Abstract
Gliomas are one of the most common primary malignant tumours of the central nervous system (CNS), of which glioblastomas (GBMs) are the most common and destructive type. The glioma tumour microenvironment (TME) has unique characteristics, such as hypoxia, the blood-brain barrier (BBB), reactive oxygen species (ROS) and tumour neovascularization. Therefore, the traditional treatment effect is limited. As cellular oxidative metabolites, ROS not only promote the occurrence and development of gliomas but also affect immune cells in the immune microenvironment. In contrast, either too high or too low ROS levels are detrimental to the survival of glioma cells, which indicates the threshold of ROS. Therefore, an in-depth understanding of the mechanisms of ROS production and scavenging, the threshold of ROS, and the role of ROS in the glioma TME can provide new methods and strategies for glioma treatment. Current methods to increase ROS include photodynamic therapy (PDT), sonodynamic therapy (SDT), and chemodynamic therapy (CDT), etc., and methods to eliminate ROS include the ingestion of antioxidants. Increasing/scavenging ROS is potentially applicable treatment, and further studies will help to provide more effective strategies for glioma treatment.
Keywords: glioma, ROS, tumor microenvironment, antioxidants, photodynamic therapy, sonodynamic therapy, chemodynamic therapy, nanodrug delivery platforms
1. Introduction
Gliomas are the most common primary malignant tumours of the central nervous system (CNS), accounting for approximately 30% of all primary brain and CNS tumours and 80% of malignant brain tumours (1). According to the criteria set by the World Health Organization (WHO), the malignancy of gliomas is divided into grades I-IV, ranging from mild to severe. Glioblastomas (GBMs) are grade IV gliomas and are the most common type. Unfortunately, GBMs are also the most dangerous, with relapses being inevitable even after rigorous treatment (2). Due to the unique characteristics of the glioma tumour microenvironment (TME), such as hypoxia, the blood–brain barrier (BBB), reactive oxygen species (ROS), and tumour neovascularization, treatment often show poor efficacy (3–5). The standard treatment for GBMs is resection followed by radiotherapy and temozolomide (TMZ) chemotherapy, but the median survival of GBM patients is only 14.6 months (6). In addition, the humanized IgG1 monoclonal antibody bevacizumab is also commonly used in the clinical treatment of GBMs (7). According to the available studies, neither TMZ nor bevacizumab is sufficient to treat gliomas. TMZ causes alkylation of genomic DNA at the N7 and O6 sites of guanine and at the N3 site of adenine. When the alkylation lesion at the guanine O6 position is not repaired, it leads to mispairing during DNA replication, which triggers a break in the DNA strand and causes GBM cell death (8–10). However, O6-methylguanine-DNA methyltransferase (MGMT) exists in GBM cells, cleans the alkyl group produced by TMZ and repairs damaged DNA. The presence of MGMT is an important reason for the resistance of GBMs to TMZ (11). Bevacizumab targets a protein called vascular endothelial growth factor-A (VEGF-A) and slows tumour growth and proliferation by preventing tumour angiogenesis, thereby depriving GBM cells of nutrient uptake (7). However, due to tumour heterogeneity and insufficient pharmacokinetics, it is still difficult to prevent GBM recurrence with antiangiogenic therapy (12–14). Therefore, the search for new treatment methods for gliomas has become a hotspot of current research.
ROS are reactive substances produced by oxygen reduction, including hydrogen peroxide (H2O2), organic hydroperoxide (ROOH), singlet oxygen (1O2), ozone (O3), superoxide anion (O2˙‾ ), hydroxyl radical (OH·), and peroxyl radical (ROO·) (15), etc. Certain levels of ROS are required for cell survival and are involved in cell proliferation and differentiation (16), skeletal muscle contraction (17), immune response (18) and other processes. These physiological effects are based on the regulation of multiple signalling pathways by ROS, such as the nuclear factor-kappaB (NF-κB), phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT), and mitogen-activated protein kinases (MAPKs) (19, 20). The normal function of cells also depends on the ROS threshold, which represents the critical point of intracellular ROS levels (15, 21). A level of ROS slightly below the threshold is helpful to maintain normal cell function. However, when ROS persistently accumulate abnormally beyond the threshold, they may cause irreversible oxidative damage to cells or even lead to cell death (21).
In gliomas, appropriate amounts of ROS can activate growth-related signalling pathways, induce DNA mutations, and promote invasion and metastasis (22–24). However, it has been shown that inducing ROS accumulation leads to glioma cell death (25, 26). In contrast, given the critical role of ROS in the cell, the depletion of ROS also makes it difficult for glioma cells to survive (27, 28). Therefore, controlling the level of ROS becomes a potential strategy for glioma treatment. According to the literature, methods to induce massive ROS production include photodynamic therapy (PDT) (29), sonodynamic therapy (SDT) (30) and chemodynamic therapy (CDT) (31). The main approach to ROS reduction is the application of various antioxidants (27, 28, 32). All these methods have the potential to be used to treat gliomas. Therefore, we need to better understand the mechanisms of ROS production and clearance in gliomas, as well as their role in the glioma TME. Meanwhile, the methods based on ROS generation/scavenging also contribute to the prevention and treatment of gliomas.
2. ROS production and antioxidant defence systems
ROS production is caused by exogenous environmental stimuli or endogenous metabolism. Exogenous ROS can be generated by environmental pollutants, such as heavy metals (33), ultraviolet radiation (34), asbestos (35), sulfur dioxide (36), and particulate matter with a diameter of less than 2.5 µm (PM2.5) (37). Endogenous ROS production is mainly dependent on the mitochondrial electron transport chain (ETC) (38) and NADPH oxidases (NOXs) (39). In some cases, peroxisomes (40) and endoplasmic reticulum membranes (41) have also been identified as ROS production sites.
When ROS levels are elevated, glioma cells initiate their own antioxidant defence system in response to oxidative stress (OS). These antioxidant defence systems consist of a series of enzymes, such as superoxide dismutase (SOD) (42), catalase (CAT) (43), glutathione peroxidase (GPX) (44), glutathione reductase (GSR) (45), haem oxygenase (HMOX) (46), peroxiredoxin (PRDX) (47), thioredoxin (TRX) (48), and quinone oxidoreductase 1 (NQO1) (49). Nonenzymes include glutathione (GSH) (50), α-lipoic acid (51), and coenzyme Q10 (CoQ10) (52). Of note, nuclear factor erythroid 2-related factor 2 (NRF2) is a basic leucine zipper (bZIP) transcription factor that is an important controller of the activation of cellular antioxidant defence systems (53). Under normal conditions, Kelch-like ECH-associated protein 1 (KEAP1) can promote the polyubiquitination and degradation of NRF2 to maintain a certain level of NRF2. However, under OS, KEAP1 is oxidized, and NRF2 enters the nucleus and binds to the antioxidant response element (ARE) sequence, thereby activating the expression of the abovementioned series of antioxidant enzymes (54–58). In addition, after DNA damage caused by OS, DNA repair mechanisms in glioma cells are activated to repair damaged DNA and exert indirect antioxidant effects, such as direct repair (59–61), base excision repair (BER) (62), mismatch repair (MMR) (63, 64), and nucleotide excision repair (NER) (65, 66). A summary of the antioxidant defence systems in glioma cells is presented in Table 1 .
Table 1.
Glioma-associated antioxidant defence systems.
| Classification | Name | Function | Related research | Reference |
|---|---|---|---|---|
| Antioxidant enzymes | SOD | It catalyses O2 •- to form molecular oxygen and H2O2. | 1) After treatment with the EZH2 inhibitor GSK343, the levels of SOD decrease and the production of ROS increases in GBM cells, ultimately leading to cell death. 2) After knocking down the eIF4E gene, there is a decrease in SOD levels and an increase in H2O2 levels in glioma cells, ultimately leading to cell death. 3) Mutation of BRG1 in gliomas leads to elevated levels of ROS and reduced expression of SOD, thereby increasing the sensitivity of gliomas to TMZ treatment. 4) After TMZ treatment, there is an increase in the expression of Sp1, an upregulation of SOD2, a reduction in ROS levels, ultimately promoting the survival of GBM cells. |
(42, 67–70) |
| CAT | It decomposes H2O2 generated by SOD. | 1) The overexpression of CAT and reduction of H2O2 contribute to the resistance of glioma cells to TMZ. 2) Knocking down CEBPD downregulates CAT expression and increases H2O2 levels, consequently inducing GBM cell death. |
(43, 71) | |
| GPX | They are selenium-containing enzymes that ensure the detoxification of H2O2 and lipid peroxides. | 1) The curcumin analogue ALZ003 promotes AR degradation, enhances ROS levels, and inhibits GPX4, ultimately resulting in GBM cell death. 2) Plumbagin induces the degradation of GPX4 and elevates ROS levels, consequently inhibiting the growth of GBMs. |
(44, 72, 73) | |
| GSR | It binds to NADPH and prevents oxidative damage. | Overexpression of GSR decreases ROS levels, thereby promoting glioma resistance to TMZ. | (45, 74) | |
| HMOX | It catalyses the formation of the antioxidant bilirubin from heme. | 1) Chaetocin sensitizes GBM cells to TRAIL-induced apoptosis by inducing ROS production and DNA damage. The deficiency of HMOX1 can enhance the sensitizing effect of chaetocin on TRAIL. 2) Overexpression of NRF2 can increase HMOX1 expression, reduce ROS, reduce the cytotoxicity of carmustine, and promote glioma cell survival. 3) ATO promotes glioma cell damage and HMOX1 expression by inducing the production of ROS. Inhibitors of HMOX1 significantly increase glioma cell death and ROS generation induced by ATO. |
(46, 75–77) | |
| PRDX | It contains cysteine residues that transmit REDOX signals. | Overexpression of PRDX4 leads to the downregulation of ROS, contributing to the promotion of GSC cell survival. | (47, 78) | |
| TRX | It has a reducing effect and can eliminate ROS. | The use of TRX inhibitors leads to an increase in ROS levels in GBM cells, triggering cell death. | (48, 79, 80) | |
| NQO1 | It neutralizes ROS in the plasma membrane and prevent lipid peroxidation. | 1) The drug MNPC inhibits NQO1, leading to increased ROS levels and promoting GBM cell death. 2) C/EBPβ can regulate the transcription of NQO1, neutralize ROS in GBM cells, and promote proliferation. 3) NQO1 can also bind with the substrate TSB, resulting in the significant generation of ROS, and promoting GBM cell death. |
(49, 81–83) | |
| Antioxidant nonenzymes |
GSH | It contains active mercaptan groups. | 1)The use of ciglitazone promotes the production of ROS, leading to a decrease in GSH levels and cell death in glioma cells. 2) SAS decreases GSH levels, induces ROS production, and promotes GBM cell death. 3) Silibinin induces autophagy in glioma, resulting in the depletion of GSH, elevation of H2O2, and BNIP3-dependent nuclear translocation of AIF, ultimately leading to glioma cell death. |
(50, 84–86) |
| α-lipoic acid | It has both pro-oxidation and antioxidation effects. | Activation of TRPA1 induces hypoxia and OS in gliomas, potentially resulting in apoptosis. However, α-lipoic acid has been shown to reverse these effects, thereby promoting glioma cell survival. | (51, 87) | |
| CoQ10 | Its reduced form protects against lipid peroxidation damage. | CoQ10 reduces ROS levels and shifts the oxidative balance towards a pro-oxidant state, thereby enhancing the sensitivity of GBM cells to radiation therapy and chemotherapy. | (52, 88) | |
| DNA repair enzymes | MGMT | It is one of the direct DNA repair proteins. It repairs DNA damage caused by OS by removing methyl groups. | The upregulation of GBP3 contributes to TMZ resistance in GBMs through the induction of NRF2 and MGMT expression. | (59–61) |
| PARP1 | PARP1 belongs to BER, which can recognize, cleave, and repair DNA damage caused by OS. | PARP1 plays a crucial role in the repair of DNA damage caused by ROS and facilitates the survival of GBM cells. | (62, 89) | |
| MSH2 | MSH2 belongs to MMR, which can recognize and repair incorrectly paired nucleotides generated during DNA replication. | After TMZ treatment, MEX3A expression is increased in GBM cells, binding to MSH2 mRNA and recruiting the CCR4-NOT complex to facilitate its degradation. Consequently, this leads to reduced DNA mismatch repair activity and decreased sensitivity of GBM cells to TMZ. | (63) | |
| MSH6 | MSH6 belongs to MMR and participates in DNA mismatch repair. | MSH6 leads to TMZ resistance in GBM, and the hypoxic TME induced by MSH6 may promote GBM metastasis through EMT and angiogenesis. | (64) | |
| XPC | XPC belongs to NER, which can recognize, excision and repair DNA damage caused by OS. | Nuclear translocation of XPC leads to TMZ resistance in MGMT-deficient GBMs. | (65, 66, 90) | |
| Transcription factors | NRF2 | It can lead to activation of the transcription of AREs. | 1) APOC1 reduces ferroptosis in GBMs by inhibiting KEAP1, promoting NRF2 nuclear translocation, increasing HMOX1 and NQO1 expression, and downregulating ROS. 2) IR-TMZ can induce the generation of ROS, leading to the upregulation of NRF2 and promoting GBM recurrence. Blocking the activation of NRF2 can enhance the sensitivity of GBMs to chemoradiotherapy. 3) S-guanylation of KEAP1 in glioma cells is induced by 8-nitro-cGMP, which leads to the activation of NRF2. Subsequently, the expression of HMOX1 is induced, while the level of H2O2 decreases, resulting in the survival of glioma cells. |
(91–94) |
EZH2, enhancer of zeste homologue 2; eIF4E, eukaryotic translation initiation factor 4E; BRG1, Brahma-related gene 1; Sp1, Specificity protein 1; CEBPD, CCAAT enhancer-binding protein delta; AR, androgen receptor; TRAIL,TNF-related apoptosis-inducing ligand; ATO, arsenic trioxide; C/EBPβ, CCAAT/enhancer binding protein (C/EBP)beta; TSB, tanshindiol B; SAS, sulfasalazine; BNIP3, Bcl-2 19-kDa interacting protein 3; AIF,apoptosis inducing factor; TRPA1, transient receptor potential ankyrin 1; GBP3,guanylate binding protein 3; PARP1, poly(ADP-ribose) polymerase 1; MSH2/6, MutS homologue 2/6; MEX3A, Mex-3 RNA binding family member A; CCR4-NOT, carbon catabolite-repression 4-Not; XPC, xeroderma pigmentosum complementation group C; APOC1, apolipoprotein C1; IR, irradiation; 8-nitro-cGMP, 8-nitroguanosine 3’,5’-cyclic monophosphate.
3. The role of ROS in the glioma TME
The glioma TME plays an important role in the growth, invasion, recurrence and drug resistance of gliomas. Its major components include glioma cells, immune cells, signalling molecules, stromal cells, and extracellular matrix (ECM) (95). Immune cells include glioma-associated macrophages/microglia (GAMs), myeloid-derived suppressor cells (MDSCs), T cells, monocytes, neutrophils, dendritic cells (DCs) and natural killer (NK) cells. Signalling molecules include chemokines, cytokines, growth factors, and angiogenesis factors. Stromal cells include astrocytes and endothelial cells. The extracellular matrix (ECM) is a three-dimensional structure composed of fibrin, proteoglycans and other molecules that provides biochemical and structural support for surrounding cells and plays an important role in glioma invasion and metastasis (95, 96). Among them, as important regulatory molecules, the presence of ROS have a significant impact on the glioma TME. ROS not only affect the function of immune cells ( Figure 1 ) but also participate in the process of glioma cell proliferation, invasion, metastasis and death. These studies will be discussed in this section.
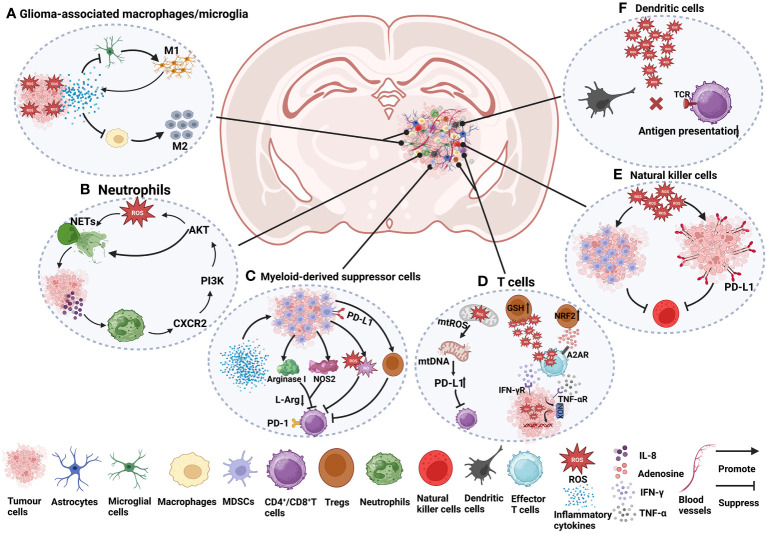
Figure 1.
The role of ROS in immune cells in the glioma TME. (A) Under ROS stress, tumour cells secrete many cytokines, such as IL-4, IL-6, IL-10, and TGF-β, which cause macrophage immunosuppression and facilitate the recruitment of M2 tumour-associated macrophages (97–99). The activation of microglia is mainly manifested as the M1 type, accompanied by the release of a series of inflammatory factors (96, 100). (B) NETs induce glioma cells to secrete IL-8 to recruit neutrophils, promote the CXCR2/PI3K/AKT/ROS signalling axis, and finally promote the formation of NETs, forming a positive feedback pathway (101). (C) Cytokines and growth factors, such as granulocyte-macrophage colony stimulating factor (GM-CSF), granulocyte colony stimulating factor (G-CSF), IL-2, IL-1β, IL-6, and VEGF, can induce the aggregation of MDSCs in tumour hosts (102, 103). In the plasma of GBM patients, the level of arginase is often increased, which is related to the inhibitory function of MDSCs (102). Arginase I reduces L-arginine (L-Arg) levels (104), thereby inhibiting T-cell activation (103). Nitric oxide synthase 2 (NOS2) is another major catabolic enzyme for L-Arg metabolism in MDSCs (105). MDSCs also secrete NO and ROS, which induce T-cell inhibition (105). MDSCs also indirectly affect the activation of T cells by inducing Tregs (103). CD4+ effector memory T cells (CD4+ TEM) infiltrated by GBM strongly upregulate PD-1, and the corresponding ligand PD-L1 is expressed in MDSCs from tumours, which are involved in functional T-cell exhaustion (106). (D) The increase in mtROS causes mitochondrial DNA damage and upregulates the expression of PD-L1 to inhibit T-cell activation (97, 107). ROS produced by Tregs can suppress effector T cells (CD4+ and CD8+). Effector T cells can induce an increase in ROS in tumour cells through IFN-γ and TNF-α, which can damage tumour cell DNA and lead to tumour cell death. Tregs themselves are more resistant to oxidative stress due to the increased activity of the antioxidant system, for example, by increasing GSH and upregulating NRF2 (108). Adenosine produced by Tregs can also inhibit effector T-cell function in an A2AR-dependent manner (109). (E) ROS induce the proliferation of MDSCs and inhibit NK cell function (110). In addition, high levels of ROS promote PD-L1 expression on cancer cells, thereby inactivating NK cells (111). (F) High levels of ROS can disrupt antigen presentation between T cells and DCs, which in turn affects the recognition of tumour antigens by T cells (98, 108).
3.1. GAMs
Macrophages and microglia are important cell types in the immune system. Macrophages are primarily derived from bone marrow-resident haematopoietic stem cells (112). After entering the blood, mature mononuclear macrophages can settle in different tissues, such as the liver, lung, brain, lymph nodes and other organs and tissues, at which time they will become macrophages. Macrophages are involved in phagocytosis and clearance of pathogenic microorganisms, necrotic tissues, and secretion of a variety of inflammatory mediators involved in immune regulation and tissue repair (113–115). Microglia are induced by the colony-stimulating factor 1 receptor (CSF1R) and are generated from red myeloid progenitors of the yolk sac. They are self-renewing and reside in the CNS for a long time (116). Microglia play an important role in maintaining the homeostasis of the nervous system, including phagocytosis (117), promoting synapse formation (118), and supplying nutrients (119).
In the TME, macrophages can manifest as the M1 type (characterized by inflammatory and antitumour responses) or M2 type (involved in the repair of damaged tissues and anti-inflammation), but the TME tends to induce the differentiation of macrophages towards the M2 type (120–122). Anti-inflammatory factors released by tumours, such as interleukin (IL)-4, IL-10, and transforming growth factor-β (TGF-β), can promote the transformation of macrophages into the M2 type (123). M2 macrophages similarly release growth factors, such as vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), and fibroblast growth factor (FGF), which promote tumour cell proliferation, invasion, and metastasis (124).
Glioma-infiltrated macrophages and microglia are collectively referred to as GAMs, which represent the largest population of cells infiltrating tumours, accounting for more than 1/3 of the total tumour mass (125, 126). GAMs play an important role in the glioma TME and promote tumour progression. First, anti-inflammatory factors such as IL-10 and TGF-β produced by GAMs inhibit the function of other immune cells in the TME and weaken the antitumour immune response (127, 128). Second, GAMs also secrete matrix metallopeptidase 2 (MMP2) and MMP9, which are able to breakdown matrix proteins, such as collagen and fibronectin, thereby enabling glioma cells to penetrate and invade the surrounding stromal tissues (129). Finally, GAMs also secrete proangiogenic molecules, such as VEGF and CXC motif chemokine ligand 2 (CXCL2), which have been shown to promote glioma growth and metastasis (129, 130).
In the glioma TME, ROS generally induce the generation of M2 GAMs (96, 131). ROS modulator 1 (Romo1), a membrane protein located on mitochondria, was found to regulate mitochondrial ROS (mtROS) production in GBMs (132). In GBM mouse models, overexpression of Romo1 induces ROS generation via mTORC1 signalling, which in turn promotes the polarization of bone marrow-derived macrophages (BMDMs) to the M2 type, resulting in a significant suppressive TME (133). In addition, a prognostic model of human GBMs and ROS showed that high expression of ROS-related genes such as HSPB1, LSP1 and PTX3 was closely associated with M2 macrophages and correlated with shorter survival of GBM patients. This suggests that ROS-related genes may be potential targets for GBM treatment. Therefore, inhibiting the polarization of macrophages towards M2 type and promoting the polarization towards M1 type may be beneficial for the treatment of GBMs (134). Besides, GAMs could survive in a high ROS environment mainly due to the action of antioxidant enzymes. A study of GBM tissues in humans and mice showed that the active antioxidant enzyme GPX1 was expressed at higher levels in GAMs than in GBM cells, resulting in GAMs being able to survive in a high ROS environment (135). It is known that GPX1 plays an important role in H2O2 detoxification (136). In summary, the antioxidant enzymes in GAMs protect them from ROS damage, which is necessary for the formation of M2 GAMs.
