Abstract
The interplay between immune activation and immune regulation is a fundamental aspect of the functional harmony of the immune system. This delicate balance is essential to triggering correct and effective immune responses against pathogens while preventing excessive inflammation and the immunopathogenic mechanisms of autoimmunity. The knowledge of all the mechanisms involved in immune regulation is not yet definitive, and, probably, the overall picture is much broader than what has been described in the scientific literature so far. Given the plasticity of the immune system and the diversity of organisms, it is highly probable that numerous other cells and molecules are still to be ascribed to the immune regulation process. Here, we report a general overview of how immune activation and regulation interact, based on the involvement of molecules and cells specifically dedicated to these processes. In addition, we discuss the role of TR3-56 lymphocytes as a new cellular candidate in the immune regulation landscape.
Keywords: immune regulation, immune regulatory cell phenotypes, TR3-56
1. Introduction
The immune system protects the body from infections and maintains overall health [1,2,3]. This protection occurs through the activation of the immune system, which represents a complex process by which the immune response is stimulated in response to the presence of pathogens (such as viruses, bacteria, fungi, etc.), foreign substances, or abnormal cells (e.g., cancer cells) in the body [1,2,3,4]. This process is usually called “immune activation” and can involve various cells and immune molecules harmonically acting to create a defense against these threats [1,2,3,4,5].
Immune activation processes are expressed by the innate and adaptive immune responses of the immune system, each with distinct roles and mechanisms to defend the body against infections and other threats [1,2,3,4,5].
The innate immune response is rapidly acting and represents the first line of defense, thus providing immediate but relatively non-specific protection [1,2,3,4,5,6]. In fact, the innate response does not discriminate among specific pathogens but recognizes common characteristics shared by many pathogens, such as certain molecules on the surface of the pathogen [7,8,9,10,11].
Components of the innate immune system include physical barriers such as the skin and mucous membranes, as well as cellular and biochemical elements such as phagocytes (white blood cells that engulf and digest pathogens) [7,8,9,10,11] and natural killer (NK) cells (infected host or anomalous cells) [12,13,14].
The innate response often promotes pro-inflammatory phases and is itself triggered by inflammation, which helps in the recruitment of immune cells to the site of infection and improves the body’s overall defense [15,16,17].
The adaptive immune response develops more slowly but is highly specific and targets particular pathogens precisely, adapting to the microenvironmental conditions during the immune response itself [1,2,3]. Such a response is characterized by “immunological memory”, which is a fundamental feature of the adaptive immune system offering an effector advantage upon subsequent encounters with the pathogen [1,2,3,18,19]. In this regard, after encountering a specific pathogen, the adaptive immune system “remembers” previous encounters and responds more effectively upon subsequent exposures to the same pathogen [1,2,3,18,19].
The adaptive response involves specialized white blood cells called B and T lymphocytes [1,2,3]. Briefly, B cells are immune cells specialized in the production and secretion of antibodies, proteins specifically capable of recognizing and binding to specific antigens, expressed by pathogens such as bacteria or viruses [1,2,3,20,21]. This binding can either directly neutralize pathogens or flag them for elimination by other immune cells, thereby contributing to the battle against infections and the maintenance of immune balance in the body [1,2,3,20,21]. Moreover, T cells perform various functions [1,2,3,22], including assisting B cell functions (T helper, Th) [1,2,3,23], directly killing infected cells (cytotoxic T lymphocytes, CTL) [1,2,3,24], and regulating the immune response [25]. The functions of T cells are expressed in a marked versatility (or plasticity), which takes on considerable value in coordinating immune responses, adapting to different challenges, and guaranteeing an effective but controlled defense against infections and other threats linked to the control exercised by the immune system [1,2,3,22,23,24,25].
In a perspective, immune cells have several highly specialized roles in the body, including the identification and neutralization of threats (the effector functions of immune activation), as well as the ability to activate or inhibit the response itself (the regulatory mechanisms) [1,2,3,15,16,17,18,19,20,21,22,23,24,25,26].
2. The Immune Regulation
The orchestration of the immune response is a sophisticated and intricately managed process that guarantees the immune system’s efficiency while preventing exaggerated or detrimental reactions [25,26,27,28,29,30]. Regulation involves an ample network of immune cells, signaling molecules, and regulatory mechanisms that work together to maintain immune balance and prevent immune-related diseases [25,26,27,28,29,30].
In this regard, both the inappropriate initiation and incorrect termination of the immune response can lead to various serious health issues, including chronic conditions, autoimmune diseases, and even cancer [31,32,33,34,35].
On the basis of the “danger model”, originally postulated by P. Matzinger, the initiation of immune cell responses when there is no actual threat or presence of harmful pathogens (such as viruses, bacteria, fungi, etc.) in the body represents a risk for the emergence of several immune-mediated diseases [36,37,38]. Physiologically, once the immune system has eliminated the pathogen, it should return to its basal state without expressing functional residues that are dangerous for the health of the host organism’s own components [1,2,3,4,5,6,7,8,9]. The continuation of an active immune response in the absence of a threat can seriously damage the molecular and cellular components of body tissues (the self) [1,2,3,4,5,6,7,8,9].
The inappropriate initiation and non-termination of immune effector functions, dependent on an immune regulatory failure, represents the basis for immune cells to act in an autoaggressive way in the absence of the pathogen, generating damage to healthy tissues [38,39,40,41].
2.1. The Interplay between Immune Activation and Regulation
Taking a broader perspective on the functions and organization of the immune system, the prevailing hypothesis suggests that immune responses are remarkably flexible and adaptable [42,43,44]. Individual immune cells therefore possess the ability to adapt their functional capabilities over time, responding to the specific demands of their microenvironment, whether it is to trigger an active response (the effector or activation phase) [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24] or to maintain control through immune regulation [25,26,27,28,29,30].
This intricate balancing act within the immune response evokes the concept of “immune plasticity” [45,46]. Consequently, it is reasonable to consider that disruptions in immune plasticity could serve as a major factor in the failure of both immune activation and regulation, resulting in immune system-related disorders such as immunodeficiencies [47] and autoimmune diseases [38,39,40,41].
Current research is dedicated to gaining insight into the mechanisms governing immune regulation and exploring new therapies tailored to address conditions related to the immune system [48].
2.2. The Main Features of Immune Regulation: Aspects, Molecules, and Cells
The regulation of immune responses is a complex and finely orchestrated process that involves several aspects and key mechanisms crucial to maintaining the delicate balance between an effective defense and the restoration of the state of health, avoiding harmful excessive reactions [25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48].
A peculiar feature of the immune system is the ability to distinguish between the body’s own cells and tissues (self) and foreign invaders (non-self) [1,2,3,4,5,6,7,8,9]. Discrimination between self and non-self is critical to prevent the immune system from mistakenly attacking the body cells, which can lead to autoimmune diseases [31,32,33]. Self-recognition [42,43,44] is largely based on tolerance mechanisms [42,43,44,49].
The immune system has mechanisms to recognize and tolerate self-antigens, preventing the immune response from targeting and attacking the body’s own cells and tissues [49]. Central tolerance occurs during the development of immune cells in the thymus (for T cells) and bone marrow (for B cells), where self-reactive cells are eliminated or rendered non-functional [30,49,50,51,52,53,54]. Peripheral tolerance mechanisms further suppress or regulate self-reactive immune cells in the periphery to prevent autoimmune reactions in tissue [49,55].
Cytokines are signaling molecules produced by immune cells that regulate the immune response [56]. They can have pro-inflammatory or anti-inflammatory properties. For example, pro-inflammatory cytokines like interleukin (IL)-1, IL-6, interferon-gamma (IFN-γ), and tumor necrosis factor-alpha (TNF-α) promote inflammation and immune activation [56], while anti-inflammatory cytokines like IL-10 and transforming growth factor beta (TGF-β) dampen immune responses and promote tolerance [57].
Checkpoint molecules, such as programmed cell death protein 1 (PD-1) [58] and cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) [59], are involved in regulating immune responses and preventing excessive immune activation [60]. They act as “brakes” on immune cells and can inhibit their activation and effector functions [60]. Targeting these checkpoint molecules has been successful in immunotherapy approaches, particularly in autoimmunity and cancer treatment [60].
