Abstract
Access to and utilization of consumer credit remains an understudied social determinant of health. We examined associations between a novel, small-area, multidimensional credit insecurity index (CII), and the prevalence of self-reported frequent mental distress across US cities in 2020. The census tract-level CII was developed by the Federal Reserve Bank of New York using Census population information and a nationally representative sample of anonymized Equifax credit report data. The CII was calculated for tracts in 766 cities displayed on the City Health Dashboard at the time of analysis, predominantly representing cities with over 50,000 residents. The CII combined data on tract-level participation in the formal credit economy with information on the percent of individuals without revolving credit, percent with high credit utilization, and percent with deep subprime credit scores. Tracts were classified as credit-assured, credit-likely, mid-tier, at-risk, or credit-insecure. We used linear regression to examine associations between the CII and a modeled tract-level measure of frequent mental distress, obtained from the CDC PLACES project. Regression models were adjusted for neighborhood economic and demographic characteristics. We examined effect modification by US region by including two-way interaction terms in regression models. In adjusted models, credit-insecure tracts had a modestly higher prevalence of frequent mental distress (prevalence difference = 0.38 percentage points; 95% CI = 0.32, 0.44), compared to credit-assured tracts. Associations were most pronounced in the Midwest. Local factors impacting credit access and utilization are often modifiable. The CII, a novel indicator of community financial well-being, may be an independent predictor of neighborhood health in US cities and could illuminate policy targets to improve access to desirable credit products and downstream health outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-023-00792-1.
Keywords: Mental health, Credit insecurity, Mental distress
Introduction
Access to and utilization of consumer credit—like other dimensions of financial well-being—influence health outcomes through multiple pathways, including through impacting levels of psychosocial stress, access to resources, and investment opportunities [1]. While access to credit can mitigate the effects of financial shocks and offer opportunities to invest in careers and education, poor credit histories—including low or subprime credit scores, or high levels of indebtedness—make it difficult to obtain credit products on favorable terms and may also negatively impact access to employment, housing, and affordable insurance [2].
Individual and community credit histories are multidimensional, though prior health outcome-focused studies have typically assessed a single aspect of consumer credit such as credit scores [3–5], levels of indebtedness [6–9], mortgage delinquency [10], or experiences of foreclosure [11]. These studies—conducted over a range of geographic areas and using both ecologic and individual-level credit measures—have established associations between consumer credit and a range of health outcomes [4, 5]. With regard to mental health, systematic reviews have found that higher levels of indebtedness are associated with a higher likelihood of reporting depressive symptoms, suicidal ideation, suicide completion or attempt, and psychotic disorders [6, 7]. While evidence regarding the health effects of credit access and utilization is growing, examining credit as a social determinant of health remains relatively rare compared to other measures of financial well-being, including income. Understanding associations between credit and health may be particularly informative for health policymaking, as aspects of credit access and utilization may be more responsive in the short-term to interventions or other external shocks compared to other measures of socioeconomic status (SES) [12].
In this study, we explored a multidimensional, small-area measure of “credit insecurity,” developed by the Federal Reserve Bank of New York. The credit insecurity index (CII) combines census tract-level information on participation in the formal credit economy with credit use measures—including revolving credit product use (e.g., credit card use), levels of credit utilization, and credit scores—that collectively reflect the extent to which a community has access to desirable credit products [2]. As a multidimensional, neighborhood measure, it provides insight into a community’s potential financial resilience to economic shocks [2], while also capturing potential peer effects (for example, spillover effects related to neighborhood foreclosures) [13] and neighborhood access to financial institutions. For example, prior research has established the social and geographic patterning of banking deserts, resulting in a concentrated lack of access to mainstream credit products in certain neighborhoods [14, 15]. We used tract-level CII data from US cities in 2020 to address interrelated research questions. First, given the growing body of literature exploring associations between financial well-being and mental health outcomes, as well as survey data suggesting that financial concerns are a leading source of stress among US adults [16], we examined whether the CII was associated with modeled tract-level prevalence of frequent mental distress in urban areas. Second, to shed light on potential patterns of geographic variation, we leveraged our nationwide dataset to explore whether this association varied by US. region.
