Abstract
Introduction
Rising facility births in sub-Saharan Africa (SSA) mask inequalities in higher-level emergency care—typically in hospitals. Limited research has addressed hospital use in women at risk of or with complications, such as high parity, linked to poverty and rurality, for whom hospital care is essential. We aimed to address this gap, by comparatively assessing hospital use in rural SSA by wealth and parity.
Methods
Countries in SSA with a Demographic and Health Survey since 2015 were included. We assessed rural hospital childbirth stratifying by wealth (wealthier/poorer) and parity (nulliparity/high parity≥5), and their combination. We computed percentages, 95% CIs and percentage-point differences, by stratifier level. To compare hospital use across countries, we produced a composite index, including six utilisation and equality indicators.
Results
This cross-sectional study included 18 countries. In all, a minority of rural women used hospitals for childbirth (2%–29%). There were disparities by wealth and parity, and poorer, high-parity women used hospitals least. The poorer/wealthier difference in utilisation among high-parity women ranged between 1.3% (Mali) and 13.2% (Rwanda). We found use and equality of hospitals in rural settings were greater in Malawi and Liberia, followed by Zimbabwe, the Gambia and Rwanda.
Discussion
Inequalities identified across 18 countries in rural SSA indicate poor, higher-risk women of high parity had lower use of hospitals for childbirth. Specific policy attention is urgently needed for this group where disadvantage accumulates.
Keywords: Epidemiology, Maternal health, Obstetrics, Health systems
WHAT IS ALREADY KNOWN ON THIS TOPIC
Increases in facility births in sub-Saharan Africa (SSA) mask inequalities in access to hospitals and other facilities providing emergency obstetric care.
Use of hospitals is particularly important in women with pre-existing obstetric risk factors, including high parity, which is common in SSA and closely linked to poverty.
Previous studies from rural Tanzania have suggested that hospital-based childbirth care among poor high-parity women was very low (10% in 2015/2016) and had not increased in 25 years.
WHAT THIS STUDY ADDS
We found that a minority of rural births in 18 sub-Saharan African countries were in hospitals (range 2%–29%).
There were differences in use of hospitals for childbirth by wealth and parity in rural settings. Socioeconomic inequality in the use of hospitals for childbirth was prevalent among high-parity women in rural settings.
In this comparative analysis, some countries achieved greater utilisation and equality in hospital-based childbirth among rural women at high parity.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Our simple approach to assessing inequalities in use of childbirth care can be applied to other studies.
We identified countries with greater utilisation and equality which may serve as exemplars of how equitable use of hospital-based life-saving care can be achieved for rural, high-parity women in sub-Saharan Africa.
Introduction
The large number of deaths of women and their babies in sub-Saharan Africa (SSA) challenges the United Nations’ Sustainable Development Goals pledge of leaving no-one behind.1 In 2020 alone, 881 000 stillbirths,2 1.1 million neonatal deaths2 and 202 000 maternal deaths3 were estimated to have taken place in SSA contributing 46%, 46% and 70% to the global burden of stillbirths, neonatal and maternal deaths, respectively. The death toll is disproportionately high in view that the continent is home to only one-sixth of world population.2 3 Urgent action is needed to address these highly preventable deaths as recent estimates have shown progress in maternal mortality reduction is stagnating.3 Maternal and perinatal mortality are closely linked to poverty.4 5 Providing appropriate, adequate and timely childbirth care to poor women to address these deaths is a major challenge, particularly in rural settings where 59% of SSA population resided in 2020.6
The importance of hospitals in provision of childbirth care in low-resource settings has been raised as part of the Lancet Commission on High-Quality Health Services7 against the background that rising percentages of women giving birth in health facilities have not been paralleled by the expected gains in survival.8 The reason behind the shift to recommend births in hospitals is the limited access to emergency obstetric care in the first, lower level of care (from here on referred to as primary care facilities) coupled with the difficulties of ensuring timely referral.9–12 Though the evidence to recommend hospital care is limited, studies have indicated reduced perinatal morbidity and direct maternal mortality reduce with proximity to hospitals, while the role of primary care facilities in reducing mortality is less certain.13 14
Despite this limited evidence and the debate around the shift away from primary care facilities,15 16 high hospital utilisation generally indicates sufficient accessibility. Good accessibility is important particularly for women with obstetric risk factors, such as those with a high number of previous births. Though high-parity women in different SSA countries are advised to have a hospital birth,17–19 our previous analysis in Tanzania20 21 found high-parity, poor, rural women had low use of hospitals for childbirth.
The objective of this study is to assess the overall use of childbirth care in hospitals in rural SSA with a focus on equality by socioeconomic status and parity. It will contribute to filling a knowledge gap on inequalities within the health system for childbirth. We intend to identify countries which achieved higher utilisation and equality of hospital-based childbirth care among rural women. This knowledge can be used by countries to identify context-specific strategies to reach these higher-risk women.
Methods
Data
We analysed recent Demographic and Health Survey (DHS) data, collected since 2015 and available in March 2022 from low-income and lower middle-income countries in SSA (table 1).22 For countries with more than one DHS in the period examined (Ethiopia and Rwanda), the most recent survey was analysed. Senegal has a continuous DHS; for this analysis, the dataset from 2019 was used.
Table 1.
Background characteristics of countries included in the study (n=18)
| Country | Year DHS | Population*† (millions) | Maternal mortality ratio (maternal deaths/100 000 live births)‡§ | Neonatal mortality rate (Neonatal deaths/1000 live births)‡† | Fertility rate, total (births/woman)*† | Rural population (%)*† | Rural population under national poverty line (%)*§ | Women of childbearing age living ≤2 hours' travel time to a public hospital¶ |
| Angola | 2015 | 27.9 | 251 | 31 | 5.8 | 37 | 32 | 63 |
| Benin | 2017 | 11.2 | 397 | 31 | 4.9 | 53 | 39 | 76 |
| Burundi | 2016 | 10.5 | 558 | 22 | 5.6 | 88 | 65 | 96 |
| Cameroon | 2018 | 25.2 | 529 | 27 | 4.8 | 44 | 38 | 83 |
| Ethiopia | 2019 | 112.1 | 401 | 28 | 4.1 | 79 | 24 | 51 |
| The Gambia | 2019 | 2.3 | 597 | 26 | 5.2 | 38 | 49 | 71 |
| Guinea | 2018 | 12.4 | 576 | 31 | 4.7 | 64 | 44 | 63 |
| Liberia | 2019 | 4.9 | 661 | 31 | 4.2 | 48 | 51 | 62 |
| Malawi | 2015 | 16.3 | 370 | 23 | 4.5 | 84 | 51 | 93 |
| Mali | 2018 | 19.1 | 562 | 33 | 5.9 | 58 | 44 | 65 |
| Nigeria | 2018 | 195.9 | 917 | 36 | 5.4 | 50 | 40 | 92 |
| Rwanda | 2019 | 12.7 | 248 | 18 | 4.0 | 83 | 38 | 89 |
| Senegal | 2019 | 16.3 | 315 | 21 | 4.6 | 52 | 47 | 60 |
| Sierra Leone | 2019 | 7.8 | 1120 | 32 | 4.2 | 58 | 57 | 60 |
| Tanzania | 2015 | 51.5 | 556 | 22 | 5.1 | 68 | 26 | 75** |
| Uganda | 2016 | 39.7 | 381 | 21 | 5.2 | 77 | 21 | 83 |
| Zambia | 2018 | 17.4 | 213 | 25 | 4.6 | 56 | 54 | 60 |
| Zimbabwe | 2015 | 13.8 | 480 | 28 | 3.9 | 68 | 30 | 79 |
*Data from http://data.worldbank.org.