The immune system employs feedback mechanisms to regulate its own activity. Various immune cells and molecules can produce inhibitory or activating signals that modulate the immune response [23,24,25,26,27,28,29,30,56,57,58,59,60]. These feedback mechanisms help maintain immune balance and prevent excessive or prolonged immune activation [44,45,46].
The local tissue environment can profoundly influence immune responses. The presence of specific molecules or cells in tissue can boost or dampen immune reactions [8,9,10,11,36,37,38,41,42,43,44].
All these aspects can account for the enormous value of environmental factors in determining immune plasticity and, therefore, positively or negatively influencing immune regulation [42,43,44,45,46].
The scientific literature has highlighted the role of numerous cells with regulatory functions of the immune response. In this sense, the aforementioned characteristics of immune plasticity make it highly probable that immune regulation is mediated by a large and non-definitive number of cells functionally capable of being involved in immune regulation [42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60].
In this review, we will address the synthetic description of the main cells described as possessing immune regulation ability.
Regulatory T cells (Tregs) are a specialized subset of CD4+ T lymphocytes (T cells) that play a crucial role in immune regulation and maintaining immune tolerance [26,29,30,55,61,62]. They are essential in preventing excessive immune responses and controlling immune-related diseases, including autoimmune disorders, allergies, and graft rejection in transplantation [61,62,63]. Tregs are characterized by the expression of a transcription factor called FoxP3 (Forkhead box P3), which is considered a master regulator of their development and function [62,63]. Mutations or deficiencies in FoxP3 lead to severe autoimmune diseases [61,62,63], highlighting the critical role of Tregs in immune homeostasis.
Two subtypes of Tregs have been described: the natural constitutive (nTreg) [29,61,62,63] and the inducible (iTreg) cells [61,62,63,64]. nTregs develop in the thymus and derive from some progenitor T cells that undergo a selection process conferring them regulatory properties [29,61,62,63]. nTregs are characterized by specific surface markers, such as CD4 and CD25 (interleukin-2 receptor alpha chain) [29,61,62,63]. They have a natural ability to suppress the activation and proliferation of other immune cells, including effector T cells, which helps maintain immune homeostasis and prevent autoimmune reactions [29,61,62,63]. iTregs are generated in peripheral tissues, such as the gut or sites of inflammation, in response to specific environmental cues [61,62,63,64]. The iTreg subtype arises from the differentiation of conventional CD4+ T cells (non-regulatory T cells) in response to signals from the local tissue microenvironment and the presence of certain cytokines, such as transforming growth factor-beta (TGF-β) [61,62,63,64]. iTregs can tailor their regulatory functions to specific tissues [61,62,63,64].
Tregs use various mechanisms to suppress immune responses: They secrete immunosuppressive cytokines like interleukin-10 (IL-10) and transforming growth factor-beta (TGF-β). These cytokines can suppress the activity and proliferation of other immune cells, such as T cells, B cells, and antigen-presenting cells, thereby limiting immune activation [29,61,62,63,64]; Tregs can directly interact with and suppress the function of other immune cells through cell-to-cell contact [29,61,62,63,64]. This interaction involves molecules such as cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) and lymphocyte activation gene 3 (LAG-3) on the surface of Tregs, which interact with ligands on target cells, leading to the inhibition of immune responses [63,64,65]; Tregs can also modulate the metabolic environment to suppress immune responses. They use metabolic pathways, such as increased adenosine production or the consumption of IL-2, to create an immunosuppressive milieu that dampens immune activation [61].
Tregs are crucial for maintaining self-tolerance and preventing autoimmune diseases [29,61,62,63,64,65]. They recognize self-antigens and suppress the activation and function of autoreactive T cells that could potentially cause harm to the body’s own tissues [29,61,62,63,64,65]. However, the balance between Tregs and effector T cells can be disrupted in certain conditions, leading to immune dysregulation [29,41,42,44,55,61,62,63,64,65]. The deficiency or dysfunction of Tregs can result in uncontrolled immune activation and the development of autoimmune diseases [29,41,42,44,55,61,62,63,64,65]. On the other hand, an excessive or overactive Treg response can contribute to immune suppression and hinder effective immune responses against infections or cancer [29,41,42,44,55,61,62,63,64,65].
Research on Tregs and their role in immune regulation is a rapidly evolving field. Several approaches to harnessing the therapeutic potential of Tregs in treating autoimmune diseases, allergies, transplant rejection, and other immune-related disorders have been evaluated [66,67]. Strategies include Treg-based cellular therapies and the modulation of Treg function and stability for therapeutic interventions [66,67].
CD8+ suppressor T cells represent a subtype of Tregs and have been described as having a unique ability to suppress immune responses, which may be useful in preventing autoimmune reactions [68,69,70]. CD8+ Tregs appear to be a specialized subset of cytotoxic T cells, whose functions and mechanisms of action are still not entirely clear but play several crucial roles in immune regulation [68,69,70].
In the context of T lymphocytes with immunoregulatory abilities, Type 1 (Tr1) and Type 2 (Tr2) regulatory T cells are certainly worth mentioning. The Tr1 subset plays a crucial role in regulating the immune response and maintaining immune tolerance [71]. The mechanisms and functions of Tr1 cells are not fully understood [71,72,73]. However, the scientific literature has described that Tr1 cells predominantly produce the anti-inflammatory cytokines IL-10 [71,72,73]. Such cytokines suppress the activity of other immune cells, including T cells and macrophages, dampening inflammation [71,72,73]. The ability of Tr1 cells to regulate immune responses makes them an interesting target for potential therapeutic interventions in conditions involving immune dysregulation, such as autoimmune diseases and allergies [72,73]. In this regard, it is worth noting that Tr1 cells have been described as contributing to the immune evasion of tumors by suppressing the anti-tumor immune response [72,73]. This can be a promising challenge in cancer immunotherapy. Moreover, Tr1 cells are involved in preventing excessive allergic responses by inhibiting the activation of immune cells responsible for allergy-related inflammation [73,74]. The Tr2 subset has also been described as Th3 cells and is involved in immune regulation and suppressing inflammatory responses [75,76]. They play a crucial role in maintaining immune homeostasis by dampening excessive immune activation and preventing immune-mediated tissue damage [75,76]. Tr2 cells exert their immunosuppressive effects through the secretion of TGF-β, which has anti-inflammatory properties and can inhibit the activity of various immune cells, including T cells, B cells, and APCs [75,76]. Tr2 cells have been implicated in the regulation of immune responses in a variety of contexts, including allergic reactions, autoimmune diseases, and tissue inflammation [75,76]. The differentiation and development of Tr1 and Tr2 cells are influenced by various factors, including the cytokine environment and interactions with other immune cells [77]. They can arise from different sources, including conventional CD4+ T cells that have been exposed to specific signals, as well as from the conversion of other regulatory T cell subsets [77].
Natural killer T (NKT) cells are a unique subset of immune cells that possess both T cell and natural killer cell characteristics [78,79]. These cells express both the T cell receptor (the CD3 molecule) and the natural killer cell marker (the CD56 molecule) on their surface [78,79]. NKT cells play a critical role in the immune response by bridging the innate and adaptive immune systems [80]. They recognize a variety of lipid and glycolipid antigens presented by the non-classical major histocompatibility complex (MHC) molecule, CD1d [80,81]. Upon activation, NKT cells rapidly produce large amounts of cytokines, such as IFN-γ and IL-4, which can modulate the immune response and suppress the activation and proliferation of other immune cells, such as T cells and NKs [79,80]. Moreover, NKT cells have been found to play a role in various immune-related diseases and conditions, including infectious diseases, cancer, and autoimmune disorders [82,83,84,85]. Their functional plasticity and ability to modulate immune responses render them a promising target for immunotherapy approaches [84].
Some other cell types, with various mechanisms, have been described as capable of regulating immune responses.
In this regard, the anti-inflammatory role of regulatory B cells (Bregs) has been described [86]. Bregs represent a subset of B lymphocytes with immunosuppressive functions, mainly mediated by the production of anti-inflammatory cytokines such as IL-10, IL-35, and TGF-β [86,87]. Bregs are characterized by differential expression of CD5 and CD1d in the mouse immune system and CD24 and CD38 in the human immune system [86,87,88]. Some evidence suggests that Bregs are involved in infections, inflammation, and autoimmunity [86].