3.2. MDSCs
MDSCs, which are mainly differentiated from haematopoietic stem cells in the bone marrow, are a group of myeloid cells with heterogeneous and immature characteristics (137). In normal organisms, the levels of MDSCs in the peripheral blood tend to be very low (138). MDSCs have certain immunomodulatory effects, which can regulate the inflammatory response, inhibit overactivated immune cells, prevent excessive immune responses, and reduce tissue damage (105, 139).
Upon tumour stimulation, MDSCs are activated and released into peripheral blood and tissues. However, MDSCs often suppress the immune response and cause tumour escape (140, 141). The suppressive effect of MDSCs is mainly manifested by inhibiting the activity of other immune cells, including macrophages (142), CD4+ T cells (106), CD8+ T cells (143), NK cells (144), and DCs (145). First, MDSCs can highly express arginase-1 (ARG-1), which can convert arginine to uric acid and ornithine, thereby reducing the concentration of arginine in the internal environment (105). Arginine deficiency leads to limited activation of immune cells such as T cells (146) and NK cells (147), thereby impairing the immune response and promoting tumour development and metastasis. Second, MDSCs can secrete immunosuppressive cytokines, such as TGF-β and IL-10, which can inhibit the secretion of IL-12 by macrophages, thereby blocking the activity of cytotoxic T lymphocytes (CTLs) (148, 149). TGFβ-1 secreted by MDSCs also promotes the transformation of CD4+ T cells into immunosuppressive Tregs (150). Finally, MDSCs can also express immunosuppressive ligands, such as programmed death ligand-1 (PD-L1), which in turn suppresses T-cell priming and activation (151).
In gliomas, MDSCs comprise approximately 30% to 50% of the tumour entity (152). The increase in MDSCs is thought to be associated with glioma progression and immune escape (153). Generally, MDSCs can be divided into two main subsets based on their phenotype and function: monocytic (mMDSCs) and granulocyte/polymorphonuclear (gMDSCs) (154). Specifically, mMDSCs represent the major subset in the GBM TME. mMDSCs in the GBM TME of humans and mice expressed higher levels of adhesion molecules, such as integrin β1 and dipeptidyl peptidase 4 (DPP4), leading to enhanced cell adhesion and further promoting tumour migration and invasion (155). In addition, MDSCs can promote angiogenesis through the release of VEGF (156), as well as the release of cytokines such as IL-10, IL-6, and TGF-β under hypoxic conditions (157), thereby promoting glioma growth and invasion.
In the TME, MDSCs can survive in a high ROS environment because of their high expression of NRF2. On the one hand, NRF2 upregulated anti-OS genes in MDSCs and protected MDSCs from OS damage. On the other hand, NRF2 enhances the immunosuppressive activity of MDSCs by increasing their ability to produce ROS (158). In gliomas, ROS in MDSCs play an important role in maintaining the function of MDSCs (159). ROS can prevent the differentiation of MDSCs and promote the formation of an immunosuppressive TME (160). Specifically, ROS maintain the undifferentiated state of MDSCs by inhibiting the differentiation of MDSCs into mature immune cells such as macrophages and DCs (145, 161, 162). This undifferentiated state allows MDSCs to continue expressing immunosuppressive molecules such as TGF-β, IL-10 and PD-L1 (163). In addition to being able to impair the antigen presentation capacity of DCs (164–166), these immunosuppressive molecules can also inhibit the activity of T cells and induce the differentiation of T cells into Tregs (141, 167). Collectively, high levels of ROS play an important role in maintaining the undifferentiated state of MDSCs, which in turn mediates the immunosuppressive TME. Therefore, targeting MDSCs may become a promising therapeutic strategy.
3.3. T cells
T cells are members of the adaptive immune system that respond to antigens presented by antigen-presenting cells such as DCs and macrophages (168). T cells can be divided into CD4+ T cells and CD8+ T cells based on surface markers and function (169). CD4+ T cells have antigen receptors on their surface, which can recognize antigen fragments presented by MHC class II molecules on the surface of antigen-presenting cells and exert immune functions by activating other types of immune cells. CD8+ T cells generally refer to CTLs that can directly kill infected cells by MHC class I molecules (170). Regulatory T cells (Tregs) are a subset of CD4+ T cells that express the transcription factor forkhead box protein 3 (FOXP3) and play a role in inhibiting pathological immune responses and maintaining homeostasis in the body (171).
In tumours, CD4+ T cells mainly activate other immune cells, such as CD8+ T cells and NK cells, to enhance the immune response (172). CD4+ T cells can secrete cytokines, such as interferon-gamma (IFN-γ) and tumour necrosis factor-alpha (TNF-α), which directly kills tumour cells (173). CD8+ T cells carry specific T-cell antigen receptors (TCRs) that recognize and bind to tumour cells expressing specific antigens, thereby releasing cytotoxins, such as perforin and granzyme, to directly kill tumour cells (174). In addition, CD8+ T cells can also secrete cytokines, such as IFN-γ and TNF-α, which directly inhibit tumour cell growth and proliferation (175). Tregs play an indispensable role in maintaining the homeostasis of the immune system. Tregs suppress other immune cells and prevent excessive immune responses by producing inhibitory cytokines such as IL-10, IL-35, and TGF-β. However, overactive Tregs in turn limit the antitumour ability of immune cells (176).
In gliomas, T-cell dysfunction is often caused by the strong immune escape ability of glioma cells. Some studies have shown that human GBM cells are capable of producing the immunosuppressive factor TGF-β (177), which inhibits T-cell activation, thereby weakening the immune response (178). In addition, the human glioma TME has many immunosuppressive cells, such as M2 macrophages and Tregs, whose presence usually inhibits the activity and function of T cells and is associated with reduced overall survival of patients (179–181). Moreover, human glioma cells often express immune escape sites on the surface, such as PD-L1 and B7 homologue 3 (B7-H3), which can bind to immune checkpoint receptors, thereby inhibiting the activity and function of T cells (182).
ROS play an important role in regulating T-cell function and activity. Low levels of ROS can promote the activation and proliferation of T cells to enhance immune responses (183). However, higher levels of ROS can inhibit the secretion of cytokines by T cells and induce apoptosis (184). In the TME, excessive ROS may induce apoptosis of T cells, leading to decreased antitumour ability. For example, ROS produced by neutrophils or tumour cells can be transferred to T cells and cause OS, thereby causing hyporeactivity of T cells in cancer patients (185). In mouse glioma models, the administration of hyperbaric oxygen (HBO) can induce the generation of ROS in the thymus, which subsequently inhibits the generation of CD3+ T cells and promotes glioma growth in vivo (186). Therefore, high levels of ROS in the TME may lead to impaired T-cell function, which in turn enhances tumour escape. Targeting ROS in the TME to enhance the killing ability of T cells may be a potential therapeutic option.
3.4. Neutrophils
Neutrophils are derived from haematopoietic stem cells in the bone marrow through differentiation and maturation. When neutrophils mature, they enter the circulation and are distributed throughout the body through the blood (187, 188). Neutrophils are important immune cells of the body that are capable of engulfing and eliminating pathogens, such as bacteria and viruses (189, 190). In addition, when tissues are injured or infected, neutrophils rapidly migrate to the damaged site and release cytokines and chemokines to trigger local inflammation (191).
The role of neutrophils in tumours is complex. On the one hand, neutrophils are capable of killing tumour cells by releasing cytotoxic ROS (192) and by direct cell contact (193). On the other hand, neutrophils also promote tumour growth and metastasis by secreting immunosuppressive factors such as TGF-β, IL-6 and IL-8 (194) and interacting with circulating tumour cells (195). Furthermore, neutrophil extracellular traps play an important role in tumour progression. In the early stages of tumour invasion and metastasis, neutrophils can release neutrophil extracellular traps (NETs), which include DNA, tissue proteins and other substances. NETs can form channels suitable for tumour cell migration and protect tumour cells from immune system attack (196, 197).
Neutrophils, as mediators of inflammation, are early markers of GBM progression (198). Overall, neutrophils promote tumour growth, invasion, and angiogenesis. Neutrophils contribute to glioma infiltration by secreting elastase (199). Furthermore, neutrophils may also become resistant to antineoplastic therapy. In patients receiving anti-VEGF therapy, neutrophils contribute to glioma resistance to anti-VEGF therapy by increasing S100A4 expression and angiogenesis in glioma tissues (200). S100A4 is known to be a biomarker expressed in glioma stem-like cells (GSCs) that induces the tumorigenic activity of neutrophils (201). In addition, some studies have shown that the expression of MDSCs is increased in the peripheral blood of GBM patients, of which the neutrophilic MDSC subset accounts for the largest proportion, accounting for approximately 60% (102). Neutrophilic MDSCs derived from the peripheral blood of GBM patients can inhibit T-cell proliferation in vitro, which is related to the high expression of PD-L1 on effector memory CD4+ T cells (106).
Several studies have shown that ROS are important factors in promoting the formation of NETs (202–204). In chronic granulomas, NOXs are activated by protein kinase C (PKC) and produces ROS. These ROS can act as signalling molecules, causing neutrophils to release DNA and form a mesh-like structure, which then combines with the adhered granule proteins to form NETs (202). Furthermore, in primary mouse and human neutrophils, members of the MAPK family, such as c-Jun N-terminal kinases (JNKs) (203), extracellular signal-regulated kinases (ERKs) and p38 (204), can activate NOXs to generate ROS, which in turn induces the production of NETs. Similarly, ROS are similarly closely related to NETs in GBM TME. A study in human GBMs showed that NETs promote IL-8 secretion in GBMs by stimulating the NF-κB signalling pathway, which in turn stimulates endothelial cells to generate blood vessels to deliver essential nutrients and oxygen to the tumour site (101). When IL-8 binds to C-X-C motif receptor 2 (CXCR2) on neutrophils, it mediates the formation of NETs through the CXCR2/PI3K/AKT/ROS axis. This positive feedback loop stimulates the interaction between NETs and GBM cells and leads to profound changes in the TME (101). Recent studies in murine models of GBMs have additionally demonstrated that neutrophils promote the necrosis of GBM cells by transferring particles containing myeloperoxidase into these cells. This phenomenon induces OS, which is a result of the iron-dependent accumulation of lipid peroxides in GBM cells (205).
3.5. DCs
DCs, which differentiate from bone marrow haematopoietic stem cells through common DC progenitors (CDPs), play an important immunomodulatory role by presenting antigens (206). In tissues, DCs are usually naturally present and are considered to serve as a bridge connecting innate and adaptive immunity and are able to promote the transformation of innate to adaptive immune responses (207). Innate immunity refers to the immunity possessed by individuals at birth, which has a wide range of effects and is not triggered by specific antigens (208). Adaptive immunity is mainly the ability to respond to and adapt to a specific antigen or pathogen, which is achieved through T-cell-mediated cellular immunity and antibody-mediated humoral immunity (209).
Tumour formation is often accompanied by the expression of tumour antigens. Tumour antigens can be captured and processed by DCs and subsequently presented to naive T cells to induce their proliferation and differentiation into effector cells, such as CD8+ T cells, which subsequently kill the tumours (210). Furthermore, DCs can produce a variety of immune stimulating factors, such as cytokines and chemokines, which induce DCs and NK cells to reach inflammatory sites (211), as well as induce the activation of tumour-specific T cells (212).
Antigens released by glioma cells can be captured and processed by DCs, presented to T cells, and activate effector T-cell function (213). However, glioma cells can often evade immune surveillance by inhibiting the maturation of DCs. Studies have shown that tumour-conditioned medium (TCM) collected from the supernatant of human primary glioma cells can upregulate the expression of suppressor of cytokine signalling 1 (SOCS1) in DCs and then inhibit the NF-κB signalling pathway, thereby limiting the maturation of DCs. The subsequent suppression of T-cell activity, as well as IFN-γ secretion, results in immune escape of glioma cells (214). A previous study revealed that mouse gliomas have the ability to secrete cell factors including TGF-β and IL-10 (215). These factors are known to impede the maturation and functionality of DCs within the TME (216).
In addition, recent studies on the role of DCs in the progression of human GBMs have focused on the maintenance of DC homeostasis. Overexpression of NRF2 in DCs leads to the inhibition of DC maturation and subsequently reduces effector T-cell activation, which may be related to the decrease in ROS levels mediated by NRF2. In contrast, inhibition of NRF2 promotes the maturation of CD80+ and CD86+ DCs (217).
3.6. NK cells
NK cells belong to a type of lymphocyte that can eliminate tumour cells without specific antigens and are an important part of innate immunity (218). NK cells are derived from bone marrow haematopoietic stem cells and enter the circulation after maturation (219). Approximately 5-15% of lymphocytes in normal blood are NK cells (220).
NK cells have the ability to kill tumour cells. First, NK cells kill tumour cells by making direct contact with tumour cells that express specific ligands. There are a variety of activated receptors on the surface of NK cells, such as natural killer group 2 member D (NKG2D) and natural cytotoxicity receptors (NCRs; NKp46, NKp44 and NKp30) (221), etc. Among them, NKG2D is one of the most studied receptors and is able to recognize ligands on the surface of tumour cells, such as major histocompatibility complex class I polypeptide-related sequence A and B (MICA/B) and UL16-binding protein (ULBP). This recognition activates NK cells and prompts them to kill tumour cells (222). Second, NK cells can kill tumour cells through the antibody-dependent cellular cytotoxicity (ADCC) mechanism. When the antigens on the surface of tumour cells are labelled with specific antibodies, NK cells can bind to the specific antibodies through the CD16 (FcγRIIIa) receptor on their surface. Activated NK cells then release particles containing perforin and granzyme, which trigger apoptosis of antibody-labelled tumour cells (223, 224). Furthermore, NK cells can produce cytokines, such as IFN-γ and TNF-α, which can enter tumour cells and thus kill them (225). Moreover, IFN-γ released by NK cells can also inhibit tumour angiogenesis, thereby impeding tumour nutrient supply (226).
NK cells also have a killing effect on gliomas. First, NK cells can kill glioma cells by secreting perforin and granzyme B upon induction by IFN-β (227). Second, NK cells kill gliomas by specific activating receptors on their surface. When NKG2D and DNAX accessory molecule-1 (DNAM-1) on the surface of human NK cells bind to their ligands on the surface of GBM cells, they can trigger NK cell cytotoxicity and cause GBM cell death (228, 229). However, human GBM-derived TGF-β may lead to downregulation of NKG2D receptors on the surface of NK cells and contribute to GBM cell survival, suggesting that blocking TGF-β may be beneficial in the treatment of GBMs (230). Similarly, NK cells can also kill GBM cells through ADCC. Cetuximab is a monoclonal antibody that binds epidermal growth factor receptor (EGFR) on tumour cells (231). When administered, cetuximab binds to a human GBM surface antigen (EGFRvIII) and activates fragment crystallizable (Fc) receptors on NK cells, leading to NK cell-mediated cytotoxicity against GBM cells (232).
NK cells are often particularly sensitive to the cytotoxic effects of ROS, and their antitumour activity is often inhibited by ROS in the solid tumour TME, whereas antioxidant therapy may partially restore NK cell function (110, 233). Previous studies have shown that high levels of ROS in rats with fibrosarcoma can limit the adhesion of NK cells to similarly charged tumour cells by promoting the accumulation of anionic charges on their surface. This disadvantage can be prevented by antioxidant molecules such as CAT and SOD (234). Similarly, in vitro, the CD20 antibody rituximab triggered monocyte ROS production, which in turn inhibited the ADCC effect of NK cells on human primary leukaemia cells. However, antioxidant treatment (histamine dihydrochloride and diphenylene iodonium chloride) partially restored the ADCC effect of NK cells (235). At present, although some studies have suggested the inhibitory effect of ROS on NK cell activity in the TME, the study of ROS in NK cells in the glioma TME is still limited. Further studies will help to understand the effect of ROS on NK cell function in the glioma TME.
3.7. Glioma cells
The threshold of ROS is very important in cancer therapy. When ROS produced by tumour cells exceed a certain threshold and cannot be detoxified by antioxidants, it results in high levels of OS, which drives cancer cell death or cause them to become more sensitive to treatment. However, a low level of ROS in tumour cells contributes to their growth, proliferation, invasion and metastasis (236). Therefore, tumour cells need to maintain their ROS levels to maintain their survival and invasive abilities (237).
A study of tumour tissues and blood samples from glioma patients found that abnormal increases in ROS caused DNA damage in glioma cells, resulting in high expression of the DNA damage marker 8-oxo-deoxyguanosine (8-oxo-dG) and low expression of the epigenetic marker 5-methylcytosine (m5C). This is associated with increased malignancy of gliomas (22). In mouse models, glioma cells can overexpress aquaporin 8 (AQP8), which increases ROS levels, resulting in decreased expression of phosphatase and tensin homolog (PTEN) and increased expression of phosphorylated (p)-AKT, thereby promoting the growth and proliferation of gliomas (23). Moreover, the production of a significant amount of ROS induced by 12-O-tetradecanoylphorbol-13-acetate (TPA) can activate the MAPK pathway and cyclooxygenase-2 (COX-2)/prostaglandin E2 (PGE2) pathways, subsequently enhancing the in vitro migration and invasion capability of glioma cells (24). In contrast, high levels of ROS activate regulated glioma cell death programs, including apoptosis, necrosis, autophagy, ferroptosis, etc. For example, in vitro, salinomycin can activate p53, trigger the opening of mitochondrial permeability transition pore (mPTP), and induce the production and accumulation of mtROS, leading to the necrosis of glioma cells (25). The activation of transient receptor potential mucolipin 1 (TRPML1) inhibits autophagy in glioma cells in vitro, leading to ROS production and subsequent induction of apoptosis (238). Similarly, the increase in ROS induced by isoaaptamine also leads to apoptosis and autophagy in GBM cells in vitro (26). Furthermore, the heat shock protein 90 (HSP90) and dynamin-related protein 1 (DRP1) increase ROS production by regulating the expression of acyl-coenzyme A synthetase long-chain family member 4 (ACSL4) and mitochondrial morphology, leading to ferroptosis of gliomas in mice in vitro and in vivo (239).
Glioma stem-like cells (GSCs) are a subpopulation of GBM cells with stem cell characteristics. They have self-renewal, tumourigenicity and multidirectional differentiation potential and are closely related to the occurrence, development, treatment resistance and recurrence of GBMs (240). Many studies have confirmed that ROS are involved in the proliferation, self-renewal and differentiation of GSCs (241, 242). In a study conducted on human-derived GSCs, it was found that TGF-β upregulated the expression of the NOX4 gene, leading to the generation of ROS. Consequently, this ROS generation promoted GSC proliferation and maintained their stem cell state (241). Other studies have shown that serum stimulation in an in vitro environment is able to cause an increase in mitochondrial ROS within GSCs and modulate differentiation signalling pathways in GSCs. Interestingly, in the in vivo environment, increased ROS could greatly enhance glioma formation, which may be related to the activation of the NF-κB pathway by ROS (243). Compared with other tumour cells, GSCs have stronger antioxidant capacity (47). In vitro, the highly expressed antioxidant protein PRDX4 was able to mitigate OS in GSCs by reducing ROS generated by the protein folding process (47, 244). Furthermore, GSCs also inhibit mitochondrial respiration by increasing the expression of mitochondrial uncoupling protein 2 (UCP2), thereby alleviating OS caused by high levels of intracellular ROS and ensuring their own survival (245).
However, the understanding of the ROS threshold in cancer cells is still unclear. Measurement of the ROS threshold requires the consideration of multiple factors, including the concentration and type of ROS, the activity of intracellular antioxidant enzymes, and the type and physiological state of tumour cells (246–249). Therefore, more studies are needed to fully assess ROS thresholds and determine their impact on tumour cells. Overall, both ROS and thresholds play a crucial role in glioma cells. This provides a new research direction for ROS-based glioma therapy.
4. ROS-based glioma therapy
High levels of ROS are usually present in the glioma TME. On the one hand, these ROS are involved in the formation of a suppressive TME. On the other hand, they are involved in the process of glioma proliferation, invasion and migration. However, there is also a threshold for the levels of ROS in glioma cells. The induction of ROS production above the threshold can lead to an excessive OS response, causing DNA and protein damage and leading to glioma cell death (250). Conversely, depletion of ROS may also lead to the blocking of important signalling pathways involved in ROS, thereby promoting glioma death (27, 28, 32). Based on these findings, it is suggested that both methods of inducing ROS production and ROS scavenging have potential in the glioma treatment. These two therapeutic strategies may help to suppress glioma growth, enhance the immune response and improve the efficacy of other antitumour therapies.
4.1. Treatment to increase ROS levels
Excessive ROS can induce tumour death, so amplifying the effect of ROS may be a good way to kill tumours. For example, the use of PDT (251), SDT (252), CDT (253), can be beneficial therapies for GBMs. This part mainly summarizes the research progress of PDT, SDT and CDT in the treatment of gliomas, and discusses the application of nanodrug delivery platforms in them.
4.1.1. PDT
PDT is a technique that relies on ROS production to treat nononcological diseases as well as tumours. Its main components are excitation light, photosensitizers (PSs) and ROS (254). PSs are important components in determining the efficacy of PDT (255). Photoactivated PSs can produce cytotoxic ROS in the presence of oxygen, resulting in the killing of target cells (256, 257). To date, numerous PSs have been applied in the studies of gliomas, such as 5-aminolevulinic acid (5-ALA) (258), boronated porphyrin (BOPP) (259), talaporfin (260), and temoporfin (261). The wavelength of the light is also important. The optimal PDT wavelength is between 650 and 850 nm and should be consistent with the longest wavelength absorption band of the PSs, that is, the wavelength range corresponding to sufficient energy for maximum tissue penetration to result in sufficient ROS production (262). Notably, ROS produced by PSs, such as 1O2, O2˙‾ , OH, OOH·and H2O2, are essential for killing tumours. The formation of O2˙‾ and free radicals is called a type I reaction, and the formation of 1O2 is called a type II reaction (263, 264).
PDT has been approved by the United States Food and Drug Administration (FDA) for the treatment of a variety of cancers, including skin cancer, oesophageal cancer, and lung cancer (265–267). PDT has been studied since the 1980s (268, 269), and has shown promising efficacy in many glioma preclinical studies (270–272). A bibliometric analysis of literature in the field of cancer PDT (CPDT) reveals that research on CPDT is showing a rapid growth trend over the past 20 years. Among them, nanotechnology-based PDT and enhanced PDT are the current research hotspots (273). However, PDT has still not been widely adopted due to its potential toxicity to healthy brain tissues, limited light penetration, and poor targeting (251, 274, 275).
