Abstract
Myofascial pain (MFP) is characterized by localized pain in the maxillofacial region attributed to the presence of hypersensitive spots known as trigger points (TrPs). This condition is particularly prevalent in the maxillofacial area, warranting a comprehensive examination of evidence-based management techniques. This review aims to equip healthcare professionals with a more profound insight into evidence-based MFP management techniques, facilitating improved patient care and treatment outcomes. In this review, we conducted a thorough literature search using Google Scholar, Scopus, Web of Science (WOS), and MEDLINE, with the keywords "Myofascial pain syndrome," "Pain," and "Orofacial pain." Articles were selected based on their relevance to the study's objective.
Pharmacological interventions, such as analgesics and muscle relaxants, are frequently prescribed. Additionally, a range of non-pharmacological modalities, including transcutaneous electrical nerve stimulation (TENS), ultrasound therapy, topical applications, dry needling, TrP injections, oral myofunctional therapy, and stretching exercises, have demonstrated efficacy in MFP management. The authors hope to give clinicians a more thorough understanding of the therapies for MFP by conducting a rigorous evidence-based evaluation of pharmacologic and non-pharmacological treatments. Our findings support the use of a combined approach that integrates both pharmacological and non-pharmacological strategies for the holistic management of TrPs.
Keywords: myofascial pain, evidence-based treatment, temporomandibular disorders, trigger points, physical therapy
Introduction and background
Myofascial pain (MFP) is a complex condition characterized by localized muscle pain attributed to the presence of tender trigger points (TrPs) within the musculature [1]. These trigger points, or TrPs, represent a focal area of hypersensitivity within a muscle, and they play a pivotal role in the manifestation of MFP. While the clinical diagnosis of MFP primarily relies on the recognition of motor and sensory features, it is important to note that not all these symptoms need to be concurrently present for a diagnosis [2,3]. Furthermore, TrPs may exhibit autonomic characteristics, but these features are not imperative for clinical identification. Instead, the presence of taut bands within a muscle stands as a fundamental hallmark distinguishing a TrP from general muscle tenderness [4].
The development of TrPs is understood through two key concepts. Firstly, some factors directly traumatize a muscle, either through direct injury or recurrent micro traumas stemming from habits that generate tension within the muscle [5]. Common examples encompass poor postural habits and parafunctional oral habits, with poor posture representing a frequent contributor. Secondly, some factors weaken and predispose a muscle to the formation of TrPs. Such factors may include nutritional imbalances, structural disharmony, insufficient exercise, sleep disturbances, or underlying joint disorders. The intricate clinical features of MFP can make diagnosis challenging [2]. To suspect an MFP diagnosis, healthcare practitioners must adeptly discern pain descriptors, associated symptoms, and potential modifying factors. Upon suspecting MFP, practitioners rely on their knowledge and palpation skills to locate and assess possible TrPs. The gold standard for detecting taut bands in muscles with TrPs is palpation, which requires practitioners to undergo training and develop precise skills for accurate identification of these tense areas [6].
Notably, the prevalence of TrPs is high within the maxillofacial region, and symptoms of MFP in this area are predominantly associated with muscles such as the masseter, temporalis, and medial pterygoid. Importantly, the existence of MFP transcends age, with peak incidence observed between 40 and 50 years of age, and it displays a higher occurrence among women [7].
In this article, we take a deep dive into the multifaceted realm of MFP, with a keen focus on exploring the nuanced strategies for treating TrPs in the maxillofacial region. By thoroughly reviewing the most recent and relevant literature, our primary objective is to equip clinicians with a thorough, contemporary, and evidence-based understanding, thereby empowering them to effectively manage MFP in their practice. The research question was: "What are the evidence-based management techniques for MFP?
Review
Methods
Search Strategy
In this review, we conducted a thorough literature search using Google Scholar, Scopus, Web of Science (WOS), and MEDLINE, with the keywords "myofascial pain syndrome," "pain," “trigger points," "tender trigger points,” and "orofacial pain." Articles were selected based on their relevance to the study's objective. The following search strategy was used: ("Myofascial Pain Syndrome") AND ("Pain" OR "Discomfort" OR "Ache" OR "Soreness") AND ("Trigger Points" OR "Tender Points") AND ("Orofacial Pain")
Inclusion/Exclusion Criteria
Studies that were published in English and used non-invasive treatment approaches including pharmacological and non-pharmacological intervention were included in the current review. Studies not published in the English language with insufficient information regarding treatment interventions or outcomes were excluded.
