ABSTRACT
Social Determinant of Health (SDOH) data are important targets for research and innovation in Health Information Systems (HIS). The ways we envision SDOH in “smart” information systems will play a considerable role in shaping future population health landscapes. Current methods for data collection can capture wide ranges of SDOH factors, in standardised and non-standardised formats, from both primary and secondary sources. Advances in automating data linkage and text classification show particular promise for enhancing SDOH in HIS. One challenge is that social communication processes embedded in data collection are directly related to the inequalities that HIS attempt to measure and redress. To advance equity, it is imperative thatcare-providers, researchers, technicians, and administrators attend to power dynamics in HIS standards and practices. We recommend: 1. Investing in interdisciplinary and intersectoral knowledge generation and translation. 2. Developing novel methods for data discovery, linkage and analysis through participatory research. 3. Channelling information into upstream evidence-informed policy.
KEYWORDS: Social Determinants of Health, digital transformation, electronic health records, big data, population health, precision medicine, health equity
1. Introduction
1.1. Social Determinants of Health (SDOH) and Health Information Systems (HIS)
Social determinants of health (SDOH) refer to “the conditions in which people are born, grow, live, work and age” (Marmot et al., 2008). SDOH arise from various forces (social, political, economic) which contribute to individual factors with significant influence over health status, e.g., income, education, culture, and so on. Individual and population-level data reveal predictable, independent, and intersectional associations between SDOH variables and health outcomes (Conway et al., 2019; Gold et al., 2018; Gottlieb et al., 2015; Lofters et al., 2017; Marmot et al., 2008). There are various material, psychosocial, and neo-material pathways (Raphael et al., 2020) leading to intersections of access and privilege contributing to health status (Crenshaw, 2017; Hankivsky & Christoffersen, 2008). Health inequities (variations in health outcomes, which are unjust due to their relationship to social determinants, as per Kawachi et al., 2002), are primarily measured by availability and quality of resources, level and quality of social connectedness, and relative status within a population. Health equity is a core concept of population health promotion, and a primary objective of SDOH paradigms (Lucyk, 2018; Lucyk & McLaren, 2017).
Greater attention to SDOH and health equity has facilitated international and interdisciplinary partnerships to alleviate and advance our understanding of health disparities through health metrics, e.g., the Institute of Medicine Measures of Social and Behavioural Determinants (Bambas, 2005; Giuse et al., 2017). In a health information system (HIS), SDOH may be codified based on individual attributes, such as annual income, level of education, occupation, domestic status, as well as by the characteristics of a population. These can include median income level, density of services, level and type of education, paid employment, cultural values, migration, etc. (Public Health Agency of Canada [PHAC], 2016; Raphael et al., 2020). Measurements of SDOH are relevant for profiling, prediction, and targeted response; facilitating comprehensive care, treatment, and prevention (Hewner et al., 2017; Monsen et al., 2017; Winden et al., 2018). Combined with effective knowledge dissemination and translation, SDOH data provide potential for novel insights into determinants of health, which can lead to more comprehensive and precise healthcare decision-making, both in clinical and policy-making spheres (Barbosa & Nelson, 2016; Brewer et al., 2020; Chiolero & Buckeride, 2020; Hunter et al., 2015; Zhang et al., 2017).
As HIS digitise, health data are becoming more frequently managed in Electronic Health Records (EHRs) or similar virtual health information storage and management (e.g., Community Health Records, Electronic Medical Records, etc.; Beck et al., 2012; Winden et al., 2018). These tools can facilitate data sharing (Bazemore et al., 2016; Shahmoradi et al., 2017) and generate greater quantities of standardised data suitable for analysis (Mooney & Pejaver, 2018). Through large data sets, SDOH information in health systems may enhance capacity to identify and predict health risk, and may promote better understanding of relationships between health determinants in complex systems (Kasthurirathne et al., 2020; Kwon et al., 2021; Thapa et al., 2021). With EHRs becoming more prevalent, greater quantities of patient data will be available in digitised and analysis-ready format (Ehrenstein et al., 2019).
“Smart” health systems are capable of continuously enhancing their capacity to incorporate, manage, analyse, and share information. Automating data collection processes are important developments towards unlocking the potential of “Big Data”/AI in the health sector. Improving the technological efficiency of HIS strengthens the flow of health data (Figure 1). As EHRs are increasingly adopted in health systems, there are many anticipated opportunities for innovation in research and design (R&D), including improvements to surveillance and forecasting, better interoperability between data-holders and enhanced communication for data-driven decision-making (Bauer et al., 2020; Chiolero & Buckeride, 2020; Mooney & Pejaver, 2018). From a methodological point of view, however, there is still a considerable need for applied and theoretical research on data collection and incorporating SDOH as meaningful data points into HIS (Theiss & Regenstein, 2017). In this viewpoint article, we aim to explore avenues for SDOH data collection from technical and social perspectives.
Figure 1.
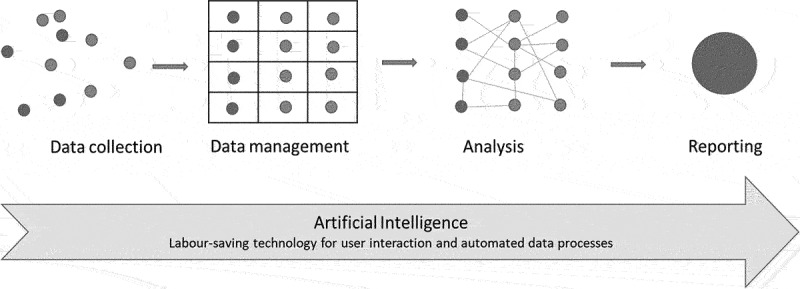
Stages in information flow.
