Abstract
Metacarpal fractures are common and may require operative treatment; however, there is no gold standard fixation technique. K-wires are used for simplicity and flexibility but require immobilization and can lead to complications. Dorsal plating provides greater stability than K-wires but is subject to its own limitations. Intramedullary threadless nails have reduced time to union and improved range of motion (ROM) but may not provide the stability of plating. Intramedullary screws allow rapid return to activity and increased stability; however, compression forces may shorten metacarpals, producing non-anatomic reduction.
The ExsoMed INnateTM threaded intramedullary nail (ExsoMed, Aliso Viejo, CA, USA) was developed with tall threads, a diameter fitting the metacarpal canal cortical purchase, stability, and no compression to prevent fracture displacement and shortening. We designed a prospective study to evaluate INnateTM nail fixation in metacarpal fractures. Visual analog scale (VAS) pain score, total active motion (TAM), radiographic union, and return to normal activity were recorded at each postoperative visit. Descriptive statistics were performed for endpoints.
Fifty-eight patients were included with a median age of 38.7 years. The INnateTM nail was used in 80 fractured metacarpals. The 4th and 5th metacarpals were most frequently involved. The most common mechanisms of injury were blunt trauma and motor vehicle collisions. Approximately 31% of patients had multiple, concurrent fractures (16 patients required two nails; two required three nails). The mean follow-up was 9.9 weeks. The mean time to radiographic union was 9.1 weeks. The final visual analog scale (VAS) pain score was 1.1. The mean time to return to work and/or normal activities was 9.7 weeks, and the mean percentage of normal activity resumed was 89.1%.
Keywords: threaded intramedullary nail, intramedullary nail, intramedullary fixation, metacarpal fracture fixation, metacarpal fracture
Introduction
Metacarpal fractures are common, particularly among young males (age 10-40), comprising 30% of all hand fractures and 18% of all below-elbow fractures in the United States [1,2]. Despite their frequent occurrence, treatment modalities for metacarpal fractures are varied and continue to evolve. While many metacarpal fractures can be treated nonoperatively, there is a growing tendency to choose operative treatment as it may prevent deformity and mobility deficits in these often young and active patients [3]. Fixation techniques vary by patient characteristics and type of fracture [4].
Historically, percutaneous K-wires have been used due to their simplicity [5-9]. Unfortunately, these can tether the surrounding tissue, especially the sagittal bands, limiting the range of motion (ROM) in the early stages (up to 3-4 months) of healing and rehabilitation [4]. Pin tract infections also remain a risk of K-wire fixation [4]. Dorsal metacarpal plating has been used as a straightforward alternative to K-wires pinning. Plating offers greater stability but has been associated with complication rates as high as 35% including tendon adhesion, persistent stiffness, hardware failure, and infection [6-9].
Given the limitations of K-wires and dorsal plating, Gonzalez et al. developed a technique using pre-bent, flexible intramedullary nails for internal stabilization of metacarpal fractures [10]. This technique was improved by Orbay and Touhami by adding a locking pin to the proximal end of the nail [5]. Outcomes of this fixation technique compare favorably to K-wire fixation with an average time to union of 6.3-8.0 weeks and a 16-day earlier return to work [3,4,11,12].
More recently, intramedullary compression screws have been used to hold reduction and prevent rotational instability. These headless screws are buried within the metacarpal and do not need to be removed. Intramedullary compression screws allow for early mobilization (5 days or earlier) while providing fixation strength comparable to traditional techniques [13]. Early studies evaluating this technique have shown improved functional outcomes [13-22].
The INnateTM threaded intramedullary nail (ExsoMed, Aliso Viejo, CA, USA) was developed with increased thread height and diameter comparable to metacarpals to create cortical purchase and stability. Increased thread pitch was added to control rotation and speed up insertion and extraction. Non-compressive thread design was added to prevent shortening and fracture displacement during device insertion. Threaded intermedullary nails have previously been shown to have improved rotational stability when compared to K-wire fixation, with a higher load to failure [23]. Currently, very few studies exist that compare INnateTM intramedullary nails to other more commonly used techniques. Given the paucity of data on this novel product and the lack of consensus gold standard fixation methods, we designed a prospective study evaluating the utility of the INnateTM intramedullary threaded nail in metacarpal fracture fixation.
