Abstract
Machine learning (ML) analyses using 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET)/computed tomography (CT) radiomics features have been applied in the field of oncology. The current review aimed to summarize the current clinical articles about 18F-FDG PET/CT radiomics-based ML analyses to solve issues in classifying or constructing prediction models for several types of tumors. In these studies, lung and mediastinal tumors were the most commonly evaluated lesions, followed by lymphatic, abdominal, head and neck, breast, gynecological, and other types of tumors. Previous studies have commonly shown that 18F-FDG PET radiomics-based ML analysis has good performance in differentiating benign from malignant tumors, predicting tumor characteristics and stage, therapeutic response, and prognosis by examining significant differences in the area under the receiver operating characteristic curves, accuracies, or concordance indices (> 0.70). However, these studies have reported several ML algorithms. Moreover, different ML models have been applied for the same purpose. Thus, various procedures were used in 18F-FDG PET/CT radiomics-based ML analysis in oncology, and 18F-FDG PET/CT radiomics-based ML models, which are easy and universally applied in clinical practice, would be expected to be established.
Keywords: 18F-FDG, PET/CT, Radiomics, Machine learning, Oncology
Introduction
Positron emission tomography (PET)/computed tomography (CT) with 18F-fluorodeoxyglucose (18F-FDG), a glucose analog that reflects metabolic glucose activity, is widely used in oncology [1]. Radiomics refers to different mathematical methods for extracting several quantitative features to obtain useful biological information [2], and radiomics-based 18F-FDG PET has also been applied in oncology [3–6].
The development of artificial intelligence (AI) is associated with relevant psychological, ethical, and medicolegal issues, which should be addressed before AI can be completely considered in patient management. However, the ultra-rapid analysis of large datasets is a major strength of AI in healthcare applications. In the field of medical imaging, AI has been significantly beneficial in predicting individual patient outcomes [7, 8]. Machine learning (ML) can resolve complex interactions among numerous variables to construct a prediction model as accurate as possible [9–11]. The flexibility and scalability of ML are superior to those of conventional statistical approaches. Hence, ML is useful in several tasks including diagnosis and classification.
Recently, the ML or deep learning (DL) models using 18F-FDG PET/CT radiomic features have been applied to resolve issues in classification (i.e., “benign or malignant tumor,” “primary or metastatic tumor,” “classification of histological subtypes,” and “recurrence or non-recurrence”) or to construct prediction models (i.e., “tumor characteristic,” “tumor stage,” or “survival”) [12]. The current review aimed to summarize the current clinical studies on 18F-FDG PET/CT radiomics-based ML analyses to address issues in classification or to construct prediction models for several types of tumors.
Literature search and screening
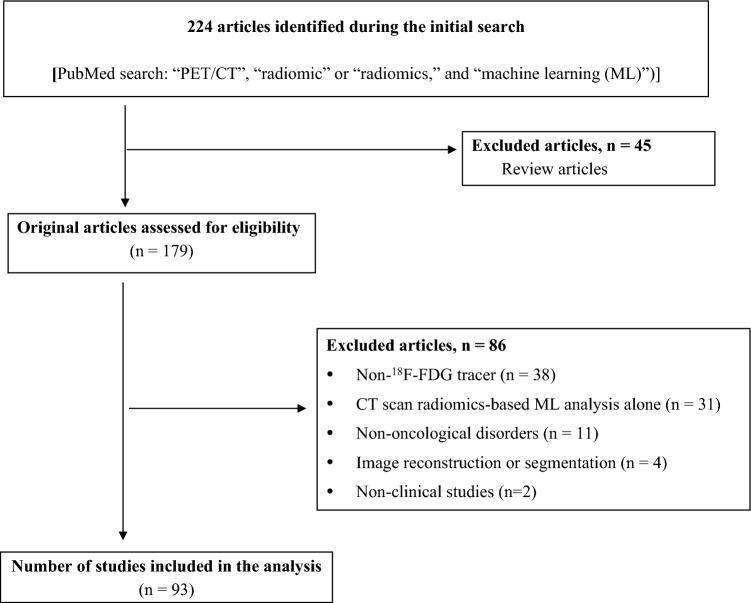
On April 20, 2023, we searched studies with the following terms in the title from PubMed: “PET/CT” and “radiomic” or “radiomics” and “machine learning.”
In total, 224 articles were identified during the initial search. The titles, abstracts, and texts were assessed to identify relevant articles. The inclusion criteria were as follows: (1) studies written in English, (2) original clinical studies about oncology, and (3) studies describing the application of the 18F-FDG PET/CT radiomics-based ML approach for solving issues associated with classifying or constructing prediction models. The exclusion criteria were as follows: 1) reports only describing the CT radiomics-based ML approach, 2) studies using ML for image reconstruction or segmentation, 3) cohort studies with < 20 patients, and 4) review articles. Of 224 articles identified, 45 were review articles; hence, they were not included in the study. Among the remaining 179 original articles, 86 were excluded because of non-18F-FDG tracer (n = 38), only CT-based radiomic ML analysis (n = 31), non-oncological disorders (n = 11), application of ML for image reconstruction or image segmentation (n = 4) and nonclinical studies (n = 2). Finally, 93 articles were included in the analysis, and all articles were published after 2018 (Fig. 1).
Fig. 1.
Flowchart of study retrieval via literature search and inclusion in the analysis
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in lung or mediastinal tumors
Difference between benign and malignant tumors and between primary and metastatic tumors
Pulmonary nodules are common clinical findings, and lung cancer frequently presents as a solitary pulmonary nodule (SPN) on diagnostic imaging at the early disease stage [13]. SPNs are often incidentally detected. Thus, benign SPNs should be clinically differentiated from malignant SPNs.
Ren et al. [14] reported that the ML model with the least absolute shrinkage and selection operator (LASSO) regression algorithm using combined clinical data and PET-radiomics had a good diagnostic performance for distinguishing benign from malignant SPNs, with an area under the receiver operating characteristic curve (AUC) of 0.94. Zhou et al. [15] examined the ability of 18F-FDG PET/CT radiomics-based ML analysis in differentiating primary from metastatic lung lesions. Results showed that the ML model with the gradient boosting decision tree algorithm with PET-radiomics had the highest classification accuracy, with an AUC of 0.983. Some studies have found similar results [16–19] (Table 1). Thus, 18F-FDG PET/CT radiomics-based ML analysis can have a great potential in characterizing SPNs.
Table 1.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in lung and mediastinal tumors
| Authors | Year | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resulta |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating benign from malignant tumors or primary from metastatic tumors | |||||||||
| Ren et al. [14] | 2022 | SPN | Benign vs. malignant | n = 280 |
Clinical model PET radiomics-based model Combined model |
LASSO regression | Combined model | Training and validation cohorts | AUC: 0.94 |
| Zhou et al. [15] | 2021 | SPN | Primary vs. metastatic | n = 769 |
CT radiomics-based model PET radiomics-based model |
GBDT | PET radiomics-based model | Training and validation cohorts | AUC: 0.983 |
| Salihoğlu et al. [16] | 2022 | SPN | Benign vs. malignant | n = 48 | PET radiomics-based model alone | Deep neural network | – |
Internal validation (cross-validation) |
AUC: 0.81 |
| Zhang et al. [17] | 2019 | SPN | Benign vs. malignant | n = 135 |
CT radiomics-based model PET radiomics-based model Combined model |
SVM | Combined model |
Internal validation (cross-validation) |
AUC:0.887 |
| Yan et al. [18] | 2020 | SPN | Primary vs. metastatic | n = 445 |
CT radiomics-based model PET radiomics-based model Combined model |
SMO | Combined model |
Internal validation (cross-validation) |
AUC: 0.98 |
| Agüloğlu et al. [19] | 2023 | Consolidated lesion | Lung cancer vs. infection | n = 106 | PET radiomics-based model only | LR | – | Training and validation cohorts | AUC: 0.813 |
| Classifying tumors according to histological subtypes | |||||||||
| Zhao et al. [22] | 2022 | NSCLC | ADC vs. SCC | n = 120 |
Clinical model PET radiomics-based model Combined model |
SVM | Combined model | Training and validation cohorts | AUC: 0.876 |
| Han et al. [23] | 2021 | NSCLC | ADC vs. SCC | n = 1419 | PET radiomics-based model only | VGG16 DL | – | Training and validation cohorts | AUC: 0.903 |
| Ren et al. [24] | 2021 | NSCLC | ADC vs. SCC | n = 315 |
Clinical laboratory model CT radiomics-based model PET radiomics-based model Combination of all models |
LASSO regression | Combined model | Training and validation cohorts | AUC: 0.901 |
| Koyasu et al. [25] | 2020 | NSCLC | ADC vs. SCC | n = 188 | Combined CT + PET radiomics-based model alone | XGB | – | Internal validation (cross-validation) | AUC: 0.843 |
| Hyun et al. [26] | 2019 | NSCLC | ADC vs. SCC | n = 396 | Combined clinical + PET radiomics-based model alone | LR | – | Internal validation (cross-validation) | AUC: 0.859 |
| Nakajo et al. [27] | 2022 | TET | Thymic carcinoma vs thymoma | n = 79 | Combined PET radiomics- + CNN-based feature model | LR | – | Internal validation (cross-validation) | AUC: 0.90 |
| Ozkan et al. [28] | 2022 | TET | Low-risk thymoma vs. high-risk thymoma | n = 27 | Combined clinical + PET radiomics-based model alone | LASSO + artificial neural network | – | Training and validation cohorts | AUC: 0.88 |
| Predicting tumor characteristics | |||||||||
| Gao et al. [33] | 2023 | Lung ADC | EGFR status | n = 515 |
Clinical model CT radiomics-based model PET radiomics-based model Combined models |
RF | Combined model | Training and validation cohorts | AUC: 0.730 |
| Chang et al. [34] | 2021 | Lung ADC | ALK status | n = 526 |
CT radiomics-based model PET radiomics-based model Combined PET and CT radiomics-based model Combined clinical, PET, and CT models |
LASSO regression | Combined clinical, PET and CT model | Training and validation cohorts | AUC: 0.88 |
| Shiri et al. [35] | 2020 | NSCLC | EGFR and KRAS status | n = 150 | Combined CT + PET radiomics-based model alone | Stochastic gradient descent | – | Training and validation cohorts |
AUC for EGFR: 0.82 AUC for KRAS: 0.83 |
| Liu et al. [36] | 2020 | Lung ADC | EGFR status | n = 148 | Combined CT + PET radiomics-based model alone | XGB | – | Training and validation cohorts | AUC: 0.870 |
| Agüloğlu et al. [37] | 2022 | NSCLC | EGFR and ALK status | n = 189 | PET radiomics-based model alone | Naïve Bayes algorithm | – | Training and validation cohorts |
AUC for EGFR: 0.797 AUC for ALK: 0.814 |
| Nair et al. [38] | 2021 | NSCLC | EGFR status | n = 50 |
CT radiomics-based model PET radiomics-based model |
LR | PET-radiomics model | Internal validation (cross-validation) | AUC: 0.870 |
| Li. et al. [39] | 2019 | NSCLC | EGFR status | n = 115 |
CT radiomics-based model PET radiomics-based model Combined model |
LASSO regression | Combined model | Internal validation (cross-validation) | AUC: 0.822 |
| Lim et al. [40] | 2022 | NSCLC | PD-L1 expression | n = 312 | Combined model only (CT + PET radiomics feature) | Naïve Bayes algorithm | – | Internal validation (cross-validation) | AUC: 0.712 |
| Mu et al. [41] | 2021 | NSCLC | PD-L1 expression | n = 697 | Combined CT + PET radiomics-based model alone | SRecCNN | – | Training and validation cohorts | AUC: 0.82 |
| Tong et al. [42] | 2022 | NSCLC | CD8 expression | n = 1367 |
CT radiomics-based model PET radiomics-based model Combined PET and CT scan model Combined clinical, PET, and CT scan model |
LR | Combined clinical, PET and CT model | Training and validation cohorts | AUC: 0.932 |
| Predicting tumor stage | |||||||||
| Wang et al. [44] | 2023 | NSCLC | N stage | n = 192 |
Combined clinical, tumor PET, and tumor CT model Combined clinical, lymph node PET, and lymph node CT model Combination of all models |
XGB | Combination of all models | Training and validation cohorts | N2 stage, AUC: 0.94 |
| Laros et al. [45] | 2022 | NSCLC | LNM | n = 148 | Combined tumor and lymph node PET radiomics-based model alone | XGB | – | Training and validation cohorts | Accuracy: 0.88 |
| Onozato et al. [46] | 2023 | Lung cancer | Highly invasive lung cancer | n = 873 |
CT radiomics-based model PET radiomics-based model Combined model |
Ensemble ML algorithm | Combined model | Training and validation cohorts | AUC: 0.880 |
| Predicting treatment response or survival | |||||||||
| Zhao et al. [47] | 2022 | Lung ADC | OS | n = 421 |
Combined clinical + CT radiomics-based + PET radiomics-based model alone |
Ensemble ML algorithm | – | Training and validation cohorts |
3-year OS, AUC: 0.84; 4-year OS, AUC: 0.88 |
| Huang et al. [48] | 2022 | Malignant lung tumor | OS | n = 965 |
Clinical model CT radiomics-based model PET radiomics-based model Combined PET and CT scan model Combined clinical, PET, and CT scan model |
CNN + RSF | Combined clinical, PET, and CT scan models | Training and validation cohorts | C-index: 0.737 |
| Ahn et al. [49] | 2019 | NSCLC | Disease recurrence after surgery | n = 93 | PET radiomics-based model alone | RF | – | Training and validation cohorts | AUC: 0.956 |
| Kirienko et al.[50] | 2021 | NSCLC | Disease recurrence after surgery | n = 151 |
Genomic model Combined PET and CT model Combination of all models |
Logic learning machine | Combination of all models | Internal validation (cross-validation) | AUC: 0.87 |