Methods
Study Design
We used ecologic, cross-sectional neighborhood (proxied by census tracts) data from the City Health Dashboard (CHDB), an interactive, online resource providing social determinant and health indicator data for hundreds of cities across the USA [17]. Exposure and outcome data were obtained at the tract level for 2020. Our analysis focused on 766 cities on the CHDB at the time of writing; the majority of cities (753) had populations of at least 50,000. Given that factors impacting credit access and utilization—including concentrations of financial institutions—may vary widely by urbanicity [18], our focus on cities allowed us to examine the unique dynamics of credit access and utilization in high-population areas.
Exposure
The CII was developed by the Federal Reserve Bank of New York using information from Census Bureau population estimates and from the New York Fed Consumer Credit Panel (CPP), which is based on a nationally representative sample of anonymized Equifax credit report data [2, 19]. Briefly, the index was constructed from two components, measured among adults at least 18 years of age. The first component represented the percent of adults without a formal credit history (i.e., individuals without a credit file or score). The second component captured the percent of adults in each tract with a formal credit history, multiplied by the average of three equally weighted quantities: percent without revolving credit (i.e., individuals without open-ended credit products, such as credit cards), percent with high credit utilization (i.e., individuals utilizing > = 100% of credit lines), and percent with deep subprime credit scores (defined as an Equifax Risk Score 3.0 of less than or equal to 580). By incorporating these three elements, the second component reflected factors that limit access to credit-at-choice, among those who participate in the credit economy. The two components were then added together to produce the CII value for each tract, with higher tract-level scores indicating higher levels of credit insecurity. For this analysis, 2020 CII scores were grouped into six mutually exclusive tiers based on categories previously developed by the Federal Reserve Bank: credit-assured (CII < 19), credit-likely (CII = 19–23), mid-tier (CII 24–28), at-risk (CII 29–35), credit-insecure (> = 36), and missing [2]. Due to CCP suppression rules, a tract was considered to be “missing” CII data if there were fewer than 50 individuals in the random sample of Equifax credit report data. Estimates were developed using 2010 census tract boundaries and accessed via the CHDB.
Outcome
The outcome was modeled tract-level prevalence of frequent mental distress, or the modeled proportion of adults ages 18 + years who reported that their mental health was “not good” for at least 14 of the last 30 days. Data was obtained from the CDC PLACES project 2022 data release—which used 2020 survey data for frequent mental distress [17, 20]. Briefly, CDC PLACES produces modeled health data using small-area estimation techniques and information from the CDC’s Behavioral Risk Factor Surveillance System (BRFSS), the US Census, and the American Community Survey (ACS). Multi-level regression models were used to predict mental distress based on age, race/ethnicity, and education, county-level poverty indicators, and state and county random effects [21]. Prior studies suggest alignment between modeled estimates and directly measured outcomes at multiple geographic levels [21], though validity may vary by measure and geography [22].
Covariates
Adjusted models included several covariates to examine whether the CII was associated with mental distress after controlling for other neighborhood-level economic and demographic measures. We included variables based on the socioeconomic status (SES) dimension of the CDC’s Social Vulnerability Index [23], including percent of households with incomes below the federal poverty level, percent unemployed, median household income, and percent of adults ages 25 + without a high school diploma. We also adjusted for neighborhood racial/ethnic composition (including tract-level percent of the population that is non-Hispanic Black, percent Hispanic, and percent non-Hispanic White), population age distribution (percent under 18, 18–24, 25–59, and 60 +), and US region (Northeast, Midwest, South, and West). We anticipated that the CII would be correlated with other economic characteristics and with demographic factors, given examples of racial discrimination in credit provisioning mechanisms [24, 25]. In addition, age is correlated with components of the CII, as young adults are less likely to participate in the formal credit economy. These variables are also associated with patterns of mental health outcomes [26]. All covariates with the exception of US region were derived from ACS 5-year estimates (2015–2019) [27]. We chose to use 2015–2019 ACS data, rather than 2016–2020 ACS data, because our exposure and outcome variables were based on 2010 tract boundaries, which aligned with 2015–2019 ACS estimates. All continuous covariates were standardized.
