Abstract
Racial discrimination is a well-known risk factor of racial disparities in health. Although progress has been made in identifying multiple levels through which racism and racial discrimination influences health, less is known about social factors that may buffer racism’s associations with health. We conducted a systematic review of the literature with a specific focus on social connectedness, racism, and health, retrieving studies conducted in the United States and published between January 1, 2012, and July 30, 2022, in peer-reviewed journals. Of the 787 articles screened, 32 were selected for full-text synthesis. Most studies (72%) were at the individual level, cross-sectional, and among community/neighborhood, school, or university samples. Studies had good methodological rigor and low risk of bias. Measures of racism and racial discrimination varied. Discrimination scales included unfair treatment because of race, schedule of racist events, experiences of lifetime discrimination, and everyday discrimination. Measures of social connectedness (or disconnectedness) varied. Social-connectedness constructs included social isolation, loneliness, and social support. Mental health was the most frequently examined outcome (75%). Effect modification was used in 56% of studies and mediation in 34% of studies. In 81% of studies, at least 1 aspect of social connectedness significantly buffered or mediated the associations between racism and health. Negative health associations were often weaker among people with higher social connectedness. Social connectedness is an important buffering mechanism to mitigate the associations between racial discrimination and health. In future studies, harmonizing metrics of social connectedness and racial discrimination can strengthen causal claims to inform interventions.
Keywords: racism, discrimination, social connectedness, racial disparities, health, social cohesion, health equity
Introduction
A plethora of evidence from observational and randomized controlled studies as well as real-world events establishes that racism and racial discrimination (note, we use these terms interchangeably to indicate racial discrimination) negatively affect health, including premature mortality.1–8 The field of epidemiology has contributed to robust measurement of racial discrimination9 at multiple levels, such as the interpersonal, organizational, community, and institutional or structural levels.1,2,10 Epidemiology also contributed to larger-scale studies that allowed for population-based assessments and rigorous analysis to isolate confounders and test mechanisms (eg, through material, socioeconomic, and other stressors, or psychosocial pathways).11–13
Despite a trove of evidence on the associations between racism and racial discrimination on health, a glaring gap remains. Specifically, limited work has been conducted to evaluate how social and community context mechanisms buffer racism or racial discrimination’s deleterious associations on health.14,15 Identifying such evidence is important for advancing health equity and moving the field forward beyond assessing differences toward identifying the resources that should be leveraged to keep all people healthy.1,15,16
Here, we summarize the peer-reviewed scientific literature to identify what is known about 1 specific buffering mechanism, social connectedness, and the evidence documenting how it changes the strength or direction of the associations between racial discrimination and health. Social connectedness encompasses perceived and actual connections to others; an individual’s perception of belongingness to neighborhoods, social groups or networks; and the extent of psychological or material resources potentially available within a family, network, or geographically defined area.17–19 The concept can be organized across 3 conceptual components: structural, functional, and quality.18,19 The structural aspects focus on the existence of interconnections among different social relationships. Functional aspects focus on functions provided by or perceived to be available because of social relationships. Quality focuses on the positive and negative aspects of social relationships. Social connectedness can involve the frequency and number of relationships with oneself in connection to others, strengths of networks, and extent of participation in activities at the macro level that facilitate group action or coordinated events to enact a specific type of change.
Although there are other potential mechanisms that mitigate the associations between racism and discrimination on health, such as religion and spirituality,20–22 social connectedness has been at the forefront of policy efforts as a public health priority.23,24 Fostering quantity and quality of social connectedness with others is a public health priority and is recognized as a key driver of economic productivity, civil stability, and subjective well-being in society that everyone should care about.25,26
There is also a growing availability of larger-scale big data on social connectedness27,28 and these are being used in policy studies that can be applied to epidemiologic research.29 Thus, focusing on this social factor as an intervention strategy for addressing racism, discrimination, and racial disparities in health is pertinent.30–32 In this review, we identify what is known about the associations among social connectedness, racism, racial discrimination, and racial disparities in health.
Methods
Search strategy
This review was designed by domain experts (Y.R., D.L.E., and T.L.T.) in consultation with a medical librarian (K.N.). We searched the PubMed database for research published (in print or electronically) in English between January 1, 2012, and July 30, 2022. The search used both text word searches and controlled vocabulary for 2 key concepts: racism and discrimination and social connectedness (see Web Table 1 for a full list of search terms).
Selection criteria
The articles selected for this review were screened for relevance, duplication, and meeting the selection criteria. The inclusion criteria were (1) a primary focus on social connectedness and racism, racial discrimination, or race-based or racial health disparities; (2) quantitative analyses of the association between social connectedness and racism, racial discrimination, or race-based health disparities; (3) sample includes any minoritized racial or ethnic group (eg, Black or African American, Hispanic or Latino/a/x, Asian American, or Native American); (4) sample size is at least 100 people; (5) conducted in the United States;, and (6) published in a peer-reviewed journal between January 1, 2012, and July 30, 2022. We excluded studies that were (1) qualitative, (2) primary focused on scale validation, (3) from outside United States, (4) not in English, and (5) commentaries, letters to the editor or opinion pieces, dissertations, protocols, retrospective chart reviews, or feature articles.
Data management
Covidence, a systematic review data management program, was used for deduplication and to conduct abstract and full-text review (Figure. 1). Working in pairs, the full research team independently reviewed and evaluated all retrieved abstracts and full texts using the aforementioned criteria. Discrepancies during abstract and full-text review were discussed and resolved by the first and senior authors (Y.R., T.L.T.).
Figure 1.
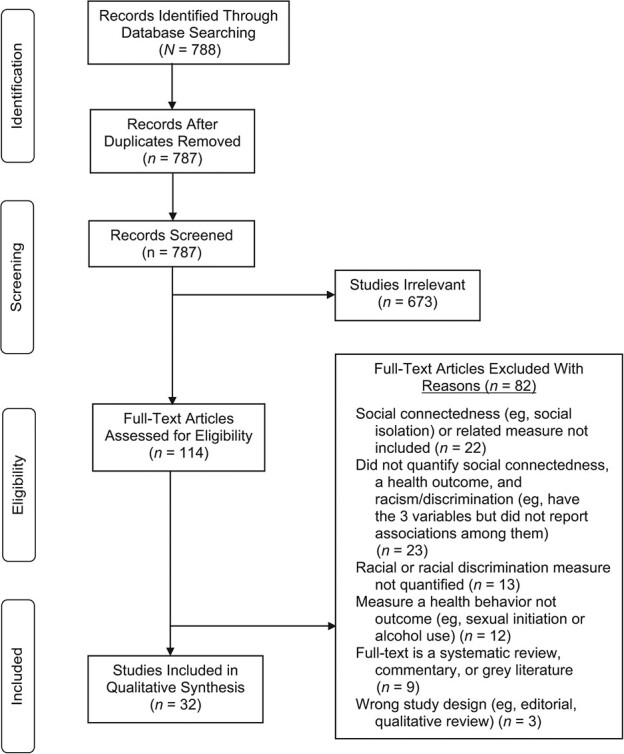
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) diagram for selected studies.
Data extraction and study quality
Data were extracted from full text articles using a set of defined fields related to the study design, methods, outcomes, and implications; measures of racism and racial discrimination, social connectedness, and health outcomes; and study sample characteristics and size. Given the importance of using theory in epidemiologic studies, we extracted data to quantify studies in which authors stated theories or theoretical frameworks they used to guide their work. Members of the research team independently extracted data from each article. The first and senior authors reviewed all extracted data for accuracy and completeness. The 10 most relevant fields are included in Table 1.
Table 1.
Characteristics of the included articles for analysis, N = 32.
