Summary
Background
Hypertension is a leading cause of morbidity and mortality worldwide, yet a substantial proportion of cases are undiagnosed. Understanding the scale of undiagnosed hypertension and identifying groups most at risk is important to inform approaches to detection.
Methods
In this cross-sectional cohort study, we used data from the 2015 to 2019 Health Survey for England, an annual, cross-sectional, nationally representative survey. The survey follows a multi-stage stratified probability sampling design, involving a random sample of primary sampling units based on postcode sectors, followed by a random sample of postal addresses within these units. Within each selected household, all adults (aged ≥16 years) and up to four children, were eligible for participation. For the current study, individuals aged 16 years and over who were not pregnant and had valid blood pressure data were included in the analysis. The primary outcome was undiagnosed hypertension, defined by a measured blood pressure of 140/90 mmHg or above but no history of diagnosis. Age-adjusted prevalence of undiagnosed hypertension was estimated across sociodemographic and health-related characteristics, including ethnicity, region, rural-urban classification, relationship status, highest educational qualification, National Statistics Socio-Economic Classification (NS-SEC), Body Mass Index (BMI), self-reported general health, and smoking status. To assess the independent association between undiagnosed hypertension and each characteristic, we fitted a logistic regression model adjusted for sociodemographic factors.
Findings
The sample included 21,476 individuals, of whom 55.8% were female and 89.3% reported a White ethnic background. An estimated 30.7% (95% confidence interval 29.0–32.4) of men with hypertension and 27.6% (26.1–29.1) of women with hypertension were undiagnosed. Younger age, lower BMI, and better self-reported general health were associated with an increased likelihood of hypertension being undiagnosed for men and women. Living in rural areas and in regions outside of London and the East of England were also associated with an increased likelihood of hypertension being undiagnosed for men, as were being married or in a civil partnership and having higher educational qualifications for women.
Interpretation
Hypertension is commonly undiagnosed, and some of the groups that are at the lowest risk of hypertension are the most likely to be undiagnosed. Given the high lifetime risk of hypertension and its strong links with morbidity and mortality, our findings suggest a need for greater awareness of the potential for undiagnosed hypertension, including among those typically considered ‘low risk’. Further research is needed to assess the impact of extending hypertension screening to lower-risk groups.
Funding
None.
Keywords: Hypertension, High blood pressure, Undiagnosed hypertension, Health inequalities
Research in context.
Evidence before this study
We searched PubMed from database inception to June 26, 2023 using the search terms (“high blood pressure” OR “hypertension”) AND “undiagnosed”, with no language restrictions. Several studies reported undiagnosed hypertension prevalence estimates for countries including England, the United States, India, Rwanda, Croatia, and France. These studies used a variety of methods to assess undiagnosed hypertension, and some were focused on specific groups such as hospital in-patients, immigrants, older adults, or people with overweight/obesity. Only a handful of studies reported the prevalence of undiagnosed hypertension by characteristics using a general population sample. For example, a 2023 study in Croatia found that men and younger adults were more likely to be undiagnosed than women and older adults, and a 2019 study in France found that men, individuals with no cardiovascular disease or diabetes, and those with a lower waist circumference had the highest odds of undiagnosed hypertension. There was very little evidence for undiagnosed hypertension by characteristics among adults in England, with one study, published in 2020, investigating differences in undiagnosed hypertension in England by income. That study found that men in high-income households were more likely to be undiagnosed than men in low-income households but found no difference by income for women.
Added value of this study
To our knowledge, there has been no previous research to examine undiagnosed hypertension by a wide range of sociodemographic and health-related characteristics among adults in England. We estimated the prevalence of hypertension and undiagnosed hypertension by sex and age, followed by age-adjusted estimates by ethnicity, region, rural-urban classification, relationship status, highest educational qualification, National Statistics Socio-Economic Classification (NS-SEC), Body Mass Index (BMI), self-reported general health, and smoking status. We fitted logistic regression models to assess the independent association of each characteristic with undiagnosed hypertension after adjusting for sociodemographic factors. This study adds to the existing evidence on the prevalence of undiagnosed hypertension in England and provides novel insights into which groups of the population are most at risk of being undiagnosed.
Implications of all the available evidence
A substantial proportion of hypertension cases in England are undiagnosed. Some of the groups who are less likely to have hypertension, such as younger adults and those with a lower BMI, are more likely to be undiagnosed if they do have hypertension. Given the high lifetime risk of hypertension, its strong associations with morbidity and mortality, and the health and economic benefits of early identification and intervention, the available evidence suggests a need for awareness among healthcare professionals and the public of the potential for undiagnosed hypertension across all population groups, including those typically considered low risk. There may be substantial benefit in ensuring accessibility of blood pressure assessment for all groups, including young adults and individuals who are not routinely in contact with healthcare services. However, further evidence is needed to understand the effectiveness of community-based or self-screening methods for reducing hypertension-related morbidity and mortality.
Introduction
Hypertension is a leading cause of morbidity and mortality worldwide and is responsible for between 8 and 10 million deaths each year,1, 2, 3 while high blood pressure accounted for an estimated 9% of global Disability-Adjusted Life Years in 2019.4 In England, 28% of adults had hypertension in 2019, defined as having a measured blood pressure of 140/90 mmHg or above or self-reporting antihypertensive medication use.5 Hypertension also places considerable burden on health services and is responsible for 12% of all visits to General Practitioners in England, with an estimated annual cost to the National Health Service of over £2 billion.6
Lowering blood pressure is a well-established strategy for reducing the incidence of cardiovascular diseases such as stroke, myocardial infarction, and coronary heart disease, and is associated with a significant reduction in all-cause mortality.7,8 Early identification and treatment are associated with significant health and economic benefits because they reduce the need for more elaborate and costly interventions required to treat the complications of hypertension.2,3 Hypertension prevention focuses on lifestyle interventions such as eating a healthy diet, taking regular exercise, and reducing alcohol consumption, and the National Institute for Health and Care Excellence (NICE) in England recommends the same lifestyle interventions for individuals diagnosed with hypertension.9 This is followed by antihypertensive medication if blood pressure is not successfully controlled through lifestyle interventions alone.
Hypertension rarely causes symptoms in the early stages and a substantial proportion of cases are undiagnosed.2,3 A review of hypertension trends between 1990 and 2019 found that 41% of women and 51% of men with hypertension globally did not report a diagnosis,2 and previous estimates suggest that around one third of hypertension cases in England are undiagnosed.10 In 2019, a new coalition led by Public Health England and NHS England outlined plans to improve detection and prevention of the major causes of cardiovascular disease, including an ambition to diagnose 80% of hypertension cases by 2029.11 However, there was a substantial decrease in the proportion of hypertension cases diagnosed and treated during the COVID-19 pandemic, leading to a backlog of care and an urgent need to identify those who are undiagnosed.12,13
Previous research has identified groups who are at increased risk of hypertension. This includes older adults, males, individuals belonging to Black ethnic groups, and those living in more deprived areas, as well as those with known health-related risk factors such as being overweight or physically inactive.3,5,14,15 However, less is known about which groups are most likely to be undiagnosed. Limited evidence from international research has suggested that among those with hypertension, younger adults, men, and those without common comorbidities like diabetes or cardiovascular disease are more likely to be undiagnosed than older adults, women, and those with comorbidities.16,17 One previous study in England found that men in high-income households were more likely to have undiagnosed hypertension than men in low-income households, but no differences were found by income for women.10 However, there have been no studies to explore undiagnosed hypertension by a wide-range of sociodemographic and health-related characteristics among adults in England. Better understanding of inequalities in undiagnosed hypertension could lead to improved rates of diagnosis through targeted screening or public health campaigns. This study aims to identify sociodemographic and health- and lifestyle-related differences in undiagnosed hypertension using a nationally representative sample of adults in England.
