Abstract
Objective
To analyze the current research status, hotspots, and frontiers in the field of Gastrointestinal (GI) cancer and quality of life (QoL) through the bibliometrics method, and to provide references and guidance for future research.
Methods
Literature related to GI cancer and QoL from April 1, 2003 to March 31, 2023 was retrieved from the Web of Science Core Collection database. CiteSpace 6.2.R1 was performed for collaboration analysis, keyword co-occurrence analysis, and document co-citation analysis.
Results
A total of 1224 publications were included in this study. There has been a significant increase in the number of publications in this field over the past two decades. The United States, the Karolinska Institute and the University of Amsterdam, and Pernilla Lagergren are the most prolific country, institution, and author, respectively. The links between most of the research constituents were relatively thin (centrality <0.1). The keyword analysis indicates that the benefits of physical activity on QoL, the levels of psychological distress and its relationship with QoL, as well as the development and validation of QoL measurement tools have been the research hotspots. Open-label/double-blind trials exploring therapeutic interventions and more targeted new drugs or more effective drug combinations, and longitudinal studies determining the direction of the association between psychological distress and QoL at different time points, may be emerging trends in this field.
Conclusion
The cooperation among countries, institutions, and authors in this field should be strengthened. In addition, the health benefits of light physical activity, interventions for QoL, trajectory and direction of the relationship between psychological distress and QoL may be the focus of future research.
Keywords: Gastrointestinal cancer, Quality of life, Frontiers, Bibliometric analysis
1. Introduction
Gastrointestinal (GI) cancer is a malignant tumor occurring in the digestive tract and digestive gland, with a high incidence rate and mortality. It mainly includes colorectal cancer (CRC), esophageal cancer, gastric cancer (GC), liver cancer, pancreatic cancer, biliary tract cancer, and anal cancer. It is estimated that there were 5.1 million new cases and 3.6 million deaths of GI cancer worldwide in 2020, accounting for more than one-quarter (26.7 %) and over one-third (36.5 %) of the global cancer incidence and cancer-related deaths, respectively [1]. Moreover, the cancer burden will further increase in the next two decades, with an expected increase of 49 % in new cases and 62 % in deaths compared with 2020 [2]. With the continuous optimization of treatment programs, the survival rate of GI cancer patients has greatly increased [3,4], and the 5-year relative survival rates of pancreatic cancer, esophageal cancer, GC, and CRC have reached 12 %, 21 %, 33 %, and 65 %, respectively [5]. However, many studies have shown that GI cancer seriously affects the quality of life (QoL) of survivors, making them suffer from different psychological and physiological torments, as well as pain at different time periods and stages, such as neuropathy, sleep disorders, gastrointestinal reactions, stress, and depression [6,7]. Therefore, improving the QoL for GI cancer survivors is crucial.
In recent decades, a growing number of researchers have been paying attention to GI cancer patients’ QoL, including the development, translation, and validation of measurement tools [[8], [9], [10]], the investigation of the current status and influencing factors of QoL [11,12], the exploration of pathways that affect QoL [13,14], the trial of treatment methods [15,16] and interventions [17,18] for QoL. Although there have been some qualitative reviews summarizing the efficacy of treatment methods [19,20], the effectiveness of interventions such as diet, exercise, and nursing modes [[21], [22], [23]], as well as the measurement tools [24,25], status [24,26], and influencing factors [[27], [28], [29]] of QoL, the research direction and hotspots in this field are still unclear, and the bibliometric method has not been applied to quantitatively describe the research status of QoL for GI cancer survivors.
Bibliometrics is a widely accepted statistical method that utilizes quantitative techniques through developed algorithms to obtain and analyze indicators (e.g., countries, institutions, journals, and keywords) of existing literature to summarize knowledge structure and hotspots evolution in a field [30], providing visual information and potential research directions for researchers. The CiteSpace software [31] is a visual analysis tool that uses nodes representing keywords and references to intuitively indicate hotspots and evolution processes, and make predictions about the frontier and development trends of a field. The aim of this study is to map the scientific networks in the field of GI cancer and QoL over the past two decades through bibliometric analysis, reveal the research hotspots and frontiers in this field, and further enhance the understanding of relevant scientific knowledge to promote the determination of future research directions.
2. Methods
2.1. Data source and retrieval strategies
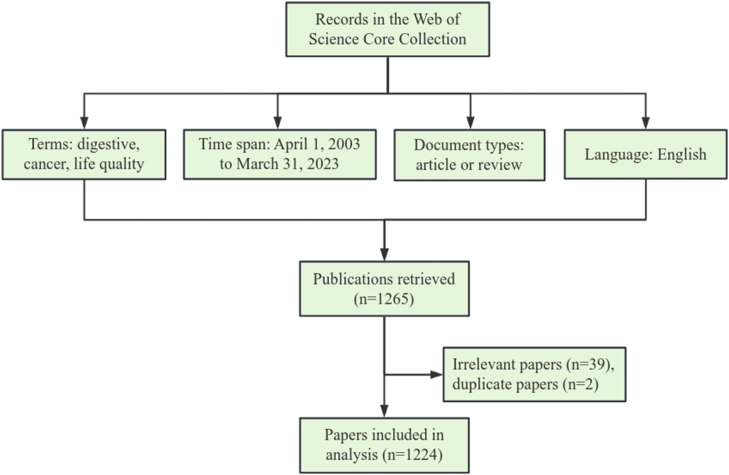
The publications with the period of April 1, 2003 to March 31, 2023 were retrieved from the Web of Science Core Collection (WoSCC) database. The research strategies were as follows: TI=(“digestive” OR “gastrointestinal” OR “gastric” OR “stomach” OR “colon” OR “rectum” OR “colorectum” OR “colorectal” OR “esophagus” OR “esophagus” OR “esophageal” OR “esophageal” OR “esophagogastric” OR “gastroesophageal” OR “esophago-gastric” OR “anal” OR “pancreatic” OR “liver” OR “biliary tract” OR “gallbladder” OR “hepatocellular”) AND TI=(“cancer*” OR “tumor*” OR “tumour*” OR “neoplas*” OR “malignan*” OR “carcinoma*” OR “adenocarcinoma*”) AND TI=(“quality of life” OR “life quality” OR “QoL”) AND DOP=(2003-04-01/2023-03-31). After setting the publication language to “English” and limiting the type of paper to “article” or “review”, a total of 1265 relevant documents were retrieved. The irrelevant literature involving animal studies or “quality-adjusted life years” (n = 39) and duplicate papers (n = 2) were manually deleted, and then the remaining 1224 documents were downloaded in “Plain Text” format of “Full Records and References” for final analysis (Fig. 1). The above procedures were independently conducted by two researchers.
Fig. 1.
Flowchart of data collection process.
