Abstract
PURPOSE
Portal hypertension (PHT) and its sequelae are the most clinically important manifestations in cystic fibrosis-related liver disease (CFLD). This paper aimed to evaluate the safety and efficacy of a pre-emptive transjugular intrahepatic portosystemic shunt (TIPS) to prevent PHT-related complications in pediatric patients with CFLD.
METHODS
This was a prospective single-arm study on pediatric patients with CFLD, signs of PHT, and preserved liver function who underwent a pre-emptive TIPS in a single tertiary CF center between 2007 and 2012. The long-term safety and clinical efficacy were assessed.
RESULTS
A pre-emptive TIPS was performed on seven patients with a mean age of 9.2 years (± standard deviation: 2.2). The procedure was technically successful in all patients, with an estimated median primary patency of 10.7 years [interquartile range (IQR) 0.5–10.7)]. No variceal bleeding was observed during the median follow-up of 9 years (IQR 8.1–12.9). In two patients with advanced PHT and rapidly progressive liver disease, severe thrombocytopenia could not be stopped. Subsequent liver transplantation revealed biliary cirrhosis in both patients. In the remaining patients with early PHT and milder porto-sinusoidal vascular disease, symptomatic hypersplenism did not occur, and liver function remained stable until the end of the follow-up. Inclusion for pre-emptive TIPS was discontinued in 2013 following an episode of severe hepatic encephalopathy.
CONCLUSION
TIPS is a feasible treatment with encouraging long-term primary patency to avoid variceal bleeding in selected patients with CF and PHT. However, as the progression of liver fibrosis, thrombocytopenia, and splenomegaly is inevitable, the clinical benefits due to pre-emptive placement appear to be minor.
Keywords: Cystic fibrosis, liver diseases, portal hypertension, children, transjugular intrahepatic portosystemic shunt, primary prophylaxis, variceal bleeding, hypersplenism
Main points
• A transjugular intrahepatic portosystemic shunt (TIPS) in pediatric cystic fibrosis-related liver disease (CFLD) is technically feasible, but there is an inherent risk of hepatic encephalopathy, especially alongside a high protein intake.
• In the long term, pre-emptive TIPS protects pediatric patients with CFLD from complications related to non-cirrhotic portal hypertension.
• Long-term TIPS patency in pediatric CFLD is encouraging and comparable with that in adult non-CF.
• Obliterative portal venopathy was the most prominent histological feature on biopsy and supports, at least partially, vascular disease in CFLD.
Cystic fibrosis (CF) is the most frequent autosomal recessive disorder in Caucasians and is caused by a mutation in the CF transmembrane conductance regulator gene.1 Cystic fibrosis-associated liver disease (CFLD) is a well-known manifestation of CF and includes a wide range of hepatobiliary diseases.2 Generally, CFLD remains subclinical, but 5% to 10% of patients will develop cirrhosis or portal hypertension (PHT).2,3 As liver failure is rather exceptional, the clinical outcome is determined mainly by PHT.4,5,6,7 Variceal bleeding is the most feared complication. While its prevalence is under debate, the physical and psychological impacts of a severe bleeding episode cannot be underestimated.3,4,5,6,7
The pathophysiological mechanism of CFLD and PHT remains poorly understood. Besides the main manifestation of focal biliary fibrosis leading to multilobular cirrhosis, an alternative vascular mechanism with obliterative portal venopathy (OPV) has been attributed to non-cirrhotic PHT (NCPH).8,9,10,11,12 Therefore, since PHT can develop independently of cirrhosis, it should be evaluated carefully.12 In NCPH, the hepatic venous pressure gradient does not represent the actual degree of PTH, and other non-invasive markers are required.8,12,13 An ultrasound (US) is a key examination for the predication and evaluation of PHT.12,13,14,15,16,17,18
Currently, treatment in CFLD focuses on screening and managing the complications of PHT and optimizing the nutritional status of the patient.19 In the absence of large prospective studies, there remains much ambiguity on the actual benefits, timing, and indications of different therapeutic interventions for PHT.20 Endoscopic treatment is recommended for acute variceal bleeding but not for primary prevention in children.5,19,21,22 Nevertheless, primary prophylaxis by endoscopy is often pursued in children with a high risk of bleeding.2,23 However, the risks of repeated general anesthesia for the complete endoscopic eradication of varices should be considered in CF. In addition, it does not treat underlying PHT and other complications. Non-selective ß-blockers are not endorsed because of poor tolerance and bronchoconstriction in CFLD.2,19 Liver transplantation (LT) is an effective therapeutic option in CFLD with end-stage liver failure and treatment-resistant and complicated PHT.5,20 However, because of the involvement of multiple organs in CF, the decisions for transplant listing, graft selection, and timing are challenging.20
A transjugular intrahepatic portosystemic shunt (TIPS) is a well-established procedure for portal vein decompression in adults.24 In children with severe CFLD cirrhosis, TIPS has been proven as a feasible option in acute or refractory variceal bleeding or as a bridge to LT.6,25,26,27 However, as liver function may never deteriorate in CFLD with NCPH, portosystemic shunting to alleviate PHT might be preferable over LT.8 Currently, little data are available on the long-term outcome of interventional TIPS or surgical (distal splenorenal or portocaval) shunts to mitigate PHT.19 The purpose of this prospective study was to evaluate early portal decompression with a TIPS as a safe and effective strategy to prevent PHT-related complications in the long term.
Methods
Study design and participants
This was a prospective single-arm study on pediatric patients with CFLD who underwent pre-emptive TIPS placement in a single CF center between January 2007 and December 2012. According to the trial protocol (Supplementary Figure 1) and following a multidisciplinary discussion, patients with CFLD with preserved liver function but early signs of PHT (thrombocytopenia, splenomegaly, US liver score, flow reduction/reversal in portal vein or portosystemic collaterals on US) were eligible for a pre-emptive TIPS.15 In these selected patients, it was assumed that fibrosis would progress, and the development of complications related to PHT would be highly probable. Inclusion was discontinued in 2013 due to some reluctance against pre-emptive TIPS after an episode of severe hepatic encephalopathy (HE) in one of the enrolled patients. Patient data were longitudinally evaluated from the time of the TIPS procedure to death, LT, or loss of follow-up. All data were censored on Dec 31, 2020. Written informed consent was obtained from each patient or representative. The trial protocol was reviewed and approved by Ghent University Hospital’s Ethics Committee (EC UZG 2006/283, date: 03.15.2007). Prior to the enrolment of the first patient, the trial was registered with the National Trial Register (B67020071504).
