Abstract
Study Design
Retrospective Cohort Study
Objectives
To investigate and compare the prevalence of low bone mineral density (BMD) and abnormal laboratory bone metabolism parameters in patients undergoing elective primary discectomy, decompression, and fusion and to outline possible differences in these parameters between patients undergoing revision for skeletal vs non-skeletal complications.
Methods
We retrospectively evaluated BMD measurements by dual-energy x-ray absorptiometry (DXA) in 389 consecutive patients scheduled for elective lumbar spine surgery. Next to demographic characteristics, laboratory bone metabolism parameters were assessed. Group comparisons were performed between primary discectomy, decompression, and fusion. In patients scheduled for revision surgery after fusion, potential differences in the skeletal status between those with skeletal vs non-skeletal complications were analyzed.
Results
Osteoporosis by T-score was detected in 6.7%, 11.0% and 14.7% of the patients undergoing discectomy, decompression and fusion, respectively. While vitamin D deficiency (67.6%) and hyperparathyroidism (16.4%) were frequently detected, no differences in laboratory bone metabolism markers could be found between the groups. Female sex (P<.001), higher age (P=.01) and lower BMI (P<.001) were associated with lower BMD. In the cohort of patients undergoing revision surgery due to complications after fusion, those with skeletal complications did not differ in BMD or bone metabolism from those with non-skeletal complications.
Conclusions
Osteoporosis represents a relevant comorbidity in patients scheduled for elective spine surgery, which is why DXA should be routinely performed in these patients. However, DXA may provide limited information in identifying patients at increased risk for skeletal complications after fusion.
Keywords: dual-energy x-ray absorptiometry, spine surgery, revision, osteoporosis, vitamin D
Introduction
Surgical interventions for disorders of the lumbar spine are generally effective in terms of pain relief and restoration of function in affected patients. Specifically, while lumbar disc herniation can often be treated conservatively, a surgical approach in the form of a discectomy is indicated in patients with insufficient improvement in symptoms or neurologic deficits 1 . In older patients with degenerative lumbar spine conditions (including spinal stenosis and degenerative spondylolisthesis), a surgical procedure offers an effective treatment option in terms of improved functional outcome and pain reduction 2 . Both decompression and fusion are possible surgical methods, depending on the stage of the disease as well as other factors. Nevertheless, these procedures also have a relevant complication rate. Complications after fusion can be divided into skeletal (eg, rod breakage, screw loosening, pseudarthrosis, or adjacent segment fracture) and non-skeletal (eg, infection, degeneration and/or spinal stenosis in an adjacent segment) complications 3 .
Osteoporosis, defined as impaired bone quality accompanied by an increased risk of fragility fractures, is a very common condition worldwide. Fragility fractures affect 1 in 2 women and 1 in 5 men over the age 50 years 4 . While the negative effect of low bone mineral density (BMD) on the risk of vertebral fractures is well-studied, its influence on the outcome of lumbar spine surgery is insufficient. It has been shown that low BMD (ie, osteoporosis) represents a common comorbidity in patients scheduled for elective spine surgery 5 . Especially in fusion surgery involving the insertion of screws into the bone, a negative influence of a poor skeletal status on the outcome appears crucial. In this regard, local poor bone status has been associated with complications such as screw loosening 6 . Although generally recommended 7 , BMD assessment prior to elective spine surgery is often not performed on a routine basis.
The frequency of osteoporosis in patients undergoing spine surgery ranges from 9.6 % to 42.3 %8-12, with heterogenous findings primarily attributable to risk profiles, sex and geographic factors. Nonetheless, it remains unclear whether differences in the frequency of low bone density as well as abnormalities in laboratory bone metabolism occur between different spinal conditions and surgical treatments. Although low BMD could be a possible factor increasing the risk of skeletal complications after fusion, evidence is insufficient. In this study, we aimed to compare BMD measured by dual-energy X-ray absorptiometry (DXA) in a consecutive series of 389 patients undergoing different types of elective, primary or revision surgical procedures of the lumbar spine. We also compared patients scheduled for revision due to skeletal vs non-skeletal complications.
Methods
Study Cohort
We retrospectively analyzed 389 consecutive patients who underwent lumbar spine surgery in our department from 2015 and 2021. The cohort consisted of n=250 patients undergoing primary surgery including discectomy (n=30), decompression (n=145) and fusion (n=75). The indication for discectomy was disc herniation, whereas the indication for decompression and fusion was lumbar spinal stenosis and/or degenerative spondylolisthesis in all cases. We also included n=139 patients indicated for revision surgery, of which n=70 previously underwent decompression and n=69 patients previously underwent fusion. Form the patients with revision surgery after fusion, n=31 had skeletal complications and n=39 patients had non-skeletal complications. Skeletal complications were defined as rod breakage, screw loosening, pseudarthrosis, or adjacent segment fracture as previously defined 3 . Non-skeletal complications were defined as degeneration and/or spinal stenosis in an adjacent segment.
Patients with active cancer, skeletal metastases or inoperability due to severe medical conditions were excluded from the study. Demographic parameters (age, sex, BMI) and relevant clinical risk factors for osteoporosis and increased fracture risk (oral glucocorticoid intake for longer than 3 months in the past or at present, smoking) were obtained in all patients. Only patients with available BMD measurement within 4 weeks before surgery were included.
Dual-Energy X-Ray Absorptiometry and Laboratory Assessment
We assessed the bone mineral density (BMD) at the left and right proximal femur as well as the lumbar spine (L1-L4) by DXA (Lunar Prodigy enCore 2007, GE Healthcare; Madison, WI, USA). T-scores expressing BMD standard deviations for young, sex-matched healthy adults were generated using the manufacturer's software. Based on the T-score, osteoporosis and osteopenia were diagnosed according to World Health Organization (WHO) guidelines (ie, normal T-score >-1.0, osteopenia T-score >-2.5≤-1.0, osteoporosis T-score ≤-2.5) 13 . The lowest T-score of each of the evaluations (with corresponding absolute BMD and Z-score) was used for further analysis. In the cases before revision, the DXA values of the lumbar spine were only evaluated if at least 2 vertebral bodies were measurable (ie, no instrumentation in this scan area). This way, only 10/31 (32.3%) and 14/38 (36.8%) of the lumbar spine measurements in patients with non-skeletal and skeletal complications, respectively, could be considered.
