Significance
Population-level trends in mental health have been declining in developed nations for many years, especially among young people. However, whether these declines represent temporary changes that will recover with age or time or a more permanent change associated with the birth cohort and thus represent a potential lifetime difference is unclear. Using data from a large, nationally representative survey which tracks the mental health of Australians over a 20-y period, we were able to distinguish the decline in mental health is largely driven by young adults born in the 1990s, and to a lesser extent people born in the 1980s. This represents important evidence that declines in mental health among young adults may not be expected to spontaneously recover or disappear.
Keywords: subjective well-being, psychological distress, age–period–cohort effects, generalized additive mixed models, longitudinal
Abstract
Given the observed deterioration in mental health among Australians over the past decade, this study investigates to what extent this differs in people born in different decades—i.e., possible birth cohort differences in the mental health of Australians. Using 20 y of data from a large, nationally representative panel survey (N = 27,572), we find strong evidence that cohort effects are driving the increase in population-level mental ill-health. Deteriorating mental health is particularly pronounced among people born in the 1990s and seen to a lesser extent among the 1980s cohort. There is little evidence that mental health is worsening with age for people born prior to the 1980s. The findings from this study highlight that it is the poorer mental health of Millennials that is driving the apparent deterioration in population-level mental health. Understanding the context and changes in society that have differentially affected younger people may inform efforts to ameliorate this trend and prevent it continuing for emerging cohorts.
There is recent evidence from many countries that population mental health has worsened over time, even prior to the COVID-19 pandemic. In Australia, this pattern is most strikingly illustrated by the increasing rates of reported mental and behavioural disorders in the regular National Health Survey series, increasing from 9.6% of Australians aged 15 y old and over in 2001 to 20.1% in 2017/18 (1) and increasing even further to 21.4% in 2020/21 (2). Such evidence of worsening mental health is consistent with data showing the increasing use of both psychotropics and therapeutic services within populations (3). This worsening mental health over time is also shown in measures of psychological distress, including research using large longitudinal panel surveys such as the Household, Income and Labour Dynamics in Australia (HILDA) Survey, which showed a broad increase in overall rates of psychological distress (Kessler-10 scores) in Australia from 4.8 to 7.4% between 2007 and 2017 across the 18 to 64 age ranges (4). Most other OECD countries have observed similar worsening in population levels of mental health, particularly among young people in the United Kingdom, United States, Netherlands, and Japan (5–8), though this pattern is not ubiquitous, e.g., not in Canada, (9). This paper seeks to better understand the factors potentially driving this increase in mental ill-health among Australians over time, in relation to period, age, and cohort effects.
The worsening of population mental health over time may be a period effect to the extent that it reflects a common change experienced by all groups in the population at the same point in time, regardless of age. This could, for example, reflect a change in risks that affect everyone (e.g., climate change). Alternatively, recent widespread international disruptions, such as the global financial crisis (GFC) or the COVID-19 pandemic which both resulted in loss of economic opportunity, may have also broadly impacted the mental health of all (10, 11).
An overall worsening of population mental health over time may be a consequence of age effects in the context of changing population age structures, e.g., associated with population ageing (12–14). Such “age effects” reflect differences in rates of poor mental health tied to age but independent of the period and cohort. Comparing age groups over the population has revealed a U-shaped pattern in mental well-being in large cross-sectional surveys. These hedonic aspects of well-being (often measured using questions similar to those used to assess distress, but with a different valence) decline from young age groups (e.g., 18 to 20 y) to middle-age (50 to 55 y) before increasing to a peak at 70 to 75 y old, although there are cultural and national differences (15, 16). In Australia, Burns et al. (17) evaluated age-related changes in the mental health of Australian adultsusing 17 y of HILDA data (2001 to 2017). Using the mental health inventory (MHI-5) derived from the SF-36, they report only very small differences in mental health over age groups, but an emerging downward trend for the youngest (18 to 24 y) and very oldest adults (75+ y) in 2017 data, which suggests that age-related changes may be distinguished in more recent data.
In contrast to age-related changes, which reflect consistent variation in mental health over the lifespan irrespective of time, mental health may also vary by birth cohort. Cohort effects refer to variance over time that is specific to individuals born in or around certain years (e.g., generational differences between “Millennials” and “Baby Boomers”). Cohort differences in mental health are more likely to reflect widespread societal changes in risk factors or vulnerability that differentially affect cohorts, such as the penetration of social media, and are associated with the person-specific differences which persist over the age range.
Because of the linear dependency between age-, cohort-, and period-effects (18, 19), disentangling age-related effects from cohort effects in mental health is fraught, but crucial if we are to identify the groups most at risk and potentially target effective prevention or early treatment approaches. There is no technical way to solve the dependency and identify the unique effect of each in a linear model (19, 20). The only way to solve this issue is by fiat; that is by conceding some constraint whose appropriateness cannot be tested. Other authors examining age-, period-, cohort-effects in mental health have elected to impose equality constraints (21), or assumed the period effects are negligible (22), or estimated the line of solution rather than distinguishing the effects themselves (23, 24). Most methods impose constraints that are either not testable or often not theoretically derived (18, 25, 26). However, nonlinear effects (and some interactions) that occur around the linear effects are estimable (27). We sought to determine whether the cohort differences in mental health are increasing or decreasing with age relative to earlier cohorts (i.e., an age-cohort interaction), and therefore, these nonlinear effects are the proper focus of our study (27).
Our aim is to distinguish whether the widely observed rise in mental ill-health, an observed period effect, in Australia is due to variation with age or differences between birth cohorts. To remove the linear dependency and identify any differences in trends between cohorts, we model mental health (MHI-5 scores) for each cohort as a nonlinear smooth function of age in an age-cohort model. Cohort effects are captured by directly estimating the differences between the smooth age trends of adjacent cohorts. These directly estimated differences represent a nonlinear age-by-cohort interaction and reveal how mental health is changing over age in one cohort relative to the other cohort. Thus, our age-cohort model allows us to determine whether the trajectory of mental health is improving or deteriorating over age relative to earlier cohorts.
