Abstract
Background
Neuro-cranio-vertebral syndrome (NCVS) includes a set of idiopathic diseases: Arnold-Chiari syndrome type 0,1 and 1.5, idiopathic scoliosis, and idiopathic syringomyelia. It is caused by the pathological traction transmitted by the filum terminale on the neuraxis. Considering that the filum terminale is inserted at sacrococcygeal level, it is logical to think that an alteration of this segment’s anatomy, such as an anterior coccyx dislocation, can increase the tension exerted by the filum terminale on the neuraxis, which in turn triggers NCVS.
Methods
We collected data from 372 patients with NCVS and 15 patients with coccygeal dislocation and NCVS from our database. We analyzed the relationship between the sacrococcygeal and intercoccygeal angles with signs, symptoms and associated diagnoses. T-tests for independent samples and linear regression were used for analysis (p <0.05). We describe the MRI findings and clinical features of NCVS caused by coccygeal dislocation and compare its prevalence with that of a sample without coccygeal dislocation.
Results
65% of the signs, symptoms, and imaging features were present in similar proportions in both samples. There was a similar prevalence of cerebellar tonsillar descent and scoliosis in both groups, whereas the incidence of syringomyelia differed. A sacrococcygeal angle between 89-110° prevails in cases of syringomyelia while an intercoccygeal angle between 90-140° prevails in cases with cerebellar tonsillar descent.
Conclusions
The high clinical and radiological prevalence of coccygeal dislocation in patients with Neuro-cranio-vertebral syndrome suggests an association between them. The mechanism involved in coccygeal dislocation can directly influence the development of Neuro-cranio-vertebral syndrome.
Keywords: Coccygeal dislocation, Neuro-cranio-vertebral syndrome, Sacrococcygeal angle, Intercoccygeal angle
1. Introduction
A Coccygeal Dislocation (CD) implies a misalignment of the coccygeal segments in the coccygeal and sacrococcygeal joint with the sacrococcygeal segments.
Fracture-dislocation, on the other hand, implies an interruption in the alignment with a fracture of the involved bones, as per the publications that have been found on the Salter-Harris type I coccyx fracture.1,2 Coccygeal dislocations and fracture-dislocations are generally related to a traumatic injury, such as a fall, pressure on the coccyx during childbirth, or repetitive trauma from activities such as cycling.1, 2, 3, 4, 5 Nevertheless, 33.33 % of cases are idiopathic.6
CD usually causes acute pain in the coccyx (Coccydynia), first described by Simpson in 1859,7 which worsens in a sitting position,8 when leaning backward, standing up from a sitting position,9,10 during defecation and sexual intercourse.11 Physical examination shows sensitivity or pain upon rectal palpation of the coccyx, and frequently allows detection of an abnormally mobile coccygeal segment3,8,9,11,12 or lump.2,5
Although the cause of Coccydynia can vary, in the case of CD or fracture-dislocations, patients usually present with a history of acute trauma at least six months prior to the initial consultation,2,5,10 although this can vary up to six years.5 Coccydynia can also be caused by a degenerative “wear and tear” of the ligaments and of other protective tissues that are necessary for joint stability.4,9 Some authors have described that coccyx hypermobility, with a coccygeal flexion of more than 25° when the patient is seated, may cause Coccydynia.13 Tailbone dislocations are often due to “dynamic instability,” which occurs only when weight is placed on the coccyx. This is an important distinction because standard X-rays of the coccyx often do not show CD.9
Most of the current literature on CD consists of case reports, as the research on coccygeal instability is scarce. Most publications emphasize the presence of Coccydynia in CD, whether idiopathic or traumatic.
1.1. Diagnosis coccygeal dislocations
Lateral-view X-rays are used to diagnose CD,9,11 although they may go unseen. For this reason, a dynamic X-ray is used to view coccyx displacement when comparing standing and sitting positions.8,10 Computerized tomography is also used for the diagnosis of CD and fracture-dislocation, although it exposes the pelvic/reproductive organs to radiation. Posterior dislocation has been proven to be more common than anterior dislocation.10
Magnetic resonance imaging (MRI) has been clinically useful in the diagnosis of CD, allowing it to differentiate from other etiologies that can cause Coccydynia.8,11 However, CD is usually easy to diagnose, thus reducing the need for magnetic resonance imaging, which is more commonly used to check for fusion after treatment.2
1.2. Treatment of coccygeal dislocations
The usual CD treatment is conservative and includes antalgic and anti-inflammatory therapy, rest, and avoiding pressure in the coccyx area, all of which are generally successful in the elimination of Coccydynia.9,13 However, several cases of chronic Coccydynia resistant to treatment have been described, in which resection of the coccyx is applied. A higher success rate is observed with the disappearance of Coccydynia in cases of total coccygectomy.14 Partial coccyx resection is considered when the sacrococcygeal joint is fused or appears normal.
