Abstract
As the global population ages, the prevalence of Parkinson’s disease (PD) is steadily on the rise. PD demonstrates chronic and progressive characteristics, and many cases can transition into dementia. This increases societal and economic burdens, emphasizing the need to find effective treatments. Among the widely recognized causes of PD is the abnormal accumulation of proteins, and autophagy dysfunction accelerates this accumulation. The resultant Lewy bodies are also commonly found in Alzheimer’s disease patients, suggesting an increased potential for the onset of dementia. Additionally, the production of free radicals due to mitochondrial dysfunction contributes to neuronal damage and degeneration. The activation of astrocytes and the M1 phenotype of microglia promote damage to dopamine neurons. The drugs currently used for PD only delay the clinical progression and exacerbation of the disease without targeting its root cause, and come with various side effects. Thus, there is a demand for treatments with fewer side effects, with much potential offered by natural products. In this study, we reviewed a total of 14 articles related to herbal medicines and natural products and investigated their relevance to possible PD treatment. The results showed that the reviewed herbal medicines and natural products are effective against lysosomal disorder, mitochondrial dysfunction, and inflammation, key mechanisms underlying PD. Therefore, natural products and herbal medicines can reduce neurotoxicity and might improve both motor and non-motor symptoms associated with PD. Furthermore, these products, with their multi-target effects, enhance bioavailability, inhibit antibiotic resistance, and might additionally eliminate side effects, making them good alternative therapies for PD treatment.
Keywords: Parkinson’s disease, natural products, alpha synuclein, neuroinflammation, oxidative stress, mitochondrial dysfunction, neurodegeneration
1. Introduction
Parkinson’s Disease (PD) is the second most common neurodegenerative disease worldwide [1]. The incidence rate of PD in women shows an increasing trend from 2.94 per 100,000 persons in the age group 40–49 years to a peak of 104.99 per 100,000 between 70–79 years, which then declines to 66.02 per 100,000 in those aged 80 and above. For men, it rises from 3.59 per 100,000 in the 40–49 years age group to a peak of 132.72 per 100,000 between ages 70 and 79, and then drops to 110.48 per 100,000 in those 80 and older. Both genders display an increased incidence rate with age [2]. The prevalence of PD in Asia is lower compared to the West. According to the age-standardized 2000 WHO population, the prevalence of PD in Asian studies was found to be 51.3–176.9/100,000 from field surveys and 35.8–68.3/100,000 from record-based surveys, whereas Western studies reported higher prevalence rates of 101–439.4/100,000 from field surveys and 61.4–141.1/100,000 from record-based surveys [3]. The number of workdays lost due to PD increased from 27.6 days three years before diagnosis to 61.5 days three years after diagnosis, and indirect costs increased from $3549 to $7892. Caregivers also took more time off work after the diagnosis, resulting in an indirect cost rising from $302 to $850 [4]. With increasing longevity, the prevalence of PD is expected to double within the next 20 years. Without more effective treatments, the social and economic burdens associated with PD are anticipated to grow [5].
PD typically manifests with symptoms that gradually develop over several years, making diagnosis difficult [6]. On average, 15 years after PD onset, patients frequently experience falls, become immobile, show cognitive decline, and are often admitted to care facilities in an exacerbated state [7]. Additionally, out of 178 idiopathic PD patients, 109 (61.2%) died during the tracking period. Among the deceased, 77 (53.8% of 143) were from the PD group, 12 (92.3% of 13) were from the multiple system atrophy group, and 16 (88.9% of 18) were from the progressive supranuclear palsy group [8]. PD patients had a higher mortality rate compared to controls across all age groups and genders. Other studies also indicate that PD is a significant factor in increased mortality, regardless of age and gender [9,10,11].
Symptoms of PD can be divided into non-motor neurological abnormalities and motor abnormalities. Non-motor symptoms include olfactory dysfunction, cognitive impairment, psychosis, and sleep disorders [12,13]. Motor symptoms manifest as tremors, rigidity, and gait abnormalities [14]. PD progresses in three stages: the preclinical phase, where neurodegenerative processes start but do not yet cause noticeable symptoms; the prodromal phase, where noticeable symptoms arise from the evident neurodegeneration in various regions of the central nervous system (CNS) and peripheral nervous system (PNS); and the clinical phase, where classical motor symptoms become prominently evident [15].
