Abstract
This review discusses the safety concerns associated with diving while using psychotropic medication and the limited literature available on the topic. Despite the risks, some divers continue to dive while taking these medications, and their reasons for doing so are unclear. The exact mechanisms of action of these drugs in hyperbaric environments are poorly understood. While current standards and advice for fitness-to-dive assessments are based on limited evidence and expert opinion, developing evidence-based strategies could improve patient care and optimise diving safety. This review appraises relevant literature in diving medicine and provides clinical perspectives for diving physicians conducting fitness-to-dive assessments on patients using psychotropic medication.
Keywords: Fitness-to-dive, Medications, Mental health, Pharmacology, Psychiatry, Scuba
Introduction
Despite the generally healthy status of the diving community, diving with comorbidities or medications seems to be increasing.[ 1 , 2] This trend has raised questions regarding the safety of diving under these conditions and underlines the importance of standards and policies for preventing diving accidents. Despite the risks associated with diving under conditions sometimes considered incompatible with diving, such as the use of psychotropic medications, studies have shown that some divers continue to do so.[ 3 - 6] Interestingly, divers do not always consider diving with psychotropic medication a safety risk.[ 7] The reasons for this behaviour are unclear and it is uncertain if these divers have refrained to seek advice from a physician or were given incorrect advice. Diving under medically hazardous conditions might increase the risk of diving accidents, but evidence remains equivocal.[ 5 , 8] More specifically, while many reports on diving accidents are published worldwide, the link between psychotropic medication and the outcome of an incident might not be picked up in an accident investigation due to the complex and multifactorial pathway in the chain of events leading up to an accident.[ 1 , 8]
Although numerous studies have reported the potential dangers associated with cardiovascular disease, the hazards stemming from the utilisation of psychotropic medication have received comparatively limited attention.[ 4 , 9 - 11] The findings of two surveys indicate that the utilisation of psychotropic medications among active divers is minimal and largely restricted to antidepressants, probably due to reporting bias.[ 5 , 12] This stands in contrast to the increasing use of psychotropic medication in the general population.[ 13 , 14] In addition, the exact mechanisms of action of psychotropic drugs are poorly understood. This holds especially true in hyperbaric medicine, and available data are mostly derived from animal studies.[ 12 , 15 , 16]
Recently, a large diving organisation launched a campaign to promote the positive effects of diving on mental wellbeing. This may attract more divers struggling with mental health issues and, consequently, users of psychotropic drugs.[ 17] Extensive fitness-to-dive assessments and guidance from a specialised physician are the cornerstones to prevent diving accidents. However, current standards and advice are mostly based on limited evidence, expert opinion, and theoretical concepts.[ 12] In addition, many standards in the field are relatively restrictive regarding the use of psychotropic drugs in relation to diving, which might be at least partially explained by the fact that diving physicians are not always familiar with psychotropic medications. This may give rise to policies that are excessively permissive or restrictive, each with its unique set of attendant risks and cost. Developing evidence-based strategies for optimising diving safety and health could assist physicians in providing state-of-the art patient care.
Therefore, we reviewed the current literature to provide clinical guidance regarding the use of psychotropic medications during fitness-to-dive assessments for diving physicians. In addition, we reviewed relevant literature in psychiatry and share our clinical experience in fitness-to-dive assessments.
Methods
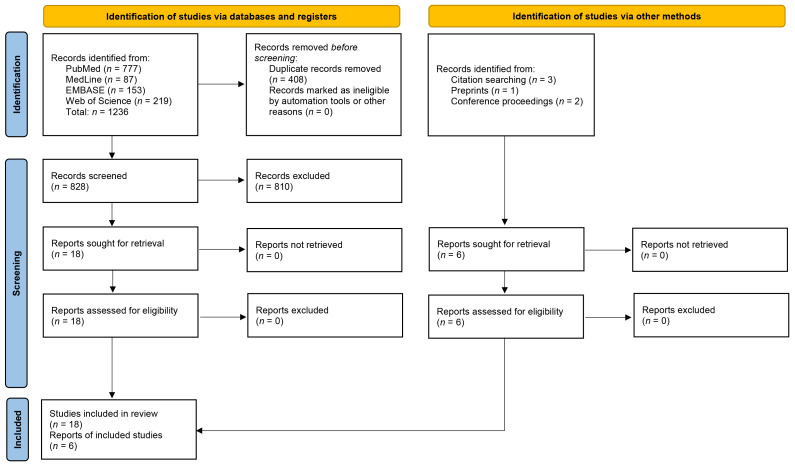
The protocol for objectives, literature search strategies, inclusion and exclusion criteria and outcome measurements were prepared a priori, according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[ 18] The objective of this search was to identify studies investigating the effects of the hyperbaric environment on the pharmacodynamic and pharmacokinetic characteristics of psychotropic medications and the associated risks of diving disorders when used while diving. Electronic database searches were conducted in PubMed, Medline, Embase Science Citation Index Expanded, and the Web of Science up to December 31, 2022. The search was conducted using the keywords "(scuba) diving", "hyperbaric", "medication", "drugs", and "psychiatry", and their synonyms. In case of limited results, fewer keywords were used to avoid missing relevant publications. Snowballing was performed to identify additional studies. Hits were screened on title and abstract. Studies were included if they were published in peer-reviewed journals and covered aspects of psychotropic medication and diving. We focused on five types of psychotropic medications: antipsychotics, antidepressants, sedatives, psychostimulants, and mood stabilisers. Two authors (BQ and TW) independently selected the studies and extracted the data. Any inconsistencies were discussed until consensus was reached. The evaluation of study quality was conducted using appropriate instruments tailored to the specific study type when applicable.
