Abstract
In Ethiopia, the WHO strategies to stop coronavirus transmission were implemented rapidly. As a result, there was a rapid change in hygiene behavior, which are basic for preventing COVID-19 and other contagious diseases. This research was designed to examine the sustainability of the COVID-19 imposed hygiene behaviors for future challenges. The study was conducted in 2 major nexus areas in Addis Ababa. The data were collected using a questionnaire and spot-check from 622 respondents selected by systematic random sampling. The questionnaire was given at every 15th interval in several spots of the site. Observational hygiene-check was done through observing key personal hygiene conditions. Proportion, χ2 test, and Poisson’s regression were applied for the analysis. The χ2-test analyses showed that the hand washing frequency before, during, and post-COVID-19 was statistically significant (P < .005). Findings from the spot-check also show that the hands of 76.8%, the nails of 68.7%, and the hairs of 70.7% of the respondents were clean. The major driving factors for the rapid changes in hygiene behavior were the awareness developed (95%), the fear and panic (90%), and increased access to water and soap (63%). Nevertheless, the major reasons for failing to continue the COVID-19-imposed good hygiene practice in the post-COVID-19 times include the decline in infection and death rates (26%) and the decline in facility access (20%). Hand washing frequency significantly changed during the COVID-19 pandemic indicating that the practice as part of the preventive strategy was successful. However, as this was mainly due to the fear and panic in the community, the COVID-19 imposed hand washing practice did not bring real and sustainable behavioral changes. This indicates that for long-lasting changes in hygiene behavior, continuous and better approach need to be introduced.
Keywords: coronavirus, COVID-19, Ethiopia, fear and panic, hand hygiene, hand washing frequency, pandemics
Background information
Handwashing is a key practice in reducing the spread and transmission of infectious diseases and it has been considered as the key strategy to COVID-19 pandemic prevention.
The contribution of this research to the field
This research contributes valuable information on how to sustain behavioral changes observed under turbulent conditions.
The implications of this research towards theory, practice, or policy
The findings showed the importance of hygiene facility for sustainable hygiene behavioral change over panic and fear-induced changes implying that access to facility is more important than promotion and fear to sustain hygiene behavioral change.
Introduction
According to WHO and public health research institutions, the current pandemic is the most contagious and the quickest transmission recorded in the history of humankind. COVID-19 has threatened all countries in the world, albeit to a different extent and in different ways. The pandemic touched every corner of the globe within less than 2 years. During times of a global pandemic, protective health behaviors are of particular public interest, with health agencies and governments highlighting the importance to slow down the spread of SARS-CoV-2 infections. 1 Although several aspects of the emergence of new variants, and treatments were not clear for several months, scientists agreed on key prevention strategies (social distancing, hand washing, mask-wearing, and staying at home) to protect oneself and others from SARS-CoV-2 infections. People in all nations around the world including Ethiopia were practicing the 4 key prevention strategies since the pandemic has officially informed. If these key preventive measures are well understood and habituated, they are taken as effective measures to control the pandemic. 2
According to the WHO guidelines, effective hand washing is defined as an act of cleaning hands for at least 20s with water and soap (or equivalent materials), and in critical situations such as before preparing a meal, after coming home, or after arriving at work. 3 The contribution of water, sanitation, and hygiene (WASH) to the COVID-19 response is done primarily by promoting good hygiene behavior, and mainly by ensuring frequent and proper handwashing practice, which has been shown as one of the most important measures to prevent infections with the virus. 4 WHO underscores the importance of proper handwashing as general infection prevention control measures for individuals and for health care settings. 5
The epidemiological evidence on the importance of handwashing for the prevention of water-borne and respiratory infections was accumulated even before the outset of COVID-19. By improving WASH, the risk of diarrhea (water-borne illness) is reduced by about 42% to 47% as well as the respiratory infections by more than 21%.6,7 Handwashing is a key practice in reducing the spread and transmission of infectious diseases such as pneumonia, influenza, HIV-related infections, and environmental enteropathies.3,8,9 According to WHO, 88% of diarrhea cases worldwide are attributed to unsafe water, inadequate sanitation, or insufficient hygiene, and these cases result in 1.5 million deaths each year. 10 Because of this, there was a long tradition of handwashing promotion in many health campaigns mainly focusing on hand washing before food preparation, before eating or feeding a child, after using the toilet, and cleaning a child such as after changing diapers. 11 Promoting the frequency of hand washing can prevent about 30% of diarrhea-related illnesses 12 and about 20% of respiratory infections. 6
Numerous studies show how important healthcare workers’ (HCWs) hands are in the spread of microorganisms to patients and the hospital environment. 13 Hand hygiene is the leading measure for preventing the spread of antimicrobial resistance and reducing healthcare-associated infections. 14 Hand hygiene prevents the transmission of bacteria, which is critical in health facilities. When new infections are prevented, the use of antibiotics is reduced and, consequently, the development of resistance is also prevented.15,16 In response to the rising burden of healthcare-associated infections, the severity of sickness, and the complexity of treatment brought on by illnesses caused by drug-resistant pathogens, health professionals are returning to the basics of infection prevention using simple practices like hand washing. Several reports justified this is because of the presence of sufficient scientific evidence to support the idea that hand hygiene alone, when properly implemented, may significantly reduce the risk of infection cross-transmission in healthcare facilities.17 -19
Although vaccines appear to be effective for preventing hospitalization and mortality from COVID-19, 20 those who are vaccinated may be less motivated to protect themselves using distancing, mask wearing and hand hygiene because of lower perceived risk of COVID-19. 21
While some studies have shown that increasing the frequency of hand washing can effectively prevent illness, there is no advice regarding the specific frequency of washing hands that is needed. 22 A systematic review showed that the more frequently hands were washed, the lower risk of the disease, however, from their analysis the authors stated that they could not get high-quality evidence indicating the best range of hand washing frequency for a disease prevention. 22 Clean water, sanitation, and hygiene (WASH) services are considered the key part of preventing and protecting human health from the current COVID-19 pandemic. 3 For effective removal of germs, hands should be washed with soap and water for at least 20 seconds during an emergency by taking special attention to the germs that may be trapped under nails and in crevices. 23 Therefore, enfranchising hand-washing behavior is not only just to prevent the present pandemic transmission but also it can play a key role in the prevention of other contagious and WASH-related diseases.