2. Perspective
2.1. SDOH data collection practices in EHR systems
EHR data on SDOH can include individual and population-level variables. These vary by site but can include variables such as: income status, education, occupation, housing status, food security, race, ethnicity, immigration status, sexual orientation, gender identity, intimate partner violence, social connectedness, disability status, family size and status, religion and spirituality, access to services, and neighbourhood socioeconomic conditions, and others (Lindemann et al., 2017; Lofters et al., 2017; Monsen et al., 2016; Pinto et al., 2019, 2016; Winden et al., 2018). EHR systems can prompt data collection within a standard set of variables. These may be based on calls to research and action from stakeholders in the health system at large (professional organisations, research institutes, patient groups, etc.) or specific HIS goals (e.g., effective resource allocation, population surveillance, clinical/epidemiological research agendas; Adler & Stead, 2015; Chen et al., 2014; Chhabra et al., 2019; Gold et al., 2017; Gottlieb et al., 2015; Hripcsak et al., 2015; Lewis et al., 2016).
Currently, research on SDOH data collection in EHR systems focuses on data available through patient–provider interactions in health care settings. HIS SDOH input may come from human transcribers (e.g., in clinical notes or carts), or automated survey instruments (e.g., intake questionnaires). This does not necessarily need to take place in physical health care settings, with the internet playing a greater role in digital transmission of health information. Similarly, although not mainstream, it is a promising avenue for data science, nonetheless, incorporating geocoded census data (Biro et al., 2016) or other records relevant to the patient available through public repositories or archives, is a promising entry point for SDOH into HIS. Additional data sources and data holders for SDOH may include social media, satellite imagery, public archives, and so on and can be merged with data sets for population health analysis (Thapa et al., 2021).
Some of the potential for AI in SDOH data retrieval and analysis in EHR systems comes from the ability to mine relevant SDOH information captured in clinical notes through Machine Learning (ML), such as Natural Language Processing (NLP), or other text classification methods (Feller et al., 2018; Kino et al., 2021; Stemerman, 2020; Teng & Wilcox, 2022). Advanced computational analysis of SDOH variables collected through EHRs has contributed to great accuracy in assessing risk factors for various health outcomes (Comer et al., 2011; Feller et al., 2018; Jamei et al., 2017; Navathe et al., 2018; Oreskovic et al., 2017; Roth et al., 2014; Ye et al., 2018). These may be applied to assessing psychosocial conditions, infectious disease transmission, and risk of hospital (re)admissions. The use of free-text data may increase as NLP algorithms and other ML coding advances and is incorporated into HIS (Lindemann et al., 2017). Enhancing the volume and quality of data, for example, by linking multiple sources of information, can lead to considerable analytical advantages through ML (Jamei et al., 2017; Roth et al., 2014; Teng & Wilcox, 2022; Ye et al., 2018). Linking data from multiple sources, through fair and transparent relationships between partners and stakeholders, is a vital step in encoding comprehensive SDOH data in HIS (Jain et al., 2017). The availability and usability of SDOH data depends on how HIS uses technology to maintain and strengthen relationships with end users (Zulman et al., 2016).
2.2. Avoiding inequities in health and social communication processes
The widespread adoption of standardised collection tools in EHRs is an important direction for applied research (Adler & Stead, 2015; Gold et al., 2017). Currently, clinical notes and screening questions are key sources of SDOH data. One challenge is that although SDOH are highly relevant for health, screening or dialogue on SDOH is not often part of standard clinical exchanges (Gottlieb et al., 2015; Winden et al., 2018). The nature of SDOH and the information they represent, which are subjective, intersectional, and socially constructed (Lucyk & McLaren, 2017), may also complicate the development of data collection methods and tools. There may also be deficits in the ability to conceptualise or use SDOH data in the health care setting (Hatef et al., 2019), especially the ability to translate SDOH information into meaningfully enhanced care plans or population health efforts (Breen et al., 2019). These, and other challenges pertaining to translating such complex constructs into valid measurements (e.g., social desirability bias (Krumpal, 2013)), often result in missing or unreliable information of interest when it comes to SDOH (Pinto et al., 2016).
In addition to the way in which individuals interact socially in care settings, health information collection also faces the issue of who may be systematically excluded from certain care or data collection settings (Pinto et al., 2016). SDOH data currently collected through EHR systems may represent only a subset of the population (e.g., primary care users and/or those routinely participating in census surveys). EHR-derived data for population-level analyses of social risk would therefore be limited due to limitations in who is represented in the sample. EHR systems can conceivably incorporate various details on socio-economic conditions to patient records from multiple sources. Geocoded data or other types of linked data, including from GPS or personal smartphone apps, are also realistic possibilities for capturing and representing SDOH in EHR systems. However, global HIS are still in the early stages of developing robust legal and ethical frameworks to protect privacy and user-rights (World Health Organization [WHO], 2021).