2.2. Data analysis
This study used CiteSpace 6.2.R1 (64-bit) software [32] to visually analyze the current status, hotspots, and research trends in the field of GI cancer and QoL, and create knowledge maps, including collaboration network diagrams, keyword clustering diagrams, burst keyword analysis, and timeline diagrams of reference co-citation. The nodes in different visual knowledge maps represent the author, institution, country, keyword, and reference, respectively. The size of nodes indicates the number of publications for research constituents. The links between nodes show the collaboration relationships, with thicker lines indicating closer connections. The betweenness centrality (BC) strength can reflect the influence and intermediary connection degree of constituents in the networks, and nodes with BC ≥ 0.1 will be marked with purple rings on the periphery (the thicker the purple ring, the greater its influence, and the closer its connection with others) [33].
The parameter settings for CiteSpace in this study were as follows: (a) timespan from April 1, 2003 to March 31, 2023, year per slice = 1; (b) term source = title/abstract/author/keywords/keywords plus; (c) node types = author/institution/country/keyword/reference; (d) threshold selection criteria = the top 50 items for each time slice; (e) the settings for other parameters were set as default. The two indicators of Modularity Q value (Q) and Weighted Mean Silhouette value (S), displayed in the upper left corner of the diagrams generated by Citespace software, are the basis for evaluating the effectiveness of graph drawing. Q > 0.3 suggests that the division of cluster structure is significant. S > 0.5 indicates that the clustering results are reasonable, and S > 0.7 is generally considered to have strong convincingness in the clustering results [34].
3. Results
3.1. Annual publications
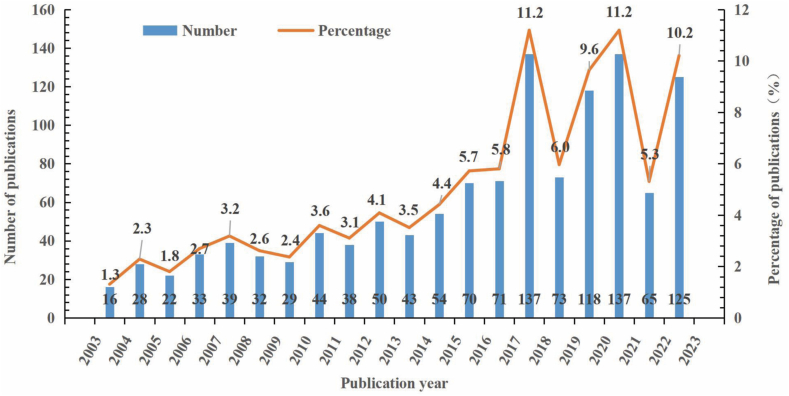
A total of 1224 publications retrieved from WoSCC database were included in this analysis. Before 2017, the quantity of publications increased slowly with some slight fluctuations (Fig. 2). From 2017 to 2021, the growth rate of annual publications soared with significant fluctuations. It was worth noting that the number of publications reached its peak from April 2017 to March 2018, and from April 2020 to March 2021 (n = 137, 11.2 %). Subsequently, the number of publications decreased, but the proportion of annual publications from April 2022 to March 2023 remained high (>10 %). Obviously, the research on GI cancer and QoL remains a potential hot field in the coming years.
Fig. 2.
The annual number of publications on GI cancer and QoL from 2003 to 2023. Note: April of the first year to March of the following year represents a year in the horizontal axis, e.g., 2003–2004 represents April 1, 2003 to March 31, 2004.
3.2. Distribution of journals
The 1224 papers included have been published in 360 journals. The top 10 journals with the largest output accounted for 22.7 % of the whole publications, among which Supportive Care in Cancer was far ahead (n = 52, 4.2 %), followed by European Journal of Cancer (n = 37, 3.0 %) (Table S1). Of note, 60 % of the top 10 journals were in Q1, and the impact factors (IF) of those journals ranged from 2.1 (European Journal of Cancer Care, Q2) to 45.3 (Journal of Clinical Oncology, Q1), with an average of 8.74.
3.3. Collaboration analysis
3.3.1. Country/region collaboration analysis
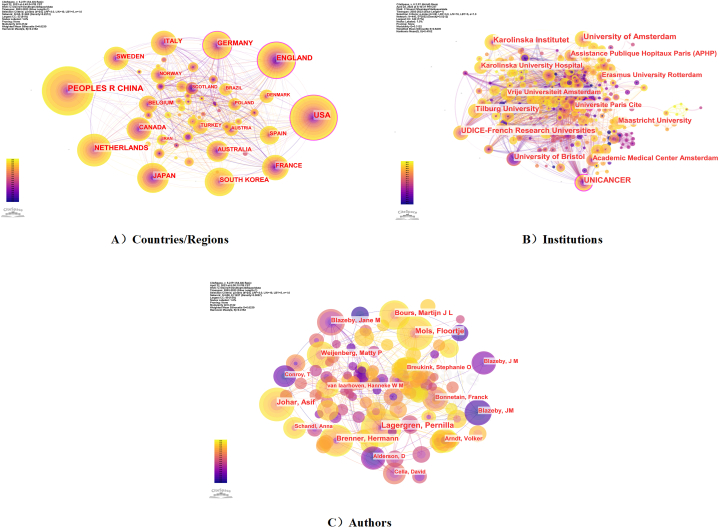
The countries/regions collaboration network consisted of 65 nodes and 460 links, with a network density of 0.2212, indicating the contribution level of scientific research and the degree of cooperation of each country/region in the field of GI cancer and QoL (Fig. 3A). The USA was the leading country in this field (n = 218, 17.8 %), followed by China (n = 209, 17.1 %) and England (n = 145, 11.8 %). The top three countries have published 572 papers, accounting for 46.7 % of the total publications (Table 1). Of note, among the ten countries with the highest productivity, only China belongs to developing countries. The cooperation relationships among high-production countries/regions such as England (centrality = 0.23), the USA (centrality = 0.14), and Germany (centrality = 0.13) were relatively active, while the strength of links between others was thin (centrality <0.1).
Fig. 3.
Collaboration network among research constituents. A) Collaboration network of countries/regions; B) Collaboration network of institutions; C) Collaboration network of authors. Note: The size of nodes indicates the number of publications for research constituents. The links between nodes show the collaboration relationships, with thicker lines indicating closer connections. The colors of nodes and links represent publication and first association time. Nodes with purple rings indicate their centrality >0.1. The thickness of the purple ring around the node shows the strength of centrality (i.e., the thicker the purple ring, the greater its influence, and the closer its connection with other units).
Table 1.