However, it is hard to believe that the behavioral change observed in the community during this pandemic has been naturalized to tackle the resurgence of COVID-19 and other WASH-related contagious infections. In Ethiopia, particularly in Addis Ababa, several efforts have been done to improve the hygiene behavior of the community to stop the virus transmission. The determinants of handwashing behavior in domestic settings include perceived risk, access to water and soap, availability of handwashing facilities, habitual background, and social and cultural norms.24 -26 Nevertheless, it is hardly clear to conclude whether the behavioral change observed is superficial and fear-induced or partly/fully sustained for future advantage. Therefore, it is prudent to evaluate the sustainability of the change in hygiene behavior and assure its future promise. The aim of this study was to evaluate the changes in hygiene behavior the due to the COVID-19 pandemic and examine its sustainability and associated deterring factors.
Research Method
Study Sites
This research was carried out in 2 sub-cities of Addis Ababa: Yeka and Arada Sub-cities. Addis Ababa is the most COVID-19 pandemic-hit city in Ethiopia. Study population was selected from 2 sites of the 2 sub-cities: Megenagna in Yeka Sub-cities and Piazza in Arada Sub-cities. Megenagna and Piazza Sub-cities are the 2 most busiest and nexus point in the city next to Mercato. The areas, where the sample population was taken, are the nexus of the city where people from every corner of the city meet. We believe that the sample population is representative of the source population. According to assessment reports, the city is ranked among the highest in its WASH-related diseases such as diarrhea, mainly in its slum areas. 27 Access to sanitation services and solid waste management is generally poor. Only 64% of the solid waste generated is properly disposed of; 74% of the residents use pit latrines, only 7% use flush toilets and 17% use open field toilets. 28 Previously, there were 2 public domestic wastewater treatment plants with a limited treatment capacity of 30% of collected gray and black water.
Sample Size, Study Design, and Data Collection
The sample size for this descriptive study was calculated using a single population proportion formula for population.
n = the required sample size;
P = assuming 50% expected true proportion;
Z(1 − α\2) = the critical value at 99% confidence level; and
d = precision (margin of error) = 5%
Accordingly, n = 623.
This study was conducted by using cross-sectional study design. It was carried out 2 times: during and after the peak-COVID-19 pandemic. The information before COVID-19 was collected using a retrospective design. The 2 sampling sites contain heterogeneous community in terms of socio-economic status, age, educational status, and job types. This helps to catch different people with different socioeconomic and socio-demographic backgrounds. The quantitative data were collected using 2 approaches: a semi-structured questionnaire, and observational hygiene-check approaches. Standardized questionnaire was designed to collect information about socio-economic and demographic conditions, the trend of changes in hygiene behavior (pre-COVID-19, during COVID-19, and post-COVID-19) and factors influencing the hygiene behavior.
In both study sites, systematic random sampling was used to select the study population. The questionnaire was given at every 15th interval in several spots of the site. The observational hygiene-check approach was used to collect information about the practice of the recommended key prevention strategies on the ground. The checklist was designed to test how individuals are practicing the so-called behavioral change on the ground and without informing the respondent so that the individual would display the actual behavior.
Data Analysis
All the data collected were categorical type and thus all the variables/items were coded. The data were first filled in an excel spreadsheet with the code and meanings side by side. Then, the data were exported to a predesigned dataset in STATA software. Proportions, contingency coefficients, and chi-square were used to describe selected groups, to see the association between outcome and predictor variables, and compare unpaired groups (respondents’ hygiene practice behavior such as before and after COVID-19 pandemic). Poisson logistic regression was used to determine the association between the factors and the practice hand washing. P < .05 (2-sides) was considered significant in the analysis.
