Abstract
People exposed to more unfavourable social circumstances are more vulnerable to poor mental health over their life course, in ways that are often determined by structural factors which generate and perpetuate intergenerational cycles of disadvantage and poor health. Addressing these challenges is an imperative matter of social justice. In this paper we provide a roadmap to address the social determinants that cause mental ill health. Relying as far as possible on high‐quality evidence, we first map out the literature that supports a causal link between social determinants and later mental health outcomes. Given the breadth of this topic, we focus on the most pervasive social determinants across the life course, and those that are common across major mental disorders. We draw primarily on the available evidence from the Global North, acknowledging that other global contexts will face both similar and unique sets of social determinants that will require equitable attention. Much of our evidence focuses on mental health in groups who are marginalized, and thus often exposed to a multitude of intersecting social risk factors. These groups include refugees, asylum seekers and displaced persons, as well as ethnoracial minoritized groups; lesbian, gay, bisexual, transgender and queer (LGBTQ+) groups; and those living in poverty. We then introduce a preventive framework for conceptualizing the link between social determinants and mental health and disorder, which can guide much needed primary prevention strategies capable of reducing inequalities and improving population mental health. Following this, we provide a review of the evidence concerning candidate preventive strategies to intervene on social determinants of mental health. These interventions fall broadly within the scope of universal, selected and indicated primary prevention strategies, but we also briefly review important secondary and tertiary strategies to promote recovery in those with existing mental disorders. Finally, we provide seven key recommendations, framed around social justice, which constitute a roadmap for action in research, policy and public health. Adoption of these recommendations would provide an opportunity to advance efforts to intervene on modifiable social determinants that affect population mental health.
Keywords: Mental health, mental disorder, social determinants, social risk factors, prevention, marginalized groups, population mental health, social justice
Social determinants of health represent the most modifiable set of targets for intervention currently available to prevent the onset of mental health problems and disorders, and to promote positive mental health in our populations. Social determinants of mental health encompass the set of structural conditions to which people are exposed across the life course, from conception to death, which affect individual mental health outcomes, and contribute to mental health disparities within and between populations. These structural conditions include factors such as income, employment, socioeconomic status, education, food security, housing, social support, discrimination, childhood adversity, as well as the neighbourhood social and physical conditions in which people live, and the ability to access acceptable and affordable health care. Importantly, our chances of being exposed to protective or harmful social determinants of (mental) health are “shaped by the distribution of money, power and resources at global, national and local levels, which are themselves influenced by policy choices” 1 . Such determinants are therefore not randomly or benignly distributed within or between populations, but are manifested by systems and institutions of power that often produce and reproduce intergenerational inequities in people's opportunities to realize safe, secure, prosperous and healthy lives.
There is now compelling evidence that the risk of developing any mental health condition is inextricably linked to our life circumstances 2 , meaning that a higher burden of population‐level psychiatric morbidity is disproportionately experienced by those closer to the margins of our societies. Since poor mental health can be the invisible hand that suppresses life chances, including both how long we live 3 and the quality of years lived 4 , improving population mental health by designing effective prevention strategies that intervene on modifiable social risk factors should be seen as a central issue of social justice 5 .
We stand at a threshold moment not only in understanding the potential causal role of modifiable social determinants in the onset (or exacerbation) of mental health problems, but also in defining our response to them through effective prevention strategies that reduce inequities in the burden of psychiatric morbidity experienced between and within different populations. Arguably, the last two decades have brought about some progress in our biomedical understanding of psychiatric disorders, while investigating the importance of psychosocial factors in causing mental disorder has remained a peripheral focus for scientific discovery and clinical psychiatry. We have expanded our knowledge about the immutable, overlapping (pleiotropic) and polygenic bases of psychiatric disorders that can help explain why some individuals are more at risk of a diverse array of psychopathologies than others 6 . We have also achieved a better understanding of how complex the neurobiology of different psychiatric conditions is likely to be 7 , including depression, psychosis and bipolar disorder. This progress has, however, simultaneously exposed limitations in our ability to translate the acquired knowledge into effective clinical targets to prevent or alleviate symptoms of mental distress. The promise of personalized prediction and treatment remains out of reach in routine clinical practice 8 . Frontline pharmacological treatments for depression, anxiety, psychosis and bipolar disorder have remained largely unchanged since they were first developed in the 20th century 9 ; treatment resistance affects 20‐60% of our patients 10 ; and the pharmaceutical industry has largely withdrawn from psychiatric drug discovery in the last 20 years 11 .
These last two decades have simultaneously witnessed at least two seismic transformations in the mental health landscape. First, unprecedented increases in public awareness and advocacy about mental health, well‐being and illness, albeit concentrated in the Global North, have raised political pressure on institutions and governments to act to address the global burden of psychiatric morbidity 2 . Such has been the transformation that promoting mental health and well‐being is now identified as a specific outcome in the United Nations (UN) Sustainable Development Goals 12 , alongside targets to tackle various social determinants of health – including poverty, inequality, gender equality, and social justice – by 2030. The World Health Organization (WHO) also recognizes the urgent need to address how our environments affect mental health. In the recent World Mental Health Report 2 , T. Ghebreyesus, the WHO Director‐General, reaffirmed the Organization's commitment in “transforming the environments that influence our mental health” to promote mental well‐being and prevent mental disorder.
Second, longitudinal declines in public stigma and more positive attitudes towards major psychiatric conditions such as depression – particularly in so‐called Millennial and Gen Z generations 13 , 14 – have been paralleled by sustained increases in the number of people seeking help for mental health issues over the last 20 years. In some contexts, this has placed overwhelming pressure on clinical services tasked with providing primary, secondary and tertiary treatment for mental health conditions, with evidence globally that economic investment in mental health service provision continues to fall far short of need for care 2 . For example, in England, a 54% increase in referrals to public mental health services from 2016 to 2022 was accompanied by a mere 10.9% real‐terms increase in service funding 15 , 16 , highlighting the growing treatment gap in population mental health. This gap has been reported globally for depression 17 and psychosis 2 , and is particularly high in low‐ and middle‐income countries (LMICs) 18 .
The increased need for mental health care over the last two decades is not randomly distributed within populations, but follows clearly the social, demographic and economic lines along which experiences of poor mental health and receipt of mental health care are inequitably distributed 2 .
Nowhere is this more evident than in the case of children and young people. Given that adolescence represents a critical period of neural, psychological, behavioural and social development, it is perhaps no surprise that so many mental health problems emerge for the first time during this period. A recent systematic review of the pre‐pandemic literature estimated that the onset of around one third, half and two thirds of any mental disorder will have already occurred by ages 14, 18 and 25, respectively 19 . In the US, the proportion of university students – typically aged 18‐22 years – who reported having been treated for mental health problems has risen from 19% in 2007 to 34% in 2017 20 . A rapid increase in self‐reported depressive symptoms amongst younger adolescents in the US since 2012 has also been reported, peaking in 2018 (the last date of available survey data) 21 . These are not isolated findings. Further research from the US 22 , Canada 23 , Europe 24 , France 25 , Iceland 26 and Australia 27 , 28 all suggest that rates of depression, anxiety, self‐harm, eating disorders, attention‐deficit/hyperactivity disorder (ADHD) and suicide have risen rapidly amongst teenagers since 2010 29 , particularly in females 26 , 27 , 30 , 31 . By contrast, there is some evidence that the prevalence of alcohol and drug use disorders 24 , 32 and behaviours 33 has decreased over this period.
Observed changes in the prevalence of mental health problems in children and young people have been attributed to both period 21 and cohort 22 effects. While the COVID‐19 pandemic – a textbook period effect – appears to have had only minimal impact on long‐term mental health in the general population 34 , 35 , impacts on children and young people, who have often borne the brunt of restrictive lockdown policies, are more pronounced 25 , 34 , 35 . For example, in England, the number of people less than 18 years old accessing public mental health services in the previous 12 months increased by 20.4% between the start of the pandemic and July 2022 15 . These patterns have been observed in several different countries 34 , 35 , and extend to suicidal outcomes, particularly amongst girls 34 . Inequalities in poor mental health following the COVID‐19 pandemic have also been reported for women 36 , 37 , 38 , low‐income households 36 , and several groups minoritized by race and ethnicity 38 , gender identity and sexual orientation 39 , or migrant status 40 .
Other shocks (i.e., food, energy and economic crises, global conflicts, racial injustice), in addition to ongoing climate change, also contribute to the inequitable distribution of mental health and disorder in our populations. These shocks affect people's freedom of movement, social connectedness, and levels of isolation and loneliness. They influence people's economic precarity through impacts on employment, income, education, food and housing security. They affect people's agency and autonomy by threat to life, livelihood and civil liberties, whether via experiences of interpersonal, institutional or systematic racism, or displacement through conflict and violence, political instability, or climate‐related events. Most inescapably, these acute shocks belie a more chronic, pervasive exposure to negative social determinants which erode people's opportunities to sustain good mental health, recover from poor mental health, and prevent illness in the future. Repeated exposure to these determinants can create cycles of intergenerational disadvantage, which affect individual, familial and area‐level inequalities in mental health 2 , 41 .
At this critical juncture, we argue for the need to fully integrate a social determinants perspective into the biopsychosocial model of mental health and illness. This requires establishing the extent to which various social determinants are causally implicated in producing poor mental health, and generating inequalities in risk for mental disorders. It also involves understanding the mechanisms and pathways through which these outcomes arise. Armed with this knowledge, we will be in a stronger position to fund, develop, test and implement evidence‐based prevention strategies tackling the social determinants of mental health that shift the population‐level expression of mental disorders. In turn, this can reduce gross inequities in the mental, physical and social outcomes that arise as a result of poor mental health. Such public mental health strategies should sit alongside existing evidence‐based strategies in clinical psychiatry that have proved effective in treating individuals.
In this paper, we provide a roadmap towards this ambitious but necessary revolution. We first review the evidence that exists to support a causal association between key social determinants and mental health and disorder. We focus on those determinants which may have broad effects on several major mental disorders globally, and/or which may be highly prevalent in society, and thus have the potential to offer the biggest gains for public mental health prevention. These include social determinants that occur at the individual or family level (including socioeconomic disadvantage, discrimination, isolation and loneliness, early life adversities, childhood traumas), and those in the wider social environment (including neighbourhood disadvantage, social capital, the physical environment, and climate change). Our review pays special attention to inequalities experienced by women; lesbian, gay, bisexual, transgender and queer (LGBTQ+) people; migrants and ethnoracial minoritized groups. Throughout, we cite the strongest quantitative evidence, where available, and acknowledge any gaps in knowledge. One limitation of this approach is that the majority of the evidence we draw from – though by no means alle.g.,42 – comes from high‐income countries (HICs) in the Global North. Redressing the inequitable production of knowledge in this field is beyond the scope of our review, but provides a direct challenge to make global progress on the UN Sustainable Development Goal for mental health 12 , 43 . Where available, we highlight evidence collected in the Global South, but recognize that different contexts will also face unique social determinants of mental health that require dedicated attention.
We then introduce a preventive framework for conceptualizing how such social determinants affect the expression of mental health and disorder at the population level, and how this understanding can ground and guide prevention strategies to improve public mental health. In this framework, we introduce the fundamental idea of treating whole populations, which should sit alongside prevailing models of individual clinical care in psychiatry. Treatments here, broadly defined, may include universal, selective or indicated primary prevention strategies that intervene on social determinants of health aiming to affect the population‐level expression of mental health and illness, as well as secondary and tertiary prevention strategies to help those with existing mental health problems. Using this framework, we then review the current strength of evidence on the efficacy and effectiveness of a (non‐exhaustive) set of universal, selective and indicated strategies that intervene on social determinants for the prevention and alleviation of mental distress. In the final section of the paper, drawing together current evidence, we provide a set of seven recommendations for action, as a roadmap for improving population mental health and reducing inequities in mental health and disorder.
SOCIAL DETERMINANTS THAT IMPACT MENTAL HEALTH AND DISORDER: THE EVIDENCE
Social determinants at the individual level
Socioeconomic disadvantage
Socioeconomic disadvantage is a fundamental determinant of mental health outcomes over the life course 44 , 45 , 46 . Strong socioeconomic gradients have been observed for an array of mental health outcomes in HIC 45 and LMIC settings 42 . Socioeconomic disadvantage can be operationalized in several ways, and is a multifaceted construct encompassing different dimensions, including education 47 , 48 , finance 49 , 50 , occupation 51 , 52 , 53 , and living standards 54 , 55 . All these dimensions have been associated with mental health and disorder, and social inequalities in mental health may arise from a series of interrelated structural and cultural processes operating in society.
According to structural explanations, social stratification creates unequal access to resources – such as wealth and knowledge – that help individuals avoid exposure to harmful stressors 46 . Higher levels of wealth and income enable access to key determinants of positive mental health, including adequate and safe housing 55 , sufficient food security 54 , and effective health care. Income losses appear to have a far greater impact on mental health than income gains 49 , with further financial stressors such as income volatility, perceived job insecurity and moving into debt all linked to worsening mental health 50 , 56 , 57 . Poor mental health itself can also impact earnings and contribute to financial stress, meaning that the relationship between socioeconomic disadvantage and mental health is likely to be bi‐directional 58 . Indeed, while there is a long‐standing debate about the so‐called “social causation” and “social drift” theories of mental disorders 46 , recognizing the bi‐directional and cyclical relationship between socioeconomic disadvantage and mental health is likely to be vital for promoting prevention strategies that interrupt the intergenerational transmission of environmental risks for mental disorders 2 . Since socioeconomic disadvantage is both a risk factor for, and a consequence of, mental disorders, establishing key periods over the life course to intervene is a critical step towards effective prevention. We note here the need for stronger causal inference methods to address these challenges in observational studies.
Early life exposure to socioeconomic disadvantage may be particularly harmful for later mental health. For example, in a systematic review of evidence in children and adolescents 59 , 52 of 55 studies (mostly from HICs), including 25 longitudinal ones, reported an inverse association of mental health problems with socioeconomic position. Children growing up in socioeconomic disadvantage were 2‐3 times more likely to experience mental health problems than their non‐disadvantaged peers, with risk associated with both duration and severity of exposure. A systematic review reported similar associations with respect to ADHD 60 . An inverse relationship between parental income during a child's upbringing and later schizophrenia risk has been also found in Denmark 61 , 62 , independent of parental mental health and education. Birth cohort evidence from the UK also suggests that children growing up or transitioning into poverty are more likely to experience mental health problems by age 11, independent of maternal mental health 63 . Finally, there is also systematic review evidence from LMICs that supports (mostly cross‐sectional, but extending to longitudinal) associations between poverty and depression in adulthood 42 .
If causal, early life exposure to socioeconomic disadvantage may increase risk of mental health problems through several different mechanisms, based on potential biological, psychological and social pathways 64 . In LMIC settings, a systematic review concluded that education, food insecurity, socioeconomic position and financial stress had more consistent effects on risk for common mental disorders than income and employment 42 . Families lacking financial resources are less likely to have their basic needs met, including adequate nutrition, which prenatally has been shown to increase the risk of some psychiatric disorders, including schizophrenia, later in life (see below) 65 . Ongoing familial socioeconomic disadvantage is also likely to contribute to chronic stress for parents, which may affect parenting behaviours and the stability of family environments, and may also result in fewer longer‐term educational and employment opportunities for children. Mental health inequalities according to education level have been seen across the lifespan. Leaving school at a younger age, fewer years in formal education, and having a lower level of education are each associated with poorer future mental health and increased risk of suicide 48 , 66 . Education is likely to impact mental health through a variety of means, such as determining one's future social status and income, although these associations are likely to be partially due to confounding by early‐life factors such as childhood adversity 67 .
Early life adversity
There is strong evidence that several early life (defined here as prenatal and perinatal) adversities – including maternal stress, obstetric complications, and malnutrition – can have profound effects on mental health and disorder decades later 68 . These events do not affect all people equally, making them strongly socially determined risk factors for offspring mental health. For example, parental socioeconomic status and experiences of income inequality are associated with adverse birth outcomes 69 . Furthermore, in the US, there is consistent evidence of racial/ethnic disparities in adverse maternal and neonatal outcomes (including preterm birth, low birthweight and infant mortality) and receipt of prenatal care 70 , all of which are higher for Black, Hispanic and Indigenous groups than non‐Hispanic White and Asian groups. These disparities are hypothesized to arise through structural racism that operates on a number of levels to affect “a woman's knowledge of prenatal care (individual); the amount of support she receives from her family, friends, and community (social); experiences with racism and other social and environmental stressors (social); the way she is treated by her care provider (institutional); and the policies and practices of her insurer (systemic)” 70, p.124 .
There is good evidence that exposure to prenatal maternal stressors – including financial stress and relationship difficulties – is associated with increased risk of many (though not all) offspring behavioural and mental health outcomes, including neurocognitive development 71 , negative affectivity 71 , externalizing and internalizing problems in childhood 71 , autistic traits 71 , borderline personality disorder 71 , anxiety 71 , depression 71 , 72 , and psychosis 68 . Nevertheless, this association has not been universally observed. For example, a systematic review on ADHD and autism spectrum disorder found that evidence was limited to low‐quality case‐control studies, raising doubts about the likelihood of a causal association 73 .
Prenatal malnutrition following famine exposure has also been strongly associated with risk of psychotic disorders 65 , notwithstanding similar issues around causality. A systematic review also found evidence to support a protective effect of prenatal multivitamin supplementation on autism spectrum disorder 74 , but this was restricted to high‐quality studies. Surprisingly few studies have examined the association between prenatal nutrition and common mental disorders, with no systematic review available, although some longitudinal evidence exists for childhood mood and behavioural outcomes 75 , 76 , 77 , with associations persisting after adjustment for maternal perinatal mental health, prenatal smoking and alcohol use. Early life vitamin D deficiency has also been proposed as an explanation for higher risk of various psychiatric disorders 78 , but recent causally‐informed evidence does not support this for depression 79 , 80 , 81 , schizophrenia 82 and Alzheimer's disease 81 .
Understanding the causal mechanisms through which any prenatal exposure may affect offspring mental health remains a critical objective for psychiatric epidemiology. These associations may be particularly vulnerable to unobserved confounding and selection effects, most importantly by maternal mental health and behaviour. Cyclical relationships between poor perinatal mental health, social adversity, maternal stress, maternal behaviour (including alcohol and substance use), maternal care and prenatal nutrition 83 may lead to a sociodevelopmental cascade that increases exposure to adverse child outcomes (all of which have been associated with risk of mental disorders), including early life infections (with a stronger relationship between some infections and psychosis 68 rather than depression 84 ), obstetric complications 68 , 85 , altered neurodevelopment 86 , childhood adversities 87 , and behavioural and mental health difficulties 88 . If proven, this would warrant public mental health strategies focused on improving prenatal maternal, parental and familial conditions as an intervention strategy that could benefit multiple parent‐child outcomes.
Childhood adversity
Childhood adversity is an especially well‐characterized social determinant of mental ill health. Whilst no consensus definition exists, McLaughlin defines these adversities as “experiences that are likely to require significant adaptation by an average child and that represent a deviation from the expectable environment” 89, p.363 . To date, much research has focused on a “core set” of adversities that includes child maltreatment (i.e., physical, sexual or emotional abuse; neglect; exposure to domestic violence) and household dysfunction (e.g., substance use, mental ill health, or incarceration of a parent or other household member; parental separation or divorce). In a seminal study on these adverse childhood experiences 90 , they were found to be associated with a 4‐ to 12‐fold increased risk of depression, suicide attempt and substance abuse. Increasingly, the conceptualization of childhood adversity has expanded to include interpersonal adversities occurring outside of the home environment (e.g., bullying victimization) 91 .
Experience of childhood adversity is unfortunately common 89 , 92 , 93 . For example, the World Mental Health Surveys estimate that around two in five individuals have experienced at least one form of childhood adversity 94 . These experiences are clustered in patterns that are unequally distributed throughout the population 95 . In particular, greater socioeconomic disadvantage, which can place increased stress on parents and families 96 , is one of the clearest and strongest determinants of exposure to childhood adversities 95 , 97 ; recent evidence suggests that this may be mediated by effects on parental mental health 97 . Children who grow up experiencing more family discord 98 , 99 , who are born to adolescent mothers 95 , and who grow up in single‐parent households 99 are more likely to experience multiple childhood adversities. Moreover, given systemic inequalities in socioeconomic disadvantage, there is also strong evidence that women, people from ethnoracially minoritized backgrounds, and Indigenous populations are more likely to experience multiple childhood adversities 100 , 101 .
Clear and consistent evidence has demonstrated associations between childhood adversity (both prospectively‐ and retrospectively‐measured) and several poor mental health outcomes in childhood, adolescence and adulthood, including general psychopathology, depression, anxiety, self‐harm, psychosis and suicide 95 , 102 , 103 , 104 , 105 . If causal, the population‐attributable risk proportions (the percentage of disorder that could hypothetically be prevented via removal of the exposure) for childhood adversity are substantial, calculated at 28.2% of all psychiatric disorders amongst children and adolescents 92 , and 29.8% amongst adults 94 .
This epidemiological evidence strongly suggests that approaches to reduce childhood adversities and their impact are promising routes for reducing the incidence of mental disorders in the population 96 . Importantly, however, there is still much to learn about the complex relationship between childhood adversity and mental disorders. Recent findings from studies pertaining to measurement 91 , 106 and prediction modelling 107 , 108 offer important opportunities to support the development and evaluation of policies and interventions to address this widespread societal problem.
Migration
Migrants are exposed to a complex set of social determinants of mental health. This has resulted in a disproportionate burden of some mental health problems, in particular psychotic disorders. Elevated rates of psychotic disorders in migrants were first noted in 1932 by Ødergaard amongst Norwegian migrants to the US 109 , and subsequent research has highlighted the consistency of this phenomenon amongst many migrant groups and their descendants 110 , including both economic migrants 111 and refugees 112 , 113 . There is also consistent evidence of a high prevalence of post‐traumatic stress disorders (PTSD) amongst refugees and asylum seekers 114 .
Whether other psychiatric disorders – including depression, anxiety, non‐psychotic bipolar disorder, and substance use disorders – and suicide are elevated amongst migrant groups is less clear, with some evidence suggesting that the rates of these conditions may even be lower among migrants than in the non‐migrant majority population 111 , 115 , 116 , 117 . Most studies specifically concerned with common mental disorders in refugees, asylum seekers or forced migrants generally lack a comparator, but available evidence suggests that the prevalence of depression and anxiety may be higher in these displaced groups than in the general population 114 , 118 .
Several explanations for these potentially divergent results exist. These include the possibility of selection effects, so that people with pre‐existing mental health problems do not migrate. These effects are much less likely to exist amongst displaced persons. Elevated psychosis rates amongst both economic and refugee migrants may – prima facie – challenge these explanations, but younger age‐at‐migration has been associated with greater psychosis risk 119 , meaning that the influence of positive selection would be weaker amongst those who emigrate at earlier ages.
Other explanations for elevated rates of psychotic disorders in migrants and their descendants, and of several psychiatric disorders in refugees and asylum seekers, include chronic exposure to socioeconomic disadvantage and social adversities before, during and after index migration 120 , 121 . For example, migrant groups may be exposed to many social, economic, political and environmental conditions that serve as push factors prior to migration and increase risk of mental health problems. These may include poverty, lack of employment opportunities, food insecurity, conflict, violence, and natural disasters 122 , 123 . The act of migrating also involves displacement and dislocation, which may be traumatic, compromise personal safety, create uncertainty and stress, and involve prolonged separation from family 124 , 125 , 126 , and high levels of risk to life or personal safety 124 . For example, between 40 and 90% of asylum seekers report traumatic experiences during migration 118 , 122 , 127 , including violence, exploitation, and detainment during the asylum‐seeking process 128 . Finally, adapting to life in a host country can introduce challenges for migrants and refugees, including high levels of acculturative stress, exclusion from labour markets, precarious employment, housing insecurity, and socioeconomic deprivation 129 , 130 .
There is strong evidence that the post‐migratory environment is causally related to mental health problems amongst migrants and their descendants 131 . While lower rates of mood and anxiety disorders have been noted in migrants compared with the host population 132 , rates in children of migrants are similar or elevated compared with the majority population 132 , 133 . Risk of psychosis also remains elevated in children of migrants, and may persevere into the grandchildren generation 134 . Post‐migratory experiences include exposure to discrimination and structural racism 135 , 136 , 137 , 138 , 139 , and high levels of social isolation and exclusion 135 , 140 , 141 . It has been theorized that such experiences lead to psychosocial disempowerment 142 , 143 , and there is recent evidence that this pathway may explain inequities in psychosis risk experienced by both migrants and ethnoracial minoritized groups 144 . Most people also migrate with the expectation of finding better opportunities in the host country 145 , 146 , which may potentially affect mental health if they are not met 147 . Migrants also face barriers to high‐quality, timely and culturally appropriate psychiatric care 148 , 149 , 150 , affecting recovery from and long‐term consequences of experiencing mental disorder.