Results
The demographics of each cohort are shown in Table 1. The characteristics associated with the latest observation from each person are presented.
Table 1.
Demographics stratified by birth cohort
| Characteristic | 1940s* N = 2,791 |
1950s* N = 3,890 |
1960s* N = 4,564 |
1970s* N = 4,614 |
1980s* N = 6,133 |
1990s* N = 5,265 |
|---|---|---|---|---|---|---|
| Female | 1,417 (51%) | 2,043 (53%) | 2,385 (52%) | 2,368 (51%) | 3,118 (51%) | 2,718 (52%) |
| Age (years) | 72 (65, 75) | 62 (55, 66) | 53 (46, 56) | 42 (34, 46) | 31 (24, 35) | 24 (21, 27) |
| MHI-5 score | 80 (60, 88) | 80 (64, 88) | 76 (60, 84) | 76 (60, 84) | 72 (60, 84) | 72 (56, 80) |
| Very high distress (K10 29) | 82 (3.7%) | 190 (6.3%) | 243 (6.8%) | 290 (8.4%) | 407 (8.8%) | 594 (13%) |
| Employment | ||||||
| Employed | 587 (21%) | 1,993 (51%) | 3,458 (76%) | 3,646 (79%) | 4,722 (77%) | 3,779 (72%) |
| Not in labour force | 2,189 (78%) | 1,820 (47%) | 928 (20%) | 741 (16%) | 1,000 (16%) | 965 (18%) |
| Unemployed | 15 (0.5%) | 77 (2.0%) | 178 (3.9%) | 227 (4.9%) | 411 (6.7%) | 521 (9.9%) |
| Highest Ed. | ||||||
| Did not finish school | 1,252 (45%) | 1,201 (31%) | 1,213 (27%) | 808 (18%) | 1,150 (19%) | 1,140 (22%) |
| Highschool | 1,044 (37%) | 1,728 (44%) | 2,165 (47%) | 2,292 (50%) | 3,147 (51%) | 2,965 (56%) |
| College | 490 (18%) | 960 (25%) | 1,184 (26%) | 1,511 (33%) | 1,832 (30%) | 1,160 (22%) |
| Chronic illness | 1,524 (55%) | 1,518 (39%) | 1,348 (30%) | 999 (22%) | 1,011 (16%) | 945 (18%) |
| Relationship | ||||||
| Married/De Facto | 1,889 (68%) | 2,750 (71%) | 3,258 (71%) | 3,197 (69%) | 3,551 (58%) | 2,346 (45%) |
| Separated/Divorced/Widowed | 774 (28%) | 866 (22%) | 778 (17%) | 427 (9.3%) | 213 (3.5%) | 37 (0.7%) |
| Single | 127 (4.6%) | 271 (7.0%) | 528 (12%) | 989 (21%) | 2,367 (39%) | 2,881 (55%) |
*n (%); Median (IQR).
Table 1 shows later cohorts in our sample were more likely to have poorer mental health (lower MHI-5 score), higher distress, more likely to be single and unemployed, and less likely to be chronically ill or disabled.
The complete range of ages within each cohort, which includes every observation of every person in every year included in the final model, is shown in Table 2. This clearly demonstrates the overlap in age between the adjacent cohorts.
Table 2.
Age distribution by birth cohort
| Cohort | Youngest | Median | Oldest | Observations |
|---|---|---|---|---|
| 1940s | 52 | 66 | 80 | 31,871 |
| 1950s | 42 | 56 | 70 | 43,472 |
| 1960s | 32 | 46 | 60 | 48,800 |
| 1970s | 22 | 37 | 50 | 42,379 |
| 1980s | 15 | 27 | 40 | 45,391 |
| 1990s | 15 | 21 | 30 | 30,184 |
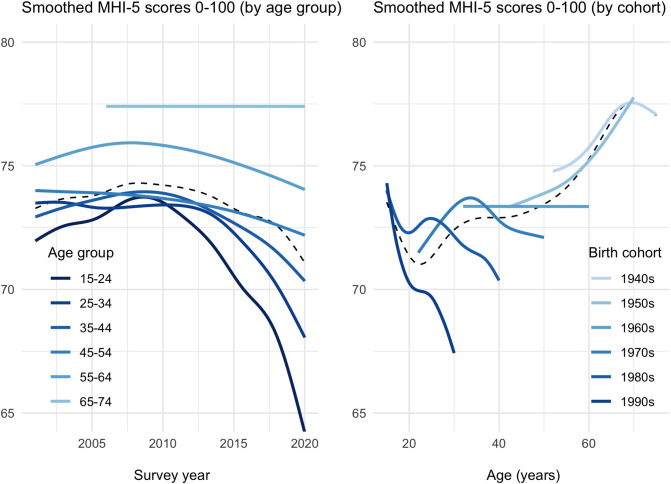
Fig. 1, Left panel shows mental health was worse for younger age groups in each survey year, but the deviations from the dotted line (average period effect) indicate this age-related discrepancy is much greater in more recent surveys—consistent with a birth cohort effect. The Fig. 1, Right shows that mental health was worse for more recent generations, where deviations from the dotted line indicate the cohort effect. In particular, Millennials (those born in the 1990s) had a lower score at the same age as earlier generations, and the later cohorts did not show the age-related improvement seen in other earlier cohorts as they aged. At age 30, the average MHI-5 score of those born in the 1990s was 67 on the 0 to 100 scale, compared to 72.5 and 74 for people born in the 1980s and 1970s, respectively.
Fig. 1.
Age and cohort effects on mental health over the past two decades. Changes in mental health scores (MHI-5) in each survey year by age group at time of survey (Left panel) and the trends in each birth cohort as it ages (Right panel), where the dotted line represents the average period effect ignoring age (Left panel) or the average age-effect ignoring cohort (Right panel). Deviations from the dotted line indicate the presence of a cohort effect in each case.