Effect Modification Analysis
There is pronounced geographic variation across the USA in economic indicators, as well as patterns of health outcomes, including mental health outcomes [28]. We examined whether associations between the CII and mental distress varied across regions (Northeast, Southeast, Midwest, and West).
Statistical Analysis
We examined descriptive characteristics stratified by CII tier. We also explored Pearson correlation coefficients for frequent mental distress, the CII, and economic and demographic (racial composition) characteristics. We estimated prevalence differences for frequent mental distress associated with CII categories using a series of ordinary least squares linear regression models, including bivariate models, models adjusted for demographic characteristics (and region), and models additionally incorporating economic covariates. For the effect modification analyses, we included two-way interaction terms between the CII and region, evaluating the interaction p-value on the additive scale. For all regression models, we accounted for uncertainty in the modeled outcome variable by simulating a sampling distribution for each tract, based on mean and standard error information provided in the PLACES data file. We then sampled point estimates from each tract’s distribution to create 20 independent datasets and combined estimates across datasets using Rubin’s rules [29].
As a sensitivity analysis, we estimated multi-level models including city-level random intercepts. We also conducted an alternative analysis where we excluded tracts with missing CII data and incorporated inverse probability weights to account for the probability of selection into the sample among tracts with complete CII information. All analyses were conducted in Stata version 17.0. As a secondary analysis using publicly available data, this study was not considered human subjects research.
Results
Table 1 includes descriptive characteristics for all census tracts (N = 32,004), stratified by CII category. Approximately 22% of tracts were classified as credit-insecure. Higher levels of credit insecurity were associated with lower per capita income, higher percentage of individuals with less than a high school education, higher percentage of households within income below the poverty level, and higher percent unemployed. Credit-insecure tracts had more non-Hispanic Black residents and Hispanic residents, fewer non-Hispanic White residents, and more individuals between the ages of 18 and 24. The prevalence of frequent mental distress was higher at higher levels of the CII, with a 4.5 percentage point difference between credit-assured tracts and credit-insecure tracts. Tracts missing CII information (N = 1757) were more likely to have a smaller population and were most similar to the credit-insecure tracts with regard to economic characteristics. Tracts missing CII data also had a high average proportion of Black individuals (44.0%) and a high average proportion of residents ages 18–24 (17.1%).
Table 1.
Census tract-level descriptive characteristics by credit insecurity tier, 2020
| Variable (mean) | All | Credit-assured (< 19) | Credit-likely (19–23) | Credit mid-tier (24–28) | Credit-at-risk (29–35) | Credit-insecure (36 +) | Missing |
|---|---|---|---|---|---|---|---|
| CII score | 25.0 | 11.4 | 21.4 | 26.4 | 32.3 | 46.3 | NA |
| Median income | $33,683 | $44,005 | $34,318 | $31,287 | $28,093 | $22,320 | $21,133 |
| % less than high school education | 14.4% | 7.8% | 12.7% | 15.2% | 18.0% | 23.1% | 20.4% |
| % below poverty level | 16.9% | 8.6% | 13.3% | 16.2% | 19.7% | 27.9% | 34.2% |
| % unemployed | 6.4% | 4.3% | 5.4% | 6.1% | 6.9% | 9.0% | 12.1% |
| % Non-Hispanic Black | 18.4% | 7.4% | 13.6% | 18.4% | 22.9% | 31.5% | 44.0% |
| % Hispanic | 24.0% | 16.8% | 24.9% | 27.8% | 30.2% | 32.7% | 18.0% |
| % Non-Hispanic White | 46.5% | 61.8% | 49.8% | 43.2% | 37.1% | 28.1% | 30.7% |
| Population size | 4542 | 4990 | 4749 | 4593 | 4524 | 4337 | 1689 |
| % < age 18 | 22.1% | 21.3% | 21.5% | 22.1% | 22.8% | 23.7% | 21.8% |
| % ages 18–24 | 10.2% | 7.4% | 9.1% | 9.6% | 10.5% | 14.3% | 17.1% |
| % ages 25–59 | 47.8% | 48.6% | 49.1% | 49.0% | 48.4% | 45.9% | 43.4% |
| % ages 60 + | 19.9% | 22.7% | 20.3% | 19.3% | 18.4% | 16.1% | 17.8% |
| Prevalence of frequent mental distress | 15.4% | 13.4% | 14.9% | 15.5% | 16.2% | 17.9% | 18.6% |
| N tracts | 32,004 | 12,467 | 3,596 | 3,269 | 3,976 | 6,939 | 1,757 |
Pearson correlations between frequent mental distress prevalence, the CII (measured continuously), and other tract-level standardized characteristics are provided in Appendix Table 1. The CII was most strongly correlated with economic characteristics, including the percent below the poverty level (rho = 0.68). CII scores were lowest in the West, compared to other regions (Appendix Table 2).