Another issue with PD is the emergence of complications. Postural instability and associated falls, combined with other central features, are among the most common complications in PD patients [16,17]. Other issues like tremors, abnormal movements, dementia, depression, hallucinations, and autonomic nervous system dysfunction symptoms are also observed in PD patients [18].
PD is difficult to control with medical treatment, especially with the continuous growth in the elderly population [19]. Although drugs have been developed to delay PD progression, current medications have limitations and side effects [20,21,22]. Therefore, with the limitations and side effects of commonly used drugs, there is a demand for new medicines without these drawbacks. Consequently, there has been a surge in research on traditional Korean medicine and natural extracts [23,24,25]. Therefore, this study aims to investigate the potential of herbal medicines and plant-derived extracts used in traditional Korean medicine for improving PD.
2. Pathophysiology of Parkinson’s Disease
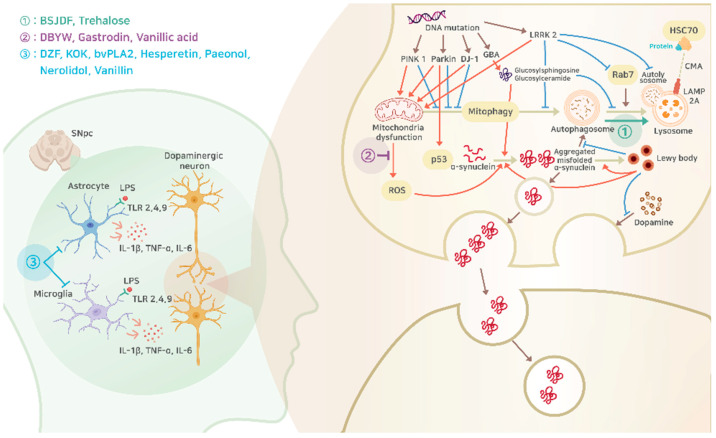
PD arises from the interplay of various genetic and environmental factors, with the primary pathology being the abnormal accumulation of the α-synuclein (α-Syn) protein within neurons. This irregular accumulation impacts the dopamine-producing neurons in the substantia nigra, eventually leading to neuronal death. This results in an imbalance of dopamine levels, inducing various motor symptoms of PD [26,27,28]. Additionally, pathological observations in PD include mitochondrial dysfunction, lysosomal disorders, and inflammation (Figure 1).
Figure 1.
Schematic pathophysiologic mechanism of PD with potential intervention of natural products, the details of which are explained in the following sections. Circled number 1 (green letters), promotion of α-Syn removal through autophagy; circled number 2 (purple letters), inhibition of ROS synthesis from mitochondria dysfunction; circled number 3 (blue letters), inhibition of inflammatory responses from astrocyte and microglia. BSJDF, Bu-Shen-Jie-Du-Fang; DBYW, Da-Bu-Yin-Wan; DZF, Duzhong Fang; KOK, Kyung-Ok-Ko; bvPLA2, bee venom phospholipase A2; SNpc, substantia nigra pars compacta; LPS, lipopolysaccharide; TLR, toll-like receptor; IL, interleukin; TNF-α, tumor necrosis factor α; LRRK2, leucine-rich repeat serine/threonine-protein kinase 2; HSC70, heat shock cognate 71 kDa; ROS, reactive oxygen species; CMA, chaperone-mediated autophagy; LAMP2A, lysosome-associated membrane protein 2a.
2.1. The Main Cause of Parkinson’s Disease
Beyond the loss of dopaminergic neurons, a pathological diagnosis of PD requires the presence of Lewy bodies, consisting of protein α-Syn, in the neurons [29]. α-Syn, comprising 140 amino acids, is a neuron-specific protein abundantly found in synapses and potentially participates in neurotransmission [30]. At a neutral pH, α-Syn exists in an irregular form, but it is assumed to form an α-helix structure when bound to membranes or vesicles containing acidic lipids. In its normal state, α-Syn is believed to assist synaptic vesicle release, providing a stabilizing effect [31]. However, in PD, mutations in the α-Syn-related gene or post-translational modifications such as cleavage, nitrosylation, ubiquitination, and phosphorylation, transform a-Syn into an aggregation-prone toxic beta-sheet form [32]. Many studies support the notion that small amounts of misfolded pathological α-Syn can accelerate the misfolding of endogenous α-Syn, acting as a template and amplifying the pathology [33,34]. Lewy bodies are pathological products primarily composed of α-Syn, but also incorporate hundreds of other proteins. Recent studies suggest a relationship between Lewy bodies and aggresomes [35]. The misfolding and pathological changes of α-Syn differ depending on conditions. In multiple system atrophy, the cellular environment of oligodendrocytes has been observed to intensify the altered forms of α-Syn, leading to increased toxicity [36]. α-Syn exhibits prion-like characteristics. Abnormal α-Syn is released from donor neurons and endocytosed into recipient neurons, propagating from one neuron to another [37]. α-Syn aggregates can be transported in both anterograde and retrograde directions along axons. Notably, synaptic contact is not necessarily required for transfer from axons to neuronal bodies [38]. Neuronal degeneration can occur without the spread of α-Syn pathology and the formation of Lewy bodies [39]. This is supported by clinical trial results wherein PD patients who underwent dopaminergic neuron transplantation showed motor function improvement for up to 18 years after transplantation without pharmacological dopamine treatment [40].