Literature Search
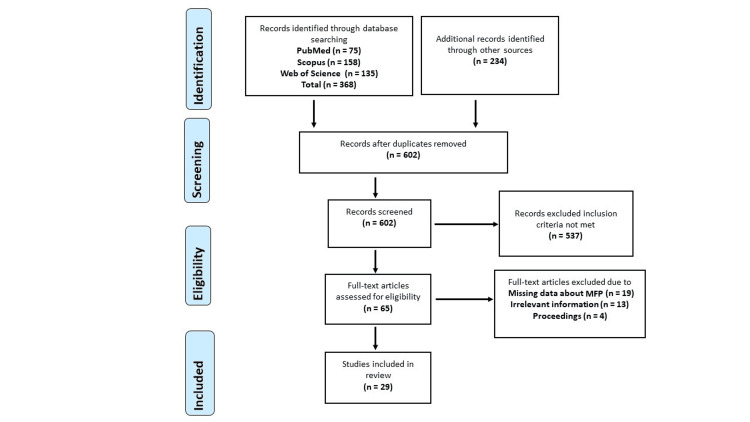
A comprehensive search yielded 602 studies from databases such as Scopus (158), Web of Science (135), and PubMed (75). Furthermore, 234 additional reports were discovered through supplementary sources, including Google Scholar and ResearchGate, and by examining the reference lists of the initially sourced articles. Following a rigorous screening process, 537 studies were excluded due to not meeting the inclusion criteria, including 19 studies with insufficient data about MFP, 13 studies that were considered irrelevant, and four studies that were conference proceedings. Ultimately, the review incorporated 29 studies (12 pharmacological interventions and 17 non-pharmacological interventions) that met the specified criteria (Figure 1).
Figure 1. Flowchart showing the selection process of the studies.
WOS: Web of Science; MFP: myofascial pain
Pharmacological interventions
Analgesics
Non-steroidal anti-inflammatory drugs (NSAIDs) are highly effective in managing mild to severe inflammatory pain. They work by inhibiting the activity of cyclooxygenase (COX), which subsequently reduces the production of prostaglandins, thromboxane, and prostacyclin. This makes NSAIDs a valuable choice for treating various inflammatory conditions which are also proven for the management of acute musculoskeletal disorders [8].
Comparatively, opioid analgesics have shown similar effectiveness in addressing inflammatory pain when compared to NSAIDs [9]. Codeine is one of the most commonly prescribed opioid analgesics. However, opioids are not as frequently used as NSAIDs due to their propensity to cause a wide range of adverse effects and the risk of dependence and addiction associated with long-term use [10].
In cases where NSAIDs alone prove insufficient, or when prolonged usage is required for managing moderate to severe pain, a combination approach can be employed. This involves combining an opioid analgesic or a steroid with an NSAID. This combination therapy can provide enhanced pain relief while potentially mitigating some of the side effects associated with individual opioid use [8].
Muscle Relaxants
Tizanidine, a centrally acting alpha2 agonist, offers a valuable therapeutic option for alleviating spasticity. Its mode of action involves enhancing pre-synaptic inhibition of motor neurons, operating within both the brain and the spinal cord [11]. In a clinical treatment study, patients experiencing acute painful muscle spasms found relief with a regimen of 2 mg of tizanidine hydrochloride three times a day. This treatment resulted in a significant reduction in the frequency and intensity of painful muscle spasms [12]. The extensive research conducted by Hutchinson et al., involving 2251 participants from around the world, demonstrated the effectiveness of tizanidine hydrochloride in managing painful muscular spasms. A remarkable 89 percent of the patients in this global study reported positive outcomes, affirming the therapeutic value of tizanidine in the treatment of painful muscle spasms [12].
Antidepressants
Tricyclic antidepressants represent a class of medications known for their multifaceted therapeutic effects, including anti-inflammatory, anti-fibromyalgia, and anti-neuropathic pain properties [13]. Despite their wide use, there has been limited research focused specifically on their effectiveness in treating MFP. One study delved into the therapeutic potential of amitriptyline in managing chronic tension headaches, aiming to elucidate its mechanism of action. In this crossover research, amitriptyline demonstrated its therapeutic significance by yielding statistically significant results. It notably reduced pain (p = 0.01) and markedly alleviated headache severity when compared to a placebo [14]. Similarly, another investigation explored the use of amitriptyline in the context of chronic temporomandibular pain. After a six-week treatment period, all pain levels saw statistically significant reductions [15]. While there is currently no concrete evidence supporting the use of these therapies for MFP management, a growing body of research suggests their effectiveness in the realm of chronic pain syndromes, particularly when conventional treatments fall short [16].
Botulinum Toxin
Botulinum injections offer a multifaceted approach to relieving discomfort. They work by promoting increased blood flow to affected muscles, thus aiding in the release of nerve fibers that may have been compressed due to abnormal muscle contractions. This dual action contributes significantly to pain alleviation [17]. Moreover, botulinum injections exert immediate effects. This can be attributed to various mechanisms at play. Firstly, these injections lead to the direct release of endogenous endorphins, the body's natural pain-relieving substances. Additionally, they induce changes in the central neurotransmitter balance, primarily through the local inhibition of pain peptides originating from sensory ganglions and nerve terminals. Furthermore, botulinum injections exhibit anti-inflammatory properties, and they counteract the actions of glutamate, an excitatory neurotransmitter, which can further contribute to their pain relief effects [18].
