Abstract
Cytotoxic anticancer therapies activate programmed cell death in the context of underlying stress and inflammatory signaling to elicit the emission of danger signals, cytokines, and chemokines. In a concerted manner, these immunomodulatory secretomes stimulate antigen presentation and T cell–mediated anticancer immune responses. In some instances, cell death–associated secretomes attract immunosuppressive cells to promote tumor progression. As it stands, cancer cell death–induced changes in the tumor microenvironment that contribute to antitumor or protumor effects remain largely unknown. This is complicated to examine because cell death is often subverted by tumors to circumvent natural, and therapy-induced, immunosurveillance. Here, we provide insights into important but understudied aspects of assessing the contribution of cell death to tumor elimination or cancer progression, including the role of tumor-associated genetics, epigenetics, and oncogenic factors in subverting immunogenic cell death. This perspective will also provide insights on how future studies may address the complex antitumor and protumor immunologic effects of cell death, while accounting for variations in tumor genetics and underlying microenvironment.
The Contribution of Programmed Cell Death to Immunity
The maintenance of organismal development and tissue homeostasis requires a balance between the production of new cells and clearance of stressed and dying cells. Programmed cell death is a highly regulated process used to not only clear unneeded cells, but also to communicate homeostatic disturbances, such as danger and tissue injury, to the immune system. Hence, cell death can elicit immune responses against malignancies (1, 2) and pathogens (3). The interaction of dying cancer cells with the immune system has been intensively studied across a variety of model systems, revealing that programmed cell death can elicit an antitumor (4–9) or protumor immune response (10–12).
Studies investigating the role of cell death in the initiation of anticancer immunity started with the exploration of how apoptotic cells communicate with dendritic cells (DC; refs. 13–19). Subsequent studies using cytotoxic anticancer agents, such as cytotoxic chemotherapies (20), radiation (21), oncolytic viruses (22), photodynamic therapy (23), extracorporeal photochemotherapy (24, 25), facilitated the rapid identification of mechanistic details associated with the immunogenicity of cell death and its contribution to anticancer immunity (20, 26–29). Two decades later, we have gained a remarkable understanding of the types of cell stress and programmed cell death that contribute to the emission of molecules (Fig. 1) and their role in shaping anticancer immunity (Fig. 2).
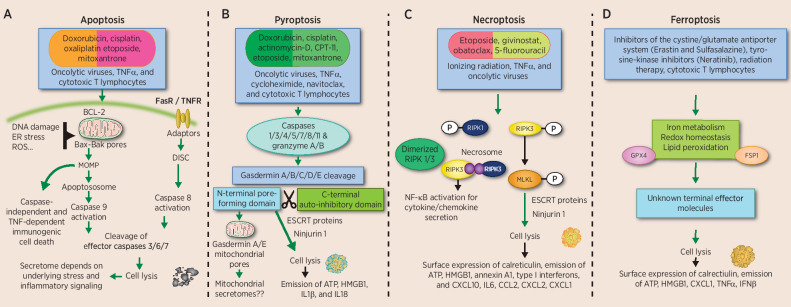
Figure 1.
Lethal stimuli and signaling pathways leading to activation of programmed cell death. Many cytotoxic anticancer treatments including chemotherapeutics, radiation, photodynamic therapy, biologics, and oncolytic viruses can trigger cell death. Apoptosis (A) can be initiated via the intrinsic or extrinsic pathway, both activating distinct signaling to emit secretomes that can differentially activate immunity against cancer. The role of pyroptosis (B) in anticancer immunity is accumulating. Activated caspases cleave gasdermin proteins to release the N-terminal domain that creates pores in the mitochondria (N-terminal gasdermin A and E) and the plasma membrane (all gasdermins, except Pejvakin). How the involvement of mitochondria and/or other organelles during pyroptosis affects immunogenicity remains unknown. Effector T cells and NK cells can also initiate tumor pyroptosis, although the role of this in further expanding T-cell responses needs to be investigated. Necroptosis (C) has been extensively studied in the context of cancer. The involvement of NFkB during necroptosis signaling contributes to inflammatory cytokines and chemokines that either result in antitumor or protumor outcome. In addition, MLKL overexpression can also initiate cell death and antitumor immunity. Ferroptosis (D) is an iron-dependent cell death involving lipid peroxidation. The immunogenicity of ferroptotic tumor cells is conflicting, although several immunostimulatory secretomes are released after this type of cell death. In addition, T cell–secreted IFNγ can trigger ferroptosis to potentiate the anticancer immunity cycle.
Figure 2.
Mechanisms of immune stimulation (A) and immunosuppression (B) mediated by secretomes emitted from dying cancer cells. Several types of cancer cell death result in the surface expression of calreticulin and/or the emission of danger signals (ATP and HMGB1), cytokines and chemokines. In a concerted approach, all these molecules activate antitumor immune responses, mediated by DCs priming T cells to become cytotoxic against tumors expressing cognate antigens. In addition, the NKp46 receptor of NK cells can directly recognize calreticulin on the surface of stressed cells to engage in tumor cell killing. Immunostimulatory secretomes are also essential for T-cell activation and trafficking into malignant lesions. In some cancers, cell death can attract immunosuppressive B cells and MDSCs, thereby contributing to tumor progression.
Danger signals, cytokines, and chemokines emitted during immunogenic cell death (ICD) promote the activation, maturation, and trafficking of innate immune cells. Specifically, surface-expressed “eat me” signals, such as calreticulin, attract antigen-presenting cells (mainly DCs) to take up dying cells, along with a variety of immunomodulatory secretomes that stimulate DCs to migrate to the lymph nodes to present antigens to naïve T cells for generating cytotoxic T-cell responses (refs. 20, 26–29; Fig. 2A). It is worthy of mention that T-cell responses after ICD are suspected to spread across multiple neoantigens, creating a broad T-cell repertoire and thus, making it attractive to target tumors with high heterogeneity (21, 30, 31). In addition to effective CD8+ T-cell activation, ICD-associated secretomes, mainly chemokines, can facilitate their trafficking into non–T cell–inflamed tumors (32–34). On the contrary, in some tumor types, such as pancreatic and prostate cancer, the secretomes emitted after gemcitabine or oxaliplatin promote the recruitment of immunosuppressive cells, such as myeloid-derived suppressor cells (MDSC; refs. 10, 11) and IgA+PD-L1+IL10-producing plasmocytes (12), thereby promoting disease progression (Fig. 2B).
In line with the antitumor effects of ICD, chemoradiotherapies exert immune-mediated anticancer effect in patients (4–9) and can synergize with immune checkpoint inhibitors (35–40); although, biomarkers to select patients and predict response are poorly defined (41, 42). To fill these gaps, mechanistic understanding of ICD processes, specifically the individual types of premortem stress and programmed cell death that contributes to anticancer immunity, are highly desired. Unfortunately, many types of chemotherapies simultaneously activate multiple types of premortem stress and cell death in neoplastic cells and actively dividing immune cells. Hence, the specific processes and mechanisms, from the dying cancer cell and the immune cell compartment, that contribute to therapeutic efficacy of ICD remain largely unknown.
What Types of Programmed Cell Death Are Immunostimulatory?
During cytotoxic anticancer treatments, cell death takes place in the context of underlying stress [genotoxic, endoplasmic reticulum, and mitochondrial stress, as well as reactive oxygen species (ROS) overload] that also facilitates the emission of secretomes, thus, complicating the direct assessment of cell death–associated immunologic events. There is a surge of genetically engineered cell death systems that specifically activate each type of cancer cell death in isolation, thereby facilitating the discovery of how specific cell death types influence the anticancer immunity cycle (43–50). Overall, past studies have largely focused on secretome-mediated effects of cell death; as a result, its indirect effects on the tumor microenvironment remain understudied. Depending on tumor type, cancer cell death can indirectly affect anticancer immunity by remodeling the tumor architecture and vasculature, thereby influencing the trafficking of antitumor and protumor immune cells and modulating the function of supporting stroma and fibroblasts (51). In the next sections, we will describe the individual types of programmed cell death and their effect on anticancer immunity.
Box 1. The unknown territories in cell death and immunity research.
-
1.
Does cell death activated by different pore-forming proteins (gasdermin proteins, MLKL) result in different immune outcomes?
-
2.
What is the individual contribution of cell stress to anticancer immunity?
-
3.
What types of cell death and secretomes predict the outcome of ICD in patients?
-
4.
What dose of cytotoxic therapies can activate the immunostimulatory type and rate of cell death for a durable anticancer effect?
-
5.
What are the effects of cell death on the tumor architecture and overall microenvironment?
-
6.
What types of oncogenic drivers and interactions are circumventing the induction of immunostimulatory cell death?