Supplementary Figure 1.
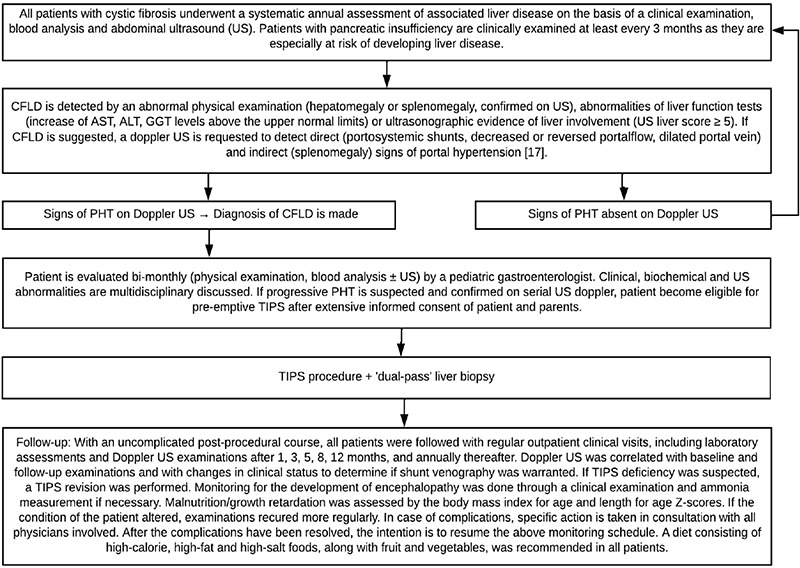
Pre-emptive TIPS protocol. TIPS, transjugular intrahepatic portosystemic shunt; CFLD, cystic fibrosis liver disease; US, ultrasound; AST, aspartate aminotransferase; ALT, alanine aminotransferase; GGT, gamma-glutamyl transferase; PHT, portal hypertension; PPG, portosystemic pressure gradient.
TIPS procedure
All procedures were performed under general anesthesia by an experienced interventional radiologist (L.D.). Depending on the patient’s age and physiognomy, a TIPS was created following a conventional transjugular technique for adults or by a dedicated combined percutaneous transhepatic–transjugular approach for small children.28 The principle of the latter technique is illustrated in Figure 1. Routinely, an expanded polytetrafluoroethylene (ePTFE)-covered endoprosthesis (Viatorr TIPS endoprosthesis, Gore) was used for shunt creation. If the sheath could not be negotiated into the main portal vein, a self-expandable non-covered stent (Wallstent, Boston Scientific) was placed. In all cases, stent dilatation was performed using an 8 mm angioplasty balloon. This was followed by direct portography and portosystemic pressure gradient (PPG) measurements. If the flow through the shunt was not sufficient, dilatation up to 10 mm was performed. We did not pursue a minimum gradient reduction. Prophylactic anticoagulant therapy after TIPS placement was not administered. Percutaneous “dual-pass” liver biopsy 18-Gauge Tru-Cut, throw length: 20 mm) was performed during the TIPS procedure. All patients were admitted to the pediatric intensive care unit following the TIPS procedure for overnight observation and then transferred to the pediatric floor. The follow-up data of these patients after discharge are shown in Supplementary Figure 1.
Figure 1.
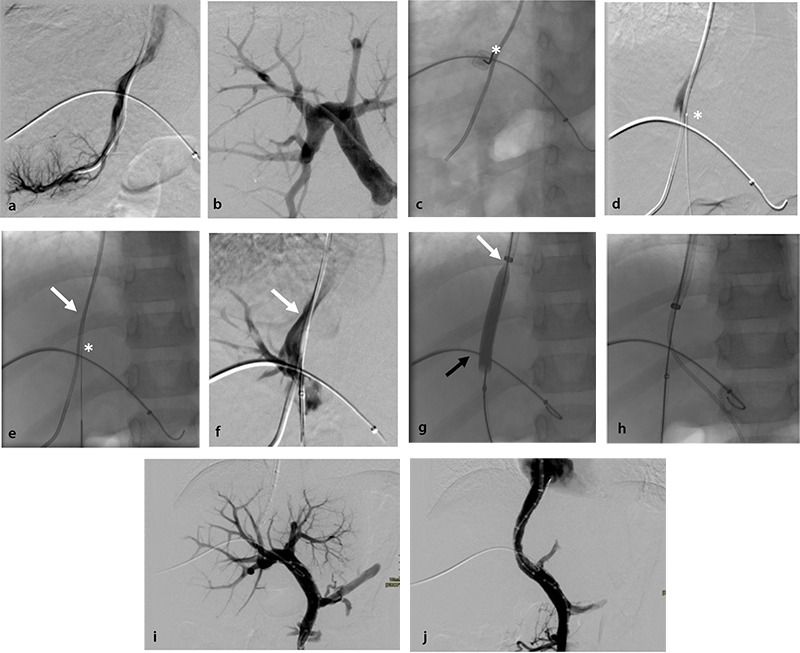
Modified percutaneous transhepatic–transjugular approach for small children. (a) Right transjugular vein access was used to advance a 10-F sheath (Flexor Check-flo II introducer set, Cook Medical) over a 5-F Headhunter-type catheter into the right hepatic vein. (b) Right-sided (midaxillary line) peripheral portal vein access was then obtained by percutaneous puncture, and a 5-F Cobra type was advanced through a 5-F introducer sheath into the main portal vein. (c) Subsequently, by inclining the X-ray tube, a favorable crossing of the catheters in the hepatic and portal vein was identified. From a ventral subcostal position, a third percutaneous puncture was performed using a long 21-gauge Chiba-type needle (white asterisk) directed perpendicular to the junction of the venous catheters, first perforating the portal vein and then entering the hepatic vein through the hepatic parenchyma. (d) The correct position of the needle (white asterisk) in the hepatic vein (white arrow) was confirmed by blood aspiration and a contrast medium injection performing digital subtraction angiography. (e) A 0.018 inch hydrophilic guidewire (Radifocus, Terumo) was introduced trough the needle (white asterisk) into the right hepatic vein (white arrow). (f) The correct passing of the portal vein was confirmed by withdrawing the needle into the portal vein (black arrow) and through a contrast medium injection via a hemostatic valve (AccessPLUS hemostasis valve, Merit Medical). In this case, it also demonstrated the hepatic vein (white arrow). Over the 0.018 inch guidewire connecting the hepatic and portal veins, a 6-F coaxial access set (AccuStick II Introducer System, Boston Scientific) was advanced transhepatic into the hepatic vein. The small guidewire was then exchanged for a 300 cm long 0.035 inch stiff hydrophilic guidewire (Radiofocus Glidewire Advantage, Terumo), which was pushed upstream to the caval vein. (g) This guidewire was captured transjugular with a 25 mm snare (Amplatz GooseNeck Snare Kit, Covidien) (black asterisk) and used to guide the 6 mm balloon angioplasty of the parenchymal tract between the hepatic (white arrow) and portal vein (black arrow). (h) Subsequently, the transjugular sheath could be pushed towards the portal vein, and a 5-F Cobra-type catheter was introduced