Top 10 countries/regions, institutions and authors of publications.
| No. | Countries/Regions | Count (%) | Centrality | Institution | Count (%) | Centrality | Authors | Count (%) | Centrality |
|---|---|---|---|---|---|---|---|---|---|
| 1 | USA | 218 (17.8) | 0.14 | Karolinska Institute | 40 (3.3) | 0.04 | Pernilla Lagergren | 22 (1.8) | 0.01 |
| 2 | China | 209 (17.1) | 0.03 | University of Amsterdam | 40 (3.3) | 0.02 | Jane M Blazeby | 21 (1.7) | <0.01 |
| 3 | England | 145 (11.8) | 0.23 | Unicancer | 39 (3.2) | 0.21 | Floortje Mols | 18 (1.5) | <0.01 |
| 4 | Netherlands | 124 (10.1) | 0.02 | Udice, French Research Universities | 36 (2.9) | 0.05 | Asif Johar | 17 (1.4) | 0.01 |
| 5 | Germany | 104 (8.5) | 0.13 | University of Bristol | 33 (2.7) | 0.05 | Hermann Brenner | 15 (1.2) | 0.01 |
| 6 | Japan | 92 (7.5) | 0.04 | Tilburg University | 31 (2.5) | 0.01 | Martijn J L Bours | 13 (1.1) | 0.01 |
| 7 | South Korea | 84 (6.9) | 0.04 | Maastricht University | 28 (2.3) | <0.01 | Matty P Weijenberg | 11 (0.9) | <0.01 |
| 8 | France | 75 (6.1) | 0.05 | Amsterdam Academic Medical Center | 26 (2.1) | 0.05 | Volker Arndt | 10 (0.8) | <0.01 |
| 9 | Italy | 74 (6.0) | 0.06 | Assistance Publique Hopitaux Paris (APHP) | 26 (2.1) | 0.08 | Franck Bonnetain | 9 (0.7) | <0.01 |
| 10 | Sweden | 65 (5.3) | 0.01 | Karolinska University Hospital | 25 (2.0) | 0.01 | Stephanie O Breukink | 9 (0.7) | <0.01 |
3.3.2. Institution collaboration analysis
The 440 nodes and 2052 links composed the institutional cooperation network map (network density = 0.0212), which showed the number of publications and the degree of collaboration with other institutions for each institution (Fig. 3B). Among the top 10 institutions in terms of output, universities, hospitals, and research centers accounted for 60 %, 20 %, and 20 %, respectively (Table 1). The Karolinska Institute and the University of Amsterdam were the leading institutions in this field (n = 40, 3.3 %), followed by Unicancer (n = 39, 3.2 %) and the French Research Universities (n = 36, 2.9 %). The Unicancer was the most central institution (centrality = 0.21) and served as a bridge for institutional cooperation.
3.3.3. Author collaboration analysis
The author collaboration network consisted of 658 nodes and 1227 links (network density = 0.0057), showing the core authors and their potential collaborators (Fig. 3C). Among the top 10 authors with the highest output (Table 1), Pernilla Lagergren was identified as the most contributing author (n = 22, 1.8 %) in this field, followed by Jane M Blazeby (n = 21, 1.7 %), Floortje Mols (n = 18, 1.5 %) and Asif Johar (n = 17, 1.4 %). Among them, both Pernilla Lagergren and Asif Johar come from the Karolinska Institute in Sweden and collaborate with each other. Many authors tended to form relatively stable cooperative relationships with others, but overall, the cooperation between all authors was still weak (centrality <0.01).
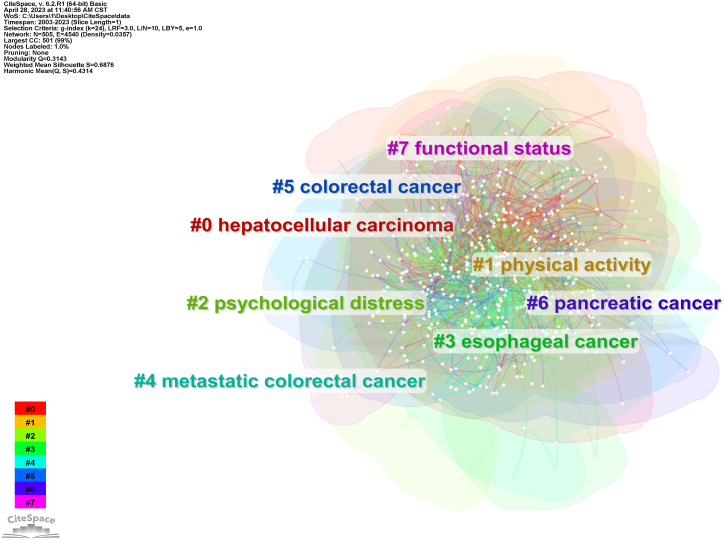
3.4. Keyword co-occurrence analysis
To reflect the research hotspots of research on GI cancer and QoL, the keyword co-occurrence analysis was conducted (Fig. 4). This network consisted of 505 nodes and 4540 links (Q = 0.3143, S = 0.6876), and divided into 8 clusters, including “hepatocellular carcinoma”, “physical activity”, “psychological distress”, “esophageal cancer”, “metastatic colorectal cancer”, “colorectal cancer”, “pancreatic cancer”, and “functional status”. Furthermore, the most frequent keyword in this field was “quality of life” (n = 658), followed by “colorectal cancer” (n = 288), “European organization” (n = 149), “validation” (n = 147) (Table 2). The top-ranked items by centrality were “colorectal cancer” (centrality = 0.11), “carcinoma” (centrality = 0.09), and “functional assessment” (centrality = 0.08).
Fig. 4.
Cluster map of co-occurring of keywords on GI cancer and QoL. Note: Nodes (small white dots) represent the publications included in the analysis. The links between nodes display publications with the same keywords (including synonyms), and their colors are consistent with the colors of keyword clusters.
Table 2.
Top 10 keywords in terms of counts and centrality.
