Abstract
Background
Invasive pulmonary aspergillosis is a complication of severe COVID-19, with regional variation in reported incidence and mortality. We describe the incidence, risk factors and mortality associated with COVID-19-associated pulmonary aspergillosis (CAPA) in a prospective, multicentre UK cohort.
Methods
From March 2020 to March 2021, 266 mechanically ventilated adults with COVID-19 were enrolled across 5 UK hospital intensive care units (ICUs). CAPA was defined using European Confederation for Medical Mycology and the International Society for Human and Animal Mycology criteria and fungal diagnostics performed on respiratory and serum samples.
Results
Twenty-nine of 266 patients (10.9%) had probable CAPA, 14 (5.2%) possible CAPA and none proven CAPA. Probable CAPA was diagnosed a median of 9 (IQR 7–16) days after ICU admission. Factors associated with probable CAPA after multivariable logistic regression were cumulative steroid dose given within 28 days prior to ICU admission (adjusted OR (aOR) 1.16; 95% CI 1.01 to 1.43 per 100 mg prednisolone-equivalent), receipt of an interleukin (IL)-6 inhibitor (aOR 2.79; 95% CI 1.22 to 6.48) and chronic obstructive pulmonary disease (COPD) (aOR 4.78; 95% CI 1.13 to 18.13). Mortality in patients with probable CAPA was 55%, vs 46% in those without. After adjustment for immortal time bias, CAPA was associated with an increased risk of 90-day mortality (HR 1.85; 95% CI 1.07 to 3.19); however, this association did not remain statistically significant after further adjustment for confounders (adjusted HR 1.57; 95% CI 0.88 to 2.80). There was no difference in mortality between patients with CAPA prescribed antifungals (9 of 17; 53%) and those who were not (7 of 12; 58%) (p=0.77).
Interpretation
In this first prospective UK study, probable CAPA was associated with corticosteroid use, receipt of IL-6 inhibitors and pre-existing COPD. CAPA did not impact mortality following adjustment for prognostic variables.
Keywords: COVID-19, critical care, aspergillus lung disease, viral infection
WHAT IS ALREADY KNOWN ON THIS TOPIC
Estimates of COVID-19-associated pulmonary aspergillosis (CAPA) incidence vary considerably (3–39%) according to geographical location and are primarily derived from small, retrospective studies. To our knowledge, this is the largest CAPA incidence study to employ a truly prospective methodology and the largest, regardless of methodology, performed in the UK.
WHAT THIS STUDY ADDS
We report an incidence of proven or probable CAPA of 10.9% and show that steroid dosing, receipt of an interleukin 6 inhibitor and pre-existing chronic obstructive pulmonary disease were all independently associated with a diagnosis of probable CAPA, an important consideration when managing critical care patients with COVID-19.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
We found no association between 90-day mortality and probable CAPA after adjustment for confounders. The difficulty in identifying cases of truly invasive disease in a critical care setting likely contributes to this finding and highlights the importance of improving upon current diagnostic criteria.
Introduction
Invasive pulmonary aspergillosis (IPA) is increasingly recognised as a complication of severe viral respiratory infection in patients who lack host factors traditionally associated with invasive fungal disease.1 Preceding viral infection increases susceptibility to secondary IPA by damaging the lung epithelium and transiently impairing the host immune response required for Aspergillus clearance,2 with influenza-associated pulmonary aspergillosis (IAPA) estimated to occur in up to 19% of mechanically ventilated patients.1 Despite differences in viral tropism and host immune responses between influenza and SARS-CoV-2,3 the shared features of epithelial damage and proinflammatory cytokine responses, combined with the administration of exogenous steroids, suggest a similar risk of development of secondary IPA in cases of severe COVID-19.
The reported incidence of COVID-19-associated pulmonary aspergillosis (CAPA) differs considerably between studies, with estimates ranging between 3% and 39%.4 While this may in part reflect true geographical variability, diverse utilisation of case definitions and fungal diagnostics makes such comparisons challenging.4 5
The publication of CAPA diagnostic criteria by the European Confederation for Medical Mycology and the International Society for Human and Animal Mycology (ECMM/ISHAM)6 have standardised reporting, but are not without limitations. Having been extrapolated from critically ill and influenza populations,1 7 8 these definitions’ ability to discriminate patients with COVID-19 with invasive fungal disease from those with Aspergillus airway colonisation requires further validation, particularly with respect to how a diagnosis of ‘probable CAPA’ relates to clinical outcomes, benefit from antifungal treatment9 and evidence of invasive disease on autopsy.5 10 11
To date, this is the only multicentre study in the UK to prospectively enrol intensive care unit (ICU) patients with the purpose of determining the incidence of secondary aspergillosis and identifying risk factors for its development. Adjusted mortality analyses were used to clarify the clinical significance of a ‘probable CAPA’ diagnosis in the context of current ECMM/ISHAM definitions.
Materials and methods
Study design and participating centres
We performed a multicentre, prospective cohort study across five UK hospital ICUs: St George’s University Hospital (SGH); St Thomas’ Hospital (STH); King’s College Hospital (KCH), London; Glenfield University Hospital (GUH), Leicester; University Hospital of Wales (UHW), Cardiff. STH and GUH serve as regional extracorporeal membrane oxygenation (ECMO) referral centres. Inclusion criteria were age ≥18 years and ICU admission for mechanical ventilation or ECMO due to respiratory failure from COVID-19, confirmed by SARS-CoV-2 RNA PCR from a respiratory specimen taken <7 days pre-admission, or 3 days post-admission to the participating study ICU. Patients with a history of IPA were excluded.
Patient enrolment
Patients were prospectively enrolled during the first and second COVID-19 waves (23 March 2020–23 March 2021). Since all patients lacked capacity, personal (friend or family member) or nominated (healthcare professional independent of study) consultee consent was obtained, followed by retrospective consent (from the patient) for those who recovered.
Study procedures
Serum sampling was performed within 72 hours of enrolment and repeated 5–10 days later for those still in the ICU. Surplus material from bronchoalveolar lavage (BAL), non-directed bronchoalveolar lavage (NBL) and endotracheal aspirates (ETAs) performed as part of routine clinical care was also stored. Demographic and clinical data were collected using REDCap electronic data capture tools.12 13 Corticosteroid doses were standardised using equivalent prednisolone dosing (pred-eq) and mould-active antifungal therapy was defined as any regimen containing voriconazole, isavuconazole, posaconazole, an echinocandin or amphotericin B given for ≥2 days.
