Abstract
We report a surge of patients, especially children and adolescents, with respiratory disease caused by Mycoplasma pneumoniae in Denmark since October 2023. While the surge has reached an epidemic level, no impact on hospital capacity has been observed; only 14% (446/3,195) of cases, primarily adults, required hospitalisation. Macrolide resistance was detected in less than 2% of samples tested. Timely monitoring of hospitalisations linked to M. pneumoniae infections has been established to inform the healthcare system, decisionmakers and the public.
Keywords: epidemiology; M. pneumoniae, surveillance; respiratory infection; resurgence; public health
Mycoplasma pneumoniae is a common cause of bacterial respiratory tract infections and atypical pneumonia [1]. Since late October 2023, an epidemic of M. pneumoniae has occurred in Denmark. Here, we present data from our national surveillance system with patients with a laboratory-confirmed infection, stratified by age and linked to information on hospital admissions.
Surveillance of Mycoplasma pneumoniae
Mycoplasma pneumoniae epidemics have occurred in Denmark about every 4 years since the 1940s [2], with seasonal variation and the number of cases typically peaking in November and December. The most recent epidemic of M. pneumoniae in Europe was during the 2019/20 season [3]. The first line antibiotics to treat M. pneumoniae infection are macrolides such as azithromycin.
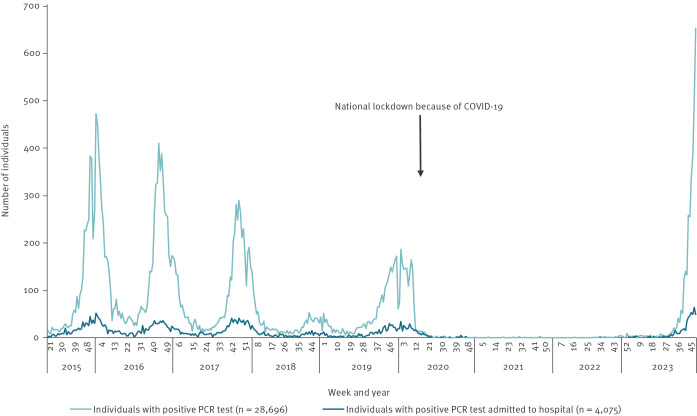
The non-pharmaceutical interventions implemented to reduce COVID-19-related morbidity and mortality were successful in reducing the transmission of numerous other respiratory infections, including M. pneumoniae infections [4]. As restrictions were lifted at different stages during the pandemic, several pathogens started to recirculate in Denmark, including influenza viruses [5] and respiratory syncytial virus (RSV) [6], as well as invasive group A streptococcus infections [7]. In contrast, M. pneumoniae infections were nearly non-existent from March 2020 until August 2023 in Denmark (Figure 1). Since week 32 of 2023, a steady rise in the number of M. pneumoniae cases has been observed across the country.
Figure 1.
Weekly number of individuals with a positive Mycoplasma pneumoniae PCR test result and the proportion of patients admitted to a hospital, Denmark, week 21 2015–week 48 2023
In Denmark, M. pneumoniae surveillance is centrally administered at the national public health and research institute, Statens Serum Institut (SSI) in Copenhagen, under the Danish Ministry of Health. Mycoplasma pneumoniae infections are laboratory notifiable and information is recorded in the national microbiology database (MiBa), which is used for continuous surveillance [8]. There are no national guidelines on the requirements for M. pneumoniae testing in Denmark, which also applies to most other European countries [9]. On suspicion of M. pneumoniae infection, a throat swab is collected from most patients, while fewer will have a sample collected from the lower respiratory tract; swabs are taken by physicians at both general practices and hospitals. The samples are submitted for real-time PCR testing at local microbiology laboratories or at SSI [10]. At SSI, all M. pneumoniae PCR-positive samples received for routine diagnostics or submitted from other laboratories upon suspicion of macrolide resistance are investigated for macrolide resistance-associated mutations in the 23 sRNA gene [11]. The PCR test results and information on macrolide resistance are recorded in MiBa [12]. Surveillance of infections can be individually linked through the unique personal identification number (the CPR number) to the Danish National Patient Registry to survey M. pneumoniae-related hospital admissions. In the present report, a hospital admission related to M. pneumoniae was defined as an admission of more than 12 h within 14 days after a positive PCR test for M. pneumoniae or a positive test during admission.