| No. | Keywords | Counts | Keywords | Centrality |
|---|---|---|---|---|
| 1 | Quality of life | 658 | Colorectal cancer | 0.11 |
| 2 | Colorectal cancer | 288 | Carcinoma | 0.09 |
| 3 | European organization | 149 | Functional assessment | 0.08 |
| 4 | Validation | 147 | Survival | 0.07 |
| 5 | Outcm | 137 | Chemotherapy | 0.07 |
| 6 | Surgery | 132 | Health-related quality of life | 0.07 |
| 7 | Survival | 130 | Rectal cancer | 0.07 |
| 8 | Chemotherapy | 130 | Colon cancer | 0.07 |
| 9 | Health-related quality of life | 130 | European organization | 0.06 |
| 10 | Survivors | 124 | validation | 0.06 |
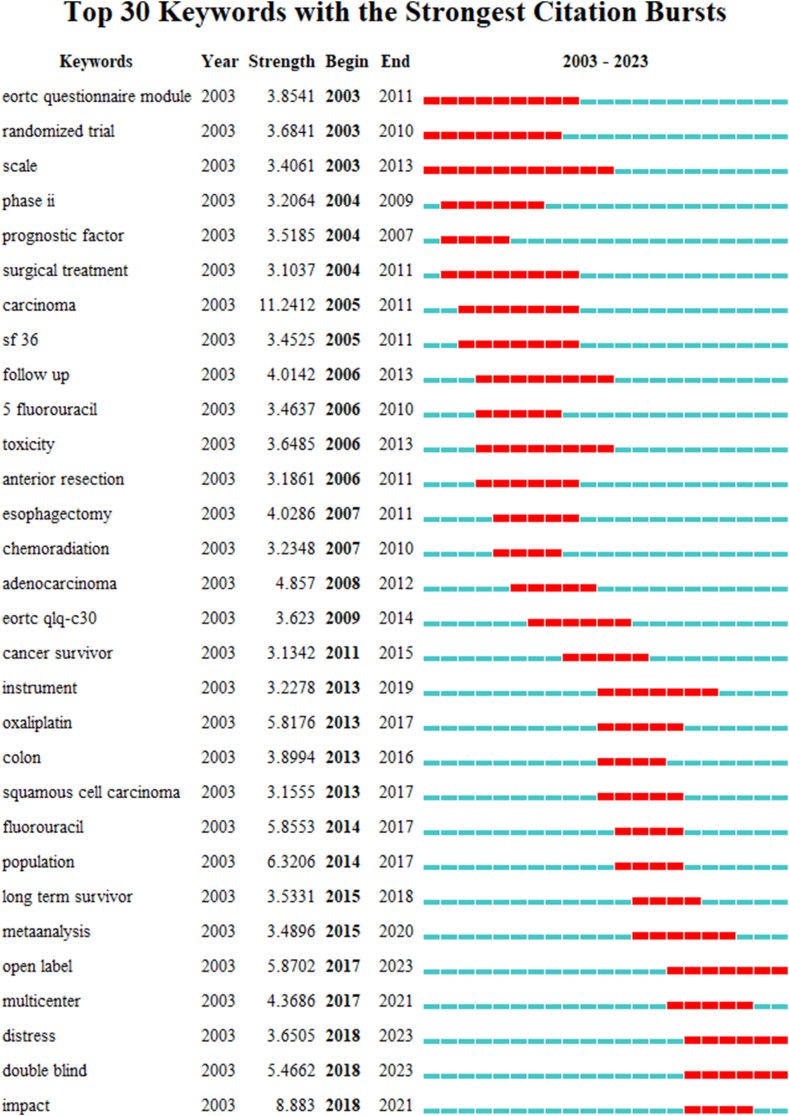
3.5. Burst keyword analysis
Burst keyword analysis showed the frontiers and trends of a field by revealing significant changes in keywords. This study listed the top 30 keywords with the highest citation burst intensity (strength >3.1) (Fig. 5). “Carcinoma” was the keyword with the strongest burst (strength = 11.2412), followed by “impact” (strength = 8.883), and “population” (strength = 6.3206). Besides, “scale” was the keyword with the longest duration of burst, lasting for 10 years. The keywords “open-label”, “distress”, and “double-blind” have been bursting until 2023, and may also be hot topics for future research.
Fig. 5.
Top 30 keywords with the strongest citation bursts from 2003 to 2023. Note: “Strength” represents the citation bursts intensity of the keyword, the higher the value, the higher the frequency of the keyword appearing during this period. The blue short line represents the citation time of the keyword, marking it in red indicates that the keyword is in the active period of strongest citation bursts.
3.6. Co-citation timeline analysis
Timeline analysis of reference co-citation not only unmasked the changing trends and development in research priorities, but also revealed the core paper that plays a crucial role in a field (Fig. S1). The clustering was relatively concentrated (Q = 0.8099, S = 0.9262). The largest cluster mainly included #0 colorectal cancer, #1 gastric cancer, #2 gastrectomy, #3 prognosis, and #4 esophagectomy. It was evident that #1 gastric cancer and #2 gastrectomy mainly occurred between 2015 and 2022, indicating that these clusters were the most focused directions for research on GI cancer and QoL in the near future.
In addition, the top 10 representative references were listed by title, lead author, journal, and year of publication to reveal the knowledge structure of the research field (Table 3). Among them, 80 % were published in Q1, and the paper ranked first had the highest IF (IF = 286.130) and the highest citation count (n = 94). The 5th ranked [35] was closely related to other references (centrality = 0.24), revealing that compared to the general population, CRC survivors had lower physical QoL scores, slightly higher psychological QoL scores, and there was a significant negative association between QoL and the risk of death. The other 9 references included a status report on the global cancer burden using GLOBOCAN estimates (n = 2) [36,37], questionnaire development/validation (n = 2) [38,39], review article (n = 2) [40,41], longitudinal study (n = 2) [42,43], and treatment guideline (n = 1) [44].
Table 3.
The top 10 cited references on GI cancer and QoL.
| No. | Count | Centrality | Title | Author | Journal | Published year |
|---|---|---|---|---|---|---|
| 1 | 94 | 0.05 | Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. | Bray F et al. | CA Cancer J Clin | 2018 |
| 2 | 27 | 0.14 | Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. | Ferlay J et al. | Int J Cancer | 2015 |
| 3 | 21 | 0.12 | Development of an EORTC disease-specific quality of life questionnaire for use in patients with liver metastases from colorectal cancer. | Kavadas V et al. | Eur J Cancer | 2003 |
| 4 | 18 | <0.01 | Japanese gastric cancer treatment guidelines 2018 (5th edition) | Japanese Gastric Cancer Association | Gastric Cancer | 2021 |
| 5 | 16 | 0.24 | Quality of life and mortality of long-term colorectal cancer survivors in the seattle colorectal cancer family registry | Scott V Adams et al. | PLoS One | 2016 |
| 6 | 16 | 0.04 | Candidate predictors of health-related quality of life of colorectal cancer survivors: a systematic review | Martijn J L Bours et al. | Oncologist | 2016 |
| 7 | 16 | 0.07 | Quality of life among long-term (≥5 years) colorectal cancer survivors--systematic review. | Jansen L et al. | Eur J Cancer | 2010 |
| 8 | 16 | 0.02 | Prospective evaluation of quality of life in patients with localized esophageal cancer treated by multimodality therapy or surgery alone. | Reynolds JV et al. | Br J Surg | 2006 |
| 9 | 15 | 0.05 | Health-related quality of life during neoadjuvant treatment and surgery for localized esophageal carcinoma. | Blazeby JM et al. | Cancer | 2005 |
| 10 | 15 | 0.04 | Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. | Johannes M Giesinger et al. | J Clin Epidemiol | 2016 |
4. Discussion
As far as we know, this is the first paper that used CiteSpace software to conduct bibliometric analysis on GI cancer and QoL to reveal its research status, hotspots, and research trends. In addition to being richer in color and style than the graph exported by VOSviewer, CiteSpace also has strong operability, including extracting information to generate clustering labels based on log-likelihood rate (LLR), latent semantic indexing (LSI), and mutual information (MI) algorithms, merging nodes, and adjusting the size of fonts and nodes [32,33]. This study found that the field of GI cancer and QoL is a constantly updated and iterative topic, and a multi-disciplinary research field highly concerned by the community. The number of publications was gradually increasing, while the cooperation was scattered. In addition, the research hotspots in this field can be summarized into the effect of physical activity (PA) on QoL, the status and influencing factors of psychological distress and its relationship with QoL, and the development and validation of measurement tools. Multi-center, open-label/double-blind trials on the exploration of better treatment programs among GI cancer survivors, and longitudinal studies on the complex interaction between psychological distress and QoL may be the emerging trends of research.