Apoptosis
Apoptosis is a type of cell death that is integral to the maintenance of tissue homeostasis, and organism development, as well as numerous pathologies, including cancer. Apoptosis can be initiated by the intrinsic or extrinsic pathway, both of which can result in distinct anticancer immune outcomes (Fig. 1A). Apoptotic cells activate diverse immune-mediated anticancer outcomes, depending on the type of cell death stimuli, upstream stress (26, 28, 52, 53), and cell death signaling and tumor type (34, 54). Unlike chemoradiotherapy-induced immunogenic apoptosis (20), induction of apoptosis by dimerizing C-terminal caspase 8 or caspase 9 has demonstrated less-immunogenic outcomes (43, 44). This is not surprising given apoptotic caspases dampen IFN secretion after the sensing of mitochondrial DNA (55–57). Despite that, apoptosis can be immunogenic when it takes place after mitochondrial membrane permeabilization in a caspase-independent fashion (58) or when the cytotoxic agent concurrently activates endoplasmic reticulum (ER) stress and autophagic response that contributes to the surface expression of calreticulin, promoting phagocytosis (26, 59) and/or natural killer (NK) cell–mediated killing (60), as well as the emission of danger signals, ATP, high mobility group 1 (HMGB1), annexin A1, type I IFNs, and C-X-C motif chemokine ligand 10 (CXCL10; refs. 20, 26–28). These danger signals are sensed by pathogen recognition receptors on DCs and, in concert with cytokines and chemokines, stimulate DCs to undergo activation, maturation, and migration into the draining lymph node to efficiently prime T cells (Fig. 2A). The cytokines and chemokines produced during immunogenic apoptosis are also crucial to allow T-cell activation, differentiation, and migration into malignant lesions (32).
Pyroptosis
Upstream pyroptotic signaling activates caspases and granzymes (46, 47) to cleave gasdermin (GSDM) proteins, freeing the pore-forming N-terminal domain from the autoinhibitory C-terminal domain. The pores formed by N-terminal gasdermin protein activate the formation of higher-order ninjurin-1 polymers that mediate plasma membrane rupture (refs. 61–65; Fig. 1B). Many chemotherapeutics, including doxorubicin, cisplatin, actinomycin-D, CPT-11, etoposide, and mitoxantrone, activate gasdermin E-mediated pyroptosis (45). Moreover, photodynamic therapy activates pyroptosis in pancreatic tumors (66). Furthermore, oncolytic viruses (48), as well as the combination of TNFα, cycloheximide, and navitoclax, activate pyroptosis (67). In addition, granzyme B from cytotoxic CD8+ T cells (46) and granzyme A from NK cells and T cells (47) can cleave gasdermin E and B, respectively, to induce tumor pyroptosis. Unlike their natural T-cell counterpart, chimeric antigen receptor–loaded T cells secrete higher amounts of granzyme B, thereby activating gasdermin E–mediated tumor pyroptosis and the associated cytokine release syndrome (68).
Pyroptosis is highly inflammatory, although detailed investigation on the nature of secretomes that mediate anticancer immunity remain to be identified (63). For example, the N-terminal domain of gasdermin A and E can induce mitochondrial oxidative stress and pore formation prior to plasma membrane rupture, which allows the release of danger signals and intracellular contents that contributes to the immunogenicity (69–71). Pyroptosis allows the release of cytokines, such as IL1β and IL18, as well as danger signals, HMGB1, and ATP (63). These immunomodulatory secretomes stimulate a variety of immune cells, including NK cells, macrophages, DCs, and the subsequent generation of antigen-specific CD8+ and CD4+ T-cell responses (46, 47, 49, 66). In tumors undergoing pyroptosis, there is decreased FoxP3+CD4+ regulatory T cells, monocytes, neutrophils, and MDSCs (46, 47, 49). Thus, pyroptosis can induce robust anti-immune responses and improve the survival of tumor-bearing mice (46, 47, 49).
Necroptosis
Necroptosis is initiated by a variety of stimuli, including the engagement of death receptors (TNFR1 and Fas/FasL), Toll-like receptors, or intracellular nucleic acid sensors under a caspase-8 inhibited state (72). Necroptosis execution involves the kinases receptor-interacting serine/threonine-protein kinase 1 (RIPK1) and RIPK3 to activate NFκB-mediated inflammation and to phosphorylate mixed lineage kinase domain-like (MLKL), which executes cell lysis (73, 74). Several chemotherapies such as etoposide, givinostat, obatoclax, and 5-fluorouracil trigger necroptosis (75–77). Furthermore, ionizing radiotherapy and targeted receptor therapy also activate necroptosis (75, 78–80). Along similar lines, certain oncolytic virus monotherapies can induce necroptosis and combine favorably with chemotherapies to potentiate anticancer effect (refs. 34, 81, 82; Fig. 1C).
Necroptotic fibroblasts, induced after dimerization of RIPK3, release danger signals HMGB1, ATP, and proinflammatory cytokines (IFNγ, IL6) and chemokines (CCL3, CCL4, CCL5; refs. 43, 44). Intratumoral inoculation of necroptotic fibroblasts elicits a CD103+ cell–mediated T-cell response (43, 44). Furthermore, necroptosis induces an appreciable increase in intratumoral neutrophils and macrophages (34). It is worthy of mentioning that RIPK3 lacking the RIP homotypic interaction motif domain fails to elicit NFκB-mediated inflammation and tumor control (43). Meanwhile, another study reports that necroptotic cell death induced by intratumoral injection of MLKL mRNA exerts durable antitumor effects, suggesting that necroptotic cell death in the absence of NFκB activation can also elicit antitumor immunity (82, 83).
Ferroptosis
Ferroptosis is driven by iron-dependent, excessive phospholipid peroxidation that compromises plasma membrane integrity and cell lysis (84). It is regulated by a variety of metabolic pathways, including redox homeostasis, iron handling, mitochondrial activity, and the metabolism of lipids and amino acids (ref. 85; Fig. 1D). Phospholipid peroxidation relies on iron, ROS, and phospholipids containing polyunsaturated fatty acid chains. An important regulator of ferroptosis is the micronutrient selenium, which is required for the biosynthesis of selenoproteins that scavenge ROS. A key inhibitor of phospholipid peroxidation is glutathione peroxidase 4 (GPX4; ref. 86). In addition, a variety of factors can influence the induction of ferroptosis by regulating cellular metabolism and ROS levels. Despite a wealth of knowledge in the mechanisms regulating ferroptosis, the exact molecular events and terminal effectors of ferroptotic cell death are unknown.
Ferroptosis is activated in cancer cells after treatment with inhibitors of the cystine/glutamate antiporter system, such as erastin (87, 88) and sulfasalazine (89, 90), tyrosine kinase inhibitors (91), radiotherapy (92), and neratinib (a potent, irreversible pan-tyrosine kinase inhibitor; ref. 93). Ferroptosis inducers ML161, RSL, and erastin, as well as inducible genetic depletion of GPX4 in cancer cells, promotes the surface expression of calreticulin and emission of danger signals ATP and HMGB1 and cytokines (50, 94). However, there is conflicting evidence on the effects of ferroptotic cancer cells on DC activation and cross-priming (50, 94). A recent study shows that ferroptotic cancer cells suppress DC function and fail to protect against tumor growth (50). However, previous work using RSL3 reports that early ferroptosis has the opposite effect of potentiating DC function and the associated antitumor effects (94). Interestingly, both studies used the MCA205 tumor model, hence the conflicting findings could be attributed to animal facility-associated microbiome differences (95). There are also two instances where ferroptosis is shown to promote tumor progression via immunosuppressive intratumoral macrophage infiltrate (96, 97).
Recent studies demonstrate that T cell–mediated tumor killing involves ferroptosis (98, 99). In vitro IFNγ alone fails to induce ferroptosis but synergizes with arachidonic acid to activate ACSL4-dependent tumor ferroptosis (99). However, in established tumors, IFNγ secreted by cytotoxic CD8+ T cells inhibits the glutamate–cystine antiporter system xc− in tumors to promote lipid peroxidation and ferroptosis (98). Furthermore, forcing tumors to undergo immunogenic ferroptosis by cyst(e)inase, an engineered enzyme that degrades both cystine and cysteine, synergizes with immune checkpoint inhibitor therapy (98). Overall, because ferroptosis is a relatively new type of cell death, additional studies are required to clarify the immunologic outcomes of inducing ferroptosis in distinct tumor types with variable immune landscapes and microenvironments.
