Abstract
Neuroblastoma (NB), a childhood cancer arising from the neural crest, poses significant clinical challenges, particularly in cases featuring amplification of the MYCN oncogene. Epigenetic factors play a pivotal role in normal neural crest and NB development, influencing gene expression patterns critical for tumorigenesis. This review delves into the multifaceted interplay between MYCN and known epigenetic modifications during NB genesis, shedding light on the intricate regulatory networks underlying the disease. We provide an extensive survey of known epigenetic mechanisms, encompassing DNA methylation, histone modifications, non-coding RNAs, super-enhancers (SEs), bromodomains (BET), and chromatin modifiers in MYCN-amplified (MNA) NB. These epigenetic changes collectively contribute to the dysregulated gene expression landscape observed in MNA NB. Furthermore, we review emerging therapeutic strategies targeting epigenetic regulators, including histone deacetylase inhibitors (HDACi), histone methyltransferase inhibitors (HMTi), and DNA methyltransferase inhibitors (DNMTi). We also discuss and summarize current drugs in preclinical and clinical trials, offering insights into their potential for improving outcomes for MNA NB patients.
Keywords: neuroblastoma, MYCN, epigenetics
1. Introduction
Neuroblastoma (NB), an embryonal tumor arising from the peripheral sympathetic nervous system, represents a challenging clinical entity characterized by heterogeneity in clinical presentation, prognosis, and treatment response [1]. Among the various genetic alterations observed in NB, amplification of the MYCN oncogene has emerged as an adverse prognostic genetic event. MYCN-amplification (MNA) occurs in approximately 20% of NB cases. MNA is associated with an aggressive phenotype, treatment resistance, and poor prognosis [1,2]. Treatment of high-risk NB involves intense genotoxic multiagent chemo- and radiation therapy [3,4]. About half of the high-risk patients relapse. Tragically, for survivors, genotoxic therapies can cause severe treatment-related morbidities, including hearing loss, infertility, endocrine deficiencies, and secondary cancers [5].
In recent years, the field of epigenetics has garnered significant attention in cancer research, unraveling the intricate regulatory mechanisms that dictate gene expression patterns beyond the DNA sequence itself. Epigenetic modifications, including DNA methylation, histone modifications, and chromatin remodeling, play fundamental roles in cellular development, differentiation, and disease pathogenesis [6]. Moreover, aberrant epigenetic alterations have been increasingly implicated in various cancers, providing a promising avenue for targeted therapeutic interventions [7].
In the context of MNA NB, understanding the interplay between genetic and epigenetic factors is of utmost importance. Epigenetic modifications have been recognized as crucial determinants of MYCN expression levels during neural crest development and in NB development [8]. Epigenetic modifications can indeed modulate the accessibility of transcriptional machinery to the MYCN locus, consequently influencing downstream gene networks involved in cell proliferation, differentiation, and apoptosis. Moreover, MYCN itself can regulate epigenetic processes in MNA NB. In this review, we summarize the latest advances in understanding the epigenetic dysregulation in MNA NB, and we highlight new therapeutic avenues targeting epigenetics for this high-risk pediatric malignancy.
2. Epigenetic Regulation of MYCN Expression during Neural Crest Development
2.1. Neural Crest (NC) and NB Development
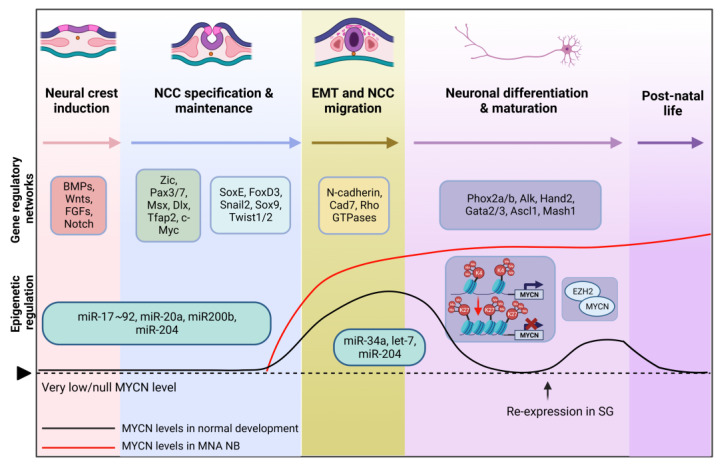
Neural crest cells (NCC) arise at the neural plate border during gastrulation and neurulation in the third week of human development. NCCs undergo a series of developmental processes, including specification, migration, differentiation, and maturation. These processes are tightly regulated by gene regulatory networks involving various transcription factors (TFs) activated by bone morphogenetic proteins (BMPs), fibroblast growth factors (FGFs), wingless-type (WNT), and Notch signaling pathways (Figure 1) [9,10,11,12]. These inductive signals from the surrounding tissues activate the expression of NCC specifiers in the neural folds and define cells with NC identity. During neurulation, NCCs undergo epithelial-to-mesenchymal transition (EMT) and migrate extensively to distant locations in the embryo [13]. Throughout their migration, NCCs continuously respond to environmental cues, giving rise to diverse lineages and cell types that contribute to specific organ systems, such as the peripheral nervous system [14,15]. Notably, NC-derived cells persist into adulthood and possess stemness properties, potentially playing important roles not only in tissue regeneration but also in the initiation of cancer [16]. Information regarding the development of the neural crest is comprehensively outlined in multiple review papers [13,15,17,18].
Figure 1.
Neural crest development. The figure highlights key gene regulatory networks shaping neural crest induction, NCC specification, migration, and differentiation. The graph illustrates varying MYCN protein expression levels during normal NCC development (black line) and in MNA NB (red line). MYCN amplification might occur during early NCC migration or sympathetic lineage specification, leading to NB formation. Epigenetic mechanisms (miRNAs, histone methylation, and chromatin remodeling) regulating MYCN expression are also captured [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37]. (SG: sympathetic ganglia). Created with Biorender.com, accessed on 3 November 2023.
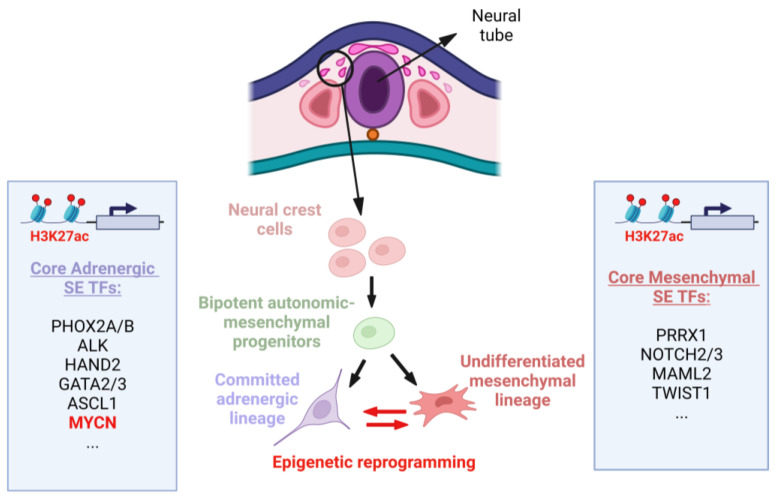
NB specifically originates from the sympathetic lineage of NCCs [1,17]. Instead of differentiating into mature sympathetic neurons, NB cells maintain a more primitive and undifferentiated state, contributing to tumor heterogeneity and resistance to differentiation-inducing therapies [2,19]. Two distinct phenotypic subpopulations can be identified: adrenergic-type (ADRN) cells committed to the sympathetic lineage and undifferentiated mesenchymal-type (MES) cells resembling NC-derived precursors (Figure 2). These subpopulations exhibit different gene expression signatures and can interconvert via epigenetic reprogramming, mimicking cells from different stages of lineage differentiation [17,18].
Figure 2.
Early stages of NB development from NCCs. NB tumors exhibit two super-enhancer (SE)-associated cell types: committed adrenergic (ADRN) and undifferentiated mesenchymal (MES) cell types, originating from bipotent progenitors. These cells can spontaneously interconvert into one another via epigenetic mechanisms. This bidirectional conversion is controlled by core regulatory circuitries, where core TFs bind to their own SEs and each other’s SEs, creating feed-forward transcriptional loops that underlie lineage identity. The main core ADRN and MES SE-associated TFs are listed in the blue boxes. SEs were identified using genome-wide profiling of histone H3 lysine 27 acetylation (H3K27ac) enhancer signature in NB tumors and cell lines [18,25]. Created with Biorender.com, accessed on 5 October 2023.
2.2. MYCN Levels during Neural Crest and MNA NB Development
One of the master regulators of NCC development is the MYCN TF. The expression levels of MYCN vary during NCC development (Figure 1). During early nervous system development, MYCN is excluded from NCC stem cells, and MYC, a paralogue of MYCN, is transcribed, maintaining the multipotent NCC progenitors [17]. Later, MYCN is expressed in the migratory and post-migratory NCCs. MYCN initially exhibits a uniform expression pattern in migrating NCCs, but then its expression is subsequently downregulated to very low levels before the cells gather to form the ganglia, with later re-expression in NC-derived lineages [26]. After migration, MYCN expression becomes specifically limited to cells that are actively engaged in neuronal differentiation. This suggests that MYCN expression is a critical factor that influences whether NCCs become neurons or adopt a non-neuronal fate [27]. Indeed, its re-expression is associated with the maintenance of neural fate and the promotion of differentiation and functionality of sympathetic neurons [17,18,20,21]. Notably, MYCN is essential for inhibiting neuronal differentiation during neurogenesis, with limited impact on progenitor cell apoptosis [3,22]. MYCN was found to be re-expressed in differentiating sympathetic ganglia (SG) following the initiation of expression of lineage-determining transcription factors (TF) such as PHOX2B and HAND2 [23,24]. However, the role of MYCN extends beyond migration and differentiation, as it also influences cell growth and apoptosis during murine sympathoadrenal (SA) development. After birth, MYCN is not expressed in the SG and is nearly entirely absent in all tissues of adult mice [24,25].
Aberrations in MYCN expression influence NC cell fate decisions, impairing the normal processes of neuronal differentiation and migration. In mice, loss of MYCN results in decreased size of the entire nervous system, along with a reduction in the number of mature neurons in the spinal ganglia [17]. Notably, enforced expression of MYCN in mouse migrating NCCs leads to the development of NB-like tumors, while its overexpression in SA progenitors is not sufficient for neoplasia [30,38]. Patients with low-risk NB do not exhibit MNA nor progression to more metastatic and invasive disease, indicating that MNA serves as an early and potentially initiating event in the development of high-risk NB tumors [4].
The importance of MYCN in NB development is supported by findings from genetically engineered animal models of NB. Transgenic mice expressing perinatal MYCN under the tyrosine hydroxylase (TH) promoter, which is active in early migrating sympathetic precursors, spontaneously develop morphologically and phenotypically similar tumors to high-risk NB in humans [20,39,40]. The development of NB in these models is dependent on MYCN dosage, as MYCN alone is sufficient to drive NB formation [19,21]. In zebrafish models, ectopic MYCN expression in sympathetic precursor cells hinders the development of chromaffin cells, leading to NB formation [21,41]. Altogether, these findings suggest that the early exposure of NCCs to elevated MYCN levels is what could play a significant role in triggering the onset of MNA NB.
2.3. Epigenetic Regulation of MYCN Expression during NC Development and Implications for MNA NB
Several epigenetic mechanisms involved in NC development are known to be disrupted in NB genesis.
MicroRNAs (miRNAs) play important regulatory roles during NC development, where they work in coordination with other regulatory mechanisms to fine-tune gene expression and ensure the proper development of NCCs into diverse cell types, including neurons. MYCN influences the expression of multiple miRNAs and is itself subject to miRNA regulation. This feedback mechanism is disrupted in NB, where upregulated levels of MYCN coincide with altered expression of specific miRNA clusters [28,29]. In normal NC development, miR-200b, miR-17~92, miR-20a, and miR-204 are known to be involved in NC induction/specification, while miR-34a, let-7, and miR-204 play roles in NCC EMT and migration (Figure 1, Table 1) [42]. Together, they contribute to NCC identity by inhibiting specific growth signaling pathways, eventually regulating key TFs such as MYCN. In the context of MNA NB, let-7, miR-34a, miR-200b, and miR-204 are tumor suppressor miRNAs found to be downregulated, while miR-17-92 and miR-20a are oncogenic miRNAs that are upregulated [29,31,32]. As MYCN levels need to be tightly controlled to ensure proper development, dysregulation in the MYCN-miRNA interplay could thereby impact the balance between cell proliferation and differentiation of NCCs, potentially leading to tumorigenesis.
Table 1.
Epigenetic mechanisms in normal NC and in MNA NB development.
| Epigenetic Mechanism | Role in Normal NC Development | Aberration in MNA NB | Citation |
|---|---|---|---|
| miR-200b | NC induction/specification | Tumor suppressor; downregulated | [28,32,42] |
| miR-17~92 | NC induction/specification | Oncogenic; upregulated | [28,29,42] |
| miR-20a | NC induction/specification | Oncogenic; upregulated | [28,29,42] |
| miR-204 | NC induction/specification, NCC EMT/migration | Tumor suppressor; downregulated | [28,42] |
| miR-34a | NCC EMT/migration | Tumor suppressor; downregulated | [28,29,31,32,42] |
| let-7 | NCC EMT/migration | Tumor suppressor; downregulated | [28,29,42] |
| Histone modifications of the MYCN gene | Shift from active H3K4me3 to repressive H3K27me3 mark for MYCN downregulation during neuronal differentiation/maturation | The active H3K4me3 mark is kept; MYCN expression is sustained | [34] |
| EZH2 | Controls the expression of genes crucial for neuronal differentiation/maturation via histone methylation, H3K27me3 is associated with gene repression | Recruitment of PRC2 by MYCN for EZH2-mediated epigenetic silencing | [35,37] |
Investigation of histone modifications at the MYCN gene between normal and NB cells during mouse sympathetic cervical ganglia (SCG) development (E11.5) revealed a failure in the shift of histone marks from active H3K4me3 (trimethylation of lysine residue K4 on histone H3) to repressive H3K27me3 (trimethylation of lysine residue K27 on histone H3) [34]. Indeed, as mentioned earlier, MYCN expression is gradually downregulated to low levels for differentiation in normal development, consistent with a change to repressive H3K27me3 marks. Therefore, a lack of proper epigenetic repression during SCG development could lead to sustained expression of MYCN, potentially resulting in uncontrolled cell proliferation and NB formation [34].
Enhancer of Zeste Homolog 2 (EZH2), a core catalytic subunit of the Polycomb Repressive Complex 2 (PRC2), is a histone methyltransferase (HMT) that represses transcription via H3K27me3 [43]. The comparison of transcriptomes between wild-type (WT) and early-stage cancer cells from TH-MYCN mice (at E13.5) demonstrated a significant downregulation of PRC2 target genes, indicated by an increase in H3K27me3 levels around their promoters. Specific inhibition of EZH2 reversed the repression of target genes and eventually suppressed in vivo tumor growth in TH-MYCN mice [35,36]. Moreover, a physical interaction between MYCN and EZH2 was reported, suggesting recruitment of PRC2 by MYCN at specific genomic loci for EZH2-mediated epigenetic silencing of target genes [35,37] (Table 1).
Collectively, these findings indicate that MNA NB initiation occurs during early migration or sympathetic lineage specification and necessitates continued perinatal expression of MYCN for tumorigenesis [20]. Persistent expression of MYCN in maturing sympathetic precursor cells can inhibit apoptotic signaling and sustain proliferation, thereby promoting NB development [21].
3. Altered Epigenetic Mechanisms in MNA Neuroblastoma
MYCN, in addition to its classical function as a TF, also plays a critical role in tumorigenesis via epigenetic regulation. In fact, MYCN has been shown to control multiple epigenetic mechanisms, including DNA methylation, histone modifications, miRNAs, and chromatin remodeling by directly regulating the transcription of epigenetic modifiers or via protein–protein interactions. The interplay between MYCN and chromatin-modifying mechanisms strongly influences disease progression and metastasis, highlighting these processes as key therapeutic vulnerabilities in MNA NB [44,45].
3.1. DNA Methylation in MNA NB
Methylation of DNA is one of several epigenetic mechanisms that cells use to alter gene expression. CpG islands (CGIs) are specific genomic regions characterized by a high frequency of cytosine–guanine (CpG) dinucleotides. These regions are often associated with gene promoters, transcription start sites, and first exons. DNA methylation at CpG islands is a crucial epigenetic mechanism implicated in cell fate determination during development, generally leading to gene silencing [45].