Results
A total of 1,236 studies were initially identified from the four electronic databases using the search strategy described above (Figure 1). After removing 408 duplicate records, 828 studies were screened for eligibility. After applying the inclusion and exclusion criteria, 18 studies were deemed relevant and included in the final analysis. An additional six studies were identified from the reference lists of the included studies, resulting in a total of 24 studies being included in the review. These are summarised in Table 1.
Figure 1.
PRISMA diagram for the search and study selection
Table 1.
| Ref | Study type | Subject | Main outcome |
| 19 | Animals (mice) | Protection against nitrogen narcosis by lithium | Lithium prevented the nitrogen-narcosis-induced loss of righting response but significantly potentiated the pressure (depth) at which convulsions and tremors occurred |
| 20 | Animals (mice) | Protection against decompression sickness by fluoxetine | Platelets and red cells were significantly decreased after decompression in controls but not in the treated mice. Fluoxetine reduced circulating IL-6 |
| 2 | Survey | Health status of divers | Better mental health in divers than in controls |
| 21 | Position paper | Diving by children | Clinical guidance on diving with ADHD in children |
| 22 | Animals (rats) | Risk factors associated with oxygen toxicity | Superoxide dismutase and catalase activity was reduced in the brains of rats exposed to hyperbaric hyperoxia. Glutathione peroxidase activity was reduced in the hippocampus |
| 7 | Survey (divers) | Usage of medication amongst divers | Fifteen percent of the divers used long-term medications when diving. 59.4% considered that they were putting themselves at risk by self-medicating |
| 23 | Animals (rats) | Effects of diazepam in hyperbaric conditions | Convulsions provoked by high helium pressure were prevented by diazepam and the symptoms of high-pressure nervous syndrome (HPNS) were reduced |
| 12 | Review | Effects of medication in hyperbaric conditions | No evidence of significant risks due to changes in pharmacologic mechanisms were revealed and most medication is not a contraindication to diving |
| 3 | Survey (divers) | Medication usage amongst divers | 60% reported using non-prescribed medications; 1.2% reported psychiatric illnesses |
| 5 | Survey (divers) | Medication usage and effect on nitrogen narcosis | 15.2% reported the use of psychiatric medications. No obvious effect on nitrogen narcosis |
| 1 | Survey (divers) | Medical conditions involved in diving accidents | Many divers have medical conditions and use medications |
| 24 | Review | Risk factors associated with oxygen toxicity | GABA and NMDA modulating drugs affect the risk of seizures related to oxygen toxicity |
| 25 | Position paper | Diving with antidepressants | Clinical guidance on diving with antidepressants |
| 26 | Position paper | Diving with ADHD | Clinical guidance on diving with ADHD medication |
| 27 | Review | Diving with cardiovascular medications | A risk-based approach on diving with medications |
| 15 | Review | Effects of hyperbaric conditions on pharmacokinetics | Hyperbaric or hyperoxic exposure doesn’t affect pharmacokinetics of drug elimination |
| 28 | Case series | Effects of medication on oxygen toxicity | Antidepressants or tramadol might increase risk of central nervous system oxygen toxicity |
| 11 | Case series | Medication used in diving accidents | Several divers involved in accidents used (psychoactive) medications |
| 6 | Survey (divers) | Usage of recreational drugs amongst divers | Report on divers using illicit drugs, with a clear relation to depression or anxiety disorders |
| 4 | Survey (divers) | Diving with mental health issues | Similar incidence in mental health issues in divers compared to the general population and many of them are diving with psychoactive medications |
| 10 | Survey (divers) | Medication usage amongst divers | Less than 2% of divers use anti-epileptic, antidepressants, or antipsychotic medications |
| 9 | Survey (divers) | Medication usage in diving accidents | 6.4% of divers reported the use of psychotropic medications |
| 29 | Animals (mice) | Protection of fluoxetine against nitrogen narcosis | Fluoxetine decreased decompression sickness severity and survival in mice |
| 30 | Review | Risks associated with oxygen toxicity | GABA and NMDA modulating drugs affect the risk of seizures related to oxygen toxicity |
Discussion
To the best of our knowledge, this is the first structured literature review to investigate the effects of psychoactive medication on fitness-to-dive assessments. In the following section, we summarise our findings and share our clinical expertise for individuals who require psychotropic medication while diving. Following careful consideration of the available evidence and general considerations, we provide recommendations for the use of antipsychotics, antidepressants, sedatives, stimulants, and mood stabilisers.[ 31]
GENERAL CONSIDERATIONS
Psychotropic medications are widely prescribed, with their use on the rise.[ 14 , 32] While the present study does not aim to evaluate the validity of such prescribing practices, it is important to recognise that mental health complaints amongst divers can vary widely in severity. Furthermore, most psychotropic medications have multiple indications, making it overly simplistic to base dive medical advice solely on the drug used. We emphasise that the use of psychotropic medications is often underreported in fitness to dive assessments, and we urge diving physicians to take the time to explore this carefully.[ 4] When assessing a diver’s use of psychotropic medications, it is essential to first consider the indication, as this may be a reason to temporarily restrict diving activity. While diving should not be seen as a treatment for psychiatric disorders, many divers report positive effects of diving on their mental wellbeing and its potential therapeutic benefits should be considered. Although severe adverse effects of psychotropic medications are possible, the majority of patients tolerate these drugs well and experience only mild side effects.[ 33] Side effects are especially common in the first few weeks of treatment and when multiple medications are used simultaneously. We advise colleagues who are unfamiliar with psychotropic medications to seek expert consultation when assessing fitness to dive, i.e., from a psychiatrist or clinical pharmacologist, to evaluate the possibly relevant side effects for diving. Finally, it should be noted that most psychotropic medications alter the activation threshold of nerve cells, and there is some evidence from animal studies in rats to suggest that these drugs may increase the risk of cerebral oxygen toxicity.[ 22 , 24] In a study of 4,357 hyperbaric oxygen treatments conducted in human subjects, all of whom were concurrently taking psychotropic medications (including antidepressants, sedatives, or narcotics), seven cases of seizures were reported.[ 28] Although other factors may have contributed to these cases, the association between neuromodulating agents and cerebral oxygen toxicity warrants further investigation.