Finally, as technology permits further automation in analytics and communication processes, existing biases in communication processes can have detrimental and multifaceted implications for health (Ntoutsi et al., 2020). For example, implicit biases increase the risk of inappropriate diagnosis and/or treatment recommendations (Syed, 2021). Furthermore, when biases manifest in social interactions, this can distort communication channels required for SDOH data collection, as well as trusting and caring connections at the centre of healing relationships (Allan & Smylie, 2015; Armstrong et al., 2001; Browne et al., 2018). The convergence of data streams, the manner in which information is determined to be relevant or irrelevant, and the complexities of coding and encoding in communication systems (Hall, 2009) affect embodied experiences within systems. There is therefore a risk that automating SDOH data collection processes, within systems currently characterised by many forms of social biases, could exacerbate health inequity.
2.3. Advancing health equity through SDOH perspectives
The SDOH perspective relies on interdisciplinary explanations for mechanisms and causal relationships within the data (Bryant, 2009; Raphael & Bryant, 2015). For example, from an SDOH perspective, poverty is not necessarily a phenomenon resulting from behaviour or lifestyle choices, but is equally related to features intrinsic to the social environment (languages, roles, abilities, and relationships available to an individual), and the circumstances one is born into (Marmot et al., 2008). Disadvantages experienced by patients contribute to each other, and compound across multiple dimensions of health, in ways directly related to their access to communication and information systems. The overall complexity of SDOH variables therefore presents complex system-level methodological and ethical challenges.
Higher quality and quantity of information increases accuracy of prediction, and ostensibly improves our knowledge of needs and promising care and prevention practices (Hassan et al., 2015; Rabovsky et al., 2017; Tan-McGrory et al., 2018; Vest et al., 2017). Yet, capturing medical information is not an objective process (Mykhalovskiy, 2001). As with all social data, findings only form a representation of social reality, the interpretation and representation of which forms its own material reality, constructed through social exchange of information and constrained by pre-existing social and cultural structures (Alvesson & Sköldberg, 2017; Schutz, 2012). Standardised data collection determines how individual patients are represented through health data and “live” in the health system.
Essentially, when considering EHRs and the collected data they hold, we can anticipate that implicit biases present at data entry serve to perpetuate the bias at reporting and end use stages (Leslie et al., 2021) and that HIS are responsible for measuring and disrupting health inequities from multiple perspectives. Although there is considerable perceived potential for automating SDOH data collection, health researchers and practitioners must recognise that long-term population health improvements through health analytics rely on the assumption that clarity of information will disrupt systematic reproduction of inequality. Siloed and/or uncritical development of technology in HIS can exacerbate existing systemic inequities through reproducing barriers to care and service access. Further understanding the effects and processes of stakeholder engagement in EHR/HIS development and decision-making may provide insight into the health equity potential of partnerships.
As local, global, and interconnected health systems prepare to develop AI for health purposes, a focus on just and equitable application of technology is a guiding principle (World Health Organization (WHO), 2021). Researchers have observed that automated decision algorithms have perpetuated marginalising biases in the public sector (Carter et al., 2019; Ntoutsi et al., 2020). Systemic and ideological political economic drivers in local contexts are the essence of SDOH. Critical equity perspectives may permit greater awareness for the role of actors within health institutions in creating or maintaining inequalities (Liebel, 2020). Researchers in the field should provide space for contemplating how processes for acquisition, management, and use of information can variously maintain or subvert value systems (Harding, 2006). For example, gender perspectives, which are crucial to the SDOH approach, can provide evidence of “institutional erasure” of non-gender conforming individuals in the health system (Bauer et al., 2009; Vermeir et al., 2018). At a population-level, we must also attend to the historical use of routine collection of demographic data (Legg, 2005) in structuring inequalities, especially racialised identities entangled in national mentalities (Anderson, 1991).
3. Conclusion
Health care surveillance and decision-making in health care provision can benefit from technological automation. However, there is a significant risk that advancement in this area could inadvertently exacerbate health existing disparities. Data collection in newly emerging digital spaces can offer opportunities to generate meaningful analyses of personal or community-level data, as well as moderately large quantities of data to support precision population health. Bringing SDOH perspectives into HIS R&D can facilitate an integrated schema of risk factor data for the context (i.e., the patient or population under surveillance), thereby providing opportunities to adequately address health equity by bringing attention to power dynamics inherent in cultural contexts of the HIS. As health systems incorporate AI technologies into HIS for risk factor surveillance, precision medicine, and population health equity, we will need to address systemic biases from many fronts. This should incorporate local, relational, critical, and trans-disciplinary forms of research.
3.1. Future research directions
Bringing together insights from existing frameworks, theories, and applied research, we propose three general guidelines to support equity-driven advances in automation and SDOH data collection:
Investing in and planning for interdisciplinary, intersectoral, and participatory knowledge information translation
Fostering interdisciplinary research, especially across social sciences, medicine, and computer science/engineering is an important aspect of future equity-oriented research. Interdisciplinary perspectives on health information systems may offer a realistic and sustainable balance of R&D goals (e.g., precision, comprehensiveness, equity, efficiency, security, user rights, etc.). The lived experiences of practitioners and patients, particularly patients considered to be “at-risk” for poor health based on SDOH, should also be values in all stages of R&D in HIS. This may better capture a broad range of perspectives and potential concerns in experiential participation in HIS (Brewer et al., 2020; Palacio et al., 2017). Continuing to evaluate and consult with providers and patients on promising tools and practices may lead to continually improving processes for capturing and applying SDOH information. In addition to promoting long-term goals of interoperability, this type of participatory and cross-sectoral research partnerships in HIS may help to address the digital divide through cognisance of frequently intersecting inequities in both access to health care and IT services. Overall, equity-driven methodological decisions for capturing SDOH data require critical engagement with power structures embedded in collection locations.