aside the safety guidewire into the portal vein. Through this catheter, a super-stiff guidewire (SupraCore, Abbott) was advanced in the splenic or mesenteric vein. (i) Direct portography was performed via a 5-F calibrated pigtail catheter to select the appropriate length for the endoprosthesis, followed by the measurement of the transhepatic portosystemic pressure gradient. Then, following the 8 mm balloon angioplasty of the parenchymal tract, the transjugular sheath was pushed into the main portal vein and the safety guidewire removed. From here, the procedure followed the same technique as for adults. (j) Final direct photography after transjugular intrahepatic portosystemic shunt placement. The percutaneous intrahepatic parenchymal tracts were closed using acrylic glue (Glubran2, GEM or Histoacryl, Braun) and diluted (1:2) with an oily contrast agent (Lipiodol UF, Guerbet).
Outcome and definitions
The primary and secondary outcomes for efficacy were the prevention of variceal bleeding and the prevention of symptomatic hypersplenism (severe thrombocytopenia and/or splenomegaly requiring additional intervention/surgery), respectively, during the follow-up period. Thrombocytopenia was defined as a platelet count (PLT) of <150.000/μL, with a severe sub-definition of <50.000/μL. The spleen length for the age Z score was used to monitor the evolution of splenomegaly,29 and the body-mass-index for-age and height-for-age Z scores were used to monitor growth and nutritional status.30
Safety was assessed according to immediate and late complications. Immediate complications were recorded in the 30-day post-procedural time frame.31 Late complications of TIPS placement, including the incidence of HE and the number of shunt revisions required, were monitored and recorded during the follow-up. Primary TIPS patency was defined as patency without shunt dysfunction requiring revision. Secondary patency was defined as restored full patency after shunt revision.
Following the new insights into NCPH, all liver biopsy samples were retrospectively re-analyzed by a hepatopathologist.32 For fibrosis scoring, the METAVIR scoring system was used (F0: no fibrosis, F4: cirrhosis).33
Statistical analysis
The Shapiro–Wilk normality test was used to examine the normal distribution of variables. Data were expressed as the median with an interquartile range (IQR) if non-normally distributed and as the mean ± standard deviation (SD) if normally distributed. A paired dot plot and the Wilcoxon signed-rank test were used to compare the paired pre-TIPS and end follow-up measurements. A Kaplan–Meier plot was created to describe the primary and secondary TIPS patency. All analyses were performed using SPSS software version 27 and RStudio 4.0.2., with P <0.05 considered significant.
Results
Patient selection
Seven children (five males and two females) with CFLD underwent a pre-emptive TIPS. The included patients had a mean age of 9.2 years (± SD 2.2) and a mean weight of 27.3 kg (± SD 6.9) (Table 1). They all exhibited signs of liver fibrosis on US, with a median US liver score of 7 (IQR 7–9).15 Clinical signs of PHT were hypersplenism (patients 1, 4, and 7) and splenomegaly without thrombocytopenia (patients 2 and 6). In patient 5, a progressive decline in PLT prompted a pre-emptive TIPS before reaching the threshold of thrombocytopenia. In patient 3, a pre-emptive TIPS was performed due to hepatomegaly and early signs of PHT on US. None had a variceal bleeding episode before TIPS treatment.
Table 1. Individual baseline characteristics at the time of the TIPS procedure.
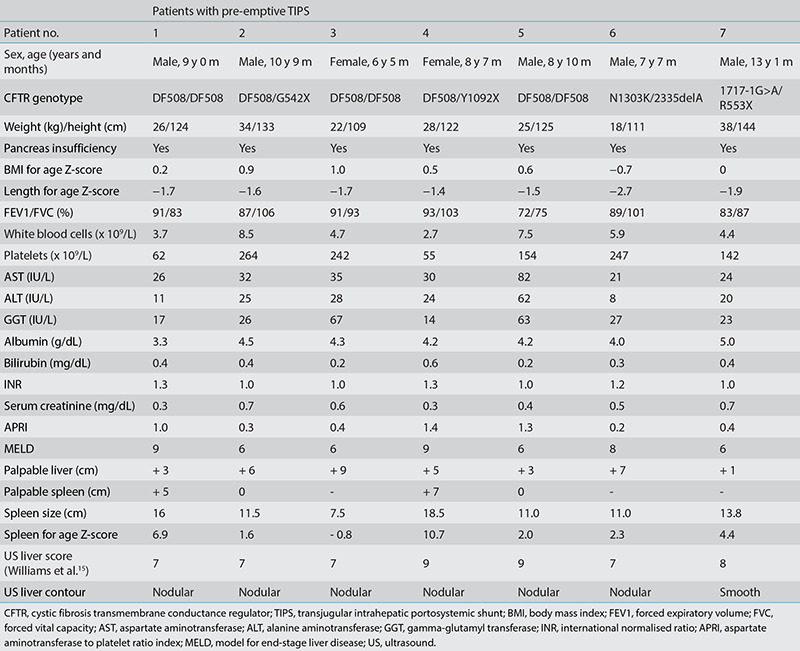
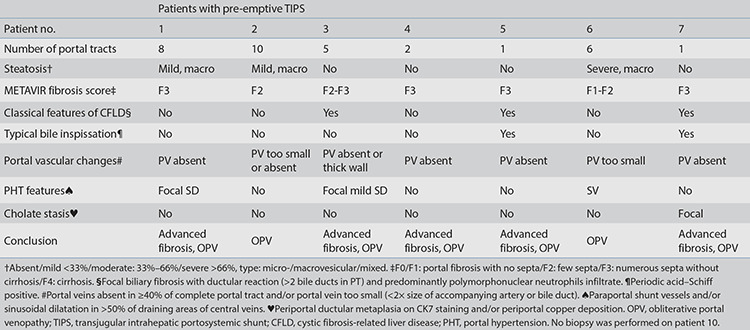
During the TIPS, direct PPG measurements confirmed the presence of early PHT (PPG 6–10 mmHg) in five patients, with patients 1 and 4 unexpectedly having more severe PHT (17 mmHg). Some esophageal collaterals were seen (patients 1, 4, 6, and 7) during direct portal vein phlebography. Histopathological evidence of liver fibrosis was confirmed via biopsy in all patients, ranging from F1–F3 (Table 2). All had features suggestive of OPV, with different patterns, as illustrated in Supplementary Figure 2.