Local Anesthetic
Lidocaine functions as a non-specific sodium channel blocker, which, in turn, stabilizes neuronal cell membranes, thereby hampering the initiation and transmission of nerve impulses. However, it is important to be aware of potential side effects associated with lidocaine injections, including anaphylaxis, central nervous system depression, epilepsy, and arrhythmia [19]. In a study conducted by Affaitati et al., the efficacy of a lidocaine injection was compared to that of a lidocaine patch in addressing MFP. Surprisingly, both methods proved equally successful in reducing pain [20]. However, it was noted that patients reported a lower level of treatment unpleasantness when utilizing the lidocaine patch. This finding sheds light on the overall patient experience and preferences regarding these pain management approaches [21].
Non-pharmacological interventions
Behavioral Therapy
Behavioral therapy serves as a valuable conservative approach in the management of temporomandibular disorders (TMDs). These disorders are characterized by a complex interplay of factors, where psychological elements and parafunctional hyperactivity play pivotal roles in their pathophysiology. It is increasingly evident that mood changes have a significant influence on pain threshold levels in individuals, contributing to the intricate connection between pain responses and psychological factors [22].
The relationship between psychological factors and pain responses in TMDs is multifaceted and often challenging to decipher. Experimental studies have underscored the importance of mood alterations in shaping an individual's experience of pain. However, the precise mechanisms and interactions involved in this complex relationship continue to be a subject of ongoing research.
Emerging evidence suggests that a comprehensive approach, addressing both psychological and dental factors, yields superior outcomes in the management of TMDs. This holistic strategy incorporates interventions such as intraoral appliances, biofeedback training, and stress reduction techniques. Remarkably, studies indicate that the combined management of these factors surpasses the results obtained by addressing either intraoral appliances or stress management in isolation [23].
Dry Needling
TrP dry needling is a therapeutic technique where an acupuncture-like needle is precisely inserted into the skin and muscle at the site of TrPs. These needles are removed once the TrPs have been successfully inactivated [24]. Typically, stretching exercises complement the dry-needling process.
This method often induces a localized twitch response, disrupting the activity of the motor end-plate, which, in turn, creates an analgesic (pain-relieving) effect. Additionally, the tight bands of actin-myosin linkages within the muscle tend to release due to the localized twitch response and the subsequent incorporation of stretching exercises [25]. The dry needling is equally effective compared to TrP injections, establishing its eligibility as a primary treatment for acute cases [2].
It is noteworthy that, in two separate trials, both lidocaine and botulinum toxin injections demonstrated more effective pain reduction when compared to dry needling. These findings underscore the potential advantages of alternative treatments in managing pain associated with TrPs [25].
Injection Therapy and Electro Manual Therapeutic Approaches
In the management of MFP, TrPs within taut muscle bands are typically addressed through a combination of injection therapy and physical interventions [19]. Traditional treatment modalities encompass a spectrum of approaches, which include manual therapies, electrical stimulation, heat and cold applications, local anesthetics, and needle injections.
Manual therapies often involve techniques such as stretching, massage, ischemic compression, and myofascial release. These methods are aimed at alleviating muscular tension and discomfort associated with TrPs. Among these approaches, "spray and stretch" is a commonly used technique for managing TrPs due to its effectiveness in providing immediate pain relief [19,21]. The spray and stretch approach requires the passive extension of contracted muscles with the simultaneous application of vapocoolant such as dichlorodifluoromethane-trichloromonofluoromethane or ethyl chloride [26]. Pain relief with therapeutic ultrasound is linked to the uptake of pain mediators by increased blood circulation, alteration in nerve conduction, or changes in cell membrane permeability that reduce inflammation [27].
Myofascial release, on the other hand, is a therapeutic method focused on repositioning surface tissues over underlying structures. The objective is to enhance mobility and mitigate the subcutaneous stiffness commonly seen in panniculosis. These diverse treatment options collectively offer a comprehensive strategy for addressing MFP by directly targeting the source of discomfort within the muscle tissue [28].
Transcutaneous Electric Nerve Stimulation (TENS)
TENS has been used successfully for the treatment of acute and chronic conditions of MFP. TENS relieves the pain by increasing the endogenous opiates in the circulation by its peripheral mechanism or central effects or autonomic response. It also increases blood circulation and oxygen supply eliminating toxic metabolic products. The TENS pain-relieving effect could be due to a peripheral mechanism or central actions that boost circulating endogenous opiates or regulate autonomic response [29]. Results were recorded by El Fatih et al. that the ultrasound group showed a higher success rate with pain improvement of 93.3 percent while the TENS showed only 53.3 percent success [30].
Oral Myofunctional Therapy
A variety of exercise regimens have been recommended for the treatment of TMDs. However, a specialized therapeutic approach aimed at restoring stomatognathic function, known as oral myofunctional therapy (OMT), has gained prominence. OMT primarily revolves around a series of carefully designed mouth exercises and interventions, offering a unique strategy for TMD management [21,31].
Notably, in a study conducted, individuals undergoing OMT experienced significant benefits. They reported a substantial reduction in pain sensitivity when the masticatory muscles were palpated. Additionally, measurements of mandibular range of motion displayed marked improvements. These findings underscore the potential efficacy of OMT in addressing TMD-related issues, suggesting that targeted exercises and therapies can contribute positively to the management of this condition [32].
