Abstract
Obesity is a complex, chronic disease requiring a multidisciplinary approach to its management. In clinical practice, body mass index and waist-related measurements can be used for obesity screening. The estimated prevalence of obesity among adults worldwide is 12%. With the expected further increase in overall obesity prevalence, clinicians will increasingly be managing patients with obesity. Energy balance is regulated by a complex neurohumoral system that involves the central nervous system and circulating mediators, among which leptin is the most studied. The functioning of these systems is influenced by both genetic and environmental factors. Obesity generally occurs when a genetically predisposed individual lives in an obesogenic environment for a long period. Cardiologists are deeply involved in evaluating patients with obesity. Cardiovascular risk profile is one of the most important items to be quantified to understand the health risk due to obesity and the clinical benefit that a single patient can obtain with weight loss. At the individual level, appropriate patient involvement, the detection of potential obesity causes, and a multidisciplinary approach are tools that can improve clinical outcomes. In the near future, we will probably have new pharmacological tools at our disposal that will facilitate achieving and maintaining weight loss. However, pharmacological treatment alone cannot cure such a complex disease. The aim of this paper is to summarize some key points of this field, such as obesity definition and measurement tools, its epidemiology, the main mechanisms underlying energy homeostasis, health consequences of obesity with a focus on cardiovascular diseases and the obesity paradox.
Level of evidence V: report of expert committees.
Keywords: Obesity, Energy homeostasis, BMI, Weight loss, Fat tissue, Cardiology, Adult
Introduction
Most physicians, upon encountering a patient with obesity, often attribute this condition to excessive food consumption and/or a sedentary lifestyle, perceived as resulting from a lack of knowledge about healthy living, or a lack of willpower to establish healthy habits. At the societal level, this simplistic approach is frequently associated with a moral judgment that connects obesity with a weakness of character or, more derogatorily, other negative traits. Such attitudes rapidly lead to social stigma. In healthcare settings, this stigma surrounding obesity can result in a lower quality of care [1]. Some cardiologists may not be aware of the underlying diseases or factors that could trigger or perpetuate this chronic and complex condition and may skip the diagnostic step to jump directly to the therapeutic phase by recommending weight loss. Occasionally, the patient is referred to a dietitian, nutritionist, or personal trainer as though obesity were not a chronic disease but simply the outcome of poor habits. However, these habits rely on many factors, not all of which are under the patient’s control. The achievement of weight loss often becomes the primary goal, eclipsing the importance of promoting overall health and understanding the complex, heterogeneous, multifactorial, and chronic nature of obesity as an epidemic. Understanding the underlying factors can aid in tailoring treatment, guiding patients, improving their understanding of the disease, increasing their commitment and self-efficacy, and enhancing their treatment adherence. Offering accurate advice also discourages patients from turning to commercial weight-loss programmes, which can be not only ineffective but also detrimental to physical and mental health. The aim of this article is to summarize what cardiologists need to know to effectively manage patients living with obesity, and to underscore the importance of a multidisciplinary approach. We discuss the primary pathophysiological mechanisms underlying obesity and obesity-related cardiovascular diseases. Moreover, this document focuses on measurement tools useful in identifying patients with obesity and assessing the cardiovascular risk associated with obesity.
Definition and measurement tools
Obesity is defined as an abnormal or excessive fat accumulation that poses a health risk [2]. Visceral abdominal fat is more strongly associated with adverse health effects as compared to the amount of total body fat [3, 4].
Body Mass Index (BMI) is the most used obesity measure both in scientific literature and in clinical practice. This measure is obtained by dividing weight in kilograms by the square of height in meters [5]. BMI is a simple, easy, and inexpensive way to identify patients living with obesity. However, at the individual level, using BMI as the only tool for the diagnosis and staging of obesity presents important critical issues. BMI cannot distinguish body composition, it does not consider the location of adipose tissue in the body, so it may under- or over-estimate metabolic and cardiovascular risk related to the obesity.
In general, overall obesity and abdominal obesity are directly related [5]. However, it is possible to find patients with a BMI of less than 30 kg/m2 and abnormal visceral fat accumulation (normal-weight obesity) [5]. On the other hand, a person classified as affected by obesity only using BMI, could have a non-visceral fat distribution [5].
The simultaneous presence of excess fat and loss of lean body mass is defined as sarcopenic obesity. Recently, a joint ESPEN (the European Society for Clinical Nutrition and Metabolism) and EASO (the European Association for the Study of Obesity) international consensus proposed screening and diagnostic criteria that concern both body composition and functional and strength tests, inviting to consider the co-presence of the two pathologies as a separate pathology different from sarcopenia or obesity alone, due to the synergistic effect and the consequent increase in the risk of dysmetabolic pathologies [6].
Furthermore, BMI does not take into account different body composition age-related [e.g., due to the loss of fat-free mass (FFM) associated with ageing], sex- and ethnicity-related. Different cut offs should be used in patients belonging to populations with different characteristics [7]. As an example, lower BMI cut offs should be used to define overweight and obesity in Asian populations [8, 9]. In these populations overweight and obesity should start, respectively, at BMI 23 kg/m2 and 27.4 kg/m2, [9].
Subcutaneous and visceral adipose tissues have numerous anatomic and functional differences. Subcutaneous adipose tissue (SAT) accounts for approximately 80% of total fat, while visceral adipose tissue (VAT) accounts for 10–20% [10]. Blood from the VAT is drained directly to the liver via the portal vein system, whereas blood from the SAT is drained via the systemic venous system.
The quality and quantity of cytokines secreted appears to differ particularly with the increase in fat mass [11].
When VAT increases and exceeds a certain level, pathological processes begin. They are mediated by an increased quantity of cytokine secreted, a quantitative and qualitative change in immune system activity, fat hypertrophy, increased fibrosis, and impaired vascular function and structure [11–13]. All these tissue and functional changes are referred to as adiposopathy [12].
The increase in the accumulation of adipose tissue in the subcutaneous tissue is progressively associated with an increase in visceral adipose tissue with a non-linear and very individual relationship. The organs most involved are the liver, pancreas, epicardium and pericardium, and muscle tissue. In such cases, it is called ectopic fat, which must be considered equal to visceral fat in terms of cardiovascular risk [4].
Due to the above mentioned limits of BMI as a measure of body fat, several other measures have been proposed to better define the presence and distribution of adipose tissue (Table 1) [14, 15], including waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), the fat mass index (FMI), fat-free mass index (FFMI), fat mass body percentage (FM%), but none of these alone has been consistently found to be a better predictor for clinical purposes [16, 17].
Table 1.
Weight categories and waist circumference cut-off values
| Weight categories according to BMI in adults [8] | ||
|---|---|---|
| kg/m2 | ||
| Underweight | < 18.5 | |
| Normal weight | ≥ 18.5 and < 25 | |
| Overweight | ≥ 25 and < 30 | |
| Obesity | > 30 | |
| Class I | ≥ 30 and < 35 | |
| Class II | ≥ 35 and < 40 | |
| Class III | ≥ 40 | Also named severe, extreme, or morbid obesity |
| Waist circumference cut-off indicating increased health risk in various ethnicities [18, 19] | ||
|---|---|---|
| M (cm) | F (cm) | |
| Caucasian Europid/United States/Mid-East Mediterraneanb | 102 | 88 |
| Latino Central/South Americanb | 94 | 90 |
| Sub-Saharan Africana | 95 | 99 |
| Africanb | 80.5 | 81.5 |
| Koreanb | 90 | 85 |
| Chinesea | 83 | 81 |
World Health Organization classification of body weight for Caucasian people. In people with an Asian, Chinese, Middle Eastern, Black African, or Afro-Caribbean family background, obesity classes 2 and 3 are usually identified by reducing the values used for Caucasian people by 2.5 kg/m2 because they are prone to central adiposity and their cardiometabolic risk occurs at a lower BMI. In these populations overweight and obesity start respectively at BMI 23 kg/m2 and 27.4 kg/m2 [8]
aIncreased cardiovascular risk
bGreater increasing cardiovascular risk
Probably, WC is the simplest and most economical measure of abdominal obesity [18]. Of note, as well as for BMI, to define increased adiposity different waist circumference cutoff values have been proposed on the basis of sex and ethnicity [19, 20].
To obtain the most accurate measurement of VAT without resorting to complex instrumental examinations, the use of certain anthropometric measurements have been proposed and validated [21].
Proximal thigh circumference (PTC) and WC have been identified as proxy indicators of subcutaneous abdominal adipose tissue (SAAT) and the sum of SAAT and VAT, respectively. By subtracting the SAAT value from the waist circumference and correcting the result for age, sex, and BMI, a VAT value is obtained, which correlates with VAT measured with computed tomography (CT) [21]. This, along with magnetic resonance imaging (MRI) are currently gold standard methods to measure VAT.
The amount of adipose tissue in the human body can be detected using different invasive and non-invasive techniques. Non-invasive methods include hydrostatic weighing (densitometry—HW), air displacement plethysmography (ADP), bioelectrical impedance analysis (BIA), dual-energy X-ray absorptiometry (DXA), CT, MRI [14]. Table 2 presents some characteristics of these techniques.
Table 2.
Body composition evaluation methods
| Ability to assess FM and FFM | Ability to assess fat regional distribution | Precision and accuracy in measuring VAT | Use of ionizing radiation | |
|---|---|---|---|---|
| Circumferences | Yes | Yes | Low | No |
| Skinfold thickness | Yes | Yes | Low | No |
| Ultrasound | No | Yes | Low | No |
| Hydrostatic weighing densitometry | Yes | No | High | No |
| Air displacement plethysmography | Yes | No | High | No |
| Bioelectrical impedance analysis | Yes | No | Medium | No |
| Dual-energy X-ray absorptiometry | Yes | Partially | High | Yes |
| Computed Tomography | Yes | Yes | Gold standard | Yes |
| Magnetic Resonance Imaging | Yes | Yes | Gold standard | No |
Most used methods to evaluate body composition
FM, fat mass; FFM, fat-free mass; VAT, visceral adipose tissue
In summary HW, ADP and BIA can give information on the overall body density and so can provide a measure of total body fat and lean tissue, but they cannot specify fat regional distributions. With this purpose, CT and MRI are the most accurate and precise techniques. They can detect and measure fat distribution, such as visceral, muscle, or liver fat. In some instances, a subject with normal BMI but elevated intra-abdominal fat could be differentiated from a high BMI subject with normal intra-abdominal fat, resulting in a more accurate cardiovascular risk assessment. Other details, if needed, can be obtained in Borga et al. [14].
Despite the limitation expressed above, an elevated BMI remains a simple, inexpensive, measure, associated with a poorer outcome and constitutes the basis for the World Health Organization (WHO) definition of overweight and obesity (see Table 3).
Table 3.