According to the Braak’s staging model, PD begins its development associated with the olfactory brain or the peripheral autonomic system and adrenal medulla [41,42]. It then progresses through the brainstem, followed by cerebral pathways, higher cortical areas responsible for autonomous function regulation, higher-order sensory association regions, frontal areas, and eventually the entire neocortex (from stages 1 to 6). Based on this model, pathological changes in Lewy bodies are observed in the substantia nigra by stage 3 [43], and stages prior to this are considered to be asymptomatic or pre-symptomatic. Non-motor symptoms, such as olfactory and autonomic symptoms (e.g., gastrointestinal and urinary symptoms), appear during the pre-symptomatic stage [44]. However, some retrospective clinical–pathological studies have shown that at least 15% of PD patients did not have α-Syn progression in accordance with Braak’s criteria [45]. Pathological changes can initially start in areas like the brain’s relay nuclei or the olfactory brain and propagate downward to the brainstem [46].
Furthermore, recent studies have evidenced that α-Syn pathology can propagate from the enteric nervous system to the brain [47]. Several pathways, including the vagal nerve route, immune system mediators, gut-related hormones, and microbial-derived signaling molecules, have been suggested, but further research is required to identify the exact mechanism of the transmission of α-Syn pathology from the gut to the brain [48]. Neuroimaging techniques such as positron emission tomography and magnetic resonance imaging (MRI) have evaluated structural damages at various levels in the peripheral autonomic system and CNS. In MRI studies, structural changes in the brainstem, including prominent pontine lesions, were observed in body-predominant PD patients [49,50]. The detection rates of α-Syn in the skin and intestines were also higher in body-predominant PD compared to brain-predominant PD [51,52,53,54,55]. Dopamine transporter imaging revealed more asymmetric degeneration of the nigrostriatal pathway in brain-predominant PD [56].
2.2. Mitochondrial Dysfunction
Mitochondria exhibit a decline in quality and function with aging, and mitochondrial dysfunction has been observed in various neurodegenerative diseases [57]. Mitochondrial dysfunction has been recognized as a significant factor in the loss of dopaminergic neurons [58].
The first hint of a crucial role of mitochondria in the pathogenesis of PD was found in the 1980s when a group of heroin users in California developed PD induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydrodropyridine (MPTP) [59]. Various toxins, such as MPTP, rotenone, paraquat, pyridaben, trichloroethylene, and fenpyroximate, have been associated with PD-like symptoms, have been shown to inhibit mitochondrial complexes [60], and the resulting disturbances in energy production and cellular functions could lead to damage in dopaminergic neurons and symptoms similar to PD.
Patients with PD exhibit reduced Complex I activity in the CNS and the prefrontal cortex [61,62]. This is due to the detrimental impact of abnormal α-Syn expression on mitochondrial function [26,63]. The N-terminus of α-Syn possesses a mitochondrial inner membrane-targeting sequence, and it interacts with Complex I, resulting in reduced activity both in vitro and in vivo. Additionally, mitophagy, a type of macroautophagy that selectively removes dysfunctional mitochondria to maintain mitochondrial homeostasis, is also associated with PD. Incomplete mitophagy, resulting from mutations in the genes Parkin and PTEN-induced putative kinase 1 (PINK1), causes autosomal recessive PD and is also associated with idiopathic PD [64].