Results
Socio-Economic Aspects of the Study Population
The socioeconomic information about the study population is given in Table 1. The population included 62% male and 38% female with heterogeneous age groups ranging from <20 years (5%) to above 51 years (3%). The majority of the respondents (>70%) were in the range of 21 to 40 years. The high proportion of the middle-aged groups (20-40 years) is clearly due to the fact that majority of the aged-people were staying at home, which may be due to the pandemic. Most of the respondents (76%) of the study population were employed either in the government or in private sectors. In terms of education, the study population were nearly equal proportion of all educational status from high school complete to higher education.
Table 1.
Socio-Economic Aspects of the Respondents.
| Variables | Category | Proportion (%) |
|---|---|---|
| Sex | Male | 62 |
| Female | 38 | |
| Age (years) | <20 | 5.1 |
| 31-30 | 39.8 | |
| 41-50 | 20.4 | |
| >50 | 3.1 | |
| Job | Unemployed | 5.1 |
| Daily laborers | 10.2 | |
| Employed | 76.5 | |
| Private business | 8.2 | |
| Educational status | No education | 22.4 |
| 1-12 | 21.4 | |
| Diploma | 36.0 | |
| ≥BSc | 19.2 | |
| Income | <1000 | 29.6 |
| 1001-3000 | 19.4 | |
| 3001-5000 | 16.3 | |
| 5001-10 000 | 25.5 | |
| >10 000 | 9.2 | |
| Marital status | Single | 54.6 |
| Married | 19.26 | |
| Divorced | 22.15 | |
| Separated | 3.85 |
Hand-Washing Behavior Before, During, and Post-COVID-19
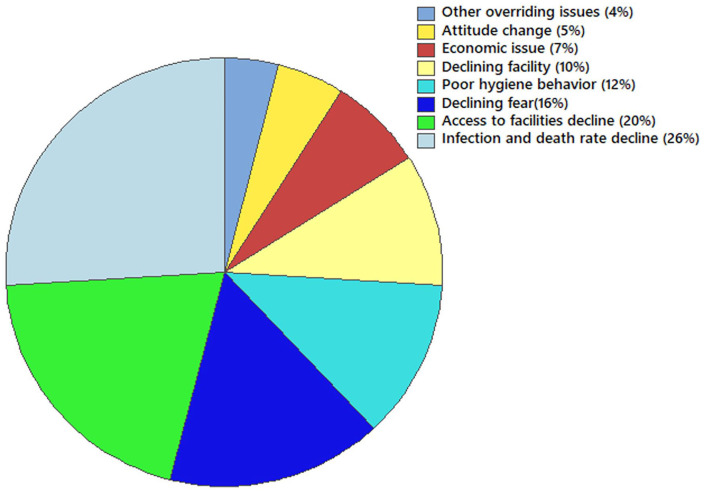
Hand washing frequency of the respondents ranged between 2 and 5 times before COVID-19; 5 and 13 times during COVID-19, and 3 and 9 times in post-COVID-19 pandemic (Figure 1). Two sample t-test analyses showed that the hand washing frequency before COVID-19 and during COVID-19, and post-COVID-19 is statistically significant (P < .005). The hand washing frequency rapidly increased as of WHO declared COVID-19 pandemic, May 2020, with an increasing mean hand washing frequency of 4 times before the pandemic to 8 times during the pandemic.
Figure 1.
Hand washing frequency of the respondents before, during, and post-COVID-19 pandemic (n = 622).
The finding in this assessment shows that before COVID-19 pandemic, about 92% of the respondents wash their hands 4 to 7 times a day. After the emergence of the pandemic, the respondents’ hand washing practice varies in the frequency and duration of washing and in using soap. During COVID-19 pandemic, more than 96% of the respondents wash their hands from 6 to 12 times in a day with majority of them wash 8 times in a day. However, in post-COVID-19, the frequency declined; more than 92% of the respondents wash their hands from 4 to 7 times a day.
Before the emergence of COVID-19, about 36% of them always wash with soap, 48% sometimes use soap and 16% of the respondents wash without soap. However, after the emergence of COVID-19, more than 72% of the respondents were using soap in every hand washing moments. Respondents also asked whether they prefer handwashing with water or hand rubbing with sanitizer to clean their hands. Among the study population, 48.5% use soap for handwashing, 6.9% prefer using sanitizer whilst, 44.6% preferably use both soap and sanitizer depending on conditions including availability, the level of hand contamination, and types of contaminants. For many of the respondents, the use of both washing and rubbing is mainly associated with fear of the virus transmission.
Table 2 shows major community perceptions to the pandemic-induced hygiene behaviors. Among the respondents, 83% of them believe that the current good hygiene behavior is due to the fear and panic they developed due to the COVID-19 pandemic. As a result, 68% of the participants believe that the hygiene behavior is could not be sustainable. In fact, 79% of them think that the pandemic could be an opportunity to change the poor hygiene behavior of the society before the pandemic.
Table 2.
