Abstract
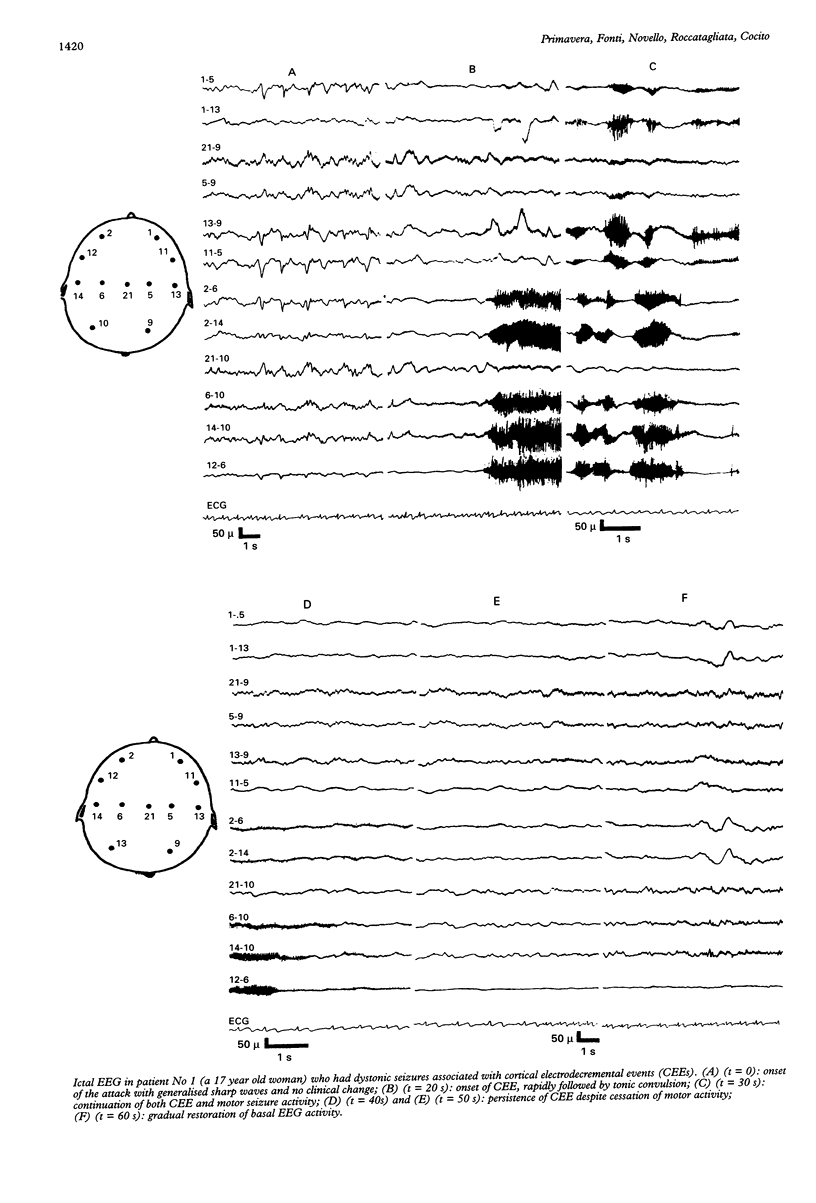
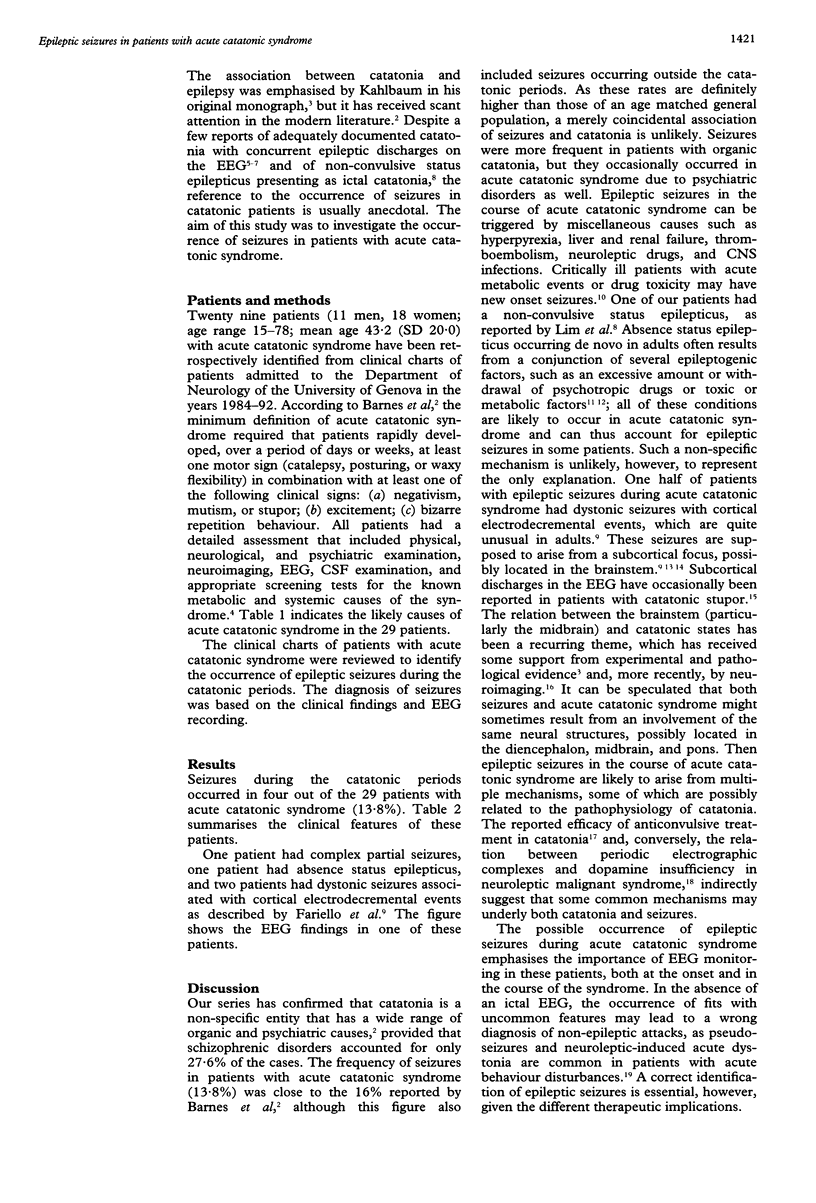
Acute catatonic syndrome is a condition that can be caused by a variety of metabolic, neurological, psychiatric, and toxic conditions, including neuroleptic malignant syndrome. Although ictal catatonia as a manifestation of non-convulsive status epilepticus has been described, reference to the occurrence of seizures in patients with acute catatonic syndrome is anecdotal. Twenty nine patients with acute catatonic syndrome were reviewed to identify patients with seizures after the onset of acute catatonic syndrome. Patients were divided into four diagnostic groups: affective (15), schizophrenic (eight), toxic (two), and organic (four). Seizures occurred in four patients (13.8%): two patients with dystonic seizures had viral encephalitis and schizophrenic disorder respectively; one patient with complex partial seizures had viral encephalitis and one patient with absence status had neuroleptic malignant syndrome. The results indicate the value of EEG in detection of epileptic activity in patients with acute catatonic syndrome, both at onset and in the course of such disturbance, particularly to provide a differential diagnosis between pseudo-seizures and neuroleptic-induced acute dystonia.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barnes M. P., Saunders M., Walls T. J., Saunders I., Kirk C. A. The syndrome of Karl Ludwig Kahlbaum. J Neurol Neurosurg Psychiatry. 