In cases of neurological deficits, decompression and stabilization of the area have been proposed1; however neurological involvement is not usually associated with dislocations in the lower part of the sacrum or in the sacrococcygeal joint. These consequences are related to proximal dislocations or fractures in the sacrum. Neurological deficits include cauda equina syndrome and sphincter dysfunctions.15,16
1.3. Relationship between the Neuro-cranio-vertebral syndrome and coccygeal dislocation
The concept of spinal cord traction syndrome was first described by Garceau et al in 1953,17 and we have since developed and redefined this concept by reformulating a new theory called Neuro-cranio-vertebral syndrome (NCVS), and filum disease. NCVS results from an acquired abnormal traction on the neuraxis, whereas filum disease results from congenital abnormal traction.18
The review of current publications does not associate cases of coccyx dislocation or fracture-dislocation with neurological involvement. However, research carried out at our center suggests that CD or hypermobility of the coccyx may influence the tension of the filum terminale, resulting in traction of the filum terminale and related neurological and morphological consequences. Thus, some cases of NCVS are likely to occur because of CD.
The objectives of this study were fourfold.
-
1.
To describe the clinical picture, including imaging results, of cases with coccygeal dislocation and Neuro-cranio-vertebral syndrome.
-
2.
To compare the clinical and radiological pictures of 15 cases with coccygeal dislocation and Neuro-cranio-vertebral syndrome to 372 cases with Neuro-cranio-vertebral syndrome alone.
-
3.
To compare the coccygeal dislocation angulation grade with the clinical prevalence of Neuro-cranio-vertebral syndrome.
-
4.
To propose a theoretical model that explains Neuro-cranio-vertebral syndrome triggered by coccygeal dislocation.
2. Methods
A sample of 15 cases diagnosed with CD was obtained from our center's database from December 2013 to March 2020. A separate sample of 372 patients with NCVS was obtained from our center's database from April 2009 to December 2015.
Magnetic resonance imaging and complete spine radiography were used to diagnose NCVS, and the analysis was carried out following the criteria listed in Table 1.
Table 1.
Imaging criteria for the diagnosis of Neuro-cranio-vertebral syndrome. Where FM: foramen magnum. From ‘The Filum disease and the Neuro-Cranio-vertebral syndrome: definition, clinical
picture and imaging features’. Royo-Salvador et al. BMC Neurology (2020) 20:175.
| Level of conus medullaris | Level of descent cerebellar tonsils | Syringomyelia | Scoliosis |
|---|---|---|---|
| 1. D12-L1 | 0. None | 0.None | 0. None |
| 2. L1 upper 1/3 | 1. FM-C1 upper 1/3 | 1. Less than a vertebral segment | 1. Mild |
| 3. L1 medium 1/3 | 2.FM-C1 medium 1/3 | 2. 1–2 vertebral segments | 2. Moderate |
| 4. L1 lower 1/3 | 3. FM-C1 lower 1/3 | 3. 2–4 vertebral segments | 3. Severe |
| 5. L1-L2 | 4. Between C1 upper and lower border | 4. More than 5 vertebral segments | |
| 6. L2 upper 1/3 | 5. Below C1 lower border | ||
| 7. L2 medium 1/3 | |||
| 8. L2 lower 1/3 | |||
| 9. Below L2 lower border |
Sacrococcygeal and intercoccygeal angles were measured using the OsiriX® program (Geneva, Switzerland). To identify the sacrococcygeal angle, we drew a line between the midpoint of the upper borders of the first sacral segment and the first coccygeal segment, with a line between the first coccygeal segment and the tip of the coccyx.6 Normal sacrococcygeal angles were 168° for males and 164° for females. The intercoccygeal angle was set as the intersection between the middle of the first and last coccygeal segments in the median plane, and normal values were considered to be 138° for males and 147° for females.6 A description of the variables analyzed is presented in Table 2.
Table 2.