Methods to assess body adiposity [14]
| Measurement | Acronymous | Measured/calculated | Screening | Clinical setting: diagnosis/ management |
Research Setting |
|---|---|---|---|---|---|
| Body mass, Kg | BM | Measured (Kg) | + | + | + |
| Body mass Index, Kg/m2 | BMI | Weight in kilograms divided by height (h) in meters squared (m2) | + | + | + |
| Body fat mass, Kg | FM | Measured by instruments (BIA–DEXA–MRI–CT) | + | + | |
| Body fat mass index, Kg/m2 | FMI | FM/h2 | + | + | |
| Fat-free mass, Kg | FFM | Measured by instruments (BIA–DEXA–MRI–CT); calculated: BM–FM | + | + | |
| Body fat percentage, % | %BF | FM*100/BM | + | + | |
| Fat-free mass index, Kg/m2 | FFMI | FFM/h2 | + | + | |
| Visceral adipose tissue, L, ml, Kg, gr, cm2 | VAT | Measured or calculated by anthropometric measures, MRI and CT gold standard | + | + | |
| Waist Circumference, cm | WC | Tape measure | + | + | + |
| Thigh Circumference, cm | TC | Tape measure | + | ||
| Neck Circumference, cm | NC | Tape measure | + | ||
| Hip circumference, cm | HC | Tape measure | + | + | |
| Total abdominal adipose tissue, cm2 | TAAT | Measured by RMI | + | ||
| Subcutaneous adipose tissue, cm2, or as CT/MRI | SAT | Measured or calculated by anthropometric measures, MRI and CT gold standard | + | ||
| Subcutaneous abdominal adipose tissue, cm2, or as CT/MRI | SAAT | Measured or calculated by anthropometric measures, MRI and CT gold standard | + | ||
| Waist-to-hip ratio | WHR | Calculated (WC/HC) | + | + | + |
| Waist-to-height ratio | WHtR | Calculated (WC/h) | + | + | + |
| Waist-to-thigh ratio | WTR | Calculated (WC/TC) | + |
h, height in meters; L, litres; ml, millilitres; Kg, kilograms; gr, grams; BIA, bioelectrical impedance analysis; DXA, dual-energy X-ray absorptiometry; CT, Computer Tomography; MRI, Magnetic Resonance Imaging
A BMI between 25 and 29.9 identifies an overweight individual, a BMI of 30 or more indicates individuals with obesity [2].
In people with an Asian, Chinese, Middle Eastern, Black African, or Afro-Caribbean family background, obesity classes 2 and 3 are usually identified by reducing the values used for Caucasian people by 2.5 kg/m2, because they are prone to central adiposity and their cardiometabolic risk occurs at a lower BMI. In these populations overweight and obesity start, respectively, at BMI 23 kg/m2 and 27.4 kg/m2 [9]. Table 1 reports obesity classification based on BMI values and waist circumference cutoff [19].
Take-home message
Although CT and MRI are the gold standard for adipose tissue quantification and localization these methods are infrequently used in clinical practice. BMI and waist-related measures (WC, WHtR, WHR) cannot completely replace them but, in a simple daily clinical purpose, can be used as excellent screening tools. They should be integrated, in individual cases, with additional tools for a better definition of individual patient body composition and related risk (DXA, BIA) [9, 15].
Epidemiology
More than 50% and nearly 15% of adults in the Organisation for Economic Co-operation and Development (OECD) countries are, respectively, overweight or obese [22]. In Italy, 35% of the population is overweight and more than 9.8% is obese [23]. In high-income countries, such as the United States, nearly, 40% of adults met the BMI criteria for obesity in 2015–2016, with approximately 8% meeting criteria for grade 3 obesity (6.2% in males and 10.5 in females) [24].
In 2015, all over the world 107.7 million children and 603.7 million adults were living with obesity [25]. The overall prevalence of obesity was 5% among children and 12% among adults [26]. The expected growth is impressive. The United States, Mexico, and England are expected to have 47%, 39%, and 35% of the population obese, respectively [22]. A large increase in overweight and obesity is also evident in low- and middle-income countries [25].
Take-home message
Epidemiology shows that it is very difficult for physicians, regardless of their specialty, not to encounter patients with obesity in their clinical practice.
Energy homeostasis
Human beings can regulate the amount of adipose tissue possessed in the long term using homeostatic systems that modify caloric consumption and food intake based on their own energy reserves [27].
The brain and peripheral organs communicate intensely and bidirectionally to regulate the energy balance. In the brain, the hypothalamus is the main target for neuronal, hormonal, or food-derived chemical signals that activate neural circuits with orexigenic or anorexigenic functions [28].
A reduction in fat mass activates biological systems that cause a reduction in metabolism and an increase in hunger [29]. On the contrary, an increase in food intake leads to an increase in energy consumption and a sense of satiety [29]. These two pathways, together create a homeostatic energy system, and are intensely influenced by genetic, environmental, and behavioural factors.
In humans, the mechanism that is supposed to protect against excessive fat mass expansion appears to be less efficient than the system that regulate energy balance in case of reduced reserves. The reasons why this occurs have not yet been clarified [30]. Obesity generally occurs when a genetically predisposed individual lives in an obesogenic environment for a long period.
Environmental factors are probably the most influential elements of the epidemic weight gain documented in the last 30 years [31, 32]. Several changes that have affected the labour market as well as personal life, and leisure, have led to a sedentary lifestyle. This, combined with the easy availability of highly processed food creates the conditions for weight gain. In addition, people living in high-income countries are bombarded with advertisements touting cheap food and drinks that should allow the achievement the hypothetical happiness in everyday life. Despite this, among individuals exposed to the same environmental conditions, there is a notable difference in FM suggesting a complex interaction between individual characteristics and environment. Evidence for relevant genetic contributions to body weight comes from family, twin, and adoption studies [33–36], and both human and animal models [33–37].
Genetics can contribute in many ways to generating and maintaining obesity [38–40]. Genetic mutations affecting some specific key proteins of energy homeostasis have been reported [41]. However, these mutations account for a minority of obesity cases. In the vast majority of cases, the individual propensity derives from a set of genes which individually give only a modest contribution, but all together determine an important individual predisposition [37–40]. Large-scale human genome-wide association studies (GWAS) have identified > 500 genetic loci statistically associated with obesity or increased WHR. Although it is not clear what is the function of these identified loci and, more importantly, to what molecular mechanisms the stronger predisposition of some populations compared with others is due, it seems clear that given equal environmental exposure, genetics plays a fundamental role in defining who will be affected by obesity and who among these individuals will more easily develop the common complications [39].
In experimental rat models, destruction of the ventral hypothalamic portion rapidly leads to an overfeeding compulsion in animals, making them develop obesity in a short time [42]. In contrast, stimulation of the same areas leads to a reduction in food craving and consequent weight loss [43]. After these pioneering works, other hypothalamic centres have been identified [44]. These centres are correlated in some way with different moments of eating, such as the phase of food seeking, the moment in which the food is introduced into the body, and with the feeling of satiety [28]. Moreover, studies on the neuronal circuits that trigger feeling of satiety and hunger have shown how a high fat diet (HFD) alters the functioning of some of these circuits and causes the patient to continue consuming unhealthy foods over time [45]. These data show that difficulty in changing diet may also have neural causes and that obesity activates a self-reinforcing harmful cycle [45]. A HFD maintained for a sufficiently long period of time may also induce anatomic changes in the hypothalamus, mainly due to local inflammatory processes [46]. These processes, which have been widely demonstrated in animal models [29, 46–51] and that have been proved to occur in humans as well [47], may be the cause of the difficulty in reducing food intake and may be an organic reason for the maintenance of obesity [29, 46–50].
In human and animal models, some studies seem to show that maternal obesity and maternal nutrition have an impact on the future health of the offspring [52–55]. HFD even during breastfeeding alters hypothalamic melanocortin circuitry, leading to malformation of neuronal projections [55]. The development of the hypothalamus appears to be modulated by the maternal diet, which affect its microscopic anatomy and its function, leading to changes in offspring energetic homeostasis [55]. If a high-fat diet depends on environmental and individual behaviour, it should be emphasized that not all individuals respond to this diet in the same way. Genetics likely plays an important role in determining the magnitude of the inflammatory response to environmental stimuli, although this aspect is not yet well-understood [56, 57].
Summarizing and simplifying the neurohumoral system that regulates energy balance and reserves, we can say that leptin, ghrelin, insulin, and various types of nutrients, especially fatty acids, bind to receptors on first-order neurons located in the nucleus arcuatus of the hypothalamus [49, 58]. These cells are connected by a neuronal network to second-order neurons located in the paraventricular nucleus, which has an anorexigenic function, and the lateral hypothalamic area which, in contrast, has a predominantly orexigenic function [49, 58].
Two orexigenic neuropeptides, neuropeptide Y (NPY) and agouti-related protein (AgRP), are produced by first-order neurons. They stimulate second-order neurons in the lateral hypothalamic area to produce orexin (ORX) and melanin-concentrating hormone (MCH), and inhibit second-order neurons in the paraventricular nucleus [49, 58] to produce oxytocin (OT), thyrotropin-releasing hormone (TRH), and corticotropin-releasing hormone (CRH).
In contrast, the anorexigenic neuropeptides proopio-melanocortin (POM) and cocaine- and amphetamine-regulated transcript (CART), which are produced by first-order neurons, have an opposite effect, i.e., they stimulate the paraventricular nucleus, area that has an anorexigenic effect on behaviour, and inhibit second-order neurons located in the lateral hypothalamic area which on the contrary produce an orexigenic effect [49, 58].
Other extra-hypothalamic circuits are involved in feeding control [49, 58]. The mesolimbic reward system, the nucleus accumbens, the nucleus tractus solitarius, the nucleus parabrachial, the ventral cortex, the tegmental cortex, and other sites are also involved in different ways in the process of food intake regulation [58]. Reward-related brain regions are deeply involved in excess weight gain. They are stimulated by the sight of desired foods and, through unconscious processes of learning/conditioning mechanisms, promote further craving and pursuit of these foods regardless of hunger feeling [59].
In addition to a neuronal system, energy homeostasis is also controlled by a circulating humoral system whose main element is leptin [60]. The two systems are closely linked. Leptin is a 16 kilodalton protein (167 amino-acids) that is produced primarily by white adipose tissue and mediates numerous functions in the body [60]. The gene encoding leptin (Ob) is expressed not only in white adipose tissue but also in the stomach, placenta, and mammary glands [60]. Serum leptin levels are positively correlated with fat mass [60]. Leptin increases after the meal and decreases during fasting, which suggests a direct role in informing the central nervous system about the amount of fat available in the stores and the energy balance, suppressing the feeling hunger and promoting the feeling of satiety [61]. Leptin is released into the bloodstream, where it can be detected both freely and bound to the soluble form of its receptor [62]. Leptin also acts by binding to specific receptors in the central nervous system by altering the expression of various neuropeptides [63]. Since leptin is produced mainly in adipose tissue and its preferred target is in the central nervous system, there must be a system through which it passes the blood–brain barrier. It is likely that entry into the central nervous system is mediated by an active system that can be saturated, which explain at least in part, the phenomenon of leptin resistance [64]. Although regulation of fat stores is probably its main function, leptin also has other functions and plays an important role in lactation, regulates bone density and immune system functions, mediates pathophysiological processes activated in pathological conditions as diabetes and hypertriglyceridemia [63, 65]. In fact, leptin receptors are also expressed in many peripheral tissues, such as lung, kidney, liver, pancreas, adrenal glands, ovaries, hematopoietic stem cells and skeletal muscle [60]. Alteration of leptin structure, an inability to bind to its specific receptor or leptin resistance can lead to obesity through complex and not fully understood mechanisms [61]. The discovery of leptin [66], adiponectin [67], ghrelin [68] and many other hormones and cytokines [69] produced by adipose tissue, gives this tissue a role that goes far beyond energy storage, and leads to identify it as the largest endocrine organ [70]. A complete description of all hormones and cytokines and their functions as well as all neuronal circuits and cell types involved in energy homeostasis, although fascinating, is beyond the scope of this text [28, 42–44, 63, 69, 70].