Table 2.
Prevalence differences and 95% confidence intervals for associations between tract-level credit insecurity and tract-level frequent mental distress: results from linear regression models (N = 32,004 tracts), 2020
| Model 1a | Model 2b | Model 3c | |
|---|---|---|---|
| CII tier (Assured ref.) | |||
| Likely | 1.53 (1.44, 1.62) | 0.89 (0.82, 0.97) | 0.22 (0.16, 0.28) |
| Mid-tier | 2.15 (2.05, 2.24) | 1.18 (1.11, 1.26) | 0.25 (0.19, 0.31) |
| At-risk | 2.82 (2.73, 2.90) | 1.51 (1.43, 1.59) | 0.25 (0.19, 0.31) |
| Insecure | 4.52 (4.45, 4.59) | 2.32 (2.25, 2.40) | 0.38 (0.32, 0.44) |
| Missing | 5.16 (5.04, 5.29) | 2.63 (2.51, 2.75) | 0.43 (0.33, 0.52) |
aBivariate model
bAdjusts for racial/ethnic composition, population size, age distribution, and US region. All continuous covariates are standardized
cAdjusts for Model 2 covariates, plus median income, % with less than a high school education, % households below the federal poverty level, and % unemployed. All continuous covariates are standardized
Table 2 includes bivariate, minimally adjusted, and fully adjusted estimates from linear regression models. Across all models, the prevalence of frequent mental distress was higher in tracts with higher levels of credit insecurity, with the most pronounced association in the bivariate model. Estimates attenuated with the inclusion of demographic characteristics and attenuated further with the incorporation of economic characteristics. In the fully adjusted regression model, “credit-insecure” tracts had a 0.38 percentage point (95% confidence interval (CI): 0.32, 0.44) higher prevalence of frequent mental distress, compared with credit-assured tracts.
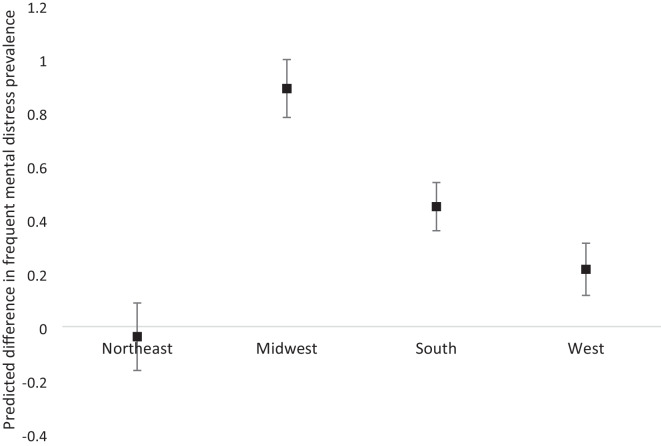
We observed a significant interaction between the CII and US region (p = < 0.001, Appendix Table 3). To aid interpretability, we estimated average marginal effects from the interaction model and plotted the predicted difference in the prevalence of frequent mental distress between credit-insecure and credit-assured tracts, by region. The association between higher credit insecurity and higher prevalence of frequent mental distress was most pronounced in the Midwest (Fig. 1). Associations appeared relatively flat in the Northeast.
Fig. 1.
Predicted difference (in percentage points) in the prevalence of frequent mental distress between credit-insecure and credit-assured tracts, by region. Predictions generated from average marginal effects from linear regression model (Appendix Table 3), 2020
Results from a model including city-level random intercepts were similar to the primary model, though point estimates were slightly attenuated (Appendix Table 4). The intraclass correlation coefficient from the fully adjusted multi-level model was 0.53. In the fully adjusted regression model, credit-insecure tracts had a higher prevalence of frequent mental distress by 0.27 percentage points (95% CI: 0.22, 0.32), compared to credit-assured tracts. Results from the model incorporating inverse probability weights to account for tracts with missing CII data were similar in sign and magnitude to the primary model (Appendix Table 5).
