Abstract
Purpose
The World Health Organization-Five Well-Being Index (WHO-5) is widely used to assess subjective well-being. Nevertheless, measurement invariance and optimal cutoff point of the WHO-5 have not been examined in Chinese samples. We aimed to assess measurement properties of the Chinese version of the WHO-5 (WHO-5-C) among healthcare students.
Patients and Methods
A two-wave longitudinal assessment was conducted among 343 Chinese healthcare students from September to November 2022. Measurement properties of the WHO-5-C were assessed through structural validity using confirmatory factor analysis (CFA), measurement invariance using multigroup CFA (MGCFA) and longitudinal CFA (LCFA), convergent validity using correlation analysis with the Self-Rated Health Questionnaire (SRHQ) and Patient Health Questionnaire-4 (PHQ-4), reliability using internal consistency and test–retest reliability, and optimal cutoff point using receiver operating characteristic (ROC) analysis.
Results
The WHO-5-C demonstrated satisfactory structural validity with comparative fit index (CFI) of 0.968 at baseline and 0.980 at follow-up, and adequate measurement invariance in different sociodemographic variables at baseline (gender, age, major, home location, being only child, monthly household income, part-time job, physical exercise, hobby, frequency of visiting home, and stress coping strategy) (CFI changes [ΔCFI] = −0.009–0.003) and over a week (ΔCFI = −0.006–0.000). The WHO-5-C also had good internal consistency (Cronbach’s α = 0.907–0.934; McDonald’s ω = 0.908–0.935) and test–retest reliability (intraclass correlation coefficient [ICC] = 0.803). Convergent validity was supported by moderate correlations of the WHO-5-C with the SRHQ and PHQ-4. The optimal cutoff point of the WHO-5-C was found to be 50, with an area under the ROC curve of 0.882 at baseline data, with sensitivity of 0.803 and specificity of 0.762 at follow-up.
Conclusion
The WHO-5-C demonstrated adequate measurement properties, especially concerning cross-sectional and longitudinal measurement invariance, with a recommended optimal cutoff point of ≥ 50 for assessing adequate level of psychological well-being in healthcare students.
Keywords: WHO-5 Well-Being Index, subjective well-being, measurement properties, diagnostic performance, observational longitudinal design, healthcare students
Introduction
Subjective well-being (SWB) refers to an individual’s ability to develop their potential, to work productively and creatively, to build strong and positive relationships with others, and to contribute to their community.1 SWB involves multiple dimensions and its contribution to all aspects of human life, eg, optimistic attitude, positive affect, psychological resilience, and happiness.2 Positive SWB is recognized as having crucial consequences for better physical outcomes in both healthy populations and patients suffering from various diseases, such as fewer self-perceived symptoms, fewer pain sensations, and longer survival.3–5 As such, positive SWB has been regarded as a conducive health asset given its explicit associations with salutary outcomes of mental health,6 behaviors,7 and disease progression and rehabilitation.8 Therefore, identifying SWB carries clinical significance for public and psychosomatic health.
There has been increasing evidence showing that college students are exposed to excessive academic pressures that may affect their academic performance, lifestyle, physical health, and even psychosomatic disorders.9–11 Healthcare students are expected to provide professional support in health services for individuals and societies in the future12 and are at risk of physical and mental disorders.13,14 Worldwide, approximately one-third of healthcare students suffer from negative emotions, which is notably higher than general population and non-healthcare students.15,16 A meta-analysis of mental health problems among healthcare students in China showed that the prevalence of depression, anxiety, and suicidal ideation were 29%, 21%, and 11%, respectively, underlining the severity of the issue and urgency to understand their well-being more.17 Therefore, instruments with a positive focus can suggest to respondents that such programs are for individuals with pleased SWB and in this way support, rather than detract from, these initiatives.
There are numerous approaches in explaining and assessing well-being, and several instruments have been developed to monitor well-being.18 To date, the popular instruments for assessing SWB state are mostly symptom-based, eg, stress, anxiety, depression and bipolar disorders.19–21 Existing instruments developed to evaluate well-being are mostly based on a single perspective.18 For instance, one of the most widely used for evaluating SWB is the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS), a 14-item instrument developed to assess hedonic and eudaimonic elements of mental health.22 Despite previous researches have endorsed the WEMWBS presented appropriate capacity for mental well-being in Chinese samples, it does not consider purpose in physical condition which is an essential component of overall well-being.23,24 Likewise, other instruments introduced into China to determine SWB include the Personal Wellbeing Index (PWI),25 Psychological Well-Being Scale (PWBS),26 etc., and most only assess satisfaction level in terms of health-related quality of life. It is necessary to unearth an instrument that can capture a comprehensive conception of SWB, including affective-emotional aspects and physiological feelings.
The positively worded World Health Organization-Five Well-Being Index (WHO-5) is one of the measures from a positive perspective, aiming to measure overall wellness and cover healthy elements psychologically and physically.27 As a multidimensional screening instrument, the WHO-5 initially comprised twenty-eight items and progressively shortened to five positive items to produce a brief and comprehensive scale of well-being.27,28 To date, there are more than thirty official language versions of the WHO-5 that have been endorsed by the World Health Organization (WHO).27 The scale has been adapted and validated across numerous cultures, including Arabic,29 Brazilian,30 Chinese,31 German,32 Icelandic,33 Japanese,34 Malay,35 Polish,36 Portuguese,30 Sinhala,37 Spanish,38 Swahili,39 Swedish,40 and Turkish.41 The original English version of the WHO-5,42 as well as the Japanese34 and Polish36 versions, had a single-factor structure with excellent reliability and validity in adolescents with type 1 diabetes and a cutoff point below 50 was established to identify worsened well-being. Moreover, the WHO-5 has revealed correlations with adverse health conditions among different samples of diverse cultures, including Spanish, Swedish, and Turkish.38,40,41 The WHO-5, overall, has sufficient validity to measure SWB in patients and general populations across study fields, and the scale has been extensively applied in endocrinology, psychiatry, and clinical as well as positive psychology.28,37 Therefore, the WHO-5 demonstrated adequate effectiveness as both an outcome measure in clinical trials and a screening instrument in community settings.
The WHO-5 has been adapted and validated in Chinese university students43 and medical educators.44 Measurement properties of the Chinese version of the WHO-5 (WHO-5-C) were assessed in a recent multi-site study among a sample of university students and reported a stable one-factor structure and adequate internal consistency, factorial validity, construct validity and concurrent validity.43 According to the COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) guideline,45 it would be integral to further ascertain test–retest reliability, measurement invariance, measurement error, and recommended cutoff point of the WHO-5-C, intending to select the most appropriate outcome measurement instruments in research and clinical practice. This study aimed to achieve the goal of validating the WHO-5-C as a screening and monitoring instrument of SWB using data collected from healthcare students. This two-wave longitudinal study specifically assessed structural validity, measurement invariance, convergent validity and reliability; identified the optimal cutoff point by conducting receiver operating characteristic (ROC) analysis; and determined cross-sectional and longitudinal measurement invariance with respect to sociodemographic variables and approximately one-week interval, respectively. We hypothesized that the WHO-5 can serve as both an assessment and a screening instrument for routine monitoring of SWB in Chinese samples.
Materials and Methods
Participants and Procedures
This study was a two-wave longitudinal assessment and a convenience sample from a university in Hangzhou, China, participated in a paper-based survey in simplified Chinese from September to November 2022 upon informed consent. We recruited healthcare students who were enabled to read and write simplified Chinese and had the ability to conduct the response process freely. Respondents were excluded if they: 1) had difficulty understanding or writing Chinese; 2) were on leave or out of school; or 3) disagreed to participate in the study. The self-report paper-and-pencil survey was administered during breaks between classes or evening self-study and required about 10 minutes to complete the questionnaires. The trained investigators were responsible for implementing assessment and ensuring its onsite quality control. All participants were required to complete two-wave longitudinal measurements with an average interval of 7 days + 3 hours, given that 1) the appropriate interval varies from an hour to a year depending on the task, but generally speaking, a retest interval of 2 to 14 days is usual;46 and 2) reproducibility of health status measures intended for longitudinal use may best be measured at intervals of 1 to 2 weeks.47 Respondents were compensated with 2 CNY (1 CNY ≈ 0.150 US dollars) each. The valid questionnaires in this study (N = 343) reached recommended sample size for factor analyses: 1) the sample size of 300 is considered as good;48 2) the appropriate minimum for sample size include from 3 to 20 times the number of variables, and sample size above 200 is suggested when the variables-to-factors is six.49
The current study was conducted in accordance with the Declaration of Helsinki50 and approved by the Institutional Review Board of the School of Public Health, Hangzhou Normal University, China (Reference No. 20210014). All healthcare students freely consented to respond to the questionnaires and provided their informed consents before inclusion into the assessments. The authors confirmed full respect and protection of individual privacy rights before, during, and after the data collection and processing.