Mycological testing
Prospective mycological testing was performed at the discretion of the treating physicians and results of fungal cultures/biomarkers, and Aspergillus PCR recorded. Excess respiratory samples and protocol-mandated serum samples were stored at −80°C and batch tested at study end for galactomannan (GM) using an Aspergillus antigen assay (GM-EIA) (BioRad, Hemel Hempstead, UK), Aspergillus PCR (BioMerieux Emag extractor and the Fungiplex Aspergillus IVD PCR Kit, Bruker, Glasgow, UK) and (1-3)-β-D-glucan (Fungitell, Associates of Cape Cod, Liverpool, UK).
Outcomes
The primary outcome was the incidence of ‘proven’, ‘probable’ and ‘possible’ CAPA as per ECMM/ISHAM criteria (online supplemental table 1), calculated over the course of a patient’s ICU stay, up to a maximum of 90 days. To maximise specificity, for all analyses unless otherwise stated, we dichotomised patients as having either ‘proven/probable CAPA’ or as ‘no evidence of proven/probable CAPA’. Possible cases were therefore not considered to have CAPA and were categorised alongside patients without evidence of CAPA. Risk factors associated with proven/probable CAPA were assessed, as was the association between proven/probable CAPA and 90-day mortality following ICU admission. Sensitivity analyses were performed, both comparing patients with either probable or possible CAPA with those without, as well as excluding cases of possible CAPA from the analysis completely. We also report on the impact of using alternative diagnostic criteria proposed by White et al,14 Verweij et al 8 and Bassetti et al 15 on incidence and survival (criteria in online supplemental table 1).
thorax-2023-220002supp001.pdf (349.1KB, pdf)
Statistical analysis
Analyses were performed using R Statistical Software.16 Χ2 or Fisher’s exact test was used for categorical variables, and Wilcoxon rank-sum test or t-test for continuous variables. Adjusted p values, calculated using the false discovery rate method, are displayed to account for multiple testing. The 95% CIs for incidence were calculated using Clopper-Pearson intervals.
Logistic regression was performed to identify factors associated with proven/probable CAPA. To prevent overfitting, four variables were chosen a priori according to best evidence (all risk factors known to occur before the development of CAPA): total steroid dose given within the 28 days prior to ICU admission (per 100 mg pred-eq),14 17–19 receipt of interleukin (IL)-6 inhibitor,17 20 21 disease severity (Acute Physiology and Chronic Health Evaluation II (APACHE II) score at ICU admission per 3-point increase)17 19 and chronic obstructive pulmonary disease (COPD).18 22
To eliminate time bias (patients with CAPA cannot die between ICU admission and CAPA diagnosis), the diagnosis of proven/probable CAPA was treated as a time-dependent variable and included in a Cox proportional hazards model to better investigate the association between proven/probable CAPA and 90-day mortality. Age, disease severity (APACHE II), ECMO (started prior to CAPA development) and COPD were selected a priori for inclusion in the multivariable analysis. Schoenfeld residuals were used to test the assumption of proportional hazards. Kaplan-Meier and Simon-Makuch plots23 are displayed to allow visualisation of mortality differences calculated by a Cox proportional hazards model.
Role of funding source
The funding source had no role in study design, conduct, analysis or write-up.
Results
Between 23 March 2020 and 23 March 2021, we enrolled 271 mechanically ventilated patients with COVID-19: 4 withdrew consent and 1 did not meet inclusion criteria, leaving 266 in the final analysis (table 1).
Table 1.
Patient characteristics and factors associated with a diagnosis of ‘probable CAPA’
| Overall, N=266 | No CAPA, N=237 | Probable CAPA, N=29 | P value | q-value* | |
| Age (years), median (IQR) | 56 (47–65) | 56 (46–65) | 58 (53–64) | 0.75† | 0.79 |
| Female gender, n (%) | 86 (32) | 78 (33) | 8 (28) | 0.56‡ | 0.70 |
| Ethnicity, n (%) | 0.15§ | 0.37 | |||
| White | 133 (50) | 114 (48) | 19 (66) | ||
| Asian | 66 (25) | 63 (27) | 3 (10) | ||
| Black | 39 (15) | 36 (15) | 3 (10) | ||
| Other | 28 (11) | 24 (10) | 4 (14) | ||
| APACHE II at admission, median (IQR) | 13 (10–18) | 13 (10–17) | 16 (9–20) | 0.18¶ | 0.40 |
| SOFA at admission, median (IQR) | 7 (5–8) | 7 (5–8) | 7 (5–8) | 0.26¶ | 0.43 |
| COPD, n (%) | 11 (4.1) | 7 (3.0) | 4 (14) | 0.022§ | 0.19 |
| Smoking history, n (%) | 59 (22) | 49 (21) | 10 (34) | 0.091‡ | 0.26 |
| BMI, median (IQR) | 30 (26–35) | 30 (26–35) | 31 (26–35) | 0.91† | 0.91 |
| Diabetes, n (%) | 77 (29) | 71 (30) | 6 (21) | 0.30‡ | 0.46 |
| Hypertension, n (%) | 102 (38) | 92 (39) | 10 (34) | 0.65‡ | 0.72 |
| Chronic kidney disease, n (%) | 15 (5.6) | 11 (4.6) | 4 (14) | 0.067§ | 0.22 |
| Neutrophil count at ICU admission, median (IQR) | 8.5 (5.8–11.5) | 8.6 (6.1–11.5) | 7.3 (5.6–11.6) | 0.63† | 0.72 |
| Lymphocyte count at ICU admission, median (IQR) | 0.60 (0.40–0.80) | 0.60 (0.40–0.86) | 0.60 (0.40–0.69) | 0.22† | 0.40 |
| Received renal replacement therapy, n (%) | 81 (31) | 70 (30) | 11 (38) | 0.38‡ | 0.50 |
| EORTC host criteria, n (%) | 14 (5.3) | 10 (4.2) | 4 (14) | 0.053§ | 0.21 |
| ECMO, n (%) | 51 (19) | 43 (18) | 8 (28) | 0.22‡ | 0.40 |
| Received IL-6 inhibitor, n (%) | 86 (32) | 71 (30) | 15 (52) | 0.018‡ | 0.15 |
| Received IL-1 inhibitor, n (%) | 15 (5.6) | 14 (5.9) | 1 (3.4) | >0.99† | >0.99 |
| Steroid dose (pred-eq) 28 days prior to ICU admission, mean (SD) | 86 (299) | 65(138) | 253 (810) | 0.16† | 0.36 |
| Length of ICU stay (days), median (IQR) | 20 (13–35) | 20 (12–34) | 28 (22–42) | 0.029† | 0.19 |
| 90-day mortality, n (%) | 125 (47) | 109 (46) | 16 (55) | 0.35‡ | 0.50 |
Possible CAPA classified as no CAPA for this analysis. Bold values denote statistical significance at the p < 0.05 level.
