Abstract
Neurological disorders are a diverse group of conditions that affect the nervous system and include neurodegenerative diseases (Alzheimer’s disease, multiple sclerosis, Parkinson’s disease, Huntington’s disease), cerebrovascular conditions (stroke), and neurodevelopmental disorders (autism spectrum disorder). Although they affect millions of individuals around the world, only a limited number of effective treatment options are available today. Since most neurological disorders express mitochondria-related metabolic perturbations, metformin, a biguanide type II antidiabetic drug, has attracted a lot of attention to be repurposed to treat neurological disorders by correcting their perturbed energy metabolism. However, controversial research emerges regarding the beneficial/detrimental effects of metformin on these neurological disorders. Given that most neurological disorders have complex etiology in their pathophysiology and are influenced by various risk factors such as aging, lifestyle, genetics, and environment, it is important to identify perturbed molecular functions that can be targeted by metformin in these neurological disorders. These molecules can then be used as biomarkers to stratify subpopulations of patients who show distinct molecular/pathological properties and can respond to metformin treatment, ultimately developing targeted therapy. In this review, we will discuss mitochondria-related metabolic perturbations and impaired molecular pathways in these neurological disorders and how these can be used as biomarkers to guide metformin-responsive treatment for the targeted therapy to treat neurological disorders.
Keywords: Alzheimer’s disease, Huntington’s disease, metformin, mitochondrial perturbation, multiple sclerosis, neural degenerative diseases, Parkinson’s disease, stroke, targeted therapy
Introduction: the Development and Therapeutic Use of Metformin
In medieval times, Gallega officinalis, a perennial herbaceous plant, was used as a folk medicine in Europe to relieve the frequent urination caused by the disease that is now known as diabetes mellitus. This plant is also named goat’s rue, French lilac, Spanish sainfoin, Italian fitch, or false indigo. In 1914, this plant was found to be rich in guanidine and derivatives (Tanret, 1914), these compounds account for 0.10–0.7% of the plant’s dry matter. In 1918, guanidine was found to be able to lower blood glucose levels in rabbits, but it was too toxic for clinical use (Watanabe, 1918). In 1929, several biguanides, including metformin, were synthesized. These biguanides preserve the anti-diabetic effect of their parent compound guanidine, however, with reduced toxicity. Physician Jean Sterne tested several biguanides in animal studies and eventually selected metformin for clinical trials. He termed the name “Glucophage” for metformin and published his studies in 1957 (Sterne, 1957). After 20 years of use in Europe, Canada, and other countries, the Food and Drug Administration approved the clinical use of metformin to treat patients with type 2 diabetes (T2D) in the USA in 1995. Metformin has been recommended by the American Diabetes Association and the European Association for the Study of Diabetes as the initial drug for the treatment of patients with T2D in 2012 (Inzucchi et al., 2012). Metformin is a time-proven effective agent for the treatment of patients with T2D, due to its safety and affordable price, it is now the most commonly prescribed oral anti-diabetic agent worldwide, taken by over 150 million people annually (He and Wondisford, 2015).
In the last decades, several studies have shown that patients with T2D treated with metformin had a reduction in cancer incidence (Yu et al., 2019). In experimental models, metformin can increase the mean lifespan of Caenorhabditis elegans (C. elegans) and mice (Cabreiro et al., 2013; Martin-Montalvo et al., 2013). The life expectancy of patients with T2D is typically reduced by up to 10 years (Waugh et al., 1989), while a study reported that diabetic patients treated with metformin monotherapy had longer survival rates than a matched, non-diabetic control (Bannister et al., 2014). The ability of metformin to extend the lifespan and improve the health of T2D patients and animal models has sparked interest in the drug as an anti-aging agent. More recently, metformin has been shown to promote neurogenesis, leading to the improvement of spatial memory formation, cognition, and motor function (Wang et al., 2012; Dadwal et al., 2015). These studies demonstrate that metformin has additional benefits beyond its anti-diabetic effect.
Metformin not only acts on peripheral systems (liver, gut, muscle, and adipose tissues) by regulating glucose and lipid metabolism but can also easily pass through the blood-brain barrier to directly impact brain function (Łabuzek et al., 2010). Multiple processes in the central nervous system, including neuroprotection, neural regeneration, angiogenesis, and anti-inflammation, can all be stimulated by metformin, making it an ideal drug candidate to treat neurological degenerative diseases. Metformin acts through multiple signaling pathways including energy sensing (AMP-activated protein kinase (AMPK) signaling), phosphatidylinositol 3-kinase (PI3K)-protein kinase B (AKT)-mammalian target of rapamycin (mTOR) signaling, lipid signaling (phospholipids and eicosanoids), inflammatory signaling, and mitochondrial-related signaling to modulate brain function (Rena et al., 2017; Rotermund et al., 2018). This review will highlight recent literature on the role of metformin in mitochondria-related metabolic perturbations and impaired molecular pathways in various neurologic diseases and provide insights into the potential use of biomarker-guided metformin treatment for personalized medicine.
Search Strategy and Selection Criteria
Studies cited in this narrative review on the effect of metformin on neuroprotection, neural regeneration, angiogenesis, and anti-inflammation in the brain were obtained from searching the PubMed database. Articles written between 2007 and 2022 in English were included. Five independent searches were completed by the authors JW and AL in February 2023.
The search queries were:
1) ((Alzheimer*)) AND ((brain) OR (neuro*) OR (CNS) OR (central nervous system)) AND ((metformin)) NOT (Review[Publication Type])
2) ((Parkinson*) OR (rotenone) OR (MPTP)) AND ((brain) OR (neuro*) OR (CNS) OR (central nervous system)) AND ((metformin)) NOT (Review[Publication Type])
3) ((multiple sclerosis) OR (demyelin*) OR (cuprizone) OR (experimental autoimmune encephalomyelitis) OR (EAE) OR (ethidium bromide)) AND ((brain) OR (neuro*) OR (CNS) OR (central nervous system)) AND ((metformin)) NOT (Review[Publication Type])
4) ((stroke) OR (ischem*)) AND ((brain) OR (neuro*) OR (CNS) OR (central nervous system)) AND ((metformin)) NOT (Review[Publication Type]))
5) ((Huntington*)) AND ((brain) OR (neuro*) OR (CNS) OR (central nervous system)) AND ((metformin)) NOT (Review[Publication Type])
Effects of Metformin on Neuroprotection
Many research groups have studied the role of metformin in neuroprotection in multiple facets. In one instance researchers utilized chemotherapy to impair the learning and memory of rodents. Treatment with metformin promoted cell survival and ameliorated memory impairments (Sritawan et al., 2020). Similar neuroprotective qualities have been observed in experimental epilepsy (Hussein et al., 2019) and pneumococcal meningitis (Muri et al., 2019). The role of metformin has also been studied extensively in the context of various neurodegenerative diseases, which will be examined below.
Parkinson’s disease
Parkinson’s disease (PD) is a neurodegenerative disorder that causes unintended and uncontrollable movements. Recent epidemiological studies have aimed to study the relationship between PD occurrence/progression and T2D patients receiving metformin therapy. A longitudinal study investigation veterans with T2D found that treatment with metformin for longer than 4 years decreased the risk of PD onset (Shi et al., 2019). However, another study in T2D patients over 50 years old found that the protective effects of metformin were dose-dependent, and lower odds of PD were only observed in T2D patients who received low-dose metformin (Huang et al., 2022). Interestingly, a recent bioinformatic analysis identified that metformin can be used as a candidate drug to target a set of PD-related genes on mitochondrial pathways (Xu et al., 2018). The pathogenic role of mitochondria in PD has mainly been linked to their function as energy producers for cells and the consequent effect of generators of reactive oxygen species (ROS) (Pirooznia et al., 2020). The importance of mitochondrial energy and ROS-associated production is underscored by some autosomal recessive forms of hereditary early-onset PD, whose genes (Parkin and PTEN-induced putative kinase 1 (PINK1)) have a role in mitochondrial bioenergetics and oxidative stress (Gautier et al., 2008; Larsen et al., 2018; Nicoletti et al., 2021). Recent work using an isogenic human induced pluripotent stem cell PD model showed that nitrosative stress-induced dysfunction in myocyte enhancer factor 2 stimulated peroxisome proliferator-activated receptor-γ coactivator-1α (PGC1α) transcription can lead to reduced mitochondrial biogenesis, contributing to the pathogenesis of PD (Ryan et al., 2013). Other work using genetically modified C. elegans as a PD model has implicated mitochondrial hyperactivity in the pathogenesis of PD (Mor et al., 2020).
In PD, the pathological characteristic is the presence of Lewy bodies which mainly contain a protein named α-synuclein that is highly phosphorylated at Ser129 (p-Ser129) to trigger protein aggregation (Arawaka et al., 2017). Both culture and in vivo work have shown that metformin treatment can reduce p-Ser129 α-synuclein either by epigenetic regulator enhancer of zeste homolog 2-mediated proteasomal degradation or by inhibition of the mTOR to activate protein phosphatase 2A (PP2A) in both AMPK-dependent and AMPK-independent manners (Figure 1; Pérez-Revuelta et al., 2014; Sardoiwala et al., 2020). Metformin-stimulated PP2A activity which can reduce α-synuclein phosphorylation has been confirmed in a neurotoxin 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced PD model where metformin possesses neuroprotective properties (Katila et al., 2017). When different MPTP-PD models (acute vs. chronic) and different doses of co-treatment metformin (low vs. high) are used in animal studies, metformin has produced contradictory results in terms of neuroprotection of tyrosine hydroxylase-positive (TH+) dopamine neurons (Patil et al., 2014; Ismaiel et al., 2016). Low-dose metformin in an acute MPTP-PD model accelerates TH+ dopamine neuron cell death by facilitating ROS production (Ismaiel et al., 2016). While high-dose metformin in a chronic MPTP-PD model reduces TH+ dopamine neuron death via restoration of MPTP-induced reduction of anti-oxidant mediator’s superoxide dismutase, catalase, and glutathione (Patil et al., 2014). Metformin also protects TH+ dopamine neurons from cell death via AMPK-independent pathways. A study found that metformin administration before and after MPTP injection (peri-treatment) was shown to protect TH+ dopamine neurons from cell death through the upregulation of mitochondrial proteins, such as PGC-1a via activation of the ATF2-CREB pathway (Kang et al., 2017). Similar results found that metformin was able to preserve TH+ dopaminergic cell number and volume after MPTP exposure (Bayliss et al., 2016).
Figure 1.
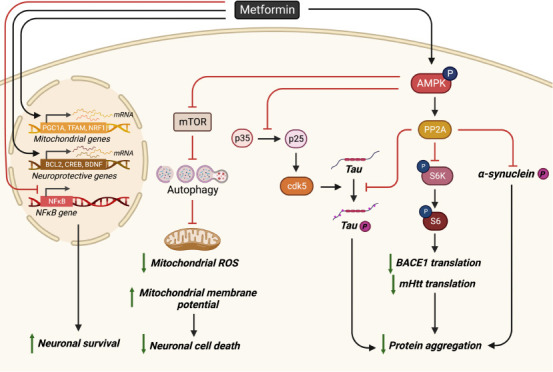
Schematic of metformin’s neuroprotective effects.
Metformin reduces protein aggregation through (1) AMPK-PP2A pathway to inhibit p-Ser129 α-synuclein in PD, (2) AMPK-mediated inhibition of p35 cleavage to p25, (3) through activation of the AMPK-PP2A-S6K-BACE1 pathway in AD, and (4) by disrupting the mitotic disruption-induced protein phosphatase 2A complex to activate PP2A via AMPK to reduce tau-phosphorylation in AD. Metformin can also increase neuronal survival via increased neuroprotective genes (Bcl-2 and CREB), mitochondria-associated genes (PGC1α, nuclear respiratory factor 1, and transcription factor A mitochondrial) expression, and reduced NF-κB gene expression that is AMPK dependent. Metformin treatment can reduce neuronal cell death by activating the AMPK-mTOR pathway to restore impaired autophagy, lower ROS production, mitochondrial fission, and increase mitochondrial membrane depolarization. Created with BioRender.com. AMPK: AMP-activated protein kinase; BACE1: beta-secretase 1; Bcl-2: B-cell lymphoma 2; BDNF: brain-derived neurotrophic factor; cdk5: cyclin-dependent kinase 5; CREB: cAMP response element-binding protein; mHtt: mutant huntingtin; mTOR: mammalian target of rapamycin; NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells; Nrf1: nuclear respiratory factor 1; PGC1α: peroxisome proliferator-activated receptor gamma coactivator 1-alpha; PP2A: protein phosphatase 2A; p-Ser129: phosphorylated at Ser129; ROS: reactive oxygen species; TFAM: transcription factor A, mitochondrial.
In addition to PD rodent animal models, C. elegans have been widely used as another model of PD for drug screening and discovery studies. One group utilized a high-throughput platform for automated scoring of worm postures and identified metformin as a potential candidate treatment for PD (Sohrabi et al., 2021). Another group generated a C. elegans model of 6-hydroxydopamine-induced dopaminergic neurodegeneration and α-synuclein protein aggregation and found that metformin significantly decreases neurodegeneration in 6-hydroxydopamine-induced worms, inhibits α-synuclein aggregation, and recovers food-sensing behavior. Associated with this, metformin can also upregulate the cat-2 gene (a putative tyrosine hydroxylase) and SOD-3 gene expression (Saewanee et al., 2021).
Recent work showed that metformin can rescue PD phenotypes in both chemically-induced and genetically-muted PD models that link to mitochondria hyperactivity/pathology (Adedeji et al., 2014; Lu et al., 2016; Fitzgerald et al., 2017; Chanthammachat and Dharmasaroja, 2019; Hang et al., 2019). Therefore, metformin may impact mitochondrial dysfunction at different stages of PD by modulating the expression of genes implicated in anti-oxidant protection, mitochondrial respiration, fragmentation, membrane potential, and biogenesis (Chanthammachat and Dharmasaroja, 2019). Importantly, metformin not only impacts mitochondria dysfunction but also induces the autophagy pathway by activation of AMPK-inhibited mTOR signaling for clearance of aggregated proteins, such as α-synuclein in PD models (Dulovic et al., 2014; Lu et al., 2016; Yan et al., 2017; Ozbey et al., 2020).
Alzheimer’s disease
In Alzheimer’s disease (AD), the classical pathological feature is the presence of beta-amyloid (Aβ) plaques and the formation of neurofibrillary tangles caused by tau accumulation. The amyloid cascade hypothesis of AD has been the central focus for the development of therapeutic strategies, although recent clinical failures with several classes of anti-Aβ drugs have made the research community rethink the current strategies being used to develop appropriate treatments for AD (Panza et al., 2019). Recent work showed that metformin treatment can reduce brain Aβ deposition, tau hyperphosphorylation, and tau pathology, and prevent neuronal cell death. Furthermore, metformin can rescue learning and memory deficits in APPswe/PS1DE9 (APP/PS1), SAMP8 and tau-seeded PS19 AD mice, and streptozotocin-induced diabetic rodents exhibiting tau pathology and Aβ deposition (Ou et al., 2018; Farr et al., 2019; Lu et al., 2020; Nassar et al., 2020; Pilipenko et al., 2020; Wang et al., 2020b; Oliveira et al., 2021; Zeng et al., 2021; Kazkayasi et al., 2022; Zhao et al., 2022). In addition, metformin treatment improves the spatial memory of aged mice in an APOE genotype-dependent manner (Zhang et al., 2019). Furthermore, in diabetic patients, metformin promoted a slower cognitive decline and a lower dementia risk (Bohlken et al., 2018; Shi et al., 2019; Sluggett et al., 2020; Secnik et al., 2021; Charpignon et al., 2022; Pomilio et al., 2022; Torrandell-Haro et al., 2022; Zheng et al., 2022), while in AD patients metformin promotes improved learning and memory (Koenig et al., 2017).
Multiple metformin-mediated mechanisms have been investigated to alleviate AD pathological hallmarks and behavioral deficits. Both AMPK-mTOR-S6K-BACE1 and AMPK-P65 NF-κB signaling pathways contribute to metformin-improved neurological deficits (Figure 1; Ou et al., 2018). Using the APP/PS1-AD mouse model, other researchers showed that chronic metformin treatment can disrupt the mitotic disruption-induced PP2A complex to activate PP2A. This not only reduces tau-phosphorylation to inhibit the formation of neurofibrillary tangles (Kickstein et al., 2010) but also down-regulates mTOR-initiated translational machinery to reduce amyloid precursor (APP) synthesis, consequently reducing Aβ (Figure 1; Hettich et al., 2014; Matthes et al., 2018). A recent study in the APP/PS1-AD mouse model further revealed that metformin inhibits the calpain-dependent cleavage of p35 into p25 to suppress cyclin-dependent kinase 5 hyper-activation and cyclin-dependent kinase 5-dependent tau hyperphosphorylation in the hippocampus (Figure 1). As an outcome, metformin treatment restores spine density, surface GluA1 trafficking, long-term potentiation expression, and spatial memory (Wang et al., 2020c). A new single-cell RNA-sequencing analysis reveals that 253 genes expressed abnormally in APP/PS1-AD mice were reversed by metformin at the molecular levels (Qiu-Yue et al., 2022).
Interestingly, mitochondrial dysfunction is known to play a critical role in AD either as a primary or secondary event (Wang et al., 2020b). One study has shown that mitochondrial fragmentation and abnormal mitochondrial distribution were observed in pyramidal neurons of an AD animal model, along with mitochondrial dysfunction, even before the accumulation of amyloid pathology (Misrani et al., 2021). Other studies show that mitophagy, the autophagy/lysosome pathway that removes damaged mitochondria, is compromised in AD (Chakravorty et al., 2019). The impaired mitophagy due to failed autophagy induction contributes to synaptic dysfunction and cognitive deficits by triggering Aβ and tau accumulation through increases in oxidative damage and cellular energy deficits, which in turn impaired mitophagy (Mary et al., 2022). On the other hand, mitophagy enhancement abolishes AD-related tau hyperphosphorylation in human neuronal cells and reverses memory impairment in transgenic tau nematodes and mice (Fang et al., 2019). These findings support the notion that mitochondrial fragmentation and impaired mitophagy act as a primary event and play a causal role in mitochondrial dysfunction and AD-related pathological and cognitive impairments in vivo. Both Aβ deposition, misfolded, and hyperphosphorylated tau protein are shown to disrupt Ca2+ homeostasis in mitochondria, contributing to AD progression by promoting superoxide generation, metabolic dysfunction, and neuronal cell death (Calvo-Rodriguez and Bacskai, 2021). These second mitochondrial dysfunction events triggered by amyloid and hyperphosphorylated tau contribute to AD progression to worsen clinical deficits.