Methods
Study population
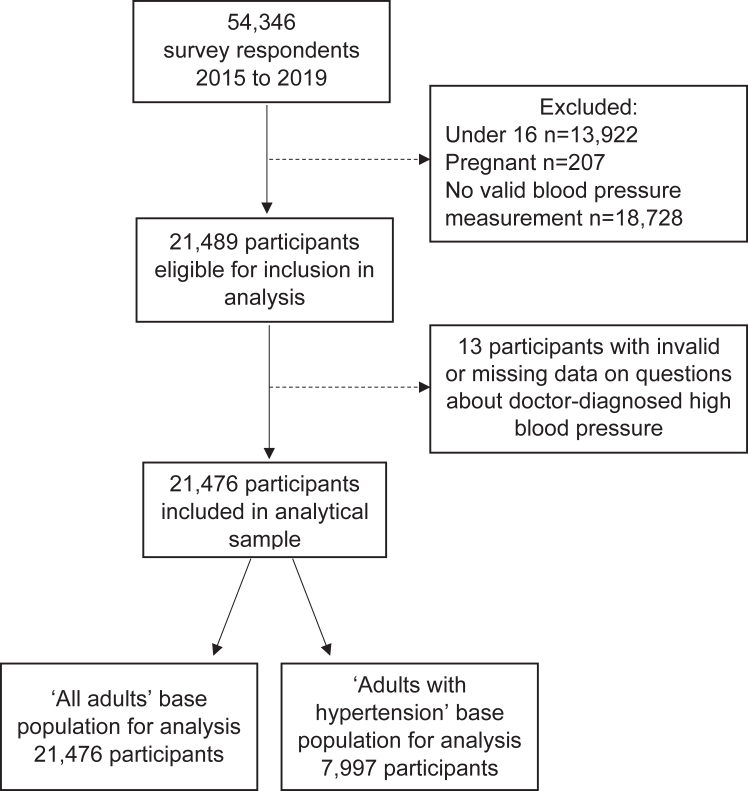
We used data from the Health Survey for England (HSE), an annual cross-sectional survey of people living in private households in England.5 We pooled data from the 2015 to 2019 surveys, which were the most recent data years available at the time of analysis. Aggregating five years of survey data was considered to achieve a good balance between achieving an adequate sample size for analysis while minimising the risk of changes in associations that may occur over time. The HSE follows a multi-stage stratified probability sampling design, involving a random sample of primary sampling units (PSUs) based on postcode sectors, followed by a random sample of postal addresses within PSUs. Within each selected household, all adults aged 16 years and over, and up to four children, were eligible for participation. Full details of the sampling methods are available via NHS Digital.5 All adult participants complete a health interview, which includes questions on demographic characteristics and health history. Participants are then visited by a study nurse who takes measurements such as blood pressure. Prior to 2018 all adult participants were eligible for a nurse visit and in 2018–2019 89% of surveyed addresses were randomly selected for a nurse visit. However, some eligible participants did not complete the nurse visit. The proportion of adult participants who completed a nurse visit between 2015 and 2019 ranged from 59% to 67%. Our analytical sample was restricted to respondents from the 2015 to 2019 HSE who were aged 16 years and over, were not pregnant at the time of interview, and had valid blood pressure data. Fig. 1 shows the flow of survey respondents.
Fig. 1.
Flow chart of sample selection.
Outcomes
Self-reported diagnosis of hypertension
Participants were asked “Do you now have, or have you ever had high blood pressure (sometimes called hypertension)?”. If answered yes, participants were asked “Were you told by a doctor or nurse that you had high blood pressure?”. We classified participants as having self-reported diagnosed hypertension if they answered ‘yes’ to both questions and the high blood pressure didn't occur only during pregnancy.
Blood pressure measurement
During the nurse visit, three consecutive blood pressure readings were taken. We used the mean of the second and third measurements, in line with previous research and guidelines.10,18 We classified participants as having high blood pressure if their systolic pressure was 140 mmHg or above or their diastolic pressure was 90 mmHg or above.
Total hypertension and undiagnosed hypertension
We used the variables above to derive our two outcomes of interest: (1) total hypertension - individuals who self-reported a diagnosis of hypertension or had a blood pressure measurement of 140/90 mmHg or above; and (2) undiagnosed hypertension – individuals whose blood pressure measurement was 140/90 mmHg or above but who did not self-report a diagnosis of hypertension.
Predictors
We explored a variety of sociodemographic and health-related predictors of hypertension and undiagnosed hypertension, based on the literature, theoretical relevance, and data availability. These were: sex, age group, ethnicity, region, rural-urban classification, relationship status, highest educational qualification, National Statistics Socio-Economic Classification (NS-SEC), Body Mass Index (BMI), self-reported general health, and smoking status. These were all collected during the health interview. Details of data collection methods and variable levels for all predictors are available in Supplementary Material Table S1.
Statistical analysis
All analyses accounted for the complex survey design and incorporated weights that were pre-calculated by the HSE survey team. These accounted for selection, non-response, and population profile in the main sample, as well as non-response bias introduced through the nurse visits. Full details of the methodology for deriving each of these weights are provided in the HSE methods report.5 Weights were re-scaled to the pooled dataset and sub-sample of interest (adults who were not pregnant and had valid blood pressure data), following guidance provided by the HSE survey team. This involved calculating the mean value of the weight for each year within the subsample and dividing the combined weights by their respective means.
For each predictor we estimated the age-adjusted prevalence of (a) total hypertension among all adults and (b) undiagnosed hypertension among those with hypertension, by fitting logistic regression models adjusted for age (in five-year age bands, the most granular level available). Marginal means were then used to estimate the age-adjusted prevalence with hypertension and undiagnosed hypertension in each group. Second, we examined the odds of hypertension being undiagnosed for each of our predictors after adjusting for other factors. We fitted minimally adjusted logistic regression models (adjusted for age and stratified by sex) followed by fully adjusted models that adjusted for age, ethnicity, region, urban-rural classification, relationship status, highest educational qualification, and NS-SEC. These covariates were selected based on previous research and topic knowledge and excluded any variables we considered likely to be on the causal pathway between the predictors and the outcome. Statistically significant interactions were identified between sex and several of our predictor variables, therefore all analyses were stratified by sex. All analyses were performed on a complete case basis as there were negligible missing data (<0.2%) for all variables except BMI (10% missing). As BMI was not a covariate in adjusted models this only impacted analysis where BMI was the predictor. Tests of statistical significance were not performed as the analysis was primarily descriptive in nature. All analyses were specified a-priori in the study protocol (see Supplementary Material). Analyses were conducted using R version 4.0.2.