The oral myofascial treatment encompasses the alleviation of pain and the relaxation of muscles in the jaw, shoulders, and neck, emphasizing the establishment of an appropriate resting posture for the mandible. The treatment involves promoting lubrication of the temporomandibular joint (TMJ) and ensuring controlled and symmetrical mobility of the mandible. Furthermore, it incorporates the application of both active and passive exercises aimed at enhancing mandibular mobility, including exercises for mouth opening and closing. Distinct exercises targeting mobility and isometric strength are applied individually for the tongue, lips, and cheeks. Isometric exercises for the tongue entail pressing the tip against a tongue depressor. Lip isometrics involve using tools like patakara or an oral rehabilitation device to train lip closure. Cheek isometrics consist of pressing palms into the cheeks while attempting to lift them upward [32].
Splint Therapy
The predominant approach to pain management for patients with TMD often involves the utilization of occlusal splints, either as a standalone treatment or in combination with other therapeutic interventions [33,34]. The choice of occlusal splints depends on the specific issue being addressed, as well as the individual needs of the patient. A dentist evaluates the condition and recommends the most appropriate type of splint for the situation. There are several types of occlusal splints: 1. Soft splints: Made from soft materials such as silicone or rubber and provide cushioning for the teeth and jaw, 2. Hard splints: Constructed from rigid materials like acrylic, 3. Dual laminate splints: Combines both soft and hard materials and provides comfort while maintaining durability, 4. Anterior Repositioning Splints (ARS): Designed to reposition the lower jaw (mandible) forward and used to alleviate symptoms of TMDs and certain types of jaw misalignment, 5. Flat Plane Splints: Have a flat surface that allows the teeth to contact evenly, 6. Stabilization splints:Aimed at stabilizing the jaw and reducing muscle hyperactivity, 7. Neuromuscular splints: Focus on achieving a balanced relationship between the muscles and the TMJ and designed to relax the jaw muscles and optimize jaw function, and 8. Michigan splints: Full-coverage splints that cover all the teeth in one arch and are often used for diagnostic purposes [33].
The precise mechanism underlying the action of occlusal splints remains a subject of ongoing investigation and has not been fully elucidated [35,36]. Numerous theories have been proposed in an attempt to shed light on how occlusal splints exert their effects. These theories encompass various mechanisms, including 1. Occlusal Condition Alteration: Some suggest that occlusal splints may work by modifying or enhancing the occlusal condition, potentially reducing the stress and strain on the TMJ and associated structures [37], 2. Peripheral Impulse Modification: Another theory postulates that occlusal splints could influence peripheral impulses, both motor and afferent, transmitted to the central nervous system, ultimately impacting pain perception [37], 3. Vertical dimension adjustment: Alterations in the vertical dimension, which can occur with occlusal splints, might contribute to changes in TMJ condylar position, potentially leading to symptom relief [37], 4. Enhanced cognitive awareness: It is also proposed that occlusal splints might improve cognitive awareness of jaw positioning and habits, leading to behavioral adjustments that mitigate TMD symptoms [38], 5. Placebo effect:The psychological component of relief should not be underestimated. For some patients, the use of occlusal splints may trigger a placebo effect, where the expectation of improvement itself leads to symptom alleviation [38], and 6. Regression to the Mean: In some cases, TMD symptoms may naturally fluctuate, and patients may seek treatment during a period of heightened discomfort. Subsequent improvement may be attributed to the natural regression of symptoms [38,39].
In summary, the precise workings of occlusal splints in TMD management remain a topic of ongoing exploration. It is likely that multiple factors, both physical and psychological, contribute to the relief experienced by patients using occlusal splints. As research continues, a clearer understanding of their mechanisms will likely emerge.
Low-Level Laser Therapy
Low-level laser therapy (LLLT), also known as cold laser therapy or photobiomodulation therapy, involves the use of low-intensity lasers or light-emitting diodes (LEDs) to stimulate cellular function and promote tissue healing. The results of a systematic review indicate that LLLT appears to be efficacious in alleviating pain among individuals with temporomandibular MFP, supported by evidence of moderate quality [40].
Findings
The included studies reported a range of pharmacological interventions, such as analgesics and muscle relaxants, as well as non-pharmacological modalities, including TENS, ultrasound therapy, topical applications, dry needling, TrP injections, oral myofunctional therapy, LLLT, and stretching exercises, are available (Table 1). We conducted a quality assessment of the included articles using the JBI criteria, and two authors independently evaluated each study. Studies with a JBI score ranging from 20 to 49% were classified as having a high risk of bias, those with scores between 50-79% were considered to have a moderate risk of bias, and those scoring 80-100% were categorized as having a low risk of bias (Table 1).
Table 1. Characteristics and quality assessment of included studies .