Very recent work identifies differentially expressed genes within the mitochondrial genome from AD patient brain tissues. This work has suggested that specific mitochondrial molecular alterations are potential biomarkers for AD (Cavalcante et al., 2022). Significant defects in electron transport chain (ETC) complex I, II, IV, and V are also observed in AD patients’ hippocampus, entorhinal cortex, and temporal cortex, possibly contributing to impaired energy generation (Wang et al., 2020b). Finally, a redox proteomics study of AD/mild cognitive impairment patient brains showed an increase in oxidative stress proteins (Swomley and Butterfield, 2015). In this regard, targeting mitochondrial defects seems to be a promising strategy to combat AD.
Several studies have focused on understanding how metformin acts through mitochondrial and metabolic pathways to alleviate Aβ-induced cell death and pathology. Using a human neural stem cell culture model, researchers found that metformin can prevent Aβ-induced neuronal cell death. This occurs by restoring Aβ-decreased AMPK activity, rescuing Aβ-induced mitochondria deficiency, promoting neuroprotective gene expression including B-cell lymphoma 2 (Bcl-2) and cAMP response element-binding protein (CREB), and stimulating mitochondria-associated genes including PGC1α, nuclear respiratory factor 1, and transcription factor A mitochondrial (Figure 1; Chiang et al., 2016). Recent studies using a neuroblastoma cell line SH-SY5Y and hippocampal neurons revealed that metformin can inhibit Aβ-induced apoptosis by decreasing ROS and reversing autophagy defects (Figure 1; Chen et al., 2016; Li et al., 2019). Furthermore, metformin showed neuroprotective function in an Aβ-induced rat model via increasing long-term potentiation that was disrupted by Aβ injection and a high-fat diet (Asadbegi et al., 2016). Using a transgenic C. elegans strain overexpressing human Aβ peptide specifically in neurons, other researchers found that metformin can reverse Aβ-induced metabolic defects well before protein aggregation and normalize the lifespan of the mutant strain (Teo et al., 2019).
Contrary to the beneficial effects of metformin on neuroprotection in AD highlighted above, several studies pointed out that metformin may potentially worsen AD progression. In neuroblastoma cell culture models and other AD models, such as Tg6799-AD and P301S taupathy-AD models, metformin increased Aβ generation through APP cleavage. APP cleavage in the amyloidogenic pathway is a critical step in the generation of Aβ peptides, which accumulate in the brains of individuals with AD (Chen et al., 2009; Picone et al., 2015; Son et al., 2016). Interestingly, most of these studies focus on delineating underlying molecular mechanisms that mediate metformin-induced Aβ generation and tau aggregation, without measuring its effects on neuronal death. In addition, metformin also promoted tau aggregation independent of tau phosphorylation (Barini et al., 2016), increased memory dysfunction in male mice (DiTacchio et al., 2015), or has shown no effect on learning and memory (Li et al., 2012). Furthermore, in human patients with T2D metformin may increase the risk of developing AD/dementia (Moore et al., 2013; Kuan et al., 2017; Ha et al., 2021).
Stroke
A stroke occurs when the blood supply to a region of the brain is blocked or when a blood vessel in the brain bursts. Stroke-related ischemia/reperfusion causes mitochondria-associated dysfunction, including an imbalance between ROS production and clearance (oxidative stress), altered mitochondrial membrane potential, and high Ca2+ influx. These mitochondrial abnormalities can lead to neuronal damage and trigger apoptotic processes since the mitochondria are the starting place of many key apoptotic protein pathways, such as Bcl-2, cytochrome c, and apoptosis-inducing factor. Mitochondrial dynamics (fusion, fission, and mitophagy) are an important defense against cellular damage (Liu et al., 2018; Yang et al., 2018; He et al., 2020). Some research studies show that blocking proteins involved in mitochondrial fragmentation and mitophagy is protective and associated with decreased cytochrome c and apoptosis-inducing factor release from mitochondria (Yang et al., 2018; Shen et al., 2021). On the other hand, ischemia can also increase mitochondrial membrane potential to promote mitophagy which is protective against ischemic injury-induced cell death. While autophagy plays a detrimental effect during acute cerebral ischemic injury by accelerating cell death, the protective role of autophagy during reperfusion may be attributable to mitophagy-related mitochondrial clearance and inhibition of downstream apoptosis (Shi et al., 2021).
In stroke, metformin treatment has been shown to effectively protect the brain from ischemic injury either as a pre-stroke preconditioning agent or post-stroke drug treatment (Jiang et al., 2014; Liu et al., 2014a; Zhu et al., 2015; Ge et al., 2017; Westphal et al., 2020; Cao et al., 2022; Tu et al., 2022). Recent epidemiological studies have revealed that metformin use in pre-stroke T2D patients resulted in a less severe stroke (Castilla-Guerra et al., 2018; Westphal et al., 2020), lowered mortality (Horsdal et al., 2012; Wu et al., 2016), and improved outcome and recovery (Mima et al., 2016; Kersten et al., 2022). Similar neuroprotective effects of metformin have been shown in multiple in vivo and in vitro stroke models (Sheng et al., 2012; Farbood et al., 2015; Meng et al., 2016). In rodent models, metformin reduced stroke severity (Hollander et al., 2017) and promoted structural improvements including reduced infarct size and volume (Deng et al., 2016; Guo et al., 2017; Karimipour et al., 2018; Wang et al., 2021; Zemgulyte et al., 2021; Liu et al., 2022b), and reduced apoptosis (Fang et al., 2017; Gabryel and Liber, 2018; Ruan et al., 2021).
Metformin reduces ischemic injury-induced cell death via multiple signaling pathways induced by AMPK activation. These include reduced nuclear factor-κβ activity, induced autophagy pathway, increased Akt survival pathway, and enhanced mitochondria biogenesis and antioxidant pathway (Jiang et al., 2014; Liu et al., 2014a; Ashabi et al., 2014, 2015; Zhu et al., 2015; Ge et al., 2017; Cao et al., 2022). A derivative of metformin, metformin threonate, was able to promote more rapid AMPK activation and reduce infarct volume, lower mortality, and improve cognition in rats compared to metformin hydrochloride, highlighting the importance of AMPK activation (Zhang et al., 2022). Additionally, metformin has been shown to inhibit complex I activity providing neuroprotection and potentially stabilizing Ca2+ homeostasis after hypoxia (Skemiene et al., 2020; Jankeviciute et al., 2021; Svirskiene et al., 2021). In contrast, other studies have shown that metformin does not attenuate hypoxia-induced damage and may further exacerbate the effect of stroke dependent on timing and dosage (Li et al., 2010; Silva et al., 2022).
The neuroprotective effects of metformin can lead to improved behavioral outcomes in rodent stroke models. For example, ischemia pre-treatment with metformin has been shown to improve learning and memory (Ghadernezhad et al., 2016; Ashabi et al., 2017) and anxiety (Sarkaki et al., 2015).
Huntington’s disease
A Huntington’s disease (HD) is a rare, inherited disease caused by abnormal CAG repeats within the first exon of the huntingtin gene, Htt, which generates a mutant huntingtin (mHtt) showing toxic gain-of-function properties. The aggregation of mHtt impairs cell viability with particularly severe effects in neurons of the striatum. The pathogenesis of HD often associates with impaired autophagy and mitochondria dysfunction. mHtt can inhibit PGC1a expression at the transcriptional level to reduce mitochondrial biogenesis (Intihar et al., 2019), directly disrupt mitochondrial proteostasis through high-affinity binding with the mitochondrial inner membrane 23 (Yablonska et al., 2019), and affect the mitochondrial respiratory chain (Jędrak et al., 2018). The mitochondrial fragmentation/fission in the HD mouse striatum disrupts endoplasmic reticulum-mitochondria contacts leading to disturbances in Ca2+ efflux and ROS homeostasis (Cherubini et al., 2020). Recent work using single nuclear RNA sequencing and translating ribosome affinity purification sequencing showed that mHtt mediates the release of mitochondrial RNA which then binds to the innate immune sensor protein kinase R, resulting in the activation of innate immune signaling in the most vulnerable HD neurons: spiny projection neurons (Lee et al., 2020). More importantly, using human embryonic stem cell (hESC) culture models, researchers showed that these mitochondrial dysfunction signatures occur in HD-affected hESCs but not HD-affected hESCs-derived neural lineage cells, while a shift to transcriptional dysregulation and cytoskeletal abnormalities, the primary HD pathologies, appears in HD-affected differentiating hESCs along neural lineages in vitro (Monk and Connor, 2021). These results suggest that mitochondrial dysfunction may become an essential cause of HD pathology. In this regard, it seems plausible to target mitochondrial fission and oxidative stress for potential therapeutic strategies. Recent work has reported that metformin can reduce mHtt aggregation and restore impaired autophagy and mitochondria dysfunction via AMPK activation to protect neurons from mHtt-induced toxicity (Figure 1; Jin et al., 2016; Vázquez-Manrique et al., 2016; Sanchis et al., 2019; Gómez-Escribano et al., 2020). Interestingly, metformin is also shown to disrupt the MID1/PP2A/mTOR protein complex and reduce the translation rate of Htt mRNA, resulting in a reduction of mHtt protein production in an HD mouse model (Figure 1; Arnoux et al., 2018). Furthermore, metformin can both alleviate motor and neuropsychiatric phenotypes in an experimental-HD mouse model (Sanchis et al., 2019) and improve the cognition of T2D/HD patients (Hervás et al., 2017).
Multiple sclerosis
In multiple sclerosis (MS), the autoimmune system attacks myelin and myelin-producing cells, oligodendrocytes, causing demyelination which halts neurotransmission. This results in a wide array of motor and cognitive impairments including numbness, lack of coordination, and fatigue. Mitochondrial dysfunction has been considered to be involved in the pathogenesis of MS (Patergnani et al., 2017). First, mitochondrial DNA mutations can increase the risk of developing MS (Alharbi et al., 2019). Second, MS patient lesion sites are associated with reduced expression of nuclear respiratory factor 2 which impairs the expression of mitochondrial ETC subunits and increases oxidative damage/stress (Maldonado et al., 2022). However, the enhanced density of mitochondria and upregulated mitochondrial complex IV activity in MS lesion sites are also observed to be associated with increased mitochondrial stress protein mtHSP70, suggesting that enhanced density of mitochondria in MS lesions might also contribute to the formation of free radicals and subsequent tissue damage (Witte et al., 2009). Energy production and mitochondrial physiology are recognized as the main regulators of autophagy. Coincidently, ATG5 and Parkin, molecular markers of autophagy and mitophagy respectively, are elevated in the cerebral spinal fluid of MS patients during the active phases of the disease. This suggests that these processes play a role in MS pathogenesis and the possible use of these molecules as biomarkers of disease activity (Patergnani et al., 2018). Metformin has been shown to protect oligodendrocytes from immune system attack in both experimental autoimmune encephalomyelitis (EAE) models and cuprizone-induced multiple sclerosis models (Paintlia et al., 2013b; Largani et al., 2019). Recent work showed that metformin treatment improves spatial memory in a rat MS model induced by local ethidium bromide injection into the rat hippocampus (Arabmoazzen and Mirshekar, 2021). In addition, using lysophosphatidylcholine-induced demyelination in the optic chiasm revealed that metformin treatment attenuates lysophosphatidylcholine-induced demyelination and protects functional conductivity of the optic tract (Esmaeilnejad et al., 2021).
In summary, metformin can protect neurons and oligodendrocytes from pathogenic conditions in various neurodegenerative diseases, although controversial studies point out that metformin may have detrimental effects on some neurodegenerative diseases by accelerating their pathological features.
Effect of Metformin on Neural Regeneration
Neural regeneration has become a promising therapeutic strategy to treat neurodegenerative diseases. Interestingly, in the last decade, compelling evidence has emerged to show that metformin has the potential to be repurposed as a neural regenerative and remyelinating agent to treat various neurodegenerative diseases. Neural regeneration can be delivered in two ways, one is through the transplantation of exogenous neural cells from various sources, and the second way is to activate endogenous neural stem and progenitor cells to produce neural cells, including neurons and oligodendrocytes (Trueman et al., 2013). We have pioneered this line of research by publishing a ground-breaking paper a decade ago showing that metformin promotes adult neurogenesis and enhances spatial memory (Wang et al., 2012). Further work targeting endogenous neural stem cells in both rodent and human studies of radiation injury found that metformin improves the cognition of rodents and patients following radiation relative to a control/placebo (Ayoub et al., 2020; Derkach et al., 2021). Now more work has been done to examine metformin-induced neural regeneration in various neurodegenerative disease models.
Our recent work used a 3×Tg-AD model to show that dysregulated expression of monoacylglycerol lipase (Mgll) caused by the impaired atypical protein kinase C (aPKC) mediated CREB binding protein (CBP) phosphorylation in AD can be used as a marker to guide metformin-targeted therapy (reactivating the impaired aPKC-CBP pathway) to correct perturbed neurogenesis and spatial memory in AD (Syal et al., 2020). Others found that metformin can lead to neural repair and functional recovery in a model of childhood brain injury by activating both neurogenesis and oligodendrogenesis (Dadwal et al., 2015). A recent single-cell RNA-sequencing analysis showed that metformin increases the differentiation of neural stem cells and expands the population of neural stem cells and oligodendrocyte precursors in APP/PS1-AD mice (Qiu-Yue et al., 2022). In addition, metformin can promote central nervous system (CNS) remyelination in multiple models (Neumann et al., 2019; Kosaraju et al., 2020), and improve social interaction in a juvenile lysolecithin-induced focal demyelination mouse model (Kosaraju et al., 2020). Recent work on cuprizone-induced demyelination models showed that metformin treatment increases endogenous oligodendrogenesis via activated AMPK-Nrf2-mTOR signaling and facilitated neurotrophic factors (brain-derived neurotrophic factor, nerve growth factor, and ciliary neurotrophic factor) release (Houshmand et al., 2019; Sanadgol et al., 2020).
More importantly, metformin promotes neural regeneration by acting in multiple distinct molecular pathways. First, metformin not only induces subventricular zone neural stem and progenitor cell proliferation through increased expression of a protein called TAp73 but also enhances the differentiation of adult subventricular zone neural stem and progenitor cells into newborn neurons via the activation of the epigenetic AMPK-aPKC-CBP pathway (Figure 2; Fatt et al., 2015). Second, metformin acts through two distinct molecular pathways to enhance oligodendrocyte precursor (OPC) proliferation and differentiation, respectively. Metformin enhances OPC proliferation through early-stage autophagy inhibition, while it promotes OPC differentiation into mature oligodendrocytes by activating the AMPK-aPKC-CBP pathway (Figure 2; Kosaraju et al., 2020). Thus, the AMPK-aPKC-CBP pathway serves as a pro-differentiation pathway, stimulated by metformin, to enhance the genesis of newborn neurons and oligodendrocytes to replace lost neural cells in neurodegenerative diseases. Intriguingly, aPKC activity/expression exhibits double-edge outcomes in AD. Our work and other human brain studies showed that aPKC activity/expression is reduced in an AD animal model and human post-mortem brain samples (Moore et al., 1998; Tan et al., 2010; Syal et al., 2020), while others disclose that hyperactivity of aPKC provokes increases in brain β-secretase, Aβ40/42 and p-Thr231 tau (Sajan et al., 2018) under an insulin-resistant condition. In this regard, it is important to identify molecular markers that can stratify subpopulations of AD patients to guide metformin-targeted therapy (Syal et al., 2020).
Figure 2.
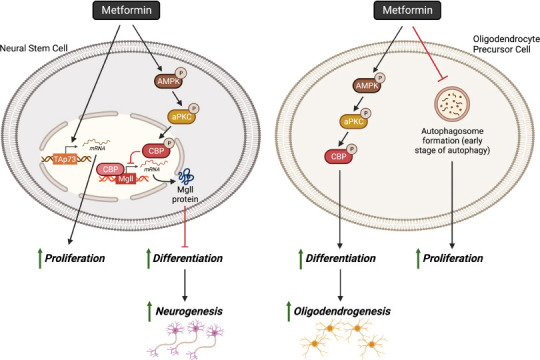
Schematic of metformin’s neural regenerative effects.
Metformin can stimulate the proliferation of NSCs by increased expression of TAp73. Metformin also promotes neurogenesis via the activation of the AMPK-aPKC-CBP pathway, which inhibits the transcription of Mgll, leading to enhanced differentiation. Metformin enhances OPC proliferation through early-stage autophagy inhibition, while it promotes OPC differentiation into mature oligodendrocytes through the AMPK-aPKC-CBP pathway to enhance the genesis of newborn oligodendrocytes. Created with BioRender.com. AMPK: AMP-activated protein kinase; aPKC: atypical protein kinase C; CBP: CREB-binding protein; Mgll: monoacylglycerol lipase; Tap73: tumor protein p73.
Metformin is not only a great regenerating and remyelinating agent to activate endogenous neural precursors, but also a promising candidate as a preconditioning reagent to maximize the grafting and differentiation potential of transplanted exogenous neural stem cells in vivo. It has been shown that pre-treatment of human induced pluripotent stem cell-derived neural stem cells with metformin before transplantation into the rat stroke brain can enhance their capability to graft and differentiate into neurons, astrocytes, and oligodendrocytes in vivo (Ould-Brahim et al., 2018). Metformin has been shown to promote the proliferation and differentiation of neuroblasts (Liu et al., 2014b, 2022a; Yuan et al., 2019), formation of oligodendrocytes (Livingston et al., 2020), and impact pericyte maturity and coverage (Geranmayeh et al., 2022; Liu et al., 2022a) following ischemic stroke. Interestingly, metformin’s ability to promote neural regeneration following stroke may be sex-dependent. Using a neonatal stroke model researchers have found that metformin promoted improved cognition in female, but not male, mice (Ruddy et al., 2019). Similar sex-dependent effects of metformin have also been observed in HD transgenic mouse models (Ma et al., 2007).
Effect of Metformin on Angiogenesis and Anti-Inflammation
Angiogenesis
In addition to neural cells, vascular cells in the CNS are important players to maintain healthy CNS function. The formation of new blood vessels via angiogenesis can result in disease pathogenesis or amelioration dependent on the disease. The effect of metformin on angiogenesis is highly dependent on the tissue/cell type as metformin can promote angiogenesis in some (Bakhashab et al., 2016; Zhu et al., 2020) and suppress angiogenesis in others (Han et al., 2018; El-Ghaiesh et al., 2020). For example, during cognitive decline in aged mice, metformin promotes endogenous neural stem cell recruitment via pro-angiogenic endothelial growth factor, ultimately generating neurovascular and improving memory (Zhu et al., 2020). In contrast, PD is associated with enhanced angiogenesis in humans (Yu et al., 2020) and mice (Elabi et al., 2021). Angiogenesis-related factor vascular endothelial growth factor in PD allows peripheral molecules and immune cells to contribute to the inflammatory cascade, ultimately contributing to pathogenesis. In this case, metformin has shown anti-angiogenic effects in a rotenone-induced model of PD which has been correlated to the neuroprotection of TH+ neurons in the substantia nigra (El-Ghaiesh et al., 2020).