Proportion Estimation of Major Community Perception About the COVID-19 Imposed Hygiene Practice (N = 622).
| Proportion | SE | [95% CI] | |
|---|---|---|---|
| If your current hygiene practice is due to the COVID-19 pandemic, do you think that the change is sustainable? | |||
| No | 0.6831683 | 0.0465241 | [0.5846596, 0.7676002] |
| Yes | 0.3168317 | 0.0465241 | [0.2323998, 0.4153404] |
| Is your current good hygiene practice due to fear of COVID-19 or understanding the benefit? | |||
| Fear | 0.8316832 | 0.0374147 | [0.7440905, 0.8935825] |
| Realize | 0.1683168 | 0.0374147 | [0.1064175, 0.2559095] |
| Do you believe that COVID-19 is an opportunity to bring behavioral change in the community? | |||
| No | 0.0792079 | 0.0270063 | [0.0396278, 0.1520612] |
| Yes | 0.9207921 | 0.0270063 | [0.8479388, 0.9603722] |
Handwashing Events During the COVID-19 Pandemic
According to the finding, there is highly significant perception difference between respondents to the various handwashing events before and during the pandemics (Table 3). Events indicated by the numbers 1, 4 to 7, 10, 11, 14, 15, 17 to 19 are practiced by 60% to 82% of the respondents during COVID-19 only.
Table 3.
Percentage of Respondents’ Practice for Selected Handwashing Events During the COVID-19 Pandemic.
| No. | Hand washing activities | Number of events of washing | |||
|---|---|---|---|---|---|
| Not | Before | During | Both | ||
| 1 | After touching seats | 23 | 0 | 76 | 1 |
| 2 | Before eating | 0 | 0 | 0 | 100 |
| 3 | After eating | 10 | 0 | 2 | 88 |
| 4 | After touching/opening and closing house doors | 23 | 0 | 76 | 0 |
| 5 | After any transportation use | 8 | 0 | 80 | 12 |
| 6 | If building steps or step supports are touched | 28 | 0 | 72 | 0 |
| 7 | Before entering to house from outside | 9 | 0 | 74 | 17 |
| 8 | After toilet visit | 0 | 0 | 9 | 91 |
| 9 | After removing shoes | 49 | 0 | 51 | 0 |
| 10 | Before touching eyes, mouth, and nose | 13 | 0 | 81 | 6 |
| 11 | After/before removing mouth mask | 40 | 0 | 60 | 0 |
| 12 | Before touching any food items | 0 | 0 | 17 | 83 |
| 13 | Before handling babies and children | 29 | 0 | 42 | 29 |
| 14 | After touching any items brought outside home | 12 | 0 | 80 | 9 |
| 15 | After using phone, wallet, and money | 23 | 0 | 69 | 8 |
| 16 | After coughing and sneezing | 46 | 0 | 53 | 1 |
| 17 | When entering or leaving the household or any other building | 18 | 0 | 82 | 0 |
| 18 | After physical contact with individuals outside the home | 21 | 0 | 79 | 0 |
| 19 | After touching high contact surfaces (door handles, rails, and money) | 21 | 0 | 72 | 7 |
| 20 | After visiting public space | 39 | 0 | 53 | 8 |
| 21 | After caring for a sick individual | 0 | 0 | 67 | 33 |
Not = not important at all; Before = before COVID-19 only; During = during COVID-19 only; Both = both before and during COVID-19 pandemic.
Less important hand washing events such as after removing shoes, after/before removing mouth mask, after touching any items brought from outside and after using mobile phone and wallet were practiced during the COVID-19 by 51% to 80% of the respondents.
Factors Affecting Hygiene Practice During COVID-19
Table 4 shows the respondents’ reaction to selected factors affecting hygiene practice. Among the respondents, 63% believe that an increased access to water and soap helped them to wash frequently; and for 95% of the respondents the awareness they got push them to wash frequently. About 90% of the respondents believe that the fear and panic of the COVID-19 pandemics enforced them to wash frequently and regularly during the pandemic, and 82% of them were influenced by the frequent promotion in various outlets.
Table 4.
The Relationship Between Selected Variables and Frequency of Handwashing.
| Source | DF | Adj Dev | Adj Mean | χ2 | P-value |
|---|---|---|---|---|---|
| Regression | 24 | 66.725 | 2.7802 | 66.72 | .000 |
| Sex | 1 | 5.612 | 5.6117 | 5.61 | .018 |
| Age | 4 | 11.308 | 2.8271 | 11.31 | .023 |
| Educational status | 3 | 1.423 | 0.4742 | 1.42 | .700 |
| Job | 3 | 0.736 | 0.2452 | 0.74 | .865 |
| Income | 4 | 6.308 | 1.5770 | 6.31 | .177 |
| Before COVID-19 behavior | 3 | 13.364 | 4.4547 | 13.36 | .004 |
| Awareness to the risk | 1 | 2.387 | 2.3867 | 2.39 | .122 |
| Access to water and soap | 2 | 5.101 | 2.5504 | 5.10 | .078 |
| Fear and panic | 1 | 0.144 | 0.1442 | 0.14 | .704 |
| Promotion | 2 | 0.540 | 0.2701 | 0.54 | .763 |
To examine the association of some selected factors and hand washing during COVID-19, fit Poisson’s regression analysis was employed. The analysis shows that the association was significant (χ2 = 66.71, P < .005). Among the factors, sex, age, and the hand washing habit before the pandemic associated significantly with the hand washing practice during COVID-19 (Table 4).