MYCN has been shown to bind to numerous promoters and CpG islands (CGIs) in NB, suggesting direct control of potential tumor suppressor genes via DNA methylation [6,44]. Specifically, methylation of caspase 8 (CASP8) and members of the Ras association domain family (RASSF) and protocadherin beta cluster (PCDHB) families have been extensively studied and linked to MNA [46,47,48,49]. Indeed, loss of CASP8 by methylation is believed to allow for unhinged cell proliferation and therefore contribute to MNA NB tumorigenesis [49]. However, the correlation between CASP8 methylation and MNA has been questioned by other groups [46,50].
Moreover, MYCN single-copy and MNA NB cell lines exhibit distinct promoter methylation patterns for genes like histone H3.1 (HIST1H3C) and acetyl-CoA synthetase short-chain family member 3 (ACSS3). Specifically, HIST1H3C methylation is associated with both overall and event-free survival [51]. The exception to the methylation pattern includes the hypomethylation of nuclear receptor 4A3 (NR4A3) exon 3 in MNA cells, which may be associated with a better prognosis [52], and the dual role of CD44 methylation in both MNA and non-MNA NB [53,54,55].
Various studies suggest a CpG island methylator phenotype (CIMP) in NB, which is linked to poor survival. Both Japanese and German studies showed that MNA is linked to the CIMP+ phenotype [48,56], where among others, methylation levels of PCDHB CGIs defined the CIMP+ phenotype. Giwa et al., via differential methylation analysis of MNA versus non-MNA NB (TARGET data), identified 663 differentially methylated CpGs and 14 highly methylated genes associated with MNA in NB, suggesting that MNA alters the methylation landscape in NB and that this landscape differs from that in non-MNA NB [50]. In addition, Lalchungnunga et al. performed a genome-wide methylation analysis of the TARGET study and identified five distinct DNA-methylation-based molecular subgroups, where one subgroup is strongly associated with MNA [57]. The differentially methylated regions unique to the MNA subgroup contain 291 candidate genes, including TERT (cg11625005). In addition, MNA NB showed higher TERT expression compared to non-MNA NB.
Overall, DNA methylation is a critical epigenetic mechanism involved in the development of MNA NB (Table 2). However, the relationship between MYCN and DNA methylation in NB, along with the underlying molecular mechanisms, remains largely unexplored.
Table 2.
DNA methylation patterns linked to MNA NB.
| Gene | Role | Methylation Status in MNA NB | Expression in MNA NB | Citation |
|---|---|---|---|---|
| ABCB1, CACNA1G, CD44, DUSP23, PRDM2, RBP1, CHD5, NTRK1, KRT19, PRPH, CNR1, QPCT, ASIC2, RGS5 | Involved in NB-relevant aberrant methylation | Hypermethylation | Decreased | [48] |
| CASP8 | Cell apoptosis | Hypermethylation | Decreased | [46,47,49,58] |
| CASR | Calcium-sensing receptor | Hypermethylation | Decreased | [59] |
| CD44 | Glycoprotein involved in cell–cell interactions, adhesion, and migration | Hypermethylation | Silenced | [54,60] |
|
CXCR4, GAL, LRRN1, ODC1, TWIST1, WHSC1 DDX43, PRAME, TEX14, TMEM108, NEK2, NPY |
Involved in biology of aggressive NB | Hypomethylation | Increased | [48] |
| DNAJC15, NTRK1, PYCARD | Candidate biomarker genes | Hypermethylation | Decreased | [61] |
| DUSP2, TP73, JAK2, MGMT, HPN, RB1, TDGF1 | Relevant roles in cancer biology | Hypermethylation | Increased/Decreased | [62] |
| MIR34B, MIR34C MIR124-2 | MiR-34b-3p, miR-34b-5p, miR-34c-5p, and miR-124-2-3p are tumor suppressors | Hypermethylation | Decreased | [31,63,64] |
| NR4A3 | Critical gene for neuronal development | Hypomethylation | Decreased | [52] |
| NXPH1, SOX2-OT, DLX5, TFAP2D, CAVIN3, VAX2, TERT, HHEX, KRT19, RNF207, MIRLET7BHG, CHRNE, DLX6-AS1, TMCO3 | 14 highly methylated genes in MNA NB | Hypermethylation | [50] | |
| PCDHB family | Cell–cell neural connection | Methylation | Unknown | [48] |
| RASSF family | Tumor suppressor proteins | Hypermethylation | Decreased/absent | [47] |
| TFAP2B | Transcription factor, expression associated with low-risk NB | Methylation | Decreased | [65] |
| ZAR1 | Ovary-specific maternal factor | Hypermethylation | Increased | [66] |
| ZNF206 | Transcription factor regulating embryonic stem cell gene expression and differentiation | Hypomethylation | Unknown | [67] |
| 291 genes | Candidate differentially methylated regions unique to NB subgroup associated with MNA | [57] |
3.2. Histone Modifications in MNA NB
Histone modifications, such as methylation, acetylation, phosphorylation, and sumoylation of histones, can influence the accessibility of DNA to the transcriptional machinery. Histone methylation can either activate or repress gene transcription, depending on which histone and which amino acid residue is methylated. For instance, methylation of histone H3 at lysine 4 (H3K4) is associated with gene activation, while methylation at H3K9 and H3K27 is linked to gene repression. Conversely, the addition of acetyl groups to histone tails generally results in a more open chromatin structure, facilitating increased gene transcription and is typically associated with gene activation. On the other hand, deacetylation is a hallmark of gene silencing.
3.2.1. Histone Acetylation
MYCN has been shown to impact histone acetylation, the marker of transcriptional activation [68]. Importantly, MYCN can recruit histone acetyltransferases (HAT) to maintain chromosome acetylation and thus enhance transcription, particularly of genes involved in cell cycle progression and proliferation. The HAT E1A-binding protein (EP300) plays a critical role in establishing H3K27ac marks at super-enhancers in high-risk NB. EP300 expression correlates with poor prognosis of NB patients and promotes cell proliferation in MNA NB cell lines (Table 3) [69]. EP300 regulates enhancers via interactions with a TF part of the ADRN lineage-defining core regulatory circuit (CRC) in NB, TFAP2β, and is essential for high-risk NB growth. Interestingly, EP300 interacts with MYCN and can modulate its stability via simultaneous regulation of its acetylation and ubiquitylation on Lys 199 [70]. Loss of EP300 leads to a global loss of H3K27ac marks and loss of MYCN protein expression [69].
MYCN is known to upregulate histone deacetylases (HDACs), including HDAC1/2/5 and sirtuin-1 (SIRT1), to promote gene repression and oncogenesis in both NB cell and mouse models [71,72,73]. Indeed, MYCN upregulates HDAC2 to repress the tumor suppressor miR-183 [74]. Upregulation of HDAC5 results in the transcriptional repression of tetraspanin CD9, which contributes to the invasion and metastasis of MNA NB [75]. Upregulation of SIRT1 also increases the protein stability of MYCN. SIRT1 binds to the Myc homology box I domain of MYCN, leading to MYCN phosphorylation and stabilization [72]. MYCN in complex with MIZ1 and SP1 recruits HDAC1 to the tropomyosin receptor kinase A (NTRK1) promoter and downregulates TrkA expression, which is usually associated with spontaneous regression of NB [73].
Table 3.
Regulators of histone marks in MNA NB.
| Gene | Role | Methylation/Acetylation in MNA NB | Expression in MNA NB | Citation |
|---|---|---|---|---|
| EP300 | HAT | H3K27 acetylation | Increased | [69,70] |
| HDAC2 | HDAC | Deacetylates MIR183 promoter | Increased | [74] |
| HDAC5 | HDAC | Deacetylates CD9 | Increased | [75] |
| SIRT1 | HDAC | Deacetylation of tumor suppressors | Increased | [72] |
| HDAC1 | HDAC | Deacetylates NTRK1 promoter | Unknown | [73] |
| DOT1L | HMT | H3K79 methylation | Increased | [76] |
| EZH2 | Catalytic subunit of PRC2 complex | H3K27 trimethylation | Increased | [37,55] |
| KDM4B | Histone demethylase | H3K9me3/me2 demethylation | Increased | [77] |
| PRMT5 | HMT | H3R8 and H4R3 dimethylation | Increased | [78] |
| WDR5 | Histone H3K4 presenter | H3K4 trimethylation | Increased | [79] |
3.2.2. Histone Methylation
EZH2, a subunit of PRC2, catalyzes the trimethylation of histone H3 lysine 27 (H3K27me3) at target promoters for gene silencing. MYCN directly interacts with EZH2 via the Myc homology box domain 3 [37]. MYCN was also found to interact with DOT1L, the sole known HMT catalyzing H3K79 methylation [76]. In fact, DOT1L-mediated H3K79 methylation at MYCN-responsive elements in target gene promoters is essential for MYCN-induced transcriptional activation in MNA NB cells. The authors further demonstrated that DOT1L is needed for MNA NB cell proliferation, and its suppression reduced NB tumor progression in xenograft tumor models [76].
Recently, KDM4B, a demethylase involved in histone modifications, was found to be highly expressed in MNA NB cells. KDM4B physically interacts with MYCN and prevents the accumulation of repressive H3K9me2/me3 marks at chromatin loci of target genes. Suppression of KDM4B leads to downregulation of major tumor genes, including miR-17-92a-1 cluster host gene (MIR17HG), M-phase inducer phosphatase 1 (CDC25A), SRY-box 2 (SOX2), KIT ligand (KITLG), versican (VCAN), and syndecan 1 (SDC1), while suppressing MYCN function in both NB cells and xenograft models [77]. Table 3 provides a summary of the regulators of histone methylation and acetylation linked to MNA NB.
3.2.3. Histone Phosphorylation
MYCN is known to recruit Aurora-A to chromatin in the S-phase of the cell cycle, which in turn phosphorylates histone H3 at Ser 10 and promotes the incorporation of histone H3.3 into promoters, inhibiting accumulation of RNA:DNA hybrids (R-loops) [80].
3.3. Non-Coding RNAs and MNA NB
Non-coding RNAs (ncRNAs) are a diverse group of functional RNA molecules that do not code for proteins but play essential roles in regulating gene expression and contributing to various cellular processes, development, and disease. MYCN has been found to exert its influence not only on protein-coding genes but also on non-protein-coding genes like microRNAs (miRNA) and long non-coding RNAs (lncRNAs). The deregulation of these genes, driven by MYCN, significantly contributes to the development and progression of NB [44,81]. These ncRNAs can also directly target the 3’ untranslated region (3’UTR) of MYCN mRNA or act via indirect pathways to influence tumor progression [82].
3.3.1. miRNAs
MicroRNAs (miRNAs) are small single-stranded RNA molecules that regulate gene expression by binding to target messenger RNA molecules [83]. MiRNAs can silence genes via processes like mRNA cleavage, destabilization of mRNAs, and inhibition of protein translation.
In MNA NB, MYCN is known to be predominantly a repressor of tumor suppressor miRNA expression, although several miRNAs, including the miR-17-92 cluster, were found to correlate with MYCN expression [29,84].
Several key tumor suppressor miRNAs are shown to be repressed by MYCN in the context of MNA. Indeed, miR-184 or miR-542-5p overexpression in NB xenograft models inhibited tumor growth and metastasis [29,85]. MYCN was also shown to activate critical oncogenic miRNAs in NB and other solid tumors like non-small cell lung cancer and breast cancer [86,87]. The functionally well-studied miRNAs, such as miR-9 and miR-421, are directly activated by MYCN and are thought to contribute to NB tumorigenesis [88,89].
The interaction between MYCN and miRNAs is reciprocal, as miRNAs can directly target and regulate the oncogene. In particular, miR-34a is the most extensively studied miRNA that directly regulates MYCN expression and acts as a tumor suppressor by inducing NB cell apoptosis [31,64]. MiR-506-3p was also found to regulate MYCN expression via the zinc finger PLAGL2, which binds to the MYCN promoter region [82]. Other miRNAs such as miR-15a-5p, miR-15b-5p, miR-16-5p, miR-101, miR-628-3p, and let-7 inhibit tumor progression by negatively affecting MYCN expression [90,91]. Indeed, the LIN28B–let-7–MYCN axis is known to play a critical role in sustaining the oncogenic phenotype in NB [92]. LIN28B is a protein that binds small RNA and functions as a negative regulator of let-7 miRNA tumor suppressors. LIN28B can maintain high levels of MYCN mRNA and protein levels via downregulation of let-7 miRNA in MNA but also in non-MNA NB tumors [92,93].
The interaction between MYCN and different miRNAs varies depending on their specific characteristics, and the expression of miRNAs is thereby influenced by MYCN status [45]. Indeed, a study performed on NB patients identified a set of 38 differentially expressed miRNAs between the low/intermediate and the high-risk groups [94].
MYCN direct binding to miRNAs loci at the proximal region is thought to be the mechanism for activation or repression of miRNAs in NB, as observed with the miR-17-92 cluster for example [95]. As mentioned above, MYCN also has the ability to activate DNA methyltransferases (DNMTs), which can eventually modify the promoters of miRNAs in NB. For example, miR-34b-3p, miR-34b-5p, miR-34c-5p, and miR-124-2-3p are found to be downregulated by hypermethylation in a subset of high-risk NB patients [31,63,64]. Other miRNAs such as miR-106b-5, miR-202, miR-204, let-7, miR-17-5p, and miR-26a-5p have also been reported to be regulated by MYCN in NB [33,92,96,97].
Overall, miRNAs are considered great biomarker candidates, and their modulation holds potential as a novel therapeutic strategy for NB treatment. Several reviews extensively describe the role of miRNAs in NB and their involvement in prognosis, drug response, and resistance [28,83,98]. Specific miRNAs involved in MYCN regulation in MNA NB are summarized in Table 4.
Table 4.
MYCN-related miRNAs and their function in NB.