When evaluating the fitness of a diver with mental health complaints, it is important to carefully consider the individual case rather than solely relying on the diagnosis or medication use. Factors such as therapy compliance and disease awareness should also be considered when determining a diver’s ability to comply with diving restrictions and advice. Once a patient has stabilised and returned to normal daily activities, diving can be considered. However, when using multiple psychotropic medications, diving may be discouraged due to an increased risk of side effects. Lastly, given that side effects of psychotropic medications typically manifest within the initial weeks of initiation or dosage modification, a precautionary period of refraining from diving for a duration of up to three months may be advised. If side effects persist, diving should be approached with extreme caution. Moreover, as psychotropic medications could increase susceptibility to nitrogen narcosis or oxygen toxicity, a limitation on diving depth, e.g., 18 metres (60 feet), could be recommended to prevent these conditions.[ 30]
ANTIPSYCHOTICS
The use of antipsychotics is primarily indicated for psychotic disorders, acute mania, and severe agitation, although many off-label indications exist, and the registration of antipsychotics differs between the Food and Drug Administration (FDA) and the European Medicines Agency (EMA). Despite the often-used classification into first-, second-, and third-generation, antipsychotics are a heterogeneous drug class with diverse pharmacological and clinical properties. While the effectiveness of different antipsychotic medications is similar, with the exception of clozapine, their side effects vary.[ 34] Weight gain, sedation, drowsiness, and dry mouth are commonly reported side effects, particularly those with strong antihistaminergic and anticholinergic properties (such as quetiapine, olanzapine, clozapine and ‘low-potency’ first-generation antipsychotics).[ 35] Diving should be discouraged if the patient experiences drowsiness or sedation. Movement disorders, convulsions, orthostatic hypotension, and dysregulated blood glucose levels are also relevant side effects for sports diving.[ 36 - 38] Movement disorders, such as parkinsonism, acute dystonia and tardive dyskinesia, are mainly attributed to potent dopamine D2-antagonism, a characteristic of several antipsychotics such as haloperidol, risperidone, and paliperidone. Partial D2-agonists, such as aripiprazole, are particularly associated with the development of akathisia, although any antipsychotic medication has the potential to cause this side effect. To detect (subtle) movement disorders, a thorough neurological examination is required. Although hyperglycemia is more common in patients undergoing antipsychotic treatment than in the general population, hypoglycemia is one of the idiosyncratic potentially life-threatening adverse effects of antipsychotics due to increased insulin secretion. In cases with a history of uncontrolled hypoglycemia due to side effects or diet, disqualification for diving should be considered. The International Council on Alcohol, Drugs and Traffic Safety (ICADTS) has published considerations for medication use in driving that may support clinicians in assessing fitness to dive.[ 39]
Although seizures are rare, they can be fatal when they occur while diving. Therefore, the use of clozapine, a frequently prescribed antipsychotic with a relatively high risk of seizures, is not compatible with scuba diving. Although older antipsychotics such as chlorpromazine, promazine, thioridazine, and haloperidol have been associated with an elevated risk of seizures, evidence regarding the potential seizure risk of other antipsychotic medications is limited.[ 36] While most antipsychotic medications are associated with only modest QT-interval prolongation, aripiprazole, brexpiprazole, cariprazine, and lurasidone are typically considered to pose a relatively low risk in this regard. Conversely, sertindole is regarded as particularly high-risk, and its use should ideally be avoided due to its association with a heightened risk of arrhythmias. Other cardiovascular risk factors, such as smoking or hypertension, probably increase morbidity and mortality risks more in diving.[ 27 , 40] Diving with a low dose of antipsychotic medication in the absence of side effects or other cardiovascular risk factors is probably safe.