†On year of DHS survey.
‡WHO, UNICEF, UNFPA, World Bank Group and UNPD (MMEIG), available at https://data.unicef.org/resources.
§on year of DHS survey, or closest available estimate.
¶Ouma et al, 2018.
**Only mainland Tanzania (Zanzibar 97.4%).
DHS, Demographic and Health Survey.
Population
All live births to women aged 15–49 residing in rural areas (as defined by DHS) in the surveys’ 5 years recall period were examined; thus, more than one birth per woman could be included. Births of second and third multiples were excluded, as only one decision was made on the location of childbirth. The definition of a cluster or enumeration area as rural in DHS surveys is country specific.23
Main outcome
We examined women’s responses to location of live births. Location was classified into four categories: home, primary care facility, hospital, or private/other. In the DHS surveys of three countries (Burundi, Tanzania, Malawi), it was possible to classify births at faith-based or denominational institutions by level (as hospital or primary care facility). In these countries, faith-based institutions largely function as public health facilities for the purpose of childbirth care; we classified them as such. In the remaining 15 countries, births in the private sector (non-profit and profit) could not be differentiated by level (eg, Liberia DHS, births are categorised as ‘private hospital/polyclinic’) and were classified as private/other. Thus, in these countries, the categories primary care facility and hospital refer to the public/governmental sector only. Classification of facilities in each country is shown in online supplemental table 1.
bmjgh-2023-013029supp002.pdf (1.8MB, pdf)
We created two primary indicators per country: percentage of facility births (the number of rural births in any health facility among all rural births), and percentage of hospital births (rural births in hospitals among all rural births). Additionally, we computed the percentages of all rural births in primary care and in the private sector. The percentage of all rural births by Caesarean section (CS) was also calculated. All percentages were calculated with 95% confidence intervals.
Stratifiers
We used two main stratifiers: household wealth and parity. Wealth was generated based on DHS household wealth score (variable v190a), which allows to differentiate relative wealth among rural households only. Sample size of this analysis (rural hospital births by parity and wealth) was insufficient to analyse data by wealth quintiles. Two equal wealth groups (poorer and wealthier) were generated based on the median wealth score (wealth score<median recoded as poorer 50%, wealth score≥median coded as wealthier 50%), as overall, in this group of countries, the median of population under the national poverty line (online supplemental table 2) was close to half the population (42%).
Parity level at index birth was categorised as 0, 1–4, ≥5 (high parity). We examined the percentage of births in hospital among women at parity 0 and high parity, as the two extremes of parity are associated with greatest risk of complications and are generally advised to give birth in hospital. We also looked at the intersection of these two equality stratifiers. There was no missingness in outcome and stratifier variables. Additional variables used in descriptive analysis were maternal age (at index birth, as a continuous variable), marital status at time of survey (married/cohabiting or non-married or cohabiting) and highest level of maternal education at survey (no formal education, primary, secondary or above).
Statistical analysis
STATA IC V.16 was used for analysis. We accounted for complex survey design using svyset commands to adjust for individual sampling weight, clustering and stratification.
Background characteristics of the rural births in the analysis sample were computed as proportions with 95% CIs, by country. In each country, we examined hospital births by wealth, extremes of parity (parity 0 and parity≥5), and by combinations of wealth and parity. The percent point (pp) differences between poorer and wealthier women at each level of parity (equity gap) were calculated. P values of the differences were computed using logistic regression; p values<0.05 were considered significant. The percentage point difference in hospital use for childbirth by wealthier women at parity 0 and poorer women at high parity (wealthier nullipara-poorer multipara (≥5), ‘WNPM gap’) was computed to assess the combined effect of poverty and high parity on rural hospital use within each country, with the hypothesis that wealthier, nulliparous women have the highest percentage of use of hospitals for childbirth.
Composite usage and equality index
To compare hospital use for childbirth by rural women across countries using the two stratifiers, a composite index was produced. As equality must be assessed together with use, the following four usage and two equality indicators were included in the composite usage and equality (CUE) index. First, facility births’ percentage in rural settings, as a rough proxy of accessibility of the rural health system. Second, hospital births’ percentage as an indication of the accessibility of rural emergency obstetric care. Third, the percentage of all rural births by CS (CS rate), as a crude measure of met obstetric need, assessing whether rural women are reaching appropriate facilities in case of complications (including effective referral between health system levels). Though use of the indicator is controversial,24 an upper threshold of 10%–15% CS at population level is suggested for improved maternal and neonatal outcomes.25 26 In rural contexts, we expected the CS rate to be low; thus, it was included despite its limitations. Fourth, percentage of hospital births among high-parity rural women, a measure of high-parity women’s use of hospitals in the context. Fifth, percentage point difference (equality gap) in hospital utilisation between wealthier and poorer women in rural settings. Sixth, percentage point difference between utilisation of hospitals between wealthier and poorer rural women at parity≥5 (the equality gap in hospital utilisation among rural, high-parity women).
Each indicator was assessed using the median across the included countries, as done previously.27 Quantitative cut-offs of 25% above and below the median were used, to standardise the method used. For each of the six indicators, countries were classified as worse performing (score of 1), just under (2), around (3) and just above the median (4), and best performing (score of 5). For the two equality indicators, lower values correspond to higher performance (less inequality), thus classification as best/better performing were for countries below the median, and worse/worst performing for countries above the median. Countries were ranked based on the CUE index score, which has values between 6 and 30. Countries with higher scores had greater use and equality among rural women, including at high parity.
Sensitivity analysis
On the Tanzania dataset, to examine the significance of the private (non-profit/profit) sector, we carried out a sensitivity analysis. Hospital births by wealth and parity were calculated with and without including private sector births. The difference between equality gaps using only births in public hospitals and public and private hospitals provides some a measure of the significance of the private sector on equality.
Patient and public involvement
Patients and/or the public were not involved in the design, conduct, reporting or dissemination of this research.
Results
Sample description
We analysed 138 977 live births to 96 647 women residing in rural areas from 18 SSA countries (table 2 and online supplemental table 3). A substantial proportion of rural births were to high-parity women, above 20% in all countries except in Zimbabwe, Malawi, Rwanda and Sierra Leone, with a median across countries of 22%. There were differences in women’s educational profile across countries. The percentage of women with secondary education or above was lowest in Guinea (5%) and highest in Zimbabwe (57%), with a median across countries of 16%.
Table 2.