| miRNA | Expression in MNA NB | Associated Function | Citation |
|---|---|---|---|
| let-7 | Downregulated | Tumor suppressor. Controls sympathetic neurogenesis; promotes neuronal differentiation | [29,99,100] |
| miR-7 | Upregulated | Oncogenic. Involved in cortical development and embryonic stem cell differentiation | [101,102] |
| miR-9 | Upregulated | Oncogenic. Regulates neurogenesis (neuronal migration and differentiation) | [88,103] |
| miR-15a-5p | Downregulated | Tumor suppressor. Antiangiogenic in the brain | [90,104] |
| miR-15b-5p | Downregulated | Tumor suppressor | [90] |
| miR-16-5p | Downregulated | Tumor suppressor. Antiangiogenic in the brain | [90,104] |
| miR-17-5p | Upregulated | Oncogenic. Master regulator of neurogenesis in both developmental and adult brains | [29,105] |
| miR-19a-3p | Upregulated | Oncogenic. Enriched in NPCs and downregulated during neuronal development in the adult hippocampus | [29,106] |
| miR-19b-3p | Downregulated | Tumor suppressor. Enriched in NPCs and downregulated during neuronal development in the adult hippocampus | [106,107] |
| miR-20a-5p | Upregulated | Oncogenic. Inhibits cyclin D1 level, involved in differentiation and proliferation of cortical progenitors | [29,108] |
| miR-26a | Downregulated | Tumor suppressor. Regulates neural differentiation | [92,109] |
| miR-29 (miR-29a-3p, miR-29b-3p, miR-29c) | Downregulated | Tumor suppressor. Inhibits apoptotic neural death by targeting the proapoptotic protein BCL2 | [49,101,110] |
| miR-34a | Downregulated | Tumor suppressor. Regulates neural stem/progenitor cell differentiation | [31,64,111] |
| miR-34c-5p | Upregulated/Downregulated | Oncogenic/Tumor suppressor. Regulates neural stem/progenitor cell differentiation | [29,31,64,112] |
| miR-93-5p | Downregulated | Tumor suppressor. Maintenance/proliferation/differentiation of NSCs; downregulated in mature neurons | [29,113] |
| miR-98-5p | Downregulated | Tumor suppressor | [114] |
| miR-101-3p | Downregulated | Tumor suppressor. Involved in neuronal plasticity | [91,115] |
| miR-106a-5p | Upregulated | Oncogenic | [116] |
| miR-106b-5 | Upregulated | Oncogenic. Involved in NSC proliferation and differentiation | [96,117] |
| miR-107 | Downregulated | Tumor suppressor. Involved in differentiation of neuronal cells; interacts with dicer to control the biogenesis of miR-9 | [32,118] |
| miR-124-2-3p | Downregulated | Tumor suppressor. Involved in neuronal identity; regulates adult neurogenesis | [63,119] |
| miR-145-5p | Downregulated | Tumor suppressor. Crucial for fate determination of neurons | [120,121] |
| miR-183 | Downregulated | Tumor suppressor. Regulates sensory neurons | [74,122] |
| miR-184 | Downregulated | Tumor suppressor. Involved in neural stem cell proliferation and differentiation | [85,123] |
| miR-193b-3p | Downregulated | Tumor suppressor | [124] |
| miR-200b-3p | Downregulated | Tumor suppressor. Controls postnatal forebrain neurogenesis | [32,125] |
| miR-202 | Downregulated | Tumor suppressor | [33] |
| miR-204 | Downregulated | Tumor suppressor. Involved in adult somatic stem cell maintenance | [97,126] |
| miR-335-3p | Downregulated | Tumor suppressor. Implicated in self-renewal of NSCs via inhibition of the p53 signaling pathway | [127,128] |
| miR-380-5p | Upregulated | Oncogenic | [129] |
| miR-421 | Upregulated | Oncogenic. Involved in NSC self-renewal via the PINK1/HDAC3/FOXO3 axis | [89,130] |
| miR-449 | Downregulated | Tumor suppressor. Essential for brain development; a key regulator of mitotic spindle orientation during neurogenesis | [131,132] |
| miR-488-5p | Downregulated | Tumor suppressor | [29] |
| miR-497 | Downregulated | Tumor suppressor | [133] |
| miR-542-3p | Downregulated | Tumor suppressor. Involved in neural development and astrogliogenesis differentiation | [29,134] |
| miR-542-5p | Downregulated | Tumor suppressor. Involved in neural development and astrogliogenesis differentiation | [29,134] |
| miR-628-3p | Downregulated | Tumor suppressor | [135] |
3.3.2. LncRNAs
LncRNAs are a class of RNA molecules that are longer than 200 nucleotides which are often associated with chromatin-modifying complexes. Although very little is known about the role of lncRNAs in NB, a study identified “non-coding RNA expressed in aggressive neuroblastoma” (ncRAN; also known as small nucleolar RNA host gene 16, SNHG16) and lncUSMycN, as being associated with aggressive MNA NBs and poor prognosis (Table 5) [136,137]. LncUSMycN is located at the 2p 130-kb amplicon that is co-amplified with MYCN and is found to upregulate MYCN mRNA expression via binding to NonO protein. Knocking down of lncUSMycN expression was shown to reduce MYCN at the mRNA and protein level, thereby inhibiting MNA NB cell proliferation and tumor growth in in vitro and in vivo NB models, respectively [136]. In addition, overexpression of small nucleolar RNA host gene 1 (SNHG1) is also linked to MNA NB. SNHG1 might downregulate miR338-3p, which in turn leads to PLK4 overexpression, thus promoting proliferation, migration, and invasion [138]. Another lncRNA upregulated by MYCN is the “lncRNA highly expressed in neuroblastoma 1” (lncNB1), and it is linked to poor prognosis. LncNB1 upregulates E2F1 expression by binding RPL35, which leads to the transcription of DEPDC1B [139]. In addition, neuroblastoma differentiation marker 29 (NDM29) might be downregulated in MNA NB, and overexpression of NDM29 in MNA NB cells leads to differentiation [140].
Moreover, transcribed ultraconserved regions (T-UCRs), a novel subgroup of lncRNAs, have been discovered to be abnormally expressed in NB. These RNA transcripts are highly conserved across human, rat, and mouse genomes. Specific UCR expression profiles can be correlated with prognosis in high-risk patients and MNA status in NB [84].
Furthermore, the MYCN opposite-strand (MYCNOS) lncRNA, specifically MYCNOS-01 and 02, were found to regulate MYCN protein expression [141]. MYCNOS-02 interacts with specific binding partners like Ras GTPase-activating protein 1 (G3BP1) and recruits 11-zinc finger protein (CTCF) to the MYCN promoter, resulting in increased MYCN expression. This positive regulation of MYCN by MYCNOS-02 leads to suppressed differentiation and increased growth, invasion, and metastasis of NB cells. On the other hand, silencing of MYCNOS-01 in MNA NB cell lines had a similar effect to MYCN reduction, suggesting the potential of these two lncRNAs as therapeutic targets [141,142].
3.3.3. circRNAs
Circular RNAs (circRNAs) are a type of RNA molecule where the 3′ and 5′ ends are joined together in a closed-loop structure. This circular formation is produced via a mechanism known as back-splicing, where a downstream splice donor site is joined to an upstream splice acceptor site, resulting in a circRNA molecule. They have been implicated in various cellular processes, including acting as microRNA sponges and regulating gene expression.
In a study characterizing circRNAs in NB cell lines, seven were located within MNA regions and were upregulated: hsa_circ_0003287, hsa_circ_0008083, hsa_circ_0052767, hsa_circ_0000978, hsa_circ_0117720, chr2:15467874|15567918, and hsa_circ_0008261 [41]. Importantly, has_circ_0000978 was also identified as a potential prognostic biomarker of acute myeloid leukemia resistance [143]. Investigating the global circRNA landscape in NB, Fuchs et al. highlighted a distinct circRNA expression profile in MNA NB [144]. They showed that MYCN suppresses circRNA expression via the DHX9 RNA helicase. In addition, circARID1A was identified as promoting the proliferation and survival of NB cells via its direct interaction with the KH-type splicing regulatory RNA-binding protein (KHSRP) [144]. Importantly, this circRNA is derived from the ARID1 SWI/SNF tumor suppressor gene, which is almost always mutated in MNA NB, as described in Section 3.6. below [145,146]. Together, these studies highlight the importance of MYCN regulating circRNAs and their contribution to NB pathogenesis (Table 5).
Table 5.
LncRNAs and circRNAs in MNA NB.
| Non-Coding RNA | Expression in MNA NB | Associated Function | Citation |
|---|---|---|---|
| ncRAN | Upregulated | Oncogenic | [137] |
| lncUSMycN | Co-amplified with MYCN | Oncogenic; upregulates MYCN mRNA expression via binding to NonO | [136] |
| SNHG1 | Upregulated | Oncogenic; downregulates miR338-3p, leading to PLK4 overexpression | [138] |
| lncNB1 | Upregulated | Upregulates E2F1 expression by binding RPL35, leading to transcription of DEPDC1B | [139] |
| NDM29 | Downregulated | Induces differentiation of MNA NB cells when overexpressed | [140] |
| T-UCRs (uc.347, uc.350, uc.279, uc.460, uc.379, uc.446 and uc.364) | Upregulated | Oncogenic; involved in proliferation, apoptosis, and differentiation | [84] |
| MYCNOS-01 | Co-amplified with MYCN | Oncogenic; regulates MYCN protein expression | [141,142] |
| MYCNOS-02 | Co-amplified with MYCN | Oncogenic; interacts with G3BP1 and recruits CTCF to the MYCN promoter, thereby increasing MYCN expression. Suppresses differentiation and increases growth, invasion, and metastasis of NB cells | [141] |
| circ_0003287, circ_0008083, circ_0052767, circ_0000978, circ_0117720, chr2:15467874|15567918, circ_0008261 | Upregulated | Oncogenic | [41] |
| circARID1A | Upregulated | Oncogenic; promotes proliferation and survival of NB cells via direct interaction with KHSRP | [144] |
3.4. Super-Enhancers as Epigenetic Modifiers Regulating MYCN in NB
Enhancers are DNA sequences that can increase the transcriptional activity of nearby genes. Super enhancers (SEs) have a higher density of TF binding sites compared to typical enhancers. They are particularly associated with genes that control cell fate and cell-type-specific functions. The formation of SEs involves the binding of TFs, co-activators, and chromatin regulators to the DNA. This assembly of regulatory proteins leads to a highly accessible and active chromatin state, facilitating robust and specific gene expression, including oncogenes such as MYCN [147]. As mentioned earlier in Section 2.1, NB consists of two distinct cellular identities: committed ADRN and undifferentiated MES cell types [148]. These cells can switch between each other, leading to cellular and intra-tumoral heterogeneity. Both identities are shown to be associated with a distinct SE landscape. Most NB tumors show ADRN characteristics, but some exhibit MES features, especially in metastatic and relapsed cases associated with chemotherapy resistance (Figure 2) [148].
Indeed, the activation of MYCN in NB occurs via a process known as “enhancer hijacking”, where structural rearrangements or translocations bring distal regulatory elements into proximity with other genes, resulting in enhanced expression [149]. MNA in NB involves the co-amplification of proximal enhancers driven by the noradrenergic CRC or the loss of local gene regulatory elements due to ectopic enhancer hijacking [150]. MYCN also interacts with Twist-related protein 1 (TWIST1) and Achaete-scute family bHLH TF 1 (ASCL1) at enhancers to activate developmental genes crucial for MYCN-dependent proliferation and NB tumorigenesis [151,152].
Using genome-wide profiles of H3K27ac in primary and relapsed NB patients, Gartlgruber et al. identified four epigenetic subtypes driven by SEs. Specifically, three of these subtypes are characterized by ADRN-specific signatures that align with known clinical groups: MNA, non-MNA high-risk, and non-MNA low-risk NBs [153]. The fourth subtype with MES features is linked to relapsed NB. This study also identified highly specific modules of CRC TFs associated with particular subtypes. Notably, the MNA CRC TF subtype module includes MYCN, TWIST1, SRY-box TF 11 (SOX11), and T-box TF 2 (TBX2) [153].
To summarize, MNA allows stabilization of the CRC, thereby activating the MYCN transcriptional regulatory network and promoting an immature neuroblast cell state [148,154]. Disrupting the MYCN enhancer regulatory axis and targeting SEs holds promise as therapeutic strategies in NB, offering potential avenues to inhibit oncogenic transcription and inhibit tumor growth [154,155].
3.5. Bromodomains in MNA NB
The bromodomain and extraterminal (BET) subfamily consists of proteins that possess bromodomains, which recognize and bind to acetylated lysine residues on histones. These proteins, including BRD2, BRD3, BRD4, and BRDT, play important roles in regulating gene transcription and are involved in various cellular processes linked to chromatin remodeling. BRD4 is known to have two distinct enzymatic functions: kinase and HAT activity. Indeed, BRD4 plays a crucial role in regulating transcription via the phosphorylation of various interacting partners, including RNA polymerase II (RNAPII) and MYC. BRD4 also acetylates nucleosomes and influences chromatin architecture via its HAT activity [156]. Moreover, BRD4 serves as a significant regulatory factor for active enhancers and SEs throughout the genome. It has been demonstrated that BRD4 directly controls the MYC SE in acute myeloid leukemia cells, highlighting its critical role in SE regulation. In MNA NB, the elevated levels of MYCN promote increased histone acetylation, thereby creating more binding sites for bromodomain proteins. Due to their involvement in cancer-related processes, BET proteins have garnered significant attention as potential therapeutic targets. Several small molecule inhibitors targeting BRD4 specifically have been developed and tested in preclinical and clinical studies, showing promise as anti-tumor agents in NB [157,158,159].
3.6. Chromatin Remodeling Complexes in MNA NB
Chromatin remodeling complexes depend on ATP to mobilize and restructure selected nucleosomes. These multi-subunit protein complexes can be divided into four subfamilies: switch/sucrose non-fermentable (SWI/SNF), imitation switch (ISWI), chromodomain helicase DNA-binding (CHD), and inositol 80 (INO80) chromatin remodelers. These complexes are conserved across eukaryotes and are involved in dynamic changes of nucleosome architecture, allowing better or less access to DNA by various cellular machinery, including TFs and RNA polymerases.
Mammalian SWI/SNF complexes are part of three subfamilies: canonical BAF, polybromo-associated BAF, and non-canonical BAF. Mutations or alterations in SWI/SNF subunits are often associated with cancer, including NB [145,146]. ARID1A encodes a subunit of the canonical BAF complex and is deleted on one allele in at least 87% of NB cases with loss of chromosome 1p. The chromosome 1p36 region is almost always missing in MNA NB, resulting in at least one-third of NB cases harboring haploinsufficiency for ARID1A. Using a transgenic MYCN zebrafish model of high-risk NB, researchers demonstrated that disrupting ARID1A enhances MYCN-induced cell proliferation in the SA lineage. In ARID1A homozygous mutant MNA NB cell lines, the differentiation status shifted from adrenergic to mesenchymal, resulting in increased invasiveness. This transition is orchestrated by modifications in enhancer-driven gene expression via the modification of binding sites for both BAF and PBAF complexes [146]. In line with those results, a more recent study investigated the role of SMARCE1, a BAF subunit, in MNA NB [160]. SMARCE1 is located on chromosome 17q, which is frequently gained in NB and correlates with MNA and poor prognosis. High SMARCE1 expression is found to correlate with poor prognosis and is necessary for the proliferation and survival of MNA NB cells. Moreover, not only does MYCN directly upregulate SMARCE1 transcription by binding to its promoter, but both proteins interact to regulate MYCN target genes. These results underscore the possibility for SMARCE1 to modify nucleosome structure and chromatin accessibility, aiding in the transcriptional regulation of MYCN. Altogether, targeting chromatin modifiers belonging to the SWI/SNF complexes could help restore normal gene expression patterns in MNA NB [160].
CHD5 is also encoded at 1p36, and it is frequently lost or silenced in high-risk NB [161]. CHD5 is a chromodomain-helicase-DNA-binding protein that forms a nucleosome remodeling and deacetylation (NuRD) complex. It was shown that CHD5 induces the transcription of neuronal genes and represses the transcription of Polycomb target genes by maintaining H3K27me3 [162]. CHD5 function is required for neuronal differentiation, and loss of CHD5 is often observed in high-risk NB, including MNA NB. However, this is irrespective of MYCN amplification [161].
4. Epigenetic Therapies for MNA NB
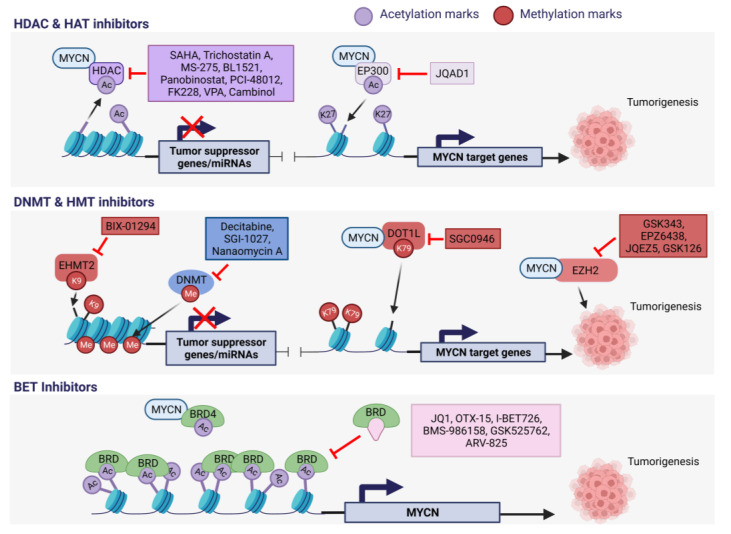
To date, there are not many studies on epigenetic drug targets for MNA NB. So far, the major classes of epigenetic drugs that have shown promise in MNA NB are histone deacetylase inhibitors (HDACi) and BET inhibitors (BETi), mostly in preclinical studies. A comprehensive summary of the existing literature on epigenetic drugs and their corresponding targets in the context of MNA NB is provided in Table 6 and illustrated in Figure 3.
4.1. HDAC and HAT Inhibitors in MNA NB
A compound screen performed by Krstic et al. revealed that NB cells are vulnerable to various classes of epigenetic regulators, and they showed that C646, a CBP/p300 HAT inhibitor, is specifically effective in reducing the viability of NB cells with MNA [163].
As already mentioned above, MNA in NB leads to the suppression of tumor suppressor genes via the recruitment of DNMTs and increased expression of HDACs. Promising preclinical studies using HDAC inhibitors in the TH-MYCN NB mouse model have been conducted. Indeed, a positive feedback loop between MYCN and the HDAC SIRT1 has been described, and treatment with the SIRT1 inhibitor cambinol was able to reduce tumorigenesis in the transgenic NB model [72]. Additionally, trichostatin A, another HDAC inhibitor, restored the expression of the differentiation protein transglutaminase 2 (TG2), usually repressed by MYCN in NB cells, resulting in reduced tumor volume in the same mouse model [164].
Other HDAC inhibitors, such as MS-275, BL1521, and vorinostat (SAHA), were shown to decrease the cell viability of several NB cell lines [165,166,167]. Specifically, SAHA treatment is more efficient on cell lines carrying MNA and is extensively studied in clinical trials alone or in combination with other drugs. It is the first HDACi that has been approved by the US Food and Drug Administration (FDA), on 6 October 2006, for the treatment of cutaneous T cell lymphoma [165,168]. Together with panobinostat, which is also FDA-approved, they have successfully completed phase II of clinical trials in NB patients [169].