Mycoplasma pneumoniae epidemic since week 43 2023
The number of individuals with M. pneumoniae infection reached an epidemic level in week 43 in October 2023 (Figure 1). We define M. pneumoniae epidemics as occurring when M. pneumoniae is circulating and 10% of the PCR-tested individuals per week are positive. For the current 2023/24 season, in total, 14% (446/3,195) of all patients with a positive PCR for M. pneumoniae have been admitted to the hospital. Around 7% (99/1,406) of children aged 6–12 years and adolescents (13–18 years) were admitted, whereas 19% (292/1,520) of adults aged 19–75 years required admission (Table). Both proportions are comparable to previous seasons before COVID-19, whereas the proportion of people admitted aged above 75 years (48%; 31/65), is slightly lower than the proportion in previous seasons (Table).
Table. Mycoplasma pneumoniae test activity, proportion of individuals with positive PCR tests and proportion admitted to the hospital, by age group and season, Denmark, 2015/16–2023/24 up to week 48 2023.
| Age group (years) | Season | Total number of PCR tests | Individuals with a positive PCR | Individuals with a positive PCR admitted to the hospital | ||
|---|---|---|---|---|---|---|
| n | n | % | n | % | ||
| 0–5 | 2015/16 | 7,865 | 822 | 10.5 | 72 | 8.8 |
| 2016/17 | 8,832 | 764 | 8.7 | 60 | 7.9 | |
| 2017/18 | 6,690 | 499 | 7.5 | 49 | 9.8 | |
| 2018/19 | 3,846 | 103 | 2.7 | 18 | 17.5 | |
| 2019/20 | 5,356 | 356 | 6.6 | 21 | 5.9 | |
| 2020/21 | 1,708 | 5 | 0.3 | < 5 | 0 | |
| 2021/22 | 7,108 | < 5 | 0 | < 5 | 0 | |
| 2022/23 | 5,465 | < 5 | 0 | < 5 | 50.0 | |
| 2023/24a | 2,985 | 204 | 6.8 | 24 | 11.8 | |
| 6–12 | 2015/16 | 6,733 | 2,253 | 33.5 | 114 | 5.1 |
| 2016/17 | 6,606 | 2,048 | 31.0 | 104 | 5.1 | |
| 2017/18 | 5,121 | 1,292 | 25.2 | 80 | 6.2 | |
| 2018/19 | 2,557 | 278 | 10.9 | 27 | 9.7 | |
| 2019/20 | 4,189 | 1,025 | 24.5 | 58 | 5.7 | |
| 2020/21 | 839 | 11 | 1.3 | < 5 | 0.0 | |
| 2021/22 | 1,762 | < 5 | 0.1 | < 5 | 0.0 | |
| 2022/23 | 1,724 | 8 | 0.5 | < 5 | 12.5 | |
| 2023/24a | 2,349 | 914 | 38.9 | 64 | 7.0 | |
| 13–18 | 2015/16 | 5,260 | 898 | 17.1 | 68 | 7.6 |
| 2016/17 | 5,953 | 776 | 13.0 | 46 | 5.9 | |
| 2017/18 | 4,573 | 560 | 12.2 | 47 | 8.4 | |
| 2018/19 | 3,330 | 134 | 4.0 | 19 | 14.2 | |
| 2019/20 | 5,123 | 505 | 9.9 | 31 | 6.1 | |
| 2020/21 | 814 | 8 | 1.0 | < 5 | 25.0 | |
| 2021/22 | 2,921 | < 5 | 0 | < 5 | 0 | |
| 2022/23 | 2,379 | 29 | 1.2 | < 5 | 3.4 | |
| 2023/24a | 3,101 | 492 | 15.9 | 35 | 7.1 | |
| 19–39 | 2015/16 | 16,099 | 1,563 | 9.7 | 303 | 19.4 |
| 2016/17 | 19,641 | 1,522 | 7.7 | 239 | 15.7 | |
| 2017/18 | 17,800 | 1,297 | 7.3 | 285 | 22.0 | |