Characteristics of rural women with live births in the surveys’ recall period, across 18 sub-Saharan African countries with a recent DHS survey
| Country | DHS year | Births analysed | Facility births % (95% CI) | Hospital births (% all births) (95% CI) | CS out of all births (95% CI) | Parity at index birth % (95% CI) | Mean maternal age in years at index birth (SD) | % women married/cohabiting (95% CI) | Women with secondary or higher education | |
| 0 | ≥5 | |||||||||
| Angola | 2015 | 6302 | 18.6 (16.0 to 21.6) | 5.7 (4.6 to 7.1) | 1.1 (0.7 to 1.6) | 18.4 (17.2 to 19.6) |
24.2 (22.5 to 26.0) | 26.4 (7.3) | 77.5 (75.5 to 79.4) | 7.8 (6.2 to 9.8) |
| Benin | 2017 | 7979 | 82.0 (79.3 to 84.5) | 14.2 (12.4 to 16.3) | 3.2 (2.8 to 3.8) | 21.0 (20.1 to 22.1) | 20.9 (19.6 to 22.2) | 27.2 (6.7) | 94.3 (93.4 to 95.1) | 10.8 (9.6 to 12.1) |
| Burundi | 2016 | 10 900 | 87.3 (86.1 to 88.4) | 15.3 (13.5 to 17.4) | 3.8 (3.4 to 4.4) | 18.4 (17.6 to 19.2) | 22.9 (21.7 to 24.1) | 28.6 (6.6) | 90.8 (90.0 to 91.5) | 7.3 (6.3 to 8.3) |
| Cameroon | 2018 | 5326 | 49.9 (45.2 to 54.5) | 6.1 (5.0 to 7.4) | 1.6 (1.2 to 2.1) | 18.8 (17.7 to 19.9) | 24.3 (22.6 to 26.0) | 26.1 (6.8) | 87.6 (85.8 to 89.2) | 23.1 (20.6 to 25.9) |
| Ethiopia | 2019 | 4357 | 41.1 (35.0 to 47.5) | 6.0 (4.7 to 7.6) | 3.8 (2.7 to 5.3) | 19.8 (17.6 to 22.3) | 25.9 (23.2 to 29.0) | 26.5 (6.5) | 95.5 (94.2 to 96.6) | 5.9 (4.6 to 7.6) |
| The Gambia | 2019 | 4538 | 76.4 (73.5 to 79.1) | 14.3 (11.2 to 18.1) | 1.5 (1.1 to 1.9) | 18.7 (17.4 to 20.2) | 26.9 (25.1 to 28.9) | 27.7 (6.8) | 96.6 (95.9 to 97.1) | 18.7 (16.4 to 21.3) |
| Guinea | 2018 | 5575 | 39.8 (36.0 to 43.6) | 4.2 (3.4 to 5.1) | 1.4 (1.0 to 1.8) | 17.8 (16.7 to 19.0) | 20.0 (18.4 to 21.7) | 27.2 (7.3) | 96.0 (95.2 to 96.6) | 4.9 (4.0 to 6.1) |
| Liberia | 2019 | 3730 | 76.8 (73.3 to 80.0) | 15.9 (13.7 to 18.3) | 3.7 (2.9 to 4.6) | 20.1 (18.7 to 21.7) | 24.2 (22.2 to 26.4) | 27.4 (7.8) | 75.2 (72.5 to 77.6) | 20.2 (17.6 to 23.1) |
| Malawi | 2015 | 14 232 | 92.3 (91.2 to 93.2) | 29.2 (27.2 to 31.4) | 5.0 (4.6 to 5.6) | 25.1 (24.1 to 26.0) | 15.6 (14.8 to 16.5) | 26.1 (6.8) | 83.4 (82.9 to 84.7) | 14.9 (13.9 to 16.0) |
| Mali | 2018 | 7299 | 60.4 (55.9 to 64.8) | 1.5 (1.1 to 2.1) | 1.7 (1.3 to 2.1) | 17.0 (15.9 to 18.1) | 27.3 (25.5 to 29.3) | 26.9 (7.0) | 97.8 (97.3 to 98.3) | 9.5 (8.0 to 11.2) |
| Nigeria | 2018 | 21 804 | 26.6 (24.9 to 28.3) | 8.2 (7.4 to 9.1) | 1.1 (0.9 to 1.3) | 18.4 (17.7 to 19.1) | 27.1 (26.1 to 28.1) | 27.1 (6.9) | 96.3 (95.8 to 96.7) | 23.6 (22.0 to 25.3) |
| Rwanda | 2019 | 6300 | 93.9 (92.8 to 94.9) | 27.3 (25.5 to 29.2) | 12.7 (11.6 to 13.9) | 24.3 (23.1 to 25.4) | 13.9 (12.8 to 15.0) | 29.7 (6.5) | 83.6 (82.3 to 84.8) | 17.7 (16.1 to 19.5) |
| Senegal | 2019 | 4274 | 71.8 (66.8 to 76.3) | 5.9 (4.8 to 7.2) | 4.3 (3.4 to 5.5) | 21.7 (20.2 to 23.2) | 21.6 (19.9 to 23.5) | 27.5 (6.9) | 96.8 (96.1 to 97.4) | 10.5 (8.9 to 12.2) |
| Sierra Leone | 2019 | 6720 | 80.7 (78.1 to 83.1) | 16.5 (14.1 to 19.2) | 2.7 (1.8 to 4.1) | 20.4 (19.2 to 21.5) | 18.1 (16.7 to 19.5) | 27.4 (7.1) | 88.4 (87.2 to 89.6) | 19.7 (18.0 to 21.5) |
| Tanzania | 2015 | 7699 | 55.7 (52.3 to 58.8) | 21.0 (18.9 to 23-3) | 3.6 (3.0 to 4.2) | 22.6 (21.4 to 23.8) | 23.3 (21.9 to 24.9) | 27.5 (7.2) | 85.2 (83.8 to 86.5) | 8.5 (7.5 to 9.7) |
| Uganda | 2016 | 12 506 | 71.1 (69.0 to 73.1) | 15.9 (14.3 to 17.5) | 4.8 (4.2 to 5.5) | 20.5 (19.6 to 21.4) | 25.5 (24.2 to 26.8) | 26.5 (6.8) | 85.1 (83.9 to 86.1) |
20.5 (18.9 to 22.2) |
| Zambia | 2018 | 6865 | 80.2 (77.7 to 82.5) | 13.7 (12.1 to 15.5) | 2.7 (2.3 to 3.3) | 23.5 (22.4 to 24.6) | 22.8 (21.4 to 24.3) | 26.5 (7.3) | 79.9 (78.4 to 81.4) | 25.5 (23.6 to 27.5) |
| Zimbabwe | 2015 | 3755 | 73.3 (70.0 to 76.4) | 27.2 (28.2 to 34.5) | 3.4 (2.7 to 4.4) | 24.5 (23.0 to 26.0) | 9.6 (8.3 to 11.0) | 26.4 (6.6) | 87.0 (85.4 to 88.5) | 56.5 (53.2 to 60.0) |
| Median | 72.6 | 14.3 | 3.3 | 20.3 | 22.2 | 88.0 | 16.3 | |||
| Lowest value | Highest value | standard deviation (SD) | ||||||||
DHS, Demographic and Health Survey.