(2) Incorporating new SDOH data sources and novel collection methods with existing data sets through data linkage
Discovering novel data sources and building sustainable pathways to data from the SDOH perspective is also important for future research. This includes space to question boundaries around data currently held and maintained by information-holders, as exemplified by practitioners calling for access to data on population mental health trends currently held by social media conglomerates (e.g., Meta Platforms Inc. (Oxford Institute of Information, 2021)). There are also opportunities to collect SDOH data through technological devices and systems outside of traditional care settings. Possibilities include crowdsourcing data for public use or public access to data mined from social media programs or smartphone applications. Existing datasets from ministries of population statistics, economic and other environmental conditions may be available for use in academic and applied research. Researchers have been able to automate parts of these processes by using search algorithms to extract postal codes from patient EHRs to facilitate linkage to population data sets (Biro et al., 2016). Self-monitoring is also extremely relevant in producing health knowledge. Various personal devices and software applications could conceivably be points of access for SDOH information into HIS. Details on the social institutions in which patients and population members navigate are continuously collecting information. There are myriad sources of SDOH data, which can all contribute to robust patient and population health profiles. Building sustainable and equitable information gathering and sharing processes are crucial directions in HIS research.
(3) Channelling health system generated information into upstream evidence-informed health policy
A paramount concern with SDOH data collection is the capacity for health care providers, and health systems in general, to address the social inequalities that SDOH variables represent. Given the upstream nature of SDOH, to effectively reduce or eliminate the inequitable conditions that contribute to health disparities, policy interventions are a necessary complement to patient-focused interventions (Bambas, 2005; Bambra et al., 2005). More precise data and generally greater quality and quantity of information could lead to a greater capacity to measure determinants, effects, and mitigating factors in social inequality, especially with regard to macro-level interventions. Better SDOH data in the health care system could therefore potentially lead to policy interventions that are more comprehensive, amenable to evaluation, and likely to reduce social risk factors for morbidity and mortality at individual and population levels. Policies to ensure transparency in data collection, surveillance, and public benefit from AI and automation in the HIS are also integral features of population health. The balance of evidence-informed system-level changes, as well as individually focused health promotion strategies, are important goals for SDOH data collection methodologies in systems to which we aim to support equitable health promotion.
3.2. Closing remarks
Health systems are developing research methods and technologies for improving SDOH data collection, and maintaining information infrastructure and data repositories. Streamlining and enhancing SDOH information in health system dataflow may improve the efficiency of healthcare administration and systemic capacity to address health inequalities. Our research emphasises the need for collaborative, interdisciplinary, and intersectoral research partnerships when it comes to standardising and automating data collection methods. Maintaining an awareness of the holistic and interconnected nature of health and the political, economic, and cultural drivers of SDOH should be guiding principles in HIS design for advancing health equity.
Funding Statement
This work was supported by the Canadian Institute of Health Research(CIHR) grant 397824 Data collection initiative using artificially intelligent technology for social determinants and risk factors surveillance.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Adler, N. E., & Stead, W. W. (2015). Patients in context–EHR capture of social and behavioral determinants of health. The New England Journal of Medicine, 372(8), 698–701. 10.1056/NEJMp1413945 [DOI] [PubMed] [Google Scholar]
- Allan, B., & Smylie, J. (2015). First peoples, second class treatment: The role of racism in the health and well-being of Indigenous peoples in Canada. Wellesley Institute. [Google Scholar]
- Alvesson, M., & Sköldberg, K. (2017). Reflexive methodology: New vistas for qualitative research. SAGE Publications. [Google Scholar]
- Anderson, B. (1991). Imagined Communities. Verso. [Google Scholar]
- Armstrong, P., Armstrong, H., & Coburn, D. (2001). Unhealthy times: Political economy perspectives on health and care. Oxford University Press. [Google Scholar]
- Bambas, L. (2005). Integrating equity into health information systems: A human rights approach to health and information. PLoS Medicine, 2(4), e102. 10.1371/journal.pmed.0020102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambra, C., Fox, D., & Scott-Samuel, A. (2005). Towards a politics of health. Health Promotion International, 20(2), 187–193. 10.1093/heapro/dah608 [DOI] [PubMed] [Google Scholar]
- Barbosa, R. M., & Nelson, D. R. (2016). The use of support vector machine to analyze food security in a region of Brazil. Applied Artificial Intelligence, 30(4), 318–330. 10.1080/08839514.2016.1169048 [DOI] [Google Scholar]