Description of the variables analyzed. * For statistical analysis, the value “present” has been assigned to the SYMPTOM variable if the patient reports any of the symptoms. If no symptoms are reported, the value assigned to the SYMPTOM variable is “absent”. ** Decreased reflex, muscle contraction can be palpated but not visible/Very lively reflex even with small stimuli, can be accompanied by clonus. ***Difference perceived by the patient when applying cold and punch in 26 anatomical regions symmetrically in each hemibody. ****Decreased reflex, muscle contraction can be palpated but not visible/Very lively reflex even with small stimuli, can be accompanied by clonus. ***** By rubbing or scratching the anterior wall of the belly, a contraction of the abdominal muscles on the same side is produced and the belly is retracted. There are three abdominal reflexes: the superior or epigastric (above the navel), the middle (at the umbilical level) and the inferior (below the navel); pathologically, these reflexes may be exaggerated (hyperreflexia) or decreased (hyporeflexia).
| NEUROLOGICAL SYMPTOM | FINDINGS* |
|---|---|
| Headache | Frequency, location and intensity |
| Tinnitus | Uni or bilateral |
| Dizziness | Subjective/objective vertigo |
| Dysphagia | Solids, liquids or both |
| Cervical spine pain | Frequency, location and intensity |
| Upper back pain | |
| Low back pain | |
| Paresthesias | paresthesias in at least one limb |
| Gait balance | straight or lateralized gait |
| Sphincter disorder | Incontinence, urgency, pollakiuria |
| Loss of limb strength | Patient's subjective strength loss feeling or clumsiness |
| Upper/lower deep tendon reflexes | hypo/hyperreflexia in one or both extremities** |
| Thermal dysesthesia | Dysesthesia***in more than 70 % of total anatomical regions explored |
| Thermal dysesthesia | |
| Deep tendon reflexes | hypo/hyperreflexia in one or both extremities**** |
| Abdominal skin reflex | hypo/hyperreflexia and/or asymmetry***** |
| Plantar skin reflex | Babinski's sign or indifferent |
| Grip strength measurement with Jamar dynamometer | Unilateral or bilateral decrease below the 10th centile of the corresponding age and gender group |
The general data, clinical symptoms, clinical signs, and imaging features of each patient were stored in a digital database (FileMaker Pro Advanced 11.0v2, FileMaker, Inc. Santa Clara, CA, USA). The data were exported to a Microsoft Excel 2011 spreadsheet for Mac version 14.1.0 (Microsoft Corporation, Redmond, WA, USA), and then to SPSS version 21 (IBM Corporation, Armonk, NY, USA). Descriptive statistics were used to describe the clinical pictures of the CD cases. After assuming a normal distribution, the means between samples were compared with an independent samples t-test (p < 0.05), and linear regressions (p < 0.05) were used to identify the relationship between the sacrococcygeal and intercoccygeal angles and signs and symptoms, as well as radiological signs.
3. Results
3.1. Analysis of 15 cases with coccygeal dislocation and Neuro-cranio-vertebral syndrome
3.1.1. Signs & symptoms
We conducted a retrospective study of 15 patients (14 females and 1 male) aged between 11 and 54 years. All the patients were diagnosed with CD. 80 % of the patients were diagnosed with descent of the cerebellar tonsils, 33 % had idiopathic scoliosis, and 26 % had idiopathic syringomyelia. 53 % reported a history of trauma with an impact on the gluteal region. The signs and symptoms of the 15 patients are reported in Table 3, with the most common being altered plantar and deep tendon reflexes, altered grip strength, and hypoesthesia.
Table 3.
Pathological signs & symptoms prevalence in 15 cases with Coccygeal Dislocation (CD).
| Signs & Symptoms | Frequency (%) |
|---|---|
| Plantar reflexes | 100 |
| Deep tendon reflexes upper extremities | 100 |
| Deep tendon reflexes lower extremities | 93 |
| Handgrip strength | 93 |
| Tactile sensitivity | 93 |
| Thermal sensitivity | 73 |
| Abdominal reflexes | 67 |
| Headache | 100 |
| Neck pain | 93 |
| Upper back pain | 80 |
| Lower back pain | 80 |
| Dizziness | 80 |
| Loss of strength upper extremities | 73 |
| Loss of strength lower extremities | 73 |
| Tinnitus | 60 |
| Dysphagia | 53 |
| Gait balance | 53 |
| Sphincters | 40 |
We found a weak but significant association between CD and altered cutaneous plantar reflexes (p = .02, r = .12), altered tactile sensitivity (p = .02, r = .12), and decreased grip strength (p = .04, r = .10). We also found an association between patients with a sacrococcygeal angle of 100–110° and altered gait (p = .02, r = .58). There was an association between intercoccygeal angles in the range of 110–140° and altered plantar reflexes (p = .02, r = .12), decreased grip strength (p = .046, r = .10), and altered tactile sensitivity (p = .02, r = .12). Intercoccygeal angles between 90 and 109° were associated with a sensation of loss of strength in the lower extremities (p = .04, r = .10).