Measures
Sociodemographic Variables
We collected sociodemographic variables, including gender (male, female), age, major (clinical medicine, preventive medicine), home location (urban, rural, suburban), being only child (yes, no), monthly household income (< 10,000 CNY, ≥ 10,000 CNY), part-time job (yes, no), physical exercise [exercise goals to improve health (yes, no)], hobby (yes, no), frequency of visiting home [frequently (once per week, twice per week, and once per month); occasionally (once per quarter, once per semester, and once per academic year)], and self-reported preferred stress coping strategy (emotion-focused, solution-focused, avoidance coping).
World Health Organization-Five Well-Being Index (WHO-5)
The WHO-5 developed by the WHO is a brief self-report instrument used to assess SWB. The WHO-5 was translated into simplified Chinese in 2007 and is available on the WHO-5 official website.27,51 Respondents were asked how well each of the five statements applies to them when considering the last two weeks. The five items of the scale cover positive emotions (in good spirits, feeling relaxed), vitality (feeling active, waking up refreshed and rested), and being interested in things.27 Each item was scored on a six-point Likert scale, ranging from 0 (at no time) to 5 (all the time). Multiplying the original score by four is usually recommended because quality-of-life-related scales are often converted to a percentage scale.27,28 The final score from 0 representing the worst imaginable well-being to 100 representing the best imaginable well-being. All items of the WHO-5-C are loaded on a potential factor with adequate reliability (Cronbach’s α = 0.810–0.850, McDonald’s ω = 0.820–0.860) and validity (comparative fit index [CFI] = 0.974, Tucker-Lewis index [TLI] = 0.947, and root mean square error of approximation [RMSEA] = 0.080).43
Patient Health Questionnaire-4 (PHQ-4)
The PHQ was designed to facilitate recognition and diagnosis of the most common mental disorders in primary care patients.52 The PHQ-4 is a validated instrument for detecting anxiety and depression two weeks prior to assessment administration. The PHQ-4 consists of two ultra-short scales, one is the Generalized Anxiety Disorder-2 (GAD-2) for anxiety detection53 and another is the PHQ-2 that reflects depression.54 Each item of the PHQ-4 is scored on a four-point Likert scale, ranging from 0 (not at all) to 3 (nearly every day), with higher scores indicating more severe symptom levels.55,56 The Chinese version of the PHQ-4 (PHQ-4-C) is publicly available and has shown good internal consistency and test–retest reliability (Cronbach’s α = 0.870–0.904, McDonald’s ω = 0.894–0.904, intraclass correlation coefficient [ICC] = 0.697).57,58
Self-Rated Health Questionnaire (SRHQ)
A simple two-item questionnaire was applied to assess the self-perceived health of all participants, with one item estimating their physical health and one assessing their mental health. Each item was rated on a five-point Likert scale, from 1 (excellent) to 5 (extremely poor), with higher scores indicating worse overall health.59,60 The SRHQ was demonstrated to have satisfactory internal consistency and test–retest reliability in our previous studies (Cronbach’s α = 0.706–0.857, ICC = 0.565–0.710).59–61
Statistical Analysis
Data analysis was performed using R (version 4.1.3) and JASP (version 0.16.1). The R packages used in this analysis were “lavvan (0.6–11)”,62 “MBESS (4.9.2)”,63 “irr (0.84.1)”,64 “semTools (0.5–6)”,65 and “pROC (1.18.2)”.66 We matched data according to student ID, and missingness in the present study ranged from 0.29% to 1.46% (< 5%). We used mean imputation for continuous variables and median imputation for categorical variables.67 Means, standard deviations (SDs), skewness, and kurtosis were used to assess multivariate normality. We selected maximum likelihood estimation (MLE) method to evaluate all confirmatory factor analysis (CFA) results given 1) data of the WHO-5-C is nonnormality (skew < 2, kurtosis < 7), and 2) the number of ordered categories is more than five.68 All measurement properties of the WHO-5-C were assessed in accordance with the requirements of the COSMIN guideline.69
Structural Validity
We assessed structural validity of the WHO-5-C by CFA to evaluate the extent to which the scores reflected underlying dimensions. Since the WHO-5 has been widely recognized as a single-factor scale, we evaluated structural validity of the scale based on a single-factor model. A satisfactory model fit was indicated for CFI and TLI ≥ 0.900, RMSEA ≤ 0.080, and standardized root mean square residual (SRMR) ≤ 0.080.70,71
Measurement Invariance
To assess measurement invariance of the WHO-5-C with regard to demographic variables and time, we conducted a series of multi-group CFA (MGCFA) and longitudinal CFA (LCFA). This method involved progressively constraining parameters to be equal between subgroups (sociodemographic variables) and across time intervals, and then comparing changes in fit indices to determine whether the relationship between observed variables and underlying traits was equivalent.72 Herein, a series of nested models with increasing constraints were established, including the configural (same pattern of factors), metric (same pattern of factors and loadings), scalar (same pattern of factors, loadings, and item thresholds), and strict (same pattern of factors, loadings, item thresholds, and residual variances) models. Measurement invariance was defined as the fit statistic not significantly changing in an iterative procedure of progressively strict constraints. We considered the change in CFI (ΔCFI) to be an applicable metric for measurement invariance, with a change ≤ 0.010 indicating an appropriate measurement invariance.73,74
Convergent Validity
To evaluate convergent validity of the WHO-5-C, we calculated Pearson correlation coefficients of the WHO-5-C with the SRHQ and PHQ-4-C, as these instruments are developed to assess an individual’s subjective feelings, considering mental and physical health often influence and accompany each other.75 We additionally analyzed inter-item and item-total correlations. We hypothesized that the WHO-5-C would be moderately correlated with the PHQ-4-C and SRHQ in expected directions, given that these instruments measure interrelated constructs. The absolute magnitude of correlation coefficient was categorized as very strong correlation (r > 0.900), strong correlation (r = 0.700–0.900), moderate correlation (r = 0.400–0.700), and weak correlation (r < 0.400).76
Reliability
We assessed internal consistency of the WHO-5-C using Cronbach’s α and McDonald’s ω coefficients, with coefficient ≥ 0.700 considered satisfactory.77 To measure test–retest reliability, we used ICC between two separate times and coefficient below 0.400, between 0.400 and 0.590, between 0.600 and 0.740, and greater than 0.750 indicating poor, fair, good, and excellent reliability, respectively.78 Moreover, standard error of measurement (SEM) was calculated as additional evidence to determine measurement accuracy when evaluating test–retest reliability.79
Sensitivity and Specificity
To evaluate the WHO-5-C as a screening scale for SWB, area under the ROC curve (AUC), optimal cutoff point, sensitivity, and specificity were calculated using the ROC analysis. As the PHQ-2 was an ultra-brief and useful screening instrument in depression with excellent operating characteristics, the score ≥ 3 is used as a criterion to determine the optimal cutoff point of the WHO-5-C.52 The optimal cutoff point was obtained from the point closest to the top left-hand corner of ROC curve in baseline data and examined in follow-up data. The AUC value ranges from 0.500 to 1.000, with higher value indicating better prediction. A value greater than or equal to 0.800 was regarded as a good discrimination.80,81
Results
Sociodemographic Variables
The sample consisted of 216 females (62.974%) with an average age of 19.650 (SD = 1.414) years, ranging from 17 to 23 years. Tables 1 and S1 summarized the participants’ sociodemographic variables and scores of the measured scales at baseline and follow-up.
Table 1.
Sociodemographic Variables (N = 343)
| Variables | N (%) | Mean (SD) | |
|---|---|---|---|
| Baseline | Follow-Up | ||
| Gender | |||
| Male | 127 (37.026) | 57.732 (17.168) | 57.827 (18.425) |
| Female | 216 (62.974) | 56.741 (17.873) | 58.167 (18.578) |
| Age | |||
| < 20 years | 150 (43.732) | 58.800 (17.264) | 60.773 (17.468) |
| ≥ 20 years | 193 (56.268) | 55.793 (17.785) | 55.917 (19.030) |
| Major | |||
| Clinical medicine | 154 (44.898) | 53.039 (17.232) | 54.883 (19.518) |
| Preventive medicine | 189 (55.102) | 60.423 (17.234) | 60.614 (17.246) |
| Home location | |||
| Urban | 156 (45.481) | 58.179 (17.885) | 59.256 (19.050) |
| Rural | 101 (29.446) | 56.356 (18.401) | 57.188 (17.786) |
| Suburban | 86 (25.073) | 56.047 (16.135) | 56.837 (18.367) |
| Being only child | |||
| Yes | 128 (37.318) | 57.094 (16.864) | 57.531 (19.246) |
| No | 215 (62.682) | 57.116 (18.058) | 58.344 (18.072) |
| Monthly household income | |||
| < 10,000 CNY | 141 (41.108) | 55.489 (18.663) | 57.135 (19.197) |
| ≥ 10,000 CNY | 202 (58.892) | 58.238 (16.767) | 58.673 (18.010) |
| Part-time job | |||
| Yes | 33 (9.621) | 56.364 (17.360) | 57.333 (18.806) |
| No | 310 (90.379) | 57.187 (17.648) | 58.116 (18.491) |
| Physical exercise | |||
| Yes | 257 (74.927) | 58.646 (17.513) | 59.564 (18.532) |
| No | 86 (25.073) | 52.512 (17.134) | 53.488 (17.720) |
| Hobby | |||
| Yes | 244 (71.137) | 58.639 (17.849) | 59.770 (18.492) |
| No | 99 (28.863) | 53.333 (16.443) | 53.778 (17.891) |
| Frequency of visiting home | |||
| Frequently | 51 (14.869) | 63.294 (17.283) | 62.824 (17.386) |
| Occasionally | 292 (85.131) | 56.027 (17.456) | 57.205 (18.584) |
| Stress coping strategy | |||
| Emotion-focused | 189 (55.102) | 58.455 (16.103) | 59.111 (17.952) |
| Solution-focused | 121 (35.277) | 57.983 (18.656) | 59.240 (18.757) |
| Avoidance coping | 33 (9.621) | 45.182 (18.550) | 47.515 (17.798) |
Abbreviations: SD, standard deviation; Mean (SD), mean scores and SDs of the Chinese World Health Organization-Five Well-Being Index.