- Bauer, G. R., Hammond, R., Travers, R., Kaay, M., Hohenadel, K. M., & Boyce, M. (2009). “I don’t think this is theoretical; This is our lives”: How erasure impacts health care for transgender people. Janac-Journal of the Association of Nurses in Aids Care, 20(5), 348–361. 10.1016/j.jana.2009.07.004 [DOI] [PubMed] [Google Scholar]
- Bauer, G. R., Mahendran, M., Braimoh, J., Alam, S., & Churchill, S. (2020). Identifying visible minorities or racialized persons on surveys: Can we just ask? Canadian Journal of Public Health= Revue Canadienne de Sante Publique 111(3). doi: 10.17269/s41997-020-00325-2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazemore, A. W., Cottrell, E. K., Gold, R., Hughes, L. S., Phillips, R. L., Angier, H., Burdick, T. E., Carrozza, M. A., & DeVoe, J. E. (2016). “Community vital signs”: Incorporating geocoded social determinants into electronic records to promote patient and population health. Journal of the American Medical Informatics Association, 23(2), 407–412. 10.1093/jamia/ocv088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. F., Klein, M. D., & Kahn, R. S. (2012). Identifying social risk via a clinical social history embedded in the electronic health record. Clinical Pediatrics (Phila), 51(10), 972–977. 10.1177/0009922812441663 [DOI] [PubMed] [Google Scholar]
- Biro, S., Williamson, T., Leggett, J. A., Barber, D., Morkem, R., Moore, K., Belanger, P., Mosley, B., & Janssen, I. (2016). Utility of linking primary care electronic medical records with Canadian census data to study the determinants of chronic disease: An example based on socioeconomic status and obesity. BMC Medical Informatics and Decision Making, 16(1), 1–8. 10.1186/s12911-016-0272-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen, N., Berrigan, D., Jackson, J. S., Wong, D. W. S., Wood, F. B., Denny, J. C., Zhang, X., & Bourne, P. E. (2019). Translational health disparities research in a data-rich world. Health Equity, 3(1), 588–600. 10.1089/heq.2019.0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer, L. C., Fortuna, K. L., Jones, C., Walker, R., Hayes, S. N., Patten, C. A., & Cooper, L. A. (2020). Back to the future: Achieving health equity through health informatics and digital health. JMIR mHealth and uHealth, 8(1), e14512. 10.2196/14512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne, A. J., Varcoe, C., Ford-Gilboe, M., Wathen, C. N., Smye, V., Jackson, B. E., Lavoie, J. G., Herbert, C. P., Lavoie, J. G., Wong, S. T., Blanchet Garneau, A., & Wallace, B. (2018). Disruption as opportunity: Impacts of an organizational health equity intervention in primary care clinics. International Journal for Equity in Health, 17(1), 1–16. 10.1186/s12939-018-0820-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant, T. (2009). Social inequalities, public policy, and health. Humanity & Society, 33(1–2), 118–144. 10.1177/016059760903300108 [DOI] [Google Scholar]
- Carter, S., Win, K., Wang, L., Rogers, W., Richards, B., & Houssami, N. (2019). 65 Ethical, legal and social implications of artificial intelligence systems for screening and diagnosis. Royal Society of Medicine. [Google Scholar]
- Chen, C., Weider, K., Konopka, K., & Danis, M. (2014). Incorporation of socioeconomic status indicators into policies for the meaningful use of electronic health records. Journal of Health Care for the Poor and Underserved, 25(1), 1–16. 10.1353/hpu.2014.0040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhabra, M., Sorrentino, A. E., Cusack, M., Dichter, M. E., Montgomery, A. E., & True, G. (2019). Screening for housing instability: Providers’ reflections on addressing a social determinant of health. Journal of General Internal Medicine, 34(7), 1213–1219. 10.1007/s11606-019-04895-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiolero, A., & Buckeridge, D. (2020, June). Glossary for public health surveillance in the age of data science. Journal of Epidemiology and Community Health, 74(7), 612–616. Epub 2020 Apr 24. PMID: 32332114; PMCID: PMC7337230 10.1136/jech-2018-211654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer, K. F., Grannis, S., Dixon, B. E., Bodenhamer, D. J., & Wiehe, S. E. (2011). Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Reports, 126(Suppl3_suppl), 54–61. 10.1177/00333549111260s310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway, M., Keyhani, S., Christensen, L., South, B. R., Vali, M., Walter, L. C., Chapman, W. W., Abdelrahman, S., & Chapman, W. W. (2019). Moonstone: A novel natural language processing system for inferring social risk from clinical narratives. Journal of Biomedical Semantics, 10(1), 6. 10.1186/s13326-019-0198-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw, K. W. (2017). On intersectionality: Essential writings. The New Press. [Google Scholar]
- Ehrenstein, V., Kharrazi, H., Lehmann, H., & Taylor, C. O.2019.Obtaining data from electronic health records. In Tools and technologies for registry interoperability, registries for evaluating patient outcomes: A user’s guide, 3rd edition, Addendum 2 [Internet]. Agency for Healthcare Research and Quality (US). [PubMed] [Google Scholar]