NK cells [1,2,3,4,5,12,13,14,89] are a vital component of the innate immune system, and although their primary role is to recognize and eliminate infected or abnormal cells, a large body of literature suggests that they also play a role in immune regulation [90,91,92]. NK cells recognize and kill tissue cells that display abnormal characteristics, such as infected cells, tumor cells, or cells lacking major histocompatibility complex class I (MHC-I) molecules, based on the missing-self hypothesis [93]. NK cytotoxic function helps prevent the spread of infections and the development of tumors [89,93]. NK cells can also produce numerous cytokines that have both pro-inflammatory and immunosuppressive effects, thus contributing to immune regulation [90,91,92,93]. In addition, they also contribute to immune tolerance by shedding potentially harmful autoreactive or infected cells and sparing healthy ones [94,95,96,97]. NK cells and Tregs can interact, influencing the balance between the activation and inhibition of immune responses [98,99]. Furthermore, NK cells play a crucial role in establishing immune tolerance during pregnancy, facilitating the development of a semi-allogeneic fetus (with different genetic material) within the maternal environment and preventing its rejection [92].
Gamma delta (γδ) T cells are a subset of T lymphocytes that possess a T cell receptor (TCR) composed of γ and δ chains, in contrast to the more common α and β chains of conventional T cells [100,101]. γδ T cells are a relatively small population of T cells in the peripheral blood and have more limited diversity than αβ-TCRs, which allows them to recognize a distinct set of antigens, including non-peptide molecules [101,102]. γδ T cells are often found in tissues such as the skin, the intestinal mucosa, and the respiratory epithelium [102]. γδ T cells contribute to immune surveillance by recognizing and responding to a wide range of stress-induced or non-peptide antigens, such as those produced by infected or transformed cells [101,102]. They can also produce numerous cytokines, such as IFN-γ and TNF-α, which influence the immune response [101]. For their production and roles, they have been implicated in some autoimmune diseases, where they can contribute to inflammation and tissue damage [101].
Dendritic cells (DCs) and macrophages are key players in the immune system, and their versatility extends beyond their role as immune sentinels and scavengers and their known ability to present antigens to T lymphocytes [1,2,3,4,5,6,7,8,9,10]. Indeed, DCs and macrophages are specialized antigen-presenting cells (APCs) that have attracted attention for their intriguing immunomodulatory properties, which allow them to fine-tune immune responses based on the unique signals they encounter and the specific context of the immune challenge [1,2,3,4,5,6,7,8,9,10]. DCs can also interact with Tregs and other immune modulators to further optimize the immune response [103]. Therefore, DCs serve as central coordinators in the immune response, ensuring the body’s defenses are alert against threats (immunogenic DCs) and the immune responses are contained to prevent damage to one’s own tissues (tolerogenic DCs) [104]. This immunomodulation testifies to the complexity of our immune system and its ability to maintain balance in the face of different challenges. Macrophages can assume distinct functional states based on the signals they receive. They can be “classically activated” (M1) to promote inflammation and defense against pathogens or “alternatively activated” (M2) to resolve inflammation, promote tissue repair, and suppress excessive immune responses, reflecting their ability to influence immune modulation [105,106].
Myeloid-derived suppressor cells (MDSCs) represent a heterogeneous group of leukocytes with the ability to suppress immune responses [107,108]. MDSCs originate from myeloid progenitor cells [107,108]. Under certain pathological conditions, such as chronic inflammation or cancer, MDSCs can undergo expansion and become an important component of the immune cell population [107,108].
Finally, the literature highlights a pathogenetic role for some clusters of circulating cells (CIC cells) [109]. CICs express different genetic markers (see previous reference), and there is evidence that the loss of function of specific CIC populations is a contributing factor in T1D [109,110].
3. A New Cell Candidate for Immune Regulation: The TR3-56
In 2020, we investigated the role of CD3+CD56+ regulatory T cells in the progression of type 1 diabetes (T1D) [111]. We found that individuals with T1D had a significant reduction in the number of CD3+CD56+ regulatory T cells compared to healthy individuals [111]. Such an occurrence was associated with an increase in the activation and effector functions of CD8+ T cells, which are known to contribute to the destruction of insulin-producing beta cells in the pancreas [111]. The study also demonstrated that the reduced numbers of CD3+CD56+ regulatory T cells correlated with disease progression in T1D patients. The decline in these regulatory T cells was associated with increased insulin requirements, indicating a worsening of the disease [111]. Overall, the study suggested that the loss of CD3+CD56+ regulatory T cells contributes to the progression of T1D by allowing for the activation and effector functions of CD8+ T cells. The findings highlight the importance of these regulatory T cells in maintaining immune tolerance and controlling autoimmune responses in T1D.
In this study, we also demonstrated that this CD3+CD56+ T regulatory subset [111] is different from the NKT subset [78,79,80,81,82,83,84,85]. Specifically, CD3+CD56+ regulatory cells (i) are not CD1d-restricted; (ii) do not express Valpha24/Vbeta11 chains but display a heterogeneous V-beta repertoire; and (iii) are unable to kill K562 cells in vitro. In addition, (iv) only 1–5% of CD1d-restricted T cells are positive for the CD56 molecule. We also demonstrated that this CD3+CD56+ regulatory subset is genetically, metabolically, and functionally distinct from the NKT subset [111].
We called this subset TR3-56 [111].
In addition, we investigated the role of bone marrow TR3-56 cells in patients with very-low-risk/low-risk myelodysplastic syndrome (MDS) [112,113] according to the Revised International Prognostic Scoring System (IPSS-R) [112,113]. MDS comprises a group of blood disorders characterized by ineffective hematopoiesis and a consistent risk of leukemia evolution [112]. We found that in patients with very-low-risk/low-risk MDS, there was an inverse association between the number of TR3-56 cells and the activation and expansion of bone marrow cytotoxic T cells [112,113]. Such evidence suggests that TR3-56 cells may play a role in regulating the activity of cytotoxic T cells in the bone marrow. Furthermore, the study showed that TR3-56 cells from MDS patients exhibited a regulatory phenotype and were capable of suppressing the proliferation and activation of cytotoxic T cells [112,113]. This indicates that TR3-56 cells may have immunosuppressive functions in the bone marrow microenvironment, as we previously described for Tregs [114]. Indeed, the imbalance between TR3-56 cells and cytotoxic T cells in the bone marrow of very-low-risk/low-risk MDS patients may contribute to the immune-mediated elimination of healthy hematopoiesis, affecting MDS pathogenesis. On the other hand, an increased number and activity of TR3-56 cells could contribute to the generation of an immune-suppressed microenvironment in high-risk MDS, which may contribute to the progression of acute leukemia [112,113].
Moreover, we also described the role of TR3-56 in chronic lymphocytic leukemia (CLL) with stable disease [115]. We observed that the Treg and TR3-56 percentages decreased when evaluated in the context of total lymphocytes. However, when specifically analyzed in the T cell compartment alone, the Treg and TR3-56 percentages decreased in CLL subjects. Furthermore, the absolute number of circulating Treg and TR3-56 cells is significantly higher in CLL patients than in healthy controls. Since lymphocytes are mainly composed of B cells in CLL patients, the small percentage of T cells within the lymphocyte compartment appears to exhibit a preferential expansion of the Treg and TR3-56 regulatory cell subsets as a possible immune escape mechanism [115].