Some combinations of ages/years were not observed for all age groups (Fig. 1, Left) or cohorts (Fig. 1, Right). For example, people born prior to 1940 were excluded and so the earliest year observed for the oldest age group (65 to 74) was 2006, and the Fig. 1, Left shows the trend line for that age group does not extend earlier than 2006. Likewise, the earliest age observed of people born in the 1940s was 52, and so the trend line for that cohort does not extend earlier than that age (Fig. 1, Right).
Some trend lines in Fig. 1 are flat (e.g., Fig. 1, Left, ages 65 to 74; Fig. 1, Right, 1960s cohort), which is a result of the penalised smoothing spline determining that no additional degrees of freedom were required to support curvature to explain the variance in that group over years/ages. The Fig. 1, Left suggests that the negative effect of time (survey year) on mental health gets smaller as age increased, and for those aged 65 and above, there was no time trend. In the Fig. 1, Right, in contrast, the flat line for the 1960s cohort reflects that this is the middle point of cohorts when moving from worsening mental health with age for more recent cohorts and more distant cohorts showing improving mental health with increasing age.
Uncertainty is not quantified (e.g., CIs) in Fig. 1, but pairwise comparisons of the average difference between each cohort and the immediately prior cohort (reference cohort) is presented in Table 3. Moreover, Fig. 2 presents the difference smooths for each pairwise comparison, along with 95% confidence intervals, in order to statistically compare the trends over age between cohorts.
Table 3.
Pairwise differences in average mental health between cohorts
| Contrast | Conf.Low | Estimate | Conf.High | P.value |
|---|---|---|---|---|
| 90s to 80s | 4.094 | 3.576 | 3.059 | 0.000 |
| 80s to 70s | 2.381 | 1.603 | 0.824 | 0.000 |
| 70s to 60s | 1.594 | 0.995 | 0.395 | 0.001 |
| 60s to 50s | 1.294 | 0.790 | 0.287 | 0.002 |
| 50s to 40s | 1.326 | 0.738 | 0.150 | 0.014 |
Fig. 2.
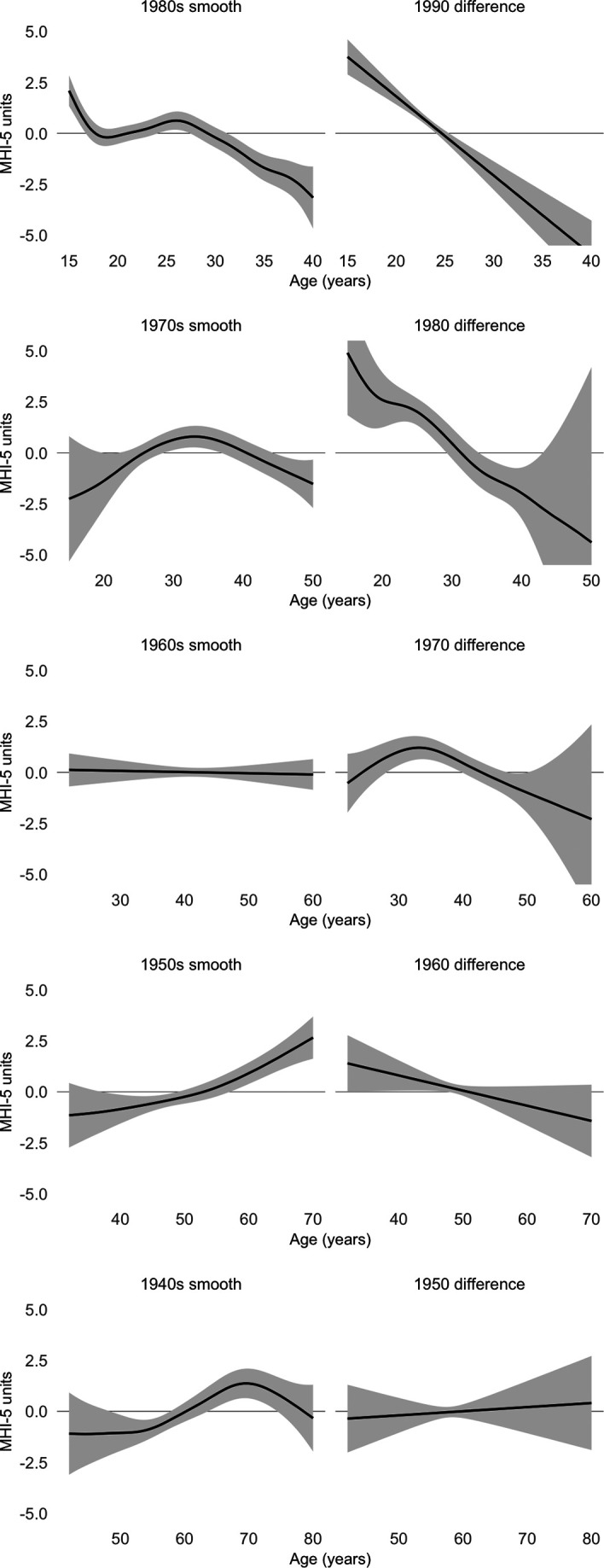
Centered smooth estimates of cohort trajectories (Left) and their differences to the subsequent cohort (Right). The shaded area represents 95% CIs which include the uncertainty about the overall mean as well as the centered smooth itself.
Table 3 shows there were significant pairwise differences between each cohort and its reference cohort (Ps .05), indicating poorer mental health scores in the later cohort of each comparison. These results represent the mean differences in MHI-5 scores of each cohort and as such interpreting these differences is difficult given the presence of age effects within each cohort. For example, the mean difference could be due to a decreasing trend with age in the later cohort, or an increasing trend in the earlier cohort, rather than differences in mental health over all ages. Pairwise comparisons of the smooth trends over age for each cohort are thus presented in Fig. 2.