Take-home messages
The hypothalamus (the main control centre of energetic homeostasis), the mesolimbic system (involved in the reward network), and the prefrontal cortex (the centre responsible for executive control) are closely connected to each other. They regulate food intake in response to environmental stimuli and/or bodily needs [44, 45, 59]. This neuro-endocrine central system constantly receives information from the periphery about the amount of adipose tissue present and about energy balance [49]. The neuro-endocrine system that regulates energy homeostasis also includes circulating mediators, the main one being leptin.
Neurons and glial cells in the hypothalamus jointly regulate various metabolic functions in response to information coming from the periphery, from adipose tissue, and the gut [71].
Hypothalamic inflammation could be the primary mechanism leading to unwanted weight loss or obesity [50]. Obesity creates a self-reinforcing harmful cycle [45].
Causes of obesity
In general, patient management includes a diagnostic phase, with the collection of anamnestic data and objective information and a subsequent treatment strategy proposal. Unfortunately, most of these steps are often overlooked or sometimes skipped in the management of patients with obesity.
The diagnosis of obesity often coincides with the finding of a BMI of 30 kg/m2 or more. The search for modifiable causes and the presence of conditions favouring the development or maintenance of obesity are usually omitted. Indeed, when physicians frequently focus on the management of obesity, they directly propose to the patient a strategy aimed at reducing the adipose tissue or the consequences of their obesity.
In clinical practice, it must be considered that obesity is a multifactorial disease. In simple terms, it is a chronic disease that occurs when the amount of calories ingested exceeds the amount consumed. Although the amount of calories supplied depends on the quantity and quality of food ingested, and the amount of those consumed depends primarily on the level of the physical activity (apart from basal metabolic rate), many factors can influence both calorie intake and expenditure.
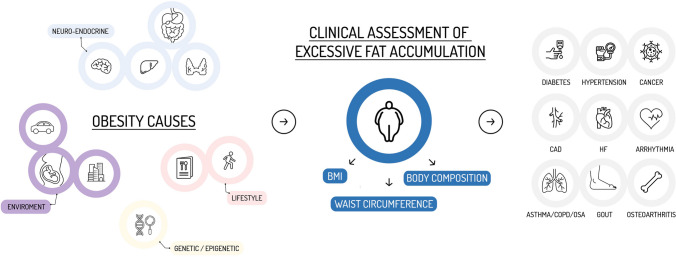
Individual factors (genetic [72, 73], epigenetic [73, 74], immunological [75], endocrinological [76], pharmacological [77] or behavioural [78]) and environmental factors [79] contribute in different ways in each person to the development of a chronic caloric excess that generates and maintains the excess adipose tissue (Fig. 1) [77, 80].
Fig. 1.
Causes, assessment, and consequences of obesity
The clinical conditions that can produce or maintain an abnormal amount of adipose tissue have been summarize by van der Valk et al. [77] into six groups. These include genetic or syndromic, hypothalamic, endocrine, pharmacological, mental, or lifestyles-related conditions. It is not easy for a cardiologist to know and remember all these clinical conditions, but it is much more difficult to understand the importance and relative weight that each factor has in the single patient. Sometimes, a medical condition is likely to be a cause, other times the same condition can be a consequence of obesity, such as hypothyroidism and hypogonadism [77]. For these reasons, a multidisciplinary approach is mandatory. A working team should include physicians specialized in obesity (obesiologists, cardiologists, pneumologists and bariatric surgeons), dietitians, clinical psychologists, exercise trainers, nurse trainers, social workers.
A mono-disciplinary approach is less effective [81].
Throughout the diagnostic assessment of patients with obesity, every element that is known to potentially contributes to produce or to maintain abnormal fat tissue should be systematically investigated. Genetics, endocrine diseases, medications, prenatal dietary influences of the mother and postnatal dietary influences of both mother and patient, unhealthy diet, low physical activity, a behaviour with unhealthy habits, and the diet culture are all factors that contribute to the genesis of the increase in fat mass. All the elements mentioned above are intertwined with each other, sometimes being obesity cause, sometimes the consequence. In the individual, to deal with this complexity, it is necessary to search, identify, and modify the single thread of the skein through a multidisciplinary approach. The patient should receive concrete tools, such as drugs, but this might not be enough. They must become aware of the scenario in which they move, the elements at play, and the ways to impact on them.
Take-home message
The cardiologist must become aware that obesity is a chronic and complex disease [2].
The evaluation of a patient with obesity must include the search for causes or favouring conditions [77]. A multidisciplinary team should perform the complex diagnostic assessment [81–85].
If the cardiologist is not a part of a multidisciplinary team, he should advise the patient to contact one by providing the relevant contact during the visit.
Health consequences of obesity
Numerous studies highlight that excess body weight is a major risk factor for mortality and morbidity [25]. At least 4.0 million deaths are thought to be attributable to obesity each year worldwide [25]. Obesity is a medical problem [81]. It is not simply a phenotype but itself a disease in its own right [86, 87], intricately linked with many other diseases and risk factor [25].
However, a high BMI is not necessarily associated with risk factors for other diseases, organ damage, or comorbidities. In addition, obesity-related psychological symptoms or functional limitations may result from a specific patient predisposition or the duration of obesity persistence. For this reason, it is vital to classify obesity not only based on weight but also on the previously mentioned factors. [88]. The Edmonton Obesity Staging System (EOSS) is a frequently used classification to better describe the patient and to better identify the presence of obesity-related risk factors, physical symptoms, psychological symptoms, functional limitations, or comorbidities [88]. It aids clinical decision-making. An EOSS stage 3 has been found to predict clinical outcomes [89, 90]. Among adults with overweight or obesity, EOSS is a more accurate predictor of polypharmacy and health service use than the BMI [90]. Furthermore, a higher perioperative surgical risk in subjects undergoing bariatric surgery with similar BMI has been found in patients with higher EOSS stages [91]. In addition, at the individual level, a clinical staging such as EOSS predicts mortality better than BMI [92]. Table 4 reports a simplified version of EOSS [88, 90, 93].
Table 4.
Schematic report of the Edmonton Obesity staging system
| Area | Stage 0 | Stage 1 | Stage 2 | Stage 3 | Stage 4 |
|---|---|---|---|---|---|
| Clinical | No risk factor | Subclinical risk factor | Established disease | Severe disease | End stage disease |
| Mental | No risk factor | Subclinical risk factor | Established disease | Severe disease | End stage disease |
| Functional | No risk factor | Subclinical risk factor | Established disease | Severe disease | End stage disease |
Other clinical staging systems have also been proposed to be added to the anthropometric evaluations to better define the patient's health needs and help clinicians in their decisions making, for example, the King's System [94], and the Cardiometabolic Staging System [95]. The latter is focused on the attempt to identify individual cardiovascular risk.
Table 5 summarizes most of diseases related to excess of fat tissue. They could be divided in a simplistic way in two broad categories. The first comprises all clinical situations correlated with the state of chronic inflammation resulting from the increase in adipose tissue, especially visceral, and circulating mediators release, and the second includes the consequences of the mechanical effects of increased body weight and body shape changes (Fig. 2).
Table 5.
Obesity-related disease
| Disease | References |
|---|---|
| Asthma | [93, 94, 96, 97] |
| COPD | [93, 95, 96, 98] |
| OSA | [96, 97, 99, 100] |
| IHD | [98, 99, 101, 102] |
| Hypertension | [100, 101, 103, 104] |
| Ischemic Stroke | [21] |
| Metabolic Disease | [100, 102, 103, 105] |
| Gallbladder | [103, 106] |
| Metabolic Syndrome | [3, 104, 105, 107, 108] |
| Diabetes | [106, 109] |
| Dyslipidemia | [100, 103] |
| Gout | [107, 110] |
| Non-alcoholic fatty liver disease | [108, 111] |
| Venous thromboembolic disease, | [109, 112] |
| Pulmonary embolism | [110, 113] |
| Heart failure | [111, 112, 114, 115] |
| Arrhythmias | [113, 114, 116, 117] |
| Cancer | [115, 116, 118, 119] |
| Colon | [117, 118, 120, 121] |
| Kidney | [117, 119, 120, 122, 123] |
| Oesophagus | [117, 121, 120, 124] |
| Endometrium | [117, 120, 122, 123, 125, 126] |
| Postmenopausal breast | [117, 120, 122, 123, 125, 126] |
| Liver | [124–126, 127-129] |
| Pancreas | [127, 128, 130, 131] |
| Thyroid | [129, 132] |
| Osteoarthritis | [130, 133] |
| Depression, anxiety, and other mental disorders | [131–134, 136] |
CVD, cardiovascular disease; COPD, Chronic Obstructive Pulmonary Disease; IHD, Ischaemic Heart Disease; OSA, Obstructive Sleep Apnoea
Fig. 2.
Dual consequences of obesity: mechanical and humoral-metabolic effects
Take home message
Obesity is a medical problem. Patients with similar BMI may have different metabolic conditions, different fit status, and different cardiovascular risk. The EOSS can assist in better understanding the patient health status, and the risk of morbidity or death.
Obesity paradox
Although epidemiological studies have shown that the presence of obesity is associated with numerous diseases, as reported in Table 5, for some specific diseases, a better outcome has been reported in those overweight or with first-degree obesity (BMI ≥ 30 kg/m2 and < 35 kg/m2), compared to those who had a BMI < 25 kg/m2 [137]. Since the first identification of this counterintuitive finding, numerous similar studies have been published in different fields, such as cardiovascular diseases [138], cancer [139], diabetes [140], respiratory diseases [141] and in other clinical contexts [142]. A recent large cohort study including patients with stable coronary heart disease has found a U‐shaped relationship between BMI and cardiovascular outcomes, with the lowest cardiovascular risk in patients with a BMI of 27 kg/m2, which are usually classified as overweight patients [143].
This topic has also been examined through rigorous meta-analyses [144–149] but its interpretation remains not yet clear. Possible explanations range from the real existence of the phenomenon [150], to the presence of various population selection biases [149–152], or the lack of discriminatory power of BMI to differentiate between body fat and lean mass [153].
