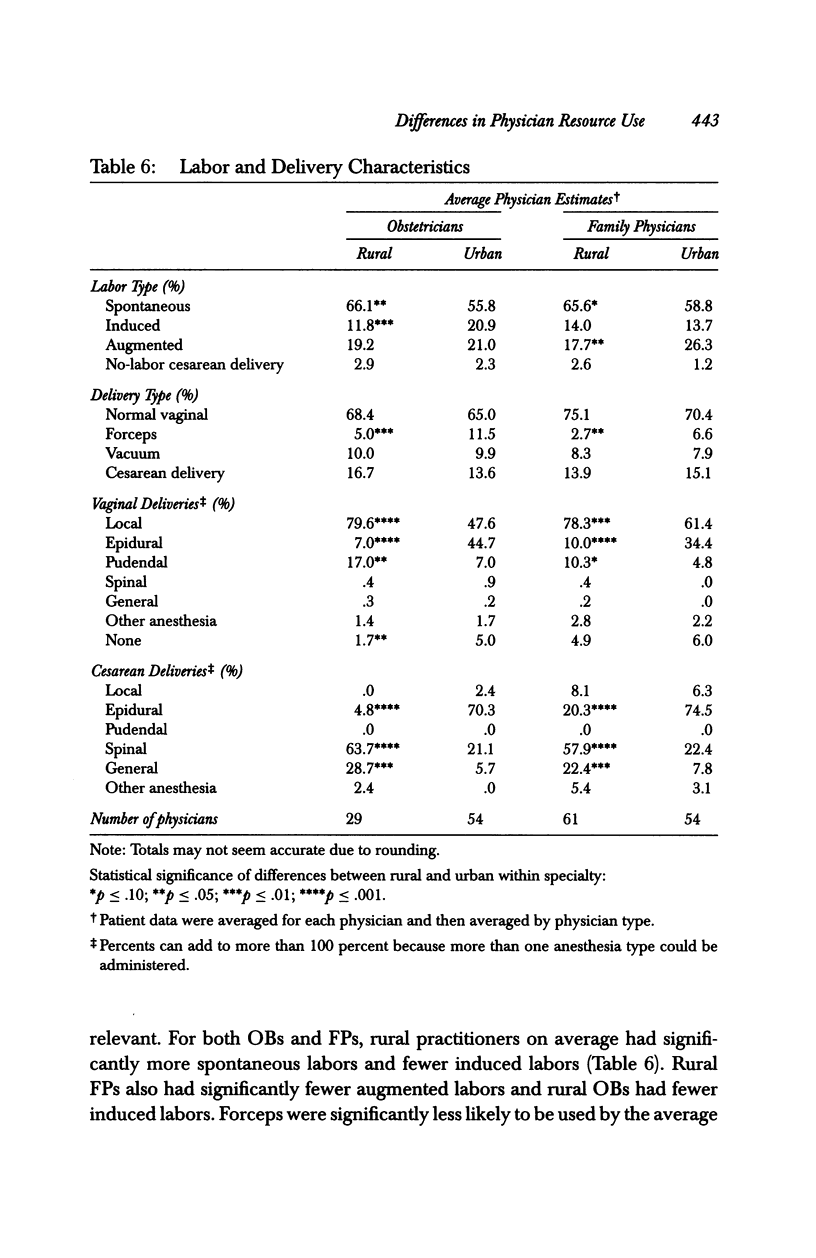
OBJECTIVE: To explore the hypothesis that rural obstetricians (OBs) and family physicians (FPs) utilized fewer resources during the care of the low-risk women who initially booked with them than did their urban counterparts of the same specialties. DATA SOURCES/STUDY DESIGN: A stratified random sample of Washington state rural and urban OBs and FPs was selected during 1989. A participation rate of 89 percent yielded 209 participating physicians. The prenatal and intrapartum medical records of a random sample of the low-risk patients who initiated care with the sampled providers during a one-year period were abstracted in detail and analyzed with the physician as the unit of analysis. Complete data for 1,683 patients were collected. Resource use elements (e.g., urine culture) were combined by standardizing them with average charge data so that aggregate resource use could be analyzed. Intraspecialty comparisons for resource use by category and overall were performed. FINDINGS/CONCLUSIONS: Results show that rural physicians use fewer overall resources in caring for nonreferred low-risk-booking obstetric patients than do their urban colleagues. Resource use unit expenditures showed the hypothesized pattern for both specialties for total, intrapartum, and prenatal care with the exception of FPs for prenatal care. Approximately 80 percent of the resource units used by each physician type were related to hospital care. No differences were shown in patterns of care for most clinically important aspects of care (e.g., cesarean delivery rates), and no evidence suggested that outcomes differed. The overall differences were due to specific components of care (e.g., fewer intrapartum hospital days and less epidural anesthesia).