Indications for use of the INnateTM nail include, but are not limited to fixation of intra-articular and extra-articular fractures and non-of small bones and bone fragments in the scaphoid, carpals, metacarpals, tarsals, and metatarsals. Contraindications for the use of INnateTM Nail fixation include active or latent infection or sepsis, insufficient quantity or quality of bone and/or soft tissue to support fixation, and suspicion of material sensitivity.
Materials and methods
Approval was obtained from the Texas Tech University Health Sciences Center (TTUHSC) Lubbock/Odessa Institutional Review Board (approval number: L20-034), and appropriate informed consent as well as any necessary HIPAA consent was obtained. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Fifty-eight patients (80 fractured metacarpals) were treated with INnateTM intramedullary nail fixation and were prospectively included in our study (Table 1).
Table 1. Distribution of metacarpal fractures in the INnateTM intramedullary nail cohort.
INnateTM threaded intramedullary nail (ExsoMed, Aliso Viejo, CA, USA).
| Placement | Number Injured |
| 2nd Metacarpal | 9 (11.3%) |
| 3rd Metacarpal | 10 (12.5%) |
| 4th Metacarpal | 30 (37.5%) |
| 5th Metacarpal | 31 (38.8%) |
| Total: | 80 (100%) |
| Injuries involving multiple metacarpals | Number of Patients |
| 4th & 5th Metacarpals | 12 |
| 3rd & 4th Metacarpals | 2 |
| 2nd & 3rd Metacarpals | 2 |
| 2nd, 3rd, & 4th Metacarpals | 1 |
| 3rd, 4th, & 5th Metacarpals | 1 |
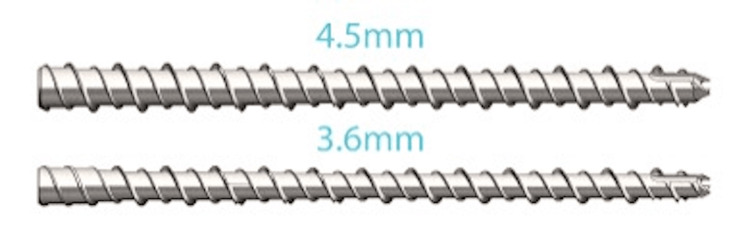
The surgical repair involved the use of either a 3.6 or 4.5mm INnateTM nail, with nail lengths varying from 25 to 65 mm (Figure 1). The surgical technique involved longitudinal incision of the skin, extensor tendon, and capsule. In accordance with the INnateTM surgical technique guide, a K-wire was used to measure the length of each metacarpal and provide preliminary fixation. Appropriate INnateTM nails were then selected, and placed under fluoroscopic guidance (Figure 2). Fluoroscopic evaluation and intraoperative physical exam including gross inspection and wrist tenodesis were performed to evaluate for correct metacarpal rotation.
Figure 1. INnateTM intramedullary threaded nails.
INnateTM threaded intramedullary nail (ExsoMed, Aliso Viejo, CA, USA).
Figure 2. Intraoperative fluoroscopic image.
The image shows INnateTM intramedullary threaded nail placement in the fourth and fifth metacarpals.
Data was collected at routine follow-up visits. Outcome measures included visual analog scale (VAS) pain scores, total active motion (TAM), time to radiographic union, and return to normal activities. Descriptive statistics were performed to evaluate endpoints.
Results
A total of 58 patients (41 males, 17 females) were included. Median age was 38.7 (range: 14-88). 80 fractured metacarpals were treated with ExsoMed INnateTM intramedullary nailing. The 4th (37.5%) and 5th (38.8%) metacarpals were the most commonly injured. The most common mechanism of injury was blunt trauma, followed by motor vehicle collision (Table 1). Approximately 31% of patients had multiple, concurrent metacarpal fractures (16 patients required two nails; two patients required three nails) (Table 1). Two patients had concurrent fractures that required fixation across the carpometacarpal (CMC) joint, one with a proximal 4th metacarpal fracture and one with a displaced intra-articular 5th metacarpal base fracture, in which both nails were advanced into the hamate for stability.