Table 2. Histopathological features on liver biopsy during the TIPS procedure.
Supplementary Figure 2.
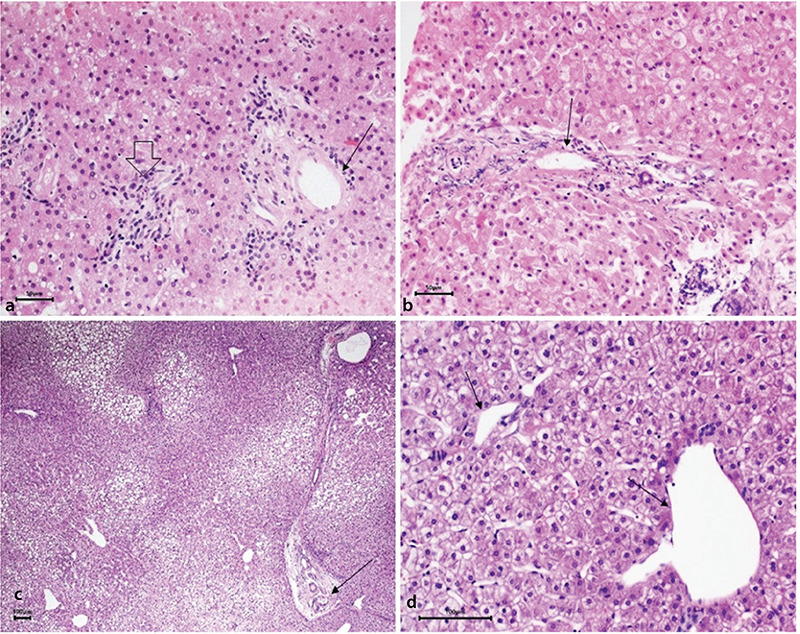
Obliterative portal venopathy. (a) Liver biopsy patient 4. Portal tract lacking a portal vein radicle (open arrow) next to a portal tract showing a portal vein radicle of reduced size (thin arrow). These two portal tracts are abnormally approximated to each other. (b) Liver biopsy patient 2. Portal tract showing a portal vein radicle of reduced size with a fibrous wall (arrow). (c) Liver biopsy patient 8. Thin fibrous septum connecting two portal tracts. The portal vein radicle shows a thick wall and a reduced size (arrow), while in other areas, the portal veins appear dilated. (d) Liver biopsy patient 8. Dilated portal veins herniating outside of the portal tracts in the periportal area indicating portal hypertension (arrows).
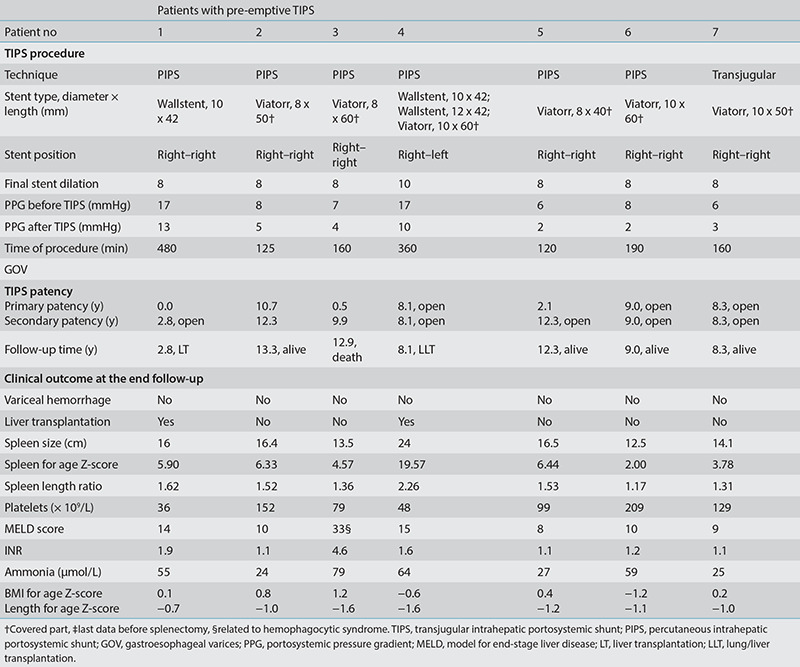
Technical and clinical outcomes (Table 3)
Table 3. Procedure details and outcome.
The pre-emptive TIPS procedure was technically successful in all patients, with no immediate post-procedural complications. An ePTFE-covered stent was placed in all patients except one. In patient 6, an uncovered stent was required because the 10-F sheath could not be passed into the main portal vein. All patients were discharged in a good condition after a hospitalization period of 2 to 5 days. Patient 1 suffered from intermittent hyperammonemia with doubtful neurological symptoms 19 days after the TIPS, which was treated medically without the recurrence of symptoms. Patient 6 was admitted because of rapid progressive HE, which evolved into a deep comatose state. This was related to a peptide-based drip-feed after receiving a gastrostomy because of poor nutritional intake 19 months after a TIPS. The patient was treated successfully with sodium benzoate. Then, lactulose and metronidazole were administered for 1 week per month, the drip feed was reduced and changed to a type with a lower protein load. Subsequently, the patient has been in a good condition for many years.