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baldwin L. M., Raine T., Jenkins L. D., Hart L. G., Rosenblatt R. Do providers adhere to ACOG standards? The case of prenatal care. Obstet Gynecol. 1994 Oct;84(4):549–556. [PubMed] [Google Scholar]
- Black D. P., Fyfe I. M. The safety of obstetric services in small communities in northern Ontario. Can Med Assoc J. 1984 Mar 1;130(5):571–576. [PMC free article] [PubMed] [Google Scholar]
- Detsky A. S. Regional variation in medical care. N Engl J Med. 1995 Aug 31;333(9):589–590. doi: 10.1056/NEJM199508313330911. [DOI] [PubMed] [Google Scholar]
- Gortmaker S. L., Clark C. J., Graven S. N., Sobol A. M., Geronimus A. Reducing infant mortality in rural America: evaluation of the Rural Infant Care Program. Health Serv Res. 1987 Apr;22(1):91–116. [PMC free article] [PubMed] [Google Scholar]
- Hein H. A. Evaluation of a rural perinatal care system. Pediatrics. 1980 Oct;66(4):540–546. [PubMed] [Google Scholar]
- Kosecoff J., Kanouse D. E., Rogers W. H., McCloskey L., Winslow C. M., Brook R. H. Effects of the National Institutes of Health Consensus Development Program on physician practice. JAMA. 1987 Nov 20;258(19):2708–2713. [PubMed] [Google Scholar]
- Larson E. H., Hart L. G., Rosenblatt R. A. Rural residence and poor birth outcome in Washington state. J Rural Health. 1992 Summer;8(3):162–170. doi: 10.1111/j.1748-0361.1992.tb00348.x. [DOI] [PubMed] [Google Scholar]
- Long S. H., Marquis M. S., Harrison E. R. The costs and financing of perinatal care in the United States. Am J Public Health. 1994 Sep;84(9):1473–1478. doi: 10.2105/ajph.84.9.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nesbitt T. S., Connell F. A., Hart L. G., Rosenblatt R. A. Access to obstetric care in rural areas: effect on birth outcomes. Am J Public Health. 1990 Jul;80(7):814–818. doi: 10.2105/ajph.80.7.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramin S. M., Gambling D. R., Lucas M. J., Sharma S. K., Sidawi J. E., Leveno K. J. Randomized trial of epidural versus intravenous analgesia during labor. Obstet Gynecol. 1995 Nov;86(5):783–789. doi: 10.1016/0029-7844(95)00269-w. [DOI] [PubMed] [Google Scholar]
- Rosenblatt R. A., Hart L. G., Gamliel S., Goldstein B., McClendon B. J. Identifying primary care disciplines by analyzing the diagnostic content of ambulatory care. J Am Board Fam Pract. 1995 Jan-Feb;8(1):34–45. [PubMed] [Google Scholar]
- Rosenblatt R. A., Mayfield J. A., Hart L. G., Baldwin L. M. Outcomes of regionalized perinatal care in Washington State. West J Med. 1988 Jul;149(1):98–102. [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt R. A., Saunders G. R., Tressler C. J., Larson E. H., Nesbitt T. S., Hart L. G. The diffusion of obstetric technology into rural U.S. hospitals. Int J Technol Assess Health Care. 1994 Summer;10(3):479–489. doi: 10.1017/s0266462300006693. [DOI] [PubMed] [Google Scholar]
- Thorp J. A., Eckert L. O., Ang M. S., Johnston D. A., Peaceman A. M., Parisi V. M. Epidural analgesia and cesarean section for dystocia: risk factors in nulliparas. Am J Perinatol. 1991 Nov;8(6):402–410. doi: 10.1055/s-2007-999426. [DOI] [PubMed] [Google Scholar]
- Thorp J. A., Hu D. H., Albin R. M., McNitt J., Meyer B. A., Cohen G. R., Yeast J. D. The effect of intrapartum epidural analgesia on nulliparous labor: a randomized, controlled, prospective trial. Am J Obstet Gynecol. 1993 Oct;169(4):851–858. doi: 10.1016/0002-9378(93)90015-b. [DOI] [PubMed] [Google Scholar]
- Welch H. G., Larson E. H., Hart L. G., Rosenblatt R. A. Readmission after surgery in Washington State rural hospitals. Am J Public Health. 1992 Mar;82(3):407–411. doi: 10.2105/ajph.82.3.407. [DOI] [PMC free article] [PubMed] [Google Scholar]