3.1.2. Imaging results
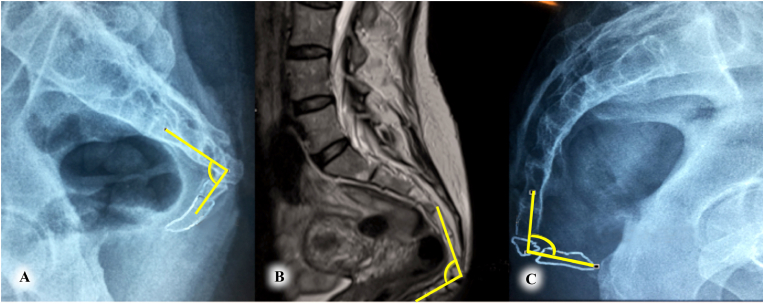
In 60 % of cases, CD was identified between the first and last coccygeal vertebrae. In the remaining 40 % of the cases, CD was identified between the sacral and coccygeal vertebrae. Only 27 % of the cases presented with intramedullary cysts. The details of the imaging results for each case are outlined in Table 4, and images of various intercoccygeal angles are displayed in Fig. 1.
Table 4.
Summary of the main imaging findings for 15 patients with CD.
| Case | Level of conus medullaris | Level of descent cerebellar tonsils | Degree of syringomyelia | Degree of scoliosis | Sacrococcygeal angle | Intercoccygeal angle |
|---|---|---|---|---|---|---|
| 1 | L1 lower 1/3 | FM-C1 lower 1/3 | None | Moderate | 90° | 117° |
| 2 | L1 lower 1/3 | FM-C1 lower 1/3 | None | None | 90° | 129° |
| 3 | L1-L2 | Between C1 upper and lower border | More than 5 vertebral segments | Mild | 100° | 137° |
| 4 | L1-L2 | FM-C1 medium 1/3 | None | None | 100° | 114° |
| 5 | L1-L2 | Between C1 upper and lower border | None | Mild | 90° | 93° |
| 6 | L1-L2 | Between C1 upper and lower border | None | Moderate | 91° | 118° |
| 7 | L2 upper 1/3 | FM-C1 lower 1/3 | 1–2 vertebral segments | None | 106° | 109° |
| 8 | L2 medium 1/3 | None | None | Moderate | 94° | 94° |
| 9 | L2 lower 1/3 | FM-C1 medium 1/3 | None | Mild | 92° | 113° |
| 10 | L1-L2 | a | More than 5 vertebral segments | Severe | 124° | 104° |
| 11 | L1-L2 | None | None | Moderate | 100° | 103° |
| 12 | Below L2 lower border | FM-C1 medium 1/3 | None | MIld | 90° | 114° |
| 13 | L1 medium 1/3 | None | 2–4 vertebral segment | Moderate | 109° | 109° |
| 14 | L2 upper 1/3 | FM-C1 lower 1/3 | None | Moderate | 46° | 92° |
| 15 | L1 medium 1/3 | Between C1 upper and lower border | None | 0 | 70° | 131° |
Not determined due to prior tonsillectomy.
Fig. 1.
Representation of the intercoccygeal angle in three different cases. (a) Illustrates case 14, with an angle of 92.3°. (b) Represents case 10, with an angle of 104.2°. (c) Depicts case 11, with an angle of 103.3°.
We found a moderate association between the sacrococcygeal angle and syringomyelia when the angle was in the range of 100–110° (p = .03, r = .53), and in the range of 89–99° (p = .04, r = .56). On the other hand, we found that the intercoccygeal angle was associated with the descent of the cerebellar tonsils when it had an angle between 90 and 109° (p = .04, r = .54), as well as when the angle was between 110 and 140° (p = .04, r = .54).
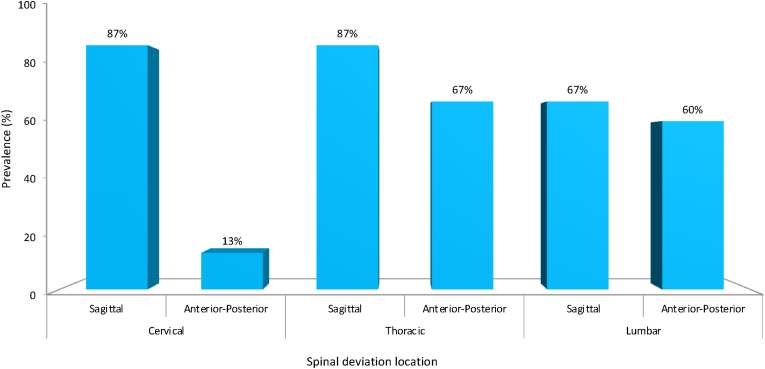
Dorsal-lumbar scoliosis was the most common spinal deviation in this group (Fig. 2).