4.1. General information
In the past 20 years, a total of 1224 publications on GI cancer and QoL were published by 658 authors from 440 institutions in 65 countries, co-citing 934 references from 681 journals. Most of the top 10 prolific journals are from the United States (n = 4) and England (n = 4), and 60 % of the top 10 institutions and authors were from the Netherlands (n = 4) and Sweden (n = 2). The cooperative relationships between counties/regions, institutions, and authors were relatively scattered. Based on this, it can be found that developed countries are still in a leading position in this field, and developing countries should strengthen cooperation with them. More cooperation is also needed between countries, authors, and institutions.
4.2. Research hotspots
Survivors of liver cancer, CRC, esophageal cancer, and pancreatic cancer after surgery or during chemotherapy were the main research subjects in the field of GI cancer and QoL. Taking the clusters of keywords co-occurrence, as well as the frequency and centrality of keywords into account, the research hotspots in this field were summarized as follows. Firstly, physical activity was a hot topic when exploring the effect of behavior changes on QoL for GI cancer survivors [23,45,46]. Moderate to intense PA has been demonstrated to be beneficial in improving the QoL of GI cancer survivors [47,48], but the health benefits of light PA were still uncertain. Studies have found that light PA has a beneficial effect on the QoL of CRC survivors, especially women with multiple comorbidities [49], and that greater amounts of low PA may significantly increase both physical and mental health scores [50]. While others have shown no correlation between light PA and any dimensions of QoL [47,51]. Among the four studies, only one study [47] was conducted among breast cancer and CRC survivors aged over 18, and the rest [[49], [50], [51]] were conducted among long-term elderly CRC survivors. The identification criteria for light PA and differences in medical technology levels between countries and different periods may be the reasons for the discrepancy. It is necessary to establish an international standard for the intensity of PA among cancer survivors, in order to achieve comparability between experiments and lay the foundation for future multi-center, large-scale study. What's more, exercise interventions on the QoL for GI cancer survivors have also attracted researchers' interest. Aerobic exercise, resistance exercise, and strengthening exercise, each or the combination of which were common exercise interventions, have been proven to improve fatigue, functional status, and QoL [52,53]. The underlying pathways may include enhancing QoL via modulating circadian rhythms [54] and improving sleep quality [55] and self-efficacy [56] in GI cancer survivors.
Distress, especially psychological distress, was another popular research topic. On the one hand, psychological distress was regarded as an outcome indicator like QoL. A study demonstrated that 36 % of I ∼ III CRC survivors experienced moderate to high levels of psychological distress, and after a 2-year follow-up, 13 % of survivors still reported low QoL or high levels of psychological distress [57]. Besides, women, survivors with lower education levels, and symptoms of fatigue, sleep disorders, and pain were more likely to suffer from high levels of psychological distress [57,58], thus it is necessary to strengthen the health education [59] and lifestyle interventions [46,60] for them. On the other hand, the association between psychological distress and QoL was also a hot research direction. Although a bunch of cross-sectional studies provided clues to the negative correlation between psychological distress and QoL [[61], [62], [63]], only a few longitudinal studies have provided evidence for the effect of psychological distress on QoL [64,65]. In the future, more high-quality, multicenter longitudinal studies are needed to explore the trajectory of psychological distress and QoL among GI cancer survivors during their survival period, as well as the effectiveness of psychological intervention at special time points (e.g., newly diagnosed, before and after surgery/chemoradiotherapy), so as to determine the optimal intervention timing and programs.
Testing the validity and reliability of scales is the third research hotspot. It was mainly divided into two aspects: the translation and validation of questionnaires developed by the European Organization for Cancer Research and Treatment (e.g., QLQ-PAN26, QLQ-C30, QLQ-CR29, and QLQ-OG 25) [8,10], and the development and validation of more targeted modules or scales [66,67]. With the continuous progress of medical technology and the deepening of research on survivors’ symptom burden, some unique symptoms may not be properly evaluated using existing universal or specific scales. Future research should choose the most suitable measurement tool based on the characteristics of the research subject, and develop more detailed tools.
4.3. Research frontiers
Analysis of burst keywords and keywords timeline map of reference co-citation revealed the development process and frontiers in the field of GI cancer and QoL. Before 2010, the study of GI cancer and QoL was at the beginning stage, focusing on exploring the effects of treatment methods (e.g., surgical treatment, chemotherapy protocol, and radiotherapy regimen) on QoL and the status of survivors’ QoL. Since 2010, researchers placed greater emphasis on the influencing factors and interventions for the QoL of GI cancer survivors, especially in terms of psychology and lifestyle [17,68]. More importantly, the burst time of keywords including “open-label”, “distress”, and “double-blind” continued until 2023, and may be ongoing in the future. “Open-label” and “double-blind” are two different research designs in clinical trials, in the past five years, the former has mainly focused on verifying the feasibility of treatment, including the effectiveness of chemotherapy regimens [69] and other treatment interventions [70,71], as well as the efficacy of surgical programs [72], while the latter has mostly been used for more subjective outcome indicators (e.g., pain and fatigue) [73,74] and clinical trials related to the efficacy and safety of new drugs [75,76]. It indicated that exploring better treatment intervention programs and developing more targeted new drugs or more effective drug combinations were considered to be emerging trends in this field. In addition, there is a complex interaction between psychological distress and QoL, and the direction of their causal relationship is still unclear. Psychological distress is an important predictor of QoL [64], which in turn significantly affects the psychological management of survivors [61]. In the future, well-designed multi-center longitudinal studies are needed to explore the dose-response relationship between psychological distress and the QoL of GI cancer survivors at different time points, as well as the levels and differences of different types of cancer.
4.4. Strengths and limitations
To our knowledge, this is the first bibliometric analysis to evaluate the characteristics and trends of literature related to GI cancer and QoL based on WoSCC. This study mapped the current status in terms of journals, country, authors, institution, keywords, and references, providing a one-stop overview for scholars in this field. The time span of the data is wide, covering 20 years of research in this field, which increases the comprehensiveness of this study. However, the limitations of this study should also be considered. Firstly, only English publications from the WoSCC database were extracted for bibliometric analysis, which may lead to research bias and incomplete data in the published literature. While considering the different properties of different databases, converting data formats to merge papers from multiple databases may affect the accuracy of the results, and the WoSCC database contains the world's most prestigious and influential academic journals, making it the most representative database. Secondly, only publications from April 1, 2003 to March 31, 2023 were retrieved, and recent publications may be underestimated. However, it is almost impossible to include all relevant literature in the analysis, and we believe that existing findings can effectively represent the global status of this field.