*False discovery rate correction for multiple testing.
†Wilcoxon rank-sum test.
‡Pearson’s Χ2 test.
§Fisher’s exact test.
¶Welch two-sample t-test.
APACHE II, Acute Physiology and Chronic Health Evaluation II; BMI, body mass index; CAPA, COVID-19-associated pulmonary aspergillosis; COPD, chronic obstructive pulmonary disease; ECMO, extracorporeal membrane oxygenation; EORTC, European Organization for Research and Treatment of Cancer; ICU, intensive care unit; IL, interleukin; pred-eq, prednisolone equivalent; SOFA, Sequential Organ Failure Assessment.
Incidence risk of CAPA
There were no cases of proven CAPA, 29 (10.9%; 95% CI 7.4% to 15.3%) of probable CAPA, 14 (5.2%; 95% CI 2.9% to 8.7%) of possible CAPA and 223 (83.8%; 95% CI 78.8% to 88.0%) with no evidence of CAPA (recorded over the length of each patient’s ICU stay, up to a maximum of 90 days). A diagnosis of probable CAPA occurred at a median of 9 days (IQR: 7–16) from ICU admission. Table 1 summarises patient characteristics. There were no statistically significant differences in baseline demographics between patients who were diagnosed with probable CAPA and those who were not. Receipt of an IL-6 inhibitor (52% (15 of 29) vs 30% (71 of 237), p=0.018), COPD (14% (4 of 29) vs 3% (7 of 237), p=0.02) and longer ICU stays (28 days (22–42) vs 20 days (12–34), p=0.03) were more common in patients diagnosed with probable CAPA (table 1). The incidence risk of CAPA according to site was as follows: SGH 6.9% (6 of 87), STH 50% (6 of 12), KCH 12.8% (5 of 39), GUH 12.7% (11 of 86), UHW 11.9% (5 of 42).
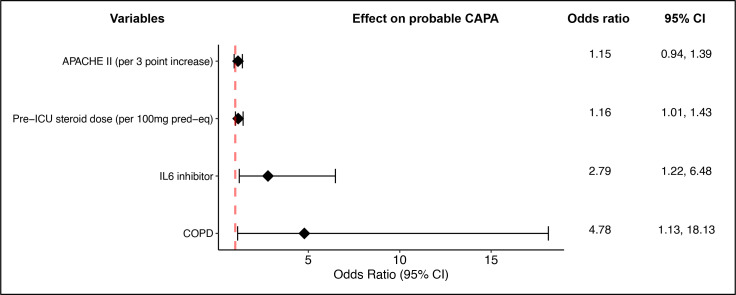
Factors associated with probable CAPA
In a multivariable logistic regression model, cumulative steroid dose given within 28 days prior to ICU admission (adjusted OR (aOR) 1.16; 95% CI 1.01 to 1.43 per 100 mg pred-eq), receipt of an IL-6 inhibitor (aOR 2.79; 95% CI 1.22 to 6.48) and COPD (aOR 4.78; 95% CI 1.13 to 18.13) were associated with the development of probable CAPA (figure 1). These factors remained statistically significant following sensitivity analyses excluding possible CAPA cases completely (ie, proven/probable CAPA compared only against patients with no evidence of CAPA). When possible cases were included with proven/probable CAPA cases and compared with those with no evidence of CAPA, only cumulative pre-ICU steroid dose (aOR 1.16; 95% CI 1.01 to 1.41) remained statistically significant (online supplemental figure 1).
Figure 1.
Factors associated with the development of probable CAPA. Multivariable logistic regression model. All coefficients exponentiated. APACHE II, Acute Physiology and Chronic Health Evaluation II, CAPA, COVID-19-associated pulmonary aspergillosis; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; IL, interleukin; pred-eq, prednisolone equivalent.
Survival analysis
Overall, 90-day mortality in our cohort was 47% (125 of 266). Mortality was similar in patients with and without probable CAPA (55% (16 of 29) vs 46% (109 of 237), p=0.35). In unadjusted univariable analysis (table 2), age (HR 1.15; 95% CI 1.07 to 1.25 per 5-year increase), baseline APACHE II score (HR 1.18; 95% CI 1.09 to 1.27, per 3-point increase), COPD (HR 2.39; 95% CI 1.21 to 4.71) and steroid dose prior to ICU admission (HR 1.06; 95% CI 1.01 to 1.12) were associated with 90-day mortality. There was no statistically significant difference in mortality between sites.
Table 2.
Factors associated with 90-day mortality: unadjusted univariable Cox regression analysis
| Characteristic | Estimate of effect HR (95% CI) | P value | q-value* |
| Probable CAPA | 1.15 (0.68 to 1.95) | 0.59 | 0.72 |
| Female gender | 0.76 (0.51 to 1.12) | 0.17 | 0.47 |
| Age (per 5-year increase) | 1.15 (1.07 to 1.25) | <0.001 | 0.002 |
| Ethnicity | |||
| White | — | ||
| Asian | 1.40 (0.93 to 2.11) | 0.11 | 0.37 |
| Black | 0.76 (0.43 to 1.37) | 0.36 | 0.68 |
| Other | 1.23 (0.70 to 2.16) | 0.48 | 0.68 |
| COPD | 2.39 (1.21 to 4.71) | 0.012 | 0.051 |
| Smoking history | 1.18 (0.78 to 1.78) | 0.43 | 0.68 |
| BMI (per point increase) | 0.99 (0.96 to 1.02) | 0.42 | 0.68 |
| Diabetes | 0.88 (0.59 to 1.31) | 0.52 | 0.69 |
| Hypertension | 0.94 (0.66 to 1.36) | 0.76 | 0.86 |
| EORTC host criteria | 1.31 (0.64 to 2.68) | 0.46 | 0.68 |
| APACHE II (per 3-point increase) | 1.18 (1.09 to 1.27) | <0.001 | <0.001 |
| Received ECMO | 0.97 (0.63 to 1.51) | 0.90 | 0.95 |
| Received IL-6 inhibitor | 0.82 (0.56 to 1.21) | 0.30 | 0.68 |
| Steroid dose 28 days prior to ICU admission (per 100 mg pred-eq) | 1.06 (1.01 to 1.12) | 0.016 | 0.056 |
Possible CAPA classified as no CAPA for this analysis. Bold values denote statistical significance at the p < 0.05 level.