| First author, yearreference no. | Level of analysis | Study design | Study population | Racism/racial discrimination | Social connectedness | Health outcome | Statistical approach (effect modification, or mediation) | Did social connectedness significantly affect associations between racial discrimination and health? | Theory | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Race and/or ethnicity a , b | Mean (SD) age, years | Age range, years | % | |||||||||
| Beach, 201934 | Individual level | Cross-sectional | Black/African American | 24–29 years | Self-reported experiences of racial discriminatory events | Perceived relationship, warmth, and support | Proinflammatory and anti-inflammatory cytokines (an index of IL-7, IL-8, IL-10, IL-13, MIP1B, and TNF-α) | Effect modification | Yes | Broad evolutionary explanatory framework | ||
| Bergeron, 202055 | Individual level | Cross-sectional | Black, White, Latino, Asian/Pacific Islander, Other | 18–24 24–44 45–64 ≥ 65 | 11 43 30 16 | Self-reported lifetime interpersonal discrimination based on race, ethnicity, or color in 9 domains | Frequency of social contacts | HrQOL-4 | Effect modification | Yes | None | |
| Busby, 202056 | Individual level | Cross-sectional | White, Black, Asian, Hispanic, Other | N/A | N/A | Everyday discrimination in the past 12 months | Social connectedness | Depressed mood and anhedonia using the PHQ-2 | Effect modification | No | Minority stress theory | |
| Garcini, 202049 | Individual level | Cross-sectional | Latinx | 46 (15.0) | N/A | Perceived discrimination subscale | Social support | Depression using the CESD-R | Effect modification | Yes | Social support as buffer theory | |
| Goosby, 201257 | Individual level | Cross-sectional | Non-Hispanic White, Non-Hispanic Black | 16.1 (11.4) | N/A | Perceived discrimination | School connectedness; loneliness; parental support | Self-rated general health | Effect modification | Yes | Integrative and biopsychosocial theory | |
| Jang, 202145 | Individual level | Cross-sectional | Black/African American | 73.4 (8.0) | N/A | Self-report of ever been discriminated against or treated unfairly because of their race or ethnicity | Social connectedness to one’s ethnic community | Psychological distress using the 6-item Kessler Psychological Distress Scale | Effect modification | Yes | None | |
| Kim, 201446 | Individual level | Cross-sectional | Korean | 30.3 (12.2) | N/A | The racial discrimination experience measure | Perceived social support | Depression using the CESD | Effect modification | Yes | Empowerment theory | |
| Lee, 201558 | Multilevel | Cross-sectional | White, Black | 45.2 (6.6) | N/A | Individual racial prejudice | Neighborhood social capital | Death | Mediation | Yes | Social capital theory | |
| Liao, 201636 | Multilevel | Cross-sectional | Black/African American | 30.23 (12.0) | N/A | Racial microaggressions against Black individuals | Social connectedness to one’s ethnic community; social connectedness to mainstream society | Anxiety using the short form of the Depression, Anxiety, and Stress Scale | Effect modification | Yes | Social Identity theory and diathesis of stress theory | |
| Lorenzo-Blanco, 201950 | Individual level | Longitudinal | Latinx | 14.51 (0.9) | N/A | Perceived discrimination | Social neighborhood cohesion; informal social control; adolescents’ perceived neighborhood characteristics | Parent and adolescent depressive symptoms using the CESD | Effect modification | Yes | Social stress theory | |
| Majeno, 201859 | Individual level | Cross-sectional | Latino, European American, Asian, Other | 16 (0.7) | N/A | Everyday discrimination in the past 12 months | Loneliness | Sleep outcomes (duration, variability, global PSQI score, PSQI quality, PSQI efficiency, PSQI disturbances) | Mediation | Yes | None | |
| Maleku, 202160 | Multilevel | Cross-sectional | Asian, Latino, White, Other | 27.8 (5.5) | N/A | Everyday discrimination in the past 12 months | Loneliness | Depressive Symptoms using the PHQ-9 scale | Mediation | Yes | None | |
| Mama, 201637 | Multilevel | Cross-sectional | Black/African American | 45.2 (12.9) | N/A | Experiences of a situation based on their race, ethnicity, or skin color | Perceived social support | Mental health using the Medical Outcomes Study’s 12-item Short-Form Survey–12, version 2 | Mediation | Yes | Social Ecological Theory | |
| Marshall, 201238 | Multilevel | Cross-sectional | Black/African American, Caribbean Black | 66.5 (10.9) | N/A | Everyday discrimination in the past 12 months | Social support; social connectedness | Depressive symptoms using a 12-item version of the original 20-item CESD | Effect modification | No | Stress Process Theory | |
| Nair, 201351 | Multilevel | Cross-sectional | Mexican or Mexican American | 35.9 | N/A | Self-reported perceptions of discrimination from teachers and peers against their ethnic group or directed at themselves | Family cohesion | Adolescents internalizing and externalizing symptoms using the Diagnostic Interview Schedule for Children | Effect modification | Yes | Strain Theory | |
| Negi, 201365 | Individual | Cross-sectional | Latino | 37 (10.7) | N/A | Self-reported perceptions of stress associated with discrimination and stigma | Social isolation | Psychological distress using the 6-item Kessler Psychological Distress Scale | Mediation and qualitative | Yes | Minority stress theory | |
| Nelson, 202139 | Individual level | Cross-sectional | Black/African American | 34.2 (11.4) | N/A | Measure the stress associated with experiencing racist and sexists events during the past year and throughout the lifetime | Loneliness | Depressive symptoms using the CESD-R | Mediation | Yes | None | |
| Nguyen, 201840 | Individual level | Cross-sectional | Black/African American, Caribbean Black | N/A | 18–34 35–54 55 | N/A | Everyday discrimination in the past 12 months | Church-based emotional support | Psychological distress using the 6-item Kessler Psychological Distress Scale | Effect modification | Yes | None |
| Priest, 202041 | Individual level | Cross-sectional | African American | 51.6 (11.9) | N/A | Experiences of racial discrimination | Family support | Disease activity using an index of chronic conditions and prescription medications | Mediation | Yes | Biobehavioral family model | |
| Rodriguez, 201652 | Individual level | Cross-sectional | Hispanic | 61.7 (8.7) | N/A | Lifetime exposures to ethnic discrimination within a social or interpersonal context | Social support | Sleep outcomes (nocturnal blood pressure dipping) | Effect modification | No | None | |
| Rollock, 201647 | Individual-level | Cross-sectional | Asian American | 42 | N/A | Experiences of perceived inequity in social interactions Experiences of racial discrimination | Family cohesion; neighborhood social cohesion; social network support; spousal support | Psychological distress using the 10-item Kessler Psychological Distress Scale | Effect modification | No | Discrimination and psychosocial stress theory | |
| Roth, 202253 | Individual level | Cross-sectional | Puerto Rican, Cuban, Mexican, Other | 40 (15.6) | N/A | Discrimination based on day-to-day life experiences or attributed to race/ethnicity differences | Neighborhood social cohesion | Depressive symptoms; anxiety disorders; substance use disorders using the DSM-IV module of a modified version of the World Mental Health Composite International Diagnostic Interview | Latent profile analysis | Yes | Social ccological theory and acculturation theory | |
| Saasa, 202142 | Individual level | Cross-sectional | South African, East African, Central African, West African, North African | 33.9 (9.2) | N/A | Frequency of experiences of everyday mistreatment | Loneliness | Mental health symptoms using the 4-item PHQ | Effect modification | Yes | Biopsychosocial theory | |
| Scheuermann, 202061 | Multilevel | Longitudinal | Black/African American, White | N/A | <40 >40 | N/A | Frequency of experiences of everyday mistreatment | Neighborhood social cohesion | Psychological distress using the GAD 7item scale | Effect modification | No | Environmental Affordances model |
| Sheikh, 202262 | Individual-level | Cross-sectional | South Asian, Middle Eastern, North Africa, Other | 29 (4.8) | N/A | Severity of perceived discrimination, Everyday Discrimination Scale, revised | Social connectedness | Trauma and/or PTSD using the DSM-5 Primary Care PTSD Screen | Effect modification | Yes | Adapted model of acculturation | |
| Singh, 201566 | Individual level | Cross-sectional | Asian American | 40.6 male, 41.2 female | N/A | Acculturative stress based on Asian descent | Family and friend social support | Psychological distress using the 10-item Kessler Psychological Distress Scale | Effect modification | Yes | Acculturative stress, and stress oping theory | |
| Steers, 201943 | Individual level | Cross-sectional | African American | 49.0 (11.5) | N/A | Perceived discrimination experienced on a day-to-day basis | Social support | Psychological distress using the Global Severity Index from the 53-item Brief Symptom Inventory | Effect modification | Yes | Social support as a buffer theory | |
| Torres, 202254 | Multilevel | Cross-sectional | Puerto Rican, Central and South American, Other | 43.57 (15.1) | N/A | Lifetime exposures to racial/ethnic discrimination within a social or interpersonal context | Neighborhood social cohesion | Depressive symptoms using a brief version of the CESD | Moderated-mediation | Yes | Discrimination and psychosocial stress theory | |
| Walton, 201264 | Multileve | Cross-sectional | Asian American | 40.97 (14.7) | N/A | Frequency of routine experiences of unfair treatment | Neighborhood social cohesion | Self-rated physical health | Mediation | No | Resurgent ethnicity perspective | |
| Wei, 201248 | Individual level | Cross-sectional | Chinese, Taiwanese, Hong Kong | 24.9 (4.5) | N/A | Perceived racial discrimination in the context of being an international student in the United States | Social connectedness to one’s ethnic community; social connectedness to mainstream society | PTSD using the 6-item PTSD Checklist | Effect modification | Yes | Acculturation theory | |
| Wong, 201444 | Individual level | Cross-sectional | Black/African American men, multiethnicity | 23.6 (6.0) | N/A | Lifetime experiences of minority stress | Social network connectedness, emotional support; instrumental support | Psychological distress using a brief version of the CESD | Effect modification | Yes | Minority stress theory | |
| Yang, 201863 | Individual level | Cross-sectional | White, Black/African American, Hispanic, Other | 52 (16.2) | N/A | Perceived racial discrimination | Neighbor’s willingness to help; sense of belonging; sense of neighborhood trust; neighborhood improvement | Self-rated stress | Mediation | Yes | Stress coping theory | |
Abbreviations: CESD, Center for Epidemiologic Studies Depression; CESD-R, Center for Epidemiologic Studies Depression, Revised; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAD, Generalized Anxiety Disorder; HRQoL4, Health-Related Quality of Life–4; IL, interleukin; MIP1B, macrophage inflammatory protein-1β; N/A, not reported, not available based on the study design, or unclear in the study; PHQ, Patient Health Questionnaire; PSQI, Pittsburgh Sleep Quality Index; PTSD, post-traumatic stress disorder; TNF, tumor necrosis factor.
a For race/ethnic composition column, where only 1 race was reported, the sample was 100%. In cells where 2 or more races were reported and no percentages; these data were was unknown or not reported in the study. Race/ethnic terms may vary based on what authors reported in their study (eg, Latinx or Hispanic or Latino, or non-Hispanic Black or Black/African American). For the age column, some studies did not report the SD of the mean age or percentage. For the social connectedness column, multiple items are reported if authors use more than 1 measure either together or as part of a composite.
b We report, where possible, terms used by the study authors; hence, there are differences in reporting (eg, between Black, and non-Hispanic Black, and African Americans). Some authors used Latino, others used Latinx, others use Hispanic).