Furthermore, serum biochemical bone metabolism markers including calcium, 25-hydroxyvitamin D, parathyroid hormone (PTH), phosphate, and alkaline phosphatase (ALP) were assessed. Creatinine, c-reactive protein (CRP), leukocyte count and hemoglobin levels were also measured.
Statistical Analysis
GraphPad Prism® (version 9.0, GraphPad Software, La Jolla, CA) was used for statistical analysis. Continuous variables are given as median with confidence interval (CI) and categorical variables are expressed as number and percentage. The Shapiro–Wilk test was used to evaluate the normal distribution of the data. To compare 2 groups, student’s t-test was used for normally distributed data and the Mann-Whitney-U test for non-parametric data. For categorical data, the Chi-Squared test was used. For comparison of normally distributed data among 3 groups, one-way ANOVA and with Tukey’s multiple comparison test was applied, and for non-parametric data, the Kruskal–Wallis test with Dunn’s multiple comparison test was performed. Age- and weight-associated changes in T-scores were analyzed by linear regression analysis. The P-value, coefficient of determination R2 and 95% confidence interval (CI) of the respective regression slopes were determined. Statistical significance was set to a P-value of .05.
Results
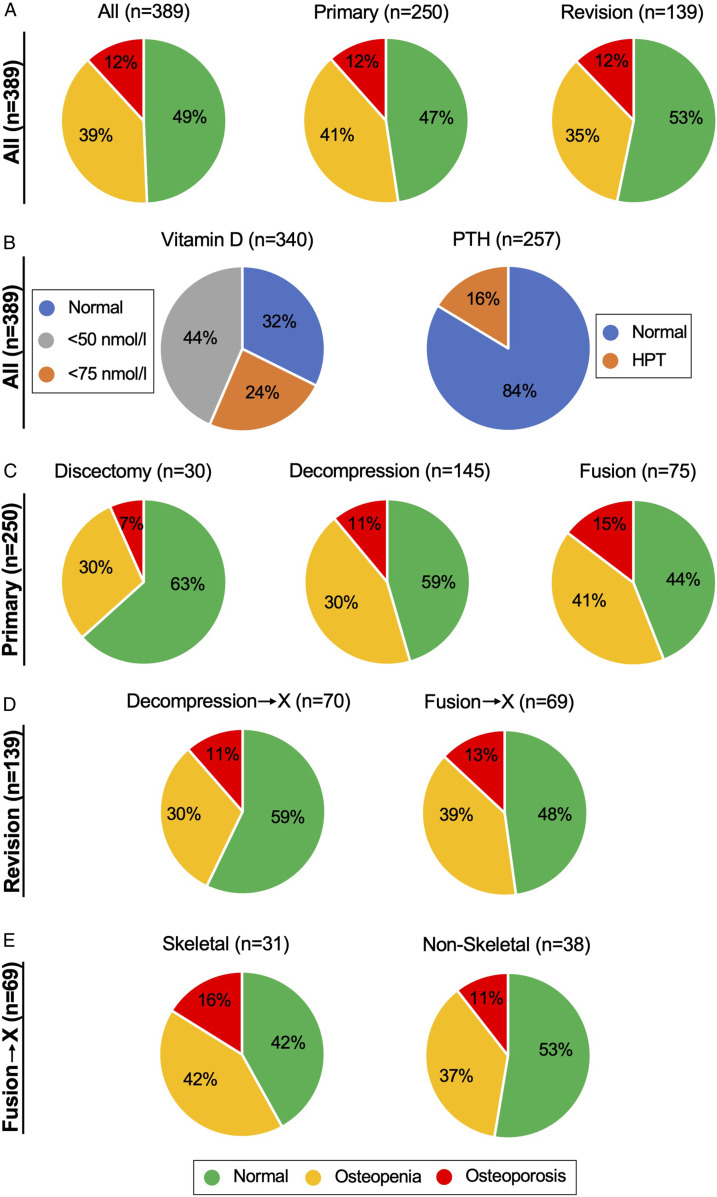
In the total cohort of 389 patients (224 women and 165 men), the proportion of osteoporosis was 11.8% and that of osteopenia 38.8% (women: osteoporosis 13.4%, osteopenia 39.3% and men: osteoporosis 9.7%, osteopenia 38.8%), with no differences found between patients with primary and secondary (ie, revision) lumbar spine surgery (Figure 1A). There was also a high proportion of vitamin D deficiency with a total of 67.6% vitamin D deficient patients (Figure 1B). Based on laboratory results, vitamin supplementation was initiated or adjusted in all patients. A relevant proportion of patients (16.4%) had hyperparathyroidism, of which 3 patients had primary hyperparathyroidism and the remaining patients had secondary hyperparathyroidism. The indication for specific osteoporosis treatment was made according to the osteoporosis guidelines of the Dachverband Osteologie (DVO) 14 . Of the 46 affected patients in the total cohort (30 women, 16 men), respective treatment was initiated in 41 patients. In addition, treatment was indicated in 4 elderly women with osteopenia. The type of the specific osteoporosis therapy was determined based on the risk profile and consisted of either bisphosphonates, denosumab, or teriparatide.
Figure 1.