Ethnoracial discrimination
Ethnoracial disparities across various mental disorders have been documented for decades, independent of migrant status, especially in HICs 110 . The patterns of disparities across racial and ethnic categories are complex, with levels of psychological distress and symptoms of common mental disorders higher in minoritized groups than White groups 151 , but lower prevalence/incidence of diagnosed depression, anxiety, or substance use disorders in many ethnoracially minoritized groups 152 , 153 . In contrast, there is more consistent evidence of increased rates of psychotic symptoms and disorders in ethnoracial minoritized groups, particularly amongst groups perceived as more socioculturally distant from the racial or ethnic majority population in HICs 144 , 152 . For those with diagnosed mental disorders, there is strong evidence that many ethnoracial minoritized groups – and particularly people of Black ethnicities – experience more negative pathways into care and psychiatric treatment 154 , 155 , 156 , resulting in higher levels of morbidity 157 .
Many of these ethnoracial differences in the incidence, course and treatment of mental disorders have been linked with increased exposure to racial discrimination and structural racism among minoritized groups 144 . Socioenvironmental risk factors are thought to be driven by structural racism – i.e., by interconnected, racially inequitable systems (e.g., housing, education, employment, health care, the legal system) that reinforce each other 158 to stigmatize, discriminate and disempower marginalized people 159 .
Racial discrimination involves major events such as experiencing interpersonal racism, exclusion from labour markets, and police harassment 159 , 160 . These experiences extend to racial microaggressions, which are more subtle everyday expressions of discrimination through being slighted, made to feel inferior, stereotyped, and/or invalidated due to race or ethnicity 161 , 162 . Racial discrimination has been prospectively associated with poorer mental health and distress 163 , common mental disorders 164 , 165 , psychotic disorders 166 , and risk for conversion to psychosis among those at high risk 167 . Racial discrimination is also identified as a reason why, even among non‐poor upwardly mobile Black Americans, the risk of negative health outcomes is higher than for their poor White American counterparts 168 .
Structural racism can also increase exposure to other risk factors for mental disorders at the individual level. For example, recent research from the Adolescent Brain Cognitive Development (ABCD) study in the US 169 found that Black children were more likely to be exposed to traumatic events, family conflict and material hardship compared with White children. Black children also had lower brain volumes in key areas associated with mental health problems, including the amygdala, the hippocampus and prefrontal cortex. These race‐related disparities were attenuated after adjustment for exposure to childhood adversities. Data from the same study indicated that Black and Hispanic children are more likely to report psychotic‐like experiences than White children, and that this is partially accounted for by experiences of racial discrimination 170 . This supports further research from Europe and Brazil showing that elevated rates of psychotic disorders in several ethnoracially minoritized groups are attenuated to the null after accounting for experiences of structural inequalities (socioeconomic disadvantage, poor education, childhood adversity) and psychosocial disempowerment (discrimination, social exclusion) 144 . Further research is now required to identify the biopsychosocial pathways through which stressors associated with experiences of minoritization and discrimination shape mental health outcomes 171 .
Inequalities experienced by the LGBTQ+ community
Interest in the social determinants of health and mental health in LGBTQ+ people has surged in recent years. Acceptance and social inclusion of these people have improved consistently over recent decades, rising steadily from the late 1970s to the early 2010s 172 , and show signs of increasing further during the current decade 173 . Nonetheless, LGBTQ+ people continue to be exposed to acts of marginalization and moral panics 51 , 174 , 175 , 176 , which can have harmful effects on mental health 51 , 177 , 178 . Marginalization occurs through discrimination, stigma, anti‐queer and anti‐trans policies, bullying/harassment, and other violence occurring at both micro‐levels (e.g., microaggressions) and macro‐levels (e.g., denial of human rights and health service access) 177 , 179 , 180 , 181 , 182 , 183 , placing these people at greater risk of social exclusion and loneliness 182 . Minority stress following exposure to these experiences is thought to be a key process in determining mental health outcomes amongst LGBTQ+ people 184 , 185 , 186 , 187 , 188 .
There is substantial evidence to suggest that experiences of prejudice, stigma, discrimination, violence, and assumptions of cis‐heteronormativity (i.e., the implicit and explicit assumption and building of society which views everyone as cisgender and heterosexual) hold substantial associations with poor mental health and well‐being in LGBTQ+ people across the lifespan 178 , 189 , 190 , 191 . Parental and peer support, the formation of romantic relationships, and navigating the coming‐out process, appear to affect some of the initial mental health outcomes in LGBTQ+ youth 192 , 193 . For those who are supported in these processes, there is evidence of higher self‐esteem and lower depressive symptomatology, compared with people who do not receive such support 193 , 194 . Similarly, in recent research, navigating homophobia, biphobia and transphobia, as well as feeling unable to talk about their experiences and navigating cis‐heteronormativity, all increase the risk of poor mental health, specifically depression, anxiety and suicidality 192 , 195 , 196 . There is some evidence that mental health outcomes are worse for LGBTQ+ people who experience poverty, or who are from ethnoracial minoritized backgrounds, highlighting the intersectional ways in which social inequalities affect mental health 187 .
Sex‐based inequalities
The incidence and prevalence of many psychiatric disorders differ by biological sex. For example, depression and anxiety are approximately twice as common in women than men 197 , a pattern that seems reversed in non‐affective psychotic disorders (although this is most pronounced for first onset in early adulthood) 198 . Bipolar disorder occurs with more uniformity 198 . The lifetime prevalence of externalizing and substance use disorders is higher in males 197 , who are also more likely to die by suicide throughout the world regions 199 . The extent to which these differences are biologically and/or socially determined remains unclear for some conditions, as discussed below.
Several potential drivers for sex differences in the incidence/prevalence of common mental disorders have been proposed, including ascertainment biases, family environment, social norms, social support, hormones and neurotransmitters 200 . Although available research is limited, there is some evidence challenging the notion that these differences are solely biologically determined 200 . First, the magnitude of sex differences in common mental disorders varies substantially between countries 201 , which would not be predicted on the basis of biological determinism alone. Second, there is accumulating evidence for the causal role of certain gendered social risk factors 202 . For example, the contexts in which children grow up and are socialized, alongside differences in social and cultural norms and behaviours, are important considerations when trying to understand sex differences in mental health and disorder. Some risk factors are strongly gendered (i.e., intimate partner violence is more commonly experienced by women), and preventive efforts to tackle their causes are required in education, law and wider society 203 .
Other conditions, including eating disorders and autism spectrum disorder, have traditionally exhibited more dramatic sex differences in their occurrence, with systematic review evidence that the prevalence of eating disorders is up to four times greater in biological females than males 204 , a ratio reversed for autism spectrum disorder 205 . Recent research on this latter condition has investigated the extent to which these sex differences arise from biases in case ascertainment and detection 205 , 206 , 207 . Some evidence suggests that part of the gap could be due to the validity of diagnostic criteria and instruments used to diagnose the disorder, which prioritize symptoms labelled as male‐typic (e.g., overt restricted interests) over symptoms labelled as female‐typic (e.g., internalizing problems and emotional difficulties) 207 , 208 . Likewise, some authors have questioned whether eating disorders are likely to be underdiagnosed in biological males 206 , partly as a result of gendered social determinants including stigmatization, trauma and perceptions of masculinity.
An important consideration in understanding how inequalities contribute to sex and gender differences in mental health is that most societies are structured in ways that generally privilege cismen over all other genders, with even legal equality being achieved only in a few countries worldwide 209 . Nonetheless, the relationship between gender equality and gendered differences in mental health problems is complex. For example, wider gender gaps in depression have been observed in countries with higher levels of gender equality amongst both adults and adolescents 201 , 210 . Various theories have been proposed to explain this evidence. For example, women may experience a mismatch between expectations of equality and reality 211 , and/or face the burden of multiple roles as their involvement in the labour market increases in ways that are not matched by compensatory increases in men's involvement in domestic, childrearing and other domains 212 . Indeed, in countries with a dual‐earner model, where employment, wage earning, and domestic and childcare tasks are shared more equitably between men and women, gender inequality in mental health risks appears to be smaller 213 .
Loneliness and social isolation
Interest in loneliness 214 , 215 and social isolation 43 , 215 as social determinants of mental health and disorder has burgeoned in the last decade. The distinction between these conditions is important, and has implications for causal pathways, which have not yet been well described, as well as for targeted intervention.
While social isolation is an objective measure of the number of social connections, quantified in terms of social network size and number of meaningful ties 216 , loneliness describes the subjective and distressing mismatch between a person's desired and perceived quantity and/or quality of social relationships 217 . It is therefore possible to have a large number of social contacts but still experience feelings of loneliness, or vice versa. Transient experiences of social isolation or loneliness are common after moving house, migration or bereavement, serving as a prompt to form friendships, such that loneliness could be viewed as an evolutionary advantage in this context 218 . However, where chronic loneliness sets in, as indicated by consistent problems with fostering meaningful relationships 219 , this is more likely to adversely impact mental health. Estimates of the prevalence of loneliness internationally range from 9 to 14% in adolescents, falling to 3‐10% in middle age, and rising again to 5‐21% in older adults 220 . Prevalence estimates for social isolation (around 25%) tend to relate to older adults, and derive from low‐quality evidence 221 .
The majority of studies investigating longitudinal associations between loneliness or social isolation and mental health have focused on depression, reporting a longitudinal (and bi‐directional 222 , 223 , 224 ) association of loneliness with depression onset 214 , severity 225 and recovery 226 . Such research estimates that 11‐18% of cases could potentially be prevented if loneliness were eliminated 225 , predicated on causality. There is also evidence that loneliness is longitudinally (and bi‐directionally 227 ) associated with anxiety 214 , as well as with suicide attempt 228 . Both social isolation and loneliness are also associated with suicide among men 229 . In children, whose mental health and well‐being were a particular concern in periods of social restriction during the COVID‐19 pandemic, both loneliness and social isolation are also associated with depression onset 230 . A mediation analysis has found support for a pathway from social isolation to loneliness and subsequent depression and anxiety symptoms 223 , though again bi‐directionality was observed. Depression itself may also be a mediator of the association between loneliness and suicide attempt 228 .
For other mental health outcomes, longitudinal evidence is just emerging. Cross‐sectional research has found associations between loneliness and dementia, paranoia and psychotic symptoms 231 , but these tell us little about causal pathways. Recent longitudinal evidence is often based on selected and/or small samples, though providing some evidence that loneliness in young adults is longitudinally associated with psychotic‐like symptoms (but not vice versa) 232 . For dementia, a systematic review of mostly longitudinal studies reported stronger associations with measures of social engagement and isolation than of loneliness 233 .
Such is the interest in addressing loneliness to prevent and reduce the severity of mental health problems 234 that the UK government has issued an international review of evidence gaps with a call for researchers to address them 234 . Particular priorities in relation to mental health are understanding mechanisms, investigating the impact of loneliness and social isolation in marginalized groups, and addressing the lack of rigorous trials of psychological and social interventions to address these key risk factors. Additional gaps related to this field are estimates of the prevalence and correlates of social isolation in groups other than older adults.
Social determinants in the wider social environment
Neighbourhood socioeconomic disadvantage and inequality
Some of the earliest studies in psychiatric epidemiology investigated whether neighbourhood social determinants were associated with the incidence and prevalence of mental disorders 235 . Early cross‐sectional studies in high‐income settings identified particularly high incidence rates of some severe mental disorders – especially schizophrenia and non‐affective psychotic disorders more generally 235 , 236 , 237 – in more urban and socioeconomically disadvantaged neighbourhoods 235 , 236 . As with individual socioeconomic status (see above), these studies generated considerable debate about the relative contributions of social selection (i.e., downward drift of vulnerable individuals into socially disadvantaged environments) and social causation. This debate continues to date. While there is now consistent evidence that people who are born and raised in more urban and socially disadvantaged neighbourhoods in HICs are at greater risk of non‐affective psychotic disorders 238 , 239 , 240 , 241 , even after adjustment for individual‐level measures of socioeconomic status 239 , 240 , 241 , 242 , other research has suggested that this may be due to intergenerational selection 243 , whereby families with greater genetic liability to severe mental disorders are more likely to remain or drift into more disadvantaged neighbourhoods over time.
In the last decade, epidemiological studies that attempt to leverage genetic information to strengthen causal inference from observational data have been published on this issue, with equivocal results. For example, a nationwide longitudinal study of population density and neighbourhood deprivation at age 15 and risk for later schizophrenia (and depression) found that associations were progressively attenuated to the null in analyses restricted to first‐degree cousins and siblings 243 , who shared, on average, 12.5% and 50% of genes respectively, implying that such associations in unrestricted population samples are due to unmeasured familial confounding. Some additional studies, based on polygenic risk scores (PRS) for schizophrenia, have also found that increased genetic liability predicts living in more densely populated 244 , urban 245 , 246 and disordered 245 areas in adulthood 244 and adolescence 245 , 246 . By contrast, two studies have found no relationship between PRS for schizophrenia and population density at birth 246 , 247 . One further study found no evidence that PRS for schizophrenia predicted deprivation in adolescence 245 , although another study has shown such a relationship at birth 247 . Of these studies, three went on to test whether genetic liability confounded longitudinal associations of neighbourhood deprivation 245 , 247 and population density 246 /urbanicity 245 with psychosis risk; all found that these associations persisted after adjustment for measures of genetic liability.
Studies of other mental disorders, including depression, anxiety and bipolar disorder, have generally found less consistent gradients with neighbourhood social disadvantage and urban‐rural status 248 , 249 . Most evidence has been cross‐sectional, remains equivocal and is largely based in high‐income settings 248 , 249 . Longitudinal studies of incidence are sparse, and those that have been conducted have shown mixed results. Studies based on treated depression diagnosed in secondary care support an association with urban birth and upbringing 243 , 250 , while no such pattern has been observed in comparable studies of bipolar disorder 251 , or in longitudinal population‐based samples of depression and anxiety 252 , 253 . For suicide, there is consistent evidence that risk is elevated in more disadvantaged, socially fragmented rural rather than urban communities 249 .
Neighbourhood socioeconomic disadvantage is, of course, a multidimensional construct. Interestingly, a recent systematic review found that one aspect of neighbourhood disadvantage – i.e., perceived or objective levels of crime – was associated with several mental health outcomes, including depression, psychological distress, anxiety and psychosis 254 , suggesting that specific aspects of that disadvantage may represent putative targets for prevention. Nonetheless, the causal nature of this effect remains to be clarified, since the effects of crime were diminished after adjustment for socioeconomic deprivation, and samples where perceived crime and mental health are measured in the same respondents may be prone to both same‐source bias and reverse causality.
Another important neighbourhood social determinant, related to absolute socioeconomic deprivation, is socioeconomic inequality. The aforementioned studies typically estimated associations between average levels of neighbourhood socioeconomic disadvantage and mental health. In contrast, studies concerned with inequality seek to understand whether the unequal distribution of resources (typically based on income) within a population, community or neighbourhood is associated with health. Across HICs, there is robust correlational evidence that countries with higher levels of income inequality experience worse population mental health 255 . A recent systematic review on within‐country income inequality also found that two thirds of included studies observed statistically significant associations, with the majority (55%) supportive of a relationship between higher inequality and worse mental health (the so‐called “income inequality hypothesis”) 256 . A further 12% of studies found evidence that higher income inequality was associated with better mental health (supportive of the so‐called “mixed neighbourhood hypothesis”, which purports that the presence of people with higher income levels in a neighbourhood results in universal improvements in living standards, access to resources and health). Studies supportive of the income inequality hypothesis were more common for all outcomes studied, including depression, psychosis and general mental health, and were conducted in both HICs and LMICs 256 : Their findings persisted after control for absolute levels of socioeconomic deprivation.
Although different theories exist on how higher levels of inequality may lead to worse mental health 256 , one possible explanation is that highly unequal neighbourhoods erode levels of trust, weaken social ties, and reduce positive reciprocity, leading to greater exposure to stressogenic environments that negatively affect mental health. This raises the possibility that neighbourhood social capital and other related constructs may be important social determinants of mental health, as reviewed in the next section.
Social capital, fragmentation and ethnic density
Social capital encapsulates the nature and stock of shared social resources, relationships and networks available for groups to achieve common goals or outcomes. It encompasses concepts of trust, reciprocity, norms of behaviour, rules for cooperation, collective attitudes, shared language, and the size and structure of informal and formal networks. As such, it is a complex, multidimensional construct, theorized to operate at different levels (i.e., individual, school, workplace, neighbourhood, regional, national); be a property of individuals or groups; and have different conceptual dimensions (e.g., structural/cognitive/relational, bonding/bridging/linking 257 ). Given such complexities, it would be surprising if there was a universal effect of social capital on health. Rather, particular dimensions of social capital could be either protective or harmful, dependent on the dimension, level and/or group exposed.
Despite this challenge, a recent umbrella review concluded that higher levels of social capital were generally associated with better mental health outcomes 258 , based on a set of systematic reviews that covered psychological distress, depression and anxiety, and behavioural problems and well‐being in children. Two reviews from that paper found evidence of a stronger effect of cognitive (shared language, values and codes) than structural (networks, rules, roles) social capital on common mental disorders 258 .
To our knowledge, systematic review evidence on social capital and suicidal outcomes is missing. Most studies in this space are ecological 259 , 260 , 261 , 262 , 263 , with several reporting national 263 , regional 261 , 262 or neighbourhood‐level 259 associations between higher levels of social capital (particularly trust) and lower suicide rates. Nonetheless, effect sizes for suicidal outcomes appear modest, and are often limited to – or stronger in – various subgroups, including White men and women 261 , non‐Hispanic Black groups 262 , men alone 262 , younger groups 259 or unmarried people 259 , or are sometimes not found at all 260 . One of the few longitudinal studies conducted to date reported that higher structural social capital was associated with lower suicide rates in South Korea 264 , but further high‐quality evidence is required.
A recent scoping review of social capital and psychosis found mixed evidence of an association 257 , with considerable heterogeneity in study design, definitions of social capital, assessment instruments, setting, control for confounders, and findings. As with other mental health outcomes, longitudinal evidence is generally missing. Of nine studies, four reported an overall protective effect of higher social capital on psychosis risk, two found null results, and three reported subgroup or nonlinear effects; here, protective effects were restricted to women 265 , those with a family history of psychosis 266 , or people living in areas with either the lowest or highest levels of social capital 267 , especially among ethnoracially minoritized groups.
These subgroup and curvilinear effects may provide important opportunities to triangulate evidence about how exposure to contextual factors in the social environment generates inequalities in mental health between different groups. In the example above, from the ÆSOP study of first‐episode psychosis in Southeast London 267 , rates of schizophrenia were higher for people living in low or high social capital neighbourhoods, compared with moderate levels. Social capital was estimated in a random sample of residents via a separate cross‐sectional survey. Importantly, response bias meant that White residents were over‐represented in the survey, biasing estimates of social capital towards those perceived by this group. In areas with high social capital – as disproportionately perceived by White respondents – psychosis rates were only substantially elevated amongst ethnoracial minoritized residents, who may have been excluded from accessing this social capital. Interestingly, this has recently been replicated in longitudinal research from Sweden amongst people with a migrant heritage 268 , and similar findings have been observed in other contexts 269 .
These findings may provide a mechanistic explanation for observations from a related literature that higher levels of ethnic density – the degree to which one's ethnoracial group is represented in a neighbourhood – are associated with lower levels of psychosis 270 . Such findings also extend to migrants 271 . Ethnic density is theorized to have a protective effect on mental health via increased social capital (particularly bonding social capital) amongst people who share more similar language, norms, codes, customs and cultural backgrounds. These resources may help buffer against social stressors 144 , 272 . Relatedly, higher rates of psychosis are observed in more socially fragmented neighbourhoods 273 , an effect that appears to persist at school level for young people 274 . A systematic review 275 has demonstrated that evidence for a protective ethnic density effect is strongest for psychosis 270 , 276 , and extends to suicide 277 , 278 , 279 , but is less consistent or strong for anxiety and depressive disorders. Recent systematic review evidence also suggests that the protective effect of high ethnic density on psychosis risk is more consistent for Black and Latino populations, with mixed findings for Asian ones 270 .
Ethnic density and social capital may be particularly important during childhood. For example, one study found evidence that low ethnic density during childhood was associated with later increased psychosis risk 276 . This may be linked to greater social and cultural isolation, or increased exposure to other risk factors for mental health problems, such as bullying 280 . There is also longitudinal evidence that social capital in childhood buffers the impact of earlier childhood adversity on adolescent mental health problems 281 . Recent cross‐sectional data from the National Comorbidity Survey (Adolescent Supplement) in the US also suggest that both school‐level bonding and perceived neighbourhood social capital are associated with lower risk of mood and anxiety disorders in young people 282 .
As with social capital, the relationship between ethnic density and mental health outcomes may be nonlinear 283 . Very high levels of ethnic density (>80%) are indicative of racial segregation 283 , and may be related to poorer mental health for Black Americans and Asian Americans in the US 283 , as well as for some South Asian groups in the UK 284 . In this latter country, mental well‐being was found to be poorest for people living in the most segregated communities, an effect larger for Black participants and independent of ethnic density 285 . In highly segregated neighbourhoods, the buffering effect of high ethnic density may be eroded as exposure to a range of other risk factors for mental health problems increases, including social exclusion, deprivation, discrimination, violence and crime. These social determinants tend to arise as downstream effects of interpersonal, institutional and structural processes and policies that govern patterns of residential organization 286 .
Physical environment
Physical environment encompasses the built environment (housing quality, density and type; urban design), exposure to pollution (particularly air and noise pollution), access to green and blue space, and climate change. We consider physical environment as a potential social determinant of mental health because exposure to protective or harmful physical environments is rarely randomly distributed within or between populations. Rather, exposure is influenced by many factors already described in this paper, including socioeconomic position, minoritization, and structural discrimination in policies, institutions and systems that govern (in)equitable access to housing, education, employment and income 287 . Given the high correlation between physical and social environmental adversities, teasing out their causal mechanisms remains a challenge, which has led two systematic reviews conducted in 2007 288 and 2018 289 to conclude that there was a lack of robust research on the role of physical environment in mental health, with a particular paucity of high‐quality longitudinal research.
Nonetheless, some evidence supports an association between mental health and specific aspects of the physical environment. For example, longitudinal research suggests that housing regeneration programs are associated with improvements in depression, anxiety and general mental health outcomes 55 , 288 . Housing disadvantage is also associated with worse mental health in longitudinal research 55 , and may lead to increased residential mobility during childhood, which itself has been longitudinally associated with more emotional and behavioural problems 290 , depression 290 and psychosis 291 later in life, independent of material disadvantage, education and social adversities. In further longitudinal research, children growing up in poorer built environments experienced more emotional symptoms and conduct problems at age 3 years 292 .
Exposure to some air pollutants has been associated with mental health and disorder, including in case‐only study designs (i.e., self‐controlled case series, case‐crossover designs) that control for short‐term time invariant confounders 293 . A systematic review of the effects of particulate matter (PM2.5 or PM10, i.e. finer than 2.5 or 10 microns in diameter) reported consistent evidence that short‐ and long‐term exposure to PM2.5 was associated with increased risk of depression and anxiety, while short‐term exposure to PM10 was associated with suicide risk 293 . The depression association has since been confirmed in a subsequent review 294 , and may extend to other air pollutants, including ozone (O3) and nitrogen dioxide (NO2). However, limitations remain, including publication bias, failure to consider multiple pollutants simultaneously, and a predominantly Global North focus (although with exceptions 295 ). It also remains unclear whether observed associations are mediated by effects of pollution on physical health, particularly on early life neurodevelopment 296 , 297 . Systematic review evidence supports a link between prenatal/perinatal exposure to PM2.5 and risk of autism spectrum disorder in offspring 298 . Findings for other mental health outcomes remain sparse, although there is emerging evidence of a relationship between nitrogen oxides and psychosis 299 , 300 .
Evidence on the association of green and blue space with mental health is predominantly based on heterogeneous measures, unrepresentative samples, and cross‐sectional study designs, resulting in mixed findings 301 , 302 , 303 , 304 . Overall, there are currently insufficient high‐quality data to support this association.
Interest is growing in the role that climate change may have on mental health. Various mechanisms may be involved, from increased anxiety or depression arising from existential concerns for the future, to exposure to social adversities arising as a result of climate change, including job loss, housing insecurity, displacement, food insecurity and conflict. While high‐quality direct evidence of an impact of climate change on mental health remains missing, our review highlights how social adversities that may occur following climate change could exacerbate mental health inequalities.