| 2018/19 | 12,802 | 339 | 2.6 | 61 | 18.0 | |
| 2019/20 | 16,323 | 1,099 | 6.7 | 229 | 20.8 | |
| 2020/21 | 7,272 | 7 | 0.1 | < 5 | 42.9 | |
| 2021/22 | 14,194 | < 5 | 0 | < 5 | 0 | |
| 2022/23 | 11,162 | 33 | 0.3 | 9 | 27.3 | |
| 2023/24a | 8,428 | 683 | 8.1 | 131 | 19.2 | |
| 40–75 | 2015/16 | 41,225 | 1,797 | 4.4 | 331 | 18.4 |
| 2016/17 | 52,568 | 1,753 | 3.3 | 316 | 18.0 | |
| 2017/18 | 52,087 | 1,434 | 2.8 | 335 | 23.4 | |
| 2018/19 | 42,558 | 426 | 1.0 | 107 | 25.1 | |
| 2019/20 | 49,984 | 1,322 | 2.6 | 300 | 22.7 | |
| 2020/21 | 32,297 | 26 | 0.1 | 18 | 69.2 | |
| 2021/22 | 43,585 | 5 | 0 | < 5 | 60.0 | |
| 2022/23 | 43,148 | 41 | 0.1 | 12 | 29.3 | |
| 2023/24a | 25,931 | 837 | 3.2 | 161 | 19.2 | |
| > 75 | 2015/16 | 10,684 | 89 | 0.8 | 50 | 56.2 |
| 2016/17 | 15,592 | 97 | 0.6 | 48 | 49.5 | |
| 2017/18 | 17,567 | 114 | 0.6 | 66 | 57.9 | |
| 2018/19 | 17,868 | 28 | 0.2 | 17 | 60.7 | |
| 2019/20 | 22,316 | 108 | 0.5 | 61 | 56.5 | |
| 2020/21 | 27,156 | 12 | 0 | 11 | 91.7 | |
| 2021/22 | 31,798 | < 5 | 0 | < 5 | 100.0 | |
| 2022/23 | 31,987 | < 5 | 0 | < 5 | 75.0 | |
| 2023/24a | 15,168 | 65 | 0.4 | 31 | 47.7 | |
a A season in Denmark is from week 21 to week 20. Data collection for the ongoing season 2023/24 is not complete as the season is not finished; data were collected up to week 48.
The highest proportion of PCR-positive tests was observed in those aged 6–12 years (39%), followed by those aged 13–18 years (16%) (Table). For all age groups above children of 0–5 years, the proportion of positive tests decreased with increasing age, while the proportion of individuals with a positive test who were admitted to the hospital increased with age. The proportion of individuals who tested PCR-positive and admitted to the hospital was not higher in 2023 than the proportion in the pre-pandemic seasons, for any age group (Table). While we anticipated an increase in testing practices given the COVID-19 pandemic, the current number of PCR tests this season is comparable to those from previous seasons.
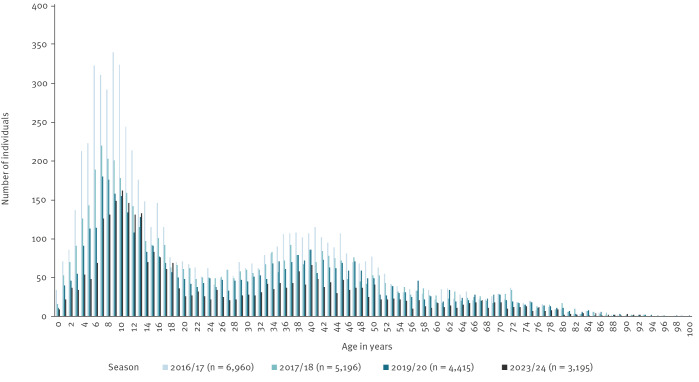
Compared with the pre-pandemic seasons, there appears to be a shift in the age distribution towards older children testing positive for M. pneumoniae. In the current season up until the end of 2023, there is a peak among children aged 8–12 years, whereas the pre-pandemic seasons had a peak among children aged 5–10 years (Figure 2). A second peak is observed among adults aged around 40 years, similarly to that in previous seasons, and possibly parents to young children with M. pneumoniae infections, although this was not further investigated here.
Figure 2.