A few genes have been confirmed to cause familial PD [65,66], and they are directly associated with autosomal dominant mutations in Synuclein Alpha (SNCA) and Leucine-rich repeat serine/threonine-protein kinase 2 (LRRK2) and autosomal recessive mutations in Parkin and PINK1 [67]. Parkin promotes mitophagy by attaching ubiquitin to outer mitochondrial membrane proteins [68]. However, Parkin mutations lead to increased p53 expression, which can potentially induce cell death [69]. Located in the mitochondria, PINK1 protects neuronal cells during acute oxidative stress, and promotes mitophagy. Defects in PINK1 lead to mitochondrial dysfunction and accumulation. As PD patients age, PINK1 plays a role in the loss of dopaminergic neurons [70]. DJ-1 is a multifunctional protein involved in transcriptional regulation, mitochondrial protection, antioxidant activities, and chaperone activation [71]. Being essential for mitophagy, defects in DJ-1 result in incomplete mitophagy, contributing to autosomal recessive PD [72]. LRRK2 is found in the mitochondrial outer membrane, nucleus, and cytoplasmic membrane. Mutations in LRRK2 lead to increased mitochondrial fission and augmented mitochondrial reactive oxygen species (ROS) production, adversely affecting mitochondria and inducing the autosomal dominant form of PD [73].
2.3. Lysosomal Disorders
Lysosomal dysfunction triggers the onset of PD and the initial deposition of α-Syn lesions, accelerating the progression of the disease [74]. Damage to degradation activity and reduced proteostasis are features of aging, and lysosomes mediate the interaction between related genetic mutations and aging. This can influence the onset of PD [75,76]. Gradual abnormalities in endolysosomal function adversely affect other pathological mechanisms of PD, such as synaptic and mitochondrial dysfunctions.
2.3.1. Autophagy–Lysosomal Pathway
Lysosomes play a crucial role in maintaining cellular homeostasis by regulating the metabolism of proteins, lipids, and large molecules through endocytosis, phagocytosis, and autophagy. Through the autophagy–lysosomal pathway, proteostasis of the α-Syn protein is maintained. However, lysosomal dysfunction hinders the removal of α-Syn, leading to its accumulation and propagation through synapses, causing cellular toxicity [77]. This forms a positive feedback loop where the toxic forms of α-Syn disrupt lysosomal biogenesis, contributing to the pathogenesis of PD.
Autophagy is the process by which cells eliminate abnormal or damaged proteins, damaged organelles, and unnecessary cellular components via lysosomes. Autophagy can be broadly classified into three types: macroautophagy, microautophagy, and chaperone-mediated autophagy (CMA). Macroautophagy involves the formation of autophagosomes, which fuse with lysosomes for content degradation. Microautophagy directly engulfs cytoplasmic components in the lysosome. CMA involves the direct transfer of substrate proteins through the lysosomal membrane, interacting with the lysosomal receptor lysosome-associated membrane protein 2a (LAMP2a) without forming additional vesicles [78,79]. PD patients exhibit abnormalities in these autophagy systems, with reduced levels of LAMP2a and heat shock cognate 71 kDa (Hsc70) protein in the CNS.
2.3.2. Glucocerebrosidase (GCase)
Beta-glucosidase (GBA) is a gene encoding glucocerebrosidase, an enzyme that hydrolyzes glucosylceramide into ceramide and glucose [80]. Loss-of-function mutations in GBA are common and potent risk factors for PD. However, even among PD patients without GBA mutations, GCase activity can be reduced [81]. When GBA function is lost, accumulation of glucosylceramide and glucosylsphingosine due to GCase dysfunction disrupts autophagy, leading to α-Syn accumulation [82]. Accumulation of glucosylceramide promotes the formation and stabilization of oligomeric α-Syn intermediates in human-induced pluripotent stem cell-derived neuronal cultures [64]. Defects in lysosomal function can lead to lysosomal storage diseases, some of which can progress to neurodegeneration. It has been shown that patients with Gaucher disease and individuals with heterozygous mutations in GBA have an increased risk of developing PD. Loss-of-function mutations in the GBA1 gene, which encodes the lysosomal hydrolase β-glucocerebrosidase, lead to the accumulation of lipid substrates in Gaucher’s disease. This dysfunction is linked to Parkinson’s disease through the accumulation of α-synuclein in Lewy bodies and neurites, contributing to neuronal death. GBA1 mutations increase the risk of Parkinson’s disease, and Parkinson’s patients exhibit decreased β-glucocerebrosidase activity. Loss of β-glucocerebrosidase activity also promotes α-synuclein accumulation and toxicity, and conversely, α-synuclein accumulation further contributes to decreased lysosomal β-glucocerebrosidase activity by disrupting its trafficking to lysosomes. This disruption extends to other lysosomal hydrolases, exacerbating lysosomal dysfunction and neuronal dyshomeostasis [81,82].