Factors Deterring Handwashing Practice in Post-COVID-19
A 2-sample t-test analysis shows that there is significant decline of hand washing frequency in few months of the pandemic emergence. During covid-19, the frequency of hand washing was increased.
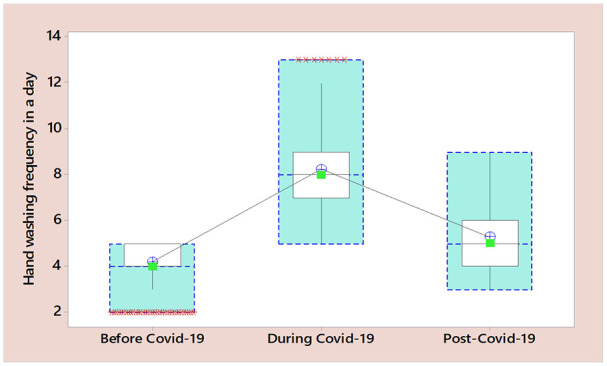
A list of several potential factors inhibiting individuals’ effort to continue the COVID-19-imposed hygiene behavior for post-pandemic life were given to the respondents. For the respondents, the major reasons deterring the continuation of the hygiene behavior are numerous and complex (Figure 2). According to the participants, the major reasons for failing to continue the COVID-19-imposed good hygiene practice include decline in infection and death rate (26%), the decline in facility access (20%), the decline in COVID-related panic (16%), poor hygiene behavior (12%), and decline in hand washing facility (10%).
Figure 2.
Proportion of the participants’ response on the reasons for failing to sustain COVID-19 imposed good hygiene behavior.
Potential Benefits of COVID-19-Imposed Hygiene Practice
The responses of the study population on the possible benefits of the COVID-19 imposed hygiene behavior are given in Table 5. To the majority of the respondents (92%), the COVID-19 pandemic is an opportunity to bring about behavioral changes to the community’s hygiene practice. About 71% of the respondents replied that they had been infected 1 or more than 1 times by common cold, every month before the pandemic. However, during the pandemics, 85% of the respondents had not been infected by common cold/flue and other WASH-related diseases since COVID-19 emerged. About 82% of the respondents still wash their hands more frequently than pre-COVID-19 era.
Table 5.
Potential Benefits of COVID-19 Imposed Hygiene Behavior.
| Benefits related with COVID-19-induced changes | Proportions (%) |
|---|---|
| Hand washing frequency compared with pre-COVID-19 | |
| No change | 18 |
| Decreased | 0 |
| Increased | 82 |
| Planning to upgrade hygiene facility | |
| No plan | 49 |
| Planned | 51 |
| Physical activity at home | |
| No change | 13 |
| Increased physical activities at home | 85 |
| Decreased physical activities | 2 |
| Prevalence of contagious diseases | |
| No change | 5 |
| Decreased | 75 |
| Increased | 20 |
| Access to water and soap for hand washing | |
| No change | 10 |
| Increased | 80 |
| Decreased | 10 |
The Impact of Hygiene Promotion on Post-COVID-19 Hygiene Behavior
Pearson’s Chi-square test analysis shows significant statistical differences between handwashing frequency before, during, and post-COVID periods. The statistically significant differences between during and post-COVID-19 era handwashing frequency (χ2 = 12, P < .05) and the weak differences between pre-and post-COVID-19 era confirm the decline in handwashing frequency when the pandemic stops.
Table 6 shows respondents’ perception of the COVID-19 promotion and their commitments to sustain their current behavior. For about half of the study population (51%), the promotions were not appropriate to bring adherable and long staying behavioral change, instead, they seem to be planned to bring short-term changes by predicting fearful atrocities and horrific effects of the pandemic. According to 47.5% of the respondents, the interventions could not bring sustainable behavioral changes that can help the community to tackle the resurgence of COVID-19 and the transmission of other similar hygiene-related contagious diseases. However, none of the respondents denied the crucial role played by the promotion. About 87% of the respondents replied that the promotion should be wired with different types of strategies for sustainable behavioral change.
Table 6.
Respondents’ Perception of the COVID-19 Promotion and Their Commitments to Sustain the Behavior.
| Proportion | SE | |
|---|---|---|
| Do you think that the way of promoting to hygiene behavioral change is appropriate? | ||
| No | 0.505 | 0.0499975 |
| Yes | 0.495 | 0.0499975 |
| Do you think that the change in hygiene practice is nurtured in the community? | ||
| No | 0.475 | 0.0499 |
| Yes | 0.525 | 0.0499 |
| Do you think that the promotion should be continued for more future impact? | ||
| No | 0.129 | 0.0334882 |
| Yes | 0.871 | 0.033488 |
| Do you have a plan to improve your hygiene practice better than the present? | ||
| No | 0.119 | 0.0323567 |
| Yes | 0.881 | 0.0323567 |
| Do you continue your current good hygiene practice if the pandemic stops? | ||
| No | 0.0990099 | 0.0298675 |
| Yes | 0.9009901 | 0.0298675 |
Interestingly, more than 90% of the respondents showed commitment to continue their current hygiene behavior; and 88% of them have planned to improve their hygiene behavior even better than the present.