Pie charts showing the distribution of BMD based on DXA T-scores as well as vitamin D and PTH levels. (A) Among all patients indicated for lumbar spine surgery (n=389), 12% had osteoporosis. No differences between patients undergoing primary or revision surgery were found. (B) Frequency of vitamin D deficiency and hyperparathyroidism. (C) In patients undergoing primary surgery, a trend toward increasing osteoporosis incidence was noted between patients undergoing discectomy, decompression, and fusion. (D) Patients who underwent revision surgery for complications after fusion were diagnosed with osteoporosis or osteopenia slightly more frequently than patients who underwent revision after decompression. (E) Among the patients being revised after fusion, those with skeletal complications tended to have higher rates of osteoporosis and osteopenia compared to those with non-skeletal complications.
Within the group of patients undergoing primary surgery, the proportion of osteoporosis increased between discectomy, decompression, and fusion (Figure 1C). Within the patient cohort scheduled for revision surgery, there were 70 patients with complications after decompression and 69 with complications after fusion, with similar distributions of BMD categories found (Figure 1D). Within the patients who underwent surgery for complications after fusion, there appeared to be a higher frequency of osteoporosis for patients with skeletal compared with non-skeletal complications (Figure 1E).
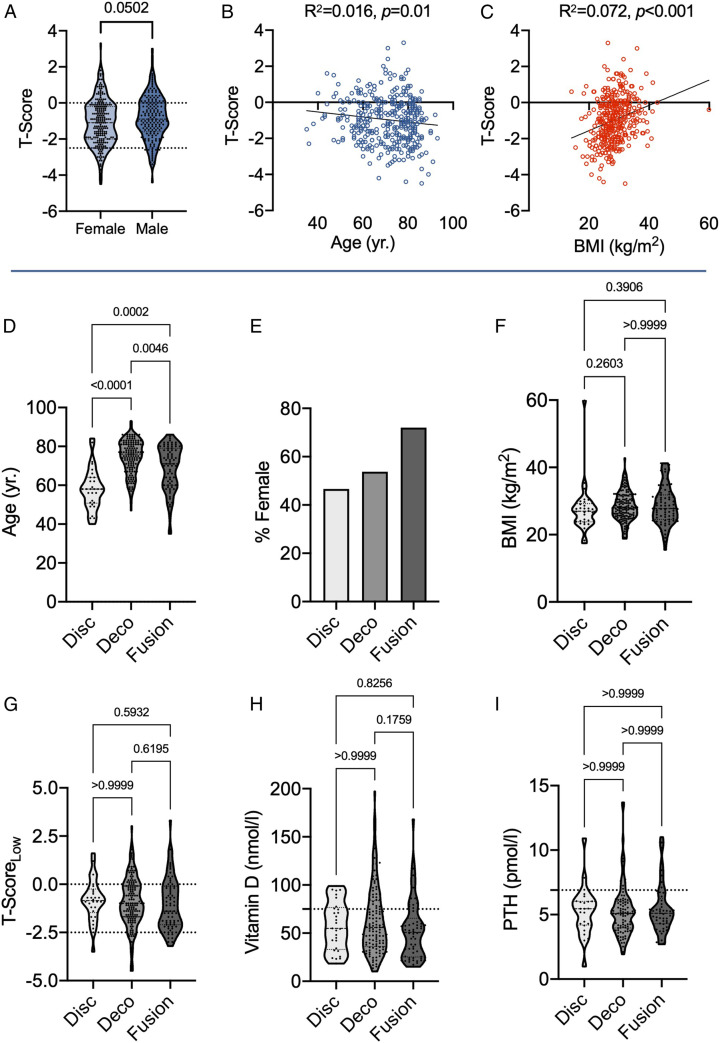
For the total cohort (n=389), we also analyzed the main factors influencing BMD. While BMD was significantly lower in women compared to men (P<.001), no significant differences in T-scores between women and men were detected, indicating that sex is not an additional risk factor compared to the reference cohort (Figure 2A). Age and BMI yielded significant but weak associations with T-score (Figure 2B and C). We next compared BMD and laboratory findings of the different types of primary surgeries (n=250) in more detail. Demographic and disease specific characteristics are presented in Table 1. While the patients undergoing discectomy were significantly younger than those scheduled for decompression and fusion, the patients before fusion were also younger than those scheduled for decompression (Figure 2D). Within the patients undergoing fusion, the proportion of females was highest (Figure 2E), with no differences in BMI between the groups (Figure 2F). We detected significant differences regarding the spinal BMD and T-score between the groups, which was attributed to a lower BMD and T-Score in patients scheduled for fusion compared to those scheduled for decompression (P<.05). However, no differences were found in any of the other BMD parameters and skeletal regions between the 3 groups discectomy, decompression, and fusion, including the lowest T-score of all regions measured (Figure 2G, Table 2). Likewise, there was no difference in any of the laboratory bone metabolism parameters, including vitamin D and PTH (Figure 2H and I, Table 2). The only difference in laboratory parameters between groups was found in CRP, and this difference was due to slightly higher values in the fusion compared to the decompression group (P<.05) (Table 2). Importantly, we detected a high rate between 70.0% and 77.3% of vitamin D deficiency and between 12.5% and 16.3% hyperparathyroidism, without differences between groups. Osteoporosis was previously undiagnosed in most patients, representing a relevant underdiagnosis (Table 2).
Figure 2.
Assessment of factors influencing T-score in the entire cohort (n=389) and comparison of demographic and bone parameters between types of primary lumbar spine surgery (n=250). (A) Comparison of BMD T-scores between females and males (whole cohort). (B) Associations between age and T-score. (C) Associations between BMI and T-score. (D) Comparison of age, (E) sex distribution, and (F) BMI between discectomy (Disc), decompression (Deco) and fusion. (G) Comparison of DXA-T scores (lowest value of the measuring sites), (H) vitamin D, and (I) PTH levels. The dashed lines of the truncated violin plots represent the median and quartiles. P-values are given above the diagrams.
Table 1.