Structural Validity
Structural validity of the WHO-5-C was explored using CFA based on a one-factor model. As shown in Table 2, the fit indices of both baseline (CFI = 0.968, TLI = 0.937, SRMR = 0.028) and follow-up (CFI = 0.980, TLI = 0.961, SRMR = 0.020) analyses indicated that the WHO-5-C had a satisfactory fit with a single-factor structure.
Table 2.
Model Fit Indices of the Single-Factor Model for the WHO-5-C (N = 343)
| χ2 (df) | P | CFI | TLI | RMSEA (90% CI) | SRMR | |
|---|---|---|---|---|---|---|
| Baseline | 42.372 (5) | < 0.001 | 0.968 | 0.937 | 0.148 (0.109, 0.190) | 0.028 |
| Follow-up | 35.051 (5) | < 0.001 | 0.980 | 0.961 | 0.132 (0.093, 0.175) | 0.020 |
| Threshold | N/A | > 0.050 | ≥ 0.900 | ≥ 0.900 | ≤ 0.080 | ≤ 0.080 |
Abbreviations: WHO-5-C, Chinese World Health Organization-Five Well-Being Index; χ2, chi-square; df, degrees of freedom; CFI, comparative fit index; TLI, Tucker-Lewis index; RMSEA, root mean square error of approximation; CI, confidence interval; SRMR, standardized root mean square residual; N/A, not applicable.
Measurement Invariance
Cross-sectional measurement invariance of the WHO-5-C was analyzed across healthcare students’ sociodemographic variables. Tables 3 and S2 showed that the WHO-5-C was well-fixed in four nested models among all subgroups, with all CFI and TLI values greater than 0.900 and SRMR values below 0.080. Meanwhile, MGCFA tests demonstrated that all ΔCFI values (ΔCFI = −0.009–0.003) were within the recommended range, indicating that the WHO-5-C had acceptable measurement invariance across different sociodemographic variables.
Table 3.
Cross-Sectional Measurement Invariances of the WHO-5-C (N = 343)
| Hypothesis | Baseline | Follow-up | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 (df) | P | Δχ2 (Δdf) | CFI | ΔCFI | TLI | SRMR | χ2 (df) | P | Δχ2 (Δdf) | CFI | ΔCFI | TLI | SRMR | |
| Gender (male vs female) | ||||||||||||||
| Configural | 52.934 (10) | < 0.001 | 0.964 | 0.929 | 0.027 | 41.874 (10) | < 0.001 | 0.979 | 0.959 | 0.018 | ||||
| Metric | 55.992 (14) | < 0.001 | 3.058 (4) | 0.965 | 0.001 | 0.950 | 0.037 | 51.370 (14) | < 0.001 | 9.496 (4) | 0.976 | −0.003 | 0.965 | 0.044 |
| Scalar | 63.280 (18) | < 0.001 | 7.288 (4) | 0.962 | −0.003 | 0.958 | 0.042 | 55.458 (18) | < 0.001 | 4.088 (4) | 0.976 | 0.000 | 0.973 | 0.046 |
| Strict | 79.479 (23) | < 0.001 | 16.200 (5)* | 0.953 | −0.009 | 0.959 | 0.041 | 65.966 (23) | < 0.001 | 10.508 (5) | 0.972 | −0.004 | 0.976 | 0.046 |
| Age (< 20 years vs ≥ 20 years) | ||||||||||||||
| Configural | 49.244 (10) | < 0.001 | 0.967 | 0.934 | 0.025 | 41.665 (10) | < 0.001 | 0.979 | 0.958 | 0.018 | ||||
| Metric | 57.824 (14) | < 0.001 | 8.580 (4) | 0.963 | −0.004 | 0.947 | 0.051 | 49.650 (14) | < 0.001 | 7.985 (4) | 0.976 | −0.003 | 0.966 | 0.043 |
| Scalar | 70.454 (18) | < 0.001 | 12.630 (4)* | 0.956 | −0.007 | 0.951 | 0.058 | 54.244 (18) | < 0.001 | 4.594 (4) | 0.976 | 0.000 | 0.973 | 0.046 |
| Strict | 74.182 (23) | < 0.001 | 3.728 (5) | 0.957 | 0.001 | 0.963 | 0.054 | 59.088 (23) | < 0.001 | 4.844 (5) | 0.976 | 0.000 | 0.979 | 0.046 |
| Major (clinical medicine vs preventive medicine) | ||||||||||||||
| Configural | 46.837 (10) | < 0.001 | 0.968 | 0.936 | 0.026 | 42.164 (10) | < 0.001 | 0.979 | 0.958 | 0.019 | ||||
| Metric | 57.528 (14) | < 0.001 | 10.691 (4)* | 0.962 | −0.006 | 0.946 | 0.060 | 58.085 (14) | < 0.001 | 15.921 (4) | 0.971 | −0.008 | 0.958 | 0.056 |
| Scalar | 63.445 (18) | < 0.001 | 5.917 (4) | 0.961 | −0.001 | 0.956 | 0.064 | 70.981 (18) | < 0.001 | 12.895 (4) | 0.965 | −0.006 | 0.961 | 0.063 |
| Strict | 69.586 (23) | < 0.001 | 6.140 (5) | 0.960 | −0.001 | 0.965 | 0.062 | 78.824 (23) | < 0.001 | 7.844 (5) | 0.963 | −0.002 | 0.968 | 0.059 |
| Home location (urban vs rural vs suburban) | ||||||||||||||
| Configural | 52.121 (15) | < 0.001 | 0.969 | 0.938 | 0.028 | 47.354 (15) | < 0.001 | 0.979 | 0.958 | 0.020 | ||||
| Metric | 56.444 (23) | < 0.001 | 4.323 (8) | 0.972 | 0.003 | 0.963 | 0.042 | 50.249 (23) | 0.001 | 2.895 (8) | 0.982 | 0.003 | 0.977 | 0.031 |
| Scalar | 71.353 (31) | < 0.001 | 14.909 (8) | 0.966 | −0.006 | 0.967 | 0.051 | 57.660 (31) | 0.003 | 7.411 (8) | 0.983 | 0.001 | 0.983 | 0.037 |
| Strict | 85.508 (41) | < 0.001 | 14.155 (10) | 0.963 | −0.003 | 0.973 | 0.056 | 69.440 (41) | 0.004 | 11.780 (10) | 0.981 | −0.002 | 0.986 | 0.036 |
| Threshold | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 |
| Being only child (yes vs no) | ||||||||||||||
| Configural | 55.642 (10) | < 0.001 | 0.962 | 0.923 | 0.027 | 45.525 (10) | < 0.001 | 0.977 | 0.954 | 0.019 | ||||
| Metric | 57.227 (14) | < 0.001 | 1.585 (4) | 0.964 | 0.002 | 0.948 | 0.031 | 55.883 (14) | < 0.001 | 10.358 (4) | 0.973 | −0.004 | 0.961 | 0.051 |
| Scalar | 58.106 (18) | < 0.001 | 0.879 (4) | 0.966 | 0.002 | 0.962 | 0.032 | 58.072 (18) | < 0.001 | 2.189 (4) | 0.974 | 0.001 | 0.971 | 0.052 |
| Strict | 59.867 (23) | < 0.001 | 1.760 (5) | 0.969 | 0.003 | 0.973 | 0.032 | 63.610 (23) | < 0.001 | 5.539 (5) | 0.974 | 0.000 | 0.977 | 0.048 |
| Monthly household income (<10,000 CNY vs ≥10,000 CNY) | ||||||||||||||
| Configural | 52.339 (10) | < 0.001 | 0.964 | 0.928 | 0.028 | 42.364 (10) | < 0.001 | 0.979 | 0.958 | 0.019 | ||||
| Metric | 54.249 (14) | < 0.001 | 1.911 (4) | 0.966 | 0.002 | 0.951 | 0.035 | 46.149 (14) | < 0.001 | 3.785 (4) | 0.979 | 0.000 | 0.970 | 0.036 |
| Scalar | 59.468 (18) | < 0.001 | 5.219 (4) | 0.965 | −0.001 | 0.961 | 0.038 | 49.460 (18) | < 0.001 | 3.311 (4) | 0.979 | 0.000 | 0.977 | 0.038 |