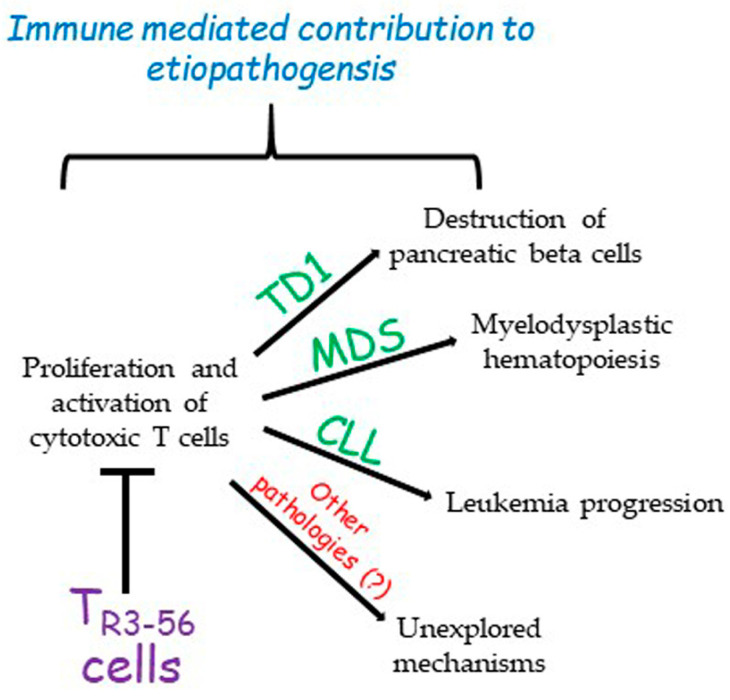
The role of TR3-56 cells in the regulation of immune response in specific contexts such as diabetes, cancer, or MDS opens a new scenario towards the possibility of individuating possible molecular targets on these cells to tune the control that this cell subset exerts over the immune system (Figure 1).
Figure 1.
The described role of TR3-56 cells. So far, TR3-56 cells have been described as playing a role in the determinism of type 1 diabetes (TD1), myelodysplastic syndromes (MDSs), and chronic lymphocytic leukemia (CLL). However, it is possible that this regulatory cell population could be involved in other pathologies. This contribution remains to be explored.
For instance, diabetes represents a typical disease for which an effective therapy has not been precisely identified, considering that insulin administration per se does not preserve organs and tissues from the pathological consequences of a hyperglycemic environment [116,117,118]. Indeed, focusing on the role of TR3-56 cells in their modulatory action over CD8+ cytotoxic lymphocytes could represent a favorable target to keep the self-destruction of pancreatic cells releasing insulin under control. The identification of specific targets/pathways on these cells could lead to the generation of monoclonal antibodies or small synthetic molecules able to intervene in the treatment of diabetes, better controlling the disease progression and allowing for second-organ preservation. Similarly, this approach could be pursued in the fields of cancer and MDS.
4. Previous Observations on CD3+CD56+ Co-Expressing T Cells in Cancer Immune Surveillance
Several studies in recent decades have detected a T lymphocyte population co-expressing CD3+CD56+ molecules, often defining it as NKT-like cells, giving a confusing and non-definitive characterization of the phenotype and role of these cells. CD3+CD56+ T cells are increased in the peripheral blood of patients with solid tumors [119,120]. Such immune cells have been observed in women undergoing in vitro fertilization treatments [121]. A role for CD3+CD56+ T cells has been reported in the pathogenesis of non-alcoholic fatty liver disease [122] and in the development of allergic and autoimmune disorders [123]. Several studies have evaluated the contribution of the CD3+CD56+ T cell population in the pathophysiology and evolution of hematological malignancies: CD3+CD56+ T cell dysfunction has been hypothesized to contribute to the failure of the host immune response against leukemic blasts in acute myeloid and acute lymphocytic leukemia patients [124]; CD3+CD56+ T cells are expanded in the bone marrow of patients with chronic myeloid leukemia (CML) [125] and are decreased in CML patients treated with tyrosine kinase inhibitors [126]; and a higher proportion of CD3+CD56+ lymphocytes has been revealed in lymph nodes affected by large B cell lymphoma [127].
Overall, all these data reveal a general increase in the number of CD3+CD56+ T lymphocytes in cancer patients without addressing a possible explanation for this phenomenon.
Therefore, it is legitimate to argue that the current knowledge does not allow a definitive understanding of these cells. However, a more extensive phenotypic and functional characterization of all the lymphocyte subtypes co-expressing CD3 and CD56 represents the only approach to determining their role and possible involvement in effector and/or immune regulation mechanisms. In this regard, our original and pioneering research on TR3-56 cells in the TD1, MDS, and CLL models revealed the phenotypic and functional characteristics of this distinct subpopulation of CD3+ CD56+ T cells, highlighting its distinctiveness in immunoregulation [111,112,113,114].
Nonetheless, it is currently not possible to exclude that CD3+CD56+ cell phenotypes are more numerous or that plastic elements may influence their functions.
5. Conclusions
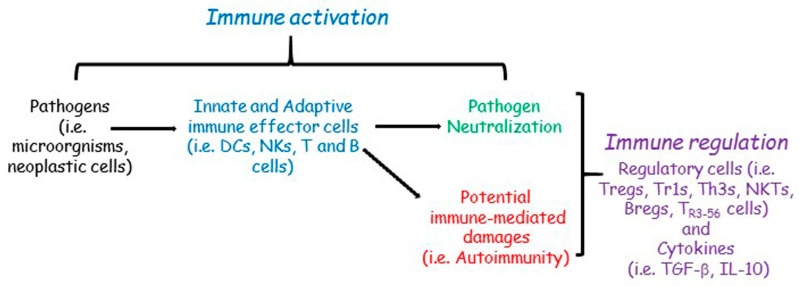
The immune response is ultimately the result of a balance between activation and inhibition; the success and/or failure of the immune response depends on a set of genetic/epigenetic factors and an array of molecules, cells, and tissue microenvironments involved in both activating and inhibitory mechanisms of immune regulation (Figure 2).
Figure 2.
Simplified immune plasticity network. Pathogens activate the innate and adaptive immune effector cells (dendritic cells, DCs; natural killers, NKs; T and B cells) that induce pathogen neutralization during the immune activation phase. However, immune activation could also exert potential immune-mediated damage as a sort of side effect. The immune regulation phase (T regulatory cells, Tregs; Type 1 regulatory cells, Tr1s; T helper 3 cells, Th3s; natural killer T cells, NKTs; B regulatory cells, Bregs; T CD3+ CD56+ regulatory cells, TR3-56 cells; transforming growth factor beta, TGF-β; interleukin 10, IL-10) modulates immune activation and avoids immune-mediated damages.
The knowledge of all the mechanisms involved in immune regulation is not yet definitive, and, probably, the overall picture is much broader than what has been described in the scientific literature so far. Given the plasticity of the immune system and the diversity of organisms, it is highly probable that numerous other cells and molecules are still to be ascribed to the immune regulation process.
Therefore, it cannot be excluded that other factors and cells other than those reported in this review should be taken into consideration to fully understand the complex harmony between the activation and inhibition of the immune system.
At the same time, it is equally probable that some current knowledge about the role of cells that have hitherto been specifically described as immunoregulatory might need to be revised. Such cells might have different, broader, and more plastic roles in the complex balance between the activation and inhibition of innate and adaptive immune responses.
In this complex framework, it appears highly compelling to propose to the scientific community the investigation of some “new cells”, such as TR3-56, in their role as immunoregulatory cell populations, contributing to deepening our knowledge of the immune system and its plastic and dynamic complexity.