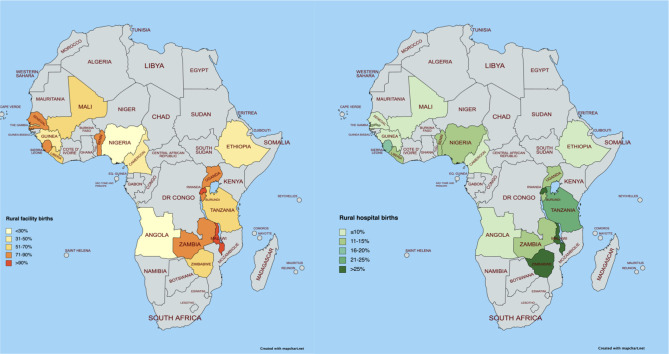
Location of childbirth in rural settings in 18 SSA countries
Overall facility births in rural areas ranged between 19% and 94% across countries with a median of 73% (figure 1 A and table 2, full table in online supplemental table 3). Hospital births in rural areas varied considerably across countries, ranging from 2% in Mali to 29% in Malawi, with a median of 14% (figure 1B). Median of births in primary care facilities was 55%, ranging from 11% in Angola to 65% in Burundi. Online supplemental fi gure 1 shows the distribution of births by level of health facility across countries.
Figure 1.
A - percentage of facility births, B - percentage of hospital births, among women with a live birth in the surveys’ recall period in rural settings of 18 SSA countries with a recent DHS survey.
bmjgh-2023-013029supp001.pdf (1.1MB, pdf)
Hospital use for childbirth in rural areas by wealth and parity stratifiers
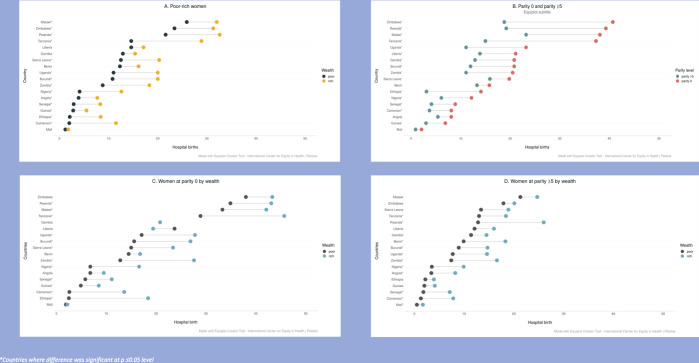
In rural areas of all countries (online supplemental table 4 and figure 2), wealthier women used hospitals for childbirth more than poorer ones (figure 2A), although in four countries the difference was not statistically significant (Benin, the Gambia, Liberia, Mali). Rural Tanzania had the largest percentage point difference between wealthier and poorer women’s use of hospitals. Hospital births were also higher at first birth than at parity 5+ in all countries (figure 2B), although the difference was not significant in Mali, Angola and Benin. Largest inequalities between the two extremes of parity were seen in countries with relatively high utilisation of hospital for births (Malawi, Rwanda, Zimbabwe, Tanzania).
Figure 2.
Equiplots of hospital births in rural settings of 18 SSA countries with a recent DHS survey, by: A. wealth among all women, B. parity (0 and high parity ≥5), C. wealth among women at parity 0, D. wealth among women at high parity (≥5).
Examining wealth and parity together, in nulliparous rural women hospital births were significantly higher among wealthier women, except in the Gambia, Liberia and Mali. In wealthier nulliparous women, they ranged between 2% in Mali to 45% in Tanzania (median 20%), while in nulliparous women from poorer households, they ranged from 2% in Mali to 38% in Zimbabwe (median 15%). The percentage point difference among nulliparous rural women’s use of hospitals for childbirth between poorer and wealthier women ranged from −4pp (pro-poor) in Liberia to 17pp in Tanzania (figure 2).
Among rural women at high parity (figure 2), hospital use ranged from 1% in Mali to 21% in Malawi among those from poorer households, and from 2% in Mali to 26% in Rwanda among women from wealthier households. The percentage point difference between poorer and wealthier women at high-parity women was greatest in Rwanda (13pp).
Overall, hospital use was much lower in high-parity women than in those at first birth in all countries, except in those with very low overall use of hospitals (Mali, Angola). The gap in use of hospitals for childbirth among rural women between poorer multipara (≥5) compared with wealthier nullipara (WNPM gap) was generally large, with a median of 15pp. The largest gap was in Tanzania (33pp) and Rwanda (30pp). The exception was Mali, with very low utilisation of facility and hospital births in all wealth/parity groups in rural areas, and therefore no substantive differences between them.
Equality analysis using CUE index
Using indicators detailed in table 2 (facility births, hospital births, CS rate) and online supplemental table 3 (hospital births at high parity, pp difference between wealthier and poorer women and pp difference between wealthier and poorer women at parity≥5), we constructed table 3, summarising the six indicators used for the CUE index. Cells were colour coded, according to relative performance in five predefined categories relative to the median values in this group of countries.
Table 3.
Heatmap showing scores for six indicators of composite usage and equality of obstetric services in rural areas in countries with a recent Demographic and Health Survey, used to calculate a composite usage and equality (CUE) index, by country
| Country | Percentage rural facility births | Percentage rural hospital births | Percentage CS in rural women | Percentage of hospital births in rural women at high parity | Percentage point difference between wealthier and poorer women | Percentage point difference between wealthier and poorer women at high parity | CUE score | |
| Malawi | 92.3 | 29.5 | 5.2 | 23.4 | 6.2 | 3.3 | 29 | |
| Liberia | 76.9 | 16.4 | 4.0 | 14.4 | 2.5 | 3.9 | 25 | |
| Zimbabwe | 73.6 | 27.2 | 3.7 | 19.1 | 7.8 | 2.2 | 23 | |
| Gambia | 76.6 | 14.4 | 1.6 | 13.0 | 2.5 | 3.1 | 22 | |
| Rwanda | 93.9 | 27.7 | 12.8 | 20.5 | 10.9 | 13.2 | 22 | |
| Benin | 82.2 | 14.4 | 3.4 | 13.5 | 3.8 | 8.5 | 20 | |
| Sierra Leone | 80.7 | 16.5 | 2.9 | 15.8 | 7.8 | 5.5 | 20 | |
| Tanzania | 55.6 | 21.0 | 3.7 | 14.7 | 14.4 | 4.5 | 20 | |
| Burundi | 87.3 | 15.5 | 3.9 | 12.1 | 9.1 | 5.7 | 18 | |
| Senegal | 71.9 | 6.0 | 4.5 | 4.1 | 5.5 | 5.3 | 17 | |
| Uganda | 71.1 | 16.0 | 4.9 | 11.3 | 9.0 | 7.0 | 16 | |
| Mali | 60.6 | 1.5 | 1.7 | 1.0 | 0.7 | 1.3 | 15 | |
| Ethiopia | 41.3 | 6.2 | 4.0 | 3.4 | 6.3 | 1.7 | 15 | |
| Guinea | 40.2 | 4.3 | 1.4 | 3.0 | 2.7 | 2.1 | 14 | |
| Angola | 18.6 | 5.7 | 1.1 | 5.2 | 3.8 | 4.9 | 12 | |
| Zambia | 80.2 | 13.9 | 2.9 | 11.2 | 9.4 | 9.2 | 12 | |
| Nigeria | 26.8 | 8.4 | 1.2 | 6.2 | 8.5 | 6.4 | 8 | |
| Cameroon | 50.0 | 6.2 | 1.7 | 3.9 | 9.5 | 6.5 | 6 | |
| Median | 72.7 | 14.4 | 3.5 | 11.7 | 7.0 | 5.1 | ||
| Best performing (score 5) | ||||||||
| Performance ≤25% above median (score 4) | ||||||||
| Performance at median (score 3) | ||||||||
| Performance≤25% below median (score 2) | ||||||||
| Worst performing (score 1) | ||||||||
Countries are ordered by decreasing ranking of the CUE index score.