| Strict | 60.943 (23) | < 0.001 | 1.475 (5) | 0.968 | 0.003 | 0.972 | 0.037 | 52.133 (23) | < 0.001 | 2.673 (5) | 0.981 | 0.002 | 0.983 | 0.038 |
| Part-time job (yes vs no) | ||||||||||||||
| Configural | 47.502 (10) | < 0.001 | 0.968 | 0.937 | 0.026 | 37.583 (10) | < 0.001 | 0.982 | 0.964 | 0.018 | ||||
| Metric | 53.590 (14) | < 0.001 | 6.088 (4) | 0.966 | −0.002 | 0.952 | 0.038 | 39.405 (14) | < 0.001 | 1.822 (4) | 0.983 | 0.001 | 0.976 | 0.022 |
| Scalar | 54.664 (18) | < 0.001 | 1.075 (4) | 0.969 | 0.003 | 0.966 | 0.038 | 39.965 (18) | 0.002 | 0.559 (4) | 0.986 | 0.003 | 0.984 | 0.023 |
| Strict | 56.380 (23) | < 0.001 | 1.716 (5) | 0.972 | 0.003 | 0.975 | 0.037 | 43.980 (23) | 0.005 | 4.015 (5) | 0.986 | 0.000 | 0.988 | 0.023 |
| Physical exercise (yes vs no) | ||||||||||||||
| Configural | 48.218 (10) | < 0.001 | 0.967 | 0.934 | 0.027 | 45.160 (10) | < 0.001 | 0.977 | 0.953 | 0.018 | ||||
| Metric | 49.586 (14) | < 0.001 | 1.368 (4) | 0.969 | 0.002 | 0.956 | 0.031 | 46.897 (14) | < 0.001 | 1.737 (4) | 0.978 | 0.001 | 0.969 | 0.023 |
| Scalar | 55.063 (18) | < 0.001 | 5.477 (4) | 0.968 | −0.001 | 0.965 | 0.034 | 50.420 (18) | < 0.001 | 3.523 (4) | 0.979 | 0.001 | 0.976 | 0.025 |
| Strict | 58.785 (23) | < 0.001 | 3.722 (5) | 0.969 | 0.001 | 0.973 | 0.036 | 55.071 (23) | < 0.001 | 4.651 (5) | 0.979 | 0.000 | 0.982 | 0.028 |
| Threshold | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 |
| Hobby (yes vs no) | ||||||||||||||
| Configural | 45.443 (10) | < 0.001 | 0.970 | 0.939 | 0.025 | 41.634 (10) | < 0.001 | 0.979 | 0.958 | 0.018 | ||||
| Metric | 54.322 (14) | < 0.001 | 8.879 (4) | 0.966 | −0.004 | 0.951 | 0.047 | 45.428 (14) | < 0.001 | 3.794 (4) | 0.979 | 0.000 | 0.970 | 0.030 |
| Scalar | 60.352 (18) | < 0.001 | 6.030 (4) | 0.964 | −0.002 | 0.960 | 0.051 | 50.697 (18) | < 0.001 | 5.269 (4) | 0.978 | −0.001 | 0.976 | 0.033 |
| Strict | 64.862 (23) | < 0.001 | 4.511 (5) | 0.964 | 0.000 | 0.969 | 0.049 | 58.747 (23) | < 0.001 | 8.050 (5) | 0.976 | −0.002 | 0.979 | 0.033 |
| Frequency of visiting home (frequently vs occasionally) | ||||||||||||||
| Configural | 59.381 (10) | < 0.001 | 0.958 | 0.916 | 0.030 | 44.238 (10) | < 0.001 | 0.978 | 0.955 | 0.020 | ||||
| Metric | 60.465 (14) | < 0.001 | 1.084 (4) | 0.961 | 0.003 | 0.944 | 0.033 | 55.843 (14) | < 0.001 | 11.604 (4) | 0.973 | −0.005 | 0.961 | 0.034 |
| Scalar | 67.474 (18) | < 0.001 | 7.010 (4) | 0.958 | −0.003 | 0.953 | 0.037 | 63.186 (18) | < 0.001 | 7.343 (4) | 0.970 | −0.003 | 0.967 | 0.036 |
| Strict | 74.911 (23) | < 0.001 | 7.437 (5) | 0.956 | −0.002 | 0.962 | 0.037 | 64.914 (23) | < 0.001 | 1.728 (5) | 0.972 | 0.002 | 0.976 | 0.038 |
| Stress coping strategy (emotion-focused vs solution-focused vs avoidance coping) | ||||||||||||||
| Configural | 64.714 (15) | < 0.001 | 0.957 | 0.914 | 0.030 | 56.192 (15) | < 0.001 | 0.973 | 0.945 | 0.021 | ||||
| Metric | 72.264 (23) | < 0.001 | 7.550 (8) | 0.958 | 0.001 | 0.945 | 0.047 | 61.663 (23) | < 0.001 | 5.471 (8) | 0.974 | 0.001 | 0.967 | 0.040 |
| Scalar | 84.429 (31) | < 0.001 | 12.165 (8) | 0.954 | −0.004 | 0.955 | 0.052 | 72.893 (31) | < 0.001 | 11.230 (8) | 0.972 | −0.002 | 0.973 | 0.044 |
| Strict | 97.831 (41) | < 0.001 | 13.402 (10) | 0.951 | −0.003 | 0.964 | 0.060 | 86.189 (41) | < 0.001 | 13.296 (10) | 0.970 | −0.002 | 0.978 | 0.044 |
| Threshold | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 | N/A | > 0.050 | N/A | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.080 |
Note: *P < 0.05.
Abbreviations: WHO-5-C, Chinese World Health Organization-Five Well-Being Index; χ2, chi-square; df, degrees of freedom; CFI, comparative fit index; TLI, Tucker-Lewis index; SRMR, standardized root mean square residual; Δ, change in χ2, df, and CFI; N/A, not applicable.
In LCFA tests of the WHO-5-C, all fit indices were in line with the proposed thresholds (CFI = 0.974–0.980, TLI = 0.968–0.976, REMSA = 0.070–0.081, SRMR = 0.022–0.027), and there were no substantial CFI changes in each nested model (ΔCFI = −0.006–0.000), supporting that the WHO-5-C had good longitudinal measurement invariance (Table 4).
Table 4.
Longitudinal Measurement Invariances of the WHO-5-C (N = 343)
| Hypothesis | χ2 (df) | P | Scaled Chi-Square Difference Test Statistics | CFI | ΔCFI | TLI | ΔTLI | RMSEA (90% CI) | ΔRMSEA | SRMR | ΔSRMR | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Δχ2 (Δdf) | P | |||||||||||
| Configural | 94.419 (29) | < 0.001 | 0.980 | 0.968 | 0.081 (0.063, 0.100) | 0.022 | ||||||
| Metric | 95.342 (33) | < 0.001 | 0.923 (4) | 0.921 | 0.980 | 0.000 | 0.973 | 0.005 | 0.074 (0.057, 0.092) | −0.007 | 0.024 | 0.002 |
| Scalar | 99.464 (37) | < 0.001 | 4.122 (4) | 0.390 | 0.980 | 0.000 | 0.976 | 0.003 | 0.070 (0.054, 0.087) | −0.004 | 0.025 | 0.001 |
| Strict | 125.095 (42) | < 0.001 | 25.631 (5) | < 0.001 | 0.974 | −0.006 | 0.972 | −0.004 | 0.076 (0.061, 0.091) | 0.006 | 0.027 | 0.002 |
| Threshold | N/A | > 0.050 | N/A | > 0.050 | ≥ 0.900 | ≤ 0.010 | ≥ 0.900 | ≤ 0.010 | ≤ 0.080 | ≤ 0.015 | ≤ 0.080 | ≤ 0.030 |
Abbreviations: WHO-5-C, Chinese World Health Organization-Five Well-Being Index; χ2, chi-square; df, degrees of freedom; CFI, comparative fit index; TLI, Tucker-Lewis index; RMSEA, root mean square error of approximation; CI, confidence interval; SRMR, standardized root mean square residual; Δ, change in χ2, df, CFI, TLI, RMSEA, and SRMR; N/A, not applicable.