Other drugs targeting HDAC1/2/8, which are associated with poor prognosis in NB, have sparked interest [170]. In fact, treatment with a small-molecule inhibitor of HDAC8 showed great inhibitory activity against NB growth in vitro and in vivo and enhanced retinoic-acid-mediated differentiation [170].
Romidepsin (FK228), an HDAC1/2i FDA-approved drug, has been shown to be specifically potent in MNA NB cells by increasing histone acetylation and thereby cell death via caspase-dependent apoptosis [171]. Further, the grainyhead-like 1 (GRHL1) gene was identified as an early response gene following HDACi treatment, which is usually repressed by MYCN via HDAC3. This TF, conserved throughout evolution, plays a crucial role in the development of the nervous system in Drosophila [172]. Importantly, high levels of GRHL1 in NB tumors correlate with event-free patient survival and favorable tumor biology [172].
One HAT inhibitor, JQAD1, has been recently investigated in pre-clinical trials on MNA NB cells [69]. JQAD1 is a proteolysis-targeting chimera (PROTAC) compound, developed to selectively degrade the HAT EP300. The role of EP300 in MNA NB is discussed in Section 3.2.1. The small innovative PROTAC degrader showcases a time-dependent depletion of EP300, resulting in rapid loss of MYCN expression and apoptosis of NB cells. Importantly, JQAD1 demonstrates low toxicity towards healthy cells while exerting growth-inhibitory effects of NB tumor xenografts [69].
Altogether, these findings highly suggest that targeting HDACs and, to a lesser extent, HATs, could be a potential approach to treat MNA NB.
4.2. HMT Inhibitors in MNA NB
As mentioned in Section 2.3 and Section 3.2.2, the HMT EZH2 is a protein of major importance during NB development. EZH2 levels are significantly higher in MNA cells than in non-MNA cells and this leads to the inactivation of a tumor suppressor program in NB [55]. Multiple studies have provided evidence supporting the therapeutic validity of S-adenosyl-methionine (SAM)-competitive EZH2 inhibitors in NB. SAM is a methyl donor for catalytic reactions of HMTs. Overall, inhibiting EZH2 directly via the occupation of the site for S-adenosyl-L-methionine (SAM) in the EZH2′s binding pocket inhibits MNA NB cell and tumor growth.
For example, GSK343 significantly reduced tumor growth in a MNA xenograft mouse model without noticeable toxicity [173]. Nonetheless, GSK343 is confined to pre-clinical use due to its inadequate pharmacokinetic characteristics [174]. Tazemetostat (EPZ6438) is an FDA-approved drug with high selectivity towards EZH2, which demonstrates a significant reduction in tumor weight in the TH-MYCN mouse model with no related adverse effect [35]. GSK126 also showed growth-inhibitory effects in in vitro and in vivo MNA NB models [55,175], but phase II clinical trials were halted due to insufficient efficacy in cancer patients [176]. Lastly, the effect of GSK126 was tested in combination with another EZH2 inhibitor, JQEZ5. The combination increased apoptosis in MNA cells, and JQEZ5 alone was able to significantly reduce tumor volume in an MNA xenograft mouse model [55].
In an immunology-related study, Seier and al. suggested exploring the use of H3K9 euchromatic histone-lysine methyltransferase (EHMT) inhibitors in combination with EZH2 inhibitors as an immunomodulation strategy for MNA NB treatment. Essentially, EHMT1 and EHMT2 were identified as key epigenetic factors involved in the malignancy of MNA NB and suppressors of interferon signaling. Inhibiting EHMT enhances the expression of Th1-chemokines, therefore facilitating T-cell infiltration into the tumor microenvironment and improving responsiveness to immune checkpoint blockade therapy [177]. Indeed, BIX-01294, an EHMT2 inhibitor, was shown to specifically decrease global H3K9me2 levels [178]. EHMT2 inhibition not only restrains the proliferation of NB cells but also triggers their apoptosis. BIX-01294 impedes MNA NB cell motility and invasion while concurrently suppressing the expression of the MYCN oncogene. Moreover, EHMT2 inhibition was found to synergize with doxorubicin, further hampering cell proliferation [178].
4.3. BET Inhibitors in MNA NB
Over the last few years, targeting BET family proteins has emerged as an eminent strategy in the treatment of cancers and other diseases. These proteins have a close association with the regulation of the MYC oncogene, making BET inhibitors effective in MYC-dependent cancers. By reducing the expression of oncoproteins like MYC, they effectively hinder the growth of malignant cells [179]. To date, targeting MYCN in MNA NB with BET inhibitors has been tested in preclinical and clinical studies. Via high-throughput pharmacological screening of more than 650 cancer cell lines, it was discovered that MNA strongly predicts the cytotoxic response to the prototypic BRD4 inhibitor, JQ1 [180]. JQ1 disrupts the recruitment of BRD4 to the MYCN canonical promoter by competitively binding to acetyl lysine sites, resulting in the downregulation of MYCN and its transcriptional outputs. In NB cells, JQ1 treatment leads to cell cycle arrest, apoptosis, and increased differentiation. Importantly, cell lines harboring MNA were found to be more sensitive to JQ1 than the non-amplified ones. Promising results were also observed in in vivo studies using MNA NB xenograft models, showing a significant decrease in tumor volume and increased overall survival without noticeable toxicity [180,181].
Figure 3.
Epigenetic drug targets explored for MNA NB. In the realm of epigenetic regulation, inhibitors targeting three distinct epigenetic mechanisms: DNA methylation, histone methylation or acetylation, and epigenetic readers have been investigated in pre-clinical or clinical trials for MNA NB [35,55,69,72,164,165,166,167,168,169,171,173,174,175,177,178,180,181,182,183,184,185,186]. Created with Biorender.com, accessed on 3 November 2023.
Building upon these findings, three JQ1 derivatives (OTX015, I-BET726, and BMS-986158) are currently under investigation, with BMS-986158 currently entering phase I in clinical trials (NCT03936465). OTX015, an orally available inhibitor of BRD2/3/4, demonstrates potent inhibition of tumor growth and increased overall survival in MNA NB cells and xenograft models. OTX015 has been found to exhibit specific activity against MYCN target genes, and this activity is correlated with high levels of MYCN expression and MNA in several NB cell lines [182].
Another small molecule BETi, GSK525762, exhibits anti-proliferative effects and cytotoxicity in NB cell models regardless of MYCN status, suggesting alternative mechanisms of action. A phase I study involving hematological and solid tumor cancers has shown therapeutic activity and tolerability of GSK525762, paving the way for potential translation to NB clinical studies [183]. However, the predictive value of MYCN overexpression for therapeutic response to GSK525762 remains unclear.
Additionally, preclinical studies exploring combinations of BET inhibitors with other therapeutic agents, such as phosphoinositide 3-kinase (PI3K), cyclin-dependent kinase 7 (CDK7), mitogen-activated protein kinase (MEK), HDAC, and Aurora A inhibitors, have shown synergistic effects, and potential to overcome resistance, and reduce treatment-related toxicities [158,159,187,188]. These combinatorial approaches hold promise in maximizing treatment efficacy and addressing concerns regarding drug resistance and lack of specificity associated with genotoxic treatments.
4.4. DNA Methyltransferase Inhibitors in MNA NB
Only very few hypomethylating agents have been tested so far in preclinical and phase I clinical trials against NB. Decitabine and 5-azacytidine are DNMT inhibitors (DNMTi) primarily used in the treatment of myelodysplastic syndromes (MDS). Decitabine was found to epigenetically activate miR-34a when combined with retinoic acid, resulting in MYCN downregulation in acute myeloid leukemia patients and cultured cells [184]. This is particularly interesting since miR-34a is a tumor suppressor that is downregulated in the context of MNA NB [31,64]. Decitabine was part of three phase I clinical trials involving NB patients and is typically used in combination with chemotherapy to enhance its effectiveness. However, when combined with doxorubicin, it seemed that doses of decitabine that could have a substantial clinical impact were associated with poor tolerance [189].
Recently, two less toxic DNMTi, SGI-1027 and nanaomycin A, displayed enhanced NB cell death when combined with doxorubicin, compared to doxorubicin alone. Even though this effect was MYCN-independent, cell lines harboring MNA were at least 20 times more sensitive to the DNMT3b inhibitor nanaomycin A [185]. In line with this finding, retinoic acid treatment of MNA NB cells was shown to downregulate DNMT3b and upregulate miR-26a/b, a DNMT targeting miRNA normally repressed by MYCN [186]. Therefore, these results suggest that the downregulation of DNMTs leading to demethylation and reactivation of specific genes and miRNAs might offer new alternatives of specific treatment against MNA NB.
A table showcasing the comprehensive range of epigenetic drugs currently being explored in preclinical and clinical trials for the treatment of MNA NB is summarized in Table 6.
Table 6.
Drugs and associated epigenetic targets in the context of MNA NB.
| Name | Drug Target in NB | Effect on MYCN in MNA NB | Clinical Status | Citation |
|---|---|---|---|---|
| ARV-825 | BRD4 inhibitor | Downregulation | Pre-clinical | [190] |
| BIX-01294 | EHMT2 (HMT) inhibitor | Downregulation | Pre-clinical | [178] |
| BL1521 | Pan-HDAC inhibitor | Downregulation | Pre-clinical | [166,191] |
| BMS-986158 | BRD4 inhibitor | Not specifically characterized | Pre-clinical and clinical Phase I:
|
[169] |
| Cambinol | SIRT1 (HDAC) inhibitor | Not specifically characterized | Pre-clinical | [72] |
| Decitabine (5-Azacytidine) | DNMT 1 inhibitor | Not specifically characterized | Pre-clinical and clinical Phase I:
|
[184,192] |
| Entinostat (MS-275) | HDAC I inhibitor | Downregulation | Pre-clinical | [167] |
| GSK343, Tazemetostat (EPZ6438), JQEZ5, GSK126 | EZH2 inhibitors | Downregulation (GSK343), others not specifically characterized | Pre-clinical and clinical Phase II (EPZ6439):
|
[35,55,173,175,193] |
| I-BET726 (GSK726) | BRD4 inhibitor | Downregulation | Pre-clinical | [194] |
| JQ1/OTX-015 | BRD4 inhibitor | Downregulation | Pre-clinical | [159] |
| JQAD1 | EP300 (HAT) inhibitor | Downregulation | Pre-clinical | [69] |
| Molibresib (GSK525762, I-BET762) | BRD2/3/4 | Downregulation | Pre-clinical and clinical Phase I:
|
[195] |
| Panobinostat | Pan-HDAC inhibitor | Downregulation | Pre-clinical and clinical Phase II:
|
[159] |
| PCI-48012 | HDAC 8 inhibitor | Downregulation | Pre-clinical | [170] |
| Romidepsin (FK228) | HDAC I inhibitor | Not specifically characterized | Pre-clinical | [171] |
| SGC0946 | DOT1L (HMT) inhibitor | Unknown | Pre-clinical | [76] |
| SGI-1027, Nanaomycin A | DNMT1/3 inhibitors | Not specifically characterized | Pre-clinical | [185] |
| Trichostatin A | HDAC I/II inhibitor | Downregulation | Pre-clinical | [164] |
| Valproic acid (VPA) | HDAC I inhibitor | Downregulation | Pre-clinical and clinical Phase I:
|
[196] |
| Vorinostat (SAHA) | HDAC I inhibitor | Downregulation | Pre-clinical and clinical Phase I:
Phase II:
|
[165] |
5. Conclusions
Half of the children with high-risk NB do not respond to current treatments and relapse. Genotoxic chemotherapy is the mainstay of therapy for high-risk NB as we lack targeted treatments for this aggressive pediatric malignancy. Therefore, better and less toxic treatments are desperately needed. Targeting epigenetic machinery is a promising approach as MYCN regulates epigenetic processes. Epigenetic dysregulation is a hallmark of cancer, including NB, and contributes to NB development, tumor growth, and progression. By specifically targeting the aberrant epigenetic modifications, epigenetic drugs have the potential to restore normal gene expression patterns, inhibit tumor growth, and overcome drug resistance. The major classes of epigenetic drugs that have so far shown promise in MNA NB are histone deacetylase inhibitors and BET inhibitors, with a more recent focus on drug combination therapies.
Epigenetic drugs offer the advantage of potentially greater specificity, targeting cancer cells while minimizing damage to normal cells. They can potentially enhance the efficacy of conventional chemotherapy and reduce the reliance on highly toxic agents, thereby mitigating some of the side effects associated with genotoxic treatments in young patients. Additionally, exploring epigenetic drugs in high-risk NB may provide alternative treatment options for patients who do not respond well to standard chemotherapy or who experience disease relapse. However, further research and clinical trials are needed to establish their safety, efficacy, and optimal use in the context of high-risk NB. Efforts are also being made to identify biomarkers that can help predict patient response to epigenetic drugs and guide personalized treatment decisions.
Moving forward, further research into novel treatment targets involving epigenetic-related molecules and their interactions with MYCN holds promise. By focusing on these avenues, we can advance our understanding and potentially discover more effective therapies for MYCN-driven NB.