ANTIDEPRESSANTS
Antidepressants are prescribed primarily for major depression and anxiety disorders, but are also used for post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), somatoform disorders, sleeping disorders, and chronic (neuropathic) pain syndromes as well as off-label indications.[ 41] There are several classes of antidepressants, including tricyclic antidepressants (TCAs), serotonin reuptake inhibitors (SSRIs), serotonin-noradrenaline reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs) and others such as bupropion (a noradrenaline-dopamine reuptake inhibitor, NDRI), mirtazapine (a noradrenergic and specific serotonergic antidepressant, NaSSA), trazodone (a serotonin-antagonist and reuptake-inhibitor, SARI) and vortioxetine (a multi-modal antidepressant, MMA).
Tricyclic antidepressants commonly cause side effects due to their anticholinergic (dry mouth, blurred vision, constipation, urinary retention, and tachycardia), antihistaminergic (weight gain, sedation, and drowsiness) and anti-adrenergic properties (orthostatic hypotension and sedation).[ 42] Although SSRIs and SNRIs are generally better tolerated than TCAs due to their more selective pharmacological properties, they still have a similar incidence of side effects, albeit qualitatively different.[ 43 - 45] Common side effects of SSRI’s, SNRI’s and vortioxetine include headaches, gastrointestinal symptoms, insomnia, and sexual dysfunction. Additionally, they can increase bleeding risk, cause weight gain, somnolence, agitation, and hyponatremia, although these side effects are less common. An increased bleeding tendency has a theoretical risk of making any neurological decompression sickness (DCS) worse but is only clinically relevant in patients using warfarin or non-steroidal anti-inflammatories (NSAIDs) and in patients with a history of bleeding complications.[ 25]
In the context of diving, the most relevant side-effects of antidepressants include sedation, hypotension, and seizures. In particular, tertiary TCA’s and mirtazapine, due to their very high affinity for the histamine H1-receptor, are not recommended for diving as they belong to the most sedating antidepressants. Besides TCA’s, virtually all antidepressants, including SSRIs and SNRIs can induce hypotension, although SNRIs can also cause hypertension due to their noradrenergic enhancing properties by inhibiting the noradrenaline transporter (NET). Irreversible MAOIs are associated with a high probability of severe and dose-dependent orthostatic hypotension, which makes them unsuitable for diving.[ 46 , 47]
All antidepressants lower the threshold for epileptic seizures, with possibly a higher risk for clomipramine and bupropion.[ 48] Although the absolute risk is low, it might increase with long-term use.[ 49] The risk of convulsions with bupropion is dose-dependent, particularly with doses exceeding 450 mg and in immediate-release formulations.[ 50] Consequently, due to its potential to lower the seizure threshold, bupropion should preferably be avoided for diving. On the other hand, two studies in mice suggest a possible neuroprotective effect of fluoxetine (50 mg·kg-1) when administered before hyperbaric exposure, resulting in lower decompression sickness (DCS) incidence and better neurological recovery.[ 20 , 29] Although one study shows that fluoxetine might have subtle anti-inflammatory effects, these are most likely clinically insignificant in the prevention or treatment of DCS.[ 51] During fitness-to-dive assessments, if antidepressants are required, SSRIs and SNRIs should be suggested over TCAs, mirtazapine and trazodone due to their lower incidence of sedation and drowsiness.[ 25] However, diving with SSRIs and SNRIs should be temporarily discontinued when the dosage is reduced or the medication is stopped due to the risk of withdrawal symptoms.
SEDATIVES
Sedatives, such as benzodiazepines and Z-drugs, are frequently used in the treatment of sleep and anxiety disorders in individuals with psychiatric illness. However, chronic usage of these drugs may result in dependency, cognitive impairment, and an increased risk of falls and accidents due to sedation, drowsiness, confusion, dizziness, and amnesia.[ 52] Most sedatives are classified as ICADTS category III, which prohibits their use when operating a vehicle.[ 39] Additionally, although animal studies suggest that diazepam may prevent high pressure nervous syndrome (HPNS), the sedative effects of this medication likely outweigh any potential benefits.[ 23] Therefore, diving while taking benzodiazepines or other Z-drugs is contraindicated. If these medications are used occasionally to treat sleep disorders, diving may be permitted after discontinuation for at least one week, depending on the specific drug’s elimination half-life. In individuals with anxiety disorders, the underlying illness should be prioritised, and diving may be considered only after an appropriate medication-free period has elapsed. It is important to note that discontinuing or abruptly reducing the dosage of these drugs in long-term usage may cause withdrawal effects. Consultation with an expert should be sought if discontinuation or dosage reduction is being considered.
PSYCHOSTIMULANTS
Stimulants are commonly used to treat attention deficit hyperactivity disorder (ADHD) and narcolepsy, among other off-label indications. A small study has suggested that ADHD is fairly common among commercial divers.[ 53] Psychostimulants include methylphenidate, amphetamines (such as mixed amphetamine salts, dexamfetamine and lisdexamfetamine) and modafinil. Also, non-stimulants are used in ADHD, such as the alpha-2 adrenergic agonists (clonidine and guanfacine), atomoxetine, and bupropion. The most common side effects of psychostimulants and atomoxetine are mild, such as insomnia, reduced appetite, headache, and palpitations. Among adults, treatment with psychostimulants has been linked to a modest increase on average in systolic blood pressure (2 mmHg) and heart rate (5.7 beats·min-1).[ 54] Although these cardiovascular changes are not typically considered clinically significant in the short term, there are concerns regarding their long-term implications. However, observational studies have shown that the use of psychostimulants does not significantly increase the risk of cardiovascular events at the population level, or only to a limited extent.[ 55] It is important to note, however, that in individual patients, blood pressure and heart rate can increase substantially, with increases of approximately 10–25 mmHg and 15 or more beats·min-1 respectively.