*False discovery rate correction for multiple testing.
APACHE II, Acute Physiology and Chronic Health Evaluation II; BMI, body mass index; CAPA, COVID-19-associated pulmonary aspergillosis; COPD, chronic obstructive pulmonary disease; ECMO, extracorporeal membrane oxygenation; EORTC, European Organization for Research and Treatment of Cancer; ICU, intensive care unit; IL, interleukin; pred-eq, prednisolone equivalent.
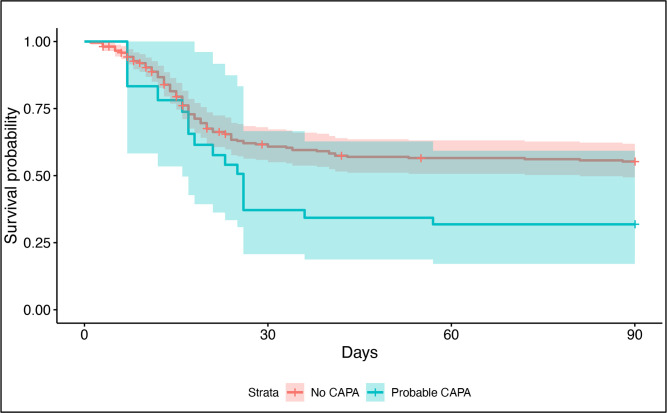
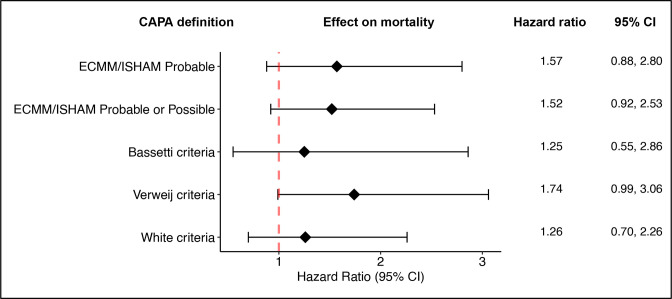
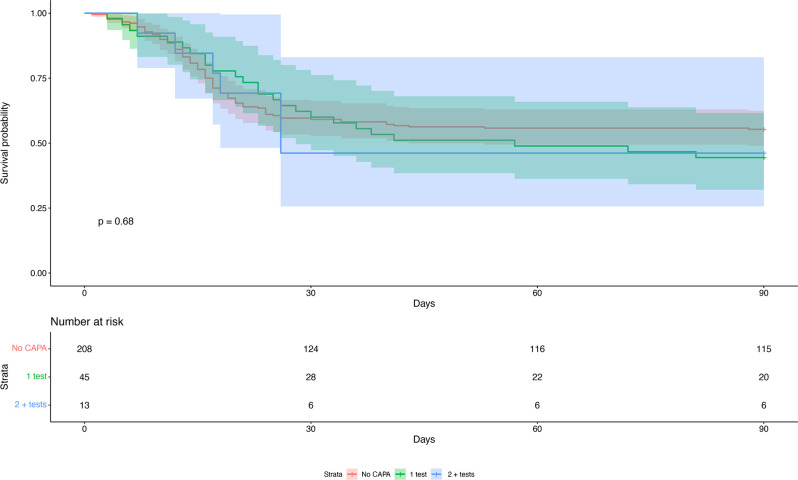
After immortal time bias (pertaining to the timing of CAPA diagnosis) was eliminated using a time-dependent Cox regression model, probable CAPA was associated with an increased risk of 90-day mortality (HR 1.85; 95% CI 1.07 to 3.19) (figure 2, Simon-Makuch plot); however, this association did not remain statistically significant after adjustment for confounders (adjusted HR (aHR) 1.57; 95% CI 0.88 to 2.80) (figure 3). In sensitivity analyses, these results were unaltered if possible cases were excluded entirely, or were considered to have CAPA (online supplemental figure 2).
Figure 2.
Simon-Makuch plot displaying time-adjusted survival probability over time in patients with a diagnosis of probable CAPA versus those without. Probability curves and p value calculated using an unadjusted time-dependent Cox proportional hazards model. CAPA, COVID-19-associated pulmonary aspergillosis.
Figure 3.
Risk of death according to published CAPA definitions. Point estimates and HRs calculated using a time-dependent Cox hazards regression model adjusted for age, APACHE II score, receipt of ECMO and COPD. All coefficients exponentiated. APACHE II, Acute Physiology and Chronic Health Evaluation II; CAPA, COVID-19-associated pulmonary aspergillosis; COPD, chronic obstructive pulmonary disease; ECMM/ISHAM, European Confederation for Medical Mycology and the International Society for Human and Animal Mycology; ECMO, extracorporeal membrane oxygenation.
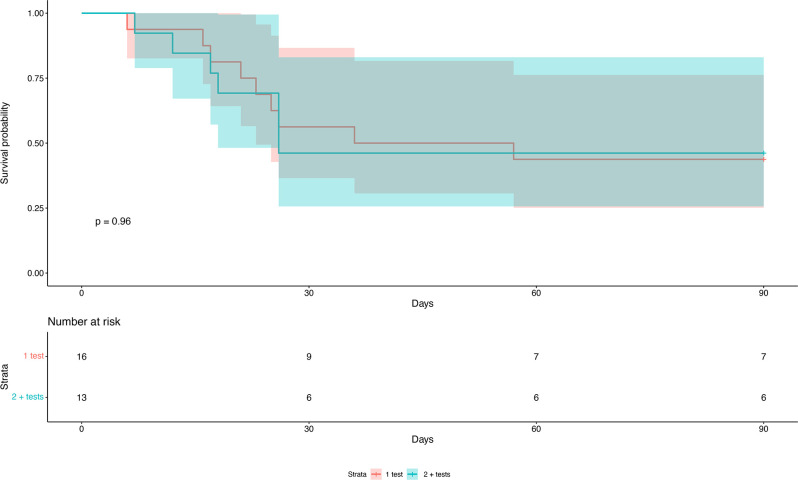
A differential diagnosis of CAPA assigned by the clinical care team was not predictive of 90-day mortality (HR 1.02; 95% CI 0.6 to 1.72), although 74% (23 of 31) of these patients were given timely antifungal therapy. There was also no difference in mortality according to the number of positive mycological tests a patient had (figures 4 and 5), or according to BAL-GM values (HR 1.02, CI 0.88 to 1.17 per 1.0 increase in galactomannan index (GMI)). Similarly, serum biomarker positivity (serum β-D-glucan and/or GM) in patients with probable CAPA (58% vs 53%, p=0.8) was not associated with increased mortality. There was insufficient evidence for an association between any of the published CAPA case definitions and risk of mortality when immortal time bias and confounders were adjusted for. However, point estimates for the HR were all above 1.2, with the Verweij et al criteria approaching statistical significance (figure 3).