1986 Sep;49(9):991–996. doi: 10.1136/jnnp.49.9.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fariello R. G., Doro J. M., Forster F. M. Generalized cortical electrodecremental event. Clinical and neurophysiological observations in patients with dystonic seizures. Arch Neurol. 1979 May;36(5):285–291. doi: 10.1001/archneur.1979.00500410063009. [DOI] [PubMed] [Google Scholar]
- GOLDENSOHN E. S., GOLD A. P. Prolonged behavioral disturbances as ictal phenomena. Neurology. 1960 Jan;10:1–9. doi: 10.1212/wnl.10.1.1. [DOI] [PubMed] [Google Scholar]
- Gelenberg A. J. The catatonic syndrome. Lancet. 1976 Jun 19;1(7973):1339–1341. doi: 10.1016/s0140-6736(76)92669-6. [DOI] [PubMed] [Google Scholar]
- Gomez E. A., Comstock B. S., Rosario A. Organic versus functional etiology in catatonia: case report. J Clin Psychiatry. 1982 May;43(5):200–201. [PubMed] [Google Scholar]
- Johnson J. Catatonia: the tension insanity. Br J Psychiatry. 1993 Jun;162:733–738. doi: 10.1192/bjp.162.6.733. [DOI] [PubMed] [Google Scholar]
- Johnson J. Stupor: a review of 25 cases. Acta Psychiatr Scand. 1984 Oct;70(4):370–377. doi: 10.1111/j.1600-0447.1984.tb01222.x. [DOI] [PubMed] [Google Scholar]
- Joseph A. B., Anderson W. H., O'Leary D. H. Brainstem and vermis atrophy in catatonia. Am J Psychiatry. 1985 Mar;142(3):352–354. doi: 10.1176/ajp.142.3.352. [DOI] [PubMed] [Google Scholar]