Convergent Validity
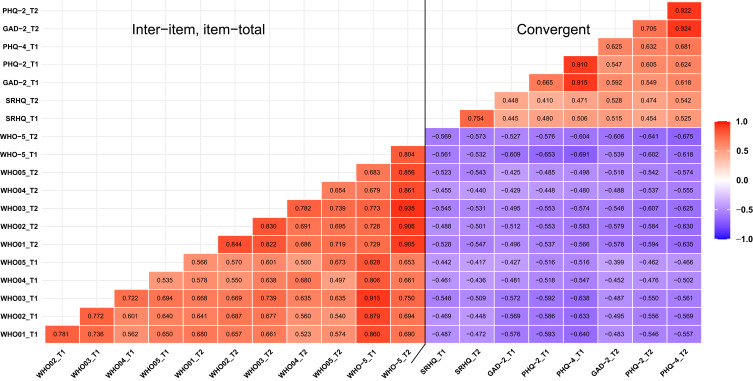
As shown in Figure 1, inter-item coefficients of the WHO-5-C ranged from 0.535 to 0.844 and item-total coefficients ranged from 0.806 to 0.935, indicating moderate to super strong correlations. Moderate correlations were observed between the WHO-5-C and SRHQ (Time 1: r = −0.561, Time 2: r = −0.573), as well as the PHQ-4-C (Time 1: r = −0.691, Time 2: r = −0.675), demonstrating adequate convergent validity.
Figure 1.
Inter-item and item-total correlations between the Chinese WHO-5, PHQ-4, and SRHQ (N=343).
Abbreviations: WHO-5, World Health Organization-Five Well-Being Index; WHO01-05, item 01–05 of the WHO-5; PHQ-2, Patient Health Questionnaire-2; GAD-2, Generalized Anxiety Disorder-2; PHQ-4, Patient Health Questionnaire-4; SRHQ, Self-Rated Health Questionnaire; T1, Time 1; T2, Time 2.
Reliability
Cronbach’s α and McDonald’s ω coefficients of the WHO-5-C at baseline were 0.907 (range of α-if-item-deleted = 0.865–0.905) and 0.908 (range of α-if-item-deleted = 0.865–0.905), respectively; and at follow-up were 0.934 (range of α-if-item-deleted = 0.906–0.930) and 0.935 (range of α-if-item-deleted = 0.904–0.931), respectively. The WHO-5-C demonstrated excellent test–retest reliability, with an ICC of 0.803 (range of ICC-if-item-deleted = 0.785–0.799), and stability of the scale was also demonstrated by SEM indices. No significant increase in indices was observed when any item was deleted. Similarly, the SRHQ and PHQ-4-C showed good internal consistencies and test–retest reliabilities (Table 5).
Table 5.
Internal Consistency and Test–Retest Reliability of the WHO-5-C, SRHQ, and PHQ-4-C (N = 343)
| Scales | Cronbach’s α | McDonald’s ω | ICC (95% CI) | SEM | |||
|---|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | Baseline | Follow-Up | ||
| WHO-5-C | 0.907 (0.891, 0.922) | 0.934 (0.923, 0.945) | 0.908 (0.893, 0.924) | 0.935 (0.924, 0.946) | 0.803 (0.762, 0.838) | 7.810 | 8.209 |
| WHO-5-C01 | 0.883 (0.863, 0.903) | 0.915 (0.900, 0.929) | 0.885 (0.865, 0.905) | 0.915 (0.900, 0.930) | 0.796 (0.754, 0.832) | 6.578 | 6.875 |
| WHO-5-C02 | 0.877 (0.857, 0.898) | 0.914 (0.899, 0.929) | 0.881 (0.860, 0.901) | 0.915 (0.901, 0.930) | 0.799 (0.757, 0.834) | 6.394 | 6.682 |
| WHO-5-C03 | 0.865 (0.843, 0.888) | 0.906 (0.890, 0.921) | 0.865 (0.841, 0.888) | 0.904 (0.887, 0.921) | 0.785 (0.741, 0.822) | 6.484 | 6.820 |
| WHO-5-C04 | 0.905 (0.889, 0.921) | 0.930 (0.918, 0.942) | 0.905 (0.889, 0.922) | 0.931 (0.918, 0.943) | 0.791 (0.748, 0.828) | 6.521 | 6.772 |
| WHO-5-C05 | 0.898 (0.881, 0.916) | 0.930 (0.918, 0.942) | 0.900 (0.883, 0.918) | 0.931 (0.919, 0.943) | 0.798 (0.756, 0.833) | 6.347 | 6.712 |
| SRHQ | 0.727 | 0.805 | N/A | N/A | 0.749 (0.697, 0.793) | 0.637 | 0.675 |
| PHQ-4-C | 0.818 (0.786, 0.849) | 0.846 (0.820, 0.872) | 0.820 (0.789, 0.851) | 0.849 (0.823, 0.875) | 0.681 (0.620, 0.734) | 1.234 | 1.263 |
Note: The McDonald’s ω and the 95% CI of Cronbach’s α cannot be calculated due to the SRHQ containing only 2 items.
Abbreviations: WHO-5-C, Chinese World Health Organization-Five Well-Being Index; WHO-5-C01-05, item 01–05 of the WHO-5-C was deleted; SRHQ, Self-Rated Health Questionnaire; PHQ-4-C, Chinese Patient Health Questionnaire-4; ICC, intraclass correlation coefficient; CI, confidence interval; SEM, standard error of measurement, calculated as “SD × sqrt (1-ICC)”.
Sensitivity and Specificity
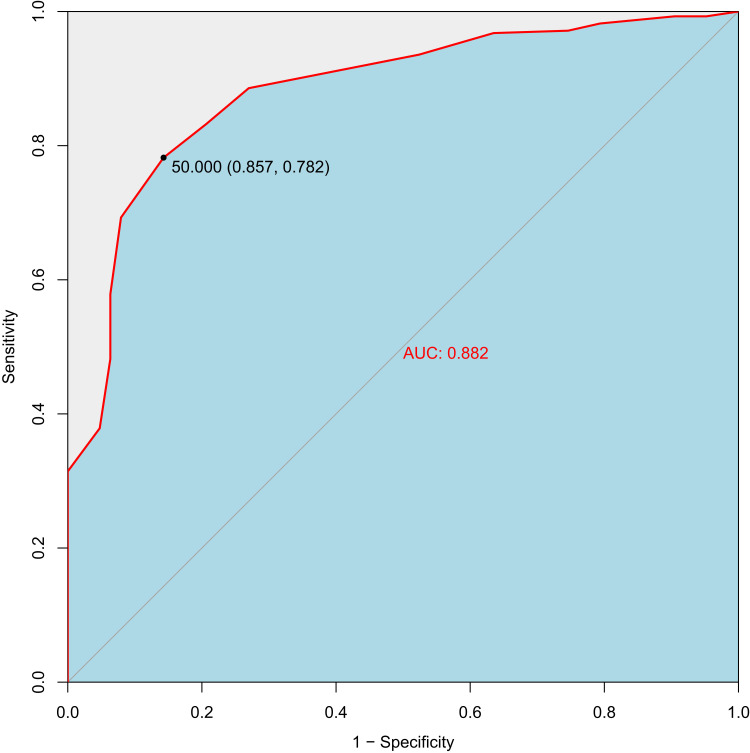
Based on baseline data, ROC curve analysis indicated that the WHO-5-C had an AUC value of 0.882, and the optimal cutoff point of ≥ 50 had sensitivity of 0.782 and specificity of 0.857 for screening satisfactory SWB in healthcare students (Figure 2). Sensitivity and specificity of the WHO-5-C were 0.803 and 0.762, respectively, in follow-up data when the cutoff point of 50 was applied as the threshold for predicting SWB (Table 6).
Figure 2.
ROC curve of the Chinese WHO-5 for well-being (N=343).
Abbreviations: WHO-5, World Health Organization-Five Well-Being Index; ROC, receiver operating characteristic; AUC, area under the curve.
Table 6.
Sensitivity and Specificity of the WHO-5-C for Identifying Well-Being in Healthcare Students (N = 343)
| WHO-5-C | PHQ-2-C | Total | Sensitivity | Specificity | |
|---|---|---|---|---|---|
| < 3 | ≥ 3 | ||||
| ≥ 50 | 211 | 13 | 224 | 0.803 | 0.762 |
| < 50 | 66 | 53 | 119 | ||
| Total | 277 | 66 | 343 | ||
Abbreviations: WHO-5-C, Chinese World Health Organization-Five Well-Being Index; PHQ-2-C, Chinese Patient Health Questionnaire-2.