Psychostimulants and bupropion may lower the convulsive threshold in patients with a prior history of seizures, and rarely in patients without a history of convulsions and no electroencephalogram abnormalities.[ 26 , 56] Relevant side effects of alpha-2 adrenergic agonists include somnolence, headache, and fatigue, and they can also cause a serious withdrawal syndrome characterised by an excessive increase in heart rate and blood pressure. In general, psychostimulants and atomoxetine are well tolerated, and are not considered contraindicated for diving in the absence of serious side effects.[ 53] However, due to their sedative effects, particularly during the initiation of treatment, diving with clonidine and guanfacine is not advisable.
MOOD STABILISERS
Mood stabilisers are primarily used to treat bipolar disorders and include lithium, anticonvulsants, and antipsychotics. Lithium, valproic acid, carbamazepine, and lamotrigine are the most commonly used mood stabilisers. Lithium, although effective, has a significant side effect profile with polyuria, polydipsia, tremors, and weight gain. Moreover, long-term use of lithium is associated with gradual decline of renal functioning and diabetes insipidus, leading to dehydration.[ 57] Interestingly, there are some data suggesting that lithium reduces the effects of nitrogen narcosis, but potentiates convulsions and tremors.[ 19] Valproic acid is generally well-tolerated, with side effects such as gastrointestinal complaints, weight gain, sedation, and tremor.[ 58] Carbamazepine can cause gastrointestinal complaints, drowsiness, and weight gain.[ 59] Lamotrigine is well tolerated, with some studies even suggesting that its side effect profile is comparable to placebo.[ 60] In general, side effects of these anticonvulsants are dose-dependent and tend to decrease when the dosage is reduced. In fitness-to-dive assessments, lithium is the most problematic mood stabiliser. Dehydration caused by lithium is further potentiated in diving due to breathing dry air, immersion diuresis, and sweating when diving in tropical environments. This can be addressed by adequate rehydration after diving. Additionally, the narrow therapeutic range of lithium can be disturbed by the aforementioned factors, leading to lithium toxicity. Therefore, diving with lithium should be considered cautiously. Conversely, the other mood stabilisers are generally well-tolerated and are not contraindicated for diving, taking the general considerations into account.
LIMITATIONS
While this review provides recommendations for diving with psychotropic medications based on the available literature, it is important to note that very little literature is currently available in this area. Therefore, this review should be regarded as an effort to provide guidance for diving physicians, considering that recommendations are sometimes based more on expert opinion and pharmacology than on rigorous scientific evidence. To further develop the knowledge base in this area, we encourage diving physicians and psychiatrists with experience in the treatment of divers to publish their experiences and results.
Additionally, it is important to acknowledge that there is likely an underreporting of psychotropic medication usage in divers, which may limit the practical application of the recommendations provided in this review. We urge clinicians to actively inquire about psychiatric conditions and medication usage during dive medical assessments.
As a side note, in relation to diving incidents seemingly linked to use of psychotropic medications it is often difficult to assess which of the medication or the psychiatric illness that it has been prescribed for is the most important contributor to the chain of events leading to the diving accident. Therefore, it is difficult to appraise the actual risk of diving due to psychotropic medications per se. Another important implication is that although the focus of this review has been on psychopharmacology, irrespective of the suitability of a particular drug for diving, assessing physicians should also consider the compatibility of each individual patient’s psychiatric presentation with this activity.
It should also be noted that this review is focused on adult recreational divers, and whether the recommendations can be applied to commercial or military divers remains to be determined. Furthermore, diving by children who have psychiatric conditions presents unique challenges that have not been thoroughly explored.[ 21] Lastly, it is crucial to acknowledge that psychiatry represents a specialised area of medicine where the application of standardised guidelines and checklists is often limited. This is particularly relevant when assessing psychiatric patients who engage in diving activities, given the unique challenges and considerations that arise in this context. As such, we recommend that diving physicians consult with psychiatrists when they are uncertain about the suitability of diving for a particular patient.
Conclusions
In conclusion, this review provides a summary of the limited literature available on psychotropic medication use and fitness to dive, supplemented with expert opinion from psychiatrists with medical expertise in the field. The recommendations presented in this paper aim to provide guidance for diving physicians, but it is crucial to emphasise the importance of individual patient assessment and case-by-case decision making. Diving with psychiatric disease and psychotropic medication use is often possible, but it requires careful evaluation and consideration of potential risks and benefits. We encourage further research and publication in this area to continue advancing the knowledge base and supporting safe diving practices.
Footnotes
Conflict of interest and funding: nil
Contributor Information
Abraham L Querido, Praktijk Querido, Hilversum, the Netherlands; Dutch Society of Diving and Hyperbaric Medicine, Bilthoven, the Netherlands.