Demographic data, medical history and skeletal risk factors in the patients undergoing primary different types of primary spine surgery.
| Parameter | Discectomy (n=30) | Decompression (n=145) | Fusion (n=75) | P-value |
|---|---|---|---|---|
| Age (yr.) | 58.0 (52.0 to 62.0) | 76.0 (74.0 to 77.0) | 71.0 (66.0 to 75.0) | < .001 |
| Sex f/m (n) | 14/16 | 88/57 | 54/21 | .043 |
| BMI (kg/m2) | 27.0 (24.2 to 27.9) | 28.0 (27.3 to 28.7) | 27.8 (26.3 to 29.7) | .22 |
| Prednisolone ≤7.5 mg (n, %) | 1 (3.3%) | 8 (5.5%) | 8 (10.7%) | .26 |
| Smoking (n, %) | 1 (3.3%) | 10 (6.9%) | 6 (8.0%) | .69 |
Results are presented as median with 95% confidence intervals or n (%). Bold indicates significant differences (P < .05).
Table 2.
DXA and laboratory results in the patients undergoing primary spine surgery.
| Parameter | Discectomy (n=30) | Decompression (n=145) | Fusion (n=75) | P-value |
|---|---|---|---|---|
| DXA | ||||
| BMD left hip (g/cm2) | 1.03 (.93 to 1.10) | .95 (.91 to .97) | .99 (.92 to 1.02) | .21 |
| T-score left hip | -.4 (-.9 to .3) | -.8 (-1.0 to -.5) | -.5 (-1.1 to .0) | .38 |
| BMD right hip (g/cm2) | 1.01 (.91 to 1.06) | .95 (.90 to .99) | .92 (.88 to 1.00) | .22 |
| T-score right hip | -.3 (-.9 to .1) | -.8 (-1.0 to -.3) | -.8 (-1.2 to -.3) | .42 |
| BMD lumbar spine (g/cm2) | 1.16 (1.09 to 1.24) | 1.19 (1.15 to 1.25) | 1.08 (1.03 to 1.18) | .03 |
| T-score lumbar spine | -.3 (-.7 to .6) | .1 (-.4 to .5) | -.7 (-1.3 to .0) | .04 |
| T-score lowest | -.9 (-1.2 to -.5) | -1.0 (-1.2 to -.7) | -1.4 (-1.9 to -.7) | .32 |
| Osteopenia (%) | 9 (30.0%) | 63 (43.4%) | 31 (41.3%) | .40 |
| Osteoporosis (%) | 2 (6.7%) | 16 (11.0%) | 11 (14.7%) | .49 |
| - Diagnosed before? | 0/2 (.0%) | 4/16 (25.0%) | 4/11 (36.4%) | |
| - Women | 2/16 (12.5%) | 10/88 (11.4%) | 9/54 (16.7%) | |
| - Men | 0/14 (.0%) | 6/57 (10.5%) | 2/21 (9.5%) | |
| Laboratory | ||||
| Calcium (mmol/l) | 2.35 (2.30 to 2.40) | 2.35 (2.32 to 2.37) | 2.32 (2.30 to 2.34) | .18 |
| 25-OH-D3 (nmol/l) | 54.9 (42.2 to 74.5) | 55.9 (47.4 to 65.1) | 50.8 (35.9 to 57.6) | .16 |
| - Vitamin D deficiency (n, %) | 21/30 (70.0%) | 92/129 (71.3%) a | 51/66 (77.3) a | .63 |
| PTH (pmol/l) | 5.46 (4.30 to 6.03) | 5.10 (4.44 to 5.30) | 5.11 (4.70 to 5.38) | .69 |
| - HPT (n, %) | 3/24 (12.5%) a | 14/98 (14.3%) a | 8/49 (16.3%) a | .90 |
| Phosphate (pmol/l) | 3.00 (2.80 to 3.20) | 3.00 (2.90 to 3.10) | 3.10 (2.80 to 3.20) | .98 |
| ALP (U/l) | 77.0 (69.0 to 85.0) | 73.5 (70.0 to 77.0) | 72.0 (65.0 to 77.0) | .19 |
| Creatinine (mg/dl) | .89 (.81 to .97) | .89 (.84 to .94) | .86 (.80 to .92) | .65 |
| CRP (mg/dl) | .24 (.00 to .40) | .10 (.10 to .20) | .20 (.10 to .60) | .03 |
| Leukocytes (G/l) | 8.15 (6.90 to 9.50) | 7.00 (6.60 to 7.50) | 7.10 (6.40 to 8.00) | .22 |
| Hemoglobin (g/dl) | 13.4 (13.0 to 13.9) | 14.0 (13.6 to 14.2) | 13.7 (13.5 to 14.2) | .66 |
Results are presented as median with 95% confidence intervals or n (%). Bold indicates significant differences (P < .05).
aindicates deviating number of measured patients for the individual parameter. HPT: hyperparathyroidism.