| Mu et al.[51] | 2020 | NSCLC | PFS in patients treated with EGFR-TKI | n = 616 | Combined CT + PET radiomics-based model alone | SRecCNN | – | Training and validation cohorts | HR: 0.24 |
| Mu et al. [52] | 2020 | NSCLC | PFS and OS in patients treated with ICI | n = 194 | Combined CT radiomics-based + PET radiomics-based + PET/CT scan-based (minimum Kullback–Leibler divergence features) model alone | LASSO + Cox proportional hazard model | – | Training and validation cohorts |
PFS, C-index: 0.77; OS, C-index: 0.80 |
| Bertolini.et al. [53] | 2022 | NSCLC | 2-year PFS in patients treated with RT | n = 117 |
Harmonized CT radiomics-based model Harmonized PET radiomics-based model Combined model |
SVM | Combined model | Training and validation cohorts | AUC: 0.77 |
| Sepehri et al. [54] | 2021 | NSCLC | OS in patients treated with CRT | n = 138 | Combined CT + PET radiomics-based model alone | Ensemble ML algorithm | – | Training and validation cohorts | Accuracy: 0.78 |
| Afshar et al. [55] | 2020 | NSCLC | OS in patients treated with RT | n = 132 |
Combined clinical + CT radiomics-based + PET radiomics-based model alone |
CNN + Cox proportional hazard model | – | Training and validation cohorts | C-index: 0.68 |
| Astaraki et al. [56] | 2019 | NSCLC | OS in patients treated with CRT | n = 30 |
CT radiomics-based model PET radiomics-based model Combined model |
SVM | Combined model | Internal validation (cross-validation) | AUC: 0.95 |
| Park et al. [57] | 2023 | NSCLC | Disease recurrence in patients treated with surgery or RT | n = 77 | Combined clinical + PET radiomics-based model alone | Naïve Bayes algorithm | – | Training and validation cohorts | AUC: 0.816 |
| Pavic et al. [58] | 2020 | MPM | PFS in patients treated with surgery | n = 72 |
CT radiomics-based model PET radiomics-based model |
PCA + cox proportional hazard model | PET radiomics-based model | Training and validation cohorts | C-index: 0.66 |
ADC adenocarcinoma, ALK anaplastic lymphoma kinase, AUC area under the receiver operating characteristic curve, C-index concordance index, CNN convolutional neural network, CRT chemoradiotherapy, DL deep learning, EGFR epidermal growth factor receptor, GBDT gradient boosting decision tree, HR hazard ratio, ICI immune checkpoint inhibitor, KRAS kirsten rat sarcoma viral oncogene, LASSO least absolute shrinkage and selection operator algorithm, LNM lymph node metastasis, LR logistic regression, ML machine learning, MPM malignant pleural mesothelioma, NSCLC non-small cell lung cancer, OS overall survival, PCA principal component analysis, PD-L1 programmed death ligand, PFS progression-free survival, RF random forest, RSF random survival forests, RT radiotherapy, SCC squamous cell carcinoma, SMO sequential minimal optimization, SPN solitary pulmonary nodule, SRecCNN small-residual-convolutional-network, SVM support vector machine, TET thymic epithelial tumor, TKI tyrosine kinase inhibitor, XGB gradient tree boosting
aPerformance only presents the result of the best machine learning model
Classification according to histological types
Due to the different histologic and biological characteristics of lung adenocarcinoma (ADC) and lung squamous cell carcinoma (SCC), their treatment regimen, prognosis, and relapse rate significantly vary [20, 21]. Thus, it is important to distinguish these two subtypes of non-small cell lung cancer (NSCLC) before treatment for appropriate clinical decision-making.
18F-FDG PET/CT radiomics-based ML analysis might improve the classification of ADC and SCC [22–26]. Zhao et al. [22] established combined ML models based on clinical characteristics (sex and smoking status), laboratory findings (carcinoembryonic antigen and squamous cell carcinoma antigen levels), and PET-radiomics to classify ADC and SCC. The support vector machine (SVM) algorithm accurately distinguished ADC from SCC, with an AUC of 0.876. This algorithm had a significantly better prediction performance than the clinical model (AUC:0.712, p = 0.037). Han et al. [23] examined the usefulness of PET radiomics-based ML/DL algorithms for obtaining differential diagnosis in patients with ADC and SCC. They reported that ML analyses with either the linear discriminant analysis (AUC: 0.863) or the SVM (AUC: 0.863) algorithm had optimal performance. Moreover, the VGG16 DL algorithm (AUC: 0.903) outperformed all conventional ML algorithms. Similar studies have successfully differentiated ADC from SCC [24–26] (Table 1).
18F-FDG PET/CT radiomics-based ML analysis can characterize histological subtypes in thymic epithelial tumors (TETs) [27, 28]. The ML model trained using 18F-FDG PET radiomics and DL-based features with the logistic regression (LR) algorithm was proposed for predicting the histological subtypes of TETs [27]. This model can accurately differentiate thymic cancer from thymoma, with an AUC of 0.90.
Prediction of tumor characteristics
Recently, the treatment options for NSCLC significantly improved with advancements in targeted therapies against mutated genes such as epidermal growth factor receptor (EGFR), kirsten rat sarcoma viral oncogene (KRAS), and anaplastic lymphoma kinase (ALK) [29, 30]. Moreover, immune checkpoint inhibitors targeting programmed cell death protein 1 (PD-1) or programmed death ligand 1 (PD-L1) are associated with better survival outcomes compared with conventional chemotherapy in patients with advanced-stage NSCLC [31, 32]. Thus, in patients with NSCLC, gene mutations or the immune checkpoint status of tumors should be identified to determine the appropriate treatment strategy.
Several reports have examined the usefulness of 18F-FDG PET/CT radiomics-based ML analysis for predicting gene mutation. Previous studies commonly showed that 18F-FDG PET/CT radiomics-based ML analysis had a promising performance for predicting gene mutation [33–39] (Table 1). Gao et al. [33] constructed radiomics-based models based on 18F-FDG PET/CT features using ML to predict EGFR mutation status in patients with lung ADC. Results showed that the ML model with the random forest (RF) algorithm using combined clinical data, CT-radiomics and PET-radiomics had the highest performance, with an AUC of 0.730. Chang et al. [34] revealed that the combined clinical data and PET/CT-based ML model with the LASSO regression algorithm is significantly advantageous in predicting ALK mutation status in patients with lung ADC compared with the clinical model (AUC:0.88 vs. 0.74, p < 0.001). Shiri et al. [35] reported that the ML model with the stochastic gradient descent algorithm using CT-radiomics and PET-radiomics outperformed conventional methods (peak of standardized uptake value [SUVpeak] or metabolic tumor volume [MTV]) in predicting EGFR and KRAS gene mutation status in NSCLC (EGFR: SUVpeak [AUC: 0.69] vs. ML model [AUC: 0.82]; KRAS: MTV [AUC: 0.55] vs. ML model [AUC: 0.83]). Previous studies have shown that the 18F-FDG PET/CT radiomics-based ML model have a similar performance, with AUCs of 0.797–0.870 [36–39].
Several studies have assessed the predictive ability of 18F-FDG PET/CT radiomics-based ML analysis for immune checkpoint status in NSCLC [40–42]. Lim et al. [40] predicted the PD-L1 expression level in patients with NCSLC using the 18F-FDG PET/CT radiomics-based ML model. Results showed that the ML model with the Naïve Bayes algorithm using the top five features (CT_gray-level run length matrix [GLRLM]_long run high grey-level emphasis, CT_grey-level co-occurrence matrix [GLCM]_homogeneity, CT_mean Hounsfield unit, CT_GLRLM_long run emphasis, and PET_SUVmax) had the best predictive performance (AUC: 0.712). Mu et al. [41] developed a 18F-FDG PET/CT-based DL model to evaluate PD-L1 status. Results showed that the deep learning score (DLS) could significantly distinguish PD-L1-positive from PD-L1-negative patients (AUC: 0.82).
Predicting tumor stage
The clinical outcome of NSCLC is directly related to its stage at diagnosis [43]. Moreover, there were reports showing the usefulness of the 18F-FDG PET/CT radiomics-based ML method for predicting tumor stage in lung cancer [44–46]. Wang et al. [44] reported that the ML model with the gradient tree boosting (XGB) ML algorithm using combined clinical data and PET/CT radiomics of the primary tumor and lymph node had the highest diagnostic performance in predicting lymph node metastasis (LNM) in NSCLC (AUC: 0.93). Moreover, this model had a great potential in predicting N2 stage NSCLC (AUC: 0.94). In addition, Laros et al. [45] reported that the combined PET-radiomics of the primary tumor and lymph node had good performance in predicting LNM from NSCLC, with an accuracy of 0.88.
Predicting treatment response or survival
Previous studies have examined the potential of ML analysis using pretreatment 18F-FDG PET/CT radiomic features for predicting patient response and survival in malignant lung tumors [47–57] (Table 1).
Zhao et al. [47] examined the ability of ML models trained using clinical data and 18F-FDG PET/CT radiomics for predicting overall survival (OS) in patients with lung ADC who underwent surgery and received radiotherapy (RT), chemotherapy, or immunotherapy. The ensemble ML models, which were constructed with clinical data and 18F-FDG PET/CT radiomic features, could predict the 3- and 4-year OS, with an AUC of 0.84 and 0.88, respectively. Huang et al. [48] showed that the convolutional neural networks (CNNs) trained by 18F-FDG PET/CT had good performance in predicting OS in patients with malignant lung tumor who received RT, chemotherapy, or immunotherapy. To predict OS, the CNNs trained using clinical data and 18F-FDG PET/CT radiomics with the random survival forest (RSF) ML model (concordance index [C-index]: 0.737) had a similar performance to CT alone (C-index: 0.730). However, it had a better performance than PET (C-index: 0.595) and clinical models (C-index: 0.595) alone.
Previous studies have assessed the ability of 18F-FDG PET/CT radiomics-based ML models for predicting outcomes in not only patients with surgically treated NSCLC [49, 50] but also those with nonsurgically treated NSCLC [51–56]. Ahn et al. [49] used the 18F-FDG PET/CT radiomics-based ML approach to predict disease recurrence in patients with NSCLC who underwent surgery. Results showed that the ML model with the RF algorithm had good performance for predicting recurrence, with an AUC of 0.956. Mu et al. [51] established the 18F-FDG PET-based DLSs, which is useful for predicting EGFR mutation status (EGFR-DLS) (AUC: 0.81). EGFR-DLS was significantly and positively associated with a longer progression-free survival (PFS) in patients treated with EGFR-tyrosine kinase inhibitors (hazard ratio [HR]:0.24, p < 0.001). Mu et al. [52] reported that the 18F-FDG PET/CT radiomics-based ML model had a good AUC for predicting response to immune checkpoint inhibitors (0.81). Moreover, the constructed nomogram models (C-indices of 0.77 and 0.80 for predicting OS and PFS, respectively) had good performance in predicting prognosis. Similar studies have successfully predicted treatment responses or survival in patients with NSCLC [50, 53–57] (Table 1).
The 18F-FDG PET/CT radiomics-based ML analysis has been applied to predict PFS in malignant pleural mesothelioma [58]. This study showed the prognostic potential of the cox regression ML model established using specific PET radiomics-based on the principal component analysis for PFS with a C-index of 0.66.
Summary
Previous studies commonly showed that 18F-FDG PET radiomics-based ML analysis had a high predictive performance for differentiating benign from malignant tumors, predicting tumor characteristics, staging tumors, and assessing treatment outcome or prognosis in lung or mediastinal tumors, with AUCs, accuracies, or C-indices of > 0.70. Thus, the 18F-FDG PET radiomics-based ML analysis might play important roles in supporting clinicians in diagnostic and patient management including precision medicine for lung or mediastinal tumors. However, as shown in Table 1, previous studies have reported several ML processes including ML algorithms, and different ML models have been applied for the same purpose.
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in head and neck tumors
Differentiating benign and malignant tumors and predicting tumor characteristics
In head and neck tumors, 18F-FDG PET/CT radiomics-based ML analyses have been applied to differentiate benign from malignant tumors or to predict tumor characteristics. The following articles have reported about differentiating benign from malignant tumors.
In thyroid incidentalomas, distinguishing benign from malignant tumors based on SUVmax on 18F-FDG PET/CT is challenging due to a significant overlap between these lesions [59]. Aksu et al. [60] reported that the ML model with the RF algorithm had a better performance in differentiating benign from malignant thyroid incidentalomas based on SUVmax (AUC: 0.849 vs. 0.758).