Author Contributions
Conceptualization, F.C., V.R., S.L., R.M., V.B., G.R. and G.T.; writing—original draft preparation, F.C. and G.T.; writing—review and editing, F.C., V.R., S.L., V.B., G.R. and G.T.; supervision, G.R. and G.T. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Parkin J., Cohen B. An overview of the immune system. Lancet. 2001;357:1777–1789. doi: 10.1016/S0140-6736(00)04904-7. [DOI] [PubMed] [Google Scholar]
- 2.Delves P.J., Roitt I.M. The immune system. First of two parts. N. Engl. J. Med. 2000;343:37–49. doi: 10.1056/NEJM200007063430107. [DOI] [PubMed] [Google Scholar]
- 3.Janeway C.A., Jr. Approaching the asymptote? Evolution and revolution in immunology. Cold Spring Harb. Symp. Quant. Biol. 1989;54:1–13. doi: 10.1101/SQB.1989.054.01.003. [DOI] [PubMed] [Google Scholar]
- 4.Paul W.E. Infectious diseases and the immune system. Sci. Am. 1993;269:90–97. doi: 10.1038/scientificamerican0993-90. [DOI] [PubMed] [Google Scholar]
- 5.Medzhitov R. Recognition of microorganisms and activation of the immune response. Nature. 2007;449:819–826. doi: 10.1038/nature06246. [DOI] [PubMed] [Google Scholar]
- 6.Vivier E., Malissen B. Innate and adaptive immunity: Specificities and signaling hierarchies revisited. Nat. Immunol. 2005;6:17–21. doi: 10.1038/ni1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janeway C.A., Jr., Medzhitov R. Innate immune recognition. Annu. Rev. Immunol. 2002;20:197–216. doi: 10.1146/annurev.immunol.20.083001.084359. [DOI] [PubMed] [Google Scholar]
- 8.Mogensen T.H. Pathogen recognition and inflammatory signaling in innate immune defenses. Clin. Microbiol. Rev. 2009;22:240–273. doi: 10.1128/CMR.00046-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Takeda K., Akira S. Toll-like receptors. Curr. Protoc. Immunol. 2015;109:11–14. doi: 10.1002/0471142735.im1412s109. [DOI] [PubMed] [Google Scholar]
- 10.Riera Romo M., Pérez-Martínez D., Castillo Ferrer C. Innate immunity in vertebrates: An overview. Immunology. 2016;148:125–139. doi: 10.1111/imm.12597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amarante-Mendes G.P., Adjemian S., Branco L.M., Zanetti L.C., Weinlich R., Bortoluci K.R. Pattern Recognition Receptors and the Host Cell Death Molecular Machinery. Front. Immunol. 2018;9:2379. doi: 10.3389/fimmu.2018.02379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freud A.G., Caligiuri M.A. Human natural killer cell development. Immunol. Rev. 2006;214:56–72. doi: 10.1111/j.1600-065X.2006.00451.x. [DOI] [PubMed] [Google Scholar]
- 13.Chiossone L., Dumas P.Y., Vienne M., Vivier E. Natural killer cells and other innate lymphoid cells in cancer. Nat. Rev. Immunol. 2018;18:671–688. doi: 10.1038/s41577-018-0061-z. [DOI] [PubMed] [Google Scholar]
- 14.Shin E., Bak S.H., Park T., Kim J.W., Yoon S.R., Jung H., Noh J.Y. Understanding NK cell biology for harnessing NK cell therapies: Targeting cancer and beyond. Front. Immunol. 2023;14:1192907. doi: 10.3389/fimmu.2023.1192907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Netea M.G., Schlitzer A., Placek K., Joosten L.A.B., Schultze J.L. Innate and Adaptive Immune Memory: An Evolutionary Continuum in the Host’s Response to Pathogens. Cell Host Microbe. 2019;25:13–26. doi: 10.1016/j.chom.2018.12.006. [DOI] [PubMed] [Google Scholar]
- 16.Cronkite D.A., Strutt T.M. The Regulation of Inflammation by Innate and Adaptive Lymphocytes. J. Immunol. Res. 2018;2018:1467538. doi: 10.1155/2018/1467538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumar V. Innate lymphoid cell and adaptive immune cell cross-talk: A talk meant not to forget. J. Leukoc. Biol. 2020;108:397–417. doi: 10.1002/JLB.4MIR0420-500RRR. [DOI] [PubMed] [Google Scholar]
- 18.Zinkernagel R.M. On differences between immunity and immunological memory. Curr. Opin. Immunol. 2002;14:523–536. doi: 10.1016/S0952-7915(02)00367-9. [DOI] [PubMed] [Google Scholar]
- 19.Lau C.M., Sun J.C. The widening spectrum of immunological memory. Curr. Opin. Immunol. 2018;54:42–49. doi: 10.1016/j.coi.2018.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cyster J.G., Allen C.D.C. B Cell Responses: Cell Interaction Dynamics and Decisions. Cell. 2019;177:524–540. doi: 10.1016/j.cell.2019.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akkaya M., Kwak K., Pierce S.K. B cell memory: Building two walls of protection against pathogens. Nat. Rev. Immunol. 2020;20:229–238. doi: 10.1038/s41577-019-0244-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sun L., Su Y., Jiao A., Wang X., Zhang B. T cells in health and disease. Signal Transduct. Target Ther. 2023;8:235. doi: 10.1038/s41392-023-01471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zielinski C.E. T helper cell subsets: Diversification of the field. Eur. J. Immunol. 2023:e2250218. doi: 10.1002/eji.202250218. [DOI] [PubMed] [Google Scholar]
- 24.Barry M., Bleackley R. Cytotoxic T lymphocytes: All roads lead to death. Nat. Rev. Immunol. 2002;2:401–409. doi: 10.1038/nri819. [DOI] [PubMed] [Google Scholar]
- 25.Grover P., Goel P.N., Greene M.I. Regulatory T Cells: Regulation of Identity and Function. Front. Immunol. 2021;12:750542. doi: 10.3389/fimmu.2021.750542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chang J., Wherry E., Goldrath A. Molecular regulation of effector and memory T cell differentiation. Nat. Immunol. 2014;15:1104–1115. doi: 10.1038/ni.3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pelanda R., Piccirillo C.A. Tolerance, immune regulation, and autoimmunity: Cells and cytokines that make a difference. Curr. Opin. Immunol. 2008;20:629–631. doi: 10.1016/j.coi.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Devenish L.P., Mhlanga M.M., Negishi Y. Immune Regulation in Time and Space: The Role of Local- and Long-Range Genomic Interactions in Regulating Immune Responses. Front. Immunol. 2021;12:662565. doi: 10.3389/fimmu.2021.662565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sakaguchi S. Naturally arising CD4+ regulatory T cells for immunologic self-tolerance and negative control of immune responses. Annu. Rev. Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 30.Sakaguchi S., Miyara M., Costantino C.M., Hafler D.A. FOXP3+ regulatory T cells in the human immune system. Nat. Rev. Immunol. 2010;10:490–500. doi: 10.1038/nri2785. [DOI] [PubMed] [Google Scholar]
- 31.Davidson A., Diamond B. Autoimmune diseases. N. Engl. J. Med. 2001;345:340–350. doi: 10.1056/NEJM200108023450506. [DOI] [PubMed] [Google Scholar]
- 32.McInnes I.B., Gravallese E.M. Immune-mediated inflammatory disease therapeutics: Past, present and future. Nat. Rev. Immunol. 2021;21:680–686. doi: 10.1038/s41577-021-00603-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang L., Wang F.S., Gershwin M.E. Human autoimmune diseases: A comprehensive update. J. Intern. Med. 2015;278:369–395. doi: 10.1111/joim.12395. [DOI] [PubMed] [Google Scholar]
- 34.Fridman W.H., Pagès F., Sautès-Fridman C., Galon J. The immune contexture in human tumors: Impact on clinical outcome. Nat. Rev. Cancer. 2012;12:298–306. doi: 10.1038/nrc3245. [DOI] [PubMed] [Google Scholar]
- 35.O’Donnell J.S., Teng M.W.L., Smyth M.J. Cancer immunoediting and resistance to T cell-based immunotherapy. Nat. Rev. Clin. Oncol. 2019;16:151–167. doi: 10.1038/s41571-018-0142-8. [DOI] [PubMed] [Google Scholar]
- 36.Matzinger P. Tolerance, danger, and the extended family. Annu. Rev. Immunol. 1994;12:991–1045. doi: 10.1146/annurev.iy.12.040194.005015. [DOI] [PubMed] [Google Scholar]