- Feller, D. J., Zucker, J., Yin, M. T., Gordon, P., & Elhadad, N. (2018). Using clinical notes and natural language processing for automated HIV risk assessment. Journal of Acquired Immune Deficiency Syndromes, 77(2), 160. 10.1097/QAI.0000000000001580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giuse, N. B., Koonce, T. Y., Kusnoor, S. V., Prather, A. A., Gottlieb, L. M., Huang, L. C., Phillips, S. E., Shyr, Y., Adler, N. E., & Stead, W. W. (2017). Institute of medicine measures of social and behavioral determinants of health: A feasibility study. American Journal of Preventive Medicine, 52(2), 199–206. 10.1016/j.amepre.2016.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, R., Bunce, A., Cowburn, S., Dambrun, K., Dearing, M., Middendorf, M., Cottrell, E., Hollombe, C., Mahr, P., Melgar, G., Davis, J., Gottlieb, L., & Cottrell, E. (2018). Adoption of social determinants of health EHR tools by community health centers. The Annals of Family Medicine, 16(5), 399–407. 10.1370/afm.2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold, R., Cottrell, E., Bunce, A., Middendorf, M., Hollombe, C., Cowburn, S., Melgar, G., & Melgar, G. (2017). Developing Electronic Health Record (EHR) strategies related to health center patients’ social determinants of health. The Journal of the American Board of Family Medicine, 30(4), 428–447. 10.3122/jabfm.2017.04.170046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb, L. M., Tirozzi, K. J., Manchanda, R., Burns, A. R., & Sandel, M. T. (2015). Moving electronic medical records upstream: Incorporating social determinants of health. American Journal of Preventive Medicine, 48(2), 215–218. 10.1016/j.amepre.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Hall, S. (2009). Encoding/decoding. In Durham M. G. & Kellner D. M. (Eds.), Media and cultural studies: Keyworks (pp. 163–173). Wiley. [Google Scholar]
- Hankivsky, O., & Christoffersen, A. (2008). Intersectionality and the determinants of health: A Canadian perspective. Critical Public Health, 18(3), 271–283. 10.1080/09581590802294296 [DOI] [Google Scholar]
- Harding, S. G. (2006). Science and social inequality: Feminist and postcolonial issues. University of Illinois Press. [Google Scholar]
- Hassan, A., Scherer, E. A., Pikcilingis, A., Krull, E., McNickles, L., Marmon, G., Fleegler, E. W., & Fleegler, E. W. (2015). Improving social determinants of health: Effectiveness of a web-based intervention. American Journal of Preventive Medicine, 49(6), 822–831. 10.1016/j.amepre.2015.04.023 [DOI] [PubMed] [Google Scholar]
- Hatef, E., Weiner, J. P., & Kharrazi, H. (2019). A public health perspective on using electronic health records to address social determinants of health: The potential for a national system of local community health records in the United States. International Journal of Medical Informatics, 124, 86–89. 10.1016/j.ijmedinf.2019.01.012 [DOI] [PubMed] [Google Scholar]
- Hewner, S., Casucci, S., Sullivan, S., Mistretta, F., Xue, Y., Johnson, B., Fox, C., Lin, L., & Fox, C. (2017). Integrating social determinants of health into primary care clinical and informational workflow during care transitions. EGEMS (Wash DC), 5(2), 2. 10.13063/2327-9214.1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hripcsak, G., Forrest, C. B., Brennan, P. F., & Stead, W. W. (2015). Informatics to support the IOM social and behavioral domains and measures. Journal of the American Medical Informatics Association, 22(4), 921–924. 10.1093/jamia/ocv035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter, R. F., Davis, M., Tully, M. A., Valente, T. W., Kee, F., & Kee, F. (2015). “Hidden” social networks in behavior change interventions. American Journal of Public Health, 105(105), 513–516. 10.2105/AJPH.2014.302399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain, A., van Hoek, A. J., Walker, J. L., Mathur, R., Smeeth, L., & Thomas, S. L. (2017). Identifying social factors amongst older individuals in linked electronic health records: An assessment in a population based study. PLoS ONE, 12(11), e0189038. 10.1371/journal.pone.0189038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamei, M., Nisnevich, A., Wetchler, E., Sudat, S., & Liu, E. (2017). Predicting all-cause risk of 30-day hospital readmission using artificial neural networks. PLoS ONE, 12(7), e0181173. 10.1371/journal.pone.0181173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasthurirathne, S. N., Grannis, S., Halverson, P. K., Morea, J., Menachemi, N., & Vest, J. R. (2020). Precision health-enabled machine learning to identify need for wraparound social services using patient- and population-level data sets: Algorithm development and validation. JMIR Medical Informatics, 8(7), e16129–e16129. 10.2196/16129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi, I., Subramanian, S. V., & Almeida-Filho, N. (2002). A glossary for health inequalities. Journal of Epidemiology & Community Health, 56(9), 647–652. 10.1136/jech.56.9.647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kino, S., Hsu, Y. T., Shiba, K., Chien, Y. S., Mita, C., Kawachi, I., & Daoud, A. (2021). A scoping review on the use of machine learning in research on social determinants of health: Trends and research prospects. SSM-Population Health, 15, 100836. 10.1016/j.ssmph.2021.100836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumpal, I. (2013). Determinants of social desirability bias in sensitive surveys: A literature review. Quality & Quantity, 47(4), 2025–2047. 10.1007/s11135-011-9640-9 [DOI] [Google Scholar]
- Kwon, I. G., Kim, S. H., & Martin, D. (2021). Integrating social determinants of health to precision medicine through digital transformation: An exploratory roadmap. International Journal of Environmental Research and Public Health, 18(9), 5018. 10.3390/ijerph18095018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Legg, S. (2005). Foucault’s population geographies: Classifications, biopolitics and governmental spaces. Population, Space and Place, 11(3), 137–156. 10.1002/psp.357 [DOI] [Google Scholar]