The assessment of human papillomavirus (HPV) status plays an important role in treatment planning for oropharyngeal cancer [61]. Haider et al. [62] showed that the AUC of combined tumor and lymph node PET/CT radiomics-based ML model with the XGB algorithm for predicting HPV status in oropharyngeal cancer was 0.83.
Predicting treatment response or survival
Previous studies have reported the predictive ability of 18F-FDG PET/CT radiomics-based ML analysis for treatment outcomes in head and neck cancers [63–71] (Table 2). Haider et al. [63] showed that the ML model with the RSF algorithm using clinical and pretreatment 18F-FDG PET/CT radiomics had good predictive performance for locoregional progression in patients with HPV-associated oropharyngeal cancer who received RT (C-index: 0.76). In hypopharyngeal cancers, the ML model with the LR algorithm constructed based on UICC stage, T and N stage, and pretreatment 18F-FDG PET-radiomics with GLCM_entropy and GLRLM_ run length non-uniformity (RLNU) is a significant predictor of PFS (HR:3.22, p = 0.045) [64].
Table 2.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in head and neck tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating benign from malignant tumors | |||||||||
| Aksu et al. [60] | 2020 | Thyroid incidentaloma | Benign vs. malignant | n = 60 | PET radiomics only | RF | – | Training and validation cohorts | AUC: 0.849 |
| Predicting tumor characteristics | |||||||||
| Haider et al. [62] | 2020 | OPC | HPV status | n = 435 |
Tumor PET/CT Lymph node PET/CT Tumor and lymph node PET/CT |
XGB | Tumor and lymph node PET/CT | Training and validation cohorts | AUC: 0.83 |
| Predicting treatment response or survival | |||||||||
| Haider et al. [63] | 2021 | OPC | Locoregional recurrence after RT | n = 190 |
Clinical model CT radiomics-based model PET radiomics-based model Combined PET and CT model Combined clinical, PET, and CT model |
RSF | Combined model | Internal validation (cross-validation) | C-index: 0.76 |
| Nakajo et al. [64] | 2023 | HPC | PFS after RT, CRT, or surgery | n = 100 | Combined clinical + PET radiomics-based model alone | LR | – | Training and validation cohorts | HR: 3.22 |
| Lafata. et al. [65] | 2021 | OPC | Recurrence-free survival after RT | n = 64 | Intra-treatment PET radiomics-based model | Unsupervised data clustering algorithm | – | Internal validation | HR: 2.69 |
| Spielvogel et al. [66] | 2023 | HNSCC | 3-year OS | n = 127 | Combined genomic + CT radiomics-based + PET radiomics-based model alone | Ensemble ML algorithm | – | Internal validation (cross-validation) | AUC: 0.75 |
| Haider et al. [67] | 2020 | OPC | OS after RT, CRT, or surgery | n = 306 |
Clinical model CT radiomics-based model PET radiomics-based model Combined PET and CT model Combined clinical, PET, and CT model |
RSF | Combined model | Training and validation cohorts |
5-year OS, HPV-associated oropharyngeal cancer (p = 0.02); 5-year OS, HPV-negative oropharyngeal cancer (p = 0.01) |
| Zhong et al. [68] | 2021 | HPC and LC | Disease progression at 1 year after chemotherapy or RT | n = 72 |
CT radiomics-based model PET radiomics-based model Combined model |
RF | Combined model | Training and validation cohorts | AUC: 0.94 |
| Du et al. [69] | 2019 | NPC | Local recurrence after chemotherapy or RT | n = 76 | PET radiomics-based model alone | RF | – | Internal validation (cross-validation) | AUC: 0.892 |
| Peng et al. [70] | 2019 | NPC | 5-year DFS after chemotherapy or CRT | n = 707 | Combined PET radiomics-based + CNN-based model alone | LASSO regression | – | Training and validation cohorts | C-index: 0.722 |
| Liu et al. [71] | 2020 | HNSCC | OS after RT | n = 171 | PET radiomics-based model alone | LASSO regression | – | Internal validation (cross-validation) | C-index: 0.77 |
aPerformance only presents the result of the best machine learning model
AUC area under the receiver operating characteristic curve, C-index concordance index, CNN convolutional neural network, CRT chemoradiotherapy, DFS disease-free survival, HNSCC head and neck squamous cell carcinoma, HPC hypopharyngeal cancer, HPV human papillomavirus, HR hazard ratio, LASSO least absolute shrinkage and selection operator algorithm, LC laryngeal cancer, LR logistic regression, ML machine learning, NPC nasopharyngeal cancer, OPC oropharyngeal cancer, OS overall survival, PFS progression-free survival, RF random forest, RSF random survival forest, RT radiotherapy, XGB gradient tree boosting
Previous studies have reported the usefulness of intra-treatment 18F-FDG PET/CT radiomics-based ML analysis for outcome prediction in head and neck cancers. Lafata et al. [65] showed that the unsupervised clustering of intra-treatment 18F-FDG PET/CT radiomics, which were obtained 2 weeks after RT (at a dose of 20 Gy), was significantly associated with recurrence-free survival (HR:2.69, p = 0.04) in patients with oropharyngeal cancer who received definitive RT. Moreover, a previous study assessed the ability of ML analysis using the combined 18F-FDG PET radiomics and genomic data for predicting 3-year OS in head and neck cancers (AUC: 0.75) [66]. Similar studies have successfully predicted prognosis in head and neck cancer [67–71] (Table 2).
Summary
Previous studies revealed that 18F-FDG PET/CT radiomics-based ML analysis had good predictive performances for predicting treatment outcome or prognosis, with AUCs or C-indices of > 0.70, in head and neck tumors. Thus, 18F-FDG PET/CT radiomics-based ML analysis might be expected to be an important tool for patient management in head and neck tumors. However, several ML processing approaches have also been discussed (Table 2).
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in lymphatic tumors
Differentiating benign from malignant tumors and primary from metastatic tumors or classifying tumors according to histological types
The conventional semi-quantitative 18F-FDG PET parameters such as SUVmax, MTV, and total lesion glycolysis (TLG) are useful biomarkers for characterizing malignant lymphoma [72, 73]. However, the ability of these parameters in identifying tumor heterogeneity, which ultimately contributes to tumor aggressiveness and poor prognosis, remains limited [74]. Recently, 18F-FDG PET/CT radiomics-based ML analysis has been applied to overcome these issues [75]. Previous studies have revealed that 18F-FDG PET/CT radiomics-based ML analysis is useful in not only classifying tumors based on histological subtypes but also differentiating malignant lymphoma from other diseases [76–80].
Abenavoli et al. [76] showed that the ML model with the RF algorithm using PET-radiomics had a better performance in differentiating diffuse large B-cell lymphoma (DLBCL) from Hodgkin’s lymphoma (HD) based on SUVmax (AUC: 0.87 vs. 0.78). de Jesus et al. [77] reported that the ML model with the gradient boosting algorithm using PET/CT radiomics had a significantly higher AUC in distinguishing DLBCL and follicular lymphoma according to SUVmax (AUC:0.86 vs. 0.79, p < 0.01). Lovinfosse et al. [78] also showed that the ML model with the RF algorithm using clinical data and PET-radiomics had good performance in differentiating DLBCL from HD, with an AUC of 0.95. Further, the authors showed that the constructed ML model with the RF algorithm had good performance in differentiating malignant lymphoma and sarcoidosis, with an AUC of 0.94. Yang et al. [79] revealed that the ML model with the SVM algorithm constructed according to combined CNN-based features and PET-radiomics had a great potential in distinguishing malignant lymphoma from enlarged metastatic cervical lymph nodes (AUC: 0.948).
Predicting treatment response or survival
For the treatment assessment of malignant lymphoma, the visual assessment of the Deauville score (DC) has been a useful 18F-FDG PET/CT criterion: DC1–DC3, complete metabolic response; DC4 and DC5, incomplete metabolic response [81–83]. However, there might be difficulties in predicting treatment outcomes based on DC alone because of the inter- or intra-variability of DC definition. Thus, 18F-FDG PET/CT radiomics-based ML analysis can be a novel approach for predicting treatment outcomes in malignant lymphoma.
Frood et al. [84] examined the ability of pretreatment 18F-FDG PET/CT radiomics-based ML analysis for predicting recurrence after DLBCL treatment. Results showed that the ML model with the ridge regression algorithm using combined clinical and PET-radiomics had good performance, with an AUC of 0.73. Cui et al. [85] assessed the potential of the 18F-FDG PET/CT radiomics-based ML approach for identifying patients with DLBCL who are at high risk for progression or relapse after receiving first-line therapy. Results showed that the ML model with the RF algorithm using clinical data, baseline, end-of-treatment and delta PET-radiomics features was a significant predictor of PFS (C-index: 0.853). By contrast, 18F-FDG PET/CT radiomics-based ML analysis was found to be useful for predicting recurrence after HD treatment [86, 87]. Frood et al. [86] showed that the ML model with the ridge regression algorithm using combined clinical data and PET-radiomics had good predictive performance, with an AUC of 0.81. Similar studies have successfully predicted treatment responses or survival in malignant lymphoma [87–91] (Table 3).
Table 3.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in lymphatic tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating benign from malignant tumors and primary from metastatic tumors or classifying tumors according to pathological subtypes | |||||||||
| Abenavoli et al. [76] | 2023 | Malignant lymphoma | DLBCL vs. HD | n = 117 | PET radiomics-based model alone | RF | – | Training and validation cohorts | AUC: 0.87 |
| de Jesus et al. [77] | 2022 | Malignant lymphoma | DLBCL vs. FL | n = 120 | Combined CT + PET radiomics-based model alone | Gradient boosting | – | Training and validation cohorts | AUC: 0.86 |
| Lovinfosse et al. [78] | 2022 | Malignant lymphoma |
1. Malignant lymphoma vs. sarcoidosis 2. DLBCL vs. HD |
n = 420 | Combined clinical + PET radiomics-based model alone | RF | – | Training and validation cohorts |
1. AUC: 0.94 2. AUC: 0.95 |
| Yang et al. [79] | 2023 | Cervical lymph node | Malignant lymphoma vs. metastasis | n = 165 |
CNN model Combined PET radiomics-based + CNN-based model alone |
SVM | Combined model | Training and validation cohorts | AUC: 0.948 |
| Cui et al. [80] | 2023 | Brain tumor | Malignant lymphoma vs. metastasis | n = 51 | PET radiomics-based model alone | RF | – | Training and validation cohorts | AUC: 0.93 |
| Predicting treatment response or survival | |||||||||
| Frood et al. [84] | 2022 | DLBCL | Recurrence after chemotherapy | n = 229 | Combined clinical + PET radiomics-based model alone | Ridge regression | – | Training and validation cohorts | AUC: 0.73 |
| Cui et al. [85] | 2022 | DLBCL | PFS after chemotherapy | n = 271 |
Clinical model PET radiomics-based model Combined clinical + PET radiomics-based model alone |
RF + cox proportional hazard | Combined model | Training and validation cohorts | C-index: 0.853 |
| Frood et al. [86] | 2022 | HD | Recurrence after chemotherapy or RT | n = 289 | Combined clinical + PET radiomics-based model alone | Ridge regression | – | Training and validation cohorts | AUC: 0.81 |
| Ritter et al. [87] | 2022 | DLBCL | Recurrence after chemotherapy | n = 85 | PET radiomics-based model alone | Ensemble ML algorithm | – | Training and validation cohorts | AUC: 0.85 |
| Jiang et al. [88] | 2022 | DLBCL | OS and PFS after chemotherapy | n = 383 |
Clinical model PET radiomics-based model Combined clinical + PET radiomics-based model alone |
Ensemble ML algorithm | Combined model | Training and validation cohorts |
PFS, C-index: 0.758, OS, C-index: 0.794, |
| Jiang et al. [89] | 2022 | GI DLBCL | OS and PFS after chemotherapy | n = 140 |
Clinical model Combined clinical + PET radiomics-based model alone |
SVM + cox proportional hazard | Combined model | Training and validation cohorts |
PFS, C-index: 0.831 OS, C-index: 0.877 |
| Coskun et al. [90] | 2021 | DLBCL | Incomplete response after chemotherapy | n = 45 | PET radiomics-based model alone | LR | – | Internal validation | AUC: 0.81 |
| Milgrom et al. [91] | 2019 | HD | Recurrence after chemotherapy | n = 251 | PET radiomics-based model alone | SVM with AdaBoost | – | Internal validation | AUC: 0.952 |
AUC area under the receiver operating characteristic curve, C-index concordance index, CNN convolutional neural network, DLBCL diffuse large B-cell lymphoma disease-free survival, FL follicular lymphoma, GI gastrointestinal, HD Hodgkin’s lymphoma, LR logistic regression, ML machine learning, OS overall survival, PFS progression-free survival, RF random forest, RT radiotherapy, SVM support vector machine
aPerformance only presents the result of the best machine learning model
Summary
Previous studies have shown that 18F-FDG PET/CT radiomics-based ML analysis is useful in not only differentiating but also predicting treatment outcome or prognosis in patients with malignant lymphomas. Each best ML model had good predictive performance, with AUCs or C-indices of > 0.70 (Table 3). Thus, it might be expected to promote the translation of 18F-FDG PET/CT radiomics-based ML analysis into clinical practice in the field of lymphatic tumors. However, the articles included in this review showed heterogeneity among various ML approaches.