Discussion
Handwashing is a key practice in reducing the spread and transmission of infectious diseases such as pneumonia, influenza, HIV-related infections, and environmental enteropathies.8,9,29 Although there have been repeated hand hygiene promotion interventions by different international and national organizations for years, the change was not significant until the emergence of the COVID-19 pandemic. After the emergence of the pandemic, the respondents’ handwashing practices had significantly changed. At the beginning of the COVID-19 pandemic, cleaning hands with water and soap or rubbing with an alcohol-based sanitizer was done strictly beyond the instructions known as “My 5 Moments for Hand Hygiene.” The key handwashing times under normal conditions, including hand washing before and after eating, before touching food items, and after toilet visits, became regular and routine activities.
The increased hand-washing frequency was associated with fear and panic and the implementation of more effective promotion of hand-washing practice globally and nationwide by using unique approaches such as using famous and public figures, politicians, social activists, and ferocious images for promotion. These phenomena resulted in changes in the existing poor hygiene behavior in the community and reduced the prevalence of other hygiene-related infections, such as the common cold. Research comparing the occurrence of 19 major infectious diseases during the COVID-19 epidemic showed that the overall incidence of most infectious diseases has been in precipitous decline because of the implementation of COVID-19 measure. 30 During the pandemic, associated with numerous factors, fear and panic were also heightened, which made people wash their hands more frequently. 25 Therefore, for most of the study population, COVID-19 was an opportunity to bring about appropriate behavioral change so that it could play crucial roles in controlling the incidence and transmission of other hygiene-related contagious diseases.
Less important hand washing events such as after removing shoes, after or before removing a mouth mask, after touching any items brought from outside, and after using a mobile phone and wallet were observed. Similar events such as hand washing before touching your eyes, nose, or mouth, after touching your mask, after leaving a public place, and after touching high-contact objects or surfaces such as door handles, tables, gas pumps, shopping carts, or electronic cashier registers or screens were also documented. 31 This was mainly associated with unprecedented fear and panic resulting from the severity, the fast transmission rate, the difficult routes of exposure, and the scale of the promotion. The fear and panic were exacerbated by the social isolation imposed by the COVID-19 lockdown and led to anxiety and consequently a decline in mental health in the general population.32,33
Although hand-washing practice during COVID-19 was frequent, its sustainability was under question because many believed that the necessity of hand hygiene during such events was tied to the current pandemics. Educated respondents believe that the current good hygiene practices such as frequent washing, using soap for handwashing, using hand-rubbing sanitizers, and avoiding touching the mouth, nose, and eyes with unclean hands or fingers were not a true behavioral change; rather, they were a superficial type of behavior that resulted from the fear and panic of COVID-19.
Many of the handwashing facilities installed in every business area, in public places, and in street yards at the beginning of the COVID-19 pandemic declined rapidly. This resulted in a decline in the frequency of handwashing. Moreover, the hygiene behavior of society before COVID-19 was poor, and thus this could not provide a comfortable background to continue the good hygiene behavior post-COVID-19.
Therefore, hand hygiene programs are more likely to be effective if they are designed to address the factors that enable or prevent hand hygiene from being practiced in a particular context. 25 Moreover, since the major driving force for current hygiene behavior is the fear and panic associated with COVID-19, it would be difficult to sustain the practice. Although the fear and panic declined, for the majority of the respondents, there was a tendency and commitment to continue the hand washing behavior if the hygiene facility continued. This is clearly reflected by the majority of the respondents’ plans to install hand-washing facilities at home.
Hygiene promotion is not a new phenomenon. Efforts have been made for decades to improve hygiene behavior using different intervention techniques such as information and education, community-based approaches, social and commercial marketing, psychology, and social theory. 25 Traditional hygiene promotion is an age-old approach to stopping the transmission of different contagious and fecal-oral diseases. During the pandemic, traditional hygiene promotion was inefficient in stopping the transmission, and thus the usual hygiene protocols were modified in a way effectively tackle new emerging problems. In this respect, promotion plays a key role in nurturing the new strategies in the community.