Direct estimation of the (pairwise) differences between smooth trends shown in Fig. 2 reveals that the mental health of later cohorts was declining faster than earlier cohorts, adjusted for age. In each row, the earlier cohort is shown in the Left column as the “reference smooth,” and the estimated difference between the reference cohort and the cohort born in the subsequent decade is shown in the Right column as the “difference smooth.” A significant difference in trend or slope is indicated by 95% CIs which exclude zero (horizontal line) in opposite directions at each endpoint. The trend in the centered difference smooths (Fig. 2, Right) reveals whether the change in MHI-5 scores, or slope, of the later cohort is significantly different from the slope of the earlier reference cohort (Fig. 2, Left) over the same age range, i.e., a cohort effect. For example, a significant negative slope in the Right panel demonstrates MHI-5 scores were declining over time in the later cohort at a faster rate than the earlier (reference) cohort. However, a negative slope in the Right panel does not by itself indicate whether average MHI-5 scores were deteriorating in that cohort as they age. Inspection of the reference cohort in the Left panel is also necessary to determine whether the decline observed in the Right panel represents a true deterioration in mental health. For example, the 1990s difference panel (Right panel) reveals the 1990s cohort’s mental health trajectory is significantly declining with age relative to the 1980s cohort, and the 1980s smooth trend (reference in the Left panel) is also significantly deteriorating relative to its own mean baseline. Together, this represents evidence that MHI-5 scores in the 1990s cohort were declining even faster than the deteriorating mental health of the 1980s cohort. Compare this to the 1960s difference smooth in the Fig. 2, Right, where there is also a significant negative slope. Here, the trend in the 1950s reference smooth (Fig. 2, Left) is positive, so the negative difference in the Right panel was not due to changes in the 1960s cohort but rather improvement in mental health with age in the 1950s cohort. In general, no cohort shows a steeper decline relative to its reference than the 1990s cohort, and when cohorts prior to the 1990s cohort tend to decline relative to their earlier reference cohort (Fig. 2, Right), it was not due to a deterioration relative to their own mean baseline (Fig. 2, Left).
The statistical significance of the smooth differences indicates where the slope in differences between cohorts is nonzero (i.e., positive or negative). As such, they reveal the presence of cohort-effects adjusted for age. Table 4 reports relevant P-values based on Nychka (28). The P-values indicate that cohort effects existed between each of the recent adjacent cohorts, but the effect was weaker for earlier cohorts and is not evident between the earliest two cohorts examined (i.e., between the 1950s and 1940s cohorts).
Table 4.
Approximate significance of smooth differences
| Term | K-index* | Edf† | F-value | P-value |
|---|---|---|---|---|
| 1990s difference | 1.00 | 1.00 | 60.24 | 0.000 |
| 1980s difference | 1.00 | 4.37 | 8.55 | 0.000 |
| 1970s difference | 1.01 | 3.30 | 6.21 | 0.000 |
| 1960s difference | 1.00 | 1.00 | 3.27 | 0.071 |
| 1950s difference | 1.01 | 1.00 | 0.15 | 0.698 |
*Ratio of residual variance (near-neighbour/total).
†Effective degrees of freedom (increases with nonlinearity).
Sensitivity Tests.
In addition to the main analysis, we conducted several sensitivity tests for other cohort definitions, as well as period effects, alternate measures of mental illness, gender differences, social demand characteristics, and panel attrition. The full details of each are reported in SI Appendix.
We assessed the impact of our birth cohort definitions that were based on the calendar decade by testing other arbitrary cohort definitions. We re-estimated the smooth cohort differences when cohorts were defined by a birth range that commenced and ended up to 4 y earlier than the calendar decade in 1-y increments. Thus, the first definition used a range shifted by 1 y earlier than the calendar decade (e.g., the youngest cohort, nee 1990s, was born between 1989 and 1998), while the fourth and final definition used a range shifted 4 y earlier (the youngest cohort was born between 1986 to 1995). SI Appendix, Fig. S1 shows that in each new cohort definition, the younger cohorts tended to have steeper differences from the next oldest cohort, confirming greater declines in mental health with age for younger cohorts relative to older cohorts, regardless of the cohort definition.
The period effect showed a slow decline in average MHI-5 scores from 2007 but which become more exaggerated from around 2017 (e.g., dotted line in Fig. 1, Left). However, this trajectory was not the same across all age groups or cohorts. We tested sensitivity to period effects by recalculating the difference smooths between cohorts after including a linear term for year (SI Appendix, Fig. S2). Adding a linear term for year did not substantially influence the difference smooths we report in Fig. 2 (compare to SI Appendix, Fig. S2).
We tested alternate measures of mental ill-health available in the HILDA survey. We modelled the Kessler-10 [K10, (29)] psychological distress scale which was collected in the HILDA Survey in alternate years from 2007 to 2019. The corresponding psychological distress trajectories for each cohort are shown in SI Appendix, Fig. S3, where higher K10 scores represent greater psychological distress. The trajectory patterns are consistent with (and essentially the mirror image of) those observed for the MHI-5 scale in Fig. 1, Right), as psychological distress was higher for more recent cohorts than earlier cohorts at the same age. We also modelled the prevalence of mental illness defined by an MHI-5 score below 52 (30–32) and observed very similar trajectories, such that the prevalence of mental illness was higher in more recent than earlier cohorts adjusted for age (SI Appendix, Fig. S4).
We checked for any gender differences in cohort effects of mental health by estimating the smooth trends for each gender separately (SI Appendix, Fig. S5). The results for each gender were very similar to those reported for the full sample in Fig. 1. The intercepts for men and women were different, with men’s average mental health better than women’s average mental health. However, men and women have similar mental health trajectory differences between cohorts.
We also assessed the sensitivity of results to the addition of a new set of respondents that occurred in 2011 in the HILDA Survey (via a top-up sample which was performed to maintain representativeness of the survey). This was also around the same time that we start observing declines in mental health (Fig. 1, Left), and so we conducted an analysis excluding these top-up sample members. The results confirm the declining mental health trajectories were not driven by the specific respondents in the top-up sample (SI Appendix, Fig. S6).
We also checked whether trajectories were influenced by social demand characteristics of the survey. Because people may be unwilling to provide poor mental health responses, especially in an unfamiliar survey or to a new interviewer, we excluded the first survey response for each individual and reconducted the analysis. The resulting pattern of cohort differences was somewhat muted due to the loss of variation, as shown in SI Appendix, Fig. S7, but remained consistent with the main findings.