In the past 10 years, three promising phase I/II clinical trials of PDT for glioma treatment have been conducted in adults and one has been conducted in minors. A total of four clinical trials were conducted for three drugs (photofrin, ALA, photobac®) ( Table 2 ). Among them, NCT01682746 included 5 adolescent patients with brain tumours. The incidence of serious adverse events within 1 month of PDT treatment, the progression-free survival and the overall survival within 3 years were recorded, but no results of this clinical trial were reported. NCT03048240 included 10 adult patients with newly diagnosed GBM who were treated with 5-ALA fluorescence-guided surgery followed by intraoperative PDT (based on clinicaltrials.gov). At the interim analysis, the median progression-free survival (mPFS) was 17.1 months, and the median overall survival (mOS) was 23.1 months (276). This clinical trial result indicates that intraoperative PDT is a good option for treating recurrent gliomas.
Table 2.
Summary of completed/ongoing phase I/II clinical trials of ROS-generated PDT/SDT for glioma treatment by July 2023 (based on clinicaltrials.gov).
| NCT Number | Phases | Conditions | Interventions | Age | Enrolment | Primary endpoint and duration | Status | Related publications | |
|---|---|---|---|---|---|---|---|---|---|
| PDT | NCT01682746 | Phase 1 | Brain Tumour | Photofrin photodynamic therapy | 6 months to 18 years |
5 | More than 33% of subjects experienced neurotoxicity, photosensitivity, ocular sensitivity, or other toxicities greater than or equal to CTCAE grade 4 (4 weeks). | Completed in 2018 | _____ |
| NCT03048240 | Not Applicable |
GBM | 5-ALA photodynamic therapy | ≥18 years | 10 | At least 6/10 patients benefited without unacceptable and unexpected toxicities (4 weeks). | Completed in 2021 | (276) | |
| NCT04391062 | Phase 2 | GBM | 5-ALA photodynamic therapy | ≥18 years | 21 | Dose level above which dose-limiting toxicities is observed in more than 33%of subjects in an arm (4 weeks). | Enrolment ongoing | _____ | |
| NCT05363826 | Phase 1 | GBM or Gliosarcoma |
Photobac® photodynamic therapy | ≥18 years | 30 | Toxicity (24 hours); MTD (1 week); Photobac® concentration in tumour tissues (1 hour); Photobac® concentration in blood (12 weeks); PFS (18 months); OS (18 months) |
Enrolment ongoing | _____ | |
| NCT04469699 | Phase 2 | GBM Multiforme |
Drug: Stereotactic biopsy followed by stereotactical photodynamic therapy with 5-aminolevulinic acid | 18 years to 75 years |
106 | PFS (at least 1.5 years and a maximum of 5 years) or until progression or death | Enrolment ongoing | _____ | |
| NCT03897491 | Phase 2 | GBM | 5-aminolevulinic acid powder for oral solution | 18 years to 70 years | 20 | To determine the incidence of treatment-emergent Adverse Events (2 weeks) | Enrolment ongoing | _____ | |
| SDT | NCT04559685 | Early phase 1 | High Grade Glioma | Sonodynamic therapy with MRg-FUS combined with ALA | ≥18 years | 30 | Biological changes; Imaging changes before and after surgery (14 days) | Enrolment ongoing | _____ |
| NCT05362409 | Phase 1 | High Grade Glioma | Sonodynamic therapy with 5-ALA combined with CV01-delivered ultrasound | ≥18 years | 48 | Incidence of adverse events; To determine the MTDu (12 months) | Enrolment ongoing | _____ | |
| NCT05123534 | Phase1/Phase2 | Glioma | Sonodynamic therapy with MRg-FUS combined with ALA | ≥5 years | 27 | Safety and Tolerability of SDT (12 months); MTD (3 weeks); Recommended Phase 2 Dose (3 weeks) | Enrolment ongoing | _____ |
CTCAE, Common Terminology Criteria for Adverse Events; MTD, Maximum tolerated dose; MRg-FUS, MR-Guided Focused Ultrasound device; MTDu, Maximum Tolerable Duration.
The tumour killing mechanisms of PDT are various, including inducing immunogenic cell death (ICD), destroying tumour blood vessels and inducing the release of inflammatory mediators in addition to the direct killing caused by high ROS. The combination of PDT and subsequent immune response induced by PDT is referred to as photodynamic immunotherapy (PDIT) (262, 277, 278). ICD refers to the death of tumour cells after PDT, which stimulates the immune system to produce a strong immune response by releasing damage-associated molecular patterns (DAMPs), cytokines, tumour-associated antigens (TAA) and other signalling molecules (279). These DAMPs can be recognized by the immune system and activate antitumour immune responses. DAMPs mainly include calreticulin (CALR), heat shock proteins 70/90 (HSP70/90), ATP, high-mobility group box-1 (HMGB1) nuclear protein, type I interferons (IFNs) and members of the IL-1 cytokine family, etc. In addition, ROS produced by PDT can destroy tumour blood vessels, limit tumour nutrient supply, and stimulate antitumour immune responses (262). Cytokines are able to trigger an inflammatory response that further enhances immune cell infiltration and activation (280, 281). The mechanism of PDIT in gliomas is illustrated in Figure 2 .
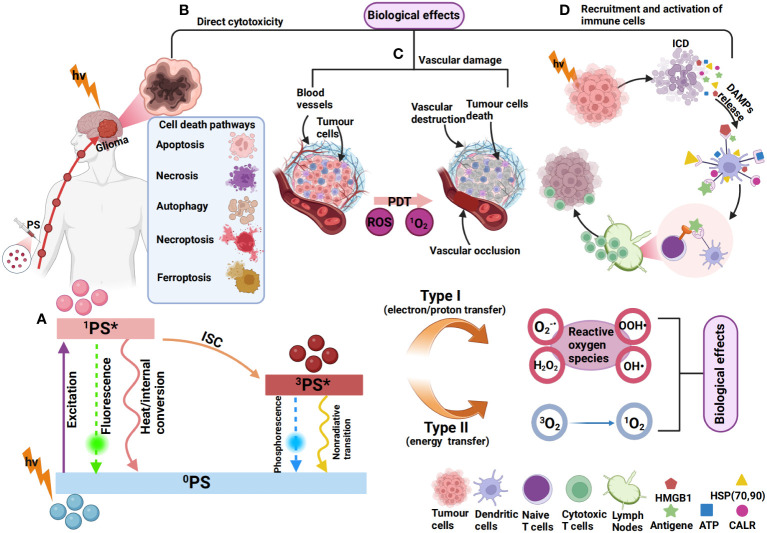
Figure 2.
Mechanism of photodynamic immunotherapy for gliomas. (A) 0PS is activated to a singlet state (1PS*) after absorbing photons (hv). 1PS* can lose energy through internal conversion to heat and fluorescence. 1PS* can form a triplet state (3PS*) through the intersystem crossing process (ISC). 3PS* can be restored to 0PS by emitting phosphorescence and can also react with neighbouring molecules in two types of reactions (type I and type II). In type I reactions, 3PS* transfers an electron or a proton to form organic free radicals (O2-, OOH·, H2O2, OH·, etc.) that interact with cellular oxygen to produce cytotoxic ROS. In a type II reaction, the energy of 3PS* can be directly transferred to molecular oxygen (3O2) to form singlet oxygen (1O2). This results in various biological effects (264, 282, 283). (B) The most common types of cell death induced by PDT include apoptosis (284), autophagy (285), necrosis (286), necroptosis (287), and ferroptosis (270). (C) ROS produced by PDT can also cause vascular occlusion, leading to vascular damage, thereby affecting the blood supply of tumour cells (288). (D) PSs can induce immunogenic cell death (ICD), resulting in the exposure and release of DAMPs, such as ATP, HMGB1, CALR, HSP70/90, etc (262). The released DAMPs promote DC recruitment and maturation and present tumour antigens to T cells, leading to the activation of CD8+ T cells, which subsequently migrate in vivo to kill tumour cells (264).
4.1.2. SDT
Ultrasound (US) is a kind of mechanical vibration wave with strong tissue penetration ability that has been widely used in ultrasound imaging and ultrasound therapy. Among the US-derived techniques, SDT based on ROS production is a good strategy. Research on SDT began in the 1990s (289, 290). Based on the bibliometric analysis of SDT, studies have shown that since 2000, SDT has experienced rapid growth and has mainly focused on the fields of nanomaterials and cancer treatment, achieving significant results (291). The mechanism of SDT is to use low-frequency ultrasound to trigger sonosensitizers that accumulate at the tumour site, producing ROS and cavitation bubbles to kill the tumours. These ROS produce significant toxic effects on tumour cells in the 1 μm range (292, 293). The advantage of SDT is mainly that ultrasound can penetrate to a depth of 10 cm, which can kill tumours in deeper locations (294, 295). At present, most of the sonosensitizers used in reported SDT are photosensitizers or are derived from photosensitizers (296). However, SDT also has difficulty achieving the ideal tumour killing effect due to the presence of the BBB and the poor targeting effect of sonosensitizers such as porphyrins (297). Notably, TMZ can not only penetrate the BBB but also act as a sonosensitizer to induce necroptosis in GBMs. This provides new potential options for treating GBMs with SDT (293).
According to the literature, although SDT has been studied in gliomas for less than 20 years, it has shown promising efficacy in preclinical studies (30, 298, 299). However, due to the maturity of the technology and the factors of ultrasound equipment and other objective reasons, the research results of SDT are less than those of PDT, and clinical research is also in its infancy. At present, there are three clinical trials of SDT in gliomas under recruitment (based on clinicaltrials.gov), as shown in Table 2 . More clinical trials are needed to verify the efficacy of SDT in the glioma treatment.
4.1.3. CDT
The concept of CDT was first proposed in 2016 by Bu, Shi et al. (300). CDT is dependent on transition metal ions in the TME to produce high levels of OH· through Fenton/Fenton-like reactions, resulting in tumour killing (301). The Fenton reaction refers to the complex chemical reaction of ferrous ions with H2O2, which eventually generates highly toxic OH· (302). Catalysts for Fenton-like reactions are usually other transition metals, such as copper (Cu) and manganese (Mn) (303, 304). Compared with PDT, the advantage of CDT is that it does not require laser irradiation, so it can avoid the limitations caused by light penetrating the tissues. Alternatively, the TME is characterized by acidity and H2O2 overexpression, which favours Fenton/Fenton-like reactions. However, when the pH at the tumour site is too high or H2O2 production within the tumour is insufficient, the Fenton/Fenton-like reaction will be insensitive, and CDT efficiency will be reduced (305). In general, CDT has the advantages of strong targeting, low adverse reactions, regulation of TME hypoxia, and low treatment cost, so it has great potential to be used in tumour therapy (301). In the glioma treatment, CDT is still in the preclinical stage, and no clinical trials have been carried out. However, it has been shown that CDT has good therapeutic efficacy and can exert more anti-glioma effects in combination with PDT (306) and photothermal therapy (PTT) (307).
4.1.4. Breaking through the BBB to enhance PDT/SDT/CDT
The BBB is a physical, chemical and biological barrier structure formed by capillary endothelial cells in the brain, surrounding astrocytes and muscle rings. The main function of the BBB is to maintain the stability of the brain environment, regulate the entry of nutrients, and prevent harmful substances from entering the brain through the blood (308, 309). Brain endothelial cells are composed of hydrophobic lipid bilayers with tight junctions. Therefore, drugs with large polarity and molecular weight often have difficulty passing the BBB (310). However, research has shown that human glioma cells can infiltrate through the perivascular space and extensively invade the brain away from the tumour mass. In this process, glioma cells displace the end feet of astrocytes, thereby disrupting the BBB, which may be beneficial for drug therapy (311, 312). However, effectively overcoming the limitations of the BBB remains a challenge. Currently, nanodrug delivery platforms (313), microbubble-enhanced focused ultrasound (MB-FUS) (314) and magnetic resonance-guided focused ultrasound (MRg-FUS) (315) are three promising approaches to break through the BBB.
Nanotechnology is the study and application of particles or structures between 1 and 100 nm, where it can maximize drug transport and targeted delivery (316–318). Nanodrug delivery platforms are the application of nanotechnology in medicine. In general, nanodrug delivery platforms are usually composed of nanocores, nanocarriers, targeting ligands, drugs and surface modifications or may not completely contain these parts. Among them, the nanocore is the main component of the platform, mainly serving to support and stabilize the nanodrug delivery platform. It can be composed of materials such as gold (319), silicon (320), magnetic materials (321), etc. Nanocarriers refer to carriers that carry drugs on nanocores. An ideal nanocarrier can stably encapsulate drugs inside and release them at the appropriate time (322). Types of nanocarriers include gold nanoparticles, magnetic nanoparticles, carbon nanotubes, polymer micelles, and liposomes (323), etc. Targeting ligands attached to the nanocore include antibodies (324) and targeting peptides (325), which can precisely target the target. Nanocarriers can carry drugs, which include PSs such as chlorin e6 (Ce6) (326), immune checkpoint inhibitors such as nivolumab (327), and chemotherapy drugs such as doxorubicin (DOX) (328). Surface modification refers to the modification of the surface of the nanoplatform, such as polyethylene glycol (PEG), to enhance the hydropathy, stability, and biocompatibility of the nanoplatform and improve the retention time in vivo (329).
In general, a well-functioning nanodrug delivery platform can typically enhance the therapeutic effects of PDT (330), SDT (331), and CDT (332) for the treatment of glioma. Moreover, optimizing key components of nanodrug delivery platforms can be an effective strategy to break through the BBB. First, the targeting of the nanoplatform should be enhanced. Transferrin (TF), for example, targets a transferrin receptor (TFR) that is overexpressed on the surface of brain capillary endothelial cells and malignant brain tumours. Related studies have shown that TF-bound nanoplatforms can effectively cross the BBB and target gliomas (333, 334). Second, the development of new nanocarriers, such as nanotubes, gold nanoparticles, and magnetic nanoparticles, makes it easier for drugs to reach the glioma site (335–337). Furthermore, polymers such as polyethylene glycol (PEG) and polylactic-co-glycolic acid (PLGA) can be used to encapsulate the drug to allow crossing of the BBB. The advantages of such polymers are good biocompatibility, easy surface modification, etc., and the ability to control the rate of drug release (329, 338). When a nanodrug delivery platform is combined with PDT, SDT, and CDT, it will greatly increase the targeting ability of the three therapeutic strategies and the level of ROS production, leading to a “1 + 1 > 2” therapeutic effect. The summary of glioma-related research on the nanodrug delivery platforms combined with PDT, SDT, and CDT is shown in Table 3 .
Table 3.
Summary of nanodrug delivery platforms used for glioma PDT/SDT/CDT.
| Categories | Nanocarriers | Drugs | Targeting ligands | Target receptors | Results | References |
|---|---|---|---|---|---|---|
| PDT | MRN | [Ru(bpy)2(tip)]2+ | TF, aptamer AS1411 | TFR, nucleolin | The glioma cells undergo apoptosis. | (334) |
| nanotube | IR780, DOX | ——— | ——— | The glioma cells undergo apoptosis. | (335) | |
| AuNs | ICG, DOX | TF | TFR | It effectively kills glioma cells. | (336) | |
| GuIX nanoparticle | porphyrin molecule | KDKPPR | NRP-1 | Glioma vessels are occluded, causing growth delay. | (337) | |
| polyethylene glycol | IR780, camptothecin | iRGD peptide | αvβ3/5, NRP-1 | The glioma cells undergo apoptosis. | (339) | |
| albumin | CAP | _____ | _____ | The glioma cells undergo apoptosis and necrosis. | (340) | |
| lipidosome | Ce6, LOMs | _____ | _____ | The generation of a large amount of O2 promotes the effect of PDT in the glioma treatment. | (341) | |
| BN | Ce6, DOX | platelet | tumour vascular endothelium | A large amount of ROS is generated, which subsequently leads to the death of glioma cells. | (342) | |
| FLs | ICG, DOX | G-Anti G | neuropilin-1 on glioma cells |
The production of ROS leads to the death of the majority of glioma cells. | (325) | |
| SDT | liposome | sinoporphyrin sodium | iRGD peptide | αvβ3/5, NRP-1 | SDT enhances its effect by increasing the production of a significant quantity of ROS, leading to the subsequent death of glioma cells. | (331) |
| liposome | Ce6, HCQ | ANG-2 | LRP1 | Nanosensitizers have a strong response to ultrasound, leading to the generation of a large amount of ROS and subsequently causing glioma cell apoptosis. |
(343) | |
| SiO2 nanoparticle | CAT, ICG | aptamer AS1411 | nucleolin | CAT catalyzes the generation of O2 from H2O2, alleviating tumour hypoxia and improving the efficiency of SDT. | (344) | |
| nanocrystal | ppIX, MnO2 | holo-TF | TFR | O2 is produced in large quantities and Mn2+
is released to achieve efficient SDT. |
(345) | |
| CDT | polymeric micelle | Mn2+, TMZ | iRGD | αvβ3 integrin, NRP-1 | TMZ、Mn2+and O2 release. Subsequently, glioma cells undergo death. |
(346) |
| Hb@GOx nanoparticle | Hb, GOx | _____ | _____ | The levels of H2O2 and OH· increase in glioma cells. Subsequently, glioma cells undergo death. |
(253) | |
| liposome | Ce6, SPIOCs | _____ | _____ | The levels of H2O2 and OH· increase in glioma cells. Glioma cells subsequently die. |
(347) |
MRN, mesoporous ruthenium nanoparticles; AuNs, gold nanoparticles; ICG, indocyanine green; DOX, doxorubicin; TF(R), transferrin (receptor); NRP-1, neuropilin-1; αvβ3/5, integrin alpha V beta 3/5; CAP , chloro-aluminiumphtalocyanine; LOMs, lipid-coated oxygen microbubbles; BN, boron nitride; FLs, fluorescent poly(levodopamine) nanoparticles; HCQ, hydroxychloroquine; ANG-2, angiopep-2; LRP1, low density lipoprotein receptor-related protein 1; ppIX, protoporphyrin; holo-TF, holo-transferrin; Hb, hemoglobin; Gox, glucose oxidase; SPIOCs, superparamagnetic iron oxide nanoclusters
In addition to nanodrug delivery platforms, the use of MB-FUS (348–350) and MRg-FUS (315) to open the BBB for drug delivery both has great potential. Microbubbles are essentially small bubbles of biocompatible gases, such as nitrogen or perfluorocarbon, encapsulated in a lipid, protein, or polymer membrane (351). As blood with microbubbles flows through the brain, ultrasound waves are emitted precisely to target areas. The ultrasound stimulates microbubbles to oscillate violently and burst, producing a temporary, local pressure change that can temporarily open the tight junctions of the BBB and increase its permeability. In this way, drugs or macromolecules that cannot penetrate the BBB can enter the brain tissues, thus allowing for the effective treatment of gliomas (343, 352, 353). In recent studies, MB-FUS achieved BBB opening and increased drug aggregation in GBM regions to enhance antitumour effects (354–357). Notably, the method of opening the BBB using ultrasound microbubbles is reversible, does not damage neurons, and the BBB heals a few hours after exposure (358). Thus, this method has great potential for application. This technique is still in its early stages, and promising results have been demonstrated in clinical trials in glioma patients (359). Furthermore, as another method to open the BBB, MRg-FUS can accurately focus ultrasonic waves on the GBM region and provide real-time monitoring and guidance during therapy provided through magnetic resonance imaging (MRI). Ultrasound energy can raise the temperature of the BBB region, thus enhancing permeability. Consequently, platinum nanoparticles can more effectively penetrate the GBM tissues, thereby inhibiting the growth of GBM cells (315).
4.2. Treatment to scavenge/reduce ROS levels
Antioxidants are a class of compounds that inhibit oxidation by scavenging ROS and reducing OS, and they can help reduce or block oxidative reactions in cells (360). When OS occurs, antioxidants interact with ROS to capture and neutralize ROS, thereby protecting cells from oxidative damage (361). Common antioxidants include vitamin C, vitamin E, α-carotene, selenium, etc., which can be obtained through food intake or supplements (362). Furthermore, the use of antioxidants can inhibit tumorigenesis by preventing OS caused by various causes, and the mechanism is to repair damaged DNA and inhibit cancer occurrence, including gene mutations, oxidative chromosomal damage, and lipid peroxidation of cell membranes (131, 363).
There is considerable evidence that intake of antioxidants may help reduce the risk of gliomas (364). For example, CoQ10 can act as a ROS scavenger to increase the sensitivity of gliomas to TMZ, thereby inhibiting the invasion of glioma cells in vitro and in vivo. Mechanistically, CoQ10 can integrate into the mitochondrial membrane and reduce ROS production. It also reduced the expression of MMP9 and epithelial-mesenchymal transition (EMT) markers (28, 365). Naringenin is an antioxidant. Naringenin supplementation for 1 month can reduce lipid peroxidation and decrease the expression of PKC, NF-κB, cyclin D1(CCND1) and cyclin-dependent kinase 4 (CDK4), thereby inhibiting the proliferation of glioma cells in mouse models (27). Astaxanthin is a natural carotenoid, and adonixanthin is a product of its formation (366). Studies have confirmed that both have strong antioxidant capacity, which can cross the BBB and protect brain tissues from ischaemia or hemorrhage (367, 368). In mouse glioma models, astaxanthin and adonixanthin intake increased p38 phosphorylation in glioma cells, leading to cell cycle arrest. Furthermore, adonixanthin was able to reduce the expression of MMP2 and fibronectin downstream of ERK1/2 and AKT signalling pathways and inhibit invasion and metastasis in both in vitro and in vivo GBM models (369). Chrysin is a kind of flavonoid with antioxidant properties. The p38-MAPK pathway is activated in rat glioma cells treated with chrysin, resulting in the accumulation of p21 (WAF1/CIP1) protein, decreased activities of CDK2 and CDK4, and cell cycle arrest in G1 phase (32). Similarly, hypoxia-inducible factor-1alpha (HIF-1α) expression was blocked when the antioxidant melatonin was used, resulting in a significant inhibition of MMP2 and VEGF expression, thereby inhibiting GBM cell migration and invasion in vitro (370). Moreover, antioxidants quercetin (QE), baicalein (BE) and myricetin (ME) effectively downregulated ROS and MMP9 and inhibited glioma cell invasion/migration events in vitro (24).
However, some studies have shown that intake of antioxidants, such as carotenoids (371), vitamin E (372), and coffee (373), is not associated with the risk of developing gliomas. This may be related to factors such as bioavailability, dose, BBB permeability, and tumour heterogeneity (364). Therefore, the role of ROS scavenging using antioxidants in glioma therapy still needs to be confirmed by more studies.