CS, births by ceaserean section.
From the CUE score, (median 18, range 6–29), Malawi and Liberia were the countries with higher use and equality of rural hospitals for childbirth among high-parity women followed by Zimbabwe, Rwanda and the Gambia. Among countries with the highest CUE score, Malawi had the highest score in all indicators except the pp difference in hospital use between wealthier and poorer. Liberia, though scoring just above the median for most indicators, had a small pp difference in hospital use between wealthier and poorer women. Rwanda had high scores for all indicators, including percentage of rural births by CS, but with large equality gaps.
Births in the private sector were not homogeneous across countries, ranging between 1% (Sierra Leone)—15% (Cameroon and Uganda), median 4%. From a sensitivity analysis on the Tanzanian dataset, we found all the equality gaps were greater when faith-based hospitals were included in the numerators (online supplemental table 5).
Discussion
Using recent nationally representative data, we analysed 138 977 live births across 18 African countries, focusing on hospital use for childbirth in rural areas. Across these countries, we found that use of hospitals was low ranging between 2% and 29% of all births. In all countries, rural women from poorer households used hospitals less than wealthier ones, and high-parity women used hospitals less compared with those having their first baby. Poorer women at high parity had very limited hospital use, ranging between 1% in Mali and 21% in Malawi. In this comparative analysis, we identified Malawi and Liberia, followed by Zimbabwe, the Gambia and Rwanda, as countries with greater use and equality of hospitals for childbirth among rural women, particularly at high parity.
Lower use of hospitals by rural women
Our analysis needs to be viewed against the background that there is no established benchmark on an optimal proportion of hospital births in low-income countries.8 28 In all countries, only a minority of rural women reported having given birth in hospitals. In the countries with higher scores, 25%–30% of rural births were in hospitals (Malawi, Zimbabwe and Rwanda). The lowest use was seen in Mali (2%) and Guinea (4%). As positive examples in our analysis, Rwanda, with an adequate percentage of CS among rural births (12.7%) and where international estimates confirm remarkable progress in maternal mortality reduction,29 approximately a quarter of births were in hospitals, and Malawi, the second highest percentage of rural births by CS (5%) and substantial progress in neonatal survival,30 approximately 3 out of 10 rural births were in a hospital. In most countries, use of hospitals by rural women was very low, suggesting that access to life-saving procedures in rural settings was insufficient.
Disparities by wealth and parity
A second key finding is that in all 18 countries, rural women from poorer households used hospitals significantly less than those from wealthier households. Furthermore, the effect of poverty was aggravated by high parity. This means that poorer, high-parity women were the subgroup that used hospitals least, expanding our previous findings from Tanzania.20 21 Socioeconomic inequality among high-parity women was larger in countries where rural hospital use was greater, such as Benin, Rwanda and Zambia. In addition, the WNPM gap was larger in countries with higher hospital use. Where overall hospital use was low, like in Guinea and Mali, all women used them very little.
Among all countries, Rwanda had high use of hospitals for childbirth at both extremes of parity, but the equality gap at high parity was large at 13%. In Africa, inequities in skilled birth attendance31—often equated to a facility birth32—have been described. Our study highlights a socioeconomic inequality in the process of care,33 affecting women of high parity. Our study was not designed to systematically investigate reasons for lower use of hospitals. Commonly reported reasons are: geographical accessibility,34 costs,35 worsened in rural contexts, disrespect and abuse.36–39 Women’s preferences in childbirth care are particularly important in rural settings and among multiparous women.40
Nonetheless, low use of hospitals for childbirth by poor rural women particularly at high parity in SSA is concerning. First, women at high parity face higher risk of complications, including anaemia, haemorrhage, malpresentation, placenta previa, obstructed labour and uterine rupture,41–44 leading to higher maternal mortality.45 Similarly, the risk of newborn morbidity and perinatal death among high-parity women are higher.43 44 46–48 Thus, women among whom poverty, rurality and obstetric risk intersect, are not accessing appropriate care for the management of complications. Second, the already limited use of higher-level care by this group must be taken into consideration in the present debate on centralization of childbirth care.7 9
Countries which have achieved greater utilisation and equality for rural women
We compared countries using the CUE index to detail inequality in provision of care. Our analysis indicated that Malawi and Liberia had the highest CUE index, closely followed by Zimbabwe, the Gambia and Rwanda. The higher-ranking countries in this analysis are a good example of what can be achieved in the specific context of rural SSA. Further analysis will be needed to explore why some countries had greater use and equality than others and may assess aspects of national commitment, financial measures, ensuring geographical accessibility, linking communities and health facilities, and ensuring respectful maternity care in hospitals.
For example, we found a strong national commitment to reach all women with appropriate care in countries scoring high in the CUE index. The importance of political leadership has been underlined in Rwanda,29 Malawi49 50 and Liberia.51 In Nigeria, on the other hand, where individual states, with differences in income and political will,52 are responsible for primary care delivery, lack of federal government coordination weakened efforts to universal healthcare. In countries high in the CUE index, such as Zimbabwe and Rwanda, multisectoral policies have improved female education, resulting in women’s greater agency in the obstetric continuum.
Reduction of financial barriers may be another important facilitator. Most countries in the top half of the CUE index had abolished user fees for maternity services.53 Examples of removal of economic barriers despite user fees come from Rwanda, where enrolment into Community-based Health Insurance (Mutuelles de Santè) is mandatory and includes exemptions for the poorest,54 and from Benin and Mali, where CS fee exemptions have improved access.55 In Zimbabwe, performance-based financing schemes enabled hospitals to provide assistance to poor women.56
Among countries ranking in the top half of the CUE index were nations with good accessibility to public hospitals such as Malawi, Burundi, Rwanda and Uganda.34 Other countries had established clear measures to improve geographical accessibility. For example, in Liberia, maternity waiting homes (MWH) have been scaled up nationally.57 Similarly, Tanzania and Malawi invested into MWH, and there is evidence they are preferentially used by poorer women.58 59 In Zimbabwe, there is a national policy supporting referral readiness from the nearby facility to a hospital.60 In Ethiopia, with low geographical accessibility and a very difficult terrain, a distinct referral and ambulance approach targeting women living far from health facilities was installed.61
Several of the countries with higher scores have invested into strategies to link communities and facilities, such as Malawi50 and Rwanda.29 62 In Liberia, a national salaried Community Health Assistant programme was established in 2016, focusing on communities living remotely with evidence suggesting the programme had an impact on access barriers.63 Rwanda has invested into salaried community health workers further incentivised by performance-based financing,62 with a female cadre providing maternal and newborn preventive services in villages, linking communities to facilities.29 In Ethiopia, where home births are culturally embedded and CUE ranking was low, health extension workers may improve women’s access to the maternal continuum of care.64
Efforts to improve women’s experience of care were seen in Liberia. Lack of respectful maternity care disproportionately affects poorer women,65 is more common in hospitals,66 and high-parity women who have experienced disrespect in previous births are likely to prefer a home birth. In Liberia, trained traditional midwives are included in national policy,51 facilitate use of MWH in rural settings and can successfully collaborate with skilled birth attendants.67 The strong trust women and communities have towards traditional birth attendants is an opportunity in countries such as Nigeria, where home births are common, to integrate community-based providers into formal health services.68 69
A high CUE index for rural settings does not ensure averting preventable maternal and newborn mortality without high-quality health services. Some countries—Liberia, the Gambia, Sierra Leone—with a high CUE index had high maternal mortality ratios,30 while countries with lower maternal mortality ratios—such as Angola and Zambia—had low ranking. Our results are largely concordant with those of a recent study of wealth-based inequality in the maternal care continuum in SSA.70
Countries included in this analysis comprise very different contexts, thus there is no one size fits all model of care. Further qualitative and mixed-methods studies are required to understand drivers of low use among rural, poor, high-parity women in each country. Women’s involvement in identifying context-specific solutions, taking into account their choice and preferences,40 is needed. Our analysis highlights the need to focus on women who are poor, rural and at high parity to leave no one behind.