Finally, we estimated the effect of panel attrition on our main results since differences between cohorts in attrition due to poor mental health may generate the observed results. We found a small effect of poorer mental health on the probability of attrition in line with other research (33); however, the important issue is whether the dependency varies with age or cohort. We estimated the interaction between mental health and cohort on attrition, and SI Appendix, Table S1 shows that post hoc tests revealed only the 1950s cohort was more likely to suffer attrition with poorer mental health than the 1960s cohort—no other cohort comparisons were significant. We also re-estimated the smooth differences between cohorts after excluding people whose final observation was missing (i.e., due to panel attrition) and confirmed the trend in mental health was declining faster in more recent cohorts relative to earlier cohorts at the same age: SI Appendix, Fig. S8 shows the smooth differences after excluding people who are ultimately lost to attrition.
Discussion
Population mental health in Australia has been worsening over the past decade, even prior to the COVID-19 pandemic and its sequelae. This is especially the case for younger adults aged between 15 and 35 y old. Others have suggested that it is even more marked in recent adolescent cohorts (34). Although there has been much debate about the possible drivers of these trajectories of worsening mental health (35–37), it is challenging to precisely identify the source of these patterns and the assumption often is that these are temporary period effects.
Using 20 y of nationally representative, longitudinal data, we modelled the changes in mental ill-health for people born in the 1940s to the 1990s in Australia. Our flexible nonlinear model allowed us to compare mental ill-health between birth cohorts, adjusted for age, and we find that the observed deterioration in mental health in the Australian population over time is most consistent with a cohort effect rather than a temporary age or period effect. Importantly, it is those individuals from the more recent cohorts, especially the 1990s birth cohort (Millennials), who show the worst mental health trajectories over time. Individuals in this cohort report worse mental health than individuals in earlier cohorts at the same ages. Thus, the deterioration in mental health over time which has been reported in large cross-sectional surveys likely reflects cohort-specific effects related to the experiences of young people born in the Millennial generation and, to a lesser extent, those from the immediately prior cohort born in the 1980s. The findings are similar for men and women, and the results are robust to alternative samples and measures used. In fact, sensitivity analyses reported in the SI Appendix using alternative cohort definitions suggested cohort differences in mental ill-health trajectories may have begun to emerge as early as the 1960s cohort (SI Appendix, Fig. S1). If the current differences between cohorts continue, we expect the deterioration among the younger generations will worsen as they age, and furthermore, that emerging generations may suffer a similar or worse deterioration in mental health. We think these recent trends are unlikely to spontaneously resolve without addressing the new or exaggerated risks that may be differentially affecting these recent cohorts.
Findings in the international literature support our conclusions of a deterioration in mental health specific to younger generations. In the United States, Twenge et al. reported larger increases in psychological distress (K6) and suicide-related outcomes among younger cohorts born in the 1980s and 1990s than older cohorts for the period between 2010 and 2017. The difference was observed across gender and socioeconomic groups, with the largest differences among white women of high socioeconomic status (8) [see also Daly et al. (38)]. In the United Kingdom, Patalay et al. found evidence of cohort differences in depressive symptoms among adolescents (born in the early 2000s) relative to a 1990s cohort at the same age (39). Beller reports German adults born after World War II increasingly report more depressive symptoms than older generations, however only includes adults born up to 1975 (21). Thus, while cohort differences in mental ill-health may be getting worse in younger cohorts, these differences may have begun to emerge much earlier than currently thought (34). In other countries, the worsening trajectories have occurred during a period of economic expansion (i.e., post-GFC) along with declining rates of substance use (e.g., smoking, alcohol, cannabis). Likewise, Australia has experienced largely positive economic growth since 1991 until the COVID-19 pandemic in 2020, along with declining rates of substance use in younger adults. Thus, our results also support observations that the deterioration in population mental health may not reflect broad economic indicators (e.g., unemployment) or substance abuse. Others have speculated that lack of physical activity, increased weight concerns, poor sleep, and heavy social media use may be contributors (8, 39, 40); however, identifying the causal path among these factors remains to be done. Moreover, there are a number of global trends that might explain deterioration in mental health in younger generations, including climate change (41), lack of job security (42), and financial strains and unaffordable housing costs (43, 44) that are also shared across developed countries.
Many studies have investigated age-effects on subjective well-being, often measured by a single-item life-satisfaction question and also known as cognitive well-being (45). This literature typically finds evidence of a U-shaped association of life satisfaction with age, and the mental health trajectory we report also displays a similar U-shape with improvement at older ages/cohorts (Fig. 1, Right, dotted line). The presence of biased age-effects due to endogenous selection of happier people with age has been proposed as a possible source of the U-shaped happiness pattern (46). A similar confound may produce the age-cohort interaction we observe in our main results if people with poor mental health in older cohorts are more likely to suffer attrition from the HILDA survey than younger cohorts. People with poor mental health are more likely to leave the HILDA survey; however, the effects are small (33), and a sensitivity analysis that excluded people who are ultimately lost to attrition replicated the main results; i.e., the trend in mental health declined faster in more recent cohorts relative to earlier cohorts at the same age. Thus, while endogenous selection of mentally healthy people is a problem, the effect is very small and is not a source of substantial bias in our results.
We did not include major life events in our model because they can act as mediators that result from age and affect the response variable (i.e., MHI-5 scores) (47). We also did not include other potential mediators of the effect of age on mental ill-health such as health status, relationship status, employment status, household income, or region. As such, our results should be considered a description of the total effect of age on mental health, rather than providing a causal explanation of the individual drivers of such trajectories. Our aim here was to describe the cohort-related differences rather than explain them. Likewise, our aim was not to build a prediction model to extrapolate beyond the range of data, and instead, we prefer to note the expansion of the appropriately adjusted 95% CIs when estimating future observations for any particular cohort.