Quality assessment and risk of bias
Two members of the research team (G.L.C., C.H.) conducted a risk-of-bias quality assessment using the Joanna Briggs Institute Checklist for Analytical Studies checklist tool for systematic reviews.33 The checklist contains 8 questions about the research methods, design, and analyses to evaluate the quality of each study. We determined that a minimum of 6 of 8 (75%) of the checklist items must be met for the study to be included as low risk of bias.
Results
Our search results yielded 788 articles. After duplicates were removed, the study team screened the titles and abstracts of 787 articles. Next, the study team similarly reviewed 114 full-text articles and 82 were excluded for irrelevant measures (eg, did not meet criteria for quantifying the associations between social connectedness, racism, racial discrimination, or race-based health disparities) and outcome (eg, measured a health behavior and not a health outcome). In all, 32 studies met the inclusion criteria (Figure 1).
Descriptive characteristics of studies
Data extraction of population characteristics from the 32 relevant studies included age, race/ethnicity of the study population, and study design (Table 1). The mean age of study participants ranged from 16.1 years (SD, 11.4) to 73.4 years (SD, 7.97). Eleven studies (34%) included only participants identifying as African American, African, Black, or Caribbean Black.34–44 Four studies (13%) included only participants identifying as Asian and Pacific Islander, Korean, Asian American, Chinese, Taiwanese, or “Hong Kong.”45–48 Six studies (19%) included only participants identifying as Latino/a/x, Mexican/Mexican American, Caribbean Hispanic, Puerto Rican, Cuban, or Central and South American.49–54 Nine studies (28%) included participants from multiple racial/ethnic groups.55–63 Analyses were conducted mainly at the individual level (65%). For study design, 30 studies (94%) were cross-sectional, with no randomized controlled or intervention trials. Two studies (6%) used data from a prospective sample,61 but it was only clear from 1 study that the level of analysis was longitudinal50 (Table 1).
Risk of bias
Most of the included studies showed overall good methodological rigor and low risk of bias. That is, studies had to fulfill the criteria that corresponded to “yes” across 6 of the 8 dimensions. Among studies not meeting criteria, the most frequent category of weakness was from the criterion “Was the exposure measured in a valid and reliable way?” Three of these studies reported Cronbach’s α below 0.70. However, all studies exemplified low risk of bias because each met at least 75% of the criteria (see Web Table 2 for the list of studies and criteria).
Measurement of racism and racial discrimination
Thirty percent of studies assessed discrimination based on race and/or ethnicity. Of these, 1 study assessed discrimination based on race and gender,39 and another assessed discrimination on the basis of race and sexual orientation.44 Eleven studies (34%) used either the full, revised, or brief versions of the Everyday Discrimination Scale,38,40,42,43,53,56,59–62,64 followed by the Schedule of Racist Events,34,39 the Experiences of Discrimination Scale,55 and Day-to-Day Unfair Treatment Scale.37 Six studies (19%) measured racism and discrimination, using items from an unspecified but previously administered survey57,58,63 or did not report using a specific measure of racism and discrimination.41,45,47 The number of items included from each scale varied across studies. For instance, Majeno et al.59 used the 10-item version of the Everyday Discrimination Scale, whereas Marshall and Rue38 used a 6-item version of the scale. Nevertheless, most studies used validated instruments. The Cronbach’s α reliability coefficients ranged between 0.63 and 0.99.
Measurement of social connectedness
Measures of social connectedness varied, with most studies including scales that reflected the presence of social networks, family, friend, or ethnicity-specific social support, and social cohesion. Approximately 88% of studies examined at least 1 of these measures. In the remainder of the results, we refer broadly to “social connectedness” to streamline results and ease of interpretation, but the specific items or constructs details are given in Table 1. Fewer studies assessed measures indicating a lack of social connectedness, such as social isolation (3%)57 and loneliness (16%).39,42,57,59,60 Among those using formal social connectedness measures, 25 studies (78%) used validated scales such as those of Bergeron et al.,55 Busby et al.,56 Beach et al.,34 and Garcini et al.49 The Cronbach’s α reliability coefficients across these studies ranged between 0.46 and 0.97. Most of these measures were at the individual level, although 6 studies also assessed perceived neighborhood-level social connectedness, with the caveat that the unit of analysis of the social connectedness variable was among individuals,47,50,53,54,61,64 with the exception of Lee et al., who used multilevel modeling.58 Last, 17 of the article measures (53%) reflected mainly functional aspects of social connectedness,39–43,47,48,51,53,54,57,60,62,64–66 7 (22%) reflected mainly structural aspects,34,36,37,45,55,58,61 6 (19%) reflected both structural and functional aspects,38,44,49,52,59,63 and 1 included a measure that assessed the quality aspect.46
Health outcomes studied
Twenty-five studies (78%) examined some type of mental or psychiatric health outcome such as depression or depressive symptoms, anxiety, post-traumatic stress disorder (PTSD), or other psychological distress.35–40,42–51,53–56,60–62,65,66 Measures of mental health varied, including the Kessler-6 scale; Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) measures; Center for Epidemiologic Studies Depression Scale; Short Form-12, version 2 Scale; Patient Health Questionnaire, and self-reported days of poor mental health. Studies examining mental or psychiatric health either used self-rated descriptions of mental health using a numerical scale34,43,48,55,63,65,66 or a rating of the frequency with which one would experience certain aspects of mental distress.36–39,44–46,49,54,56,57 For example, Yang and Chen63 asked participants to self-assess how much day-to-day stress they experienced, given that a rating of 1 would mean no stress and a rating of 10 representing an extreme amount of stress. Six studies (19%) examined psychological distress in particular.40,43,47,61,65,66 Evaluating levels of distress varied across studies. Not all authors included the same items in their evaluation scales. Negi65 and Nguyen et al.40 used a 6-point scale measuring frequency of symptoms relating to mental distress, whereas Rollock and Lui47 and Steers et al.43 used a 10-item frequency scale. Scheuermann et al.61 used a 7-item scale addressing generalized anxiety. Singh et al.66 used a 53-item scale evaluating psychological distress as it relates to acculturative stress. Two studies (6%) examined sleep outcomes.52,59 Other health measures assessed in the studies include health-related quality of life, proinflammatory biomarkers, self-rated health, death, sleep disorders, and physiologic stress (Table 1).
Use of theory in studies
Overall, in 92% of studies, researchers used some theory to underpin the rationale for their analytic choice or reason for the study. These included constructs or concepts from acculturation theory, biobehavioral theory, biopsychosocial theory, discrimination and psychosocial stress, empowerment theory, environment affordances theory, social capital, social ecological theory, social identity, social stress theory, social support as a buffer, train theory, stress and coping, and minority stress theory.
Effect modification studies
Overall, 16 studies (50%) conducted some form of effect modification, moderation, or interaction.34,36,38,40,42–45,47–50,52,55,56,66 Studies typically included a main association model with racism or racial discrimination and predicting the health outcome, then in a second stage, an interaction was created between social connectedness and the discrimination measure. Studies often reported a single interaction coefficient and rarely stratified the results once a significant interaction was detected. All but 1 study34 conditioned by the social connectedness variable, meaning that the authors examined the association between discrimination and the health outcome conditioned on levels of social connectedness. Among those 16 studies, 14 reported a significant interaction or effect moderation result,34,36,40,42–45,48–51,55,62,66 with the majority finding that the associations of some measure of discrimination on some poor health outcome was weaker (ie, flatter slope or smaller coefficient) among people reporting higher social connectedness. These types of interactions are called statistical interactions. The effects or associations within 2 subgroups go in the same direction but differ in magnitude of the coefficient or degree of significance.67
In the following section, the coefficients presented are what the authors reported in their articles. Therefore, there is substantial variation in the consistency of reporting (eg, not all authors included standard errors or t values along with β coefficients), and some authors included unstandardized β coefficients whereas others reported standardized β coefficients (or both coefficients, with 1 for the interaction test and another for main effects). Some authors reported relative risk (RR) or odds ratios (ORs) with P values whereas others reported with 95% CIs, and some reported exact P values whereas others reported P values less than a specific significance value (eg, <0.05, <0.001).