Author Contributions
Conceptualization, S.E., S.M.C. and M.H.; writing—original draft preparation, S.E. and S.M.C.; writing—review and editing, M.H.; visualization, S.E.; supervision, M.H.; funding acquisition, S.M.C. and M.H. The authors S.E. and S.M.C. contributed equally to this work. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research was funded by Science Foundation Ireland and Children’s Health Ireland via the Precision Oncology Ireland grant 18/SPP/3522, Pathological Society of Great Britain and Ireland Intercalated Degree Award grant ID 0322 02, and with the financial support of Children’s Health Foundation and under the management of Science Foundation Ireland under the Frontiers for the Future Programme Grant Number 21/FFP-P/10130.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Nakagawara A., Li Y., Izumi H., Muramori K., Inada H., Nishi M. Neuroblastoma. Jpn. J. Clin. Oncol. 2018;48:214–241. doi: 10.1093/jjco/hyx176. [DOI] [PubMed] [Google Scholar]
- 2.Westermark U.K., Wilhelm M., Frenzel A., Henriksson M.A. The MYCN Oncogene and Differentiation in Neuroblastoma. Semin. Cancer Biol. 2011;21:256–266. doi: 10.1016/j.semcancer.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Liu Z., Chen S.S., Clarke S., Veschi V., Thiele C.J. Targeting MYCN in Pediatric and Adult Cancers. Front. Oncol. 2020;10:623679. doi: 10.3389/fonc.2020.623679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matthay K.K., Maris J.M., Schleiermacher G., Nakagawara A., Mackall C.L., Diller L., Weiss W.A. Neuroblastoma. Nat. Rev. Dis. Primers. 2016;2:16078. doi: 10.1038/nrdp.2016.78. [DOI] [PubMed] [Google Scholar]
- 5.Friedman D.N., Henderson T.O. Late Effects and Survivorship Issues in Patients with Neuroblastoma. Children. 2018;5:107. doi: 10.3390/children5080107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Domingo-Fernandez R., Watters K., Piskareva O., Stallings R.L., Bray I. The Role of Genetic and Epigenetic Alterations in Neuroblastoma Disease Pathogenesis. Pediatr. Surg. Int. 2013;29:101–119. doi: 10.1007/s00383-012-3239-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatziapostolou M., Iliopoulos D. Epigenetic Aberrations during Oncogenesis. Cell. Mol. Life Sci. 2011;68:1681–1702. doi: 10.1007/s00018-010-0624-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rezaei O., Honarmand Tamizkar K., Hajiesmaeili M., Taheri M., Ghafouri-Fard S. Non-Coding RNAs Participate in the Pathogenesis of Neuroblastoma. Front. Oncol. 2021;11:617362. doi: 10.3389/fonc.2021.617362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marchant L., Linker C., Ruiz P., Guerrero N., Mayor R. The Inductive Properties of Mesoderm Suggest That the Neural Crest Cells Are Specified by a BMP Gradient. Dev. Biol. 1998;198:319–329. doi: 10.1016/S0012-1606(98)80008-0. [DOI] [PubMed] [Google Scholar]
- 10.Streit A., Berliner A.J., Papanayotou C., Sirulnik A., Stern C.D. Initiation of Neural Induction by FGF Signalling before Gastrulation. Nature. 2000;406:74–78. doi: 10.1038/35017617. [DOI] [PubMed] [Google Scholar]
- 11.Saint-Jeannet J.P., He X., Varmus H.E., Dawid I.B. Regulation of Dorsal Fate in the Neuraxis by Wnt-1 and Wnt-3a. Proc. Natl. Acad. Sci. USA. 1997;94:13713–13718. doi: 10.1073/pnas.94.25.13713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsarovina K., Schellenberger J., Schneider C., Rohrer H. Progenitor Cell Maintenance and Neurogenesis in Sympathetic Ganglia Involves Notch Signaling. Mol. Cell Neurosci. 2008;37:20–31. doi: 10.1016/j.mcn.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Simões-Costa M., Bronner M.E. Establishing Neural Crest Identity: A Gene Regulatory Recipe. Development. 2015;142:242–257. doi: 10.1242/dev.105445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barlow A.J., Dixon J., Dixon M.J., Trainor P.A. Balancing Neural Crest Cell Intrinsic Processes with Those of the Microenvironment in Tcof1 Haploinsufficient Mice Enables Complete Enteric Nervous System Formation. Human Mol. Genet. 2012;21:1782–1793. doi: 10.1093/hmg/ddr611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Muñoz W.A., Trainor P.A. Chapter One—Neural Crest Cell Evolution: How and When Did a Neural Crest Cell Become a Neural Crest Cell. In: Trainor P.A., editor. Current Topics in Developmental Biology. Volume 111. Neural Crest and Placodes; Academic Press; Cambridge, MA, USA: 2015. pp. 3–26. [DOI] [PubMed] [Google Scholar]
- 16.Li H.-Y., Say E.H.M., Zhou X.-F. Isolation and Characterization of Neural Crest Progenitors from Adult Dorsal Root Ganglia. Stem Cells. 2007;25:2053–2065. doi: 10.1634/stemcells.2007-0080. [DOI] [PubMed] [Google Scholar]
- 17.Otte J., Dyberg C., Pepich A., Johnsen J.I. MYCN Function in Neuroblastoma Development. Front. Oncol. 2021;10:624079. doi: 10.3389/fonc.2020.624079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ponzoni M., Bachetti T., Corrias M.V., Brignole C., Pastorino F., Calarco E., Bensa V., Giusto E., Ceccherini I., Perri P. Recent Advances in the Developmental Origin of Neuroblastoma: An Overview. J. Exp. Clin. Cancer Res. 2022;41:92. doi: 10.1186/s13046-022-02281-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ruiz-Pérez M.V., Henley A.B., Arsenian-Henriksson M. The MYCN Protein in Health and Disease. Genes. 2017;8:113. doi: 10.3390/genes8040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomolonis J.A., Agarwal S., Shohet J.M. Neuroblastoma Pathogenesis: Deregulation of Embryonic Neural Crest Development. Cell Tissue Res. 2018;372:245–262. doi: 10.1007/s00441-017-2747-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Johnsen J.I., Dyberg C., Wickström M. Neuroblastoma-A Neural Crest Derived Embryonal Malignancy. Front. Mol. Neurosci. 2019;12:9. doi: 10.3389/fnmol.2019.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen J., Guan Z. Function of Oncogene Mycn in Adult Neurogenesis and Oligodendrogenesis. Mol. Neurobiol. 2022;59:77–92. doi: 10.1007/s12035-021-02584-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincentz J.W., VanDusen N.J., Fleming A.B., Rubart M., Firulli B.A., Howard M.J., Firulli A.B. A Phox2- and Hand2-Dependent Hand1 Cis-Regulatory Element Reveals a Unique Gene Dosage Requirement for Hand2 during Sympathetic Neurogenesis. J. Neurosci. 2012;32:2110–2120. doi: 10.1523/JNEUROSCI.3584-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ke X.-X., Zhang D., Zhao H., Hu R., Dong Z., Yang R., Zhu S., Xia Q., Ding H.-F., Cui H. Phox2B Correlates with MYCN and Is a Prognostic Marker for Neuroblastoma Development. Oncol. Lett. 2015;9:2507–2514. doi: 10.3892/ol.2015.3088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang M., Weiss W.A. Neuroblastoma and MYCN. Cold Spring Harb. Perspect. Med. 2013;3:a014415. doi: 10.1101/cshperspect.a014415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khudyakov J., Bronner-Fraser M. Comprehensive Spatiotemporal Analysis of Early Chick Neural Crest Network Genes. Dev. Dyn. 2009;238:716–723. doi: 10.1002/dvdy.21881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wakamatsu Y., Watanabe Y., Nakamura H., Kondoh H. Regulation of the Neural Crest Cell Fate by N-Myc: Promotion of Ventral Migration and Neuronal Differentiation. Development. 1997;124:1953–1962. doi: 10.1242/dev.124.10.1953. [DOI] [PubMed] [Google Scholar]
- 28.Aravindan N., Subramanian K., Somasundaram D.B., Herman T.S., Aravindan S. MicroRNAs in Neuroblastoma Tumorigenesis, Therapy Resistance, and Disease Evolution. Cancer Drug Resist. 2019;2:1086–1105. doi: 10.20517/cdr.2019.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Misiak D., Hagemann S., Bell J.L., Busch B., Lederer M., Bley N., Schulte J.H., Hüttelmaier S. The MicroRNA Landscape of MYCN-Amplified Neuroblastoma. Front. Oncol. 2021;11:647737. doi: 10.3389/fonc.2021.647737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mobley B.C., Kwon M., Kraemer B.R., Hickman F.E., Qiao J., Chung D.H., Carter B.D. Expression of MYCN in Multipotent Sympathoadrenal Progenitors Induces Proliferation and Neural Differentiation, but Is Not Sufficient for Tumorigenesis. PLoS ONE. 2015;10:e0133897. doi: 10.1371/journal.pone.0133897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moccia M., Mercurio F.A., Langella E., Piacenti V., Leone M., Adamo M.F.A., Saviano M. Structural Insights on Tiny Peptide Nucleic Acid (PNA) Analogues of miRNA-34a: An in Silico and Experimental Integrated Approach. Front. Chem. 2020;8:568575. doi: 10.3389/fchem.2020.568575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ramaiah M.J., Pushpavalli S.N.C.V.L., Lavanya A., Bhadra K., Haritha V., Patel N., Tamboli J.R., Kamal A., Bhadra U., Pal-Bhadra M. Novel Anthranilamide-Pyrazolo[1,5-a]Pyrimidine Conjugates Modulate the Expression of P53-MYCN Associated Micro RNAs in Neuroblastoma Cells and Cause Cell Cycle Arrest and Apoptosis. Bioorg Med. Chem. Lett. 2013;23:5699–5706. doi: 10.1016/j.bmcl.2013.08.018. [DOI] [PubMed] [Google Scholar]
- 33.Li Y.-G., He J.-H., Yu L., Hang Z.-P., Li W., Shun W.-H., Huang G.X. microRNA-202 Suppresses MYCN Expression under the Control of E2F1 in the Neuroblastoma Cell Line LAN-5. Mol. Med. Rep. 2014;9:541–546. doi: 10.3892/mmr.2013.1845. [DOI] [PubMed] [Google Scholar]
- 34.Kobayashi K., Jakt L.M., Nishikawa S.-I. Epigenetic Regulation of the Neuroblastoma Genes, Arid3b and Mycn. Oncogene. 2013;32:2640–2648. doi: 10.1038/onc.2012.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsubota S., Kishida S., Shimamura T., Ohira M., Yamashita S., Cao D., Kiyonari S., Ushijima T., Kadomatsu K. PRC2-Mediated Transcriptomic Alterations at the Embryonic Stage Govern Tumorigenesis and Clinical Outcome in MYCN-Driven Neuroblastoma. Cancer Res. 2017;77:5259–5271. doi: 10.1158/0008-5472.CAN-16-3144. [DOI] [PubMed] [Google Scholar]
- 36.Tsubota S., Kadomatsu K. Origin and Initiation Mechanisms of Neuroblastoma. Cell Tissue Res. 2018;372:211–221. doi: 10.1007/s00441-018-2796-z. [DOI] [PubMed] [Google Scholar]
- 37.Corvetta D., Chayka O., Gherardi S., D’Acunto C.W., Cantilena S., Valli E., Piotrowska I., Perini G., Sala A. Physical Interaction between MYCN Oncogene and Polycomb Repressive Complex 2 (PRC2) in Neuroblastoma: Functional And Therapeutic Implications. J. Biol. Chem. 2013;288:8332–8341. doi: 10.1074/jbc.M113.454280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kerosuo L., Neppala P., Hsin J., Mohlin S., Vieceli F.M., Török Z., Laine A., Westermarck J., Bronner M.E. Enhanced Expression of MycN/CIP2A Drives Neural Crest toward a Neural Stem Cell-like Fate: Implications for Priming of Neuroblastoma. Proc. Natl. Acad. Sci. USA. 2018;115:E7351–E7360. doi: 10.1073/pnas.1800039115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hansford L.M., Thomas W.D., Keating J.M., Burkhart C.A., Peaston A.E., Norris M.D., Haber M., Armati P.J., Weiss W.A., Marshall G.M. Mechanisms of Embryonal Tumor Initiation: Distinct Roles for MycN Expression and MYCN Amplification. Proc. Natl. Acad. Sci. USA. 2004;101:12664–12669. doi: 10.1073/pnas.0401083101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weiss W.A., Aldape K., Mohapatra G., Feuerstein B.G., Bishop J.M. Targeted Expression of MYCN Causes Neuroblastoma in Transgenic Mice. EMBO J. 1997;16:2985–2995. doi: 10.1093/emboj/16.11.2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zhang L., Zhou H., Li J., Wang X., Zhang X., Shi T., Feng G. Comprehensive Characterization of Circular RNAs in Neuroblastoma Cell Lines. Technol. Cancer Res. Treat. 2020;19:1533033820957622. doi: 10.1177/1533033820957622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Antonaci M., Wheeler G.N. MicroRNAs in Neural Crest Development and Neurocristopathies. Biochem. Soc. Trans. 2022;50:965–974. doi: 10.1042/BST20210828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Corley M., Kroll K.L. The Roles and Regulation of Polycomb Complexes in Neural Development. Cell Tissue Res. 2015;359:65–85. doi: 10.1007/s00441-014-2011-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Braoudaki M., Hatziagapiou K., Zaravinos A., Lambrou G.I. MYCN in Neuroblastoma: “Old Wine into New Wineskins”. Diseases. 2021;9:78. doi: 10.3390/diseases9040078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fetahu I.S., Taschner-Mandl S. Neuroblastoma and the Epigenome. Cancer Metastasis Rev. 2021;40:173–189. doi: 10.1007/s10555-020-09946-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lázcoz P., Muñoz J., Nistal M., Pestaña A., Encío I., Castresana J.S. Frequent Promoter Hypermethylation of RASSF1A and CASP8 in Neuroblastoma. BMC Cancer. 2006;6:254. doi: 10.1186/1471-2407-6-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Djos A., Martinsson T., Kogner P., Carén H. The RASSF Gene Family Members RASSF5, RASSF6 and RASSF7 Show Frequent DNA Methylation in Neuroblastoma. Mol. Cancer. 2012;11:40. doi: 10.1186/1476-4598-11-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Henrich K.-O., Bender S., Saadati M., Dreidax D., Gartlgruber M., Shao C., Herrmann C., Wiesenfarth M., Parzonka M., Wehrmann L., et al. Integrative Genome-Scale Analysis Identifies Epigenetic Mechanisms of Transcriptional Deregulation in Unfavorable Neuroblastomas. Cancer Res. 2016;76:5523–5537. doi: 10.1158/0008-5472.CAN-15-2507. [DOI] [PubMed] [Google Scholar]
- 49.Teitz T., Inoue M., Valentine M.B., Zhu K., Rehg J.E., Zhao W., Finkelstein D., Wang Y.-D., Johnson M.D., Calabrese C., et al. Th-MYCN Mice with Caspase-8 Deficiency Develop Advanced Neuroblastoma with Bone Marrow Metastasis. Cancer Res. 2013;73:4086–4097. doi: 10.1158/0008-5472.CAN-12-2681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Giwa A., Rossouw S.C., Fatai A., Gamieldien J., Christoffels A., Bendou H. Predicting Amplification of MYCN Using CpG Methylation Biomarkers in Neuroblastoma. Future Oncol. 2021;17:4769–4783. doi: 10.2217/fon-2021-0522. [DOI] [PubMed] [Google Scholar]
- 51.Decock A., Ongenaert M., Hoebeeck J., De Preter K., Van Peer G., Van Criekinge W., Ladenstein R., Schulte J.H., Noguera R., Stallings R.L., et al. Genome-Wide Promoter Methylation Analysis in Neuroblastoma Identifies Prognostic Methylation Biomarkers. Genome Biol. 2012;13:R95. doi: 10.1186/gb-2012-13-10-r95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Uekusa S., Kawashima H., Sugito K., Yoshizawa S., Shinojima Y., Igarashi J., Ghosh S., Wang X., Fujiwara K., Ikeda T., et al. NR4A3, a Possibile Oncogenic Factor for Neuroblastoma Associated with CpGi Methylation within the Third Exon. Int. J. Oncol. 2014;44:1669–1677. doi: 10.3892/ijo.2014.2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Asada K., Watanabe N., Nakamura Y., Ohira M., Westermann F., Schwab M., Nakagawara A., Ushijima T. Stronger Prognostic Power of the CpG Island Methylator Phenotype than Methylation of Individual Genes in Neuroblastomas. Jpn. J. Clin. Oncol. 2013;43:641–645. doi: 10.1093/jjco/hyt058. [DOI] [PubMed] [Google Scholar]