***low risk of bias
** moderate risk of bias
| Study | Design | Intervention | Outcome | Quality assessment |
| Cigerim, and Kaplan (2023) [8]. | Randomized, double-blind, controlled trial | Naproxen-codeine, naproxen, dexamethasone, and naproxen | Significant reduction in pain intensity in all three groups Both naproxen-codeine and naproxen-dexamethasone demonstrated efficacy in treating myofascial pain. | *** |
| Jayadev et al. (2014) [9]. | Observational study | Analgesics | High prevalence of antibiotic and non-narcotic analgesic prescription for pulpal and periapical pathologies | *** |
| Şermet et al. (2012) [10]. | Observational study | Non-steroidal anti-inflammatory drug (NSAID) | High prevalence of non-steroidal anti-inflammatory drug (NSAID) prescription for dental pain | ** |
| Annaswamy et al. (2011) [11]. | Review | Medications, topical agents, and modalities | Most interventions for myofascial pain lack adequate evidence, while certain medications, topical agents, and modalities show moderate to strong support. | N/A |
| Malanga et al. (2002) [12]. | Randomized, double-blind, controlled trial | Tizanidine | Tizanidine showed significant reduction in pain intensity and improvement in function in myofascial pain. | *** |
| Micó et al. (2006) [13]. | Review | antidepressants | Pain and depression share common biochemical mechanisms, implying that antidepressants possess a legitimate analgesic effect. | N/A |
| Bendtsen and Jensen (2000) [14]. | Randomized, controlled trial | Amitriptyline | Amitriptyline was effective in significant reduction in myofascial tenderness | ** |
| Plesh et al. (2000) [15]. | Case series | Amitriptyline | Amitriptyline Improved the pain and function in patients with temporomandibular disorders | ** |
| Desai et al. (2013) [16]. | Review | Physical therapy and self-care measures. | Myofascial pain can be effectively addressed through diverse treatments, encompassing medications, physical therapy, and self-care measures. | N/A |
| von Lindern et al. (2003) [17]. | Case series | Botulinum toxin | Botulinum toxin showed improvement in pain and function in patients with chronic facial pain associated with masticatory hyperactivity. | ** |
| Chaurand et al. (2017) [18]. | Randomized, controlled trial | Botulinum toxin | Botulinum toxin demonstrated effectiveness in reducing pain and enhancing jaw function in individuals with myofascial pain. | *** |
| Galasso et al. (2020) [21]. | Review | Lidocaine | The efficacy of a lidocaine injection and that of a lidocaine patch equally successful in reducing pain. | N/A |
| Bogart et al. (2007) [22]. | Randomized, controlled trial | Group cognitive behavior therapy | Significant reduction in pain intensity and improvement in function. | *** |
| Michelotti et al. (2004) [23]. | Randomized, controlled trial | Home physical therapy regimen | A home-based physical therapy routine proved more effective than sole patient education in alleviating pain and enhancing jaw function in individuals with myofascial jaw muscle pain. | ** |
| Kietrys et al. (2013) [25]. | Systematic review and meta-analysis | Dry needling | Dry needling is an effective treatment for upper-quarter myofascial pain. | *** |
| Koole et al. (2020) [26]. | Randomized, controlled trial | Spray and stretch technique | The spray and stretch technique resulted in a notable increase in maximal mouth opening, particularly in individuals with orofacial pain, and the effect was more pronounced in women than in men. | *** |
| Xia et al. (2017) [27]. | Systematic review and meta-analysis | Ultrasound therapy | Current evidence indicates a notable impact of ultrasound therapy on pain in patients with myofascial pain, although it does not appear to have a significant effect on range of motion. | *** |
| Werenski (2011) [28]. | Review | Myofascial release techniques | Myofascial release treatments, characterized by diverse applications, show notable effectiveness when addressing injuries related to myofascial tissue. The treatments vary in factors such as pressure, duration, motion, and tension, leading to varied results and outcomes. | N/A |
| Hou et al. (2002) [29]. | Randomized, controlled trial | Various physical therapeutic modalities: hot pack, transcutaneous electric nerve stimulation (TENS), stretch with spray. | Various physical therapeutic modalities, such as massage, stretching, and heat, prove effective in alleviating cervical myofascial pain and reducing sensitivity in trigger points and improvement in function. | *** |
| Rai, Ranjan, Misra, Panjwani (2016) [30]. | Randomized Controlled Trial (RCT) | Therapeutic ultrasound and transcutaneous electrical nerve stimulation | Therapeutic ultrasound and transcutaneous electrical nerve stimulation effective for myofascial pain management. | ** |