Figure 4.
Kaplan-Meier survival analysis comparing 90-day mortality in patients with probable CAPA according to mycological test positivity. Tests included in analysis: serum β-D-glucan >80 (not part of ECMM/ISHAM criteria), serum GM >0.5, serum Aspergillus PCR CT <36, BAL culture, BAL-GM >1.0, BAL Aspergillus PCR CT <36. Probability curves and p value calculated using Cox proportional hazards model. BAL, bronchoalveolar lavage; CAPA, COVID-19-associated pulmonary aspergillosis; CT, cycle threshold; ECMM/ISHAM, European Confederation for Medical Mycology and the International Society for Human and Animal Mycology; GM, galactomannan.
Figure 5.
Kaplan-Meier survival analysis comparing 90-day mortality in patients without any positive mycology tests with those with one positive test and those with two or more positive tests (all patients in cohort included). Tests included: serum β-D-glucan >80 (not part of ECMM/ISHAM criteria), serum GM >0.5, serum Aspergillus PCR CT <36, BAL culture, BAL-GM >1.0, BAL Aspergillus PCR CT <36. Probability curves and p value calculated using Cox proportional hazards model. BAL, bronchoalveolar lavage; CAPA, COVID-19-associated pulmonary aspergillosis; CT, cycle threshold; ECMM/ISHAM, European Confederation for Medical Mycology and the International Society for Human and Animal Mycology; GM, galactomannan.
Effect of antifungal therapy
Of the 29 patients with probable CAPA, 17 (58%) received mould-active antifungal agents within 2 weeks of CAPA diagnosis. There was no difference in 90-day mortality between patients with probable CAPA prescribed mould-active antifungals (9 of 17; 53%) and those who were not (7 of 12; 58%) (p=0.77). For the 17 patients with CAPA who were prescribed them, antifungals were commenced between 21 days prior to 9 days after CAPA diagnosis (median +2 days, IQR −1 to +5) and continued for median duration of 13 days (IQR 8–21 days). Excluding the five patients receiving antifungals late (>48 hours after CAPA diagnosis), there remained no statistically significant difference in 90-day mortality (3 of 6 (50%) in the antifungal group vs 10 of 17 (59%) for none, p=0.64). In these 17 patients, the most commonly prescribed agents were voriconazole (148 patient-days), amphotericin B (58 patient-days), echinocandins (50 patient-days) and isavuconazole (5 patient-days). Of the 12 patients with probable CAPA who did not receive mould-active antifungals, a diagnosis of CAPA was made via retrospective sample testing in 4 of 12 (33%) and thus not known to the clinical care teams. When analysis was restricted to patients in the study cohort who did not receive antifungals, there remained no statistical difference in mortality between those with probable CAPA (7 of 12, 58%) and those without (86 of 190, 45%) (p=0.37).
Mycological sampling
In total, 461 sera were collected; all patients had at least one serum sample and 196 (74%) had two. One hundred thirty (48%) patients had at least one BAL (229 BALs total), and 156 (59%) at least some form of deep respiratory sample (additional 52 NBLs). BAL-GM was performed in 113 (42%) patients.
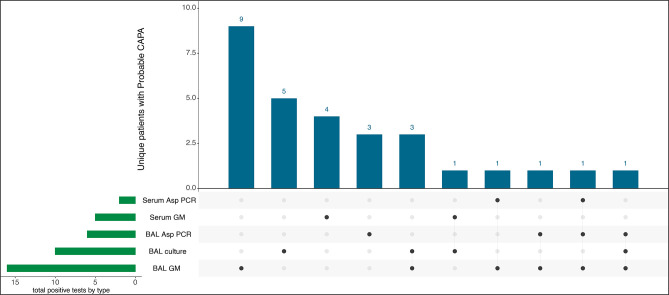
Mycological criteria
Test modalities used to define probable CAPA are shown in figure 6. The majority of probable CAPA cases (21 of 29; 72%) were defined by a single positive mycological test only, with nine attributed to BAL-GM positivity alone. Sixteen (55.2%) of 29 had at least one positive BAL-GM result. Serum GM was an insensitive marker for CAPA, with only 5 of 29 (17.2%) positive. Fifteen (51.7%) of 29 probable CAPA cases cultured Aspergillus spp from a respiratory sample (ETA/NBL/BAL) vs 10 (4.2%) of 237 without probable CAPA (eight of which were classified as possible CAPA). Ten (3.7%) of the 266 enrolled patients had cavities on CT imaging; of these, only two fulfilled the mycological criteria of probable CAPA. Tracheobronchitis was only seen in two (0.8%) patients (1.5% of patients who had at least one BAL), neither had any positive Aspergillus diagnostics so did not fulfil ECMM/ISHAM criteria for probable or possible CAPA. β-D-glucan is not included in the ECMM/ISHAM criteria but is in the White et al definition; in our series, 9 (31%) of 29 patients with probable CAPA had a positive serum β-D-glucan (≥80 pg/mL) compared with 21 (9%) of 237 without probable CAPA. Twenty-five of 29 (86.2%) of patients with CAPA could be classified using prospective clinical testing alone (without additional retrospective laboratory testing). Ten of 29 (34%) patients identified as having probable CAPA using ECMM/ISHAM criteria fulfilled case definitions proposed by White et al, Bassetti et al and Verweij et al 8 14 15 (online supplemental figure 3).
Figure 6.
UpSet diagram displaying positive test modalities in patients classified as probable CAPA. This diagram shows the number of diagnoses of probable CAPA made according to diagnostic test or combination of diagnostic tests. BAL, bronchoalveolar lavage; CAPA, COVID-19-associated pulmonary aspergillosis; GM, galactomannan.