Fig. 2.
Spinal deviation in 15 cases with CD.
Discopathies were detected at a higher incidence in the cervical (80 %) and lumbar (73 %) regions than in the thoracic region (40 %).
Comparison of 15 cases with coccygeal dislocation and Neuro-cranio-vertebral syndrome with 372 cases with Neuro-cranio-vertebral syndrome.
The symptomatology comparison between the 15 patients with CD and 372 patients with NCVS is presented in Fig. 3. The predominant spinal symptoms in both groups were neck pain, upper and lower back pain, altered gait balance, sensation of loss of strength in the upper and lower extremities, and altered sphincter function. The predominant cranial symptoms were headache, tinnitus, dysphagia, and lack of balance.
Fig. 3.
Comparison of the most common symptoms in both samples, where CD is the sample of 15 cases with coccygeal dislocation and NCVS is the sample of 372 cases with Neuro-cranio-vertebral syndrome.
A comparison of neurological signs is shown in Fig. 4, with the most predominant being altered plantar and deep tendon reflexes, loss of handgrip strength, altered tactile and thermal sensitivity, and altered abdominal reflexes.
Fig. 4.
Comparison of the most common signs in both samples. Where CD the sample of 15 cases with coccygeal dislocation and NCVS is the sample of 372 cases with Neuro-cranio-vertebral syndrome.
Signs, symptoms, and imaging features were present in 65 %, in similar proportions in both the groups. These included the following: altered balance (p = .91), dysphagia (p = .23), tinnitus (p = .29), lumbosacral pain (p = .51), loss of strength in the upper extremities (p = .06), loss of strength in the lower extremities (p = .15), descent of cerebellar tonsils (p = .97), syringomyelia (p = .05), altered sphincters (p = .40), altered gait (p = .27), scoliosis (p = .49), altered tendon reflexes in lower extremities (p = .16), altered abdominal cutaneous reflexes (p = .90), altered plantar cutaneous reflexes (p = .08), and altered thermal sensitivity (p = .71).
Signs, symptoms, and imaging features analyzed were present in 35 %, with different proportions between the groups. These included the following: headache (p = 0.00), neck pain (p = .00), mid-back pain (p = .04), extent of syringomyelia (p = .00), level of conus medullaris (p = .00), altered tendon reflexes in upper extremities (p = .00), loss of handgrip strength (p = .05), altered tactile sensitivity (p = .00).
The prevalence of scoliosis and descent of the cerebellar tonsils was >70 % in both groups. The prevalence of syringomyelia differed between the groups, although the difference was not significant (p = .05), with a greater incidence in the group of patients with NCVS. The presence of syringomyelia, descent of cerebellar tonsils, and scoliosis in each group is outlined in Table 5.
Table 5.
Summary of MRI results. CD is the coccygeal dislocation and NCVS is the Neuro-cranio-vertebral syndrome sample. Refer to Table 1 for the definitions of the conus medullaris levels.
| Diagnosis | CD (%) | NCVS (%) |
|---|---|---|
| Idiopathic syringomyelia | 27 | 52 |
| Descent cerebellar tonsils | 80 | 73 |
| Idiopathic scoliosis | 73 | 76 |
| Conus medullaris level 1-2 | 0 | 23 |
| Conus medullaris level 3-4 | 27 | 36 |
| Conus medullaris level 5-6 | 53 | 31 |
| Conus medullaris level 7-8 | 20 | 10 |
4. Discussion
4.1. Neuro-cranio-vertebral syndrome
NCVS is a redefined and updated spinal cord traction syndrome that includes Arnold-Chiari syndrome type 1, and/or idiopathic syringomyelia, and/or idiopathic scoliosis, with signs and symptoms common to these diseases.18 Considering that NCVS is a pathological process of multifactorial acquired etiology (tumor, infection, trauma, vascular alterations, iatrogenic, etc.), CD should be added to the list of etiologic factors.