During the median follow-up of 9 years (IQR 8.1–12.9) after the TIPS, none of the patients had an episode of variceal bleeding. In patients 1 and 4 with advanced PHT and marked hypersplenism at a young age, PLT continued to decrease even after TIPS treatment, ultimately resulting in severe thrombocytopenia with bleeding diathesis. Both underwent an LT because of progressive liver insufficiency, which was 2.8 years (LT in patient 1) and 8.1 years (LT in patient 4) following TIPS treatment. The histology of the explant showed a biliary pattern of cirrhosis. In the remaining patients, three (3, 5, and 7) evolved to hypersplenism without the need for medical treatment. The PLT significantly decreased after TIPS, with an estimated median difference of 55.000/μL (P = 0.018, Wilcoxon signed-rank test), whereas the spleen length for the age Z score did not increase (Figure 2). Patient 3 died after 12.9 years because of a sudden severe hemophagocytic syndrome with secondary multiple organ failure, which was not related to CFLD. On the last annual assessment, this patient had a stable liver function (model for end-stage liver disease 8). In the remaining patients with early PHT, liver function remained stable, and LT could be avoided until the end of the follow-up. No patients developed ascites. Regarding growth, the height for the age Z score significantly increased after the TIPS, with an estimated median difference of 0.6 (P = 0.043, Wilcoxon signed-rank test).
Figure 2.
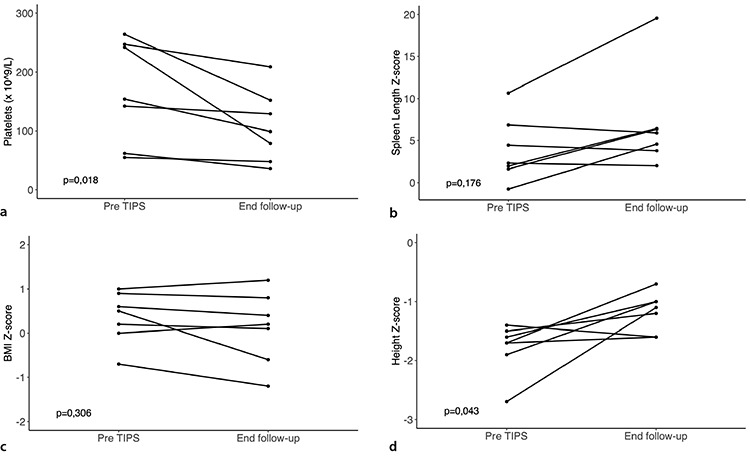
Individual evolution of hypersplenism, malnutrition, and growth. The paired dot plot and Wilcoxon signed-rank test for the paired results of (a) platelet count, (b) spleen length-for-age Z score, (c) body-mass-index (BMI)-for-age Z score, and (d) height-for-age Z score at the time of the transjugular intrahepatic portosystemic shunt (TIPS) procedure and at the end of the follow-up. A value of P < 0.05 was considered significant.
Four in seven patients required one or more revisions, resulting in an estimated median primary patency of 10.7 years (IQR 0.5–10.7) after TIPS treatment (Figure 3). The primary patency rates at 2, 4, and 6 years were 71.4%, 57.1%, and 57.1%, respectively. A total of 10 TIPS dysfunctions were detected by US, and the revisions revealed four stenoses and six occlusions. Patient 5 presented with progressive hypersplenism, despite no shunt deficiency on the duplex US. A subsequent 10 mm balloon angioplasty was performed with a PPG decrease from 5 to 4 mmHg. Except for patients 1 and 4, the PPG during the revision never exceeded the threshold of 10 mmHg. Patients 2 and 3 demonstrated a revision refractory occlusion of the TIPS after 12.3 and 9.9 years, respectively. In both patients, a new left–left TIPS was created to reduce the PPG (from 10 to 4 mmHg and from 9 to 5 mmHg, respectively). The first TIPS in five patients and the second TIPS in two patients were open at the end of the follow-up.
Figure 3.
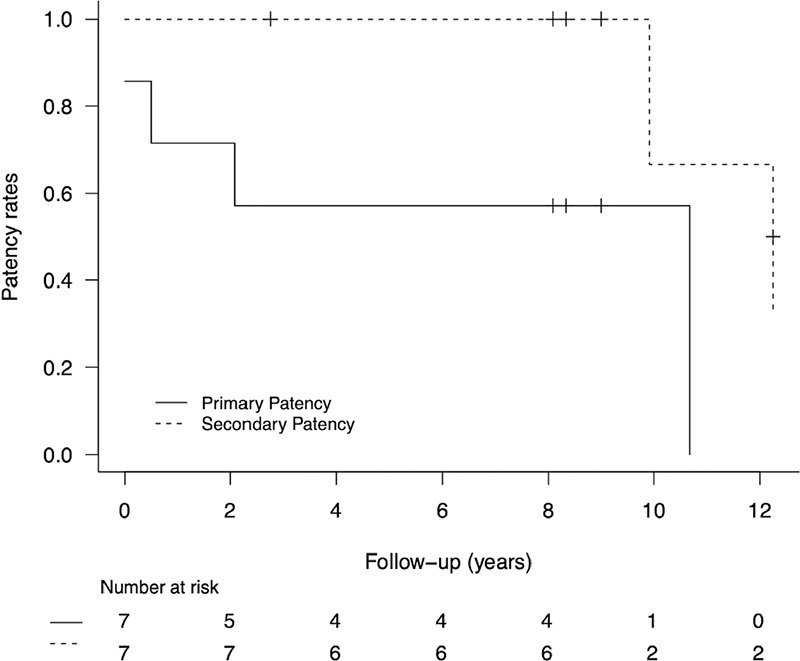
Primary and secondary patency of transjugular intrahepatic portosystemic shunt. Kaplan–Meier plot.