5. Conclusion
To sum up, the present study conducted a qualitative and quantitative bibliometric analysis of publications related to GI cancer and QoL published from 2003 to 2023, and summarized research hotspots including the benefits of PA on QoL, the status, changing trajectory, and interventions of psychological distress, the relationship between psychological distress and QoL, and the development and validation of QoL measurement tools. In addition, prospective open-label trials or randomized double-blind trials targeting the exploration of better treatment interventions and more targeted new drugs or more effective drug combinations, as well as the complex interaction between psychological distress and QoL in different types of cancer may be the research trends in this field. It is recommended that strengthening cooperation between authors, institutions, and countries to further prosper this field.
Data availability statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This research was funded by the Natural Science Foundation of Shaanxi Province (No.: 2023-YBSF-027).
CRediT authorship contribution statement
Xiaoqin Wang: Writing – review & editing, Conceptualization. Caihua Wang: Writing – original draft, Conceptualization. Wenjin Han: Software, Data curation. Jiaru Sun: Software, Methodology. Zhaozhao Hui: Writing – review & editing. Shuangyan Lei: Software, Formal analysis. Huili Wu: Software, Formal analysis. Xiaohong Liu: Writing – review & editing, Conceptualization.
Declaration of competing interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:Xiaoqin Wang reports financial support was provided by Natural Science Foundation of Shaanxi Province (No.: 2023-YBSF-027). If there are other authors, they declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
Not applicable.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e23377.
List of abbreviations
- GI
gastrointestinal
- QoL
quality of life
- PA
physical activity
- CRC
colorectal cancer
- WoSCC
Web of Science Core Collection
- Q
modularity Q value
- S
weighted mean silhouette value
- IF
impact factors
No additional information is available for this paper.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Sung H., et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Cao W., et al. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin. Med. J. 2021;134(7):783–791. doi: 10.1097/CM9.0000000000001474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen Q., et al. Primary tumor resection improves survival of gastrointestinal neuroendocrine carcinoma patients with nonresected liver metastases. J. Surg. Oncol. 2023;127(6):945–955. doi: 10.1002/jso.27213. [DOI] [PubMed] [Google Scholar]
- 4.Hashemzadeh A., et al. When metal-organic framework mediated smart drug delivery meets gastrointestinal cancers. J. Mater. Chem. B. 2021;9(19):3967–3982. doi: 10.1039/d1tb00155h. [DOI] [PubMed] [Google Scholar]
- 5.Siegel R.L., et al. Cancer statistics, 2023. CA A Cancer J. Clin. 2023;73(1):17–48. doi: 10.3322/caac.21763. [DOI] [PubMed] [Google Scholar]
- 6.Shin J., et al. Exploring socio-demographic, physical, psychological, and quality of life-related factors related with fear of cancer recurrence in stomach cancer survivors: a cross-sectional study. BMC Cancer. 2022;22(1):414. doi: 10.1186/s12885-022-09507-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Emery J., et al. Management of common clinical problems experienced by survivors of cancer. Lancet. 2022;399(10334):1537–1550. doi: 10.1016/S0140-6736(22)00242-2. [DOI] [PubMed] [Google Scholar]
- 8.Akduran F., Durna Z. Turkish validation and reliability of the EORTC QLQ-CR29 quality of life scale for colorectal cancer. Turk. J. Gastroenterol. 2021;32(4):357–364. doi: 10.5152/tjg.2021.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fujita T., et al. Translation, validation of the EORTC esophageal cancer quality-of-life questionnaire for Japanese with esophageal squamous cell carcinoma: analysis in thoraco-laparoscopic esophagectomy versus open esophagectomy. Jpn. J. Clin. Oncol. 2016;46(7):615–621. doi: 10.1093/jjco/hyw040. [DOI] [PubMed] [Google Scholar]
- 10.Wagh M.S., et al. Validation of Malayalam translation of the European organization for the research and treatment of cancer quality of life instrument OG25 for esophagogastric junction cancers. Indian J. Palliat. Care. 2020;26(3):295–301. doi: 10.4103/IJPC.IJPC_135_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bunkon S., et al. A model of factors influencing health-related quality of life among Thais with colorectal cancer and a permanent colostomy. Pacific Rim Int. J. Nursing Research. 2023;27(1):185–199. [Google Scholar]
- 12.Fu L., et al. Symptom clusters and quality of life in gastric cancer patients receiving chemotherapy. J. Pain Symptom Manag. 2022;63(2):230–243. doi: 10.1016/j.jpainsymman.2021.09.003. [DOI] [PubMed] [Google Scholar]
- 13.Chen N.Y., et al. The impact of symptom distress on health-related quality of life in liver cancer patients receiving arterial chemoembolization: the mediating role of hope. BMC Gastroenterol. 2022;22(1) doi: 10.1186/s12876-022-02529-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sheikh-Wu S.F., et al. Positive psychology mediates the relationship between symptom frequency and quality of life among colorectal cancer survivors during acute cancer survivorship. Eur. J. Oncol. Nurs. 2022;58 doi: 10.1016/j.ejon.2022.102136. [DOI] [PubMed] [Google Scholar]
- 15.Silva K.D., et al. Time after ostomy surgery and type of treatment are associated with quality of life changes in colorectal cancer patients with colostomy. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0239201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Cutsem E., et al. Tislelizumab versus chemotherapy as second-line treatment of advanced or metastatic esophageal squamous cell carcinoma (RATIONALE 302): impact on health-related quality of life. Esmo Open. 2022;7(4) doi: 10.1016/j.esmoop.2022.100517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ho M., et al. Effects of dietary and physical activity interventions on generic and cancer-specific health-related quality of life, anxiety, and depression in colorectal cancer survivors: a randomized controlled trial. J. Cancer Survivorship. 2020;14(4):424–433. doi: 10.1007/s11764-020-00864-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gao J., et al. Influence of early predictive nursing on complications and quality of life in patients after colorectal cancer surgery. Evid. base Compl. Alternative Med. 2022:2022. doi: 10.1155/2022/8410664. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 19.Cloyd J.M., et al. Patient experience and quality of life during neoadjuvant therapy for pancreatic cancer: a systematic review and study protocol. Support. Care Cancer. 2021;29(6):3009–3016. doi: 10.1007/s00520-020-05813-2. [DOI] [PubMed] [Google Scholar]