- 54.Hoebeeck J., Michels E., Pattyn F., Combaret V., Vermeulen J., Yigit N., Hoyoux C., Laureys G., Paepe A.D., Speleman F., et al. Aberrant Methylation of Candidate Tumor Suppressor Genes in Neuroblastoma. Cancer Lett. 2009;273:336–346. doi: 10.1016/j.canlet.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 55.Chen L., Alexe G., Dharia N.V., Ross L., Iniguez A.B., Conway A.S., Wang E.J., Veschi V., Lam N., Qi J., et al. CRISPR-Cas9 Screen Reveals a MYCN-Amplified Neuroblastoma Dependency on EZH2. J. Clin. Investig. 2017;128:446–462. doi: 10.1172/JCI90793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abe M., Ohira M., Kaneda A., Yagi Y., Yamamoto S., Kitano Y., Takato T., Nakagawara A., Ushijima T. CpG Island Methylator Phenotype Is a Strong Determinant of Poor Prognosis in Neuroblastomas. Cancer Res. 2005;65:828–834. doi: 10.1158/0008-5472.828.65.3. [DOI] [PubMed] [Google Scholar]
- 57.Lalchungnunga H., Hao W., Maris J.M., Asgharzadeh S., Henrich K.-O., Westermann F., Tweddle D.A., Schwalbe E.C., Strathdee G. Genome Wide DNA Methylation Analysis Identifies Novel Molecular Subgroups and Predicts Survival in Neuroblastoma. Br. J. Cancer. 2022;127:2006–2015. doi: 10.1038/s41416-022-01988-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Banelli B., Gelvi I., Di Vinci A., Scaruffi P., Casciano I., Allemanni G., Bonassi S., Tonini G.P., Romani M. Distinct CpG Methylation Profiles Characterize Different Clinical Groups of Neuroblastic Tumors. Oncogene. 2005;24:5619–5628. doi: 10.1038/sj.onc.1208722. [DOI] [PubMed] [Google Scholar]
- 59.Casalà C., Gil-Guiñón E., Ordóñez J.L., Miguel-Queralt S., Rodríguez E., Galván P., Lavarino C., Munell F., de Alava E., Mora J., et al. The Calcium-Sensing Receptor Is Silenced by Genetic and Epigenetic Mechanisms in Unfavorable Neuroblastomas and Its Reactivation Induces ERK1/2-Dependent Apoptosis. Carcinogenesis. 2013;34:268–276. doi: 10.1093/carcin/bgs338. [DOI] [PubMed] [Google Scholar]
- 60.Yan P., Mühlethaler A., Bourloud K.B., Beck M.N., Gross N. Hypermethylation-Mediated Regulation of CD44 Gene Expression in Human Neuroblastoma. Genes Chromosomes Cancer. 2003;36:129–138. doi: 10.1002/gcc.10150. [DOI] [PubMed] [Google Scholar]
- 61.Lau D.T., Hesson L.B., Norris M.D., Marshall G.M., Haber M., Ashton L.J. Prognostic Significance of Promoter DNA Methylation in Patients with Childhood Neuroblastoma. Clin. Cancer Res. 2012;18:5690–5700. doi: 10.1158/1078-0432.CCR-12-0294. [DOI] [PubMed] [Google Scholar]
- 62.Yáñez Y., Grau E., Rodríguez-Cortez V.C., Hervás D., Vidal E., Noguera R., Hernández M., Segura V., Cañete A., Conesa A., et al. Two Independent Epigenetic Biomarkers Predict Survival in Neuroblastoma. Clin. Epigenetics. 2015;7:16. doi: 10.1186/s13148-015-0054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parodi F., Carosio R., Ragusa M., Di Pietro C., Maugeri M., Barbagallo D., Sallustio F., Allemanni G., Pistillo M.P., Casciano I., et al. Epigenetic Dysregulation in Neuroblastoma: A Tale of miRNAs and DNA Methylation. Biochim. Biophys. Acta. 2016;1859:1502–1514. doi: 10.1016/j.bbagrm.2016.10.006. [DOI] [PubMed] [Google Scholar]
- 64.Piacenti V., Langella E., Autiero I., Nolan J.C., Piskareva O., Adamo M.F.A., Saviano M., Moccia M. A Combined Experimental and Computational Study on Peptide Nucleic Acid (PNA) Analogues of Tumor Suppressive miRNA-34a. Bioorg. Chem. 2019;91:103165. doi: 10.1016/j.bioorg.2019.103165. [DOI] [PubMed] [Google Scholar]
- 65.Ikram F., Ackermann S., Kahlert Y., Volland R., Roels F., Engesser A., Hertwig F., Kocak H., Hero B., Dreidax D., et al. Transcription Factor Activating Protein 2 Beta (TFAP2B) Mediates Noradrenergic Neuronal Differentiation in Neuroblastoma. Mol. Oncol. 2016;10:344–359. doi: 10.1016/j.molonc.2015.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sugito K., Kawashima H., Yoshizawa S., Uekusa S., Hoshi R., Furuya T., Kaneda H., Hosoda T., Konuma N., Masuko T., et al. Non-Promoter DNA Hypermethylation of Zygote Arrest 1 (ZAR1) in Neuroblastomas. J. Pediatr. Surg. 2013;48:782–788. doi: 10.1016/j.jpedsurg.2012.08.008. [DOI] [PubMed] [Google Scholar]
- 67.Sugito K., Kawashima H., Uekusa S., Yoshizawa S., Hoshi R., Furuya T., Kaneda H., Hosoda T., Masuko T., Ohashi K., et al. Identification of Aberrant Methylation Regions in Neuroblastoma by Screening of Tissue-Specific Differentially Methylated Regions. Pediatr. Blood Cancer. 2013;60:383–389. doi: 10.1002/pbc.24282. [DOI] [PubMed] [Google Scholar]
- 68.Knoepfler P.S., Zhang X., Cheng P.F., Gafken P.R., McMahon S.B., Eisenman R.N. Myc Influences Global Chromatin Structure. EMBO J. 2006;25:2723–2734. doi: 10.1038/sj.emboj.7601152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Durbin A.D., Wang T., Wimalasena V.K., Zimmerman M.W., Li D., Dharia N.V., Mariani L., Shendy N.A.M., Nance S., Patel A.G., et al. EP300 Selectively Controls the Enhancer Landscape of MYCN-Amplified Neuroblastoma. Cancer Discov. 2022;12:730–751. doi: 10.1158/2159-8290.CD-21-0385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cheng C., He T., Chen K., Cai Y., Gu Y., Pan L., Duan P., Wu Y., Wu Z. P300 Interacted With N-Myc and Regulated Its Protein Stability via Altering Its Post-Translational Modifications in Neuroblastoma. Mol. Cell Proteom. 2023;22:100504. doi: 10.1016/j.mcpro.2023.100504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Marshall G.M., Gherardi S., Xu N., Neiron Z., Trahair T., Scarlett C.J., Chang D.K., Liu P.Y., Jankowski K., Iraci N., et al. Transcriptional Upregulation of Histone Deacetylase 2 Promotes Myc-Induced Oncogenic Effects. Oncogene. 2010;29:5957–5968. doi: 10.1038/onc.2010.332. [DOI] [PubMed] [Google Scholar]
- 72.Marshall G.M., Liu P.Y., Gherardi S., Scarlett C.J., Bedalov A., Xu N., Iraci N., Valli E., Ling D., Thomas W., et al. SIRT1 Promotes N-Myc Oncogenesis through a Positive Feedback Loop Involving the Effects of MKP3 and ERK on N-Myc Protein Stability. PLoS Genet. 2011;7:e1002135. doi: 10.1371/journal.pgen.1002135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Iraci N., Diolaiti D., Papa A., Porro A., Valli E., Gherardi S., Herold S., Eilers M., Bernardoni R., Valle G.D., et al. A SP1/MIZ1/MYCN Repression Complex Recruits HDAC1 at the TRKA and p75NTR Promoters and Affects Neuroblastoma Malignancy by Inhibiting the Cell Response to NGF. Cancer Res. 2011;71:404–412. doi: 10.1158/0008-5472.CAN-10-2627. [DOI] [PubMed] [Google Scholar]
- 74.Lodrini M., Oehme I., Schroeder C., Milde T., Schier M.C., Kopp-Schneider A., Schulte J.H., Fischer M., De Preter K., Pattyn F., et al. MYCN and HDAC2 Cooperate to Repress miR-183 Signaling in Neuroblastoma. Nucleic Acids Res. 2013;41:6018–6033. doi: 10.1093/nar/gkt346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fabian J., Opitz D., Althoff K., Lodrini M., Hero B., Volland R., Beckers A., de Preter K., Decock A., Patil N., et al. MYCN and HDAC5 Transcriptionally Repress CD9 to Trigger Invasion and Metastasis in Neuroblastoma. Oncotarget. 2016;7:66344–66359. doi: 10.18632/oncotarget.11662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wong M., Tee A.E.L., Milazzo G., Bell J.L., Poulos R.C., Atmadibrata B., Sun Y., Jing D., Ho N., Ling D., et al. The Histone Methyltransferase DOT1L Promotes Neuroblastoma by Regulating Gene Transcription. Cancer Res. 2017;77:2522–2533. doi: 10.1158/0008-5472.CAN-16-1663. [DOI] [PubMed] [Google Scholar]
- 77.Yang J., AlTahan A.M., Hu D., Wang Y., Cheng P.-H., Morton C.L., Qu C., Nathwani A.C., Shohet J.M., Fotsis T., et al. The Role of Histone Demethylase KDM4B in Myc Signaling in Neuroblastoma. J. Natl. Cancer Inst. 2015;107:djv080. doi: 10.1093/jnci/djv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Park J.H., Szemes M., Vieira G.C., Melegh Z., Malik S., Heesom K.J., Von Wallwitz-Freitas L., Greenhough A., Brown K.W., Zheng Y.G., et al. Protein Arginine Methyltransferase 5 Is a Key Regulator of the MYCN Oncoprotein in Neuroblastoma Cells. Mol. Oncol. 2015;9:617–627. doi: 10.1016/j.molonc.2014.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sun Y., Bell J.L., Carter D., Gherardi S., Poulos R.C., Milazzo G., Wong J.W.H., Al-Awar R., Tee A.E., Liu P.Y., et al. WDR5 Supports an N-Myc Transcriptional Complex That Drives a Protumorigenic Gene Expression Signature in Neuroblastoma. Cancer Res. 2015;75:5143–5154. doi: 10.1158/0008-5472.CAN-15-0423. [DOI] [PubMed] [Google Scholar]
- 80.Roeschert I., Poon E., Henssen A.G., Garcia H.D., Gatti M., Giansanti C., Jamin Y., Ade C.P., Gallant P., Schülein-Völk C., et al. Combined Inhibition of Aurora-A and ATR Kinase Results in Regression of MYCN-Amplified Neuroblastoma. Nat. Cancer. 2021;2:312–326. doi: 10.1038/s43018-020-00171-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Westphal M.S., Lee E., Schadt E.E., Sholler G.S., Zhu J. Identification of Let-7 miRNA Activity as a Prognostic Biomarker of SHH Medulloblastoma. Cancers. 2021;14:139. doi: 10.3390/cancers14010139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhao Z., Shelton S.D., Oviedo A., Baker A.L., Bryant C.P., Omidvarnia S., Du L. The PLAGL2/MYCN/miR-506-3p Interplay Regulates Neuroblastoma Cell Fate and Associates with Neuroblastoma Progression. J. Exp. Clin. Cancer Res. 2020;39:41. doi: 10.1186/s13046-020-1531-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Buechner J., Einvik C. N-Myc and Noncoding RNAs in Neuroblastoma. Mol. Cancer Res. 2012;10:1243–1253. doi: 10.1158/1541-7786.MCR-12-0244. [DOI] [PubMed] [Google Scholar]
- 84.Mestdagh P., Fredlund E., Pattyn F., Rihani A., Van Maerken T., Vermeulen J., Kumps C., Menten B., De Preter K., Schramm A., et al. An Integrative Genomics Screen Uncovers ncRNA T-UCR Functions in Neuroblastoma Tumours. Oncogene. 2010;29:3583–3592. doi: 10.1038/onc.2010.106. [DOI] [PubMed] [Google Scholar]
- 85.Chen Y., Stallings R.L. Differential Patterns of microRNA Expression in Neuroblastoma Are Correlated with Prognosis, Differentiation, and Apoptosis. Cancer Res. 2007;67:976–983. doi: 10.1158/0008-5472.CAN-06-3667. [DOI] [PubMed] [Google Scholar]
- 86.Qin X.-Y., Gailhouste L. Non-Genomic Control of Dynamic MYCN Gene Expression in Liver Cancer. Front. Oncol. 2020;10:618515. doi: 10.3389/fonc.2020.618515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Yasukawa K., Liew L.C., Hagiwara K., Hironaka-Mitsuhashi A., Qin X., Furutani Y., Tanaka Y., Nakagama H., Kojima S., Kato T., et al. MicroRNA-493-5p-mediated Repression of the MYCN Oncogene Inhibits Hepatic Cancer Cell Growth and Invasion. Cancer Sci. 2020;111:869–880. doi: 10.1111/cas.14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ma L., Young J., Prabhala H., Pan E., Mestdagh P., Muth D., Teruya-Feldstein J., Reinhardt F., Onder T.T., Valastyan S., et al. miR-9, a MYC/MYCN-Activated microRNA, Regulates E-Cadherin and Cancer Metastasis. Nat. Cell Biol. 2010;12:247–256. doi: 10.1038/ncb2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hu H., Du L., Nagabayashi G., Seeger R.C., Gatti R.A. ATM Is Down-Regulated by N-Myc-Regulated microRNA-421. Proc. Natl. Acad. Sci. USA. 2010;107:1506–1511. doi: 10.1073/pnas.0907763107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chava S., Reynolds C.P., Pathania A.S., Gorantla S., Poluektova L.Y., Coulter D.W., Gupta S.C., Pandey M.K., Challagundla K.B. miR-15a-5p, miR-15b-5p, and miR-16-5p Inhibit Tumor Progression by Directly Targeting MYCN in Neuroblastoma. Mol. Oncol. 2020;14:180–196. doi: 10.1002/1878-0261.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Buechner J., Tømte E., Haug B.H., Henriksen J.R., Løkke C., Flægstad T., Einvik C. Tumour-Suppressor microRNAs Let-7 and Mir-101 Target the Proto-Oncogene MYCN and Inhibit Cell Proliferation in MYCN-Amplified Neuroblastoma. Br. J. Cancer. 2011;105:296–303. doi: 10.1038/bjc.2011.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Beckers A., Van Peer G., Carter D.R., Gartlgruber M., Herrmann C., Agarwal S., Helsmoortel H., Althoff K., Molenaar J.J., Cheung B.B., et al. MYCN-Driven Regulatory Mechanisms Controlling LIN28B in Neuroblastoma. Cancer Lett. 2015;366:123–132. doi: 10.1016/j.canlet.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Molenaar J.J., Domingo-Fernández R., Ebus M.E., Lindner S., Koster J., Drabek K., Mestdagh P., van Sluis P., Valentijn L.J., van Nes J., et al. LIN28B Induces Neuroblastoma and Enhances MYCN Levels via Let-7 Suppression. Nat. Genet. 2012;44:1199–1206. doi: 10.1038/ng.2436. [DOI] [PubMed] [Google Scholar]
- 94.Bienertova-Vasku J., Mazanek P., Hezova R., Curdova A., Nekvindova J., Kren L., Sterba J., Slaby O. Extension of microRNA Expression Pattern Associated with High-Risk Neuroblastoma. Tumor Biol. 2013;34:2315–2319. doi: 10.1007/s13277-013-0777-0. [DOI] [PubMed] [Google Scholar]
- 95.Chen W., Hao X., Yang B., Zhang Y., Sun L., Hua Y., Yang L., Yu J., Zhao J., Hou L., et al. MYCN-Amplified Neuroblastoma Cell-Derived Exosomal miR-17-5p Promotes Proliferation and Migration of Non-MYCN Amplified Cells. Mol. Med. Rep. 2021;23:245. doi: 10.3892/mmr.2021.11884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mastropasqua F., Marzano F., Valletti A., Aiello I., Di Tullio G., Morgano A., Liuni S., Ranieri E., Guerrini L., Gasparre G., et al. TRIM8 Restores P53 Tumour Suppressor Function by Blunting N-MYC Activity in Chemo-Resistant Tumours. Mol. Cancer. 2017;16:67. doi: 10.1186/s12943-017-0634-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ooi C.Y., Carter D.R., Liu B., Mayoh C., Beckers A., Lalwani A., Nagy Z., De Brouwer S., Decaesteker B., Hung T.-T., et al. Network Modeling of microRNA-mRNA Interactions in Neuroblastoma Tumorigenesis Identifies miR-204 as a Direct Inhibitor of MYCN. Cancer Res. 2018;78:3122–3134. doi: 10.1158/0008-5472.CAN-17-3034. [DOI] [PubMed] [Google Scholar]
- 98.Salomão K.B., Pezuk J.A., de Souza G.R., Chagas P., Pereira T.C., Valera E.T., Brassesco M.S. MicroRNA Dysregulation Interplay with Childhood Abdominal Tumors. Cancer Metastasis Rev. 2019;38:783–811. doi: 10.1007/s10555-019-09829-x. [DOI] [PubMed] [Google Scholar]
- 99.Powers J.T., Tsanov K.M., Pearson D.S., Roels F., Spina C.S., Ebright R., Seligson M., de Soysa Y., Cahan P., Theiβen J., et al. Multiple Mechanisms Disrupt the Let-7 microRNA Family in Neuroblastoma. Nature. 2016;535:246–251. doi: 10.1038/nature18632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hennchen M., Stubbusch J., Abarchan-El Makhfi I., Kramer M., Deller T., Pierre-Eugene C., Janoueix-Lerosey I., Delattre O., Ernsberger U., Schulte J.B., et al. Lin28B and Let-7 in the Control of Sympathetic Neurogenesis and Neuroblastoma Development. J. Neurosci. 2015;35:16531–16544. doi: 10.1523/JNEUROSCI.2560-15.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Cheung I.Y., Farazi T.A., Ostrovnaya I., Xu H., Tran H., Mihailovic A., Tuschl T., Cheung N.-K.V. Deep MicroRNA Sequencing Reveals Downregulation of miR-29a in Neuroblastoma Central Nervous System Metastasis. Genes Chromosomes Cancer. 2014;53:803–814. doi: 10.1002/gcc.22189. [DOI] [PubMed] [Google Scholar]