5. Conclusion
ROS are products of cellular redox and play important functions in cells. Excessively high or low ROS levels are detrimental to cell survival. That is, there is a threshold for intracellular ROS, and when a large accumulation of ROS exceeds the threshold and cannot be neutralized by the antioxidant defence system, it leads to OS and thus cell death. For gliomas, there is also a threshold for ROS. Appropriate ROS levels can aid survival, but high levels of ROS can also lead to their own death. Therefore, ROS-based therapies are particularly important.
Currently, there are two common therapeutic approaches involving ROS in the therapy of glioma, which are increasing ROS levels to induce cell death or using antioxidants to inhibit progression. In terms of increasing ROS, PDT/SDT/CDT is the representative approach. With the development of modern nanotechnology, the corresponding drugs can better pass through the BBB. Preclinical studies have shown that PDT/SDT/CDT combined with nanotechnology shows potent antiglioma effects and has good potential for clinical application. Conversely, ROS reduction using antioxidants has also been shown to inhibit glioma initiation and progression. Nonetheless, both strategies have limitations. In addition to the unclear clinical efficacy of antioxidants for cancer treatment reported in the literature, there are also issues such as the uncertain toxicity and biosafety of nanomaterials (374, 375), and the uncertain stability and retention time of nanodrug delivery platforms (376). Therefore, in the future development of nanodrug delivery platforms targeting gliomas, it is necessary to enhance the targeting and stability of nanoparticles and improve the ability to cross the BBB and biosafety to provide effective treatment while reducing adverse reactions. At present, although there are still many obstacles to ROS-based therapy, ROS still have the potential to be widely used as a therapeutic target for gliomas.
Author contributions
Y-CY: Writing – original draft. YZ: Writing – original draft. S-JS: Visualization, Writing – original draft. C-JZ: Writing – review & editing. YB: Writing – review & editing. JW: Writing – review & editing. L-TM: Supervision, Writing – original draft, Writing – review & editing.
Acknowledgments
We would like to express our heartfelt thanks to Dr. Jin Zheng, Director of TCM Department of Tangdu Hospital for her invaluable supportand guidance.
Funding Statement
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The preparation of this review was supported by the National Natural Science Foundation of China (No. 82101318 to YB), the Social Talent Fund Funding Program Project (2021SHRC044 to C-JZ), the Scientific Research Project Book of Traditional Chinese Medicine Administration of Shaanxi Province (SZY-KJCYC-2023-003 to C-JZ), and the Special Fund for the Cultivation and Enhancement of Military Traditional Chinese Medicine Service Capabilities (2021ZY021 to Jin Zheng).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1. Anjum K, Shagufta BI, Abbas SQ, Patel S, Khan I, Shah SAA, et al. Current status and future therapeutic perspectives of glioblastoma multiforme (Gbm) therapy: A review. Biomed Pharmacother = Biomed Pharmacotherapie (2017) 92:681–9. doi: 10.1016/j.biopha.2017.05.125 [DOI] [PubMed] [Google Scholar]
- 2. Paw I, Carpenter RC, Watabe K, Debinski W, Lo HW. Mechanisms regulating glioma invasion. Cancer Lett (2015) 362(1):1–7. doi: 10.1016/j.canlet.2015.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barthel L, Hadamitzky M, Dammann P, Schedlowski M, Sure U, Thakur BK, et al. Glioma: molecular signature and crossroads with tumor microenvironment. Cancer metastasis Rev (2022) 41(1):53–75. doi: 10.1007/s10555-021-09997-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huang H, Zhang S, Li Y, Liu Z, Mi L, Cai Y, et al. Suppression of mitochondrial ros by prohibitin drives glioblastoma progression and therapeutic resistance. Nat Commun (2021) 12(1):3720. doi: 10.1038/s41467-021-24108-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ou A, Yung WKA, Majd N. Molecular mechanisms of treatment resistance in glioblastoma. Int J Mol Sci (2020) 22(1):315. doi: 10.3390/ijms22010351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Stupp R, Mason WP, van den Bent MJ, Weller M, Fisher B, Taphoorn MJ, et al. Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. New Engl J Med (2005) 352(10):987–96. doi: 10.1056/NEJMoa043330 [DOI] [PubMed] [Google Scholar]
- 7. Diaz RJ, Ali S, Qadir MG, de la Fuente MI, Ivan ME, Komotar RJ. The role of bevacizumab in the treatment of glioblastoma. J neuro-oncol (2017) 133(3):455–67. doi: 10.1007/s11060-017-2477-x [DOI] [PubMed] [Google Scholar]
- 8. Chien CH, Hsueh WT, Chuang JY, Chang KY. Dissecting the mechanism of temozolomide resistance and its association with the regulatory roles of intracellular reactive oxygen species in glioblastoma. J Biomed Sci (2021) 28(1):18. doi: 10.1186/s12929-021-00717-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Thomas A, Tanaka M, Trepel J, Reinhold WC, Rajapakse VN, Pommier Y. Temozolomide in the era of precision medicine. Cancer Res (2017) 77(4):823–6. doi: 10.1158/0008-5472.Can-16-2983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tomar MS, Kumar A, Srivastava C, Shrivastava A. Elucidating the mechanisms of temozolomide resistance in gliomas and the strategies to overcome the resistance. Biochim Biophys Acta Rev Cancer (2021) 1876(2):188616. doi: 10.1016/j.bbcan.2021.188616 [DOI] [PubMed] [Google Scholar]
- 11. Lee SY. Temozolomide resistance in glioblastoma multiforme. Genes Dis (2016) 3(3):198–210. doi: 10.1016/j.gendis.2016.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Beal K, Abrey LE, Gutin PH. Antiangiogenic agents in the treatment of recurrent or newly diagnosed glioblastoma: analysis of single-agent and combined modality approaches. Radiat Oncol (London England) (2011) 6:2. doi: 10.1186/1748-717x-6-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fu M, Zhou Z, Huang X, Chen Z, Zhang L, Zhang J, et al. Use of bevacizumab in recurrent glioblastoma: A scoping review and evidence map. BMC Cancer (2023) 23(1):544. doi: 10.1186/s12885-023-11043-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Fazio S, Russo E, Ammendola M, Donato Di Paola E, De Sarro G. Efficacy and safety of bevacizumab in glioblastomas. Curr medicinal Chem (2012) 19(7):972–81. doi: 10.2174/092986712799320646 [DOI] [PubMed] [Google Scholar]
- 15. Sies H, Jones DP. Reactive oxygen species (Ros) as pleiotropic physiological signalling agents. Nat Rev Mol Cell Biol (2020) 21(7):363–83. doi: 10.1038/s41580-020-0230-3 [DOI] [PubMed] [Google Scholar]
- 16. Kumari S, Badana AK G, Mohan M, Shailender G, Malla R. Reactive oxygen species: A key constituent in cancer survival. biomark Insights (2018) 13:1177271918755391. doi: 10.1177/1177271918755391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Powers SK, Deminice R, Ozdemir M, Yoshihara T, Bomkamp MP, Hyatt H. Exercise-induced oxidative stress: friend or foe? J sport Health Sci (2020) 9(5):415–25. doi: 10.1016/j.jshs.2020.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Eckert D, Rapp F, Tsedeke AT, Molendowska J, Lehn R, Langhans M, et al. Ros- and radiation source-dependent modulation of leukocyte adhesion to primary microvascular endothelial cells. Cells (2021) 11(1):72. doi: 10.3390/cells11010072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Roy J, Galano JM, Durand T, Le Guennec JY, Lee JC. Physiological role of reactive oxygen species as promoters of natural defenses. FASEB J (2017) 31(9):3729–45. doi: 10.1096/fj.201700170R [DOI] [PubMed] [Google Scholar]
- 20. Gao Q. Oxidative stress and autophagy. Adv Exp Med Biol (2019) 1206:179–98. doi: 10.1007/978-981-15-0602-4_9 [DOI] [PubMed] [Google Scholar]
- 21. Poprac P, Jomova K, Simunkova M, Kollar V, Rhodes CJ, Valko M. Targeting free radicals in oxidative stress-related human diseases. Trends Pharmacol Sci (2017) 38(7):592–607. doi: 10.1016/j.tips.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 22. Barciszewska AM, Giel-Pietraszuk M, Perrigue PM, Naskręt-Barciszewska M. Total DNA methylation changes reflect random oxidative DNA damage in gliomas. Cells (2019) 8(9):1065. doi: 10.3390/cells8091065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hao Z, Huajun S, Zhen G, Yu X, Qian L, Ziling C, et al. Aqp8 promotes glioma proliferation and growth, possibly through the ros/pten/akt signaling pathway. BMC Cancer (2023) 23(1):516. doi: 10.1186/s12885-023-11025-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Chiu WT, Shen SC, Chow JM, Lin CW, Shia LT, Chen YC. Contribution of reactive oxygen species to migration/invasion of human glioblastoma cells U87 via erk-dependent cox-2/pge(2) activation. Neurobiol Dis (2010) 37(1):118–29. doi: 10.1016/j.nbd.2009.09.015 [DOI] [PubMed] [Google Scholar]
- 25. Qin LS, Jia PF, Zhang ZQ, Zhang SM. Ros-P53-cyclophilin-D signaling mediates salinomycin-induced glioma cell necrosis. J Exp Clin Cancer Res: CR (2015) 34(1):57. doi: 10.1186/s13046-015-0174-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wen ZH, Kuo HM, Shih PC, Hsu LC, Chuang JM, Chen NF, et al. Isoaaptamine increases ros levels causing autophagy and mitochondria-mediated apoptosis in glioblastoma multiforme cells. Biomed Pharmacother = Biomed Pharmacotherapie (2023) 160:114359. doi: 10.1016/j.biopha.2023.114359 [DOI] [PubMed] [Google Scholar]
- 27. Sabarinathan D, Mahalakshmi P, Vanisree AJ. Naringenin, a flavanone inhibits the proliferation of cerebrally implanted C6 glioma cells in rats. Chemico-biological Interact (2011) 189(1-2):26–36. doi: 10.1016/j.cbi.2010.09.028 [DOI] [PubMed] [Google Scholar]
- 28. Burić SS, Podolski-Renić A, Dinić J, Stanković T, Jovanović M, Hadžić S, et al. Modulation of antioxidant potential with coenzyme Q10 suppressed invasion of temozolomide-resistant rat glioma in vitro and in vivo. Oxid Med Cell Longevity (2019) 2019:3061607. doi: 10.1155/2019/3061607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hsia T, Small JL, Yekula A, Batool SM, Escobedo AK, Ekanayake E, et al. Systematic review of photodynamic therapy in gliomas. Cancers (2023) 15(15):3918. doi: 10.3390/cancers15153918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wang X, Jia Y, Wang P, Liu Q, Zheng H. Current status and future perspectives of sonodynamic therapy in glioma treatment. Ultrasonics sonochemistry (2017) 37:592–9. doi: 10.1016/j.ultsonch.2017.02.020 [DOI] [PubMed] [Google Scholar]
- 31. Liu D, Dai X, Ye L, Wang H, Qian H, Cheng H, et al. Nanotechnology meets glioblastoma multiforme: emerging therapeutic strategies. Wiley Interdiscip Rev Nanomed Nanobiotechnol (2023) 15(1):e1838. doi: 10.1002/wnan.1838 [DOI] [PubMed] [Google Scholar]
- 32. Weng MS, Ho YS, Lin JK. Chrysin induces G1 phase cell cycle arrest in C6 glioma cells through inducing P21waf1/cip1 expression: involvement of P38 mitogen-activated protein kinase. Biochem Pharmacol (2005) 69(12):1815–27. doi: 10.1016/j.bcp.2005.03.011 [DOI] [PubMed] [Google Scholar]
- 33. Matés JM, Segura JA, Alonso FJ, Márquez J. Roles of dioxins and heavy metals in cancer and neurological diseases using ros-mediated mechanisms. Free Radical Biol Med (2010) 49(9):1328–41. doi: 10.1016/j.freeradbiomed.2010.07.028 [DOI] [PubMed] [Google Scholar]
- 34. Wang M, Charareh P, Lei X, Zhong JL. Autophagy: multiple mechanisms to protect skin from ultraviolet radiation-driven photoaging. Oxid Med Cell Longevity (2019) 2019:8135985. doi: 10.1155/2019/8135985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Poljšak B, Fink R. The protective role of antioxidants in the defence against ros/rns-mediated environmental pollution. Oxid Med Cell Longevity (2014) 2014:671539. doi: 10.1155/2014/671539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Zhang Y, Shen W, Zhang P, Chen L, Xiao C. Gsh-triggered release of sulfur dioxide gas to regulate redox balance for enhanced photodynamic therapy. Chem Commun (Cambridge England) (2020) 56(42):5645–8. doi: 10.1039/d0cc00470g [DOI] [PubMed] [Google Scholar]
- 37. Liu K, Hua S, Song L. Pm2.5 exposure and asthma development: the key role of oxidative stress. Oxid Med Cell Longevity (2022) 2022:3618806. doi: 10.1155/2022/3618806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nolfi-Donegan D, Braganza A, Shiva S. Mitochondrial electron transport chain: oxidative phosphorylation, oxidant production, and methods of measurement. Redox Biol (2020) 37:101674. doi: 10.1016/j.redox.2020.101674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Chocry M, Leloup L. The nadph oxidase family and its inhibitors. Antioxid Redox Signaling (2020) 33(5):332–53. doi: 10.1089/ars.2019.7915 [DOI] [PubMed] [Google Scholar]
- 40. He A, Dean JM, Lodhi IJ. Peroxisomes as cellular adaptors to metabolic and environmental stress. Trends Cell Biol (2021) 31(8):656–70. doi: 10.1016/j.tcb.2021.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang Y, Qi H, Liu Y, Duan C, Liu X, Xia T, et al. The double-edged roles of ros in cancer prevention and therapy. Theranostics (2021) 11(10):4839–57. doi: 10.7150/thno.56747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gowda P, Lathoria K, Umdor SB, Sen E. Brg1 mutation alters oxidative stress responses in glioblastoma. Neurochemistry Int (2021) 150:105189. doi: 10.1016/j.neuint.2021.105189 [DOI] [PubMed] [Google Scholar]
- 43. Lin HY, Lim SW, Hsu TI, Yang WB, Huang CC, Tsai YT, et al. Ccaat/enhancer-binding protein delta regulates glioblastoma survival through catalase-mediated hydrogen peroxide clearance. Oxid Med Cell Longevity (2022) 2022:4081380. doi: 10.1155/2022/4081380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chen TC, Chuang JY, Ko CY, Kao TJ, Yang PY, Yu CH, et al. Ar ubiquitination induced by the curcumin analog suppresses growth of temozolomide-resistant glioblastoma through disrupting gpx4-mediated redox homeostasis. Redox Biol (2020) 30:101413. doi: 10.1016/j.redox.2019.101413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhu Z, Du S, Du Y, Ren J, Ying G, Yan Z. Glutathione reductase mediates drug resistance in glioblastoma cells by regulating redox homeostasis. J neurochemistry (2018) 144(1):93–104. doi: 10.1111/jnc.14250 [DOI] [PubMed] [Google Scholar]
- 46. Liu Y, Liang Y, Zheng T, Yang G, Zhang X, Sun Z, et al. Inhibition of heme oxygenase-1 enhances anti-cancer effects of arsenic trioxide on glioma cells. J neuro-oncol (2011) 104(2):449–58. doi: 10.1007/s11060-010-0513-1 [DOI] [PubMed] [Google Scholar]
- 47. Kim SH, Kwon CH, Nakano I. Detoxification of oxidative stress in glioma stem cells: mechanism, clinical relevance, and therapeutic development. J Neurosci Res (2014) 92(11):1419–24. doi: 10.1002/jnr.23431 [DOI] [PubMed] [Google Scholar]
- 48. Pires V, Bramatti I, Aschner M, Branco V, Carvalho C. Thioredoxin reductase inhibitors as potential antitumors: mercury compounds efficacy in glioma cells. Front Mol Biosci (2022) 9:889971. doi: 10.3389/fmolb.2022.889971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lei K, Xia Y, Wang XC, Ahn EH, Jin L, Ye K. C/ebpβ Mediates nqo1 and gstp1 anti-oxidative reductases expression in glioblastoma, promoting brain tumor proliferation. Redox Biol (2020) 34:101578. doi: 10.1016/j.redox.2020.101578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Sleire L, Skeie BS, Netland IA, Førde HE, Dodoo E, Selheim F, et al. Drug repurposing: sulfasalazine sensitizes gliomas to gamma knife radiosurgery by blocking cystine uptake through system xc-, leading to glutathione depletion. Oncogene (2015) 34(49):5951–9. doi: 10.1038/onc.2015.60 [DOI] [PubMed] [Google Scholar]
- 51. Deveci HA, Akyuva Y, Nur G, Nazıroğlu M. Alpha lipoic acid attenuates hypoxia-induced apoptosis, inflammation and mitochondrial oxidative stress via inhibition of trpa1 channel in human glioblastoma cell line. Biomed Pharmacother = Biomed Pharmacotherapie (2019) 111:292–304. doi: 10.1016/j.biopha.2018.12.077 [DOI] [PubMed] [Google Scholar]
- 52. Frontiñán-Rubio J, Santiago-Mora RM, Nieva-Velasco CM, Ferrín G, Martínez-González A, Gómez MV, et al. Regulation of the oxidative balance with coenzyme Q10 sensitizes human glioblastoma cells to radiation and temozolomide. Radiother Oncol (2018) 128(2):236–44. doi: 10.1016/j.radonc.2018.04.033 [DOI] [PubMed] [Google Scholar]
- 53. Lu MC, Ji JA, Jiang ZY, You QD. The keap1-nrf2-are pathway as a potential preventive and therapeutic target: an update. Medicinal Res Rev (2016) 36(5):924–63. doi: 10.1002/med.21396 [DOI] [PubMed] [Google Scholar]
- 54. Broekgaarden M, Weijer R, van Gulik TM, Hamblin MR, Heger M. Tumor cell survival pathways activated by photodynamic therapy: A molecular basis for pharmacological inhibition strategies. Cancer metastasis Rev (2015) 34(4):643–90. doi: 10.1007/s10555-015-9588-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Bellezza I, Giambanco I, Minelli A, Donato R. Nrf2-keap1 signaling in oxidative and reductive stress. Biochim Biophys Acta Mol Cell Res (2018) 1865(5):721–33. doi: 10.1016/j.bbamcr.2018.02.010 [DOI] [PubMed] [Google Scholar]
- 56. Zhan M, Wang H, Xu SW, Yang LH, Chen W, Zhao SX, et al. Variants in oxidative stress-related genes affect the chemosensitivity through nrf2-mediated signaling pathway in biliary tract cancer. EBioMedicine (2019) 48:143–60. doi: 10.1016/j.ebiom.2019.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chowdhury I, Fisher AB, Christofidou-Solomidou M, Gao L, Tao JQ, Sorokina EM, et al. Keratinocyte growth factor and glucocorticoid induction of human peroxiredoxin 6 gene expression occur by independent mechanisms that are synergistic. Antioxid Redox Signaling (2014) 20(3):391–402. doi: 10.1089/ars.2012.4634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lv H, Zhu C, Wei W, Lv X, Yu Q, Deng X, et al. Enhanced keap1-nrf2/trx-1 axis by daphnetin protects against oxidative stress-driven hepatotoxicity via inhibiting ask1/jnk and txnip/nlrp3 inflammasome activation. Phytomed: Int J Phytother Phytopharmacol (2020) 71:153241. doi: 10.1016/j.phymed.2020.153241 [DOI] [PubMed] [Google Scholar]
- 59. Xu H, Jin J, Chen Y, Wu G, Zhu H, Wang Q, et al. Gbp3 promotes glioblastoma resistance to temozolomide by enhancing DNA damage repair. Oncogene (2022) 41(31):3876–85. doi: 10.1038/s41388-022-02397-5 [DOI] [PubMed] [Google Scholar]
- 60. Wick W, Weller M, van den Bent M, Sanson M, Weiler M, von Deimling A, et al. Mgmt testing–the challenges for biomarker-based glioma treatment. Nat Rev Neurol (2014) 10(7):372–85. doi: 10.1038/nrneurol.2014.100 [DOI] [PubMed] [Google Scholar]
- 61. Knijnenburg TA, Wang L, Zimmermann MT, Chambwe N, Gao GF, Cherniack AD, et al. Genomic and molecular landscape of DNA damage repair deficiency across the cancer genome atlas. Cell Rep (2018) 23(1):239–54.e6. doi: 10.1016/j.celrep.2018.03.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Nitta M, Kozono D, Kennedy R, Stommel J, Ng K, Zinn PO, et al. Targeting egfr induced oxidative stress by parp1 inhibition in glioblastoma therapy. PloS One (2010) 5(5):e10767. doi: 10.1371/journal.pone.0010767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gan T, Wang Y, Xie M, Wang Q, Zhao S, Wang P, et al. Mex3a impairs DNA mismatch repair signaling and mediates acquired temozolomide resistance in glioblastoma. Cancer Res (2022) 82(22):4234–46. doi: 10.1158/0008-5472.Can-22-2036 [DOI] [PubMed] [Google Scholar]
- 64. Chen Y, Liu P, Sun P, Jiang J, Zhu Y, Dong T, et al. Oncogenic msh6-cxcr4-tgfb1 feedback loop: A novel therapeutic target of photothermal therapy in glioblastoma multiforme. Theranostics (2019) 9(5):1453–73. doi: 10.7150/thno.29987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ray A, Milum K, Battu A, Wani G, Wani AA. Ner initiation factors, ddb2 and xpc, regulate uv radiation response by recruiting atr and atm kinases to DNA damage sites. DNA Repair (2013) 12(4):273–83. doi: 10.1016/j.dnarep.2013.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Yi GZ, Huang G, Guo M, Zhang X, Wang H, Deng S, et al. Acquired temozolomide resistance in mgmt-deficient glioblastoma cells is associated with regulation of DNA repair by dhc2. Brain: J Neurol (2019) 142(8):2352–66. doi: 10.1093/brain/awz202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Oyewole AO, Birch-Machin MA. Mitochondria-targeted antioxidants. FASEB J (2015) 29(12):4766–71. doi: 10.1096/fj.15-275404 [DOI] [PubMed] [Google Scholar]