Discussion
This study is the first to examine associations between a multidimensional neighborhood-level measure of credit insecurity and frequent mental distress, focusing on urban areas across the USA. Building on an increasing interest in exploring the dynamics of financial well-being and health beyond measures of income [1], we found that the CII was modestly associated with the prevalence of frequent mental distress. Our findings are in line with prior research—mostly employing individual-level measures of credit well-being—that has found that low or subprime credit scores and high levels of indebtedness are associated with a range of health outcomes, including poor mental health [6–8, 11]. Associations were most pronounced in bivariate models and attenuated substantially after adjustment for a range of sociodemographic and economic characteristics, reflecting potential confounding in bivariate models by other socioeconomic predictors of mental health outcomes. Nevertheless, results from adjusted models suggest that credit insecurity may be independently associated with mental health outcomes, above and beyond more commonly measured aspects of SES. Moreover, given that credit insecurity is a relatively common phenomenon (22% of tracts in our sample were classified credit-insecure), even small-magnitude associations with mental distress could have substantial implications on the population level.
Financial precariousness experienced by many US households underscores the importance of examining credit insecurity as a health determinant. In a 2018 survey, 17% of US adults were not able to fully cover the current month’s expenses, and a further 12% would not be able to cover their bills if a $400 unexpected expense were to arise [30]. Access to consumer credit can smooth consumption, promote financial resilience, and allow for investments in housing, career, and educational opportunities [2]. Although access to traditional credit can be helpful, excessive or injudicious credit use can result in financial stress. In addition, individuals with high levels of credit insecurity may have to rely on products outside the traditional credit space (e.g., payday loans) that often have very high interest rates, further increasing financial distress [31]. The CII is a new neighborhood-level measure, designed to incorporate multiple dimensions of credit utilization and access and to capture a community’s access to credit-at-choice, including low cost credit products. Importantly, the CII includes information from individuals who do not participate in the formal credit economy, as well as those who do, which many prior analyses of credit history are not able to integrate. As a multidimensional measure, the CII also reflects multiple potentially intervenable community factors, including the extent to which communities experience equitable access to financial institutions and financial inclusion resources. Although the goal of our study was primarily descriptive, rather than causal, future research studies employing stronger causal designs could utilize the CII to shed further light on the potential for credit-related policies to impact both the CII and downstream health outcomes.
At the individual level, credit utilization measures may reflect individual psychobehavioral characteristics, including propensity for risk-taking or attitudes towards future discounting [3, 32], as well as human capital factors [33]. In the USA, inequities in credit access and utilization also reflect the social and geographic patterning of financial institutions and informal financial providers (e.g., payday lenders) [14, 15], as well as legacies of individual- and neighborhood-level discrimination and racism in mortgage and lending practices [24, 25]. For example, prior work has demonstrated associations between Home Owners’ Loan Corporation redlining practices in the 1930s and contemporary residential segregation [24], as well as neighborhood disinvestment [34], which are embodied in health outcomes to the present day [34]. In our study, we found that the CII was strongly correlated with other neighborhood factors, including racial and ethnic composition, which is in line with prior work documenting the impacts of structural racism and exclusionary lending practices on credit access and utilization. Importantly, addressing credit insecurity through targeted interventions may represent an opportunity to intervene on longstanding racial disparities in equitable credit access.