Discussion
The adaptation of existing well-being instruments in Chinese populations mostly focuses on construct validity and reliability, but rarely responds to measurement invariance and clinical diagnostic capability. As an example, the WEMWBS is an instrument of well-being considering positive aspects of mental health, and despite the Chinese version representing stable factor structure and reliability across populations, its measurement invariance and truncation value are not available.23,82,83 Herein, the current study comprehensively evaluated measurement properties of the WHO-5-C in healthcare students, intending to introduce a well-being measuring tool with all-round persuasiveness. To our knowledge, this is the first study to explore measurement invariance of the WHO-5-C and determine a cutoff point for SWB identification in healthcare students. We provide strong evidence of a one-factor model with adequate validity and reliability, as well as measurement invariance, explaining its stability across different sociodemographic variables and time intervals. ROC analysis supports the WHO-5-C as a sensitive and specific instrument in assessing positive mental and physical well-being, with a recommended cutoff point of ≥ 50 indicating adequate SWB for Chinese healthcare students. Overall, our findings highlight effectiveness of the WHO-5-C and its validity in assessing SWB among healthcare students.
Structural Validity
CFA results corroborated general consensus of previous studies that the WHO-5 had a stable single-factor structure, which has also been found in most language versions: Brazilian,30 Japanese,34 Polish,36 Sinhala,37 Spanish,38 Swedish,40 and Turkish.41 The WHO-5-C had adequate structural validity, and these findings were also found in another study in multiple samples.43 In summary, our study adds to the growing body of evidence supporting structural validity of the WHO-5.
Measurement Invariance
Our study has validated cross-cultural validity of the WHO-5-C by demonstrating adequate measurement invariance across sociodemographic variables and time intervals. Adequate measurement invariance ensured that the scale had consistent measurement properties in a heterogeneous group and that targeted measurement was stably assessed by the scale.84 While partial fitting indices of MGCFA tests were contradictory to expectations, likely due to a small degree of freedom,85,86 all CFI changes among the four progressive nested models were consistently within adequate range, which is recognized as the most pivotal indicator to assess measurement invariance of a scale.74 Only limited evidence for the WHO-5 measurement invariance was found in extant literature. The Sinhala version supported measurement invariance across gender in all four nested models.37 Our findings extend previous ones in supporting satisfactory measurement invariance of the WHO-5-C in healthcare students both by different sociodemographic variables and over time.
Convergent Validity
Our findings demonstrated that the WHO-5-C demonstrated moderate negative correlations with both the SRHQ and PHQ-4-C, showing the WHO-5-C had sufficient convergent validity. Associations of comparable strengths with its related constructs of mental and physical health have been reported in community and patient samples,33,87,88 and special populations like healthcare workers in multi-national studies.89 Our evidence for construct validity of the WHO-5 in Chinese population adds support to its cross-cultural applicability as a valid instrument for measuring SWB in diverse domains and groups.
Reliability
Similar and consistent with previous studies of other language versions of the WHO-5,29,30,33,37–39,41,90 Cronbach’s α, McDonald’s ω and ICC of the WHO-5-C across two separate time points were greater than 0.800 in our study, illustrating its high internal consistency and test–retest reliability. Despite the brevity of the WHO-5-C, our data further support coherence across items and stability over time in Chinese.
Sensitivity and Specificity
Our study showed that the WHO-5-C had a reasonable ability to distinguish those who had psychological positive components when the cutoff point was ≥ 50 (AUC = 0.882), suggesting that the scale is a suitable screening instrument for measuring adequate SWB in Chinese healthcare students. Consistent with other studies in Asia, a standard cutoff point of ≥ 13 had an excellent sensitivity/specificity trade-off in the Arabic and Japanese versions, which meant that respondents with positive mindset can be detected by this cutoff criterion.29,34 Along the same vein, a reduction of 50% indicates reduced wellness in the Brazilian version and recommends that further clinical diagnosis for depression should be undertaken.30 Other cutoff points for different purposes and samples have been identified in other language versions of the WHO-5. The German version of the WHO-5 was applied to screen depression in an elderly population (AUC = 0.886), and a standard cutoff point of ≥ 16 was sufficiently sensitive and specific in predicting a status of optimal well-being.32 The fact that the definition and feeling of wellness are notably discrepant in different stages of life due to the gains and losses in health assets, social networks, economic resources and family structures.91,92 A systematic review of the WHO-5, thoroughly, drew a conclusion that the scale had been applied successfully as a generic scale for well-being across numerous fields, and a point below 50 was defined as an obvious reduction in well-being.28 The WHO-5, briefly, has appropriate validity both as a screening instrument for subjective psychosomatic well-being and as an outcome measurement in clinical trials.
Strengths and Limitations
The present study contributes to literature on utilization of the WHO-5 in Chinese healthcare students by providing empirical findings on its measurement properties and diagnostic performance. The study supports the application of the WHO-5-C in young adults with adequate validity and reliability, laying a solid foundation for its utilization in China. To our knowledge, our study is the first to verify cutoff point and to comprehensively examine measurement invariance of the WHO-5-C among healthcare students in terms of sociological characteristics and measurement times. As such, we provide a precise threshold for evaluating SWB state for clinical and research purposes in young adults, a vulnerable group for onset of psychosomatic health problems and developmental challenges.
This study is admittedly limited in that participants involved were all young healthcare students, rendering it difficult to generalize the findings to other age groups or disciplines. Given the promising findings this study offers, it would be highly valuable to further investigate psychometric properties of the WHO-5-C in various samples or a nationally representative and to validate the optimal cutoff point in different purposes and external samples. Despite widespread utilization of the PHQ-4-C, an instrument of positive SWB should be considered as a complementary measure to capture the comprehensive and multidimensional construct of wellness.1 Moreover, despite the WHO-5-C is freely available, it is essential to examine its content validity with a view to providing credible evidence for the sustainable implementation of the scale in China.
Conclusion
In conclusion, this study supports the WHO-5-C as a reliable and valid instrument for capturing SWB in healthcare students, with satisfactory measurement invariance in different sociodemographic variables and over time, and a cutoff point of ≥ 50 for identifying significantly adequate SWB state. Together with the family of studies on the WHO-5 worldwide, our evidence enables research and clinical communities to apply the scale for screening well-being in public health and primary care settings.
Acknowledgments
The authors thank the study participants and the research assistants for their time. The authors are indebted to three anonymous reviewers and a handling editor for their insightful views and constructive comments.
Funding Statement
This study was supported by the Medical Research Fund of Zhejiang Province, Grant No. 2023RC073 and the Research Initiation Fund of Hangzhou Normal University, Grant No. RWSK20201003.