The mean follow-up interval was 9.9 weeks (range: 0.9-68.7 weeks). The final VAS pain score was 1.1 (range: 0-7). 60% of patients had 100% TAM, 16% had 90-99% TAM, 14% had 75-89% TAM, 4% had 50-74% TAM, and 6% had 25-49% TAM (Table 2). The mean time to radiographic union was 9.1 weeks (range: 5-23 weeks). The mean time to return to work and/or normal activities was 9.7 weeks (range: 1-25.6 weeks), and the mean percentage of normal activity resumed was 89.1% (range: 25-100%).
Table 2. Outcomes of INnateTM intramedullary threaded nail fixation for metacarpal fractures at mean follow-up of 9.9 weeks.
NnateTM threaded intramedullary nail (ExsoMed, Aliso Viejo, CA, USA).
| Variable | Mean ± St. Dev. |
| (Number of fractures) | (Range) |
| Radiographic union (weeks) | 9.1 ± 3.8 |
| (n = 45) | (5-23) |
| VAS Pain (points) | 1.1 ± 2.1 |
| (n = 68) | (0-7) |
| Mean % Total Active Motion (TAM) | 88.7 ± 19.6 % |
| (n = 50) | (25-100) |
| 100% TAM | 60% |
| 90-99% TAM | 16% |
| 75-89% TAM | 14% |
| 50-74% TAM | 4% |
| 25-49% TAM | 6% |
| % Normal Activity Resumed | 93.3 ± 14.3 % |
| (n = 41) | (25-100) |
| Return to Work/Daily Activities | 9.7 ± 5.3 weeks |
| (n = 36) | (1-25.6) |
There were no complications or revision procedures related to fracture fixation in our cohort. Thorough evaluation for infection, bone quantity and quality, and relevant soft tissue structures may mitigate the risk of complications.
Discussion
Metacarpal fractures are classified as open, closed, intra- or extra-articular and described as oblique, transverse, spiral, or comminuted. The degree of angulation is an important consideration of the treatment algorithm as each metacarpal can tolerate a different amount of angulation before operative care is recommended. The ring and middle fingers tolerate the least amount of angulation, which can be as low as 10° [24]. There is some physiologic compensation for angulation via hyperextension of the metacarpophalangeal (MCP) joint, however, as angulation increases, there is an inverse relation to the force generated at the proximal interphalangeal joint. This decrease in force leads to an extensor lag, also known as pseudoclawing [24]. Another consideration is the shortening of the fractured metacarpal which can create problems for the extensor mechanism.
Intra-articular fractures and fractures resulting in malrotation require special consideration. In the case of malrotation, there can be prominent flexor dysfunction leading to scissoring of the fingers when making a fist. Each degree of rotation at the metacarpal can have as much as 1.5cm overlap among fingers when making a closed fist [24]. Operative treatment has been recommended for intra-articular fractures in which 25% of the articular surface is involved or a step-off of 2 mm or more is present [24].
Current fixation techniques can be limited in their utility to provide satisfactory outcomes, particularly in cases where metacarpal shortening is of concern. Percutaneous pinning with K-wires has commonly been used for internal fixation of metacarpal fractures due to ease of availability and simplicity (Table 3) [5-9]. However, K-wires are associated with several complications including infection, loss of reduction, symptomatic non-union, and pin loosening [4]. They are limited in their utility to treat spiral or comminuted fractures [25]. Decreased construct rigidity often necessitates immobilization with a protective splint or cast, which can delay the range of motion and rehabilitation compared to other fixation techniques [24].
Table 3. Intramedullary nail or K-wire fixation outcomes for metacarpal fractures.