- 68. Scuderi SA, Filippone A, Basilotta R, Mannino D, Casili G, Capra AP, et al. Gsk343, an inhibitor of enhancer of zeste homolog 2, reduces glioblastoma progression through inflammatory process modulation: focus on canonical and non-canonical nf-Kb/Iκbα Pathways. Int J Mol Sci (2022) 23(22):13915. doi: 10.3390/ijms232213915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Liang J, Yang Y, Li X, Cai G, Cao J, Zhang B. Expression of eif4e gene in glioma and its sensitivity to oxidative stress. Oxid Med Cell Longev (2022) 2022:5413035. doi: 10.1155/2022/5413035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Chang KY, Hsu TI, Hsu CC, Tsai SY, Liu JJ, Chou SW, et al. Specificity protein 1-modulated superoxide dismutase 2 enhances temozolomide resistance in glioblastoma, which is independent of O(6)-methylguanine-DNA methyltransferase. Redox Biol (2017) 13:655–64. doi: 10.1016/j.redox.2017.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Flor S, Oliva CR, Ali MY, Coleman KL, Greenlee JD, Jones KA, et al. Catalase overexpression drives an aggressive phenotype in glioblastoma. Antioxid (Basel Switzerland) (2021) 10(12):1988. doi: 10.3390/antiox10121988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Pisoschi AM, Pop A. The role of antioxidants in the chemistry of oxidative stress: A review. Eur J Med Chem (2015) 97:55–74. doi: 10.1016/j.ejmech.2015.04.040 [DOI] [PubMed] [Google Scholar]
- 73. Zhan S, Lu L, Pan SS, Wei XQ, Miao RR, Liu XH, et al. Targeting nqo1/gpx4-mediated ferroptosis by plumbagin suppresses in vitro and in vivo glioma growth. Br J Cancer (2022) 127(2):364–76. doi: 10.1038/s41416-022-01800-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lv H, Zhen C, Liu J, Yang P, Hu L, Shang P. Unraveling the potential role of glutathione in multiple forms of cell death in cancer therapy. Oxid Med Cell Longevity (2019) 2019:3150145. doi: 10.1155/2019/3150145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Ozyerli-Goknar E, Sur-Erdem I, Seker F, Cingöz A, Kayabolen A, Kahya-Yesil Z, et al. The fungal metabolite chaetocin is a sensitizer for pro-apoptotic therapies in glioblastoma. Cell Death Dis (2019) 10(12):894. doi: 10.1038/s41419-019-2107-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Dennery PA. Signaling function of heme oxygenase proteins. Antioxid Redox Signaling (2014) 20(11):1743–53. doi: 10.1089/ars.2013.5674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sukumari-Ramesh S, Prasad N, Alleyne CH, Vender JR, Dhandapani KM. Overexpression of nrf2 attenuates carmustine-induced cytotoxicity in U87mg human glioma cells. BMC Cancer (2015) 15:118. doi: 10.1186/s12885-015-1134-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. West J, Roston T, David J, Allan K, Loberg M. Piecing together how peroxiredoxins maintain genomic stability. Antioxidants (2018) 7(12):177. doi: 10.3390/antiox7120177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Gao F, Zheng W, Gao L, Cai P, Liu R, Wang Y, et al. Au nanoclusters and photosensitizer dual loaded spatiotemporal controllable liposomal nanocomposites enhance tumor photodynamic therapy effect by inhibiting thioredoxin reductase. Advanced Healthc Mater (2017) 6(7):1601453. doi: 10.1002/adhm.201601453 [DOI] [PubMed] [Google Scholar]
- 80. Ahmadi R, Urig S, Hartmann M, Helmke BM, Koncarevic S, Allenberger B, et al. Antiglioma activity of 2,2’:6’,2”-terpyridineplatinum(Ii) complexes in a rat model–effects on cellular redox metabolism. Free Radic Biol Med (2006) 40(5):763–78. doi: 10.1016/j.freeradbiomed.2005.09.031 [DOI] [PubMed] [Google Scholar]
- 81. Lei K, Gu X, Alvarado AG, Du Y, Luo S, Ahn EH, et al. Discovery of a dual inhibitor of nqo1 and gstp1 for treating glioblastoma. J Hematol Oncol (2020) 13(1):141. doi: 10.1186/s13045-020-00979-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ross D, Siegel D. The diverse functionality of nqo1 and its roles in redox control. Redox Biol (2021) 41:101950. doi: 10.1016/j.redox.2021.101950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Zhong B, Yu J, Hou Y, Ai N, Ge W, Lu JJ, et al. A novel strategy for glioblastoma treatment by induction of noptosis, an nqo1-dependent necrosis. Free Radic Biol Med (2021) 166:104–15. doi: 10.1016/j.freeradbiomed.2021.02.014 [DOI] [PubMed] [Google Scholar]
- 84. Koehler CM, Beverly KN, Leverich EP. Redox pathways of the mitochondrion. Antioxid Redox Signaling (2006) 8(5-6):813–22. doi: 10.1089/ars.2006.8.813 [DOI] [PubMed] [Google Scholar]
- 85. Pérez-Ortiz JM, Tranque P, Vaquero CF, Domingo B, Molina F, Calvo S, et al. Glitazones differentially regulate primary astrocyte and glioma cell survival. Involvement of reactive oxygen species and peroxisome proliferator-activated receptor-gamma. J Biol Chem (2004) 279(10):8976–85. doi: 10.1074/jbc.M308518200 [DOI] [PubMed] [Google Scholar]
- 86. Wang C, He C, Lu S, Wang X, Wang L, Liang S, et al. Autophagy activated by silibinin contributes to glioma cell death via induction of oxidative stress-mediated bnip3-dependent nuclear translocation of aif. Cell Death Dis (2020) 11(8):630. doi: 10.1038/s41419-020-02866-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Fasipe B, Faria A, Laher I. Potential for novel therapeutic uses of alpha lipoic acid. Curr medicinal Chem (2023) 30(35):3942–54. doi: 10.2174/0929867329666221006115329 [DOI] [PubMed] [Google Scholar]
- 88. Pisoschi AM, Pop A, Iordache F, Stanca L, Predoi G, Serban AI. Oxidative stress mitigation by antioxidants - an overview on their chemistry and influences on health status. Eur J medicinal Chem (2021) 209:112891. doi: 10.1016/j.ejmech.2020.112891 [DOI] [PubMed] [Google Scholar]
- 89. Visnes T, Benítez-Buelga C, Cázares-Körner A, Sanjiv K, Hanna BMF, Mortusewicz O, et al. Targeting ogg1 arrests cancer cell proliferation by inducing replication stress. Nucleic Acids Res (2020) 48(21):12234–51. doi: 10.1093/nar/gkaa1048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. McAdam E, Brem R, Karran P. Oxidative stress-induced protein damage inhibits DNA repair and determines mutation risk and therapeutic efficacy. Mol Cancer Res: MCR (2016) 14(7):612–22. doi: 10.1158/1541-7786.Mcr-16-0053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Fabrizio FP, Sparaneo A, Trombetta D, Muscarella LA. Epigenetic versus genetic deregulation of the keap1/nrf2 axis in solid tumors: focus on methylation and noncoding rnas. Oxid Med Cell Longevity (2018) 2018:2492063. doi: 10.1155/2018/2492063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Zheng XJ, Chen WL, Yi J, Li W, Liu JY, Fu WQ, et al. Apolipoprotein C1 promotes glioblastoma tumorigenesis by reducing keap1/nrf2 and cbs-regulated ferroptosis. Acta Pharmacologica Sin (2022) 43(11):2977–92. doi: 10.1038/s41401-022-00917-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Cong ZX, Wang HD, Zhou Y, Wang JW, Pan H, Zhang DD, et al. Temozolomide and irradiation combined treatment-induced nrf2 activation increases chemoradiation sensitivity in human glioblastoma cells. J Neurooncol (2014) 116(1):41–8. doi: 10.1007/s11060-013-1260-x [DOI] [PubMed] [Google Scholar]
- 94. Fujii S, Sawa T, Ihara H, Tong KI, Ida T, Okamoto T, et al. The critical role of nitric oxide signaling, via protein S-guanylation and nitrated cyclic gmp, in the antioxidant adaptive response. J Biol Chem (2010) 285(31):23970–84. doi: 10.1074/jbc.M110.145441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dapash M, Hou D, Castro B, Lee-Chang C, Lesniak MS. The interplay between glioblastoma and its microenvironment. Cells (2021) 10(9):2257. doi: 10.3390/cells10092257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Gieryng A, Pszczolkowska D, Walentynowicz KA, Rajan WD, Kaminska B. Immune microenvironment of gliomas. Lab Invest (2017) 97(5):498–518. doi: 10.1038/labinvest.2017.19 [DOI] [PubMed] [Google Scholar]
- 97. Kuo CL, Ponneri Babuharisankar A, Lin YC, Lien HW, Lo YK, Chou HY, et al. Mitochondrial oxidative stress in the tumor microenvironment and cancer immunoescape: foe or friend? J Biomed Sci (2022) 29(1):74. doi: 10.1186/s12929-022-00859-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Kotsafti A, Scarpa M, Castagliuolo I, Scarpa M. Reactive oxygen species and antitumor immunity-from surveillance to evasion. Cancers (Basel) (2020) 12(7):1748. doi: 10.3390/cancers12071748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Wei J, Chen P, Gupta P, Ott M, Zamler D, Kassab C, et al. Immune biology of glioma-associated macrophages and microglia: functional and therapeutic implications. Neuro-oncology (2020) 22(2):180–94. doi: 10.1093/neuonc/noz212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kaminska B, Mota M, Pizzi M. Signal transduction and epigenetic mechanisms in the control of microglia activation during neuroinflammation. Biochim Biophys Acta (2016) 1862(3):339–51. doi: 10.1016/j.bbadis.2015.10.026 [DOI] [PubMed] [Google Scholar]
- 101. Zha C, Meng X, Li L, Mi S, Qian D, Li Z, et al. Neutrophil extracellular traps mediate the crosstalk between glioma progression and the tumor microenvironment via the hmgb1/rage/il-8 axis. Cancer Biol Med (2020) 17(1):154–68. doi: 10.20892/j.issn.2095-3941.2019.0353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Raychaudhuri B, Rayman P, Ireland J, Ko J, Rini B, Borden EC, et al. Myeloid-derived suppressor cell accumulation and function in patients with newly diagnosed glioblastoma. Neuro-oncology (2011) 13(6):591–9. doi: 10.1093/neuonc/nor042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Ostrand-Rosenberg S, Sinha P. Myeloid-derived suppressor cells: linking inflammation and cancer. J Immunol (Baltimore Md: 1950) (2009) 182(8):4499–506. doi: 10.4049/jimmunol.0802740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Rodriguez PC, Quiceno DG, Ochoa AC. L-arginine availability regulates T-lymphocyte cell-cycle progression. Blood (2007) 109(4):1568–73. doi: 10.1182/blood-2006-06-031856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol (2009) 9(3):162–74. doi: 10.1038/nri2506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Dubinski D, Wölfer J, Hasselblatt M, Schneider-Hohendorf T, Bogdahn U, Stummer W, et al. Cd4+ T effector memory cell dysfunction is associated with the accumulation of granulocytic myeloid-derived suppressor cells in glioblastoma patients. Neuro-oncology (2016) 18(6):807–18. doi: 10.1093/neuonc/nov280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Tao B, Shi J, Shuai S, Zhou H, Zhang H, Li B, et al. Cyb561d2 up-regulation activates stat3 to induce immunosuppression and aggression in gliomas. J Trans Med (2021) 19(1):338. doi: 10.1186/s12967-021-02987-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Aboelella NS, Brandle C, Kim T, Ding ZC, Zhou G. Oxidative stress in the tumor microenvironment and its relevance to cancer immunotherapy. Cancers (2021) 13(5):986. doi: 10.3390/cancers13050986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ohta A, Sitkovsky M. Extracellular adenosine-mediated modulation of regulatory T cells. Front Immunol (2014) 5:304. doi: 10.3389/fimmu.2014.00304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Ma T, Renz BW, Ilmer M, Koch D, Yang Y, Werner J, et al. Myeloid-derived suppressor cells in solid tumors. Cells (2022) 11(2):310. doi: 10.3390/cells11020310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Wang M, Zhou Z, Wang X, Zhang C, Jiang X. Natural killer cell awakening: unleash cancer-immunity cycle against glioblastoma. Cell Death Dis (2022) 13(7):588. doi: 10.1038/s41419-022-05041-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Chaplin DD. Overview of the immune response. J Allergy Clin Immunol (2010) 125(2 Suppl 2):S3–23. doi: 10.1016/j.jaci.2009.12.980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol (2005) 5(12):953–64. doi: 10.1038/nri1733 [DOI] [PubMed] [Google Scholar]
- 114. Gracia-Hernandez M, Sotomayor EM, Villagra A. Targeting macrophages as a therapeutic option in coronavirus disease 2019. Front Pharmacol (2020) 11:577571. doi: 10.3389/fphar.2020.577571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Randolph GJ, Jakubzick C, Qu C. Antigen presentation by monocytes and monocyte-derived cells. Curr Opin Immunol (2008) 20(1):52–60. doi: 10.1016/j.coi.2007.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Borst K, Dumas AA, Prinz M. Microglia: immune and non-immune functions. Immunity (2021) 54(10):2194–208. doi: 10.1016/j.immuni.2021.09.014 [DOI] [PubMed] [Google Scholar]
- 117. Brown GC, Neher JJ. Microglial phagocytosis of live neurons. Nat Rev Neurosci (2014) 15(4):209–16. doi: 10.1038/nrn3710 [DOI] [PubMed] [Google Scholar]
- 118. Nguyen PT, Dorman LC, Pan S, Vainchtein ID, Han RT, Nakao-Inoue H, et al. Microglial remodeling of the extracellular matrix promotes synapse plasticity. Cell (2020) 182(2):388–403.e15. doi: 10.1016/j.cell.2020.05.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Nayak D, Roth TL, McGavern DB. Microglia development and function. Annu Rev Immunol (2014) 32:367–402. doi: 10.1146/annurev-immunol-032713-120240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Larionova I, Tuguzbaeva G, Ponomaryova A, Stakheyeva M, Cherdyntseva N, Pavlov V, et al. Tumor-associated macrophages in human breast, colorectal, lung, ovarian and prostate cancers. Front Oncol (2020) 10:566511. doi: 10.3389/fonc.2020.566511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Zeng F, Li G, Liu X, Zhang K, Huang H, Jiang T, et al. Plasminogen activator urokinase receptor implies immunosuppressive features and acts as an unfavorable prognostic biomarker in glioma. Oncologist (2021) 26(8):e1460–e9. doi: 10.1002/onco.13750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Shan K, Feng N, Cui J, Wang S, Qu H, Fu G, et al. Resolvin D1 and D2 inhibit tumour growth and inflammation via modulating macrophage polarization. J Cell Mol Med (2020) 24(14):8045–56. doi: 10.1111/jcmm.15436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Mantovani A, Sica A, Locati M. New vistas on macrophage differentiation and activation. Eur J Immunol (2007) 37(1):14–6. doi: 10.1002/eji.200636910 [DOI] [PubMed] [Google Scholar]
- 124. Lakshmi Narendra B, Eshvendar Reddy K, Shantikumar S, Ramakrishna S. Immune system: A double-edged sword in cancer. Inflammation Res (2013) 62(9):823–34. doi: 10.1007/s00011-013-0645-9 [DOI] [PubMed] [Google Scholar]
- 125. Chen Z, Hambardzumyan D. Immune microenvironment in glioblastoma subtypes. Front Immunol (2018) 9:1004. doi: 10.3389/fimmu.2018.01004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. da Fonseca AC, Badie B. Microglia and macrophages in malignant gliomas: recent discoveries and implications for promising therapies. Clin Dev Immunol (2013) 2013:264124. doi: 10.1155/2013/264124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Chanmee T, Ontong P, Konno K, Itano N. Tumor-associated macrophages as major players in the tumor microenvironment. Cancers (2014) 6(3):1670–90. doi: 10.3390/cancers6031670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Noy R, Pollard JW. Tumor-associated macrophages: from mechanisms to therapy. Immunity (2014) 41(1):49–61. doi: 10.1016/j.immuni.2014.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Zhou W, Yu X, Sun S, Zhang X, Yang W, Zhang J, et al. Increased expression of mmp-2 and mmp-9 indicates poor prognosis in glioma recurrence. Biomed Pharmacother = Biomed Pharmacotherapie (2019) 118:109369. doi: 10.1016/j.biopha.2019.109369 [DOI] [PubMed] [Google Scholar]
- 130. Brandenburg S, Müller A, Turkowski K, Radev YT, Rot S, Schmidt C, et al. Resident microglia rather than peripheral macrophages promote vascularization in brain tumors and are source of alternative pro-angiogenic factors. Acta Neuropathologica (2016) 131(3):365–78. doi: 10.1007/s00401-015-1529-6 [DOI] [PubMed] [Google Scholar]
- 131. Ramírez-Expósito MJ, Martínez-Martos JM. The delicate equilibrium between oxidants and antioxidants in brain glioma. Curr Neuropharmacol (2019) 17(4):342–51. doi: 10.2174/1570159x16666180302120925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Yu MO, Song NH, Park KJ, Park DH, Kim SH, Chae YS, et al. Romo1 is associated with ros production and cellular growth in human gliomas. J neuro-oncol (2015) 121(1):73–81. doi: 10.1007/s11060-014-1608-x [DOI] [PubMed] [Google Scholar]
- 133. Sun G, Cao Y, Qian C, Wan Z, Zhu J, Guo J, et al. Romo1 is involved in the immune response of glioblastoma by regulating the function of macrophages. Aging (2020) 12(2):1114–27. doi: 10.18632/aging.102648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Kaushal P, Zhu J, Wan Z, Chen H, Ye J, Luo C. Prognosis and immune landscapes in glioblastoma based on gene-signature related to reactive-oxygen-species. Neuromolecular Med (2023) 25(1):102–19. doi: 10.1007/s12017-022-08719-w [DOI] [PubMed] [Google Scholar]
- 135. Dokic I, Hartmann C, Herold-Mende C, Régnier-Vigouroux A. Glutathione peroxidase 1 activity dictates the sensitivity of glioblastoma cells to oxidative stress. Glia (2012) 60(11):1785–800. doi: 10.1002/glia.22397 [DOI] [PubMed] [Google Scholar]
- 136. Zhang Y, Handy DE, Loscalzo J. Adenosine-dependent induction of glutathione peroxidase 1 in human primary endothelial cells and protection against oxidative stress. Circ Res (2005) 96(8):831–7. doi: 10.1161/01.Res.0000164401.21929.Cf [DOI] [PubMed] [Google Scholar]
- 137. Law AMK, Valdes-Mora F, Gallego-Ortega D. Myeloid-derived suppressor cells as a therapeutic target for cancer. Cells (2020) 9(3):561. doi: 10.3390/cells9030561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Peng M, Zhang Q, Liu Y, Guo X, Ju J, Xu L, et al. Apolipoprotein a-I mimetic peptide L-4f suppresses granulocytic-myeloid-derived suppressor cells in mouse pancreatic cancer. Front Pharmacol (2020) 11:576. doi: 10.3389/fphar.2020.00576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Veglia F, Perego M, Gabrilovich D. Myeloid-derived suppressor cells coming of age. Nat Immunol (2018) 19(2):108–19. doi: 10.1038/s41590-017-0022-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Wang Y, Schafer CC, Hough KP, Tousif S, Duncan SR, Kearney JF, et al. Myeloid-derived suppressor cells impair B cell responses in lung cancer through il-7 and stat5. J Immunol (Baltimore Md: 1950) (2018) 201(1):278–95. doi: 10.4049/jimmunol.1701069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Huang B, Pan PY, Li Q, Sato AI, Levy DE, Bromberg J, et al. Gr-1+Cd115+ Immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host. Cancer Res (2006) 66(2):1123–31. doi: 10.1158/0008-5472.Can-05-1299 [DOI] [PubMed] [Google Scholar]
- 142. Beury DW, Parker KH, Nyandjo M, Sinha P, Carter KA, Ostrand-Rosenberg S. Cross-talk among myeloid-derived suppressor cells, macrophages, and tumor cells impacts the inflammatory milieu of solid tumors. J Leukoc Biol (2014) 96(6):1109–18. doi: 10.1189/jlb.3A0414-210R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Zhao H, Teng D, Yang L, Xu X, Chen J, Jiang T, et al. Myeloid-derived itaconate suppresses cytotoxic cd8(+) T cells and promotes tumour growth. Nat Metab (2022) 4(12):1660–73. doi: 10.1038/s42255-022-00676-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Hoechst B, Voigtlaender T, Ormandy L, Gamrekelashvili J, Zhao F, Wedemeyer H, et al. Myeloid derived suppressor cells inhibit natural killer cells in patients with hepatocellular carcinoma via the nkp30 receptor. Hepatol (Baltimore Md) (2009) 50(3):799–807. doi: 10.1002/hep.23054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Ostrand-Rosenberg S, Sinha P, Beury DW, Clements VK. Cross-talk between myeloid-derived suppressor cells (Mdsc), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin Cancer Biol (2012) 22(4):275–81. doi: 10.1016/j.semcancer.2012.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. García-Navas R, Munder M, Mollinedo F. Depletion of L-arginine induces autophagy as a cytoprotective response to endoplasmic reticulum stress in human T lymphocytes. Autophagy (2012) 8(11):1557–76. doi: 10.4161/auto.21315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Lamas B, Vergnaud-Gauduchon J, Goncalves-Mendes N, Perche O, Rossary A, Vasson MP, et al. Altered functions of natural killer cells in response to L-arginine availability. Cell Immunol (2012) 280(2):182–90. doi: 10.1016/j.cellimm.2012.11.018 [DOI] [PubMed] [Google Scholar]