Strengths and limitations
The main strength of this study is the use of population-based data to study births among rural poor women across a range of countries in SSA. The study focuses on rural poor at high parity, a substantial higher-risk group that has received limited attention.
There are limitations that should be considered in interpreting the results. Countries without a recent survey were excluded, and countries were compared at different times within the selected time frame. Similarly to other studies on rural disparities in health outcomes,71 72 we used the DHS definitions of rural cluster, which are based on country-specific definition.23 We acknowledge that the current lack of a standard definition of rural in DHS may at least partly impair comparison of hospital use across countries.73 Limitations linked to DHS surveys have been reported in detail.74 Among these, there is recall bias and that women with a stillbirth could not be included, as the DHS programme includes only women with live births. We categorised the variable place of childbirth into hospitals and primary-level facilities, based on country specific definitions. There is no consensus on the definition of hospital and national definitions are often inadequate.34 It is possible that the hospital category includes facilities where the full range of management of obstetric complications was not available. Obstetric capacity at primary level varies between and within countries, and some countries, such as Tanzania and Ethiopia, have expanded CS availability at health centre level.75 76 This misclassification may have attenuated the equality gap we describe in these countries. Births in private sector hospitals could not be included in the analysis, and it was possible to include faith-based facility births only in 3/18 countries. From the sensitivity analysis on the Tanzania dataset, it is possible that the equality gaps reported underestimate the actual gaps. Women were divided in two wealth groups only (wealthier and poorer), as limited hospital use did not allow further subdivision, thus more detailed variation by level of wealth could not be studied.
For relative performance of countries in this analysis, we used a simple index (CUE), which included health system indicators. While we believe it is useful to compare countries, we acknowledge it is a rough tool that allows to identify countries with greater use and equality but does not have a solid statistical base. In addition, there were considerable differences across countries which the index could not capture. For example, accessibility of hospitals in a densely populated country such as Rwanda is difficult to compare to sparsely populated rural areas of Tanzania or Ethiopia. Differences in health system organisation also challenge more detailed comparisons.
Conclusion
This comparative analysis of 18 SSA countries found that a minority of rural women used hospitals for childbirth. In all countries, poorer women had lower use compared with wealthier ones, and high-parity women had lower use compared with those having their first baby. This double burden of inequality resulted in lowest use of hospitals among rural women who were poorer and high parity, despite their higher risk of negative outcomes.
Using a simple innovative composite index, we found that Malawi and Liberia and achieved greater use and equality of hospitals for childbirth care among rural women and are a positive example of what can be achieved in the context of rural SSA.
Acknowledgments
Our thanks go firstly to women from these 18 countries who agreed to be interviewed during the surveys, to the interviewers, and to the DHS program. The latter kindly provided access to the databases for analysis. Dr Clément Nshirimana provided useful advice on the health system in Burundi. We used the equiplot creator tool for Figure 2, kindly made available online by the International Centre for Equity in Health Universidade Federal de Pelotas, Pelotas, Brazil.Mapchart (www.mapchart.net) provided software used for figure 1.
Footnotes
Handling editor: Seema Biswas
Twitter: @manuelastraneo, @Coolgynae, @AntenehAsef, @lenkabenova
Contributors: MS contributed to the study design, led data analysis and visualisation, drafted the manuscript and the revisions. MS, LB, CH and TvdA conceptualised the study. LB supervised analysis and the overall study. CH contributed to interpretation and revisions of the manuscript. All authors provided intellectual contributions to the study and critically commented on the manuscript. MS is the guarantor of the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data may be obtained from a third party and are not publicly available. Data from the DHS are available for research purposes, upon registration, at www.dhsprogram.com.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by ICF Institutional Review Board (https://www.dhsprogram.com/methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm). Demographic and Health Surveys receive government permission, use informed consent, and assure respondents of confidentiality. They are ethically approved by the DHS review board. We obtained permission to use the datasets from the DHS programme. Participants gave informed consent to participate in the study before taking part.
References
- 1. United Nations . Sustainable Development Goals 2021, Available: https://unsdg.un.org/ [Accessed 5 Nov 2021].
- 2. UNICEF . Data by topic and country no date, Available: https://data.unicef.org/resources/
- 3. WHO . Trends in maternal mortality 2000-2020: estimates by WHO, UNICEF, UNFPA, World Bank Group and UNDESA/Population Division. Geneva: World Health Organization, 2023. [Google Scholar]
- 4. Houweling TAJ, Ronsmans C, Campbell OMR, et al. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ 2007;85:745–54. 10.2471/blt.06.038588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Black R, Laxminarayan R, Temmerman M, et al. Reproductive, maternal, newborn, and child health: disease control priorities. In: Black RE, Laxminarayan R, Temmerman M, eds. Levels and Causes of Maternal Mortality and Morbidity. The International Bank for Reconstruction and Development / The World Bank (c) 2016 International Bank for Reconstruction and Development / The World Bank: Washington (DC), 11 April 2016. 10.1596/978-1-4648-0348-2 [DOI] [Google Scholar]
- 6. World Bank . 2021. Available: https://data.worldbank.org [Accessed 3 Nov 2021].
- 7. Kruk ME, Gage AD, Arsenault C, et al. The Lancet Global Health Commission High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Campbell OMR, Calvert C, Testa A, et al. Series maternal health 3 the scale, scope, coverage, and capability of childbirth care. The Lancet 2016;6736:1–16. [DOI] [PubMed] [Google Scholar]
- 9. Hanson C, Schellenberg J. Redesigning maternal health services: is centralisation the answer in low-resource settings? BMJ Glob Health 2019;4:e001488. 10.1136/bmjgh-2019-001488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Virgo S, Gon G, Cavallaro FL, et al. Who delivers where? the effect of obstetric risk on facility delivery in East Africa. Trop Med Int Health 2017;22:1081–98. 10.1111/tmi.12910 [DOI] [PubMed] [Google Scholar]
- 11. Hanson C, Munjanja S, Binagwaho A, et al. National policies and care provision in pregnancy and childbirth for twins in Eastern and Southern Africa: A mixed-methods multi-country study. PLoS Med 2019;16:e1002749. 10.1371/journal.pmed.1002749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Monden CWS, Smits J. Mortality among twins and Singletons in sub-Saharan Africa between 1995 and 2014: a pooled analysis of data from 90 demographic and health surveys in 30 countries. Lancet Glob Health 2017;5:e673–9. 10.1016/S2214-109X(17)30197-3 [DOI] [PubMed] [Google Scholar]
- 13. Hanson C, Cox J, Mbaruku G, et al. Maternal mortality and distance to facility-based obstetric care in rural Southern Tanzania: a secondary analysis of cross-sectional census data in 226 000 households. The Lancet Global Health 2015;3:e387–95. 10.1016/S2214-109X(15)00048-0 [DOI] [PubMed] [Google Scholar]
- 14. Gabrysch S, Nesbitt RC, Schoeps A, et al. Does facility birth reduce maternal and perinatal mortality in Brong Ahafo, Ghana? A secondary analysis using data on 119 244 pregnancies from two cluster-randomised controlled trials. Lancet Glob Health 2019;7:e1074–87. 10.1016/S2214-109X(19)30165-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Roder-DeWan S, Nimako K, Twum-Danso NAY, et al. Health system redesign for maternal and newborn survival: Rethinking care models to close the global equity gap. BMJ Glob Health 2020;5:e002539. 10.1136/bmjgh-2020-002539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hanson C, Waiswa P, Pembe A, et al. Health system redesign for equity in maternal and newborn health must be Codesigned, country led, adapted to context and fit for purpose. BMJ Glob Health 2020;5:e003748. 10.1136/bmjgh-2020-003748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. MoHSW . Reproductive and child health card number 4 (RCHC-4). Dar es Salaam: Ministry of health and social welfare, the United Republic of Tanzania; 2006.