Ethics
Ethical approval for this analysis was granted by the UK Statistics Authority Data Ethics Team, falling under the National Statistician's Data Ethics Advisory Committee. All survey respondents provided verbal informed consent to participate in the Health Survey for England.
Role of the funding source
There was no dedicated external funding for this research.
Results
Characteristics of the sample
The sample involved 21,476 individuals; 55.8% were female, 89.3% reported a White ethnic background, and all were recruited to the Health Survey for England between January 2015 and March 2020. Table 1 summarises the characteristics of the sample.
Table 1.
Characteristics of the sample.
| Sample N (%) | |
|---|---|
| Sex | |
| Male | 9485 (44.2) |
| Female | 11,991 (55.8) |
| Age group | |
| 16–24 years | 1438 (6.7) |
| 25–34 years | 2599 (12.1) |
| 35–44 years | 3268 (15.2) |
| 45–54 years | 3643 (17.0) |
| 55–64 years | 3776 (17.6) |
| 65–74 years | 3894 (18.1) |
| 75 years and over | 2858 (13.3) |
| Ethnicity | |
| White | 19,156 (89.3) |
| Black | 527 (2.5) |
| Asian | 1340 (6.2) |
| Other | 438 (2.0) |
| Region | |
| East Midlands | 2015 (9.4) |
| East of England | 2586 (12.0) |
| London | 2262 (10.5) |
| North East | 1881 (8.8) |
| North West | 2826 (13.2) |
| South East | 3618 (16.8) |
| South West | 2281 (10.6) |
| West Midlands | 2055 (9.6) |
| Yorkshire and the Humber | 1952 (9.1) |
| Rural-urban classification | |
| Urban | 16,884 (78.6) |
| Rural | 4588 (21.4) |
| Relationship status | |
| Single | 3422 (15.9) |
| Married or civil partnership | 11,900 (55.4) |
| Cohabiting | 2446 (11.4) |
| Separated or divorced | 2060 (9.6) |
| Widowed or surviving partner | 1645 (7.7) |
| Educational qualifications | |
| Degree or equivalent qualification | 6281 (29.3) |
| Below degree qualification | 10,866 (50.7) |
| No qualification | 4303 (20.1) |
| National Statistics Socio-economic Classification (NS-SEC) | |
| Managerial and professional occupations | 9387 (43.7) |
| Intermediate occupations | 2384 (11.1) |
| Small employers and own account workers | 2366 (11.0) |
| Lower supervisory and technical occupations | 1738 (8.1) |
| Semi-routine occupations | 5135 (23.9) |
| Other | 447 (2.1) |
| Body Mass Index (BMI) | |
| Not overweight or obese | 6502 (33.6) |
| Overweight | 7223 (37.4) |
| Obese | 5602 (29.0) |
| Self-reported general health | |
| Very good or good | 15,803 (73.6) |
| Fair | 4010 (18.7) |
| Bad or very bad | 1658 (7.7) |
| Smoking status | |
| Current cigarette smoker | 2546 (11.9) |
| Ex-regular cigarette smoker | 6356 (29.6) |
| Never regular cigarette smoker | 12,536 (58.5) |
Percentage with total hypertension and undiagnosed hypertension by characteristics
Table 2, Table 3 present the percentage of men and women with hypertension and undiagnosed hypertension by characteristics. Among all men, 34.3% (95% confidence interval 33.2–35.4) had hypertension and 30.7% (29.0–32.4) of those were undiagnosed. Among all women, 29.7% (28.8–30.7) had hypertension and 27.6% (26.1–29.1) of those were undiagnosed.
Table 2.
Percentage with hypertension and undiagnosed hypertension by characteristics–females.
| Total hypertension (among all females) |
Undiagnosed hypertension (among females with hypertension) |
|||
|---|---|---|---|---|
| Weighted N | Percentage (95% CI) | Weighted N | Percentage (95% CI) | |
| Total | 10,890 | 29.7 (28.8–30.7) | 3770 | 27.6 (26.1–29.1) |
| Age group | ||||
| 16–24 years | 1350 | 4.0 (2.4–5.6) | 60 | 26.1 (8.0–44.3) |
| 25–34 years | 1740 | 7.9 (6.3–9.5) | 160 | 44.0 (33.3–54.6) |
| 35–44 years | 1670 | 13.6 (11.9–15.3) | 270 | 34.0 (27.6–40.3) |
| 45–54 years | 1880 | 25.9 (23.8–27.9) | 570 | 31.0 (27.0–35.0) |
| 55–64 years | 1600 | 40.0 (37.8–42.3) | 740 | 29.1 (25.8–32.4) |
| 65–74 years | 1430 | 57.8 (55.6–60.1) | 960 | 26.8 (24.2–29.5) |
| 75 years and over | 1220 | 71.2 (68.9–73.5) | 1010 | 21.1 (18.6–23.5) |
| Ethnicity | ||||
| White | 9390 | 28.6 (27.3–29.8) | 3400 | 22.3 (20.7–24.1) |
| Black | 360 | 46.2 (39.9–52.6) | 130 | 16.1 (10.7–23.6) |
| Asian | 880 | 31.9 (26.8–37.4) | 190 | 26.1 (18.8–34.9) |
| Other | 260 | 30.8 (23.1–39.8) | 50 | 15.3 (8.2–26.8) |
| Region | ||||
| North East | 530 | 31.1 (28.0–34.4) | 210 | 22.2 (18.3–26.7) |
| North West | 1430 | 31.3 (28.4–34.3) | 510 | 21.4 (18.3–25.0) |
| Yorkshire and the Humber | 1070 | 29.8 (26.5–33.4) | 360 | 19.0 (15.2–23.4) |
| East Midlands | 910 | 33.1 (30.1–36.2) | 360 | 24.7 (20.8–29.0) |
| West Midlands | 1120 | 31.4 (28.1–34.8) | 420 | 20.7 (16.8–25.1) |
| East of England | 1200 | 28.1 (25.5–30.8) | 440 | 21.6 (18.1–25.6) |
| London | 1590 | 28.5 (25.2–32.1) | 410 | 21.0 (16.6–26.3) |
| South East | 1850 | 26.6 (24.4–29.0) | 620 | 22.9 (19.7–26.4) |
| South West | 1180 | 28.3 (25.4–31.4) | 440 | 26.0 (22.1–30.4) |
| Rural-urban classification | ||||
| Urban | 8780 | 29.9 (28.6–31.2) | 2940 | 21.6 (19.8–23.4) |
| Rural | 2110 | 27.6 (25.4–29.8) | 830 | 24.6 (21.6–27.8) |
| Relationship status | ||||
| Single | 2130 | 33.6 (30.2–37.3) | 330 | 17.1 (13.5–21.4) |
| Married or civil partnership | 5420 | 28.4 (26.8–30.1) | 2040 | 24.4 (22.1–26.9) |
| Cohabiting | 1400 | 27.3 (24.1–30.8) | 250 | 22.3 (17.6–27.9) |
| Separated or divorced | 1030 | 29.1 (26.5–31.9) | 460 | 21.9 (18.3–25.9) |
| Widowed or surviving partner | 910 | 31.2 (27.8–34.7) | 700 | 19.7 (16.3–23.7) |
| Educational qualifications | ||||
| Degree or equivalent qualification | 3200 | 23.6 (21.9–25.5) | 670 | 26.2 (23.0–29.6) |
| Below degree qualification | 5580 | 30.1 (28.6–31.6) | 1860 | 22.2 (20.2–24.4) |
| No qualification | 2090 | 35.5 (32.8–38.3) | 1230 | 18.6 (16.0–21.7) |
| Socio-economic status (NS-SEC) | ||||
| Managerial and professional occupations | 4390 | 25.6 (24.1–27.2) | 1290 | 25.0 (22.6–27.6) |