- 148. Umansky V, Blattner C, Gebhardt C, Utikal J. The role of myeloid-derived suppressor cells (Mdsc) in cancer progression. Vaccines (2016) 4(4):36. doi: 10.3390/vaccines4040036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Su MT, Kumata S, Endo S, Okada Y, Takai T. Lilrb4 promotes tumor metastasis by regulating mdscs and inhibiting mir-1 family mirnas. Oncoimmunology (2022) 11(1):2060907. doi: 10.1080/2162402x.2022.2060907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Salminen A, Kaarniranta K, Kauppinen A. Immunosenescence: the potential role of myeloid-derived suppressor cells (Mdsc) in age-related immune deficiency. Cell Mol Life Sci (2019) 76(10):1901–18. doi: 10.1007/s00018-019-03048-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Kim ES, Kim JE, Patel MA, Mangraviti A, Ruzevick J, Lim M. Immune checkpoint modulators: an emerging antiglioma armamentarium. J Immunol Res (2016) 2016:4683607. doi: 10.1155/2016/4683607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Salemizadeh Parizi M, Salemizadeh Parizi F, Abdolhosseini S, Vanaei S, Manzouri A, Ebrahimzadeh F. Myeloid-derived suppressor cells (Mdscs) in brain cancer: challenges and therapeutic strategies. Inflammopharmacology (2021) 29(6):1613–24. doi: 10.1007/s10787-021-00878-9 [DOI] [PubMed] [Google Scholar]
- 153. Kamran N, Kadiyala P, Saxena M, Candolfi M, Li Y, Moreno-Ayala MA, et al. Immunosuppressive myeloid cells’ Blockade in the glioma microenvironment enhances the efficacy of immune-stimulatory gene therapy. Mol Ther (2017) 25(1):232–48. doi: 10.1016/j.ymthe.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. De Leo A, Ugolini A, Veglia F. Myeloid cells in glioblastoma microenvironment. Cells (2020) 10(1):18. doi: 10.3390/cells10010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Bayik D, Bartels CF, Lovrenert K, Watson DC, Zhang D, Kay K, et al. Distinct cell adhesion signature defines glioblastoma myeloid-derived suppressor cell subsets. Cancer Res (2022) 82(22):4274–87. doi: 10.1158/0008-5472.Can-21-3840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Bronte V, Brandau S, Chen SH, Colombo MP, Frey AB, Greten TF, et al. Recommendations for myeloid-derived suppressor cell nomenclature and characterization standards. Nat Commun (2016) 7:12150. doi: 10.1038/ncomms12150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Noman MZ, Desantis G, Janji B, Hasmim M, Karray S, Dessen P, et al. Pd-L1 is a novel direct target of hif-1α, and its blockade under hypoxia enhanced mdsc-mediated T cell activation. J Exp Med (2014) 211(5):781–90. doi: 10.1084/jem.20131916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Beury DW, Carter KA, Nelson C, Sinha P, Hanson E, Nyandjo M, et al. Myeloid-derived suppressor cell survival and function are regulated by the transcription factor nrf2. J Immunol (Baltimore Md: 1950) (2016) 196(8):3470–8. doi: 10.4049/jimmunol.1501785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Grabowski MM, Sankey EW, Ryan KJ, Chongsathidkiet P, Lorrey SJ, Wilkinson DS, et al. Immune suppression in gliomas. J neuro-oncol (2021) 151(1):3–12. doi: 10.1007/s11060-020-03483-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Ohl K, Tenbrock K. Reactive oxygen species as regulators of mdsc-mediated immune suppression. Front Immunol (2018) 9:2499. doi: 10.3389/fimmu.2018.02499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Kusmartsev S, Gabrilovich DI. Inhibition of myeloid cell differentiation in cancer: the role of reactive oxygen species. J Leukoc Biol (2003) 74(2):186–96. doi: 10.1189/jlb.0103010 [DOI] [PubMed] [Google Scholar]
- 162. Corzo CA, Cotter MJ, Cheng P, Cheng F, Kusmartsev S, Sotomayor E, et al. Mechanism regulating reactive oxygen species in tumor-induced myeloid-derived suppressor cells. J Immunol (Baltimore Md: 1950) (2009) 182(9):5693–701. doi: 10.4049/jimmunol.0900092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Irshad K, Srivastava C, Malik N, Arora M, Gupta Y, Goswami S, et al. Upregulation of atypical cadherin fat1 promotes an immunosuppressive tumor microenvironment via tgf-B. Front Immunol (2022) 13:813888. doi: 10.3389/fimmu.2022.813888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Shen T, Chen X, Chen Y, Xu Q, Lu F, Liu S. Increased pd-L1 expression and pd-L1/cd86 ratio on dendritic cells were associated with impaired dendritic cells function in hcv infection. J Med Virol (2010) 82(7):1152–9. doi: 10.1002/jmv.21809 [DOI] [PubMed] [Google Scholar]
- 165. Mittal SK, Cho KJ, Ishido S, Roche PA. Interleukin 10 (Il-10)-mediated immunosuppression: march-I induction regulates antigen presentation by macrophages but not dendritic cells. J Biol Chem (2015) 290(45):27158–67. doi: 10.1074/jbc.M115.682708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Li MO, Wan YY, Sanjabi S, Robertson AK, Flavell RA. Transforming growth factor-beta regulation of immune responses. Annu Rev Immunol (2006) 24:99–146. doi: 10.1146/annurev.immunol.24.021605.090737 [DOI] [PubMed] [Google Scholar]
- 167. Amarnath S, Mangus CW, Wang JC, Wei F, He A, Kapoor V, et al. The pdl1-pd1 axis converts human th1 cells into regulatory T cells. Sci Trans Med (2011) 3(111):111ra20. doi: 10.1126/scitranslmed.3003130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Muntjewerff EM, Meesters LD, van den Bogaart G. Antigen cross-presentation by macrophages. Front Immunol (2020) 11:1276. doi: 10.3389/fimmu.2020.01276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Spangler JB, Tomala J, Luca VC, Jude KM, Dong S, Ring AM, et al. Antibodies to interleukin-2 elicit selective T cell subset potentiation through distinct conformational mechanisms. Immunity (2015) 42(5):815–25. doi: 10.1016/j.immuni.2015.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Waldman AD, Fritz JM, Lenardo MJ. A guide to cancer immunotherapy: from T cell basic science to clinical practice. Nat Rev Immunol (2020) 20(11):651–68. doi: 10.1038/s41577-020-0306-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Savage PA, Klawon DEJ, Miller CH. Regulatory T cell development. Annu Rev Immunol (2020) 38:421–53. doi: 10.1146/annurev-immunol-100219-020937 [DOI] [PubMed] [Google Scholar]
- 172. Borst J, Ahrends T, Bąbała N, Melief CJM, Kastenmüller W. Cd4(+) T cell help in cancer immunology and immunotherapy. Nat Rev Immunol (2018) 18(10):635–47. doi: 10.1038/s41577-018-0044-0 [DOI] [PubMed] [Google Scholar]
- 173. Gähler A, Trufa DI, Chiriac MT, Tausche P, Hohenberger K, Brunst AK, et al. Glucose-restricted diet regulates the tumor immune microenvironment and prevents tumor growth in lung adenocarcinoma. Front Oncol (2022) 12:873293. doi: 10.3389/fonc.2022.873293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Kim KD, Bae S, Capece T, Nedelkovska H, de Rubio RG, Smrcka AV, et al. Targeted calcium influx boosts cytotoxic T lymphocyte function in the tumour microenvironment. Nat Commun (2017) 8:15365. doi: 10.1038/ncomms15365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Durgeau A, Virk Y, Corgnac S, Mami-Chouaib F. Recent advances in targeting cd8 T-cell immunity for more effective cancer immunotherapy. Front Immunol (2018) 9:14. doi: 10.3389/fimmu.2018.00014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Ni D, Tang T, Lu Y, Xu K, Shao Y, Saaoud F, et al. Canonical secretomes, innate immune caspase-1-, 4/11-gasdermin D non-canonical secretomes and exosomes may contribute to maintain treg-ness for treg immunosuppression, tissue repair and modulate anti-tumor immunity via ros pathways. Front Immunol (2021) 12:678201. doi: 10.3389/fimmu.2021.678201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Huang BR, Liu YS, Lai SW, Lin HJ, Shen CK, Yang LY, et al. Caix Regulates Gbm Motility and Tam Adhesion and Polarization through Egfr/Stat3 under Hypoxic Conditions. Int J Mol Sci (2020) 21(16):5838. doi: 10.3390/ijms21165838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Travis MA, Sheppard D. Tgf-B Activation and function in immunity. Annu Rev Immunol (2014) 32:51–82. doi: 10.1146/annurev-immunol-032713-120257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Ye Z, Zhang S, Cai J, Ye L, Gao L, Wang Y, et al. Development and validation of cuproptosis-associated prognostic signatures in who 2/3 glioma. Front Oncol (2022) 12:967159. doi: 10.3389/fonc.2022.967159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Ji H, Liu Z, Wang F, Sun H, Wang N, Liu Y, et al. Novel macrophage-related gene prognostic index for glioblastoma associated with M2 macrophages and T cell dysfunction. Front Immunol (2022) 13:941556. doi: 10.3389/fimmu.2022.941556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. DiDomenico J, Lamano JB, Oyon D, Li Y, Veliceasa D, Kaur G, et al. The immune checkpoint protein pd-L1 induces and maintains regulatory T cells in glioblastoma. Oncoimmunology (2018) 7(7):e1448329. doi: 10.1080/2162402x.2018.1448329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Wang LC, Wang YL, He B, Zheng YJ, Yu HC, Liu ZY, et al. Expression and clinical significance of vista, B7-H3, and pd-L1 in glioma. Clin Immunol (Orlando Fla) (2022) 245:109178. doi: 10.1016/j.clim.2022.109178 [DOI] [PubMed] [Google Scholar]
- 183. FranChina DG, Dostert C, Brenner D. Reactive oxygen species: involvement in T cell signaling and metabolism. Trends Immunol (2018) 39(6):489–502. doi: 10.1016/j.it.2018.01.005 [DOI] [PubMed] [Google Scholar]
- 184. Malmberg KJ, Arulampalam V, Ichihara F, Petersson M, Seki K, Andersson T, et al. Inhibition of activated/memory (Cd45ro(+)) T cells by oxidative stress associated with block of nf-kappab activation. J Immunol (Baltimore Md: 1950) (2001) 167(5):2595–601. doi: 10.4049/jimmunol.167.5.2595 [DOI] [PubMed] [Google Scholar]
- 185. Cemerski S, Cantagrel A, Van Meerwijk JP, Romagnoli P. Reactive oxygen species differentially affect T cell receptor-signaling pathways. J Biol Chem (2002) 277(22):19585–93. doi: 10.1074/jbc.M111451200 [DOI] [PubMed] [Google Scholar]
- 186. Wang YG, Long J, Shao DC, Song H. Hyperbaric oxygen inhibits production of cd3+ T cells in the thymus and facilitates malignant glioma cell growth. J Int Med Res (2018) 46(7):2780–91. doi: 10.1177/0300060518767796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Hao L, Marshall AJ, Liu L. Bam32/dapp1-dependent neutrophil reactive oxygen species in wkymvm-induced microvascular hyperpermeability. Front Immunol (2020) 11:1028. doi: 10.3389/fimmu.2020.01028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Summers C, Rankin SM, Condliffe AM, Singh N, Peters AM, Chilvers ER. Neutrophil kinetics in health and disease. Trends Immunol (2010) 31(8):318–24. doi: 10.1016/j.it.2010.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Stegelmeier AA, Chan L, Mehrani Y, Petrik JJ, Wootton SK, Bridle B, et al. Characterization of the impact of oncolytic vesicular stomatitis virus on the trafficking, phenotype, and antigen presentation potential of neutrophils and their ability to acquire a non-structural viral protein. Int J Mol Sci (2020) 21(17):6347. doi: 10.3390/ijms21176347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Qi X, Yu Y, Sun R, Huang J, Liu L, Yang Y, et al. Identification and characterization of neutrophil heterogeneity in sepsis. Crit Care (London England) (2021) 25(1):50. doi: 10.1186/s13054-021-03481-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and inflammation. Nat Rev Immunol (2013) 13(3):159–75. doi: 10.1038/nri3399 [DOI] [PubMed] [Google Scholar]
- 192. Chang Y, Syahirah R, Wang X, Jin G, Torregrosa-Allen S, Elzey BD, et al. Engineering chimeric antigen receptor neutrophils from human pluripotent stem cells for targeted cancer immunotherapy. Cell Rep (2022) 40(3):111128. doi: 10.1016/j.celrep.2022.111128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Sionov RV, Fainsod-Levi T, Zelter T, Polyansky L, Pham CT, Granot Z. Neutrophil cathepsin G and tumor cell rage facilitate neutrophil anti-tumor cytotoxicity. Oncoimmunology (2019) 8(9):e1624129. doi: 10.1080/2162402x.2019.1624129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Masucci MT, Minopoli M, Carriero MV. Tumor associated neutrophils. Their role in tumorigenesis, metastasis, prognosis and therapy. Front Oncol (2019) 9:1146. doi: 10.3389/fonc.2019.01146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Szczerba BM, Castro-Giner F, Vetter M, Krol I, Gkountela S, Landin J, et al. Neutrophils escort circulating tumour cells to enable cell cycle progression. Nature (2019) 566(7745):553–7. doi: 10.1038/s41586-019-0915-y [DOI] [PubMed] [Google Scholar]
- 196. Cools-Lartigue J, Spicer J, McDonald B, Gowing S, Chow S, Giannias B, et al. Neutrophil extracellular traps sequester circulating tumor cells and promote metastasis. J Clin Invest (2013) 123(8):3446–58. doi: 10.1172/jci67484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al. Neutrophil extracellular traps kill bacteria. Sci (New York NY) (2004) 303(5663):1532–5. doi: 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- 198. Rahbar A, Cederarv M, Wolmer-Solberg N, Tammik C, Stragliotto G, Peredo I, et al. Enhanced neutrophil activity is associated with shorter time to tumor progression in glioblastoma patients. Oncoimmunology (2016) 5(2):e1075693. doi: 10.1080/2162402x.2015.1075693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Iwatsuki K, Kumara E, Yoshimine T, Nakagawa H, Sato M, Hayakawa T. Elastase expression by infiltrating neutrophils in gliomas. Neurological Res (2000) 22(5):465–8. doi: 10.1080/01616412.2000.11740701 [DOI] [PubMed] [Google Scholar]
- 200. Liang J, Piao Y, Holmes L, Fuller GN, Henry V, Tiao N, et al. Neutrophils promote the Malignant glioma phenotype through S100a4. Clin Cancer Res (2014) 20(1):187–98. doi: 10.1158/1078-0432.Ccr-13-1279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Chow KH, Park HJ, George J, Yamamoto K, Gallup AD, Graber JH, et al. S100a4 is a biomarker and regulator of glioma stem cells that is critical for mesenchymal transition in glioblastoma. Cancer Res (2017) 77(19):5360–73. doi: 10.1158/0008-5472.Can-17-1294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell death program leads to neutrophil extracellular traps. J Cell Biol (2007) 176(2):231–41. doi: 10.1083/jcb.200606027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Lv X, Liu Z, Xu L, Song E, Song Y. Tetrachlorobenzoquinone exhibits immunotoxicity by inducing neutrophil extracellular traps through a mechanism involving ros-jnk-nox2 positive feedback loop. Environ pollut (Barking Essex: 1987) (2021) 268(Pt B):115921. doi: 10.1016/j.envpol.2020.115921 [DOI] [PubMed] [Google Scholar]
- 204. Keshari RS, Verma A, Barthwal MK, Dikshit M. Reactive oxygen species-induced activation of erk and P38 mapk mediates pma-induced nets release from human neutrophils. J Cell Biochem (2013) 114(3):532–40. doi: 10.1002/jcb.24391 [DOI] [PubMed] [Google Scholar]
- 205. Yee PP, Wei Y, Kim SY, Lu T, Chih SY, Lawson C, et al. Neutrophil-induced ferroptosis promotes tumor necrosis in glioblastoma progression. Nat Commun (2020) 11(1):5424. doi: 10.1038/s41467-020-19193-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Kurotaki D, Kawase W, Sasaki H, Nakabayashi J, Nishiyama A, Morse HC, 3rd, et al. Epigenetic control of early dendritic cell lineage specification by the transcription factor irf8 in mice. Blood (2019) 133(17):1803–13. doi: 10.1182/blood-2018-06-857789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Dudek AM, Martin S, Garg AD, Agostinis P. Immature, semi-mature, and fully mature dendritic cells: toward a dc-cancer cells interface that augments anticancer immunity. Front Immunol (2013) 4:438. doi: 10.3389/fimmu.2013.00438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Demaria O, Cornen S, Daëron M, Morel Y, Medzhitov R, Vivier E. Harnessing innate immunity in cancer therapy. Nature (2019) 574(7776):45–56. doi: 10.1038/s41586-019-1593-5 [DOI] [PubMed] [Google Scholar]
- 209. Zhang S, Zeng Z, Liu Y, Huang J, Long J, Wang Y, et al. Prognostic landscape of tumor-infiltrating immune cells and immune-related genes in the tumor microenvironment of gastric cancer. Aging (2020) 12(18):17958–75. doi: 10.18632/aging.103519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Han JA, Kang YJ, Shin C, Ra JS, Shin HH, Hong SY, et al. Ferritin protein cage nanoparticles as versatile antigen delivery nanoplatforms for dendritic cell (Dc)-based vaccine development. Nanomed: Nanotechnol Biol Med (2014) 10(3):561–9. doi: 10.1016/j.nano.2013.11.003 [DOI] [PubMed] [Google Scholar]
- 211. Cooper MA, Fehniger TA, Fuchs A, Colonna M, Caligiuri MA. Nk cell and dc interactions. Trends Immunol (2004) 25(1):47–52. doi: 10.1016/j.it.2003.10.012 [DOI] [PubMed] [Google Scholar]
- 212. Kim JW, Kane JR, Panek WK, Young JS, Rashidi A, Yu D, et al. A dendritic cell-targeted adenoviral vector facilitates adaptive immune response against human glioma antigen (Cmv-ie) and prolongs survival in a human glioma tumor model. Neurotherapeutics: J Am Soc Exp Neurother (2018) 15(4):1127–38. doi: 10.1007/s13311-018-0650-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Liu B, Ji Q, Cheng Y, Liu M, Zhang B, Mei Q, et al. Biomimetic gbm-targeted drug delivery system boosting ferroptosis for immunotherapy of orthotopic drug-resistant gbm. J Nanobiotechnol (2022) 20(1):161. doi: 10.1186/s12951-022-01360-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. He M, Chen X, Luo M, Ouyang L, Xie L, Huang Z, et al. Suppressor of cytokine signaling 1 inhibits the maturation of dendritic cells involving the nuclear factor kappa B signaling pathway in the glioma microenvironment. Clin Exp Immunol (2020) 202(1):47–59. doi: 10.1111/cei.13476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Kober C, Rohn S, Weibel S, Geissinger U, Chen NG, Szalay AA. Microglia and astrocytes attenuate the replication of the oncolytic vaccinia virus livp 1.1.1 in murine gl261 gliomas by acting as vaccinia virus traps. J Trans Med (2015) 13:216. doi: 10.1186/s12967-015-0586-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Ugele I, Cárdenas-Conejo ZE, Hammon K, Wehrstein M, Bruss C, Peter K, et al. D-2-hydroxyglutarate and L-2-hydroxyglutarate inhibit il-12 secretion by human monocyte-derived dendritic cells. Int J Mol Sci (2019) 20(3):742. doi: 10.3390/ijms20030742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Wang J, Liu P, Xin S, Wang Z, Li J. Nrf2 suppresses the function of dendritic cells to facilitate the immune escape of glioma cells. Exp Cell Res (2017) 360(2):66–73. doi: 10.1016/j.yexcr.2017.07.031 [DOI] [PubMed] [Google Scholar]
- 218. Laskowski TJ, Biederstädt A, Rezvani K. Natural killer cells in antitumour adoptive cell immunotherapy. Nat Rev Cancer (2022) 22(10):557–75. doi: 10.1038/s41568-022-00491-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Gillgrass A, Ashkar A. Stimulating natural killer cells to protect against cancer: recent developments. Expert Rev Clin Immunol (2011) 7(3):367–82. doi: 10.1586/eci.10.102 [DOI] [PubMed] [Google Scholar]
- 220. Campbell KS, Hasegawa J. Natural killer cell biology: an update and future directions. J Allergy Clin Immunol (2013) 132(3):536–44. doi: 10.1016/j.jaci.2013.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Costa VV, Ye W, Chen Q, Teixeira MM, Preiser P, Ooi EE, et al. Dengue Virus-Infected Dendritic Cells, but Not Monocytes, Activate Natural Killer Cells through a Contact-Dependent Mechanism Involving Adhesion Molecules. mBio (2017) 8(4):e00741–17. doi: 10.1128/mBio.00741-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222. Vantourout P, Willcox C, Turner A, Swanson CM, Haque Y, Sobolev O, et al. Immunological visibility: posttranscriptional regulation of human nkg2d ligands by the egf receptor pathway. Sci Trans Med (2014) 6(231):231ra49. doi: 10.1126/scitranslmed.3007579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Screpanti V, Wallin RP, Grandien A, Ljunggren HG. Impact of fasl-induced apoptosis in the elimination of tumor cells by nk cells. Mol Immunol (2005) 42(4):495–9. doi: 10.1016/j.molimm.2004.07.033 [DOI] [PubMed] [Google Scholar]
- 224. Antosova Z, Podzimkova N, Tomala J, Augustynkova K, Sajnerova K, Nedvedova E, et al. Sot101 induces nk cell cytotoxicity and potentiates antibody-dependent cell cytotoxicity and anti-tumor activity. Front Immunol (2022) 13:989895. doi: 10.3389/fimmu.2022.989895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Zhao J, Schlößer HA, Wang Z, Qin J, Li J, Popp F, et al. Tumor-derived extracellular vesicles inhibit natural killer cell function in pancreatic cancer. Cancers (2019) 11(6):874. doi: 10.3390/cancers11060874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Hayakawa Y, Takeda K, Yagita H, Smyth MJ, Van Kaer L, Okumura K, et al. Ifn-gamma-mediated inhibition of tumor angiogenesis by natural killer T-cell ligand, alpha-galactosylceramide. Blood (2002) 100(5):1728–33. doi: 10.1182/blood-2002-03-0789 [DOI] [PubMed] [Google Scholar]