- 37.Matzinger P. The danger model: A renewed sense of self. Science. 2002;296:301–305. doi: 10.1126/science.1071059. [DOI] [PubMed] [Google Scholar]
- 38.Matzinger P. The evolution of the danger theory. Interview by Lauren Constable, Commissioning Editor. Expert Rev. Clin. Immunol. 2012;8:311–317. doi: 10.1586/eci.12.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kivity S., Agmon-Levin N., Blank M., Shoenfeld Y. Infections and autoimmunity-friends or foes? Trends Immunol. 2009;30:409–414. doi: 10.1016/j.it.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 40.Sundaresan B., Shirafkan F., Ripperger K., Rattay K. The Role of Viral Infections in the Onset of Autoimmune Diseases. Viruses. 2023;15:782. doi: 10.3390/v15030782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rijkers G.T., Riccardi C., Kroese F.G.M. Editorial: Defects in Regulation: How, Where and When the Immune System Can Go Wrong. Front. Immunol. 2021;12:746418. doi: 10.3389/fimmu.2021.746418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Van Parijs L., Abbas A.K. Homeostasis and self-tolerance in the immune system: Turning lymphocytes off. Science. 1998;280:243–248. doi: 10.1126/science.280.5361.243. [DOI] [PubMed] [Google Scholar]
- 43.Chovatiya R., Medzhitov R. Stress, inflammation, and defense of homeostasis. Mol. Cell. 2014;54:281–288. doi: 10.1016/j.molcel.2014.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Huntington N.D., Gray D.H. Immune homeostasis in health and disease. Immunol. Cell Biol. 2018;96:451–452. doi: 10.1111/imcb.12043. [DOI] [PubMed] [Google Scholar]
- 45.Laurent P., Jolivel V., Manicki P., Chiu L., Contin-Bordes C., Truchetet M.E., Pradeu T. Immune-Mediated Repair: A Matter of Plasticity. Front. Immunol. 2017;8:454. doi: 10.3389/fimmu.2017.00454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Margraf A., Perretti M. Immune Cell Plasticity in Inflammation: Insights into Description and Regulation of Immune Cell Phenotypes. Cells. 2022;11:1824. doi: 10.3390/cells11111824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tuano K.S., Seth N., Chinen J. Secondary immunodeficiencies: An overview. Ann. Allergy Asthma Immunol. 2021;127:617–626. doi: 10.1016/j.anai.2021.08.413. [DOI] [PubMed] [Google Scholar]
- 48.Waldman A.D., Fritz J.M., Lenardo M.J. A guide to cancer immunotherapy: From T cell basic science to clinical practice. Nat. Rev. Immunol. 2020;20:651–668. doi: 10.1038/s41577-020-0306-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schwartz R.H. Historical overview of immunological tolerance. Cold Spring Harb. Perspect. Biol. 2012;4:a006908. doi: 10.1101/cshperspect.a006908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Burnet F.M. A modification of Jerne’s theory of antibody production using the concept of clonal selection. CA Cancer J. Clin. 1976;26:119–121. doi: 10.3322/canjclin.26.2.119. [DOI] [PubMed] [Google Scholar]
- 51.Tiegs S.L., Russell D.M., Nemazee D. Receptor editing in self-reactive bone marrow B cells. J. Exp. Med. 1993;177:1009–1020. doi: 10.1084/jem.177.4.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kappler J.W., Roehm N., Marrack P. T cell tolerance by clonal elimination in the thymus. Cell. 1987;49:273–280. doi: 10.1016/0092-8674(87)90568-X. [DOI] [PubMed] [Google Scholar]
- 53.Surh C.D., Sprent J. T-cell apoptosis detected in situ during positive and negative selection in the thymus. Nature. 1994;372:100–103. doi: 10.1038/372100a0. [DOI] [PubMed] [Google Scholar]
- 54.Nishizuka Y., Sakakura T. Thymus and reproduction: Sex-linked dysgenesia of the gonad after neonatal thymectomy in mice. Science. 1969;166:753–755. doi: 10.1126/science.166.3906.753. [DOI] [PubMed] [Google Scholar]
- 55.Sakaguchi S., Yamaguchi T., Nomura T., Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133:775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 56.Kany S., Vollrath J.T., Relja B. Cytokines in Inflammatory Disease. Int. J. Mol. Sci. 2019;20:6008. doi: 10.3390/ijms20236008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chen Z., Bozec A., Ramming A., Schett G. Anti-inflammatory and immune-regulatory cytokines in rheumatoid arthritis. Nat. Rev. Rheumatol. 2019;15:9–17. doi: 10.1038/s41584-018-0109-2. [DOI] [PubMed] [Google Scholar]
- 58.Yi M., Zheng X., Niu M., Zhu S., Ge H., Wu K. Combination strategies with PD-1/PD-L1 blockade: Current advances and future directions. Mol. Cancer. 2022;21:28. doi: 10.1186/s12943-021-01489-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Azimnasab-Sorkhabi P., Soltani-Asl M., Kfoury Junior J.R. Cytotoxic T-lymphocyte-associated protein 4 (CTLA-4) as an undetermined tool in tumor cells. Hum. Cell. 2023;36:1225–1232. doi: 10.1007/s13577-023-00893-8. [DOI] [PubMed] [Google Scholar]
- 60.Sharma P., Goswami S., Raychaudhuri D., Siddiqui B.A., Singh P., Nagarajan A., Liu J., Subudhi S.K., Poon C., Gant K.L., et al. Immune checkpoint therapy-current perspectives and future directions. Cell. 2023;186:1652–1669. doi: 10.1016/j.cell.2023.03.006. [DOI] [PubMed] [Google Scholar]
- 61.Galgani M., De Rosa V., La Cava A., Matarese G. Role of Metabolism in the Immunobiology of Regulatory T Cells. J. Immunol. 2016;197:2567–2675. doi: 10.4049/jimmunol.1600242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Panduro M., Benoist C., Mathis D. Tissue Tregs. Annu. Rev. Immunol. 2016;34:609–633. doi: 10.1146/annurev-immunol-032712-095948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sakaguchi S., Mikami N., Wing J.B., Tanaka A., Ichiyama K., Ohkura N. Regulatory T Cells and Human Disease. Annu. Rev. Immunol. 2020;38:541–566. doi: 10.1146/annurev-immunol-042718-041717. [DOI] [PubMed] [Google Scholar]
- 64.Zhu J., Yamane H., Paul W.E. Differentiation of effector CD4 T cell populations. Annu. Rev. Immunol. 2010;28:445–489. doi: 10.1146/annurev-immunol-030409-101212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Corthay A. How do regulatory T cells work? Scand. J. Immunol. 2009;70:326–336. doi: 10.1111/j.1365-3083.2009.02308.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tanaka A., Sakaguchi S. Targeting Treg cells in cancer immunotherapy. Eur. J. Immunol. 2019;49:1140–1146. doi: 10.1002/eji.201847659. [DOI] [PubMed] [Google Scholar]
- 67.Giganti G., Atif M., Mohseni Y., Mastronicola D., Grageda N., Povoleri G.A., Miyara M., Scottà C. Treg cell therapy: How cell heterogeneity can make the difference. Eur. J. Immunol. 2021;51:39–55. doi: 10.1002/eji.201948131. [DOI] [PubMed] [Google Scholar]
- 68.Jiang H., Zhang S.I., Pernis B. Role of CD8+ T cells in murine experimental allergic encephalomyelitis. Science. 1992;256:1213–1215. doi: 10.1126/science.256.5060.1213. [DOI] [PubMed] [Google Scholar]
- 69.Li S., Xie Q., Zeng Y., Zou C., Liu X., Wu S., Deng H., Xu Y., Li X.C., Dai Z. A naturally occurring CD8(+)CD122(+) T-cell subset as a memory-like Treg family. Cell Mol. Immunol. 2014;11:326–331. doi: 10.1038/cmi.2014.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mishra S., Srinivasan S., Ma C., Zhang N. CD8+ Regulatory T Cell—A Mystery to Be Revealed. Front. Immunol. 2021;12:708874. doi: 10.3389/fimmu.2021.708874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Groux H., O’Garra A., Bigler M., Rouleau M., Antonenko S., de Vries J.E., Roncarolo M.G. A CD4+ T-cell subset inhibits antigen-specific T-cell responses and prevents colitis. Nature. 1997;389:737–742. doi: 10.1038/39614. [DOI] [PubMed] [Google Scholar]