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in breast tumors
Differentiating benign from malignant tumors and predicting tumor characteristics or stage
Several studies have examined the clinical potential of 18F-FDG PET/CT radiomics-based ML analyses in differentiating benign from malignant tumors and predicting tumor characteristics or stage in breast cancer [92–96].
Eifer et al. [92] showed that ML analyses with the k-nearest neighbors (kNN) algorithm using CT-radiomics and PET-radiomics had good performance in differentiating LNM from breast cancer from post-COVID-19 vaccine-associated axillary lymphadenopathy, with an AUC of 0.98.
An accurate assessment of both hormone receptor status and human EGFR 2 (HER2) status is important for treatment planning in breast cancer [97, 98]. Moreover, an accurate pretreatment assessment of axillary lymph node is essential in managing breast cancer [99]. Chen et al. [93] showed that the constructed ML model with the XGB algorithm based on PET/CTmean radiomics had good predictive ability for HER2 status in breast cancer (AUC: 0.76). In addition, Song [94] reported that the constructed ML model with the XGB algorithm based on PET/CT radiomics had good performance for predicting axillary LNM in patients with breast cancer (AUC: 0.890). A similar study has successfully predicted hormone status in breast cancer [95] (Table 4).
Table 4.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in breast tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating benign from malignant tumors and predicting tumor characteristics or stage | |||||||||
| Eifer et al. [92] | 2022 | Axillary LN | COVID-19 vaccine-associated lymphadenopathy vs. metastasis | n = 99 |
CT radiomics-based model PET radiomics-based model Combined model |
kNN | Combined model | Training and validation cohorts | AUC: 0.98 |
| Chen et al. [93] | 2022 | Breast cancer | HER2 status | n = 217 |
CT radiomics-based model PET radiomics-based model PET/CTconcat radiomics-based model PET/CTmean radiomics-based model |
XGB | PET/CTmean radiomics model | Training and validation cohorts | AUC: 0.760 |
| Song [94] | 2021 | Breast cancer | LNM | n = 100 | PET radiomics-based model alone | XGB | – | Training and validation cohorts | AUC: 0890 |
| Krajnc et al. [95] | 2021 | Breast cancer | Triple negative hormone status | n = 170 | Combined clinical + CT radiomics-based + PET radiomics-based model alone | Ensemble ML algorithm | – |
Internal validation (cross-validation) |
AUC: 0.82 |
| Ou et al. [96] | 2020 | Breast tumor | Breast cancer vs. malignant lymphoma | n = 44 |
SUV model CT radiomics-based model PET radiomics-based model Combined clinical + PET radiomics-based model Combined clinical + CT radiomics-based model |
LASSO + LDA | Combined clinical and PET radiomics model | Training and validation cohorts | AUC: 0.806 |
| Predicting treatment response or survival | |||||||||
| Li et al. [100] | 2020 | Breast cancer | pCR after NAC | n = 100 |
CT radiomics-based model PET radiomics-based model Combined age + CT radiomics-based + PET radiomics-based model |
RF | Combined model | Training and validation cohorts | Accuracy: 0.80 |
| Gómez et al. [101] | 2022 | Metastatic breast cancer | Metabolic response after treatment | n = 48 | Combined clinical + CT radiomics-based + PET radiomics-based model alone | LASSO + SVM | – | Training and validation cohorts | AUC: 0.82 |
AUC area under the receiver operating characteristic curve, HER2 human epidermal growth factor receptor, kNN k-nearest neighbors, LASSO least absolute shrinkage and selection operator algorithm, LDA linear discriminant analysis, LN lymph node, LNM lymph node metastasis, ML machine learning, NAC neoadjuvant chemotherapy, pCR pathological complete response, RF random forest, SVM support vector machine, XGB gradient tree boosting
aPerformance only presents the result of the best machine learning model
Predicting treatment response or survival
Two studies have examined the ability of 18F-FDG PET/CT radiomics-based ML analysis for predicting treatment outcome in breast cancer [100, 101]. Li et al. [100] assessed the usefulness of 18F-FDG PET/CT radiomics-based ML analysis for predicting pathological complete response (pCR) to neoadjuvant chemotherapy (NAC) in breast cancer. Results showed that the diagnostic accuracy of the ML model with the RF algorithm constructed based on patient age and PET/CT radiomics increased compared with that of the ML model with the RF algorithm constructed according to PET/CT radiomics only (0.800 vs. 0.767). The authors hypothesized that the finding can be attributed to the fact that younger patients had a higher pCR rate than older ones. Gómez et al. [101] assessed the predictive ability of 18F-FDG PET/CT radiomics-based ML analysis for metabolic response after metastatic breast cancer treatment. Results showed that the ML model with the LASSO + SVM algorithm using combined clinical data and PET-radiomics had good performance, with an AUC of 0.82.
Summary
In breast tumors, each best ML model had good predictive performance for differentiating benign from malignant tumors and for predicting tumor characteristics and stage and treatment outcome, with AUCs or accuracies of > 0.70 (Table 4). The heterogeneity of ML approaches was also noted in the reported studies.
Although there have been several studies that have explored the usefulness of 18F-FDG PET/CT radiomics-based ML analysis associated with breast tumors, it might be expected in the 18F-FDG PET/CT radiomics-based ML analysis to be a novel tool to patient management for breast tumors.
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in abdominal tumors
Differentiating benign from malignant tumors and predicting tumor characteristics or stage
In abdominal tumors, the usefulness of 18F-FDG PET/CT radiomics-based ML analyses in differentiating benign and malignant tumors and predicting tumor characteristics or stage has been evaluated [102–108] (Table 5).
Table 5.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in abdominal tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating benign from malignant tumors | |||||||||
| Zhang et al. [102] | 2019 | Pancreatic tumor | AIP vs. PDAC | n = 251 |
CT radiomics-based model PET radiomics-based model Combined model |
SVM | Combined model | Internal validation (cross-validation) | Accuracy: 0.850 |
| Wei et al. [103] | 2023 | Pancreatic tumor | AIP vs. PDAC | n = 112 |
CT radiomics-based + PET radiomics-based model DL feature-based model Multidomain fusion model (radiomics + DL features) |
VGG11 DL algorithm | Multidomain fusion model | Internal validation (cross-validation) | Accuracy: 0.901 |
| Predicting tumor characteristics or stage | |||||||||
| Xing et al. [104] | 2021 | PDAC | Pathological grade | n = 149 |
CT radiomics-based model PET radiomics-based model Combined model |
XGB | Combined model | Training and validation cohorts | AUC: 0.921 |
| Jiang et al. [105] | 2022 | HCC or ICC | MVI | HCC: n = 76; ICC: n = 51 |
Clinical model CT radiomics-based model PET radiomics-based model Combined optimal PET and CT radiomics-based model Combined best clinical, PET radiomics-based, or CT radiomics-based model |
RF | Combined best clinical and PET feature-based model | Training and validation cohorts |
AUC for HCC: 0.88 AUC for ICC: 0.90 |
| Liu et al. [106] | 2021 | Gastric cancer | LNM | n = 185 |
CT radiomics-based model PET radiomics-based model Combined model |
Adaboost | Combined model | Training and validation cohorts | Accuracy: 0.852 |
| He et al. [107] | 2021 | Colorectal cancer | LNM | n = 199 | Combined CT + PET radiomics-based model | XGB | – | Training and validation cohorts | Accuracy: 0.7636 |
| Li et al. [108] | 2021 | Colorectal cancer | MSI | n = 173 | Combined clinical + CT radiomics-based + PET radiomics-based model alone | Adaboost | – | Training and validation cohorts | AUC: 0.828 |
| Predicting treatment response or survival | |||||||||
| Toyama et al. [109] | 2020 | Pancreatic cancer | 1-year survival after RT, CRT, or surgery | n = 161 | PET radiomics-based model alone | RF | – |
Internal validation (cross-validation) |
HR for GLZLM_GLNU: 2.0 |
| Liu et al. [110] | 2023 | Gastric cancer |
HER2 status Progression after surgery |
n = 90 |
Combined clinical + CT radiomics-based + PET radiomics-based model |
Adaboost | – | Training and validation cohorts |
Accuracy for HER2: 0.833 Accuracy for progression: 0.778 |
| Lv et al. [111] | 2022 | Colorectal cancer | Recurrence-free survival after surgery | n = 196 |
Clinical model CT radiomics-based model PET radiomics-based model Combined model |
RSF | Combined model | Training and validation cohorts |
C-index for all patients: 0.780 C-index for patients with stage III disease: 0.820 |
| Shen et al. [112] | 2020 | Rectal cancer | pCR after NCRT | n = 169 | PET radiomics-based model alone | RF | – | Internal validation | Accuracy: 0.953 |
| Agüloğlu et al. [113] | 2023 | Metastatic rectal cancer | 2-year OS | n = 62 | PET radiomics-based model alone | RF | – |
Internal validation (cross-validation) |
AUC: 0.843 |
AIP autoimmune pancreatitis, AUC area under the receiver operating characteristic curve, C-index concordance index, CRT chemoradiotherapy, DL deep learning, GLNU gray-level non-uniformity, GLZLM gray-level zone length matrix, HCC hepatocellular carcinoma, HER2 human epidermal growth factor receptor, HR hazard ratio, ICC intrahepatic cholangiocarcinoma, LNM lymph node metastasis, ML machine learning, MSI microsatellite instability, MVI microvascular invasion, NCRT neoadjuvant chemoradiotherapy, OS overall survival, pCR pathological complete response, PDAC pancreatic ductal adenocarcinoma, RF random forest, RSF random survival forest, RT radiotherapy, SVM support vector machine, XGB gradient tree boosting
aPerformance only presents the result of the best machine learning model
In pancreatic tumors, the ML model with the SVM algorithm using CT-radiomics and PET-radiomics has been a useful tool for differentiating autoimmune pancreatitis (AIP) and pancreatic ductal adenocarcinoma (PDAC), with an accuracy of 0.850 [102]. Moreover, this group established the multidomain fusion DL model using CT-radiomics, PET-radiomics, and DL features for differentiating AIP from PDAC [103]. Results showed that the accuracy of this DL model improved (0.901) compared with that of the formerly published ML model [102]. Xing et al. [104] assessed the ability of 18F-FDG PET/CT radiomics-based ML analysis for predicting the pathological grade of PDAC. Results showed that the ML model with the XGB algorithm using the combined CT-radiomics and PET-radiomics (AUC: 0.921) was better in predicting the pathological grade of PDAC than the CT-radiomics alone (AUC: 0.817) or the PET radiomics-based model alone (AUC: 0.771).
In liver tumors, Jiang et al. [105] assessed the usefulness of 18F-FDG PET radiomics-based ML analysis for predicting microvascular invasion (MVI) in hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC). Results showed that the constructed ML model with the RF algorithm using PET-radiomics and clinical features (cancer antigen 19–9 level or tumor stage) was useful for predicting MVI in either HCC (AUC: 0.88) or ICC (AUC: 0.90) [105].
Liu et al. [106] constructed a useful ML model with the Adaboost algorithm using CT-radiomics and PET-radiomics for predicting LNM in gastric cancer with an accuracy of 0.852. This model detected some metastatic lymph nodes that were missed on contrast-enhanced CT scan (19.6%). Thus, the constructed ML model might offer a potentially useful adjunct to the current staging approaches for gastric cancer. He et al. [107] showed that the ML model with the XGB algorithm using CT-radiomics and PET-radiomics was successful in classifying regional LNM from colorectal cancer, with an accuracy of 0.7636. This ML model was better in predicting LNM than lymph node status, as described in clinical 18F-FDG PET/CT scan reports (accuracy: 0.7091). Li et al. [108] reported that 18F-FDG PET/CT radiomics-based ML analysis was useful for predicting the microsatellite instability (MSI) status, which is an essential prognostic factor of colorectal cancer. Results showed that the constructed ML model with the Adaboost algorithm using two selected radiomic features (PET-Skewness and CT-RoomMeanSquared) had good predictive performance for MSI, with an AUC of 0.828.
Predicting treatment response or survival
Several reports examined the usefulness of 18F-FDG PET/CT radiomics-based ML analyses for predicting treatment outcome in abdominal tumors [109–113]. These studies showed that the 18F-FDG PET/CT radiomics-based ML analyses were the power tools for predicting treatment response or prognosis.