A PREVENTIVE FRAMEWORK FOR POPULATION MENTAL HEALTH
Preventive approaches are paramount to enable meaningful progress in reducing the prevalence and impact of social determinants that negatively affect population mental health. Prevention in psychiatry encompasses the mitigation or removal of risk modifying factors and the enhancement of protective factors linked to mental disorders 305 . Here, the goal is to lower the incidence, prevalence and recurrence of mental disorders, and the burden placed upon individuals, their families and wider society 306 . Given the huge direct and indirect costs of mental disorders to individuals and to society 307 , there are strong ethical and economic cases for prevention in psychiatry 308 . However, there are also costs to prevention, some of them paradoxical, which we consider below.
Prevention strategies are best grounded in a thorough understanding of the epidemiological characteristics of the relevant condition, and a working – although not necessarily perfect – model of causation 309 . We recognize that screening, early detection, and diagnostic testing are essential aspects of an effective prevention strategy for mental ill health 310 . While other reviews have considered these clinical tools in great detail 311 , 312 , we restrict our review of such tools to those that explicitly aim to intervene on social determinants of mental ill health.
Frameworks for prevention
The WHO recognizes three levels of prevention: primary, secondary and tertiary (see Table 1). Whilst the latter two prevention levels are critical for reducing the burden of mental disorders through early intervention (secondary prevention) and ongoing management (tertiary prevention), action regarding social determinants falls mainly within the domain of primary prevention. Therefore, although we briefly overview evidence from all three levels in the following section, we devote most of our attention to primary prevention.
Table 1.
World Health Organization's classification of preventive approaches for mental disorders (adapted from Fusar‐Poli et al 312 )
| Public health framework | US Institute of Medicine |
|---|---|
| Primary prevention aims at preventing the new onset (incidence) of one or more mental disorders, or of suicidal ideation. | |
| Universal prevention targets the general public, or a whole population that has not been identified on the basis of increased risk. | |
| Selective prevention targets individuals or subgroups of the population whose risk of developing a mental disorder is significantly higher than average, as evidenced by biological, psychological or social risk factors. | |
| Indicated prevention targets high‐risk people who are identified as having minimal but detectable signs or symptoms foreshadowing mental disorder, or biological markers indicating predisposition for mental disorders, but who do not meet diagnostic criteria for disorder at that time. | |
| Secondary prevention aims to lower the prevalence of established cases of the disorder or illness in the population (prevalence) through early identification and treatment of diagnosable diseases. | |
| Tertiary prevention includes interventions that reduce disability, enhance rehabilitation and prevent relapses or recurrences of the illness. |
Primary prevention focuses on preventing the onset of mental disorders. This level of prevention includes universal, selective and indicated strategies, with interventions classified on the basis of the risk of individuals or sub‐populations to develop a mental disorder.
Universal prevention strategies focus on entire populations, agnostic to risk status. Classic examples include fluoridation of drinking water to prevent dental caries, or folic acid fortification in flour to reduce neural tube defects during embryogenesis 313 . In a mental health context, examples may include teaching school children about emotions and mental health, or the introduction of a universal basic income, which aim to prevent mental disorders in addition to potentially bringing wider benefits to society. However, the potential benefits of any population‐centred approach need to be tempered by the fact that modifiable risk factors are usually distributed unequally. Some people are at high risk, whereas most have a lower baseline risk of developing a disorder. In other terms, most of the burden of mental disorder in the population comes not from the small proportion of people at the highest risk, but rather from the far larger proportion of people with moderate or slightly above‐average risk. The use of universal preventive interventions, therefore, has unequal costs and benefits in different individuals.
G. Rose, a British epidemiologist, considered the implications of this 309 . He noted that, when we study disease incidence in a single population, we see determinants – genetic or environmental – of the position of individuals within the risk distribution. However, this can leave us blind to huge differences in risk and disease incidence that may exist between populations, even though the individual determinants may be similar in both. These differences between populations, summarized by the population mean of a normally distributed risk factor, can be due to factors that are distinct from those that determine individual risk within those populations; individual risk can be understood only within that wider context. The crux of Rose's argument is that more cases of a disorder may be prevented by focusing on shifting the population mean (or other measure of central tendency) to make the whole distribution of the sicker population's risk profile look more like the healthier's one, rather than by targeting the minority at very high risk in the population (see Figure 1). The “prevention paradox” is the potential downside of this strategy; while the prevention may come with some costs for all – even if only a matter of inconvenience – most individuals will receive little to no benefit from the intervention, even though the benefits for the population as a whole may be large 314 .
Figure 1.
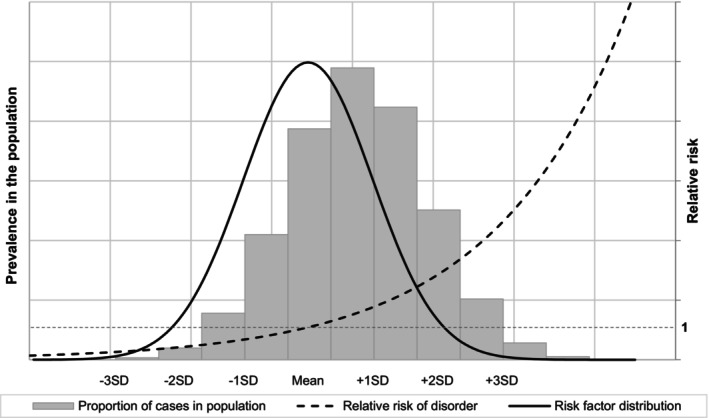
Hypothetical relationship between a normally distributed risk factor, relative risk of mental disorder and the proportion of cases in the general population. A risk factor for mental disorder is normally distributed in the population with a hypothetical mean and standard deviation, SD (bell curve indicated by solid black line). That risk factor is associated with a hypothetical relative risk of mental disorder, indicated by the dashed black exponential curve. For convenience, we set the relative risk to be 1 (grey dashed horizontal line) at the mean level of exposure to that risk factor. The hypothetical proportion of cases that arise in the population are indicated by the grey bars. Under these assumptions, most cases of disorder in the population will occur for those only exposed to moderate levels of the risk factor (from the mean to +2 SD above the mean). Fewer cases will be generated by the small proportion of the population beyond +3 SD above the mean, even though they are at substantially greater relative risk. Thus, following G. Rose's argument 309 , more cases of disorder in a population may be prevented by intervening at lower levels of exposure in the general population than by targeting high‐risk groups. This hypothetical argument has been confirmed in psychiatry (see, for example, Polek et al 315 ).
Much of Rose's work considered physical health, particularly cardiovascular disease, but he believed that the same principles would apply to mental disorders. As an example, Polek et al 315 showed the implications of a normally distributed risk factor (e.g., mental distress) for the occurrence of suicidal thoughts and non‐suicidal self‐injury in a sample of adolescents and young adults. While those with very high distress values (three standard deviations above the mean) are at highest relative risk, the majority of these outcomes occur in those at medium risk – one or two standard deviations above the mean. If the whole population distribution could be shifted to the left, then more occurrences of suicidal thoughts and non‐suicidal self‐injury would be prevented than using a strategy focused on the few at highest risk 315 . The full implications of this approach are yet to be explored throughout preventive psychiatry, but there is clear evidence that this is likely to be a fruitful area for important public mental health concerns, including common mental disorders 316 , 317 and suicidality 315 , 318 . The implications are increasingly discussed 310 , 319 , but may only be fully appreciated when large‐scale prevention studies focusing on common risk factors for multiple outcomes include measures of mental health routinely.
Although a strong proponent of universal approaches, Rose acknowledged that an effective prevention strategy should also encompass selective and indicated approaches 320 . Selective prevention strategies target individuals or sub‐populations who have higher risk than the general population for onset of mental disorder. This risk may be assessed using a biopsychosocial model, through the evaluation of biological, psychological or social risk factors for mental ill health in individuals or subgroups of the population. Intervening in this way, particularly if early in development, may serve to interrupt some of the pathways that lead from risk factors to mental disorder. Indicated prevention refers to interventions designed for high‐risk populations who are already identified as having symptomatology of mental disorder, but whose symptoms are sub‐threshold for diagnosis.
Importantly, different levels of prevention may be additive, such that an individual may at once be the target of multiple levels of prevention strategies. This is perhaps demonstrated most clearly in schools, where so‐called “multi‐tiered systems of support” offer a gradated approach to student mental health, whereby all students receive universal interventions, and a smaller proportion are offered selective and/or indicated interventions, depending on risk status 321 . Such approaches can be adapted depending on context 322 .
Prioritizing primary prevention
As we argue throughout this paper, social determinants represent some of the most modifiable intervention targets in a field where the development of new treatments for established disorders has largely stagnated. In contrast to other areas of medicine in which preventive approaches have established strong roots, approaches to prevention in psychiatry are inequitably prioritized, with the majority of available resources devoted to secondary (and tertiary) treatment of existing mental disorders (and their consequences), rather than preventing the onset of new disorders 323 . The dearth of action on primary prevention in mental health has been recast as one of the grand challenges in global mental health 324 , and very likely hinders progress in reducing the incidence, prevalence and burden of mental disorders that afflict society 319 .
PREVENTION STRATEGIES THAT ADDRESS SOCIAL DETERMINANTS: THE EVIDENCE
In this section, we use the preventive framework introduced above to review evidence for the efficacy of prevention strategies that target some of the major social determinants of mental health outlined earlier. We principally focus on primary prevention strategies, including universal, selective and indicated approaches. We also briefly review important secondary and tertiary prevention strategies that aim to promote recovery in those with established conditions. We focus on prevention strategies where we believe evidence is strongest (summarized in Figure 2), based on systematic reviews, randomized controlled trials (RCTs) or quasi‐experimental evidence, where available. Additionally, we highlight areas where the evidence base is weaker, equivocal or absent. We also draw the readers’ attention to reviews and reports of prevention strategies that aim to promote mental health and reduce mental distress and disorder 312 , 325 , 326 , 327 .
Figure 2.
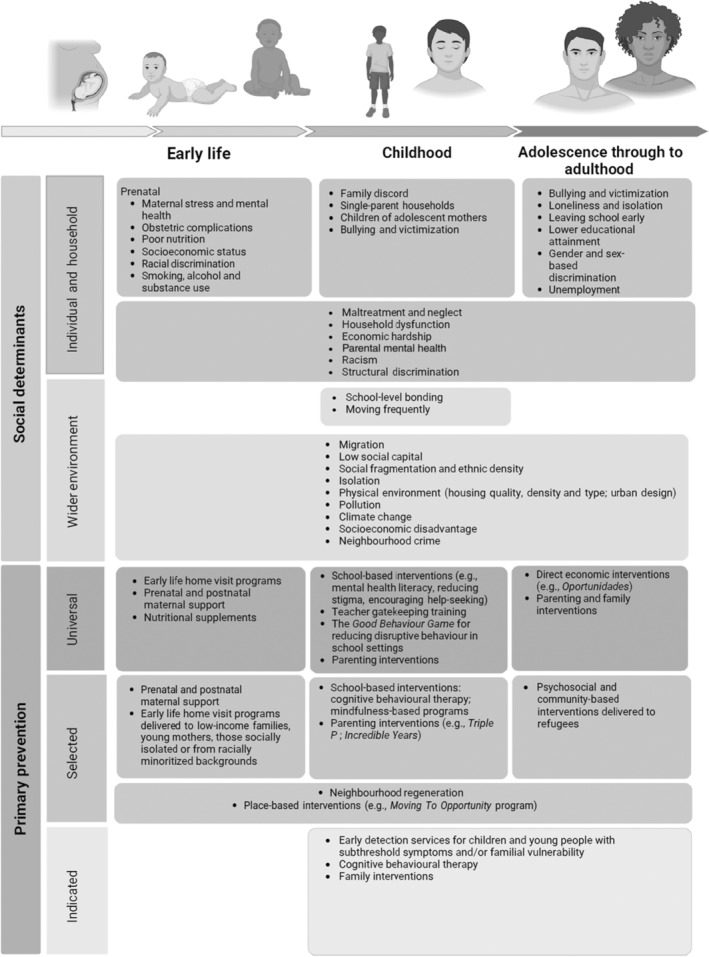
Summary of the social determinants of mental health and disorder and of the main primary prevention strategies
We believe that the strategies that are particularly crucial for effective public mental health promotion and prevention are those which target social determinants in the early life course, beginning prenatally and extending into infancy, childhood and adolescence. There are several reasons to support this: a) 50% of all mental health conditions begin by age 18 19 ; b) many of the antecedents of mental disorders begin early in life; c) preventing the onset of these problems earlier provides the best opportunity to interrupt intergenerational transmission of cyclical relationships between social determinants and mental health problems; d) the incidence and prevalence of mental health problems and disorders amongst children and young people is increasing, making this an imperative matter of social justice.
Universal prevention strategies
Parenting interventions
Parents play a crucial role in the emotional and behavioural development of a child. Consequently, many programs have been developed to enhance positive aspects of the parents’ influence. Proactive and positive parenting techniques increase parent‐child attachment and build self‐esteem and confidence, which reduce behavioural problems 328 , 329 . The most common parenting programs are group‐based, which may be a cost‐effective method of reaching their goals, and last 8‐12 weeks, with 1‐2 hour sessions weekly 328 , 329 .
Evidence consistently supports the efficacy of these programs in improving child mental health. For example, a systematic review of 24 intervention trials of short‐term group‐based parenting programs for children under 4 years old found that the programs had beneficial effects on overall child mental health and behaviour, as well as on parent‐child interaction 329 . There is further systematic review evidence that two of the most common parenting interventions – the Triple P program 330 and the Incredible Years program 331 – reduce disruptive behaviour in this age group. The effects of parenting interventions may be more pronounced for externalizing than internalizing symptoms 329 , although there is also strong systematic review evidence from RCTs supporting beneficial effects for the latter 332 . A remarkable finding from one review was that the estimated number needed to prevent one case of adolescent anxiety was only 10, a number which is much smaller than that for many common medical interventions 332 . With that in mind, it is perhaps not surprising that cost‐benefit analyses of common parenting programs demonstrate cost savings 330 .
A recent trial described a short (four 90 min sessions) perinatal parenting intervention that focused on sharing and understanding parenting roles in a co‐parenting model 333 . The intervention aimed to reduce parenting stress to improve child outcomes. When the child was aged 1 year, parents in the intervention arm rated their offspring as having lower negative emotionality and lower externalizing symptoms, although these effects did not extend to age 2 years, 20 months after the program conclusion.
There is also evidence from a review of 48 trials that parenting interventions lead to benefits for parents as well as children, including reductions in parental depression, anxiety, stress, anger and guilt, and increases in confidence and relationship satisfaction 328 . Perhaps as a consequence, studies of the Triple P parenting program have also shown that participation is associated with reductions in child abuse and maltreatment 330 . From a global perspective, it is reassuring to see that parenting programs implemented in HICs have similar positive outcomes in lower‐income settings such as sub‐Saharan Africa 334 .
Several key questions remain about optimizing parenting interventions, including whether effects persist in the absence of the intervention over the long term (observed by one 332 but not other reviews 328 , 335 ), the ideal age to intervene (with evidence of beneficial effects associated with interventions in both childhood 331 and adolescence 332 , 336 ), and whether they should be deployed universally or to selective populations (bigger effect size of parenting interventions have been found for high‐risk families 332 ). Another set of related early‐life interventions – home visits during pregnancy – have been deployed as more selective prevention strategies, reviewed later.
School‐based mental health programs
Schools are potentially optimal settings for public health practitioners to provide universal mental health promotion and prevention. Numerous such programs have been designed for school children, and may be adapted to offer nested selective and indicated interventions.
Many school‐based programs focus on mental health literacy, with the aim of educating youth about mental health, reducing stigma related to mental disorders, and encouraging help‐seeking behaviour 337 . A recent systematic review of RCTs showed that these programs increase mental health literacy and reduce stigma, although there is a lack of evidence on whether these effects persist over the long term 337 . Whether they increase help‐seeking behaviour remains unclear 338 .
School‐based interventions that focus on reducing disruptive behaviour have existed for many decades. A 2011 umbrella review concluded that these programs are effective in reducing externalizing problems 339 . The Good Behaviour Game, for example, was developed in 1969, and is a team‐based activity designed to reward children for pro‐social behaviour and discourage disruptive behaviour 340 . RCTs have shown that the Good Behaviour Game is effective in reducing conduct problems in children 340 . Although the primary focus is on behavioural regulation, the program also supports emotional regulation. A recent Australian trial showed that the program also decreased internalizing symptoms 341 . Remarkably, one study followed up students at age 21/22 who had participated in the program in school when aged 6 years, and found that participants were less likely to report suicidal thoughts and attempts compared with controls 342 .
There are several school‐based programs that specifically focus on prevention of depression and anxiety. A 2017 systematic review (updated in 2021) summarized evidence from 90 intervention studies 343 , 344 . The majority of interventions were based on 8‐12 sessions of 45‐90 min of cognitive behavioural therapy (CBT), modified for the classroom 344 . The review clearly showed that these programs were effective in reducing symptoms of depression and anxiety, though effect sizes were generally small 343 , 344 . Although such programs are often delivered universally, effect sizes for depression were larger for trials that targeted higher‐risk student populations (i.e., selective and indicated approaches) 343 , 344 . Notably, while effect sizes for preventing depression and anxiety were relatively small, they persisted in long‐term follow‐up 343 , 344 . Furthermore, the authors of the 2017 review point out that even small effects can have big impacts on prevention from a population perspective 344 , aligning with Rose's argument. Relevantly, a 2016 review estimated that universal prevention programs of depression and anxiety delivered in schools (mostly CBT‐based) prevented 50% of cases of a diagnosable internalizing disorder in the following 6 to 9 months 345 .
Recently, several mindfulness‐based programs have been developed and trialled for school‐aged children 346 . Mindfulness approaches encourage people to intensely focus on the present moment, in order to calm physiological responses and reduce stress. A 2022 systematic review of 66 RCTs found that mindfulness programs for children are successful in reducing anxiety/stress (analyzed as a combined outcome) and depressive symptoms 346 , although effect sizes tended to be small and were limited to selective rather than universal samples. Trials in universal samples found no evidence of improvements in mental health, despite small improvements in behavioural outcomes, executive function and attention. Further, there were no positive effects in studies that included follow‐up beyond program conclusion 346 .
Another group of school‐based mental health programs focus specifically on suicide prevention. These programs tend to take three forms: a) awareness and education initiatives, which seek to inform students about suicidal behaviour to reduce stigma and increase likelihood of help‐seeking behaviour; b) gatekeeper training, which seeks to teach students or teachers to identify signs of suicidality, and refer students to appropriate services; and c) screening programs, which seek to identify risk factors for suicide or suicidal thoughts, with the aim of referring people who screen positive for further assessment and/or treatment 347 , 348 . Several reviews have concluded that these programs are successful in reducing suicidal thoughts, including 12 months after program completion 347 , 349 . The most recent review concluded that similar effects are seen for suicide attempts, with some evidence that these effects may last for up to 20 years 348 .
As with many school‐based interventions, suicide prevention programs are most successful when they are multi‐faceted 347 . One excellent example is the Saving and Empowering Young Lives in Europe (SEYLE) program, a suicide prevention RCT implemented in 168 schools across 10 countries 350 . The intervention included training teachers and school staff to be gatekeepers, delivering a mental health and suicide literacy program for students, and screening for high‐risk students. At 12‐month follow‐up, participants in intervention schools were 50% less likely to have experienced suicidal thoughts and suicide attempts in the previous two weeks compared with students from control schools 350 .
Several reviews have highlighted that little evidence exists on cost‐effectiveness of school‐based programs in prevention of mental health problems 337 , 344 . One review on prevention of depression and anxiety in schools estimated that the number needed to prevent one case per 100 children was 70 students 345 , while the authors of the SEYLE trial concluded that the program could prevent one suicide attempt for every 167 students who participated in the program 350 . Depending on the resources required for these programs, these prevented outcomes could represent important cost savings. Nevertheless, rigorous economic evaluations are needed, particularly those that take a long‐term perspective. An additional limitation of research on school‐based interventions is that few studies have included functional assessment; a recent commentary argued that measuring function may better reflect the success, or lack thereof, of programs whose aim is to allow children to flourish 351 .
Finally, it should be noted that the overwhelming majority of studies in this area are from HICs, although available evidence suggests that schools are also a suitable setting to deliver mental health promotion interventions in LMICs 322 . On the other hand, rates of school enrollment vary dramatically between countries, and it cannot be excluded that school‐based programs inadvertently exacerbate mental health inequalities for those unable to access basic education. Moreover, recent concern has been raised that some aspects of school‐based mental health interventions could increase levels of distress amongst some young people 352 . This requires further investigation so that safety can be fully balanced alongside demonstration of efficacy.
Interventions that address loneliness
The evidence base is weak for preventive interventions that address loneliness, in order to prevent onset of mental health problems, or to reduce severity or improve prognosis of pre‐existing mental disorders. Such interventions might be best situated among universal approaches, given that the stigma of loneliness dissuades uptake of targeted interventions, but in reality they may need to straddle universal, selective and indicated approaches. Built environment interventions to address loneliness and mental health, whilst showing promise in terms of acceptability, have no evidence of effectiveness 353 . Systematic reviews of trials of interventions addressing loneliness do not include mental health impacts. Consequently, we need investment in evaluations that encompass both physical and mental health 354 .
Selective prevention strategies
Direct economic interventions
Given the demonstrably strong links between poverty, socioeconomic disadvantage and poor mental health reviewed earlier, selective interventions that improve people's socioeconomic position could be crucial policy levers to improve population mental health. Although economic inequality primarily affects the health of the poorest, it is also linked to worse mental health of the whole population 256 , 355 . This suggests that interventions that reduce inequality by targeting selective or indicated groups could even have universal mental health benefits. There is already evidence that policies driven by progressive welfare economics are associated with fewer mental health inequalities according to socioeconomic circumstances 356 , 357 . A recent systematic review of 136 studies found that increases in individual and household income improved mental health and well‐being, while decreases had the opposite effect 49 . These effects were strongest when individuals were lifted out of poverty.
This evidence has added to debate on whether guaranteed incomes or cash transfers have beneficial effects on mental health. From 1974 to 1979, a guaranteed annual income experiment in rural Manitoba, Canada, ensured that families met at least 60% of what Statistics Canada considered the cut‐off to be designated as a low‐income family. Evaluations later showed a statistically significant reduction in hospitalizations during the program, primarily related to mental health, and this effect persisted for at least 6 years after program completion 358 .
Much of the research on the potential benefits of cash transfer programs have focused on child and adolescent mental health. For example, a recent systematic review found causal evidence that adolescent mental health (specifically, internalizing problems) improved when their families were lifted from poverty 359 , and a review of child benefit programs introduced in Canada since 1945 showed that they had positive effects on child mental health and behaviour 360 .
It should be noted, however, that the success of cash transfer programs may vary according to economic context, gender, implementation of program, and local culture 361 . For example, the aforementioned systematic review on changes in income and mental health found stronger effects of poverty alleviation programs on mental health in LMICs 49 , and other reviews have found similar positive effects for cash transfer programs in these contexts in adults 362 and children 359 , 361 . These effects may be long‐lasting. For example, a cash transfer program in Kenya showed that, 4 years after program implementation, youth whose families participated in the program had significantly fewer depressive symptoms 363 . Similar findings may also extend to low‐income settings in HICs. For example, a natural experiment in the US investigated the role of income supplementation on child mental health following the opening of a casino on American Indian reserve land 364 . It demonstrated that children who were lifted out of poverty had statistically significant reductions in symptoms of conduct and oppositional defiant disorders compared with those who remained in poverty, falling to levels seen amongst children never exposed to poverty in the same region 364 .
Some cash transfer programs include mandatory conditions for recipients. Oportunidades, one of the first conditional cash transfer programs, was implemented in Mexico, and supplemented participants’ income by 20‐30% on the conditions that children were enrolled in school, and that family members took part in preventive medicine programs and attended health‐related presentations. For families who enrolled when their child was less than 2 years old, children had fewer behavioural problems when aged 8‐10 years compared with children who were enrolled in the program 18 months later 365 .
Critics of conditional cash transfer programs have pointed out that they are highly paternalistic in nature, exacerbate gender‐based inequalities, and do not solve structural problems that lead to long‐term poverty 366 . Indeed, one systematic review found that placing conditions on monetary interventions may have detrimental effects on adolescent mental health in some sub‐populations, in particular girls, for whom conditional cash transfers may add to existing pressures including household duties and caring responsibilities 359 .