- 18. Ministry of Health . Department; Rach, editor. Kampala, Uganda2022. In: Essential Maternal and Newborn Clinical Care Guidelines for Uganda. [Google Scholar]
- 19. Republic of Zambia, Ministry of Health . Zambia National Maternal and neonatal Referral Guidelines; 2018. www.moh.gov.zm,
- 20. Straneo M, Benova L, Hanson C, et al. Inequity in uptake of hospital-based childbirth care in rural Tanzania: analysis of the 2015-16 Tanzania demographic and health survey. Health Policy Plan 2021;36:1428–40. 10.1093/heapol/czab079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Straneo M, Beňová L, van den Akker T, et al. No increase in use of hospitals for childbirth in Tanzania over 25 years: accumulation of inequity among poor, rural, high parity women. PLOS Glob Public Health 2022;2:e0000345. 10.1371/journal.pgph.0000345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. DHS program . The DHS program. n.d. Available: https://dhsprogram.com/
- 23. Croft TN, Marshall AMJ, Allen CK, et al. Guide to DHS Statistics DHS-7. Rockville, Maryland, USA: ICF, 2018. [Google Scholar]
- 24. Ronsmans C, Campbell OMR, McDermott J, et al. Questioning the indicators of need for obstetric care. Bull World Health Organ 2002;80:317–24. [PMC free article] [PubMed] [Google Scholar]
- 25. Ye J, Zhang J, Mikolajczyk R, et al. Association between rates of Caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG 2016;123:745–53. 10.1111/1471-0528.13592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Betran AP, Torloni MR, Zhang JJ, et al. WHO working group on Caesarean section. WHO Statement on Caesarean Section Rates BJOG 2016;123:667–70. 10.1111/1471-0528.13526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wong KL, Banke-Thomas A, Sholkamy H, et al. Tale of 22 cities: utilisation patterns and content of maternal care in large African cities. BMJ Glob Health 2022;7:e007803. 10.1136/bmjgh-2021-007803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Boerma T, Campbell OMR, Amouzou A, et al. Maternal mortality, stillbirths, and neonatal mortality: a transition model based on analyses of 151 countries. Lancet Glob Health 2023;11:e1024–31. 10.1016/S2214-109X(23)00195-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ministry of Health Rwanda, PMNCH, WHO . Success factors for women’s and children’s health: Rwanda. Geneva: World Health Organization, 2015. [Google Scholar]
- 30. UNICEF data by topic and country . 2023. Available: https://data.unicef.org/countdown-2030/country
- 31. Ogundele OJ, Pavlova M, Groot W. Socioeconomic inequalities in reproductive health care services across sub-Saharan Africa. A systematic review and meta-analysis. Sex Reprod Healthc 2020;25:100536.:S1877-5756(20)30174-9. 10.1016/j.srhc.2020.100536 [DOI] [PubMed] [Google Scholar]
- 32. Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy Childbirth 2009;9:34. 10.1186/1471-2393-9-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rodney AM, Hill PS. Achieving equity within universal health coverage: a narrative review of progress and resources for measuring success. Int J Equity Health 2014;13:72. 10.1186/s12939-014-0072-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ouma PO, Maina J, Thuranira PN, et al. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a Geocoded inventory and spatial analysis. Lancet Glob Health 2018;6:e342–50. 10.1016/S2214-109X(17)30488-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wong KL, Brady OJ, Campbell OMR, et al. Current realities versus theoretical optima: Quantifying efficiency and sociospatial equity of travel time to hospitals in low-income and middle-income countries. BMJ Glob Health 2019;4:e001552. 10.1136/bmjgh-2019-001552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bohren MA, Vogel JP, Hunter EC, et al. The Mistreatment of women during childbirth in health facilities globally: A mixed-methods systematic review. PLoS Med 2015;12;e1001847. 10.1371/journal.pmed.1001847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kanengoni B, Andajani-Sutjahjo S, Holroyd E. Women’s experiences of disrespectful and abusive maternal health care in a low resource rural setting in Eastern Zimbabwe. Midwifery 2019;76:125–31. 10.1016/j.midw.2019.06.003 [DOI] [PubMed] [Google Scholar]
- 38. White Ribbon Alliance . Respectful maternity care: the universal rights of childbearing women. 2011, Washington, DC,
- 39. Ishola F, Owolabi O, Filippi V. Disrespect and abuse of women during childbirth in Nigeria: A systematic review. PLoS One 2017;12:e0174084. 10.1371/journal.pone.0174084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Fantaye AW, Gunawardena N, Yaya S. Preferences for formal and traditional sources of childbirth and postnatal care among women in rural Africa: A systematic review. PLoS One 2019;14:e0222110. 10.1371/journal.pone.0222110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Solomons B. The dangerous Multipara. The Lancet 1934;224:8–11. 10.1016/S0140-6736(00)90086-2 [DOI] [Google Scholar]
- 42. Mgaya AH, Massawe SN, Kidanto HL, et al. Grand Multiparity: is it still a risk in pregnancy BMC Pregnancy Childbirth 2013;13:241. 10.1186/1471-2393-13-241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Teguete I, Maiga AW, Leppert PC. Maternal and neonatal outcomes of grand Multiparas over two decades in Mali. Acta Obstet Gynecol Scand 2012;91:580–6. 10.1111/j.1600-0412.2012.01372.x [DOI] [PubMed] [Google Scholar]
- 44. Agrawal S, Agarwal A, Das V. Impact of Grandmultiparity on obstetric outcome in low resource setting. J Obstet Gynaecol Res 2011;37:1015–9. 10.1111/j.1447-0756.2010.01476.x [DOI] [PubMed] [Google Scholar]
- 45. Ezegwui H, Onoh R, Ikeako L, et al. Investigating maternal mortality in a public teaching hospital, Abakaliki, Ebonyi state, Nigeria. Ann Med Health Sci Res 2013;3:75–80. 10.4103/2141-9248.109511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Muniro Z, Tarimo CS, Mahande MJ, et al. Grand Multiparity as a Predictor of adverse pregnancy outcome among women who delivered at a tertiary hospital in northern Tanzania. BMC Pregnancy Childbirth 2019;19:222. 10.1186/s12884-019-2377-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Kamala BA, Mgaya AH, Ngarina MM, et al. Predictors of low birth weight and 24-hour perinatal outcomes at Muhimbili national hospital in Dar es Salaam, Tanzania: a five-year retrospective analysis of obstetric records. Pan Afr Med J 2018;29:220. 10.11604/pamj.2018.29.220.15247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Bai J, Wong FWS, Bauman A, et al. Parity and pregnancy outcomes. Am J Obstet Gynecol 2002;186:274–8. 10.1067/mob.2002.119639 [DOI] [PubMed] [Google Scholar]
- 49. Montagu D, Sudhinaraset M, Diamond-Smith N, et al. Where women go to deliver: understanding the changing landscape of childbirth in Africa and Asia. Health Policy Plan 2017;32:1146–52. 10.1093/heapol/czx060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zimba E, Kinney MV, Kachale F, et al. Newborn survival in Malawi: a decade of change and future implications. Health Policy Plan 2012;27 Suppl 3:iii88–103. 10.1093/heapol/czs043 [DOI] [PubMed] [Google Scholar]
- 51. Republic of Liberia, Ministry of health and social welfare . National-health-policy-plan-MOH-2011-2021; 2011.