This study provides a starting point for more in-depth analysis, and we hope it will encourage other researchers to more closely examine the changes that have happened in mental ill-health in Australia in the last decade. This is apparent from the trends depicted in the Fig. 1, Left showing the divergence in mental health beginning roughly at the same time the 1990s cohort would have entered the survey for the first time. Future research should aim to identify and build understanding of the causes of these patterns, such as whether later cohorts are less resilient to similar risk factors experienced by earlier cohorts or whether they experience more and/or a greater severity of risks for mental ill-health. Such evidence is critical if the deteriorating pattern of mental health is to be arrested or shifted.
Materials and Methods
Data and Study Design.
This analysis draws on 20 annual waves of longitudinal data from the Household Income and Labour Dynamics in Australia survey. The HILDA Survey is a nationally representative household panel (aside from those in very remote Australia and those in nonprivate dwellings) that commenced in 2001 with 13,969 participants within 7,682 households. The study design follows all original household members over time, includes people who join households in which an original household member resides, and included a top-up sample (adding an additional 2,153 households) in 2011. Attrition rates from the study are low by international standards, with the reinterview rate increasing from 87% in wave 2, to over 95% in wave 8 and subsequently.
At each wave, data are collected through a face-to-face interview (with an option for a telephone survey) and a separate self-completion questionnaire (SCQ). Given the key measures in the current study are drawn from the SCQ, the current sample is limited to those who completed the SCQ in a given year. For this analysis, the birth cohort of each person was defined by the decade of birth year (1940s, 1950s, 1960s, 1970s, 1980s, and 1990s). Thus, persons can only contribute to a single birth cohort but can be observed multiple times across survey years/ages. Persons were excluded if they were born prior to 1940 or after 1999 due to inadequate sample sizes. Demographic details of the sample are provided in Table 1.
Mental Ill-Health Measurement.
The MHI-5 is a subscale of five items assessing positive and negative aspects of mental health from the SF-36 (48, 49). It is well validated as a screening instrument or dichotomised to provide a proxy of common mental disorders in population research (31, 50, 51), including in Australia (30). Respondents are asked to state how often they have experienced each of the following during the past 4 wk:
“Been a nervous person”
“Felt so down in the dumps nothing could cheer you up”
“Felt calm and peaceful”
“Felt down”
“Been a happy person”
The response to each item was selected from a 6-point scale “All of the time,” “Most of the time,” “A good bit of the time,” “Some of the time,” “A little of the time,” “None of the time.” The scale was created according to Ware et al. (32). Each response was scored 0 to 5, and items were recoded so that higher scores indicated better mental health. Raw scores were summed across the items and then linearly transformed to a 0 to 100 scale. In accordance with the manual, a person-specific score was estimated in any year in which there were valid responses on three or more items, the average being calculated and applied to missing items.
In sensitivity analysis, we repeat the key analysis using the 10-item Kessler scale of psychological distress [K10, (29)] that has been included in every second wave of the HILDA Survey since 2007.
Analysis.
We estimate penalized smooth trends for each cohort using restricted maximum likelihood (REML) in a generalized additive mixed modelling (GAMM) setting (52–55). This is an analogue to a linear multilevel model with varying intercepts and slopes among the cohorts, but here, the slopes are allowed to “wiggle.” The model includes a global smoothing term for the effect of age as well as cohort-specific terms, so each cohort is allowed to have its own functional response, but the penalty ensures that functions too far from average are penalized.
Each smoother is represented by a sum of simpler, fixed basis functions. The basis functions (splines) were estimated by quadratically penalized likelihood maximization for automatic smoothness selection, with a starting value of :
where is the continuous MHI-5 score for each person over age ; is the mean MHI-5 estimate for each birth cohort, after accounting for variations in trend over age; and are smooth functions for the trend in MHI-5 scores over age for each cohort.
The smooth trends were centered for identifiability reasons (56, 57); however, the resulting model estimation allowed two important comparisons: First, the mean MHI-5 estimates () provided comparisons for the average difference in mental health between cohorts. However, interpreting these differences is difficult in the presence of trends over age in each cohort. For example, a mean difference could be due to a decreasing trend with age in one cohort or an increasing trend in the other cohort, rather than consistent differences in mental health over the age range. Thus, an important advantage provided by the current model is the centered smooth functions from which differences in trends between cohorts are directly estimated. The resulting difference smooths are also centered around zero, and so mean differences in mental health are not accounted for by these smooths, but they will reveal whether mental health is changing with age in one cohort relative to the other reference cohort. The difference smooths also directly estimate the uncertainty around the difference, with CIs that include the uncertainty about the mean difference as well as the centered smooth itself. This results in intervals with close to nominal (frequentist) coverage probabilities (56).
We did not compare cohorts more than a decade apart since there are few or no overlapping age groups observed, so we restricted ourselves to the five () pairwise comparisons between each cohort and the next oldest cohort (i.e., the reference cohort).
To account for the person-level dependency when survey participants are measured more than once, we included a first-order autoregressive AR(1) term for the residuals based on the unique cross-wave ID for each person , which is equivalent to including the person-level random intercept nested within cohort. In sensitivity analyses, we explored the impact of alternate cohort definitions, as well as the influence of period effects, sex, and first interview, and performed comparisons with mental illness and psychological distress. The results are presented in SI Appendix.
Supplementary Material
Appendix 01 (PDF)
Acknowledgments
This paper uses unit record data from the HILDA Survey conducted by the Australian Government Department of Social Services (DSS) https://doi.org/10.26193/YP7MNU. The findings and views reported in this paper, however, are those of the authors and should not be attributed to the Australian Government, DSS, or any of DSS’ contractors or partners. This research was supported by the Australian Government through the Australian Research Council’s Centre of Excellence for Children and Families over the Life Course (Project ID CE200100025).
Author contributions
F.B., R.W.M., P.B., and N.G. designed research; R.W.M. performed research; R.W.M. contributed new reagents/analytic tools; R.W.M. analyzed data; and F.B., R.W.M., P.B., and N.G. wrote the paper.