- 20.You L., et al. Partial pancreatic tail preserving subtotal pancreatectomy for pancreatic cancer: improving glycemic control and quality of life without compromising oncological outcomes. World J. Gastrointest. Surg. 2020;12(12) doi: 10.4240/wjgs.v12.i12.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Molenaar C.J.L., et al. Prehabilitation versus no prehabilitation to improve functional capacity, reduce postoperative complications and improve quality of life in colorectal cancer surgery. Cochrane Database Syst. Rev. 2022;(5) doi: 10.1002/14651858.CD013259.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Machado P., et al. Effect of exercise training on quality of life after colorectal and lung cancer surgery: a meta-analysis. Cancers. 2021;13(19) doi: 10.3390/cancers13194975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Balhareth A., Aldossary M.Y., McNamara D. Impact of physical activity and diet on colorectal cancer survivors' quality of life: a systematic review. World J. Surg. Oncol. 2019;17(1) doi: 10.1186/s12957-019-1697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toms C., et al. Quality of life instruments and trajectories after pancreatic cancer resection A systematic review. Pancreas. 2021;50(8):1137–1153. doi: 10.1097/MPA.0000000000001896. [DOI] [PubMed] [Google Scholar]
- 25.Rowsell A., et al. Systematic review of health-related quality of life (HRQoL) issues associated with gastric cancer: capturing cross-cultural differences. Gastric Cancer. 2022;25(4):665–677. doi: 10.1007/s10120-022-01309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Norman E.M.L., Weil J., Philip J. Hepatocellular carcinoma and its impact on quality of life: a review of the qualitative literature. Eur. J. Cancer Care. 2022;31(6) doi: 10.1111/ecc.13672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rupp S.K., Stengel A. Influencing factors and effects of treatment on quality of life in patients with gastric cancer-A systematic review. Front. Psychiatr. 2021;12 doi: 10.3389/fpsyt.2021.656929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sritan S. Factors contributing to the quality of life among Thai patients diagnosed with colorectal cancer with a stoma: an integrative review. J. Adv. Nurs. 2023;79(1):1–14. doi: 10.1111/jan.15460. [DOI] [PubMed] [Google Scholar]
- 29.Zou H.M., et al. Economic burden and quality of life of hepatocellular carcinoma in greater China: a systematic review. Front. Public Health. 2022;10 doi: 10.3389/fpubh.2022.801981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Donthu N., et al. How to conduct a bibliometric analysis: an overview and guidelines. J. Bus. Res. 2021;133:285–296. [Google Scholar]
- 31.Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc. Natl. Acad. Sci. U. S. A. 2004;101(Suppl 1):5303–5310. doi: 10.1073/pnas.0307513100. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Synnestvedt M.B., Chen C., Holmes J.H. CiteSpace II: visualization and knowledge discovery in bibliographic databases. AMIA Annu. Symp. Proc. 2005;2005:724–728. [PMC free article] [PubMed] [Google Scholar]
- 33.Wu H., et al. Knowledge structure and emerging trends on osteonecrosis of the femoral head: a bibliometric and visualized study. J. Orthop. Surg. Res. 2022;17(1):194. doi: 10.1186/s13018-022-03068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabé M., et al. A century of research on neuromodulation interventions: a scientometric analysis of trends and knowledge maps. Neurosci. Biobehav. Rev. 2023;152 doi: 10.1016/j.neubiorev.2023.105300. [DOI] [PubMed] [Google Scholar]
- 35.Adams S.V., Ceballos R., Newcomb P.A. Quality of life and mortality of long-term colorectal cancer survivors in the Seattle colorectal cancer family registry. PLoS One. 2016;11(6) doi: 10.1371/journal.pone.0156534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bray F., et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA A Cancer J. Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 37.Ferlay J., et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136(5):E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 38.Kavadas V., et al. Development of an EORTC disease-specific quality of life questionnaire for use in patients with liver metastases from colorectal cancer. Eur. J. Cancer. 2003;39(9):1259–1263. doi: 10.1016/s0959-8049(03)00236-3. [DOI] [PubMed] [Google Scholar]
- 39.Giesinger J.M., et al. Replication and validation of higher order models demonstrated that a summary score for the EORTC QLQ-C30 is robust. J. Clin. Epidemiol. 2016;69:79–88. doi: 10.1016/j.jclinepi.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 40.Bours M.J., et al. Candidate predictors of health-related quality of life of colorectal cancer survivors: a systematic review. Oncol. 2016;21(4):433–452. doi: 10.1634/theoncologist.2015-0258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jansen L., et al. Quality of life among long-term (≥5 years) colorectal cancer survivors--systematic review. Eur. J. Cancer. 2010;46(16):2879–2888. doi: 10.1016/j.ejca.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 42.Reynolds J.V., et al. Prospective evaluation of quality of life in patients with localized oesophageal cancer treated by multimodality therapy or surgery alone. Br. J. Surg. 2006;93(9):1084–1090. doi: 10.1002/bjs.5373. [DOI] [PubMed] [Google Scholar]
- 43.Blazeby J.M., et al. Health-related quality of life during neoadjuvant treatment and surgery for localized esophageal carcinoma. Cancer. 2005;103(9):1791–1799. doi: 10.1002/cncr.20980. [DOI] [PubMed] [Google Scholar]
- 44.Japanese gastric cancer treatment guidelines 2018 (5th edition) Gastric Cancer. 2021;24(1):1–21. doi: 10.1007/s10120-020-01042-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bezerra K.H.D., et al. Physical exercise and quality of life of patients diagnosed with colorectal cancer: systematic literature review. J. Gastrointest. Cancer. 2021;52(1):17–22. doi: 10.1007/s12029-020-00506-9. [DOI] [PubMed] [Google Scholar]
- 46.Eyl-Armbruster R.E., et al. Change toward healthier lifestyles is associated with better health-related quality of life in long-term colorectal cancer survivors. J. Natl. Compr. Cancer Netw. 2022;20(11):1233–+. doi: 10.6004/jnccn.2022.7049. [DOI] [PubMed] [Google Scholar]
- 47.Park J.H., et al. Moderate to vigorous physical activity participation associated with better quality of life among breast and colorectal cancer survivors in Korea. BMC Cancer. 2020;20(1) doi: 10.1186/s12885-020-06819-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kenkhuis M.F., et al. Longitudinal associations of sedentary behavior and physical activity with quality of life in colorectal cancer survivors. Med. Sci. Sports Exerc. 2021;53(11):2298–2308. doi: 10.1249/MSS.0000000000002703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.van Roekel E.H., et al. Light physical activity is associated with quality of life after colorectal cancer. Med. Sci. Sports Exerc. 2015;47(12):2493–2503. doi: 10.1249/MSS.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 50.Thraen-Borowski K.M., et al. Dose-response relationships between physical activity, social participation, and health-related quality of life in colorectal cancer survivors. J. Cancer Survivorship. 2013;7(3):369–378. doi: 10.1007/s11764-013-0277-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Johnson B.L., et al. Physical activity and function in older, long-term colorectal cancer survivors. Cancer Causes Control. 2009;20(5):775–784. doi: 10.1007/s10552-008-9292-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Simonsen C., et al. Effects of high-intensity exercise training on physical fitness, quality of life and treatment outcomes after oesophagectomy for cancer of the gastro-oesophageal junction:PRESETpilot study. Bjs Open. 2020;4(5):855–864. doi: 10.1002/bjs5.50337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Weyhe D., et al. Effects of intensive physiotherapy on Quality of Life (QoL) after pancreatic cancer resection: a randomized controlled trial. BMC Cancer. 2022;22(1) doi: 10.1186/s12885-022-09586-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Su C.C., et al. Circadian rhythm mediates the relationship between physical activity and quality of life in younger and older cancer survivors. Chronobiol. Int. 2015;32(10):1417–1426. doi: 10.3109/07420528.2015.1102150. [DOI] [PubMed] [Google Scholar]