Ischemic stroke results in the loss of both neural and vascular cells. Angiogenesis improves blood supply which provided oxygen and nutrients to the brain to aid in stroke recovery. The level of functional recovery after stroke is positively correlated with the extent of both post-stroke neurogenesis and angiogenesis (Angels Font et al., 2010). Metformin has been shown to have promising therapeutic potential in improving functional recovery following stroke. The beneficial effects of metformin on post-stroke functional recovery are associated with increased post-stroke neurogenesis and angiogenesis, and reduced blood-brain barrier disruption (Jin et al., 2014; Liu et al., 2014b; Venna et al., 2014).
Inflammation
Proinflammatory and anti-inflammatory effects mediated by immune cells contribute to the pathogenesis of multiple neurodegenerative diseases, such as AD, MS, PD, and stroke. Intriguingly, metformin has been shown to act on anti-inflammatory pathways to prevent/reduce the progression of these neural degenerative diseases.
Alzheimer’s disease
Using an APP/PS1-AD mouse model, researchers have shown that metformin can reduce the release of proinflammatory factors, interleukin-1 beta (IL-1β), tumor necrosis factor-alpha (TNF-α), and interleukin-6 (IL-6) in the hippocampus and cortex. At the same time, it can decrease the glial reactivity via activation of AMPK to suppress P65 (NF-κB), mTOR, and S6K activity (Figure 3; Ou et al., 2018; Lu et al., 2020). In addition, several animal studies have reported Mgll as a promising therapeutic target for AD to ameliorate AD-associated neuropathology, neuroinflammation, and memory decline (Piro et al., 2012). Mgll is a lipid hydrolase that breaks down the endocannabinoid 2-arachidonoyl glycerol to produce arachidonic acid (ARA) (and ARA-derived proinflammatory eicosanoids). Inhibition of Mgll activity not only enhances 2-arachidonoyl glycerol levels but also reduces ARA and ARA-derived proinflammatory eicosanoid levels (Figure 3; Piro et al., 2012). Since Mgll inhibitors provide many of the beneficial effects observed with direct cannabinoid receptor agonists or cyclooxygenase inhibitors without exerting their respective unwanted side effects, Mgll inhibitors have been put forth as a potential next-generation strategy for combating AD. Intriguingly, our recently published report showed that metformin can repress Mgll in the 3×Tg-AD animal model to rescue AD-associated memory decline (Syal et al., 2020). All of this work suggests that metformin may repress Mgll expression in AD to reduce AD-associated neuroinflammation.
Figure 3.
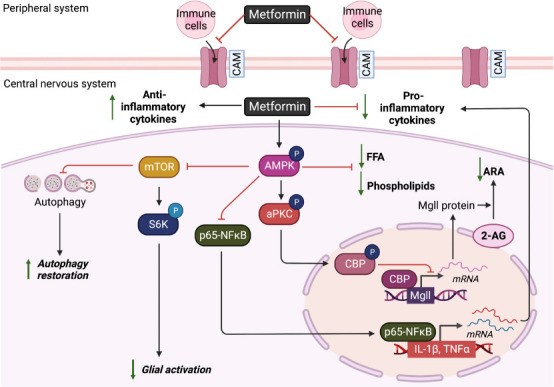
Schematic of metformin’s effects on angiogenesis and anti-inflammation in the central nervous system.
Metformin treatment reduces inflammatory molecules by (1) lowering mononuclear cells entering the central nervous system through CAMs; (2) increasing production of Th1 and Th17 to reduce proinflammatory cytokines (interferon-γ, TNF-α, IL-6, IL-17, and inducible nitric oxide synthase) release; (3) inhibiting transcription of Mgll via the AMPK-aPKC-CBP pathway to reduce the conversion of 2-AG to inflammatory ARA; and (4) activating AMPK-P65 NF-κB pathway to suppress the transcription of proinflammatory cytokines (IL-1β and TNF-α). Metformin treatment also reduces glial activation through the AMPK-mTOR-S6K pathway. Finally, metformin can also restore autophagy via the AMPK-mTOR pathway. Created with BioRender.com. 2-AG: 2-Arachidonoylglycerol; AMPK: AMP-activated protein kinase; aPKC: atypical protein kinase C; ARA: arachidonic acid; CAM: cell adhesion molecule; CBP: CREB-binding protein; FFA: free fatty acid; IL-1β: interleukin-1 beta; Mgll: monoacylglycerol lipase; mTOR: mammalian target of rapamycin; p65-NF-κB: nuclear factor kappa-light-chain-enhancer of activated B cells subunit p65; Th1: T helper 1; Th17: T helper 17; TNF-α: tumor necrosis factor-alpha.
In addition to the work done on Mgll, other research has shown that metformin can promote the phagocytosis of pathological Aβ and tau proteins by enhancing microglial autophagy capability. It reduces Aβ deposits and limits the spreading of tau pathology, which was injected in the hippocampus of APP/PS1 mice (Chen et al., 2021). Using streptozotocin-induced diabetic AD rats, other groups showed that metformin treatment improves learning and memory in streptozotocin-AD rats, associated with reduced astrogliosis, microgliosis, cytokine levels of IL1-β, TNF-α, and TGF-β in hippocampal tissues of rats with AD (Pilipenko et al., 2020; Saffari et al., 2020). Furthermore, metformin treatment can improve the cognitive function of aging mice via alleviation of microglial activation, enhancement of autophagy, and reduced gut inflammation to beneficially modulate Gut Microbiome/Goblet Cell/Mucin Axis (Ahmadi et al., 2020; Kodali et al., 2021).
Multiple sclerosis
MS is a progressive neuroinflammatory demyelinating disease caused by an immune system attack, mainly driven by adaptive T cells-mediated autoimmune insults. Using an EAE model, researchers have found that metformin can restrict the infiltration of mononuclear cells into the CNS, down-regulate the expression of proinflammatory cytokines (interferon-gamma, TNF-α, IL-6, interleukin-17 (IL-17), and inducible nitric oxide synthase), and restore lipid alterations (total phospholipids in free fatty acids) induced by EAE via AMPK activity (Figure 3; Nath et al., 2009). Using a cuprizone demyelinating mouse model, another research group showed that metformin treatment can attenuate proinflammatory microglia phenotypes by suppressing NF-κB activity (Abdi et al., 2021). In addition, metformin inhibits T cell-mediated immune responses including Ag-specific recall responses and production of Th1 or Th17 cytokines, while it raised Treg cells and anti-inflammatory cytokines and induced the generation of interleukin-10 (IL-10) in spleen cells of treated EAE animals (Nath et al., 2009; Paintlia et al., 2013a; Sun et al., 2016). The anti-inflammatory effects associated with metformin treatment are observed in patients with MS as well (Negrotto et al., 2016).
Parkinson’s disease
In PD pathophysiology, cytoplasmic aggregates of α-synuclein promote glial reactivity inflammatory cytokines such as TNF-α, IL-1β, and IL-6 (Mendonça et al., 2022b). In PD patients, the increased expression of inflammatory cytokines was positively correlated with the severity of depression and anxiety (Mendonça et al., 2022b). Thus, using a rotenone-induced PD model exhibiting both depression and motor deficits phenotypes, a research group showed that metformin treatment after PD model induction can prevent depressive-like behavior, improve motor impairments and increase TH+ cells via the induction of the autophagy process (Mendonça et al., 2022a, 2022b). Associated with this, metformin also reduced IBA-1+ microglia and GFAP+ reactive astrocytes, as well as proinflammatory factors NF-κB, IL-1β and inducible nitric oxide synthase levels in the hippocampus and prefrontal cortex (Wang et al., 2020a; Mendonça et al., 2022b). Another research group used the 6-OHDA-induced PD mouse model to reveal that metformin treatment effectively improves motor symptoms without effects on TH+ neurons. However, metformin treatment ameliorated astrocyte activation in the dopamine-depleted striatum (Ryu et al., 2020). Interestingly, when using lipopolysaccharide to induce an inflammatory rat PD model, researchers found that metformin has divergent effects: metformin can inhibit microglia activation and minimize the expression levels of pro- and anti-inflammatory cytokines, while it exacerbates the damage of dopaminergic neurons (Tayara et al., 2018).
Stroke
In stoke, metformin has been shown to have anti-inflammatory properties. Metformin reduces ROS formation following oxygen-glucose deprivation/reoxygenation injury in culture (Gabryel and Liber, 2018) and in Drosophila melanogaster following hypoxia (Kokott-Vuong et al., 2021). Furthermore, metformin administration pre- and post-stroke has been shown to elevate antioxidant defense molecules that reduce ROS, including SOD (Zeng et al., 2019; Fatemi et al., 2020), and glutathione peroxidase (Zeng et al., 2019), while other studies have previously found that metformin decreased levels of SOD, glutathione peroxidase, and catalase (Abd-Elsameea et al., 2014). Finally, metformin has been shown to lower stroke-induced lipid peroxides including malondialdehyde which contributes to cellular damage (Abd-Elsameea et al., 2014; Karimipour et al., 2018; Zeng et al., 2019). Furthermore, following neonatal stroke metformin has been shown to reduce microglial activation and enhance motor function (Bourget et al., 2022).
Metformin Has Biphasic Effects on Mitochondrial Respiration
The mitochondria are often referred to as the powerhouse of the cell as it is able to generate energy in the form of adenosine triphosphate. In the early 20th century, high concentrations of guanidine (the parent compound of metformin) were reported to inhibit mitochondrial respiration in dissected muscle (Meyerhof, 1921) and isolated mitochondria from the liver and kidney (Hollunger, 1955). However, lower concentrations of guanidine were also reported to activate mitochondrial respiration (Dickens, 1939). Together, this data suggests that guanidine has a biphasic effect on mitochondrial respiration, with low concentrations stimulating mitochondrial activity, while high concentrations suppress mitochondrial activity.
High concentrations of metformin suppress mitochondrial respiration
Early studies showed that very high concentrations of metformin (20 mM) significantly decreased mitochondrial oxygen uptake (Hollunger, 1955) and inhibited mitochondrial complex I activity (El-Mir et al., 2000), which was considered the principal molecular mechanism of metformin (Miller et al., 2013). However, the half maximal inhibitory concentration (IC50) of mitochondrial complex I by metformin is around 19–66 mM, indicating that metformin is a weak inhibitor of mitochondrial complex I (Bridges et al., 2014). A recent study using the supra-pharmacological concentration of metformin (1 mM) further demonstrated that this high concentration of metformin in culture can reduce mitochondrial oxygen consumption and increase the mitochondrial membrane potential without altering mitochondrial complex I activity. Instead, researchers found that treatment with supra-pharmacological concentrations of metformin can decrease adenosine diphosphate (ADP) levels by reduction of adenine synthesis and that the addition of exogenous adenosine diphosphate could restore inhibited mitochondrial oxygen consumption by the supra-pharmacological metformin concentrations (Wang et al., 2019). This high-concentration metformin (1 mM) has been shown to inhibit mitochondrial respiration in a variety of cell types including hepatocytes (Wang et al., 2019), intestinal cells (Yang et al., 2021), and cardiac cells (Emelyanova et al., 2021).
Low concentrations of metformin stimulate mitochondrial respiration
In contrast with supra-pharmacological concentrations of metformin treatment, pharmacological concentrations of metformin (50–100 μM) have been shown to stimulate mitochondrial respiration. This is important as patients with T2D have reduced mitochondrial numbers and decreased mitochondrial respiration in metabolic tissues. In the liver of mice, metformin significantly increases mitochondrial ETC complex I activity (Wang et al., 2019). Interestingly, reduced activity of the ETC complex had been observed in PD (Nicoletti et al., 2021) and AD brains (Mastroeni et al., 2017; Sorrentino et al., 2017). Pharmacological metformin concentrations (100 μM) also cause increased mitochondrial oxidative phosphorylation in the liver and primary hepatocytes (Alshawi and Agius, 2019), while some AD patients show downregulation of mitochondrial oxidative phosphorylation (Wang et al., 2009). In combination, these results suggest that metformin could alleviate PD/AD-impaired mitochondrial respiration.
In hepatocytes of the liver, metformin can promote mitochondrial fission via AMPK to eliminate compromised mitochondria through mitophagy (Wang et al., 2019). Similarly, in brown adipose tissue of mice, metformin is able to promote mitochondrial biogenesis by activating PGC-1α and AMPK expression (Geerling et al., 2014; Karise et al., 2019). Activated AMPK can drive mitochondrial fission to eliminate compromised mitochondria through mitophagy.
Utilizing metformin
As highlighted above repurposing metformin to treat neurologic diseases is an emerging area of research that has shown promise in recent studies. However, inter-person variability in the expression and function of the organic cation transporters family (OCTs) can greatly affect the efficacy of metformin in individuals with neurologic disorders. OCTs play a crucial role in the transport and uptake of metformin. Studies have found that responsiveness to metformin can highly vary among individuals due to OCT1 single nucleotide polymorphism (Kawoosa et al., 2022), and changes in OCT expression, modulated by weight (Moreno-Navarrete et al., 2011). In the brain, OCT1 is widely distributed in neurons (Koepsell et al., 2007). Therefore, variations in genetics or OCT1 expression may contribute to the efficacy of metformin treatment in neurological disorders. Thus, understanding the inter-person variability of OCTs is an important consideration when using metformin for the treatment of neurologic diseases.
Moreover, dosing is a critical factor that must be considered in order to maximize the effectiveness of metformin. In MS treatment, appropriate metformin dosing will be critical. In MS, some lesion sites are associated with impaired expression of mitochondrial ETC (Vogler et al., 2005; Witte et al., 2013) while other MS lesions exhibit enhanced mitochondrial complex activity (Witte et al., 2009). As mentioned previously, metformin has a biphasic effect on mitochondrial respiration. This suggests that metformin could benefit or worsen mitochondrial ETC activity in MS lesions dependent on dosing and MS lesion type. This highlights the importance of dosing to facilitate effective metformin treatment. However, there are other factors that must also be considered including disease progression and patient diversity.
Disease progression is important to consider in stroke recovery. AMPK activity is immediately increased right after ischemic injury. This contributes to injury-induced cell death (McCullough et al., 2005). Introducing metformin, an AMPK activator, at this stage could potentially worsen the effects of ischemic injury (Jia et al., 2015). However, stroke patients exhibiting reduced brain AMPK activity could benefit from metformin treatment due to its neurogenic properties (Jia et al., 2015).
Patient diversity is critical in AD. Metformin treatment has been shown to correct impaired adult neurogenesis and lower Aβ deposition via the aPKC-CBP pathway (Syal et al., 2020). However, other research shows that aPKC overactivity provokes increases in brain β-secretase and Aβ deposition. Interestingly, the second study was conducted in an insulin-resistant animal model, which suggests that hyperinsulinemia and aPKC activators contribute to AD progression (Sajan et al., 2018). In order to evaluate the effectiveness of metformin as a potential treatment, we must fully characterize mitochondrial dysfunction in neurologic disorders. This will inform decisions around personalized medicine and provide a comprehensive view of appropriate dosing in regard to disease progression, and patient diversity.
Biomarkers-Guided Metformin-Responsive Treatment in Neurological Diseases
Given that most neurological disorders have a complex etiology in their pathophysiology and are influenced by various risk factors such as aging, lifestyle, genetics, and environmental exposure, past clinical interventions directed at a “fit-for-all” therapy to treat neurodegenerative diseases seem to be less effective (Syal and Wang, 2021). More importantly, metformin, a Food and Drug Administration-approved anti-diabetic drug, has been extensively studied in one neurodegenerative disease, AD, and shows contradictory evidence in both animal and human AD subjects with regard to its therapeutic potential. As introduced previously, several retrospective clinical studies show that metformin treatment in diabetic patients or amnestic mild cognitive impairment patients without diabetes have slower cognitive decline and lower dementia risk (Bohlken et al., 2018; Shi et al., 2019; Tseng, 2019; Wium-Andersen et al., 2019; Sluggett et al., 2020; Zhou et al., 2020; Pomilio et al., 2022; Tang et al., 2022; Torrandell-Haro et al., 2022; Zheng et al., 2022). Two recent prospective clinical trials have found that both nondiabetic patients with mild dementia due to AD and diabetic patients when receiving metformin treatment, show improved executive functioning and learning/memory and indicate low dementia risk, respectively (Koenig et al., 2017; Samaras et al., 2020). Another group deployed a causal inference approach accounting for the competing risk of death in emulated clinical trials and showed that metformin use is associated with a lower hazard of all-cause mortality and a lower hazard of dementia onset, relative to sulfonylureas, another anti-diabetic drug (Charpignon et al., 2022). They further used a human neural cell culture system to identify that expression of genes associated with AD pathologies, such as SPP1 and APOE, were both uniquely and significantly reduced by exposure to metformin, relative to the vehicle and sulfonylureas (Charpignon et al., 2022). These results suggest that metformin’s anti-aging actions in the human brain act beyond its hypoglycemic actions. However, other work reported that metformin treatment can increase the risk of developing AD/dementia in patients associated with T2D (Imfeld et al., 2012; Moore et al., 2013; Kuan et al., 2017; Ha et al., 2021). Coincidently, metformin treatment in various animal AD models shows contradictory results. It efficiently prevents AD pathologies including amyloid plaque deposition and taupathy and blocks memory impairment in APP/PS1-AD mouse model (Kickstein et al., 2010; Ou et al., 2018; Lu et al., 2020; Xu et al., 2021), but metformin can also aggravate neurodegenerative processes, promotes tau aggregation, and exacerbates abnormal memory in other AD animal models, such as APOE–/–, P301S taupathy, and APP AD models (DiTacchio et al., 2015; Barini et al., 2016; Kuhla et al., 2019), while other animals models show no change in learning and memory at all following metformin treatment (Li et al., 2012). These positive (Additional Table 1 (149.5KB, pdf) ), moderate (Additional Table 2), and negative results (Additional Table 3) raise an important question in terms of how we can best use metformin to treat neurological degenerative diseases. In this regard, biomarker-directed targeted therapy has emerged in the field as novel personalized medicine. It is important to identify perturbed molecular functions in neurological degenerative diseases that can be targeted by metformin treatment. These perturbed molecules can then be used as biomarkers to stratify subpopulations of patients that will respond to metformin treatment, ultimately developing tailored/targeted therapy for neurological disorders.