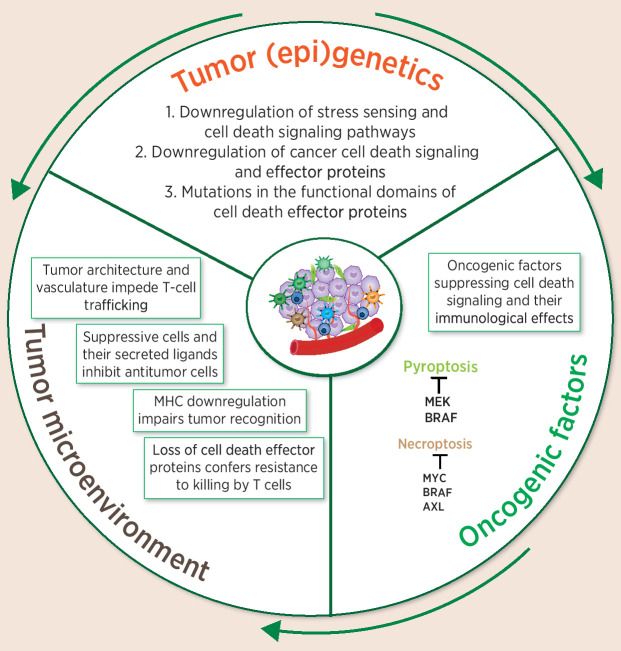
Tumors (Epi)genetics, the Associated Oncogenic Signaling, and the Tumor Microenvironment Dictate the Outcome of Cancer Cell Death
Tumors evolve to evade anticancer immunity via acquisition of genetic or epigenetic aberrations in pyroptosis and necroptosis effector proteins (refs. 46, 100–105; Fig. 3). Mutations in RIPK3 and MLKL are well documented in several tumor types (102, 106–108). RIPK3 expression is epigenetically regulated at different stages of tumor progression (100, 109), and treatment with a hypomethylating agent, decitabine, can restore RIPK3 expression and significantly improve responses to chemotherapy in human tumor xenografts (100).
Figure 3.
Inhibiting cell death confers cancer's proliferative capacity and ability to hide from immune-mediated detection and attack. Cancer cells evade immunogenic cell death by downregulating the initiation and execution of cell death. In addition to downregulating the cell death machinery via (epi)genetics, a variety of cancers employ tumor-intrinsic oncogenic pathways to selectively shut off ICD. In some cases, the immunosuppressive microenvironment renders ICD-primed antitumor cells to lose functionality.
Lung adenocarcinoma, colon adenocarcinoma, and uterine corpus endometrioid carcinoma possess the most frequent gasdermin E linker region mutations, with lung and colon adenocarcinoma commonly containing loss-of-function mutations (46, 110). In addition, selection pressure to downregulate gasdermin E coincides with emerging data suggesting it can regulate anticancer immunity (46). Tumors express five spliced variants of gasdermin B, whereby N-terminal fragments of isoforms 3 and 4 induce pyroptosis, but isoforms 1, 2, and 5 lack the motif that allows gasdermin B to insert in the membrane. These mutated gasdermin B 3/4 isoforms block pyroptosis caused by other cytotoxic gasdermin B isoforms (111). Gasdermin proteins can also undergo cancer-specific methylation. Methylation of gasdermin A, C, and E promotor sites has been observed in both gastric cancer and esophageal squamous cell carcinoma (104, 112). Treatment with decitabine successfully restores gasdermin A expression and induction of pyroptosis in gastric cancers (113, 114). Furthermore, gasdermin E is hypermethylated at the CpG islands near the transcription site in over half of breast cancers (105). Human tumors frequently mutate gasdermin E and C in the linker region between the N- and C-terminal domain, abrogating cleavage and activation of their pore-forming activities (46).
Tumor genetics and associated oncogenic factors can establish immunosuppressive intratumoral niches, as has been comprehensively reviewed elsewhere (115). In addition to these noncell autonomous effects, oncogenic pathways involving oncogenes and tumor suppressors can also interfere with the cancers own cell death machinery to either provide a proliferative advantage or allow escape from immune-mediated attack (100, 116–121). In many cancers, distinct combinations of oncogenes and loss of tumor suppressors drive tumorigenesis and regulate signaling, leading to apoptosis. In most instances, tumor suppressors p53 (122–125), Rb (126–128), and PTEN (129) stimulate proapoptotic signaling to clear premalignant cells, whereas oncogenic Kirsten rat sarcoma virus (KRAS) positively regulates cancer cell survival and proliferative capacity by downregulating apoptotic pathways (130–132). It is not known whether inhibition of KRAS or any other antiapoptotic oncogenic pathway results in immunostimulatory apoptosis.
Oncogenic drivers suppress the expression of necroptotic and pyroptotic effector proteins and ablation of oncogenic signaling results in the enhancement of ICD, thereby reigniting antitumor immunity. For example, c-Myc interacts with RIPK3 and RIPK1 to prevent necrosome formation (119). Depletion of c-MYC reinstates necroptosis-promoting antitumor immunity (119). Yet another oncogene that compromises the ICD machinery is BRAF. BRAF/AXL ablates RIPK3 expression in patient-derived xenografts (120). In a separate study, the combined inhibition of BRAF and MEK in mutant melanoma has proven successful at promoting pyroptosis, with the hallmark of HMGB1 release and expansion of tumor-specific CD8+ T cells (121, 133). Finally, inhibition of KRASG12C regresses patient-derived colorectal, lung, and pancreatic xenografts through activation of ICD (116). Indeed, such an outcome has been translated into patients and has garnered clinical efficacy (116). Yet it is not known what type of specific cell death is activated upon KRASG12C inhibition after treatment with AMG510. Cancer cell ferroptosis is also regulated by oncogenic Ras (134–137) and the tumor suppressor p53 (138, 139), yet it remains unknown whether this directly influences immune outcome. In summary, all of these studies highlight the need for comprehensive and systematic studies to elucidate how distinct oncogenic pathways influence cell death–mediated immunity and antitumor effects (1). The findings are foundational to apply chemoradiotherapies in combination with oncogenic inhibitors to stimulate patient antitumor responses.
A Perspective of Factors That Dictate the Antitumor and Protumor Effects of Cancer Cell Death
Specific cell death types have been associated with natural and therapy-induced antitumor or protumor effects. Tumors that endogenously express higher levels of immunostimulatory cell death effectors proteins, such as RIPK3, gasdermins, and ACSL4, show an elevated CD8+ T-cell infiltrate and prolonged patient survival (8, 9, 46, 47, 99, 111). In the context of ICD-inducing treatments, the nature of the lethal stimuli, along with tumor type, its underlying genetics, and the microenvironment, dictate the type of immunostimulatory secretomes emitted to predict the initiation of anticancer or protumor immunity. As reviewed elsewhere (140, 141), additional host factors, such as germline mutations in pathogen recognition receptors and host microbiota, affect immune response and survival response after chemoradiotherapies.
There are many clinical trials combining ICD-inducing treatments with immune checkpoint inhibitors (35–40), although there is lack of defined clinical biomarkers to select patients and to predict treatment outcomes. Regarding biomarker development, care must be taken in correlating the level of transcripts or full-length cell death proteins with immune cell infiltration, functionality, and patient survival. In addition to widely known discrepancies between transcript and protein expression patterns, cell death effector proteins have multiple functions, and their specific role in programmed cell death requires active protein modifications, such as cleavage or phosphorylation. In addition, tumors express dominant-negative isoforms of cell death effector proteins to evade ICD. For example, gasdermin B has five isoforms, and tumors preferentially overexpress isoforms with a dominant-negative effect to escape NK cell– and T cell–mediated attack (111); thus, correlating the totality of gasdermin B isoforms with immune function would lead to incorrect interpretation. To add to this complexity, there is extensive cross-talk among cell death pathways, with many of the upstream signaling and effector proteins shared between distinct cell death modalities and other inflammatory processes. Hence, careful analysis is warranted when correlating the extent of cell death with immune infiltration and survival outcomes. To this end, we recommend future studies to comprehensively quantify all the forms of cell death to define the major modality of cell death induced by specific ICD-inducing treatments in a specific cancer type and how that shapes the tumor immune landscape. In parallel, preclinical studies using genetic systems to activate specific cell death modalities will provide fundamental insight of the transcriptional, immunologic, and microenvironmental signatures for further biomarker development and integration into existing clinical biomarkers.