| Intermediate occupations | 1340 | 30.6 (27.9–33.5) | 550 | 21.2 (17.8–25.0) |
| Small employers and own account workers | 1150 | 24.4 (21.7–27.4) | 340 | 27.4 (22.7–32.5) |
| Lower supervisory and technical occupations | 810 | 31.1 (27.6–34.9) | 280 | 21.1 (16.6–26.4) |
| Semi-routine occupations | 2810 | 35.5 (33.3–37.8) | 1180 | 18.7 (16.4–21.3) |
| Other | 360 | 38.2 (30.5–46.6) | 120 | 19.2 (11.8–29.7) |
| Body Mass Index (BMI) | ||||
| Not overweight or obese | 4000 | 17.8 (16.3–19.3) | 780 | 24.9 (21.7–28.4) |
| Overweight | 3090 | 26.7 (24.9–28.5) | 1100 | 24.1 (21.4–27.0) |
| Obese | 2730 | 43.9 (41.6–46.2) | 1390 | 20.5 (18.2–22.9) |
| Self-reported general health | ||||
| Very good or good | 8150 | 25.3 (24.1–26.5) | 2260 | 27.5 (25.4–29.8) |
| Fair | 1910 | 39.6 (37.0–42.4) | 1020 | 14.4 (12.4–16.7) |
| Bad or very bad | 830 | 45.3 (41.1–49.5) | 500 | 13.9 (11.1–17.4) |
| Cigarette smoking status | ||||
| Current cigarette smoker | 1400 | 29.6 (26.5–32.8) | 380 | 22.2 (18.3–26.6) |
| Ex-regular cigarette smoker | 2550 | 30.7 (28.7–32.8) | 1140 | 20.7 (18.3–23.4) |
| Never regular cigarette smoker | 6910 | 29.0 (27.7–30.5) | 2260 | 23.3 (21.3–25.5) |
CI – confidence interval. All estimates are weighted, and all are age-adjusted except where the predictor is age or where there is no predictor (i.e., total population estimates). Weighted sample sizes are rounded to the nearest 10. Base population for total hypertension is all females; base population for undiagnosed hypertension is females with hypertension.
Table 3.
Percentage with hypertension and undiagnosed hypertension by characteristics–males.
| Total hypertension (among all males) |
Undiagnosed hypertension (among males with hypertension) |
|||
|---|---|---|---|---|
| Weighted N | Percentage (95% CI) | Weighted N | Percentage (95% CI) | |
| Total | 10,590 | 34.3 (33.2–35.4) | 4220 | 30.7 (29.0–32.4) |
| Age group | ||||
| 16–24 years | 1470 | 6.9 (4.6–9.2) | 120 | 66.2 (49.9–82.5) |
| 25–34 years | 1740 | 12.7 (10.6–14.9) | 260 | 55.3 (46.3–64.2) |
| 35–44 years | 1680 | 22.0 (19.6–24.4) | 430 | 44.1 (37.8–50.4) |
| 45–54 years | 1810 | 34.7 (32.1–37.3) | 730 | 35.0 (30.5–39.5) |
| 55–64 years | 1610 | 51.8 (49.2–54.5) | 970 | 29.1 (25.9–32.3) |
| 65–74 years | 1330 | 63.7 (61.4–66.0) | 980 | 23.0 (20.4–25.6) |
| 75 years and over | 960 | 65.9 (63.3–68.6) | 730 | 16.6 (14.2–19.0) |
| Ethnicity | ||||
| White | 9140 | 37.6 (36.3–39.0) | 3820 | 34.6 (32.3–36.9) |
| Black | 270 | 48.1 (37.1–59.2) | 110 | 40.6 (28.6–53.8) |
| Asian | 880 | 33.1 (28.3–38.3) | 220 | 31.1 (23.8–39.4) |
| Other | 280 | 36.6 (27.2–47.1) | 70 | 24.7 (12.6–42.6) |
| Region | ||||
| North East | 530 | 39.1 (35.3–43.0) | 230 | 34.1 (28.3–40.5) |
| North West | 1350 | 43.6 (40.0–47.3) | 620 | 36.8 (31.7–42.1) |
| Yorkshire and the Humber | 1010 | 38.8 (34.9–42.9) | 420 | 35.1 (29.4–41.2) |
| East Midlands | 890 | 37.8 (34.4–41.4) | 370 | 39.6 (34.0–45.6) |
| West Midlands | 1140 | 38.9 (35.2–42.7) | 470 | 34.3 (28.8–40.3) |
| East of England | 1230 | 35.7 (32.6–38.9) | 480 | 30.6 (25.8–35.9) |
| London | 1590 | 36.4 (32.4–40.6) | 510 | 25.9 (20.5–32.2) |
| South East | 1750 | 33.4 (30.7–36.2) | 650 | 36.1 (31.6–40.9) |
| South West | 1090 | 36.6 (32.6–40.8) | 470 | 37.4 (32.0–43.0) |
| Rural-urban classification | ||||
| Urban | 8580 | 37.7 (36.3–39.2) | 3310 | 32.3 (30.0–34.6) |
| Rural | 2000 | 36.7 (33.9–39.5) | 920 | 41.9 (37.8–46.1) |
| Relationship status | ||||
| Single | 2610 | 43.6 (39.9–47.4) | 600 | 36.9 (31.8–42.2) |
| Married or civil partnership | 5570 | 35.2 (33.6–36.8) | 2590 | 32.7 (30.0–35.5) |
| Cohabiting | 1460 | 36.3 (32.7–40.1) | 410 | 38.9 (32.7–45.4) |
| Separated or divorced | 610 | 41.4 (37.2–45.7) | 360 | 30.1 (24.7–36.0) |
| Widowed or surviving partner | 330 | 42.5 (37.1–48.2) | 260 | 38.1 (31.0–45.7) |
| Educational qualifications | ||||
| Degree or equivalent qualification | 3250 | 32.5 (30.4–34.7) | 1050 | 35.0 (31.2–39.0) |
| Below degree qualification | 5520 | 38.6 (36.9–40.4) | 2140 | 34.9 (32.1–37.7) |
| No qualification | 1800 | 42.3 (39.5–45.2) | 1030 | 31.8 (28.0–35.9) |
| Socio-economic status (NS-SEC) | ||||
| Managerial and professional occupations | 4590 | 34.9 (33.0–36.7) | 1710 | 34.9 (32.1–37.9) |
| Intermediate occupations | 970 | 36.6 (32.4–41.1) | 370 | 34.8 (28.6–41.5) |
| Small employers and own account workers | 1310 | 37.8 (34.3–41.3) | 570 | 37.6 (32.5–42.9) |
| Lower supervisory and technical occupations | 930 | 36.4 (32.7–40.3) | 380 | 31.9 (26.7–37.6) |
| Semi-routine occupations | 2500 | 43.5 (40.8–46.3) | 1150 | 32.5 (28.9–36.4) |
| Other | 270 | 33.2 (22.8–45.7) | 60 | 30.2 (14.1–53.4) |
| Body Mass Index (BMI) | ||||
| Not overweight or obese | 3160 | 24.0 (21.9–26.2) | 660 | 43.5 (38.1–49.2) |
| Overweight | 3950 | 34.9 (33.1–36.8) | 1600 | 35.8 (32.7–39.1) |
| Obese | 2570 | 52.6 (50.0–55.2) | 1520 | 30.0 (26.9–33.3) |
| Self-reported general health | ||||
| Very good or good | 8160 | 33.7 (32.3–35.2) | 2720 | 41.0 (38.4–43.6) |
| Fair | 1750 | 46.2 (43.4–49.1) | 1010 | 21.3 (18.2–24.8) |
| Bad or very bad | 680 | 55.5 (50.8–60.1) | 490 | 18.3 (14.4–23.1) |
| Cigarette smoking status | ||||
| Current cigarette smoker | 1560 | 40.1 (36.6–43.8) | 540 | 37.0 (31.5–42.8) |
| Ex-regular cigarette smoker | 2960 | 40.0 (38.0–42.1) | 1620 | 29.5 (26.6–32.6) |
| Never regular cigarette smoker | 6020 | 35.6 (33.9–37.3) | 2060 | 36.5 (33.7–39.3) |
CI – confidence interval. All estimates are weighted, and all are age-adjusted except where the predictor is age or where there is no predictor (i.e., total population estimates). Weighted sample sizes are rounded to the nearest 10. Base population for total hypertension is all males; base population for undiagnosed hypertension is males with hypertension.