Bergeron et al.55 investigated this topic among a racially diverse sample of adults in New York City and found that among people exposed to racial discrimination, the likelihood of experiencing days of poor mental health was lower among those with high social connections (measured by frequency of contact with people once or more a week). This study was among the few to stratify the results of their interaction tests. In the low-frequency connectedness group (contact with others ≤5 times a month) compared with those with no discriminatory events, the RR between 1 or 2 discriminatory events (RR =1.54; P = 0.041) and 3 or more events (RR = 2.33; P = 0.000) was significantly higher. However, in the high-frequency connectedness group (contact with others at least once per week), compared with those with no discriminatory events, the RR between 1 or 2 discriminatory events (RR = 0.91: P = 0.061) and 3 or more discriminatory events (RR = 1.24; P = 0.196) was not significant.
Sheikh et al.62 conducted a study among people exposed to trauma and who identified as Muslim and as a refugee, asylum seeker, or internally displaced. They found a significant interaction association between perceived discrimination and social connectedness on post-traumatic cognitions (PTCs) (b = −0.02; 95% CI, 0.04-0.001; P = 0.03). The moderation analysis yielded a significant overall model (F(3, 95) = 18.90; P = 0.001). Lower social connectedness exacerbated the associations between discrimination and PTC. In stratified analysis, Sheikh et al.62 found that among people who were scored 2 SD below the mean, the association was b = 0.32 (95% CI, 0.13-0.51) for perceived discrimination on PTC; among those who scored 1 SD below the mean, the association was b = −0.23 (95% CI, 0.11-0.35), and among those at the mean, it was b = 0.14 (95% CI, 0.04-0.24). However, the associations were not significant for people 1 SD above the mean (b = 0.05; 95% CI, −0.09 to 0.18) and those 2 SD above the mean (b = −0.05; 95% CI, −0.26 to 0.16).
Jang et al.45 conducted a study among older Korean American adults and found a statistically significant interaction between perceived racial discrimination and sense of community (belongingness to a Korean community) (B = −1.86; SE = 0.28: P < 0.001). This model explained an additional 2% in variance beyond a main associations model, controlling for confounders. In stratified analyses, those in the group with low sense of community (ie, below the mean), the association between perceived racial discrimination was substantially higher (B = 3.75; SE = 0.44; P < 0.001) compared with those in the group with high sense of community (ie, above the mean) (B = 1.03; SE = 0.22; P < 0.001).
Lorenzo-Blanco et al.50 conducted a study among recent immigrant Latinx adolescents and found that parent cultural stress (which included a measure of perceived racial discrimination) was associated with lower depressive symptoms among adolescents when social connectedness (adolescent-perceived social support) was low (B = −0.357; P < 0.05). When social connectedness was 2 SD below the mean, the association was negative and significant (B = −0.36; P = 0.002), but the association was positive and not significant when social connectedness was 2 SD above the mean (B = 0.26, P = 0.34).
Although the predominant pattern of the interactions was differences by strength of association, 1 study found a “qualitative or cross over interaction”67 whereby the direction of associations differed. For example, Beach et al.34 examined a sample of African American adults between ages 24 and 29 years. They found that perceived relationship warmth and support significantly moderated the association between contextual stress (which included a measure of racial discrimination) and pro- and anti-inflammation markers (B = −1.14; SE = 0.44; P < 0.05). Those with greater perceived support had a weaker and nonsignificant association between contextual stress and inflammation (b = −0.036; P = not significant), whereas those with low support had a significant positive association (b = 0.192; P < 0.001).
Not all studies aligned with the pattern that social connectedness buffered the impact of racism on health. Nguyen et al.40 examined a sample of African American men and found the opposite, such that the association between discrimination and poor health was stronger among those with higher social connectedness (measured by church-based social support). Stratification was not conducted, but the interaction results were displayed in graphs showing the slopes. The authors referenced the resource mobilization perspective to postulate that a potential reason for these unexpected findings could be that individuals under racial distress reach out to members within their network to mobilize support for coping (but reverse causality cannot be ruled out). The authors also postulated that support-group members may have recognized the visible signs of a person’s distress and mobilized to provide support to that person.
Subpopulation influences in effect modification studies
Studies rarely included additional subpopulation analyses by sociodemographic characteristics such as gender or age. Among those that did and reported results, there were subgroup differences such that the interaction between social connectedness and racial discrimination on health was only present in 1 group or was larger in 1 group. Nguyen et al.40 found age-group differences where the associations between racial discrimination and mental health was only significant for young (ages 18–34 years) African American men (b = 0.01; SE = 0.01;, P < 0.01) and older men (age ≥55 years; (b = 0.01 [SE = 0.01], P < 0.05), but not significant for those in midlife (ages 35–54 years).
Nair et al.51 examined a sample of Mexican American youth and found subgroup differences by sex (boys vs girls) with a 3-way interaction (γ = −1.08; SE = 0.49; P < 0.01). For boys, greater racial discrimination was significantly associated with higher externalizing symptoms (sum of DSM-IV diagnosed conduct, attention deficit/hyperactivity, and oppositional defiant disorders) when social connectedness (neighborhood social cohesion) was high (B = −2.43; t(1) = −2.19; P = 0.04). The remaining studies found no statistically significant effect modification.38,47,52
All but 1 of the significant effect modification studies operationalized social connectedness as the presence of some contact or support (eg, social support, frequency of contact). However, 1 study operationalized social connectedness in terms of levels of loneliness. This conceptual difference is important because the possible mechanisms might differ such that loneliness refers to the subjective experiences even when people have social contacts,18 and both have distinct pathways to health.68,69 Saasa and Miller42 examined a sample of first-generation Black African immigrant adults and found that frequent feelings of loneliness exacerbated the negative influence of discrimination on depression and anxiety symptoms (the interaction model explained 42% of the variance in mental health symptoms). Infrequent feelings of loneliness mitigated the negative effect (B = 0.43; SE = 0.13; P < 0.05).
Referent-group specific social connectedness associations
There was some evidence that negative associations between racial discrimination and health are buffered by ethnic or cultural group–specific social connectedness rather than generic or population average support. Wei et al.48 examined these associations among Chinese international students at 2 midwestern universities. They found that social connectedness received specifically from Chinese or Taiwanese individuals weakened the strength of association between perceived racial discrimination and PTSD. Those with higher ethnic social connectedness had a flatter slope (B = 0.29; P = 0.001), indicating discrimination had a weaker impact on health, compared with the association among those with lower ethnic social connectedness (B = 0.53; P < 0.001), which had a steeper slope. However, social connectedness from mainstream society did not buffer the impact of discrimination on PTSD.
Liao et al.36 studied these associations among a sample of Black Americans. They found that social connectedness received or in relation to being Black American (eg, African American, Caribbean Black community) weakened the strength of association between racial microaggressions on anxiety, with the effect modification accounting for 9% of the variance in anxiety. Those with higher ethnic social connectedness had flatter slope that was nonsignificant (B = 0.35; P > 0.05), indicating discrimination had a weak or no impact on health, compared with the association among those with lower ethnic social connectedness (B = 1.49; P < 0.001), which had a steeper and significant slope.
Latent profile analysis studies
Only 1 study used latent profile analysis whereby the authors created latent classes of individuals on the basis of combinations of racial discrimination and social connectedness. Roth et al.53 identified 4 groups in a study among Latinx adults. Groups were those who shared positive experiences (lowest discrimination and family conflict, and highest ethnic identity, neighborhood social cohesion, and safety); those in cohesive conflicts (highest neighborhood social cohesion, but increased neighborhood danger, racial discrimination, and family conflict); those in marginalized conflict (highest discrimination and conflict, but lower levels of family and neighborhood social cohesion); and those in marginalized profiles (lowest levels of social cohesion and moderate levels of racial discrimination and family conflict).
Significant differences were found across these profiles, especially between the positive-experience versus marginalized profile groups (Wald test for depressive symptoms, χ2 = 40.392; for anxiety, χ2 = 36.230; and for substance use disorders, χ2 = 34.330; all P < 0.0001). Those in the marginalized conflict profile had the highest prevalence of all disorders and differed significantly for depressive symptoms (difference = −0.192; P < 0.001) and for substance use disorders (difference = −0.155; P < 0.001).53
Mediation analysis studies
Some formal mediation, path analysis, or stepwise analysis was the second most used approach to investigate the impact between social connectedness and racial discrimination associations on health.37,39,41,46,57–60,63,64 Although not all studies stated this approach explicitly or used theories to guide their approach, a mediation methodological approach is possibly based on research showing that racism and discrimination results in reduced social connections, which then exacerbates any existing negative associations on health.70 This specific reasoning may be called the social connectedness erosion hypothesis. Using a sample of racially diverse adolescents from the National Longitudinal Study of Adolescent Health, Goosby and Walsemann57 found that the associations between discrimination (ie, unfair treatment by teachers) on self-rated health was mediated by 57% once social connectedness (level of connectedness to peers in their school and perceived loneliness) was included. The coefficients for unfair treatment on health was B = −0.028 (P < 0.05), and after adjustment for social connectedness was B = − 0.016 (P < 0.05).