Early‐life home visit programs
As evidence has accumulated supporting the effects of perinatal stress on brain development 367 , public health practitioners have focused more attention on supporting healthy development early in life. Home visitation programs for pregnant or post‐partum mothers, their partners, and their children have often been delivered to selected populations at risk of experiencing considerable social disadvantage, adversity and negative health outcomes. These groups have often included low‐income families, and mothers who are young, unmarried, socially isolated or from ethnoracial minoritized backgrounds 368 .
Home visitation programs vary in delivered activities, but the general aim is to improve the home environment for the new child. These programs often include aspects of social support for new parents, education about child development, informal training about positive parenting techniques (and avoidance of negative parenting behaviours), and facilitation of mother‐child interaction. This is important because different parenting practices have been consistently associated with levels of child aggression, delinquency and socioemotional functioning, with authoritarian (e.g., harsh) parenting styles leading to poorer child outcomes than authoritative (e.g., affection balanced with discipline) approaches 369 . A systematic review of 34 RCTs and quasi‐experimental studies that investigated the effect of home visitation programs found that they resulted in improvements in the home environment, particularly in studies that used robust measures of parenting behaviours 368 .
Some notable RCTs in the US have examined perinatal monthly home visit interventions by nurses. For example, in a trial conducted in Memphis, TN, women received nurse visits during pregnancy, immediately post‐partum, and several times until the child's second birthday, while the control group received usual perinatal care 370 . At age 6 years, children of mothers who received the nurse visits had fewer behavioural problems and were less likely to be aggressive. In another trial in rural New York state, women at higher risk of mental health difficulties due to their social position were randomized to receive nurse home visits until the child's second birthday or treatment as usual 371 . At age 15 years, children of mothers who received nurse visits drank less alcohol and were less likely to be involved in criminal activity compared with children in the control arm; this intervention was also highly cost‐effective, with a return on investment realized by the time the child reached age 4 years. This intervention continued to exhibit marked dividends into adolescence, through reduced welfare and justice system involvement 372 . A similar intervention study in Australia, that also included monthly nurse home visits for the first two years of the child's life, showed that children of mothers who received nurse visits had overall lower scores on the Strengths and Difficulties Questionnaire, indicating fewer emotional and behavioural problems 373 . Interestingly, the same study showed positive outcomes for parents across a wide range of domains, including less hostility, less parent‐child conflict, higher well‐being and quality of life, and increased self‐efficacy. Whether such interventions would show the same effect if implemented universally remains unclear.
Neighbourhood interventions
The neighbourhood may offer an effective level at which to prevent mental disorders and promote mental health. Nonetheless, designing, testing and implementing interventions which seek to modify social or physical environments in order to improve public health is notoriously difficult. For this reason, most research to date remains observational 353 , 374 .
The classic example of an RCT to lift people out of neighbourhood poverty is Moving To Opportunity, conducted in five US cities, in which families in high‐poverty neighbourhoods were randomized to receive housing vouchers to move to low‐poverty neighbourhoods 375 . At 3‐year follow‐up, there was evidence of reduced distress/anxiety symptoms amongst parents in the intervention arm, and reduced depressive/anxiety symptoms in children, though these results were restricted to boys and younger children (8‐13 years) 375 . Nonetheless, later follow‐ups have found differential effects on adolescent mental health, including higher risk of conduct disorder, PTSD and depression in boys, and lower risk of conduct disorder in girls in the intervention arm 376 , 377 , 378 . The reasons for this are likely to be multifaceted, but may include sex‐specific differences in interactions with new social environments, including the social skills required to navigate more affluent environments, or the consequences of increased residential and school moves on social integration and support 378 . Such issues further highlight the potential unintended harms that may result from some forms of intervention that attempt to lift people out of poverty.
Neighbourhood regeneration programs 379 have been rarely tested. One exception is a cluster randomized trial in Philadelphia 380 , which reported lower depressive symptoms and improved self‐worth amongst residents in intervention settings where a greening initiative focused on improving the physical quality of the built environment by planting trees, removing litter, and landscaping vacant land in urban settings. A recent review of interventions to promote housing affordability and stability found no evidence of improved mental health outcomes in selective populations (particularly homeless and Veteran groups) 381 .
The paucity of evidence for neighbourhood interventions reflects the complexity of delivering such interventions and their possible unintended consequences, despite evidence that neighbourhood social disadvantage, fragmentation and social capital are significantly associated with mental health.
Public mental health interventions for specific populations
Several minoritized groups are at increased risk of developing mental health problems and disorders, so selective interventions in these groups may be particularly effective in reducing mental health inequalities at the population level. One clear example is providing interventions to refugee groups who are vulnerable to worse mental health. There is systematic review evidence from RCTs that providing psychosocial interventions to refugees is effective in reducing PTSD symptoms 382 . Encouragingly, brief individual 383 or group‐based 384 , 385 psychological and behavioural interventions appear to reduce depressive and internalizing symptoms in refugees, including children 386 and adolescents 384 , though these may not be sustained in the long‐term post‐intervention 385 , and some evidence is of low quality 386 . A recent systematic review also found evidence that community‐based interventions which provided refugees with greater bridging and linking social capital (i.e., building ties with others in the community, helping them navigate new structures, systems and institutions) may be most effective in reducing mental health symptoms in this population 387 . Nonetheless, the variable quality and small number of studies included in these reviews requires this promising evidence base to be strengthened.
Selective interventions in ethnoracial minoritized groups have also been investigated. In many contexts, the intersectionality with socioeconomic disadvantage means that interventions targeted at low‐income parents, families or neighbourhoods are sometimes implicitly selected on a high proportion of people from ethnoracial minoritized backgrounds 371 . Generally, evidence suggests that these interventions are effective in benefiting mental health across different ethnic groups, including the aforementioned Incredible Years parenting intervention in both European 388 and North American 389 settings. While these studies lend some support to the effectiveness of culturally‐agnostic interventions, there is also evidence that culturally‐adapted mental health interventions offer more benefits in some ethnoracial minoritized groups over non‐adapted treatments or treatment‐as‐usual 390 , 391 . Further, given that experiences of discrimination and stigma operate at various levels as barriers to mental health help‐seeking, understanding how cultural and structural factors intersect to produce mental health inequalities in ethnoracial minoritized groups remains a critical prerequisite to developing effective selective interventions that reduce these experiences and promote mental health 392 .
There is also emerging evidence that selective interventions for sexual and gender minority groups can be effective in improving mental health outcomes 393 . These include policy‐level interventions, family interventions, and provision of coordinated mental health services, with evidence of beneficial effects on mental health, substance use and bullying victimization amongst minoritized youth 393 . Others have highlighted the importance of building up cultural competence amongst health care professionals as a vital intervention to reducing mental health inequities for LGBTQ+ people 187 . Nonetheless, as for other minoritized groups, barriers around mistrust of health care providers represent a further obstacle (and target) for improving timely access to preventive mental health care and support.
Indicated prevention strategies
Indicated strategies to prevent the onset of mental disorders typically seek to identify high‐risk individuals on the basis of emerging sub‐threshold psychopathology or family history of psychiatric illness with an associated decline in functioning. The delivery of indicated prevention has principally focused on youth‐oriented mental health care provision to prevent transition to disorder. This ranges from specialist secondary care (e.g., early detection services for psychosis) through to disorder‐agnostic youth mental services that adopt clinical staging models to provide care according to illness stage. Most recently, these models are being repositioned as broad‐spectrum integrated primary care services for youth mental health that deliver indicated prevention in a variety of innovative ways, and in a variety of contexts, including digitally, in educational settings, workplaces, the community, and clinical spaces 311 . They offer various interventions to indicated populations, ranging from clinical therapy to peer advocacy and psychosocial interventions to promote resilience, improve mental health literacy or improve social support. Only some of these interventions aim to explicitly tackle social determinants of mental health (social support, loneliness, bullying), usually as part of a multidisciplinary approach.
Just as the pattern of risk for mental disorders is socially inequitable, so too is the likelihood of receiving clinical care that is delivered in a timely, appropriate and proportionate manner according to need 187 , 396 . This is a global challenge driven by various issues in different settings, including stigma, health literacy, cultural norms, system capacity and economic development. Because indicated prevention strategies predominantly originated from clinical systems of care, identification and inclusion of high‐risk populations is subject to similar barriers and inequities. For example, there is evidence that people from socioeconomically disadvantaged, migrant and ethnoracial minoritized backgrounds are under‐represented in services for early detection of psychosis 397 , 398 , 399 , as well as in child and adolescent mental health services 400 . These biases may be compounded by the instruments used to identify high‐risk individuals, which are often developed 394 , 401 and tested 402 in unrepresentative, help‐seeking samples. These inequalities mean that those already exposed to substantial disadvantage are least likely to receive indicated prevention, and less likely to take part in research that informs us about what works for whom, making this an imperative matter of social justice 403 .
Furthermore, as currently configured, indicated prevention strategies are unlikely to substantially reduce the incidence and prevalence of mental disorders, because they currently lack sufficient population coverage to do so. For example, studies in England 398 and Australia 399 have shown that only 4‐22% of people diagnosed with first‐episode psychosis in services for early intervention in psychosis had prior contact with early detection services before illness onset. This calls for broader‐based transdiagnostic indicated prevention solutions which could be integrated into community and school settings, as recently evidenced and advocated by McGorry et al 311 , explicitly addressing social determinants of mental health.
Secondary and tertiary prevention strategies
In this section, we present a brief overview of existing social interventions that aim to optimize various aspects of recovery in people with established mental disorders.
Social prescribing
Social prescribing, primarily adopted by primary care physicians, connects individuals with established mental disorders to sources of social support within local communities 404 . Examples include volunteering, befriending, and hobby groups 405 . Despite its popularity, the evidence base lags behind practice, with studies currently lacking methodological rigour 406 , 407 . Although positive effects on various mental health outcomes have been observed in systematic reviews 404 , 408 , 409 , 410 , the quality of evidence is generally low 408 , 409 , 410 , 411 , and restricted to uncontrolled samples 408 , 409 , 411 or selective subgroups 410 . There is also initial evidence that minoritized groups are under‐represented in social prescribing 412 ; factors such as finance, language and cultural barriers may pose issues around access and engagement.
Vocational interventions
Given the cyclical relationship between socioeconomic disadvantage and mental health, secondary and tertiary interventions that help people return to work or education should be considered an important component of public mental health policies. One such example is Individual Placement and Support (IPS), where an employment specialist supports an individual with mental health problems to seek competitive employment. IPS has been consistently demonstrated to be superior over other forms of vocational interventions to help individuals with severe mental illnesses obtain and maintain competitive employment 413 , 414 , 415 . These findings hold across geographical locations and across high‐ and low‐resource settings 413 , though success and uptake may depend on motivation and self‐efficacy in job seeking, which may introduce additional barriers for those already exposed to greater structural and systemic disadvantage 416 , 417 , 418 . While these interventions may benefit people with other mental health outcomes, they appear most effective for severe mental disorders 419 .
Family interventions
It is well known that family interventions can help reduce risk of relapse for people with psychosis 420 , 421 . They also appear to reduce depression and suicidal ideation in young people 422 , 423 , though these effects could be restricted to older adolescents and may be affected by risk of bias concerns 424 . Secondary and tertiary family interventions can also lead to reductions in parental stress and depression, and improvements in parenting behaviours 422 , 425 , which may be particularly relevant to interrupting intergenerational transmission of familial risks for mental health problems 424 . These effects also extend to LMICs, with 65% of interventions being delivered by non‐specialist workers 425 , 426 .
Trauma‐informed interventions
Traumatic events contribute substantially to mental health inequalities, as we highlighted earlier. Given this, models of trauma‐informed care have gained traction in secondary prevention, and may be particularly pertinent to recovery for specific groups, including victims of intimate partner violence, ethnoracial minoritized groups, and refugees and asylum seekers with established mental disorders. To date, the most commonly adopted and evaluated approaches include eye movement desensitization and reprocessing (EMDR) and trauma‐focused CBT 427 , 428 . Despite this, a recent systematic review 429 , which largely focused on interpersonal traumas in women, found inconsistent evidence that trauma‐informed interventions improve a range of psychological outcomes, including symptoms of PTSD, anxiety and depression. The authors attributed this to inadequate study designs, also observed by other reviews 430 , 431 , and called for broader trauma types and outcomes to be rigorously evaluated. For children and young people exposed to trauma, systematic reviews show moderate effects for EMDR and trauma‐focused CBT – but not conventional CBT 428 – in the treatment of PTSD 428 , 432 . Meta‐analytic evidence also demonstrates moderate effectiveness of trauma interventions in reducing symptoms of PTSD, depression and anxiety for displaced persons in HICs 382 and LMICs 433 . Greatest effects were found for trauma‐focused CBT, particularly with extensive cultural adaptations 434 .
RECOMMENDATIONS FOR ACTION
In this paper we have highlighted the social gradients in the incidence and prevalence of psychological distress and mental disorders within and between populations. This evidence consistently shows that those exposed to adverse social determinants of health – whether through poverty, discrimination, trauma or exclusion – are most likely to experience poor mental health over their lifetime, as well as downstream physical health, social and economic sequalae that can perpetuate cycles of intergenerational inequality in health and social outcomes. We have also shown how these inequalities arise through a broader set of structural processes and policies that disadvantage minoritized and marginalized individuals and communities through experiences of interpersonal, institutional and systemic discrimination. These experiences prevent equitable access to adequate education, employment, housing, social support and health care, which subsequently increase exposure to stressful life events and risk of poor mental health.
What, then, can and should be done? We argue that primary prevention should be prioritized to address and remove social inequities in order to prevent the onset of mental disorder and lower the burden of psychiatric morbidity in the population. There are at least three compelling reasons for this case. First, equality is central to human rights 435 , and so efforts to reduce social inequities that affect population mental health are a matter of social justice. Second, since many psychiatric disorders exhibit such social gradients, universal, selective or indicated primary prevention strategies would not only promote more equitable mental health, but also achieve substantial gains in improving the mental health of whole populations. Finally, while recognizing the vitality of secondary and tertiary prevention in treatment, recovery and relapse prevention for people with existing mental disorders, primary prevention needs to be integrated into equitable and accessible whole‐population care systems. Here, parity of investment in effective primary prevention would represent a win‐win‐win for individuals, populations and health care systems, both in LMIC contexts, where secondary and tertiary mental health care services are often extremely limited, and in HIC contexts, where need for care has outstripped capacity 41 .
In this concluding section, we identify seven recommendations for action (see Table 2), which provide a roadmap for mental health professionals, policy makers and researchers to improve population mental health and reduce inequities in mental health problems by prioritizing intervention on social determinants.
Table 2.
Overview of recommendations for action to intervene on social determinants to improve population mental health and reduce inequities in mental health problems
| 1. Make social justice central to all public mental health interventions. Mental health problems are inequitably distributed between and within populations, principally arising from systemic structural inequalities. Making social justice core to all public mental health interventions and policies would reduce these inequities. |
| 2. Invest in interventions that pay off in multiple domains. Few social determinants solely affect mental health. Investing in interventions that target key social determinants will improve physical, mental and social outcomes for individuals and communities. Intervention programs should routinely measure mental health alongside these other outcomes. |
| 3. Invest in interventions that target critical windows of the life course to interrupt intergenerational transmission of mental health inequalities. Providing good‐quality and accessible parental and familial support early in life can interrupt the intergenerational transmission of mental health inequalities within families or communities. |
| 4. Prioritize interventions that focus on poverty alleviation. Any comprehensive public health approach to reduce the burden of poor mental health must include efforts to reduce poverty. Poverty is inextricably linked to most social determinants of mental health, and could be considered a root cause. |
| 5. Strengthen causal inference in research on social determinants of mental health and primary prevention. Most research on social determinants of mental health is observational, often subject to selection and confounding bias. Stronger causal inference methods are needed, as well as larger, interdisciplinary observational and experimental studies in representative and adequately powered samples to accelerate progress of knowledge and develop effective primary interventions. |
| 6. Establish inclusive longitudinal population mental health monitoring. Many countries struggle to accurately estimate psychiatric morbidity in their populations, which inhibits both clinical and public mental health provision. Samples are often unrepresentative. Reliable, inclusive and precise longitudinal monitoring of population mental health is the essential basis for effective prevention. |
| 7. Ensure parity between primary, secondary and tertiary prevention in mental health. Investing sufficiently in primary prevention to stop the onset of mental disorders prevents suffering, improves quality of life and societal outcomes, and reduces demand for secondary and tertiary prevention. |
1. Make social justice central to all public mental health interventions
Social justice is concerned with the fair (equitable) distribution of wealth, power, opportunities and privileges within society. No society is perfectly just. To a greater or lesser extent, different societies will have differing levels of fairness in access to the economic, social and political means that allow individuals or groups to determine and realize their preferred goals and outcomes. The equitable (fair, just) distribution of resources is closely related, but not always identical to the equal (balanced, proportionate) distribution of resources. For example, on average, older adults (of working age) tend to have higher incomes than younger adults, holding all other variables constant, as a result of accumulated knowledge and experience; income is thus surely unequally distributed by age, but we may choose not to consider this inequitable.
Accordingly, not all differences in mental health are, per se, inequitable. Men are more prone to develop schizophrenia than women 198 , potentially due to biological differences 436 , but this difference is likely not to be a matter of social justice. By contrast, while the elevated prevalence of depression in women may also be partly biologically determined 437 , there is strong evidence that it may also result from greater exposure to interpersonal violence, childhood trauma or other gendered social or psychological factors 200 , 437 , making interventions to prevent these inequitable experiences a remedial matter of social justice.
We consider that most social differences in the onset and maintenance of mental health problems arise from inequitable exposure to structural disadvantage, thus requiring the principles of social justice to be embedded at the heart of all public mental health policy efforts to prevent mental disorders. It has been argued that “the job of justice in its most pressing role demands a permanent vigilance and attention to social and economic determinants that compound and reinforce insufficiencies in a number of dimensions of well‐being” 5, p.78 . Logically, then, this requires public mental health, and public policy more broadly, to ensure that all prevention strategies explicitly redress social, economic, political and environmental insufficiencies that both increase the risk of mental disorders and inhibit people's recovery from them. Prevention strategies and policies that embed social justice theory from their conception are most likely to be effective in reducing social inequities in mental disorders, and in shifting the entire population distribution of risk. This approach requires careful theoretical and empirical consideration of various issues, including what sufficient conditions would look like, and which social determinants should be prioritized from the perspective of social justice. These issues will vary over time and between different contexts. For example, while poverty alleviation is a global goal likely to improve mental health universally 359 , it may be a more imperative matter of social justice in LMICs, where a much higher proportion of the population live in poverty.
Finally, the need for social justice applies not only to the strategies and policies to address social determinants of health, but also to the research that supports them. Our review has focused on the disproportionate body of evidence from HICs in the Global North. While we have highlighted evidence from LMICs where we have identified it, and while many determinants are likely to be similar, others may be different 2 . Social justice requires both accelerated investment into further high‐quality research on the most effective prevention strategies for social determinants in LMICs, and strategies to counteract the inequitable reproduction of knowledge concentrated on the Global North that reviews unavoidably perpetuate.
2. Invest in interventions that pay off in multiple domains
Most, if not all, of the social determinants discussed in this paper are associated with adverse outcomes that extend beyond the realm of mental health. As an example, experience of childhood adversity – a risk factor strongly associated with a range of negative mental health outcomes – is also associated with a host of poor physical health 103 , social 438 , and educational/occupational 439 outcomes. In a second example, whole communities are often exposed to highly intersectional, cyclical patterns of social disadvantage 2 , 138 , 374 , meaning that successive generations of families may face limited choices in navigating social determinants of health, including socioeconomic disadvantage, social exclusion, discrimination, trauma, and hostile environments, which simultaneously contribute to poor physical health, mental health, and social outcomes 41 , 45 . However, despite substantial evidence supporting such multi‐finality, progress in addressing social determinants and their associated consequences has been slow, due in part to the pervasive siloed thinking amongst researchers, practitioners and policy makers.
Greater cross‐sector collaboration and more inclusive outcome measures may help advance prevention efforts, particularly where these include approaches aimed at whole populations. At present, many promising interventions that target social determinants are not assessed in terms of mental health effects, which represents a lost opportunity to learn about their potential individual‐, community‐, and society‐level impacts 440 . For example, there are a wide range of innovative approaches being implemented within the education, social care and criminal justice sectors that may be beneficial for mental health but are not currently recognized as such due to an absence of formalized measurement of mental health outcomes. One exemplar approach is that of the Uptown Hub in New York 441 , which provides a community‐based service for youth at risk of involvement with the judicial system. The service offers a range of support to young people between the ages of 14 and 24 years, including engagement and retention in work or education, recreational involvement, peer and psychological support to foster resilience, as well as other well‐being activities to promote good mental and physical health. Evaluation of such programs is now required to carefully quantify and measure the range of direct and indirect outcomes that they could achieve.
In light of these considerations, we recommend that mental health be measured as a standard outcome in the evaluation of any policy, programme or intervention targeting social determinants. Although this requires additional data collection in the context of evaluations that may have quite separate aims, including mental health alongside other outcomes is becoming increasingly feasible with innovations such as computerized adaptive testing 442 , passive sensing technology, and administrative record linkage 443 . Furthermore, the value of such information would greatly enhance our understanding of which approaches are most effective for addressing social determinants, and which could facilitate real progress in improving population health in parallel with other social outcomes (e.g., crime, education, employment, welfare).
3. Invest in interventions that target critical windows of the life course to interrupt intergenerational transmission of mental health inequalities
Although the majority of mental disorders manifest during adolescence 19 , they are often rooted much earlier in development. A life course perspective can help us understand how exposure to various social determinants – that operate from before birth throughout life – affects one's chances of experiencing poor (or good) mental health 444 , or how it may perpetuate these outcomes through intergenerational transmission within families or communities 445 . By taking a life course approach, we can potentially develop effective interventions that interrupt the intergenerational transmission of accumulated adversities during critical windows of vulnerability 446 .
Given the importance of the prenatal period in shaping mental, physical and cognitive trajectories, providing good‐quality and accessible parental and familial support early in life is essential to affect this process 367 . Earlier, we presented evidence of positive outcomes following early‐life home visitation programs for pregnant and post‐partum mothers, with benefits extending into childhood and adolescence, and huge cost savings 371 , 373 . These interventions are particularly effective in selective groups. Ensuring that young families have sufficient financial support to alleviate stress and meet their needs, including adequate food and housing security, also warrants targeting direct economic interventions at selective groups during critical periods of child development. Stable, secure relationships, particularly in the early years of life, appear fundamental to buffer against life stressors, meaning that family‐based interventions hold enormous potential for mental health prevention and breaking intergeneration cycles of disadvantage.
Interventions that support stable, secure and cohesive communities in the wider social environment may also help buffer children from the impact of social adversity on mental health 281 . For young people, educational settings are likely to be particularly relevant environments in which to implement interventions that promote life‐long mental health. For example, schools can nurture socioemotional, academic and cognitive skills, which can bolster against future disadvantages (e.g., unemployment). This could lead to improved educational attainment and increased socioeconomic status to disrupt intergenerational cycles of exposure to some social adversities that increase risk of mental health problems. Further, the onset of many mental health problems occurs during the transition from adolescence to adulthood, a point at which the stakes are high for achieving socio‐developmental milestones. Preventing onset in this period could have a profound impact on future social and economic trajectories 447 .
We have also seen how some neighbourhood environments can act as reservoirs for structural racism and discrimination that increases the likelihood of exposure to individual‐level stressors 448 . Systemic underinvestment, disenfranchisement and lack of opportunities in such neighbourhoods restrict upward social mobility, and so these experiences – including deleterious mental health outcomes – become highly intractable, intergenerational and systemic forms of disadvantage and oppression. Effective public mental health interventions must create opportunities to break these cycles of exposure within our communities, with evidence that this may be particularly important early in life 449 .
4. Prioritize interventions that focus on poverty alleviation
Any comprehensive public health approach to reducing the burden of poor mental health must include a focus on poverty alleviation. Poverty is inextricably linked to most social determinants of mental health, and could be considered a root cause. It is incumbent on all stakeholders in the public health sphere to advocate for poverty alleviation in order to mitigate its deleterious, multi‐final effects. In addition to improving population mental health, reducing poverty would make major contributions towards improving population physical health, reducing societal inequalities, and reducing barriers to social justice, thus connecting with other recommendations we outline here.
Poverty has particularly pernicious effects early in life, with consequences that stretch across the life course. Children who grow up in poverty tend to live dramatically different lives compared with those who do not. This begins with their immediate environment, as children in poverty are more likely to be living in crowded and/or poor‐quality housing, and to be exposed to food insecurity and pollution 450 . Poverty also has strong effects on their parents, as the stress of living in poverty affects parental well‐being, and introduces conflicts that negatively influence parenting behaviours and the strength of the parent‐child relationship 450 , 451 . Worse, poverty is strongly and consistently linked with child maltreatment and neglect 451 . Children living in poverty are more likely to be exposed to violence, either in their homes or in the communities where they live 450 .