Symptoms related to spinal traction were first described by Garceau, who reported three cases of paraparesis, scoliosis, headache, and dysesthesia.17 A few years later, other authors made the same observations, and the term tight filum was used to diagnose this clinical picture.19
Several causes of Neuro-cranio-vertebral syndrome have been proposed. Roth hypothesized that spinal cord stretching is responsible for scoliosis and Arnold-Chiari syndrome type 1.20 Porter considered uncoupled-osseus development to be the cause of idiopathic scoliosis.21,22 Lowe et al have suggested that neurological dysfunction plays a key role in the genesis of idiopathic scoliosis.23 Finally, Roth and Porter hypothesized that local neural dysfunction within the spinal cord may cause of idiopathic scoliosis.20, 21, 22
Some researchers have hypothesized that there is a direct correlation between cervico-medullary compression in the foramen magnum (due to the herniated cerebellar structure) and vascular insufficiency of the cervical medulla at a caudal distance from that level. In autopsy studies of syringomyelia associated with Chiari malformation, Lichtenstein and Foster et al suggested that herniated cerebellar structures compress the neuraxis as well as vessels that pass through the foramen magnum, resulting in vascular insufficiency in the cervical medulla caudal to that level.24,25 Therefore scoliosis represents an attempt by spinal cord to compensate for the medullary traction force, while syringomyelia represents the lytic and cavitary expression of the neuraxis elongation and restriction with altered central medullary perfusion. Finally, according to different authors, Arnold-Chiari syndrome type 1 could be the result of the descending traction of the neuraxis in accordance, or not, with the currently more accepted theory of a small posterior fossa.26,24
4.2. Coccygeal dislocation and Neuro-cranio-vertebral syndrome
Signs and symptoms were present in similar proportions, 65 % in both the groups, with a predominance of spinal signs and symptoms in the CD group. The high prevalence of spinal symptoms and neurological signs in patients with CD may be due to the presence of subclinical or undiagnosed NCVS that worsens with the slow and progressive increase in tension caused by CD. Long periods of time between the moment of coccyx trauma and the onset of Neuro-cranio-vertebral syndrome suggest a subclinical evolution of the disease, probably in relation to a minimal but sufficient traction of the filum terminale. This suggests that the intensity of spinal traction as important as its duration.
In cases of CD the most common associated condition was descent of the cerebellar tonsils (80 %). This differs from NCVS, in which idiopathic scoliosis is the most frequent condition (76 %). In CD cases, it may be easier to displace the nervous system and descend the cerebellar tonsils rather than twist a mature spine. The high prevalence of cerebellar tonsils descent in patients with CD suggests that the NCVS is the result of an acquired medullary traction triggered by the CD. It is interesting to consider that specific intercoccygeal angles in CD patients are associated with descent of the cerebellar tonsils. It may be important to consider this when assessing patients. Our sample size for patients with CD was small (n = 15).
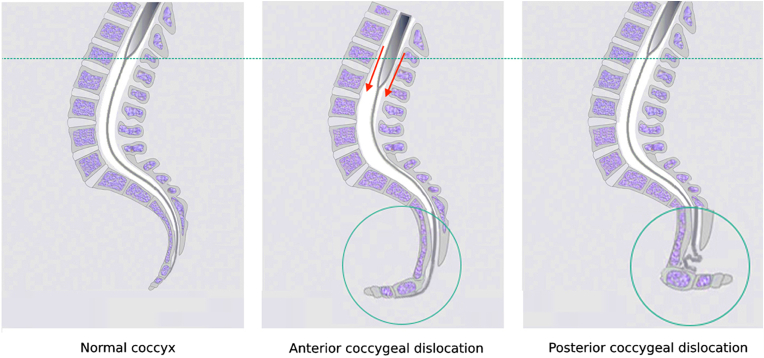
Only 8 (53 %) of the 15 patients with CD reported a traumatic antecedent because surely they have forgotten the coccygeal trauma that happened years ago. And the lack of radiological documentation is because frequent falls on the buttocks are usually not interpreted as requiring medical assistance. There may not be a relationship between the time of the traumatic incident and appearance of the first symptoms of NCVS. There may not be a relationship between the time of the traumatic incident and appearance of the first symptoms of NCVS. In addition, the impact of falling on the buttocks is minimized by the gluteal muscles. The coccyx is well protected by the gluteal muscles, but under axial pressure, it can dislocate or subdislocate. If the dislocation occurs backward, in the form of posterior coccygeal dislocation, it has fewer consequences. The anatomical relationship between the position of the coccyx, filum terminale and dural sac is illustrated in Fig. 5.
Fig. 5.
Model explaining the effect of the coccyx on the filum terminale and dural sac. From left to right: normal filum terminale tension, abnormal filum terminale tension in anterior coccyx dislocation, and posterior coccyx dislocation releasing the tension.
A limitation of this study was the small sample size of patients with CD. Therefore, we cannot confirm or generalize these findings to all patients with CD. Nevertheless, we hope that this study will invite further research in this area so that the results may be more representative and stronger conclusions can be drawn and to better extrapolate these results to the population.
5. Conclusions
Can a simple fall on the buttocks eventually cause a neurological condition called Neuro-cranio-vertebral syndrome? We propose that it is possible. In this article we describe a new syndrome: Neuro-cranio-vertebral syndrome due to coccygeal dislocation.