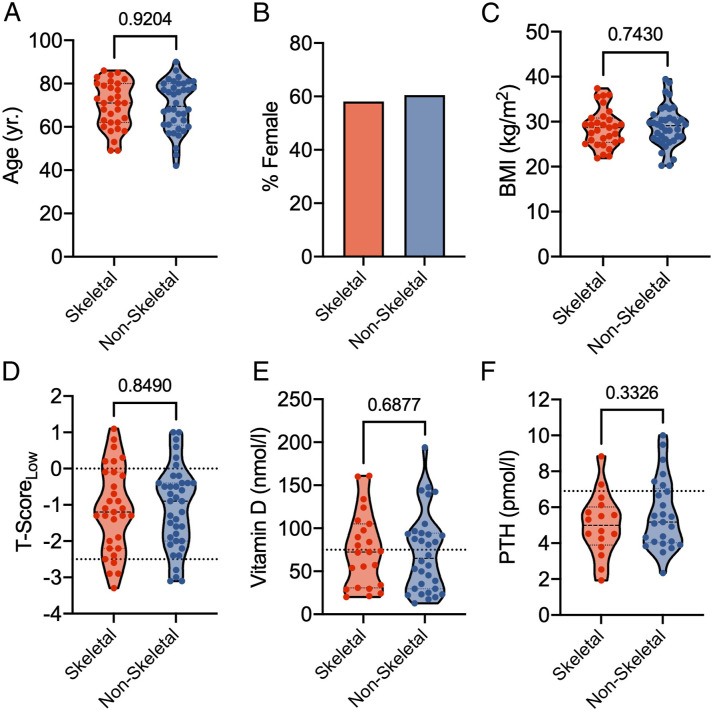
To test the hypothesis that low BMD is a risk factor for skeletal complications after fusion, we compared a cohort of 31 patients with skeletal complications to 38 patients with non-skeletal complications. Skeletal complications included adjacent segment fracture, screw loosening, pseudarthrosis, and rod breakage (Table 3). Non-skeletal conditions were spinal stenosis or degeneration in an adjacent segment. Both groups did not differ in age, sex distribution, BMI, or other risk factors (Figure 3A-C, Table 3). Only the time between primary surgery and revision (ie, follow-up) was significantly lower in patients with skeletal complications (Table 3). Contrary to our assumption, there were no differences in BMD T-scores or vitamin D and PTH levels between the 2 groups (Table 4, Figure 3D-F). Several other laboratory parameters such as phosphate or alkaline phosphatase were also not different between patients with skeletal and non-skeletal complications (Table 4).
Table 3.
Demographics, medical history, risk factors, and diagnoses underlying revision in patients undergoing revision surgery for skeletal vs non-skeletal complications.
| Parameter | Skeletal (n=31) | Non-Skeletal (n=38) | P-value |
|---|---|---|---|
| Age (yr.) | 71.0 (63.0 to 78.0) | 69.5 (63.0 to 77.0) | .92 |
| Sex f/m (n) | 18/13 | 23/15 | .84 |
| BMI (kg/m2) | 28.7 (25.9 to 29.8) | 29.1 (26.8 to 30.4) | .74 |
| Follow-Up (yr.) | 2.0 (1.0 to 2.0) | 5.0 (3.0 to 7.0) | < .001 |
| 1 vs ≥2 Revisions | 17/14 | 27 /11 | .16 |
| Prednisolone ≤7.5 mg (n, %) | 4 (12.9%) | 3 (7.9%) | .49 |
| Smoking (n, %) | 5 (16.1%) | 3 (7.9%) | .29 |
| Diagnoses /Complications | - Fracture (n=4) | - Spinal stenosis (n=21) | |
| - Screw loosening (n=7) | |||
| - Pseudarthrosis / rod breakage (n=20) | - Adjacent segment degeneration (n=17) |
Results are presented as median with 95% confidence intervals or n (%). Bold indicates significant differences (P < .05).
Figure 3.
Comparison of demographics, DXA results and laboratory bone metabolism parameters between patients with skeletal and non-skeletal complications after fusion. (A) Comparison of age, (B) sex distribution, (C) BMI, (D) T-score (lowest value of the measuring sites), (E) vitamin D, and (F) PTH. The dashed lines of the truncated violin plots represent the median and quartiles. P-values are given above the diagrams.
Table 4.
DXA and laboratory results in patients undergoing revision surgery due to skeletal vs non-skeletal complications.
| Parameter | Skeletal (n=31) | Non-Skeletal (n=38) | P-value |
|---|---|---|---|
| DXA results | |||
| BMD left hip (g/cm2) | .92 (.87 to 1.00) | .96 (.88 to 1.03) | .88 |
| T-score left hip | -.8 (-1.1 to -.2) | -.5 (-1.0 to .10) | .88 |
| BMD right hip (g/cm2) | .92 (.84 to 1.00) | .94 (.85 to .99) | .96 |
| T-score right hip | -.9 (-1.4 to -.1) | -.6 (-1.4 to -.2) | .83 |
| BMD lumbar spine (g/cm2) | 1.15 (.96 to 1.40) | 1.08 (.93 to 1.23) | .21 |
| T-score lumbar spine | -.5 (-2.0 to 1.7) | -.8 (-1.9 to .2) | .35 |
| T-score lowest | -1.2 (-1.9 to -.5) | -.9 (-1.6 to -.5) | .85 |
| Osteopenia (%) | 12 (38.7%) | 14 (36.8%) | .87 |
| Osteoporosis (%) | 5 (16.1%) | 4 (10.5%) | .49 |
| - Diagnosed before? | 4/5 (80.0%) | 3/4 (75.0%) | |
| Laboratory | |||
| Calcium (mmol/l) | 2.29 (2.24 to 2.35) | 2.31 (2.25 to 2.36) | .54 |
| 25-OH-D3 (nmol/l) | 72.4 (34.0 to 97.7) | 65.2 (35.4 to 92.9) | .69 |
| - Vitamin D deficiency (n, %) | 14 (45.2%) | 16 (42.1%) | .80 |
| PTH (pmol/l) | 4.98 (3.77 to 6.10) | 5.17 (4.10 to 6.66) | .33 |
| - HPT (n, %) | 2 (6.5%) | 5 (13.2%) | .36 |
| Phosphate (pmol/l) | 3.00 (2.60 to 3.40) | 3.10 (3.00 to 3.30) | .54 |
| ALP (U/l) | 78.5 (73.0 to 91.0) | 78.5 (70.0 to 88.0) | .72 |
| Creatinine (mg/dl) | .80 (.70 to .86) | .78 (.73 to .85) | .71 |
| CRP (mg/dl) | .1 (.1 to .3) | .2 (.1 to .6) | .80 |
| Leukocytes (G/l) | 7.1 (6.6 to 7.9) | 7.8 (7.0 to 8.3) | .46 |
| Hemoglobin (g/dl) | 13.2 (12.4 to 13.9) | 13.0 (12.4 to 13.5) | .44 |
Results are presented as median with 95% confidence intervals or n (%). HPT: hyperparathyroidism.