The adversity faced by children in poverty leaves them less prepared for school, as they rate lower on numerous aspects of readiness at school entry age, including social and behavioural skills, language development, and cognitive abilities 452 , 453 . This results in a socio‐developmental cascade with long‐lasting impacts, as children who grow up in low‐income families are less likely to achieve academically through all levels of schooling, and are more likely to leave school early, or with lower qualifications 452 , 454 . Although they are more likely to enter the labour market early, they have lower incomes throughout adulthood 454 . Beyond educational and economic outcomes, living in poverty also influences the social lives of those experiencing it. Low income also limits individuals’ capacity to engage in social, leisure and civic activities, leaving them less able to mitigate stressful experiences via larger social networks and increased social support and capital 455 .
Given the numerous pathways through which poverty influences social determinants of mental health, only some of which are mentioned here, efforts to alleviate poverty should result in mental health benefits. Any public health campaign to improve population mental health that does not address poverty will be unlikely to meet its goal.
5. Strengthen causal inference in research on social determinants of mental health and primary prevention
We have sought to identify the strongest evidence regarding those social factors that contribute most substantially to population‐level mental health and disorder, and single out which public health interventions are most likely to prevent adverse mental health. While high‐quality RCT and/or longitudinal evidence is available in some domains, there is still much to learn about the causal pathways between social determinants and mental health.
One common and emergent theme in our review is the extent to which these associations arise from non‐causal mechanisms such as genetic selection or unobserved confounding. Effective prevention strategies that target social determinants will only improve population mental health if those determinants induce a change in the outcome under study (i.e., they have a causal effect on the outcome). Proponents of biological determinism argue that nearly all socially‐constructed “exposures” result from the selection of people with greater genetic vulnerabilities to mental disorders into more adverse social environments 456 . Thus, under this paradigm, social adversities are – like mental ill health – seen as just another consequence of genetic influences. However, while genetic selection may contribute to social patterns of disease occurrence 457 , neither genetic nor environmental factors alone will be sufficient or necessary in the aetiology of mental disorders. More research is required to understand the myriad of causal sets that lead to psychiatric disorder, and their relative impacts at the population level. Here, we propose that modern causal inference methods 458 should become de rigueur when using observational data to investigate the social determinants of mental health. Further, these methods are only as strong as the underlying measures, samples and assumptions upon which they are predicated, so accelerating the use of longitudinal, well‐characterized and epidemiological representative samples – and synthesizing expertise and data from across academia, psychiatry and industry – should be a priority to make substantial progress in identifying the social causes on which to intervene.
Our review also raises the need to avoid social reductionism. Many social factors – operating from proximal to distal ranges – are likely to contribute to cyclical disadvantage, structural discrimination and mental health. We may worry less about which specific cause (e.g., which type of abuse or neglect, which domain of deprivation or inequality) is the determinant of risk, but rather focus on identifying the causal structure through which risk manifests itself, and across which holistic interventions are required. Adopting a causal architecture framework 459 and grounding our research in theoretical models of causation would accelerate understanding of how, where and when to intervene effectively.
Finally, many systematic reviews of interventions in this paper were caveated by observations around low quality, small samples and heterogeneous methodologies, while very few RCTs of complex social interventions have been attempted. Arguably, the funding landscape around these issues needs transformation. Many small, low‐quality observational studies hamper the synthesis of reliable evidence on what works for whom 460 . Larger, ambitious, interdisciplinary and multisectoral collaborations that attempt to tackle a big idea through the triangulation of high‐quality evidence, including experimental paradigms – although more difficult, costly and risky – could help transform our understanding of primary prevention strategies that improve population health across multiple domains.
6. Establish inclusive longitudinal population mental health monitoring
Psychiatry has a long‐held fascination with the determinants of mental health across disorders and dimensions that still rely upon phenomenological interpretation. This is true for both clinical psychiatry and psychiatric epidemiology. But the cornerstone of both approaches is the need to count. Accurately monitoring the incidence and prevalence of mental disorders, as well as the distribution of underlying symptomatology, in the population over time, serves at least two crucial purposes. First, it establishes the basic need for clinical treatment in a population, upon which appropriate resourcing can be set for secondary and tertiary prevention. Second, it allows empirical quantification of the potential gains in population mental health that could be achieved through the effective deployment of universal, selective and indicated primary prevention strategies.
Many countries struggle with basic monitoring of the burden of psychiatric morbidities in their populations 461 , which inhibits both clinical and public mental health provision. In LMIC settings, the reasons for this may be self‐evident, since limited resources may mean political prioritization of other vital issues. Recent reviews have highlighted the evidence gap in incidence and prevalence estimates of psychiatric disorders between HIC and LMIC settings 462 . In HIC settings, the lack of routine data on psychiatric morbidity in the population is sometimes surprising. In England, for example, while the National Health System collects routine mental health service contact data for planning purposes, it is difficult to obtain reliable estimates of incidence and prevalence from help‐seeking samples that often lack validated assessment data about psychopathology. Even in countries with well‐established disease registries, such as Denmark, Sweden or Finland, incidence is based on contact with secondary mental health care services, and may therefore be less useful for some psychiatric conditions, including depression and anxiety. Prevalence estimates from survey data, while more population‐based, are often drawn from smaller samples, which limits inferences that can be made about psychiatric morbidity in different subgroups. Finally, all methods of population mental health monitoring will suffer to a greater or lesser extent from unrepresentative sampling, whether due to biases in case detection or help‐seeking.
In order to respond effectively across primary, secondary and tertiary levels of prevention, modern paradigms for reliable, inclusive and precise longitudinal monitoring of population mental health at scale are needed. In the context of social determinants, it is particularly vital that these include representative and well‐powered samples from socially disadvantaged and minoritized backgrounds. In many contexts this could be achieved by better routine recording of mental health data and the use of harmonized data management platforms that harness technological advances in data security and linkage with clinical and population health data, of which some examples already exist 463 .
7. Ensure parity between primary, secondary and tertiary prevention in mental health
The need for primary prevention in mental health should be examined closely by policy makers worldwide. The advantages of this prevention are evident in terms of improving quality of life, social functioning and workforce participation, and reducing suicides. Such approaches have been outlined in this paper, and encompass creating environments where people (particularly members of marginalized groups) know where to access early support after an adverse life event or when facing chronic difficulties, have opportunities for social connectedness, and are supported to function optimally in their work, family and social roles. As an overarching principle, it is also important to address the reduced uptake of interventions among socially disadvantaged groups 464 . Beyond this, the ultimate societal ambition is to achieve primordial prevention, i.e. to prevent the emergence of risk factors for mental disorders and suicidality. Responsibility for this lies outside the remit of public health, and relies on societal systems that engender the socioeconomic and cultural conditions that promote mental health and well‐being in a population.
There are also strong reasons why investment in primary prevention of mental ill health should have parity with that in secondary and tertiary prevention. The social determinants we have outlined above generally contribute to the onset, severity and prognosis of mental disorders. Therefore, any efforts to arrest the progression of mental disorders (implemented as secondary and tertiary prevention) will falter where the conditions needed for primary prevention do not exist.
CONCLUSIONS
In this review, we have highlighted the major social determinants that generate and sustain intergenerational inequalities in risk and maintenance of mental health problems and disorders. Although stronger causal evidence is required for some determinants, we have shown that a variety of primary prevention strategies to alleviate social inequalities, which often have their origins in early life, can be effective in reducing the population burden of potentially life‐long mental health problems that will typically emerge in adolescence.
Various forms of discrimination and minoritization, including structural racism, are likely to exacerbate intergenerational social inequalities in mental health. We have outlined seven recommendations aligned around social justice that policy makers, practitioners and clinicians are invited to adopt to advance efforts to intervene on modifiable social determinants that place populations in peril of poor mental health.
ACKNOWLEDGEMENTS
J.B. Kirkbride acknowledges funding from a Wellcome Trust Collaborative Award (no. 222499/Z/21/Z); J. Dykxhoorn from the UK National Institute for Health and Care Research (NIHR) (advanced fellow, NIHR302266); P.B. Jones from a NIHR programme grant for applied research (no. 0616‐20003). J.B. Kirkbride, J. Dykxhoorn, A. Pitman and T. Wright are also funded by the NIHR University College London Hospitals Biomedical Research Centre. J.B. Kirkbride and A. Pitman are also supported by a UK research and innovation grant (no. ES/S004440/1). T. Steare is funded by a Wellcome Trust fellowship, and T. Wright by an UK Economic and Social Research Council fellowship. The views expressed in this paper are those of the authors and not necessarily those of the funding bodies. The authors would like to thank M. Kingsbury, D.‐L. Blair, H. Eccles, S. Semchishen, D. Lemaire, I. Obeegadoo and F. Solmi for providing background information during the drafting of the manuscript.
REFERENCES
- 1. World Health Organization . Taking action on the social determinants of health. www.who.int/westernpacific/activities.
- 2. World Health Organization . World mental health report: transforming mental health for all. Geneva: World Health Organization, 2022. [Google Scholar]
- 3. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications. JAMA Psychiatry 2015;72:334‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Global Burden of Disease 2019 Mental Disorders Collaborators . Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990‐2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 2022;9:137‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Powers M, Faden RR. Social justice: the moral foundations of public health and health policy. Oxford: Oxford University Press, 2006. [DOI] [PubMed] [Google Scholar]
- 6. Gandal MJ, Geschwind DH. Polygenicity in psychiatry – like it or not, we have to understand it. Biol Psychiatry 2021;89:2‐4. [DOI] [PubMed] [Google Scholar]
- 7. Ferrari F, Villa RF. The neurobiology of depression: an integrated overview from biological theories to clinical evidence. Mol Neurobiol 2017;54:4847‐65. [DOI] [PubMed] [Google Scholar]
- 8. Kambeitz‐Ilankovic L, Koutsouleris N, Upthegrove R. The potential of precision psychiatry: what is in reach? Br J Psychiatry 2022;220:175‐8. [DOI] [PubMed] [Google Scholar]
- 9. Howes OD, Baxter L. The drug treatment deadlock in psychiatry and the route forward. World Psychiatry 2023;22:2‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Howes OD, Thase ME, Pillinger T. Treatment resistance in psychiatry: state of the art and new directions. Mol Psychiatry 2022;27:58‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tricklebank MD, Robbins TW, Simmons C et al. Time to re‐engage psychiatric drug discovery by strengthening confidence in preclinical psychopharmacology. Psychopharmacology 2021;238:1417‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. United Nations . Sustainable development goals. www.un.org/sustainabledevelopment.
- 13. Pescosolido BA, Halpern‐Manners A, Luo L et al. Trends in public stigma of mental illness in the US, 1996‐2018. JAMA Netw Open 2021;4:e2140202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Henderson C, Potts L, Robinson EJ. Mental illness stigma after a decade of Time to Change England: inequalities as targets for further improvement. Eur J Public Health 2020;30:497‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. NHS Digital . Mental health services monthly statistics dashboard. https://digital.nhs.uk.
- 16. NHS England . NHS mental health dashboard. www.england.nhs.uk.
- 17. Moitra M, Santomauro D, Collins PY et al. The global gap in treatment coverage for major depressive disorder in 84 countries from 2000‐2019: a systematic review and Bayesian meta‐regression analysis. PLoS Med 2022;19:e1003901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization . Mental health atlas 2020. Geneva: World Health Organization, 2021. [Google Scholar]
- 19. Solmi M, Radua J, Olivola M et al. Age at onset of mental disorders worldwide: large‐scale meta‐analysis of 192 epidemiological studies. Mol Psychiatry 2022;27:281‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lipson SK, Lattie EG, Eisenberg D. Increased rates of mental health service utilization by U.S. college students: 10‐year population‐level trends (2007‐2017). Psychiatr Serv 2019;70:60‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Keyes KM, Gary D, O'Malley PM et al. Recent increases in depressive symptoms among US adolescents: trends from 1991 to 2018. Soc Psychiatry Psychiatr Epidemiol 2019;54:987‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Twenge JM, Cooper AB, Joiner TE et al. Age, period, and cohort trends in mood disorder indicators and suicide‐related outcomes in a nationally representative dataset, 2005‐2017. J Abnorm Psychol 2019;128:185‐99. [DOI] [PubMed] [Google Scholar]
- 23. Wiens K, Bhattarai A, Pedram P et al. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci 2020;29:e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Castelpietra G, Knudsen AKS, Agardh EE et al. The burden of mental disorders, substance use disorders and self‐harm among young people in Europe, 1990‐2019: findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur 2022;16:100341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hazo JB, Costemalle V. Spring 2020 lockdown: an increase in depressive syndromes, especially among 15‐24 year olds results from the 1st wave of the EpiCov Survey and comparison with the European Health Surveys (EHIS) of 2014 and 2019. https://drees.solidarites‐sante.gouv.fr.
- 26. Thorisdottir IE, Asgeirsdottir BB, Sigurvinsdottir R et al. The increase in symptoms of anxiety and depressed mood among Icelandic adolescents: time trend between 2006 and 2016. Eur J Public Health 2017;27:856‐61. [DOI] [PubMed] [Google Scholar]
- 27. Australian Bureau of Statistics . First insights from the National Study of Mental Health and Wellbeing, 2020‐21. Belconnen: Australian Bureau of Statistics, 2021. [Google Scholar]
- 28. McGorry PD. About 40 per cent of young Australians have experienced mental illness – and it's high time we do something about it. ABC News, August 4, 2022. [Google Scholar]
- 29. Burn‐Murdoch J. Smartphones and social media are destroying children's mental health. Financial Times, March 10, 2023. [Google Scholar]
- 30. Wiens K, Bhattarai A, Pedram P et al. A growing need for youth mental health services in Canada: examining trends in youth mental health from 2011 to 2018. Epidemiol Psychiatr Sci 2020;29:e115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gimbrone C, Bates LM, Prins SJ et al. The politics of depression: diverging trends in internalizing symptoms among US adolescents by political beliefs. SSM Ment Health 2022;2:100043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Grucza RA, Krueger RF, Agrawal A et al. Declines in prevalence of adolescent substance use disorders and delinquent behaviors in the USA: a unitary trend? Psychol Med 2018;48:1494‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ng Fat L, Shelton N, Cable N. Investigating the growing trend of non‐drinking among young people; analysis of repeated cross‐sectional surveys in England 2005‐2015. BMC Public Health 2018;18:1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Sun Y, Wu Y, Fan S et al. Comparison of mental health symptoms before and during the covid‐19 pandemic: evidence from a systematic review and meta‐analysis of 134 cohorts. BMJ 2023;380:e074224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. ten Have M, Tuithof M, van Dorsselaer S et al. Prevalence and trends of common mental disorders from 2007‐2009 to 2019‐2022: results from the Netherlands Mental health Survey and Incidence Studies (NEMESIS), including comparison of prevalence rates before vs. during the COVID‐19 pandemic. World Psychiatry; 2023;22:275‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fancourt D, Steptoe A, Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID‐19 in England: a longitudinal observational study. Lancet Psychiatry 2021;8:141‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Borrescio‐Higa F, Valenzuela P. Gender inequality and mental health during the COVID‐19 pandemic. Int J Public Health 2021;66:1604220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Niedzwiedz CL, Green MJ, Benzeval M et al. Mental health and health behaviours before and during the initial phase of the COVID‐19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health 2020;75:224‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Akré ER, Anderson A, Stojanovski K et al. Depression, anxiety, and alcohol use among LGBTQ+ people during the COVID‐19 pandemic. Am J Public Health 2021;111:1610‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mengesha Z, Alloun E, Weber D et al. “Lived the pandemic twice”: a scoping review of the unequal impact of the COVID‐19 pandemic on asylum seekers and undocumented migrants. Int J Environ Res Public Health 2022;19:6624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Vereeken S, Peckham E, Gilbody S. Can we better understand severe mental illness through the lens of Syndemics? Front Psychiatry 2023;13:1092964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lund C, Breen A, Flisher AJ et al. Poverty and common mental disorders in low and middle income countries: a systematic review. Soc Sci Med 2010;71:517‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Lund C, Brooke‐Sumner C, Baingana F et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry 2018;5:357‐69. [DOI] [PubMed] [Google Scholar]
- 44. Allen J, Balfour R, Bell R et al. Social determinants of mental health. Int Rev Psychiatry 2014;26:392‐407. [DOI] [PubMed] [Google Scholar]
- 45. Kivimäki M, Batty GD, Pentti J et al. Association between socioeconomic status and the development of mental and physical health conditions in adulthood: a multi‐cohort study. Lancet Public Health 2020;5:e140‐9. [DOI] [PubMed] [Google Scholar]
- 46. Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav 1995;35:80‐94. [PubMed] [Google Scholar]
- 47. Fryers T, Melzer D, Jenkins R. Social inequalities and the common mental disorders – A systematic review of the evidence. Soc Psychiatry Psychiatr Epidemiol 2003;38:229‐37. [DOI] [PubMed] [Google Scholar]
- 48. Esch P, Bocquet V, Pull C et al. The downward spiral of mental disorders and educational attainment: a systematic review on early school leaving. BMC Psychiatry 2014;14:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Thomson RM, Igelström E, Purba AK et al. How do income changes impact on mental health and wellbeing for working‐age adults? A systematic review and meta‐analysis. Lancet Public Health 2022;7:e515‐28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Guan N, Guariglia A, Moore P et al. Financial stress and depression in adults: a systematic review. PLoS One 2022;17:e0264041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Miller KK, Watson R, Eisenberg M. The intersection of family acceptance and religion on the mental health of LGBTQ youth. Ann LGBTQ Public Popul Health 2020;1:27‐42. [Google Scholar]
- 52. Kim TJ, von dem Knesebeck O. Perceived job insecurity, unemployment and depressive symptoms: a systematic review and meta‐analysis of prospective observational studies. Int Arch Occup Environ Health 2016;89:561‐73. [DOI] [PubMed] [Google Scholar]
- 53. Utzet M, Valero E, Mosquera I et al. Employment precariousness and mental health – Understanding a complex reality: a systematic review. Int J Occup Med Environ Health 2020;33:569‐98. [DOI] [PubMed] [Google Scholar]
- 54. Pourmotabbed A, Moradi S, Babaei A et al. Food insecurity and mental health: a systematic review and meta‐analysis. Public Health Nutr 2020;23:1778‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Singh A, Daniel L, Baker E et al. Housing disadvantage and poor mental health: a systematic review. Am J Prev Med 2019;57:262‐72. [DOI] [PubMed] [Google Scholar]
- 56. Rohde N, Tang KK, Osberg L et al. The effect of economic insecurity on mental health: recent evidence from Australian panel data. Soc Sci Med 2016;151:250‐8. [DOI] [PubMed] [Google Scholar]
- 57. Kopasker D, Montagna C, Bender KA. Economic insecurity: a socioeconomic determinant of mental health. SSM Popul Health 2018;6:184‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lund C, Cois A. Simultaneous social causation and social drift: longitudinal analysis of depression and poverty in South Africa. J Affect Disord 2018;229:396‐402. [DOI] [PubMed] [Google Scholar]
- 59. Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 2013;90:24‐31. [DOI] [PubMed] [Google Scholar]
- 60. Russell AE, Ford T, Williams R et al. The association between socioeconomic disadvantage and attention deficit/hyperactivity disorder (ADHD): a systematic review. Child Psychiatry Hum Dev 2016;47:440‐58. [DOI] [PubMed] [Google Scholar]
- 61. Hakulinen C, Webb RT, Pedersen CB et al. Association between parental income during childhood and risk of schizophrenia later in life. JAMA Psychiatry 2020;77:17‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Byrne M, Agerbo E, Eaton WW et al. Parental socio‐economic status and risk of first admission with schizophrenia – a Danish national register based study. Soc Psychiatry Psychiatr Epidemiol 2004;39:87‐96. [DOI] [PubMed] [Google Scholar]
- 63. Fitzsimons E, Goodman A, Kelly E et al. Poverty dynamics and parental mental health: determinants of childhood mental health in the UK. Soc Sci Med 2017;175:43‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Ridley MW, Rao G, Schilbach F et al. Poverty, depression, and anxiety: causal evidence and mechanisms. Science 2020;370:eaay0214. [DOI] [PubMed] [Google Scholar]
- 65. Susser E, Hoek HW, Brown A. Neurodevelopmental disorders after prenatal famine: the story of the Dutch Famine Study. Am J Epidemiol 1998;147:213‐6. [DOI] [PubMed] [Google Scholar]
- 66. Lorant V, De Gelder R, Kapadia D et al. Socioeconomic inequalities in suicide in Europe: the widening gap. Br J Psychiatry 2018;212:356‐61. [DOI] [PubMed] [Google Scholar]
- 67. Lorant V, Kapadia D, Perelman J. Socioeconomic disparities in suicide: causation or confounding? PLoS One 2021;16:e0243895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Davies C, Segre G, Estradé A et al. Prenatal and perinatal risk and protective factors for psychosis: a systematic review and meta‐analysis. Lancet Psychiatry 2020;7:399‐410. [DOI] [PubMed] [Google Scholar]
- 69. Kim D, Saada A. The social determinants of infant mortality and birth outcomes in Western developed nations: a cross‐country systematic review. Int J Environ Res Public Health 2013;10:2296‐335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. National Academies of Sciences, Engineering, and Medicine . Systemic influences on outcomes in pregnancy and childbirth. In: Backes EP, Scrimshaw SC (eds). Birth settings in America: outcomes, quality, access, and choice. Washington: National Academies Press, 2020:113‐44. [PubMed] [Google Scholar]
- 71. Van den Bergh BRH, van den Heuvel MI, Lahti M et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci Biobehav Rev 2020;117:26‐64. [DOI] [PubMed] [Google Scholar]
- 72. Kingsbury M, Weeks M, MacKinnon N et al. Stressful life events during pregnancy and offspring depression: evidence from a prospective cohort study. J Am Acad Child Adolesc Psychiatry 2016;55:709‐16.e2. [DOI] [PubMed] [Google Scholar]
- 73. Manzari N, Matvienko‐Sikar K, Baldoni F et al. Prenatal maternal stress and risk of neurodevelopmental disorders in the offspring: a systematic review and meta‐analysis. Soc Psychiatry Psychiatr Epidemiol 2019;54:1299‐309. [DOI] [PubMed] [Google Scholar]
- 74. Friel C, Leyland AH, Anderson JJ et al. Prenatal vitamins and the risk of offspring autism spectrum disorder: systematic review and meta‐analysis. Nutrients 2021;13:2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. van den Broek T, Fleischmann M. Prenatal famine exposure and mental health in later midlife. Aging Ment Health 2019;23:166‐70. [DOI] [PubMed] [Google Scholar]
- 76. Collet OA, Heude B, Forhan A et al. Prenatal diet and children's trajectories of anxiety and depression symptoms from 3 to 8 years: the EDEN mother‐child cohort. J Nutr 2021;151:162‐9. [DOI] [PubMed] [Google Scholar]
- 77. Galera C, Heude B, Forhan A et al. Prenatal diet and children's trajectories of hyperactivity‐inattention and conduct problems from 3 to 8 years: the EDEN mother‐child cohort. J Child Psychol Psychiatry 2018;59:1003‐11. [DOI] [PubMed] [Google Scholar]
- 78. McGrath J. Does ‘imprinting’ with low prenatal vitamin D contribute to the risk of various adult disorders? Med Hypotheses 2001;56:367‐71. [DOI] [PubMed] [Google Scholar]
- 79. Arathimos R, Ronaldson A, Howe LJ et al. Vitamin D and the risk of treatment‐resistant and atypical depression: a Mendelian randomization study. Transl Psychiatry 2021;11:561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Mulugeta A, Lumsden A, Hyppönen E. Relationship between serum 25(OH)D and depression: causal evidence from a bi‐directional Mendelian randomization study. Nutrients 2020;13:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Liu D, Meng X, Tian Q et al. Vitamin D and multiple health outcomes: an umbrella review of observational studies, randomized controlled trials, and Mendelian randomization studies. Adv Nutr 2022;13:1044‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Taylor AE, Burgess S, Ware JJ et al. Investigating causality in the association between 25(OH)D and schizophrenia. Sci Rep 2016;6:26496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Najman JM, Plotnikova M, Williams GM et al. Maternal depression and family adversity: linked pathways to offspring depression? J Psychiatr Res 2017;88:97‐104. [DOI] [PubMed] [Google Scholar]
- 84. Simanek AM, Meier HCS. Association between prenatal exposure to maternal infection and offspring mood disorders: a review of the literature. Curr Probl Pediatr Adolesc Health Care 2015;45:325‐64. [DOI] [PubMed] [Google Scholar]
- 85. Cannon M, Jones PB, Murray RM. Obstetric complications and schizophrenia: historical and meta‐analytic review. Am J Psychiatry 2002;159:1080‐92. [DOI] [PubMed] [Google Scholar]
- 86. Boots A, Wiegersma AM, Vali Y et al. Shaping the risk for late‐life neurodegenerative disease: a systematic review on prenatal risk factors for Alzheimer's disease‐related volumetric brain biomarkers. Neurosci Biobehav Rev 2023;146:105019. [DOI] [PubMed] [Google Scholar]
- 87. Liu Y, Heron J, Hickman M et al. Prenatal stress and offspring depression in adulthood: the mediating role of childhood trauma. J Affect Disord 2022;297:45‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Lipner E, Murphy SK, Ellman LM. Prenatal maternal stress and the cascade of risk to schizophrenia spectrum disorders in offspring. Curr Psychiatry Rep 2019;21:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. McLaughlin KA. Future directions in childhood adversity and youth psychopathology. J Clin Child Adolesc Psychol 2016;45:361‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Felitti VJ, Anda RF, Nordenberg D et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med 1998;14:245‐58. [DOI] [PubMed] [Google Scholar]
- 91. Lacey RE, Minnis H. Practitioner review: Twenty years of research with adverse childhood experience scores – Advantages, disadvantages and applications to practice. J Child Psychol Psychiatry 2020;61:116‐30. [DOI] [PubMed] [Google Scholar]
- 92. McLaughlin KA, Greif Green J, Gruber MJ et al. Childhood adversities and first onset of psychiatric disorders in a national sample of US adolescents. Arch Gen Psychiatry 2012;69:1151‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Bruffaerts R, Demyttenaere K, Borges G et al. Childhood adversities as risk factors for onset and persistence of suicidal behaviour. Br J Psychiatry 2010;197:20‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Kessler RC, McLaughlin KA, Green JG et al. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry 2010;197:378‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Dunn VJ, Abbott RA, Croudace TJ et al. Profiles of family‐focused adverse experiences through childhood and early adolescence: the ROOTS project a community investigation of adolescent mental health. BMC Psychiatry 2011;11:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Centres for Disease Control and Prevention . Preventing adverse childhood experiences (ACEs): leveraging the best available evidence. Atlanta: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 2019.