- 72.Battaglia M., Gregori S., Bacchetta R., Roncarolo M.G. Tr1 cells: From discovery to their clinical application. Semin. Immunol. 2006;18:120–127. doi: 10.1016/j.smim.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 73.Roncarolo M.G., Gregori S., Bacchetta R., Battaglia M., Gagliani N. The Biology of T Regulatory Type 1 Cells and Their Therapeutic Application in Immune-Mediated Diseases. Immunity. 2018;49:1004–1019. doi: 10.1016/j.immuni.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 74.Matsuda M., Terada T., Kitatani K., Kawata R., Nabe T. Roles of type 1 regulatory T (Tr1) cells in allergen-specific immunotherapy. Front. Allergy. 2022;3:981126. doi: 10.3389/falgy.2022.981126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Weiner H.L. Oral tolerance: Immune mechanisms and the generation of Th3-type TGF-beta-secreting regulatory cells. Microbes Infect. 2001;3:947–954. doi: 10.1016/S1286-4579(01)01456-3. [DOI] [PubMed] [Google Scholar]
- 76.Weiner H.L. Induction and mechanism of action of transforming growth factor-beta-secreting Th3 regulatory cells. Immunol. Rev. 2001;182:207–214. doi: 10.1034/j.1600-065X.2001.1820117.x. [DOI] [PubMed] [Google Scholar]
- 77.Horwitz D.A., Zheng S.G., Gray J.D. The role of the combination of IL-2 and TGF-beta or IL-10 in the generation and function of CD4+ CD25+ and CD8+ regulatory T cell subsets. J. Leukoc. Biol. 2003;74:471–478. doi: 10.1189/jlb.0503228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Makino Y., Kanno R., Ito T., Higashino K., Taniguchi M. Predominant expression of invariant V alpha 14+ TCR alpha chain in NK1.1+ T cell populations. Int. Immunol. 1995;7:1157–1161. doi: 10.1093/intimm/7.7.1157. [DOI] [PubMed] [Google Scholar]
- 79.Hammond K.J., Pelikan S.B., Crowe N.Y., Randle-Barrett E., Nakayama T., Taniguchi M., Smyth M.J., van Driel I.R., Scollay R., Baxter A.G., et al. NKT cells are phenotypically and functionally diverse. Eur. J. Immunol. 1999;29:3768–3781. doi: 10.1002/(SICI)1521-4141(199911)29:11<3768::AID-IMMU3768>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 80.Godfrey D.I., MacDonald H.R., Kronenberg M., Smyth M.J., Van Kaer L. NKT cells: What’s in a name? Nat. Rev. Immunol. 2004;4:231–237. doi: 10.1038/nri1309. [DOI] [PubMed] [Google Scholar]
- 81.Gadola S.D., Dulphy N., Salio M., Cerundolo V. Valpha24-JalphaQ-independent, CD1d-restricted recognition of alpha-galactosylceramide by human CD4(+) and CD8alphabeta(+) T lymphocytes. J. Immunol. 2002;168:5514–5520. doi: 10.4049/jimmunol.168.11.5514. [DOI] [PubMed] [Google Scholar]
- 82.Vogt S., Mattner J. NKT Cells Contribute to the Control of Microbial Infections. Front. Cell Infect. Microbiol. 2021;11:718350. doi: 10.3389/fcimb.2021.718350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McEwen-Smith R.M., Salio M., Cerundolo V. The regulatory role of invariant NKT cells in tumor immunity. Cancer Immunol. Res. 2015;3:425–435. doi: 10.1158/2326-6066.CIR-15-0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kriegsmann K., Kriegsmann M., von Bergwelt-Baildon M., Cremer M., Witzens-Harig M. NKT cells—New players in CAR cell immunotherapy? Eur. J. Haematol. 2018;101:750–757. doi: 10.1111/ejh.13170. [DOI] [PubMed] [Google Scholar]
- 85.Van Kaer L., Wu L. Therapeutic Potential of Invariant Natural Killer T Cells in Autoimmunity. Front. Immunol. 2018;9:519. doi: 10.3389/fimmu.2018.00519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rosser E.C., Mauri C. Regulatory B cells: Origin, phenotype, and function. Immunity. 2015;42:607–612. doi: 10.1016/j.immuni.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 87.Catalán D., Mansilla M.A., Ferrier A., Soto L., Oleinika K., Aguillón J.C., Aravena O. Immunosuppressive Mechanisms of Regulatory B Cells. Front. Immunol. 2021;12:611795. doi: 10.3389/fimmu.2021.611795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dasgupta S., Dasgupta S., Bandyopadhyay M. Regulatory B cells in infection, inflammation, and autoimmunity. Cell Immunol. 2020;352:104076. doi: 10.1016/j.cellimm.2020.104076. [DOI] [PubMed] [Google Scholar]
- 89.Quatrini L., Della Chiesa M., Sivori S., Mingari M.C., Pende D., Moretta L. Human NK cells, their receptors and function. Eur. J. Immunol. 2021;51:1566–1579. doi: 10.1002/eji.202049028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sivori S., Della Chiesa M., Carlomagno S., Quatrini L., Munari E., Vacca P., Tumino N., Mariotti F.R., Mingari M.C., Pende D., et al. Inhibitory Receptors and Checkpoints in Human NK Cells, Implications for the Immunotherapy of Cancer. Front. Immunol. 2020;11:2156. doi: 10.3389/fimmu.2020.02156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kucuksezer U.C., Aktas Cetin E., Esen F., Tahrali I., Akdeniz N., Gelmez M.Y., Deniz G. The Role of Natural Killer Cells in Autoimmune Diseases. Front. Immunol. 2021;12:622306. doi: 10.3389/fimmu.2021.622306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang F., Qualls A.E., Marques-Fernandez L., Colucci F. Biology and pathology of the uterine microenvironment and its natural killer cells. Cell Mol. Immunol. 2021;18:2101–2113. doi: 10.1038/s41423-021-00739-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ljunggren H.G., Kärre K. In search of the ‘missing self’: MHC molecules and NK cell recognition. Immunol. Today. 1990;11:237–244. doi: 10.1016/0167-5699(90)90097-S. [DOI] [PubMed] [Google Scholar]
- 94.Carbone E., Terrazzano G., Ruggiero G., Zanzi D., Ottaiano A., Manzo C., Kärre K., Zappacosta S. Recognition of autologous dendritic cells by human NK cells. Eur. J. Immunol. 1999;29:4022–4429. doi: 10.1002/(SICI)1521-4141(199912)29:12<4022::AID-IMMU4022>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 95.Terrazzano G., Pisanti S., Grimaldi S., Sica M., Fontana S., Carbone E., Zappacosta S., Ruggiero G. Interaction between natural killer and dendritic cells: The role of CD40, CD80 and major histocompatibility complex class i molecules in cytotoxicity induction and interferon-gamma production. Scand. J. Immunol. 2004;59:356–362. doi: 10.1111/j.0300-9475.2003.01387.x. [DOI] [PubMed] [Google Scholar]
- 96.Terrazzano G., Sica M., Gianfrani C., Mazzarella G., Maurano F., De Giulio B., de Saint-Mezard S., Zanzi D., Maiuri L., Londei M., et al. Gliadin regulates the NK-dendritic cell cross-talk by HLA-E surface stabilization. J. Immunol. 2007;179:372–381. doi: 10.4049/jimmunol.179.1.372. [DOI] [PubMed] [Google Scholar]
- 97.Ruggiero G., Sica M., Luciano L., Savoia F., Cosentini E., Alfinito F., Terrazzano G. A case of myelodysplastic syndrome associated with CD14(+)CD56(+) monocytosis, expansion of NK lymphocytes and defect of HLA-E expression. Leuk. Res. 2009;33:181–185. doi: 10.1016/j.leukres.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 98.Pedroza-Pacheco I., Madrigal A., Saudemont A. Interaction between natural killer cells and regulatory T cells: Perspectives for immunotherapy. Cell Mol. Immunol. 2013;10:222–229. doi: 10.1038/cmi.2013.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bozward A.G., Warricker F., Oo Y.H., Khakoo S.I. Natural Killer Cells and Regulatory T Cells Cross Talk in Hepatocellular Carcinoma: Exploring Therapeutic Options for the Next Decade. Front. Immunol. 2021;12:643310. doi: 10.3389/fimmu.2021.643310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Saito H., Kranz D.M., Takagaki Y., Hayday A.C., Eisen H.N., Tonegawa S. A third rearranged and expressed gene in a clone of cytotoxic T lymphocytes. Nature. 1984;312:36–40. doi: 10.1038/312036a0. [DOI] [PubMed] [Google Scholar]