Number of individuals with a positive Mycoplasma pneumoniae PCR by age and season, Denmark, 2016/17–2023/24 up to week 48 2023
A season in Denmark is from week 21 to week 20. Data collection for the ongoing season 2023/24 is not complete as the season is not finished; data were collected up to week 48.
Antimicrobial susceptibility
During 2023 up to the end of November, macrolide resistance-associated mutations were not detected in any of the 114 positive samples tested at SSI, of which 46% (n = 52) were from individuals under 20 years of age. Ninety-eight of the samples were collected during November 2023. Of 288 tested individuals from 1 to 18 December, 83 samples were positive for M. pneumoniae, and mutations associated with macrolide resistance were demonstrated in 3 of 83 (3.6%). The overall rate for 2023 is low in total (3/197, 1.5%). The slight increase in macrolide resistance detected the first 18 days of December may be a coincidence but will be monitored throughout the epidemic.
Discussion
Since late October 2023, there has been an epidemic of M. pneumoniae in Denmark. According to the European Centre for Disease Prevention and Control (ECDC), an increase in incidence of respiratory infections caused by M. pneumoniae has been observed in six European countries during the 2023/24 season, mostly among children and adolescents, with one country reporting an increase in severe disease cases admitted to intensive care units [13]. A recent global study showed the same tendency in several countries, with the increase most pronounced in some northern and central European countries [14]. In November 2023, China reported an increase in the incidence of respiratory diseases, predominantly affecting children, which was later attributed to the increase of known pathogens including M. pneumoniae [15].
In Denmark, M. pneumoniae epidemics typically occur about every 4 years but can span over two to three consecutive seasons. The current 2023/24 season surge may reflect the typical periodic recurrence and could potentially be exacerbated after a period of 3.5 years with nearly no occurrence in the country. The temporary period with many fewer respiratory infections during the COVID-19 pandemic because of lockdowns and restrictions appears to have affected the typical incidence patterns seen; a lack of exposure to commonly circulating pathogens may have caused potentially higher susceptibility to certain infections in the population, especially among children [16,17]. Diagnosis of M. pneumoniae infection can be challenging, as the symptoms may resemble those of other respiratory infections. However, the infection is characterised by a prolonged coughing period, which may last several weeks. In Denmark, the majority of patients with mild respiratory infection or influenza-like symptoms are not tested for M. pneumoniae infection. Therefore, the true incidence of M. pneumoniae and related disease burden in the country are under-reported and largely unknown.
Although admission rates have been comparable to those in pre-pandemic seasons, it is still noteworthy that 19% (131/683) of adults aged 19–39 years with positive M. pneumoniae tests have been admitted to the hospital during the current epidemic. Since the COVID-19 pandemic, there has been an increased awareness of hospital capacity. To assess severity of different pathogens and to contribute to assessments of hospital capacity, hospitalisations in Denmark are regularly surveyed especially during peak seasons such as during the current M. pneumoniae epidemic, which is co-occurring with high numbers of cases of pertussis, influenza, RSV and COVID-19 [18].
Moreover, monitoring macrolide resistance is important. Our national surveillance system enables us to identify and respond to fluctuations in macrolide resistance levels. In case of increased resistance, we might increase the number of samples undergoing resistance testing in Denmark. However, macrolide resistance is currently low in Denmark at 1.5% and similar to previous seasons (on average, 1.5%) [9,11], which is low compared with other European countries [19]. Notably, China has, over several years, reported a high proportion of macrolide resistance in M. pneumoniae ranging from 65 to 100% [20-22].
In most European countries, cases of M. pneumoniae infection are not notifiable. In Denmark, however, we have a unique possibility to monitor the infection, as laboratory detections of M. pneumoniae are notifiable and surveillance is made possible by a national database including all diagnostic laboratory results. Data are logged at the individual level, making it possible to track and link information across other national registries. In this way, information on hospital admissions can be surveyed simultaneously, providing an overview of the burden to the healthcare system.
Conclusion
A nationwide epidemic of M. pneumoniae infections in Denmark has occurred since late October 2023, especially among school-aged children. Resistance against macrolides has been low, and the proportion of hospitalised cases is similar to previous epidemics. Although the hospital capacity is not currently challenged by M. pneumonia admissions, continuous surveillance of infections, admissions and antimicrobial resistance are important to inform the health sector.