Discussion
In this, the only multicentre, prospective UK CAPA study, we report a probable CAPA incidence risk of 10.9% among mechanically ventilated patients with COVID-19, diagnosed a median of 9 days after ICU admission, comparable with the 10–15% recently reported from retrospective multisite European cohorts,17 20 22 and 14% from the only other large UK cohort reported to date (using a different diagnostic classification).14 Given the reported regional and centre-specific variation in prevalence,4 prospectively collected, multicentre, country-specific data on CAPA epidemiology and outcomes are essential; however, pinpointing truly invasive fungal disease and therefore judging whom to treat with antifungal therapy in this ICU population, remain challenging.
Similar to Kariyawasam et al,5 we found limited agreement between different CAPA diagnostic criteria with only 10 of 29 (34%) patients with probable CAPA meeting case definitions as proposed by White et al, Bassetti et al and Verweij et al 8 14 15 (online supplemental figure 3). BAL-GM positivity has been shown to correlate with postmortem-confirmed invasive aspergillosis in immunosuppressed ICU patients without COVID-19,24 warranting its inclusion in the modified AspICU criteria proposed by Schauwvlieghe et al.1 Its utility in a clinically divergent COVID-19 population, however, does not appear to be as robustly supported.
While Bartoletti et al showed an association between BAL-GM and mortality,21 this finding has not been replicated elsewhere.25 Interestingly, one large multicentre cohort demonstrated that while combined BAL-GM and Aspergillus culture positivity was associated with mortality, BAL-GM positivity on its own (in culture-negative samples) was not.26 In a large review of autopsy studies, only 2% (6 of 320) of mechanically ventilated patients with COVID-19 had evidence of proven CAPA—much lower than one might expect from antemortem prevalence studies using ECMM/ISHAM criteria.10 It should be noted, however, that <10% of patients received IL-6 inhibitors or corticosteroids and only 38% had specific fungal histological staining (although fungal hyphae may be evident on H&E staining).27 Interestingly, one single-centre autopsy study did find postmortem rates of CAPA comparable with antemortem studies (20%), although it is possible that autopsies were selectively requested in patients with especially long or complex disease courses.11
With an inability to easily confirm invasive disease, mortality has been used as a proxy against which the validity of diagnostic criteria are judged, assuming that true IPA should be associated with higher mortality28: indeed, several prospective14 21 and retrospective17 19 20 29 studies have reported excess mortality with CAPA. However, others have not shown a difference, especially after adjustment for covariables.22 30 In our cohort, probable CAPA was associated with an almost twofold increase in the risk of death at 90 days after adjustment for immortal time bias. However, this association did not remain statistically significant after adjustment for confounders (aHR 1.57; 95% CI 0.88 to 2.80). It is possible that CAPA does influence mortality, but events were underpowered after adjustment. Similarly, although treatment with mould-active antifungals in those with probable CAPA was not associated with a reduction in mortality (p=0.87) (in keeping with a recent meta-analysis5), numbers were small.
Most intubated patients with COVID-19 fulfil clinical and radiological criteria for CAPA, placing a disproportionate emphasis on available mycological evidence. ECMM/ISHAM criteria maximise sensitivity by incorporating GM and Aspergillus PCR testing; however, with only a single positive test required, it is likely that patients with Aspergillus colonisation are classified alongside those with invasive disease, particularly if positivity is solely in respiratory samples. Interstudy differences in CAPA-related mortality may therefore reflect differences in the underlying prevalence of true invasive aspergillosis in the populations studied—with criteria-based ‘probable CAPA’ potentially capturing Aspergillus colonisation (ie, a false positive) in a low prevalence setting. Similarly, while a strength of our study, the fact that mycological screening was performed on any enrolled ICU patient with COVID-19 may have resulted in more false positives than where clinical deterioration/suspicion of CAPA prompts such investigations.14
Using quantitative biomarker indices and/or stratifying patients according to the number or type of positive mycological tests has been proposed as a tool to identify those with higher fungal burden and greater likelihood of invasive disease.31 Bartoletti et al reported greater mortality in those with higher BAL-GM values21 and in those diagnosed using the original AspICU criteria (reliant on positive Aspergillus culture rather than biomarkers).7 Similarly, Dellière et al found that multiple positive mycological tests and lower Aspergillus quantitative PCR cycle threshold values were associated with increased mortality.32 In contrast, we did not find statistically significant survival differences according to the number of positive mycological tests (figures 4 and 5) or higher BAL-GM values (HR 1.02, CI 0.88 to 1.17 per 1.0 increase in GMI). Interestingly however, the more stringent Verweij et al definition8 (which considers non-BAL respiratory samples only when lung cavitation is present) trended towards a more robust mortality association than the arguably less specific White et al criteria14 (which includes NBL samples and positive serum β-D-glucan) or Bassetti et al criteria15 (which specify a lower BAL-GM cut-off at 0.8) (figure 3).
Van de Veerdonk et al recently proposed that Aspergillus–host interaction in CAPA occurs on a spectrum, ranging from colonisation to angioinvasive disease.33 The threshold for angioinvasive disease is reached according to the cumulative effects of intrinsic and extrinsic factors such as those caused by the viral pathogen, immunomodulatory treatment and pre-existing host factors. In reference to this model, Ergün et al 25 proposed serum biomarker positivity as an indicator of angioinvasion, reporting a 30-day mortality of 83.3% in patients with CAPA with a positive serum β-D-glucan and/or GM, compared with 35% in those with negative serum biomarkers (p=0.014).25 In our study, however, 12 (41%) of 29 patients with CAPA with a positive serum β-D-glucan and/or GM had similar mortality to the 17 without (58% vs 53%, p=0.8). This again may suggest a lower prevalence of invasive disease in the UK setting. Of interest, of five patients with positive serum biomarkers alive at 90 days, only one did not receive timely antifungal therapy, although the small number of patients in this subgroup precludes meaningful analysis.