- 101.Ribot J.C., Lopes N., Silva-Santos B. γδ T cells in tissue physiology and surveillance. Nat. Rev. Immunol. 2021;21:221–232. doi: 10.1038/s41577-020-00452-4. [DOI] [PubMed] [Google Scholar]
- 102.Mensurado S., Blanco-Domínguez R., Silva-Santos B. The emerging roles of γδ T cells in cancer immunotherapy. Nat. Rev. Clin. Oncol. 2023;20:178–191. doi: 10.1038/s41571-022-00722-1. [DOI] [PubMed] [Google Scholar]
- 103.Li R., Li H., Yang X., Hu H., Liu P., Liu H. Crosstalk between dendritic cells and regulatory T cells: Protective effect and therapeutic potential in multiple sclerosis. Front. Immunol. 2022;13:970508. doi: 10.3389/fimmu.2022.970508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Steinman R.M., Hawiger D., Nussenzweig M.C. Tolerogenic dendritic cells. Annu. Rev. Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- 105.Mills C.D. M1 and M2 Macrophages: Oracles of Health and Disease. Crit. Rev. Immunol. 2012;32:463–488. doi: 10.1615/CritRevImmunol.v32.i6.10. [DOI] [PubMed] [Google Scholar]
- 106.Chen S., Saeed A.F.U.H., Liu Q., Jiang Q., Xu H., Xiao G.G., Rao L., Duo Y. Macrophages in immunoregulation and therapeutics. Signal Transduct. Target Ther. 2023;8:207–242. doi: 10.1038/s41392-023-01452-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mantovani A. The growing diversity and spectrum of action of myeloid-derived suppressor cells. Eur. J. Immunol. 2010;40:3317–3320. doi: 10.1002/eji.201041170. [DOI] [PubMed] [Google Scholar]
- 108.Veglia F., Sanseviero E., Gabrilovich D.I. Myeloid-derived suppressor cells in the era of increasing myeloid cell diversity. Nat. Rev. Immunol. 2021;21:485–498. doi: 10.1038/s41577-020-00490-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lehuen A., Diana J., Zaccone P., Cooke A. Immune cell crosstalk in type 1 diabetes. Nat. Rev. Immunol. 2010;10:501–513. doi: 10.1038/nri2787. [DOI] [PubMed] [Google Scholar]
- 110.Ochsner S.A., Pillich R.T., Rawool D., Grethe J.S., McKenna N.J. Transcriptional regulatory networks of circulating immune cells in type 1 diabetes: A community knowledgebase. iScience. 2022;25:104581. doi: 10.1016/j.isci.2022.104581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Terrazzano G., Bruzzaniti S., Rubino V., Santopaolo M., Palatucci A.T., Giovazzino A., La Rocca C., de Candia P., Puca A., Perna F., et al. T1D progression is associated with loss of CD3+CD56+ regulatory T cells that control CD8+ T cell effector functions. Nat. Metab. 2020;2:142–152. doi: 10.1038/s42255-020-0173-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Leone S., Rubino V., Palatucci A.T., Giovazzino A., Carriero F., Cerciello G., Pane F., Ruggiero G., Terrazzano G. Bone marrow CD3+CD56+ regulatory T lymphocytes (TR3-56 cells) are inversely associated with activation and expansion of bone marrow cytotoxic T cells in IPSS-R very-low/low risk MDS patients. Eur. J. Haematol. 2022;109:398–405. doi: 10.1111/ejh.13822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rubino V., Leone S., Carriero F., Pane F., Ruggiero G., Terrazzano G. The potential etiopathogenetic role and diagnostic utility of CD3+CD56+ regulatory T lymphocytes in Myelodysplastic Syndromes. Eur. J. Haematol. 2023;110:578–579. doi: 10.1111/ejh.13931. [DOI] [PubMed] [Google Scholar]
- 114.Giovazzino A., Leone S., Rubino V., Palatucci A.T., Cerciello G., Alfinito F., Pane F., Ruggiero G., Terrazzano G. Reduced regulatory T cells (Treg) in bone marrow preferentially associate with the expansion of cytotoxic T lymphocytes in low risk MDS patients. Br. J. Haematol. 2019;185:357–360. doi: 10.1111/bjh.15496. [DOI] [PubMed] [Google Scholar]
- 115.Rubino V., Carriero F., Palatucci A.T., Giovazzino A., Leone S., Nicolella V., Calabrò M., Montanaro R., Brancaleone V., Pane F., et al. Adaptive and Innate Cytotoxic Effectors in Chronic Lymphocytic Leukaemia (CLL) Subjects with Stable Disease. Int. J. Mol Sci. 2023;24:9596. doi: 10.3390/ijms24119596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Akbari C.M., Saouaf R., Barnhill D.F., Newman P.A., LoGerfo F.W., Veves A. Endothelium-dependent vasodilatation is impaired in both microcirculation and macrocirculation during acute hyperglycemia. J. Vasc. Surg. 1998;28:687–694. doi: 10.1016/S0741-5214(98)70095-3. [DOI] [PubMed] [Google Scholar]
- 117.Williams S.B., Goldfine A.B., Timimi F.K., Ting H.H., Roddy M.A., Simonson D.C., Creager M.A. Acute hyperglycemia attenuates endothelium-dependent vasodilation in humans in vivo. Circulation. 1998;97:1695–1701. doi: 10.1161/01.CIR.97.17.1695. [DOI] [PubMed] [Google Scholar]
- 118.Mannucci E., Dicembrini I., Lauria A., Pozzilli P. Is glucose control important for prevention of cardiovascular disease in diabetes? Diabetes Care. 2013;36((Suppl. 2)):259–263. doi: 10.2337/dcS13-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Zdrazilova-Dubska L., Valik D., Budinska E., Frgala T., Bacikova L., Demlova R. NKT-like cells are expanded in solid tumor patients. Klin. Onkol. 2012;25((Suppl. 2)):2S21–2S25. [PubMed] [Google Scholar]
- 120.Wang H., Yang D., Xu W., Wang Y., Ruan Z., Zhao T., Han J., Wu Y. Tumor-derived soluble MICs impair CD3(+)CD56(+) NKT-like cell cytotoxicity in cancer patients. Immunol. Lett. 2008;120:65–71. doi: 10.1016/j.imlet.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 121.Zhou J., Zhao X., Wang Z., Wang J., Sun H., Hu Y. High circulating CD3+CD56+CD16+ natural killer-like T cell levels predict a better IVF treatment outcome. J. Reprod. Immunol. 2013;97:197–203. doi: 10.1016/j.jri.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 122.Tajiri K., Shimizu Y., Tsuneyama K., Sugiyama T. Role of liver-infiltrating CD3+CD56+ natural killer T cells in the pathogenesis of nonalcoholic fatty liver disease. Eur. J. Gastroenterol. Hepatol. 2009;21:673–680. doi: 10.1097/MEG.0b013e32831bc3d6. [DOI] [PubMed] [Google Scholar]
- 123.Atanackovic D., Nowottne U., Freier E., Weber C.S., Meyer S., Bartels K., Hildebrandt Y., Cao Y., Kröger N., Brunner-Weinzierl M.C., et al. Acute psychological stress increases peripheral blood CD3+CD56+ natural killer T cells in healthy men: Possible implications for the development and treatment of allergic and autoimmune disorders. Stress. 2013;16:421–428. doi: 10.3109/10253890.2013.777702. [DOI] [PubMed] [Google Scholar]
- 124.Guo W., Xing C., Dong A., Lin X., Lin Y., Zhu B., He M., Yao R. Numbers and cytotoxicities of CD3+CD56+ T lymphocytes in peripheral blood of patients with acute myeloid leukemia and acute lymphocytic leukemia. Cancer Biol. Ther. 2013;14:916–921. doi: 10.4161/cbt.25938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Rohon P., Porkka K., Mustjoki S. Immunoprofiling of patients with chronic myeloid leukemia at diagnosis and during tyrosine kinase inhibitor therapy. Eur. J. Haematol. 2010;85:387–398. doi: 10.1111/j.1600-0609.2010.01501.x. [DOI] [PubMed] [Google Scholar]
- 126.Almeida J.S., Couceiro P., López-Sejas N., Alves V., Růžičková L., Tarazona R., Solana R., Freitas-Tavares P., Santos-Rosa M., Rodrigues-Santos P. NKT-Like (CD3+CD56+) Cells in Chronic Myeloid Leukemia Patients Treated with Tyrosine Kinase Inhibitors. Front. Immunol. 2019;10:2493. doi: 10.3389/fimmu.2019.02493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gibson S.E., Swerdlow S.H., Felgar R.E. Natural killer cell subsets and natural killer-like T-cell populations in benign and neoplastic B-cell proliferations vary based on clinicopathologic features. Hum. Pathol. 2011;42:679–687. doi: 10.1016/j.humpath.2010.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]