- 52. Nigeria Federal Ministry of Health . Nigeria national health policy final; 2017.
- 53. Yates R. Universal health care and the removal of user fees. Lancet 2009;373:2078–81. 10.1016/S0140-6736(09)60258-0 [DOI] [PubMed] [Google Scholar]
- 54. Koch R, Nkurunziza T, Rudolfson N, et al. Does community-based health insurance protect women from financial catastrophe after cesarean section? A prospective study from a rural hospital in Rwanda. BMC Health Serv Res 2022;22:717. 10.1186/s12913-022-08101-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ravit M, Audibert M, Ridde V, et al. Removing user fees to improve access to Caesarean delivery: a quasi-experimental evaluation in Western Africa. BMJ Glob Health 2018;3:e000558. 10.1136/bmjgh-2017-000558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. World Bank . Zimbabwe-impact-evaluation-overview-report; 2016.
- 57. Lori JR, Perosky JE, Rominski S, et al. Maternity waiting homes in Liberia: results of a countrywide multi-sector scale-up. PLoS ONE 2020;15:e0234785. 10.1371/journal.pone.0234785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Fogliati P, Straneo M, Mangi S, et al. A new use for an old tool: maternity waiting homes to improve equity in rural childbirth care. results from a cross-sectional hospital and community survey in Tanzania. Health Policy Plan 2017;32:1354–60. 10.1093/heapol/czx100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Singh K, Speizer I, Kim ET, et al. Reaching vulnerable women through maternity waiting homes in Malawi. Intl J Gynecology & Obste 2017;136:91–7. 10.1002/ijgo.12013 Available: https://obgyn.onlinelibrary.wiley.com/toc/18793479/136/1 [DOI] [PubMed] [Google Scholar]
- 60. Zimbabwe Ministry of Health and Childcare . The national health strategy for Zimbabwe 2016 - 2020 equity and quality in health: leaving no one behind; 2016.
- 61. Selbana DW, Derese M, Sewmehone Endalew E, et al. A culturally sensitive and supportive maternity care service increases the uptake of maternity waiting homes in Ethiopia. Int J Womens Health 2020;12:813–21. 10.2147/IJWH.S268245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Farmer PE, Nutt CT, Wagner CM, et al. Reduced premature mortality in Rwanda: lessons from success. BMJ 2013;346:f65. 10.1136/bmj.f65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Luckow PW, Kenny A, White E, et al. Implementation research on community health workers' provision of maternal and child health services in rural Liberia. Bull World Health Organ 2017;95:113–20. 10.2471/BLT.16.175513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Jackson R, Hailemariam A. The role of health extension workers in linking pregnant women with health facilities for delivery in rural and Pastoralist areas of Ethiopia. Ethiop J Health Sci 2016;26:471–8. 10.4314/ejhs.v26i5.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Afulani PA, Kelly AM, Buback L, et al. Providers' perceptions of disrespect and abuse during childbirth: a mixed-methods study in Kenya. Health Policy Plan 2020;35:577–86. 10.1093/heapol/czaa009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Mocumbi S, Högberg U, Lampa E, et al. Mothers' satisfaction with care during facility-based childbirth: a cross-sectional survey in Southern Mozambique. BMC Pregnancy Childbirth 2019;19:303. 10.1186/s12884-019-2449-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lori JR, Munro ML, Moore JE, et al. Lessons learned in Liberia: preliminary examination of the Psychometric properties of trust and teamwork among maternal Healthcare workers. BMC Health Serv Res 2013;13. 10.1186/1472-6963-13-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Abubakar I, Dalglish SL, Angell B, et al. The Lancet Nigeria Commission: investing in health and the future of the nation. Lancet 2022;399:1155–200. 10.1016/S0140-6736(21)02488-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nguenda Anya SB, Yene A. The determinants of the choice of treatment of pregnant women in Cameroon. Health Econ Rev 2016;6:48. 10.1186/s13561-016-0127-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Asefa A, Gebremedhin S, Marthias T, et al. Wealth-based inequality in the continuum of maternal health service utilisation in 16 sub-Saharan African countries. Int J Equity Health 2023;22:203. 10.1186/s12939-023-02015-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Yaya S, Uthman OA, Okonofua F, et al. Decomposing the rural-urban gap in the factors of under-five mortality in sub-Saharan Africa? evidence from 35 countries. BMC Public Health 2019;19:616. 10.1186/s12889-019-6940-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Norris M, Klabbers G, Pembe AB, et al. A growing disadvantage of being born in an urban area? analysing urban-rural disparities in neonatal mortality in 21 African countries with a focus on Tanzania. BMJ Glob Health 2022;7:e007544. 10.1136/bmjgh-2021-007544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Fish TD, Janocha B, Dontamsetti T, et al. Geospatial Covariates: Proxies for Mapping Urban-Related Indicators.DHS Spatial Analysis Reports no.19. Rockville, Maryland, USA: ICF, 2020. [Google Scholar]
- 74. Benova L, Dennis ML, Lange IL, et al. Two decades of Antenatal and delivery care in Uganda: a cross-sectional study using demographic and health surveys. BMC Health Serv Res 2018;18:758. 10.1186/s12913-018-3546-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Nyamtema AS, Mwakatundu N, Dominico S, et al. Enhancing maternal and perinatal health in under-served remote areas in sub-Saharan Africa: A Tanzanian model. PLoS One 2016;11:e0151419. 10.1371/journal.pone.0151419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Gessessew A, Barnabas GA, Prata N, et al. Task shifting and sharing in Tigray, Ethiopia, to achieve comprehensive emergency obstetric care. Int J Gynaecol Obstet 2011;113:28–31. 10.1016/j.ijgo.2010.10.023 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-013029supp002.pdf (1.8MB, pdf)
bmjgh-2023-013029supp001.pdf (1.1MB, pdf)
Data Availability Statement
Data may be obtained from a third party and are not publicly available. Data from the DHS are available for research purposes, upon registration, at www.dhsprogram.com.