Toyama et al. [109] revealed that PET-radiomics with gray-level zone length matrix (GLZLM)_gray-level non-uniformity (GLNU) was the most important feature on the ML model with the RF algorithm for predicting 1-year survival in pancreatic cancer, and multivariate analysis with Cox hazard regression revealed GLZLM_GLNU as the only statistically significant PET-radiomics for predicting 1-year survival (HR:2.0, p = 0.0094). Liu et al. [110] constructed the ML model with the Adaboost algorithm using clinical data, CT-radiomics and PET-radiomics for predicting HER2 expression status or disease progression in gastric cancer. The predictive accuracies of constructed ML model for HER2 expression status and disease progression were 83.3% and 77.8%, respectively. Lv et al. [111] developed the ML mode with the RSF algorithm using clinical data, CT-radiomics and PET-radiomics to predict recurrence-free survival in patients with colorectal cancer who received surgery, and revealed that the constructed ML model had good performance in predicting the prognosis (C-index for all patients, 0.780; C-index for stage III patients, 0.820). Shen et al. [112] constructed the ML model with the RF algorithm using PET-radiomics for predicting pCR after neoadjuvant chemoradiotherapy (CRT) in rectal cancer, and this ML model showed high predictive performance with an accuracy of 0.953. Moreover, the ability of ML model with the RF algorithm using PET-radiomics for predicting 2-year OS has also been reported in metastatic rectal cancer (2-year OS; AUC:0.843) [113].
Summary
In abdominal tumors, each best 18F-FDG PET radiomics-based ML model had good predictive performance for differentiating benign and malignant tumors, predicting tumor characteristics, staging tumors, or assessing treatment outcome with AUCs, accuracies, or C-indices of > 0.70 (Table 5). The application of 18F-FDG PET radiomics-based ML analyses might be especially expected in the field of gastrointestinal cancers.
Clinical application of 18F-FDG PET/CT radiomics ML analyses in gynecological tumors
Predicting tumor stage
The expression of some protein molecules such as cyclooxygenase-2 (COX-2) is associated with LNM and lymphovascular space invasion (LVSI) in cervical cancer [114, 115]. Tumor budding (TB) is defined as a single neoplastic cell or cell cluster of up to four neoplastic cells at the invasive front of the tumor or within the tumor mass (intratumoral budding) [116]. Moreover, TB is associated with LNM, LVSI, and prognosis in cervical cancer [117]. Some investigators applied the 18F-FDG PET/CT radiomics-based ML models for predicting not only LNM or LVSI but also the expression of COX-2 or TB status in cervical cancer [118–121] (Table 6).
Table 6.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in gynecological tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Predicting tumor stage | |||||||||
| Lucia et al. [118] | 2023 | Cervical cancer | LNM | n = 178 |
Clinical model PET radiomics-based model Combined clinical and PET radiomics-based model Combat PET radiomics-based model Combined clinical and combat PET radiomics-based model |
Neural network | Combat PET-radiomics model | Training and validation cohorts | AUC: 0.96 |
| Zhang et al. [119] | 2022 | Cervical cancer |
COX-2 status N status |
n = 148 | PET radiomics-based model alone | LASSO + LR | – | Training and validation cohorts |
AUC for COX-2: 0.814 AUC for LNM: 0.817 |
| Li et al. [120] | 2021 | Cervical cancer | LVSI | n = 112 | PET radiomics-based model alone | LASSO + LR | – | Training and validation cohorts | AUC: 0.806 |
| Chong et al. [121] | 2021 | Cervical cancer | ITB | n = 76 | PET radiomics-based model alone | LASSO + SVM | – | Training and validation cohorts | AUC: 0.784 |
| Predicting treatment response or survival | |||||||||
| Ferreira et al. [122] | 2021 | Cervical cancer | Disease progression after CRT | n = 158 | Combined clinical + PET radiomics-based model | RF | – | Training and validation cohorts | AUC: 0.78 |
| Nakajo et al. [123] | 2022 | Cervical cancer | PFS after RT, CRT, or surgery | n = 50 | Combined clinical + PET radiomics-based model | Naïve base algorithm | – |
Internal validation (cross-validation) |
HR: 6.89 |
| Nakajo et al. [124] | 2021 | Endometrial cancer | PFS and OS after RT, CRT, or surgery | n = 53 | Combined clinical + PET radiomics-based model | kNN | – |
Internal validation (cross-validation) |
PFS—HR for coarseness: 0.65; OS—HR for coarseness: 0.52 |
AUC area under the receiver operating characteristic curve, COX-2 cyclooxygenase-2, CRT chemoradiotherapy, HR hazard ratio, ITB intratumoral budding, kNN k-nearest neighbors, LASSO least absolute shrinkage and selection operator algorithm, LNM lymph node metastasis, LR logistic regression, LVSI lymphovascular space invasion, ML machine learning, OS overall survival, PFS progression-free survival, RF random forest, RT radiotherapy, SVM support vector machine
aPerformance only presents the result of the best machine learning model
Lucia et al. [118] developed the ML model with the neural network algorithm using combat harmonized PET-radiomics acquired from the different PET scanners (analog and digital PET) for predicting para-aortic LNM in cervical cancer. Results showed that the constructed ML model had an extremely high predictive ability, with an AUC of 0.96. Zhang et al. [119] showed that the constructed ML model with the LR algorithm using the PET-radiomics scores established using the LASSO regression had good predictive performance for not only pelvic LNM (AUC: 0.817) but also the expression of COX-2 (AUC: 0.814) in cervical cancers. Li et al. [120] revealed that the ML model with the LR algorithm using the PET-radiomics scores constructed using the LASSO regression had good predictive performance for LVSI in cervical cancer, with an AUC of 0.806. Chong et al. [121] showed that the constructed ML model with the SVM algorithm using conventional parameters (SUVmax, MTV, and TLG) and selected 29 PET-radiomics using the LASSO regression algorithm had good predictive performance for intratumoral budding in cervical cancer (AUC: 0.784).
Predicting treatment response or survival
A few reports have addressed the efficacy of 18F-FDG PET/CT radiomics-based ML analysis for predicting treatment outcomes or prognosis in cervical or endometrial cancer [122–124] (Table 6).
Ferreira et al. [122] showed that the ML model with the RF algorithm using clinical data and PET-radiomics had good performance for predicting disease-free survival in patients with advanced-stage cervical cancer who received CRT (AUC: 0.78). Another study revealed that the ML model with the Naïve Bayes algorithm constructed based on FIGO stage and four pretreatment PET-radiomics features (including surface area, MTV, GLRLM_RLNU, and GLRLM_GLNU) was a significant predictor of PFS (HR:6.89, p = 0.003) in patients with cervical cancer who underwent surgery and/or received CRT or chemotherapy [123]. In endometrial cancers, the ML model with the kNN algorithm established using combined clinical data and PET-radiomics has been useful for predicting disease progression, with an AUC of 0.890 [124]. In this study, coarseness, which was the best PET-radiomics feature, was considered a significant and independent factor of PFS (HR:0.65, p = 0.003) and OS (HR:0.52, p < 0.001) in the multivariate Cox regression analysis.
Summary
In cervical or endometrial cancers, each best ML model had good predictive performance for predicting tumor stage with an AUC or accuracy of > 0.70. Moreover, the best ML model or best PET-radiomics feature is a significant predictor of survival, and the heterogenous ML approaches were also observed among the reported studies. Although there are not so many reports that have explored the usefulness of 18F-FDG PET/CT radiomics-based ML analysis associated with gynecological tumors, the 18F-FDG PET/CT radiomics-based ML analysis might provide useful information about patient management with gynecological tumors for clinicians.
Clinical application of 18F-FDG PET/CT radiomics-based ML analyses in other tumors
In hematological malignancies including multiple myeloma and acute leukemia, 18F-FDG PET/CT radiomics-based ML analyses have been applied to identify skeletal metastases, predict diffuse infiltration in the bone marrow, or predict prognosis [125–128] (Table 7).
Table 7.
Summary of representative studies on 18F-FDG PET/CT radiomics-based machine learning analyses in other types of tumors
| Authors | Years | Tumor type | Aim | Sample size | Constructed ML models | Core ML algorithm | Best ML model | Validation | Resultsa |
|---|---|---|---|---|---|---|---|---|---|
| Differentiating primary from metastatic tumors | |||||||||
| Mannam et al. [125] | 2022 | MM | MM vs. skeletal metastasis | n = 40 |
CT radiomics-based model PET radiomics-based model Combined model |
Multilayer perceptron | Combined model | Training and validation cohorts | AUC: 0.9538 |
| Predicting tumor stage, treatment response, or survival | |||||||||
| Mesguich et al. [126] | 2021 | MM | Diffuse infiltration in the bone marrow | n = 30 | Combined CT + PET radiomics-based model | RF | – | Training and validation cohorts | AUC: 0.90 |
| Li et al. [127] | 2019 | Acute leukemia | Diffuse infiltration in the bone marrow | n = 41 | Combined CT + PET radiomics-based model | RF | – | Training and validation cohorts | Accuracy: 0.886 |
| Ni et al. [128] | 2023 | MM | PFS | n = 98 |
Clinical model Combined PET and CT radiomics-based model Combined clinical, PET radiomics-based, and CT radiomics-based model |
LASSO + cox regression | Combined clinical, PET radiomics-based, and CT radiomics-based model | Training and validation cohorts | C-index: 0.698 |
| Feng et al. [130] | 2022 | Neuroblastoma | MKI status | n = 102 |
Clinical model Combined PET and CT radiomics-based model Combined clinical, PET, and CT radiomics-based model |
XGB | Combined PET and CT radiomics-based model | Training and validation cohorts | AUC: 0.951 |
AUC area under the receiver operating characteristic curve, C-index concordance index, LASSO least absolute shrinkage and selection operator algorithm, MKI mitosis-karyorrhexis index, ML machine learning, MM multiple myeloma, PFS progression-free survival, RF random forest, XGB gradient tree boosting
aPerformance only presents the result of the best machine learning model
Mannam et al. [125] showed that the ML model with the multilayer perceptron algorithm established based on CT-radiomics and PET-radiomics had good classification accuracy between multiple myeloma and skeletal metastases, with an AUC of 0.9538. Mesguich et al. [126] developed an ML model with the RF algorithm using five PET/CT radiomics for predicting diffuse infiltration in the bone marrow in multiple myeloma. Results showed that the constructed ML model had an extremely high predictive ability, with an AUC of 0.90. Further, the ML model with the RF algorithm using CT-radiomics and PET-radiomics had good performance in predicting bone marrow involvement in acute leukemia [127]. The diagnostic accuracy of this model was significantly higher than that of visual analysis (0.886 vs. 0.686, p = 0.041). Ni et al. [128] evaluated the ability of 18F-FDG PET/CT radiomics-based ML analysis for predicting PFS after multiple myeloma treatment. Results showed that the ML model with the LASSO + cox regression algorithm trained using the combined clinical and PET/CT radiomics-based model had a higher predictive performance (C-index: 0.698) than the ML model with clinical data (C-index: 0.563) or PET/CT radiomics-based model (C-index: 0.651) alone.
The mistosis-karyorrhexis index (MKI) status is an independent prognostic factor of neuroblastoma [129]. Feng et al. [130] developed the 18F-FDG PET/CT radiomics-based ML model for predicting MKI status in neuroblastoma. The constructed ML model with the XGB algorithm using PET/CT radiomics had an extremely high predictive ability, with an AUC of 0.951. Thus, the ML model can be used to noninvasively predict MKI status in pediatric neuroblastoma. Further, it is a significantly effective tool for the long-term management of pediatric neuroblastoma.
Conclusion
The efficacy of 18F-FDG PET/CT radiomics-based ML analyses in various tumors was investigated. The number of studies about this topic has been increasing after 2018. The 18F-FDG PET/CT radiomics-based ML analyses might be expected to be important tools for patient management in several types of tumors. However, previous studies have reported numerous ML procedures including the use of algorithms, and different ML models have been applied for the same purpose. Thus, various approaches are used to perform 18F-FDG PET/CT radiomics-based ML analysis in oncology. Moreover, 18F-FDG PET/CT radiomics-based ML models, which can be easily and universally applied in clinical practice, should be established.
Funding
No funding.
Declarations
Conflict of interest
The authors declare that they have no conflict interest.