Despite mounting evidence underpinning the contribution of stress responses in ICD (142), expression of cell death effector proteins MLKL (82, 83) and gasdermin A/E (46, 49) induce robust anticancer immunity, highlighting the immunogenicity of cancer cell death in the absence of underlying stress and inflammatory signaling. However, there is limited knowledge on how the induction of cancer cell death in acute and chronic setting shapes immunity. It is likely that the type, rate, and amount of cell death may dictate immunity by influencing the activation and trafficking of immune cells and the availability of secretomes and tumor antigens. In a recent work, pyroptosis induction in less than 15% the cancer cells eradicates entire established mammary tumors (49). Relating this to a clinical setting, the dose regimen of chemoradiotherapies that preferentially activate ICD and anticancer effects are unknown. However, sublethal doses are suspected to exert better anticancer effects, mainly by enhancing cancer cell genotoxic and ER stress to stimulate T-cell responses (143) and/or activating cancer cell senescence that potently activates T cell–mediated immunity (144). Future clinical studies correlating the type and extent of cancer cell death with T-cell infiltrate and anticancer effects are highly desired.
In a variety of immune-responsive and spontaneously arising murine tumors, chemoradiotherapy-mediated rapid activation of ICD results in immune-mediated tumor elimination (145). On the contrary, the protumor effects of cell death are presented in chronic inflammatory settings, where elevated expression of cell death effector proteins accelerates tumor progression (10, 11, 146–152). For example, necroptosis is frequently reported as immunostimulatory in the context of chemoradiotherapy (34, 153) or when it is activated by expressing dimerizable RIPK3 or MLKL (30, 43, 44, 154). In contrast, pancreatic tumors overexpressing RIPK1/3 accelerate tumor progression by secreting CXCL1 to attract MDSCs. Accordingly, ablating necrosome formation generates a T cell–inflamed pancreatic tumor microenvironment (10, 11). Although previously unexplored, defining the mechanisms by which pancreatic ductal adenocarcinoma (PDA) prevents plasma membrane rupture downstream of pathologically elevated necrosome formation (10) may identify therapeutic opportunities to trigger PDA cell lysis and possibly kickstart the antitumor immunity cycle.
It remains intriguing under what tumor microenvironmental conditions a specific type of cell death becomes antitumor or protumor. Tumor type, genetics, and anatomical location can shape the underlying microenvironment, which in turn dictates the immune-mediated anticancer effect of ICD-inducing therapies. In this respect, a highly immunostimulatory cell death may not overcome an immunosuppressive tumor when administered as a monotherapy (33, 34, 54), and a less-ICD may readily exert durable anticancer immunity in immune-responsive tumors (20, 155). Hence, investigating how cell death affects the overall immune landscape using tumors arising in different anatomical locations with variable intratumoral environments is highly desired. Future studies are needed to investigate how tumors with varying immune landscape respond to a similar lethal stimulus, with the goal to define the type and amount of cell death, the composition of their secretomes, or the recruitment and functionality of innate and adaptive immune cells. Furthermore, given the microenvironment-based immune cell plasticity and distinct immunoregulatory networks in tumor-draining lymph nodes (156), it is possible for tumors and draining lymph nodes to subvert the entry or functionality of cell death–activated immune cells. Elucidating how the tumor microenvironment shapes immune-mediated outcomes of ICD will have profound effects in the design of biomarkers for patient selection and to predict treatment efficacy.
Acknowledgments
S.T. Workenhe is funded by Canadian Institute of Health Research (PJT 185868 and PJT 190071), SickKids New Investigator award (NI23-1064R), Cancer Research Society (ID# 942502 and 1056603), Ontario Veterinary College (OVC) Pet Trust, Ontario Institute for Cancer Research funding from The Joseph and Wolf Lebovic Cancer Genomics and Immunity Program. J.M. Inkol is supported by OVC PhD Scholarship and Ontario Graduate Scholarship. M.J. Westerveld is supported by OVC PhD Scholarship. S.G. Verburg is supported by CGS-M, OVC MSc Scholarship and Ontario Graduate Scholarship. S.M. Worfolk is supported by Queen Elizabeth II Graduate Scholarship in Science & Technology.
Authors' Disclosures
S.T. Workenhe reports grants from Alivid LLC and POINT Biopharma outside the submitted work. No disclosures were reported by the other authors.
References
- 1. Workenhe ST, Pol J, Kroemer G. Tumor-intrinsic determinants of immunogenic cell death modalities. OncoImmunology 2021;10:1893466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kroemer G, Galluzzi L, Kepp O, Zitvogel L. Immunogenic cell death in cancer therapy. Annu Rev Immunol 2013;31:51–72. [DOI] [PubMed] [Google Scholar]
- 3. Verburg SG, Lelievre RM, Westerveld MJ, Inkol JM, Sun YL, Workenhe ST. Viral-mediated activation and inhibition of programmed cell death. PLoS Pathog 2022;18:e1010718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Di Blasio S, Wortel IM, van Bladel DA, de Vries LE, Duiveman-de Boer T, Worah K, et al. Human CD1c(+) DCs are critical cellular mediators of immune responses induced by immunogenic cell death. Oncoimmunology 2016;5:e1192739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fucikova J, Becht E, Iribarren K, Goc J, Remark R, Damotte D, et al. Calreticulin expression in human non–small cell lung cancers correlates with increased accumulation of antitumor immune cells and favorable prognosis. Cancer Res 2016;76:1746–56. [DOI] [PubMed] [Google Scholar]
- 6. Hodge JW, Garnett CT, Farsaci B, Palena C, Tsang KY, Ferrone S, et al. Chemotherapy-induced immunogenic modulation of tumor cells enhances killing by cytotoxic T lymphocytes and is distinct from immunogenic cell death. Int J Cancer 2013;133:624–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zappasodi R, Pupa SM, Ghedini GC, Bongarzone I, Magni M, Cabras AD, et al. Improved clinical outcome in indolent B-cell lymphoma patients vaccinated with autologous tumor cells experiencing immunogenic death. Cancer Res 2010;70:9062–72. [DOI] [PubMed] [Google Scholar]
- 8. Lomphithak T, Akara-amornthum P, Murakami K, Hashimoto M, Usubuchi H, Iwabuchi E, et al. Tumor necroptosis is correlated with a favorable immune cell signature and programmed death-ligand 1 expression in cholangiocarcinoma. Sci Rep 2021;11:11743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nicolè L, Sanavia T, Cappellesso R, Maffeis V, Akiba J, Kawahara A, et al. Necroptosis-driving genes RIPK1, RIPK3 and MLKL-p are associated with intratumoral CD3+ and CD8+ T cell density and predict prognosis in hepatocellular carcinoma. J Immunother Cancer 2022;10:e004031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Seifert L, Werba G, Tiwari S, Giao Ly NN, Alothman S, Alqunaibit D, et al. The necrosome promotes pancreatic oncogenesis via CXCL1 and mincle-induced immune suppression. Nature 2016;532:245–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang W, Marinis JM, Beal AM, Savadkar S, Wu Y, Khan M, et al. RIP1 kinase drives macrophage-mediated adaptive immune tolerance in pancreatic cancer. Cancer Cell 2018;34:757–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Shalapour S, Font-Burgada J, Di Caro G, Zhong Z, Sanchez-Lopez E, Dhar D, et al. Immunosuppressive plasma cells impede T-cell-dependent immunogenic chemotherapy. Nature 2015;521:94–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lauber K, Blumenthal SG, Waibel M, Wesselborg S. Clearance of apoptotic cells: getting rid of the corpses. Mol Cell 2004;14:277–87. [DOI] [PubMed] [Google Scholar]
- 14. Fadok VA, Bratton DL, Henson PM. Phagocyte receptors for apoptotic cells: recognition, uptake, and consequences. J Clin Invest 2001;108:957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hoffmann PR, Kench JA, Vondracek A, Kruk E, Daleke DL, Jordan M, et al. Interaction between phosphatidylserine and the phosphatidylserine receptor inhibits immune responses in vivo. J Immunol 2005;174:1393–404. [DOI] [PubMed] [Google Scholar]