It is known that information- and education-based promotions for hygiene and sanitation interventions, which require real behavioral change, have failed in many instances, particularly during pandemics. According to Dreibelbis and co-workers, 34 education and an information-based approach for COVID-19 pandemic prevention intervention show mixed pieces of evidence, while for information adherence and sustainability, the approach is likely ineffective. Previous experiences also show that promotion with community-based approaches was found to be more effective for information uptake and adherence than other approaches, but still, with mixed shreds of evidence, bringing about real and sustainable behavioral change is more effective. 35
Limitations of the Study
This study raised the future relevance of one of the preventive measures to the current puzzling issue, the timely assessment, and the sustainability of COVID-19-induced hygiene behavior. However, the study did not include people with stay-at-home conditions. It may also be important to further investigate and follow up on the changes in hygiene behavior in the post-COVID-19 era. Moreover, since the study was questionnaire-based, the responses of the respondents may not illustrate the true picture, but there was no way to control this response bias.
Conclusion
Hand washing frequency significantly changed during the COVID-19 pandemic, indicating that the practice as part of the preventive strategy was successful. This was mainly due to the easily accessible hygiene facilities installed in most public areas in the city and the fear and panic in the community caused by uncontrolled media outlets and conspiracies. However, the significant decrease in post-COVID-19 hand washing practices indicates that the COVID-19-imposed hand washing practices did not bring about real changes in hygiene behavior in the community. The findings showed the importance of access to hygiene facilities such as water supply, soap, and washing facilities to bring about sustainable hygiene behavioral change over panic and fear-induced changes, indicating the importance of hygiene facilities for sustainable hygiene behavioral change. Although the hand washing frequency in post-COVID-19 countries decreases, several positive attributes indicate that the pandemic-imposed changes in hygiene behavior will have positive consequences for the future. Additionally, modest hygiene practices can play crucial roles in avoiding a variety of infectious illnesses, such as diarrhea, respiratory infections, eye and skin infections, and other infections. Though the majority of the respondents prefer the promotion to continue, education-based promotion is not the right strategy to sustainably nurture the practice and make it part of community behavior.
Supplemental Material
Supplemental material, sj-xlsx-1-inq-10.1177_00469580231218421 for Hygiene Behavior and COVID-19 Pandemic: Opportunities of COVID-19-Imposed Changes in Hygiene Behavior by Adnan Sirage Ali, Meseret W. Yohannes and Tsedey Tesfahun in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Footnotes
Author Contributions: Adnan Sirage Ali – Corresponding author, Conceptualization, Methodology, Software, Formal analysis, Writing—Original Draft, and Writing—Review & Editing. Tsedey Tesfahun—Financing, Coordination, Data entry, Conceptualization, and Writing—Review & Editing. Meseret W. Yohaness—Financing, Coordination, Writing—Review & Editing, and Data interpretation.
Availability of Data and Materials: The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval Statement: This research was carried out in accordance with the National Research Ethics Review Guidelines Fifth edition. We obtained ethical approval and clearance from National Research Ethics Review Committee, under Ethiopian Ministry of Education.
Consent to Participate: Before the data collection started, all the participants signed a written consent containing details on name of the researcher, research title, purpose of research, specific procedures to be used, benefits to the individual, risks to an individual, confidentiality, and human subject statement.
ORCID iD: Adnan Sirage Ali  https://orcid.org/0000-0003-1962-1774
https://orcid.org/0000-0003-1962-1774
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Vally Z. Public perceptions, anxiety and the perceived efficacy of health-protective behaviours to mitigate the spread of the SARS-Cov-2/COVID-19 pandemic. Public Health. 2020;187:67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO. Key Messages and Actions for COVID-19 Prevention and Control in Schools. World Health Organization; 2020. [Google Scholar]
- 3. WHO. WHO COVID-19 Dashboard. World Health Organization; 2020. [Google Scholar]
- 4. Giné-Garriga R, Requejo D, Molina JL, Pérez-Foguet A. A novel planning approach for the water, sanitation and hygiene (WaSH) sector: the use of object-oriented Bayesian networks. Environ Model Softw. 2018;103:1-15. doi: 10.1016/j.envsoft.2018.01.021 [DOI] [Google Scholar]
- 5. World Health Organization. Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions: Scientific Brief, 09 July 2020. WHO; 2020. [Google Scholar]