- 227. Shah D, Comba A, Faisal SM, Kadiyala P, Baker GJ, Alghamri MS, et al. A novel mir1983-tlr7-ifnβ Circuit licenses nk cells to kill glioma cells, and is under the control of galectin-1. Oncoimmunology (2021) 10(1):1939601. doi: 10.1080/2162402x.2021.1939601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Huang L, Zhu P, Xia P, Fan Z. Wash has a critical role in nk cell cytotoxicity through lck-mediated phosphorylation. Cell Death Dis (2016) 7(7):e2301. doi: 10.1038/cddis.2016.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229. Shida Y, Nakazawa T, Matsuda R, Morimoto T, Nishimura F, Nakamura M, et al. Ex vivo expanded and activated natural killer cells prolong the overall survival of mice with glioblastoma-like cell-derived tumors. Int J Mol Sci (2021) 22(18):9975. doi: 10.3390/ijms22189975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Crane CA, Han SJ, Barry JJ, Ahn BJ, Lanier LL, Parsa AT. Tgf-beta downregulates the activating receptor nkg2d on nk cells and cd8+ T cells in glioma patients. Neuro-oncology (2010) 12(1):7–13. doi: 10.1093/neuonc/nop009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Humblet Y. Cetuximab: an igg(1) monoclonal antibody for the treatment of epidermal growth factor receptor-expressing tumours. Expert Opin Pharmacother (2004) 5(7):1621–33. doi: 10.1517/14656566.5.7.1621 [DOI] [PubMed] [Google Scholar]
- 232. Avril T, Vauleon E, Hamlat A, Saikali S, Etcheverry A, Delmas C, et al. Human glioblastoma stem-like cells are more sensitive to allogeneic nk and T cell-mediated killing compared with serum-cultured glioblastoma cells. Brain Pathol (Zurich Switzerland) (2012) 22(2):159–74. doi: 10.1111/j.1750-3639.2011.00515.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Whiteside TL. Nk cells in the tumor microenvironment and thioredoxin activity. J Clin Invest (2020) 130(10):5115–7. doi: 10.1172/jci141460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Nakamura K, Matsunaga K. Susceptibility of natural killer (Nk) cells to reactive oxygen species (Ros) and their restoration by the mimics of superoxide dismutase (Sod). Cancer Biother Radiopharmaceuticals (1998) 13(4):275–90. doi: 10.1089/cbr.1998.13.275 [DOI] [PubMed] [Google Scholar]
- 235. Werlenius O, Aurelius J, Hallner A, Akhiani AA, Simpanen M, Martner A, et al. Reactive oxygen species induced by therapeutic cd20 antibodies inhibit natural killer cell-mediated antibody-dependent cellular cytotoxicity against primary cll cells. Oncotarget (2016) 7(22):32046–53. doi: 10.18632/oncotarget.8769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Wang J, Yi J. Cancer cell killing via ros: to increase or decrease, that is the question. Cancer Biol Ther (2008) 7(12):1875–84. doi: 10.4161/cbt.7.12.7067 [DOI] [PubMed] [Google Scholar]
- 237. Sosa V, Moliné T, Somoza R, Paciucci R, Kondoh H, ME LL. Oxidative stress and cancer: an overview. Ageing Res Rev (2013) 12(1):376–90. doi: 10.1016/j.arr.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 238. Liu Y, Wang X, Zhu W, Sui Z, Wei X, Zhang Y, et al. Trpml1-induced autophagy inhibition triggers mitochondrial mediated apoptosis. Cancer Lett (2022) 541:215752. doi: 10.1016/j.canlet.2022.215752 [DOI] [PubMed] [Google Scholar]
- 239. Miao Z, Tian W, Ye Y, Gu W, Bao Z, Xu L, et al. Hsp90 induces acsl4-dependent glioma ferroptosis via dephosphorylating ser637 at drp1. Cell Death Dis (2022) 13(6):548. doi: 10.1038/s41419-022-04997-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Ji CC, Hu YY, Cheng G, Liang L, Gao B, Ren YP, et al. A ketogenic diet attenuates proliferation and stemness of glioma stem−Like cells by altering metabolism resulting in increased ros production. Int J Oncol (2020) 56(2):606–17. doi: 10.3892/ijo.2019.4942 [DOI] [PubMed] [Google Scholar]
- 241. García-Gómez P, Golán I, Dadras MS, Mezheyeuski A, Bellomo C, Tzavlaki K, et al. Nox4 regulates tgfβ-induced proliferation and self-renewal in glioblastoma stem cells. Mol Oncol (2022) 16(9):1891–912. doi: 10.1002/1878-0261.13200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Iranmanesh Y, Jiang B, Favour OC, Dou Z, Wu J, Li J, et al. Mitochondria’s role in the maintenance of cancer stem cells in glioblastoma. Front Oncol (2021) 11:582694. doi: 10.3389/fonc.2021.582694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Yuan S, Lu Y, Yang J, Chen G, Kim S, Feng L, et al. Metabolic activation of mitochondria in glioma stem cells promotes cancer development through a reactive oxygen species-mediated mechanism. Stem Cell Res Ther (2015) 6:198. doi: 10.1186/s13287-015-0174-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Tavender TJ, Bulleid NJ. Peroxiredoxin iv protects cells from oxidative stress by removing H2o2 produced during disulphide formation. J Cell Sci (2010) 123(Pt 15):2672–9. doi: 10.1242/jcs.067843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Vallejo FA, Vanni S, Graham RM. Ucp2 as a potential biomarker for adjunctive metabolic therapies in tumor management. Front Oncol (2021) 11:640720. doi: 10.3389/fonc.2021.640720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Lu J, Tan M, Cai Q. The warburg effect in tumor progression: mitochondrial oxidative metabolism as an anti-metastasis mechanism. Cancer Lett (2015) 356(2 Pt A):156–64. doi: 10.1016/j.canlet.2014.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Hyun DH. Insights into the New Cancer Therapy through Redox Homeostasis and Metabolic Shifts. Cancers (2020) 12(7):1822. doi: 10.3390/cancers12071822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Li P, Wu M, Wang J, Sui Y, Liu S, Shi D. Nac selectively inhibit cancer telomerase activity: A higher redox homeostasis threshold exists in cancer cells. Redox Biol (2016) 8:91–7. doi: 10.1016/j.redox.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Zucker SN, Fink EE, Bagati A, Mannava S, Bianchi-Smiraglia A, Bogner PN, et al. Nrf2 amplifies oxidative stress via induction of klf9. Mol Cell (2014) 53(6):916–28. doi: 10.1016/j.molcel.2014.01.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Wang YF, Hu JY. Natural and synthetic compounds for glioma treatment based on ros-mediated strategy. Eur J Pharmacol (2023) 953:175537. doi: 10.1016/j.ejphar.2023.175537 [DOI] [PubMed] [Google Scholar]
- 251. Bhanja D, Wilding H, Baroz A, Trifoi M, Shenoy G, Slagle-Webb B, et al. Photodynamic therapy for glioblastoma: illuminating the path toward clinical applicability. Cancers (2023) 15(13):3427. doi: 10.3390/cancers15133427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Wan Q, Zou C, Hu D, Zhou J, Chen M, Tie C, et al. Imaging-guided focused ultrasound-induced thermal and sonodynamic effects of nanosonosensitizers for synergistic enhancement of glioblastoma therapy. Biomater Sci (2019) 7(7):3007–15. doi: 10.1039/c9bm00292h [DOI] [PubMed] [Google Scholar]
- 253. Zheng T, Wang W, Ashley J, Zhang M, Feng X, Shen J, et al. Self-assembly protein superstructures as a powerful chemodynamic therapy nanoagent for glioblastoma treatment. Nano-micro Lett (2020) 12(1):151. doi: 10.1007/s40820-020-00490-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Kwiatkowski S, Knap B, Przystupski D, Saczko J, Kędzierska E, Knap-Czop K, et al. Photodynamic therapy - mechanisms, photosensitizers and combinations. Biomed Pharmacother = Biomed Pharmacotherapie (2018) 106:1098–107. doi: 10.1016/j.biopha.2018.07.049 [DOI] [PubMed] [Google Scholar]
- 255. Yu Y, Jia H, Liu Y, Zhang L, Feng G, Tang BZ. Recent progress in type I aggregation-induced emission photosensitizers for photodynamic therapy. Mol (Basel Switzerland) (2022) 28(1):332. doi: 10.3390/molecules28010332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Semyachkina-Glushkovskaya O, Kurths J, Borisova E, Sokolovski S, Mantareva V, Angelov I, et al. Photodynamic opening of blood-brain barrier. Biomed Optics Express (2017) 8(11):5040–8. doi: 10.1364/boe.8.005040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Verger A, Brandhonneur N, Molard Y, Cordier S, Kowouvi K, Amela-Cortes M, et al. From molecules to nanovectors: current state of the art and applications of photosensitizers in photodynamic therapy. Int J Pharmaceutics (2021) 604:120763. doi: 10.1016/j.ijpharm.2021.120763 [DOI] [PubMed] [Google Scholar]
- 258. Mahmoudi K, Garvey KL, Bouras A, Cramer G, Stepp H, Jesu Raj JG, et al. 5-aminolevulinic acid photodynamic therapy for the treatment of high-grade gliomas. J neuro-oncol (2019) 141(3):595–607. doi: 10.1007/s11060-019-03103-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Rosenthal MA, Kavar B, Hill JS, Morgan DJ, Nation RL, Stylli SS, et al. Phase I and pharmacokinetic study of photodynamic therapy for high-grade gliomas using a novel boronated porphyrin. J Clin Oncol (2001) 19(2):519–24. doi: 10.1200/jco.2001.19.2.519 [DOI] [PubMed] [Google Scholar]
- 260. Shimizu K, Nitta M, Komori T, Maruyama T, Yasuda T, Fujii Y, et al. Intraoperative photodynamic diagnosis using talaporfin sodium simultaneously applied for photodynamic therapy against Malignant glioma: A prospective clinical study. Front Neurol (2018) 9:24. doi: 10.3389/fneur.2018.00024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Mannino S, Molinari A, Sabatino G, Ciafrè SA, Colone M, Maira G, et al. Intratumoral vs systemic administration of meta-tetrahydroxyphenylchlorin for photodynamic therapy of malignant gliomas: assessment of uptake and spatial distribution in C6 rat glioma model. Int J Immunopathol Pharmacol (2008) 21(1):227–31. doi: 10.1177/039463200802100126 [DOI] [PubMed] [Google Scholar]
- 262. Donohoe C, Senge MO, Arnaut LG, Gomes-da-Silva LC. Cell death in photodynamic therapy: from oxidative stress to anti-tumor immunity. Biochim Biophys Acta Rev Cancer (2019) 1872(2):188308. doi: 10.1016/j.bbcan.2019.07.003 [DOI] [PubMed] [Google Scholar]
- 263. Chilakamarthi U, Giribabu L. Photodynamic therapy: past, present and future. Chem Rec (New York NY) (2017) 17(8):775–802. doi: 10.1002/tcr.201600121 [DOI] [PubMed] [Google Scholar]
- 264. Alzeibak R, Mishchenko TA, Shilyagina NY, Balalaeva IV, Vedunova MV, Krysko DV. Targeting immunogenic cancer cell death by photodynamic therapy: past, present and future. J Immunother Cancer (2021) 9(1):e001926. doi: 10.1136/jitc-2020-001926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Kawase Y, Iseki H. Parameter-finding studies of photodynamic therapy for approval in Japan and the USA. Photodiagnosis Photodyn Ther (2013) 10(4):434–45. doi: 10.1016/j.pdpdt.2013.03.001 [DOI] [PubMed] [Google Scholar]
- 266. Kessel D. Photodynamic therapy: A brief history. J Clin Med (2019) 8(10):1581. doi: 10.3390/jcm8101581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Champeau M, Vignoud S, Mortier L, Mordon S. Photodynamic therapy for skin cancer: how to enhance drug penetration? J Photochem Photobiol B Biol (2019) 197:111544. doi: 10.1016/j.jphotobiol.2019.111544 [DOI] [PubMed] [Google Scholar]
- 268. Kostron H, Swartz MR, Martuza RL. Photodynamic therapy is potentiated by co60 and intratumoral injection of hematoporphyrin derivative. J neuro-oncol (1988) 6(2):185–91. doi: 10.1007/bf02327395 [DOI] [PubMed] [Google Scholar]
- 269. Wilson BC, Muller PJ, Yanch JC. Instrumentation and light dosimetry for intra-operative photodynamic therapy (Pdt) of Malignant brain tumours. Phys Med Biol (1986) 31(2):125–33. doi: 10.1088/0031-9155/31/2/002 [DOI] [PubMed] [Google Scholar]
- 270. Turubanova VD, Balalaeva IV, Mishchenko TA, Catanzaro E, Alzeibak R, Peskova NN, et al. Immunogenic cell death induced by a new photodynamic therapy based on photosens and photodithazine. J Immunother Cancer (2019) 7(1):350. doi: 10.1186/s40425-019-0826-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Omura N, Nonoguchi N, Fujishiro T, Park Y, Ikeda N, Kajimoto Y, et al. Ablation efficacy of 5-aminolevulinic acid-mediated photodynamic therapy on human glioma stem cells. Photodiagnosis Photodyn Ther (2023) 41:103119. doi: 10.1016/j.pdpdt.2022.103119 [DOI] [PubMed] [Google Scholar]
- 272. Zhang X, Guo M, Shen L, Hu S. Combination of photodynamic therapy and temozolomide on glioma in a rat C6 glioma model. Photodiagnosis Photodyn Ther (2014) 11(4):603–12. doi: 10.1016/j.pdpdt.2014.10.007 [DOI] [PubMed] [Google Scholar]
- 273. Cheng K, Guo Q, Shen Z, Yang W, Wang Y, Sun Z, et al. Bibliometric analysis of global research on cancer photodynamic therapy: focus on nano-related research. Front Pharmacol (2022) 13:927219. doi: 10.3389/fphar.2022.927219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Vanaclocha V, Sureda M, Azinovic I, Rebollo J, Cañón R, Sapena NS, et al. Photodynamic therapy in the treatment of brain tumours. A feasibility study. Photodiagnosis Photodyn Ther (2015) 12(3):422–7. doi: 10.1016/j.pdpdt.2015.05.007 [DOI] [PubMed] [Google Scholar]
- 275. Wang X, Wu M, Li H, Jiang J, Zhou S, Chen W, et al. Enhancing penetration ability of semiconducting polymer nanoparticles for sonodynamic therapy of large solid tumor. Advanced Sci (Weinheim Baden-Wurttemberg Germany) (2022) 9(6):e2104125. doi: 10.1002/advs.202104125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Vermandel M, Dupont C, Lecomte F, Leroy HA, Tuleasca C, Mordon S, et al. Standardized intraoperative 5-ala photodynamic therapy for newly diagnosed glioblastoma patients: A preliminary analysis of the indygo clinical trial. J neuro-oncol (2021) 152(3):501–14. doi: 10.1007/s11060-021-03718-6 [DOI] [PubMed] [Google Scholar]
- 277. Wei X, Song M, Jiang G, Liang M, Chen C, Yang Z, et al. Progress in advanced nanotherapeutics for enhanced photodynamic immunotherapy of tumor. Theranostics (2022) 12(12):5272–98. doi: 10.7150/thno.73566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278. Maeding N, Verwanger T, Krammer B. Boosting tumor-specific immunity using pdt. Cancers (2016) 8(10):91. doi: 10.3390/cancers8100091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279. Li D, Chen F, Cheng C, Li H, Wei X. Biodegradable materials with disulfide-bridged-framework confine photosensitizers for enhanced photo-immunotherapy. Int J Nanomed (2021) 16:8323–34. doi: 10.2147/ijn.S344679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Ahmed A, Tait SWG. Targeting immunogenic cell death in cancer. Mol Oncol (2020) 14(12):2994–3006. doi: 10.1002/1878-0261.12851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Mishchenko T, Balalaeva I, Gorokhova A, Vedunova M, Krysko DV. Which cell death modality wins the contest for photodynamic therapy of cancer? Cell Death Dis (2022) 13(5):455. doi: 10.1038/s41419-022-04851-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Lan M, Zhao S, Liu W, Lee CS, Zhang W, Wang P. Photosensitizers for photodynamic therapy. Advanced Healthc Mater (2019) 8(13):e1900132. doi: 10.1002/adhm.201900132 [DOI] [PubMed] [Google Scholar]
- 283. Hu T, Wang Z, Shen W, Liang R, Yan D, Wei M. Recent advances in innovative strategies for enhanced cancer photodynamic therapy. Theranostics (2021) 11(7):3278–300. doi: 10.7150/thno.54227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Wang C, Chen X, Wu J, Liu H, Ji Z, Shi H, et al. Low-dose arsenic trioxide enhances 5-aminolevulinic acid-induced ppix accumulation and efficacy of photodynamic therapy in human glioma. J Photochem Photobiol B Biol (2013) 127:61–7. doi: 10.1016/j.jphotobiol.2013.06.001 [DOI] [PubMed] [Google Scholar]
- 285. Coupienne I, Bontems S, Dewaele M, Rubio N, Habraken Y, Fulda S, et al. Nf-kappab inhibition improves the sensitivity of human glioblastoma cells to 5-aminolevulinic acid-based photodynamic therapy. Biochem Pharmacol (2011) 81(5):606–16. doi: 10.1016/j.bcp.2010.12.015 [DOI] [PubMed] [Google Scholar]
- 286. Tetard MC, Vermandel M, Leroy HA, Leroux B, Maurage CA, Lejeune JP, et al. Interstitial 5-ala photodynamic therapy and glioblastoma: preclinical model development and preliminary results. Photodiagnosis Photodyn Ther (2016) 13:218–24. doi: 10.1016/j.pdpdt.2015.07.169 [DOI] [PubMed] [Google Scholar]
- 287. Miki Y, Akimoto J, Moritake K, Hironaka C, Fujiwara Y. Photodynamic therapy using talaporfin sodium induces concentration-dependent programmed necroptosis in human glioblastoma T98g cells. Lasers Med Sci (2015) 30(6):1739–45. doi: 10.1007/s10103-015-1783-9 [DOI] [PubMed] [Google Scholar]
- 288. Correia JH, Rodrigues JA, Pimenta S, Dong T, Yang Z. Photodynamic therapy review: principles, photosensitizers, applications, and future directions. Pharmaceutics (2021) 13(9):1332. doi: 10.3390/pharmaceutics13091332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Miyoshi N, Misík V, Fukuda M, Riesz P. Effect of gallium-porphyrin analogue atx-70 on nitroxide formation from a cyclic secondary amine by ultrasound: on the mechanism of sonodynamic activation. Radiat Res (1995) 143(2):194–202. doi: 10.2307/3579157 [DOI] [PubMed] [Google Scholar]
- 290. Miyoshi N, Misík V, Riesz P. Sonodynamic toxicity of gallium-porphyrin analogue atx-70 in human leukemia cells. Radiat Res (1997) 148(1):43–7. doi: 10.2307/3579537 [DOI] [PubMed] [Google Scholar]
- 291. Wu Z, Cheng K, Shen Z, Lu Y, Wang H, Wang G, et al. Mapping knowledge landscapes and emerging trends of sonodynamic therapy: A bibliometric and visualized study. Front Pharmacol (2022) 13:1048211. doi: 10.3389/fphar.2022.1048211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292. Lin X, Song J, Chen X, Yang H. Ultrasound-activated sensitizers and applications. Angewandte Chemie (International ed English) (2020) 59(34):14212–33. doi: 10.1002/anie.201906823 [DOI] [PubMed] [Google Scholar]
- 293. Wang F, Xu L, Wen B, Song S, Zhou Y, Wu H, et al. Ultrasound-excited temozolomide sonosensitization induces necroptosis in glioblastoma. Cancer Lett (2023) 554:216033. doi: 10.1016/j.canlet.2022.216033 [DOI] [PubMed] [Google Scholar]
- 294. Wan G, Chen X, Wang H, Hou S, Wang Q, Cheng Y, et al. Gene augmented nuclear-targeting sonodynamic therapy via nrf2 pathway-based redox balance adjustment boosts peptide-based anti-pd-L1 therapy on colorectal cancer. J Nanobiotechnol (2021) 19(1):347. doi: 10.1186/s12951-021-01094-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295. Geng X, Chen Y, Chen Z, Wei X, Dai Y, Yuan Z. Oxygen-carrying biomimetic nanoplatform for sonodynamic killing of bacteria and treatment of infection diseases. Ultrasonics sonochemistry (2022) 84:105972. doi: 10.1016/j.ultsonch.2022.105972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Tung CH, Han MS, Kim Y, Qi J, O’Neill BE. Tumor ablation using low-intensity ultrasound and sound excitable drug. J Controlled Release: Off J Controlled Release Soc (2017) 258:67–72. doi: 10.1016/j.jconrel.2017.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297. Guo QL, Dai XL, Yin MY, Cheng HW, Qian HS, Wang H, et al. Nanosensitizers for sonodynamic therapy for glioblastoma multiforme: current progress and future perspectives. Military Med Res (2022) 9(1):26. doi: 10.1186/s40779-022-00386-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298. Bunevicius A, Pikis S, Padilla F, Prada F, Sheehan J. Sonodynamic therapy for gliomas. J neuro-oncol (2022) 156(1):1–10. doi: 10.1007/s11060-021-03807-6 [DOI] [PubMed] [Google Scholar]
- 299. Song D, Yue W, Li Z, Li J, Zhao J, Zhang N. Study of the mechanism of sonodynamic therapy in a rat glioma model. OncoTargets Ther (2014) 7:1801–10. doi: 10.2147/ott.S52426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Zhang C, Bu W, Ni D, Zhang S, Li Q, Yao Z, et al. Synthesis of iron nanometallic glasses and their application in cancer therapy by a localized fenton reaction. Angewandte Chemie (International ed English) (2016) 55(6):2101–6. doi: 10.1002/anie.201510031 [DOI] [PubMed] [Google Scholar]
- 301. Jia C, Guo Y, Wu FG. Chemodynamic therapy via fenton and fenton-like nanomaterials: strategies and recent advances. Small (Weinheim an der Bergstrasse Germany) (2022) 18(6):e2103868. doi: 10.1002/smll.202103868 [DOI] [PubMed] [Google Scholar]
- 302. Qian X, Zhang J, Gu Z, Chen Y. Nanocatalysts-augmented fenton chemical reaction for nanocatalytic tumor therapy. Biomaterials (2019) 211:1–13. doi: 10.1016/j.biomaterials.2019.04.023 [DOI] [PubMed] [Google Scholar]