| Melis, Di Giosia , Zawawi (2022) [31]. | Systematic Review | Oral myofunctional therapy | Oral myofunctional therapy beneficial for treating temporomandibular disorders (TMD). | *** |
| de Felício, Melchior, da Silva (2010) [32]. | Randomized Controlled Trial (RCT) | Orofacial myofunctional therapy | Orofacial myofunctional therapy shows positive effects on temporomandibular disorders compared to control group | *** |
| Truelove, Huggins, Mancl, Dworkin (2006) [33]. | Randomized Controlled Trial (RCT) | Traditional, low-cost, and splint therapies | Traditional, low-cost, and splint therapies effective in randomized controlled trial for temporomandibular disorder. | *** |
| Wassell, Adams, Kelly (2006) [34]. | Randomized Controlled Trial (RCT) | Stabilizing splints in general dental practice | Stabilizing splints show positive outcomes in treating temporomandibular disorders over a one-year follow-up. | *** |
| Scopel, Alves da Costa, Urias (2005) [35]. | Observational study | Electromyographic study of Masseter and anterior temporalis muscles in extra-articular myogenous TMJ pain patients compared to asymptomatic and normal population | Electromyographic study reveals differences in masseter and anterior temporalis muscles in TMJ pain patients compared to asymptomatic individuals. | *** |
| Türp, Komine, Hugger (2004) [36]. | Systematic Review | Efficacy of stabilization splints for masticatory muscle pain | Stabilization splints efficacy examined through qualitative systematic review for managing masticatory muscle pain. | *** |
| Kreiner, Betancor, Clark (2001) [37]. | Review | Occlusal stabilization appliances | Evidence supports efficacy of occlusal stabilization appliances in the management of temporomandibular disorders. | *** |
| Alencar Jr, Becker (2009) [39]. | Double-blind controlled clinical trial | Evaluation of different occlusal splints and counseling in the management of myofascial pain dysfunction | The findings indicated that all three types of appliances (hard, soft, or non-occluding occlusal splints) paired with counseling demonstrated equal effectiveness in reducing both the Modified Symptom Severity Index (Mod-SSI) and tenderness to palpation. | *** |
| Munguia, Jang, Salem, Clark, Enciso (2018) [40]. | Systematic Review and Meta-analysis | Low-level laser therapy (LLLT) | The results of this systematic review indicate that Low-level laser therapy (LLLT) appears to be efficacious in alleviating pain among individuals with myofascial pain associated with temporomandibular disorders, supported by evidence of moderate quality. | .*** |
Limitations
It is important to recognize the limitations when interpreting the findings of this review. These limitations included the lack of a rigorous and systematic approach to study selection, data extraction, and analysis can lead to a less objective synthesis of evidence. A notable limitation in the existing literature is the lack of comprehensive comparisons regarding treatment duration between these modalities. Moreover, physical therapeutic modalities like TENS, ultrasound, spray, and stretch have also shown marked improvement in pain, but further research is required to establish evidence-based treatment.
Conclusions
MFP is due to TrPs in the muscles. Many treatment modalities are effective for the management of MFP. Mostly, patients are treated with analgesics and muscle relaxants that reduce the symptoms of MFP. Dry needling and TrP injections are the interventional treatment options; some studies also support such types of treatment. Our findings support the use of a combined approach that integrates both pharmacological and non-pharmacological strategies for the holistic management of TrPs. For acute cases, the effectiveness of analgesics, muscle relaxants, dry needling, and TENS has been demonstrated. Future robust research including a systematic review and metanalysis is required to establish an evidence-based management of MFP.
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Junaid Amin, Yasser Riaz Malik, Abdullah Faraj Alshammari, Sattam S. Alshammari, Salman Amin, Ammar Ahmed Siddiqui
Drafting of the manuscript: Junaid Amin, Yasser Riaz Malik, Abdullah Faraj Alshammari, Sattam S. Alshammari, Salman Amin, Ammar Ahmed Siddiqui
Critical review of the manuscript for important intellectual content: Junaid Amin, Yasser Riaz Malik, Abdullah Faraj Alshammari, Sattam S. Alshammari, Ammar Ahmed Siddiqui
Supervision: Junaid Amin, Salman Amin
References
- 1.A brief overview and update of myofascial pain syndrome and myofascial trigger points. Gerber NL, Sikdar S, Hammond J, Shah J. https://www.semanticscholar.org/paper/A-Brief-Overview-and-Update-of-Myofascial-Pain-and-Gerber-D./2ae6c11f83ebd22e36a0487e2286b36e1644861a J Spinal Res Found Spring. 2011;6:55–64. [Google Scholar]