Competing interests
The authors declare no competing interest.
Footnotes
This article is a PNAS Direct Submission.
Data, Materials, and Software Availability
Code to generate the main analyses and Figs. 1 and 2, along with software libraries and the model fit objects generated by the main analyses data have been deposited in Github (https://github.com/datarichard/the-kids-are-alright) (58). The full dataset used in this report is available by application to the Australian Government Department of Social Services https://dataverse.ada.edu.au/dataverse/DSSLongitudinalStudies) (59).
Supporting Information
References
- 1.Australian Bureau of Statistics, National Health Survey: First Results (ABS, 2018).
- 2.Australian Bureau of Statistics, National Study of Mental Health and Wellbeing (ABS, 2022).
- 3.Peach N., et al. , The mental health of adolescents and young people experiencing traumatic stress and problematic substance use. Drug Alcoh. Rev. 41, 16–17 (2022). [Google Scholar]
- 4.Butterworth P., Watson N., Wooden M., Trends in the prevalence of psychological distress over time: Comparing results from longitudinal and repeated cross-sectional surveys. Front. Psy. 11, 1345 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hidaka B. H., Depression as a disease of modernity: Explanations for increasing prevalence. J. Affect. Disord. 140, 205–214 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nishi D., Susukida R., Usuda K., Mojtabai R., Yamanouchi Y., Trends in the prevalence of psychological distress and the use of mental health services from 2007 to 2016 in Japan. J. Affect. Disord. 239, 208–213 (2018). [DOI] [PubMed] [Google Scholar]
- 7.Ormel J., Hollon S. D., Kessler R. C., Cuijpers P., Monroe S. M., More treatment but no less depression: The treatment-prevalence paradox. Clin. Psychol. Rev. 91, 102111 (2022). [DOI] [PubMed] [Google Scholar]
- 8.Twenge J. M., Cooper A. B., Joiner T. E., Duffy M. E., Binau S. G., Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J. Abnor. Psychol. 128, 185 (2019). [DOI] [PubMed] [Google Scholar]
- 9.S. B. Patten et al., Major depression in Canada: What has changed over the past 10 years? Can. J. Psych. 61, 80–85 (2016). [DOI] [PMC free article] [PubMed]
- 10.Butterworth P., Schurer S., Trinh T. A., Vera-Toscano E., Wooden M., Effect of lockdown on mental health in Australia: Evidence from a natural experiment analysing a longitudinal probability sample survey. Lancet Public Heal. 7, e427–e436 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glozier N., Morris R., Schurer S., What happened to the predicted Covid-19-induced suicide epidemic, and why? Aust. New Zeal. J. Psych. 57, 11–16 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baxter A. J., et al. , Challenging the myth of an “epidemic’’ of common mental disorders: Trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress. Anxiet. 31, 506–516 (2014). [DOI] [PubMed] [Google Scholar]
- 13.Ferrari A. J., et al. , Burden of depressive disorders by country, sex, age, and year: Findings from the global burden of disease study 2010. PLoS Med. 10, e1001547 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vos T., et al. , Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1545–1602 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Steptoe A., Deaton A., Stone A. A., Subjective wellbeing, health, and ageing. Lancet 385, 640–648 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stone A. A., Schwartz J. E., Broderick J. E., Deaton A., A snapshot of the age distribution of psychological well-being in the United States. Proc. Natl. Acad. Sci. U.S.A. 107, 9985–9990 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burns R. A., Butterworth P., Crisp D. A., Age, sex and period estimates of Australia’s mental health over the last 17 years. Aust. New Zeal. J. Psych. 54, 602–608 (2020). [DOI] [PubMed] [Google Scholar]
- 18.Bell A., Age period cohort analysis: A review of what we should and shouldn’t do. Ann. Hum. Biol. 47, 208–217 (2020). [DOI] [PubMed] [Google Scholar]
- 19.Fienberg S. E., Mason W. M., Identification and estimation of age-period-cohort models in the analysis of discrete archival data. Sociol. Methodol. 10, 1–67 (1978). [Google Scholar]
- 20.Mason W. M., Fienberg S., Cohort Analysis in Social Research: Beyond the Identification Problem (Springer Science & Business Media, 1985). [Google Scholar]
- 21.Beller J., Age-period-cohort analysis of depression trends: Are depressive symptoms increasing across generations in Germany? Euro. J. Ageing 19, 1493–1505 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Ours J. C., What a drag it is getting old? Mental health and loneliness beyond age 50 Appl. Econ. 53, 3563–3576 (2021). [Google Scholar]
- 23.Kino S., Jang Sn., Gero K., Kato S., Kawachi I., Age, period, cohort trends of suicide in Japan and Korea (1986–2015): A tale of two countries. Soc. Sci. Med. 235, 112385 (2019). [DOI] [PubMed] [Google Scholar]
- 24.Martínez-Alés G., et al. , Age, period, and cohort effects on suicide death in the United States from 1999 to 2018: Moderation by sex, race, and firearm involvement. Mol. Psych. 26, 3374–3382 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo L., Hodges J. S., Constraints in random effects age-period-cohort models. Sociol. Methodol. 50, 276–317 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo L., Assessing validity and application scope of the intrinsic estimator approach to the age-period-cohort problem. Demography 50, 1945–1967 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fienberg S. E., Cohort analysis’ unholy quest: A discussion. Demography 50, 1981–1984 (2013). [DOI] [PubMed] [Google Scholar]
- 28.Nychka D., Bayesian confidence intervals for smoothing splines. J. Am. Stat. Assoc. 83, 1134–1143 (1988). [Google Scholar]
- 29.Kessler R. C., et al. , Screening for serious mental illness in the general population. Archives General Psych. 60, 184–189 (2003). [DOI] [PubMed] [Google Scholar]
- 30.Batterham P., Sunderland M., Slade T., Calear A., Carragher N., Assessing distress in the community: Psychometric properties and crosswalk comparison of eight measures of psychological distress. Psychol. Med. 48, 1316–1324 (2018). [DOI] [PubMed] [Google Scholar]
- 31.Rumpf H. J., Meyer C., Hapke U., John U., Screening for mental health: Validity of the MHI-5 using DSM-IV axis i psychiatric disorders as gold standard. Psych. Res. 105, 243–253 (2001). [DOI] [PubMed] [Google Scholar]
- 32.Ware J., Snow K., Kosinski M., Sf-36 Version 2 Health Survey: Manual and Interpretation Guide (Qualilty Metric Inc., Lincoln, Rhode Island, Manual, 2000). [Google Scholar]
- 33.Perales Perez F., Baffour B., Respondent mental health, mental disorders and survey interview outcomes. Survey Res. Methods 12, 161–176 (2018). [Google Scholar]
- 34.J. Haidt, J. Twenge, Adolescent mood disorders since 2010: A collaborative review (2023).