Ethical statement
No ethical approval was required for this register study based on routine surveillance data.
Acknowledgements
The Clinical Microbiological Laboratories are thanked for submitting data to the Danish Microbiology Database (MiBa), and Randi Føns Petersen and the SSI PCR laboratory are acknowledged for the macrolide-resistance data.
Findings have been previously published at https://www.ssi.dk/aktuelt/nyheder/2023/der-er-epidemi-med-mycoplasmainfektioner-ogsaa-kendt-som-kold-lungebetaendelse.
Conflict of interest: None declared.
Authors’ contributions: HDE, SU and BS conceptualised the study. KLM, HDE and SU provided all data. KLM, LFS and HDE performed the data analyses. ACN contributed to data management and drafted the original manuscript. BS and HDE supervised the data interpretation and revised the first draft. PJ, TGH, HDE, BS, SU, KLM, LFS all contributed to the critical reviewing and editing the manuscript. All authors have read and approved the final manuscript for publication.
References
- 1. Waites KB, Xiao L, Liu Y, Balish MF, Atkinson TP. Mycoplasma pneumoniae from the respiratory tract and beyond. Clin Microbiol Rev. 2017;30(3):747-809. 10.1128/CMR.00114-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lind K, Benzon MW, Jensen JS, Clyde WA, Jr. A seroepidemiological study of Mycoplasma pneumoniae infections in Denmark over the 50-year period 1946-1995. Eur J Epidemiol. 1997;13(5):581-6. 10.1023/A:1007353121693 [DOI] [PubMed] [Google Scholar]
- 3. Meyer Sauteur PM, Beeton ML, Uldum SA, Bossuyt N, Vermeulen M, Loens K, et al. Mycoplasma pneumoniae detections before and during the COVID-19 pandemic: results of a global survey, 2017 to 2021. Euro Surveill. 2022;27(19):1. 10.2807/1560-7917.ES.2022.27.19.2100746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Meyer Sauteur PM, Chalker VJ, Berger C, Nir-Paz R, Beeton ML, ESGMAC and the ESGMAC–MyCOVID study group . Mycoplasma pneumoniae beyond the COVID-19 pandemic: where is it? Lancet Microbe. 2022;3(12):e897. 10.1016/S2666-5247(22)00190-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Emborg HD, Carnahan A, Bragstad K, Trebbien R, Brytting M, Hungnes O, et al. Abrupt termination of the 2019/20 influenza season following preventive measures against COVID-19 in Denmark, Norway and Sweden. Euro Surveill. 2021;26(22):1. 10.2807/1560-7917.ES.2021.26.22.2001160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munkstrup C, Lomholt FK, Emborg HD, Møller KL, Krog JS, Trebbien R, et al. Early and intense epidemic of respiratory syncytial virus (RSV) in Denmark, August to December 2022. Euro Surveill. 2023;28(1):2200937. 10.2807/1560-7917.ES.2023.28.1.2200937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johannesen TB, Munkstrup C, Edslev SM, Baig S, Nielsen S, Funk T, et al. Increase in invasive group A streptococcal infections and emergence of novel, rapidly expanding sub-lineage of the virulent Streptococcus pyogenes M1 clone, Denmark, 2023. Euro Surveill. 2023;28(26):2300291. 10.2807/1560-7917.ES.2023.28.26.2300291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Indenrigs- og Sundhedsministeriet. Sundhedsstyrelsens bekendtgørelse om anmeldelse af smitsomme sygdomme: BEK nr. 1260 af 27/10 2023. [Executive Order on notification of communicable diseases. The Danish Health Authority's executive order no. 1260 of 27/10 2023]. Copenhagen: Indenrigs- og Sundhedsministeriet. [Accessed: 8 Jan 2024]. Danish. Available from: http://www.socialjura.dk/content-storage/regler/2023/bek-1260-af-2710-2023/menu/all//new