- Leslie, D., Mazumder, A., Peppin, A., Wolters, M. K., & Hagerty, A. (2021). Does “AI” stand for augmenting inequality in the era of covid-19 healthcare? BMJ (Online), 372, n304–n304. 10.1136/bmj.n304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, J. H., Whelihan, K., Navarro, I., & Boyle, K. R. (2016). Community health center provider ability to identify, treat and account for the social determinants of health: A card study. BMC Family Practice, 17(1), 121. 10.1186/s12875-016-0526-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebel, A. M. (2020). Applying critical theory to disrupt deficit perspectives in patient communication and health literacy: “10 Minutes to better patient communication” podcast series. Journal of Consumer Health on the Internet, 24(4), 416–429. 10.1080/15398285.2020.1831354 [DOI] [Google Scholar]
- Lindemann, E. A., Chen, E. S., Wang, Y., Skube, S. J., & Melton, G. B. (2017). Representation of social history factors across age groups: A topic analysis of free-text social documentation. AMIA Annual Symposium Proceedings, 2017, 1169–1178. [PMC free article] [PubMed] [Google Scholar]
- Lofters, A. K., Schuler, A., Slater, M., Baxter, N. N., Persaud, N., Pinto, A. D., & Kiran, T. (2017). Using self-reported data on the social determinants of health in primary care to identify cancer screening disparities: Opportunities and challenges. BMC Family Practice, 18(1), 31. 10.1186/s12875-017-0599-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucyk, K. (2018). “It’s a tradition of naming injustice”: An oral history of the social determinants of health–Canadian reflections, 1960s-present. SSM-Population Health, 6, 178–183. 10.1016/j.ssmph.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucyk, K., & McLaren, L. (2017). Taking stock of the social determinants of health: A scoping review. PLoS ONE, 12(5), e0177306. 10.1371/journal.pone.0177306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot, M., Friel, S., Bell, R., Houweling, T. A., Taylor, S., & Health, C. o. S. D. o . (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet, 372(9650), 1661–1669. 10.1016/S0140-6736(08)61690-6 [DOI] [PubMed] [Google Scholar]
- Monsen, K. A., Brandt, J. K., Brueshoff, B. L., Chi, C. L., Mathiason, M. A., Swenson, S. M., & Thorson, D. R. (2017). Social determinants and health disparities associated with outcomes of women of childbearing age who receive public health nurse home visiting services. Journal of Obstetric, Gynecologic & Neonatal Nursing, 46(2), 292–303. 10.1016/j.jogn.2016.10.004 [DOI] [PubMed] [Google Scholar]
- Monsen, K. A., Kapinos, N., Rudenick, J. M., Warmbold, K., McMahon, S. K., & Schorr, E. N. (2016). Social determinants documentation in electronic health records with and without standardized terminologies. Western Journal of Nursing Research, 38(10), 1399–1400. 10.1177/0193945916658208 [DOI] [PubMed] [Google Scholar]
- Mooney, S., & Pejaver, V. (2018). Big data in public health: Terminology, machine learning, and privacy. Annual Review of Public Health, 39(1), 95–112. 10.1146/annurev-publhealth-040617-014208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mykhalovskiy, E. (2001). Towards a sociology of knowledge in health care: Exploring health services research as active discourse. In Armstrong H., Armstrong P., & Coburn D. (Eds.), Unhealthy times: Political economy perspectives on health and care in Canada. Oxford University Press Canada. pp. 146–165. [Google Scholar]
- Navathe, A. S., Zhong, F., Lei, V. J., Chang, F. Y., Sordo, M., Topaz, M., Zhou, L., Rocha, R. A., & Zhou, L. (2018). Hospital readmission and social risk factors identified from physician notes. Health Services Research, 53(2), 1110–1136. 10.1111/1475-6773.12670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ntoutsi, E., Fafalios, P., Gadiraju, U., Iosifidis, V., Nejdl, W., Vidal, M. E., & Krasanakis, E. (2020). Bias in data‐driven artificial intelligence systems—An introductory survey. Wiley Interdisciplinary Reviews: Data Mining and Knowledge Discovery, 10(3), e1356. [Google Scholar]
- Oreskovic, N. M., Maniates, J., Weilburg, J., & Choy, G. (2017). Optimizing the use of electronic health records to identify high-risk psychosocial determinants of health. JMIR Medical Informatics, 5(3), e25. 10.2196/medinform.8240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford Institute of Information . (2021). An open letter to Mr. Mark Zuckerberg: A global call to act now on child and adolescent mental health science. https://www.oii.ox.ac.uk/an-open-letter-to-mark-zuckerberg/#continue
- Palacio, A., Suarez, M., Tamariz, L., & Seo, D. (2017). A road map to integrate social determinants of health into electronic health records. Population Health Management, 20(6), 424–426. 10.1089/pop.2017.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto, A. D., Bondy, M., Rucchetto, A., Ihnat, J., & Kaufman, A. (2019). Screening for poverty and intervening in a primary care setting: An acceptability and feasibility study. Family Practice 36(5), 634–638. 10.1093/fampra/cmy129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto, A. D., Glattstein-Young, G., Mohamed, A., Bloch, G., Leung, F. H., & Glazier, R. H. (2016). Building a foundation to reduce health inequities: Routine collection of sociodemographic data in primary care. Journal of the American Board of Family Medicine, 29(3), 348–355. 10.3122/jabfm.2016.03.150280 [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada . (2016). Social determinants of health. https://cbpp-pcpe.phac-aspc.gc.ca/public-health-topics/social-determinants-of-health