Ethical approval
Not applicable because of a review article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.von Schulthess GK, Steinert HC, Hany TF. Integrated PET/CT: Current applications and future directions. Radiology. 2006;238:405–422. doi: 10.1148/radiol.2382041977. [DOI] [PubMed] [Google Scholar]
- 2.Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278:563–577. doi: 10.1148/radiol.2015151169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tamaki N, Hirata K, Kotani T, Nakai Y, Matsushima S, Yamada K. Four-dimensional quantitative analysis using FDG-PET in clinical oncology. Jpn J Radiol. 2023 doi: 10.1007/s11604-023-01411-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsujikawa T, Rahman T, Yamamoto M, Yamada S, Tsuyoshi H, Kiyono Y, et al. 18F-FDG PET radiomics approaches: comparing and clustering features in cervical cancer. Ann Nucl Med. 2017;31:678–685. doi: 10.1007/s12149-017-1199-7. [DOI] [PubMed] [Google Scholar]
- 5.Peng L, Hong X, Yuan Q, Lu L, Wang Q, Chen W. Prediction of local recurrence and distant metastasis using radiomics analysis of pretreatment nasopharyngeal [18F]FDG PET/CT images. Ann Nucl Med. 2021;35:458–468. doi: 10.1007/s12149-021-01585-9. [DOI] [PubMed] [Google Scholar]
- 6.Kim M, Gu W, Nakajima T, Higuchi T, Ogawa M, Shimizu T, et al. Texture analysis of [18F]-fluorodeoxyglucose-positron emission tomography/computed tomography for predicting the treatment response of postoperative recurrent or metastatic oral squamous cell carcinoma treated with cetuximab. Ann Nucl Med. 2021;35:871–880. doi: 10.1007/s12149-021-01623-6. [DOI] [PubMed] [Google Scholar]
- 7.Coppola F, Faggioni L, Gabelloni M, De Vietro F, Mendola V, Cattabriga A, et al. Human, all too human? an all-around appraisal of the "artificial intelligence revolution" in medical imaging. Front Psychol. 2021;12:710982. doi: 10.3389/fpsyg.2021.710982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeste DV, Graham SA, Nguyen TT, Depp CA, Lee EE, Kim HC. Beyond artificial intelligence: exploring artificial wisdom. Int Psychogeriatr. 2020;32:993–1001. doi: 10.1017/S1041610220000927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Erickson BJ, Korfiatis P, Akkus Z, Kline TL. Machine learning for medical imaging. Radiographics. 2017;37:505–515. doi: 10.1148/rg.2017160130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waljee AK, Higgins PD. Machine learning in medicine: a primer for physicians. Am J Gastroenterol. 2010;105:1224–1226. doi: 10.1038/ajg.2010.173. [DOI] [PubMed] [Google Scholar]
- 11.Panch T, Szolovits P, Atun R. Artificial intelligence, machine learning and health systems. J Glob Health. 2018;8:020303. doi: 10.7189/jogh.08.020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hirata K, Sugimori H, Fujima N, Toyonaga T, Kudo K. Artificial intelligence for nuclear medicine in oncology. Ann Nucl Med. 2022;36:123–132. doi: 10.1007/s12149-021-01693-6. [DOI] [PubMed] [Google Scholar]
- 13.Sim YT, Poon FW. Imaging of solitary pulmonary nodule-a clinical review. Quant Imaging Med Surg. 2013;3:316–326. doi: 10.3978/j.issn.2223-4292.2013.12.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ren C, Xu M, Zhang J, Zhang F, Song S, Sun Y, et al. Classification of solid pulmonary nodules using a machine-learning nomogram based on 18F-FDG PET/CT radiomics integrated clinicobiological features. Ann Transl Med. 2022;10:1265. doi: 10.21037/atm-22-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou Y, Ma XL, Zhang T, Wang J, Zhang T, Tian R. Use of radiomics based on 18F-FDG PET/CT and machine learning methods to aid clinical decision-making in the classification of solitary pulmonary lesions: an innovative approach. Eur J Nucl Med Mol Imaging. 2021;48:2904–2913. doi: 10.1007/s00259-021-05220-7. [DOI] [PubMed] [Google Scholar]
- 16.Salihoğlu YS, Uslu Erdemir R, Aydur Püren B, Özdemir S, Uyulan Ç, Ergüzel TT, et al. Diagnostic performance of machine learning models based on 18F-FDG PET/CT radiomic features in the classification of solitary pulmonary nodules. Mol Imaging Radionucl Ther. 2022;31:82–88. doi: 10.4274/mirt.galenos.2021.43760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang R, Zhu L, Cai Z, Jiang W, Li J, Yang C, et al. Potential feature exploration and model development based on 18F-FDG PET/CT images for differentiating benign and malignant lung lesions. Eur J Radiol. 2019;121:108735. doi: 10.1016/j.ejrad.2019.108735. [DOI] [PubMed] [Google Scholar]
- 18.Yan M, Wang W. Development of a radiomics prediction model for histological type diagnosis in solitary pulmonary nodules: the combination of CT and FDG PET. Front Oncol. 2020;10:555514. doi: 10.3389/fonc.2020.555514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agüloğlu N, Aksu A, Unat DS. Machine learning approach using 18F-FDG PET-based radiomics in differentiation of lung adenocarcinoma with bronchoalveolar distribution and infection. Nucl Med Commun. 2023;44:302–308. doi: 10.1097/MNM.0000000000001667. [DOI] [PubMed] [Google Scholar]
- 20.Ma Y, Feng W, Wu Z, Liu M, Zhang F, Liang Z, et al. Intra-tumoural heterogeneity characterization through texture and colour analysis for differentiation of non-small cell lung carcinoma subtypes. Phys Med Biol. 2018;63:165018. doi: 10.1088/1361-6560/aad648. [DOI] [PubMed] [Google Scholar]
- 21.Fukui T, Taniguchi T, Kawaguchi K, Fukumoto K, Nakamura S, Sakao Y, et al. Comparisons of the clinicopathological features and survival outcomes between lung cancer patients with adenocarcinoma and squamous cell carcinoma. Gen Thorac Cardiovasc Surg. 2015;63:507–513. doi: 10.1007/s11748-015-0564-5. [DOI] [PubMed] [Google Scholar]
- 22.Zhao H, Su Y, Wang M, Lyu Z, Xu P, Jiao Y, et al. The machine learning model for distinguishing pathological subtypes of non-small cell lung cancer. Front Oncol. 2022;12:875761. doi: 10.3389/fonc.2022.875761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han Y, Ma Y, Wu Z, Zhang F, Zheng D, Liu X, et al. Histologic subtype classification of non-small cell lung cancer using PET/CT images. Eur J Nucl Med Mol Imaging. 2021;48:350–360. doi: 10.1007/s00259-020-04771-5. [DOI] [PubMed] [Google Scholar]
- 24.Ren C, Zhang J, Qi M, Zhang J, Zhang Y, Song S, et al. Machine learning based on clinico-biological features integrated 18F-FDG PET/CT radiomics for distinguishing squamous cell carcinoma from adenocarcinoma of lung. Eur J Nucl Med Mol Imaging. 2021;48:1538–1549. doi: 10.1007/s00259-020-05065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Koyasu S, Nishio M, Isoda H, Nakamoto Y, Togashi K. Usefulness of gradient tree boosting for predicting histological subtype and EGFR mutation status of non-small cell lung cancer on 18F FDG-PET/CT. Ann Nucl Med. 2020;34:49–57. doi: 10.1007/s12149-019-01414-0. [DOI] [PubMed] [Google Scholar]
- 26.Hyun SH, Ahn MS, Koh YW, Lee SJ. A Machine-learning approach using PET-based radiomics to predict the histological subtypes of lung cancer. Clin Nucl Med. 2019;44:956–960. doi: 10.1097/RLU.0000000000002810. [DOI] [PubMed] [Google Scholar]
- 27.Nakajo M, Takeda A, Katsuki A, Jinguji M, Ohmura K, Tani A, et al. The efficacy of 18F-FDG-PET-based radiomic and deep-learning features using a machine-learning approach to predict the pathological risk subtypes of thymic epithelial tumors. Br J Radiol. 2022;95:20211050. doi: 10.1259/bjr.20211050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ozkan E, Orhan K, Soydal C, Kahya Y, Seckin Tunc S, et al. Combined clinical and specific positron emission tomography/computed tomography-based radiomic features and machine-learning model in prediction of thymoma risk groups. Nucl Med Commun. 2022;43:529–539. doi: 10.1097/MNM.0000000000001547. [DOI] [PubMed] [Google Scholar]
- 29.Herbst RS, Morgensztern D, Boshoff C. The biology and management of non-small cell lung cancer. Nature. 2018;553:446–454. doi: 10.1038/nature25183. [DOI] [PubMed] [Google Scholar]
- 30.Linardou H, Dahabreh IJ, Kanaloupiti D, Siannis F, Bafaloukos D, Kosmidis P, et al. Assessment of somatic k-RAS mutations as a mechanism associated with resistance to EGFR-targeted agents: a systematic review and meta-analysis of studies in advanced non-small-cell lung cancer and metastatic colorectal cancer. Lancet Oncol. 2008;9:962–972. doi: 10.1016/S1470-2045(08)70206-7. [DOI] [PubMed] [Google Scholar]
- 31.Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csőszi T, Fulop A, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375:1823–1833. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 32.Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–128. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gao J, Niu R, Shi Y, Shao X, Jiang Z, Ge X, et al. The predictive value of [18F]FDG PET/CT radiomics combined with clinical features for EGFR mutation status in different clinical staging of lung adenocarcinoma. EJNMMI Res. 2023;13:26. doi: 10.1186/s13550-023-00977-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chang C, Sun X, Wang G, Yu H, Zhao W, Ge Y, et al. A machine learning model based on PET/CT radiomics and cinical characteristics predicts ALK rearrangement status in lung adenocarcinoma. Front Oncol. 2021;11:603882. doi: 10.3389/fonc.2021.603882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shiri I, Maleki H, Hajianfar G, Abdollahi H, Ashrafinia S, Hatt M, et al. Next-generation radiogenomics sequencing for prediction of EGFR and KRAS mutation status in NSCLC patients using multimodal imaging and machine learning algorithms. Mol Imaging Biol. 2020;22:1132–1148. doi: 10.1007/s11307-020-01487-8. [DOI] [PubMed] [Google Scholar]
- 36.Liu Q, Sun D, Li N, Kim J, Feng D, Huang G, et al. Predicting EGFR mutation subtypes in lung adenocarcinoma using 18F-FDG PET/CT radiomic features. Transl Lung Cancer Res. 2020;9:549–562. doi: 10.21037/tlcr.2020.04.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agüloğlu N, Aksu A, Akyol M, Katgı N, Doksöz TÇ. Importance of pretreatment 18F-FDG PET/CT texture analysis in predicting EGFR and ALK mutation in patients with non-small cell lung cancer. Nuklearmedizin. 2022;61:433–439. doi: 10.1055/a-1868-4918. [DOI] [PubMed] [Google Scholar]
- 38.Nair JKR, Saeed UA, McDougall CC, Sabri A, Kovacina B, Raidu BVS, et al. Radiogenomic models using machine learning techniques to predict EGFR mutations in non-small cell lung cancer. Can Assoc Radiol J. 2021;72:109–119. doi: 10.1177/0846537119899526. [DOI] [PubMed] [Google Scholar]
- 39.Li X, Yin G, Zhang Y, Dai D, Liu J, Chen P, et al. Predictive power of a radiomic signature based on 18F-FDG PET/CT images for EGFR mutational status in NSCLC. Front Oncol. 2019;9:1062. doi: 10.3389/fonc.2019.01062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lim CH, Koh YW, Hyun SH, Lee SJ. A machine learning approach using PET/CT-based radiomics for prediction of PD-L1 expression in non-small cell lung cancer. Anticancer Res. 2022;42:5875–5884. doi: 10.21873/anticanres.16096. [DOI] [PubMed] [Google Scholar]
- 41.Mu W, Jiang L, Shi Y, Tunali I, Gray JE, Katsoulakis E, et al. Non-invasive measurement of PD-L1 status and prediction of immunotherapy response using deep learning of PET/CT images. J Immunother Cancer. 2021;9:e002118. doi: 10.1136/jitc-2020-002118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tong H, Sun J, Fang J, Zhang M, Liu H, Xia R, et al. A machine learning model based on PET/CT radiomics and clinical characteristics predicts tumor immune profiles in non-small cell lung cancer: a retrospective multicohort study. Front Immunol. 2022;13:859323. doi: 10.3389/fimmu.2022.859323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WEE, et al. The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol. 2016;11:39–51. doi: 10.1016/j.jtho.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 44.Wang M, Liu L, Dai Q, Jin M, Huang G. Developing a primary tumor and lymph node 18F-FDG PET/CT-clinical (TLPC) model to predict lymph node metastasis of resectable T2–4 NSCLC. J Cancer Res Clin Oncol. 2023;149:247–261. doi: 10.1007/s00432-022-04545-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laros SSA, Dieckens D, Blazis SP, van der Heide JA. Machine learning classification of mediastinal lymph node metastasis in NSCLC: a multicentre study in a Western European patient population. EJNMMI Phys. 2022;9:66. doi: 10.1186/s40658-022-00494-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Onozato Y, Iwata T, Uematsu Y, Shimizu D, Yamamoto T, Matsui Y, et al. Predicting pathological highly invasive lung cancer from preoperative [18F]FDG PET/CT with multiple machine learning models. Eur J Nucl Med Mol Imaging. 2023;50:715–726. doi: 10.1007/s00259-022-06038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao M, Kluge K, Papp L, Grahovac M, Yang S, Jiang C, et al. Multi-lesion radiomics of PET/CT for non-invasive survival stratification and histologic tumor risk profiling in patients with lung adenocarcinoma. Eur Radiol. 2022;32:7056–7067. doi: 10.1007/s00330-022-08999-7. [DOI] [PubMed] [Google Scholar]