In contrast to IAPA, CAPA appears less likely to occur in the absence of additional risk factors1 25 33; therefore, identifying these factors is imperative in enabling patient risk stratification. Steroids and tocilizumab are frontline therapies in hypoxaemic patients with COVID-1934 to counter hyperinflammation characterising severe disease.35 However, by dampening the activation of innate and adaptive antimicrobial responses, they can also predispose to secondary fungal infections. With COPD, impaired ciliary activity and inhaled corticosteroids are likely to contribute to susceptibility.36 Our results strengthen the findings from other published cohorts in identifying these factors as independently contributing to the risk of developing CAPA.17 18 20 22 25 30
A limitation of our study was that bronchoscopy and BAL sampling was not protocol mandated. Early in the pandemic, the avoidance of aerosol-generating procedures meant that fewer patients had a BAL performed, and in those who did, excess sample was often not available for retrospective testing. There was also intercentre heterogeneity in mycological sampling and real-time availability of fungal diagnostics. While this is the largest UK prospective CAPA study to date, the relatively small number of patients with probable CAPA (29) limits the power to detect mortality associations and differences within subgroup analyses (eg, on the impact of antifungal therapy); therefore, any absence of statistical significance is not definitive evidence of a lack of association.
In summary, despite a prospective design and universal serum screening, the reported incidence of probable CAPA in this UK ICU cohort is at the lower end of the range of European estimates. We found no statistically significant excess mortality in patients diagnosed with CAPA after adjustment for prognostic covariables. Further postmortem studies evaluating current diagnostic criteria against histological evidence of invasive aspergillosis would be valuable but are logistically and ethically challenging. In the absence of a proven diagnosis, the benefit of antifungal therapy in patients with suspected CAPA must be carefully weighed against the cost, toxicity, potential for drug–drug interaction and development of antifungal resistance. We propose that criteria requiring >2 positive Aspergillus-specific tests, that is, GM or PCR from blood or BAL, or positive BAL culture, ideally from temporally separated samples, or a single test in the presence of additional clinical risk factors or specific radiological signs, would target antifungal therapy to those most likely to benefit. While this would require further validation and must be considered against the need to maintain diagnostic sensitivity, we believe that a single positive mycological test should act as the start, not the end, of investigation for CAPA.
Acknowledgments
We would like to acknowledge all the hard work of the research teams at each enrolling site; the laboratory personnel who performed the diagnostic testing; the patients for partaking in the study; the relatives and friends who provided consultee declarations during what must have been a difficult time and the Guy’s and St Thomas’ ECMO patient group who helped develop the research protocol.
Footnotes
WH and JY contributed equally.
DW and TB contributed equally.
Presented at: Provisional results of the Aspiflu Study were presented at the European Congress of Clinical Microbiology and Infectious Diseases (ECCMID) conference: ESCMID eAcademy. Hurt W. 07/09/21; 332512; 2753.
Contributors: DW, TB and JY conceived and designed the study. WH, JY, JB, JE, PH, DRJ, SS, MPW, PLW, HY, DW and TB all oversaw and administered the study. WH and PLW performed the retrospective diagnostic testing. WH and JY collected data. WH, AM and SFM analysed and visualised the data. WH, JY and TB wrote the original draft. All authors critically revised, read and approved the final manuscript. Guarantor, TB.
Funding: This study was supported by three successive UK & Ireland Invasive fungal disease fellowships 2019–2021 competitively awarded to TB by Gilead Sciences (grant numbers 07512, 11023, 14442). We also acknowledge funding from the MRC Centre for Medical Mycology at the University of Exeter (MR/N006364/2 and MR/V033417/1), the NIHR Exeter Biomedical Research Centre and the MRC Doctoral Training Grant (MR/W502649/1).
Disclaimer: Gilead had no role in study design, data collection, data analysis, data interpretation, writing of the manuscript or in the decision to publish.
Competing interests: MPW, WH and TB have received speaker fees from Gilead Sciences. JY has received honoraria from Pfizer for contributing to a CAPA working group. TB has received Advisory Board fees from Gilead Sciences and Mundipharma and funding from MSD and Pfizer. DRJ is the president of the British Society for Antimicrobial Chemotherapy and has received honoraria from Pfizer, Shionogi, Menarini and Tillots. SS has received honoraria from Pfizer and Gilead for educational purposes. PLW performed diagnostic evaluations and received meeting sponsorship from Associates of Cape Cod, Bruker, Dynamiker and Launch Diagnostics; speaker fees, expert advice fees and meeting sponsorship from Gilead; and speaker and expert advice fees from Pfizer and expert advice fees from F2G.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. All de-identified, individual participant data that underlie the reported results of this article, as well as the data dictionary, study material (protocols, consent forms, patient information sheets) and the R analytical code, are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by the National Research Ethics Committee (England and Wales REC 19/WA/0310, IRAS 271269). Participants gave informed consent to participate in the study before taking part.
References
- 1. Schauwvlieghe A, Rijnders BJA, Philips N, et al. Invasive aspergillosis in patients admitted to the intensive care unit with severe influenza: a retrospective cohort study. Lancet Respir Med 2018;6:782–92. 10.1016/S2213-2600(18)30274-1 [DOI] [PubMed] [Google Scholar]
- 2. Salazar F, Bignell E, Brown GD, et al. Pathogenesis of respiratory viral and fungal coinfections. Clin Microbiol Rev 2022;35:e00094-21. 10.1128/CMR.00094-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Youngs J, Provine NM, Lim N, et al. Identification of immune correlates of fatal outcomes in critically ill COVID-19 patients. PLoS Pathog 2021;17:e1009804. 10.1371/journal.ppat.1009804 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Feys S, Almyroudi MP, Braspenning R, et al. A visual and comprehensive review on COVID-19-associated pulmonary aspergillosis (CAPA). J Fungi (Basel) 2021;7:1067. 10.3390/jof7121067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kariyawasam RM, Dingle TC, Kula BE, et al. Defining COVID-19-associated pulmonary aspergillosis: systematic review and meta-analysis. Clin Microbiol Infect 2022;28:920–7. 10.1016/j.cmi.2022.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Koehler P, Bassetti M, Chakrabarti A, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis 2021;21:e149–62. 10.1016/S1473-3099(20)30847-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Blot SI, Taccone FS, Van den Abeele A-M, et al. A clinical algorithm to diagnose invasive pulmonary aspergillosis in critically ill patients. Am J Respir Crit Care Med 2012;186:56–64. 10.1164/rccm.201111-1978OC [DOI] [PubMed] [Google Scholar]