- Rabovsky, A. J., Rothberg, M. B., Rose, S. L., Brateanu, A., Kou, L., & Misra-Hebert, A. D. (2017). Content and outcomes of social work consultation for patients with diabetes in primary care. Journal of the American Board of Family Medicine, 30(1), 35–43. 10.3122/jabfm.2017.01.160177 [DOI] [PubMed] [Google Scholar]
- Raphael, D., & Bryant, T. (2015). Power, intersectionality and the life-course: Identifying the political and economic structures of welfare states that support or threaten health. Social Theory & Health, 13(3–4), 245–266. 10.1057/sth.2015.18 [DOI] [Google Scholar]
- Raphael, D., Bryant, T., Mikkonen, J., & Raphael, A. 2020. Social determinants of health: The Canadian facts (2nd ed.). Ontario Tech University Faculty of Health Sciences, York University School of Health Policy and Management. [Google Scholar]
- Roth, C., Foraker, R. E., Payne, P. R., & Embi, P. J. (2014). Community-level determinants of obesity: Harnessing the power of electronic health records for retrospective data analysis. BMC Medical Informatics and Decision Making, 14(1), 36. 10.1186/1472-6947-14-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schutz, A. (2012). Collected papers I. The problem of social reality (Vol. 11). Springer Science & Business Media. [Google Scholar]
- Shahmoradi, L., Safadari, R., & Jimma, W. (2017). Knowledge management implementation and the tools utilized in healthcare for evidence-based decision making: A systematic review. Ethiopian Journal of Health Sciences, 27(5), 541–558. 10.4314/ejhs.v27i5.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stemerman, R. A. (2020). Machine learning approaches to identifying social determinants of health in electronic health record clinical notes. [Dissertation/Thesis] ProQuest Dissertations Publishing. https://go.exlibris.link/B7113LXk [Google Scholar]
- Syed, I. U. (2021). Feminist political economy of health: Current perspectives and future directions. Healthcare, 9(2), 233. 10.3390/healthcare9020233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan-McGrory, A., Bennett-AbuAyyash, C., Gee, S., Dabney, K., Cowden, J. D., Williams, L., Lopez, L., Nettles, A., Pagura, S., Holmes, L., Goleman, J., Caldwell, L., Page, J., Oceanic, P., McMullen, E. J., Lopera, A., Beiter, S., & López, L. (2018). A patient and family data domain collection framework for identifying disparities in pediatrics: Results from the pediatric health equity collaborative. BMC Pediatrics, 18(1), 18. 10.1186/s12887-018-0993-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng, A., & Wilcox, A. (2022). Simplified data science approach to extract social and behavioural determinants: A retrospective chart review. BMJ Open, 12(1), e048397. 10.1136/bmjopen-2020-048397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thapa, B., Torres, I., Koya, S. F., Robbins, G., Abdalla, S. M., Arah, O. A., Larson, H. J., Zhang, L., Asma, S., Morales, J. V., Galea, S., Rhee, K., & Larson, H. J. (2021). Use of data to understand the social determinants of depression in two middle‐income countries: The 3‐D commission. Journal of Urban Health, 98(Suppl S1), 41–50. 10.1007/s11524-021-00559-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theiss, J., & Regenstein, M. (2017). Facing the need: Screening practices for the social determinants of health. The Journal of Law, Medicine & Ethics, 45(3), 431–441. 10.1177/1073110517737543 [DOI] [Google Scholar]
- Vermeir, E., Jackson, L. A., & Marshall, E. G. (2018). Barriers to primary and emergency healthcare for trans adults. Culture, Health & Sexuality, 20(2), 232–246. 10.1080/13691058.2017.1338757 [DOI] [PubMed] [Google Scholar]
- Vest, J. R., Grannis, S. J., Haut, D. P., Halverson, P. K., & Menachemi, N. (2017). Using structured and unstructured data to identify patients’ need for services that address the social determinants of health. International Journal of Medical Informatics, 107, 101–106. 10.1016/j.ijmedinf.2017.09.008 [DOI] [PubMed] [Google Scholar]
- Winden, T. J., Chen, E. S., Monsen, K. A., Wang, Y., & Melton, G. B. (2018). Evaluation of flowsheet documentation in the electronic health record for residence, living situation, and living conditions. AMIA Summits on Translational Science Proceedings, 2017, 236–245. [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2021). Ethics and governance of artificial intelligence for health: WHO guidance.
- Ye, C., Fu, T., Hao, S., Zhang, Y., Wang, O., Jin, B., & Ling, X. (2018). Prediction of incident hypertension within the next year: Prospective study using statewide electronic health records and machine learning. Journal of Medical Internet Research, 20(1), e22. 10.2196/jmir.9268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, X., Perez-Stable, E. J., Bourne, P. E., Peprah, E., Duru, O. K., Breen, N., Denny, J., Wood, F., Jackson, J. S., Wong, D. W. S., & Denny, J. (2017). Big data science: Opportunities and challenges to address minority health and health disparities in the 21st century. Ethnicity & Disease, 27(2), 95–106. 10.18865/ed.27.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zulman, D. M., Shah, N. H., & Verghese, A. (2016). Evolutionary pressures on the electronic health record: Caring for complexity. JAMA, 316(9), 923–924. 10.1001/jama.2016.9538 [DOI] [PubMed] [Google Scholar]