- 16. Steinman RM, Turley S, Mellman I, Inaba K. The induction of tolerance by dendritic cells that have captured apoptotic cells. J Exp Med 2000;191:411–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Liu K, Iyoda T, Saternus M, Kimura Y, Inaba K, Steinman RM. Immune tolerance after delivery of dying cells to dendritic cells in situ. J Exp Med 2002;196:1091–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ferguson TA, Herndon J, Elzey B, Griffith TS, Schoenberger S, Green DR. Uptake of apoptotic antigen-coupled cells by lymphoid dendritic cells and cross-priming of CD8+ T cells produce active immune unresponsiveness. J Immunol 2002;168:5589–95. [DOI] [PubMed] [Google Scholar]
- 19. Albert ML, Sauter B, Bhardwaj N. Dendritic cells acquire antigen from apoptotic cells and induce class I-restricted CTLs. Nature 1998;392:86–9. [DOI] [PubMed] [Google Scholar]
- 20. Casares N, Pequignot MO, Tesniere A, Ghiringhelli F, Roux S, Chaput N, et al. Caspase-dependent immunogenicity of doxorubicin-induced tumor cell death. J Exp Med 2005;202:1691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lhuillier C, Rudqvist NP, Yamazaki T, Zhang T, Charpentier M, Galluzzi L, et al. Radiotherapy-exposed CD8+ and CD4+ neoantigens enhance tumor control. J Clin Invest 2021;131:e138740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Workenhe ST, Simmons G, Pol JG, Lichty BD, Halford W, Mossman KL. Immunogenic HSV mediated oncolysis shapes the antitumor immune response and contributes to therapeutic efficacy. Mol Ther 2014;22:123–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Alzeibak R, Mishchenko TA, Shilyagina NY, Balalaeva IV, Vedunova MV, Krysko DV. Targeting immunogenic cancer cell death by photodynamic therapy: past, present and future. J Immunother Cancer 2021;9:e001926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Coppard C, Hannani D, Humbert M, Gauthier V, Plumas J, Merlin E, et al. In vitro PUVA treatment triggers calreticulin exposition and HMGB1 release by dying T lymphocytes in GVHD: new insights in extracorporeal photopheresis. J Clin Apher 2019;34:450–60. [DOI] [PubMed] [Google Scholar]
- 25. Tatsuno K, Yamazaki T, Hanlon D, Han P, Robinson E, Sobolev O, et al. Extracorporeal photochemotherapy induces bona fide immunogenic cell death. Cell Death Dis 2019;10:578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Obeid M, Tesniere A, Ghiringhelli F, Fimia GM, Apetoh L, Perfettini JL, et al. Calreticulin exposure dictates the immunogenicity of cancer cell death. Nat Med 2007;13:54–61. [DOI] [PubMed] [Google Scholar]
- 27. Ma Y, Adjemian S, Mattarollo SR, Yamazaki T, Aymeric L, Yang H, et al. Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity 2013;38:729–41. [DOI] [PubMed] [Google Scholar]
- 28. Michaud M, Martins I, Sukkurwala AQ, Adjemian S, Ma Y, Pellegatti P, et al. Autophagy-dependent anticancer immune responses induced by chemotherapeutic agents in mice. Science 2011;334:1573–7. [DOI] [PubMed] [Google Scholar]
- 29. Apetoh L, Ghiringhelli F, Tesniere A, Criollo A, Ortiz C, Lidereau R, et al. The interaction between HMGB1 and TLR4 dictates the outcome of anticancer chemotherapy and radiotherapy. Immunol Rev 2007;220:47–59. [DOI] [PubMed] [Google Scholar]
- 30. Aaes TL, Verschuere H, Kaczmarek A, Heyndrickx L, Wiernicki B, Delrue I, et al. Immunodominant AH1 antigen-deficient necroptotic, but not apoptotic, murine cancer cells induce antitumor protection. J Immunol 2020;204:775–87. [DOI] [PubMed] [Google Scholar]
- 31. Rudqvist N-P, Pilones KA, Lhuillier C, Wennerberg E, Sidhom J-W, Emerson RO, et al. Radiotherapy and CTLA-4 blockade shape the TCR repertoire of tumor-infiltrating T cells. Cancer Immunol Res 2018;6:139–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Srivastava S, Furlan SN, Jaeger-Ruckstuhl CA, Sarvothama M, Berger C, Smythe KS, et al. Immunogenic chemotherapy enhances recruitment of CAR-T cells to lung tumors and improves antitumor efficacy when combined with checkpoint blockade. Cancer Cell 2021;39:193–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pfirschke C, Engblom C, Rickelt S, Cortez-Retamozo V, Garris C, Pucci F, et al. Immunogenic chemotherapy sensitizes tumors to checkpoint blockade therapy. Immunity 2016;44:343–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Workenhe ST, Nguyen A, Bakhshinyan D, Wei J, Hare DN, MacNeill KL, et al. De novo necroptosis creates an inflammatory environment mediating tumor susceptibility to immune checkpoint inhibitors. Commun Biol 2020;3:645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Janjigian YY, Shitara K, Moehler M, Garrido M, Salman P, Shen L, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. Lancet 2021;398:27–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cortes J, Cescon DW, Rugo HS, Nowecki Z, Im S-A, Yusof MM, et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for previously untreated locally recurrent inoperable or metastatic triple-negative breast cancer (KEYNOTE-355): a randomised, placebo-controlled, double-blind, phase 3 clinical trial. Lancet 2020;396:1817–28. [DOI] [PubMed] [Google Scholar]
- 37. Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G Jr, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 2019;394:1915–28. [DOI] [PubMed] [Google Scholar]
- 38. Schmid P, Adams S, Rugo HS, Schneeweiss A, Barrios CH, Iwata H, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer. N Engl J Med 2018;379:2108–21. [DOI] [PubMed] [Google Scholar]
- 39. Voorwerk L, Slagter M, Horlings HM, Sikorska K, van de Vijver KK, de Maaker M, et al. Immune induction strategies in metastatic triple-negative breast cancer to enhance the sensitivity to PD-1 blockade: the TONIC trial. Nat Med 2019;25:920–8. [DOI] [PubMed] [Google Scholar]
- 40. Akamatsu H, Teraoka S, Hayashi H, Fujimoto D, Hayata A, Haratani K, et al. Pembrolizumab plus amrubicin in patients with relapsed SCLC: multi-institutional, single-arm phase 2 study. JTO Clin Res Rep 2021;2:100184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cortes J, Rugo HS, Cescon DW, Im S-A, Yusof MM, Gallardo C, et al. Pembrolizumab plus chemotherapy in advanced triple-negative breast cancer. N Engl J Med 2022;387:217–26. [DOI] [PubMed] [Google Scholar]
- 42. Rizvi N, Ademuyiwa FO, Cao ZA, Chen HX, Ferris RL, Goldberg SB, et al. Society for immunotherapy of cancer (SITC) consensus definitions for resistance to combinations of immune checkpoint inhibitors with chemotherapy. J Immunother Cancer 2023;11:e005920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Snyder AG, Hubbard NW, Messmer MN, Kofman SB, Hagan CE, Orozco SL, et al. Intratumoral activation of the necroptotic pathway components RIPK1 and RIPK3 potentiates antitumor immunity. Sci Immunol 2019;4:eaaw2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Yatim N, Jusforgues-Saklani H, Orozco S, Schulz O, Barreira da Silva R, Reis e Sousa C, et al. RIPK1 and NF-κB signaling in dying cells determines cross-priming of CD8+ T cells. Science 2015;350:328–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wang Y, Gao W, Shi X, Ding J, Liu W, He H, et al. Chemotherapy drugs induce pyroptosis through caspase-3 cleavage of a gasdermin. Nature 2017;547:99–103. [DOI] [PubMed] [Google Scholar]
- 46. Zhang Z, Zhang Y, Xia S, Kong Q, Li S, Liu X, et al. Gasdermin E suppresses tumour growth by activating anti-tumour immunity. Nature 2020;579:415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zhou Z, He H, Wang K, Shi X, Wang Y, Su Y, et al. Granzyme a from cytotoxic lymphocytes cleaves GSDMB to trigger pyroptosis in target cells. Science 2020;368:eaaz7548. [DOI] [PubMed] [Google Scholar]
- 48. Lin J, Sun S, Zhao K, Gao F, Wang R, Li Q, et al. Oncolytic parapoxvirus induces gasdermin E-mediated pyroptosis and activates antitumor immunity. Nat Commun 2023;14:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wang Q, Wang Y, Ding J, Wang C, Zhou X, Gao W, et al. A bioorthogonal system reveals antitumour immune function of pyroptosis. Nature 2020;579:421–6. [DOI] [PubMed] [Google Scholar]