- 102.Chen H., Shalom-Feuerstein R., Riley J., Zhang S.-D., Tucci P., Agostini M., Aberdam D., Knight R.A., Genchi G., Nicotera P., et al. miR-7 and miR-214 Are Specifically Expressed during Neuroblastoma Differentiation, Cortical Development and Embryonic Stem Cells Differentiation, and Control Neurite Outgrowth in Vitro. Biochem. Biophys. Res. Commun. 2010;394:921–927. doi: 10.1016/j.bbrc.2010.03.076. [DOI] [PubMed] [Google Scholar]
- 103.Radhakrishnan B., Alwin Prem Anand A. Role of miRNA-9 in Brain Development. J. Exp. Neurosci. 2016;10:101–120. doi: 10.4137/JEN.S32843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Ma Q., Zhang L., Pearce W.J. MicroRNAs in Brain Development and Cerebrovascular Pathophysiology. Am. J. Physiol. Cell Physiol. 2019;317:C3–C19. doi: 10.1152/ajpcell.00022.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Xia X., Wang Y., Zheng J.C. The microRNA-17 ~ 92 Family as a Key Regulator of Neurogenesis and Potential Regenerative Therapeutics of Neurological Disorders. Stem Cell Rev. Rep. 2022;18:401–411. doi: 10.1007/s12015-020-10050-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Han J., Kim H.J., Schafer S.T., Paquola A., Clemenson G.D., Toda T., Oh J., Pankonin A.R., Lee B.S., Johnston S.T., et al. Functional Implications of miR-19 in the Migration of Newborn Neurons in the Adult Brain. Neuron. 2016;91:79–89. doi: 10.1016/j.neuron.2016.05.034. [DOI] [PubMed] [Google Scholar]
- 107.Mogilyansky E., Rigoutsos I. The miR-17/92 Cluster: A Comprehensive Update on Its Genomics, Genetics, Functions and Increasingly Important and Numerous Roles in Health and Disease. Cell Death Differ. 2013;20:1603–1614. doi: 10.1038/cdd.2013.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ghosh T., Aprea J., Nardelli J., Engel H., Selinger C., Mombereau C., Lemonnier T., Moutkine I., Schwendimann L., Dori M., et al. MicroRNAs Establish Robustness and Adaptability of a Critical Gene Network to Regulate Progenitor Fate Decisions during Cortical Neurogenesis. Cell Rep. 2014;7:1779–1788. doi: 10.1016/j.celrep.2014.05.029. [DOI] [PubMed] [Google Scholar]
- 109.Sauer M., Was N., Ziegenhals T., Wang X., Hafner M., Becker M., Fischer U. The miR-26 Family Regulates Neural Differentiation-Associated microRNAs and mRNAs by Directly Targeting REST. J. Cell Sci. 2021;134:jcs257535. doi: 10.1242/jcs.257535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ouyang Y.-B., Xu L., Lu Y., Sun X., Yue S., Xiong X.-X., Giffard R.G. Astrocyte-Enriched miR-29a Targets PUMA and Reduces Neuronal Vulnerability to Forebrain Ischemia. Glia. 2013;61:1784–1794. doi: 10.1002/glia.22556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Chua C.E.L., Tang B.L. miR-34a in Neurophysiology and Neuropathology. J. Mol. Neurosci. 2019;67:235–246. doi: 10.1007/s12031-018-1231-y. [DOI] [PubMed] [Google Scholar]
- 112.Jauhari A., Yadav S. MiR-34 and MiR-200: Regulator of Cell Fate Plasticity and Neural Development. NeuroMol. Med. 2019;21:97–109. doi: 10.1007/s12017-019-08535-9. [DOI] [PubMed] [Google Scholar]
- 113.Lattanzi A., Gentner B., Corno D., Di Tomaso T., Mestdagh P., Speleman F., Naldini L., Gritti A. Dynamic Activity of miR-125b and miR-93 during Murine Neural Stem Cell Differentiation in Vitro and in the Subventricular Zone Neurogenic Niche. PLoS ONE. 2013;8:e67411. doi: 10.1371/journal.pone.0067411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cheng J., Xu L., Deng L., Xue L., Meng Q., Wei F., Wang J. RNA N6-Methyladenosine Modification Is Required for miR-98/MYCN Axis-Mediated Inhibition of Neuroblastoma Progression. Sci. Rep. 2020;10:13624. doi: 10.1038/s41598-020-64682-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Xylaki M., Paiva I., Al-Azzani M., Gerhardt E., Jain G., Islam M.R., Vasili E., Wassouf Z., Schulze-Hentrich J.M., Fischer A., et al. miR-101a-3p Impairs Synaptic Plasticity and Contributes to Synucleinopathy. J. Parkinson’s Dis. 2023;13:179–196. doi: 10.3233/JPD-225055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schulte J.H., Horn S., Otto T., Samans B., Heukamp L.C., Eilers U.-C., Krause M., Astrahantseff K., Klein-Hitpass L., Buettner R., et al. MYCN Regulates Oncogenic MicroRNAs in Neuroblastoma. Int. J. Cancer. 2008;122:699–704. doi: 10.1002/ijc.23153. [DOI] [PubMed] [Google Scholar]
- 117.Xia X., Lu H., Li C., Huang Y., Wang Y., Yang X., Zheng J.C. miR-106b Regulates the Proliferation and Differentiation of Neural Stem/Progenitor Cells through Tp53inp1-Tp53-Cdkn1a Axis. Stem Cell Res. Ther. 2019;10:282. doi: 10.1186/s13287-019-1387-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ristori E., Lopez-Ramirez M.A., Narayanan A., Hill-Teran G., Moro A., Calvo C.-F., Thomas J.L., Nicoli S. A Dicer-miR-107 Interaction Regulates Biogenesis of Specific miRNAs Crucial for Neurogenesis. Dev. Cell. 2015;32:546–560. doi: 10.1016/j.devcel.2014.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Pons-Espinal M., de Luca E., Marzi M.J., Beckervordersandforth R., Armirotti A., Nicassio F., Fabel K., Kempermann G., De Pietri Tonelli D. Synergic Functions of miRNAs Determine Neuronal Fate of Adult Neural Stem Cells. Stem Cell Rep. 2017;8:1046–1061. doi: 10.1016/j.stemcr.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Zhao J., Zhou K., Ma L., Zhang H. MicroRNA-145 Overexpression Inhibits Neuroblastoma Tumorigenesis in Vitro and in Vivo. Bioengineered. 2020;11:219–228. doi: 10.1080/21655979.2020.1729928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Jauhari A., Singh T., Yadav S. Expression of miR-145 and Its Target Proteins Are Regulated by miR-29b in Differentiated Neurons. Mol. Neurobiol. 2018;55:8978–8990. doi: 10.1007/s12035-018-1009-9. [DOI] [PubMed] [Google Scholar]
- 122.Li H., Kloosterman W., Fekete D.M. MicroRNA-183 Family Members Regulate Sensorineural Fates in the Inner Ear. J. Neurosci. 2010;30:3254–3263. doi: 10.1523/JNEUROSCI.4948-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Liu C., Teng Z.-Q., Santistevan N.J., Szulwach K.E., Guo W., Jin P., Zhao X. Epigenetic Regulation of miR-184 by MBD1 Governs Neural Stem Cell Proliferation and Differentiation. Cell Stem Cell. 2010;6:433–444. doi: 10.1016/j.stem.2010.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Roth S.A., Hald Ø.H., Fuchs S., Løkke C., Mikkola I., Flægstad T., Schulte J., Einvik C. MicroRNA-193b-3p Represses Neuroblastoma Cell Growth via Downregulation of Cyclin D1, MCL-1 and MYCN. Oncotarget. 2018;9:18160–18179. doi: 10.18632/oncotarget.24793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Beclin C., Follert P., Stappers E., Barral S., Coré N., de Chevigny A., Magnone V., Lebrigand K., Bissels U., Huylebroeck D., et al. miR-200 Family Controls Late Steps of Postnatal Forebrain Neurogenesis via Zeb2 Inhibition. Sci. Rep. 2016;6:35729. doi: 10.1038/srep35729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lepko T., Pusch M., Müller T., Schulte D., Ehses J., Kiebler M., Hasler J., Huttner H.B., Vandenbroucke R.E., Vandendriessche C., et al. Choroid Plexus-derived miR-204 Regulates the Number of Quiescent Neural Stem Cells in the Adult Brain. EMBO J. 2019;38:e100481. doi: 10.15252/embj.2018100481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lynch J., Fay J., Meehan M., Bryan K., Watters K.M., Murphy D.M., Stallings R.L. MiRNA-335 Suppresses Neuroblastoma Cell Invasiveness by Direct Targeting of Multiple Genes from the Non-Canonical TGF-β Signalling Pathway. Carcinogenesis. 2012;33:976–985. doi: 10.1093/carcin/bgs114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Jia J., Yan C., Tan Z., Liu M., Jiang Y. Transcriptional Factor FoxM1-Activated microRNA-335-3p Maintains the Self-Renewal of Neural Stem Cells by Inhibiting P53 Signaling Pathway via Fmr1. Stem Cell Res. Ther. 2021;12:169. doi: 10.1186/s13287-021-02191-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Swarbrick A., Woods S.L., Shaw A., Balakrishnan A., Phua Y., Nguyen A., Chanthery Y., Lim L., Ashton L.J., Judson R.L., et al. miR-380-5p Represses P53 to Control Cellular Survival and Is Associated with Poor Outcome in MYCN-Amplified Neuroblastoma. Nat. Med. 2010;16:1134–1140. doi: 10.1038/nm.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jiang Y., Jia J., Liu M., Tan Z., Cui Y. MiR-421 Binds to PINK1 and Enhances Neural Stem Cell Self-Renewal via HDAC3-Dependent FOXO3 Activation. Front. Cell Dev. Biol. 2021;9:621187. doi: 10.3389/fcell.2021.621187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhao Z., Ma X., Sung D., Li M., Kosti A., Lin G., Chen Y., Pertsemlidis A., Hsiao T.-H., Du L. microRNA-449a Functions as a Tumor Suppressor in Neuroblastoma through Inducing Cell Differentiation and Cell Cycle Arrest. RNA Biol. 2015;12:538–554. doi: 10.1080/15476286.2015.1023495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Wu J., Bao J., Kim M., Yuan S., Tang C., Zheng H., Mastick G.S., Xu C., Yan W. Two miRNA Clusters, miR-34b/c and miR-449, Are Essential for Normal Brain Development, Motile Ciliogenesis, and Spermatogenesis. Proc. Natl. Acad. Sci. USA. 2014;111:E2851–E2857. doi: 10.1073/pnas.1407777111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Soriano A., París-Coderch L., Jubierre L., Martínez A., Zhou X., Piskareva O., Bray I., Vidal I., Almazán-Moga A., Molist C., et al. MicroRNA-497 Impairs the Growth of Chemoresistant Neuroblastoma Cells by Targeting Cell Cycle, Survival and Vascular Permeability Genes. Oncotarget. 2016;7:9271–9287. doi: 10.18632/oncotarget.7005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhang J., Zhang J., Zhou Y., Wu Y.-J., Ma L., Wang R.-J., Huang S.-Q., Gao R.-R., Liu L.-H., Shao Z.-H., et al. Novel Cerebellum-Enriched miR-592 May Play a Role in Neural Progenitor Cell Differentiation and Neuronal Maturation through Regulating Lrrc4c and Nfasc in Rat. Curr. Mol. Med. 2013;13:1432–1445. doi: 10.2174/15665240113139990072. [DOI] [PubMed] [Google Scholar]
- 135.Megiorni F., Colaiacovo M., Cialfi S., McDowell H.P., Guffanti A., Camero S., Felsani A., Losty P.D., Pizer B., Shukla R., et al. A Sketch of Known and Novel MYCN-Associated miRNA Networks in Neuroblastoma. Oncol. Rep. 2017;38:3–20. doi: 10.3892/or.2017.5701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu P.Y., Erriquez D., Marshall G.M., Tee A.E., Polly P., Wong M., Liu B., Bell J.L., Zhang X.D., Milazzo G., et al. Effects of a Novel Long Noncoding RNA, lncUSMycN, on N-Myc Expression and Neuroblastoma Progression. JNCI J. Natl. Cancer Inst. 2014;106:dju113. doi: 10.1093/jnci/dju113. [DOI] [PubMed] [Google Scholar]
- 137.Yu M., Ohira M., Li Y., Niizuma H., Oo M.L., Zhu Y., Ozaki T., Isogai E., Nakamura Y., Koda T., et al. High Expression of ncRAN, a Novel Non-Coding RNA Mapped to Chromosome 17q25.1, Is Associated with Poor Prognosis in Neuroblastoma. Int. J. Oncol. 2009;34:931–938. doi: 10.3892/ijo_00000219. [DOI] [PubMed] [Google Scholar]
- 138.Zhang N., Liu F.-L., Ma T.-S., Zhang Z.-D.Z.J.-J. LncRNA SNHG1 Contributes to Tumorigenesis and Mechanism by Targeting miR-338-3p to Regulate PLK4 in Human Neuroblastoma. Eur. Rev. Med. Pharmacol. Sci. 2019;23:8971–8983. doi: 10.26355/eurrev_201910_19296. [DOI] [PubMed] [Google Scholar]
- 139.Liu P.Y., Tee A.E., Milazzo G., Hannan K.M., Maag J., Mondal S., Atmadibrata B., Bartonicek N., Peng H., Ho N., et al. The Long Noncoding RNA lncNB1 Promotes Tumorigenesis by Interacting with Ribosomal Protein RPL35. Nat. Commun. 2019;10:5026. doi: 10.1038/s41467-019-12971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Alloisio S., Garbati P., Viti F., Dante S., Barbieri R., Arnaldi G., Petrelli A., Gigoni A., Giannoni P., Quarto R., et al. Generation of a Functional Human Neural Network by NDM29 Overexpression in Neuroblastoma Cancer Cells. Mol. Neurobiol. 2017;54:6097–6106. doi: 10.1007/s12035-016-0161-3. [DOI] [PubMed] [Google Scholar]
- 141.Vadie N., Saayman S., Lenox A., Ackley A., Clemson M., Burdach J., Hart J., Vogt P.K., Morris K.V. MYCNOS Functions as an Antisense RNA Regulating MYCN. RNA Biol. 2015;12:893–899. doi: 10.1080/15476286.2015.1063773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.O’Brien E.M., Selfe J.L., Martins A.S., Walters Z.S., Shipley J.M. The Long Non-Coding RNA MYCNOS-01 Regulates MYCN Protein Levels and Affects Growth of MYCN-Amplified Rhabdomyosarcoma and Neuroblastoma Cells. BMC Cancer. 2018;18:217. doi: 10.1186/s12885-018-4129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Li M., Meng F., Lu Q. Expression Profile Screening and Bioinformatics Analysis of circRNA, LncRNA, and mRNA in Acute Myeloid Leukemia Drug-Resistant Cells. Turk. J. Haematol. 2020;37:104–110. doi: 10.4274/tjh.galenos.2019.2019.0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Fuchs S., Danßmann C., Klironomos F., Winkler A., Fallmann J., Kruetzfeldt L.-M., Szymansky A., Naderi J., Bernhart S.H., Grunewald L., et al. Defining the Landscape of Circular RNAs in Neuroblastoma Unveils a Global Suppressive Function of MYCN. Nat. Commun. 2023;14:3936. doi: 10.1038/s41467-023-38747-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Mittal P., Roberts C.W.M. The SWI/SNF Complex in Cancer—Biology, Biomarkers and Therapy. Nat. Rev. Clin. Oncol. 2020;17:435–448. doi: 10.1038/s41571-020-0357-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shi H., Tao T., Abraham B.J., Durbin A.D., Zimmerman M.W., Kadoch C., Look A.T. ARID1A Loss in Neuroblastoma Promotes the Adrenergic-to-Mesenchymal Transition by Regulating Enhancer-Mediated Gene Expression. Sci. Adv. 2020;6:eaaz3440. doi: 10.1126/sciadv.aaz3440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Thandapani P. Super-Enhancers in Cancer. Pharmacol. Ther. 2019;199:129–138. doi: 10.1016/j.pharmthera.2019.02.014. [DOI] [PubMed] [Google Scholar]
- 148.van Groningen T., Koster J., Valentijn L.J., Zwijnenburg D.A., Akogul N., Hasselt N.E., Broekmans M., Haneveld F., Nowakowska N.E., Bras J., et al. Neuroblastoma Is Composed of Two Super-Enhancer-Associated Differentiation States. Nat. Genet. 2017;49:1261–1266. doi: 10.1038/ng.3899. [DOI] [PubMed] [Google Scholar]