An interesting clarification of this controversy could come from the distinction between metabolically healthy and metabolically unhealthy obesity, probably considering the former as a transitional phenotype towards the latter [154]. The distinction between these two forms of obesity is not easy. The presence of normal glucose metabolism, normal insulin sensitivity, no systemic arterial hypertension, no drug treatment for dyslipidaemia, diabetes, or hypertension, and no cardiovascular disease manifestation can be used in daily clinical practice to distinguish the two forms of obesity [154]. However, other aspects, such as, for example, the alteration in the secretion of the various cytokines produced by the adipose tissue or the presence of a chronic inflammatory state, if present, are not easy to identify. Of note, a study on heart failure (HF) patients recently showed no evidence of obesity paradox in terms of mortality when using an anthropometric measure different from BMI: the waist-to-height ratio [155]. Overall, to identify obesity risks, an index more efficacious in detecting greater adiposity than the BMI should be used, both in clinical studies, and clinical practice.
Take home message
Obesity paradox is a not yet clearly defined phenomenon. Studies that use an obesity index different from BMI are needed to verify the hypothesis of the existence of an obesity paradox phenomenon in cardiovascular diseases.
Cardiovascular diseases
Cardiologists are deeply involved in the evaluation of obesity and play a pivotal role in this field for several reasons. First, they have a high likelihood of encountering patients with this condition. Second, the cardiovascular risk profile is among the most crucial elements to quantify to determine the additional risk posed by obesity and to assess the extent of clinical benefit that an individual patient can achieve through weight loss [156].
Although the relationship between obesity and cardiovascular disease is very complex due to the presence of many confounding factors, Mendelian randomization studies strongly show a causal relationship [157].
Obesity is linked to many cardiovascular diseases, including stroke [158], venous thromboembolic disease [112], pulmonary embolism [113], HF [114], and arrhythmias, especially sudden cardiac death (SCD) [116] and atrial fibrillation (AF) [117]. Furthermore, it causes specific issues in key topics for cardiologic patient management, such as differences in specificity and sensitivity in non-invasive and invasive diagnostic tools [159], changes in platelet reactivity [160, 161], a different short- and long-term outcome after percutaneous coronary intervention PCI [162–164] or cardiac surgery [159].
Coronary artery disease and obesity
Patients affected by obesity show some differences in disease pathophysiology, sensitivity, and specificity of diagnostic tools, and in outcomes when compared with normal weight patients [159].
Overweight and obesity are associated with elevated coronary artery disease (CAD) risk at least in part independent of blood pressure and cholesterol levels [157, 165].
The link between increased cardiovascular risk and obesity can be explained by multiple mechanisms [166], such as increased incidence of hypertension [103, 104], type II diabetes [109] and insulin resistance [167], hypercholesterolemia [103], systemic inflammation [168], endothelial dysfunction [169] and increased platelet aggregability [161].
Weight loss improves systemic inflammation, endothelial dysfunction, and related atherosclerotic risk factors for coronary artery disease, such as hypertension, metabolic syndrome, and diabetes [159].
CAD diagnostic assessment
Electrocardiography, stress test including ergometric ECG test, nuclear medicine tests, stress echocardiography, or MRI, coronary artery calcium (CAC) scan screening, CT, and coronary angiography are CAD evaluation methods that have some specific limitations in patient living with obesity.
The electrocardiographic criteria of normality in patients with obesity may be different from those for patients with normal weight, and several electrocardiographic changes are associated with obesity resulting in lower ECG sensitivity and specificity [159].
In patients with obesity, treadmill or cycle-ergometer ECG stress tests have some limitations. The patients could not achieve the maximal theoretical heart rate for orthopaedic limitations or some degree of chronotropic incompetence [170]. Pulmonary dysfunction has been described and can limit the attainable level of work [171].
Single-photon emission CT, stress echocardiography, and cardiac CT coronary angiography all have limitations for patients with obesity [159]. The sensitivity and specificity of these techniques may decrease compared to those of normal size patients [159]. Conversely, stress cardiac MRI and rubidium PET myocardial perfusion imaging [172] may offer better results. Therefore, PET rubidium, if available, should be the nuclear imaging technique of choice for patients with obesity [172].
As far as invasive examinations are concerned, the major problems concern the difficulty in vascular access and radioscopic views. In some cases, the angiography tables may have limitations in terms of weight they can support.
Heart failure
Obesity is a major risk factor for HF development [115, 173]. When an obese patient has HF in the absence of other factors that justify it, we can refer to it as obesity cardiomyopathy [174]. Obesity causes several functional and structural changes that may lead to HF. Among these we can mention arterial hypertension, respiratory dysfunction, the increase in circulating blood volume and cardiac output, vascular remodelling, sleep apnoea syndrome, the presence of chronic systemic inflammation, abnormal secretion by the adipose tissue of numerous chemical mediators [174, 175].
A substantial weight loss positively modifies many hemodynamic parameters involved in HF development and progression. Among them we can find cardiac output, central blood volume, stroke volume and stroke work, systemic and pulmonary pressure [176].
The reduction in systemic blood pressure is probably the most relevant hemodynamic element that is observed with weight loss and may improve cardiovascular function [176].
Sudden cardiac death
Several studies identified a close relationship between obesity and the risk of SCD [177, 178]. The pathophysiological mechanisms underlying this association are numerous. Among them there is a greater number of traditional risk factors for cardiovascular diseases, the presence of both electrical and structural ventricular remodelling, the presence of chronic inflammation and of an autonomic nervous system imbalance [178].
It is not known whether weight reduction is able to modify the incidence of sudden death in this category of patients. In a Swedish study that followed 2010 patients after bariatric surgery [179] for about 11 years, a statistically non-significant increase in sudden death was observed compared to the control group, whereas a reduction in global mortality was observed in the surgery group. Further studies on this topic are needed to understand the relationship between obesity and sudden death and the consequences of weight loss.
Atrial fibrillation
Increased BMI is an established risk factor for the development of AF [180]. These data have already been highlighted many years ago by monitoring the postoperative period after cardiac surgery [181].
Furthermore, weight reduction corresponds to a reduced risk of developing AF [182], while the persistence of obesity favours the transition from paroxysmal to persistent atrial fibrillation [183].
A 1 kg/m2 increase in BMI was associated with a 4.7% increase in the likelihood of experiencing an episode of AF [184]. Conversely, a reduction of 1 kg/m2 was associated with a 7% reduction in AF incidence [182].
Although the concept of obesity paradox in which a reduction in mortality is observed in overweight or moderately obese patients compared to patients of normal weight, has been reported in AF patients, a study which set out to analyse non-healthy and healthy obesity effect showed an increase in the incidence of this arrhythmia also in the latter group of patients [185].
Obesity can induce AF through several mechanisms. First, it contributes to several hemodynamic changes, diseases, or cardiovascular disease risk factors, such as arterial hypertension, type II diabetes, sleep apnoea, volume overload, left ventricular remodelling, which in turn may contribute to AF occurrence. Furthermore, obesity also determines a series of histological and biochemical changes closely related to arrhythmic risk. The increase in epicardial fat, along with the increase in the production of inflammatory and profibrotic mediators, which have both endocrine and paracrine effects, may explain the higher risk of AF among patients with obesity [180]. Of note obesity may also affect anticoagulant drug pharmacokinetics and pharmacodynamics and in patients with severe obesity the anticoagulant treatment must be individualized [142].
Take home message
Ischemic heart disease, HF, arrythmias are more frequent in patients with obesity than in the general population. Patients affected by obesity exhibit some differences in cardiovascular pathophysiology, sensitivity, and specificity of diagnostic tests, as well as outcomes when compared to normal-weight patients.
Executive summary
Approaching a patient with obesity is not easy for many reasons. First, the patient may not be ready to face the problem; he/she may have internalized the stigma to which he/she has certainly been subjected. He/she may feel that he/she does not have the strength to face the obstacles that stand in the way of losing weight. Furthermore, BMI is not adequate to measure body composition neither to identify which patients are most prone to obesity-related complications. Different tools and methods are needed to correctly classify patients and support clinical decisions. In addition to BMI the WC, WHR, and WHtR should be used for clinical purposes (Table 1). Clinical staging systems should also be used to better identify the global health status of the patients and the risk of death or disease.
Very often these patients have experienced numerous failures in weight loss in their past or suffer from of real eating disorders. International guidelines [186] propose a systematic approach through the application of a method that can be summarized in “5As”: Ask permission, Assess their story, Advice on management, Agree on goals, Assist with drivers and barriers.
The cardiologist has a high probability of encountering patients who live with obesity in their clinical practice and, therefore, must become a privileged interlocutor for these patients.
It is necessary to recognize that obesity is not the consequence of laziness or weakness of character and become aware that factors that lead to obesity are almost never controllable by the patient without a professional support.
Cardiologists must develop the knowledge necessary to relate to patients affected by obesity and learn to distinguish which patients are at higher risk of poorer outcomes. In routine practice the assessment of a patient with obesity, as defined with BMI measurement, or with a suspicion of excess body fat, must include additional measurements to estimate fat distribution (WC, WHR, WHtR). Table 6 reports the main laboratory tests to consider in the evaluation of patients with obesity.
Table 6.
Laboratory tests in the evaluation of patients with obesity
| Renal function tests (creatinine, eGFR), electrolytes (sodium, potassium, magnesium, calcium) |
| HbA1c |
| Total cholesterol, HDL- and LDL-cholesterol, triglycerides |
| Alanine aminotransferase and Aspartate aminotransferase |
| Complete blood cell count |
| Thyroid stimulating hormone |
| Uric acid |
| Assessment of iron (total iron binding capacity; % saturation, serum ferritin, serum iron) |
| Vitamins B12 and D levels |
| Urinalysis |
| Urine for micro-proteinuria |
| Women with suspect of polycystic ovary syndrome |
| LH, FSH, total testosterone, DHEAS, prolactin and 17 hydroxyprogesterone level |
LH, luteinizing hormone; FSH, follicle stimulating hormone; DHEAS, dehydroepiandrosterone
Since the disease is very complex, a multidisciplinary approach is essential in both the diagnostic and therapeutic phases. The latter must include curative diet therapy, the prescription of drugs with documented efficacy, psychological and social support, adequate physical activity and, if necessary, bariatric surgery.
Conclusion
Obesity is a complex, chronic, and relapsing disease [2]. Due to a rapid spread of an obesogenic environment and a genetic predisposition that affects a large part of the human population, obesity has become an epidemic and is spreading in all countries of the world with a growing prevalence [22–25].
Patients living with obesity have a high probability of developing risk factors for cardiovascular diseases, such as systemic arterial hypertension, type II diabetes mellitus, sleep apnoea, and dyslipidaemia [26]. The risk of developing ischaemic heart disease, sudden death, heart failure, and atrial fibrillation is also high [159, 187].
In the near future the increase in the prevalence of the disease will also lead to an increase in its consequences, but it is also envisaged a significant increase in the weapons at our disposal. The pharmacological treatment of obesity is currently limited to a small number of drugs but a considerable increase in available products in the coming years is expected thanks to the increasing knowledge of the obesity physiopathology and the mechanisms of the energy homeostasis regulation [188].
The possibility of halting and reversing the spread of obesity will probably depend on our ability to propose a systemic view of the disease and a close collaboration among all the professional figures involved. A single discipline approach will certainly be less effective.