- 50. Wiernicki B, Maschalidi S, Pinney J, Adjemian S, Vanden Berghe T, Ravichandran KS, et al. Cancer cells dying from ferroptosis impede dendritic cell-mediated anti-tumor immunity. Nat Commun 2022;13:3676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Chryplewicz A, Scotton J, Tichet M, Zomer A, Shchors K, Joyce JA, et al. Cancer cell autophagy, reprogrammed macrophages, and remodeled vasculature in glioblastoma triggers tumor immunity. Cancer Cell 2022;40:1111–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Panaretakis T, Joza N, Modjtahedi N, Tesniere A, Vitale I, Durchschlag M, et al. The co-translocation of ERp57 and calreticulin determines the immunogenicity of cell death. Cell Death Differ 2008;15:1499–509. [DOI] [PubMed] [Google Scholar]
- 53. Panaretakis T, Kepp O, Brockmeier U, Tesniere A, Bjorklund A-C, Chapman DC, et al. Mechanisms of pre-apoptotic calreticulin exposure in immunogenic cell death. EMBO J 2009;28:578–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ciampricotti M, Hau CS, Doornebal CW, Jonkers J, de Visser KE. Chemotherapy response of spontaneous mammary tumors is independent of the adaptive immune system. Nat Med 2012;18:344–6. [DOI] [PubMed] [Google Scholar]
- 55. White Michael J, McArthur K, Metcalf D, Lane Rachael M, Cambier John C, Herold Marco J, et al. Apoptotic caspases suppress mtDNA-induced STING-mediated type I IFN production. Cell 2014;159:1549–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Rongvaux A, Jackson R, Harman Christian CD, Li T, West AP, de Zoete Marcel R, et al. Apoptotic caspases prevent the induction of type I interferons by mitochondrial DNA. Cell 2014;159:1563–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Ning X, Wang Y, Jing M, Sha M, Lv M, Gao P, et al. Apoptotic caspases suppress type I interferon production via the cleavage of cGAS, MAVS, and IRF3. Mol Cell 2019;74:19–31. [DOI] [PubMed] [Google Scholar]
- 58. Giampazolias E, Zunino B, Dhayade S, Bock F, Cloix C, Cao K, et al. Mitochondrial permeabilization engages NF-κB-dependent anti-tumour activity under caspase deficiency. Nat Cell Biol 2017;19:1116–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Obeid M. ERP57 membrane translocation dictates the immunogenicity of tumor cell death by controlling the membrane translocation of calreticulin. J Immunol 2008;181:2533–43. [DOI] [PubMed] [Google Scholar]
- 60. Sen Santara S, Lee D-J, Crespo Â, Hu JJ, Walker C, Ma X, et al. The NK cell receptor NKp46 recognizes ecto-calreticulin on ER-stressed cells. Nature 2023;616:348–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Xia S, Zhang Z, Magupalli VG, Pablo JL, Dong Y, Vora SM, et al. Gasdermin D pore structure reveals preferential release of mature interleukin-1. Nature 2021;593:607–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Liu X, Zhang Z, Ruan J, Pan Y, Magupalli VG, Wu H, et al. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature 2016;535:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Phulphagar K, Kühn LI, Ebner S, Frauenstein A, Swietlik JJ, Rieckmann J, et al. Proteomics reveals distinct mechanisms regulating the release of cytokines and alarmins during pyroptosis. Cell Rep 2021;34:108826. [DOI] [PubMed] [Google Scholar]
- 64. Kayagaki N, Kornfeld OS, Lee BL, Stowe IB, O'Rourke K, Li Q, et al. NINJ1 mediates plasma membrane rupture during lytic cell death. Nature 2021;591:131–6. [DOI] [PubMed] [Google Scholar]
- 65. Degen M, Santos JC, Pluhackova K, Cebrero G, Ramos S, Jankevicius G, et al. Structural basis of NINJ1-mediated plasma membrane rupture in cell death. Nature 2023;618:1065–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Wang M, Wu M, Liu X, Shao S, Huang J, Liu B, et al. Pyroptosis remodeling tumor microenvironment to enhance pancreatic cancer immunotherapy driven by membrane anchoring photosensitizer. Adv Sci 2022;9:e2202914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hu L, Chen M, Chen X, Zhao C, Fang Z, Wang H, et al. Chemotherapy-induced pyroptosis is mediated by BAK/BAX-caspase-3-GSDME pathway and inhibited by 2-bromopalmitate. Cell Death Dis 2020;11:281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Liu Y, Fang Y, Chen X, Wang Z, Liang X, Zhang T, et al. Gasdermin E–mediated target cell pyroptosis by CAR T cells triggers cytokine release syndrome. Sci Immunol 2020;5:eaax7969. [DOI] [PubMed] [Google Scholar]
- 69. Rogers C, Erkes DA, Nardone A, Aplin AE, Fernandes-Alnemri T, Alnemri ES. Gasdermin pores permeabilize mitochondria to augment caspase-3 activation during apoptosis and inflammasome activation. Nat Commun 2019;10:1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Riley JS, Tait SW. Mitochondrial DNA in inflammation and immunity. EMBO Rep 2020;21:e49799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Lin P-H, Lin H-Y, Kuo C-C, Yang L-T. N-terminal functional domain of gasdermin A3 regulates mitochondrial homeostasis via mitochondrial targeting. J Biomed Sci 2015;22:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Vandenabeele P, Galluzzi L, Vanden Berghe T, Kroemer G. Molecular mechanisms of necroptosis: an ordered cellular explosion. Nat Rev Mol Cell Biol 2010;11:700–14. [DOI] [PubMed] [Google Scholar]
- 73. Sun L, Wang H, Wang Z, He S, Chen S, Liao D, et al. Mixed lineage kinase domain-like protein mediates necrosis signaling downstream of RIP3 kinase. Cell 2012;148:213–27. [DOI] [PubMed] [Google Scholar]
- 74. Mompeán M, Li W, Li J, Laage S, Siemer AB, Bozkurt G, et al. The structure of the necrosome RIPK1-RIPK3 core, a human hetero-amyloid signaling complex. Cell 2018;173:1244–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Locatelli SL, Cleris L, Stirparo GG, Tartari S, Saba E, Pierdominici M, et al. BIM upregulation and ROS-dependent necroptosis mediate the antitumor effects of the HDACi givinostat and sorafenib in hodgkin lymphoma cell line xenografts. Leukemia 2014;28:1861–71. [DOI] [PubMed] [Google Scholar]
- 76. Tenev T, Bianchi K, Darding M, Broemer M, Langlais C, Wallberg F, et al. The ripoptosome, a signaling platform that assembles in response to genotoxic stress and loss of IAPs. Mol Cell 2011;43:432–48. [DOI] [PubMed] [Google Scholar]
- 77. Basit F, Cristofanon S, Fulda S. Obatoclax (GX15–070) triggers necroptosis by promoting the assembly of the necrosome on autophagosomal membranes. Cell Death Differ 2013;20:1161–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Nehs MA, Lin CI, Kozono DE, Whang EE, Cho NL, Zhu K, et al. Necroptosis is a novel mechanism of radiation-induced cell death in anaplastic thyroid and adrenocortical cancers. Surgery 2011;150:1032–9. [DOI] [PubMed] [Google Scholar]
- 79. Das A, McDonald DG, Dixon-Mah YN, Jacqmin DJ, Samant VN, Vandergrift WA 3rd, et al. RIP1 and RIP3 complex regulates radiation-induced programmed necrosis in glioblastoma. Tumour Biol 2016;37:7525–34. [DOI] [PubMed] [Google Scholar]
- 80. Mantel F, Frey B, Haslinger S, Schildkopf P, Sieber R, Ott OJ, et al. Combination of ionising irradiation and hyperthermia activates programmed apoptotic and necrotic cell death pathways in human colorectal carcinoma cells. Strahlenther Onkol 2010;186:587–99. [DOI] [PubMed] [Google Scholar]
- 81. Zhang J, Liu Y, Tan J, Zhang Y, Wong C-W, Lin Z, et al. Necroptotic virotherapy of oncolytic alphavirus M1 cooperated with Doxorubicin displays promising therapeutic efficacy in TNBC. Oncogene 2021;40:4783–95. [DOI] [PubMed] [Google Scholar]
- 82. Van Hoecke L, Riederer S, Saelens X, Sutter G, Rojas JJ. Recombinant viruses delivering the necroptosis mediator MLKL induce a potent antitumor immunity in mice. Oncoimmunology 2020;9:1802968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Van Hoecke L, Van Lint S, Roose K, Van Parys A, Vandenabeele P, Grooten J, et al. Treatment with mRNA coding for the necroptosis mediator MLKL induces antitumor immunity directed against neo-epitopes. Nat Commun 2018;9:3417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Dixon Scott J, Lemberg Kathryn M, Lamprecht Michael R, Skouta R, Zaitsev Eleina M, Gleason Caroline E, et al. Ferroptosis: an iron-dependent form of nonapoptotic cell death. Cell 2012;149:1060–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Jiang X, Stockwell BR, Conrad M. Ferroptosis: mechanisms, biology and role in disease. Nat Rev Mol Cell Biol 2021;22:266–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Seiler A, Schneider M, Förster H, Roth S, Wirth EK, Culmsee C, et al. Glutathione peroxidase 4 senses and translates oxidative stress into 12/15-lipoxygenase dependent- and AIF-mediated cell death. Cell Metab 2008;8:237–48. [DOI] [PubMed] [Google Scholar]
