Abstract
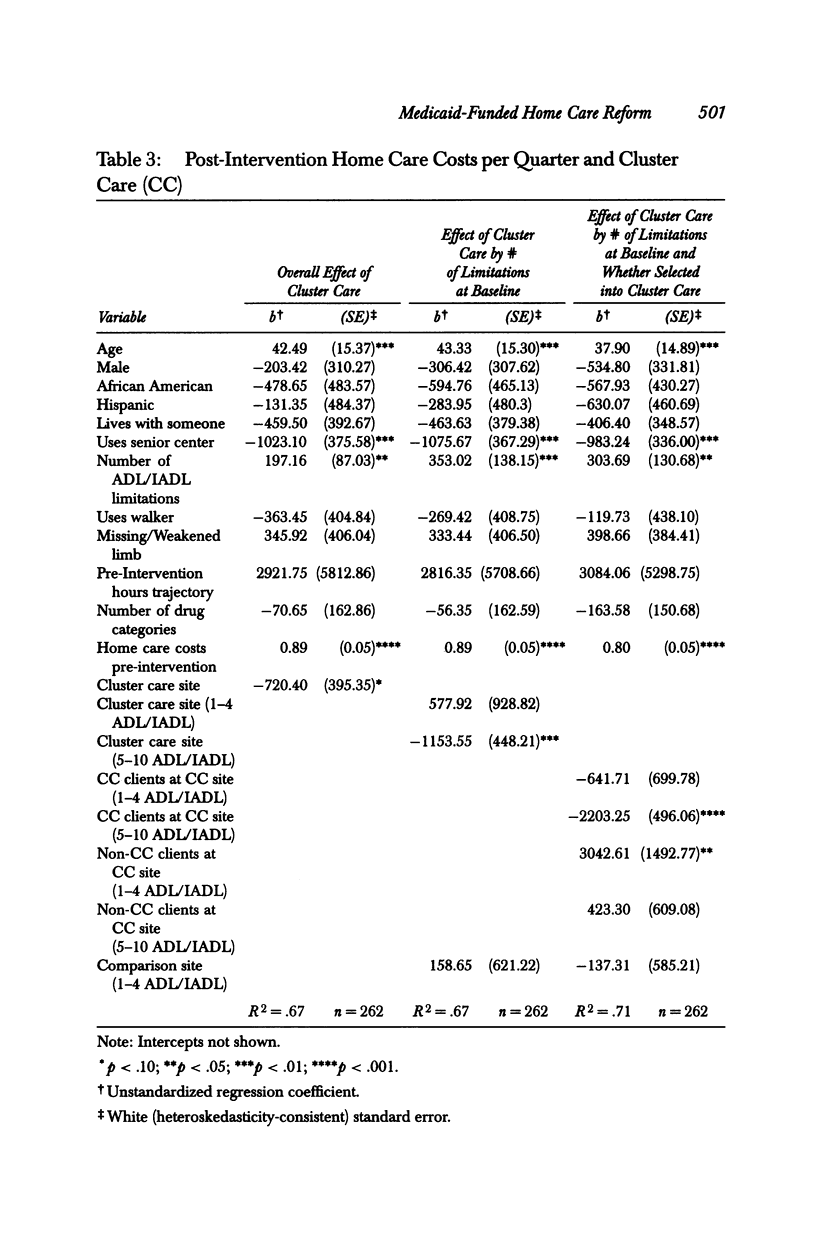
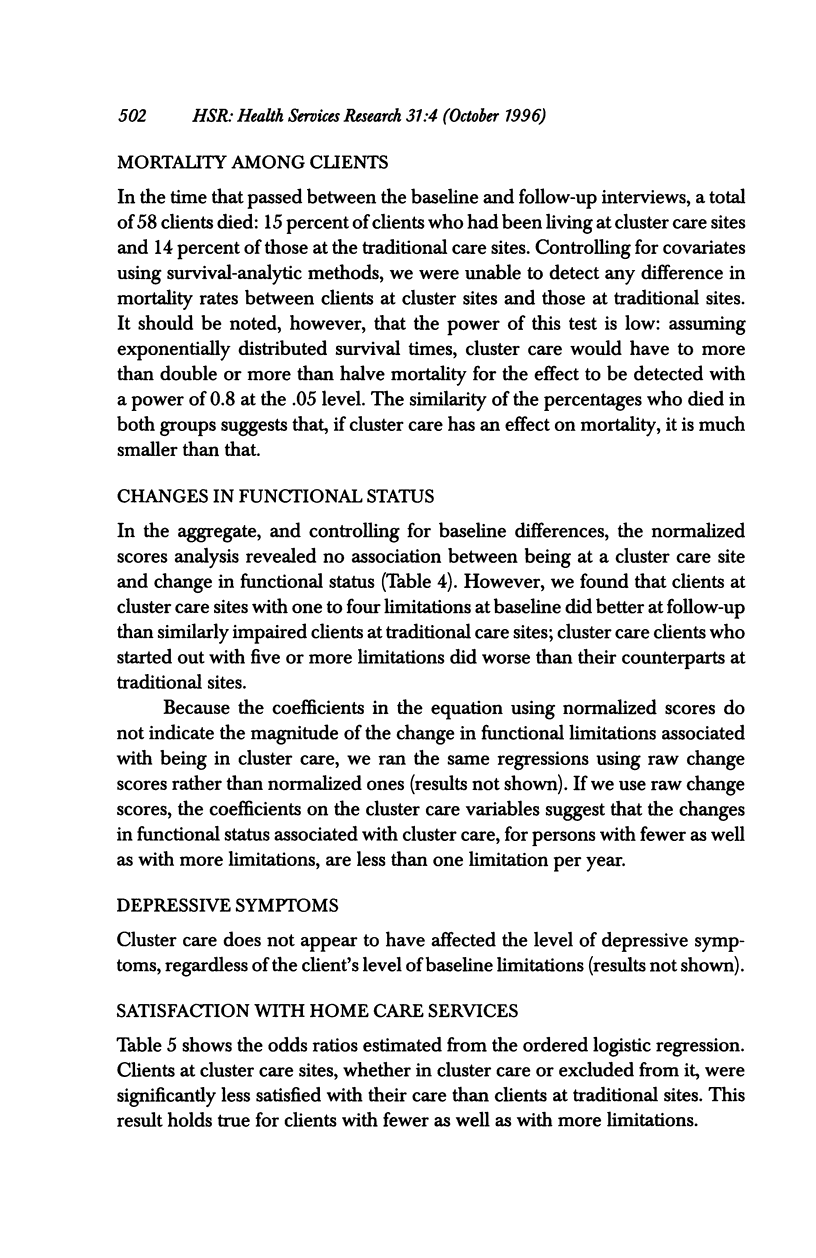
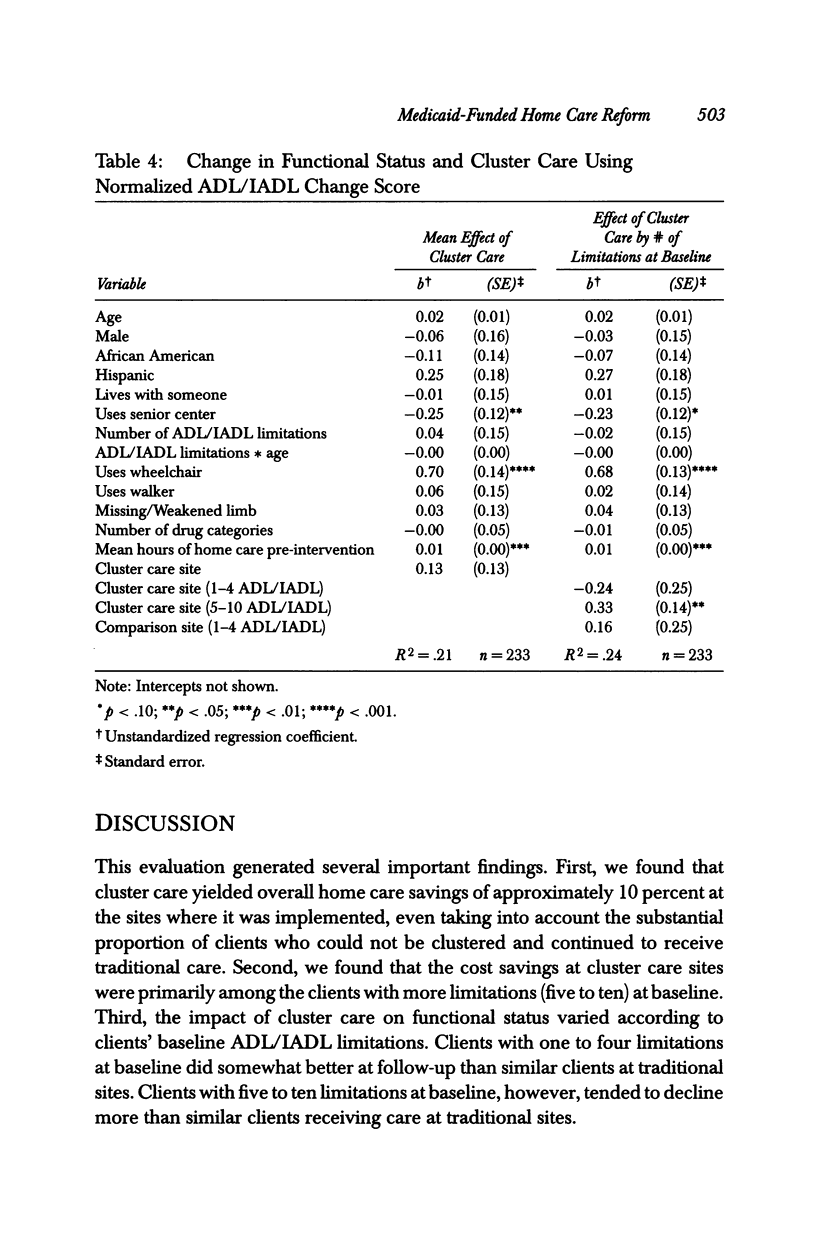
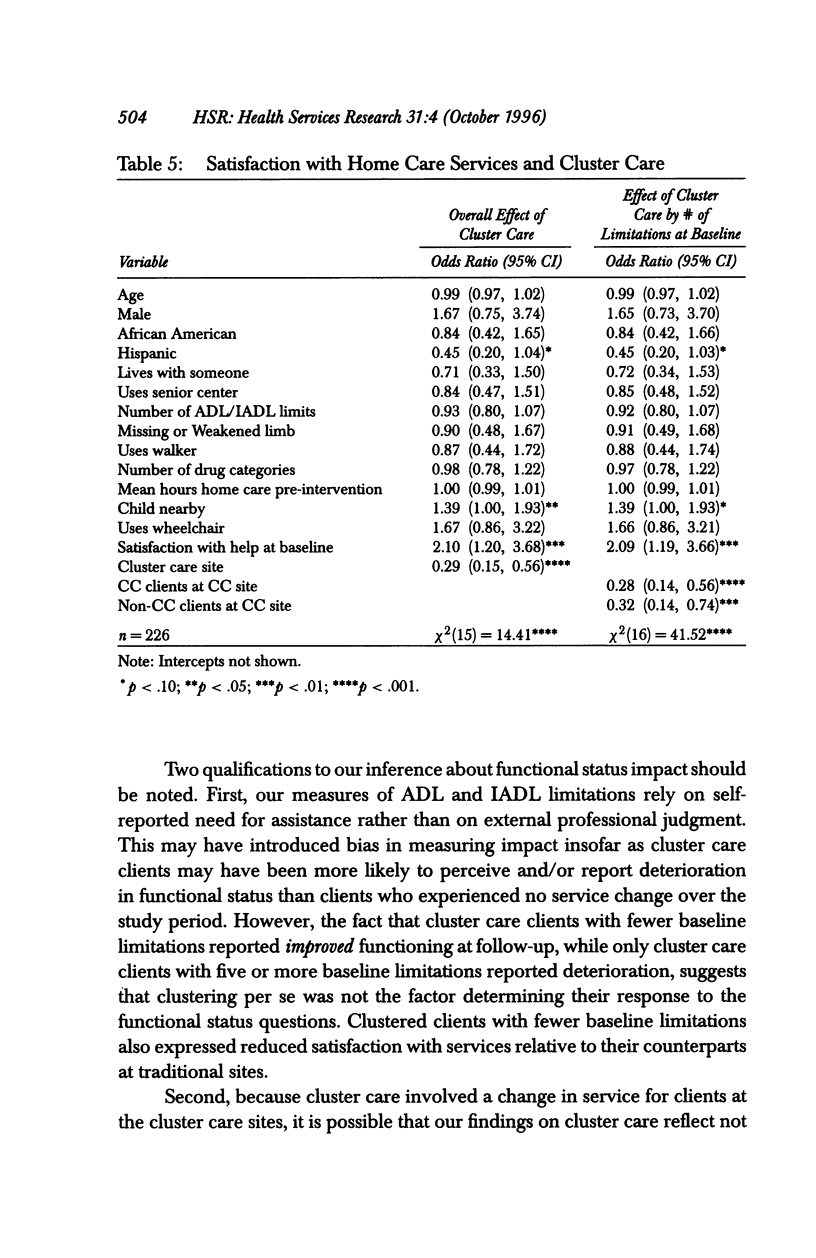
OBJECTIVES: In response to rising demand and increased costs for home care services for frail elderly and disabled Medicaid clients, New York City implemented cluster care, a shared-aide model of home care. Our objective: to evaluate the effects of cluster care on home care hours and costs, client functioning, depressive symptoms, and satisfaction. DATA SOURCES: Client interviews, conducted prior to implementation and again 16 months later; Medicaid claims records; home attendant payroll files; and vendor agency records. STUDY DESIGN: The study