2.3.3. LRRK2
LRRK2 phosphorylates 14 members of the Rab family at the switch-II domain. Some of these Rab proteins promote vesicle transport from vesicles to the Golgi apparatus [83], thereby reducing cellular toxicity caused by α-Syn accumulation in PD models. Conversely, mutant LRRK2 delays early late and late endosomal trafficking. In PD patient fibroblasts, Rab7 activity was found to be reduced compared to healthy controls due to pathogenic LRRK2 mutations [64]. Additionally, mutant LRRK2 suppresses LAMP2a, inhibiting CMA. LRRK2 knockout mice showed abnormalities in protein removal functions, and increased cell death and oxidative stress were observed due to increased α-Syn [84].
In conclusion, mutant LRRK2 acts as a negative regulator of autophagy, leading to the accumulation of α-Syn in dopaminergic neurons [85]. Furthermore, α-Syn itself disrupts the normal function of the endosomal–lysosomal (E-L) system, further promoting α-Syn accumulation [86].
2.4. Inflammation
Patients with PD manifest neuroinflammation alongside the loss of dopaminergic neurons [87,88]. This is associated with alterations in microglia activity. When microglia are activated, Tumor necrosis factor alpha (TNF-α) releases various free radicals and activates numerous genes and proteins, including inducible nitric oxide synthase (iNOS) and inflammatory cytokines. The inflammatory molecule interleukin-1β (IL-1β) cytokine family stimulate Toll-like receptors (TLRs) and hinder the phagocytic action of microglia [89]. Endotoxins, such as lipopolysaccharides (LPS), also induce inflammatory responses through TLRs. When LPS binds with TLRs, it activates several signaling pathways, including mitogen-activated protein kinase (MAPK), phosphatidylinositol 3-kinase (PI3K)/protein kinase B (AKT), and the mechanistic target of rapamycin (mTOR), initiating the inflammation. This subsequently promotes nuclear factor-κB (NF-κB) activation, enhancing microglial phagocytic action and cytokine secretion. The NF-κB protein is activated extracellularly, but after interacting with inflammatory cytokines, it moves to other tissues causing damage [90].
2.4.1. Microglia
There are two activation forms of microglia: M1 and M2. When the M1 phenotype is activated, it stimulates pathogen-associated molecular patterns (PAMPs), damage-associated molecular patterns (DAMPs), LPS, and amyloid-β aggregates, promoting dopaminergic neuronal damage. In PD models, M1 phenotype microglia are activated by both external and internal stimuli [91]. When the M2 phenotype is activated, it performs the opposite action to the M1 phenotype, producing various anti-inflammatory cytokines such as interleukins 4, 13, 10 (IL-4, IL-13, IL-10), glucocorticoids, and TGF-β [92,93]. The pathophysiology of inflammation in PD is significantly influenced by microglial activation and the polarization of microglia into M1 and M2 phenotypes, which play critical roles in neuroinflammation and neurodegeneration. In neurodegenerative diseases like PD, microglia-mediated neuroinflammation is a common feature. These cells can transition between different phenotypes, primarily classified into M1 and M2, although they also exhibit a range of intermediate states [94]. Microglia are at the forefront of the neuroinflammatory response in PD. Under normal conditions, they are in a “homeostatic” state, but pathological stimuli trigger a switch to a “reactive state.” The persistent activation of M1 microglia contributes to inflammatory diseases, including PD [95]. M1 microglia, when activated by pathogenic molecules like LPS, IFN, or protein aggregates (e.g., α-synuclein), release inflammatory molecules like ROS and pro-inflammatory cytokines (e.g., IL-1β, iNOS, TNF-α). This prolonged exposure to inflammatory mediators can result in neuronal damage. On the other hand, mediators like TGF-β, IL-4, IL-10, and IL-13 can induce the transition from M1 to M2. The M2 phenotype aids in phagocytosis, extracellular matrix (ECM) rebuilding, and neuronal survival, secreting factors such as Ym1 and FIZZ1 [95]. The phenotypic transformation of microglia from M1 to M2 is dynamic and associated with the stages and severity of neurodegenerative diseases. In later stages, M1 microglia predominate at the injury site, suppressing the immunoresolution and repair processes of M2 microglia. This transition is complex and is influenced by the presence of endogenous stimuli like aggregated α-synuclein, mutated superoxide dismutase, β-amyloid, and tau oligomers. These stimuli can continuously activate M1 pro-inflammatory responses, ultimately leading to irreversible neuron loss. Therefore, understanding and managing the stage-specific switching of microglial phenotypes could provide therapeutic benefits [96].