- 8. Verweij PE, Rijnders BJA, Brüggemann RJM, et al. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intensive Care Med 2020;46:1524–35. 10.1007/s00134-020-06091-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lamoth F, Lewis RE, Walsh TJ, et al. Navigating the uncertainties of COVID-19-associated aspergillosis: a comparison with influenza-associated Aspergillosis. J Infect Dis 2021;224:1631–40. 10.1093/infdis/jiab163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kula BE, Clancy CJ, Hong Nguyen M, et al. Invasive mould disease in fatal COVID-19: a systematic review of Autopsies. Lancet Microbe 2021;2:e405–14. 10.1016/S2666-5247(21)00091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fortarezza F, Boscolo A, Pezzuto F, et al. Proven COVID‐19—associated pulmonary aspergillosis in patients with severe respiratory failure. Mycoses 2021;64:1223–9. 10.1111/myc.13342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Minor BL, et al. The Redcap consortium: building an international community of software platform partners. J Biomed Inform 2019;95:103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (Redcap)--a metadata-driven methodology and Workflow process for providing translational research Informatics support. J Biomed Inform 2009;42:377–81. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. White PL, Dhillon R, Cordey A, et al. A national strategy to diagnose coronavirus disease 2019-associated invasive fungal disease in the intensive care unit. Clin Infect Dis 2021;73:e1634–44. 10.1093/cid/ciaa1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bassetti M, Azoulay E, Kullberg B-J, et al. EORTC/MSGERC definitions of invasive fungal diseases: summary of activities of the intensive care unit working group. Clin Infect Dis 2021;72:S121–7. 10.1093/cid/ciaa1751 [DOI] [PubMed] [Google Scholar]
- 16. R Core Team . R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2021. Available: https://www.R-project.org/ [Google Scholar]
- 17. Gangneux J-P, Dannaoui E, Fekkar A, et al. Fungal infections in mechanically ventilated patients with COVID-19 during the first wave: the French Multicentre MYCOVID study. Lancet Respir Med 2022;10:180–90. 10.1016/S2213-2600(21)00442-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Permpalung N, Chiang T-Y, Massie AB, et al. Coronavirus disease 2019-associated pulmonary aspergillosis in mechanically ventilated patients. Clin Infect Dis 2022;74:83–91. 10.1093/cid/ciab223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fekkar A, Lampros A, Mayaux J, et al. Occurrence of invasive pulmonary fungal infections in patients with severe COVID-19 admitted to the ICU. Am J Respir Crit Care Med 2021;203:307–17. 10.1164/rccm.202009-3400OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Prattes J, Wauters J, Giacobbe DR, et al. Risk factors and outcome of pulmonary aspergillosis in critically ill Coronavirus disease 2019 patients-a multinational observational study by the European Confederation of medical mycology. Clin Microbiol Infect 2022;28:580–7. 10.1016/j.cmi.2021.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bartoletti M, Pascale R, Cricca M, et al. Epidemiology of invasive pulmonary aspergillosis among intubated patients with COVID-19: a prospective study. Clin Infect Dis 2021;73:e3606–14. 10.1093/cid/ciaa1065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Janssen NAF, Nyga R, Vanderbeke L, et al. Multinational observational cohort study of COVID-19–associated pulmonary aspergillosis1 Emerg Infect Dis 2021;27:2892–8. 10.3201/eid2711.211174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Schultz LR, Peterson EL, Breslau N. Graphing survival curve estimates for time‐dependent covariates. Int J Methods Psychiatr Res 2002;11:68–74. 10.1002/mpr.124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Meersseman W, Lagrou K, Maertens J, et al. Galactomannan in bronchoalveolar Lavage fluid: a tool for diagnosing aspergillosis in intensive care unit patients. Am J Respir Crit Care Med 2008;177:27–34. 10.1164/rccm.200704-606OC [DOI] [PubMed] [Google Scholar]
- 25. Ergün M, Brüggemann RJM, Alanio A, et al. Aspergillus test profiles and mortality in critically ill COVID-19 patients. J Clin Microbiol 2021;59:e01229-21. 10.1128/JCM.01229-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Giacobbe DR, Prattes J, Wauters J, et al. Prognostic impact of bronchoalveolar lavage fluid galactomannan and aspergillus culture results on survival in COVID-19 intensive care unit patients: a post Hoc analysis from the European Confederation of medical mycology (ECMM) COVID-19-associated pulmonary aspergillosis study. J Clin Microbiol 2022;60:e02298-21. 10.1128/jcm.02298-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Egger M, Bussini L, Hoenigl M, et al. Prevalence of COVID-19-associated pulmonary aspergillosis: critical review and conclusions. J Fungi (Basel) 2022;8:390. 10.3390/jof8040390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Reichenberger F, Habicht JM, Gratwohl A, et al. Diagnosis and treatment of invasive pulmonary aspergillosis in neutropenic patients. Eur Respir J 2002;19:743–55. 10.1183/09031936.02.00256102 [DOI] [PubMed] [Google Scholar]
- 29. Dellière S, Dudoignon E, Fodil S, et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: a French multicentric retrospective cohort. Clinical Microbiology and Infection 2021;27:790. 10.1016/j.cmi.2020.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Leistner R, Schroeter L, Adam T, et al. Corticosteroids as risk factor for COVID-19-associated pulmonary aspergillosis in intensive care patients. Crit Care 2022;26:30. 10.1186/s13054-022-03902-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. D’Haese J, Theunissen K, Vermeulen E, et al. Detection of galactomannan in bronchoalveolar lavage fluid samples of patients at risk for invasive pulmonary aspergillosis: analytical and clinical validity. J Clin Microbiol 2012;50:1258–63. 10.1128/JCM.06423-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Dellière S, Dudoignon E, Voicu S, et al. Combination of Mycological criteria: a better surrogate to identify COVID-19-associated pulmonary Aspergillosis patients and evaluate prognosis? J Clin Microbiol 2022;60:e02169-21. 10.1128/JCM.02169-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van de Veerdonk FL, Wauters J, Verweij PE. Invasive aspergillus tracheobronchitis emerging as a highly lethal complication of severe influenza. Am J Respir Crit Care Med 2020;202:646–8. 10.1164/rccm.202005-1883ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med 2021;384:693–704. 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hoenigl M, Seidel D, Sprute R, et al. COVID-19-associated fungal infections. Nat Microbiol 2022;7:1127–40. 10.1038/s41564-022-01172-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bulpa P, Dive A, Sibille Y. Invasive pulmonary aspergillosis in patients with chronic obstructive pulmonary disease. Eur Respir J 2007;30:782–800. 10.1183/09031936.00062206 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thorax-2023-220002supp001.pdf (349.1KB, pdf)
Data Availability Statement
Data are available upon reasonable request. All de-identified, individual participant data that underlie the reported results of this article, as well as the data dictionary, study material (protocols, consent forms, patient information sheets) and the R analytical code, are available from the corresponding author on reasonable request.