- 2.Recent advances in diagnosis and management of myofascial pain syndrome: a narrative review. Jain S, Goyal RK, Ajmera P, Aggarwal G, Dhiman S. J Clin Diag Res. 2021;15:4–8. [Google Scholar]
- 3.Myofascial pain: diagnosis and management. Graff-Radford SB. Curr Pain Headache Rep. 2004;8:463–467. doi: 10.1007/s11916-004-0068-y. [DOI] [PubMed] [Google Scholar]
- 4.Classification, epidemiology, and natural history of myofascial pain syndrome. Gerwin RD. Curr Pain Headache Rep. 2001;5:412–420. doi: 10.1007/s11916-001-0052-8. [DOI] [PubMed] [Google Scholar]
- 5.Comparison of the effects of instrument assisted soft tissue mobilization and dry needling on active myofascial trigger points of upper trapezius muscle. Ahmadpour Emshi Z, Okhovatian F, Mohammadi Kojidi M, Akbarzadeh Baghban A, Azimi H. Med J Islam Repub Iran. 2021;35:59. doi: 10.47176/mjiri.35.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Fricton J R, Kroening R, Haley D, Siegert R. Oral Surg Oral Med Oral Pathol. 1985;60:615–623. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 7.Myofascial pain syndromes in the maxillofacial area: a common but underdiagnosed cause of head and neck pain. Manolopoulos L, Vlastarakos PV, Georgiou L, Giotakis I, Loizos A, Nikolopoulos TP. Int J Oral Maxillofac Surg. 2008;37:975–984. doi: 10.1016/j.ijom.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 8.Analgesic efficacy of naproxen-codeine, naproxen+dexamethasone, and naproxen on myofascial pain: a randomized double-blind controlled trial. Cigerim L, Kaplan V. Cranio. 2023;41:119–125. doi: 10.1080/08869634.2020.1824411. [DOI] [PubMed] [Google Scholar]
- 9.Knowledge and pattern of antibiotic and non narcotic analgesic prescription for pulpal and periapical pathologies-a survey among dentists. Jayadev M, Karunakar P, Vishwanath B, Chinmayi SS, Siddhartha P, Chaitanya B. J Clin Diagn Res. 2014;8:0–4. doi: 10.7860/JCDR/2014/9645.4536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Analgesic prescription pattern in the management of dental pain among dentists in İstanbul. Şermet S, Akgün MA, Şimşek Ş. https://openaccess.marmara.edu.tr/server/api/core/bitstreams/1d50e2d8-544b-484e-81a4-edc6062a4658/content Marmara Pharm J. 2012;16:41–47. [Google Scholar]
- 11.Emerging concepts in the treatment of myofascial pain: a review of medications, modalities, and needle-based interventions. Annaswamy TM, De Luigi AJ, O'Neill BJ, Keole N, Berbrayer D. PM R. 2011;3:940–961. doi: 10.1016/j.pmrj.2011.06.013. [DOI] [PubMed] [Google Scholar]
- 12.Tizanidine is effective in the treatment of myofascial pain syndrome. Malanga GA, Gwynn MW, Smith R, Miller D. https://pubmed.ncbi.nlm.nih.gov/16886022/ Pain Physician. 2002;5:422–432. [PubMed] [Google Scholar]
- 13.Antidepressants and pain. Micó JA, Ardid D, Berrocoso E, Eschalier A. Trends Pharmacol Sci. 2006;27:348–354. doi: 10.1016/j.tips.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Amitriptyline reduces myofascial tenderness in patients with chronic tension-type headache. Bendtsen L, Jensen R. Cephalalgia. 2000;20:603–610. doi: 10.1046/j.1468-2982.2000.00087.x. [DOI] [PubMed] [Google Scholar]
- 15.Amitriptyline treatment of chronic pain in patients with temporomandibular disorders. Plesh O, Curtis D, Levine J, McCall Jr WD. J Oral Rehabil. 2000;27:834–841. doi: 10.1046/j.1365-2842.2000.00572.x. [DOI] [PubMed] [Google Scholar]
- 16.Myofascial pain syndrome: a treatment review. Desai MJ, Saini V, Saini S. Pain Ther. 2013;2:21–36. doi: 10.1007/s40122-013-0006-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.A botulinum toxin in the treatment of chronic facial pain associated with masticatory hyperactivity’. von Lindern JJ, Niederhagen B, Bergé S, Appel T. J Maxillofac Oral Surg. 2003;61:774–778. doi: 10.1016/s0278-2391(03)00153-8. [DOI] [PubMed] [Google Scholar]
- 18.Efficacy of botulinum toxin therapy in treatment of myofascial pain. Chaurand J, Pacheco-Ruíz L, Orozco-Saldívar H, López-Valdés J. J Oral Sci. 2017;59:351–356. doi: 10.2334/josnusd.16-0614. [DOI] [PubMed] [Google Scholar]
- 19.Treatment and management of myofascial pain syndrome. Urits I, Charipova K, Gress K, et al. Best Pract Res Clin Anaesthesiol. 2020;34:427–448. doi: 10.1016/j.bpa.2020.08.003. [DOI] [PubMed] [Google Scholar]
- 20.A randomized, controlled study comparing a lidocaine patch, a placebo patch, and anesthetic injection for treatment of trigger points in patients with myofascial pain syndrome: evaluation of pain and somatic pain thresholds. Affaitati G, Fabrizio A, Savini A, et al. Clin Ther. 2009;31:705–720. doi: 10.1016/j.clinthera.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 21.A comprehensive review of the treatment and management of myofascial pain syndrome. Galasso A, Urits I, An D, et al. Curr Pain Headache Rep. 2020;24:43. doi: 10.1007/s11916-020-00877-5. [DOI] [PubMed] [Google Scholar]