Strength and limits
"This paper represents a scientific statement from the largest scientific society of Italian cardiologists. Therefore, it can be an important tool for increasing awareness about obesity among cardiologists, improving the quality of knowledge, and consequently, the quality of care. The main limitation stems from the unsystematic approach to the analysis of the literature. However, this element is not required, given the very nature of the paper as a scientific statement."
What is already known on this subject?
Patients with obesity consult doctors from numerous specializations, and among these, cardiologists are certainly some of the most frequently visited due to comorbidities and the increased risk of cardiovascular issues. Despite this, it is not always easy for doctors who do not directly deal with obesity to understand the nature of obesity as a chronic pathology. This can lead to difficulties in implementing appropriate actions without resorting to simplistic or even stigmatizing clinical approaches and therapeutic proposals.
What this study adds?
This paper reviews the literature to provide cardiologists with a theoretical and practical framework for offering adequate care to patients with obesity. This care is approached from a global perspective, with specific reference to cardiovascular pathology.
Author contributions
Conceptualization, SADF, EM and FC; writing/original draft preparation EM, SADF, MG and FO; supervision, MMG, FC and DG; All authors reviewed the manuscript.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement.
Data availability
Not applicable.
Declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Stefania Angela Di Fusco and Edoardo Mocini have contributed equally to this work.
References
- 1.Talumaa B, Brown A, Batterham RL, Kalea AZ. Effective strategies in ending weight stigma in healthcare. Obes Rev. 2022;23(10):e13494. doi: 10.1111/obr.13494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Obesity and overweight. 2023 https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed 3 July 2023.
- 3.Ritchie SA, Connell JMC. The link between abdominal obesity, metabolic syndrome and cardiovascular disease. Nutr Metab Cardiovasc Dis. 2007;17(4):319–326. doi: 10.1016/j.numecd.2006.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Neeland IJ, Ross R, Després JP, et al. Visceral and ectopic fat, atherosclerosis, and cardiometabolic disease: a position statement. Lancet Diabetes Endocrinol. 2019;7(9):715–725. doi: 10.1016/S2213-8587(19)30084-1. [DOI] [PubMed] [Google Scholar]
- 5.Bray GA. Beyond BMI. Nutrients. 2023;15(10):2254. doi: 10.3390/nu15102254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donini LM, Busetto L, Bischoff SC, et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Obes Facts. 2022;15(3):321–335. doi: 10.1159/000521241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caleyachetty R, Barber TM, Mohammed NI, et al. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. Lancet Diabetes Endocrinol. 2021;9(7):419–426. doi: 10.1016/S2213-8587(21)00088-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Expert Consultation Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 9.Overview. Obesity: identification, assessment and management. Guidance | NICE. 2014. https://www.nice.org.uk/guidance/cg189. Accessed 23 May 2023.
- 10.Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev Off J Int Assoc Study Obes. 2010;11(1):11–18. doi: 10.1111/j.1467-789X.2009.00623.x. [DOI] [PubMed] [Google Scholar]
- 11.Huang LY, Chiu CJ, Hsing CH, Hsu YH. Interferon family cytokines in obesity and insulin sensitivity. Cells. 2022;11(24):4041. doi: 10.3390/cells11244041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bays HE. Adiposopathy is “sick fat” a cardiovascular disease? J Am Coll Cardiol. 2011;57(25):2461–2473. doi: 10.1016/j.jacc.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 13.Fuster JJ, Ouchi N, Gokce N, Walsh K. Obesity-induced changes in adipose tissue microenvironment and their impact on cardiovascular disease. Circ Res. 2016;118(11):1786–1807. doi: 10.1161/CIRCRESAHA.115.306885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borga M, West J, Bell JD, et al. Advanced body composition assessment: from body mass index to body composition profiling. J Investig Med Off Publ Am Fed Clin Res. 2018;66(5):1–9. doi: 10.1136/jim-2018-000722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cornier MA, Després JP, Davis N, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 16.Mooney SJ, Baecker A, Rundle AG. Comparison of anthropometric and body composition measures as predictors of components of the metabolic syndrome in a clinical setting. Obes Res Clin Pract. 2013;7(1):e55–66. doi: 10.1016/j.orcp.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 17.Radetti G, Fanolla A, Lupi F, Sartorio A, Grugni G. Accuracy of different indexes of body composition and adiposity in identifying metabolic syndrome in adult subjects with Prader-Willi syndrome. J Clin Med. 2020;9(6):E1646. doi: 10.3390/jcm9061646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fang H, Berg E, Cheng X, Shen W. How to best assess abdominal obesity. Curr Opin Clin Nutr Metab Care. 2018;21(5):360–365. doi: 10.1097/MCO.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rueda-Clausen CF, Poddar M, Lear SA, Poirier P, Sharma AM. Canadian adult obesity clinical practice guidelines: assessment of people living with obesity. Can Adult Obes Clin Pract Guidel Assess People Living Obes. https://obesitycanada.ca/guidelines/assessment. Accessed 21 July 2002.
- 20.Alberti KG, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 21.Samouda H, Dutour A, Chaumoitre K, Panuel M, Dutour O, Dadoun F. VAT=TAAT-SAAT: innovative anthropometric model to predict visceral adipose tissue without resort to CT-Scan or DXA. Obesity. 2013;21(1):E41–E50. doi: 10.1002/oby.20033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obesity Update - OECD. 2023. https://www.oecd.org/health/obesity-update.htm. Accessed 20 Nov 2023.
- 23.EpiCentro. Obesità - sovrappeso - Dati epidemiologici in Italia. 2021. https://www.epicentro.iss.it/obesita/epidemiologia-italia. Accessed 20 Nov 2023.
- 24.Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143(8):e254–e743. doi: 10.1161/CIR.0000000000000950. [DOI] [PubMed] [Google Scholar]
- 25.Templin T, Hashiguchi TCO, Thomson B, Dieleman J, Bendavid E. The overweight and obesity transition from the wealthy to the poor in low- and middle-income countries: a survey of household data from 103 countries. PLOS Med. 2019;16(11):e1002968. doi: 10.1371/journal.pmed.1002968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.GBD 2015 Obesity Collaborators. Afshin A, Forouzanfar MH, et al. Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. 2017;377(1):13–27. doi: 10.1056/NEJMoa1614362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Klaauw AA, Farooqi IS. The hunger genes: pathways to obesity. Cell. 2015;161(1):119–132. doi: 10.1016/j.cell.2015.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Alcantara IC, Tapia APM, Aponte Y, Krashes MJ. Acts of appetite: neural circuits governing the appetitive, consummatory, and terminating phases of feeding. Nat Metab. 2022;4(7):836–847. doi: 10.1038/s42255-022-00611-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seong J, Kang JY, Sun JS, Kim KW. Hypothalamic inflammation and obesity: a mechanistic review. Arch Pharm Res. 2019;42(5):383–392. doi: 10.1007/s12272-019-01138-9. [DOI] [PubMed] [Google Scholar]
- 30.Ravussin Y, Leibel RL, Ferrante AW. A missing link in body weight homeostasis: the catabolic signal of the overfed state. Cell Metab. 2014;20(4):565–572. doi: 10.1016/j.cmet.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.A different scale: Global action to address obesity. 2022. https://www.who.int/news-room/events/detail/2022/05/24/default-calendar/a-different-scale-global-action-to-address-obesity. Accessed 13 Nov 2023.
- 32.Romieu I, Dossus L, Barquera S, et al. Energy balance and obesity: what are the main drivers? Cancer Causes Control. 2017;28(3):247–258. doi: 10.1007/s10552-017-0869-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nan C, Guo B, Warner C, et al. Heritability of body mass index in pre-adolescence, young adulthood and late adulthood. Eur J Epidemiol. 2012;27(4):247–253. doi: 10.1007/s10654-012-9678-6. [DOI] [PubMed] [Google Scholar]
- 34.Faith MS, Pietrobelli A, Nuñez C, Heo M, Heymsfield SB, Allison DB. Evidence for independent genetic influences on fat mass and body mass index in a pediatric twin sample. Pediatrics. 1999;104(1 Pt 1):61–67. doi: 10.1542/peds.104.1.61. [DOI] [PubMed] [Google Scholar]
- 35.Silventoinen K, Magnusson PKE, Tynelius P, Kaprio J, Rasmussen F. Heritability of body size and muscle strength in young adulthood: a study of one million Swedish men. Genet Epidemiol. 2008;32(4):341–349. doi: 10.1002/gepi.20308. [DOI] [PubMed] [Google Scholar]
- 36.Yam P, Albright J, VerHague M, Gertz ER, Pardo-Manuel de Villena F, Bennett BJ. Genetic background shapes phenotypic response to diet for adiposity in the collaborative cross. Front Genet. 2020;11:615012. doi: 10.3389/fgene.2020.615012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Locke AE, Kahali B, Berndt SI, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518(7538):197–206. doi: 10.1038/nature14177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goodarzi MO. Genetics of obesity: what genetic association studies have taught us about the biology of obesity and its complications. Lancet Diabetes Endocrinol. 2018;6(3):223–236. doi: 10.1016/S2213-8587(17)30200-0. [DOI] [PubMed] [Google Scholar]
- 39.Loos RJ. The genetics of adiposity. Curr Opin Genet Dev. 2018;50:86–95. doi: 10.1016/j.gde.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fairbrother U, Kidd E, Malagamuwa T, Walley A. Genetics of severe obesity. Curr Diab Rep. 2018;18(10):85. doi: 10.1007/s11892-018-1053-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pigeyre M, Yazdi FT, Kaur Y, Meyre D. Recent progress in genetics, epigenetics and metagenomics unveils the pathophysiology of human obesity. Clin Sci Lond Engl 1979. 2016;130(12):943–986. doi: 10.1042/CS20160136. [DOI] [PubMed] [Google Scholar]
- 42.Brobeck JR. Neural control of hunger, appetite, and satiety. Yale J Biol Med. 1957;29(6):565–574. [PMC free article] [PubMed] [Google Scholar]
- 43.Hoebel BG, Teitelbaum P. Hypothalamic control of feeding and self-stimulation. Science. 1962;135(3501):375–377. doi: 10.1126/science.135.3501.375. [DOI] [PubMed] [Google Scholar]
- 44.Lechan RM, Toni R. Functional anatomy of the hypothalamus and pituitary. Endotext. MDText.com, Inc.; 2000. http://www.ncbi.nlm.nih.gov/books/NBK279126/. Accessed 23 Nov 2022. [PubMed]