Additional Table 2.
The moderate effect of metformin on neurological diseases in humans and in vivo
| Disease | Model | Treatment | Outcome | Specific outcome | Author | Year |
|---|---|---|---|---|---|---|
| AD | P301S-AD mouse model | 2 mg/mL for 4 months | Mixed | Reduces tau phosphorylation and exacerbated behavioural changes | Barini et al. | 2016 |
| AD | PDAPP (J9)-AD mouse model | 350 mg/kg/day for 10 months | Mixed | Increases memory dysfunction in males, protective in females | DiTacchio et al. | 2015 |
| AD | db/db mice | 200 mg/kg/day for 18 weeks. | Mixed | No effect on learning and memory and reduces total tau protein levels | Li et al | 2012 |
| AD | Streptozocin (STZ)-induced model | 10 mg/kg for 3 weeks | Mixed | Mixed effect on inflammatory and oxidative stress markers | Zeng et al. | 2021 |
| HD | R6/2-HD mouse model | 2 or 5 mg/mL for ~10 weeks | Mixed | Increased survival time in male mice only | Ma et al. | 2007 |
| PD | Lipopolysaccharide model | Pre-and post-lipopolysaccharide | Mixed | Anti-inflammatory but does not protect against cell death | Tayara et al. | 2018 |
| PD | Human | T2D+ | Mixed | Lower risk of PD at low-doses | Huang et al. | 2022 |
| PD | Rotenone model | Simultaneous administered rotenone | Mixed | Reduced neuron death but did not improve motor function | Ozbey et al. | 2020 |
| and metformin | ||||||
| Stroke | Hypoxia-ischemia (H-I) | Post H-I | Mixed | Promotes cognitive recovery and neural precursor cell pool expansion in females, but not males. | Ruddy et al. | 2019 |
| Stroke | Ischemia by bilateral common carotid artery occlusion | Pre-and post-and pre/post-stroke | Mixed | Pre-treatment and post-treatment decreased infarct size, but pre/post-treatment did not reduce infarct size | Karimipour et al. | 2018 |
| Stroke | Middle cerebral artery occlusion (MCAO) | Pre-MCAO | Mixed | Acute metformin exacerbated stroke damage while chronic metformin was neuroprotective | Li et al. | 2010 |
AD: Alzheimer’s disease; HD: Huntington’s disease; PD: Parkinson’s disease.
Additional Table 3.
The negative effect of metformin on neurological diseases in humans and in vivo
| Disease | Model | Treatment | Outcome | Specific outcome | Author | Year |
|---|---|---|---|---|---|---|
| AD, PD | Human | T2D+ | Impair | Higher risk of AD and PD | Kuan et al. | 2017 |
| AD | C57B6/J (B6) mice | 2 mg/mL for 7 days | Impair | Up-regulates APP | Picone et al. | 2015 |
| AD | Human | AD T2D+ | Impair | Impaired cognitive performance | Moore et al. | 2013 |
| AD | Human | T2D+ | Impair | Higher risk of AD | Ha et al. | 2021 |
| AD | Tg6799-AD mouse model | N/A | Impair | Caused autophagosome accumulation | Son et al. | 2016 |
| PD | MPTP model | During and post-MPTP | Impair | Increased neuron death | Ismaiel et al. | 2016 |
AD: Alzheimer’s disease; APP: amyloid precursor protein; MPTP: 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine; PD: Parkinson’s disease.
One example of a potential biomarker is Mgll. Aging-dependent induction of Mgll is observed in the 3×Tg-AD mouse model and post-mortem human AD hippocampal tissue. Our recent research work revealed that 3×Tg-AD mice exhibit an impaired aPKC-CBP pathway that leads to increased Mgll expression, associated with perturbed adult neuronal differentiation and spatial memory deficits (Syal et al., 2020). Importantly, metformin treatment in vivo in 3×Tg-AD mice corrects the impaired aPKC-CBP pathway to repress Mgll expression, significantly rescuing impaired adult neurogenesis, preventing spatial memory decline, and reducing Aβ accumulation. Contrary to our findings, other research work has shown that aPKC overactivity in the insulin-resistant animal model provokes increases in brain β-secretase, Aβ1–40/42, and p-Thr231 tau (Sajan et al., 2018). This suggests that excessive signaling via aPKC may link hyperinsulinemia and PKC-λ/ι activators to pathological and functional abnormalities in AD (Sajan et al., 2018). Insulin resistance has been well recognized to be a major risk factor for AD (Hölscher, 2020). Indeed, AD has been considered “type 3 diabetes”, and it is postulated that insulin action in the brain is impaired in insulin-resistant states (Barilar et al., 2020; Hölscher, 2020). Peripheral hyperinsulinemia can cause the levels and/or activities of the insulin receptor and/or post-receptor insulin signaling factors to be deficient in the brains of AD humans (Craft et al., 2012; de la Monte, 2012; de Felice, 2013). Thus, the deficient insulin signaling, named brain insulin resistance, has become a rationale for using intranasal insulin therapy to treat AD and mild cognitive impairment in clinical trials (Craft et al., 2012). However, overactivated aPKC signaling in hyperinsulinemia animal models raises questions that excess insulin signaling may promote the development of AD pathology over time by overactivated aPKC that is independent of Akt activity to provoke increases in brain β-secretase, Aβ1–40/42, and p-tau (Sajan et al., 2018; Farese et al., 2020). Interestingly, some AD human brain samples show elevated aPKC activity (Farese et al., 2020), while others show reduced aPKC expression/activity (Moore et al., 1998; Tan et al., 2010). All these studies point out that AD is associated with complex etiology in their pathophysiology, and it is important to identify biomarkers in AD that can be used to stratify subpopulations of patients for potential metformin-responsive treatment. It is plausible to predict that metformin may not be able to rescue memory decline Aβ accumulation in hyperinsulinemia-linked animal models where aPKC has been overactivated. Thus, we posit that Mgll would serve as a biomarker to identify potential metformin-responsive AD patients who may have low aPKC activity since Mgll expression is specifically repressed by metformin via activation of aPKC-CBP pathway (Syal et al., 2020). One potential clinical trial could be employed in the near future to examine Mgll mRNA levels in AD patients’ peripheral blood as a screening methodology to stratify subpopulations of AD patients for effective metformin treatment (Figure 4).
Figure 4.
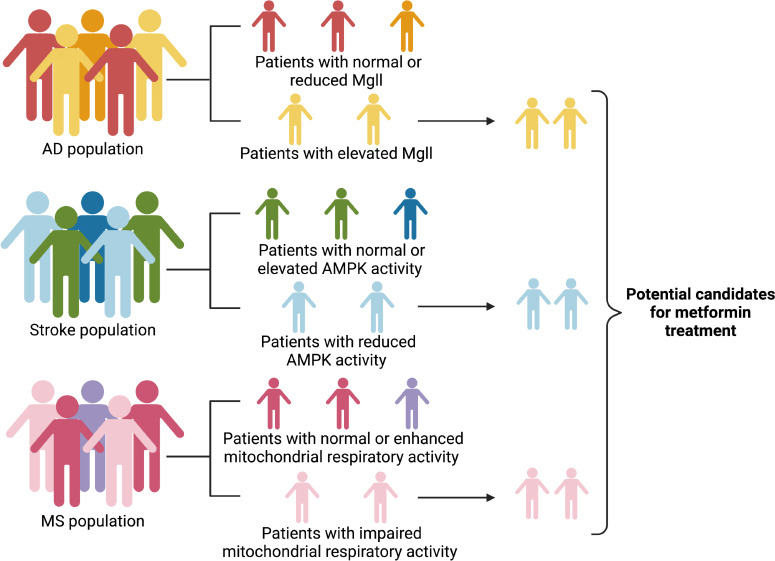
Personalized medicine: biomarkers-guided metformin-responsive treatment in neurological diseases.
Proposed biomarker screening methodology to stratify subpopulations of AD, stoke, and MS patients for metformin-responsive treatment. Subpopulations of interest would be individuals with elevated Mgll, reduced AMPK activity, and reduced mitochondrial respiration for AD, stroke, and MS patients, respectively. Created with BioRender.com. AD: Alzheimer’s disease; AMPK: AMP-activated protein kinase; Mgll: monoacylglycerol lipase; MS: multiple sclerosis.
Since mitochondria-related metabolic perturbations and impaired molecular pathways are involved in the pathogenesis of multiple neurological degenerative diseases and manifest differently at different stages of diseases, it is critical to precisely measure the perturbed mitochondria-related molecular pathways that would have a great potential to serve as biomarkers to guide metformin-effective treatment for targeted therapy at the specific stage of the disease. One example is AMPK activity status in relation to ischemic stroke conditions. AMPK activity is immediately increased right after ischemic injury to contribute to injury-induced cell death, while it is consistently reduced during the chronic phase of ischemic stroke (Castilla-Guerra et al., 2018). Metformin, an AMPK activator, would have much better therapeutic outcomes when given to stroke patients exhibiting reduced brain AMPK activity (Jia et al., 2015). Importantly, the AMPK-related autophagy pathway also plays a dynamic role during cerebral ischemic injury. Autophagy plays a detrimental effect during acute cerebral ischemic injury by accelerating cell death (Shi et al., 2021), while the protective role of autophagy during reperfusion accounts for mitophagy-related mitochondrial clearance and inhibition of downstream apoptosis (Shen et al., 2021). Thus, measuring brain AMPK activity following ischemic injury in stroke patients will be able to stratify the subpopulations of stroke patients that are suitable to receive metformin treatment when exhibiting reduced brain AMPK activity (Figure 4).
Another example relates to mitochondrial respiratory chain activity in MS lesion samples. Some MS lesion sites are associated with impaired expression of mitochondrial ETC subunits and increased oxidative damage/stress (Maldonado et al., 2022) while other MS lesions exhibit an enhanced density of mitochondria and upregulated mitochondrial complex IV activity (Witte et al., 2009). Since a recent study shows that a clinically relevant metformin dose increases liver mitochondrial density and respiratory activity along with improved hyperglycemia in high-fat- diet-fed mice (Wang et al., 2019), it is plausible to think that the former MS patients with impaired mitochondrial respiratory activity would have better therapeutic outcomes when receiving metformin treatment than the latter MS patients indicating enhanced mitochondrial density and respiratory activity (Figure 4).
Conclusion
Metabolic perturbations and impaired molecular pathways in these neurological degenerative diseases can serve as biomarkers to guide metformin-responsive treatment for targeted therapy to treat degenerative diseases. Future work will focus on how to translate the concept of personalized medicine from bench work to clinical settings for targeted therapy to precisely and effectively use metformin in treating neurological diseases.
Additional files:
Additional file 1: Open peer review report 1 (82.1KB, pdf) .
Additional Table 1 (149.5KB, pdf) : The positive effect of metformin on neurological diseases in humans and in vivo.
The positive effect of metformin on neurological diseases in humans and in vivo
Additional Table 2: The moderate effect of metformin on neurological diseases in humans and in vivo.
Additional Table 3: The negative effect of metformin on neurological diseases in humans and in vivo.
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
Data availability statement: All data relevant to the work are included in the article or uploaded as Additional files.
Open peer reviewer: Adriana Fernanda K Vizuete, Federal University of Rio Grande do Sul, Brazil.
P-Reviewer: Vizuete AFK; C-Editors: Zhao M, Liu WJ, Qiu Y; T-Editor: Jia Y
References
- 1.Abd-Elsameea AA, Moustaf AA, Mohamed AM. Modulation of the oxidative stress by metformin in the cerebrum of rats exposed to global cerebral ischemia and ischemia/reperfusion. Eur Rev Med Pharmacol Sci. (2014);18:2387–2392. [PubMed] [Google Scholar]
- 2.Abdi M, Pasbakhsh P, Shabani M, Nekoonam S, Sadeghi A, Fathi F, Abouzaripour M, Mohamed W, Zibara K, Kashani IR, Zendedel A. Metformin therapy attenuates pro-inflammatory microglia by inhibiting NF-κB in cuprizone demyelinating mouse model of multiple sclerosis. Neurotox Res. (2021);39:1732–1746. doi: 10.1007/s12640-021-00417-y. [DOI] [PubMed] [Google Scholar]
- 3.Adedeji HA, Ishola IO, Adeyemi OO. Novel action of metformin in the prevention of haloperidol-induced catalepsy in mice:potential in the treatment of Parkinson's disease? Prog Neuropsychopharmacol Biol Psychiatry. (2014);48:245–251. doi: 10.1016/j.pnpbp.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Ahmadi S, Razazan A, Nagpal R, Jain S, Wang B, Mishra SP, Wang S, Justice J, Ding J, McClain DA, Kritchevsky SB, Kitzman D, Yadav H. Metformin reduces aging-related leaky gut and improves cognitive function by beneficially modulating gut microbiome/goblet cell/mucin axis. J Gerontol A Biol Sci Med Sci. (2020);75:e9–21. doi: 10.1093/gerona/glaa056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alharbi MA, Al-Kafaji G, Khalaf N Ben, Messaoudi SA, Taha S, Daif A, Bakhiet M. Four novel mutations in the mitochondrial ND4 gene of complex I in patients with multiple sclerosis. Biomed Rep. (2019);11:257–268. doi: 10.3892/br.2019.1250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alshawi A, Agius L. Low metformin causes a more oxidized mitochondrial NADH/NAD redox state in hepatocytes and inhibits gluconeogenesis by a redox-independent mechanism. J Biol Chem. (2019);294:2839–2853. doi: 10.1074/jbc.RA118.006670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Angels Font M, Arboix A, Krupinski J. Angiogenesis, neurogenesis and neuroplasticity in ischemic stroke. Curr Cardiol Rev. (2010);6:238–244. doi: 10.2174/157340310791658802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arabmoazzen S, Mirshekar MA. Evaluation of the effects of metformin as adenosine monophosphate-activated protein kinase activator on spatial learning and memory in a rat model of multiple sclerosis disease. Biomed Pharmacother. (2021);141:111932. doi: 10.1016/j.biopha.2021.111932. [DOI] [PubMed] [Google Scholar]
- 9.Arawaka S, Sato H, Sasaki A, Koyama S, Kato T. Mechanisms underlying extensive Ser129-phosphorylation in α-synuclein aggregates. Acta Neuropathol Commun. (2017);5:48. doi: 10.1186/s40478-017-0452-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arnoux I, Willam M, Griesche N, Krummeich J, Watari H, Offermann N, Weber S, Dey PN, Chen C, Monteiro O, Buettner S, Meyer K, Bano D, Radyushkin K, Langston R, Lambert JJ, Wanker E, Methner A, Krauss S, Schweiger S, et al. Metformin reverses early cortical network dysfunction and behavior changes in Huntington's disease. Elife. (2018);7 doi: 10.7554/eLife.38744. doi:10.7554/eLife.3∨. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asadbegi M, Yaghmaei P, Salehi I, Ebrahim-Habibi A, Komaki A. Neuroprotective effects of metformin against Aβ-mediated inhibition of long-term potentiation in rats fed a high-fat diet. Brain Res Bull. (2016);121:178–185. doi: 10.1016/j.brainresbull.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 12.Ashabi G, Khodagholi F, Khalaj L, Goudarzvand M, Nasiri M. Activation of AMP-activated protein kinase by metformin protects against global cerebral ischemia in male rats:interference of AMPK/PGC-1αpathway. Metab Brain Dis. (2014);29:47–58. doi: 10.1007/s11011-013-9475-2. [DOI] [PubMed] [Google Scholar]
- 13.Ashabi G, Khalaj L, Khodagholi F, Goudarzvand M, Sarkaki A. Pre-treatment with metformin activates Nrf2 antioxidant pathways and inhibits inflammatory responses through induction of AMPK after transient global cerebral ischemia. Metab Brain Dis. (2015);30:747–754. doi: 10.1007/s11011-014-9632-2. [DOI] [PubMed] [Google Scholar]
- 14.Ashabi G, Sarkaki A, Khodagholi F, Shahamati SZ, Goudarzvand M, Farbood Y, Badavi M, Khalaj L. Subchronic metformin pretreatment enhances novel object recognition memory task in forebrain ischemia: behavioural, molecular, and electrophysiological studies. Can J Physiol Pharmacol. (2017);95:388–395. doi: 10.1139/cjpp-2016-0260. [DOI] [PubMed] [Google Scholar]
- 15.Ayoub R, Ruddy RM, Cox E, Oyefiade A, Derkach D, Laughlin S, Ades-aron B, Shirzadi Z, Fieremans E, MacIntosh BJ, de Medeiros CB, Skocic J, Bouffet E, Miller FD, Morshead CM, Mabbott DJ. Assessment of cognitive and neural recovery in survivors of pediatric brain tumors in a pilot clinical trial using metformin. Nat Med. (2020);26:1285–1294. doi: 10.1038/s41591-020-0985-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bakhashab S, Ahmed FW, Schulten HJ, Bashir A, Karim S, Al-Malki AL, Gari MA, Abuzenadah AM, Chaudhary AG, Alqahtani MH, Lary S, Ahmed F, Weaver JU. Metformin improves the angiogenic potential of human CD34+cells co-incident with downregulating CXCL10 and TIMP1 gene expression and increasing VEGFA under hyperglycemia and hypoxia within a therapeutic window for myocardial infarction. Cardiovasc Diabetol. (2016) doi: 10.1186/s12933-016-0344-2. doi:10.1186/S12933-016-0344-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bannister CA, Holden SE, Jenkins-Jones S, Morgan CL, Halcox JP, Schernthaner G, Mukherjee J, Currie CJ. Can people with type 2 diabetes live longer than those without?A comparison of mortality in people initiated with metformin or sulphonylurea monotherapy and matched, non-diabetic controls. Diabetes Obes Metab. (2014);16:1165–1173. doi: 10.1111/dom.12354. [DOI] [PubMed] [Google Scholar]