- 35.S. B. Patten et al., Why is major depression prevalence not changing? J. Affect. Disord. 190, 93–97 (2016). [DOI] [PubMed]
- 36.Jorm A. F., Patten S. B., Brugha T. S., Mojtabai R., Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries World Psych. 16, 90–99 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mulder R., Rucklidge J., Wilkinson S., Why has increased provision of psychiatric treatment not reduced the prevalence of mental disorder. Austral. New Zeal. J. Psych. 51, 1176–1177 (2017). [DOI] [PubMed] [Google Scholar]
- 38.Daly M., Sutin A. R., Robinson E., Longitudinal changes in mental health and the Covid-19 pandemic: Evidence from the UK household longitudinal study. Psychol. Med. 52, 2549–2558 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Patalay P., Gage S. H., Changes in millennial adolescent mental health and health-related behaviours over 10 years: A population cohort comparison study. Int. J. Epidemiol. 48, 1650–1664 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giuntella O., Hyde K., Saccardo S., Sadoff S., Lifestyle and mental health disruptions during Covid-19. Proc. Natl. Acad. Sci. U.S.A. 118, e2016632118 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Obradovich N., Migliorini R., Paulus M. P., Rahwan I., Empirical evidence of mental health risks posed by climate change. Proc. Natl. Acad. Sci. U.S.A. 115, 10953–10958 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.S. Hardy, Modern work: How changes to the way we work are impacting Australians’ mental health. (Black Dog Institute Sydney, White paper) (2021).
- 43.Baker E., Lester L., Mason K., Bentley R., Mental health and prolonged exposure to unaffordable housing: A longitudinal analysis. Soc. Psych. Psychiat. Epidemiol. 55, 715–721 (2020). [DOI] [PubMed] [Google Scholar]
- 44.Singh A., Aitken Z., Baker E., Bentley R., Do financial hardship and social support mediate the effect of unaffordable housing on mental health? Soc. Psych. Psychiat. Epidemiol. 55, 705–713 (2020). [DOI] [PubMed] [Google Scholar]
- 45.Diener E., et al. , Findings all psychologists should know from the new science on subjective well-being. Can. Psychol./Psychol. Can. 58, 87 (2017). [Google Scholar]
- 46.F. Kratz, J. Brüderl, The age trajectory of happiness. PsyArXiv [Preprint] (2021). https://osf.io/preprints/psyarxiv/d8f2z/ (Accessed 6 December 2022).
- 47.Kettlewell N., et al. , The differential impact of major life events on cognitive and affective wellbeing. SSM-Popul. Heal. 10, 100533 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ware J. E. Jr., Sf-36 health survey update. Spine 25, 3130–3139 (2000). [DOI] [PubMed] [Google Scholar]
- 49.Ware J. E. Jr., Sherbourne C. D., The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med. Care 30, 473–483 (1992). [PubMed] [Google Scholar]
- 50.Cuijpers P., Smits N., Donker T., Ten Have M., de Graaf R., Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item mental health inventory. Psych. Res. 168, 250–255 (2009). [DOI] [PubMed] [Google Scholar]
- 51.Hoeymans N., Garssen A. A., Westert G. P., Verhaak P. F., Measuring mental health of the Dutch population: A comparison of the GHQ-12 and the MHI-5. Heal. Qual. Life Outcomes 2, 1–6 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wood S. N., Stable and efficient multiple smoothing parameter estimation for generalized additive models. J. Am. Stat. Assoc. 99, 673–686 (2004). [Google Scholar]
- 53.Wood S. N., Low-rank scale-invariant tensor product smooths for generalized additive mixed models. Biometrics 62, 1025–1036 (2006). [DOI] [PubMed] [Google Scholar]
- 54.Wood S. N., Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. J. R. Stat. Soc.: Ser. B (Stat. Methodol.) 73, 3–36 (2011). [Google Scholar]
- 55.Wood S. N., Pya N., Säfken B., Smoothing parameter and model selection for general smooth models. J. Am. Stat. Assoc. 111, 1548–1563 (2016). [Google Scholar]
- 56.Marra G., Wood S. N., Coverage properties of confidence intervals for generalized additive model components. Scand. J. Stat. 39, 53–74 (2012). [Google Scholar]
- 57.Wood S. N., On P-values for smooth components of an extended generalized additive model. Biometrika 100, 221–228 (2013). [Google Scholar]
- 58.R. W. Morris, the-kids-are-alright. Github. https://github.com/datarichard/the-kids-are-alright. Deposited 16 May 2023.
- 59.Australian Government Department of Social Services (DSS). Household, Income and Labour Dynamics in Australia (HILDA) Survey, GENERAL RELEASE 20 (Waves 1-20). Dataverse. https://dataverse.ada.edu.au/dataverse/DSSLongitudinalStudies. Accessed 29 November 2021.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 01 (PDF)
Data Availability Statement
Code to generate the main analyses and Figs. 1 and 2, along with software libraries and the model fit objects generated by the main analyses data have been deposited in Github (https://github.com/datarichard/the-kids-are-alright) (58). The full dataset used in this report is available by application to the Australian Government Department of Social Services https://dataverse.ada.edu.au/dataverse/DSSLongitudinalStudies) (59).