| Reference | Number of Fractures | VAS Pain (Range) | Total Active Motion (Range) | Grip Strength (Range) | Radiographic Union (Range) | Return to Daily Activities (Range) |
| Orbay and Touhami, 2006 [5] - 1.1 or 1.6-mm flexible non-locking intramedullary nail | 34 | 1.4 (1-2.5) | 239 (230-270) | 89% | 5.9 weeks | n/a |
| Orbay and Touhami, 2006 [5] - 1.1 or 1.6-mm flexible locking intramedullary nail | 76 | 1.3 (1-2.75) | 244 (225-275) | 92% | 5.6 weeks | n/a |
| Ozer et al., 2008 [6] - Intramedullary nailing (Hand Innovations, Inc.) | 38 | n/a | 237 (150-270) | n/a | 5.4 weeks | |
| Facca et al., 2010 [7] - 1.6 or 2-mm intramedullary K-wire | 20 | 0.9 | 97.7% | 92.9% | n/a | 8.1 weeks |
| Fujitani et al., 2012 [8] - 2 x 1.2-mm intramedullary K-wires with bouquet technique | 15 | n/a | 94% | 67% | 2.3 months | 2.3 months |
| Dreyfuss et al., 2019 [9] - 1 or 2 x 1.2-mm intramedullary K-wires | 39 | n/a | 92.7% | 83% (40-110) | 7.1 weeks (4-41) |
As previously mentioned, plate fixation is more stable than percutaneous pinning with K-wires, and can address a variety of fracture patterns including spiral, long oblique, short oblique, and transverse fractures (Table 4) [6-9]. Additionally, dorsal plating has resulted in improved ROM when compared to K-wires [26]. One study showed mini-plates have a slightly shorter union time (11.80 versus 12.95 weeks) and non-statistically significant lower rates of complication (including infection, implant loosening, loss of reduction, and stiffness) when compared to K-wire fixation [27]. Yet, complications have been reported as high as 36% following plate fixation of metacarpal and phalangeal fractures, leaving up to 34% of patients with extensor lag or stiffness and 19% with MCP or proximal interphalangeal (PIP) contracture [28]. A more recent study noted stiffness as the most frequent complication, occurring in 40% of patients [29]. This is likely due to the open nature of plate fixation and plate to soft tissue interaction which can lead to increased scar tissue and adhesions [1].
Table 4. Plate fixation outcomes for metacarpal fractures.
| Reference | Number of Fractures | VAS Pain (Range) | Total Active Motion (Range) | Grip Strength (Range) | Radiographic Union (Range) | Return to Daily Activities (Range) |
| Ozer et al., 2008 [6] - Plate-screw fixation (Synthes) | 14 | n/a | 228o (150-270) | n/a | 5.2 weeks (4-7) | |
| Facca et al., 2010 [7] - Locking plates (Aptus Hand®, MédartisTM) | 18 | 0.94 | 58.7% | 88.4% | n/a | 7.4 weeks |
| Fujitani et al., 2012 [8] - Low profile plates | 15 | n/a | 96% | 86% | 2.0 months | n/a |
| Dreyfuss et al., 2019 [9] - Locking plates (Variable Angle Locking Hand System, Depuy Synthes & Hand Fracture System, Acumed) | 35 | n/a | 98.0% | 93% (42-125) | 8.4 weeks (5.3-15) |
Intramedullary nail fixation provides increased stability compared to K-wire fixation (Table 4) [4,6-9]. When compared to K-wires, intramedullary nails provided earlier recovery of ROM, earlier return to work, and decreased complication rates [4]. One retrospective study of 66 metacarpal fractures fixated with intramedullary nails reported an average union time of seven weeks, with nine (14%) delayed unions (>three months) and no non-unions [3]. There were three cases (5%) of nail migration, two cases of skin impingement (3%), two cases (3%) of rotational deformities, and one infection (2%) [3].
Compression screws have significant advantages over percutaneous K-wires and open reduction and internal fixation (ORIF) techniques (Table 5) [14-22]. One notable improvement is the ability to provide increased stability in simple fractures [13,30]. Multiple studies have demonstrated that early ROM and adequate time to radiographic union can be achieved without immobilization (Table 5) [13-21,30]. A study of 91 patients who were treated with headless intramedullary screws reported that all patients achieved full active MCP motion at most recent follow-up, with an average grip strength of 104.1% of the contralateral hand. Active motion was initiated 5 days postoperatively, and mean time to radiographic union was 6 weeks [30]. Despite promising outcomes data, some studies have questioned the stability of these screws in some fracture patterns. A cadaveric study compared the biomechanical stability of compression screws to other fixation techniques and found significantly lower load at failure and lower number of cycles to failure during a cyclic loading protocol [31]. Another study found that in unstable metacarpal fractures, dorsal plating was found to provide superior stability when compared to compression screws [32].