- 97. Liming KW. Examining the differing effects of economic hardship and poor maternal wellbeing on cumulative exposure to adverse childhood experiences. J Child Adolesc Trauma 2019;12:307‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Stith SM, Liu T, Davies LC et al. Risk factors in child maltreatment: a meta‐analytic review of the literature. Aggress Violent Behav 2009;14:13‐29. [Google Scholar]
- 99. Finkelhor D, Ormrod RK, Turner HA. Polyvictimization and trauma in a national longitudinal cohort. Dev Psychopathol 2007;19:149‐66. [DOI] [PubMed] [Google Scholar]
- 100. Madigan S, Deneault A‐A, Racine N et al. Adverse childhood experiences: a meta‐analysis of prevalence and moderators among half a million adults in 206 studies. World Psychiatry 2023;22:463‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Radford A, Toombs E, Zugic K et al. Examining adverse childhood experiences (ACEs) within Indigenous populations: a systematic review. J Child Adolesc Trauma 2022;15:401‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Scott KM, McLaughlin KA, Smith DAR et al. Childhood maltreatment and DSM‐IV adult mental disorders: comparison of prospective and retrospective findings. Br J Psychiatry 2012;200:469‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Hughes K, Bellis MA, Hardcastle KA et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta‐analysis. Lancet Public Health 2017;2:e356‐66. [DOI] [PubMed] [Google Scholar]
- 104. Reuben A, Moffitt TE, Caspi A et al. Lest we forget: comparing retrospective and prospective assessments of adverse childhood experiences in the prediction of adult health. J Child Psychol Psychiatry 2016;57:1103‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Shanahan L, Copeland WE, Costello EJ et al. Child‐, adolescent‐ and young adult‐onset depressions: differential risk factors in development? Psychol Med 2011;41:2265‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Baldwin JR, Reuben A, Newbury JB et al. Agreement between prospective and retrospective measures of childhood maltreatment: a systematic review and meta‐analysis. JAMA Psychiatry 2019;76:584‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Baldwin JR, Caspi A, Meehan AJ et al. Population vs individual prediction of poor health from results of adverse childhood experiences screening. JAMA Pediatr 2021;175:385‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Gondek D, Howe LD, Gilbert R et al. Association of interparental violence and maternal depression with depression among adolescents at the population and individual level. JAMA Netw Open 2023;6:e231175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Ødegaard Ø. Emigration and insanity. Acta Psychiatr Neurol Scand 1932;7(Suppl. 4):1‐206. [Google Scholar]
- 110. Selten JP, Van Der Ven E, Termorshuizen F. Migration and psychosis: a meta‐analysis of incidence studies. Psychol Med 2020;50:303‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Dykxhoorn J, Hollander AC, Lewis G et al. Risk of schizophrenia, schizoaffective, and bipolar disorders by migrant status, region of origin, and age‐at‐migration: a national cohort study of 1.8 million people. Psychol Med 2018;49:2354‐63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Hollander AC, Dal H, Lewis G et al. Refugee migration and risk of schizophrenia and other non‐affective psychoses: cohort study of 1.3 million people in Sweden. BMJ 2016;352:i1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Brandt L, Henssler J, Müller M et al. Risk of psychosis among refugees: a systematic review and meta‐analysis. JAMA Psychiatry 2019;76:1133‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Blackmore R, Boyle JA, Fazel M et al. The prevalence of mental illness in refugees and asylum seekers: a systematic review and meta‐analysis. PLoS Med 2020;17:e1003337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Harris S, Dykxhoorn J, Hollander AC et al. Substance use disorders in refugee and migrant groups in Sweden: a nationwide cohort study of 1.2 million people. PLoS Med 2019;16:e1002944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Hollander AC, Pitman A, Sjöqvist H et al. Suicide risk among refugees compared with non‐refugee migrants and the Swedish‐born majority population. Br J Psychiatry 2020;217:686‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Salas‐Wright CP, Vaughn MG, Clark TT et al. Substance use disorders among first‐ and second‐generation immigrant adults in the United States: evidence of an immigrant paradox? J Stud Alcohol Drugs 2014;75:958‐67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Henkelmann JR, de Best S, Deckers C et al. Anxiety, depression and post‐traumatic stress disorder in refugees resettling in high‐income countries: systematic review and meta‐analysis. BJPsych Open 2020;6:e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Anderson KK, Edwards J. Age at migration and the risk of psychotic disorders: a systematic review and meta‐analysis. Acta Psychiatr Scand 2020;141:410‐20. [DOI] [PubMed] [Google Scholar]
- 120. Morgan C, Hutchinson G. The social determinants of psychosis in migrant and ethnic minority populations: a public health tragedy. Psychol Med 2010;40:705‐9. [DOI] [PubMed] [Google Scholar]
- 121. Close C, Kouvonen A, Bosqui T et al. The mental health and wellbeing of first generation migrants: a systematic‐narrative review of reviews. Global Health 2016;12:47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Steel JL, Dunlavy AC, Harding CE et al. The psychological consequences of pre‐emigration trauma and post‐migration stress in refugees and immigrants from Africa. J Immigr Minor Health 2017;19:523‐32. [DOI] [PubMed] [Google Scholar]
- 123. Tinghög P, Malm A, Arwidson C et al. Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: a population‐based survey. BMJ Open 2017;7:e018899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Hvidtfeldt C, Petersen JH, Norredam M. Waiting for family reunification and the risk of mental disorders among refugee fathers: a 24‐year longitudinal cohort study from Denmark. Soc Psychiatry Psychiatr Epidemiol 2022;57:1061‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Dykxhoorn J, Hollander AC, Lewis G et al. Family networks during migration and risk of non‐affective psychosis: a population‐based cohort study. Schizophr Res 2019;208:268‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Marie N, Ana GL, Niels K et al. Risk of mental disorders in family reunification migrants and native Danes: a register‐based historically prospective cohort study. Int J Public Health 2010;55:413‐9. [DOI] [PubMed] [Google Scholar]
- 127. de Silva U, Glover N, Katona C. Prevalence of complex post‐traumatic stress disorder in refugees and asylum seekers: systematic review. BJPsych Open 2021;7:e194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Oduola S, Dykxhoorn J. Triple trauma, double uncertainty, and a singular imperative to address the mental health crises within asylum‐seekers and refugees system: a commentary on Hvidtfeldt et al. (2021). Soc Psychiatry Psychiatr Epidemiol 2022;57:2157‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129. Torres L, Driscoll MW, Voell M. Discrimination, acculturation, acculturative stress, and Latino psychological distress: a moderated mediational model. Cultur Divers Ethnic Minor Psychol 2012;18:17‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Cicognani E, Sonn CC, Albanesi C et al. Acculturation, social exclusion and resistance: experiences of young Moroccans in Italy. Int J Intercult Relat 2018;66:108‐18. [Google Scholar]
- 131. Foverskov E, White JS, Norredam M et al. Neighbourhood socioeconomic disadvantage and psychiatric disorders among refugees: a population‐based, quasi‐experimental study in Denmark. Soc Psychiatry Psychiatr Epidemiol 2023;58:711‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Cantor‐Graae E, Pedersen CB. Full spectrum of psychiatric disorders related to foreign migration. JAMA Psychiatry 2013;70:427‐35. [DOI] [PubMed] [Google Scholar]
- 133. Salas‐Wright CP, Kagotho N, Vaughn MG. Mood, anxiety, and personality disorders among first and second‐generation immigrants to the United States. Psychiatry Res 2014;220:1028‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Kirkbride J, Jones PB. The mental ill‐health of people who migrate, and their descendants: risk factors, associated disability and wider consequences. London: Government Office for Science, 2010. [Google Scholar]
- 135. Oxman‐Martinez J, Rummens AJ, Moreau J et al. Perceived ethnic discrimination and social exclusion: newcomer immigrant children in Canada. Am J Orthopsychiatry 2012;82:376‐88. [DOI] [PubMed] [Google Scholar]
- 136. Neumann R, Moy P. You're (not) welcome: the impact of symbolic boundaries, intergroup contact, and experiences with discrimination on immigration attitudes. Am Behav Sci 2018;62:458‐77. [Google Scholar]
- 137. Pascoe EA, Richman LS. Perceived discrimination and health: a meta‐analytic review. Psychol Bull 2009;135:531‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Viruell‐Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med 2012;75:2099‐106. [DOI] [PubMed] [Google Scholar]
- 139. Jannesari S, Hatch S, Prina M et al. Post‐migration social‐environmental factors associated with mental health problems among asylum seekers: a systematic review. J Immigr Minor Health 2020;22:1055‐64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Cattacin S, Naegeli P. Vulnerable migrants: coping strategies and multiple paths to social exclusion. In: Ranci C, Brandsen T, Sabatinelli S (eds). Social vulnerability in European cities. London: Palgrave Macmillan, 2014:244‐70. [Google Scholar]
- 141. Heizmann B, Böhnke P. Migrant poverty and social capital: the impact of intra‐ and interethnic contacts. Res Soc Stratif Mobil 2016;46:73‐85. [Google Scholar]
- 142. Marmot M. The health gap: the challenge of an unequal world. Lancet 2015;386:2442‐4. [DOI] [PubMed] [Google Scholar]
- 143. Marmot MG. Status syndrome: a challenge to medicine. JAMA 2006;295:1304‐7. [DOI] [PubMed] [Google Scholar]
- 144. Jongsma HE, Gayer‐Anderson C, Tarricone I et al. Social disadvantage, linguistic distance, ethnic minority status and first‐episode psychosis: results from the EU‐GEI case‐control study. Psychol Med 2021;51:1536‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Lee ES. A theory of migration. Demography 1966;3:47‐57. [Google Scholar]
- 146. de Haas H. A theory of migration: the aspirations‐capabilities framework. Comp Migr Stud 2021;9:1‐35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Allinson CH, Berle D. Association between unmet post‐arrival expectations and psychological symptoms in recently arrived refugees. Transcult Psychiatry 2023;60:39‐51. [DOI] [PubMed] [Google Scholar]
- 148. Björkenstam E, Helgesson M, Norredam M et al. Differences in psychiatric care utilization between refugees, non‐refugee migrants and Swedish‐born youth. Psychol Med 2022;52:1365‐75. [DOI] [PubMed] [Google Scholar]
- 149. Due C, Green E, Ziersch A. Psychological trauma and access to primary healthcare for people from refugee and asylum‐seeker backgrounds: a mixed methods systematic review. Int J Ment Health Syst 2020;14:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Lindert J, Schouler‐Ocak M, Heinz A et al. Mental health, health care utilisation of migrants in Europe. Eur Psychiatry 2008;23:s114‐20. [DOI] [PubMed] [Google Scholar]
- 151. Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. J Health Soc Behav 1999;40:208. [PubMed] [Google Scholar]
- 152. Barr PB, Bigdeli TB, Meyers JL. Prevalence, comorbidity, and sociodemographic correlates of psychiatric disorders reported in the All of Us research program. JAMA Psychiatry 2022;79:622‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Breslau J, Aguilar‐Gaxiola S, Kendler KS et al. Specifying race‐ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med 2006;36:57‐68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154. McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff 2008;27:393‐403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Halvorsrud K, Nazroo J, Otis M et al. Ethnic inequalities and pathways to care in psychosis in England: a systematic review and meta‐analysis. BMC Med 2018;16:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Barnett P, Mackay E, Matthews H et al. Ethnic variations in compulsory detention under the Mental Health Act: a systematic review and meta‐analysis of international data. Lancet Psychiatry 2019;6:305‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Williams DR, González HM, Neighbors H et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean Blacks, and Non‐Hispanic Whites: results from the National Survey of American Life. Arch Gen Psychiatry 2007;64:305‐15. [DOI] [PubMed] [Google Scholar]
- 158. Bailey ZD, Krieger N, Agénor M et al. Structural racism and health inequities in the USA: evidence and interventions. Lancet 2017;389:1453‐63. [DOI] [PubMed] [Google Scholar]
- 159. Guess TJ. The social construction of whiteness: racism by intent, racism by consequence. Crit Sociol 2006;32:649‐73. [Google Scholar]
- 160. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health 2019;40:105‐25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci 2013;57:1152‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Pierce C. Offensive mechanisms. In: Barbour FB (ed). The Black seventies. Boston: Porter Sargent, 1970:265‐82. [Google Scholar]
- 163. Paradies Y, Ben J, Denson N et al. Racism as a determinant of health: a systematic review and meta‐analysis. PLoS One 2015;10:e0138511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Lewis TT, Cogburn CD, Williams DR. Self‐reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annu Rev Clin Psychol 2015;11:407‐40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165. Gee GC, Spencer M, Chen J et al. The association between self‐reported racial discrimination and 12‐month DSM‐IV mental disorders among Asian Americans nationwide. Soc Sci Med 2007;64:1984‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Misra S, Gelaye B, Williams DR et al. Perceived major experiences of discrimination, ethnic group, and risk of psychosis in a six‐country case‐control study. Psychol Med 2022;52:3668‐76. [DOI] [PubMed] [Google Scholar]
- 167. Stowkowy J, Liu L, Cadenhead KS et al. Early traumatic experiences, perceived discrimination and conversion to psychosis in those at clinical high risk for psychosis. Soc Psychiatry Psychiatr Epidemiol 2016;51:497‐503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Colen CG, Ramey DM, Cooksey EC et al. Racial disparities in health among nonpoor African Americans and Hispanics: the role of acute and chronic discrimination. Soc Sci Med 2018;199:167‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Dumornay NM, Lebois LAM, Ressler KJ et al. Racial disparities in adversity during childhood and the false appearance of race‐related differences in brain structure. Am J Psychiatry 2023;180:127‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Karcher NR, Klaunig MJ, Elsayed NM et al. Understanding associations between race/ethnicity, experiences of discrimination, and psychotic‐like experiences in middle childhood. J Am Acad Child Adolesc Psychiatry 2022;61:1262‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Berger M, Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress 2015;18:1‐10. [DOI] [PubMed] [Google Scholar]
- 172. Newton DE. Gay and lesbian rights: a reference handbook, 2nd ed. Santa Barbera: ABC‐CLIO, 2009. [Google Scholar]
- 173. Jerome C, Ting SH, Podin Y et al. Public receptivity towards LGBT in recent times Malaysia: LGBT perspectives. Int J Acad Res Bus Soc Sci 2021;11:371‐83. [Google Scholar]
- 174. Pepin‐Neff C, Cohen A. President Trump's transgender moral panic. Policy Stud 2021;42:646‐61. [Google Scholar]
- 175. Sihombing KDS. Transfeminism as a social movement: the struggle to fight for trans women's rights in Indonesia post 2016 LGBT moral panic. M.A. Thesis, Utrecht University, 2020.
- 176. Rodríguez DG, Murtagh B. Situating anti‐LGBT moral panics in Indonesia. Indones Malay World 2022;50:1‐9. [Google Scholar]
- 177. Hatzenbuehler ML, Keyes KM, Hasin DS. State‐level policies and psychiatric morbidity in lesbian, gay, and bisexual populations. Am J Public Health 2009;99:2275‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Hatzenbuehler ML, Pachankis JE. Stigma and minority stress as social determinants of health among lesbian, gay, bisexual, and transgender youth. Pediatr Clin North Am 2016;63:985‐97. [DOI] [PubMed] [Google Scholar]
- 179. Wright T, Nicholls EJ, Rodger AJ et al. Accessing and utilising gender‐affirming healthcare in England and Wales: trans and non‐binary people's accounts of navigating gender identity clinics. BMC Health Serv Res 2021;21:609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Marshall A, Cahill S. Barriers and opportunities for the mental health of LGBT older adults and older people living with HIV: a systematic literature review. Aging Ment Health 2022;26:1845‐54. [DOI] [PubMed] [Google Scholar]
- 181. Langlois AJ. Making LGBT rights into human rights. In: Bosia MJ, McEvoy SM, Rahman M (eds). The Oxford handbook of global LGBT and sexual diversity politics. Oxford: Oxford University Press, 2020:74‐88. [Google Scholar]
- 182. Pega F, Veale JF. The case for the World Health Organization's commission on social determinants of health to address gender identity. Am J Public Health 2015;105:e58‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Grant JM, Motter LA, Tanis J et al. Injustice at every turn: a report of the National Transgender Discrimination Survey. Washington: National Center for Transgender Equality and National Gay and Lesbian Task Force, 2011. [Google Scholar]
- 184. Brooks VR. Minority stress and lesbian women. Lexington: Lexington Books, 1981. [Google Scholar]
- 185. Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull 2003;129:674‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Meyer IH. Minority stress and mental health in gay men. J Health Soc Behav 1995;36:38‐56. [PubMed] [Google Scholar]
- 187. Medina‐Martínez J, Saus‐Ortega C, Sánchez‐Lorente MM et al. Health inequities in LGBT people and nursing interventions to reduce them: a systematic review. Int J Environ Res Public Health 2021;18:11801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pr 2012;43:460‐7. [Google Scholar]
- 189. Lee JH, Gamarel KE, Bryant KJ et al. Discrimination, mental health, and substance use disorders among sexual minority populations. LGBT Health 2016;3:258‐65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Fredriksen‐Goldsen KI, Kim HJ, Bryan AEB et al. The cascading effects of marginalization and pathways of resilience in attaining good health among LGBT older adults. Gerontologist 2017;57:S72‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Lea T, de Wit J, Reynolds R. Minority stress in lesbian, gay, and bisexual young adults in Australia: associations with psychological distress, suicidality, and substance use. Arch Sex Behav 2014;43:1571‐8. [DOI] [PubMed] [Google Scholar]
- 192. Russell ST, Fish JN. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth. Annu Rev Clin Psychol 2016;12:465‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Scandurra C, Amodeo AL, Valerio P et al. Minority stress, resilience, and mental health: a study of Italian transgender people. J Soc Issues 2017;73:563‐85. [Google Scholar]
- 194. D'Augelli AR. Lesbian and bisexual female youths aged 14 to 21: developmental challenges and victimization experiences. J Lesbian Stud 2003;7:9‐29. [DOI] [PubMed] [Google Scholar]
- 195. McDermott E, Hughes E, Rawlings V. The social determinants of lesbian, gay, bisexual and transgender youth suicidality in England: a mixed methods study. J Public Health 2018;40:e244‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Baams L, Grossman AH, Russell ST. Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Dev Psychol 2015;51:688‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Seedat S, Scott KM, Angermeyer MC et al. Cross‐national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 2009;66:785‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Kirkbride JB, Errazuriz A, Croudace TJ et al. Incidence of schizophrenia and other psychoses in England, 1950‐2009: a systematic review and meta‐analyses. PLoS One 2012;7:e31660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Alothman D, Fogarty A. Global differences in geography, religion and other societal factors are associated with sex differences in mortality from suicide: an ecological study of 182 countries. J Affect Disord 2020;260:67‐72. [DOI] [PubMed] [Google Scholar]
- 200. Piccinelli M, Wilkinson G. Gender differences in depression. Br J Psychiatry 2000;177:486‐92. [DOI] [PubMed] [Google Scholar]
- 201. Campbell OLK, Bann D, Patalay P. The gender gap in adolescent mental health: a cross‐national investigation of 566,829 adolescents across 73 countries. SSM Popul Health 2021;13:100742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Bentivegna F, Patalay P. The impact of sexual violence in mid‐adolescence on mental health: a UK population‐based longitudinal study. Lancet Psychiatry 2022;9:874‐83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. García‐Moreno C, Zimmerman C, Morris‐Gehring A et al. Addressing violence against women: a call to action. Lancet 2015;385:1685‐95. [DOI] [PubMed] [Google Scholar]
- 204. Galmiche M, Déchelotte P, Lambert G et al. Prevalence of eating disorders over the 2000‐2018 period: a systematic literature review. Am J Clin Nutr 2019;109:1402‐13. [DOI] [PubMed] [Google Scholar]
- 205. Zeidan J, Fombonne E, Scorah J et al. Global prevalence of autism: a systematic review update. Autism Res 2022;15:778‐90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Strother E, Lemberg R, Stanford SC et al. Eating disorders in men: underdiagnosed, undertreated, and misunderstood. Eat Disord 2012;20:346‐55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Hull L, Petrides KV, Mandy W. The female autism phenotype and camouflaging: a narrative review. Rev J Autism Dev Disord 2020;7:306‐17. [Google Scholar]
- 208. Frazier TW, Georgiades S, Bishop SL et al. Behavioral and cognitive characteristics of females and males with autism in the Simons Simplex Collection. J Am Acad Child Adolesc Psychiatry 2014;53:329‐40.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. The World Bank . Women, business and the law 2023. Washington: The World Bank, 2023. [Google Scholar]
- 210. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: meta‐analyses of diagnoses and symptoms. Psychol Bull 2017;143:783‐822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Graham C, Pettinato S. Frustrated achievers: winners, losers and subjective well‐being in new market economies. J Develop Stud 2002;38:100‐40. [Google Scholar]
- 212. Garcia R, Tomlinson J. Rethinking the domestic division of labour: exploring change and continuity in the context of redundancy. Sociology 2021;55:300‐18. [Google Scholar]
- 213. McAllister A, Fritzell S, Almroth M et al. How do macro‐level structural determinants affect inequalities in mental health? – A systematic review of the literature. Int J Equity Health 2018;17:180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Mann F, Wang J, Pearce E et al. Loneliness and the onset of new mental health problems in the general population. Soc Psychiatry Psychiatr Epidemiol 2022;57:2161‐78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Leigh‐Hunt N, Bagguley D, Bash K et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017;152:157‐71. [DOI] [PubMed] [Google Scholar]
- 216. Wang J, Lloyd‐Evans B, Giacco D et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol 2017;52:1451‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. De Jong Gierveld J. A review of loneliness: concept and definitions, determinants and consequences. Rev Clin Gerontol 1998;8:73‐80. [Google Scholar]
- 218. Cacioppo JT, Cacioppo S, Boomsma DI. Evolutionary mechanisms for loneliness. Cogn Emot 2014;28:3‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Motta V. Key concept: loneliness. Philos Psychiatr Psychol 2021;28:71‐81. [Google Scholar]
- 220. Surkalim DL, Luo M, Eres R et al. The prevalence of loneliness across 113 countries: systematic review and meta‐analysis. BMJ 2022;376:e067068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Teo R, Cheng W, Cheng L et al. Global prevalence of social isolation among community‐dwelling older adults. Arch Gerontol Geriatr 2023;107:104904. [DOI] [PubMed] [Google Scholar]
- 222. Cacioppo JT, Hughes ME, Waite LJ et al. Loneliness as a specific risk factor for depressive symptoms: cross‐sectional and longitudinal analyses. Psychol Aging 2006;21:140‐51. [DOI] [PubMed] [Google Scholar]
- 223. Santini ZI, Jose PE, York Cornwell E et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 2020;5:e62‐70. [DOI] [PubMed] [Google Scholar]
- 224. Nuyen J, Tuithof M, de Graaf R et al. The bidirectional relationship between loneliness and common mental disorders in adults: findings from a longitudinal population‐based cohort study. Soc Psychiatry Psychiatr Epidemiol 2020;55:1297‐310. [DOI] [PubMed] [Google Scholar]