Chiel F Ebbelaar, PharmC, consultancy for clinical psychopharmacology, Utrecht, the Netherlands; Leiden University Medical Center, Department of Dermatology, Leiden, the Netherlands; University Medical Center Utrecht, Department of Pathology, Division of Laboratories, Pharmacy and Biomedical Genetics, University Medical Center Utrecht, Utrecht, the Netherlands.
Thijs T Wingelaar, Dutch Society of Diving and Hyperbaric Medicine, Bilthoven, the Netherlands; Royal Netherlands Navy, Diving Medical Center, Den Helder, the Netherlands.
References
- Lippmann J, Taylor DM, Stevenson C, Mitchell S. The demographics and diving behaviour of DAN Asia-Pacific members with and without pre-existing medical conditions. Diving Hyperb Med. 2016; 46: 200–6. [cited 2023 Jul 27]. Available from: https://dhmjournal.com/images/Journals/46/DHM_Vol46_No4.pdf. [PubMed] [Google Scholar]
- Buzzacott P, Edelson C, Chimiak J, Tillmans F. Health and wellbeing of recently active United States scuba divers. Diving Hyperb Med. 2022;52:16–21. doi: 10.28920/dhm52.1.16-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komdeur P, Wingelaar TT, van Hulst RA. A survey on the health status of Dutch scuba diving instructors. Diving Hyperb Med. 2021;51:18–24. doi: 10.28920/dhm51.1.18-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- St Leger Dowse M, Whalley B, Waterman MK, Conway RM, Smerdon GR. Diving and mental health: the potential benefits and risks from a survey of recreational scuba divers. Diving Hyperb Med. 2019;49:291–7. doi: 10.28920/dhm49.4.291-297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krummel T, Thiery A, Villain M, Schittly B, Brouant B. Psychotropic drug use in recreational scuba divers and its effect on severe narcosis. Int J Sports Med. 2017;38:322–8. doi: 10.1055/s-0042-122336. [DOI] [PubMed] [Google Scholar]
- St Leger Dowse M, Cridge C, Smerdon G. The use of drugs by UK recreational divers: prescribed and over-the-counter medications. Diving Hyperb Med. 2011; 41: 16-21. [cited 2023 Jul 27]. Available from: https://dhmjournal.com/images/IndividArticles/41March/StLegerDowse_dhm.41.1.9-15.pdf [PubMed] [Google Scholar]
- Fraisse T, Nicolas B, de Wazières B. [Evaluation of self-medication by scuba divers]. Therapie. 2005;60:409–12. doi: 10.2515/therapie:2005059. [DOI] [PubMed] [Google Scholar]
- Lippmann J. A review of snorkelling and scuba diving fatalities in Queensland, Australia, 2000 to 2019. Diving Hyperb Med. 2022;52:108–18. doi: 10.28920/dhm52.2.108-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Taylor DM, Pisasale D, Booth K, Lippmann J. Regular medication use by active scuba divers with a declared comorbid medical condition and victims of scuba and snorkelling-related fatalities. Diving Hyperb Med. 2021;51:264–70. doi: 10.28920/dhm51.3.264-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Taylor DM, O’Toole K, Ryan C. Medications taken daily and prior to diving by experienced scuba divers SPUMS Journal 2002; 32: 129–35. [cited 2023 Jul 27]. Available from: https://dhmjournal.com/images/IndividArticles/32Sept/Taylor_SPUMSJ.32.3.129-135.pdf. [Google Scholar]
- Smerz RW. Drugs downed divers did. Undersea Hyperb Med. 2007;34(4):283. [Google Scholar]
- Hoencamp E, van Dongen TT, van Ooij P-JA, Wingelaar TT, Vervelde ML, Koch DA, et al. Systematic review on the effects of medication under hyperbaric conditions: consequences for the diver. Diving Hyperb Med. 2019;49:127–36. doi: 10.28920/dhm49.2.127-136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brett J, Karanges EA, Daniels B, Buckley NA, Schneider C, Nassir A, et al. Psychotropic medication use in Australia, 2007 to 2015: changes in annual incidence, prevalence and treatment exposure. Aust N Z J Psychiatry. 2017;51(10):990–9. doi: 10.1177/0004867417721018. [DOI] [PubMed] [Google Scholar]
- Brauer R, Alfageh B, Blais JE, Chan EW, Chui CSL, Hayes JF, et al. Psychotropic medicine consumption in 65 countries and regions, 2008–19: a longitudinal study. Lancet Psychiatry. 2021;8(12):1071–82. doi: 10.1016/s2215-0366(21)00292-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rump AF, Siekmann U, Kalff G. Effects of hyperbaric and hyperoxic conditions on the disposition of drugs: theoretical considerations and a review of the literature. Gen Pharmacol. 1999;32(1):127–33. doi: 10.1016/s0306-3623(98)00074-3. [DOI] [PubMed] [Google Scholar]
- Cevik NG, Cevik N, Yilmaz CU, Arican N, Ahishali B, Kucuk M, et al. The effects of hyperbaric air and hyperbaric oxygen on blood-brain barrier integrity in rats. Brain Res. 2013;1531:113–21. doi: 10.1016/j.brainres.2013.07.052. [DOI] [PubMed] [Google Scholar]
- Professional Association of Diving Instructors . PADI spotlights wellness and mental health in live unfiltered campaign 2022. [cited 2023 Jul 25]. Available from: https://pros-blog.padi.com/padi-spotlights-wellness-and-mental-health-in-live-unfiltered-campaign/