Data Sharing Statement
Not available.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Beddington J, Cooper CL, Field J, et al. The mental wealth of nations. Nature. 2008;455(7216):1057–1060. doi: 10.1038/4551057a [DOI] [PubMed] [Google Scholar]
- 2.Faruk MO, Alam F, Chowdhury KUA, Soron TR. Validation of the Bangla WHO-5 Well-being Index. Glob Ment Health. 2021;8:e26. doi: 10.1017/gmh.2021.26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finan PH, Garland EL. The role of positive affect in pain and its treatment. Clin J Pain. 2015;31(2):177–187. doi: 10.1097/ajp.0000000000000092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rasmussen HN, Scheier MF, Greenhouse JB. Optimism and physical health: a meta-analytic review. Ann Behav Med. 2009;37(3):239–256. doi: 10.1007/s12160-009-9111-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chida Y, Steptoe A. Positive psychological well-being and mortality: a quantitative review of prospective observational studies. Psychosom Med. 2008;70(7):741–756. doi: 10.1097/PSY.0b013e31818105ba [DOI] [PubMed] [Google Scholar]
- 6.Bolier L, Haverman M, Westerhof GJ, Riper H, Smit F, Bohlmeijer E. Positive psychology interventions: a meta-analysis of randomized controlled studies. BMC Public Health. 2013;13:119. doi: 10.1186/1471-2458-13-119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubzansky LD, Huffman JC, Boehm JK, et al. Positive psychological well-being and cardiovascular disease: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(12):1382–1396. doi: 10.1016/j.jacc.2018.07.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Howell RT, Kern ML, Lyubomirsky S. Health benefits: meta-analytically determining the impact of well-being on objective health outcomes. Health Psychol Rev. 2007;1(1):83–136. doi: 10.1080/17437190701492486 [DOI] [Google Scholar]
- 9.Liu X, Ping S, Gao W. Changes in undergraduate students’ psychological well-being as they experience university life. Int J Environ Res Public Health. 2019;16(16):2864. doi: 10.3390/ijerph16162864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holm-Hadulla RM, Klimov M, Juche T, Möltner A, Herpertz SC. Well-being and mental health of students during the COVID-19 pandemic. Psychopathology. 2021;54(6):291–297. doi: 10.1159/000519366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sheldon E, Simmonds-Buckley M, Bone C, et al. Prevalence and risk factors for mental health problems in university undergraduate students: a systematic review with meta-analysis. J Affect Disord. 2021;287:282–292. doi: 10.1016/j.jad.2021.03.054 [DOI] [PubMed] [Google Scholar]
- 12.Sattar K, Yusoff MSB, Arifin WN, Yasin MAM, Nor MZM. A scoping review on the relationship between mental wellbeing and medical professionalism. Med Educ Online. 2023;28(1):2165892. doi: 10.1080/10872981.2023.2165892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang CY, Pan RY, Wan XY, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17(5):1729. doi: 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cao WJ, Fang ZW, Hou GQ, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moreira de Sousa J, Moreira CA, Telles-Correia D. Anxiety, depression and academic performance: a study amongst Portuguese medical students versus non-medical students. Acta Med Port. 2018;31(9):454–462. doi: 10.20344/amp.9996 [DOI] [PubMed] [Google Scholar]
- 16.Quek TT, Tam WW, Tran BX, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16(15):2735. doi: 10.3390/ijerph16152735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China: a meta-analysis. Medicine. 2019;98(18):e15337. doi: 10.1097/md.0000000000015337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cooke PJ, Melchert TP, Connor K. Measuring well-being: a review of instruments. Couns Psychol. 2016;44(5):730–757. doi: 10.1177/0011000016633507 [DOI] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 20.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30(2):191–197. doi: 10.1016/0304-3959(87)91074-8 [DOI] [PubMed] [Google Scholar]
- 21.McIntyre RS, Alda M, Baldessarini RJ, et al. The clinical characterization of the adult patient with bipolar disorder aimed at personalization of management. World Psychiatry. 2022;21(3):364–387. doi: 10.1002/wps.20997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tennant R, Hiller L, Fishwick R, et al. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): development and UK validation. Health Qual Life Out. 2007;5(1):63. doi: 10.1186/1477-7525-5-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taggart F, Friede T, Weich S, Clarke A, Johnson M, Stewart-Brown S. Cross cultural evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS)-a mixed methods study. Health Qual Life Out. 2013;11:27. doi: 10.1186/1477-7525-11-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diener E. Subjective well-being: the science of happiness and a proposal for a national index. Am Psychol. 2000;55(1):34–43. doi: 10.1037/0003-066X.55.1.34 [DOI] [PubMed] [Google Scholar]
- 25.Smyth R, Nielsen I, Zhai Q. Personal Well-being in urban China. Soc Indic Res. 2010;95(2):231–251. doi: 10.1007/s11205-009-9457-2 [DOI] [Google Scholar]
- 26.Chan DW, Chan L-K, Sun X. Developing a brief version of Ryff’s scale to assess the psychological well-being of adolescents in Hong Kong. Eur J Psychol Assess. 2019;35(3):414–422. doi: 10.1027/1015-5759/a000403 [DOI] [Google Scholar]
- 27.Wellbeing measures in primary health care/the DepCare Project: report on a WHO meeting: Stockholm, Sweden, 12–13 February 1998. World Health Organization. Regional Office for Europe; 1998. . Available from: https://iris.who.int/handle/10665/349766. Accessed January 30, 2021. [Google Scholar]
- 28.Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom. 2015;84(3):167–176. doi: 10.1159/000376585 [DOI] [PubMed] [Google Scholar]
- 29.Sibai AM, Chaaya M, Tohme RA, Mahfoud Z, Al-Amin H. Validation of the Arabic version of the 5-item WHO Well Being Index in elderly population. Int J Geriatr Psychiatry. 2009;24(1):106–107. doi: 10.1002/gps.2079 [DOI] [PubMed] [Google Scholar]
- 30.de Souza CM, Hidalgo MP. World Health Organization 5-item well-being index: validation of the Brazilian Portuguese version. Eur Arch Psychiatry Clin Neurosci. 2012;262(3):239–244. doi: 10.1007/s00406-011-0255-x [DOI] [PubMed] [Google Scholar]
- 31.Lee GL, Fan GK, Chan SW. Validation of Chinese and English versions of the Holistic Well-being Scale in patients with cancer. Support Care Cancer. 2015;23(12):3563–3571. doi: 10.1007/s00520-015-2736-3 [DOI] [PubMed] [Google Scholar]
- 32.Bonsignore M, Barkow K, Jessen F, Heun R. Validity of the five-item WHO Well-Being Index (WHO-5) in an elderly population. Eur Arch Psychiatry Clin Neurosci. 2001;251(Suppl 2):27–31. doi: 10.1007/bf03035123 [DOI] [PubMed] [Google Scholar]
- 33.Guðmundsdóttir HB, Olason DP, Guðmundsdóttir DG, Sigurðsson JF. A psychometric evaluation of the Icelandic version of the WHO-5. Scand J Psychol. 2014;55(6):567–572. doi: 10.1111/sjop.12156 [DOI] [PubMed] [Google Scholar]
- 34.Awata S, Bech P, Yoshida S, et al. Reliability and validity of the Japanese version of the World Health Organization-Five Well-Being Index in the context of detecting depression in diabetic patients. Psychiatry Clin Neurosci. 2007;61(1):112–119. doi: 10.1111/j.1440-1819.2007.01619.x [DOI] [PubMed] [Google Scholar]
- 35.Suhaimi AF, Makki SM, Tan KA, Silim UA, Ibrahim N. Translation and validation of the Malay version of the WHO-5 Well-Being Index: reliability and validity evidence from a sample of type 2 diabetes mellitus patients. Int J Environ Res Public Health. 2022;19(7):4415. doi: 10.3390/ijerph19074415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cichoń E, Kiejna A, Kokoszka A, et al. Validation of the Polish version of WHO-5 as a screening instrument for depression in adults with diabetes. Diabetes Res Clin Pract. 2020;159:107970. doi: 10.1016/j.diabres.2019.107970 [DOI] [PubMed] [Google Scholar]
- 37.Perera BPR, Jayasuriya R, Caldera A, Wickremasinghe AR. Assessing mental well-being in a Sinhala speaking Sri Lankan population: validation of the WHO-5 well-being index. Health Qual Life Out. 2020;18(1):305. doi: 10.1186/s12955-020-01532-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lucas-Carrasco R. Reliability and validity of the Spanish version of the World Health Organization-Five Well-Being Index in elderly. Psychiatry Clin Neurosci. 2012;66(6):508–513. doi: 10.1111/j.1440-1819.2012.02387.x [DOI] [PubMed] [Google Scholar]
- 39.Chongwo E, Ssewanyana D, Nasambu C, et al. Validation of a Swahili version of the World Health Organization 5-item well-being index among adults living with HIV and epilepsy in rural coastal Kenya. Glob Health Res Policy. 2018;3:26. doi: 10.1186/s41256-018-0081-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Löve J, Andersson L, Moore CD, Hensing G. Psychometric analysis of the Swedish translation of the WHO well-being index. Qual Life Res. 2014;23(1):293–297. doi: 10.1007/s11136-013-0447-0 [DOI] [PubMed] [Google Scholar]
- 41.Eser E, Çevik C, Baydur H, et al. Reliability and validity of the Turkish version of the WHO-5, in adults and older adults for its use in primary care settings. Prim Health Care Res Dev. 2019;20:e100. doi: 10.1017/s1463423619000343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Wit M, Pouwer F, Gemke RJ. Validation of the WHO-5 Well-Being Index in adolescents with type 1 diabetes. Diabetes Care. 2007;30(8):2003–2006. doi: 10.2337/dc07-0447 [DOI] [PubMed] [Google Scholar]
- 43.Fung SF, Kong CYW, Liu YM, et al. Validity and psychometric evaluation of the Chinese version of the 5-Item WHO Well-Being Index. Front Public Health. 2022;10:872436. doi: 10.3389/fpubh.2022.872436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chan L, Liu RKW, Lam TP, Chen JY, Tipoe GL, Ganotice FA. Validation of the World Health Organization Well-Being Index (WHO-5) among medical educators in Hong Kong: a confirmatory factor analysis. Med Educ Online. 2022;27(1):2044635. doi: 10.1080/10872981.2022.2044635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saracci R. The World Health Organisation needs to reconsider its definition of health. BMJ. 1997;314(7091):1409–1410. doi: 10.1136/bmj.314.7091.1409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford University Press; 2014. [Google Scholar]
- 47.Deyo RA, Diehr P, Patrick DL. Reproducibility and responsiveness of health status measures. Statistics and strategies for evaluation. Control Clin Trials. 1991;12(4 Suppl):142S–158S. doi: 10.1016/s0197-2456(05)80019-4 [DOI] [PubMed] [Google Scholar]
- 48.Kline P. An Easy Guide to Factor Analysis. New York: Routledge; 1994. [Google Scholar]
- 49.Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5(2):159–168. doi: 10.1207/s15327574ijt0502_4 [DOI] [Google Scholar]
- 50.Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 51.The Chinese version of the WHO (Five) in characters used in PR China. Psychiatric Research Unit, WHO Collaborating Center for Mental Health. Available from: https://www.psykiatri-regionh.dk/who-5/Documents/WHO5_Chinese_PR.pdf. Accessed January 30, 2021.