Table 5. Intramedullary screw fixation outcomes for metacarpal fractures.
| Reference | Number of Fractures | VAS Pain (Range) | Total Active Motion (TAM) | Grip Strength (Range) | Radiographic Union (Range) | Return to Daily Activities (Range) |
| Boulton et al., 2010 [14] - 3.0-mm cannulated headless compression screw; length, 45 mm (Synthes) | 1 | n/a | 80o Flexion, Complete extension | n/a | By 12 weeks | By 6 weeks |
| Doarn et al., 2014 [15] - 3.0-mm cannulated headless screw; length, 40 mm (Synthes); long thread for neck, short thread for shaft | 9 | 0 | 100% | 98% | 7 weeks (4-12) | 6 weeks (4-10) |
| Ruchelsman et al., 2014 [16] - 2.4-mm or 3.0-mm headless compression screw; length NA (Synthes) | 39 | n/a | 100% | 105% (58-230) | By 6 weeks | n/a |
| del Piñal et al., 2015 [17] - 3.0-mm headless cannulated screw; length, 40 mm or 4.0-mm; length 50 mm for fifth metacarpal (Small Bone Innovations) | 48 | n/a | 249o | n/a | n/a | 11 weeks (3.5-64.5) |
| Tobert et al., 2016 [13] - 3.0-mm partially threaded; length, 32–45 mm (Synthes) | 18 | n/a | All >240o | n/a | n/a | n/a |
| Lee et al., 2017 [18] - 3.0-mm headless compression screw; length to fit in head only (Synthes) | 5 | n/a | 265o | n/a | 5 weeks (5-7) | n/a |
| Romo-Rodriguez et al., 2017 [19] - 3.0-mm, 4.0-mm; length, 26–44 mm | 10 | n/a | 90% of patients had 100% TAM | n/a | By 4 weeks | By 4 weeks |
| Couceiro et al., 2018 [20] - 2.4-mm, 3.0-mm headless compression screw; length n/a | 19 | 1 (0-4) | 96% | 88.3% | n/a | 4 weeks (2-6) |
| Jann et al., 2018 [21] - 2.2-mm, 3.0-mm; length, ≤40 mm | 20 | n/a | 85% of patients had 100% TAM | 93% | 4 weeks (4-6) | n/a |
| Siddiqui et al., 2019 [22] - 2.4-mm or 3.0-mm headless compression screw; length 30-50 mm | 35 | 0 | 243o | 88.6% | 6.6 weeks | 3.6 weeks |
Threaded intramedullary nails provide a novel approach to metacarpal fracture fixation, including benefits that are not supported by other techniques. These threaded nails share similar benefits to compression screws such as improved rotational stability compared to K-wire fixation [23]. The outcomes in our cohort are similar to studies using intramedullary nails and intramedullary compression screws [3,30]. The INnateTM nail allowed stable fixation in our cohort without the need for immobilization and resulted in a comparable time to radiographic union. Threaded intramedullary nails pose less concern for compression and resultant shortening when compared to compression screws. This quality may be particularly valuable in the repair of unstable or complex fractures, in which the compression screw may not be optimal for retaining metacarpal length.
Our study was limited by a lack of a control group for direct comparison of threaded intramedullary nails with historical fixation techniques. Additionally, we did not analyze the impact of pre-existing patient factors or injury mechanisms on time to radiographic union, and further studies are needed to clarify the role of these variables in determining recovery trajectory.