Discussion
It is well known that bone quality has a significant impact on the outcome of spine surgery15,16. Complications attributed to poor bone quality (ie, skeletal complications) include adjacent segment fracture, screw loosening, pseudarthrosis, and rod breakage. Consistent results are lacking on how many patients suffer from a relevant impairment of BMD (ie, osteoporosis and osteopenia) measured by DXA and how this varies between different conditions or types of surgeries. In the present study, we provide a comprehensive overview on the skeletal status in 389 patients scheduled for elective primary and revision lumbar spine surgery. We demonstrated that osteoporosis is a relevant und underdiagnosed comorbidity in these patients, ranging from 9.7% in men to 13.4% in women, and from 9.7% in patients indicated for discectomy to 16.1% in patients indicated for revision due to skeletal complications after lumbar fusion. However, we were unable to confirm the hypothesis that impaired BMD or bone metabolism is associated with skeletal complications.
Overall, our patient cohort showed a high rate of previously undiagnosed osteoporosis. While the frequency of osteoporosis in our cohort of central European patients was slightly higher than in other comparable cohorts 17 , it was also markedly lower than in Chinese populations, some of which had 39.7% of patients with osteoporosis prior to fusion for degenerative disease 12 . The clinical issue of underdiagnosed osteoporosis has already been demonstrated in other cohorts scheduled for elective orthopaedic surgery such as total hip or knee arthroplasty18-20. Although we could not show an effect of low BMD in association with skeletal complications such as screw loosening through our case-control approach, our results are relevant because a substantial proportion of patients had previously undiagnosed osteoporosis or osteopenia. It is unquestionable that DXA represents a good predictor of vertebral fracture risk 21 . Furthermore, appropriate osteoporosis medication contributes to a significant reduction in fracture risk 22 , which is of particular relevance for patients indicated for spine surgery since vertebral fractures are one of the most common osteoporotic fractures. Importantly, it has also been shown that preoperative osteoporosis treatment is associated with a lower risk of skeletal complications and revision surgery after fusion 23 . Although less evidence exists for the association between low BMD and skeletal complications in patients with discectomy or decompression, skeletal assessment for fracture prevention appears useful in these patients as well. Biomechanical studies have shown that BMD reduces the shear force to failure after laminectomy 24 .
Comparing the groups scheduled for primary spine surgery (discectomy, decompression, fusion), the bone status in terms of lowest BMD or T-score did not differ, however, significantly lower BMD values and T-scores were measured in the lumbar spine in patients with fusion compared to decompression. This difference may be due to the higher proportion of women and the higher proportion of patients on prednisolone therapy in the fusion group. In addition, the fusion group consisted of patients suffering from osteochondrosis and spondylolisthesis as compared to spinal stenosis in the decompression group. Since degenerative spondylolisthesis has been associated with lower BMD values than in patients with spinal stenosis 25 , we additionally compared these 2 disease entities in our cohort with respect to their skeletal status and independent of the type of surgery, but no significant differences could be detected (Supplementary Figure 1). In our view, it is unlikely that these 2 degenerative diseases of the lumbar spine have different skeletal risk profiles.
In addition to BMD data, our data provide insight into bone and mineral metabolism, with 67.6% of patients being vitamin D deficient. The implications of vitamin D deficiency are evidenced not only by its negative effects on skeletal mineralization, but also by the fact that 15.2% presented with secondary hyperparathyroidism, which is known to lead to increased bone resorption 26 . Previously, a similar prevalence of vitamin D deficiency was found in patients prior to spine surgery 27 . We recommend appropriate substitution for all vitamin D deficient patients, as the beneficial effect of vitamin D supplementation on bone health are well-established. However, future longitudinal studies should investigate the influence of vitamin D status on the outcome of spine surgery.
Known risk factors for skeletal complications after spine surgery are smoking 16 , obesity 28 , and low volumetric BMD measured by computed tomography (CT) 16 . Biomechanical experiments demonstrated that BMD correlated strongly with screw pullout strength 29 or cycles to failure during fatigue testing 30 , providing explanations for BMD as a risk factor for skeletal complications. The results of a systematic review indicated that the incidence of screw loosening is higher in osteoporotic spines than with normal BMD 31 . In the present clinical cohort, BMD values measured by DXA did not appear to have the potential to predict the risk of skeletal complications. The reason for this may be that measurement of spinal BMD in patients with degenerative spinal disease is prone to error and may result in artificially high values15,32. Similar to our results, a previous study could also not confirm a significant difference between patients with and without screw loosening after fusion 33 . Another study found that while both lower T-scores by DXA and Hounsfield units were associated with skeletal complications, only Hounsfield units served as an independent predictor of skeletal complications 34 . Hounsfield units by computed tomography showed better predictive value regarding screw loosening than DXA 33 . Other studies confirmed the value of Hounsfield units in the prediction of screw loosening 6 . Importantly, patients with skeletal complications after fusion presented with an abnormal bone microarchitecture measured at peripheral skeletal sites, despite having similar DXA values 3 . Furthermore, DXA did not represent local bone structure in patients with osteoporosis 35 . Although these collective results indicate a limited value of DXA in the context of revision spine surgery, DXA also remains the global gold standard in the diagnosis of osteoporosis, with national guidelines on decisions regarding anti-osteoporotic therapy being made based on this technique.
There are some limitations of our study. While the total number of patients included was high, the retrospective, cross-sectional study design did not allow precise information on the predictive value of the measured parameters such as DXA and laboratory values on certain skeletal complications. In the case-control setup of patients indicated for revision surgery, only group comparisons could be made, but these cross-sectional data do not allow further calculations. Another limitation is that in the subgroup of patients with complications after fusion, the DXA values of the spine could only be used in a small number of cases. Thus, it is possible that certain local changes in bone quality were not adequately reflected in some patients, as only hip measurements were included in the categorization of osteoporosis.