While there were signs and symptoms that were present in similar proportions in both samples (65 %), there were also some that had different proportions (35 %). MRI results showed a similar incidence of cerebellar tonsils descent (80 % CD, 73 % NCVS) and idiopathic scoliosis (73 % CD, 76 % NCVS) and slight differences in the prevalence of syringomyelia (27 % CD, 52 % NCVS). We found that a sacrococcygeal angle between 89 and 110° could be a predictor of syringomyelia. If the intercoccygeal angle is between 90 and 140°, it could be a predictor of descent of the cerebellar tonsils.
When a patient comes to our center with medical antecedents of sacrococcygeal trauma and complaints of headaches, tinnitus, dysphagia, lack of balance, neck pain, upper and lower back pain, altered gait balance, sensations of loss of strength in the upper and lower extremities, altered sphincters, and neurological signs (altered plantar and deep tendon reflexes, loss of handgrip strength, altered tactile and thermal sensitivity, and altered abdominal reflexes), we must suspect the presence of Neuro-cranio-vertebral syndrome. We must then request imaging for complete diagnosis and appropriate treatment.
The type of coccygeal dislocation and its evolution over time can precipitate the development of Neuro-cranio-vertebral syndrome. This study emphasizes the importance of early diagnosis and treatment of coccygeal dislocation when assessing patients, to prevent the possible development of Neuro-cranio-vertebral syndrome in the future prospective studies will be necessary to better understand the pathophysiology of this disease.
Ethics approval and consent to participate
We used our center's database of patient records retrospectively. Patient data were anonymized in accordance with the legislation existing when the study was initiated, following the necessary technical and organizational guarantees and measures.
Consent for publication
Not applicable.
CRediT authorship contribution statement
Miguel B. Royo-Salvador: Writing - original draft, Supervision, Project administration, Data curation, Conceptualization. Marco V. Fiallos-Rivera: Writing - original draft, Data curation, Conceptualization. Pamela Villavicencio: Writing - review & editing, Formal analysis, Data curation.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper
Acknowledgements
We thank Ms. Katharina Kühn for her help in translating and reviewing the manuscript, Ms. Elena de’ Michieli Vitturi for her help in translating the manuscript and Mrs. Gioia Luè for her help in the management and organization of the institute's R + D + I department. We would also like to thank Ms. Amelia Peiró for her help in the literature review for the study and Mr. Juan Manuel Jené Gaspar and Mr. Anoop Tiwari for updating the FileMaker Pro database and for their help creating images. We thank Ms. Mara Espino Hernández for her help with administration, social and financial management. We thank the Chiari & Scoliosis & Syringomyelia Foundation for their support, and all the other staff at the Institut Chiari & Siringomielia & Escoliosis de Barcelona that have contributed to patient care and data collection, preparation, and analysis. We thank all our patients and caregivers, without whom this work would not have been possible.
References
- 1.Gutierrez-Gomez S., Wahl L., Blecher R., et al. Sacral fractures: an updated and comprehensive review. Injury. 2021;52(3):366–375. doi: 10.1016/j.injury.2020.11.015. [DOI] [PubMed] [Google Scholar]
- 2.Hamoud K., Abbas J. Fracture dislocation of the sacro-coccygeal joint in a 12-year-old boy. A case report and literature review. Orthop Traumatol Surg Res. 2015;101(7):871–873. doi: 10.1016/j.otsr.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 3.Bergkamp A.B., Verhaar J.A. Dislocation of the coccyx: a case report. J Bone Joint Surg Br. 1995;77(5):831–832. [PubMed] [Google Scholar]
- 4.Olemoko P.L., Mulbah R. Coccygectomy for chronic, symptomatic coccygeal dislocation: case report. East Afri Orthopaedic J. 2017;11(2):73–76. [Google Scholar]
- 5.Kim W.Y., Han C.W., Kim Y.H. Joystick reduction and percutaneous pinning for an acutely anteriorly dislocated coccyx: a case report. J Orthop Trauma. 2004;18(6):388–389. doi: 10.1097/00005131-200407000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Woon J.T.K., Perumal V., Maigne J.Y., Stringer M.D. CT morphology and morphometry of the normal adult coccyx. Eur Spine J. 2013;22(4):863–870. doi: 10.1007/s00586-012-2595-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simpson J.Y. vol. 40. Med Times Gaz; 1859. pp. 1–7.https://www.coccyx.org/medabs/simpson.htm (On Coccyodynia, and the Diseases of the Coccyx). [Google Scholar]