Conclusions
Our cohort included complex, open, and comminuted fractures. There is a paucity of literature assessing compression screw efficacy in complex fractures, as most studies exclude patients with open fractures or intra-articular fractures. Our data suggests that the INnateTM threaded intramedullary nail can provide equivalent surgical outcomes across a broader spectrum of fractures and/or concomitant injury patterns, thus improving and potentially simplifying metacarpal fracture treatment algorithms.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study. Institutional Review Board for the Protection of Human Subjects FWA # 00006767 LUBBOCK/ODESSA IRB #00000096 issued approval L20-034. Approval was obtained from the Texas Tech University Health Sciences Center (TTUHSC) Lubbock/Odessa Institutional Review Board (approval number: L20-034), and appropriate informed consent as well as any necessary Health Insurance Portability and Accountability Act (HIPAA) consent was obtained. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Current management of metacarpal fractures. Diaz-Garcia R, Waljee JF. Hand Clin. 2013;29:507–518. doi: 10.1016/j.hcl.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Intramedullary nail fixation for metacarpal fractures. Blazar PE, Leven D. Hand Clin. 2010;26:321-5, v. doi: 10.1016/j.hcl.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Closed intramedullary locking nailing for metacarpal fractures: a retrospective study of sixty-six fractures. Ghazala C, Choudhry N, Rajeev A. Malays Orthop J. 2018;12:7–14. doi: 10.5704/MOJ.1807.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Comparison between intramedullary nailing and percutaneous k-wire fixation for fractures in the distal third of the metacarpal bone. Moon SJ, Yang JW, Roh SY, Lee DC, Kim JS. Arch Plast Surg. 2014;41:768–772. doi: 10.5999/aps.2014.41.6.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The treatment of unstable metacarpal and phalangeal shaft fractures with flexible nonlocking and locking intramedullary nails. Orbay JL, Touhami A. Hand Clin. 2006;22:279–286. doi: 10.1016/j.hcl.2006.02.017. [DOI] [PubMed] [Google Scholar]
- 6.Comparison of intramedullary nailing versus plate-screw fixation of extra-articular metacarpal fractures. Ozer K, Gillani S, Williams A, Peterson SL, Morgan S. J Hand Surg Am. 2008;33:1724–1731. doi: 10.1016/j.jhsa.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 7.Fifth metacarpal neck fracture fixation: locking plate versus K-wire? Facca S, Ramdhian R, Pelissier A, Diaconu M, Liverneaux P. Orthop Traumatol Surg Res. 2010;96:506–512. doi: 10.1016/j.otsr.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 8.Comparison of the intramedullary nail and low-profile plate for unstable metacarpal neck fractures. Fujitani R, Omokawa S, Shigematsu K, Tanaka Y. J Orthop Sci. 2012;17:450–456. doi: 10.1007/s00776-012-0223-y. [DOI] [PubMed] [Google Scholar]
- 9.A comparison of locking plates and intramedullary pinning for fixation of metacarpal shaft fractures. Dreyfuss D, Allon R, Izacson N, Hutt D. Hand (N Y) 2019;14:27–33. doi: 10.1177/1558944718798854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flexible intramedullary nailing for metacarpal fractures. Gonzalez MH, Igram CM, Hall RF Jr. J Hand Surg Am. 1995;20:382–387. doi: 10.1016/S0363-5023(05)80091-7. [DOI] [PubMed] [Google Scholar]
- 11.A new technique of locked, flexible intramedullary nailing of spiral and comminuted fractures of the metacarpals: a series of 21 cases. Agashe MV, Phadke S, Agashe VM, Patankar H. Hand (N Y) 2011;6:408–415. doi: 10.1007/s11552-011-9350-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Results of locked flexible intramedullary nailing of metacarpal fractures: a case series. Venkatachalam S, Harrison J. Eur J Trauma Emerg Surg. 2011;37:519–524. doi: 10.1007/s00068-011-0074-9. [DOI] [PubMed] [Google Scholar]
- 13.Intramedullary fixation of metacarpal fractures using headless compression screws. Tobert DG, Klausmeyer M, Mudgal CS. J Hand Microsurg. 2016;8:134–139. doi: 10.1055/s-0036-1593390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. Boulton CL, Salzler M, Mudgal CS. J Hand Surg Am. 2010;35:1260–1263. doi: 10.1016/j.jhsa.2010.04.032. [DOI] [PubMed] [Google Scholar]