Hypertension prevalence increased with age, however, among those with hypertension, younger adults were more likely to be undiagnosed. The groups with the highest proportion undiagnosed were 16–24-year-old men (66.2% (95% confidence interval 49.9–82.6)) and 25–34-year-old women (44.0% (33.3–55.6)). This compared to 16.6% (14.2–19.0%) of men and 21.1% (18.6–23.5%) of women aged 75 and over.
For ethnicity, age-adjusted hypertension prevalence was highest among women who belonged to the Black ethnic group. There were no differences in hypertension prevalence by ethnicity for men, nor in the proportion who were undiagnosed for either men or women.
Men living in the North West of England and women living in the East Midlands had the highest age-adjusted hypertension prevalence, and men and women in the South East had the lowest prevalence. There were no differences in the proportion of women who were undiagnosed by region, but for men the highest proportion undiagnosed was in the East Midlands (39.6% (95% confidence interval 34.0–45.6)) and the lowest in London (25.9% (20.5–32.2)) and the East of England (30.6% (25.8–35.9)). Men living in rural areas were also more likely to be undiagnosed (41.9% (37.8–46.1)) than those living in urban areas (32.3% (30.0–34.6)).
Age-adjusted hypertension prevalence was highest among men and women in ‘semi-routine occupations’ and lowest among men and women in ‘managerial and professional occupations’ and women working for ‘small employers and own account workers’. For women, the highest percentage undiagnosed was among ‘small employers and own account workers’ (27.4% (95% confidence interval 22.7–32.5)) and ‘managerial and professional occupations’ (25.0% (22.6–27.6%) and the lowest among ‘semi-routine occupations’ (18.7% (16.4–21.3)), while there were no differences in the proportion undiagnosed by NS-SEC for men.
Men and women with no educational qualifications had the highest age-adjusted hypertension prevalence and those with degree-level or equivalent qualifications had the lowest prevalence. For women, the highest percentage undiagnosed was among those with degree-level or higher qualifications (26.2% (95% confidence interval 23.0–30.0)) and the lowest was among those with no qualifications (18.6% (16.0–21.7)), while there were no differences in the proportion of men undiagnosed by education.
Men and women who were single had the highest age-adjusted hypertension prevalence and those who were married or in a civil partnership had the lowest prevalence. For women, the highest percentage undiagnosed was among those who were married or in a civil partnership (24.4% (95% confidence interval 22.1–26.9)) and the lowest was among those who were single (17.1% (13.5–21.4)), while there were no differences by relationship status for men.
Age-adjusted hypertension prevalence was highest among men and women whose self-reported general health was ‘bad or very bad’ and lowest among those whose health was ‘very good or good’. However, among those with hypertension, adults whose health was ‘very good or good’ were the most likely to be undiagnosed (men 41.0% (95% confidence interval 38.4–43.6%), women 27.5% (25.4–29.8)) and those whose health was ‘bad or very bad’ were the least likely to be undiagnosed (men 18.3% (14.4–23.1%), women 13.9% (11.1–17.4)).
Men and women in the obese BMI category had the highest age-adjusted hypertension prevalence and those classified as not overweight or obese had the lowest prevalence. However, among those with hypertension, individuals classified as not overweight or obese were the most likely to be undiagnosed (men 43.5% (95% confidence interval 38.1–49.2%), women 24.9% (21.7–28.4)) and those classified as obese were the least likely (men 30.0% (26.9–33.3)), women 20.1% (18.2–22.9)).
Men who were ex-regular smokers were the most likely to have hypertension and those who had never regularly smoked were the least likely, however, among men with hypertension, those who had never regularly smoked were the most likely to be undiagnosed (36.5% (95% confidence interval 33.7–39.3)) and ex-regular smokers were the least likely (29.5% (26.6–32.6)). There were no differences in prevalence of hypertension or undiagnosed hypertension by smoking status for women.
Regression models
In fully adjusted models, age, BMI, and self-reported general health were independently associated with the likelihood of men and women with hypertension being undiagnosed after adjusting for sociodemographic characteristics (see Table 4). Compared with those aged 75 years and over, the age groups with the highest odds of being undiagnosed were 16–24-year-old men (odds ratio (OR) 8.5 (95% confidence interval 3.9–18.7)) and 25–34-year-old women (2.8 (1.7–4.5)). Men and women who were not classified as overweight or obese according to their BMI had 1.9 (1.4–2.4) and 1.2 (1.0–1.5) times the odds of being undiagnosed, respectively, compared with those who were classified as obese. Men and women whose self-reported general health was ‘very good or good’ had 3.5 (2.5–4.8) and 2.2 (1.7–2.9) times the odds of being undiagnosed compared with those whose self-reported general health was ‘bad or very bad’.
Table 4.