- 225. Lee SL, Pearce E, Ajnakina O et al. The association between loneliness and depressive symptoms among adults aged 50 years and older: a 12‐year population‐based cohort study. Lancet Psychiatry 2021;8:48‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Wang J, Mann F, Lloyd‐Evans B et al. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry 2018;18:1‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Lim MH, Rodebaugh TL, Zyphur MJ et al. Loneliness over time: the crucial role of social anxiety. J Abnorm Psychol 2016;125:620‐30. [DOI] [PubMed] [Google Scholar]
- 228. McClelland H, Evans JJ, Nowland R et al. Loneliness as a predictor of suicidal ideation and behaviour: a systematic review and meta‐analysis of prospective studies. J Affect Disord 2020;274:880‐96. [DOI] [PubMed] [Google Scholar]
- 229. Shaw RJ, Cullen B, Graham N et al. Living alone, loneliness and lack of emotional support as predictors of suicide and self‐harm: a nine‐year follow up of the UK Biobank cohort. J Affect Disord 2021;279:316‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230. Loades ME, Chatburn E, Higson‐Sweeney N et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID‐19. J Am Acad Child Adolesc Psychiatry 2020;59:1218‐39.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. UK Department for Culture, Media, and Sport . A connected society: a strategy for tackling loneliness. London: Department for Culture, Media, and Sport, 2018. [Google Scholar]
- 232. Tan M, Barkus E, Favelle S. The cross‐lagged relationship between loneliness, social support, and psychotic‐like experiences in young adults. Cogn Neuropsychiatry 2021;26:379‐93. [DOI] [PubMed] [Google Scholar]
- 233. Penninkilampi R, Casey AN, Singh MF et al. The association between social engagement, loneliness, and risk of dementia: a systematic review and meta‐analysis. J Alzheimer's Dis 2018;66:1619‐33. [DOI] [PubMed] [Google Scholar]
- 234. UK Department for Culture, Media, and Sport. Tackling loneliness evidence review. London: Department for Culture, Media, and Sport, 2022. [Google Scholar]
- 235. Faris R, Dunham H. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. Chicago/London: University of Chicago Press, 1939. [Google Scholar]
- 236. Giggs J. The distribution of schizophrenics in Nottingham. Trans Inst Br Geogr 1973;59:55‐76. [Google Scholar]
- 237. Hare EH. Mental illness and social conditions in Bristol. J Ment Sci 1956;102:349‐57. [DOI] [PubMed] [Google Scholar]
- 238. O'Donoghue B, Roche E, Lane A. Neighbourhood level social deprivation and the risk of psychotic disorders: a systematic review. Soc Psychiatry Psychiatr Epidemiol 2016;51:941‐50. [DOI] [PubMed] [Google Scholar]
- 239. Lewis G, David A, Andréasson S et al. Schizophrenia and city life. Lancet 1992;340:137‐40. [DOI] [PubMed] [Google Scholar]
- 240. Mortensen PB, Pedersen CB, Westergaard T et al. Effects of family history and place and season of birth on the risk of schizophrenia. N Engl J Med 1999;340:603‐8. [DOI] [PubMed] [Google Scholar]
- 241. Lewis G, Dykxhoorn J, Karlsson H et al. Assessment of the role of IQ in associations between population density and deprivation and nonaffective psychosis. JAMA Psychiatry 2020;77:729‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Werner S, Malaspina D, Rabinowitz J. Socioeconomic status at birth is associated with risk of schizophrenia: population‐based multilevel study. Schizophr Bull 2006;33:1373‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Sariaslan A, Larsson H, D'Onofrio B et al. Does population density and neighborhood deprivation predict schizophrenia? A nationwide Swedish family‐based study of 2.4 million individuals. Schizophr Bull 2015;41:494‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Colodro‐Conde L, Couvy‐Duchesne B, Whitfield JB et al. Association between population density and genetic risk for schizophrenia. JAMA Psychiatry 2018;75:901‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Newbury JB, Arseneault L, Caspi A et al. Association between genetic and socioenvironmental risk for schizophrenia during upbringing in a UK longitudinal cohort. Psychol Med 2022;52:1527‐37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Paksarian D, Trabjerg BB, Merikangas KR et al. The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychol Med 2018;48:305‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Solmi F, Lewis G, Zammit S et al. Neighborhood characteristics at birth and positive and negative psychotic symptoms in adolescence: findings from the ALSPAC birth cohort. Schizophr Bull 2020;46:581‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Richardson R, Westley T, Gariépy G et al. Neighborhood socioeconomic conditions and depression: a systematic review and meta‐analysis. Soc Psychiatry Psychiatr Epidemiol 2015;50:1641‐56. [DOI] [PubMed] [Google Scholar]
- 249. Solmi F, Dykxhoorn J, Kirkbride JB. Urban‐rural differences in major mental health conditions. In: Okkels N, Kristiansen CB, Munk‐Jorgensen P (eds). Mental health and illness in the city, Vol. 6. London: Springer‐Nature, 2016:1‐106. [Google Scholar]
- 250. Sundquist K, Frank G, Sundquist J. Urbanisation and incidence of psychosis and depression. Br J Psychiatry 2004;184:293‐8. [DOI] [PubMed] [Google Scholar]
- 251. Pedersen CB, Mortensen PB. Urbanicity during upbringing and bipolar affective disorders in Denmark. Bipolar Disord 2006;8:242‐7. [DOI] [PubMed] [Google Scholar]
- 252. De Graaf R, Bijl RV, Ravelli A et al. Predictors of first incidence of DSM‐III‐R psychiatric disorders in the general population: findings from the Netherlands Mental Health Survey and Incidence Study. Acta Psychiatr Scand 2002;106:303‐13. [DOI] [PubMed] [Google Scholar]
- 253. de Graaf R, ten Have M, Tuithof M et al. First‐incidence of DSM‐IV mood, anxiety and substance use disorders and its determinants: results from the Netherlands Mental Health Survey and Incidence Study‐2. J Affect Disord 2013;149:100‐7. [DOI] [PubMed] [Google Scholar]
- 254. Baranyi G, Di Marco MH, Russ TC et al. The impact of neighbourhood crime on mental health: a systematic review and meta‐analysis. Soc Sci Med 2021;282:114106. [DOI] [PubMed] [Google Scholar]
- 255. Pickett KE, Wilkinson RG. Inequality: an underacknowledged source of mental illness and distress. Br J Psychiatry 2010;197:426‐8. [DOI] [PubMed] [Google Scholar]
- 256. Tibber MS, Walji F, Kirkbride JB et al. The association between income inequality and adult mental health at the subnational level – a systematic review. Soc Psychiatry Psychiatr Epidemiol 2022;57:1‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Rotenberg M, Anderson KK, McKenzie K. Social capital and psychosis: a scoping review. Soc Psychiatry Psychiatr Epidemiol 2020;55:659‐71. [DOI] [PubMed] [Google Scholar]
- 258. Ehsan A, Klaas HS, Bastianen A et al. Social capital and health: a systematic review of systematic reviews. SSM Popul Health 2019;8:100425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Kunst AE, van Hooijdonk C, Droomers M et al. Community social capital and suicide mortality in the Netherlands: a cross‐sectional registry‐based study. BMC Public Health 2013;13:969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Okamoto M, Kawakami N, Kido Y et al. Social capital and suicide: an ecological study in Tokyo, Japan. Environ Health Prev Med 2013;18:306‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Smith NDL, Kawachi I. State‐level social capital and suicide mortality in the 50 U.S. states. Soc Sci Med 2014;120:269‐77. [DOI] [PubMed] [Google Scholar]
- 262. Dev S, Kim D. State‐ and county‐level social capital as predictors of county‐level suicide rates in the United States: a lagged multilevel study. Public Health Rep 2021;136:538‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263. Kelly BD, Davoren M, Mhaoláin ÁN et al. Social capital and suicide in 11 European countries: an ecological analysis. Soc Psychiatry Psychiatr Epidemiol 2009;44:971‐7. [DOI] [PubMed] [Google Scholar]
- 264. Han S. The dynamic relationship between social capital and suicide rates. Crisis 2023;44:240‐6. [DOI] [PubMed] [Google Scholar]
- 265. O'Donoghue B, Lyne JP, Renwick L et al. Neighbourhood characteristics and the incidence of first‐episode psychosis and duration of untreated psychosis. Psychol Med 2016;46:1367‐78. [DOI] [PubMed] [Google Scholar]
- 266. Binbay T, Drukker M, Alptekin K et al. Evidence that the wider social environment moderates the association between familial liability and psychosis spectrum outcome. Psychol Med 2012;42:2499‐510. [DOI] [PubMed] [Google Scholar]
- 267. Kirkbride JB, Boydell J, Ploubidis GBB et al. Testing the association between the incidence of schizophrenia and social capital in an urban area. Psychol Med 2008;38:1083‐94. [DOI] [PubMed] [Google Scholar]
- 268. Chase A, Dykxhoorn J, Hollander AC et al. Longitudinal association between neighbourhood‐level social capital and incidence of major psychiatric disorders: a cohort study of 1.4m people in Stockholm County, Sweden. PsyArXiv 2022; doi: 10.31234/osf.io/269rx. [DOI] [Google Scholar]
- 269. Gallagher HC, Block K, Gibbs L et al. The effect of group involvement on post‐disaster mental health: a longitudinal multilevel analysis. Soc Sci Med 2019;220:167‐75. [DOI] [PubMed] [Google Scholar]
- 270. Baker SJ, Jackson M, Jongsma H et al. The ethnic density effect in psychosis: a systematic review and multilevel meta‐analysis. Br J Psychiatry 2021;219:632‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Dykxhoorn J, Lewis G, Hollander AC et al. Association of neighbourhood migrant density and risk of non‐affective psychosis: a national, longitudinal cohort study. Lancet Psychiatry 2020;7:327‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Bécares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place 2009;15:700‐8. [DOI] [PubMed] [Google Scholar]
- 273. Ku BS, Compton MT, Walker EF et al. Social fragmentation and schizophrenia. J Clin Psychiatry 2021;83:21r13941. [DOI] [PubMed] [Google Scholar]
- 274. Zammit S, Lewis G, Rasbash J et al. Individuals, schools, and neighborhood: a multilevel longitudinal study of variation in incidence of psychotic disorders. Arch Gen Psychiatry 2010;67:914‐22. [DOI] [PubMed] [Google Scholar]
- 275. Bécares L, Dewey ME, Das‐Munshi J. Ethnic density effects for adult mental health: systematic review and meta‐analysis of international studies. Psychol Med 2018;48:2054‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Anglin DM, Lui F, Schneider M et al. Changes in perceived neighborhood ethnic density among racial and ethnic minorities over time and psychotic‐like experiences. Schizophr Res 2020;216:330‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277. Zammit S, Gunnell D, Lewis G et al. Individual‐ and area‐level influence on suicide risk: a multilevel longitudinal study of Swedish schoolchildren. Psychol Med 2014;44:267‐77. [DOI] [PubMed] [Google Scholar]
- 278. Evans J, Middleton N, Gunnell D. Social fragmentation, severe mental illness and suicide. Soc Psychiatry Psychiatr Epidemiol 2004;39:165‐70. [DOI] [PubMed] [Google Scholar]
- 279. Termorshuizen F, Braam AW, van Ameijden EJC. Neighborhood ethnic density and suicide risk among different migrant groups in the four big cities in the Netherlands. Soc Psychiatry Psychiatr Epidemiol 2015;50:951‐62. [DOI] [PubMed] [Google Scholar]
- 280. Lereya ST, Copeland WE, Costello EJ et al. Adult mental health consequences of peer bullying and maltreatment in childhood: two cohorts in two countries. Lancet Psychiatry 2015;2:524‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Kingsbury M, Clayborne Z, Colman I et al. The protective effect of neighbourhood social cohesion on adolescent mental health following stressful life events. Psychol Med 2020;50:1292‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282. Hirota T, Paksarian D, He JP et al. Associations of social capital with mental disorder prevalence, severity, and comorbidity among U.S. adolescents. J Clin Child Adolesc Psychol 2022;51:970‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Bécares L, Nazroo J, Jackson J. Ethnic density and depressive symptoms among African Americans: threshold and differential effects across social and demographic subgroups. Am J Public Health 2014;104:2334‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Halpern D, Nazroo J. The ethnic density effect: results from a national community survey of England and Wales. Int J Soc Psychiatry 2000;46:34‐46. [DOI] [PubMed] [Google Scholar]
- 285. Shankley W, Laurence J. Community ethnic density, ethnic segregation, and ethnic minorities’ common mental disorders in the UK. Health Place 2022;73:102723. [DOI] [PubMed] [Google Scholar]
- 286. Anglin DM, Galea S, Bachman P. Going upstream to advance psychosis prevention and improve public health. JAMA Psychiatry 2020;77:665‐6. [DOI] [PubMed] [Google Scholar]
- 287. Hajat A, Hsia C, O'Neill MS. Socioeconomic disparities and air pollution exposure: a global review. Curr Environ Health Rep 2015;2:440‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288. Clark C, Myron R, Stansfeld S et al. A systematic review of the evidence on the effect of the built and physical environment on mental health. J Public Ment Health 2007;6:14‐27. [Google Scholar]
- 289. Moore THM, Kesten JM, López‐López JA et al. The effects of changes to the built environment on the mental health and well‐being of adults: systematic review. Health Place 2018;53:237‐57. [DOI] [PubMed] [Google Scholar]
- 290. Rumbold AR, Giles LC, Whitrow MJ et al. The effects of house moves during early childhood on child mental health at age 9 years. BMC Public Health 2012;12:583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291. Price C, Dalman C, Zammit S et al. Association of residential mobility over the life course with nonaffective psychosis in 1.4 million young people in Sweden. JAMA Psychiatry 2018;75:1128‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292. Francesconi M, Flouri E, Kirkbride JB. The role of the built environment in the trajectories of cognitive ability and mental health across early and middle childhood: results from a street audit tool in a general‐population birth cohort. J Environ Psychol 2022;82:101847. [Google Scholar]
- 293. Braithwaite I, Zhang S, Kirkbride JB et al. Air pollution (particulate matter) exposure and associations with depression, anxiety, bipolar, psychosis and suicide risk: a systematic review and meta‐analysis. Environ Health Perspect 2019;127:126002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Borroni E, Pesatori AC, Bollati V et al. Air pollution exposure and depression: a comprehensive updated systematic review and meta‐analysis. Environ Pollut 2022;292:118245. [DOI] [PubMed] [Google Scholar]
- 295. Lin H, Guo Y, Kowal P et al. Exposure to air pollution and tobacco smoking and their combined effects on depression in six low‐ and middle‐income countries. Br J Psychiatry 2017;211:157‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Isaevska E, Moccia C, Asta F et al. Exposure to ambient air pollution in the first 1000 days of life and alterations in the DNA methylome and telomere length in children: a systematic review. Environ Res 2021;193:110504. [DOI] [PubMed] [Google Scholar]
- 297. Zundel CG, Ryan P, Brokamp C et al. Air pollution, depressive and anxiety disorders, and brain effects: a systematic review. Neurotoxicology 2022;93:272‐300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298. Dutheil F, Comptour A, Morlon R et al. Autism spectrum disorder and air pollution: a systematic review and meta‐analysis. Environ Pollut 2021;278:116856. [DOI] [PubMed] [Google Scholar]
- 299. Newbury JB, Arseneault L, Beevers S et al. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiatry 2019;76:614‐23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300. Antonsen S, Mok PLH, Webb RT et al. Exposure to air pollution during childhood and risk of developing schizophrenia: a national cohort study. Lancet Planet Health 2020;4:e64‐73. [DOI] [PubMed] [Google Scholar]
- 301. Geneshka M, Coventry P, Cruz J et al. Relationship between green and blue spaces with mental and physical health: a systematic review of longitudinal observational studies. Int J Environ Res Public Health 2021;18:9010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302. Vanaken GJ, Danckaerts M. Impact of green space exposure on children's and adolescents’ mental health: a systematic review. Int J Environ Res Public Health 2018;15:2668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303. Zhang Y, Mavoa S, Zhao J et al. The association between green space and adolescents’ mental well‐being: a systematic review. Int J Environ Res Public Health 2020;17:6640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. McCormick R. Does access to green space impact the mental well‐being of children: a systematic review. J Pediatr Nurs 2017;37:3‐7. [DOI] [PubMed] [Google Scholar]
- 305. World Health Organization . Prevention of mental disorders: effective interventions and policy options: summary report. Geneva: World Health Organization, 2004. [Google Scholar]
- 306. Institute of Medicine (US) Committee on Prevention of Mental Disorders. Reducing risks for mental disorders. Washington: National Academies Press, 1994. [PubMed] [Google Scholar]
- 307. Bloom DE, Cafiero ET, Jané‐Llopis E et al. The global economic burden of non‐communicable diseases. Geneva: World Economic Forum, 2011. [Google Scholar]
- 308. Beddington J, Cooper CL, Field J et al. The mental wealth of nations. Nature 2008;455:1057‐60. [DOI] [PubMed] [Google Scholar]
- 309. Rose G. Sick individuals and sick populations. Int J Epidemiol 2001;30:427‐32. [DOI] [PubMed] [Google Scholar]
- 310. Soneson E, Perez J, Jones PB. Principles of risk, screening, and prevention in psychiatry. In: Thompson AD, Broome MR (eds). Risk factors for psychosis: paradigms, mechanisms, and prevention. Cambridge: Academic Press, 2020:11‐43. [Google Scholar]
- 311. McGorry PD, Mei C, Chanen A et al. Designing and scaling up integrated youth mental health care. World Psychiatry 2022;21:61‐76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Fusar‐Poli P, Correll CU, Arango C et al. Preventive psychiatry: a blueprint for improving the mental health of young people. World Psychiatry 2021;20:200‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Pitkin RM. Folate and neural tube defects. Am J Clin Nutr 2007;85:285‐8S. [DOI] [PubMed] [Google Scholar]
- 314. Rose G. The strategy of preventive medicine. Oxford: Oxford Medical Publications, 1993. [Google Scholar]
- 315. Polek E, Neufeld SAS, Wilkinson P et al. How do the prevalence and relative risk of non‐suicidal self‐injury and suicidal thoughts vary across the population distribution of common mental distress (the p factor)? Observational analyses replicated in two independent UK cohorts of young people. BMJ Open 2020;10:e032494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Whittington JE, Huppert FA. Changes in the prevalence of psychiatric disorder in a community are related to changes in the mean level of psychiatric symptoms. Psychol Med 1996;26:1253‐60. [DOI] [PubMed] [Google Scholar]
- 317. Anderson J, Huppert F, Rose G. Normality, deviance and minor psychiatric morbidity in the community. Psychol Med 1993;23:475‐85. [DOI] [PubMed] [Google Scholar]
- 318. Lewis G, Hawton K, Jones P. Strategies for preventing suicide. Br J Psychiatry 1997;171:51‐4. [PubMed] [Google Scholar]
- 319. Lo Moro G, Soneson E, Jones PB et al. Establishing a theory‐based multi‐level approach for primary prevention of mental disorders in young people. Int J Environ Res Public Health 2020;17:1‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320. Hofman A, Vandenbroucke JP. Geoffrey Rose's big idea. BMJ 1992;305:1519‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321. Fazel M, Hoagwood K, Stephan S et al. Mental health interventions in schools in high‐income countries. Lancet Psychiatry 2014;1:377‐87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 322. Fazel M, Patel V, Thomas S et al. Mental health interventions in schools in low‐income and middle‐income countries. Lancet Psychiatry 2014;1:388‐98. [DOI] [PubMed] [Google Scholar]
- 323. Insel TR, Scolnick EM. Cure therapeutics and strategic prevention: raising the bar for mental health research. Mol Psychiatry 2006;11:11‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Collins P, Patel V, Joestl S. Grand challenges in global mental health. Nature 2011;475:27‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. World Health Organization . Guidelines on mental health promotive and preventive interventions for adolescents: helping adolescents thrive. Geneva: World Health Organization, 2020. [PubMed] [Google Scholar]
- 326. Salazar de Pablo G, De Micheli A, Solmi M et al. Universal and selective interventions to prevent poor mental health outcomes in young people: systematic review and meta‐analysis. Harv Rev Psychiatry 2021;29:196‐215. [DOI] [PubMed] [Google Scholar]
- 327. Arango C, Díaz‐Caneja CM, McGorry PD et al. Preventive strategies for mental health. Lancet Psychiatry 2018;5:591‐604. [DOI] [PubMed] [Google Scholar]
- 328. Barlow J, Smailagic N, Huband N et al. Group‐based parent training programmes for improving parental psychosocial health. Cochrane Database Syst Rev 2014;5:CD002020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Barlow J, Bergman H, Kornør H et al. Group‐based parent training programmes for improving emotional and behavioural adjustment in young children. Cochrane Database Syst Rev 2016;8:CD003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330. Haggerty KP, McGlynn‐Wright A, Klima T. Promising parenting programmes for reducing adolescent problem behaviours. J Child Serv 2013;8:229‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Gardner F, Leijten P, Melendez‐Torres GJ et al. The earlier the better? Individual participant data and traditional meta‐analysis of age effects of parenting interventions. Child Dev 2019;90:7‐19. [DOI] [PubMed] [Google Scholar]
- 332. Yap MBH, Morgan AJ, Cairns K et al. Parents in prevention: a meta‐analysis of randomized controlled trials of parenting interventions to prevent internalizing problems in children from birth to age 18. Clin Psychol Rev 2016;50:138‐58. [DOI] [PubMed] [Google Scholar]
- 333. Tomfohr‐Madsen LM, Giesbrecht GF, Madsen JW et al. Improved child mental health following brief relationship enhancement and co‐parenting interventions during the transition to parenthood. Int J Environ Res Public Health 2020;17:766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334. Devlin AM, Wight D, Fenton C. Are parenting practices associated with the same child outcomes in sub‐Saharan African countries as in high‐income countries? A review and synthesis. BMJ Glob Health 2018;3:e000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335. Wilson P, Rush R, Hussey S et al. How evidence‐based is an “evidence‐based parenting program”? A PRISMA systematic review and meta‐analysis of Triple P. BMC Med 2012;10:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Chu JTW, Bullen P, Farruggia SP et al. Parent and adolescent effects of a universal group program for the parenting of adolescents. Prev Sci 2015;16:609‐20. [DOI] [PubMed] [Google Scholar]
- 337. Ma KKY, Anderson JK, Burn A. Review: School‐based interventions to improve mental health literacy and reduce mental health stigma – a systematic review. Child Adolesc Ment Health 2023;28:230‐40. [DOI] [PubMed] [Google Scholar]
- 338. Hayes D, Mansfield R, Mason C et al. The impact of universal, school based, interventions on help seeking in children and young people: a systematic literature review. Eur Child Adolesc Psychiatry 2023; doi: 10.1007/s00787-022-02135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Weare K, Nind M. Mental health promotion and problem prevention in schools: what does the evidence say? Health Promot Int 2011;26:i29‐69. [DOI] [PubMed] [Google Scholar]
- 340. Smith S, Barajas K, Ellis B et al. A meta‐analytic review of randomized controlled trials of the Good Behavior Game. Behav Modif 2021;45:641‐66. [DOI] [PubMed] [Google Scholar]
- 341. Torok M, Rasmussen V, Wong Q et al. Examining the impact of the Good Behaviour Game on emotional and behavioural problems in primary school children: a case for integrating well‐being strategies into education. Aust J Educ 2019;63:292‐306. [Google Scholar]
- 342. Wilcox HC, Kellam SG, Brown CH et al. The impact of two universal randomized first‐ and second‐grade classroom interventions on young adult suicide ideation and attempts. Drug Alcohol Depend 2008;95:S60‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. Werner‐Seidler A, Spanos S, Calear AL et al. School‐based depression and anxiety prevention programs: an updated systematic review and meta‐analysis. Clin Psychol Rev 2021;89:102079. [DOI] [PubMed] [Google Scholar]
- 344. Werner‐Seidler A, Perry Y, Calear AL et al. School‐based depression and anxiety prevention programs for young people: a systematic review and meta‐analysis. Clin Psychol Rev 2017;51:30‐47. [DOI] [PubMed] [Google Scholar]
- 345. Stockings EA, Degenhardt L, Dobbins T et al. Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychol Med 2016;46:11‐26. [DOI] [PubMed] [Google Scholar]
- 346. Dunning D, Tudor K, Radley L et al. Do mindfulness‐based programmes improve the cognitive skills, behaviour and mental health of children and adolescents? An updated meta‐analysis of randomised controlled trials. Evid Based Ment Health 2022;25:135‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Katz C, Bolton SL, Katz LY et al. A systematic review of school‐based prevention programs. Depress Anxiety 2013;30:1030‐45. [DOI] [PubMed] [Google Scholar]