employed a pretest/posttest design, comparing 229 clients at the first seven demonstration sites to 175 clients at four comparison sites before and after cluster care implementation. Regression methods were used to analyze pre and post-intervention data. PRINCIPAL FINDINGS: Cluster care reduced costs by about 10 percent. Most savings occurred among the more vulnerable clients (those with five or more ADL/IADL limitations). Clients at cluster care sites who started out with fewer than five limitations appeared to decline somewhat more slowly than similarly impaired clients at comparison sites, while those with more than five ADL/IADLs tended to decline more rapidly. This difference was small-less than one limitation per year. Cluster care is associated with a significant decline in satisfaction but appears unrelated to depressive symptoms. CONCLUSIONS: Cluster care appears benign for home care clients with fewer limitations. For the more vulnerable, we recommend experimentation with low-cost interventions that might augment service and improve outcomes without reverting to traditional one-on-one care.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Joffe J. Economies of scale in home care. Home Health Care Serv Q. 1989;10(1-2):33–47. doi: 10.1300/J027v10n01_03. [DOI] [PubMed] [Google Scholar]
- Rodin J., Langer E. J. Long-term effects of a control-relevant intervention with the institutionalized aged. J Pers Soc Psychol. 1977 Dec;35(12):897–902. doi: 10.1037//0022-3514.35.12.897. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., Avorn J., Ross-Degnan D., Gortmaker S. Payment restrictions for prescription drugs under Medicaid. Effects on therapy, cost, and equity. N Engl J Med. 1987 Aug 27;317(9):550–556. doi: 10.1056/NEJM198708273170906. [DOI] [PubMed] [Google Scholar]
- Spector W. D., Katz S., Murphy J. B., Fulton J. P. The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40(6):481–489. doi: 10.1016/0021-9681(87)90004-x. [DOI] [PubMed] [Google Scholar]
- Weissert W. G. A new policy agenda for home care. Health Aff (Millwood) 1991 Summer;10(2):67–77. doi: 10.1377/hlthaff.10.2.67. [DOI] [PubMed] [Google Scholar]