- 8.Trouvin A.P., Goeb V., Vandhuick T., Michelin P., Lequerré T., Vittecoq O. Role for magnetic resonance imaging in Coccydynia with sacrococcygeal dislocation. Joint Bone Spine. 2013;80(2):214–216. doi: 10.1016/j.jbspin.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Foye P.M., Shah J.M., Sinha D. Musculoskeletal Sports and Spine Disorders. 2017. Coccyx fracture and dislocation. [Google Scholar]
- 10.Maigne J.Y., Doursounian L., Chatellier G. Causes and mechanisms of common Coccydynia: role of body mass index and coccygeal trauma. Spine. 2000;25(23):3072–3079. doi: 10.1097/00007632-200012010-00015. (Phila Pa 1976. [DOI] [PubMed] [Google Scholar]
- 11.Mouhsine E., Garofalo R., Chevalley F., et al. Posttraumatic coccygeal instability. Spine J. 2006;6(5):544–549. doi: 10.1016/j.spinee.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Kanabur P., Gowd A., Bulkeley J.A., Behrend C.J., Carmouche J.J. Symptomatic sacrococcygeal joint dislocation treated using closed manual reduction: a case report with 36-month follow-up and review of literature. Trauma Case Rep. 2017;12:11–15. doi: 10.1016/j.tcr.2017.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nathan S.T., Fisher B.E., Roberts C.S. Coccydynia: a review of pathoanatomy, aetiology, treatment and outcome. J Bone Joint Surg Br. 2010;92(12):1622–1627. doi: 10.1302/0301-620X.92B12.25486. [DOI] [PubMed] [Google Scholar]
- 14.Antoniadis A., Ulrich N.H.B., Senyurt H. Coccygectomy as a surgical option in the treatment of chronic traumatic coccygodynia: a single-center experience and literature review. Asian Spine J. 2014;8(6):705. doi: 10.4184/asj.2014.8.6.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalra M., Anand S. Delayed sacral laminectomy for cauda equina in a child following fracture-dislocation of Sacrum. Injury. 1997;28(8):565–566. doi: 10.1016/s0020-1383(97)00116-2. [DOI] [PubMed] [Google Scholar]
- 16.Hussin P., Chan C.Y., Saw L.B., Kwan M.K. U-shaped sacral fracture: an easily missed fracture with high morbidity. A report of two cases. Emerg Med J. 2009;26(9):677–678. doi: 10.1136/emj.2008.064972. [DOI] [PubMed] [Google Scholar]
- 17.Garceau G.J. The filum terminale syndrome (the cord-traction syndrome) J Bone Joint Surg Am. 1953;35-A(3):711–716. [PubMed] [Google Scholar]
- 18.Royo-Salvador M.B., Fiallos-Rivera M.V., Salca H.C., Ollé-Fortuny G. The Filum disease and the Neuro-Cranio-vertebral syndrome: definition, clinical picture and imaging features. BMC Neurol. 2020;20(1):175. doi: 10.1186/s12883-020-01743-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jones P.H., Love J.G. Tight filum terminale. AMA Arch Surg. 1956;73(4):556–566. doi: 10.1001/archsurg.1956.01280040010002. [DOI] [PubMed] [Google Scholar]
- 20.Roth M. Idiopathic scoliosis from the point of view of the neuroradiologist. Neuroradiology. 1981;21(3):133–138. doi: 10.1007/bf00339521. [DOI] [PubMed] [Google Scholar]
- 21.Porter R.W. Can a short spinal cord produce scoliosis? Eur Spine J. 2001;10(1):2–9. doi: 10.1007/s005860000188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Porter R.W. The pathogenesis of idiopathic scoliosis: uncoupled neuro-osseous growth? Eur Spine J. 2001;10(6):473–481. doi: 10.1007/s005860100311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lowe T.G., Edgar M., Margulies J.Y., et al. Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg Am. 2000;82(8):1157–1168. doi: 10.2106/00004623-200008000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Lichtenstein B.W. Cervical syringomyelia and syringomyelia-like states associated with Arnold-Chiari deformity and platybasia. Arch Neurol Psychiatr. 1943;49(6):881. doi: 10.1001/archneurpsyc.1943.02290180105011. [DOI] [Google Scholar]
- 25.Foster J.B., Hudgson P., Pearce G.W. The association of syringomyelia and congenital cervico-medullary anomalies: pathological evidence. Brain. 1969;92(1):25–34. doi: 10.1093/brain/92.1.25. [DOI] [PubMed] [Google Scholar]
- 26.Roth M. Cranio-cervical growth collision: another explanation of the Arnold-Chiari malformation and of basilar impression. Neuroradiology. 1986;28(3):187–194. doi: 10.1007/bf00548190. [DOI] [PubMed] [Google Scholar]