Conclusion
In patients scheduled for elective lumbar spine surgery, a relevant risk of osteoporosis was demonstrated. In terms of clinical decision making, these findings are relevant as they raise the awareness of underdiagnosed osteoporosis in patients prior to elective spine surgery, suggesting that preoperative DXA measurement should be considered in these patients, especially those with risk factors. In patients with low BMD (ie, osteoporosis) adequate bone-specific therapy should be initiated to reduce the risk of skeletal complications, and the surgical strategy should be adapted. However, our results also highlight that patients with skeletal-related complications may be inadequately identified by DXA, suggesting that other high-resolution techniques should be considered in this context.
Supplemental Material
Supplemental Material for Skeletal Status in Patients Scheduled for Elective Lumbar Spine Surgery: Comparison of Discectomy, Decompression, Fusion, and Revision by Christian Schaefer, Afshin Mafi, Frank Timo Beil, Malte Schroeder and Tim Rolvien in Global Spine Journal
Author contributions: Conceptualization: CS, AM, FTB, MS and TR; Methodology: AM, MS and TR; Formal analysis and investigation: CS, AM, FTB, MS and TR; Writing - original draft preparation: CS, AM and TR; Writing - review and editing: CS, AM, FTB, MS and TR; Funding acquisition: n/a; Resources: CS and FTB; Supervision: CS, FTB and TR.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: This retrospective study was approved by the local ethics committee (2021-300036-WF) and was performed in accordance with the most recent version of the Declaration of Helsinki. As a retrospective chart review was performed, additional consent was not required.
Supplemental Material: Supplemental material for this article is available online.
ORCID iD
Tim Rolvien https://orcid.org/0000-0003-1058-1307
References
- 1.Yoon WW, Koch J. Herniated discs: when is surgery necessary? EFORT Open Reviews. 2021;6(6):526-530. doi: 10.1302/2058-5241.6.210020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. New England Journal of Medicine. 2008;358(8):794-810. doi: 10.1056/NEJMoa0707136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim HJ, Dash A, Cunningham M, et al. Patients with abnormal microarchitecture have an increased risk of early complications after spinal fusion surgery. Bone. 2021;143:115731. doi: 10.1016/j.bone.2020.115731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. The Lancet. 2002;359(9319):1761-1767. doi: 10.1016/S0140-6736(02)08657-9 [DOI] [PubMed] [Google Scholar]
- 5.Schmidt T, Ebert K, Rolvien T, et al. A retrospective analysis of bone mineral status in patients requiring spinal surgery. BMC Musculoskeletal Disorders. 2018;19(1):53. doi: 10.1186/s12891-018-1970-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu F, Zou D, Li W, Sun Z, Jiang S, Zhou S, Li Z. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurgical Focus. 2020;49(2):E10. doi: 10.3171/2020.5.FOCUS20249 [DOI] [PubMed] [Google Scholar]
- 7.Anderson PA, Morgan SL, Krueger D, et al. Use of Bone Health Evaluation in Orthopedic Surgery: 2019 ISCD Official Position. Journal of Clinical Densitometry. 2019;22(4):517-543. doi: 10.1016/j.jocd.2019.07.013 [DOI] [PubMed] [Google Scholar]
- 8.Paz RD-R, Henríquez MS, Melián KA, Martin CB. Prevalence of Poor Bone Quality in Patients Undergoing Spine Surgery: A Comprehensive Approach. Global Spine Journal. 2021;25:219256822198968. doi: 10.1177/2192568221989684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bao J, Zou D, Li W. Characteristics of the DXA Measurements in Patients Undergoing Lumbar Fusion for Lumbar Degenerative Diseases: A Retrospective Analysis of Over 1000 Patients. Clinical Interventions in Aging. 2021;16:1131-1137. doi: 10.2147/CIA.S300873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chin DK, Park JY, Yoon YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporosis International. 2007;18(9):1219-1224. doi: 10.1007/s00198-007-0370-8 [DOI] [PubMed] [Google Scholar]
- 11.Kadri A, Binkley N, Hare KJ, Anderson PA. Bone Health Optimization in Orthopaedic Surgery. Journal of Bone and Joint Surgery. 2020;102(7):574-581. doi: 10.2106/JBJS.19.00999 [DOI] [PubMed] [Google Scholar]
- 12.Zou D, Jiang S, Zhou S, Sun Z, Zhong W, Du G, Li W. Prevalence of Osteoporosis in Patients Undergoing Lumbar Fusion for Lumbar Degenerative Diseases. Spine. 2020;45(7):E406-E410. doi: 10.1097/BRS.0000000000003284 [DOI] [PubMed] [Google Scholar]
- 13.Dimai HP. Use of dual-energy X-ray absorptiometry (DXA) for diagnosis and fracture risk assessment; WHO-criteria, T- and Z-score, and reference databases. Bone. 2017;104:39-43. doi: 10.1016/j.bone.2016.12.016 [DOI] [PubMed] [Google Scholar]
- 14.Thomasius F, Baum E, Bernecker P, et al. DVO Leitlinie 2017 zur Prophylaxe, Diagnostik und Therapie der Osteoporose bei postmenopausalen Frauen und Männern. Osteologie. 2018;27:154-160. [Google Scholar]
- 15.Pennington Z, Ehresman J, Lubelski D, et al. Assessing underlying bone quality in spine surgery patients: a narrative review of dual-energy X-ray absorptiometry (DXA) and alternatives. The Spine Journal. 2021;21(2):321-331. doi: 10.1016/j.spinee.2020.08.020 [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Dash A, Krez A, et al. Low volumetric bone density is a risk factor for early complications after spine fusion surgery. Osteoporosis International. 2020;31(4):647-654. doi: 10.1007/s00198-019-05245-7 [DOI] [PubMed] [Google Scholar]