We found that associations between the CII and mental distress in urban areas were most pronounced in the Midwest. There have been few neighborhood-level studies of credit-related measures and health outcomes using nationwide data, and none, to our knowledge, have examined variation by US region. However, there is well-documented variation across US regions with regard to numerous health outcomes [28, 35, 36]. Furthermore, prior work by the CHDB has revealed wide variation in both the mean and spread of the CII within and across cities, grouped by population and city-level characteristics [37]. For example, college cities and small post-industrial cities tend to have particularly high average CII values, compared to other city types [37]. It is possible that city characteristics impact the relationship between the CII and mental health outcomes and help to explain the geographic patterns observed in this study. Other research has also examined the variability of associations between measures of financial well-being (e.g., income) and health outcomes according to local characteristics, including finding that longer life expectancies among individuals with low-income are correlated with a higher area-level density of immigrants, higher levels of government expenditures, and higher proportions of college graduates, among other factors [35]. While our study suggests the potential for geographic region to modify associations between credit insecurity and frequent mental distress, future studies would benefit from the incorporation of additional local area characteristics, including considering differences in city characteristics by region.
Strengths of this study include the use of a multidimensional measure of credit insecurity—capturing aspects of credit access and utilization—mapped to urban areas across the USA. We examined correlations between the CII and other frequently used neighborhood economic indicators and also explored the extent to which the CII predicted the prevalence of frequent mental distress after adjusting for correlated demographic and economic characteristics. Measuring tract-level credit insecurity may provide an alternative measure of community economic well-being that is more responsive in the short-term to policies or external shocks, compared to income or education. For example, research into the Flint water crisis found that higher levels of household exposure to lead pipes was modestly associated with experiencing more past due loans and with credit score declines in the 5 years following the crisis [12]. By constructing the CII at the neighborhood level, instead of at the individual level, our measure reflects potential geographic peer effects related to neighborhood financial well-being [13], as well as local financial institution dynamics (e.g., product availability). Neighborhood-level measures can also highlight geographic areas that would potentially benefit from financial inclusion interventions or multi-component interventions that target both economic well-being and health outcomes.
The study also had several limitations. We used ecologic outcome data, which limits our ability to extend inference to the individual level. In addition, this study was observational and cross-sectional, and results could reflect confounding by other, unmeasured aspects of unmet financial need, including food or housing insecurity. Variables measured in 2020 may reflect the dynamics of the COVID-19 pandemic. For example, prior research suggests that the pandemic impacted revolving credit utilization [38] and mental health outcomes [39] among the US public. The extent to which the COVID-19 pandemic may have altered associations between the CII and frequent mental distress is unknown, and therefore the results of this analysis may not be directly transportable to other time periods. Future studies using longitudinal measures of the CII may be better suited to elucidating dynamic relationships between the CII and health outcomes. It is likely, for example, that associations between credit insecurity and mental health are bidirectional, and that poor mental and/or physical health may impact credit and other measures of financial well-being, or that individuals experiencing mental distress may be more likely to reside in neighborhoods with high levels of credit insecurity. Many tracts were missing CII data, and patterns of missingness were correlated with economic and demographic factors. While we included a missing data category in our primary analysis, tracts within this group were likely heterogeneous. While the index captured multiple dimensions of credit access and utilization, tracts within the same CII tier may vary greatly across individual dimensions of the CII. This may complicate future work that aims to identify policy intervention targets for addressing high levels of credit insecurity. In addition, the CII does not directly capture all aspects of consumer credit and does not include payment delinquency. Our measure of frequent mental distress represented a modeled prevalence. Modeled measures are based on small-area estimation techniques that do not incorporate information on local interventions or policy environments [21]. The validity of modeled measures of the prevalence of mental distress at the census tract level has not been extensively validated. Moreover, while we did not directly interpret coefficients associated with socioeconomic adjustment variables, several demographic and economic variables (e.g., age and poverty) were used to produce modeled mental distress estimates, which limits their interpretability in the outcome modeling process [22]. Future work should evaluate whether associations observed in this study can be replicated using directly measured individual-level mental health outcomes.
Local factors impacting credit access and utilization are often modifiable. Examining the CII as a potential driver of health outcomes could illuminate policy targets to improve access to desirable credit products and downstream health outcomes. Findings from this descriptive study suggest that a neighborhood measure of credit insecurity may be an independent predictor of mental health outcomes, above and beyond commonly utilized measures of neighborhood SES, including income, education, or unemployment. Future studies that build on this ecologic analysis are warranted, given the longstanding need to address historical discrimination in credit provisioning mechanisms and to identify equitable policy interventions to promote neighborhood financial resiliency.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This work was supported by the Robert Wood Johnson Foundation (Grant Numbers 78287 and 78440).