- 348. Gijzen MWM, Rasing SPA, Creemers DHM et al. Effectiveness of school‐based preventive programs in suicidal thoughts and behaviors: a meta‐analysis. J Affect Disord 2022;298:408‐20. [DOI] [PubMed] [Google Scholar]
- 349. Pistone I, Beckman U, Eriksson E et al. The effects of educational interventions on suicide: a systematic review and meta‐analysis. Int J Soc Psychiatry 2019;65:399‐412. [DOI] [PubMed] [Google Scholar]
- 350. Wasserman D, Hoven CW, Wasserman C et al. School‐based suicide prevention programmes: the SEYLE cluster‐randomised, controlled trial. Lancet 2015;385:1536‐44. [DOI] [PubMed] [Google Scholar]
- 351. Andrews JL, Schweizer S. The need for functional assessments in school‐based mental health intervention research. JAMA Psychiatry 2023;80:103‐4. [DOI] [PubMed] [Google Scholar]
- 352. Foulkes L, Stringaris A. Do no harm: can school mental health interventions cause iatrogenic harm? BJPsych Bull 2023;47:267‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353. Hsueh YC, Batchelor R, Liebmann M et al. A systematic review of studies describing the effectiveness, acceptability, and potential harms of place‐based interventions to address loneliness and mental health problems. Int J Environ Res Public Health 2022;19:4766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354. Na PJ, Jeste DV, Pietrzak RH. Social disconnection as a global behavioral epidemic – a call to action about a major health risk factor. JAMA Psychiatry 2023;80:101‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355. Wilkinson RG, Pickett KE. The enemy between us: the psychological and social costs of inequality. Eur J Soc Psychol 2017;47:11‐24. [Google Scholar]
- 356. Paul KI, Moser K. Unemployment impairs mental health: meta‐analyses. J Vocat Behav 2009;74:264‐82. [Google Scholar]
- 357. Simpson J, Albani V, Bell Z et al. Effects of social security policy reforms on mental health and inequalities: a systematic review of observational studies in high‐income countries. Soc Sci Med 2021;272:113717. [DOI] [PubMed] [Google Scholar]
- 358. Forget EL. New questions, new data, old interventions: the health effects of a guaranteed annual income. Prev Med 2013;57:925‐8. [DOI] [PubMed] [Google Scholar]
- 359. Zaneva M, Guzman‐Holst C, Reeves A et al. The impact of monetary poverty alleviation programs on children's and adolescents’ mental health: a systematic review and meta‐analysis across low‐, middle‐, and high‐income countries. J Adolesc Health 2022;71:147‐56. [DOI] [PubMed] [Google Scholar]
- 360. Fuller AE, Zaffar N, Cohen E et al. Cash transfer programs and child health and family economic outcomes: a systematic review. Can J Public Health 2022;113:433‐45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Zimmerman A, Garman E, Avendano‐Pabon M et al. The impact of cash transfers on mental health in children and young people in low‐income and middle‐income countries: a systematic review and meta‐analysis. BMJ Glob Health 2021;6:e004661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. McGuire J, Kaiser C, Bach‐Mortensen AM. A systematic review and meta‐analysis of the impact of cash transfers on subjective well‐being and mental health in low‐ and middle‐income countries. Nat Hum Behav 2022;6:359‐70. [DOI] [PubMed] [Google Scholar]
- 363. Kilburn K, Thirumurthy H, Halpern CT et al. Effects of a large‐scale unconditional cash transfer program on mental health outcomes of young people in Kenya. J Adolesc Health 2016;58:223‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Costello EJ, Compton SN, Keeler G et al. Relationships between poverty and psychopathology JAMA 2003;290:2023‐9. [DOI] [PubMed] [Google Scholar]
- 365. Fernald LC, Gertler PJ, Neufeld LM. 10‐year effect of Oportunidades, Mexico's conditional cash transfer programme, on child growth, cognition, language, and behaviour: a longitudinal follow‐up study. Lancet 2009;374:1997‐2005. [DOI] [PubMed] [Google Scholar]
- 366. Ladhani S, Sitter KC. Conditional cash transfers: a critical review. Dev Policy Rev 2020;38:28‐41. [Google Scholar]
- 367. Van den Bergh BRH. Developmental programming of early brain and behaviour development and mental health: a conceptual framework. Dev Med Child Neurol 2011;53:19‐23. [DOI] [PubMed] [Google Scholar]
- 368. Kendrick D, Elkan R, Hewitt M et al. Does home visiting improve parenting and the quality of the home environment? A systematic review and meta analysis. Arch Dis Child 2000;82:443‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369. Masud H, Ahmad MS, Cho KW et al. Parenting styles and aggression among young adolescents: a systematic review of literature. Community Ment Health J 2019;55:1015‐30. [DOI] [PubMed] [Google Scholar]
- 370. Olds DL, Kitzman H, Cole R et al. Effects of nurse home‐visiting on maternal life course and child development: age 6 follow‐up results of a randomized trial. Pediatrics 2004;114:1550‐9. [DOI] [PubMed] [Google Scholar]
- 371. Olds D, Henderson JCR, Cole R et al. Long‐term effects of nurse home visitation on children's criminal and antisocial behavior. JAMA 1998;280:1238‐44. [DOI] [PubMed] [Google Scholar]
- 372. Olds DL. Prenatal and infancy home visiting by nurses: from randomized trials to community replication. Prev Sci 2002;3:153‐72. [DOI] [PubMed] [Google Scholar]
- 373. Goldfeld S, Bryson H, Mensah F et al. Nurse home visiting to improve child and maternal outcomes: 5‐year follow‐up of an Australian randomised controlled trial. PLoS One 2022;17:e0277773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374. O'Brien DT, Farrell C, Welsh BC. Broken (windows) theory: a meta‐analysis of the evidence for the pathways from neighborhood disorder to resident health outcomes and behaviors. Soc Sci Med 2019;228:272‐92. [DOI] [PubMed] [Google Scholar]
- 375. Leventhal T, Brooks‐Gunn J. Moving to opportunity: an experimental study of neighborhood effects on mental health. Am J Public Health 2003;93:1576‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Kessler RC, Duncan GJ, Gennetian LA et al. Notice of retraction and replacement: Kessler RC et al. Associations of housing mobility interventions for children in high‐poverty neighborhoods with subsequent mental disorders during adolescence. JAMA 2016;316:227‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377. Kessler RC, Duncan GJ, Gennetian LA et al. Associations of housing mobility interventions for children in high‐poverty neighborhoods with subsequent mental disorders during adolescence. JAMA 2014;311:937‐47. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 378. Rudolph KE, Gimbrone C, Díaz I. Helped into harm. Epidemiology 2021;32:336‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379. Jongeneel‐Grimen B, Droomers M, Kramer D et al. Impact of a Dutch urban regeneration programme on mental health trends: a quasi‐experimental study. J Epidemiol Community Health 2016;70:967‐73. [DOI] [PubMed] [Google Scholar]
- 380. South EC, Hohl BC, Kondo MC et al. Effect of greening vacant land on mental health of community‐dwelling adults. JAMA Netw Open 2018;1:e180298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381. Chen KL, Miake‐Lye IM, Begashaw MM et al. Association of promoting housing affordability and stability with improved health outcomes. JAMA Netw Open 2022;5:e2239860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382. Nosè M, Ballette F, Bighelli I et al. Psychosocial interventions for post‐traumatic stress disorder in refugees and asylum seekers resettled in high‐income countries: systematic review and meta‐analysis. PLOS One 2017;12:e0171030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383. Orang TM, Missmahl I, Gardisi M et al. Rethinking mental health care provided to migrants and refugees; a randomized controlled trial on the effectiveness of Value Based Counseling, a culturally sensitive, strength‐based psychological intervention. PLoS One 2023;18:e0283889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 384. Bryant RA, Malik A, Aqel IS et al. Effectiveness of a brief group behavioural intervention on psychological distress in young adolescent Syrian refugees: a randomised controlled trial. PLoS Med 2022;19:e1004046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385. Bryant RA, Bawaneh A, Awwad M et al. Twelve‐month follow‐up of a randomised clinical trial of a brief group psychological intervention for common mental disorders in Syrian refugees in Jordan. Epidemiol Psychiatr Sci 2022;31:e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386. Cowling MM, Anderson JR. The effectiveness of therapeutic interventions on psychological distress in refugee children: a systematic review. J Clin Psychol 2023;79:1857‐74. [DOI] [PubMed] [Google Scholar]
- 387. Villalonga‐Olives E, Wind TR, Armand AO et al. Social‐capital‐based mental health interventions for refugees: a systematic review. Soc Sci Med 2022;301:114787. [DOI] [PubMed] [Google Scholar]
- 388. Gardner F, Leijten P, Mann J et al. Could scale‐up of parenting programmes improve child disruptive behaviour and reduce social inequalities? Using individual participant data meta‐analysis to establish for whom programmes are effective and cost‐effective. Southampton: NIHR Journals Library, 2017. [PubMed] [Google Scholar]
- 389. Reid MJ, Webster‐Stratton C, Beauchaine TP. Parent training in Head Start: a comparison of program response among African American, Asian American, Caucasian, and Hispanic mothers. Prev Sci 2001;2:209‐27. [DOI] [PubMed] [Google Scholar]
- 390. Ellis DM, Draheim AA, Anderson PL. Culturally adapted digital mental health interventions for ethnic/racial minorities: a systematic review and meta‐analysis. J Consult Clin Psychol 2022;90:717‐33. [DOI] [PubMed] [Google Scholar]
- 391. Arundell LL, Barnett P, Buckman JEJ et al. The effectiveness of adapted psychological interventions for people from ethnic minority groups: a systematic review and conceptual typology. Clin Psychol Rev 2021;88:102063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392. Misra S, Jackson VW, Chong J et al. Systematic review of cultural aspects of stigma and mental illness among racial and ethnic minority groups in the United States: implications for interventions. Am J Community Psychol 2021;68:486‐512. [DOI] [PubMed] [Google Scholar]
- 393. Coulter RWS, Egan JE, Kinsky S et al. Mental health, drug, and violence interventions for sexual/gender minorities: a systematic review. Pediatrics 2019;144:e20183367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394. Yung AR, Yuen HP, McGorry PD et al. Mapping the onset of psychosis: the Comprehensive Assessment of At‐Risk Mental States. Aust N Z J Psychiatry 2005;39:964‐71. [DOI] [PubMed] [Google Scholar]
- 395. McDonald K, Ding T, Ker H et al. Using epidemiological evidence to forecast population need for early treatment programmes in mental health: a generalisable Bayesian prediction methodology applied to and validated for first‐episode psychosis in England. Br J Psychiatry 2021;219:383‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396. Kapadia D, Zhang J, Salway S et al. Ethnic inequalities in healthcare: a rapid evidence review. London: NHS Race & Health Observatory, 2022. [Google Scholar]
- 397. Kirkbride JB, Stochl J, Zimbrón J et al. Social and spatial heterogeneity in psychosis proneness in a multilevel case‐prodrome‐control study. Acta Psychiatr Scand 2015;132:283‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398. Ajnakina O, Morgan C, Gayer‐Anderson C et al. Only a small proportion of patients with first episode psychosis come via prodromal services: a retrospective survey of a large UK mental health programme. BMC Psychiatry 2017;17:308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 399. Burke T, Thompson A, Mifsud N et al. Proportion and characteristics of young people in a first‐episode psychosis clinic who first attended an at‐risk mental state service or other specialist youth mental health service. Schizophr Res 2022;241:94‐101. [DOI] [PubMed] [Google Scholar]
- 400. Vostanis P, Svirydzenka N, Dugard P et al. Mental health service use by adolescents of Indian and White origin. Arch Dis Child 2013;98:764‐7. [DOI] [PubMed] [Google Scholar]
- 401. McGlashan T, Walsh B, Woods S. The psychosis‐risk syndrome: handbook for diagnosis and follow‐up. Oxford: Oxford University Press, 2010. [Google Scholar]
- 402. Mak WWS, Law RW, Alvidrez J et al. Gender and ethnic diversity in NIMH‐funded clinical trials: review of a decade of published research. Adm Policy Ment Health 2007;34:497‐503. [DOI] [PubMed] [Google Scholar]
- 403. Griffiths SL, Brown L, Kirkbride JB. Disrupting the status quo: is bolder action needed to tackle the complexity of psychosis risk and prevention? Br J Psychiatry 2023;223:394. [DOI] [PubMed] [Google Scholar]
- 404. Bickerdike L, Booth A, Wilson PM et al. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open 2017;7:e013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405. Aughterson H, Baxter L, Fancourt D. Social prescribing for individuals with mental health problems: a qualitative study of barriers and enablers experienced by general practitioners. BMC Fam Pract 2020;21:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406. Husk K, Elston J, Gradinger F et al. Social prescribing: where is the evidence? Br J Gen Pract 2019;69:6‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407. Husk K, Blockley K, Lovell R et al. What approaches to social prescribing work, for whom, and in what circumstances? A realist review. Health Soc Care Community 2020;28:309‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408. Napierala H, Krüger K, Kuschick D et al. Social prescribing: systematic review of the effectiveness of psychosocial community referral interventions in primary care. Int J Integr Care 2022;22:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409. Cooper M, Avery L, Scott J et al. Effectiveness and active ingredients of social prescribing interventions targeting mental health: a systematic review. BMJ Open 2022;12:e060214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 410. Tanner LM, Wildman JM, Stoniute A et al. Non‐pharmaceutical primary care interventions to improve mental health in deprived populations: a systematic review. Br J Gen Pract 2023;73:e242‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 411. McGrath M, Duncan F, Dotsikas K et al. Effectiveness of community interventions for protecting and promoting the mental health of working‐age adults experiencing financial uncertainty: a systematic review. J Epidemiol Community Health 2021;75:665‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412. Tierney S, Akinyemi O, Carder‐Gilbert H et al. What does the evidence tell us about accessibility of social prescribing schemes in England to people from Black and ethnic minority backgrounds? London: National Academy for Social Prescribing, 2022. [Google Scholar]
- 413. Modini M, Tan L, Brinchmann B et al. Supported employment for people with severe mental illness: systematic review and meta‐analysis of the international evidence. Br J Psychiatry 2016;209:14‐22. [DOI] [PubMed] [Google Scholar]
- 414. Crowther R, Marshall M, Bond GR et al. Vocational rehabilitation for people with severe mental illness. Cochrane Database Syst Rev 2001;2:CD003080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415. Suijkerbuijk YB, Schaafsma FG, van Mechelen JC et al. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta‐analysis. Cochrane Database Syst Rev 2017;9:CD011867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416. Fowler D, Hodgekins J, French P. Social recovery therapy in improving activity and social outcomes in early psychosis: current evidence and longer term outcomes. Schizophr Res 2019;203:99‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417. Rinaldi M, Perkins R, Glynn E et al. Individual placement and support: from research to practice. Adv Psychiatr Treat 2008;14:50‐60. [Google Scholar]
- 418. Bond GR, Drake RE, Luciano A. Employment and educational outcomes in early intervention programmes for early psychosis: a systematic review. Epidemiol Psychiatr Sci 2015;24:446‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 419. De Winter L, Couwenbergh C, Van Weeghel J et al. Who benefits from individual placement and support? A meta‐analysis. Epidemiol Psychiatr Sci 2022;31:e50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420. Kuipers E. Family interventions in schizophrenia: evidence for efficacy and proposed mechanisms of change. J Fam Ther 2006;28:73‐80. [Google Scholar]
- 421. Pharoah F, Mari J, Rathbone J et al. Family intervention for schizophrenia. Cochrane Database Syst Rev 2006;4:CD000088. [DOI] [PubMed] [Google Scholar]
- 422. Poole LA, Knight T, Toumbourou JW et al. A randomized controlled trial of the impact of a family‐based adolescent depression intervention on both youth and parent mental health outcomes. J Abnorm Child Psychol 2018;46:169‐81. [DOI] [PubMed] [Google Scholar]
- 423. Diamond GS, Wintersteen MB, Brown GK et al. Attachment‐based family therapy for adolescents with suicidal ideation: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2010;49:122‐31. [DOI] [PubMed] [Google Scholar]
- 424. Eckshtain D, Horn R, Weisz JR. Family‐based interventions for youth depression: meta‐analysis of randomized clinical trials. Child Psychiatry Hum Dev 2023;54:1737‐48. [DOI] [PubMed] [Google Scholar]
- 425. Pedersen GA, Smallegange E, Coetzee A et al. A systematic review of the evidence for family and parenting interventions in low‐ and middle‐income countries: child and youth mental health outcomes. J Child Fam Stud 2019;28:2036‐55. [Google Scholar]
- 426. Healy EA, Kaiser BN, Puffer ES. Family‐based youth mental health interventions delivered by nonspecialist providers in low‐ and middle‐income countries: a systematic review. Fam Syst Health 2018;36:182‐97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427. Nijdam MJ, Gersons BPR, Reitsma JB et al. Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing therapy for post‐traumatic stress disorder: randomised controlled trial. Br J Psychiatry 2012;200:224‐31. [DOI] [PubMed] [Google Scholar]
- 428. John‐Baptiste Bastien R, Jongsma HE et al. The effectiveness of psychological interventions for post‐traumatic stress disorder in children, adolescents and young adults: a systematic review and meta‐analysis. Psychol Med 2020;50:1598‐612. [DOI] [PubMed] [Google Scholar]
- 429. Han HR, Miller HN, Nkimbeng M et al. Trauma informed interventions: a systematic review. PLoS One 2021;16:e0252747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430. Ottisova L, Gillard JA, Wood M et al. Effectiveness of psychosocial interventions in mitigating adverse mental health outcomes among disaster‐exposed health care workers: a systematic review. J Trauma Stress 2022;35:746‐58. [DOI] [PubMed] [Google Scholar]
- 431. Bloomfield MAP, Yusuf FNIB, Srinivasan R et al. Trauma‐informed care for adult survivors of developmental trauma with psychotic and dissociative symptoms: a systematic review of intervention studies. Lancet Psychiatry 2020;7:449‐62. [DOI] [PubMed] [Google Scholar]
- 432. Gillies D, Taylor F, Gray C et al. Psychological therapies for the treatment of post‐traumatic stress disorder in children and adolescents. Cochrane Database Syst Rev 2012;12:CD006726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433. Purgato M, Gross AL, Betancourt T et al. Focused psychosocial interventions for children in low‐resource humanitarian settings: a systematic review and individual participant data meta‐analysis. Lancet Glob Health 2018;6:e390‐400. [DOI] [PubMed] [Google Scholar]
- 434. Harper Shehadeh M, Heim E, Chowdhary N et al. Cultural adaptation of minimally guided interventions for common mental disorders: a systematic review and meta‐analysis. JMIR Ment Health 2016;3:e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 435. United Nations Office of the High Commissioner for Human Rights . Equality is at the heart of human rights. www.ohchr.org.
- 436. Barendse MEA, Lara GA, Guyer AE et al. Sex and pubertal influences on the neurodevelopmental underpinnings of schizophrenia: a case for longitudinal research on adolescents. Schizophr Res 2023;252:231‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437. Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry 2010;22:429‐36. [DOI] [PubMed] [Google Scholar]
- 438. Hughes K, Ford K, Bellis MA et al. Health and financial costs of adverse childhood experiences in 28 European countries: a systematic review and meta‐analysis. Lancet Public Health 2021;6:e848‐57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 439. Bellis MA, Lowey H, Leckenby N et al. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. J Public Health 2014;36:81‐91. [DOI] [PubMed] [Google Scholar]
- 440. Fazel M, Soneson E. Recent advances in child and adolescent public mental health interventions. J Child Psychol Psychiatry 2023; doi: 10.31234/osf.io/269rx. [DOI] [PubMed]
- 441. NewYork‐Presbyterian Ambulatory Care Network . The Uptown Hub. www.nyp.org.
- 442. Stochl J, Ford T, Perez J et al. Modernising measurement in psychiatry: item banks and computerised adaptive testing. Lancet Psychiatry 2021;8:354‐6. [DOI] [PubMed] [Google Scholar]
- 443. Ford T, Mansfield KL, Markham S et al. The challenges and opportunities of mental health data sharing in the UK. Lancet Digit Health 2021;3:e333‐6. [DOI] [PubMed] [Google Scholar]
- 444. World Health Organization . Social determinants of mental health. Geneva: World Health Organization, 2014. [Google Scholar]
- 445. Campion J, Bhugra D, Bailey S et al. Inequality and mental disorders: opportunities for action. Lancet 2013;382:183‐4. [DOI] [PubMed] [Google Scholar]
- 446. Shonkoff JP, Garner AS. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012;129:e232‐46. [DOI] [PubMed] [Google Scholar]
- 447. Griffiths SL, Wood SJ, Birchwood M. Vulnerability to psychosocial disability in psychosis. Epidemiol Psychiatr Sci 2019;28:140‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448. Anglin DM, Ereshefsky S, Klaunig MJ et al. From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am J Psychiatry 2021;178:599‐610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 449. Jeffers NK, Berger BO, Marea CX et al. Investigating the impact of structural racism on black birthing people – associations between racialized economic segregation, incarceration inequality, and severe maternal morbidity. Soc Sci Med 2023;317:115622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450. Duncan GJ, Magnuson K, Votruba‐Drzal E. Moving beyond correlations in assessing the consequences of poverty. Annu Rev Psychol 2017;68:413‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451. Skinner GCM, Bywaters PWB, Kennedy E. A review of the relationship between poverty and child abuse and neglect: insights from scoping reviews, systematic reviews and meta‐analyses. Child Abuse Rev 2023;32:e2795. [Google Scholar]
- 452. Ferguson HB, Bovaird S, Mueller MP. The impact of poverty on educational outcomes for children. Paediatr Child Health 2007;12:701‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453. Ladd GW, Birch SH, Buhs ES. Children's social and scholastic lives in kindergarten: related spheres of influence? Child Dev 1999;70:1373‐400. [DOI] [PubMed] [Google Scholar]
- 454. Lesner R V. The long‐term effect of childhood poverty. J Popul Econ 2018;31:969‐1004. [Google Scholar]
- 455. Mood C, Jonsson JO. The social consequences of poverty: an empirical test on longitudinal data. Soc Indic Res 2016;127:633‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456. Sariaslan A, Mikkonen J, Aaltonen M et al. No causal associations between childhood family income and subsequent psychiatric disorders, substance misuse and violent crime arrests: a nationwide Finnish study of >650 000 individuals and their siblings. Int J Epidemiol 2021;50:1628‐38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457. Davis OSP, Haworth CMA, Lewis CM et al. Visual analysis of geocoded twin data puts nature and nurture on the map. Mol Psychiatry 2012;17:867‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458. Hernan MA, Robins JM. Causal inference: what if. Boca Raton: Chapman & Hall, 2020. [Google Scholar]
- 459. Keyes KM, Galea S. The limits of risk factors revisited: is it time for a causal architecture approach? Epidemiology 2017;28:1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460. Munafò MR, Nosek BA, Bishop DVM et al. A manifesto for reproducible science. Nat Hum Behav 2017;1:0021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461. Hayes J, Carvajal‐Velez L, Hijazi Z et al. You can't manage what you do not measure – Why adolescent mental health monitoring matters. J Adolesc Health 2023;72:S7‐8. [DOI] [PubMed] [Google Scholar]
- 462. Bastien RJB, Ding T, Gonzalez‐Valderrama A et al. The incidence of non‐affective psychotic disorders in low and middle‐income countries: a systematic review and meta‐analysis. Soc Psychiatry Psychiatr Epidemiol 2023;58:523‐36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463. McElroy E, Villadsen A, Patalay P et al. Harmonisation and measurement properties of mental health measures in six British cohorts. London: CLOSER, 2020. [Google Scholar]
- 464. Cookson R, Doran T, Asaria M et al. The inverse care law re‐examined: a global perspective. Lancet 2021;397:828‐38. [DOI] [PubMed] [Google Scholar]