Adjusted odds ratios for undiagnosed hypertension, among those with hypertension, by characteristics.
| Males |
Females |
|||
|---|---|---|---|---|
| Minimally adjusted model | Fully adjusted model | Minimally adjusted model | Fully adjusted model | |
| Age group | ||||
| 16–24 years | 9.84 (4.60–21.04) | 8.52 (3.89–18.67) | 1.32 (0.51–3.43) | 1.43 (0.53–3.90) |
| 25–34 years | 6.19 (4.13–9.28) | 6.10 (3.91–9.50) | 2.94 (1.86–4.64) | 2.75 (1.66–4.54) |
| 35–44 years | 3.96 (2.90–5.40) | 4.15 (2.95–5.83) | 1.93 (1.40–2.65) | 1.70 (1.18–2.43) |
| 45–54 years | 2.70 (2.07–3.51) | 2.79 (2.09–3.73) | 1.68 (1.33–2.13) | 1.48 (1.12–1.95) |
| 55–64 years | 2.06 (1.63–2.60) | 2.14 (1.66–2.76) | 1.53 (1.24–1.91) | 1.32 (1.04–1.69) |
| 65–74 years | 1.50 (1.20–1.87) | 1.52 (1.21–1.91) | 1.37 (1.12–1.68) | 1.27 (1.02–1.57) |
| 75 years and over | Reference Group | |||
| Ethnicity | ||||
| Black | 1.25 (0.73–2.13) | 1.53 (0.86–2.75) | 0.69 (0.42–1.11) | 0.80 (0.48–1.31) |
| Asian | 0.87 (0.59–1.27) | 1.11 (0.74–1.65) | 1.25 (0.81–1.93) | 1.24 (0.80–1.93) |
| Other | 0.68 (0.31–1.47) | 0.75 (0.37–1.53) | 0.65 (0.32–1.32) | 0.67 (0.32–1.40) |
| White | Reference Group | |||
| Region | ||||
| North East | 0.77 (0.54–1.09) | 0.79 (0.55–1.13) | 0.88 (0.64–1.21) | 0.87 (0.64–1.20) |
| North West | 0.88 (0.64–1.21) | 0.92 (0.66–1.28) | 0.84 (0.63–1.12) | 0.83 (0.61–1.11) |
| Yorkshire and the Humber | 0.81 (0.58–1.15) | 0.85 (0.60–1.20) | 0.72 (0.52–1.01) | 0.70 (0.50–0.98) |
| West Midlands | 0.80 (0.57–1.12) | 0.82 (0.58–1.17) | 0.81 (0.59–1.12) | 0.81 (0.59–1.12) |
| East of England | 0.67 (0.48–0.94) | 0.63 (0.45–0.88) | 0.85 (0.63–1.15) | 0.81 (0.60–1.10) |
| London | 0.54 (0.37–0.78) | 0.56 (0.39–0.83) | 0.85 (0.59–1.21) | 0.82 (0.57–1.18) |
| South East | 0.86 (0.64–1.17) | 0.86 (0.63–1.17) | 0.92 (0.70–1.22) | 0.88 (0.66–1.17) |
| South West | 0.89 (0.64–1.25) | 0.83 (0.59–1.17) | 1.07 (0.79–1.43) | 1.01 (0.75–1.36) |
| East Midlands | Reference Group | |||
| Rural-urban classification | ||||
| Rural | 1.50 (1.24–1.81) | 1.47 (1.21–1.79) | 1.17 (0.98–1.39) | 1.07 (0.89–1.29) |
| Urban | Reference Group | |||
| Relationship status | ||||
| Married or civil partnership | 0.85 (0.65–1.09) | 0.81 (0.62–1.05) | 1.61 (1.17–2.22) | 1.43 (1.04–1.98) |
| Cohabiting | 1.09 (0.76–1.56) | 1.03 (0.71–1.49) | 1.45 (0.97–2.16) | 1.34 (0.90–2.00) |
| Separated or divorced | 0.75 (0.53–1.05) | 0.74 (0.52–1.04) | 1.41 (0.98–2.03) | 1.37 (0.95–1.97) |
| Widowed or surviving partner | 1.11 (0.76–1.61) | 1.08 (0.74–1.59) | 1.19 (0.82–1.73) | 1.17 (0.80–1.69) |
| Single | Reference Group | |||
| Educational qualifications | ||||
| Degree or equivalent qualification | 1.15 (0.90–1.47) | 1.13 (0.86–1.48) | 1.56 (1.21–2.02) | 1.37 (1.05–1.79) |
| Below degree qualification | 1.14 (0.94–1.40) | 1.10 (0.89–1.36) | 1.26 (1.03–1.53) | 1.18 (0.97–1.44) |
| No qualification | Reference Group | |||
| Socio-economic status (NS-SEC) | ||||
| Managerial and professional occupations | 1.13 (0.92–1.39) | 1.12 (0.89–1.41) | 1.42 (1.17–1.72) | 1.23 (1.00–1.52) |
| Intermediate occupations | 1.12 (0.81–1.55) | 1.11 (0.78–1.57) | 1.14 (0.89–1.46) | 1.09 (0.84–1.41) |
| Small employers and own account workers | 1.26 (0.97–1.66) | 1.28 (0.97–1.68) | 1.62 (1.24–2.13) | 1.45 (1.09–1.92) |
| Lower supervisory and technical occupations | 0.99 (0.74–1.33) | 1.01 (0.75–1.36) | 1.15 (0.83–1.58) | 1.08 (0.78–1.51) |
| Other | 0.96 (0.38–2.45) | 1.05 (0.46–2.41) | 1.06 (0.59–1.88) | 1.16 (0.66–2.02) |
| Semi-routine occupations | Reference Group | |||
| Body Mass Index (BMI) | ||||
| Not overweight or obese | 1.78 (1.38–2.29) | 1.86 (1.44–2.40) | 1.28 (1.04–1.58) | 1.24 (1.00–1.53) |
| Overweight | 1.30 (1.08–1.56) | 1.30 (1.08–1.58) | 1.23 (1.02–1.47) | 1.20 (1.00–1.44) |
| Obese | Reference Group | |||
| Self-reported general health | ||||
| Very good or good | 3.11 (2.30–4.20) | 3.46 (2.52–4.75) | 2.32 (1.79–3.02) | 2.21 (1.70–2.87) |
| Fair | 1.21 (0.86–1.70) | 1.29 (0.91–1.82) | 1.02 (0.76–1.38) | 1.00 (0.75–1.35) |
| Bad or very bad | Reference Group | |||
| Cigarette smoking status | ||||
| Ex-regular cigarette smoker | 0.72 (0.55–0.94) | 0.71 (0.54–0.93) | 0.93 (0.70–1.23) | 0.84 (0.63–1.11) |
| Never regular cigarette smoker | 0.98 (0.75–1.27) | 0.95 (0.73–1.24) | 1.07 (0.82–1.40) | 0.95 (0.73–1.24) |
| Current cigarette smoker | Reference Group | |||
Estimates are odds ratios with 95% confidence intervals in brackets. Minimally adjusted models were adjusted for age group and stratified by sex. Fully adjusted models were adjusted for age group, ethnicity, region, rural-urban classification, relationship status, highest educational qualification, and NS-SEC, and stratified by sex.