- 18.Barilar JO, Knezovic A, Perhoc AB, Homolak J, Riederer P, Salkovic-Petrisic M. Shared cerebral metabolic pathology in non-transgenic animal models of Alzheimer's and Parkinson's disease. J Neural Transm (Vienna) (2020);127:231–250. doi: 10.1007/s00702-020-02152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barini E, Antico O, Zhao Y, Asta F, Tucci V, Catelani T, Marotta R, Xu H, Gasparini L. Metformin promotes tau aggregation and exacerbates abnormal behavior in a mouse model of tauopathy. Mol Neurodegener. (2016) doi: 10.1186/s13024-016-0082-7. doi:10.1186/S13024-016-0082-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bayliss JA, Lemus MB, Santos V V., Deo M, Davies JS, Kemp BE, Elsworth JD, Andrews ZB. Metformin prevents nigrostriatal dopamine degeneration independent of AMPK activation in dopamine neurons. PLoS One. (2016) doi: 10.1371/journal.pone.0159381. doi:10.1371/JOURNAL. PONE.0159381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bohlken J, Jacob L, Kostev K. Association between the use of antihyperglycemic drugs and dementia risk:a case-control study. J Alzheimers Dis. (2018);66:725–732. doi: 10.3233/JAD-180808. [DOI] [PubMed] [Google Scholar]
- 22.Bourget C, Adams KV, Morshead CM. Reduced microglia activation following metformin administration or microglia ablation is sufficient to prevent functional deficits in a mouse model of neonatal stroke. J Neuroinflammation. (2022) doi: 10.1186/s12974-022-02487-x. doi:10.1186/S12974-022-02487-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bridges HR, Jones AJY, Pollak MN, Hirst J. Effects of metformin and other biguanides on oxidative phosphorylation in mitochondria. Biochem J. (2014);462:475. doi: 10.1042/BJ20140620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cabreiro F, Au C, Leung KY, Vergara-Irigaray N, Cochemé HM, Noori T, Weinkove D, Schuster E, Greene NDE, Gems D. Metformin retards aging in C. elegans by altering microbial folate and methionine metabolism. Cell. (2013);153:228–239. doi: 10.1016/j.cell.2013.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Calvo-Rodriguez M, Bacskai BJ. Mitochondria and calcium in Alzheimer's disease:from cell signaling to neuronal cell death. Trends Neurosci. (2021);44:136–151. doi: 10.1016/j.tins.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 26.Cao Y, Liu C, Li G, Gao W, Tang H, Fan S, Tang X, Zhao L, Wang H, Peng A, You C, Tong A, Zhou L. Metformin alleviates delayed hydrocephalus after intraventricular hemorrhage by inhibiting inflammation and fibrosis. Transl Stroke Res. (2022) doi: 10.1007/s12975-022-01026-3. doi:10.1007/s12975-022-01026-3. [DOI] [PubMed] [Google Scholar]
- 27.Castilla-Guerra L, Fernandez-Moreno M del C, Leon-Jimenez D, Carmona-Nimo E. Antidiabetic drugs and stroke risk. Current evidence. Eur J Intern Med. (2018);48:1–5. doi: 10.1016/j.ejim.2017.09.019. [DOI] [PubMed] [Google Scholar]
- 28.Cavalcante GC, Brito LM, Schaan AP, Ribeiro-Dos-santos Â, de Araújo GS. Mitochondrial genetics reinforces multiple layers of interaction in Alzheimer disease. Biomedicines. (2022);10:880. doi: 10.3390/biomedicines10040880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chakravorty A, Jetto CT, Manjithaya R. Dysfunctional mitochondria and mitophagy as drivers of Alzheimer's disease pathogenesis. Front Aging Neurosci. (2019) doi: 10.3389/fnagi.2019.00311. doi:10.3389/FNAGI.2019.00311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chanthammachat P, Dharmasaroja P. Metformin restores the mitochondrial membrane potentials in association with a reduction in TIMM23 and NDUFS3 in MPP+-induced neurotoxicity in SH-SY5Y cells. EXCLI J. (2019);18:812–823. doi: 10.17179/excli2019-1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Charpignon ML, Vakulenko-Lagun B, Zheng B, Magdamo C, Su B, Evans K, Rodriguez S, Sokolov A, Boswell S, Sheu YH, Somai M, Middleton L, Hyman BT, Betensky RA, Finkelstein SN, Welsch RE, Tzoulaki I, Blacker D, Das S, Albers MW. Causal inference in medical records and complementary systems pharmacology for metformin drug repurposing towards dementia. Nat Commun. (2022);13:7652. doi: 10.1038/s41467-022-35157-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen B, Teng Y, Zhang X, Lv X, Yin Y. Metformin alleviated Aβ-induced apoptosis via the suppression of JNK MAPK signaling pathway in cultured hippocampal neurons. Biomed Res Int. (2016);2016:1421430. doi: 10.1155/2016/1421430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Y, Zhou K, Wang R, Liu Y, Kwak YD, Ma T, Thompson RC, Zhao Y, Smith L, Gasparini L, Luo Z, Xu H, Liao FF. Antidiabetic drug metformin (GlucophageR) increases biogenesis of Alzheimer's amyloid peptides via up-regulating BACE1 transcription. Proc Natl Acad Sci U S A. (2009);106:3907–3912. doi: 10.1073/pnas.0807991106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen Y, Zhao S, Fan Z, Li Z, Zhu Y, Shen T, Li K, Yan Y, Tian J, Liu Z, Zhang B. Metformin attenuates plaque-associated tau pathology and reduces amyloid-βburden in APP/PS1 mice. Alzheimers Res Ther. (2021);13:40. doi: 10.1186/s13195-020-00761-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cherubini M, Lopez-Molina L, Gines S. Mitochondrial fission in Huntington's disease mouse striatum disrupts ER-mitochondria contacts leading to disturbances in Ca2+ efflux and reactive oxygen species (ROS) homeostasis. Neurobiol Dis. (2020);136:104741. doi: 10.1016/j.nbd.2020.104741. [DOI] [PubMed] [Google Scholar]
- 36.Chiang MC, Cheng YC, Chen SJ, Yen CH, Huang RN. Metformin activation of AMPK-dependent pathways is neuroprotective in human neural stem cells against amyloid-beta-induced mitochondrial dysfunction. Exp Cell Res. (2016);347:322–331. doi: 10.1016/j.yexcr.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 37.Craft S, Baker LD, Montine TJ, Minoshima S, Watson GS, Claxton A, Arbuckle M, Callaghan M, Tsai E, Plymate SR, Green PS, Leverenz J, Cross D, Gerton B. Intranasal insulin therapy for Alzheimer disease and amnestic mild cognitive impairment:a pilot clinical trial. Arch Neurol. (2012);69:29–38. doi: 10.1001/archneurol.2011.233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dadwal P, Mahmud N, Sinai L, Azimi A, Fatt M, Wondisford FE, Miller FD, Morshead CM. Activating endogenous neural precursor cells using metformin leads to neural repair and functional recovery in a model of childhood brain injury. Stem Cell Rep. (2015);5:166–173. doi: 10.1016/j.stemcr.2015.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.de Felice FG. Alzheimer's disease and insulin resistance:translating basic science into clinical applications. J Clin Invest. (2013);123:531–539. doi: 10.1172/JCI64595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de la Monte SM. Brain insulin resistance and deficiency as therapeutic targets in Alzheimer's disease. Curr Alzheimer Res. (2012);9:35. doi: 10.2174/156720512799015037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deng T, Zheng YR, Hou WW, Yuan Y, Shen Z, Wu XL, Chen Y, Zhang LS, Hu WW, Chen Z, Zhang XN. Pre-stroke metformin treatment is neuroprotective involving AMPK reduction. Neurochem Res. (2016);41:2719–2727. doi: 10.1007/s11064-016-1988-8. [DOI] [PubMed] [Google Scholar]
- 42.Derkach D, Kehtari T, Renaud M, Heidari M, Lakshman N, Morshead CM. Metformin pretreatment rescues olfactory memory associated with subependymal zone neurogenesis in a juvenile model of cranial irradiation. Cell Rep Med. (2021);2:100231. doi: 10.1016/j.xcrm.2021.100231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dickens F. The metabolism of normal and tumour tissue:the action of guanidines and amidines on the Pasteur effect. Biochem J. (1939);33:2017. doi: 10.1042/bj0332017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DiTacchio KA, Heinemann SF, Dziewczapolski G. Metformin treatment alters memory function in a mouse model of Alzheimer's disease. J Alzheimers Dis. (2015);44:43–48. doi: 10.3233/JAD-141332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dulovic M, Jovanovic M, Xilouri M, Stefanis L, Harhaji-Trajkovic L, Kravic-Stevovic T, Paunovic V, Ardah MT, El-Agnaf OMA, Kostic V, Markovic I, Trajkovic V. The protective role of AMP-activated protein kinase in alpha-synuclein neurotoxicity in vitro. Neurobiol Dis. (2014);63:1–11. doi: 10.1016/j.nbd.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 46.Elabi O, Gaceb A, Carlsson R, Padel T, Soylu-Kucharz R, Cortijo I, Li W, Li JY, Paul G. Human α-synuclein overexpression in a mouse model of Parkinson's disease leads to vascular pathology, blood brain barrier leakage and pericyte activation. Sci Rep. (2021);11:1120. doi: 10.1038/s41598-020-80889-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.El-Ghaiesh SH, Bahr HI, Ibrahiem AT, Ghorab D, Alomar SY, Farag NE, Zaitone SA. Metformin protects from rotenone-induced nigrostriatal neuronal death in adult mice by activating AMPK-FOXO3 signaling and mitigation of angiogenesis. Front Mol Neurosci. (2020);13:84. doi: 10.3389/fnmol.2020.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.El-Mir MY, Nogueira V, Fontaine E, Avéret N, Rigoulet M, Leverve X. Dimethylbiguanide inhibits cell respiration via an indirect effect targeted on the respiratory chain complex I. J Biol Chem. (2000);275:223–228. doi: 10.1074/jbc.275.1.223. [DOI] [PubMed] [Google Scholar]
- 49.Emelyanova L, Bai X, Yan Y, Bosnjak ZJ, Kress D, Warner C, Kroboth S, Rudic T, Kaushik S, Stoeckl E, Ross GR, Rizvi F, Tajik AJ, Jahangir A. Biphasic effect of metformin on human cardiac energetics. Transl Res. (2021);229:5–23. doi: 10.1016/j.trsl.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Esmaeilnejad S, Semnanian S, Javan M. Metformin protects myelin from degeneration in a mouse model of iysophosphatidylcholine-induced demyelination in the optic chiasm. Cell J. (2021);23:119–128. doi: 10.22074/cellj.2021.7174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fang EF, Hou Y, Palikaras K, Adriaanse BA, Kerr JS, Yang B, Lautrup S, Hasan-Olive MM, Caponio D, Dan X, Rocktäschel P, Croteau DL, Akbari M, Greig NH, Fladby T, Nilsen H, Cader MZ, Mattson MP, Tavernarakis N, Bohr VA. Mitophagy inhibits amyloid-βand tau pathology and reverses cognitive deficits in models of Alzheimer's disease. Nat Neurosci. (2019);22:401–412. doi: 10.1038/s41593-018-0332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fang M, Jiang H, Ye L, Cai C, Hu Y, Pan S, Li P, Xiao J, Lin Z. Metformin treatment after the hypoxia-ischemia attenuates brain injury in newborn rats. Oncotarget. (2017);8:75308–75325. doi: 10.18632/oncotarget.20779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Farbood Y, Sarkaki A, Khalaj L, Khodagholi F, Badavi M, Ashabi G. Targeting adenosine monophosphate-activated protein kinase by metformin adjusts post-ischemic hyperemia and extracellular neuronal discharge in transient global cerebral ischemia. Microcirculation. (2015);22:534–541. doi: 10.1111/micc.12224. [DOI] [PubMed] [Google Scholar]
- 54.Farese RV, Kindy MA, Sajan MP. Atypical protein kinase C hyperactivity in insulin-resistant and insulin-sensitive forms of Alzheimer's disease:a potential therapeutic target. In:Alzheimer's disease:drug discovery [Internet] In: Huang X, editor. Brisbane (AU): Exon Publications; (2020). Chapter 6. [PubMed] [Google Scholar]
- 55.Farr SA, Roesler E, Niehoff ML, Roby DA, McKee A, Morley JE. Metformin improves learning and memory in the SAMP8 mouse model of Alzheimer's disease. J Alzheimers Dis. (2019);68:1699–1710. doi: 10.3233/JAD-181240. [DOI] [PubMed] [Google Scholar]
- 56.Fatemi I, Saeed-Askari P, Hakimizadeh E, Kaeidi A, Esmaeil-Moghaddam S, Pak-Hashemi M, Allahtavakoli M. Long-term metformin therapy improves neurobehavioral functions and antioxidative activity after cerebral ischemia/reperfusion injury in rats. Brain Res Bull. (2020);163:65–71. doi: 10.1016/j.brainresbull.2020.07.015. [DOI] [PubMed] [Google Scholar]
- 57.Fatt M, Hsu K, He L, Wondisford F, Miller FD, Kaplan DR, Wang J. Metformin acts on two different molecular pathways to enhance adult neural precursor proliferation/self-renewal and differentiation. Stem Cell Rep. (2015);5:988–995. doi: 10.1016/j.stemcr.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fitzgerald JC, Zimprich A, Berrio DAC, Schindler KM, Maurer B, Schulte C, Bus C, Hauser AK, Kübler M, Lewin R, Bobbili DR, Schwarz LM, Vartholomaiou E, Brockmann K, Wüst R, Madlung J, Nordheim A, Riess O, Martins LM, Glaab E, et al. Metformin reverses TRAP1 mutation-associated alterations in mitochondrial function in Parkinson's disease. Brain. (2017);140:2444–2459. doi: 10.1093/brain/awx202. [DOI] [PubMed] [Google Scholar]
- 59.Gabryel B, Liber S. Metformin limits apoptosis in primary rat cortical astrocytes subjected to oxygen and glucose deprivation. Folia Neuropathol. (2018);56:328–336. doi: 10.5114/fn.2018.80866. [DOI] [PubMed] [Google Scholar]
- 60.Gautier CA, Kitada T, Shen J. Loss of PINK1 causes mitochondrial functional defects and increased sensitivity to oxidative stress. Proc Natl Acad Sci U S A. (2008);105:11364–11369. doi: 10.1073/pnas.0802076105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ge XH, Zhu GJ, Geng DQ, Zhang HZ, He JM, Guo AZ, Ma LL, Yu DH. Metformin protects the brain against ischemia/reperfusion injury through PI3K/Akt1/JNK3 signaling pathways in rats. Physiol Behav. (2017);170:115–123. doi: 10.1016/j.physbeh.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 62.Geerling JJ, Boon MR, van der Zon GC, van den Berg SAA, van den Hoek AM, Lombès M, Princen HMG, Havekes LM, Rensen PCN, Guigas B. Metformin lowers plasma triglycerides by promoting VLDL-triglyceride clearance by brown adipose tissue in mice. Diabetes. (2014);63:880–891. doi: 10.2337/db13-0194. [DOI] [PubMed] [Google Scholar]
- 63.Geranmayeh MH, Rahbarghazi R, Saeedi N, Farhoudi M. Metformin-dependent variation of microglia phenotype dictates pericytes maturation under oxygen-glucose deprivation. Tissue Barriers. (2022);10:2018928. doi: 10.1080/21688370.2021.2018928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ghadernezhad N, Khalaj L, Pazoki-Toroudi H, Mirmasoumi M, Ashabi G. Metformin pretreatment enhanced learning and memory in cerebral forebrain ischaemia:the role of the AMPK/BDNF/P70SK signalling pathway. Pharm Biol. (2016);54:2211–2219. doi: 10.3109/13880209.2016.1150306. [DOI] [PubMed] [Google Scholar]
- 65.Gómez-Escribano AP, Bono-Yagüe J, García-Gimeno MA, Sequedo MD, Hervás D, Fornés-Ferrer V, Torres-Sánchez SC, Millán JM, Sanz P, Vázquez-Manrique RP. Synergistic activation of AMPK prevents from polyglutamine-induced toxicity in Caenorhabditis elegans. Pharmacol Res. (2020);161:105105. doi: 10.1016/j.phrs.2020.105105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo JM, Zhang L, Niu XC, Shu H, Wang L, Su DF, Zhang Y, Liu AJ, Zhu DQ, Xu JJ. Involvement of arterial baroreflex and nicotinic acetylcholine receptor α7 subunit pathway in the protection of metformin against stroke in stroke-prone spontaneously hypertensive rats. Eur J Pharmacol. (2017);798:1–8. doi: 10.1016/j.ejphar.2017.01.035. [DOI] [PubMed] [Google Scholar]
- 67.Ha J, Choi DW, Kim KJ, Cho SY, Kim H, Kim KY, Koh Y, Nam CM, Kim E. Association of metformin use with Alzheimer's disease in patients with newly diagnosed type 2 diabetes:a population-based nested case-control study. Sci Rep. (2021);11:24069. doi: 10.1038/s41598-021-03406-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Han J, Li Y, Liu X, Zhou T, Sun H, Edwards P, Gao H, Yu FS, Qiao X. Metformin suppresses retinal angiogenesis and inflammation in vitro and in vivo. PLoS One. (2018);13:e0193031. doi: 10.1371/journal.pone.0193031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hang L, Thundyil J, Goh GWY, Lim KL. AMP kinase activation is selectively disrupted in the ventral midbrain of mice deficient in Parkin or PINK1 expression. Neuromolecular Med. (2019);21:25–32. doi: 10.1007/s12017-018-8517-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.He L, Wondisford FE. Metformin action:concentrations matter. Cell Metab. (2015);21:159–162. doi: 10.1016/j.cmet.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 71.He Z, Ning N, Zhou Q, Khoshnam SE, Farzaneh M. Mitochondria as a therapeutic target for ischemic stroke. Free Radic Biol Med. (2020);146:45–58. doi: 10.1016/j.freeradbiomed.2019.11.005. [DOI] [PubMed] [Google Scholar]
- 72.Hervás D, Fornés-Ferrer V, Gómez-Escribano AP, Sequedo MD, Peiró C, Millán JM, Vázquez-Manrique RP. Metformin intake associates with better cognitive function in patients with Huntington's disease. PLoS One. (2017);12:e0179283. doi: 10.1371/journal.pone.0179283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hettich MM, Matthes F, Ryan DP, Griesche N, Schröder S, Dorn S, Krauß S, Ehninger D. The anti-diabetic drug metformin reduces BACE1 protein level by interfering with the MID1 complex. PLoS One. (2014);9:e102420. doi: 10.1371/journal.pone.0102420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hollander MC, Latour LL, Yang D, Ishii H, Xiao Z, Min Y, Ray-Choudhury A, Munasinghe J, Merchant AS, Lin PC, Hallenbeck J, Boehm M, Yang L. Attenuation of myeloid-specific TGFβsignaling induces inflammatory cerebrovascular disease and stroke. Circ Res. (2017);121:1360–1369. doi: 10.1161/CIRCRESAHA.116.310349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hollunger G. Guanidines and oxidative phosphorylations. Acta Pharmacol Toxicol (Copenh) (1955);11:1–84. doi: 10.1111/j.1600-0773.1955.tb02972.x. [DOI] [PubMed] [Google Scholar]