- 149.Zimmerman M.W., Liu Y., He S., Durbin A.D., Abraham B.J., Easton J., Shao Y., Xu B., Zhu S., Zhang X., et al. C-MYC Drives a Subset of High-Risk Pediatric Neuroblastomas and Is Activated through Mechanisms Including Enhancer Hijacking and Focal Enhancer Amplification. Cancer Discov. 2018;8:320–335. doi: 10.1158/2159-8290.CD-17-0993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Helmsauer K., Valieva M.E., Ali S., Chamorro González R., Schöpflin R., Röefzaad C., Bei Y., Dorado Garcia H., Rodriguez-Fos E., Puiggròs M., et al. Enhancer Hijacking Determines Extrachromosomal Circular MYCN Amplicon Architecture in Neuroblastoma. Nat. Commun. 2020;11:5823. doi: 10.1038/s41467-020-19452-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Zeid R., Lawlor M.A., Poon E., Reyes J.M., Fulciniti M., Lopez M.A., Scott T.G., Nabet B., Erb M.A., Winter G.E., et al. Enhancer Invasion Shapes MYCN Dependent Transcriptional Amplification in Neuroblastoma. Nat. Genet. 2018;50:515. doi: 10.1038/s41588-018-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wang L., Tan T.K., Durbin A.D., Zimmerman M.W., Abraham B.J., Tan S.H., Ngoc P.C.T., Weichert-Leahey N., Akahane K., Lawton L.N., et al. ASCL1 Is a MYCN- and LMO1-Dependent Member of the Adrenergic Neuroblastoma Core Regulatory Circuitry. Nat. Commun. 2019;10:5622. doi: 10.1038/s41467-019-13515-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gartlgruber M., Sharma A.K., Quintero A., Dreidax D., Jansky S., Park Y.-G., Kreth S., Meder J., Doncevic D., Saary P., et al. Super Enhancers Define Regulatory Subtypes and Cell Identity in Neuroblastoma. Nat. Cancer. 2020;2:114–128. doi: 10.1038/s43018-020-00145-w. [DOI] [PubMed] [Google Scholar]
- 154.Zimmerman M.W., Durbin A.D., He S., Oppel F., Shi H., Tao T., Li Z., Berezovskaya A., Liu Y., Zhang J., et al. Retinoic Acid Rewires the Adrenergic Core Regulatory Circuitry of Childhood Neuroblastoma. Sci. Adv. 2021;7:eabe0834. doi: 10.1126/sciadv.abe0834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Li G.-H., Qu Q., Qi T.-T., Teng X.-Q., Zhu H.-H., Wang J.-J., Lu Q., Qu J. Super-Enhancers: A New Frontier for Epigenetic Modifiers in Cancer Chemoresistance. J. Exp. Clin. Cancer Res. 2021;40:174. doi: 10.1186/s13046-021-01974-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kotekar A., Singh A.K., Devaiah B.N. BRD4 and MYC: Power Couple in Transcription and Disease. FEBS J. 2023;290:4820–4842. doi: 10.1111/febs.16580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Erdreich-Epstein A., Singh A.R., Joshi S., Vega F.M., Guo P., Xu J., Groshen S., Ye W., Millard M., Campan M., et al. Association of High Microvessel Avβ3 and Low PTEN with Poor Outcome in Stage 3 Neuroblastoma: Rationale for Using First in Class Dual PI3K/BRD4 Inhibitor, SF1126. Oncotarget. 2016;8:52193–52210. doi: 10.18632/oncotarget.13386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gao Y., Volegova M., Nasholm N., Das S., Kwiatkowski N., Abraham B.J., Zhang T., Gray N.S., Gustafson C., Krajewska M., et al. Synergistic Anti-Tumor Effect of Combining Selective CDK7 and BRD4 Inhibition in Neuroblastoma. Front. Oncol. 2022;11:773186. doi: 10.3389/fonc.2021.773186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Shahbazi J., Liu P.Y., Atmadibrata B., Bradner J.E., Marshall G.M., Lock R.B., Liu T. The Bromodomain Inhibitor JQ1 and the Histone Deacetylase Inhibitor Panobinostat Synergistically Reduce N-Myc Expression and Induce Anticancer Effects. Clin. Cancer Res. 2016;22:2534–2544. doi: 10.1158/1078-0432.CCR-15-1666. [DOI] [PubMed] [Google Scholar]
- 160.Hu X., Liu R., Hou J., Peng W., Wan S., Xu M., Li Y., Zhang G., Zhai X., Liang P., et al. SMARCE1 Promotes Neuroblastoma Tumorigenesis through Assisting MYCN-Mediated Transcriptional Activation. Oncogene. 2022;41:4295–4306. doi: 10.1038/s41388-022-02428-1. [DOI] [PubMed] [Google Scholar]
- 161.Laut A.K., Dorneburg C., Fürstberger A., Barth T.F.E., Kestler H.A., Debatin K.-M., Beltinger C. CHD5 Inhibits Metastasis of Neuroblastoma. Oncogene. 2022;41:622–633. doi: 10.1038/s41388-021-02081-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Egan C.M., Nyman U., Skotte J., Streubel G., Turner S., O’Connell D.J., Rraklli V., Dolan M.J., Chadderton N., Hansen K., et al. CHD5 Is Required for Neurogenesis and Has a Dual Role in Facilitating Gene Expression and Polycomb Gene Repression. Dev. Cell. 2013;26:223–236. doi: 10.1016/j.devcel.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 163.Krstic A., Konietzny A., Halasz M., Cain P., Oppermann U., Kolch W., Duffy D.J. A Chemo-Genomic Approach Identifies Diverse Epigenetic Therapeutic Vulnerabilities in MYCN-Amplified Neuroblastoma. Front. Cell Dev. Biol. 2021;9:612518. doi: 10.3389/fcell.2021.612518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Liu T., Tee A.E.L., Porro A., Smith S.A., Dwarte T., Liu P.Y., Iraci N., Sekyere E., Haber M., Norris M.D., et al. Activation of Tissue Transglutaminase Transcription by Histone Deacetylase Inhibition as a Therapeutic Approach for Myc Oncogenesis. Proc. Natl. Acad. Sci. USA. 2007;104:18682–18687. doi: 10.1073/pnas.0705524104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Cortés C., Kozma S.C., Tauler A., Ambrosio S. MYCN Concurrence with SAHA-Induced Cell Death in Human Neuroblastoma Cells. Cell Oncol. 2015;38:341–352. doi: 10.1007/s13402-015-0233-9. [DOI] [PubMed] [Google Scholar]
- 166.de Ruijter A.J.M., Kemp S., Kramer G., Meinsma R.J., Kaufmann J.O., Caron H.N., van Kuilenburg A.B.P. The Novel Histone Deacetylase Inhibitor BL1521 Inhibits Proliferation and Induces Apoptosis in Neuroblastoma Cells. Biochem. Pharmacol. 2004;68:1279–1288. doi: 10.1016/j.bcp.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 167.Jaboin J., Wild J., Hamidi H., Khanna C., Kim C.J., Robey R., Bates S.E., Thiele C.J. MS-27-275, an Inhibitor of Histone Deacetylase, Has Marked in Vitro and in Vivo Antitumor Activity against Pediatric Solid Tumors. Cancer Res. 2002;62:6108–6115. [PubMed] [Google Scholar]
- 168.Merck News Item. [(accessed on 2 November 2023)]. Available online: https://web.archive.org/web/20060914014021/http://www.merck.com/newsroom/press_releases/research_and_development/2006_0607.html.
- 169.Bartolucci D., Montemurro L., Raieli S., Lampis S., Pession A., Hrelia P., Tonelli R. MYCN Impact on High-Risk Neuroblastoma: From Diagnosis and Prognosis to Targeted Treatment. Cancers. 2022;14:4421. doi: 10.3390/cancers14184421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Rettig I., Koeneke E., Trippel F., Mueller W.C., Burhenne J., Kopp-Schneider A., Fabian J., Schober A., Fernekorn U., von Deimling A., et al. Selective Inhibition of HDAC8 Decreases Neuroblastoma Growth in Vitro and in Vivo and Enhances Retinoic Acid-Mediated Differentiation. Cell Death Dis. 2015;6:e1657. doi: 10.1038/cddis.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Hegarty S.V., Togher K.L., O’Leary E., Solger F., Sullivan A.M., O’Keeffe G.W. Romidepsin Induces Caspase-Dependent Cell Death in Human Neuroblastoma Cells. Neurosci. Lett. 2017;653:12–18. doi: 10.1016/j.neulet.2017.05.025. [DOI] [PubMed] [Google Scholar]
- 172.Fabian J., Lodrini M., Oehme I., Schier M.C., Thole T.M., Hielscher T., Kopp-Schneider A., Opitz L., Capper D., von Deimling A., et al. GRHL1 Acts as Tumor Suppressor in Neuroblastoma and Is Negatively Regulated by MYCN and HDAC3. Cancer Res. 2014;74:2604–2616. doi: 10.1158/0008-5472.CAN-13-1904. [DOI] [PubMed] [Google Scholar]
- 173.Bownes L.V., Williams A.P., Marayati R., Stafman L.L., Markert H., Quinn C.H., Wadhwani N., Aye J.M., Stewart J.E., Yoon K.J., et al. EZH2 Inhibition Decreases Neuroblastoma Proliferation and in Vivo Tumor Growth. PLoS ONE. 2021;16:e0246244. doi: 10.1371/journal.pone.0246244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Gao J., Fosbrook C., Gibson J., Underwood T.J., Gray J.C., Walters Z.S. Review: Targeting EZH2 in Neuroblastoma. Cancer Treat. Rev. 2023;119:102600. doi: 10.1016/j.ctrv.2023.102600. [DOI] [PubMed] [Google Scholar]
- 175.Mellini P., Marrocco B., Borovika D., Polletta L., Carnevale I., Saladini S., Stazi G., Zwergel C., Trapencieris P., Ferretti E., et al. Pyrazole-Based Inhibitors of Enhancer of Zeste Homologue 2 Induce Apoptosis and Autophagy in Cancer Cells. Philos. Trans. R. Soc. B Biol. Sci. 2018;373:20170150. doi: 10.1098/rstb.2017.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Gulati N., Béguelin W., Giulino-Roth L. Enhancer of Zeste Homolog 2 (EZH2) Inhibitors. Leuk. Lymphoma. 2018;59:1574–1585. doi: 10.1080/10428194.2018.1430795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Seier J.A., Reinhardt J., Saraf K., Ng S.S., Layer J.P., Corvino D., Althoff K., Giordano F.A., Schramm A., Fischer M., et al. Druggable Epigenetic Suppression of Interferon-Induced Chemokine Expression Linked to MYCN Amplification in Neuroblastoma. J. Immunother. Cancer. 2021;9:e001335. doi: 10.1136/jitc-2020-001335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lu Z., Tian Y., Salwen H.R., Chlenski A., Godley L.A., Raj J.U., Yang Q. Histone Lysine Methyltransferase EHMT2 Is Involved in Proliferation, Apoptosis, Cell Invasion and DNA Methylation of Human Neuroblastoma Cells. Anticancer Drugs. 2013;24:484–493. doi: 10.1097/CAD.0b013e32835ffdbb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Mertz J.A., Conery A.R., Bryant B.M., Sandy P., Balasubramanian S., Mele D.A., Bergeron L., Sims R.J. Targeting MYC Dependence in Cancer by Inhibiting BET Bromodomains. Proc. Natl. Acad. Sci. USA. 2011;108:16669–16674. doi: 10.1073/pnas.1108190108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Puissant A., Frumm S.M., Alexe G., Bassil C.F., Qi J., Chanthery Y.H., Nekritz E.A., Zeid R., Gustafson W.C., Greninger P., et al. Targeting MYCN in Neuroblastoma by BET Bromodomain Inhibition. Cancer Discov. 2013;3:308–323. doi: 10.1158/2159-8290.CD-12-0418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Lee S., Rellinger E.J., Kim K.W., Craig B.T., Romain C.V., Qiao J., Chung D.H. Bet Inhibition Blocks Tumor Progression and Promotes Differentiation in Neuroblastoma. Surgery. 2015;158:819–826. doi: 10.1016/j.surg.2015.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Henssen A., Althoff K., Odersky A., Beckers A., Koche R., Speleman F., Schäfers S., Bell E., Nortmeyer M., Westermann F., et al. Targeting MYCN-Driven Transcription By BET-Bromodomain Inhibition. Clin. Cancer Res. 2016;22:2470–2481. doi: 10.1158/1078-0432.CCR-15-1449. [DOI] [PubMed] [Google Scholar]
- 183.Piha-Paul S.A., Hann C.L., French C.A., Cousin S., Braña I., Cassier P.A., Moreno V., de Bono J.S., Harward S.D., Ferron-Brady G., et al. Phase 1 Study of Molibresib (GSK525762), a Bromodomain and Extra-Terminal Domain Protein Inhibitor, in NUT Carcinoma and Other Solid Tumors. JNCI Cancer Spectr. 2019;4:pkz093. doi: 10.1093/jncics/pkz093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Cao Y., Liu Y., Shang L., Wei W., Shen Y., Gu Q., Xie X., Dong W., Lin Y., Yue Y., et al. Decitabine and All-Trans Retinoic Acid Synergistically Exhibit Cytotoxicity against Elderly AML Patients via miR-34a/MYCN Axis. Biomed. Pharmacother. 2020;125:109878. doi: 10.1016/j.biopha.2020.109878. [DOI] [PubMed] [Google Scholar]
- 185.Penter L., Maier B., Frede U., Hackner B., Carell T., Hagemeier C., Truss M. A Rapid Screening System Evaluates Novel Inhibitors of DNA Methylation and Suggests F-Box Proteins as Potential Therapeutic Targets for High-Risk Neuroblastoma. Targ. Oncol. 2015;10:523–533. doi: 10.1007/s11523-014-0354-5. [DOI] [PubMed] [Google Scholar]
- 186.Das S., Foley N., Bryan K., Watters K.M., Bray I., Murphy D.M., Buckley P.G., Stallings R.L. MicroRNA Mediates DNA De-Methylation Events Triggered By Retinoic Acid During Neuroblastoma Cell Differentiation. Cancer Res. 2010;70:7874–7881. doi: 10.1158/0008-5472.CAN-10-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Iniguez A.B., Alexe G., Wang E.J., Roti G., Patel S., Chen L., Kitara S., Conway A., Robichaud A.L., Stolte B., et al. Resistance to Epigenetic-Targeted Therapy Engenders Tumor Cell Vulnerabilities Associated with Enhancer Remodeling. Cancer Cell. 2018;34:922–938.e7. doi: 10.1016/j.ccell.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Čančer M., Drews L.F., Bengtsson J., Bolin S., Rosén G., Westermark B., Nelander S., Forsberg-Nilsson K., Uhrbom L., Weishaupt H., et al. BET and Aurora Kinase A Inhibitors Synergize against MYCN-Positive Human Glioblastoma Cells. Cell Death Dis. 2019;10:881. doi: 10.1038/s41419-019-2120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.George R.E., Lahti J.M., Adamson P.C., Zhu K., Finkelstein D., Ingle A.M., Reid J.M., Krailo M., Neuberg D., Blaney S.M., et al. Phase I Study of Decitabine with Doxorubicin and Cyclophosphamide in Children with Neuroblastoma and Other Solid Tumors: A Children’s Oncology Group Study. Pediatr. Blood Cancer. 2010;55:629–638. doi: 10.1002/pbc.22607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Li Z., Lim S.L., Tao Y., Li X., Xie Y., Yang C., Zhang Z., Jiang Y., Zhang X., Cao X., et al. PROTAC Bromodomain Inhibitor ARV-825 Displays Anti-Tumor Activity in Neuroblastoma by Repressing Expression of MYCN or c-Myc. Front. Oncol. 2020;10:574525. doi: 10.3389/fonc.2020.574525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ouwehand K., de Ruijter A.J.M., van Bree C., Caron H.N., van Kuilenburg A.B.P. Histone Deacetylase Inhibitor BL1521 Induces a G1-Phase Arrest in Neuroblastoma Cells through Altered Expression of Cell Cycle Proteins. FEBS Lett. 2005;579:1523–1528. doi: 10.1016/j.febslet.2005.01.058. [DOI] [PubMed] [Google Scholar]
- 192.Carpinelli P., Granata F., Augusti-Tocco G., Rossi M., Bartolucci S. Antiproliferative Effects and DNA Hypomethylation by 5-Aza-2′-Deoxycytidine in Human Neuroblastoma Cell Lines. Anti-Cancer Drugs. 1993;4:629. doi: 10.1097/00001813-199312000-00004. [DOI] [PubMed] [Google Scholar]
- 193.Bate-Eya L.T., Gierman H.J., Ebus M.E., Koster J., Caron H.N., Versteeg R., Dolman M.E.M., Molenaar J.J. Enhancer of Zeste Homologue 2 Plays an Important Role in Neuroblastoma Cell Survival Independent of Its Histone Methyltransferase Activity. Eur. J. Cancer. 2017;75:63–72. doi: 10.1016/j.ejca.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 194.Wyce A., Ganji G., Smitheman K.N., Chung C.-W., Korenchuk S., Bai Y., Barbash O., Le B., Craggs P.D., McCabe M.T., et al. BET Inhibition Silences Expression of MYCN and BCL2 and Induces Cytotoxicity in Neuroblastoma Tumor Models. PLoS ONE. 2013;8:e72967. doi: 10.1371/journal.pone.0072967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.GlaxoSmithKline . A Phase I/II Open-Label, Dose Escalation Study to Investigate the Safety, Pharmacokinetics, Pharmacodynamics, and Clinical Activity of GSK525762 in Subjects with NUT Midline Carcinoma (NMC) and Other Cancers. Dana-Farber Cancer Institute; Boston, MA, USA: 2020. [Google Scholar]
- 196.Gu S., Tian Y., Chlenski A., Salwen H.R., Lu Z., Raj J.U., Yang Q. Valproic Acid Shows Potent Antitumor Effect with Alteration of DNA Methylation in Neuroblastoma. Anticancer Drugs. 2012;23:1054–1066. doi: 10.1097/CAD.0b013e32835739dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.