- 48.Huang B, Sollee J, Luo YH, Reddy A, Zhong Z, Wu J, et al. Prediction of lung malignancy progression and survival with machine learning based on pre-treatment FDG-PET/CT. EBioMedicine. 2022;82:104127. doi: 10.1016/j.ebiom.2022.104127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ahn HK, Lee H, Kim SG, Hyun SH. Pre-treatment 18F-FDG PET-based radiomics predict survival in resected non-small cell lung cancer. Clin Radiol. 2019;74:467–473. doi: 10.1016/j.crad.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 50.Kirienko M, Sollini M, Corbetta M, Voulaz E, Gozzi N, Interlenghi M, et al. Radiomics and gene expression profile to characterise the disease and predict outcome in patients with lung cancer. Eur J Nucl Med Mol Imaging. 2021;48:3643–3655. doi: 10.1007/s00259-021-05371-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mu W, Jiang L, Zhang J, Shi Y, Gray JE, Tunali I, et al. Non-invasive decision support for NSCLC treatment using PET/CT radiomics. Nat Commun. 2020;11:5228. doi: 10.1038/s41467-020-19116-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mu W, Tunali I, Gray JE, Qi J, Schabath MB, Gillies RJ. Radiomics of 18F-FDG PET/CT images predicts clinical benefit of advanced NSCLC patients to checkpoint blockade immunotherapy. Eur J Nucl Med Mol Imaging. 2020;47:1168–1182. doi: 10.1007/s00259-019-04625-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bertolini M, Trojani V, Botti A, Cucurachi N, Galaverni M, Cozzi S, et al. Novel harmonization method for multi-Centric radiomic studies in non-small cell lung cancer. Curr Oncol. 2022;29:5179–5194. doi: 10.3390/curroncol29080410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sepehri S, Tankyevych O, Upadhaya T, Visvikis D, Hatt M, Cheze Le Rest C. Comparison and fusion of machine learning algorithms for prospective validation of PET/CT radiomic features prognostic value in stage II-III non-small cell lung cancer. Diagnostics (Basel) 2021;11:675. doi: 10.3390/diagnostics11040675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Afshar P, Mohammadi A, Tyrrell PN, Cheung P, Sigiuk A, Plataniotis KN, et al. DRTOP: deep learning-based radiomics for the time-to-event outcome prediction in lung cancer. Sci Rep. 2020;10:12366. doi: 10.1038/s41598-020-69106-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Astaraki M, Wang C, Buizza G, Toma-Dasu I, Lazzeroni M, Smedby Ö. Early survival prediction in non-small cell lung cancer from PET/CT images using an intra-tumor partitioning method. Phys Med. 2019;60:58–65. doi: 10.1016/j.ejmp.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 57.Park SB, Kim KU, Park YW, Hwang JH, Lim CH. Application of 18F-fluorodeoxyglucose PET/CT radiomic features and machine learning to predict early recurrence of non-small cell lung cancer after curative-intent therapy. Nucl Med Commun. 2023;44:161–168. doi: 10.1097/MNM.0000000000001646. [DOI] [PubMed] [Google Scholar]
- 58.Pavic M, Bogowicz M, Kraft J, Vuong D, Mayinger M, Kroeze SGC, et al. FDG PET versus CT radiomics to predict outcome in malignant pleural mesothelioma patients. EJNMMI Res. 2020;10:81. doi: 10.1186/s13550-020-00669-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Palaniswamy SS, Subramanyam P. Diagnostic utility of PETCT in thyroid malignancies: an update. Ann Nucl Med. 2013;27:681–693. doi: 10.1007/s12149-013-0740-6. [DOI] [PubMed] [Google Scholar]
- 60.Aksu A, Karahan Şen NP, Acar E, Çapa KG. Evaluating focal 18F-FDG uptake in thyroid gland with radiomics. Nucl Med Mol Imaging. 2020;54:241–248. doi: 10.1007/s13139-020-00659-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Benson E, Li R, Eisele D, Fakhry C. The clinical impact of HPV tumor status upon head and neck squamous cell carcinomas. Oral Oncol. 2014;50:565–574. doi: 10.1016/j.oraloncology.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Haider SP, Mahajan A, Zeevi T, Baumeister P, Reichel C, Sharaf K, et al. PET/CT radiomics signature of human papilloma virus association in oropharyngeal squamous cell carcinoma. Eur J Nucl Med Mol Imaging. 2020;47:2978–2991. doi: 10.1007/s00259-020-04839-2. [DOI] [PubMed] [Google Scholar]
- 63.Haider SP, Sharaf K, Zeevi T, Baumeister P, Reichel C, Forghani R, et al. Prediction of post-radiotherapy locoregional progression in HPV-associated oropharyngeal squamous cell carcinoma using machine-learning analysis of baseline PET/CT radiomics. Transl Oncol. 2021;14:100906. doi: 10.1016/j.tranon.2020.100906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nakajo M, Kawaji K, Nagano H, Jinguji M, Mukai A, Kawabata H, et al. The usefulness of machine learning-based evaluation of clinical and pretreatment [18F]-FDG-PET/CT radiomic features for predicting prognosis in hypopharyngeal cancer. Mol Imaging Biol. 2023;25:303–313. doi: 10.1007/s11307-022-01757-7. [DOI] [PubMed] [Google Scholar]
- 65.Lafata KJ, Chang Y, Wang C, Mowery YM, Vergalasova I, Niedzwiecki D, et al. Intrinsic radiomic expression patterns after 20 Gy demonstrate early metabolic response of oropharyngeal cancers. Med Phys. 2021;48:3767–3777. doi: 10.1002/mp.14926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Spielvogel CP, Stoiber S, Papp L, Krajnc D, Grahovac M, Gurnhofer E, et al. Radiogenomic markers enable risk stratification and inference of mutational pathway states in head and neck cancer. Eur J Nucl Med Mol Imaging. 2023;50:546–558. doi: 10.1007/s00259-022-05973-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Haider SP, Zeevi T, Baumeister P, Reichel C, Sharaf K, Forghani R, et al. Potential added value of PET/CT radiomics for survival prognostication beyond AJCC 8th edition staging in oropharyngeal squamous cell carcinoma. Cancers (Basel) 2020;12:1778. doi: 10.3390/cancers12071778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhong J, Frood R, Brown P, Nelstrop H, Prestwich R, McDermott G, et al. Machine learning-based FDG PET-CT radiomics for outcome prediction in larynx and hypopharynx squamous cell carcinoma. Clin Radiol. 2021;76:78.e9–78.e17. doi: 10.1016/j.crad.2020.08.030. [DOI] [PubMed] [Google Scholar]
- 69.Du D, Feng H, Lv W, Ashrafinia S, Yuan Q, Wang Q, et al. Machine learning methods for optimal radiomics-based differentiation between recurrence and inflammation: application to nasopharyngeal carcinoma post-therapy PET/CT images. Mol Imaging Biol. 2020;22:730–738. doi: 10.1007/s11307-019-01411-9. [DOI] [PubMed] [Google Scholar]
- 70.Peng H, Dong D, Fang MJ, Li L, Tang LL, Chen L, et al. Prognostic value of deep learning PET/CT-based radiomics: potential role for future individual induction chemotherapy in advanced nasopharyngeal carcinoma. Clin Cancer Res. 2019;25:4271–4279. doi: 10.1158/1078-0432.CCR-18-3065. [DOI] [PubMed] [Google Scholar]
- 71.Liu Z, Cao Y, Diao W, Cheng Y, Jia Z, Peng X. Radiomics-based prediction of survival in patients with head and neck squamous cell carcinoma based on pre- and post-treatment 18F-PET/CT. Aging (Albany NY) 2020;12:14593–14619. doi: 10.18632/aging.103508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhao P, Yu T, Pan Z. Prognostic value of the baseline 18F-FDG PET/CT metabolic tumour volume (MTV) and further stratification in low-intermediate (L-I) and high-intermediate (H-I) risk NCCNIPI subgroup by MTV in DLBCL MTV predict prognosis in DLBCL. Ann Nucl Med. 2021;35:24–30. doi: 10.1007/s12149-020-01531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baba S, Abe K, Isoda T, Maruoka Y, Sasaki M, Honda H. Impact of FDG-PET/CT in the management of lymphoma. Ann Nucl Med. 2011;25:701–716. doi: 10.1007/s12149-011-0549-0. [DOI] [PubMed] [Google Scholar]
- 74.Dagogo-Jack I, Shaw AT. Tumour heterogeneity and resistance to cancer therapies. Nat Rev Clin Oncol. 2018;15:81–94. doi: 10.1038/nrclinonc.2017.166. [DOI] [PubMed] [Google Scholar]
- 75.Lambin P, Leijenaar RTH, Deist TM, Peerlings J, de Jong EEC, van Timmeren J, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14:749–762. doi: 10.1038/nrclinonc.2017.141. [DOI] [PubMed] [Google Scholar]
- 76.Abenavoli EM, Barbetti M, Linguanti F, Mungai F, Nassi L, Puccini B, et al. Characterization of mediastinal bulky lymphomas with FDG-PET-based radiomics and machine learning techniques. Cancers (Basel) 2023;15:1931. doi: 10.3390/cancers15071931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.de Jesus FM, Yin Y, Mantzorou-Kyriaki E, Kahle XU, de Haas RJ, Yakar D, et al. Machine learning in the differentiation of follicular lymphoma from diffuse large B-cell lymphoma with radiomic [18F]FDG PET/CT features. Eur J Nucl Med Mol Imaging. 2022;49:1535–1543. doi: 10.1007/s00259-021-05626-3. [DOI] [PubMed] [Google Scholar]
- 78.Lovinfosse P, Ferreira M, Withofs N, Jadoul A, Derwael C, Frix AN, et al. Distinction of lymphoma from Sarcoidosis on 18F-FDG PET/CT: evaluation of radiomics-feature-guided machine learning versus human reader performance. J Nucl Med. 2022;63:1933–1940. doi: 10.2967/jnumed.121.263598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang Y, Zheng B, Li Y, Li Y, Ma X. Computer-aided diagnostic models to classify lymph node metastasis and lymphoma involvement in enlarged cervical lymph nodes using PET/CT. Med Phys. 2023;50:152–162. doi: 10.1002/mp.15901. [DOI] [PubMed] [Google Scholar]
- 80.Cui C, Yao X, Xu L, Chao Y, Hu Y, Zhao S, et al. Improving the classification of PCNSL and brain metastases by developing a machine learning model based on 18F-FDG PET. J Pers Med. 2023;13:539. doi: 10.3390/jpm13030539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Tilly H, Vitolo U, Walewski J, da Silva MG, Shpilberg O, André M, et al. Diffuse large B-cell lymphoma (DLBCL): ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2012;23(Suppl 7):vii78–82. doi: 10.1093/annonc/mds273. [DOI] [PubMed] [Google Scholar]
- 82.Annunziata S, Cuccaro A, Calcagni ML, Hohaus S, Giordano A, Rufini V. Interim FDG-PET/CT in Hodgkin lymphoma: the prognostic role of the ratio between target lesion and liver SUVmax (rPET) Ann Nucl Med. 2016;30:588–592. doi: 10.1007/s12149-016-1092-9. [DOI] [PubMed] [Google Scholar]
- 83.Annunziata S, Cuccaro A, Tisi MC, Hohaus S, Rufini V. FDG-PET/CT at the end of immuno-chemotherapy in follicular lymphoma: the prognostic role of the ratio between target lesion and liver SUVmax (rPET) Ann Nucl Med. 2018;32:372–377. doi: 10.1007/s12149-018-1243-2. [DOI] [PubMed] [Google Scholar]
- 84.Frood R, Clark M, Burton C, Tsoumpas C, Frangi AF, Gleeson F, et al. Discovery of pre-treatment FDG PET/CT-derived radiomics-based models for predicting outcome in diffuse large B-cell lymphoma. Cancers (Basel) 2022;14:1711. doi: 10.3390/cancers14071711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cui Y, Jiang Y, Deng X, Long W, Liu B, Fan W, et al. 18F-FDG PET-based combined baseline and end-of-treatment radiomics model improves the prognosis prediction in diffuse large B cell lymphoma after first-line therapy. Acad Radiol. 2022;S1076–6332(22):00548–557. doi: 10.1016/j.acra.2022.10.011. [DOI] [PubMed] [Google Scholar]
- 86.Frood R, Clark M, Burton C, Tsoumpas C, Frangi AF, Gleeson F, et al. Utility of pre-treatment FDG PET/CT-derived machine learning models for outcome prediction in classical Hodgkin lymphoma. Eur Radiol. 2022;32:7237–7247. doi: 10.1007/s00330-022-09039-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ritter Z, Papp L, Zámbó K, Tóth Z, Dezső D, Veres DS, et al. Two-year event-free survival prediction in DLBCL patients based on in vivo radiomics and clinical parameters. Front Oncol. 2022;12:820136. doi: 10.3389/fonc.2022.820136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jiang C, Li A, Teng Y, Huang X, Ding C, Chen J, et al. Optimal PET-based radiomic signature construction based on the cross-combination method for predicting the survival of patients with diffuse large B-cell lymphoma. Eur J Nucl Med Mol Imaging. 2022;49:2902–2916. doi: 10.1007/s00259-022-05717-9. [DOI] [PubMed] [Google Scholar]