Among men with hypertension, other characteristics that were independently associated with the likelihood of being undiagnosed were rural-urban classification (rural OR 1.5 (95% confidence interval 1.2–1.8) compared with urban), region (London 0.6 (0.4–0.8), East of England 0.6 (0.5–0.9) compared with East Midlands), and smoking status (ex-regular smokers 0.7 (0.5–0.9) compared with current smokers). Among women with hypertension, other characteristics that were independently associated with the likelihood of being undiagnosed were NS-SEC (‘small employers and own account workers’ 1.5 (1.1–1.9), ‘managerial and professional occupations’ 1.2 (1.0–1.5) compared with ‘semi-routine occupations’), educational qualifications (degree-level qualification or equivalent 1.4 (1.1–1.8) compared with no qualification), and relationship status (married or in a civil partnership 1.4 (1.0–2.0) compared with single).
Discussion
The findings of this study show that many of the groups who were less likely to have hypertension, such as younger adults and those with a lower BMI, were more likely to be undiagnosed if they did have hypertension. Our finding that 30.7% of men and 27.6% of women with hypertension were undiagnosed aligns with previous estimates in England,10 and provides further evidence for the substantial burden of undiagnosed hypertension, which is likely to have further increased since the COVID-19 pandemic.12,13 Our findings suggest that current approaches to hypertension detection are targeting those most at risk, but also indicate that considerable numbers of young and otherwise healthy individuals have undiagnosed hypertension. Given the high lifetime risk of hypertension and its strong links with morbidity and mortality,1,2 our results suggest a need for greater awareness of the potential for undiagnosed hypertension among all groups, including those considered “low risk”. This will be especially important if the government is to achieve its ambition of diagnosing 80% of hypertension cases in England by 2029.11
Individuals with known hypertension risk factors (such as older adults and those in poor health) are likely to have more frequent contact with healthcare services, providing greater opportunity for blood pressure measurement. Those with known risk factors may also be more likely to have their blood pressure opportunistically measured during routine healthcare appointments. In our analysis, men and younger adults were more likely to be undiagnosed than women and older adults, which aligns with previous research.16,17 In 2019, 69% of men in England reported having consulted with a GP in the previous 12 months, compared with 82% of women, and sex differences were greater among younger adults.5 Women are more likely to have routine healthcare appointments where blood pressure is measured, for example during oral contraceptive check-ups or during pregnancy or post-natal healthcare checks. However, research has shown that men have fewer healthcare consultations than women even after accounting for reproductive-related contacts.19 This suggests that relying solely on contact with healthcare services for hypertension detection is likely to systematically overlook certain groups of the population, including young men.
Better self-reported general health and a lower BMI were associated with an increased likelihood of hypertension being undiagnosed. This is likely due to the relationships between general health, BMI and a variety of long-term health conditions and may therefore be related to frequency of contact with healthcare services or the likelihood of opportunistic blood pressure measurement taking place during those contacts. However, individuals with a diagnosis of hypertension may factor this into self-reports of their general health and reverse causality or a bidirectional relationship is likely. That is to say that individuals who are otherwise in good health may be less likely to have their hypertension diagnosed, but individuals who do not know they have hypertension may also be more likely to self-report their health as good.
Men who lived in London and the East of England, and those who lived in urban areas, were less likely to be undiagnosed than those living in other regions or in rural areas. A previous study found that rates of hypertension diagnosis were lower among people living in rural areas in low- and middle-income countries but not in high-income countries, although the analysis was not disaggregated by sex.19 Our findings suggest that convenience of access to healthcare may be a significant factor for hypertension diagnosis among men.
Among women, additional factors that were associated with a higher likelihood of hypertension being undiagnosed were being more highly educated, being married or in a civil partnership, and belonging to the NS-SEC classes ‘managerial and professional occupations’ or ‘small employers or own account workers’. Individuals who are more highly educated and those who belong to higher socioeconomic classes have better health on average than those who are less educated or who belong to lower socioeconomic classes,20,21 and may therefore have reduced opportunity for blood pressure monitoring as part of routine healthcare. However, in our analysis, education and NS-SEC were only associated with undiagnosed hypertension for women. Analysis of primary care data in the UK found a deprivation gradient in healthcare use among women whereby those in more deprived areas had higher rates of GP consultations than women in less deprived areas, but no difference was found for men,22 which may explain our findings. Women with higher levels of education also have fewer children on average,23 and differences in reproductive-related healthcare contacts may add to the deprivation effect for women. The difference in undiagnosed hypertension by marital status among women is unexpected and warrants further investigation.
The Health Survey for England (HSE) provided a unique opportunity to explore inequalities in undiagnosed hypertension. The rigorous survey design and weighting methods enabled us to produce estimates of undiagnosed hypertension for a representative sample of adults in England. The survey benefits from stringent blood pressure protocols designed to optimise the accuracy of readings. Nonetheless, our study had limitations. Firstly, despite efforts to boost sample size by pooling data from multiple years, limitations arose from small numbers with hypertension in some predictor groups. This was a particular issue for ethnicity, which led to wide confidence intervals for the “Black”, “Asian”, and “Other” ethnic groups, especially for men. This may explain why we found little evidence for differences in hypertension prevalence by ethnicity for men, despite previous literature demonstrating higher prevalence among Black men as well as Black women.15 Secondly, our analysis used self-reports of hypertension which will not fully align with clinical diagnoses. Research on self-reports of hypertension offer mixed evidence for their accuracy,24,25 but some suggest underestimation compared to clinical records, which would imply overestimation of undiagnosed hypertension in our analysis. However, this would only impact the interpretation of our findings if the level of disagreement varied across groups. Other studies use self-reports of anti-hypertensive medication instead of self-reports of diagnosis,5,26 however this excludes individuals with hypertension controlled by lifestyle interventions. Blood pressure measurements taken at a single point in time are not equivalent to a diagnosis of hypertension, which requires 24-h ambulatory or at-home blood pressure monitoring.9 Because the HSE cannot show individual variability in blood pressure over time, there is potential for low reproducibility of measurements and over-estimation of undiagnosed hypertension. Again, this would only impact interpretation of our findings if conversion of single-point-in-time measurements to clinical diagnoses differed between groups. Finally, there are limitations associated with the study design, including the cross-sectional design which means we cannot make inferences about causal relationships or rule out the possibility of reverse causality, and the potential for unmeasured confounding in our analysis.
In England, blood pressure checks are offered every five years to adults aged 40–75 under the NHS Health Check, and 1 in 34 Health Check attendees are diagnosed with hypertension, but the programme had an uptake of just 53% between 2012 and 2017 and this further reduced to 40% in 2021/22.27,28 There is substantial regional disparity in uptake, ranging from 25% to 85%, as well as differences by demographic factors such as sex (higher uptake among females) and age (higher uptake among older adults). Since 2021, free blood pressure checks for adults over the age of 40 have also been available at community pharmacies. Our findings demonstrate that, despite these programmes, undiagnosed hypertension remains prevalent among the adult population of England and affects groups who are not typically covered by existing screening or identification methods. Early identification and intervention are associated with better health and economic outcomes,2,3 and there may be substantial benefit in ensuring accessibility of hypertension screening for all groups, including young adults and those who are not routinely in contact with healthcare services. Nonetheless, further research is needed to understand the impact of extending hypertension screening to these groups and identify the most effective methods for providing screening to those who are not already in contact with healthcare services. A 2015 systematic review emphasised the potential of community-based, non-physician or self-screening methods to improve detection of hypertension,29 however, a recent Cochrane review highlighted the need for additional high-quality evidence on the effectiveness of different screening strategies in reducing hypertension-related morbidity and mortality.30
This study builds on the evidence for the substantial burden of undiagnosed hypertension in England and provides evidence that some of the groups who are less likely to have hypertension (such as younger adults and those with a lower BMI) are the most likely to be undiagnosed if they do have hypertension. Given the high lifetime risk of hypertension, its strong associations with morbidity and mortality, and the health and economic benefits of early identification and intervention,1, 2, 3, 4 our findings suggest a need for greater awareness of the risks of undiagnosed hypertension, including among those typically considered “low risk”.