- 45.Mazzone CM, Liang-Guallpa J, Li C, et al. High-fat food biases hypothalamic and mesolimbic expression of consummatory drives. Nat Neurosci. 2020;23(10):1253–1266. doi: 10.1038/s41593-020-0684-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jais A, Brüning JC. Hypothalamic inflammation in obesity and metabolic disease. J Clin Invest. 2017;127(1):24–32. doi: 10.1172/JCI88878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thaler JP, Yi CX, Schur EA, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122(1):153–162. doi: 10.1172/JCI59660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kreutzer C, Peters S, Schulte DM, et al. Hypothalamic inflammation in human obesity is mediated by environmental and genetic factors. Diabetes. 2017;66(9):2407–2415. doi: 10.2337/db17-0067. [DOI] [PubMed] [Google Scholar]
- 49.Le Thuc O, Stobbe K, Cansell C, Nahon JL, Blondeau N, Rovère C. Hypothalamic inflammation and energy balance disruptions: spotlight on chemokines. Front Endocrinol. 2017 doi: 10.3389/fendo.2017.00197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Barlampa D, Bompoula MS, Bargiota A, Kalantaridou S, Mastorakos G, Valsamakis G. Hypothalamic inflammation as a potential pathophysiologic basis for the heterogeneity of clinical, hormonal, and metabolic presentation in PCOS. Nutrients. 2021;13(2):520. doi: 10.3390/nu13020520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bhusal A, Rahman MH, Suk K. Hypothalamic inflammation in metabolic disorders and aging. Cell Mol Life Sci CMLS. 2021;79(1):32. doi: 10.1007/s00018-021-04019-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Steculorum SM, Vogt MC, Brüning JC. Perinatal programming of metabolic diseases: role of insulin in the development of hypothalamic neurocircuits. Endocrinol Metab Clin North Am. 2013;42(1):149–164. doi: 10.1016/j.ecl.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 53.Sullivan E, Grove K. Metabolic imprinting of obesity. Forum Nutr. 2010;63:186–194. doi: 10.1159/000264406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howie GJ, Sloboda DM, Kamal T, Vickers MH. Maternal nutritional history predicts obesity in adult offspring independent of postnatal diet. J Physiol. 2009;587(Pt 4):905–915. doi: 10.1113/jphysiol.2008.163477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vogt MC, Paeger L, Hess S, et al. Neonatal insulin action impairs hypothalamic neurocircuit formation in response to maternal high fat feeding. Cell. 2014;156(3):495–509. doi: 10.1016/j.cell.2014.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Szalanczy AM, Key CCC, Solberg Woods LC. Genetic variation in satiety signaling and hypothalamic inflammation: merging fields for the study of obesity. J Nutr Biochem. 2022;101:108928. doi: 10.1016/j.jnutbio.2021.108928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Galmés S, Cifre M, Palou A, Oliver P, Serra F. A genetic score of predisposition to low-grade inflammation associated with obesity may contribute to discern population at risk for metabolic syndrome. Nutrients. 2019;11(2):298. doi: 10.3390/nu11020298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Waterson MJ, Horvath TL. Neuronal regulation of energy homeostasis: beyond the hypothalamus and feeding. Cell Metab. 2015;22(6):962–970. doi: 10.1016/j.cmet.2015.09.026. [DOI] [PubMed] [Google Scholar]
- 59.Sinha R. Role of addiction and stress neurobiology on food intake and obesity. Biol Psychol. 2018;131:5–13. doi: 10.1016/j.biopsycho.2017.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mantzoros CS. The role of leptin in human obesity and disease: a review of current evidence. Ann Intern Med. 1999;130(8):671–680. doi: 10.7326/0003-4819-130-8-199904200-00014. [DOI] [PubMed] [Google Scholar]
- 61.Cui H, López M, Rahmouni K. The cellular and molecular bases of leptin and ghrelin resistance in obesity. Nat Rev Endocrinol. 2017;13(6):338–351. doi: 10.1038/nrendo.2016.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tartaglia LA, Dembski M, Weng X, et al. Identification and expression cloning of a leptin receptor. OB-R Cell. 1995;83(7):1263–1271. doi: 10.1016/0092-8674(95)90151-5. [DOI] [PubMed] [Google Scholar]
- 63.Akeel Al-hussaniy H, Alburghaif AH, Naji MA. Leptin hormone and its effectiveness in reproduction, metabolism, immunity, diabetes, hopes and ambitions. J Med Life. 2021;14(5):600–605. doi: 10.25122/jml-2021-0153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Banks WA. Leptin and the blood-brain barrier: curiosities and controversies. Compr Physiol. 2021;11(4):2351–2369. doi: 10.1002/cphy.c200017. [DOI] [PubMed] [Google Scholar]
- 65.Kelesidis T, Kelesidis I, Chou S, Mantzoros CS. Narrative review: the role of leptin in human physiology: emerging clinical applications. Ann Intern Med. 2010;152(2):93–100. doi: 10.1059/0003-4819-152-2-201001190-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhang Y, Proenca R, Maffei M, Barone M, Leopold L, Friedman JM. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372(6505):425–432. doi: 10.1038/372425a0. [DOI] [PubMed] [Google Scholar]
- 67.Fang H, Judd RL. Adiponectin regulation and function. Compr Physiol. 2018;8(3):1031–1063. doi: 10.1002/cphy.c170046. [DOI] [PubMed] [Google Scholar]
- 68.Nakazato M, Murakami N, Date Y, et al. A role for ghrelin in the central regulation of feeding. Nature. 2001;409(6817):194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]
- 69.Funcke JB, Scherer PE. Beyond adiponectin and leptin: adipose tissue-derived mediators of inter-organ communication. J Lipid Res. 2019;60(10):1648–1684. doi: 10.1194/jlr.R094060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Halberg N, Wernstedt-Asterholm I, Scherer PE. The adipocyte as an endocrine cell. Endocrinol Metab Clin North Am. 2008;37(3):753–768 x-xi. doi: 10.1016/j.ecl.2008.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lee CH, Suk K, Yu R, Kim MS. Cellular contributors to hypothalamic inflammation in obesity. Mol Cells. 2020;43(5):431–437. doi: 10.14348/molcells.2020.0055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Loos RJF. Genetic determinants of common obesity and their value in prediction. Best Pract Res Clin Endocrinol Metab. 2012;26(2):211–226. doi: 10.1016/j.beem.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 73.Thaker VV. Genetic and epigenetic causes of obesity. Adolesc Med State Art Rev. 2017;28(2):379–405. [PMC free article] [PubMed] [Google Scholar]
- 74.Ling C, Rönn T. Epigenetics in human obesity and type 2 diabetes. Cell Metab. 2019;29(5):1028–1044. doi: 10.1016/j.cmet.2019.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Barakat B, Almeida MEF. Biochemical and immunological changes in obesity. Arch Biochem Biophys. 2021;708:108951. doi: 10.1016/j.abb.2021.108951. [DOI] [PubMed] [Google Scholar]
- 76.Pasquali R, Casanueva F, Haluzik M, et al. European society of endocrinology clinical practice guideline: endocrine work-up in obesity. Eur J Endocrinol. 2020;182(1):G1–G32. doi: 10.1530/EJE-19-0893. [DOI] [PubMed] [Google Scholar]
- 77.van der Valk ES, van den Akker ELT, Savas M, et al. A comprehensive diagnostic approach to detect underlying causes of obesity in adults. Obes Rev Off J Int Assoc Study Obes. 2019;20(6):795–804. doi: 10.1111/obr.12836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Teixeira PJ, Marques MM. Health behavior change for obesity management. Obes Facts. 2017;10(6):666–673. doi: 10.1159/000484933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.World Health Organization. Regional Office for Europe. WHO European Regional Obesity Report 2022. World Health Organization. Regional Office for Europe; 2022. https://apps.who.int/iris/handle/10665/353747. Accessed 3 July 2023.
- 80.https://www.nhs.uk/conditions/obesity/causes/. Accessed 29 Nov 2023.
- 81.Hassapidou M, Duncanson K, Shrewsbury V, et al. EASO and EFAD position statement on medical nutrition therapy for the management of overweight and obesity in children and adolescents. Obes Facts. 2023;16(1):29–52. doi: 10.1159/000527540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Tsigos C, Hainer V, Basdevant A, et al. Management of obesity in adults: European clinical practice guidelines. Obes Facts. 2008;1(2):106–116. doi: 10.1159/000126822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Yumuk V, Tsigos C, Fried M, et al. European guidelines for obesity management in adults. Obes Facts. 2015;8(6):402–424. doi: 10.1159/000442721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Garvey WT, Mechanick JI, Brett EM, et al. American association of clinical endocrinologists and American college of endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2016;22(Suppl 3):1–203. doi: 10.4158/EP161365.GL. [DOI] [PubMed] [Google Scholar]
- 85.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25 Suppl 2):S102–138. doi: 10.1161/01.cir.0000437739.71477.ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Wilding JPH, Mooney V, Pile R. Should obesity be recognised as a disease? BMJ. 2019;366:l4258. doi: 10.1136/bmj.l4258. [DOI] [PubMed] [Google Scholar]
- 87.Gordon-Larsen P, Heymsfield SB. Obesity as a disease, not a behavior. Circulation. 2018;137(15):1543–1545. doi: 10.1161/CIRCULATIONAHA.118.032780. [DOI] [PubMed] [Google Scholar]
- 88.Sharma AM, Kushner RF. A proposed clinical staging system for obesity. Int J Obes. 2009;33(3):289–295. doi: 10.1038/ijo.2009.2. [DOI] [PubMed] [Google Scholar]
- 89.Ejima K, Xavier NA, Mehta T. Comparing the ability of two comprehensive clinical staging systems to predict mortality: EOSS and CMDS. Obes Silver Spring Md. 2020;28(2):353–361. doi: 10.1002/oby.22656. [DOI] [PubMed] [Google Scholar]
- 90.Atlantis E, Sahebolamri M, Cheema BS, Williams K. Usefulness of the Edmonton Obesity staging system for stratifying the presence and severity of weight-related health problems in clinical and community settings: a rapid review of observational studies. Obes Rev Off J Int Assoc Study Obes. 2020;21(11):e13120. doi: 10.1111/obr.13120. [DOI] [PubMed] [Google Scholar]
- 91.Chiappetta S, Stier C, Weiner RA. The Edmonton obesity staging system predicts perioperative complications and procedure choice in obesity and metabolic surgery—a German nationwide register-based cohort study (StuDoQ|MBE) Obes Surg. 2019;29(12):3791–3799. doi: 10.1007/s11695-019-04015-y. [DOI] [PubMed] [Google Scholar]
- 92.Padwal RS, Pajewski NM, Allison DB, Sharma AM. Using the Edmonton obesity staging system to predict mortality in a population-representative cohort of people with overweight and obesity. CMAJ. 2011;183(14):E1059–E1066. doi: 10.1503/cmaj.110387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Swaleh R, McGuckin T, Myroniuk TW, et al. Using the Edmonton Obesity Staging System in the real world: a feasibility study based on cross-sectional data. CMAJ Open. 2021;9(4):E1141–E1148. doi: 10.9778/cmajo.20200231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Aasheim ET, Aylwin SJB, Radhakrishnan ST, et al. Assessment of obesity beyond body mass index to determine benefit of treatment. Clin Obes. 2011;1(2–3):77–84. doi: 10.1111/j.1758-8111.2011.00017.x. [DOI] [PubMed] [Google Scholar]