Kim46 conducted a path analysis among a sample of Asian American adults and found that the indirect effect of racial discrimination was mediated by lower social support, which was related to greater depression. The total effect coefficient was b = 0.92 (P < 0.01) for discrimination, social support, and depressive symptoms. The direct effect between racial discrimination and depressive symptoms was b = 4.35 (P < 0.001).
Lee et al.58 examined participants to the General Social Survey, which is linked to mortality data. They found that living in communities with higher community-level prejudice was associated with higher mortality (OR = 1.13; 95% CI, 1.16-1.49). However, this association was attenuated to nonsignificance after adjusting for neighborhood social capital (OR = 1.17; 95% CI, 0.97-1.41).
Maleku et al.60 examined a sample of US-based international students and conducted a formal mediation analysis. They found that racial discrimination was significantly associated with higher levels of loneliness, which, in turn, was significantly associated with higher anxiety and, in turn, higher levels of depressive symptoms. For direct effect of discrimination on depression, B = 0.48 (95% CI, 0.30-0.66). In the mediation model, for discrimination to loneliness to depression, B = 0.10 (95% CI, 0.02-0.19).
Priest et al.41 found that family social support partially mediated the association between racial discrimination and disease activity (an index of chronic conditions and medication use for ailments). Specifically, discrimination was associated with lower family support, which was associated with poorer mental and emotional health, which, in turn, was associated with higher disease activity where, for indirect effect, β = 0.01 (SE = 0.005; P = 0.01).
Negi65 conducted a mixed-methods study in which they used a stepwise approach to estimate social connectedness and discrimination associations on health but did not report a change in coefficients. They reported qualitatively how racism affected the levels of social connectedness among their participants.
Subpopulation associations in mediation analysis studies
Only 1 study found subgroup differences in the mediation analyses. Yang and Chen63 investigated these topics among a sample of adults from Philadelphia, PA. They found that the association between perceived racial discrimination and stress was partially mediated by social capital (approximately 17% of the direct effect). People who have perceived discrimination had poorer social capital, which, in turn, increased stress. The proportion mediated by social capital varied by race/ethnicity (12% among Non-Hispanic White people, 10% among non-Hispanic Black people, 10% among Hispanics, and 7% among other races), although the mediation pathway was only significant for Black people and White people, but not Hispanics and other non-Hispanic races.
Moderated-mediation analysis studies
Only 1 study used a moderated-mediation analysis to focus on potential mechanisms along the pathway between discrimination and health associations. Specifically, Torres et al.54 examined whether social cohesion moderated the pathway among discrimination, higher alcohol use, and subsequent depressive symptoms. They found that alcohol use was a significant mediator between ethnic discrimination and depression symptoms, and social connectedness (as measured by social cohesion) moderated this relationship. Alcohol use was not significant at higher levels of social connectedness (b = −0.18; SE = 0.06; P < 0.01). Alcohol use was a significant mediator between discrimination and depression only at low and moderate levels but not at high social cohesion.
Levels of analysis between social connectedness and discrimination and racism associations with health
In 28 of the included studies (88%), researchers examined both individual-level social connectedness and individual racism and discrimination indicators. Only 4 studies (13%) examined the impact of higher-level social-connectedness variables, but most associations were still assessed with individual or interpersonal-level discrimination measures. One example of a study that used multilevel models to assess a higher-level social connectedness measure was that of Goosby and Walsemann,57 who examined school-level social connectedness with some questions that assessed the extent to which students agreed that they felt (1) they were part of the school, (2) close to people at their school, and (3) happy to be at their school. The multilevel model examined school-level connectedness with individual-level self-rated health. One study examined the impact of neighborhood-level social connectedness and neighborhood-level discrimination associations with individual health. Lee et al.58 used the General Social Survey and created a primary sampling unit–level (proxied by a metropolitan statistical area geographic level) social capital variable from the Robert Putnam Index that includes variables such as number of specific organizations in a geographic area. They assessed primary sampling unit–level racial prejudice by aggregating scores of individual responses to given items that include assessments such as Black/African American people having less in-born ability to learn (Table 2).
Table 2.
Levels at which the social connectedness and discrimination indicators are measured.
| First author, yearreference no. | Levels at which social connectedness is measured a | Levels at which racism and discrimination were measured | ||
|---|---|---|---|---|
| Individual and interpersonal | Community/neighborhood/school | Macro/state/structural | ||
| Individual and interpersonal | ||||
| Beach, 201934 | Yes | Yes | No | No |
| Bergeron, 202055 | Yes | Yes | No | No |
| Garcini, 202049 | Yes | Yes | No | No |
| Jang, 202145 | Yes | Yes | No | No |
| Kim, 201446 | Yes | Yes | No | No |
| Lorenzo-Bianco, 201950 | Yes | Yes | No | No |
| Majeno, 201859 | Yes | Yes | No | No |
| Maleku, 202160 | Yes | Yes | No | No |
| Mama, 201637 | Yes | Yes | No | No |
| Marshall, 201238 | Yes | Yes | No | No |
| Negi, 201365 | Yes | Yes | No | No |
| Nelson, 202139 | Yes | Yes | No | No |
| Ngyuen, 201840 | Yes | Yes | No | No |
| Priest, 202041 | Yes | Yes | No | No |
| Rodriguez, 201652 | Yes | Yes | No | No |
| Rollock, 201647 | Yes | Yes | No | No |
| Roth, 202253 | Yes | Yes | No | No |
| Saasa, 202142 | Yes | Yes | No | No |
| Scheuermann, 202061 | Yes | Yes | No | No |
| Shiekh, 202062 | Yes | Yes | No | No |
| Singh, 201566 | Yes | Yes | No | No |
| Steers, 201943 | Yes | Yes | No | No |
| Walton, 201264 | Yes | Yes | No | No |
| Wei, 201248 | Yes | Yes | No | No |
| Wong, 201444 | Yes | Yes | No | No |
| Yang, 201863 | Yes | Yes | No | No |
| Community/neighborhood/school/family | ||||
| Goosby, 201257 | Yes | Yes | No | No |
| Liao, 201636 | Yes | Yes | No | No |
| Nair, 201351 | Yes | Yes | No | No |
| Lee, 201558 | Yes | No | Yes | No |
| Macro/state/structural | No | No | No | No |
a For the social connectedness metrics, we identify levels by the unit at which it was included in the analysis, rather than the conceptual idea. For instance, perceived “neighborhood” social cohesion queries people about their cognitive appraisals of their community, but the analysis occurs at the individual level. As such, this provides an individual-level result of community associations rather than a contextual-level result of connectedness on health. Studies that are often able to distinguish those type of associations by levels are multilevel or hierarchical analyses.
A folder containing the 32 studies included in our study are available for readers to access from the Open Science Framework (see data availability statement).
Discussion
Racism and racial discrimination are well-established risk factors associated with poorer health and disease outcomes, including higher allostatic load, cardiovascular disease, low birth weight, and earlier death.15,71 Studies that evaluate social and community context mechanisms of racism and discrimination remain underexamined.15,72,73
As of July 30, 2022, we found convincing support from 32 studies that some aspect of social connectedness influenced the association between racial discrimination and health (ie, the social-connectedness buffering hypothesis). Two potentially competing hypotheses emerge from this work. The first is a social-connectedness buffering hypothesis from effect modification studies and the second is a social-connectedness erosion hypothesis from mediation studies.
A range of methodologies were used across the 32 studies. The most frequently used methodology was effect modification whereby racism and/or racial discrimination was interacted with social connectedness predicting a health or disease outcome. The second most frequently used approach was either formal mediation analysis or where some stepwise adjustment was made, typically entering social connectedness in a second step of a regression analysis after racial discrimination. More than 80% of mediation or adjustment studies showed that the association between racial discrimination and health was partially or fully attenuated by social connectedness. These findings lend support for the social-connectedness erosion hypothesis—that racism and discrimination erode social connectedness, and this erosion blocks vital resources that can alleviate or ameliorate health disparities.32,70,74
Limitations and strengths of studies included in the review
The use of theory was not consistent across studies. Some authors used theory to frame and guide their analysis, whereas others used theory post hoc to explain their findings. Similarly, among effect modification studies, several did not provide an adequate description of their conceptual models or stated a priori the specific type of interaction expected (eg, statistical interaction, differences in strength or qualitative/crossover, differences in direction). Few studies provided omnibus tests for the overall interaction coefficient, and study authors rarely stratified their analysis after a significant interaction, nor did they plot their interactions. The reporting of measures of associations and significance values was not uniform, with some reporting unstandardized β values, standardized β values, SEs, or only P values with β values, and not all reporting 95% CIs.
