Abstract
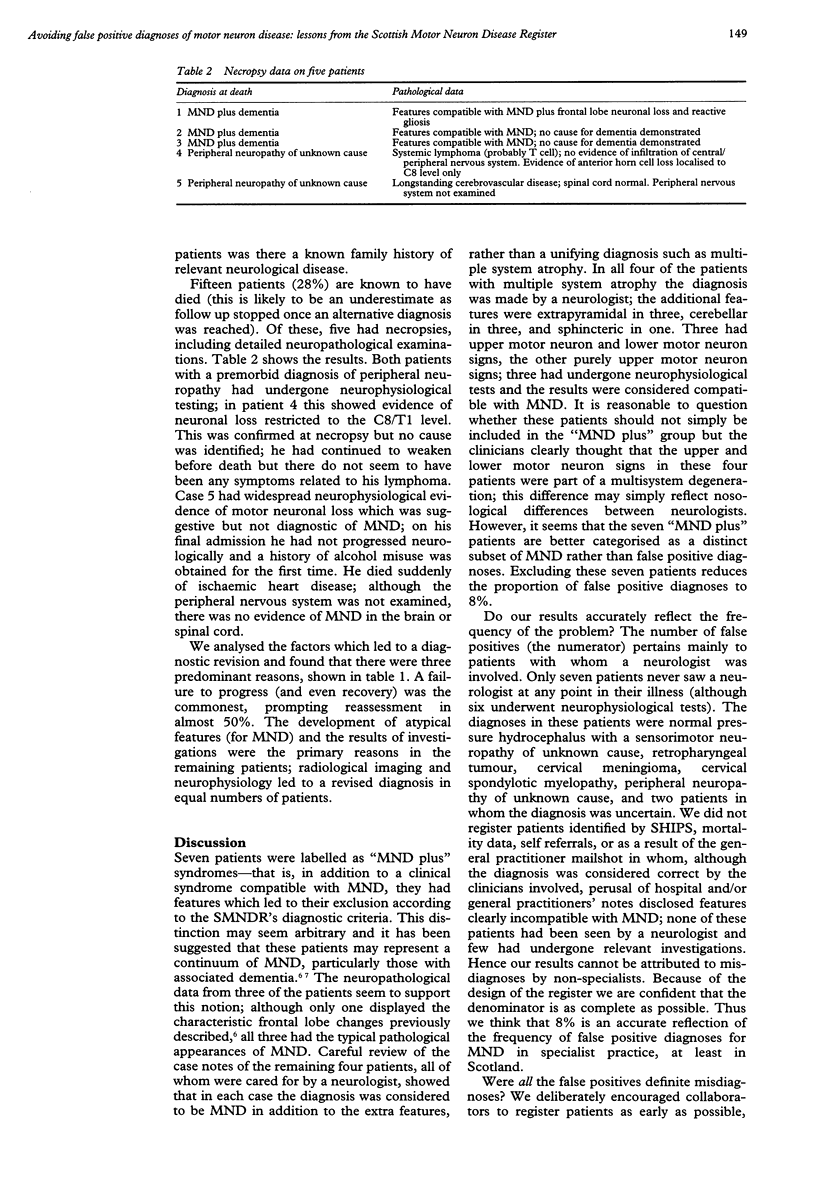
OBJECTIVES--To describe the frequency and characteristics of those patients initially registered with the Scottish Motor Neuron Disease Register (SMNDR) but who subsequently had a diagnosis other than MND made (false positives), to analyse the features which led to a revised diagnosis, and to draw conclusions which might improve routine neurological practice. METHODS--The Scottish Motor Neuron Disease Register is a community based, prospective disease register to identify and follow up all incident cases of motor neuron disease in Scotland. Fifty three patients out of a total of 552 registered are presented, who, after initial registration, were later excluded because they failed to satisfy the register's diagnostic criteria. RESULTS--Seven of these patients were labelled as "MND plus" syndromes and may represent a distinct subset of MND. The remaining 46 patients had an alternative diagnosis made (false positive group), accounting for 8% of the total. In half of these cases, potentially beneficial therapies are available. The predominant reasons which lead to a diagnostic revision were: failure of symptom progression, development of atypical clinical features for MND, and investigation results. CONCLUSIONS--Patients with MND should undergo thorough and relevant investigations at presentation with the emphasis on neuroradiological imaging and neurophysiology; all patients should be followed up by an experienced neurologist, particularly those in whom symptoms and signs are restricted to either the bulbar or spinal muscles; failure of symptom progression or development of atypical features should lead to an early reassessment; finally, patients should be informed of the diagnosis only when it is secure.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bensimon G., Lacomblez L., Meininger V. A controlled trial of riluzole in amyotrophic lateral sclerosis. ALS/Riluzole Study Group. N Engl J Med. 1994 Mar 3;330(9):585–591. doi: 10.1056/NEJM199403033300901. [DOI] [PubMed] [Google Scholar]
- Chancellor A. M., Slattery J. M., Fraser H., Swingler R. J., Holloway S. M., Warlow C. P. The prognosis of adult-onset motor neuron disease: a prospective study based on the Scottish Motor Neuron Disease Register. J Neurol. 1993 Jun;240(6):339–346. doi: 10.1007/BF00839964. [DOI] [PubMed] [Google Scholar]
- Chancellor A. M., Swingler R. J., Fraser H., Clarke J. A., Warlow C. P. Utility of Scottish morbidity and mortality data for epidemiological studies of motor neuron disease. J Epidemiol Community Health. 1993 Apr;47(2):116–120. doi: 10.1136/jech.47.2.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhry V., Corse A. M., Cornblath D. R., Kuncl R. W., Drachman D. B., Freimer M. L., Miller R. G., Griffin J. W. Multifocal motor neuropathy: response to human immune globulin. Ann Neurol. 1993 Mar;33(3):237–242. doi: 10.1002/ana.410330303. [DOI] [PubMed] [Google Scholar]
- Mulder D. W., Howard F. M., Jr Patient resistance and prognosis in amyotrophic lateral sclerosis. Mayo Clin Proc. 1976 Sep;51(9):537–541. [PubMed] [Google Scholar]
- Neary D., Snowden J. S., Mann D. M., Northen B., Goulding P. J., Macdermott N. Frontal lobe dementia and motor neuron disease. J Neurol Neurosurg Psychiatry. 1990 Jan;53(1):23–32. doi: 10.1136/jnnp.53.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot P. R., Goulding P. J., Lloyd J. J., Snowden J. S., Neary D., Testa H. J. Inter-relation between "classic" motor neuron disease and frontotemporal dementia: neuropsychological and single photon emission computed tomography study. J Neurol Neurosurg Psychiatry. 1995 May;58(5):541–547. doi: 10.1136/jnnp.58.5.541. [DOI] [PMC free article] [PubMed] [Google Scholar]