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett PB, Leventhal BL, Coggin R, Roby J, Racanska L. Lithium effects: protection against nitrogen narcosis, potentiation of HPNS. Undersea Biomed Res. 1980;7:11–6. [PubMed] [Google Scholar]
- Blatteau JE, Barre S, Pascual A, Castagna O, Abraini JH, Risso JJ, et al. Protective effects of fluoxetine on decompression sickness in mice. PLoS One. 2012;7(11):e49069. doi: 10.1371/journal.pone.0049069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buwalda M, Querido AL, van Hulst RA. Children and diving, a guideline. Diving Hyperb Med. 2020;50:399–404. doi: 10.28920/dhm50.4.399-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eynan M, Krinsky N, Biram A, Arieli Y, Arieli R. A comparison of factors involved in the development of central nervous system and pulmonary oxygen toxicity in the rat. Brain Res. 2014;1574:77–83. doi: 10.1016/j.brainres.2014.05.051. [DOI] [PubMed] [Google Scholar]
- Gran L, Coggin R, Bennett PB. Diazepam under hyperbaric conditions in rats. Acta Anaesthesiol Scand. 1980;24:407–11. doi: 10.1111/j.1399-6576.1980.tb01572.x. [DOI] [PubMed] [Google Scholar]
- Manning EP. Central nervous system oxygen toxicity and hyperbaric oxygen seizures. Aerosp Med Hum Perform. 2016;87:477–86. doi: 10.3357/amhp.4463.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Querido AL. Diving and antidepressants. Diving Hyperb Med. 2017;47:253–6. doi: 10.28920/dhm47.4.253-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Querido AL, van Hulst RA. Diving and attention deficit hyperactivity disorder. Diving Hyperb Med. 2019;49:41–7. doi: 10.28920/dhm49.1.41-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rienks R, Buwalda M, Bucx J, Dubois E, Wingelaar T, van Hulst R. Cardiovascular risk assessment in divers: toward safer diving. Undersea Hyperb Med. 2022;49:355–65. [PubMed] [Google Scholar]
- Seidel R, Carroll C, Thompson D, Diem RG, Yeboah K, Hayes AJ, et al. Risk factors for oxygen toxicity seizures in hyperbaric oxygen therapy: case reports from multiple institutions. Undersea Hyperb Med. 2013;40:515–9. [PubMed] [Google Scholar]
- Vallée N, Lambrechts K, De Maistre S, Royal P, Mazella J, Borsotto M, et al. Fluoxetine protection in decompression sickness in mice is enhanced by blocking TREK-1 potassium channel with the “spadin” antidepressant. Front Physiol. 2016;7:42. doi: 10.3389/fphys.2016.00042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingelaar TT, van Ooij PAM, van Hulst RA. Oxygen toxicity and special operations forces diving: hidden and dangerous. Front Psychol. 2017;8:1263. doi: 10.3389/fpsyg.2017.01263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute of Mental Health . Mental health medications. 2022. Available from: https://www.nimh.nih.gov/health/topics/mental-health-medications.
- Thomas CP, Conrad P, Casler R, Goodman E. Trends in the use of psychotropic medications among adolescents, 1994 to 2001. Psychiatr Serv. 2006;57:63–9. doi: 10.1176/appi.ps.57.1.63. [DOI] [PubMed] [Google Scholar]
- Ćurković M, Dodig-Ćurković K, Erić AP, Kralik K, Pivac N. Psychotropic medications in older adults: a review. Psychiatr Danub. 2016;28:13–24. [PubMed] [Google Scholar]
- Huhn M, Nikolakopoulou A, Schneider-Thoma J, Krause M, Samara M, Peter N, et al. Comparative efficacy and tolerability of 32 oral antipsychotics for the acute treatment of adults with multi-episode schizophrenia: a systematic review and network meta-analysis. Lancet. 2019;394(10202):939–51. doi: 10.1016/s0140-6736(19)31135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup TS, Gray N. Management of common adverse effects of antipsychotic medications. World Psychiatry. 2018;17:341–56. doi: 10.1002/wps.20567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury R, Ghossoub E. Antipsychotics and seizures: what are the risks? Current Psychiatry. 2019;18(3):21–3. [Google Scholar]
- Gugger JJ. Antipsychotic pharmacotherapy and orthostatic hypotension: identification and management. CNS Drugs. 2011;25:659–71. doi: 10.2165/11591710-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, et al. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1-3):15–22. doi: 10.1016/j.schres.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Verster JC, Mets MAJ. Psychoactive medication and traffic safety. Int J Environ Res Public Health. 2009;6:1041–54. doi: 10.3390/ijerph6031041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambiase PD, de Bono JP, Schilling RJ, Lowe M, Turley A, Slade A, et al. British Heart Rhythm Society clinical practice guidelines on the management of patients developing QT prolongation on antipsychotic medication. Arrhythm Electrophysiol Rev. 2019;8:161–5. doi: 10.15420/aer.2019.8.3.G1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skånland SS, Cieślar-Pobuda A. Off-label uses of drugs for depression. Eur J Pharmacol. 2019;865:172732. doi: 10.1016/j.ejphar.2019.172732. [DOI] [PubMed] [Google Scholar]