In those studies in which mediation analyses were used, only some authors conducted formal tests of mediation, yet among those, not all provided the proportion of mediation explained or the proportion of the indirect effects. In those studies that used stepwise adjustment, few authors explicitly stated the statistical adjustment approach or calculated the proportion explained. In all studies, although many examined multiracial and ethnic groups, few conducted subgroup analyses to examine whether associations held for specific racial groups or by age or sex. Most studies were cross-sectional, which cannot be used to draw causal inference about associations. There were no randomized controlled trials or intervention studies; 1 longitudinal study used prospective data.
Despite these limitations, studies were generally strong and had a low risk of bias, specifically in terms of statistical analyses conducted, which is 1 section in the Joanna Briggs Institute Checklist.33 The most frequent weakness was that some studies had low reliability coefficients, which may influence the quality of the findings. Nevertheless, these studies contribute to a solid evidence base that social connectedness is important for addressing racism and racial discrimination associations on health.
Limitations and strengths of studies included in the review
There are some limitations to this review. We focused on health outcomes and not health-related behaviors, such as alcohol use, HIV testing, or smoking, which also contribute to racial disparities in health. As noted earlier, it is well known that racism affects behaviors such as alcohol, drug use, and HIV risk. Including behavioral outcomes such as substance use are areas in which review studies are needed. This review was strengthened by the urgent need to address racism as a public health issue75 and providing recommendations and tools that can inform interventions to complement what is already known about mechanisms and measures.1
Recommendations for future research
We recommend building the evidence on this topic in several areas. First, there must be greater use of social connectedness measures at the community, family, and geographic or area levels. There were vast conceptual and methodological differences in the intra- and interpersonal racism measures used in this study. As others have suggested, there is a need to consider a universal scale that could permit consensus and cross-cultural use.76,77
Beyond intrapersonal measures of racism, more studies should assess racial discrimination at the interpersonal level, including that aimed at entire families or between partners (eg, interracial marriages). There is also a need for studies that measure structural-level racism and racial discrimination (eg, neighborhood racial residential segregation) to understand whether social connectedness buffers associations with individual and population health. For example, other studies have found that social connectedness moderates the associations between structural conditions, such as neighborhood disorder, on mental health.78,79 This direction is important because of the push to measure and develop scalable interventions to address racism and discrimination at the structural level, which includes neighborhood or place-based manifestations of its consequences.80–82
Social connectedness measures varied vastly (eg, social support or ethnic connectedness, loneliness), and no measure was bounded by time. As such, we do not have evidence for which aspect or type of social connectedness matters most for health. We also do not know about the length of time (eg, months, years) that social connectedness should be generated and cultivated to have a significant buffering impact on poor health. We also do not know how long it takes racism to erode social connectedness for it to affect health. We could not determine whether there are thresholds of social connectedness that mattered most, although studies often showed protective associations above 1 or 2 SDs of mean cut points. Future studies should include prospective samples and conduct longitudinal analyses that allow us to strengthen the ability to draw causal statements about how social connectedness affects discrimination and health.
Future studies should use the social connectedness framework to organize how they define and measure the construct, and design studies to compare the strengths of associations among the measures. This approach is important to build the evidence on which facets (eg, structural, functional, or quality) of social connectedness matter most. Intervention strategies will differ; for instance, if the focus is on addressing structural forms such as social networks versus functional forms, such as perceived loneliness.
Finally, there is greater need for assessing intersectionality within racism and discrimination studies.83,84 One approach may include assessing social connectedness as a buffer or mediator of racism, in addition to sexism or other sexual minority discrimination via the use of gendered racism scales or stratifying across multiple demographic groups.85
Conclusion
The findings strongly reveal that social connectedness is important for buffering or mitigating the negative associations of racism and racial discrimination on health. Policy or social enterprise interventions to strengthen social connectedness among racial minority groups is 1 practical suggestion that arises from this work. Ongoing and future quantitative studies should include social connectedness measures along with racism and racial discrimination items. These studies should conduct effect modification and mediation analyses in all statistical analyses. It is no longer sufficient to document disparities or conclude that discrimination is bad for one’s health; the field should strive to build evidence of what buffers or mitigates the deleterious impacts and how the mechanisms work.
In longer-term research efforts, epidemiologists should develop measures that assess anticipatory responses to racism. Specifically, what questions capture one’s anticipation of experiencing some racially discriminatory event? Next, what questions capture people’s perceived or actual readiness of resources to mitigate the stress that might be associated with that racist exposure or event? Although these suggestions may appear to be a distal (even individual-level focused) strategy for addressing racism, it is necessary and complementary to other work already being done1,2,10 to advance measuring structural-level factors of racism and discrimination.
Supplementary material
Supplementary material is available at Epidemiologic Reviews online.
Funding
This work was funded by National Institutes of Health grants R01DA056264, UG3AI169655, and K01MH111374.
Conflict of interest
The authors declare no conflicts of interest.
Disclaimer
The views expressed in this article are those of the authors and do not reflect those of the National Institutes of Health.
Data availability
The data of articles are available from the corresponding author or directly from the Open Science Framework (https://osf.io/vy5s6/).
Supplementary Material
Contributor Information
Yusuf Ransome, Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, CT 06510, United States.
Alberto D Valido, School of Education, Applied Developmental Sciences and Special Education, Human Development and Family Science, School Psychology, University of North Carolina Chapel Hill, Chapel Hill, NC 27514, United States.
Dorothy L Espelage, School of Education, Applied Developmental Sciences and Special Education, Human Development and Family Science, School Psychology, University of North Carolina Chapel Hill, Chapel Hill, NC 27514, United States.
Graceson L Clements, School of Education, Applied Developmental Sciences and Special Education, Human Development and Family Science, School Psychology, University of North Carolina Chapel Hill, Chapel Hill, NC 27514, United States.
Crystal Harrell, Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, CT 06510, United States.
Caroline Eckel, Department of Sociology, University of California, Davis, Davis, CA 95616, United States.
Natalie Price, Milken Institute School of Public Health, Department of Prevention and Community Health, The George Washington University, Washington, DC 20037, United States.
Rachel Nassau, The George Washington School of Medicine and Health Sciences, Washington, DC 20052, United States.
Kate Nyhan, Harvey Cushing/John Hay Whitney Medical Library, Yale School of Public Health, New Haven, CT 06510, United States.
Tamara L Taggart, Department of Social and Behavioral Sciences, Yale School of Public Health, New Haven, CT 06510, United States; Milken Institute School of Public Health, Department of Prevention and Community Health, The George Washington University, Washington, DC 20037, United States.