- 76.Hölscher C. Brain insulin resistance:role in neurodegenerative disease and potential for targeting. Expert Opin Investig Drugs. (2020);29:333–348. doi: 10.1080/13543784.2020.1738383. [DOI] [PubMed] [Google Scholar]
- 77.Horsdal HT, Mehnert F, Rungby J, Johnsen SP. Type of preadmission antidiabetic treatment and outcome among patients with ischemic stroke:a nationwide follow-up study. J Stroke Cerebrovasc Dis. (2012);21:717–725. doi: 10.1016/j.jstrokecerebrovasdis.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 78.Houshmand F, Barati M, Golab F, Ramezani-sefidar S, Tanbakooie S, Tabatabaei M, Amiri M, Sanadgol N. Metformin-induced AMPK activation stimulates remyelination through induction of neurotrophic factors, downregulation of NogoA and recruitment of Olig2+precursor cells in the cuprizone murine model of multiple sclerosis. Daru. (2019);27:583–592. doi: 10.1007/s40199-019-00286-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Huang KH, Chang YL, Gau SY, Tsai TH, Lee CY. Dose–response association of metformin with Parkinson's disease odds in type 2 diabetes mellitus. Pharmaceutics. (2022);14:946. doi: 10.3390/pharmaceutics14050946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hussein AM, Eldosoky M, El-Shafey M, El-Mesery M, Ali AN, Abbas KM, Abulseoud OA. Effects of metformin on apoptosis and α-synuclein in a rat model of pentylenetetrazole-induced epilepsy. Can J Physiol Pharmacol. (2019);97:37–46. doi: 10.1139/cjpp-2018-0266. [DOI] [PubMed] [Google Scholar]
- 81.Imfeld P, Bodmer M, Jick SS, Meier CR. Metformin, other antidiabetic drugs, and risk of Alzheimer's disease:a population-based case-control study. J Am Geriatr Soc. (2012);60:916–921. doi: 10.1111/j.1532-5415.2012.03916.x. [DOI] [PubMed] [Google Scholar]
- 82.Intihar TA, Martinez EA, Gomez-Pastor R. Mitochondrial dysfunction in Huntington's disease;interplay between HSF1, p53 and PGC-1αtranscription factors. Front Cell Neurosci. (2019);13:1–10. doi: 10.3389/fncel.2019.00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycemia in type 2 diabetes:a patient-centered approach:position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. (2012);35:1364–1379. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ismaiel AAK, Espinosa-Oliva AM, Santiago M, García-Quintanilla A, Oliva-Martín MJ, Herrera AJ, Venero JL, de Pablos RM. Metformin, besides exhibiting strong in vivo anti-inflammatory properties, increases mptp-induced damage to the nigrostriatal dopaminergic system. Toxicol Appl Pharmacol. (2016);298:19–30. doi: 10.1016/j.taap.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 85.Jankeviciute S, Svirskiene N, Svirskis G, Borutaite V. Effects of metformin on spontaneous Ca2+ signals in cultured microglia cells under normoxic and hypoxic conditions. Int J Mol Sci. (2021);22:9493. doi: 10.3390/ijms22179493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jędrak P, Mozolewski P, Węgrzyn G, Więckowski MR. Mitochondrial alterations accompanied by oxidative stress conditions in skin fibroblasts of Huntington's disease patients. Metab Brain Dis. (2018);33:2005–2017. doi: 10.1007/s11011-018-0308-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Jia J, Cheng J, Ni J, Zhen X. Neuropharmacological actions of metformin in stroke. Curr Neuropharmacol. (2015);13:389. doi: 10.2174/1570159X13666150205143555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jiang T, Yu JT, Zhu XC, Wang HF, Tan MS, Cao L, Zhang QQ, Gao L, Shi JQ, Zhang YD, Tan L. Acute metformin preconditioning confers neuroprotection against focal cerebral ischaemia by pre-activation of AMPK-dependent autophagy. Br J Pharmacol. (2014);171:3146–3157. doi: 10.1111/bph.12655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Jin J, Gu H, Anders NM, Ren T, Jiang M, Tao M, Peng Q, Rudek MA, Duan W. Metformin protects cells from mutant Huntingtin toxicity through activation of AMPK and modulation of mitochondrial dynamics. Neuromolecular Med. (2016);18:581–592. doi: 10.1007/s12017-016-8412-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Jin Q, Cheng J, Liu Y, Wu J, Wang X, Wei S, Zhou X, Qin Z, Jia J, Zhen X. Improvement of functional recovery by chronic metformin treatment is associated with enhanced alternative activation of microglia/macrophages and increased angiogenesis and neurogenesis following experimental stroke. Brain Behav Immun. (2014);40:131–142. doi: 10.1016/j.bbi.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 91.Kang H, Khang R, Ham S, Jeong GR, Kim H, Jo M, Lee BD, Lee YI, Jo A, Park C, Kim H, Seo J, Paek SH, Lee YS, Choi JY, Lee Y, Shin JH. Activation of the ATF2/CREB-PGC-1αpathway by metformin leads to dopaminergic neuroprotection. Oncotarget. (2017);8:48603–48618. doi: 10.18632/oncotarget.18122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Karimipour M, Shojaei Zarghani S, Mohajer Milani M, Soraya H. Pre-treatment with metformin in comparison with post-treatment reduces cerebral ischemia reperfusion induced injuries in rats. Bull Emerg Trauma. (2018);6:115–121. doi: 10.29252/beat-060205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Karise I, Bargut TC, del Sol M, Aguila MB, Mandarim-de-Lacerda CA. Metformin enhances mitochondrial biogenesis and thermogenesis in brown adipocytes of mice. Biomed Pharmacother. (2019);111:1156–1165. doi: 10.1016/j.biopha.2019.01.021. [DOI] [PubMed] [Google Scholar]
- 94.Katila N, Bhurtel S, Shadfar S, Srivastav S, Neupane S, Ojha U, Jeong GS, Choi DY. Metformin lowers α-synuclein phosphorylation and upregulates neurotrophic factor in the MPTP mouse model of Parkinson's disease. Neuropharmacology. (2017);125:396–407. doi: 10.1016/j.neuropharm.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 95.Kawoosa F, Shah ZA, Masoodi SR, Amin A, Rasool R, Fazili KM, Dar AH, Lone A, ul Bashir S. Role of human organic cation transporter-1 (OCT-1/SLC22A1) in modulating the response to metformin in patients with type 2 diabetes. BMC Endocr Disord. (2022);22:140. doi: 10.1186/s12902-022-01033-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kazkayasi I, Telli G, Nemutlu E, Uma S. Intranasal metformin treatment ameliorates cognitive functions via insulin signaling pathway in ICV-STZ-induced mice model of Alzheimer's disease. Life Sci. (2022);299:120538. doi: 10.1016/j.lfs.2022.120538. [DOI] [PubMed] [Google Scholar]
- 97.Kersten CJBA, Knottnerus ILH, Heijmans E, Haalboom M, Zandbergen AAM, den Hertog HM. Effect of metformin on outcome after acute ischemic stroke in patients with type 2 diabetes mellitus. J Stroke Cerebrovasc Dis. (2022);31:106648. doi: 10.1016/j.jstrokecerebrovasdis.2022.106648. [DOI] [PubMed] [Google Scholar]
- 98.Kickstein E, Krauss S, Thornhill P, Rutschow D, Zeller R, Sharkey J, Williamson R, Fuchs M, Köhler A, Glossmann H, Schneider R, Sutherland C, Schweiger S. Biguanide metformin acts on tau phosphorylation via mTOR/protein phosphatase 2A (PP2A) signaling. Proc Natl Acad Sci U S A. (2010);107:21830–21835. doi: 10.1073/pnas.0912793107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kodali M, Attaluri S, Madhu LN, Shuai B, Upadhya R, Gonzalez JJ, Rao X, Shetty AK. Metformin treatment in late middle age improves cognitive function with alleviation of microglial activation and enhancement of autophagy in the hippocampus. Aging Cell. (2021);20:e13277. doi: 10.1111/acel.13277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Koenig AM, Mechanic-Hamilton D, Xie SX, Combs MF, Cappola AR, Xie L, Detre JA, Wolk DA, Arnold SE. Effects of the insulin sensitizer metformin in Alzheimer disease:pilot data from a randomized placebo-controlled crossover study. Alzheimer Dis Assoc Disord. (2017);31:107–113. doi: 10.1097/WAD.0000000000000202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Koepsell H, Lips K, Volk C. Polyspecific organic cation transporters:structure, function, physiological roles, and biopharmaceutical implications. Pharm Res. (2007);24:1227–1251. doi: 10.1007/s11095-007-9254-z. [DOI] [PubMed] [Google Scholar]
- 102.Kokott-Vuong A, Jung J, Fehr AT, Kirschfink N, Noristani R, Voigt A, Reich A, Schulz JB, Huber M, Habib P. Increased post-hypoxic oxidative stress and activation of the PERK branch of the UPR in Trap1-deficient drosophila melanogaster is abrogated by metformin. Int J Mol Sci. (2021);22:11586. doi: 10.3390/ijms222111586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kosaraju J, Seegobin M, Gouveia A, Syal C, Sarma SN, Lu KJ, Ilin J, He L, Wondisford FE, Lagace D, De Repentigny Y, Kothary R, Wang J. Metformin promotes CNS remyelination and improves social interaction following focal demyelination through CBP Ser436 phosphorylation. Exp Neurol. (2020);334:113454. doi: 10.1016/j.expneurol.2020.113454. [DOI] [PubMed] [Google Scholar]
- 104.Kuan YC, Huang KW, Lin CL, Hu CJ, Kao CH. Effects of metformin exposure on neurodegenerative diseases in elderly patients with type 2 diabetes mellitus. Prog Neuropsychopharmacol Biol Psychiatry. (2017);79:77–83. doi: 10.1016/j.pnpbp.2017.06.002. [DOI] [PubMed] [Google Scholar]
- 105.Kuhla A, Brichmann E, Rühlmann C, Thiele R, Meuth L, Vollmar B. Metformin therapy aggravates neurodegenerative processes in ApoE-/- mice. J Alzheimers Dis. (2019);68:1415–1427. doi: 10.3233/JAD-181017. [DOI] [PubMed] [Google Scholar]
- 106.Kumar H, Chakrabarti A, Sarma P, Modi M, Banerjee D, Radotra BD, Bhatia A, Medhi B. Novel therapeutic mechanism of action of metformin and its nanoformulation in Alzheimer's disease and role of AKT/ERK/GSK pathway. Eur J Pharm Sci. (2023);181:106348. doi: 10.1016/j.ejps.2022.106348. [DOI] [PubMed] [Google Scholar]
- 107.Łabuzek K, Suchy D, Gabryel B, Bielecka A, Liber S, Okopień B. Quantification of metformin by the HPLC method in brain regions, cerebrospinal fluid and plasma of rats treated with lipopolysaccharide. Pharmacol Rep. (2010);62:956–965. doi: 10.1016/s1734-1140(10)70357-1. [DOI] [PubMed] [Google Scholar]
- 108.Largani SHH, Borhani-Haghighi M, Pasbakhsh P, Mahabadi VP, Nekoonam S, Shiri E, Kashani IR, Zendehdel A. Oligoprotective effect of metformin through the AMPK-dependent on restoration of mitochondrial hemostasis in the cuprizone-induced multiple sclerosis model. J Mol Histol. (2019);50:263–271. doi: 10.1007/s10735-019-09824-0. [DOI] [PubMed] [Google Scholar]
- 109.Larsen SB, Hanss Z, Krüger R. The genetic architecture of mitochondrial dysfunction in Parkinson's disease. Cell Tissue Res. (2018);373:21–37. doi: 10.1007/s00441-017-2768-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lee H, Fenster RJ, Pineda SS, Gibbs WS, Mohammadi S, Davila-Velderrain J, Garcia FJ, Therrien M, Novis HS, Gao F, Wilkinson H, Vogt T, Kellis M, LaVoie MJ, Heiman M. Cell type-specific transcriptomics reveals that mutant Huntingtin leads to mitochondrial RNA release and neuronal innate immune activation. Neuron. (2020);107:891–908. doi: 10.1016/j.neuron.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Li J, Benashski SE, Venna VR, McCullough LD. Effects of metformin in experimental stroke. Stroke. (2010);41:2645–2652. doi: 10.1161/STROKEAHA.110.589697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li J, Deng J, Sheng W, Zuo Z. Metformin attenuates Alzheimer's disease-like neuropathology in obese, leptin-resistant mice. Pharmacol Biochem Behav. (2012);101:564–574. doi: 10.1016/j.pbb.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Li LX, Liu MY, Jiang X, Xia ZH, Wang YX, An D, Wang HG, Heng B, Liu YQ. Metformin inhibits Aβ25-35 -induced apoptotic cell death in SH-SY5Y cells. Basic Clin Pharmacol Toxicol. (2019);125:439–449. doi: 10.1111/bcpt.13279. [DOI] [PubMed] [Google Scholar]
- 114.Liu C, Zhang D, Lu Z, Man J, Zhang Z, Fu X, Cui K, Wang J. Metformin protects against pericyte apoptosis and promotes neurogenesis through suppressing JNK p38 MAPK signalling activation in ischemia/reperfusion injury. Neurosci Lett. (2022a);783:136708. doi: 10.1016/j.neulet.2022.136708. [DOI] [PubMed] [Google Scholar]
- 115.Liu F, Lu J, Manaenko A, Tang J, Hu Q. Mitochondria in ischemic stroke:new insight and implications. Aging Dis. (2018);9:924. doi: 10.14336/AD.2017.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Liu K, Li L, Liu Z, Li G, Wu Y, Jiang X, Wang M, Chang Y, Jiang T, Luo J, Zhu J, Li H, Wang Y. Acute administration of metformin protects against neuronal apoptosis induced by cerebral ischemia-reperfusion injury via regulation of the AMPK/CREB/BDNF pathway. Front Pharmacol. (2022b);13:832611. doi: 10.3389/fphar.2022.832611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Liu Y, Tang G, Li Y, Wang Y, Chen X, Gu X, Zhang Z, Wang Y, Yang GY. Metformin attenuates blood-brain barrier disruption in mice following middle cerebral artery occlusion. J Neuroinflammation. (2014a);11:177. doi: 10.1186/s12974-014-0177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Liu Y, Tang G, Zhang Z, Wang Y, Yang GY. Metformin promotes focal angiogenesis and neurogenesis in mice following middle cerebral artery occlusion. Neurosci Lett. (2014b);579:46–51. doi: 10.1016/j.neulet.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 119.Livingston JM, Syeda T, Christie T, Gilbert EAB, Morshead CM. Subacute metformin treatment reduces inflammation and improves functional outcome following neonatal hypoxia ischemia. Brain Behav Immun Health. (2020);7:100119. doi: 10.1016/j.bbih.2020.100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lu M, Su C, Qiao C, Bian Y, Ding J, Hu G. Metformin prevents dopaminergic neuron death in MPTP/P-induced mouse model of Parkinson's disease via autophagy and mitochondrial ROS clearance. Int J Neuropsychopharmacol. (2016);19:pyw047. doi: 10.1093/ijnp/pyw047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Lu XY, Huang S, Chen QB, Zhang D, Li W, Ao R, Leung FCY, Zhang Z, Huang J, Tang Y, Zhang SJ. Metformin ameliorates Aβpathology by insulin-degrading enzyme in a transgenic mouse model of Alzheimer's disease. Oxid Med Cell Longev. (2020);2020:2315106. doi: 10.1155/2020/2315106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ma TC, Buescher JL, Oatis B, Funk JA, Nash AJ, Carrier RL, Hoyt KR. Metformin therapy in a transgenic mouse model of Huntington's disease. Neurosci Lett. (2007);411:98–103. doi: 10.1016/j.neulet.2006.10.039. [DOI] [PubMed] [Google Scholar]
- 123.Maldonado PP, Guevara C, Olesen MA, Orellana JA, Quintanilla RA, Ortiz FC. Neurodegeneration in multiple sclerosis:the role of Nrf2-dependent pathways. Antioxidants (Basel) (2022);11:1146. doi: 10.3390/antiox11061146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Martin-Montalvo A, Mercken EM, Mitchell SJ, Palacios HH, Mote PL, Scheibye-Knudsen M, Gomes AP, Ward TM, Minor RK, Blouin MJ, Schwab M, Pollak M, Zhang Y, Yu Y, Becker KG, Bohr VA, Ingram DK, Sinclair DA, Wolf NS, Spindler SR, et al. Metformin improves healthspan and lifespan in mice. Nat Commun. (2013);4:2192. doi: 10.1038/ncomms3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Mary A, Eysert F, Checler F, Chami M. Mitophagy in Alzheimer's disease:molecular defects and therapeutic approaches. Mol Psychiatry. (2022);28:202–216. doi: 10.1038/s41380-022-01631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mastroeni D, Khdour OM, Delvaux E, Nolz J, Olsen G, Berchtold N, Cotman C, Hecht SM, Coleman PD. Nuclear but not mitochondrial-encoded oxidative phosphorylation genes are altered in aging, mild cognitive impairment, and Alzheimer's disease. Alzheimers Dement. (2017);13:510–519. doi: 10.1016/j.jalz.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Matthes F, Hettich MM, Schilling J, Flores-Dominguez D, Blank N, Wiglenda T, Buntru A, Wolf H, Weber S, Vorberg I, Dagane A, Dittmar G, Wanker E, Ehninger D, Krauss S. Inhibition of the MID1 protein complex:a novel approach targeting APP protein synthesis. Cell Death Discov. (2018);4:4. doi: 10.1038/s41420-017-0003-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.McCullough LD, Zeng Z, Li H, Landree LE, McFadden J, Ronnett GV. Pharmacological inhibition of AMP-activated protein kinase provides neuroprotection in stroke. J Biol Chem. (2005);280:20493–20502. doi: 10.1074/jbc.M409985200. [DOI] [PubMed] [Google Scholar]