- 17.Bjerke BT, Zarrabian M, Aleem IS, et al. Incidence of Osteoporosis-Related Complications Following Posterior Lumbar Fusion. Global Spine Journal. 2018;8(6):563-569. doi: 10.1177/2192568217743727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Delsmann MM, Strahl A, Mühlenfeld M, et al. High prevalence and undertreatment of osteoporosis in elderly patients undergoing total hip arthroplasty. Osteoporosis International. 2021;32(8):1661-1668. doi: 10.1007/s00198-021-05881-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delsmann MM, Schmidt C, Mühlenfeld M, et al. Prevalence of osteoporosis and osteopenia in elderly patients scheduled for total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery. 2021; Online ahead of print. doi: 10.1007/s00402-021-04297-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang Z, Levin JE, Amen TB, Arzani A, Manzi JE, Lane JM. Total Joint Arthroplasty and Osteoporosis: Looking Beyond the Joint to Bone Health. The Journal of Arthroplasty. 2022;18. Apr. doi: 10.1016/j.arth.2022.04.010 [DOI] [PubMed] [Google Scholar]
- 21.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ. 1996;312(7041):1254-1259. doi: 10.1136/bmj.312.7041.1254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bilezikian JP. Efficacy of bisphosphonates in reducing fracture risk in postmenopausal osteoporosis. The American Journal of Medicine. 2009;122(2 suppl l):S14-S21. doi: 10.1016/j.amjmed.2008.12.003 [DOI] [PubMed] [Google Scholar]
- 23.Jain N, Labaran L, Phillips FM, et al. Prevalence of Osteoporosis Treatment and Its Effect on Post-Operative Complications, Revision Surgery and Costs After Multi-Level Spinal Fusion. Global Spine Journal. 2020;219256822097656. doi: 10.1177/2192568220976560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bisschop A, Mullender MG, Kingma I, et al. The impact of bone mineral density and disc degeneration on shear strength and stiffness of the lumbar spine following laminectomy. European Spine Journal. 2012;21(3):530-536. doi: 10.1007/s00586-011-1968-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen T, Christensen FB, Langdahl BL, et al. Degenerative spondylolisthesis is associated with low spinal bone density: a comparative study between spinal stenosis and degenerative spondylolisthesis. BioMed Research International. 2013;2013:1-8. doi: 10.1155/2013/123847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lips P. Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocrine Reviews. 2001;22(4):477-501. doi: 10.1210/edrv.22.4.0437 [DOI] [PubMed] [Google Scholar]
- 27.Ravindra VM, Godzik J, Guan J, et al. Prevalence of Vitamin D Deficiency in Patients Undergoing Elective Spine Surgery: A Cross-Sectional Analysis. World Neurosurgery. 2015;83(6):1114-1119. doi: 10.1016/j.wneu.2014.12.031 [DOI] [PubMed] [Google Scholar]
- 28.Jiang J, Teng Y, Fan Z, Khan S, Xia Y. Does obesity affect the surgical outcome and complication rates of spinal surgery? A meta-analysis. Clinical Orthopaedics & Related Research. 2014;472(3):968-975. doi: 10.1007/s11999-013-3346-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilbert SG, Johns PC, Chow DC, Black RC. Relation of vertebral bone screw axial pullout strength to quantitative computed tomographic trabecular bone mineral content. Journal of Spinal Disorders. 1993;6(6):513-521. doi: 10.1097/00002517-199306060-00007 [DOI] [PubMed] [Google Scholar]
- 30.Weiser L, Huber G, Sellenschloh K, et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: biomechanical correlation of bone mineral density and pedicle screw fixation strength. European Spine Journal. 2017;26(11):2891-2897. doi: 10.1007/s00586-017-5091-x [DOI] [PubMed] [Google Scholar]
- 31.Rometsch E., Spruit M., Zigler J. E., Menon V. K., Ouellet J. A., Mazel C., Härtl R., Espinoza K., Kandziora F.. Screw-Related Complications After Instrumentation of the Osteoporotic Spine: A Systematic Literature Review With Meta-Analysis. Global Spine Journal. 2020;10(1):69-88. doi: 10.1177/2192568218818164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Liu G, Peacock M, Eilam O, Dorulla G, Braunstein E, Johnston CC. Effect of osteoarthritis in the lumbar spine and hip on bone mineral density and diagnosis of osteoporosis in elderly men and women. Osteoporosis International. 1997;7(6):564-569. doi: 10.1007/BF02652563 [DOI] [PubMed] [Google Scholar]
- 33.Zou D, Sun Z, Zhou S, Zhong W, Li W. Hounsfield units value is a better predictor of pedicle screw loosening than the T-score of DXA in patients with lumbar degenerative diseases. European Spine Journal. 2020;29(5):1105-1111. doi: 10.1007/s00586-020-06386-8 [DOI] [PubMed] [Google Scholar]
- 34.St Jeor JD, Jackson TJ, Xiong AE, et al. Average Lumbar Hounsfield Units Predicts Osteoporosis-Related Complications Following Lumbar Spine Fusion. Global Spine Journal. 2020;23:219256822097536. doi: 10.1177/2192568220975365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pumberger M, Palmowski Y, Strube P, et al. Dual-energy X-ray Absorptiometry Does Not Represent Bone Structure in Patients with Osteoporosis: A Comparison of Lumbar Dual-Energy X-Ray Absorptiometry with Vertebral Biopsies. Spine (Phila Pa 1976). 2021;46(13):861-866. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Skeletal Status in Patients Scheduled for Elective Lumbar Spine Surgery: Comparison of Discectomy, Decompression, Fusion, and Revision by Christian Schaefer, Afshin Mafi, Frank Timo Beil, Malte Schroeder and Tim Rolvien in Global Spine Journal