- 55.Tan S.L., et al. Understanding the positive associations of sleep, physical activity, fruit and vegetable intake as predictors of quality of life and subjective health across age groups: a theory based, cross-sectional web-based study. Front. Psychol. 2018;9:977. doi: 10.3389/fpsyg.2018.00977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Phillips S.M., McAuley E. Physical activity and quality of life in breast cancer survivors: the role of self-efficacy and health status. Psycho Oncol. 2014;23(1):27–34. doi: 10.1002/pon.3366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Qaderi S.M., et al. Trajectories of health-related quality of life and psychological distress in patients with colorectal cancer: a population-based study. Eur. J. Cancer. 2021;158:144–155. doi: 10.1016/j.ejca.2021.08.050. [DOI] [PubMed] [Google Scholar]
- 58.Carbajal-Lopez E.B., et al. Psychological distress, fatigue and quality of life in patients with gastrointestinal stromal tumors. Psychology in Russia-State of the Art. 2022;15(2):3–13. doi: 10.11621/pir.2022.0201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gao Q.A., et al. Effectiveness of a comprehensive post-operative health education program in improving quality of life after gastric cancer surgery. Ann. Palliat. Med. 2020;9(3):921–926. doi: 10.21037/apm.2020.04.14. [DOI] [PubMed] [Google Scholar]
- 60.Cheng C., et al. Development and feasibility of a mobile health-supported comprehensive intervention model (CIMmH) for improving the quality of life of patients with esophageal cancer after esophagectomy: prospective, single-arm, nonrandomized pilot study. J. Med. Internet Res. 2020;22(8) doi: 10.2196/18946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ohkura Y., et al. Relationship between psychological distress and health-related quality of life at each point of the treatment of esophageal cancer. Esophagus. 2020;17(3):312–322. doi: 10.1007/s10388-019-00710-y. [DOI] [PubMed] [Google Scholar]
- 62.Abu Sharour L., et al. Health-related quality of life among patients with colorectal cancer. J. Res. Nurs. 2020;25(2):114–125. doi: 10.1177/1744987119846177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu Y., Zhang Y., Zou L.L. Effects of anxiety, depression, and fatigue on quality of life in early esophageal cancer patients following endoscopic submucosal dissection. Ann. Palliat. Med. 2020;9(6):3766–3775. doi: 10.21037/apm-20-1632. [DOI] [PubMed] [Google Scholar]
- 64.Liu Y.J., et al. Psychological distress and health-related quality of life up to 2 years after oesophageal cancer surgery: nationwide population-based study. Bjs Open. 2021;5(1) doi: 10.1093/bjsopen/zraa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shim E.J., et al. Network analyses of associations between cancer-related physical and psychological symptoms and quality of life in gastric cancer patients. Psycho Oncol. 2021;30(6):946–953. doi: 10.1002/pon.5681. [DOI] [PubMed] [Google Scholar]
- 66.Eom B.W., et al. Development and validation of a symptom-focused quality of life questionnaire (KOQUSS-40) for gastric cancer patients after gastrectomy. Cancer Research and Treatment. 2021;53(3):763–772. doi: 10.4143/crt.2020.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ramage J.K., et al. Development of a quality of life questionnaire for patients with pancreatic neuroendocrine tumours (the PANNET module) J. Neuroendocrinol. 2022;34(4) doi: 10.1111/jne.13097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wang X., et al. Personalized nutrition intervention improves nutritional status and quality of life of colorectal cancer survivors in the community: a randomized controlled trial. Nutrition. 2022:103–104. doi: 10.1016/j.nut.2022.111835. [DOI] [PubMed] [Google Scholar]
- 69.Hall P.S., et al. Efficacy of reduced-intensity chemotherapy with oxaliplatin and capecitabine on quality of life and cancer control among older and frail patients with advanced gastroesophageal cancer the GO2 phase 3 randomized clinical trial. JAMA Oncol. 2021;7(6):869–877. doi: 10.1001/jamaoncol.2021.0848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhu Y.J., et al. Acupuncture for quality of life in gastric cancer patients undergoing adjuvant chemotherapy. J. Pain Symptom Manag. 2022;63(2):210–220. doi: 10.1016/j.jpainsymman.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Keeler B.D., et al. The impact of pre-operative intravenous iron on quality of life after colorectal cancer surgery: outcomes from the intravenous iron in colorectal cancer-associated anaemia (IVICA) trial. Anaesthesia. 2019;74(6):714–725. doi: 10.1111/anae.14659. [DOI] [PubMed] [Google Scholar]
- 72.Wang J., et al. Effect of different oesophagojejunostomy methods on the quality of life of gastric cancer patients after totally laparoscopic total gastrectomy with self-pulling and latter transected technique: study protocol for a randomised trial. BMJ Open. 2022;12(4) doi: 10.1136/bmjopen-2021-058844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dong D.S., et al. Neurolytic splanchnic nerve block and pain relief, survival, and quality of life in unresectable pancreatic cancer: a randomized controlled trial. Anesthesiology. 2021;135(4):686–698. doi: 10.1097/ALN.0000000000003936. [DOI] [PubMed] [Google Scholar]
- 74.Schottker B., et al. Protocol of the VICTORIA study: personalized vitamin D supplementation for reducing or preventing fatigue and enhancing quality of life of patients with colorectal tumor - randomized intervention trial. BMC Cancer. 2020;20(1) doi: 10.1186/s12885-020-07219-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Andre T., et al. Health-related quality of life in patients with microsatellite instability-high or mismatch repair deficient metastatic colorectal cancer treated with first-line pembrolizumab versus chemotherapy (KEYNOTE-177): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22(5):665–677. doi: 10.1016/S1470-2045(21)00064-4. [DOI] [PubMed] [Google Scholar]
- 76.Kopetz S., et al. Quality of life with encorafenib plus cetuximab with or without binimetinib treatment in patients with BRAF V600E-mutant metastatic colorectal cancer: patient-reported outcomes from BEACON CRC. Esmo Open. 2022;7(3) doi: 10.1016/j.esmoop.2022.100477. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.