- 95.Guo F, Moellering DR, Garvey WT. The progression of cardiometabolic disease: validation of a new cardiometabolic disease staging system applicable to obesity. Obesity. 2014;22(1):110–118. doi: 10.1002/oby.20585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Brigham EP, Anderson JA, Brook RD, et al. Challenging the obesity paradox: extreme obesity and COPD mortality in the SUMMIT trial. ERJ Open Res. 2021;7(3):00902–02020. doi: 10.1183/23120541.00902-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Reyes-Angel J, Kaviany P, Rastogi D, Forno E. Obesity-related asthma in children and adolescents. Lancet Child Adolesc Health. 2022;6(10):713–724. doi: 10.1016/S2352-4642(22)00185-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Putcha N, Anzueto AR, Calverley PMA, et al. Mortality and exacerbation risk by body mass index in patients with COPD in TIOSPIR and UPLIFT. Ann Am Thorac Soc. 2022;19(2):204–213. doi: 10.1513/AnnalsATS.202006-722OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mitra AK, Bhuiyan AR, Jones EA. Association and risk factors for obstructive sleep apnea and cardiovascular diseases: a systematic review. Diseases. 2021;9(4):88. doi: 10.3390/diseases9040088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Pennings N, Golden L, Yashi K, Tondt J, Bays HE. Sleep-disordered breathing, sleep apnea, and other obesity-related sleep disorders: an Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022. Obes Pillars. 2022;4:100043. doi: 10.1016/j.obpill.2022.100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Owen CG, Kapetanakis VV, Rudnicka AR, et al. Body mass index in early and middle adult life: prospective associations with myocardial infarction, stroke and diabetes over a 30-year period: the British Regional Heart Study. BMJ Open. 2015;5(9):e008105. doi: 10.1136/bmjopen-2015-008105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Katta N, Loethen T, Lavie CJ, Alpert MA. Obesity and coronary heart disease: epidemiology, pathology, and coronary artery imaging. Curr Probl Cardiol. 2021;46(3):100655. doi: 10.1016/j.cpcardiol.2020.100655. [DOI] [PubMed] [Google Scholar]
- 103.Milewska EM, Szczepanek-Parulska E, Marciniak M, Krygier A, Dobrowolska A, Ruchala M. Selected organ and endocrine complications according to BMI and the metabolic category of obesity: a single endocrine center study. Nutrients. 2022;14(6):1307. doi: 10.3390/nu14061307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Leggio M, Lombardi M, Caldarone E, et al. The relationship between obesity and hypertension: an updated comprehensive overview on vicious twins. Hypertens Res. 2017;40(12):947–963. doi: 10.1038/hr.2017.75. [DOI] [PubMed] [Google Scholar]
- 105.Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126(11):1477–1500. doi: 10.1161/CIRCRESAHA.120.316101. [DOI] [PubMed] [Google Scholar]
- 106.Amaral JF, Thompson WR, et al. Gallbladder disease in the morbidly obese. Am J Surg. 1985;149(4):551–557. doi: 10.1016/s0002-9610(85)80055-6. [DOI] [PubMed] [Google Scholar]
- 107.Engin A. The definition and prevalence of obesity and metabolic syndrome. Adv Exp Med Biol. 2017;960:1–17. doi: 10.1007/978-3-319-48382-5_1. [DOI] [PubMed] [Google Scholar]
- 108.Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 109.Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89(3):309–319. doi: 10.1016/j.diabres.2010.04.012. [DOI] [PubMed] [Google Scholar]
- 110.Aune D, Norat T, Vatten LJ. Body mass index and the risk of gout: a systematic review and dose-response meta-analysis of prospective studies. Eur J Nutr. 2014;53(8):1591–1601. doi: 10.1007/s00394-014-0766-0. [DOI] [PubMed] [Google Scholar]
- 111.Longo M, Zatterale F, Naderi J, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9):2358. doi: 10.3390/ijms20092358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Heit JA, Spencer FA, White RH. The epidemiology of venous thromboembolism. J Thromb Thrombolysis. 2016;41(1):3–14. doi: 10.1007/s11239-015-1311-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rahmani J, Haghighian Roudsari A, Bawadi H, et al. Relationship between body mass index, risk of venous thromboembolism and pulmonary embolism: a systematic review and dose-response meta-analysis of cohort studies among four million participants. Thromb Res. 2020;192:64–72. doi: 10.1016/j.thromres.2020.05.014. [DOI] [PubMed] [Google Scholar]
- 114.McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42(36):3599–3726. doi: 10.1093/eurheartj/ehab368. [DOI] [PubMed] [Google Scholar]
- 115.Ebong IA, Goff DC, Rodriguez CJ, Chen H, Bertoni AG. Mechanisms of heart failure in obesity. Obes Res Clin Pract. 2014;8(6):e540–e548. doi: 10.1016/j.orcp.2013.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Margolis G, Elbaz-Greener G, Ruskin JN, Roguin A, Amir O, Rozen G. The impact of obesity on sudden cardiac death risk. Curr Cardiol Rep. 2022;24(5):497–504. doi: 10.1007/s11886-022-01671-y. [DOI] [PubMed] [Google Scholar]
- 117.Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498. doi: 10.1093/eurheartj/ehaa612. [DOI] [PubMed] [Google Scholar]
- 118.Wolin KY, Carson K, Colditz GA. Obesity and cancer. Oncologist. 2010;15(6):556–565. doi: 10.1634/theoncologist.2009-0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Loh NY, Wang W, Noordam R, Christodoulides C. Obesity, fat distribution and risk of cancer in women and men: a Mendelian randomisation study. Nutrients. 2022;14(24):5259. doi: 10.3390/nu14245259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Ackerman SE, Blackburn OA, Marchildon F, Cohen P. Insights into the link between obesity and cancer. Curr Obes Rep. 2017;6(2):195–203. doi: 10.1007/s13679-017-0263-x. [DOI] [PubMed] [Google Scholar]
- 121.Ma Y, Yang Y, Wang F, et al. Obesity and risk of colorectal cancer: a systematic review of prospective studies. PLoS ONE. 2013;8(1):e53916. doi: 10.1371/journal.pone.0053916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sanfilippo KM, McTigue KM, Fidler CJ, et al. Hypertension and obesity and the risk of kidney cancer in 2 large cohorts of US men and women. Hypertens Dallas Tex 1979. 2014;63(5):934–941. doi: 10.1161/HYPERTENSIONAHA.113.02953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Wang F, Xu Y. Body mass index and risk of renal cell cancer: a dose-response meta-analysis of published cohort studies. Int J Cancer. 2014;135(7):1673–1686. doi: 10.1002/ijc.28813. [DOI] [PubMed] [Google Scholar]
- 124.Hoyo C, Cook MB, Kamangar F, et al. Body mass index in relation to oesophageal and oesophagogastric junction adenocarcinomas: a pooled analysis from the International BEACON Consortium. Int J Epidemiol. 2012;41(6):1706–1718. doi: 10.1093/ije/dys176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Setiawan VW, Yang HP, Pike MC, et al. Type I and II endometrial cancers: have they different risk factors? J Clin Oncol Off J Am Soc Clin Oncol. 2013;31(20):2607–2618. doi: 10.1200/JCO.2012.48.2596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Dougan MM, Hankinson SE, Vivo ID, Tworoger SS, Glynn RJ, Michels KB. Prospective study of body size throughout the life-course and the incidence of endometrial cancer among premenopausal and postmenopausal women. Int J Cancer. 2015;137(3):625–637. doi: 10.1002/ijc.29427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Karagozian R, Derdák Z, Baffy G. Obesity-associated mechanisms of hepatocarcinogenesis. Metabolism. 2014;63(5):607–617. doi: 10.1016/j.metabol.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 128.Campbell PT, Newton CC, Freedman ND, et al. Body mass index, waist circumference, diabetes, and risk of liver cancer for U.S. adults. Cancer Res. 2016;76(20):6076–6083. doi: 10.1158/0008-5472.CAN-16-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chen Y, Wang X, Wang J, Yan Z, Luo J. Excess body weight and the risk of primary liver cancer: an updated meta-analysis of prospective studies. Eur J Cancer Oxf Engl 1990. 2012;48(14):2137–2145. doi: 10.1016/j.ejca.2012.02.063. [DOI] [PubMed] [Google Scholar]
- 130.Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet Lond Engl. 2008;371(9612):569–578. doi: 10.1016/S0140-6736(08)60269-X. [DOI] [PubMed] [Google Scholar]
- 131.Genkinger JM, Spiegelman D, Anderson KE, et al. A pooled analysis of 14 cohort studies of anthropometric factors and pancreatic cancer risk. Int J Cancer. 2011;129(7):1708–1717. doi: 10.1002/ijc.25794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kitahara CM, Pfeiffer RM, Sosa JA, Shiels MS. Impact of overweight and obesity on US papillary thyroid cancer incidence trends (1995–2015) J Natl Cancer Inst. 2020;112(8):810–817. doi: 10.1093/jnci/djz202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.King LK, March L, Anandacoomarasamy A. Obesity and osteoarthritis. Indian J Med Res. 2013;138(2):185–193. [PMC free article] [PubMed] [Google Scholar]
- 134.Kasen S, Cohen P, Chen H, Must A. Obesity and psychopathology in women: a three decade prospective study. Int J Obes 2005. 2008;32(3):558–566. doi: 10.1038/sj.ijo.0803736. [DOI] [PubMed] [Google Scholar]
- 135.de Wit L, Have MT, Cuijpers P, de Graaf R. Body Mass Index and risk for onset of mood and anxiety disorders in the general population: results from the Netherlands Mental Health Survey and Incidence Study-2 (NEMESIS-2) BMC Psychiatry. 2022;22(1):522. doi: 10.1186/s12888-022-04077-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Luppino FS, de Wit LM, Bouvy PF, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- 137.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Romero-Corral A, Montori VM, Somers VK, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368(9536):666–678. doi: 10.1016/S0140-6736(06)69251-9. [DOI] [PubMed] [Google Scholar]
- 139.Lennon H, Sperrin M, Badrick E, Renehan AG. The obesity paradox in cancer: a review. Curr Oncol Rep. 2016;18(9):56. doi: 10.1007/s11912-016-0539-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Carnethon MR, De Chavez PJD, Biggs ML, et al. Association of weight status with mortality in adults with incident diabetes. JAMA. 2012;308(6):581–590. doi: 10.1001/jama.2012.9282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Yamauchi Y, Hasegawa W, Yasunaga H, et al. Paradoxical association between body mass index and in-hospital mortality in elderly patients with chronic obstructive pulmonary disease in Japan. Int J Chron Obstruct Pulmon Dis. 2014;9:1337–1346. doi: 10.2147/COPD.S75175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Mocini D, Di Fusco SA, Mocini E, et al. Direct oral anticoagulants in patients with obesity and atrial fibrillation: position paper of Italian national association of hospital cardiologists (ANMCO) J Clin Med. 2021;16(10):4185. doi: 10.3390/jcm10184185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Held C, Hadziosmanovic N, Aylward PE, et al. Body mass index and association with cardiovascular outcomes in patients with stable coronary heart disease—a stability substudy. J Am Heart Assoc. 2022;11(3):e023667. doi: 10.1161/JAHA.121.023667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Niedziela J, Hudzik B, Niedziela N, et al. The obesity paradox in acute coronary syndrome: a meta-analysis. Eur J Epidemiol. 2014;29(11):801–812. doi: 10.1007/s10654-014-9961-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Bagheri M, Speakman JR, Shabbidar S, Kazemi F, Djafarian K. A dose-response meta-analysis of the impact of body mass index on stroke and all-cause mortality in stroke patients: a paradox within a paradox. Obes Rev. 2015;16(5):416–423. doi: 10.1111/obr.12272. [DOI] [PubMed] [Google Scholar]