Discussion
The prospective selection of children for a pre-emptive TIPS was based on several non-invasive indicators. The intention was to include patients with early PHT, ideally before the onset of clinically significant PHT. However, two children with thrombocytopenia and marked splenomegaly showed post-hoc more severe PHT (PPG of 17 mmHg) on invasive pressure measurements during the TIPS procedure. In both, further deterioration of CFLD could not be prevented, and a hepatic decompensation developed, with a need for LT. A histopathological re-evaluation of the biopsy samples did not show any clear distinction between them and the other patients with early PHT. In all patients, OPV was the most prominent histopathological feature, supporting porto-sinusoidal vascular disease. Nevertheless, both patients with severe PHT showed advanced fibrosis (F3), which is indistinguishable from incomplete septal cirrhosis on a needle biopsy. Further, as CFLD is a highly heterogeneous disease, there is an inherent risk of a sampling error.13,26 Eventually, explant histology demonstrated a biliary pattern of cirrhosis in both patients. Consistent with previous assumptions, these patients likely suffered from an earlier and more severe phenotype of CFLD with extensive fibrosis (or cirrhosis), PHT, and liver failure, often requiring LT.11 The remaining patients may have had a milder phenotype with a slowly progressive NCPH, as indicated by the moderately elevated PPG throughout the follow-up.
This study confirms that a TIPS, even in small children with CF, is feasible and can be performed safely without major adverse events in the immediate post-procedural period. Portal vein access from a conventional jugular approach can be problematic due to the wider anatomical variations and geometrical incompatibilities in a small child’s liver. The use of a combined transjugular and transhepatic approach in the youngest children in our series enabled us to overcome this difficulty without complications related to the percutaneous technique. Nevertheless, although HE is of major concern after TIPS, it seems only to occur in patients with a high protein intake.5 Excessive shunting should be avoided by leaving a residual PPG of ≥3 mmHg. Furthermore, controlling the protein intake and monitoring ammonium levels are key points in the follow-up of patients with CFLD after shunt placement. Intermittent or chronic mild hyperammonemia could be observed in several patients after TIPS but without the manifestation of neurodegenerative complications or cognitive impairments in the long term.
Stent dysfunction in TIPS is a well-known long-term complication in adults. This study prospectively recorded 6-year primary and secondary patencies of 57% and 100%, respectively, which is in line with previous retrospective studies on pediatric PHT.26,34 Strict follow-ups with US are mandatory to detect early stent stenosis, allowing for an uncomplicated revision. Nevertheless, after almost 10 years, two patients eventually required a second TIPS because of stent occlusion, which was refractory to revision. Overall, the long-term permeability of a TIPS in children with CFLD appears comparable to the patency in adults.35
This study achieved its objective in terms of efficacy, as pre-emptive TIPS placement avoided variceal bleeding in pediatric patients with CFLD and PHT in the long term. Except in one patient, portal decompression after primary or revisional TIPS resulted in a PPG below 12 mmHg, which is a critical threshold for bleeding protection in adults and is likely in the pediatric population.36 Previous retrospective series indicated that a TIPS could improve hypersplenism in pediatric PHT.37,38 In the present trial, we observed a significant decrease in PLT, with failure to avert severe thrombocytopenia in both patients with more advanced PTH at the time of the TIPS. It appears that hypersplenism progresses over time, despite a functional TIPS and a low PPG (5 mmHg), not even exceeding the classical threshold of PHT in adults. As portosystemic collaterals/varices were also identified in patients with a PPG below 10 mmHg, the upper limit of normal for the PPG might be lower in these pediatric patients.39 Although liver fibrosis and the slow progression of PHT appeared inevitable in the present trial, a comparative case series indicated that a surgical distal splenorenal shunt (DSRS) could improve hypersplenism in CFLD.38 This is presumably related to more effective decompression of the spleen. Moreover, while a pre-emptive TIPS prevented variceal bleeding during double the follow-up time, no episodes of HE occurred after DSRS.40
The use of TIPS may be an interesting therapeutic strategy in a pre-emptive stage of NCPH, but it remains controversial, and there are some ongoing questions. First, this study was limited by its small sample size and the lack of a conservative control group. Furthermore, the incidence of CFLD is low, and subsequently, the number of patients with early-stage PHT is even lower. Therefore, randomization was never an option. Second, as shown in the present study, it remains challenging to correctly identify patients early who will progress to severe CFLD with cirrhosis or NCPH and are subsequently at risk of developing complications.12,41 Even revisiting the original histopathology could not find a way to distinguish the two phenotypes in CFLD. However, early clinical signs of PHT with progressive thrombocytopenia or an advanced PPG on invasive pressure measurements might be indicative of a more severe phenotype. Considering normal PLT with low PPG at the time of the TIPS in several patients, a selection bias toward a more favorable disease course may exist. Third, the implementation of primary prophylaxis is debatable, as the risk of variceal bleeding is currently estimated at 5%–10% wihtin 10 years of diagnosis.3,18,42 Finally, a pre-emptive TIPS remains an invasive treatment for a fragile patient group without troublesome symptoms and with a limited tolerance for procedural complications.
In conclusion, this prospective study demonstrated TIPS as a feasible long-term treatment for selected CF patients with PHT to avert variceal bleeding. However, as the progression of liver fibrosis, thrombocytope nia, and splenomegaly is inevitable, and the bleeding risk has previously been overestimated, the clinical benefits due to pre-emptive placement appear to be minor. Moreover, there is an inherent risk of HE, especially with excessive shunting or uncontrolled protein intake. Consistent with previous reports, a liver biopsy at the time of the TIPS showed histopathological features of porto-sinusoidal vascular disease and advanced fibrosis.
Acknowledgments
We thank Ellen Delanghe (Clinical Research Assistant, Department of Vascular and Interventional Radiology, Ghent University Hospital, Ghent, Belgium now working at Pfizer Pharmaceutics, Puurs, Belgium) for her assistance with data collection and preparation, and Prof. Jeoffrey Schouten (Gastroenterologist, Department of Gastroenterology and Hepatology, AZ Nikolaas, Sint-Niklaas, Belgium) for his expert opinion on the manuscript.
Footnotes
Conflict of interest disclosure
The authors declared no conflicts of interest.