- 303. Ma W, Zhang H, Li S, Wang Z, Wu X, Yan R, et al. A multifunctional nanoplatform based on fenton-like and russell reactions of cu, mn bimetallic ions synergistically enhanced ros stress for improved chemodynamic therapy. ACS Biomater Sci Eng (2022) 8(3):1354–66. doi: 10.1021/acsbiomaterials.1c01605 [DOI] [PubMed] [Google Scholar]
- 304. Li Y, Sun J, Sun SP. Mn(2+)-mediated homogeneous fenton-like reaction of fe(Iii)-nta complex for efficient degradation of organic contaminants under neutral conditions. J Hazard Mater (2016) 313:193–200. doi: 10.1016/j.jhazmat.2016.04.003 [DOI] [PubMed] [Google Scholar]
- 305. Qiao L, Yang H, Shao XX, Yin Q, Fu XJ, Wei Q. Research progress on nanoplatforms and nanotherapeutic strategies in treating glioma. Mol Pharmaceutics (2022) 19(7):1927–51. doi: 10.1021/acs.molpharmaceut.1c00856 [DOI] [PubMed] [Google Scholar]
- 306. Cao X, Li S, Chen W, Lu H, Ye L, Min Z, et al. Multifunctional hybrid hydrogel system enhanced the therapeutic efficacy of treatments for postoperative glioma. ACS Appl Mater Interfaces (2022) 14(24):27623–33. doi: 10.1021/acsami.2c05147 [DOI] [PubMed] [Google Scholar]
- 307. Cao Y, Jin L, Zhang S, Lv Z, Yin N, Zhang H, et al. Blood-brain barrier permeable and multi-stimuli responsive nanoplatform for orthotopic glioma inhibition by synergistic enhanced chemo-/chemodynamic/photothermal/starvation therapy. Eur J Pharm Sci (2023) 180:106319. doi: 10.1016/j.ejps.2022.106319 [DOI] [PubMed] [Google Scholar]
- 308. Abbott NJ, Rönnbäck L, Hansson E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci (2006) 7(1):41–53. doi: 10.1038/nrn1824 [DOI] [PubMed] [Google Scholar]
- 309. Langen UH, Ayloo S, Gu C. Development and cell biology of the blood-brain barrier. Annu Rev Cell Dev Biol (2019) 35:591–613. doi: 10.1146/annurev-cellbio-100617-062608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310. Daneman R, Prat A. The blood-brain barrier. Cold Spring Harbor Perspect Biol (2015) 7(1):a020412. doi: 10.1101/cshperspect.a020412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Watkins S, Robel S, Kimbrough IF, Robert SM, Ellis-Davies G, Sontheimer H. Disruption of astrocyte-vascular coupling and the blood-brain barrier by invading glioma cells. Nat Commun (2014) 5:4196. doi: 10.1038/ncomms5196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Pacioni S, D’Alessandris QG, Buccarelli M, Boe A, Martini M, Larocca LM, et al. Brain invasion along perivascular spaces by glioma cells: relationship with blood-brain barrier. Cancers (2019) 12(1):18. doi: 10.3390/cancers12010018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Cui J, Wang X, Li J, Zhu A, Du Y, Zeng W, et al. Immune exosomes loading self-assembled nanomicelles traverse the blood-brain barrier for chemo-immunotherapy against glioblastoma. ACS Nano (2023) 17(2):1464–84. doi: 10.1021/acsnano.2c10219 [DOI] [PubMed] [Google Scholar]
- 314. Ting CY, Fan CH, Liu HL, Huang CY, Hsieh HY, Yen TC, et al. Concurrent blood-brain barrier opening and local drug delivery using drug-carrying microbubbles and focused ultrasound for brain glioma treatment. Biomaterials (2012) 33(2):704–12. doi: 10.1016/j.biomaterials.2011.09.096 [DOI] [PubMed] [Google Scholar]
- 315. Coluccia D, Figueiredo CA, Wu MY, Riemenschneider AN, Diaz R, Luck A, et al. Enhancing glioblastoma treatment using cisplatin-gold-nanoparticle conjugates and targeted delivery with magnetic resonance-guided focused ultrasound. Nanomed: Nanotechnol Biol Med (2018) 14(4):1137–48. doi: 10.1016/j.nano.2018.01.021 [DOI] [PubMed] [Google Scholar]
- 316. Zafar R, Zia KM, Tabasum S, Jabeen F, Noreen A, Zuber M. Polysaccharide based bionanocomposites, properties and applications: A review. Int J Biol Macromol (2016) 92:1012–24. doi: 10.1016/j.ijbiomac.2016.07.102 [DOI] [PubMed] [Google Scholar]
- 317. Pérez-Herrero E, Fernández-Medarde A. Advanced targeted therapies in cancer: drug nanocarriers, the future of chemotherapy. Eur J Pharmaceutics Biopharmaceutics (2015) 93:52–79. doi: 10.1016/j.ejpb.2015.03.018 [DOI] [PubMed] [Google Scholar]
- 318. Yetisgin AA, Cetinel S, Zuvin M, Kosar A, Kutlu O. Therapeutic nanoparticles and their targeted delivery applications. Mol (Basel Switzerland) (2020) 25(9):2193. doi: 10.3390/molecules25092193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319. Xu Q, Zhang H, Liu H, Han Y, Qiu W, Li Z. Inhibiting autophagy flux and DNA repair of tumor cells to boost radiotherapy of orthotopic glioblastoma. Biomaterials (2022) 280:121287. doi: 10.1016/j.biomaterials.2021.121287 [DOI] [PubMed] [Google Scholar]
- 320. Kang RH, Jang JE, Huh E, Kang SJ, Ahn DR, Kang JS, et al. A brain tumor-homing tetra-peptide delivers a nano-therapeutic for more effective treatment of a mouse model of glioblastoma. Nanoscale Horizons (2020) 5(8):1213–25. doi: 10.1039/d0nh00077a [DOI] [PubMed] [Google Scholar]
- 321. Qi L, Liu J, Zhu H, Li Z, Lu K, Li T, et al. Inhibition of glioma proliferation and migration by magnetic nanoparticle mediated jam-2 silencing. J Mater Chem B (2014) 2(41):7168–75. doi: 10.1039/c4tb00954a [DOI] [PubMed] [Google Scholar]
- 322. Teirlinck E, Barras A, Liu J, Fraire JC, Lajunen T, Xiong R, et al. Exploring light-sensitive nanocarriers for simultaneous triggered antibiotic release and disruption of biofilms upon generation of laser-induced vapor nanobubbles. Pharmaceutics (2019) 11(5):201. doi: 10.3390/pharmaceutics11050201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323. Chenthamara D, Subramaniam S, Ramakrishnan SG, Krishnaswamy S, Essa MM, Lin FH, et al. Therapeutic efficacy of nanoparticles and routes of administration. Biomater Res (2019) 23:20. doi: 10.1186/s40824-019-0166-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Jamali Z, Khoobi M, Hejazi SM, Eivazi N, Abdolahpour S, Imanparast F, et al. Evaluation of targeted curcumin (Cur) loaded plga nanoparticles for in vitro photodynamic therapy on human glioblastoma cell line. Photodiagnosis Photodyn Ther (2018) 23:190–201. doi: 10.1016/j.pdpdt.2018.06.026 [DOI] [PubMed] [Google Scholar]
- 325. Dube T, Kumar N, Bishnoi M, Panda JJ. Dual blood-brain barrier-glioma targeting peptide-poly(Levodopamine) hybrid nanoplatforms as potential near infrared phototheranostic agents in glioblastoma. Bioconjugate Chem (2021) 32(9):2014–31. doi: 10.1021/acs.bioconjchem.1c00321 [DOI] [PubMed] [Google Scholar]
- 326. Lee CH, Lai PS, Lu YP, Chen HY, Chai CY, Tsai RK, et al. Real-time vascular imaging and photodynamic therapy efficacy with micelle-nanocarrier delivery of chlorin E6 to the microenvironment of melanoma. J Dermatol Sci (2015) 80(2):124–32. doi: 10.1016/j.jdermsci.2015.08.005 [DOI] [PubMed] [Google Scholar]
- 327. Hu N, Li W, Hong Y, Zeng Z, Zhang J, Wu X, et al. A pd1 targeted nano-delivery system based on epigenetic alterations of T cell responses in the treatment of gastric cancer. Mol Ther Oncolytics (2022) 24:148–59. doi: 10.1016/j.omto.2021.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328. Zhao D, Liu N, Shi K, Wang X, Wu G. Preparation of a multifunctional verapamil-loaded nano-carrier based on a self-assembling pegylated prodrug. Colloids Surfaces B Biointerfaces (2015) 135:682–8. doi: 10.1016/j.colsurfb.2015.08.018 [DOI] [PubMed] [Google Scholar]
- 329. Yu T, Xu B, He L, Xia S, Chen Y, Zeng J, et al. Pigment epithelial-derived factor gene loaded novel cooh-peg-plga-cooh nanoparticles promoted tumor suppression by systemic administration. Int J Nanomed (2016) 11:743–59. doi: 10.2147/ijn.S97223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330. Kim HS, Lee DY. Nanomedicine in clinical photodynamic therapy for the treatment of brain tumors. Biomedicines (2022) 10(1):96. doi: 10.3390/biomedicines10010096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Sun Y, Wang H, Wang P, Zhang K, Geng X, Liu Q, et al. Tumor targeting dvdms-nanoliposomes for an enhanced sonodynamic therapy of gliomas. Biomater Sci (2019) 7(3):985–94. doi: 10.1039/c8bm01187g [DOI] [PubMed] [Google Scholar]
- 332. Lin L, Wang S, Deng H, Yang W, Rao L, Tian R, et al. Endogenous labile iron pool-mediated free radical generation for cancer chemodynamic therapy. J Am Chem Soc (2020) 142(36):15320–30. doi: 10.1021/jacs.0c05604 [DOI] [PubMed] [Google Scholar]
- 333. Cui Y, Xu Q, Chow PK, Wang D, Wang CH. Transferrin-conjugated magnetic silica plga nanoparticles loaded with doxorubicin and paclitaxel for brain glioma treatment. Biomaterials (2013) 34(33):8511–20. doi: 10.1016/j.biomaterials.2013.07.075 [DOI] [PubMed] [Google Scholar]
- 334. Zhu X, Zhou H, Liu Y, Wen Y, Wei C, Yu Q, et al. Transferrin/aptamer conjugated mesoporous ruthenium nanosystem for redox-controlled and targeted chemo-photodynamic therapy of glioma. Acta biomaterialia (2018) 82:143–57. doi: 10.1016/j.actbio.2018.10.012 [DOI] [PubMed] [Google Scholar]
- 335. Cai X, Wang M, Mu P, Jian T, Liu D, Ding S, et al. Sequence-defined nanotubes assembled from ir780-conjugated peptoids for chemophototherapy of malignant glioma. Res (Washington DC) (2021) 2021:9861384. doi: 10.34133/2021/9861384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Dube T, Kompella UB, Panda JJ. Near infrared triggered chemo-ptt-pdt effect mediated by glioma directed twin functional-chimeric peptide-decorated gold nanoroses. J Photochem Photobiol B Biol (2022) 228:112407. doi: 10.1016/j.jphotobiol.2022.112407 [DOI] [PubMed] [Google Scholar]
- 337. Gries M, Thomas N, Daouk J, Rocchi P, Choulier L, Jubréaux J, et al. Multiscale selectivity and in vivo biodistribution of nrp-1-targeted theranostic aguix nanoparticles for pdt of glioblastoma. Int J Nanomed (2020) 15:8739–58. doi: 10.2147/ijn.S261352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338. Zhi K, Raji B, Nookala AR, Khan MM, Nguyen XH, Sakshi S, et al. Plga nanoparticle-based formulations to cross the blood-brain barrier for drug delivery: from R&D to cgmp. Pharmaceutics (2021) 13(4):500. doi: 10.3390/pharmaceutics13040500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Lu L, Zhao X, Fu T, Li K, He Y, Luo Z, et al. An irgd-conjugated prodrug micelle with blood-brain-barrier penetrability for anti-glioma therapy. Biomaterials (2020) 230:119666. doi: 10.1016/j.biomaterials.2019.119666 [DOI] [PubMed] [Google Scholar]
- 340. Davanzo NN, Pellosi DS, Franchi LP, Tedesco AC. Light source is critical to induce glioblastoma cell death by photodynamic therapy using chloro-aluminiumphtalocyanine albumin-based nanoparticles. Photodiagnosis Photodyn Ther (2017) 19:181–3. doi: 10.1016/j.pdpdt.2017.04.017 [DOI] [PubMed] [Google Scholar]
- 341. Song R, Hu D, Chung HY, Sheng Z, Yao S. Lipid-polymer bilaminar oxygen nanobubbles for enhanced photodynamic therapy of cancer. ACS Appl Mater Interfaces (2018) 10(43):36805–13. doi: 10.1021/acsami.8b15293 [DOI] [PubMed] [Google Scholar]
- 342. Xu HZ, Li TF, Ma Y, Li K, Zhang Q, Xu YH, et al. Targeted photodynamic therapy of glioblastoma mediated by platelets with photo-controlled release property. Biomaterials (2022) 290:121833. doi: 10.1016/j.biomaterials.2022.121833 [DOI] [PubMed] [Google Scholar]
- 343. Qu F, Wang P, Zhang K, Shi Y, Li Y, Li C, et al. Manipulation of mitophagy by “All-in-one” Nanosensitizer augments sonodynamic glioma therapy. Autophagy (2020) 16(8):1413–35. doi: 10.1080/15548627.2019.1687210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344. Wu T, Liu Y, Cao Y, Liu Z. Engineering macrophage exosome disguised biodegradable nanoplatform for enhanced sonodynamic therapy of glioblastoma. Advanced Mater (Deerfield Beach Fla) (2022) 34(15):e2110364. doi: 10.1002/adma.202110364 [DOI] [PubMed] [Google Scholar]
- 345. Liang K, Li Z, Luo Y, Zhang Q, Yin F, Xu L, et al. Intelligent nanocomposites with intrinsic blood-brain-barrier crossing ability designed for highly specific mr imaging and sonodynamic therapy of glioblastoma. Small (Weinheim an der Bergstrasse Germany) (2020) 16(8):e1906985. doi: 10.1002/smll.201906985 [DOI] [PubMed] [Google Scholar]
- 346. Tan J, Duan X, Zhang F, Ban X, Mao J, Cao M, et al. Theranostic nanomedicine for synergistic chemodynamic therapy and chemotherapy of orthotopic glioma. Advanced Sci (Weinheim Baden-Wurttemberg Germany) (2020) 7(24):2003036. doi: 10.1002/advs.202003036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Tang XL, Wang Z, Zhu YY, Xiao H, Xiao Y, Cui S, et al. Hypoxia-activated ros burst liposomes boosted by local mild hyperthermia for photo/chemodynamic therapy. J Controlled Release: Off J Controlled Release Soc (2020) 328:100–11. doi: 10.1016/j.jconrel.2020.08.035 [DOI] [PubMed] [Google Scholar]
- 348. Jung O, Thomas A, Burks SR, Dustin ML, Frank JA, Ferrer M, et al. Neuroinflammation associated with ultrasound-mediated permeabilization of the blood-brain barrier. Trends Neurosci (2022) 45(6):459–70. doi: 10.1016/j.tins.2022.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Pandit R, Chen L, Götz J. The blood-brain barrier: physiology and strategies for drug delivery. Advanced Drug Delivery Rev (2020) 165-166:1–14. doi: 10.1016/j.addr.2019.11.009 [DOI] [PubMed] [Google Scholar]
- 350. Wu H, Tong L, Wang Y, Yan H, Sun Z. Bibliometric analysis of global research trends on ultrasound microbubble: A quickly developing field. Front Pharmacol (2021) 12:646626. doi: 10.3389/fphar.2021.646626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351. Lee H, Kim H, Han H, Lee M, Lee S, Yoo H, et al. Microbubbles used for contrast enhanced ultrasound and theragnosis: A review of principles to applications. Biomed Eng Lett (2017) 7(2):59–69. doi: 10.1007/s13534-017-0016-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Chan MH, Chen W, Li CH, Fang CY, Chang YC, Wei DH, et al. An advanced in situ magnetic resonance imaging and ultrasonic theranostics nanocomposite platform: crossing the blood-brain barrier and improving the suppression of glioblastoma using iron-platinum nanoparticles in nanobubbles. ACS Appl Mater Interfaces (2021) 13(23):26759–69. doi: 10.1021/acsami.1c04990 [DOI] [PubMed] [Google Scholar]
- 353. Wu H, Zhou Y, Xu L, Tong L, Wang Y, Liu B, et al. Mapping knowledge structure and research frontiers of ultrasound-induced blood-brain barrier opening: A scientometric study. Front Neurosci (2021) 15:706105. doi: 10.3389/fnins.2021.706105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354. Yang Q, Zhou Y, Chen J, Huang N, Wang Z, Cheng Y. Gene therapy for drug-resistant glioblastoma via lipid-polymer hybrid nanoparticles combined with focused ultrasound. Int J Nanomed (2021) 16:185–99. doi: 10.2147/ijn.S286221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355. Wei HJ, Upadhyayula PS, Pouliopoulos AN, Englander ZK, Zhang X, Jan CI, et al. Focused ultrasound-mediated blood-brain barrier opening increases delivery and efficacy of etoposide for glioblastoma treatment. Int J Radiat Oncol Biol Phys (2021) 110(2):539–50. doi: 10.1016/j.ijrobp.2020.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. Liang S, Hu D, Li G, Gao D, Li F, Zheng H, et al. Nir-ii fluorescence visualization of ultrasound-induced blood-brain barrier opening for enhanced photothermal therapy against glioblastoma using indocyanine green microbubbles. Sci Bull (2022) 67(22):2316–26. doi: 10.1016/j.scib.2022.10.025 [DOI] [PubMed] [Google Scholar]
- 357. Porret E, Kereselidze D, Dauba A, Schweitzer-Chaput A, Jegot B, Selingue E, et al. Refining the delivery and therapeutic efficacy of cetuximab using focused ultrasound in a mouse model of glioblastoma: an (89)Zr-cetuximab immunopet study. Eur J Pharmaceutics Biopharmaceutics (2023) 182:141–51. doi: 10.1016/j.ejpb.2022.12.006 [DOI] [PubMed] [Google Scholar]
- 358. Hynynen K. Ultrasound for drug and gene delivery to the brain. Advanced Drug Delivery Rev (2008) 60(10):1209–17. doi: 10.1016/j.addr.2008.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359. Carpentier A, Canney M, Vignot A, Reina V, Beccaria K, Horodyckid C, et al. Clinical trial of blood-brain barrier disruption by pulsed ultrasound. Sci Trans Med (2016) 8(343):343re2. doi: 10.1126/scitranslmed.aaf6086 [DOI] [PubMed] [Google Scholar]
- 360. Kim DO, Lee CY. Comprehensive study on vitamin C equivalent antioxidant capacity (Vceac) of various polyphenolics in scavenging a free radical and its structural relationship. Crit Rev Food Sci Nutr (2004) 44(4):253–73. doi: 10.1080/10408690490464960 [DOI] [PubMed] [Google Scholar]
- 361. Sökmen M, Akram Khan M. The antioxidant activity of some curcuminoids and chalcones. Inflammopharmacology (2016) 24(2-3):81–6. doi: 10.1007/s10787-016-0264-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Lin HY, Fu Q, Kao YH, Tseng TS, Reiss K, Cameron JE, et al. Antioxidants associated with oncogenic human papillomavirus infection in women. J Infect Dis (2021) 224(9):1520–8. doi: 10.1093/infdis/jiab148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363. Qi X, Jha SK, Jha NK, Dewanjee S, Dey A, Deka R, et al. Antioxidants in brain tumors: current therapeutic significance and future prospects. Mol Cancer (2022) 21(1):204. doi: 10.1186/s12943-022-01668-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Turkez H, Tozlu OO, Arslan ME, Mardinoglu A. Safety and efficacy assessments to take antioxidants in glioblastoma therapy: from in vitro experiences to animal and clinical studies. Neurochemistry Int (2021) 150:105168. doi: 10.1016/j.neuint.2021.105168 [DOI] [PubMed] [Google Scholar]
- 365. Fernández-Ayala DJ, Brea-Calvo G, López-Lluch G, Navas P. Coenzyme Q distribution in hl-60 human cells depends on the endomembrane system. Biochim Biophys Acta (2005) 1713(2):129–37. doi: 10.1016/j.bbamem.2005.05.010 [DOI] [PubMed] [Google Scholar]
- 366. Maoka T, Yasui H, Ohmori A, Tokuda H, Suzuki N, Osawa A, et al. Anti-oxidative, anti-tumor-promoting, and anti-carcinogenic activities of adonirubin and adonixanthin. J Oleo Sci (2013) 62(3):181–6. doi: 10.5650/jos.62.181 [DOI] [PubMed] [Google Scholar]
- 367. Pan L, Zhou Y, Li XF, Wan QJ, Yu LH. Preventive Treatment of Astaxanthin Provides Neuroprotection through Suppression of Reactive Oxygen Species and Activation of Antioxidant Defense Pathway after Stroke in Rats. Brain Res Bull (2017) 130:211–20. doi: 10.1016/j.brainresbull.2017.01.024 [DOI] [PubMed] [Google Scholar]
- 368. Nakamura S, Maoka T, Tsuji S, Hayashi M, Shimazawa M, Hara H. Central nervous system migration of astaxanthin and adonixanthin following their oral administration in cynomolgus monkeys. J Nutr Sci Vitaminol (2020) 66(5):488–94. doi: 10.3177/jnsv.66.488 [DOI] [PubMed] [Google Scholar]
- 369. Tsuji S, Nakamura S, Maoka T, Yamada T, Imai T, Ohba T, et al. Antitumour effects of astaxanthin and adonixanthin on glioblastoma. Mar Drugs (2020) 18(9):474. doi: 10.3390/md18090474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370. Zhang Y, Liu Q, Wang F, Ling EA, Liu S, Wang L, et al. Melatonin antagonizes hypoxia-mediated glioblastoma cell migration and invasion via inhibition of hif-1α. J Pineal Res (2013) 55(2):121–30. doi: 10.1111/jpi.12052 [DOI] [PubMed] [Google Scholar]
- 371. Holick CN, Giovannucci EL, Rosner B, Stampfer MJ, Michaud DS. Prospective study of intake of fruit, vegetables, and carotenoids and the risk of adult glioma. Am J Clin Nutr (2007) 85(3):877–86. doi: 10.1093/ajcn/85.3.877 [DOI] [PubMed] [Google Scholar]
- 372. Qin S, Wang M, Zhang T, Zhang S. Vitamin E intake is not associated with glioma risk: evidence from a meta-analysis. Neuroepidemiology (2014) 43(3-4):253–8. doi: 10.1159/000369345 [DOI] [PubMed] [Google Scholar]
- 373. Cote DJ, Bever AM, Wilson KM, Smith TR, Smith-Warner SA, Stampfer MJ. A prospective study of tea and coffee intake and risk of glioma. Int J Cancer (2020) 146(9):2442–9. doi: 10.1002/ijc.32574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374. Mohajeri M, Behnam B, Sahebkar A. Biomedical applications of carbon nanomaterials: drug and gene delivery potentials. J Cell Physiol (2018) 234(1):298–319. doi: 10.1002/jcp.26899 [DOI] [PubMed] [Google Scholar]
- 375. Yao Y, Zang Y, Qu J, Tang M, Zhang T. The toxicity of metallic nanoparticles on liver: the subcellular damages, mechanisms, and outcomes. Int J Nanomed (2019) 14:8787–804. doi: 10.2147/ijn.S212907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Zhou X, Guo L, Shi D, Meng D, Sun X, Shang M, et al. Ultrasound-responsive highly biocompatible nanodroplets loaded with doxorubicin for tumor imaging and treatment in vivo . Drug Delivery (2020) 27(1):469–81. doi: 10.1080/10717544.2020.1739170 [DOI] [PMC free article] [PubMed] [Google Scholar]