- 15.Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Doarn MC, Nydick JA, Williams BD, Garcia MJ. Hand (N Y) 2015;10:314–318. doi: 10.1007/s11552-014-9620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. Ruchelsman DE, Puri S, Feinberg-Zadek N, Leibman MI, Belsky MR. J Hand Surg Am. 2014;39:2390–2395. doi: 10.1016/j.jhsa.2014.08.016. [DOI] [PubMed] [Google Scholar]
- 17.Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. del Piñal F, Moraleda E, Rúas JS, de Piero GH, Cerezal L. J Hand Surg Am. 2015;40:692–700. doi: 10.1016/j.jhsa.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 18.Open reduction and internal fixation for intraarticular fracture of metacarpal head. Lee JK, Jo YG, Kim JW, Choi YS, Han SH. Orthopade. 2017;46:617–624. doi: 10.1007/s00132-017-3392-8. [DOI] [PubMed] [Google Scholar]
- 19.Minimal invasive osteosynthesis with cannulated screws in metacarpal fractures (Article in Spanish) Romo-Rodríguez R, Arroyo-Berezowsky C. https://www.medigraphic.com/pdfs/ortope/or-2017/or172c.pdf. Acta Ortop Mex. 2017;31:75–81. [PubMed] [Google Scholar]
- 20.Intramedullary screws versus Kirschner wires for metacarpal fixation, functional, and patient-related outcomes. Couceiro J, Ayala H, Sanchez M, De la Red MD, Velez O, Del Canto F. Surg J (N Y) 2018;4:0–33. doi: 10.1055/s-0038-1637002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Retrograde fixation of metacarpal fractures with intramedullary cannulated headless compression screws. Jann D, Calcagni M, Giovanoli P, Giesen T. Hand Surg Rehabil. 2018;37:99–103. doi: 10.1016/j.hansur.2017.12.005. [DOI] [PubMed] [Google Scholar]
- 22.Fixation of metacarpal fractures using intramedullary headless compression screws: a tertiary care institution experience. Siddiqui AA, Kumar J, Jamil M, Adeel M, Kaimkhani GM. Cureus. 2019;11:0. doi: 10.7759/cureus.4466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Threaded intramedullary nails are biomechanically superior to crossed k-wires for metacarpal neck fractures. Patel M, Castañeda P, Campbell DH, Putnam JG, McKee MD. Hand (N Y) 2023;18:55–60. doi: 10.1177/15589447211003182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Metacarpal fractures: treatment and complications. Kollitz KM, Hammert WC, Vedder NB, Huang JI. Hand (N Y) 2014;9:16–23. doi: 10.1007/s11552-013-9562-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fixation for comminuted phalangeal fractures. A biomechanical study of five methods. Lu WW, Furumachi K, Ip WY, Chow SP. J Hand Surg Br. 1996;21:765–767. doi: 10.1016/s0266-7681(96)80183-5. [DOI] [PubMed] [Google Scholar]
- 26.Comparative analysis of the effects of AO mini-plate and Kirschner wire pinning in the metacarpal fractures: a retrospective study. Lv F, Nie Q, Guo J, Tang M. Medicine (Baltimore) 2021;100:0. doi: 10.1097/MD.0000000000026566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Comparison of miniplate and K-wire in the treatment of metacarpal and phalangeal fractures. Ahmed Z, Haider MI, Buzdar MI, Bakht Chugtai B, Rashid M, Hussain N, Ali F. Cureus. 2020;12:0. doi: 10.7759/cureus.7039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. Page SM, Stern PJ. J Hand Surg Am. 1998;23:827–832. doi: 10.1016/S0363-5023(98)80157-3. [DOI] [PubMed] [Google Scholar]
- 29.Complications after plate fixation of phalangeal fractures. Kurzen P, Fusetti C, Bonaccio M, Nagy L. J Trauma. 2006;60:841–843. doi: 10.1097/01.ta.0000214887.31745.c4. [DOI] [PubMed] [Google Scholar]
- 30.Clinical outcomes of limited open intramedullary headless screw fixation of metacarpal fractures in 91 consecutive patients. Eisenberg G, Clain JB, Feinberg-Zadek N, Leibman M, Belsky M, Ruchelsman DE. Hand (N Y) 2020;15:793–797. doi: 10.1177/1558944719836235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Intramedullary screw fixation for metacarpal shaft fractures: a biomechanical human cadaver study. Labèr R, Jann D, Behm P, Ferguson SJ, Frueh FS, Calcagni M. J Hand Surg Eur Vol. 2020;45:595–600. doi: 10.1177/1753193419898066. [DOI] [PubMed] [Google Scholar]
- 32.Comparison of dorsal plate fixation versus intramedullary headless screw fixation of unstable metacarpal shaft fractures: a biomechanical study. Melamed E, Hinds RM, Gottschalk MB, Kennedy OD, Capo JT. Hand (N Y) 2016;11:421–426. doi: 10.1177/1558944716628485. [DOI] [PMC free article] [PubMed] [Google Scholar]