Research on the effects of natural and herbal medicine, specifically flavonoids, on the M2 anti-inflammatory response in neuroinflammation, including conditions like Parkinson’s Disease, has shown promising results. Flavonoids, natural compounds found in herbs, fruits, vegetables, tea, and cereals, have demonstrated an ability to alleviate neuroinflammation [97,98,99]. This effect is achieved by inhibiting the production of pro-inflammatory mediators and enhancing the secretion of anti-inflammatory factors. Flavonoids also modulate the polarization of microglia, shifting them from the M1 to the M2 phenotype. This modulation occurs through the suppression of the NLRP3 inflammasome, NF-κB, MAPK, and JAK/STAT pathways, and through the promotion of Nrf2, AMPK, BDNF/CREB, Wnt/β-Catenin, PI3k/Akt signals and SIRT1-mediated HMGB1 deacetylation [100]. Previous studies have focused on Shaoyao–Gancao Decoction (SGD), a traditional herbal medicine, which showed potential in promoting the M2 polarization of microglia. SGD induced upregulation of IL-13, which is known to drive microglia towards the M2 phenotype [101]. This transition was associated with anti-inflammatory and neuroprotective effects, suggesting that SGD could be a beneficial treatment in conditions involving neuroinflammation. Another study investigated the effects of luteolin, a flavonoid, on microglia polarization [102]. This study found that luteolin suppressed the production of pro-inflammatory mediators in LPS-stimulated primary microglia cells while promoting the expression of anti-inflammatory M2 markers. These effects were dose-dependent and were achieved by influencing the IL-17 and TNF signaling pathways, crucial for controlling microglia polarization. Specifically, luteolin was shown to inhibit the activation of the NF-κB pathway and reduce the expression of MMP9, a molecule involved in microglia activation and neuroinflammation. These results highlight luteolin’s potential as a therapeutic agent in managing neuroinflammation through modulation of microglia polarization.
2.4.2. Astrocytes
Astrocytes are induced to secrete inflammatory cytokines in response to LPS. Excessive activation of astrocytes is recognized by morphological changes such as neuronal cell body hypertrophy and increased expression of astrocyte reactivity markers like glial fibrillary acidic protein (GFAP) [103]. When astrocytes are activated, NF-κB is activated, regulating the secretion of chemokines and adhesion molecules, assisting lymphocyte infiltration, and leading to neurodegeneration [104]. In PD, astrocytes, particularly their polarized A1 proinflammatory phenotype, play a crucial role in the progression of neuroinflammation and neurodegeneration. Astrocytes, derived from neural stem cells, are critical for maintaining the balance of ions, fluid, and transmitters in the brain, as well as regulating blood flow and the blood–brain barrier (BBB) [100]. In the context of neuroinflammation, such as in PD, astrocytes can polarize into a neurotoxic A1 phenotype. This state is characterized by cellular hypertrophy, increased production of glial fibrillary acidic proteins and complements, astrogliosis, glial scar formation, and the secretion of pro-inflammatory factors. These A1 astrocytes also affect vascular and perivascular cells, altering BBB permeability. The interaction between A1 astrocytes and microglia results in a feedback loop, exacerbating neuroinflammation and contributing to neuronal damage and excitotoxicity [100]. The morphological changes in astrocytes, particularly the transition to the A1 phenotype, are indicative of the stage and severity of PD. Preventing this transition, or reverting astrocytes to a less inflammatory state, has significant therapeutic potential. For example, GLP1R agonists have been suggested to inhibit the conversion of astrocytes to the A1 phenotype, offering neuroprotection in PD models. This inhibition is key in developing treatments for neurodegenerative diseases where no disease-modifying therapies currently exist [105].
The traditional Chinese herbal medicine Astragalus membranaceus Bunge and its derivative Astragaloside IV (AS-IV) have shown promising results. AS-IV exerts anti-inflammatory and neuroprotective activities, and is particularly effective against astrocyte senescence [106]. It has been observed to inhibit replicative and premature senescence in astrocytes, reducing the pro-inflammatory senescence-associated secretory phenotype [107,108]. This effect is mediated through the promotion of mitophagy, reducing damaged mitochondria accumulation and mitochondrial reactive oxygen species generation. Consequently, AS-IV protects against dopaminergic neuron loss and behavioral deficits in PD mouse models by reducing senescent astrocyte accumulation in the substantia nigra compacta [109].