References
- 1.O’Sullivan BP, Freedman SD. Cystic fibrosis. Lancet. 2009;373(9678):1891–1904. doi: 10.1016/S0140-6736(09)60327-5. [DOI] [PubMed] [Google Scholar]
- 2.Flass T, Narkewicz MR. Cirrhosis and other liver disease in cystic fibrosis. J Cyst Fibros. 2013;12(2):116–124. doi: 10.1016/j.jcf.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boëlle PY, Debray D, Guillot L, Clement A, Corvol H; French CF Modifier Gene Study Investigators. Cystic fibrosis liver disease: outcomes and risk factors in a large cohort of French patients. Hepatology. 2019;69(4):1648–1656. doi: 10.1002/hep.30148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Debray D, Lykavieris P, Gauthier F, et al. Outcome of cystic fibrosis-associated liver cirrhosis: management of portal hypertension. J Hepatol. 1999;31(1):77–83. doi: 10.1016/s0168-8278(99)80166-4. [DOI] [PubMed] [Google Scholar]
- 5.Leung DH, Narkewicz MR. Cystic Fibrosis-related cirrhosis. J Cyst Fibros. 2017;16 (Suppl 2):S50–S61. doi: 10.1016/j.jcf.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Debray D, Kelly D, Houwen R, Strandvik B, Colombo C. Best practice guidance for the diagnosis and management of cystic fibrosis-associated liver disease. J Cyst Fibros. 2011;10 (Suppl 2):S29–S36. doi: 10.1016/S1569-1993(11)60006-4. [DOI] [PubMed] [Google Scholar]
- 7.Rowland M, Gallagher C, Gallagher CG, et al. Outcome in patients with cystic fibrosis liver disease. J Cyst Fibros. 2015;14(1):120–126. doi: 10.1016/j.jcf.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 8.Witters P, Libbrecht L, Roskams T, et al. Liver disease in cystic fibrosis presents as non-cirrhotic portal hypertension. J Cyst Fibros. 2017;16(5):e11–e13. doi: 10.1016/j.jcf.2017.03.006. [DOI] [PubMed] [Google Scholar]
- 9.Wu H, Vu M, Dhingra S, et al. Obliterative portal venopathy without cirrhosis is prevalent in pediatric cystic fibrosis liver disease with portal hypertension. Clin Gastroenterol Hepatol. 2019;17(10):2134–2136. doi: 10.1016/j.cgh.2018.10.046. [DOI] [PubMed] [Google Scholar]
- 10.Hillaire S, Cazals-Hatem D, Bruno O, et al. Liver transplantation in adult cystic fibrosis: clinical, imaging, and pathological evidence of obliterative portal venopathy. Liver Transpl. 2017;23(10):1342–1347. doi: 10.1002/lt.24842. [DOI] [PubMed] [Google Scholar]
- 11.Cipolli M, Fethney J, Waters D, et al. Occurrence, outcomes and predictors of portal hypertension in cystic fibrosis: a longitudinal prospective birth cohort study. J Cyst Fibros. 2020;19(3):455–459. doi: 10.1016/j.jcf.2019.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Dana J, Debray D, Beaufrère A, et al. Cystic fibrosis-related liver disease: clinical presentations, diagnostic and monitoring approaches in the era of CFTR modulator therapies. J Hepatol. 2022;76(2):420–434. doi: 10.1016/j.jhep.2021.09.042. [DOI] [PubMed] [Google Scholar]
- 13.Da BL, Surana P, Kapuria D, et al. Portal pressure in noncirrhotic portal hypertension: to measure or not to measure. Hepatology. 2019;70(6):2228–2230. doi: 10.1002/hep.30862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siegel MJ, Freeman AJ, Ye W, et al. Heterogeneous liver on research ultrasound identifies children with cystic fibrosis at high risk of advanced liver disease: interim results of a prospective observational case-controlled study. J Pediatr. 2020;219:62–69. doi: 10.1016/j.jpeds.2019.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Williams SG, Evanson JE, Barrett N, Hodson ME, Boultbee JE, Westaby D. An ultrasound scoring system for the diagnosis of liver disease in cystic fibrosis. J Hepatol. 1995;22(5):513–521. doi: 10.1016/0168-8278(95)80444-7. [DOI] [PubMed] [Google Scholar]
- 16.Etzion O, Takyar V, Novack V, et al. Spleen and liver volumetrics as surrogate markers of hepatic venous pressure gradient in patients with noncirrhotic portal hypertension. Hepatol Commun. 2018;2(8):919–928. doi: 10.1002/hep4.1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutton H, Dhawan A, Grammatikopoulos T. Non-invasive markers of portal hypertension: appraisal of adult experience and potential utilisation in children. J Pediatr Gastroenterol Nutr. 2018;66(4):559–569. doi: 10.1097/MPG.0000000000001882. [DOI] [PubMed] [Google Scholar]
- 18.Leung DH, Ye W, Schwarzenberg SJ, et al. Long-term follow-up and liver outcomes in children with cystic fibrosis and nodular liver on ultrasound in a multi-center study. J Cyst Fibros. 2022:S1569-1993(22)00635–X. doi: 10.1016/j.jcf.2022.07.017. [DOI] [PubMed] [Google Scholar]
- 19.Palaniappan SK, Than NN, Thein AW, Moe S, van Mourik I. Interventions for preventing and managing advanced liver disease in cystic fibrosis. Cochrane Database Syst Rev. 2017;8(8):CD012056. doi: 10.1002/14651858.CD012056.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Freeman AJ, Sellers ZM, Mazariegos G, et al. A multidisciplinary approach to pretransplant and posttransplant management of cystic fibrosis-associated liver disease. Liver Transpl. 2019;25(4):640–657. doi: 10.1002/lt.25421. [DOI] [PubMed] [Google Scholar]
- 21.Debray D, Narkewicz MR, Bodewes FAJA, et al. Cystic fibrosis-related liver disease: research challenges and future perspectives. J Pediatr Gastroenterol Nutr. 2017;65(4):443–448. doi: 10.1097/MPG.0000000000001676. [DOI] [PubMed] [Google Scholar]