- 87. Shibata Y, Yasui H, Higashikawa K, Miyamoto N, Kuge Y. Erastin, a ferroptosis-inducing agent, sensitized cancer cells to X-ray irradiation via glutathione starvation in vitro and in vivo. PLoS One 2019;14:e0225931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Pan X, Lin Z, Jiang D, Yu Y, Yang D, Zhou H, et al. Erastin decreases radioresistance of NSCLC cells partially by inducing GPX4-mediated ferroptosis. Oncol Lett 2019;17:3001–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Nagane M, Kanai E, Shibata Y, Shimizu T, Yoshioka C, Maruo T, et al. Sulfasalazine, an inhibitor of the cystine-glutamate antiporter, reduces DNA damage repair and enhances radiosensitivity in murine B16F10 melanoma. PLoS One 2018;13:e0195151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Sleire L, Skeie BS, Netland IA, Førde HE, Dodoo E, Selheim F, et al. Drug repurposing: sulfasalazine sensitizes gliomas to gamma knife radiosurgery by blocking cystine uptake through system Xc-, leading to glutathione depletion. Oncogene 2015;34:5951–9. [DOI] [PubMed] [Google Scholar]
- 91. Ma S, Henson ES, Chen Y, Gibson SB. Ferroptosis is induced following siramesine and lapatinib treatment of breast cancer cells. Cell Death Dis 2016;7:e2307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Lei G, Zhang Y, Koppula P, Liu X, Zhang J, Lin SH, et al. The role of ferroptosis in ionizing radiation-induced cell death and tumor suppression. Cell Res 2020;30:146–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Nagpal A, Redvers RP, Ling X, Ayton S, Fuentes M, Tavancheh E, et al. Neoadjuvant neratinib promotes ferroptosis and inhibits brain metastasis in a novel syngeneic model of spontaneous HER2(+ve) breast cancer metastasis. Breast Cancer Res 2019;21:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Efimova I, Catanzaro E, Van der Meeren L, Turubanova VD, Hammad H, Mishchenko TA, et al. Vaccination with early ferroptotic cancer cells induces efficient antitumor immunity. J Immunother Cancer 2020;8:e001369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti–PD-L1 efficacy. Science 2015;350:1084–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Dai E, Han L, Liu J, Xie Y, Zeh HJ, Kang R, et al. Ferroptotic damage promotes pancreatic tumorigenesis through a TMEM173/STING-dependent DNA sensor pathway. Nat Commun 2020;11:6339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Dai E, Han L, Liu J, Xie Y, Kroemer G, Klionsky DJ, et al. Autophagy-dependent ferroptosis drives tumor-associated macrophage polarization via release and uptake of oncogenic KRAS protein. Autophagy 2020;16:2069–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wang W, Green M, Choi JE, Gijón M, Kennedy PD, Johnson JK, et al. CD8(+) T cells regulate tumour ferroptosis during cancer immunotherapy. Nature 2019;569:270–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Liao P, Wang W, Wang W, Kryczek I, Li X, Bian Y, et al. CD8+ T cells and fatty acids orchestrate tumor ferroptosis and immunity via ACSL4. Cancer Cell 2022;40:365–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Koo G-B, Morgan MJ, Lee D-G, Kim W-J, Yoon J-H, Koo JS, et al. Methylation-dependent loss of RIP3 expression in cancer represses programmed necrosis in response to chemotherapeutics. Cell Res 2015;25:707–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Fukasawa M, Kimura M, Morita S, Matsubara K, Yamanaka S, Endo C, et al. Microarray analysis of promoter methylation in lung cancers. J Hum Genet 2006;51:368–74. [DOI] [PubMed] [Google Scholar]
- 102. Nugues AL, El Bouazzati H, Hétuin D, Berthon C, Loyens A, Bertrand E, et al. RIP3 is downregulated in human myeloid leukemia cells and modulates apoptosis and caspase-mediated p65/RelA cleavage. Cell Death Dis 2014;5:e1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Moriwaki K, Bertin J, Gough PJ, Orlowski GM, Chan FK. Differential roles of RIPK1 and RIPK3 in TNF-induced necroptosis and chemotherapeutic agent-induced cell death. Cell Death Dis 2015;6:e1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Akino K, Toyota M, Suzuki H, Imai T, Maruyama R, Kusano M, et al. Identification of DFNA5 as a target of epigenetic inactivation in gastric cancer. Cancer Sci 2007;98:88–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Ibrahim J, Op de Beeck K, Fransen E, Croes L, Beyens M, Suls A, et al. Methylation analysis of gasdermin E shows great promise as a biomarker for colorectal cancer. Cancer Med 2019;8:2133–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Cerhan JR, Ansell SM, Fredericksen ZS, Kay NE, Liebow M, Call TG, et al. Genetic variation in 1253 immune and inflammation genes and risk of non-Hodgkin lymphoma. Blood 2007;110:4455–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Geserick P, Wang J, Schilling R, Horn S, Harris PA, Bertin J, et al. Absence of RIPK3 predicts necroptosis resistance in malignant melanoma. Cell Death Dis 2015;6:e1884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Höckendorf U, Yabal M, Herold T, Munkhbaatar E, Rott S, Jilg S, et al. RIPK3 restricts myeloid leukemogenesis by promoting cell death and differentiation of leukemia initiating cells. Cancer Cell 2016;30:75–91. [DOI] [PubMed] [Google Scholar]
- 109. Lin C-C, Mabe NW, Lin Y-T, Yang W-H, Tang X, Hong L, et al. RIPK3 upregulation confers robust proliferation and collateral cystine-dependence on breast cancer recurrence. Cell Death Differ 2020;27:2234–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Rogers C, Fernandes-Alnemri T, Mayes L, Alnemri D, Cingolani G, Alnemri ES. Cleavage of DFNA5 by caspase-3 during apoptosis mediates progression to secondary necrotic/pyroptotic cell death. Nat Commun 2017;8:14128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kong Q, Xia S, Pan X, Ye K, Li Z, Li H, et al. Alternative splicing of GSDMB modulates killer lymphocyte–triggered pyroptosis. Sci Immunol 2023;8:eadg3196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Saeki N, Usui T, Aoyagi K, Kim DH, Sato M, Mabuchi T, et al. Distinctive expression and function of four GSDM family genes (GSDMA-D) in normal and malignant upper gastrointestinal epithelium. Genes Chromosomes Cancer 2009;48:261–71. [DOI] [PubMed] [Google Scholar]
- 113. Moussette S, Al Tuwaijri A, Kohan-Ghadr HR, Elzein S, Farias R, Bérubé J, et al. Role of DNA methylation in expression control of the IKZF3-GSDMA region in human epithelial cells. PLoS One 2017;12:e0172707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Saeki N, Kim DH, Usui T, Aoyagi K, Tatsuta T, Aoki K, et al. GASDERMIN, suppressed frequently in gastric cancer, is a target of LMO1 in TGF-beta-dependent apoptotic signalling. Oncogene 2007;26:6488–98. [DOI] [PubMed] [Google Scholar]
- 115. Wellenstein MD, de Visser KE. Cancer-cell-intrinsic mechanisms shaping the tumor immune landscape. Immunity 2018;48:399–416. [DOI] [PubMed] [Google Scholar]
- 116. Canon J, Rex K, Saiki AY, Mohr C, Cooke K, Bagal D, et al. The clinical KRAS(G12C) inhibitor AMG 510 drives anti-tumour immunity. Nature 2019;575:217–23. [DOI] [PubMed] [Google Scholar]
- 117. Abaan OD, Polley EC, Davis SR, Zhu YJ, Bilke S, Walker RL, et al. The exomes of the NCI-60 panel: a genomic resource for cancer biology and systems pharmacology. Cancer Res 2013;73:4372–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Casey SC, Tong L, Li Y, Do R, Walz S, Fitzgerald KN, et al. MYC regulates the antitumor immune response through CD47 and PD-L1. Science 2016;352:227–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Seong D, Jeong M, Seo J, Lee J-Y, Hwang CH, Shin H-C, et al. Identification of MYC as an antinecroptotic protein that stifles RIPK1–RIPK3 complex formation. Proc Natl Acad Sci U S A 2020;117:19982–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Najafov A, Zervantonakis IK, Mookhtiar AK, Greninger P, March RJ, Egan RK, et al. BRAF and AXL oncogenes drive RIPK3 expression loss in cancer. PLoS Biol 2018;16:e2005756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Erkes DA, Cai W, Sanchez IM, Purwin TJ, Rogers C, Field CO, et al. Mutant BRAF and MEK inhibitors regulate the tumor immune microenvironment via pyroptosis. Cancer Discov 2020;10:254–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Miyashita T, Reed JC. Tumor suppressor p53 is a direct transcriptional activator of the human bax gene. Cell 1995;80:293–9. [DOI] [PubMed] [Google Scholar]