2.4.3. TLRs
TLRs play a crucial role as pattern recognition receptors (PRRs) in initiating immune responses to various stimuli [104,110]. In PD patients, TLRs identify α-Syn aggregates as DAMPs, playing a pivotal role in inducing and maintaining neuroinflammation. In PD patients, TLRs mediate inflammatory responses in peripheral blood leukocytes, glial cells, and neurons [89]. While TLR2, TLR4, and TLR9 are proven to have significant roles in PD pathogenesis, the relevance of other TLRs, such as TLR7 and TLR8, remains unclear [104]. In PD patient neural cell loss sites, TLR2 and CD68+ co-expressing microglia are activated [111]. The TLR2 receptor is responsible for microglial activation, releasing toxic factors that progress neural damage [89]. TLR4 is involved in microglial α-Syn phagocytosis, so a deficiency in TLR4 can impair the α-Syn clearance function, potentially causing neurodegeneration [111].
2.4.4. Pro-Inflammatory Cytokines and Parkinson’s Disease
Cytokines are proteins acting as signaling molecules in the inflammation, infection, growth, and recovery of damaged tissues. They regulate the transportation of leukocytes in the brain and gather other proteins. Elevated concentrations of pro-inflammatory cytokines like TNF-α, IL-1β, and IL-6 have been observed in the substantia nigra pars compacta and cerebrospinal fluid of sporadic PD patients [112,113]. Such alterations in cytokine levels can be initiated by activated microglia, potentially promoting dopaminergic neuronal cell death [114]. Among them, IL-1β plays a significant role in neurodegenerative diseases like PD. It acts through IL-1 receptors found in neurons and microglia, leading to the expression of pro-inflammatory cytokines and perpetuating the inflammation cycle. In animal models of PD, administering IL-1 receptor antagonists significantly reduced TNF-α and interferon gamma (IFN-γ), decreasing the elevated loss of dopaminergic neurons induced by LPS [115].
3. Current Medications for Parkinson’s Disease
Commonly used treatments in current clinical settings aim to supplement dopamine in PD patients [116]. Medications such as Levodopa, designed to alleviate PD symptoms and improve quality of life, and others like the type-B monoamine oxidase (MAO-B) inhibitor, catechol-O-methyltransferase (COMT) inhibitor, and dopamine agonists have been developed and prescribed to address the drawbacks of Levodopa [117]. However, a complete cure for PD has not yet been discovered [118].
3.1. Levodopa
Levodopa is used to replenish dopamine in PD patients. It is a precursor of dopamine and, after crossing the blood–brain barrier (BBB), is decarboxylated by aromatic amino acid decarboxylase (AADC) to be converted into dopamine [119]. Dopamine transporters absorb exogenous dopamine from Levodopa, storing it in synaptic vesicles, maintaining a relatively stable dopamine level in the synaptic cleft during Levodopa treatment. Patients experience a stable response to Levodopa in the earlier stages of PD. However, improvements from Levodopa alone have limitations in treating Levodopa-induced dyskinesia [120]. Prolonged use of Levodopa might cause a reduction in its efficacy, and side effects such as motor complications (e.g., akinesia, bradykinesia) and psychological side effects (e.g., depression, cognitive impairment) can occur. Therefore, it is crucial to explore various potential treatments beyond dopamine supplementation using Levodopa [121].
3.2. COMT Inhibitor
COMT inhibitors are drugs that inhibit the enzyme COMT, which methylates substrates with a catechol moiety, limiting the availability of Levodopa in the brain by converting it to 3-O-methyl dopa [119]. Treating with COMT inhibitors prevents O-methylation of Levodopa and promotes its conversion to dopamine in the brain. However, the half-lives of the three widely used COMT inhibitors are very short, i.e., 2 to 3 h. This makes it challenging to achieve the desired inhibitory levels, often requiring nearly 10 doses daily, which can be inconvenient for patients. There are some adverse reactions, notably dopamine-related reactions like newly emerging dyskinesias, exacerbation of existing dyskinesias, nausea, and non-dopaminergic reactions such as diarrhea. Additionally, cases of acute liver failure have been reported, three of which resulted in death [122].