- 22.Shneider BL, de Ville de Goyet J, Leung DH, et al. Primary prophylaxis of variceal bleeding in children and the role of MesoRex bypass: summary of the Baveno VI Pediatric Satellite Symposium. Hepatology. 2016;63(4):1368–1380. doi: 10.1002/hep.28153. [DOI] [PubMed] [Google Scholar]
- 23.Jeanniard-Malet O, Duché M, Fabre A. Survey on clinical practice of primary prophylaxis in portal hypertension in children. J Pediatr Gastroenterol Nutr. 2017;64(4):524–527. doi: 10.1097/MPG.0000000000001453. [DOI] [PubMed] [Google Scholar]
- 24.Tripathi D, Stanley AJ, Hayes PC, et al. Transjugular intrahepatic portosystemic stent-shunt in the management of portal hypertension. Gut. 2020;69(7):1173–1192. doi: 10.1136/gutjnl-2019-320221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pozler O, Krajina A, Vanicek H, et al. Transjugular intrahepatic portosystemic shunt in five children with cystic fibrosis: long-term results. Hepatogastroenterology. 2003;50(52):1111–1114. [PubMed] [Google Scholar]
- 26.Johansen LC, McKiernan PJ, Sharif K, McGuirk SP. Transjugular intrahepatic portosystemic shunt insertion for the management of portal hypertension in children. J Pediatr Gastroenterol Nutr. 2018;67(2):173–179. doi: 10.1097/MPG.0000000000002006. [DOI] [PubMed] [Google Scholar]
- 27.Bertino F, Hawkins CM, Shivaram G, et al. Technical feasibility and clinical effectiveness of transjugular intrahepatic portosystemic shunt creation in pediatric and adolescent patients. J Vasc Interv Radiol. 2019;30(2):178–186. doi: 10.1016/j.jvir.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Hermie L, Dhondt E, Vanlangenhove P, Hoste E, Geerts A, Defreyne L. Model for end-stage liver disease score and hemodynamic instability as a predictor of poor outcome in early transjugular intrahepatic portosystemic shunt treatment for acute variceal hemorrhage. Eur J Gastroenterol Hepatol. 2018;30(12):1441–1446. doi: 10.1097/MEG.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 29.Megremis SD, Vlachonikolis IG, Tsilimigaki AM. Spleen length in childhood with US: normal values based on age, sex, and somatometric parameters. Radiology. 2004;231(1):129–134. doi: 10.1148/radiol.2311020963. [DOI] [PubMed] [Google Scholar]
- 30.Roelants M, Hauspie R, Hoppenbrouwers K. References for growth and pubertal development from birth to 21 years in Flanders, Belgium. Ann Hum Biol. 2009;36(6):680–694. doi: 10.3109/03014460903049074. [DOI] [PubMed] [Google Scholar]
- 31.Dariushnia SR, Haskal ZJ, Midia M, et al. Quality improvement guidelines for transjugular intrahepatic portosystemic shunts. J Vasc Interv Radiol. 2016;27(1):1–7. doi: 10.1016/j.jvir.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 32.Witters P, Libbrecht L, Roskams T, et al. Noncirrhotic presinusoidal portal hypertension is common in cystic fibrosis-associated liver disease. Hepatology. 2011;53(3):1064–1065. doi: 10.1002/hep.24183. [DOI] [PubMed] [Google Scholar]
- 33.Bedossa P, Poynard T. An algorithm for the grading of activity in chronic hepatitis C. The METAVIR Cooperative Study Group. Hepatology. 1996;24(2):289–293. doi: 10.1002/hep.510240201. [DOI] [PubMed] [Google Scholar]
- 34.Di Giorgio A, Nicastro E, Agazzi R, Colusso M, D’Antiga L. Long-term outcome of transjugular intrahepatic portosystemic shunt in children with portal hypertension. J Pediatr Gastroenterol Nutr. 2020;70(5):615–622. doi: 10.1097/MPG.0000000000002597. [DOI] [PubMed] [Google Scholar]
- 35.Perarnau JM, Le Gouge A, Nicolas C, et al. Covered vs. uncovered stents for transjugular intrahepatic portosystemic shunt: a randomized controlled trial. J Hepatol. 2014;60(5):962–968. doi: 10.1016/j.jhep.2014.01.015. [DOI] [PubMed] [Google Scholar]
- 36.Bosch J, Groszmann RJ, Shah VH. Evolution in the understanding of the pathophysiological basis of portal hypertension: How changes in paradigm are leading to successful new treatments. J Hepatol. 2015;62(Suppl 1):S121–S130. doi: 10.1016/j.jhep.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Verbeeck S, Mekhali D, Cassiman D, Maleux G, Witters P. Long-term outcome of transjugular intrahepatic portosystemic shunt for portal hypertension in autosomal recessive polycystic kidney disease. Dig Liver Dis. 2018;50(7):707–712. doi: 10.1016/j.dld.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 38.Liu J, Ma J, Yang C, et al. Impact of TIPS on splenic volume and thrombocytopenia. AJR Am J Roentgenol. 2021;216(3):698–703. doi: 10.2214/AJR.20.22958. [DOI] [PubMed] [Google Scholar]
- 39.Liu J, Ma J, Yang C, et al. Impact of TIPS on splenic volume and thrombocytopenia. AJR Am J Roentgenol. 2021;216(3):698–703. doi: 10.2214/AJR.20.22958. [DOI] [PubMed] [Google Scholar]
- 40.Lemoine C, Lokar J, McColley SA, Alonso EM, Superina R. Cystic fibrosis and portal hypertension: distal splenorenal shunt can prevent the need for future liver transplant. J Pediatr Surg. 2019;54(5):1076–1082. doi: 10.1016/j.jpedsurg.2019.01.035. [DOI] [PubMed] [Google Scholar]
- 41.Koh C, Sakiani S, Surana P, et al. Adult-onset cystic fibrosis liver disease: diagnosis and characterization of an underappreciated entity. Hepatology. 2017;66(2):591–601. doi: 10.1002/hep.29217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ye W, Narkewicz MR, Leung DH, et al. Variceal hemorrhage and adverse liver outcomes in patients with cystic fibrosis cirrhosis. J Pediatr Gastroenterol Nutr. 2018;66(1):122–127. doi: 10.1097/MPG.0000000000001728. [DOI] [PMC free article] [PubMed] [Google Scholar]