- 129.Mendonça IP, de Paiva IHR, Duarte-Silva EP, de Melo MG, da Silva RS, do Nascimento MIX, Peixoto CA. Metformin improves depressive-like behavior in experimental Parkinson's disease by inducing autophagy in the substantia nigra and hippocampus. Inflammopharmacology. (2022a);30:1705–1716. doi: 10.1007/s10787-022-01043-6. [DOI] [PubMed] [Google Scholar]
- 130.Mendonça IP, Paiva IHR de, Duarte-Silva EP, Melo MG de, Silva RS da, Oliveira WH de, Costa BL da SA da, Peixoto CA. Metformin and fluoxetine improve depressive-like behavior in a murine model of Parkinsońs disease through the modulation of neuroinflammation, neurogenesis and neuroplasticity. Int Immunopharmacol. (2022b);102:108415. doi: 10.1016/j.intimp.2021.108415. [DOI] [PubMed] [Google Scholar]
- 131.Meng X, Chu G, Yang Z, Qiu P, Hu Y, Chen X, Peng W, Ye C, He FF, Zhang C. Metformin protects neurons against oxygen-glucose deprivation/reoxygenation-induced injury by down-regulating MAD2B. Cell Physiol Biochem. (2016);40:477–485. doi: 10.1159/000452562. [DOI] [PubMed] [Google Scholar]
- 132.Meyerhof O. About the formation of lactic acid in the cut muscle. Pflug Arch Ges Physiolo. (1921);188:114. [Google Scholar]
- 133.Miller RA, Chu Q, Xie J, Foretz M, Viollet B, Birnbaum MJ. Biguanides suppress hepatic glucagon signalling by decreasing production of cyclic AMP. Nature. (2013);494:256–260. doi: 10.1038/nature11808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mima Y, Kuwashiro T, Yasaka M, Tsurusaki Y, Nakamura A, Wakugawa Y, Okada Y. Impact of metformin on the severity and outcomes of acute ischemic stroke in patients with type 2 diabetes mellitus. J Stroke Cerebrovasc Dis. (2016);25:436–446. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.016. [DOI] [PubMed] [Google Scholar]
- 135.Misrani A, Tabassum S, Yang L. Mitochondrial dysfunction and oxidative stress in Alzheimer's disease. Front Aging Neurosci. (2021);13:57. doi: 10.3389/fnagi.2021.617588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Monk R, Connor B. Cell reprogramming to model Huntington's disease:a comprehensive review. Cells. (2021);10:1565. doi: 10.3390/cells10071565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Moore EM, Mander AG, Ames D, Kotowicz MA, Carne RP, Brodaty H, Woodward M, Boundy K, Ellis KA, Bush AI, Faux NG, Martins R, Szoeke C, Rowe C, Watters DA. Increased risk of cognitive impairment in patients with diabetes is associated with metformin. Diabetes Care. (2013);36:2981. doi: 10.2337/dc13-0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Moore P, White J, Christiansen V, Grammas P. Protein kinase C-zeta activity but not level is decreased in Alzheimer's disease microvessels. Neurosci Lett. (1998);254:29–32. doi: 10.1016/s0304-3940(98)00653-3. [DOI] [PubMed] [Google Scholar]
- 139.Mor DE, Sohrabi S, Kaletsky R, Keyes W, Tartici A, Kalia V, Miller GW, Murphy CT. Metformin rescues Parkinson's disease phenotypes caused by hyperactive mitochondria. Proc Natl Acad Sci U S A. (2020);117:26438–26447. doi: 10.1073/pnas.2009838117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Moreno-Navarrete JM, Ortega FJ, Rodríguez-Hermosa JI, Sabater M, Pardo G, Ricart W, Fernández-Real JM. OCT1 expression in adipocytes could contribute to increased metformin action in obese subjects. Diabetes. (2011);60:168–176. doi: 10.2337/db10-0805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Muri L, Le ND, Zemp J, Grandgirard D, Leib SL. Metformin mediates neuroprotection and attenuates hearing loss in experimental pneumococcal meningitis. J Neuroinflammation. (2019);16:156. doi: 10.1186/s12974-019-1549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Nassar SZ, Badae NM, Issa YA. Effect of amylin on memory and central insulin resistance in a rat model of Alzheimer's disease. Arch Physiol Biochem. (2020);126:326–334. doi: 10.1080/13813455.2018.1534244. [DOI] [PubMed] [Google Scholar]
- 143.Nath N, Khan M, Paintlia MK, Hoda MN, Giri S. Metformin attenuated the autoimmune disease of the central nervous system in animal models of multiple sclerosis. J Immunol. (2009);182:8005. doi: 10.4049/jimmunol.0803563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Negrotto L, Farez MF, Correale J. Immunologic effects of metformin and pioglitazone treatment on metabolic syndrome and multiple sclerosis. JAMA Neurol. (2016);73:520–528. doi: 10.1001/jamaneurol.2015.4807. [DOI] [PubMed] [Google Scholar]
- 145.Neumann B, Baror R, Zhao C, Segel M, Dietmann S, Rawji KS, Foerster S, McClain CR, Chalut K, van Wijngaarden P, Franklin RJM. Metformin restores CNS remyelination capacity by rejuvenating aged stem cells. Cell Stem Cell. (2019);25:473–485. doi: 10.1016/j.stem.2019.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nicoletti V, Palermo G, Del Prete E, Mancuso M, Ceravolo R. Understanding the multiple role of mitochondria in Parkinson's disease and related disorders:lesson from genetics and protein–interaction network. Front Cell Dev Biol. (2021);9:636506. doi: 10.3389/fcell.2021.636506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Oliveira WH, Braga CF, Lós DB, Araújo SMR, França MER, Duarte-Silva E, Rodrigues GB, Rocha SWS, Peixoto CA. Metformin prevents p-tau and amyloid plaque deposition and memory impairment in diabetic mice. Exp Brain Res. (2021);239:2821–2839. doi: 10.1007/s00221-021-06176-8. [DOI] [PubMed] [Google Scholar]
- 148.Ou Z, Kong X, Sun X, He X, Zhang L, Gong Z, Huang J, Xu B, Long D, Li J, Li Q, Xu L, Xuan A. Metformin treatment prevents amyloid plaque deposition and memory impairment in APP/PS1 mice. Brain Behav Immun. (2018);69:351–363. doi: 10.1016/j.bbi.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 149.Ould-Brahim F, Sarma SN, Syal C, Lu KJ, Seegobin M, Carter A, Jeffers MS, Doré C, Stanford WL, Corbett D, Wang J. Metformin preconditioning of human induced pluripotent stem cell-derived neural stem cells promotes their engraftment and improves post-stroke regeneration and recovery. Stem Cells Dev. (2018);27:1085–1096. doi: 10.1089/scd.2018.0055. [DOI] [PubMed] [Google Scholar]
- 150.Ozbey G, Nemutlu-Samur D, Parlak H, Yildirim S, Aslan M, Tanriover G, Agar A. Metformin protects rotenone-induced dopaminergic neurodegeneration by reducing lipid peroxidation. Pharmacol Rep. (2020);72:1397–1406. doi: 10.1007/s43440-020-00095-1. [DOI] [PubMed] [Google Scholar]
- 151.Paintlia A, Mohan S, Singh I. Combinatorial effect of metformin and lovastatin impedes T-cell autoimmunity and neurodegeneration in experimental autoimmune encephalomyelitis. J Clin Cell Immunol. (2013a) doi: 10.4172/2155-9899.1000149. doi:10.4172/2155-9899.1000149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Paintlia AS, Paintlia MK, Mohan S, Singh AK, Singh I. AMP-activated protein kinase signaling protects oligodendrocytes that restore central nervous system functions in an experimental autoimmune encephalomyelitis model. Am J Pathol. (2013b);183:526–541. doi: 10.1016/j.ajpath.2013.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Panza F, Lozupone M, Logroscino G, Imbimbo BP. A critical appraisal of amyloid-β-targeting therapies for Alzheimer disease. Nature Rev Neurol. (2019);15:73–88. doi: 10.1038/s41582-018-0116-6. [DOI] [PubMed] [Google Scholar]
- 154.Patergnani S, Castellazzi M, Bonora M, Marchi S, Casetta I, Pugliatti M, Giorgi C, Granieri E, Pinton P. Autophagy and mitophagy elements are increased in body fluids of multiple sclerosis-affected individuals. J Neurol Neurosurg Psychiatry. (2018);89:439–441. doi: 10.1136/jnnp-2017-316234. [DOI] [PubMed] [Google Scholar]
- 155.Patergnani S, Fossati V, Bonora M, Giorgi C, Marchi S, Missiroli S, Rusielewicz T, Wieckowski MR, Pinton P. Mitochondria in multiple sclerosis:molecular mechanisms of pathogenesis. Int Rev Cell Mol Biol. (2017);328:49–103. doi: 10.1016/bs.ircmb.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 156.Patil SP, Jain PD, Ghumatkar PJ, Tambe R, Sathaye S. Neuroprotective effect of metformin in MPTP-induced Parkinson's disease in mice. Neuroscience. (2014);277:747–754. doi: 10.1016/j.neuroscience.2014.07.046. [DOI] [PubMed] [Google Scholar]
- 157.Pérez-Revuelta BI, Hettich MM, Ciociaro A, Rotermund C, Kahle PJ, Krauss S, di Monte DA. Metformin lowers Ser-129 phosphorylated α-synuclein levels via mTOR-dependent protein phosphatase 2A activation. Cell Death Dis. (2014);5:e1209. doi: 10.1038/cddis.2014.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Picone P, Nuzzo D, Caruana L, Messina E, Barera A, Vasto S, di Carlo M. Metformin increases APP expression and processing via oxidative stress, mitochondrial dysfunction and NF-κB activation:use of insulin to attenuate metformin's effect. Biochim Biophys Acta. (2015);1853:1046–1059. doi: 10.1016/j.bbamcr.2015.01.017. [DOI] [PubMed] [Google Scholar]
- 159.Pilipenko V, Narbute K, Pupure J, Langrate IK, Muceniece R, Kluša V. Neuroprotective potential of antihyperglycemic drug metformin in streptozocin-induced rat model of sporadic Alzheimer's disease. Eur J Pharmacol. (2020);881:173290. doi: 10.1016/j.ejphar.2020.173290. [DOI] [PubMed] [Google Scholar]
- 160.Piro JR, Benjamin DI, Duerr JM, Pi YQ, Gonzales C, Wood KM, Schwartz JW, Nomura DK, Samad TA. A dysregulated endocannabinoid-eicosanoid network supports pathogenesis in a mouse model of Alzheimer's disease. Cell Rep. (2012);1:617–623. doi: 10.1016/j.celrep.2012.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Pirooznia SK, Yuan C, Khan MR, Karuppagounder SS, Wang L, Xiong Y, Kang SU, Lee Y, Dawson VL, Dawson TM. PARIS induced defects in mitochondrial biogenesis drive dopamine neuron loss under conditions of parkin or PINK1 deficiency. Mol Neurodegener. (2020);15:17. doi: 10.1186/s13024-020-00363-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Pomilio C, Pérez NG, Calandri I, Crivelli L, Allegri R, Sevlever G, Saravia F. Diabetic patients treated with metformin during early stages of Alzheimer's disease show a better integral performance:data from ADNI study. Geroscience. (2022);44:1791–1805. doi: 10.1007/s11357-022-00568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Qiu-Yue X, Tian-Yuan Y, Xiao-Long W, Dong-Mei Q, Xiao-Rui C. Effects of metformin on modulating the expression of brain-related genes of APP/PS1 transgenic mice based on single cell sequencing. Curr Alzheimer Res. (2022);19:754–771. doi: 10.2174/1567205020666221201143323. [DOI] [PubMed] [Google Scholar]
- 164.Rena G, Hardie DG, Pearson ER. The mechanisms of action of metformin. Diabetologia. (2017);60:1577–1585. doi: 10.1007/s00125-017-4342-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Rotermund C, Machetanz G, Fitzgerald JC. The therapeutic potential of metformin in neurodegenerative diseases. Front Endocrinol (Lausanne) (2018);9:400. doi: 10.3389/fendo.2018.00400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Ruan C, Guo H, Gao J, Wang Y, Liu Z, Yan J, Li X, Lv H. Neuroprotective effects of metformin on cerebral ischemia-reperfusion injury by regulating PI3K/Akt pathway. Brain Behav. (2021);11:e2335. doi: 10.1002/brb3.2335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Ruddy RM, Adams KV, Morshead CM. Age- and sex-dependent effects of metformin on neural precursor cells and cognitive recovery in a model of neonatal stroke. Sci Adv. (2019);5:eaax1912. doi: 10.1126/sciadv.aax1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ryan SD, Dolatabadi N, Chan SF, Zhang X, Akhtar MW, Parker J, Soldner F, Sunico CR, Nagar S, Talantova M, Lee B, Lopez K, Nutter A, Shan B, Molokanova E, Zhang Y, Han X, Nakamura T, Masliah E, Yates JR, 3rd, et al. Isogenic human iPSC Parkinson's model shows nitrosative stress-induced dysfunction in MEF2-PGC1αtranscription. Cell. (2013);155:1351–1364. doi: 10.1016/j.cell.2013.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Ryu YK, Go J, Park HY, Choi YK, Seo YJ, Choi JH, Rhee M, Lee TG, Lee CH, Kim KS. Metformin regulates astrocyte reactivity in Parkinson's disease and normal aging. Neuropharmacology. (2020);175:108173. doi: 10.1016/j.neuropharm.2020.108173. [DOI] [PubMed] [Google Scholar]
- 170.Saewanee N, Praputpittaya T, Malaiwong N, Chalorak P, Meemon K. Neuroprotective effect of metformin on dopaminergic neurodegeneration and α-synuclein aggregation in C. elegans model of Parkinson's disease. Neurosci Res. (2021);162:13–21. doi: 10.1016/j.neures.2019.12.017. [DOI] [PubMed] [Google Scholar]
- 171.Saffari PM, Alijanpour S, Takzaree N, Sahebgharani M, Etemad-Moghadam S, Noorbakhsh F, Partoazar A. Metformin loaded phosphatidylserine nanoliposomes improve memory deficit and reduce neuroinflammation in streptozotocin-induced Alzheimer's disease model. Life Sci. (2020);255:117861. doi: 10.1016/j.lfs.2020.117861. [DOI] [PubMed] [Google Scholar]
- 172.Sajan MP, Hansen BC, Higgs MG, Kahn CR, Braun U, Leitges M, Park CR, Diamond DM, Farese RV. Atypical PKC, PKCλ/ι, activates β-secretase and increases Aβ1-40/42 and phospho-tau in mouse brain and isolated neuronal cells, and may link hyperinsulinemia and other aPKC activators to development of pathological and memory abnormalities in Alzheimer's disease. Neurobiol Aging. (2018);61:225–237. doi: 10.1016/j.neurobiolaging.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Samaras K, Makkar S, Crawford JD, Kochan NA, Wen W, Draper B, Trollor JN, Brodaty H, Sachdev PS. Metformin use is associated with slowed cognitive decline and reduced incident dementia in older adults with type 2 diabetes:the Sydney memory and ageing study. Diabetes Care. (2020);43:2691–2701. doi: 10.2337/dc20-0892. [DOI] [PubMed] [Google Scholar]
- 174.Sanadgol N, Barati M, Houshmand F, Hassani S, Clarner T, shahlaei M, Golab F. Metformin accelerates myelin recovery and ameliorates behavioral deficits in the animal model of multiple sclerosis via adjustment of AMPK/Nrf2/mTOR signaling and maintenance of endogenous oligodendrogenesis during brain self-repairing period. Pharmacol Rep. (2020);72:641–658. doi: 10.1007/s43440-019-00019-8. [DOI] [PubMed] [Google Scholar]
- 175.Sanchis A, García-Gimeno MA, Cañada-Martínez AJ, Sequedo MD, Millán JM, Sanz P, Vázquez-Manrique RP. Metformin treatment reduces motor and neuropsychiatric phenotypes in the zQ175 mouse model of Huntington disease. Exp Mol Med. (2019);51:1–16. doi: 10.1038/s12276-019-0264-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sardoiwala MN, Srivastava AK, Kaundal B, Karmakar S, Choudhury SR. Recuperative effect of metformin loaded polydopamine nanoformulation promoting EZH2 mediated proteasomal degradation of phospho-α-synuclein in Parkinson's disease model. Nanomedicine. (2020);24:102088. doi: 10.1016/j.nano.2019.102088. [DOI] [PubMed] [Google Scholar]
- 177.Sarkaki A, Farbood Y, Badavi M, Khalaj L, Khodagholi F, Ashabi G. Metformin improves anxiety-like behaviors through AMPK-dependent regulation of autophagy following transient forebrain ischemia. Metab Brain Dis. (2015);30:1139–1150. doi: 10.1007/s11011-015-9677-x. [DOI] [PubMed] [Google Scholar]
- 178.Secnik J, Xu H, Schwertner E, Hammar N, Alvarsson M, Winblad B, Eriksdotter M, Garcia-Ptacek S, Religa D. The association of antidiabetic medications and Mini-Mental State Examination scores in patients with diabetes and dementia. Alzheimers Res Ther. (2021);13:197. doi: 10.1186/s13195-021-00934-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Shen L, Gan Q, Yang Y, Reis C, Zhang Z, Xu S, Zhang T, Sun C. Mitophagy in cerebral ischemia and ischemia/reperfusion injury. Front Aging Neurosci. (2021);13:687246. doi: 10.3389/fnagi.2021.687246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sheng B, Liu J, Li GH. Metformin preconditioning protects Daphnia pulex from lethal hypoxic insult involving AMPK, HIF and mTOR signaling. Comp Biochem Physiol B Biochem Mol Biol. (2012);163:51–58. doi: 10.1016/j.cbpb.2012.04.009. [DOI] [PubMed] [Google Scholar]
- 181.Shi Q, Liu S, Fonseca VA, Thethi TK, Shi L. Effect of metformin on neurodegenerative disease among elderly adult US veterans with type 2 diabetes mellitus. BMJ Open. (2019);9:e024954. doi: 10.1136/bmjopen-2018-024954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Shi Q, Cheng Q, Chen C. The role of autophagy in the pathogenesis of ischemic stroke. Curr Neuropharmacol. (2021);19:629–640. doi: 10.2174/1570159X18666200729101913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Silva D, Rocha R, Correia AS, Mota B, Madeira MD, Vale N, Cardoso A. Repurposed edaravone, metformin, and perampanel as a potential treatment for hypoxia-ischemia encephalopathy:an in vitro study. Biomedicines. (2022);10:3043. doi: 10.3390/biomedicines10123043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Skemiene K, Rekuviene E, Jekabsone A, Cizas P, Morkuniene R, Borutaite V. Comparison of effects of metformin, phenformin, and inhibitors of mitochondrial complex I on mitochondrial permeability transition and ischemic brain injury. Biomolecules. (2020);10:1400. doi: 10.3390/biom10101400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Sluggett JK, Koponen M, Simon Bell J, Taipale H, Tanskanen A, Tiihonen J, Uusitupa M, Tolppanen AM, Hartikainen S. Metformin and risk of Alzheimer's disease among community-dwelling people with diabetes:a national case-control study. J Clin Endocrinol Metab. (2020);105:E963–972. doi: 10.1210/clinem/dgz234. [DOI] [PubMed] [Google Scholar]