- Trindade E, Menon D, Topfer LA, Coloma C. Adverse effects associated with selective serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. CMAJ. 1998;159:1245–52. [PMC free article] [PubMed] [Google Scholar]
- Carvalho AF, Sharma MS, Brunoni AR, Vieta E, Fava GA. The safety, tolerability and risks associated with the use of newer generation antidepressant drugs: a critical review of the literature. Psychother Psychosom. 2016;85:270–88. doi: 10.1159/000447034. [DOI] [PubMed] [Google Scholar]
- Wang SM, Han C, Bahk WM, Lee SJ, Patkar AA, Masand PS, et al. Addressing the side effects of contemporary antidepressant drugs: a comprehensive review. Chonnam Med J. 2018;54:101–12. doi: 10.4068/cmj.2018.54.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson IM. Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability. J Affect Disord. 2000;58:19–36. doi: 10.1016/s0165-0327(99)00092-0. [DOI] [PubMed] [Google Scholar]
- Remick RA, Froese C, Keller FD. Common side effects associated with monoamine oxidase inhibitors. Prog Neuropsychopharmacol Biol Psychiatry. 1989;13(3-4):497–504. doi: 10.1016/0278-5846(89)90137-1. [DOI] [PubMed] [Google Scholar]
- Van den Eynde V, Abdelmoemin WR, Abraham MM, Amsterdam JD, Anderson IM, Andrade C, et al. The prescriber’s guide to classic MAO inhibitors (phenelzine, tranylcypromine, isocarboxazid) for treatment-resistant depression. CNS Spectr. 2022:1–14. doi: 10.1017/s1092852922000906. [DOI] [PubMed] [Google Scholar]
- Steinert T, Fröscher W. Epileptic seizures under antidepressive drug treatment: systematic review. Pharmacopsychiatry. 2018;51:121–35. doi: 10.1055/s-0043-117962. [DOI] [PubMed] [Google Scholar]
- Hill T, Coupland C, Morriss R, Arthur A, Moore M, Hippisley-Cox J. Antidepressant use and risk of epilepsy and seizures in people aged 20 to 64 years: cohort study using a primary care database. BMC Psychiatry. 2015;15:315. doi: 10.1186/s12888-015-0701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Thase ME, Clayton A, Stahl SM, Pradko JF, et al. 15 years of clinical experience with bupropion HCl: from bupropion to bupropion SR to bupropion XL. Prim Care Companion J Clin Psychiatry. 2005;7(3):106–13. doi: 10.4088/pcc.v07n0305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abdel-Salam OM, Baiuomy AR, Arbid MS. Studies on the anti-inflammatory effect of fluoxetine in the rat. Pharmacol Res. 2004;49:119–31. doi: 10.1016/j.phrs.2003.07.016. [DOI] [PubMed] [Google Scholar]
- Seldenrijk A, Vis R, Henstra M, Ho Pian K, van Grootheest D, Salomons T, et al. [Systematic review of the side effects of benzodiazepines]. Ned Tijdschr Geneeskd. 2017;161:D1052. [PubMed] [Google Scholar]
- Van Wijk CH, Meintjes WAJ. Adult attention-deficit/hyperactivity disorder prevalence among commercial divers in South Africa. Diving Hyperb Med. 2020;50:164–7. doi: 10.28920/dhm50.2.164-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mick E, McManus DD, Goldberg RJ. Meta-analysis of increased heart rate and blood pressure associated with CNS stimulant treatment of ADHD in adults. Eur Neuropsychopharmacol. 2013;23:534–41. doi: 10.1016/j.euroneuro.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Yao H, Li L, Du Rietz E, Andell P, Garcia-Argibay M, et al. Risk of cardiovascular diseases associated with medications used in attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. JAMA Netw Open. 2022;5(11):e2243597. doi: 10.1001/jamanetworkopen.2022.43597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y, Gao X, Xu Y. The dilemma of treatments for epileptic patients with depression. Int J Neurosci. 2015;125:566–77. doi: 10.3109/00207454.2014.959122. [DOI] [PubMed] [Google Scholar]
- Tondo L, Abramowicz M, Alda M, Bauer M, Bocchetta A, Bolzani L, et al. Long-term lithium treatment in bipolar disorder: effects on glomerular filtration rate and other metabolic parameters. Int J Bipolar Disord. 2017;5(1):27. doi: 10.1186/s40345-017-0096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddad PM, Das A, Ashfaq M, Wieck A. A review of valproate in psychiatric practice. Expert Opin Drug Metab Toxicol. 2009;5:539–51. doi: 10.1517/17425250902911455. [DOI] [PubMed] [Google Scholar]
- Koliqi R, Polidori C, Islami H. Prevalence of side effects treatment with carbamazepine and other antiepileptics in patients with epilepsy. Mater Sociomed. 2015;27:167–71. doi: 10.5455/msm.2015.27.167-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowden CL, Asnis GM, Ginsberg LD, Bentley B, Leadbetter R, White R. Safety and tolerability of lamotrigine for bipolar disorder. Drug Saf. 2004;27:173–84. doi: 10.2165/00002018-200427030-00002. [DOI] [PubMed] [Google Scholar]