- 52.Spitzer RL, Kroenke JBWWK. Instructions for Patient Health Questionnaire (PHQ) and GAD-7 Measures. Available from: https://www.phqscreeners.com/. Accessed January 30, 2021.
- 53.Sapra A, Bhandari P, Sharma S, Chanpura T, Lopp L. Using Generalized Anxiety Disorder-2 (GAD-2) and GAD-7 in a Primary Care Setting. Cureus. 2020;12(5):e8224. doi: 10.7759/cureus.8224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.Mlr.0000093487.78664.3c [DOI] [PubMed] [Google Scholar]
- 55.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122(1–2):86–95. doi: 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 56.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50(6):613–621. doi: 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 57.Luo Y, Fei S, Gong B, Sun T, Meng R. Understanding the mediating role of anxiety and depression on the relationship between perceived stress and sleep quality among health care workers in the COVID-19 response. Nat Sci Sleep. 2021;13:1747–1758. doi: 10.2147/nss.S313258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Meng R, Dong L, Dzierzewski JM, et al. The RU_SATED as a measure of sleep health: cross-cultural adaptation and validation in Chinese healthcare students. BMC Psychology. 2023;11(1):200. doi: 10.1186/s40359-023-01203-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhu Y, Jiang C, Yang Y, et al. Depression and anxiety mediate the association between sleep quality and self-rated health in healthcare students. Behav Sci. 2023;13(2):82. doi: 10.3390/bs13020082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jiang C, Ma H, Luo Y, et al. Validation of the Chinese version of the Perceived Stress Scale-10 integrating exploratory graph analysis and confirmatory factor analysis. Gen Hosp Psychiatry. 2023;84:194–202. doi: 10.1016/j.genhosppsych.2023.07.008 [DOI] [PubMed] [Google Scholar]
- 61.Jiang C, Zhu Y, Luo Y, et al. Validation of the Chinese version of the Rosenberg Self-Esteem Scale: evidence from a three-wave longitudinal study. BMC Psychology. 2023;11(1):345. doi: 10.1186/s40359-023-01293-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosseel Y. Lavaan: an R package for structural equation modeling. J Stat Softw. 2012;48:1–36. doi: 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- 63.Kelley K. MBESS: the MBESS R package. 2022. Available from: https://CRAN.R-project.org/package=MBESS. Accessed January 30, 2023.
- 64.Gamer M, Lemon J, Singh IFP. irr: various coefficients of interrater reliability and agreement. 2019. Available from: https://CRAN.R-project.org/package=irr. Accessed January 30, 2023.
- 65.Jorgensen TD, Pornprasertmanit S, Schoemann AM, Rosseel Y. Useful tools for structural equation modeling. 2022. Available from: https://CRAN.R-project.org/package=semTools. Accessed January 30, 2023.
- 66.Sachs MC. plotROC: a tool for plotting ROC curves. J Stat Softw. 2017;79(2):1–19. doi: 10.18637/jss.v079.c02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dziura JD, Post LA, Zhao Q, Fu Z, Peduzzi P. Strategies for dealing with missing data in clinical trials: from design to analysis. Yale J Biol Med. 2013;86(3):343–358. [PMC free article] [PubMed] [Google Scholar]
- 68.Finney SJ, DiStefano C. Nonnormal and Categorical Data in Structural Equation Models. Structural Equation Modeling: A Second Course. Greenwich, CT: Information Age; 2006. [Google Scholar]
- 69.Mokkink LB, Terwee CB, Patrick DL, et al. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745. doi: 10.1016/j.jclinepi.2010.02.006 [DOI] [PubMed] [Google Scholar]
- 70.Hair JF, Black WC, Babin BJ, Anderson RE. Multivariate Data Analysis: Pearson New International Edition. 7th ed. London, UK: Pearson Higher Education; 2014. [Google Scholar]
- 71.Kline RB. Principles and Practice of Structural Equation Modeling. 4th ed. New York, NY, USA: Guilford Publications; 2016. [Google Scholar]
- 72.Edwards MC, Houts CR, Wirth RJ. Measurement invariance, the lack thereof, and modeling change. Qual Life Res. 2018;27(7):1735–1743. doi: 10.1007/s11136-017-1673-7 [DOI] [PubMed] [Google Scholar]
- 73.Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equ Modeling. 2002;9(2):233–255. doi: 10.1207/S15328007SEM0902_5 [DOI] [Google Scholar]
- 74.Putnick DL, Bornstein MH. Measurement invariance conventions and reporting: the state of the art and future directions for psychological research. Dev Rev. 2016;41:71–90. doi: 10.1016/j.dr.2016.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Doan T, Ha V, Strazdins L, Chateau D. Healthy minds live in healthy bodies - effect of physical health on mental health: evidence from Australian longitudinal data. Curr Psychol. 2022;42:18702–18713. doi: 10.1007/s12144-022-03053-7 [DOI] [Google Scholar]
- 76.Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018;126(5):1763–1768. doi: 10.1213/ane.0000000000002864 [DOI] [PubMed] [Google Scholar]
- 77.DeVon HA, Block ME, Moyle-Wright P, et al. A psychometric toolbox for testing validity and reliability. J Nurs Scholarsh. 2007;39(2):155–164. doi: 10.1111/j.1547-5069.2007.00161.x [DOI] [PubMed] [Google Scholar]
- 78.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi: 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. doi: 10.1519/15184.1 [DOI] [PubMed] [Google Scholar]
- 80.Walter SD. The partial area under the summary ROC curve. Stat Med. 2005;24(13):2025–2040. doi: 10.1002/sim.2103 [DOI] [PubMed] [Google Scholar]
- 81.Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993;39(4):561–577. doi: 10.1093/clinchem/39.4.561 [DOI] [PubMed] [Google Scholar]
- 82.Ng SS, Lo AW, Leung TK, et al. Translation and validation of the Chinese version of the short Warwick-Edinburgh Mental Well-being Scale for patients with mental illness in Hong Kong. East Asian Arch Psychiatry. 2014;24(1):3–9. [PubMed] [Google Scholar]
- 83.Dong A, Chen X, Zhu L, et al. Translation and validation of a Chinese version of the Warwick–Edinburgh Mental Well-being Scale with undergraduate nursing trainees. J Psychiatr Ment Health Nurs. 2016;23(9–10):554–560. doi: 10.1111/jpm.12344 [DOI] [PubMed] [Google Scholar]
- 84.Chen FF. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct Equ Modeling. 2007;14(3):464–504. doi: 10.1080/10705510701301834 [DOI] [Google Scholar]
- 85.Lai K, Green SB. The problem with having two watches: assessment of fit when RMSEA and CFI disagree. Multivariate Behav Res. 2016;51(2–3):220–239. doi: 10.1080/00273171.2015.1134306 [DOI] [PubMed] [Google Scholar]
- 86.Shi D, DiStefano C, Maydeu-Olivares A, Lee T. Evaluating SEM model fit with small degrees of freedom. Multivariate Behav Res. 2022;57(2–3):179–207. doi: 10.1080/00273171.2020.1868965 [DOI] [PubMed] [Google Scholar]
- 87.Hansen CP, Amiri M. Combined detection of depression and anxiety in epilepsy patients using the Neurological Disorders Depression Inventory for Epilepsy and the World Health Organization well-being index. Seizure. 2015;33:41–45. doi: 10.1016/j.seizure.2015.10.008 [DOI] [PubMed] [Google Scholar]
- 88.Mergl R, Seidscheck I, Allgaier AK, Möller HJ, Hegerl U, Henkel V. Depressive, anxiety, and somatoform disorders in primary care: prevalence and recognition. Depress Anxiety. 2007;24(3):185–195. doi: 10.1002/da.20192 [DOI] [PubMed] [Google Scholar]
- 89.Lara-Cabrera ML, Betancort M, Muñoz-Rubilar A, Rodríguez-Novo N, Bjerkeset O, De Las Cuevas C. Psychometric properties of the WHO-5 Well-Being Index among nurses during the COVID-19 pandemic: a cross-sectional study in three countries. Int J Environ Res Public Health. 2022;19(16):10106. doi: 10.3390/ijerph191610106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Awata S, Bech P, Koizumi Y, et al. Validity and utility of the Japanese version of the WHO-Five Well-Being Index in the context of detecting suicidal ideation in elderly community residents. Int Psychogeriatr. 2007;19(1):77–88. doi: 10.1017/s1041610206004212 [DOI] [PubMed] [Google Scholar]
- 91.Mirowsky J, Ross CE. Age and depression. J Health Soc Behav. 1992;33(3):187–205. doi: 10.2307/2137349 [DOI] [PubMed] [Google Scholar]
- 92.Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. PNAS. 2010;107(22):9985–9990. doi: 10.1073/pnas.1003744107 [DOI] [PMC free article] [PubMed] [Google Scholar]