References
- 1. Ford CL, Griffith DM, Bruce MA, Gilbert KL, eds. Racism: Science & Tools for the Public Health Professional. American Public Health Association; 2019. 10.2105/9780875533049 [DOI] [Google Scholar]
- 2. Bailey ZD, Krieger N, Agénor M, et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet. 2017;389(10077):1453–1463. ( 10.1016/S0140-6736(17)30569-X). [DOI] [PubMed] [Google Scholar]
- 3. Krieger N. Does racism harm health? Did child abuse exist before 1962? On explicit questions, critical science, and current controversies: an ecosocial perspective. Am J Public Health. 2008;98(1 Suppl):S20–S25. ( 10.2105/ajph.98.supplement_1.s20). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nazroo JY. The structuring of ethnic inequalities in health: economic position, racial discrimination, and racism. Am J Public Health. 2003;93(2):277–284. ( 10.2105/ajph.93.2.277). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Williams D, Williams-Morris R. Racism and mental health: the African American experience. Ethn Health. 2000;5(3–4):243–268. [DOI] [PubMed] [Google Scholar]
- 6. Jones CP. Levels of racism: a theoretic framework and a gardener's tale. Am J Public Health. 2000;90(8):1212–1215. ( 10.2105/ajph.90.8.1212). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Busette, C. Overcoming racism to advance economic opportunity: Dr. Camille Busette's testimony before the House Committee on Ways and Means. 2022. Accessed April 6 2022.https://www.brookings.edu/testimonies/overcoming-racism-to-advance-economic-opportunity/Accessed April 6 2022
- 8. Nguyen TT, Criss S, Michaels EK, et al. Progress and push-back: how the killings of Ahmaud Arbery, Breonna Taylor, and George Floyd impacted public discourse on race and racism on twitter. SSM Popul Health. 2021;15:100922. ( 10.1016/j.ssmph.2021.100922). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Adkins-Jackson PB, Chantarat T, Bailey ZD, et al. Measuring structural racism: a guide for epidemiologists and other health researchers. Am J Epidemiol. 2022;191(4):539–547. ( 10.1093/aje/kwab239). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Krieger N, Smith K, Naishadham D, et al. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61(7):1576–1596. ( 10.1016/j.socscimed.2005.03.006). [DOI] [PubMed] [Google Scholar]
- 11. Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. ( 10.2105/ajph.86.10.1370). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Friedman EM, Williams DR, Singer BH, et al. Chronic discrimination predicts higher circulating levels of E-selectin in a national sample: the MIDUS study. Brain Behav Immun. 2009;23(5):684–692. ( 10.1016/j.bbi.2009.01.002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Glass JE, Williams EC, Oh H. Racial/ethnic discrimination and alcohol use disorder severity among United States adults. Drug Alcohol Depend. 2020;216:108203. ( 10.1016/j.drugalcdep.2020.108203). [DOI] [PubMed] [Google Scholar]
- 14. Wyatt SB, Williams DR, Calvin R, et al. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325(6):315–331. ( 10.1097/00000441-200306000-00003). [DOI] [PubMed] [Google Scholar]
- 15. Williams DR, Lawrence J, Davis B. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105–125. ( 10.1146/annurev-publhealth-040218-043750). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. LaVeist TA. On the study of race, racism, and health: a shift from description to explanation. Int J Health Serv. 2000;30(1):217–219. ( 10.2190/LKDF-UJQ5-W1KU-GLR1). [DOI] [PubMed] [Google Scholar]
- 17. Hare-Duke L, Dening T, Oliveira D, et al. Conceptual framework for social connectedness in mental disorders: systematic review and narrative synthesis. J Affect Disord. 2019;245:188–199. ( 10.1016/j.jad.2018.10.359). [DOI] [PubMed] [Google Scholar]
- 18. Holt-Lunstad J. Social connection as a public health issue: the evidence and a systemic framework for prioritizing the “social” in social determinants of health. Annu Rev Public Health. 2022;43:193–213. ( 10.1146/annurev-publhealth-052020-110732). [DOI] [PubMed] [Google Scholar]
- 19. Holt-Lunstad J. Loneliness and social isolation as risk factors: the power of social connection in prevention. Am J Lifestyle Med. 2021;15(5):567–573. ( 10.1177/15598276211009454). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ellison CG, Musick MA, Henderson AK. Balm in Gilead: racism, religious involvement, and psychological distress among African-American adults. J Sci Study Relig. 2008;47(2):291–309. ( 10.1111/j.1468-5906.2008.00408.x). [DOI] [Google Scholar]
- 21. Hope MO, Assari S, Cole-Lewis YC, et al. Religious social support, discrimination, and psychiatric disorders among Black adolescents. Race Soc Probl. 2017;9(2):102–114. ( 10.1007/s12552-016-9192-7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bierman A. Does religion buffer the effects of discrimination on mental health? Differing effects by race. J Sci Study Relig. 2006;45(4):551–565. ( 10.1111/j.1468-5906.2006.00327.x). [DOI] [Google Scholar]
- 23. Holt-Lunstad J, Robles TF, Sbarra DA. Advancing social connection as a public health priority in the United States. Am Psychol. 2017;72(6):517–530. ( 10.1037/amp0000103). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Holt-Lunstad J. Social isolation and health. Health Affairs Health Policy Brief. June 21, 2020. ( 10.1377/hpb20200622.253235). [DOI] [Google Scholar]
- 25. Vice Chairman's Staff of the Joint Economic Committee and Senator Mike Lee . The Geography of Social Capital in America. Joint Economic Committee. 2018. Accessed August 1, 2022. https://www.jec.senate.gov/public/_cache/files/e86f09f7-522a-469a-aa89-1e6d7c75628c/1-18-geography-of-social-capital.pdf [Google Scholar]
- 26. Brooks, D. America is having a moral convulsion. 2020. Accessed August 1, 2022.https://www.theatlantic.com/ideas/archive/2020/10/collapsing-levels-trust-are-devastating-america/616581/
- 27. Bailey M, Cao R, Kuchler T, et al. Social connectedness: measurement, determinants, and effects. J Econ Perspect. 2018;32(3):259–280. ( 10.1257/jep.32.3.259). [DOI] [PubMed] [Google Scholar]
- 28. Rajkumar K, Saint-Jacques G, Bojinov I, et al. A causal test of the strength of weak ties. Science. 2022;377(6612):1304–1310. ( 10.1126/science.abl4476). [DOI] [PubMed] [Google Scholar]
- 29. Chetty R, Jackson MO, Kuchler T, et al. Social capital I: measurement and associations with economic mobility. Nature. 2022;608(7921):108–121. ( 10.1038/s41586-022-04996-4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Ransome Y, Ojikutu BO, Buchanan M, et al. Neighborhood social cohesion and inequalities in COVID-19 diagnosis rates by area-level Black/African American racial composition. J Urban Health. 2021;98(2):222–232. ( 10.1007/s11524-021-00532-3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ransome Y, Luan H, Dean LT, et al. Is race-specific neighborhood social cohesion key to reducing racial disparities in late HIV diagnosis: a multiyear ecological study. Spat Spatiotemporal Epidemiol. 2022;42:100508. ( 10.1016/j.sste.2022.100508). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gilbert KL, et al. Social capital, Black social mobility, and health disparities. Annu Rev Public Health. 2022;43:173–191. ( 10.1146/annurev-publhealth-052020-112623). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Moola S, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. Joanna Briggs Institute Reviewer's Manual. The Joanna Briggs Institute; 2017. [Google Scholar]
- 34. Beach SRH, Lei MK, Simons RL, et al. Perceived relationship support moderates the association of contextual stress with inflammation among African Americans. J Fam Psychol. 2019;33(3):338–348. ( 10.1037/fam0000509). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hicks MR, Kogan SM. The influence of racial discrimination on smoking among young Black men: a prospective analysis. J Ethn Subst Abuse. 2020;19(2):311–326. ( 10.1080/15332640.2018.1511493). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Liao KY, Weng CY, West LM. Social connectedness and intolerance of uncertainty as moderators between racial microaggressions and anxiety among Black individuals. J Couns Psychol. 2016;63(2):240–246. ( 10.1037/cou0000123). [DOI] [PubMed] [Google Scholar]
- 37. Mama SK, Li Y, Basen-Engquist K, et al. Psychosocial mechanisms linking the social environment to mental health in African Americans. PloS One. 2016;11(4):e0154035. ( 10.1371/journal.pone.0154035). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Marshall GL, Rue TC. Perceived discrimination and social networks among older African Americans and Caribbean Blacks. Fam Community Health. 2012;35(4):300–311. ( 10.1097/FCH.0b013e318266660f). [DOI] [PubMed] [Google Scholar]
- 39. Nelson T, Brown MJ, Garcia-Rodriguez I, et al. Gendered racism, anxiety, and depression: the mediating roles of gendered racialized stress and social isolation. Ethn Health. 2021;28(1):12–28. ( 10.1080/13557858.2021.2002826). [DOI] [PubMed] [Google Scholar]
- 40. Nguyen AW, Chatters LM, Taylor RJ, et al. Discrimination, serious psychological distress, and church-based emotional support among African American men across the life span. J Gerontol B Psychol Sci Soc Sci. 2018;73(2):198–207. ( 10.1093/geronb/gbx083). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Priest JB, McNeil Smith S, Woods SB, et al. Discrimination, family emotional climate, and African American health: an application of the BBFM. J Fam Psychol. 2020;34(5):598–609. ( 10.1037/fam0000621). [DOI] [PubMed] [Google Scholar]
- 42. Saasa S, Miller S. Biopsychosocial predictors of depression and anxiety symptoms among first-generation Black African immigrants. Soc Work. 2021;66(4):329–338. ( 10.1093/sw/swab038). [DOI] [PubMed] [Google Scholar]
- 43. Steers MN, Chen TA, Neisler J, et al. The buffering effect of social support on the relationship between discrimination and psychological distress among church-going African-American adults. Behav Res Ther. 2019;115:121–128. ( 10.1016/j.brat.2018.10.008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wong CF, Schrager SM, Holloway IW, et al. Minority stress experiences and psychological well-being: the impact of support from and connection to social networks within the Los Angeles House and Ball communities. Prev Sci. 2014;15(1):44–55. ( 10.1007/s11121-012-0348-4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Jang YP, Cho YJ, Park NS, et al. Perceived racial discrimination and mental distress in older Korean Americans: the moderating role of ethnic resources. Ethn Health. 2021;28(1):1–11. ( 10.1080/13557858.2021.2022105). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kim I. The role of critical ethnic awareness and social support in the discrimination-depression relationship among Asian Americans: path analysis. Cultur Divers Ethnic Minor Psychol. 2014;20(1):52–60. ( 10.1037/a0034529). [DOI] [PubMed] [Google Scholar]