- 123. Nakano K, Vousden KH. PUMA, a novel proapoptotic gene, is induced by p53. Mol Cell 2001;7:683–94. [DOI] [PubMed] [Google Scholar]
- 124. Oda E, Ohki R, Murasawa H, Nemoto J, Shibue T, Yamashita T, et al. Noxa, a BH3-only member of the Bcl-2 family and candidate mediator of p53-induced apoptosis. Science 2000;288:1053–8. [DOI] [PubMed] [Google Scholar]
- 125. Chipuk JE, Kuwana T, Bouchier-Hayes L, Droin NM, Newmeyer DD, Schuler M, et al. Direct activation of Bax by p53 mediates mitochondrial membrane permeabilization and apoptosis. Science 2004;303:1010–4. [DOI] [PubMed] [Google Scholar]
- 126. Knudsen KE, Weber E, Arden KC, Cavenee WK, Feramisco JR, Knudsen ES. The retinoblastoma tumor suppressor inhibits cellular proliferation through two distinct mechanisms: inhibition of cell cycle progression and induction of cell death. Oncogene 1999;18:5239–45. [DOI] [PubMed] [Google Scholar]
- 127. Ianari A, Natale T, Calo E, Ferretti E, Alesse E, Screpanti I, et al. Proapoptotic function of the retinoblastoma tumor suppressor protein. Cancer Cell 2009;15:184–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Hilgendorf KI, Leshchiner ES, Nedelcu S, Maynard MA, Calo E, Ianari A, et al. The retinoblastoma protein induces apoptosis directly at the mitochondria. Genes Dev 2013;27:1003–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Stambolic V, Suzuki A, de la Pompa JL, Brothers GM, Mirtsos C, Sasaki T, et al. Negative regulation of PKB/Akt-dependent cell survival by the tumor suppressor PTEN. Cell 1998;95:29–39. [DOI] [PubMed] [Google Scholar]
- 130. Kinoshita T, Yokota T, Arai K, Miyajima A. Regulation of Bcl-2 expression by oncogenic Ras protein in hematopoietic cells. Oncogene 1995;10:2207–12. [PubMed] [Google Scholar]
- 131. Jiang CC, Lai F, Tay KH, Croft A, Rizos H, Becker TM, et al. Apoptosis of human melanoma cells induced by inhibition of B-RAFV600E involves preferential splicing of bimS. Cell Death Dis 2010;1:e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Paraiso KH, Xiang Y, Rebecca VW, Abel EV, Chen YA, Munko AC, et al. PTEN loss confers BRAF inhibitor resistance to melanoma cells through the suppression of BIM expression. Cancer Res 2011;71:2750–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Lu H, Zhang S, Wu J, Chen M, Cai M-C, Fu Y, et al. Molecular targeted therapies elicit concurrent apoptotic and GSDME-dependent pyroptotic tumor cell death. Clin Cancer Res 2018;24:6066–77. [DOI] [PubMed] [Google Scholar]
- 134. Yagoda N, von Rechenberg M, Zaganjor E, Bauer AJ, Yang WS, Fridman DJ, et al. RAS-RAF-MEK-dependent oxidative cell death involving voltage-dependent anion channels. Nature 2007;447:864–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Yang WS, Stockwell BR. Synthetic lethal screening identifies compounds activating iron-dependent, nonapoptotic cell death in oncogenic-RAS-harboring cancer cells. Chem Biol 2008;15:234–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Hu K, Li K, Lv J, Feng J, Chen J, Wu H, et al. Suppression of the SLC7A11/glutathione axis causes synthetic lethality in KRAS-mutant lung adenocarcinoma. J Clin Invest 2020;130:1752–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Poursaitidis I, Wang X, Crighton T, Labuschagne C, Mason D, Cramer SL, et al. Oncogene-selective sensitivity to synchronous cell death following modulation of the amino acid nutrient cystine. Cell Rep 2017;18:2547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Jiang L, Kon N, Li T, Wang SJ, Su T, Hibshoosh H, et al. Ferroptosis as a p53-mediated activity during tumour suppression. Nature 2015;520:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Wang SJ, Li D, Ou Y, Jiang L, Chen Y, Zhao Y, et al. Acetylation is crucial for p53-mediated ferroptosis and tumor suppression. Cell Rep 2016;17:366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Kroemer G, Galassi C, Zitvogel L, Galluzzi L. Immunogenic cell stress and death. Nat Immunol 2022;23:487–500. [DOI] [PubMed] [Google Scholar]
- 141. Viaud S, Saccheri F, Mignot G, Yamazaki T, Daillère R, Hannani D, et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 2013;342:971–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Kepp O, Kroemer G. Is ferroptosis immunogenic? The devil is in the details! Oncoimmunology 2022;11:2127273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Sriram G, Milling LE, Chen JK, Kong YW, Joughin BA, Abraham W, et al. The injury response to DNA damage in live tumor cells promotes antitumor immunity. Sci Signal 2021;14:eabc4764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Marin I, Boix O, Garcia-Garijo A, Sirois I, Caballe A, Zarzuela E, et al. Cellular senescence is immunogenic and promotes antitumor immunity. Cancer Discov 2023;13:410–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. van Vloten JP, Workenhe ST, Wootton SK, Mossman KL, Bridle BW. Critical interactions between immunogenic cancer cell death, oncolytic viruses, and the immune system define the rational design of combination immunotherapies. J Immunol 2018;200:450–8. [DOI] [PubMed] [Google Scholar]
- 146. Karki R, Kanneganti T-D. Diverging inflammasome signals in tumorigenesis and potential targeting. Nat Rev Cancer 2019;19:197–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Daley D, Mani VR, Mohan N, Akkad N, Pandian GSDB, Savadkar S, et al. NLRP3 signaling drives macrophage-induced adaptive immune suppression in pancreatic carcinoma. J Exp Med 2017;214:1711–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Saijo Y, Tanaka M, Miki M, Usui K, Suzuki T, Maemondo M, et al. Proinflammatory cytokine IL-1 beta promotes tumor growth of Lewis lung carcinoma by induction of angiogenic factors: in vivo analysis of tumor-stromal interaction. J Immunol 2002;169:469–75. [DOI] [PubMed] [Google Scholar]
- 149. Tu S, Bhagat G, Cui G, Takaishi S, Kurt-Jones EA, Rickman B, et al. Overexpression of interleukin-1beta induces gastric inflammation and cancer and mobilizes myeloid-derived suppressor cells in mice. Cancer Cell 2008;14:408–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Nakamura K, Kassem S, Cleynen A, Chrétien M-L, Guillerey C, Putz EM, et al. Dysregulated IL-18 is a key driver of immunosuppression and a possible therapeutic target in the multiple myeloma microenvironment. Cancer Cell 2018;33:634–48. [DOI] [PubMed] [Google Scholar]
- 151. Terme M, Ullrich E, Aymeric L, Meinhardt K, Desbois M, Delahaye N, et al. IL-18 induces PD-1-dependent immunosuppression in cancer. Cancer Res 2011;71:5393–9. [DOI] [PubMed] [Google Scholar]
- 152. Kang JS, Bae SY, Kim HR, Kim YS, Kim DJ, Cho BJ, et al. Interleukin-18 increases metastasis and immune escape of stomach cancer via the downregulation of CD70 and maintenance of CD44. Carcinogenesis 2009;30:1987–96. [DOI] [PubMed] [Google Scholar]
- 153. Yang H, Ma Y, Chen G, Zhou H, Yamazaki T, Klein C, et al. Contribution of RIP3 and MLKL to immunogenic cell death signaling in cancer chemotherapy. Oncoimmunology 2016;5:e1149673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. Aaes Tania L, Kaczmarek A, Delvaeye T, De Craene B, De Koker S, Heyndrickx L, et al. Vaccination with necroptotic cancer cells induces efficient anti-tumor immunity. Cell Rep 2016;15:274–87. [DOI] [PubMed] [Google Scholar]
- 155. Pol J, Vacchelli E, Aranda F, Castoldi F, Eggermont A, Cremer I, et al. Trial watch: immunogenic cell death inducers for anticancer chemotherapy. Oncoimmunology 2015;4:e1008866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Zagorulya M, Yim L, Morgan DM, Edwards A, Torres-Mejia E, Momin N, et al. Tissue-specific abundance of interferon-gamma drives regulatory T cells to restrain DC1-mediated priming of cytotoxic T cells against lung cancer. Immunity 2023;56:386–405. [DOI] [PMC free article] [PubMed] [Google Scholar]