- 6. Aiello AE, Coulborn RM, Perez V, Larson EL. Effect of hand hygiene on infectious disease risk in the community setting: a meta-analysis. Am J Public Health. 2008;98(8):1372-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Curtis V, Schmidt W, Luby S, Florez R, Touré O, Biran A. Hygiene: new hopes, new horizons. Lancet Infect Dis. 2011;11(4):312-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Choi TS, Han JY, Heo CE, Lee SW, Kim HI. Electrostatic and hydrophobic interactions of lipid-associated α-synuclein: the role of a water-limited interfaces in amyloid fibrillation. Biochim Biophys Acta Biomembr. 2018;1860(9):1854-1862. doi: 10.1016/j.bbamem.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 9. Mushi V, Shao M. Tailoring of the ongoing water, sanitation and hygiene interventions for prevention and control of COVID-19. Trop Med Health. 2020;48(1):1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pruss-Ustun A, Organization WH. Safer Water, Better Health: Costs, Benefits and Sustainability of Interventions to Protect and Promote Health. World Health Organization; 2008. [Google Scholar]
- 11. Dreibelbis R. Hygiene Behavior Change and COVID-19. London School of Hygiene and Tropical Medicine; 2021. [Google Scholar]
- 12. Ejemot-Nwadiaro RI, Ehiri JE, Meremikwu MM, Critchley JA. Hand washing for preventing diarrhoea. Cochrane Database Syst Rev. 2008;1:CD004265. [DOI] [PubMed] [Google Scholar]
- 13. Pittet D, Allegranzi B, Sax H, et al. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006;6(10):641-652. [DOI] [PubMed] [Google Scholar]
- 14. Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73(4):305-315. [DOI] [PubMed] [Google Scholar]
- 15. Sax H, Allegranzi B, Uckay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007;67(1):9-21. [DOI] [PubMed] [Google Scholar]
- 16. Trampuz A, Widmer AF. Hand hygiene: a frequently missed lifesaving opportunity during patient care. Mayo Clin Proc. 2004;79(1):109-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Daniels I, Rees B. Handwashing: simple, but effective. Ann R Coll Surg Engl. 1999;81(2):117. [PMC free article] [PubMed] [Google Scholar]
- 18. WHO. Guidelines on hand hygiene in health care. First global patient safety challenge. Clean care is safer care. WHO. 2009. Accessed August 24, 2010. http://www.who.int/patientsafety/en/ [PubMed] [Google Scholar]
- 19. Kampf G, Kramer A. Epidemiologic background of hand hygiene and evaluation of the most important agents for scrubs and rubs. Clin Microbiol Rev. 2004;17(4):863-893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Buchan SA, Chung H, Brown KA, et al. Estimated effectiveness of COVID-19 vaccines against Omicron or Delta symptomatic infection and severe outcomes. JAMA Netw Open. 2022;5(9):e2232760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Brewer NT, Cuite CL, Herrington JE, Weinstein ND. Risk compensation and vaccination: can getting vaccinated cause people to engage in risky behaviors? Ann Behav Med. 2007;34(1):95-99. [DOI] [PubMed] [Google Scholar]
- 22. Xun Y, Shi Q, Yang N, et al. Associations of hand washing frequency with the incidence of illness: a systematic review and meta-analysis. Ann Transl Med. 2021;9(5):395. doi: 10.21037/atm-20-6005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Reed R, Godfrey S, Kayaga S, et al. Technical Notes on Drinking-Water, Sanitation and Hygiene in Emergencies. Loughborough University; 2013. [Google Scholar]
- 24. Kalam MA, Davis TP, Jr, Islam MA, Islam S, Kittle BL, Casas MP. Exploring behavioral determinants of handwashing with soap after defecation in an urban setting in Bangladesh: findings from a barrier analysis. J Water Sanit Hyg Dev. 2021;11(6):1006-1015. [Google Scholar]
- 25. White S, Thorseth AH, Dreibelbis R, Curtis V. The determinants of handwashing behaviour in domestic settings: an integrative systematic review. Int J Hyg Environ Health. 2020;227:113512. [DOI] [PubMed] [Google Scholar]
- 26. Zangana A, Shabila N, Heath T, White S. The determinants of handwashing behaviour among internally displaced women in two camps in the Kurdistan Region of Iraq. PLoS One. 2020;15(5):e0231694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Adane M, Mengistie B, Kloos H, Medhin G, Mulat W. Sanitation facilities, hygienic conditions, and prevalence of acute diarrhea among under-five children in slums of Addis Ababa, Ethiopia: baseline survey of a longitudinal study. PLoS One. 2017;12(8):e0182783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. CSA. Population Projection of Ethiopia for all Regions at Wereda Level From 2014–2017. CSA; 2013. [Google Scholar]
- 29. WHO. WHO Global Water, Sanitation and Hygiene: Annual Report 2020. World Health Organization; 2022. [Google Scholar]
- 30. Li H, Ling F, Zhang S, et al. Comparison of 19 major infectious diseases during COVID-19 epidemic and previous years in Zhejiang, implications for prevention measures. BMC Infect Dis. 2022;22(1):1-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. CDC. Handwashing in communities: clean hands save lives; 2023. https://www.cdc.gov/handwashing/index.html. Accessed May 04, 2023.
- 32. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Malcolm M, Frost H, Cowie J. Loneliness and social isolation causal association with health-related lifestyle risk in older adults: a systematic review and meta-analysis protocol. Syst Rev. 2019;8(1):1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Curtis V, Dreibelbis R, Sidibe M, et al. How to set up government-led national hygiene communication campaigns to combat COVID-19: a strategic blueprint. BMJ Glob Health. 2020;5(8):e002780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fewtrell L, Bartram J. Water Quality: Guidelines, Standards and Health. World Health Organization Water Series. IWA Publishing; 2001. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-xlsx-1-inq-10.1177_00469580231218421 for Hygiene Behavior and COVID-19 Pandemic: Opportunities of COVID-19-Imposed Changes in Hygiene Behavior by Adnan Sirage Ali, Meseret W. Yohannes and Tsedey Tesfahun in INQUIRY: The Journal of Health Care Organization, Provision, and Financing