- 186.Sohrabi S, Mor DE, Kaletsky R, Keyes W, Murphy CT. High-throughput behavioral screen in C. elegans reveals Parkinson's disease drug candidates. Commun Biol. (2021);4:203. doi: 10.1038/s42003-021-01731-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Son SM, Shin HJ, Byun J, Kook SY, Moon M, Chang YJ, Mook-Jung I. Metformin facilitates amyloid-βgeneration by β- and γ-secretases via autophagy activation. J Alzheimers Dis. (2016);51:1197–1208. doi: 10.3233/JAD-151200. [DOI] [PubMed] [Google Scholar]
- 188.Sorrentino V, Romani M, Mouchiroud L, Beck JS, Zhang H, D'Amico D, Moullan N, Potenza F, Schmid AW, Rietsch S, Counts SE, Auwerx J. Enhancing mitochondrial proteostasis reduces amyloid-βproteotoxicity. Nature. (2017);552:187–193. doi: 10.1038/nature25143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Sritawan N, Prajit R, Chaisawang P, Sirichoat A, Pannangrong W, Wigmore P, Welbat JU. Metformin alleviates memory and hippocampal neurogenesis decline induced by methotrexate chemotherapy in a rat model. Biomed Pharmacother. (2020);131:110651. doi: 10.1016/j.biopha.2020.110651. [DOI] [PubMed] [Google Scholar]
- 190.Sterne J. Innovations in antidiabetics. NN dimethylamine. Maroc Med. (1957);36:1295–1296. [Google Scholar]
- 191.Sun Y, Tian T, Gao J, Liu X, Hou H, Cao R, Li B, Quan M, Guo L. Metformin ameliorates the development of experimental autoimmune encephalomyelitis by regulating T helper 17 and regulatory T cells in mice. J Neuroimmunol. (2016);292:58–67. doi: 10.1016/j.jneuroim.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 192.Svirskiene N, Pampuscenko K, Svirskis G, Borutaite V. Different effects of metformin and phenformin on hypoxia-induced Ca2+ fluxes in cultured primary neurons. Brain Res. (2021);1750:147151. doi: 10.1016/j.brainres.2020.147151. [DOI] [PubMed] [Google Scholar]
- 193.Swomley AM, Butterfield DA. Oxidative stress in Alzheimer disease and mild cognitive impairment:evidence from human data provided by redox proteomics. Arch Toxicol. (2015);89:1669–1680. doi: 10.1007/s00204-015-1556-z. [DOI] [PubMed] [Google Scholar]
- 194.Syal C, Kosaraju J, Hamilton L, Aumont A, Chu A, Sarma SN, Thomas J, Seegobin M, Jeffrey Dilworth F, He L, Wondisford FE, Zimmermann R, Parent M, Fernandes K, Wang J. Dysregulated expression of monoacylglycerol lipase is a marker for anti-diabetic drug metformin-targeted therapy to correct impaired neurogenesis and spatial memory in Alzheimer's disease. Theranostics. (2020);10:6337. doi: 10.7150/thno.44962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Syal C, Wang J. Biomarker-guided drug therapy:personalized medicine for treating Alzheimer's disease. Neural Regen Res. (2021);16:2010–2011. doi: 10.4103/1673-5374.308079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Tan MG, Chua WT, Esiri MM, Smith AD, Vinters HV, Lai MK. Genome wide profiling of altered gene expression in the neocortex of Alzheimer's disease. J Neurosci Res. (2010);88:1157–1169. doi: 10.1002/jnr.22290. [DOI] [PubMed] [Google Scholar]
- 197.Tang X, Brinton RD, Chen Z, Farland LV., Klimentidis Y, Migrino R, Reaven P, Rodgers K, Zhou JJ. Use of oral diabetes medications and the risk of incident dementia in US veterans aged ≥60 years with type 2 diabetes. BMJ Open Diabetes Res Care. (2022);10:e002894. doi: 10.1136/bmjdrc-2022-002894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Tanret G. An alkaloid extracted from Galega officinalis. Compt Rend. (1914);158:1182–1184. [Google Scholar]
- 199.Tayara K, Espinosa-Oliva AM, García-Domínguez I, Ismaiel AA, Boza-Serrano A, Deierborg T, Machado A, Herrera AJ, Venero JL, de Pablos RM. Divergent effects of metformin on an inflammatory model of Parkinson's disease. Front Cell Neurosci. (2018);12:440. doi: 10.3389/fncel.2018.00440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Teo E, Ravi S, Barardo D, Kim HS, Fong S, Gassiot AC, Tan TY, Ching J, Kovalik JP, Wenk MR, Gunawan R, Moore PK, Halliwell B, Tolwinski N, Gruber J. Metabolic stress is a primary pathogenic event in transgenic Caenorhabditis elegans expressing pan-neuronal human amyloid beta. Elife. (2019);8:e50069. doi: 10.7554/eLife.50069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Torrandell-Haro G, Branigan GL, Brinton RD, Rodgers KE. Association between specific type 2 diabetes therapies and risk of Alzheimer's disease and related dementias in propensity-score matched type 2 diabetic patients. Front Aging Neurosci. (2022);14:878304. doi: 10.3389/fnagi.2022.878304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Trueman RC, Klein A, Lindgren HS, Lelos MJ, Dunnett SB. Repair of the CNS using endogenous and transplanted neural stem cells. Curr Top Behav Neurosci. (2013);15:357–398. doi: 10.1007/7854_2012_223. [DOI] [PubMed] [Google Scholar]
- 203.Tseng CH. Metformin and the risk of dementia in type 2 diabetes patients. Aging Dis. (2019);10:37. doi: 10.14336/AD.2017.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Tu WJ, Liu Z, Chao BH, Yan F, Ma L, Cao L, Ji XM, Wang L de. Metformin use is associated with low risk of case fatality and disability rates in first-ever stroke patients with type 2 diabetes. Ther Adv Chronic Dis. (2022) doi: 10.1177/20406223221076894. doi:10.1177/20406223221076894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Vázquez-Manrique RP, Farina F, Cambon K, Dolores Sequedo M, Parker AJ, Millán JM, Weiss A, Déglon N, Neri C. AMPK activation protects from neuronal dysfunction and vulnerability across nematode, cellular and mouse models of Huntington's disease. Hum Mol Genet. (2016);25:1043–1058. doi: 10.1093/hmg/ddv513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Venna VR, Li J, Hammond MD, Mancini NS, Mccullough LD. Chronic metformin treatment improves post-stroke angiogenesis and recovery after experimental stroke. Eur J Neurosci. (2014);39:2129–2138. doi: 10.1111/ejn.12556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Vogler S, Goedde R, Miterski B, Gold R, Kroner A, Koczan D, Zettl UK, Rieckmann P, Epplen JT, Ibrahim SM. Association of a common polymorphism in the promoter of UCP2 with susceptibility to multiple sclerosis. J Mol Med (Berl) (2005);83:806–811. doi: 10.1007/s00109-005-0661-5. [DOI] [PubMed] [Google Scholar]
- 208.Wang DX, Chen AD, Wang QJ, Xin YY, Yin J, Jing YH. Protective effect of metformin against rotenone-induced parkinsonism in mice. Toxicol Mech Methods. (2020a);30:350–357. doi: 10.1080/15376516.2020.1741053. [DOI] [PubMed] [Google Scholar]
- 209.Wang J, Gallagher D, Devito LM, Cancino GI, Tsui D, He L, Keller GM, Frankland PW, Kaplan DR, Miller FD. Metformin activates an atypical PKC-CBP pathway to promote neurogenesis and enhance spatial memory formation. Cell Stem Cell. (2012);11:23–35. doi: 10.1016/j.stem.2012.03.016. [DOI] [PubMed] [Google Scholar]
- 210.Wang L, Wang A, Guo H, Zhang Z, Wang S, Pei T, Liu Z, Yang D, Liu Y, Ruan C. Neuroprotective effects of long-term metformin preconditioning on rats with ischemic brain injuries. Eur Neurol. (2021);84:212–218. doi: 10.1159/000514431. [DOI] [PubMed] [Google Scholar]
- 211.Wang W, Zhao F, Ma X, Perry G, Zhu X. Mitochondria dysfunction in the pathogenesis of Alzheimer's disease:recent advances. Mol Neurodegener. (2020b);15:30. doi: 10.1186/s13024-020-00376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Wang X, Su B, Lee HG, Li X, Perry G, Smith MA, Zhu X. Impaired balance of mitochondrial fission and fusion in Alzheimer's disease. J Neurosci. (2009);29:9090–9103. doi: 10.1523/JNEUROSCI.1357-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Wang Y, An H, Liu T, Qin C, Sesaki H, Guo S, Radovick S, Hussain M, Maheshwari A, Wondisford FE, O'Rourke B, He L. Metformin improves mitochondrial respiratory activity through activation of AMPK. Cell Rep. (2019);29:1511. doi: 10.1016/j.celrep.2019.09.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Wang YL, Zhao JH, Guo FL, Gao XH, Xie X, Liu SQ, Yang X, Yang XF, Zhang LY, Ye YX, Fan LB, Wang JG. Metformin ameliorates synaptic defects in a mouse model of AD by inhibiting Cdk5 activity. Front Cell Neurosci. (2020c);14:170. doi: 10.3389/fncel.2020.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Watanabe CK. Studies in the metabolic changes induced by administration of guanidine bases. J Biol Chem. (1918);33:253–265. [Google Scholar]
- 216.Waugh NR, Dallas JH, Jung RT, Newton RW. Mortality in a cohort of diabetic patients. Causes and relative risks. Diabetologia. (1989);32:103–104. doi: 10.1007/BF00505181. [DOI] [PubMed] [Google Scholar]
- 217.Westphal LP, Widmer R, Held U, Steigmiller K, Hametner C, Ringleb P, Curtze S, Martinez-Majander N, Tiainen M, Nolte CH, Scheitz JF, Erdur H, Polymeris AA, Traenka C, Eskandari A, Michel P, Heldner MR, Arnold M, Zini A, Vandelli L, et al. Association of prestroke metformin use, stroke severity, and thrombolysis outcome. Neurology. (2020);95:e362–373. doi: 10.1212/WNL.0000000000009951. [DOI] [PubMed] [Google Scholar]
- 218.Witte ME, Lars B, Rodenburg RJ, Belien JA, Musters R, Hazes T, Wintjes LT, Smeitink JA, Geurts JJG, De Vries HE, Van Der Valk P, Van Horssen J. Enhanced number and activity of mitochondria in multiple sclerosis lesions. J Pathol. (2009);219:193–204. doi: 10.1002/path.2582. [DOI] [PubMed] [Google Scholar]
- 219.Witte ME, Nijland PG, Drexhage JAR, Gerritsen W, Geerts D, van het Hof B, Reijerkerk A, de Vries HE, van der Valk P, van Horssen J. Reduced expression of PGC-1αpartly underlies mitochondrial changes and correlates with neuronal loss in multiple sclerosis cortex. Acta Neuropathol. (2013);125:231–243. doi: 10.1007/s00401-012-1052-y. [DOI] [PubMed] [Google Scholar]
- 220.Wium-Andersen IK, Osler M, Jørgensen MB, Rungby J, Wium-Andersen MK. Antidiabetic medication and risk of dementia in patients with type 2 diabetes:a nested case-control study. Eur J Endocrinol. (2019);181:499–507. doi: 10.1530/EJE-19-0259. [DOI] [PubMed] [Google Scholar]
- 221.Wu TY, Campbell BCV, Strbian D, Yassi N, Putaala J, Tatlisumak T, Davis SM, Meretoja A, Hanley DF, Butcher K, Gregson B, Davis S, Lees KR, Lyden P, Muir K, Steiner T, Mayer S. Impact of pre-stroke sulphonylurea and metformin use on mortality of intracerebral haemorrhage. Eur Stroke J. (2016);1:302–309. doi: 10.1177/2396987316666617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Xu C, Chen J, Xu X, Zhang Y, Li J. Potential therapeutic drugs for Parkinson's disease based on data mining and bioinformatics analysis. Parkinsons Dis. (2018);2018:3464578. doi: 10.1155/2018/3464578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Xu X, Sun Y, Cen X, Shan B, Zhao Q, Xie T, Wang Z, Hou T, Xue Y, Zhang M, Peng D, Sun Q, Yi C, Najafov A, Xia H. Metformin activates chaperone-mediated autophagy and improves disease pathologies in an Alzheimer disease mouse model. Protein Cell. (2021);12:769–787. doi: 10.1007/s13238-021-00858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Yablonska S, Ganesan V, Ferrando LM, Kim JH, Pyzel A, Baranova OV, Khattar NK, Larkin TM, Baranov SV, Chen N, Strohlein CE, Stevens DA, Wang X, Chang YF, Schurdak ME, Carlisle DL, Minden JS, Friedlander RM. Mutant huntingtin disrupts mitochondrial proteostasis by interacting with TIM23. Proc Natl Acad Sci U S A. (2019);116:16593–16602. doi: 10.1073/pnas.1904101116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Yan Q, Han C, Wang G, Waddington JL, Zheng L, Zhen X. Activation of AMPK/mTORC1-mediated autophagy by metformin reverses Clk1 deficiency-sensitized dopaminergic neuronal death. Mol Pharmacol. (2017);92:640–652. doi: 10.1124/mol.117.109512. [DOI] [PubMed] [Google Scholar]
- 226.Yang JL, Mukda S, Chen S Der. Diverse roles of mitochondria in ischemic stroke. Redox Biol. (2018);16:263–275. doi: 10.1016/j.redox.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Yang M, Darwish T, Larraufie P, Rimmington D, Cimino I, Goldspink DA, Jenkins B, Koulman A, Brighton CA, Ma M, Lam BYH, Coll AP, O'Rahilly S, Reimann F, Gribble FM. Inhibition of mitochondrial function by metformin increases glucose uptake, glycolysis and GDF-15 release from intestinal cells. Sci Rep. (2021);(2529);11 doi: 10.1038/s41598-021-81349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Yu CC, Chen HL, Chen MH, Lu CH, Tsai NW, Huang CC, Chang YY, Li SH, Chen YS, Chiang PL, Lin WC. Vascular inflammation is a risk factor associated with brain atrophy and disease severity in Parkinson's disease:a case-control study. Oxid Med Cell Longev. (2020);2020:2591248. doi: 10.1155/2020/2591248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Yu H, Zhong X, Gao P, Shi J, Wu Z, Guo Z, Wang Z, Song Y. The potential effect of metformin on cancer:an umbrella review. Front Endocrinol (Lausanne) (2019);10:617. doi: 10.3389/fendo.2019.00617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Yuan R, Wang Y, Li Q, Zhen F, Li X, Lai Q, Hu P, Wang X, Zhu Y, Fan H, Yao R. Metformin reduces neuronal damage and promotes neuroblast proliferation and differentiation in a cerebral ischemia/reperfusion rat model. Neuroreport. (2019);30:232–240. doi: 10.1097/WNR.0000000000001190. [DOI] [PubMed] [Google Scholar]
- 231.Zemgulyte G, Tanaka S, Hide I, Sakai N, Pampuscenko K, Borutaite V, Rastenyte D. Evaluation of the effectiveness of post-stroke metformin treatment using permanent middle cerebral artery occlusion in rats. Pharmaceuticals (Basel) (2021);14:312. doi: 10.3390/ph14040312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Zeng H, Xu L, Zou Y, Wang S. Romidepsin and metformin nanomaterials delivery on streptozocin for the treatment of Alzheimer's disease in animal model. Biomed Pharmacother. (2021);141:111864. doi: 10.1016/j.biopha.2021.111864. [DOI] [PubMed] [Google Scholar]
- 233.Zeng J, Zhu L, Liu J, Zhu T, Xie Z, Sun X, Zhang H. Metformin protects against oxidative stress injury induced by ischemia/reperfusion via regulation of the lncRNA-H19/miR-148a-3p/Rock2 axis. Oxid Med Cell Longev. (2019);2019:8768327. doi: 10.1155/2019/8768327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Zhang G, Chen S, Jia J, Liu C, Wang W, Zhang H, Zhen X. Development and evaluation of novel metformin derivative metformin threonate for brain ischemia treatment. Front Pharmacol. (2022);13:879690. doi: 10.3389/fphar.2022.879690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Zhang J, Lin Y, Dai X, Fang W, Wu X, Chen X. Metformin treatment improves the spatial memory of aged mice in an APOE genotype-dependent manner. FASEB J. (2019);33:7748–7757. doi: 10.1096/fj.201802718R. [DOI] [PubMed] [Google Scholar]
- 236.Zhao S, Fan Z, Zhang X, Li Z, Shen T, Li K, Yan Y, Yuan Y, Pu J, Tian J, Liu Z, Chen Y, Zhang B. Metformin attenuates tau pathology in tau-seeded PS19 mice. Neurotherapeutics. (2022) doi: 10.1007/s13311-022-01316-6. doi:10.1007/S13311-022-01316-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Zheng J, Xu M, Walker V, Yuan J, Korologou-Linden R, Robinson J, Huang P, Burgess S, Au Yeung SL, Luo S, Holmes MV, Davey Smith G, Ning G, Wang W, Gaunt TR, Bi Y. Evaluating the efficacy and mechanism of metformin targets on reducing Alzheimer's disease risk in the general population:a Mendelian randomisation study. Diabetologia. (2022);65:1664–1675. doi: 10.1007/s00125-022-05743-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Zhou JB, Tang X, Han M, Yang J, Simó R. Impact of antidiabetic agents on dementia risk:a Bayesian network meta-analysis. Metabolism. (2019);109:154265. doi: 10.1016/j.metabol.2020.154265. [DOI] [PubMed] [Google Scholar]
- 239.Zhu X, Shen J, Feng S, Huang C, Liu Z, Sun YE, Liu H. Metformin improves cognition of aged mice by promoting cerebral angiogenesis and neurogenesis. Aging (Albany NY) (2020);12:17845. doi: 10.18632/aging.103693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Zhu XC, Jiang T, Zhang QQ, Cao L, Tan MS, Wang HF, Ding ZZ, Tan L, Yu JT. Chronic metformin preconditioning provides neuroprotection via suppression of NF-κB-mediated inflammatory pathway in rats with permanent cerebral ischemia. Mol Neurobiol. (2015);52:375–385. doi: 10.1007/s12035-014-8866-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The positive effect of metformin on neurological diseases in humans and in vivo