Abbreviations
- USA
United States of America
- CII
Credit Insecurity Index
- CHDB
City Health Dashboard
- CCP
Consumer Credit Panel
- BRFSS
Behavioral Risk Factor Surveillance System
- ACS
American Community Survey
- CI
Confidence interval
- SES
Socioeconomic status
Data Availability
Data used in this study are publicly available.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Swift SL, Bailey Z, Al Hazzouri AZ. Improving the epidemiological understanding of the dynamic relationship between life course financial well-being and health. Curr Epidemiol Rep. 2019;6:28–33.
- 2.Federal Reserve Bank of New York. Unequal access to credit: the hidden impact of credit constraints. https://www.newyorkfed.org/outreach-and-education/community-development/unequal-access-to-credit-hidden-impact-credit-constraints. Accessed 22 Aug 2022.
- 3.Dean LT, Nicholas LH. Using credit scores to understand predictors and consequences of disease. Am J Public Health. 2018;108:1503–5. [DOI] [PMC free article] [PubMed]
- 4.Dean LT, Knapp EA, Snguon S, Ransome Y, Qato DM, Visvanathan K. Consumer credit, chronic disease and risk behaviours. J Epidemiol Community Health. 2019;73:73–8. [DOI] [PMC free article] [PubMed]
- 5.Knapp EA, Dean LT. Consumer credit scores as a novel tool for identifying health in urban U.S. neighborhoods. Ann Epidemiol. 2018;28:724–9. [DOI] [PMC free article] [PubMed]
- 6.Turunen E, Hiilamo H. Health effects of indebtedness: a systematic review. BMC Public Health. 2014;14:489. doi: 10.1186/1471-2458-14-489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson T, Elliott P, Roberts R. The relationship between personal unsecured debt and mental and physical health: a systematic review and meta-analysis. Clin Psychol Rev. 2013;33:1148–62. [DOI] [PubMed]
- 8.Marshall GL, Kahana E, Gallo WT, Stansbury KL, Thielke S. The price of mental well-being in later life: the role of financial hardship and debt. Aging Ment Health. 2021;25:1338–1344. doi: 10.1080/13607863.2020.1758902. [DOI] [PubMed] [Google Scholar]
- 9.O’Rand AM, Hamil-Luker J. Landfall After the Perfect Storm: cohort Differences in the Relationship Between Debt and Risk of Heart Attack. Demography. 2020;57:2199–2220. doi: 10.1007/s13524-020-00930-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charters TJ, Harper S, Strumpf EC, Subramanian SV, Arcaya M, Nandi A. The effect of metropolitan-area mortgage delinquency on health behaviors, access to health services, and self-rated health in the United States, 2003–2010. Soc Sci Med. 2016;161:74–82. doi: 10.1016/j.socscimed.2016.05.021. [DOI] [PubMed] [Google Scholar]
- 11.Tsai AC. Home foreclosure, health, and mental health: a systematic review of individual, aggregate, and contextual associations. PLoS ONE. 2015;10:e0123182. doi: 10.1371/journal.pone.0123182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gorton N, Pinkovskiy M. Credit access and mobility during the Flint water crisis. Staff Report; 2021. Report No.: 960. https://www.econstor.eu/handle/10419/241153. Accessed 21 Aug 2022.
- 13.Gupta A. Foreclosure contagion and the neighborhood spillover effects of mortgage defaults. J Financ. 2019;74:2249–2301. doi: 10.1111/jofi.12821. [DOI] [Google Scholar]
- 14.Dunham IM. Landscapes of financial exclusion: alternative financial service providers and the dual financial service delivery system. Bus Soc Rev. 2019;124:365–383. doi: 10.1111/basr.12180. [DOI] [Google Scholar]
- 15.Hegerty SW. “Banking Deserts”, bank branch losses, and neighborhood socioeconomic characteristics in the city of Chicago: a spatial and statistical analysis. Prof Geogr. 2020;72:194–205. doi: 10.1080/00330124.2019.1676801. [DOI] [Google Scholar]
- 16.Stress in America: Paying with our health. American Psychological Association; 2015 Feb.