- 9. Beeton ML, Zhang XS, Uldum SA, Bébéar C, Dumke R, Gullsby K, et al. Mycoplasma pneumoniae infections, 11 countries in Europe and Israel, 2011 to 2016. Euro Surveill. 2020;25(2):1. 10.2807/1560-7917.ES.2020.25.2.1900112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dumke R, Benitez AJ, Chalker V, Gullsby K, Henrich B, Hidalgo-Grass C, et al. Multi-center evaluation of one commercial and 12 in-house real-time PCR assays for detection of Mycoplasma pneumoniae. Diagn Microbiol Infect Dis. 2017;88(2):111-4. 10.1016/j.diagmicrobio.2017.03.004 [DOI] [PubMed] [Google Scholar]
- 11. Uldum SA, Bangsborg JM, Gahrn-Hansen B, Ljung R, Mølvadgaard M, Føns Petersen R, et al. Epidemic of Mycoplasma pneumoniae infection in Denmark, 2010 and 2011. Euro Surveill. 2012;17(5):20073. 10.2807/ese.17.05.20073-en [DOI] [PubMed] [Google Scholar]
- 12. Voldstedlund M, Haarh M, Mølbak K, MiBa Board of Representatives . The Danish Microbiology Database (MiBa) 2010 to 2013. Euro Surveill. 2014;19(1):20667. 10.2807/1560-7917.ES2014.19.1.20667 [DOI] [PubMed] [Google Scholar]
- 13.European Centre for Disease Prevention and Control (ECDC). Communicable disease threats report, 26 November - 2 December 2023, week 48. Stockholm: ECDC; 2023. Available from: https://www.ecdc.europa.eu/en/publications-data/communicable-disease-threats-report-26-november-2-december-2023-week-48
- 14.Meyer Sauteur PM, Beeton ML; European Society of Clinical Microbiology and Infectious Diseases (ESCMID) Study Group for Mycoplasma and Chlamydia Infections (ESGMAC), and the ESGMAC Mycoplasma pneumoniae Surveillance (MAPS) study group. Mycoplasma pneumoniae: delayed re-emergence after COVID-19 pandemic restrictions. Lancet Microbe. 2023 Nov 23:S2666-5247(23)00344-0. doi: 10.1016/S2666-5247(23)00344-0. Epub ahead of print. PMID: 38008103. [DOI] [PubMed]
- 15.World Health Organization (WHO). Disease Outbreak News. Upsurge of respiratory illnesses among children-Northern China. Geneva: WHO; 2023. Available from: https://www.who.int/emergencies/disease-outbreak-news/item/2023-DON494
- 16. Abu-Raya B, Viñeta Paramo M, Reicherz F, Lavoie PM. Why has the epidemiology of RSV changed during the COVID-19 pandemic? EClinicalMedicine. 2023;61:102089. 10.1016/j.eclinm.2023.102089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hatter L, Eathorne A, Hills T, Bruce P, Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021;5(12):e44-5. 10.1016/S2352-4642(21)00333-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Statens Serum Institut (SSI). Overvågning af Influenza, covid-19, RS-virus og andre luftvejssygdomme. [Surveillance of Influenza, COVID-19, RS-virus, and other respiratory diseases]. Copenhagen: SSI; 2023. Danish. Available from: https://www.ssi.dk/sygdomme-beredskab-og-forskning/overvaagning-af-luftvejssygdomme
- 19. Loconsole D, De Robertis AL, Sallustio A, Centrone F, Morcavallo C, Campanella S, et al. Update on the epidemiology of macrolide-resistant Mycoplasma pneumoniae in Europe: a systematic review. Infect Dis Rep. 2021;13(3):811-20. 10.3390/idr13030073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Wang G, Wu P, Tang R, Zhang W. Global prevalence of resistance to macrolides in Mycoplasma pneumoniae: a systematic review and meta-analysis. J Antimicrob Chemother. 2022;77(9):2353-63. 10.1093/jac/dkac170 [DOI] [PubMed] [Google Scholar]
- 21. Zhao F, Liu J, Shi W, Huang F, Liu L, Zhao S, et al. Antimicrobial susceptibility and genotyping of Mycoplasma pneumoniae isolates in Beijing, China, from 2014 to 2016. Antimicrob Resist Infect Control. 2019;8(1):18. 10.1186/s13756-019-0469-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Yu HX, Zhao MM, Pu ZH, Ju YR, Liu Y. A study of community-acquired Mycoplasma pneumoniae in Yantai, China. Colomb Med (Cali). 2018;49(2):160-3. 10.25100/cm.v49i2.3813 [DOI] [PMC free article] [PubMed] [Google Scholar]