- 22.Efficacy of group cognitive behavior therapy for the treatment of masticatory myofascial pain. Bogart RK, McDaniel RJ, Dunn WJ, Hunter C, Peterson AL, Wright EF. Mil Med. 2007;172:169–174. doi: 10.7205/milmed.172.2.169. [DOI] [PubMed] [Google Scholar]
- 23.The additional value of a home physical therapy regimen versus patient education only for the treatment of myofascial pain of the jaw muscles: short-term results of a randomized clinical trial. Michelotti A, Steenks MH, Farella M, Parisini F, Cimino R, Martina R. https://pubmed.ncbi.nlm.nih.gov/15250431/ J Orofac Pain. 2004;18:114–125. [PubMed] [Google Scholar]
- 24.Trigger point dry needling. Dommerholt J, del Moral OM, Gröbli C. J Man Manip Ther. 2006;14:70–87. [Google Scholar]
- 25.Effectiveness of dry needling for upper-quarter myofascial pain: a systematic review and meta-analysis. Kietrys DM, Palombaro KM, Azzaretto E, Hubler R, Schaller B, Schlussel JM, Tucker M. J Orthop Sports Phys Ther. 2013;43:620–634. doi: 10.2519/jospt.2013.4668. [DOI] [PubMed] [Google Scholar]
- 26.Spray and stretch technique and its effects on mouth opening. Koole P, Zonnenberg AJ, Koole R. J Prosthet Dent. 2020;123:455–460. doi: 10.1016/j.prosdent.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 27.Effectiveness of ultrasound therapy for myofascial pain syndrome: a systematic review and meta-analysis. Xia P, Wang X, Lin Q, Cheng K, Li X. J Pain Res. 2017;10:545–555. doi: 10.2147/JPR.S131482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The effectiveness of myofascial release techniques in the treatment of myofascial pain: a literature review. Werenski J. https://www.logan.edu/mm/files/LRC/Senior-Research/2011-Aug-34.pdf Logan University. 2011;32:440–450. [Google Scholar]
- 29.Immediate effects of various physical therapeutic modalities on cervical myofascial pain and trigger-point sensitivity. Hou CR, Tsai LC, Cheng KF, Chung KC, Hong CZ. Arch Phys Med Rehabil. 2002;83:1406–1414. doi: 10.1053/apmr.2002.34834. [DOI] [PubMed] [Google Scholar]
- 30.Management of myofascial pain by therapeutic ultrasound and transcutaneous electrical nerve stimulation: a comparative study. Rai S, Ranjan V, Misra D, Panjwani S. Eur J Dent. 2016;10:46–53. doi: 10.4103/1305-7456.175680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oral myofunctional therapy for the treatment of temporomandibular disorders: a systematic review. Melis M, Di Giosia M, Zawawi KH. Cranio. 2022;40:41–47. doi: 10.1080/08869634.2019.1668996. [DOI] [PubMed] [Google Scholar]
- 32.Effects of orofacial myofunctional therapy on temporomandibular disorders. de Felício CM, de Oliveira MM, da Silva MA. Cranio. 2010;28:249–259. doi: 10.1179/crn.2010.033. [DOI] [PubMed] [Google Scholar]
- 33.The efficacy of traditional, low-cost and nonsplint therapies for temporomandibular disorder: a randomized controlled trial. Truelove E, Huggins KH, Mancl L, Dworkin SF. J Am Dent Assoc. 2006;137:1099–1107. doi: 10.14219/jada.archive.2006.0348. [DOI] [PubMed] [Google Scholar]
- 34.The treatment of temporomandibular disorders with stabilizing splints in general dental practice: one-year follow-up. Wassell RW, Adams N, Kelly PJ. J Am Dent Assoc. 2006;137:1089–1098. doi: 10.14219/jada.archive.2006.0347. [DOI] [PubMed] [Google Scholar]
- 35.An electromyographic study of masseter and anterior temporalis muscles in extra-articular myogenous TMJ pain patients compared to an asymptomatic and normal population. Scopel V, Alves da Costa GS, Urias D. Cranio. 2005;23:194–203. doi: 10.1179/crn.2005.028. [DOI] [PubMed] [Google Scholar]
- 36.Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Türp JC, Komine F, Hugger A. Clin Oral Investig. 2004;8:179–195. doi: 10.1007/s00784-004-0265-4. [DOI] [PubMed] [Google Scholar]
- 37.Occlusal stabilization appliances. Evidence of their efficacy. Kreiner M, Betancor E, Clark GT. J Am Dent Assoc. 2001;132:770–777. doi: 10.14219/jada.archive.2001.0274. [DOI] [PubMed] [Google Scholar]
- 38.Okeson JP. Elsevier Health Sciences. St Louis: Elsevier Health Sciences; 2019. Management of Temporomandibular Disorders and Occlusion. [Google Scholar]
- 39.Evaluation of different occlusal splints and counselling in the management of myofascial pain dysfunction. Alencar F Jr, Becker A. J Oral Rehabil. 2009;36:79–85. doi: 10.1111/j.1365-2842.2008.01913.x. [DOI] [PubMed] [Google Scholar]
- 40.Efficacy of low-level laser therapy in the treatment of temporomandibular myofascial pain: a systematic review and meta-analysis. Munguia FM, Jang J, Salem M, Clark GT, Enciso R. J Oral Facial Pain Headache. 2018;32:287–297. doi: 10.11607/ofph.2032. [DOI] [PubMed] [Google Scholar]