- 47. Rollock D, Lui PP. Do spouses matter? Discrimination, social support, and psychological distress among Asian Americans. Cultur Divers Ethnic Minor Psychol. 2016;22(1):47–57. ( 10.1037/cdp0000045). [DOI] [PubMed] [Google Scholar]
- 48. Wei M, Wang KT, Heppner PP, et al. Ethnic and mainstream social connectedness, perceived racial discrimination, and posttraumatic stress symptoms. J Couns Psychol. 2012;59(3):486–493. ( 10.1037/a0028000). [DOI] [PubMed] [Google Scholar]
- 49. Garcini LM, Chen MA, Brown R, et al. "Abrazame que Ayuda" (hug me, it helps): social support and the effect of perceived discrimination on depression among US- and foreign-born Latinxs in the USA. J Racial Ethn Health Disparities. 2020;7(3):481–487. ( 10.1007/s40615-019-00676-8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lorenzo-Blanco EI, Meca A, Unger JB, et al. Cultural stress, emotional well-being, and health risk behaviors among recent immigrant Latinx families: the moderating role of perceived neighborhood characteristics. J Youth Adolesc. 2019;48(1):114–131. ( 10.1007/s10964-018-0907-5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Nair RL, RMB W, Roosa MW, et al. Cultural stressors and mental health symptoms among Mexican Americans: a prospective study examining the impact of the family and neighborhood context. J Youth Adolesc. 2013;42(10):1611–1623. ( 10.1007/s10964-012-9834-z). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rodriguez CJ, Gwathmey TYM, Jin Z, et al. Perceived discrimination and nocturnal blood pressure dipping among Hispanics: the influence of social support and race. Psychosom Med. 2016;78(7):841–850. ( 10.1097/PSY.0000000000000341). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Roth KB, Musci RJ, Eaton WW. The relationship between Latinxs' acculturative experiences and mental and behavioral disorder in the National Latino and Asian American Study. Prev Sci. 2022;23(7):1196–1207. ( 10.1007/s11121-022-01376-2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Torres L, Pachicano JB, Bird CM, et al. Ethnic discrimination, social cohesion, and mental health among Latinx adults. Am J Orthopsychiatry. 2022;92(1):51–57. ( 10.1037/ort0000586). [DOI] [PubMed] [Google Scholar]
- 55. Bergeron G, Lundy de la Cruz N, Gould LH, et al. Association between racial discrimination and health-related quality of life and the impact of social relationships. Qual Life Res. 2020;29(10):2793–2805. ( 10.1007/s11136-020-02525-2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Busby DR, Horwitz AG, Zheng K, et al. Suicide risk among gender and sexual minority college students: the roles of victimization, discrimination, connectedness, and identity affirmation. J Psychiatr Res. 2020;121:182–188. ( 10.1016/j.jpsychires.2019.11.013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Goosby BJ, Walsemann KM. School racial composition and race/ethnic differences in early adulthood health. Health Place. 2012;18(2):296–304. ( 10.1016/j.healthplace.2011.10.002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lee Y, Muennig P, Kawachi I, et al. Effects of racial prejudice on the health of communities: a multilevel survival analysis. Am J Public Health. 2015;105(11):2349–2355. ( 10.2105/AJPH.2015.302776). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Majeno A, Tsai KM, Huynh VW, et al. Discrimination and sleep difficulties during adolescence: the mediating roles of loneliness and perceived stress. J Youth Adolesc. 2018;47(1):135–147. ( 10.1007/s10964-017-0755-8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Maleku A, Kim YK, Kirsch J, et al. The hidden minority: discrimination and mental health among international students in the US during the COVID-19 pandemic. Health Soc Care Community. 2021;30(5):e2419–e2432. ( 10.1111/hsc.13683). [DOI] [PubMed] [Google Scholar]
- 61. Scheuermann TS, Saint Onge JM, Ramaswamy M, et al. The role of neighborhood experiences in psychological distress among African American and White smokers. Race Soc Probl. 2020;12(2):133–144. ( 10.1007/s12552-020-09281-5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Sheikh IS, Alsubaie MK, Dolezal ML, et al. The role of social connectedness in buffering the effects of discrimination on post-trauma cognitions in forcibly displaced Muslims. Psychol Trauma. 2022;14(1):47–54. ( 10.1037/tra0001070). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Yang TC, Chen D. A multi-group path analysis of the relationship between perceived racial discrimination and self-rated stress: how does it vary across racial/ethnic groups? Ethn Health. 2018;23(3):249–275. ( 10.1080/13557858.2016.1258042). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Walton E. Resurgent ethnicity among Asian Americans: ethnic neighborhood context and health. J Health Soc Behav. 2012;53(3):378–394. ( 10.1177/0022146512455426). [DOI] [PubMed] [Google Scholar]
- 65. Negi NJ. Battling discrimination and social isolation: psychological distress among Latino day laborers. Am J Community Psychol. 2013;51(1–2):164–174. ( 10.1007/s10464-012-9548-0). [DOI] [PubMed] [Google Scholar]
- 66. Singh S, McBride K, Kak V. Role of social support in examining acculturative stress and psychological distress among Asian American immigrants and three sub-groups: results from NLAAS. J Immigr Minor Health. 2015;17(6):1597–1606. ( 10.1007/s10903-015-0213-1). [DOI] [PubMed] [Google Scholar]
- 67. VanderWeele TJ, Knol MJ. A tutorial on interaction. Epidemiol Methods. 2014;3(1):33–72. ( 10.1515/em-2013-0005). [DOI] [Google Scholar]
- 68. Tingley, K. We need to understand the difference between isolation and loneliness: both can pose distinct dangers to our mental and physical health. New York Times Magazine. 2021. Accessed September 2022. https://www.nytimes.com/2021/08/18/magazine/isolation-loneliness-health.html
- 69. Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community. 2017;25(3):799–812. ( 10.1111/hsc.12311). [DOI] [PubMed] [Google Scholar]
- 70. Brondolo E, Libretti M, Rivera L, et al. Racism and social capital: the implications for social and physical well-being. J Soc Issues. 2012;68(2):358–384. ( 10.1111/j.1540-4560.2012.01752.x). [DOI] [Google Scholar]
- 71. Kramer MR, Hogue CR. What causes racial disparities in very preterm birth? A biosocial perspective. Epidemiol Rev. 2009;31(1):84–98. ( 10.1093/ajerev/mxp003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Anderson RE, Lee DB, Hope MO, et al. Disrupting the behavioral health consequences of racial discrimination: a longitudinal investigation of racial identity profiles and alcohol-related problems. Health Educ Behav. 2020;47(5):706–717. ( 10.1177/1090198120923268). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Lewis TT, Cogburn CD, Williams DR. Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol. 2015;11:407–440. ( 10.1146/annurev-clinpsy-032814-112728). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Fullilove MT. Root Shock: How Tearing Up City Neighborhoods Hurts America and What We Can Do About It. Random House, Inc; 2004. [Google Scholar]
- 75. American Public Health Association . Structural Racism is a Public Health Crisis: Impact on the Black Community. 2020. Accessed September 30, 2022. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2021/01/13/structural-racism-is-a-public-health-crisis
- 76. Bastos JL, Celeste RK, Faerstein E, et al. Racial discrimination and health: a systematic review of scales with a focus on their psychometric properties. Soc Sci Med. 2010;70(7):1091–1099. ( 10.1016/j.socscimed.2009.12.020). [DOI] [PubMed] [Google Scholar]
- 77. Stewart AL, Nápoles-Springer AM. Advancing health disparities research: can we afford to ignore measurement issues? Med Care. 2003;41(11):1207–1220. ( 10.1097/01.MLR.0000093420.27745.48). [DOI] [PubMed] [Google Scholar]
- 78. Pearson AL, Sadler RC, Kruger DJ. Social integration may moderate the relationship between neighborhood vacancy and mental health outcomes: initial evidence from Flint, Michigan. Appl Res Qual Life. 2019;14(4):1129–1144. ( 10.1007/s11482-018-9646-8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Dawson CT, Wu W, Fennie KP, et al. Perceived neighborhood social cohesion moderates the relationship between neighborhood structural disadvantage and adolescent depressive symptoms. Health Place. 2019;56:88–98. ( 10.1016/j.healthplace.2019.01.001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Dougherty GB, Golden SH, Gross AL, et al. Measuring structural racism and its association with BMI. Am J Prev Med. 2020;59(4):530–537. ( 10.1016/j.amepre.2020.05.019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Egede LE, Walker RJ. Structural racism, social risk factors, and COVID-19—a dangerous convergence for Black Americans. N Engl J Med. 2020;383(12):e77. ( 10.1056/NEJMp2023616). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Bor J, Venkataramani AS, Williams DR, et al. Police killings and their spillover effects on the mental health of Black Americans: a population-based, quasi-experimental study. Lancet. 2018;392(10144):302–310. ( 10.1016/S0140-6736(18)31130-9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Holley LC, Tavassoli KY, Stromwall LK. Mental illness discrimination in mental health treatment programs: intersections of race, ethnicity, and sexual orientation. Community Ment Health J. 2016;52(3):311–322. ( 10.1007/s10597-016-9990-9). [DOI] [PubMed] [Google Scholar]
- 84. Earnshaw VA, Jonathon Rendina H, Bauer GR, et al. Methods in HIV-related intersectional stigma research: core elements and opportunities. Am J Public Health. 2022;112(S4):S413–S419. ( 10.2105/AJPH.2021.306710). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Gullett LR, Alhasan DM, Gaston SA, et al. Neighborhood social cohesion and serious psychological distress among Asian, Black, Hispanic/Latinx, and White adults in the United States: a cross-sectional study. BMC Public Health. 2022;22(1):1–17. ( 10.1186/s12889-022-13572-4). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data of articles are available from the corresponding author or directly from the Open Science Framework (https://osf.io/vy5s6/).