- 146.Tan XF, Shi JX, Chen MH. Prolonged and intensive medication use are associated with the obesity paradox after percutaneous coronary intervention: a systematic review and meta-analysis of 12 studies. BMC Cardiovasc Disord. 2016;16(1):125. doi: 10.1186/s12872-016-0310-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Antonopoulos AS, Oikonomou EK, Antoniades C, Tousoulis D. From the BMI paradox to the obesity paradox: the obesity-mortality association in coronary heart disease. Obes Rev Off J Int Assoc Study Obes. 2016;17(10):989–1000. doi: 10.1111/obr.12440. [DOI] [PubMed] [Google Scholar]
- 148.Elagizi A, Kachur S, Lavie CJ, et al. An overview and update on obesity and the obesity paradox in cardiovascular diseases. Prog Cardiovasc Dis. 2018;61(2):142–150. doi: 10.1016/j.pcad.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 149.Lavie CJ, De Schutter A, Milani RV. Healthy obese versus unhealthy lean: the obesity paradox. Nat Rev Endocrinol. 2015;11(1):55–62. doi: 10.1038/nrendo.2014.165. [DOI] [PubMed] [Google Scholar]
- 150.Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, Lavie CJ. Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag. 2019;15:89–100. doi: 10.2147/VHRM.S168946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Park Y, Peterson LL, Colditz GA. The plausibility of obesity paradox in cancer—point. Cancer Res. 2018;78(8):1898–1903. doi: 10.1158/0008-5472.CAN-17-3043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Frankenstein L, Zugck C, Nelles M, Schellberg D, Katus HA, Remppis BA. The obesity paradox in stable chronic heart failure does not persist after matching for indicators of disease severity and confounders. Eur J Heart Fail. 2009;11(12):1189–1194. doi: 10.1093/eurjhf/hfp150. [DOI] [PubMed] [Google Scholar]
- 153.Donini LM, Pinto A, Giusti AM, Lenzi A, Poggiogalle E. Obesity or BMI paradox? Beneath the tip of the iceberg. Front Nutr. 2020 doi: 10.3389/fnut.2020.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Blüher M. Metabolically healthy obesity. Endocr Rev. 2020;41(3):bnaa004. doi: 10.1210/endrev/bnaa004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Butt JH, Petrie MC, Jhund PS, et al. Anthropometric measures and adverse outcomes in heart failure with reduced ejection fraction: revisiting the obesity paradox. Eur Heart J. 2023;44(13):1136–1153. doi: 10.1093/eurheartj/ehad083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ryan DH, Deanfield JE, Jacob S. Prioritizing obesity treatment: expanding the role of cardiologists to improve cardiovascular health and outcomes. Cardiovasc Endocrinol Metab. 2023;12(1):e0279. doi: 10.1097/XCE.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Cercato C, Fonseca FA. Cardiovascular risk and obesity. Diabetol Metab Syndr. 2019;11(1):74. doi: 10.1186/s13098-019-0468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Horn JW, Feng T, Mørkedal B, et al. Obesity and risk for first ischemic stroke depends on metabolic syndrome: the HUNT study. Stroke. 2021;52(11):3555–3561. doi: 10.1161/STROKEAHA.120.033016. [DOI] [PubMed] [Google Scholar]
- 159.Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;143(21):e984–e1010. doi: 10.1161/CIR.0000000000000973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Unek IT, Bayraktar F, Solmaz D, et al. The levels of soluble CD40 ligand and C-reactive protein in normal weight, overweight and obese people. Clin Med Res. 2010;8(2):89–95. doi: 10.3121/cmr.2010.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Beavers CJ, Heron P, Smyth SS, Bain JA, Macaulay TE. Obesity and antiplatelets-does one size fit all? Thromb Res. 2015;136(4):712–716. doi: 10.1016/j.thromres.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 162.Wang Y, Wang W, Jia S, et al. Development of a nomogram for the prediction of in-hospital mortality in patients with acute ST-elevation myocardial infarction after primary percutaneous coronary intervention: a multicentre, retrospective, observational study in Hebei province, China. BMJ Open. 2022;12(2):e056101. doi: 10.1136/bmjopen-2021-056101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Biswas S, Andrianopoulos N, Dinh D, et al. Association of body mass index and extreme obesity with long-term outcomes following percutaneous coronary intervention. J Am Heart Assoc. 2019;8(21):e012860. doi: 10.1161/JAHA.119.012860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Payvar S, Kim S, Rao SV, et al. In-hospital outcomes of percutaneous coronary interventions in extremely obese and normal-weight patients: findings from the NCDR (National cardiovascular data registry) J Am Coll Cardiol. 2013;62(8):692–696. doi: 10.1016/j.jacc.2013.05.058. [DOI] [PubMed] [Google Scholar]
- 165.Bogers RP, Bemelmans WJE, Hoogenveen RT, et al. Association of overweight with increased risk of coronary heart disease partly independent of blood pressure and cholesterol levels: a meta-analysis of 21 cohort studies including more than 300 000 persons. Arch Intern Med. 2007;167(16):1720–1728. doi: 10.1001/archinte.167.16.1720. [DOI] [PubMed] [Google Scholar]
- 166.Henning RJ. Obesity and obesity-induced inflammatory disease contribute to atherosclerosis: a review of the pathophysiology and treatment of obesity. Am J Cardiovasc Dis. 2021;11(4):504–529. [PMC free article] [PubMed] [Google Scholar]
- 167.Schindler TH, Cardenas J, Prior JO, et al. Relationship between increasing body weight, insulin resistance, inflammation, adipocytokine leptin, and coronary circulatory function. J Am Coll Cardiol. 2006;47(6):1188–1195. doi: 10.1016/j.jacc.2005.10.062. [DOI] [PubMed] [Google Scholar]
- 168.Karczewski J, Śledzińska E, Baturo A, et al. Obesity and inflammation. Eur Cytokine Netw. 2018;29(3):83–94. doi: 10.1684/ecn.2018.0415. [DOI] [PubMed] [Google Scholar]
- 169.Engin A. Endothelial dysfunction in obesity. Adv Exp Med Biol. 2017;960:345–379. doi: 10.1007/978-3-319-48382-5_15. [DOI] [PubMed] [Google Scholar]
- 170.Gondoni LA, Titon AM, Nibbio F, Augello G, Caetani G, Liuzzi A. Heart rate behavior during an exercise stress test in obese patients. Nutr Metab Cardiovasc Dis. 2009;19(3):170–176. doi: 10.1016/j.numecd.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 171.Palma G, Sorice GP, Genchi VA, et al. Adipose tissue inflammation and pulmonary dysfunction in obesity. Int J Mol Sci. 2022;23(13):7349. doi: 10.3390/ijms23137349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chow BJW, Dorbala S, Di Carli MF, et al. Prognostic value of PET myocardial perfusion imaging in obese patients. JACC Cardiovasc Imaging. 2014;7(3):278–287. doi: 10.1016/j.jcmg.2013.12.008. [DOI] [PubMed] [Google Scholar]
- 173.Wang X, Dong J, Du Z, et al. Risk of heart failure between different metabolic states of health and weight: a meta-analysis of cohort studies. Nutrients. 2022;14(24):5223. doi: 10.3390/nu14245223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ren J, Wu NN, Wang S, Sowers JR, Zhang Y. Obesity cardiomyopathy: evidence, mechanisms, and therapeutic implications. Physiol Rev. 2021;101(4):1745–1807. doi: 10.1152/physrev.00030.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Alpert MA, Karthikeyan K, Abdullah O, Ghadban R. Obesity and cardiac remodeling in adults: mechanisms and clinical implications. Prog Cardiovasc Dis. 2018;61(2):114–123. doi: 10.1016/j.pcad.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 176.Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog Cardiovasc Dis. 2014;56(4):391–400. doi: 10.1016/j.pcad.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 177.Aune D, Schlesinger S, Norat T, Riboli E. Body mass index, abdominal fatness, and the risk of sudden cardiac death: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2018;33(8):711–722. doi: 10.1007/s10654-017-0353-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yao Y, Xue J, Li B. Obesity and sudden cardiac death: prevalence, pathogenesis, prevention and intervention. Front Cell Dev Biol. 2022;10:1044923. doi: 10.3389/fcell.2022.1044923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–752. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 180.Vyas V. Obesity and atrial fibrillation: epidemiology, pathophysiology and novel therapeutic opportunities. 2019. https://www.aerjournal.com/articles/obesity-and-atrial-fibrillation-epidemiology-pathophysiology-and-novel-therapeutic. Accessed 1 Feb 2023. [DOI] [PMC free article] [PubMed]
- 181.Sumeray M, Steiner M, Sutton P, Treasure T. Age and obesity as risk factors in perioperative atrial fibrillation. Lancet Lond Engl. 1988;2(8608):448. doi: 10.1016/s0140-6736(88)90433-3. [DOI] [PubMed] [Google Scholar]
- 182.Berkovitch A, Kivity S, Klempfner R, et al. Body mass index and the risk of new-onset atrial fibrillation in middle-aged adults. Am Heart J. 2016;173:41–48. doi: 10.1016/j.ahj.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 183.Sandhu RK, Conen D, Tedrow UB, et al. Predisposing factors associated with development of persistent compared with paroxysmal atrial fibrillation. J Am Heart Assoc. 2014;3(3):e000916. doi: 10.1161/JAHA.114.000916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Tedrow UB, Conen D, Ridker PM, et al. The long- and short-term impact of elevated body mass index on the risk of new atrial fibrillation the WHS (women’s health study) J Am Coll Cardiol. 2010;55(21):2319–2327. doi: 10.1016/j.jacc.2010.02.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Lee H, Choi EK, Lee SH, et al. Atrial fibrillation risk in metabolically healthy obesity: a nationwide population-based study. Int J Cardiol. 2017;240:221–227. doi: 10.1016/j.ijcard.2017.03.103. [DOI] [PubMed] [Google Scholar]
- 186.Wharton S, Lau DCW, Vallis M, et al. Obesity in adults: a clinical practice guideline. CMAJ Can Med Assoc J J Assoc Medicale Can. 2020;192(31):E875–E891. doi: 10.1503/cmaj.191707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lopez-Jimenez F, Almahmeed W, Bays H, et al. Obesity and cardiovascular disease: mechanistic insights and management strategies. A joint position paper by the World heart federation and world obesity federation. Eur J Prev Cardiol. 2022;29(17):2218–2237. doi: 10.1093/eurjpc/zwac187. [DOI] [PubMed] [Google Scholar]
- 188.Papamargaritis D, le Roux CW, Holst JJ, Davies MJ. New therapies for obesity. Cardiovasc Res. 2022 doi: 10.1093/cvr/cvac176. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.