- Lim J., Yagnik P., Schraeder P., Wheeler S. Ictal catatonia as a manifestation of nonconvulsive status epilepticus. J Neurol Neurosurg Psychiatry. 1986 Jul;49(7):833–836. doi: 10.1136/jnnp.49.7.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd G. G. Acute behaviour disturbances. J Neurol Neurosurg Psychiatry. 1993 Nov;56(11):1149–1156. doi: 10.1136/jnnp.56.11.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutani R., Bergamini L., Fariello R. A case of status epilepticus with tonic expression (so called "reticular epilepsy"). Physiopathological study. Epilepsia. 1970 Sep;11(3):321–326. doi: 10.1111/j.1528-1157.1970.tb03896.x. [DOI] [PubMed] [Google Scholar]
- Nathanson M., Krumholz A., Biddle D. Seizures of axial structures. Presumptive evidence for brain stem origin. Arch Neurol. 1978 Jul;35(7):448–452. doi: 10.1001/archneur.1978.00500310050010. [DOI] [PubMed] [Google Scholar]
- Rankel H. W., Rankel L. E. Carbamazepine in the treatment of catatonia. Am J Psychiatry. 1988 Mar;145(3):361–362. doi: 10.1176/ajp.145.3.361. [DOI] [PubMed] [Google Scholar]
- Thomas P., Lebrun C., Chatel M. De novo absence status epilepticus as a benzodiazepine withdrawal syndrome. Epilepsia. 1993 Mar-Apr;34(2):355–358. doi: 10.1111/j.1528-1157.1993.tb02421.x. [DOI] [PubMed] [Google Scholar]
- Thompson S. W., Greenhouse A. H. Petit mal status in adults. Ann Intern Med. 1968 Jun;68(6):1271–1279. doi: 10.7326/0003-4819-68-6-1271. [DOI] [PubMed] [Google Scholar]
- Wijdicks E. F., Sharbrough F. W. New-onset seizures in critically ill patients. Neurology. 1993 May;43(5):1042–1044. doi: 10.1212/wnl.43.5.1042. [DOI] [PubMed] [Google Scholar]