- 89.Jiang C, Huang X, Li A, Teng Y, Ding C, Chen J, et al. Radiomics signature from [18F]FDG PET images for prognosis predication of primary gastrointestinal diffuse large B cell lymphoma. Eur Radiol. 2022;32:5730–5741. doi: 10.1007/s00330-022-08668-9. [DOI] [PubMed] [Google Scholar]
- 90.Coskun N, Okudan B, Uncu D, Kitapci MT. Baseline 18F-FDG PET textural features as predictors of response to chemotherapy in diffuse large B-cell lymphoma. Nucl Med Commun. 2021;42:1227–1232. doi: 10.1097/MNM.0000000000001447. [DOI] [PubMed] [Google Scholar]
- 91.Milgrom SA, Elhalawani H, Lee J, Wang Q, Mohamed ASR, Dabaja BS, et al. A PET radiomics model to predict refractory mediastinal Hodgkin lymphoma. Sci Rep. 2019;9:1322. doi: 10.1038/s41598-018-37197-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Eifer M, Pinian H, Klang E, Alhoubani Y, Kanana N, Tau N, et al. FDG PET/CT radiomics as a tool to differentiate between reactive axillary lymphadenopathy following COVID-19 vaccination and metastatic breast cancer axillary lymphadenopathy: a pilot study. Eur Radiol. 2022;32:5921–5929. doi: 10.1007/s00330-022-08725-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chen Y, Wang Z, Yin G, Sui C, Liu Z, Li X, et al. Prediction of HER2 expression in breast cancer by combining PET/CT radiomic analysis and machine learning. Ann Nucl Med. 2022;36:172–182. doi: 10.1007/s12149-021-01688-3. [DOI] [PubMed] [Google Scholar]
- 94.Song BI. A machine learning-based radiomics model for the prediction of axillary lymph-node metastasis in breast cancer. Breast Cancer. 2021;28:664–671. doi: 10.1007/s12282-020-01202-z. [DOI] [PubMed] [Google Scholar]
- 95.Krajnc D, Papp L, Nakuz TS, Magometschnigg HF, Grahovac M, Spielvogel CP, et al. Breast tumor characterization using [18F]FDG-PET/CT imaging combined with data preprocessing and radiomics. Cancers (Basel) 2021;13(6):1249. doi: 10.3390/cancers13061249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ou X, Zhang J, Wang J, Pang F, Wang Y, Wei X, et al. Radiomics based on 18 F-FDG PET/CT could differentiate breast carcinoma from breast lymphoma using machine-learning approach: a preliminary study. Cancer Med. 2020;9:496–506. doi: 10.1002/cam4.2711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Harbeck N, Penault-Llorca F, Cortes J, Gnant M, Houssami N, Poortmans P, et al. Breast cancer. Nat Rev Dis Primers. 2019;5:66. doi: 10.1038/s41572-019-0111-2. [DOI] [PubMed] [Google Scholar]
- 98.Burstein HJ. The distinctive nature of HER2-positive breast cancers. N Engl J Med. 2005;353:1652–1654. doi: 10.1056/NEJMp058197. [DOI] [PubMed] [Google Scholar]
- 99.Banerjee M, George J, Song EY, Roy A, Hryniuk W. Tree-based model for breast cancer prognostication. J Clin Oncol. 2004;22:2567–2575. doi: 10.1200/JCO.2004.11.141. [DOI] [PubMed] [Google Scholar]
- 100.Li P, Wang X, Xu C, Liu C, Zheng C, Fulham MJ, et al. 18F-FDG PET/CT radiomic predictors of pathologic complete response (pCR) to neoadjuvant chemotherapy in breast cancer patients. Eur J Nucl Med Mol Imaging. 2020;47:1116–1126. doi: 10.1007/s00259-020-04684-3. [DOI] [PubMed] [Google Scholar]
- 101.Gómez OV, Herraiz JL, Udías JM, Haug A, Papp L, Cioni D, et al. Analysis of cross-combinations of feature selection and machine-learning classification methods based on [18F]F-FDG PET/CT radiomic features for metabolic response prediction of metastatic breast cancer lesions. Cancers (Basel) 2022;14:2922. doi: 10.3390/cancers14122922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhang Y, Cheng C, Liu Z, Wang L, Pan G, Sun G, et al. Radiomics analysis for the differentiation of autoimmune pancreatitis and pancreatic ductal adenocarcinoma in 18 F-FDG PET/CT. Med Phys. 2019;46:4520–4530. doi: 10.1002/mp.13733. [DOI] [PubMed] [Google Scholar]
- 103.Wei W, Jia G, Wu Z, Wang T, Wang H, Wei K, et al. A multidomain fusion model of radiomics and deep learning to discriminate between PDAC and AIP based on 18F-FDG PET/CT images. Jpn J Radiol. 2023;41:417–427. doi: 10.1007/s11604-022-01363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Xing H, Hao Z, Zhu W, Sun D, Ding J, Zhang H, et al. Preoperative prediction of pathological grade in pancreatic ductal adenocarcinoma based on 18F-FDG PET/CT radiomics. EJNMMI Res. 2021;11:19. doi: 10.1186/s13550-021-00760-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Jiang C, Zhao L, Xin B, Ma G, Wang X, Song S. 18F-FDG PET/CT radiomic analysis for classifying and predicting microvascular invasion in hepatocellular carcinoma and intrahepatic cholangiocarcinoma. Quant Imaging Med Surg. 2022;12:4135–4150. doi: 10.21037/qims-21-1167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Liu Q, Li J, Xin B, Sun Y, Feng D, Fulham MJ, et al. 18F-FDG PET/CT radiomics for preoperative prediction of lymph node metastases and nodal staging in gastric cancer. Front Oncol. 2021;11:723345. doi: 10.3389/fonc.2021.723345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.He J, Wang Q, Zhang Y, Wu H, Zhou Y, Zhao S. Preoperative prediction of regional lymph node metastasis of colorectal cancer based on 18F-FDG PET/CT and machine learning. Ann Nucl Med. 2021;35:617–627. doi: 10.1007/s12149-021-01605-8. [DOI] [PubMed] [Google Scholar]
- 108.Li J, Yang Z, Xin B, Hao Y, Wang L, Song S, et al. Quantitative prediction of microsatellite instability in colorectal cancer with preoperative PET/CT-based radiomics. Front Oncol. 2021;11:702055. doi: 10.3389/fonc.2021.702055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Toyama Y, Hotta M, Motoi F, Takanami K, Minamimoto R, Takase K. Prognostic value of FDG-PET radiomics with machine learning in pancreatic cancer. Sci Rep. 2020;10:17024. doi: 10.1038/s41598-020-73237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Liu Q, Li J, Xin B, Sun Y, Wang X, Song S. Preoperative 18F-FDG PET/CT radiomics analysis for predicting HER2 expression and prognosis in gastric cancer. Quant Imaging Med Surg. 2023;13:1537–1549. doi: 10.21037/qims-22-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Lv L, Xin B, Hao Y, Yang Z, Xu J, Wang L, et al. Radiomic analysis for predicting prognosis of colorectal cancer from preoperative 18F-FDG PET/CT. J Transl Med. 2022;20:66. doi: 10.1186/s12967-022-03262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Shen WC, Chen SW, Wu KC, Lee PY, Feng CL, Hsieh TC, et al. Predicting pathological complete response in rectal cancer after chemoradiotherapy with a random forest using 18F-fluorodeoxyglucose positron emission tomography and computed tomography radiomics. Ann Transl Med. 2020;8:207. doi: 10.21037/atm.2020.01.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Agüloğlu N, Aksu A. Evaluation of survival of the patients with metastatic rectal cancer by staging 18F-FDG PET/CT radiomic and volumetric parameters. Rev Esp Med Nucl Imagen Mol (Engl Ed) 2023;42:122–128. doi: 10.1016/j.remnie.2022.09.010. [DOI] [PubMed] [Google Scholar]
- 114.Liu H, Xiao J, Yang Y, Liu Y, Ma R, Li Y, et al. COX-2 expression is correlated with VEGF-C, lymphangiogenesis and lymph node metastasis in human cervical cancer. Microvasc Res. 2011;82:131–140. doi: 10.1016/j.mvr.2011.04.011. [DOI] [PubMed] [Google Scholar]
- 115.Hoellen F, Waldmann A, Banz-Jansen C, Rody A, Heide M, Köster F, et al. Expression of cyclooxygenase-2 in cervical cancer is associated with lymphovascular invasion. Oncol Lett. 2016;12:2351–2356. doi: 10.3892/ol.2016.4925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lugli A, Kirsch R, Ajioka Y, Bosman F, Cathomas G, Dawson H, et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod Pathol. 2017;30:1299–1311. doi: 10.1038/modpathol.2017.46. [DOI] [PubMed] [Google Scholar]
- 117.Park JY, Hong DG, Chong GO, Park JY. Tumor Budding is a Valuable diagnostic parameter in prediction of disease progression of endometrial endometrioid carcinoma. Pathol Oncol Res. 2019;25:723–730. doi: 10.1007/s12253-018-0554-x. [DOI] [PubMed] [Google Scholar]
- 118.Lucia F, Bourbonne V, Pleyers C, Dupré PF, Miranda O, Visvikis D, et al. Multicentric development and evaluation of 18F-FDG PET/CT and MRI radiomics models to predict para-aortic lymph node involvement in locally advanced cervical cancer. Eur J Nucl Med Mol Imaging. 2023;50:2514–2528. doi: 10.1007/s00259-023-06180-w. [DOI] [PubMed] [Google Scholar]
- 119.Zhang Z, Li X, Sun H. Development of machine learning models integrating PET/CT radiomic and immunohistochemical pathomic features for treatment strategy choice of cervical cancer with negative pelvic lymph node by mediating COX-2 expression. Front Physiol. 2022;13:994304. doi: 10.3389/fphys.2022.994304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Li X, Xu C, Yu Y, Guo Y, Sun H. Prediction of lymphovascular space invasion using a combination of tenascin-C, cox-2, and PET/CT radiomics in patients with early-stage cervical squamous cell carcinoma. BMC Cancer. 2021;21:866. doi: 10.1186/s12885-021-08596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Chong GO, Park SH, Jeong SY, Kim SJ, Park NJ, Lee YH, et al. Prediction model for tumor budding status using the radiomic features of F-18 fluorodeoxyglucose positron emission tomography/computed tomography in cervical cancer. Diagnostics (Basel) 2021;11:1517. doi: 10.3390/diagnostics11081517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ferreira M, Lovinfosse P, Hermesse J, Decuypere M, Rousseau C, Lucia F, et al. [18F]FDG PET radiomics to predict disease-free survival in cervical cancer: a multi-scanner/center study with external validation. Eur J Nucl Med Mol Imaging. 2021;48:3432–3443. doi: 10.1007/s00259-021-05303-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Nakajo M, Jinguji M, Tani A, Yano E, Hoo CK, Hirahara D, et al. Machine learning based evaluation of clinical and pretreatment 18F-FDG-PET/CT radiomic features to predict prognosis of cervical cancer patients. Abdom Radiol (NY) 2022;47:838–847. doi: 10.1007/s00261-021-03350-y. [DOI] [PubMed] [Google Scholar]
- 124.Nakajo M, Jinguji M, Tani A, Kikuno H, Hirahara D, Togami S, et al. Application of a machine learning approach for the analysis of clinical and radiomic features of pretreatment [18F]-FDG PET/CT to predict prognosis of patients with endometrial cancer. Mol Imaging Biol. 2021;23:756–765. doi: 10.1007/s11307-021-01599-9. [DOI] [PubMed] [Google Scholar]
- 125.Mannam P, Murali A, Gokulakrishnan P, Venkatachalapathy E, Venkata Sai PM. Radiomic analysis of positron-emission tomography and computed tomography images to differentiate between multiple myeloma and skeletal metastases. Indian J Nucl Med. 2022;37:217–226. doi: 10.4103/ijnm.ijnm_111_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mesguich C, Hindie E, de Senneville BD, Tlili G, Pinaquy JB, Marit G, et al. Improved 18-FDG PET/CT diagnosis of multiple myeloma diffuse disease by radiomics analysis. Nucl Med Commun. 2021;42:1135–1143. doi: 10.1097/MNM.0000000000001437. [DOI] [PubMed] [Google Scholar]
- 127.Li H, Xu C, Xin B, Zheng C, Zhao Y, Hao K, et al. 18F-FDG PET/CT radiomic analysis with machine learning for identifying bone marrow involvement in the patients with suspected relapsed acute leukemia. Theranostics. 2019;9:4730–4739. doi: 10.7150/thno.33841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Ni B, Huang G, Huang H, Wang T, Han X, Shen L, et al. Machine learning model based on optimized radiomics feature from 18F-FDG-PET/CT and clinical characteristics predicts prognosis of multiple myeloma: a preliminary study. J Clin Med. 2023;12:2280. doi: 10.3390/jcm12062280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Sokol E, Desai AV, Applebaum MA, Valteau-Couanet D, Park JR, Pearson ADJ, et al. Age, diagnostic category, tumor grade, and Mitosis-Karyorrhexis Index are independently prognostic in neuroblastoma: an INRG project. J Clin Oncol. 2020;38:1906–1918. doi: 10.1200/JCO.19.03285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Feng L, Qian L, Yang S, Ren Q, Zhang S, Qin H, et al. Prediction for Mitosis-Karyorrhexis Index status of pediatric neuroblastoma via machine learning based 18F-FDG PET/CT radiomics. Diagnostics (Basel) 2022;12:262. doi: 10.3390/diagnostics12020262. [DOI] [PMC free article] [PubMed] [Google Scholar]