Contributors
KF, VN and CS conceived the idea for the study. Study design was led by KF and EC with input from CS and VN. EC was responsible for curating and cleaning the data, and analysis was carried out by EC, EM, KF, and NCC. KF and CS had leadership responsibility and supervised the project. Methodological advice was provided by VN, PP and IW. AH, VR and AB provided topic expertise and contributed to validation of methods and findings. KF, EC and EM wrote the first draft of the publication. All authors reviewed and commented on the publication and approved the final version. KF, EC and EM accessed and verified the underlying data.
Data sharing statement
Data from the Health Survey for England is available for researchers to access via the UK Data Service.
Declaration of interests
AB has received research grant funding from the National Institute for Health Research (NIHR), British Medical Association, AstraZeneca, and UK Research and Innovation. All other authors declare no competing interests.
Acknowledgements
AB is chief investigator of the NIHR-funded STIMULATE-ICP programme [NIHR COV-LT2-0043].
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.102275.
Appendix A. Supplementary data
References
- 1.Zhou B., Perel P., Mensah G.A., Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18(11):785–802. doi: 10.1038/s41569-021-00559-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NCD Risk Factor Collaboration Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398(10304):957–980. doi: 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva: 2013. A global brief on hypertension: silent killer, global public health crisis. [Google Scholar]
- 4.GBD 2019 Risk Factors Collaborators Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1223–1249. doi: 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NHS Digital . NHS Digital; London: 2019. Health survey for England 2019 (National Statistics)https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2019 [Google Scholar]
- 6.Public Health England . 2019. Health matters: preventing cardiovascular disease.https://www.gov.uk/government/publications/health-matters-preventing-cardiovascular-disease/health-matters-preventing-cardiovascular-disease [Google Scholar]
- 7.Ettehad D., Emdin C.A., Kiran A., et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387(10022):957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 8.Brunström M., Carlberg B. Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels. JAMA Intern Med. 2018;178(1):28–36. doi: 10.1001/jamainternmed.2017.6015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Institute for Health and Care Excellence . Nice guideline NG136; 2019. Hypertension in adults: diagnosis and management.https://www.nice.org.uk/guidance/ng136 [PubMed] [Google Scholar]
- 10.Scholes S., Conolly A., Mindell J.S. Income-based inequalities in hypertension and undiagnosed hypertension: analysis of health survey for England data. J Hypertens. 2020;38(5):912–924. doi: 10.1097/HJH.0000000000002350. [DOI] [PubMed] [Google Scholar]
- 11.Public Health England and NHS England . 2019. Ambitions set to address major causes of cardiovascular disease.https://www.gov.uk/government/news/ambitions-set-to-address-major-causes-of-cardiovascular-disease [Google Scholar]
- 12.CVDPREVENT . Office for Health Improvement and Disparities and the NHS Benchmarking Network; London: 2022. Cvdprevent third annual report. [Google Scholar]
- 13.Dale C.E., Takhar R., Carragher R., et al. The impact of the COVID-19 pandemic on cardiovascular disease prevention and management. Nat Med. 2023;29(1):219–225. doi: 10.1038/s41591-022-02158-7. [DOI] [PubMed] [Google Scholar]
- 14.Leng B., Jin Y., Li G., Chen L., Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens. 2015;33(2):221–229. doi: 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
- 15.NHS Digital . NHS Digital; London: 2022. Health survey England additional analyses, ethnicity and health, 2011-2019 experimental statistics.https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-england-additional-analyses/ethnicity-and-health-2011-2019-experimental-statistics [Google Scholar]
- 16.Uhernik A.I., Kralj V., Čukelj P., et al. Undiagnosed hypertension in Croatia. Croat Med J. 2023;64(1):4–12. doi: 10.3325/cmj.2023.64.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chau A., Girerd N., Zannad F., Rossignol P., Boivin J.M. Health-related determinants of undiagnosed arterial hypertension: a population-based study. Fam Pract. 2019;36(3):276–283. doi: 10.1093/fampra/cmy075. [DOI] [PubMed] [Google Scholar]
- 18.Williams B., Mancia G., Spiering W., et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European society of cardiology (ESC) and the European society of hypertension (ESH) Eur Heart J. 2018;39(33):3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 19.Chow C.K., Teo K.K., Rangarajan S. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310(9):959–968. doi: 10.1093/gerona/glad155. [DOI] [PubMed] [Google Scholar]
- 20.Office for National Statistics . 2017. An overview of lifestyles and wider characteristics linked to Healthy Life Expectancy in England: June 2017.https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/articles/healthrelatedlifestylesandwidercharacteristicsofpeoplelivinginareaswiththehighestorlowesthealthylife/june2017 [Google Scholar]
- 21.Mackenbach J.P., Stirbu I., Roskam A.-J.R., et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y., Hunt K., Nazareth I., Freemantle N., Petersen I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open. 2013;3 doi: 10.1136/bmjopen-2013-003320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berrington A., Stone J., Beaujouan E. 2015. Educational differences in childbearing widen in Britain.http://www.cpc.ac.uk/docs/BP29_Educational_differences_in_childbearing_widen-in_Britain.pdf [Google Scholar]
- 24.Gonçalves V.S., Andrade K.R., Carvalho K.M., Silva M.T., Pereira M.G., Galvao T.F. Accuracy of self-reported hypertension: a systematic review and meta-analysis. J Hypertens. 2018;36(5):970–978. doi: 10.1097/HJH.0000000000001648. [DOI] [PubMed] [Google Scholar]
- 25.Okura Y., Urban L.H., Mahoney D.W., Jacobsen S.J., Rodeheffer R.J. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57(10):1096–1103. doi: 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Crim M.T., Yoon S.S., Ortiz E., et al. National surveillance definitions for hypertension prevalence and control among adults. Circ Cardiovasc Qual Outcomes. 2012;5(3):343–351. doi: 10.1161/CIRCOUTCOMES.111.963439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Patel R., Barnard S., Thompson K., et al. Evaluation of the uptake and delivery of the NHS health check programme in England, using primary care data from 9.5 million people: a cross-sectional study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-042963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Office for Health Improvement and Disparities NHS health check. 2023. https://fingertips.phe.org.uk/profile/nhs-health-check-detailed/data#page/1
- 29.Fleming S., Atherton H., McCartney D., et al. Self-screening and non-physician screening for hypertension in communities: a systematic review. Am J Hypertens. 2015;28(11):1316–1324. doi: 10.1093/ajh/hpv029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt B.-M., Durao S., Toews I., et al. Screening strategies for hypertension. Cochrane Database Syst Rev. 2020;5 doi: 10.1002/14651858.CD013212.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.