- 17.Department of Population Health, NYU Langone Health. City Health Dashboard. https://www.cityhealthdashboard.com/. Accessed 5 Jan 2022.
- 18.Kashian RD, Tao R, Drago R. Bank deserts in the USA and the Great Recession: geography and demographics. J Econ Stud. 2018;45:691–709. doi: 10.1108/JES-05-2017-0121. [DOI] [Google Scholar]
- 19.Community Credit: A new perspective on America’s communities - FEDERAL RESERVE BANK of NEW YORK. https://www.newyorkfed.org/data-and-statistics/data-visualization/community-credit-profiles#about-the-data. Accessed 24 Jan 2023.
- 20.CDC. PLACES: Local data for better health. Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/places/index.html. Accessed 10 Sep 2022.
- 21.Greenlund KJ, Lu H, Wang Y, Matthews KA, LeClercq JM, Lee B, et al. PLACES: local data for better health. Prev Chronic Dis. 2022;19:E31. doi: 10.5888/pcd19.210459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kong AY, Zhang X. The use of small area estimates in place-based health research. Am J Public Health. 2020;110:829–832. doi: 10.2105/AJPH.2020.305611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC/ATSDR Social Vulnerability Index (SVI). 2022. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html. Accessed 22 Aug 2022.
- 24.Faber JW. Segregation and the geography of creditworthiness: racial inequality in a recovered mortgage market. Hous Policy Debate. 2018;28:215–247. doi: 10.1080/10511482.2017.1341944. [DOI] [Google Scholar]
- 25.Freeman A. Racism in the credit card industry. NC L Rev. 2016;95:1071. [Google Scholar]
- 26.Mental Illness [Internet]. National Institute of Mental Health (NIMH). https://www.nimh.nih.gov/health/statistics/mental-illness. Accessed 31 Aug 2022.
- 27.U.S. Census Bureau. American Community Survey 5-year Estimates. 2018. https://data.census.gov/cedsci/. Accessed 5 Jan 2022.
- 28.Singh GK, Daus GP, Allender M, Ramey CT, Martin EK, Perry C, et al. Social determinants of health in the United States: addressing major health inequality trends for the nation, 1935–2016. Int J MCH AIDS. 2017;6:139–164. doi: 10.21106/ijma.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Royston P. Multiple imputation of missing values. Stand Genomic Sci. 2004;4:227–241. [Google Scholar]
- 30.Board of Governors of the Federal Reserve System. Report on the Economic Well-Being of U.S. Households in 2018. 2019. https://www.federalreserve.gov/publications/files/2018-report-economic-well-being-us-households-201905.pdf. Accessed 21 Aug 2022
- 31.Lee J. Credit access and household well-being: evidence from payday lending. Rochester, NY; 2019. https://papers.ssrn.com/abstract=2915197. Accessed 21 Aug 2022.
- 32.Ikeda S, Kang M-I. Hyperbolic discounting, borrowing aversion and debt holding. Jpn Econ Rev. 2015;66:421–446. doi: 10.1111/jere.12072. [DOI] [Google Scholar]
- 33.Israel S, Caspi A, Belsky DW, Harrington H, Hogan S, Houts R, et al. Credit scores, cardiovascular disease risk, and human capital. Proc Natl Acad Sci. 2014;111:17087–17092. doi: 10.1073/pnas.1409794111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krieger N, Van Wye G, Huynh M, Waterman PD, Maduro G, Li W, et al. Structural racism, historical redlining, and risk of preterm birth in New York City, 2013–2017. Am J Public Health. 2020;110:1046–1053. doi: 10.2105/AJPH.2020.305656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, et al. The association between income and life expectancy in the United States, 2001–2014. JAMA. 2016;315:1750–1766. doi: 10.1001/jama.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322:1996–2016. doi: 10.1001/jama.2019.16932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Data insights: improving health through credit access | City Health Dashboard. https://www.cityhealthdashboard.com/1639. Accessed 11 Aug 2023.
- 38.Horvath A, Kay B, Wix C. The COVID-19 shock and consumer credit: evidence from credit card data. J Bank Finance. 2023;152:106854. doi: 10.1016/j.jbankfin.2023.106854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Twenge JM, Joiner TEUS. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37:954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in this study are publicly available.