3.3. MAO-B Inhibitor
MAO catalyzes the oxidative deamination of monoamine neurotransmitters such as dopamine, phenylethylamine, 5-hydroxytryptamine, and norepinephrine. Among these, MAO-B metabolizes dopamine released in synapses and is absorbed by glial cells. MAO-B inhibitors block the metabolism of dopamine by inhibiting MAO-B activity, enhancing dopamine signaling, and selectively elevating dopamine levels in the synapse. They also offer various other benefits. The metabolism of dopamine by MAO-B forms toxic metabolites such as hydrogen peroxide and dihydroxyacetone. However, MAO-B inhibitors prevent this toxic process, thus protecting dopaminergic neurons in the substantia nigra and slowing the clinical progression of PD. They also inhibit nitric oxide synthase activity, reduce hydrogen peroxide production, improve brain mitochondrial function, and prevent the accumulation of α-Syn, thereby slowing the progression of PD [123]. However, Rasagiline, a well-known MAO-B inhibitor, showed no clear neuroprotective effects in clinical trials, limiting its therapeutic potential, and was found to have irreversible binding to active sites, causing long-term side effects. Selegiline, another MAO-B inhibitor, reported side effects such as insomnia, hallucinations, and akinesia. Additionally, safinamide, a reversible inhibitor with fewer side effects, has been reported to cause nausea, headaches, vomiting, fever, and high blood pressure [124,125].
3.4. Dopamine Agonist
Dopamine agonists provide significant anti-Parkinson symptom effects. They are used as the first-line drug for initial PD in patients under 60 years old, delaying the onset of motor complications and dysfunctions, and postponing the initiation of Levodopa therapy. Some authors advocate for starting PD treatment with dopamine agonists. However, dopamine agonist treatment is ineffective for patients who do not respond to Levodopa [126].
4. Evidence of Natural Products from Pre-Clinical Studies
Currently, drugs designed to treat PD only aim at alleviating the symptoms. However, there are no drugs that target the root cause of the disease. The most common treatment approach involves replenishing the dopamine levels in the brain. Yet, there are no therapies available that can repair the damaged brain cells. Especially in the realm of Western medicine, drugs are synthetic. The usual approach is to design a drug to act on one specific target pathway to minimize adverse side effects. However, there are some challenges where patients develop tolerance upon continued usage and increasing the dosage that leads to additional side effects. Given these challenges, there is a growing need for the development of new drugs. Our research explored alternative natural products to surpass the constraints of the current medicinal approach. Herbal medicines, made from plant-derived natural substances, have a diverse composition (Table 1). This means it is possible to address multiple pathways using a single drug, which may be a potential treatment avenue for PD (Figure 1).
4.1. Duzhong Fang
Duzhong Fang is a traditional Chinese medicine formula that consists of four ingredients: dried Eucommia ulmoides, Dendrobium, Rehmanniae Radix, and dried ginger. These ingredients are mixed in a specific weight ratio of 200:2:3:3 [127]. Duzhong Fang can regulate microglial morphology and reactivity, reducing microglial reactivity and inflammation in the central nervous system. Additionally, Duzhong Fang can directly inhibit the POMC gene, which is an upstream target for regulating inflammation and proinflammatory cytokines. By inhibiting POMC levels, Duzhong Fang can restore the homeostatic signature of microglia in Parkinsonian rats, leading to the alleviation of neuroinflammation and improvement of motor function. Duzhong Fang demonstrated anti-inflammatory effects in a mice model of PD, playing a role in managing neuroinflammation in PD by modulating microglial reactivity [128].
4.2. Kyung-Ok-Ko (KOK)
KOK’s original formula comprises juice from the root of Rehmannia glutinosa Liboschitz var. purpurae Makino (9.6 g), powder of dried fruit of Poria cocos Wolf (1.8 g), powder from the root of Panax ginseng C.A. Meyer (0.9 g), and honey (6 g). As a traditional composite herbal remedy, KOK has been employed to treat a wide range of diseases and conditions due to its action on multiple targets [129]. The MAPK (extracellular signal-regulated kinase ½ (ERK), c-Jun NH2-terminal kinase (JNK), and p38) and NF-κB signaling pathways, associated with neuronal loss, neuroinflammation, and BBB disruption in PD, can be potentially inhibited by KOK treatment according to the anti-inflammatory properties of KOK, similar to its role as a protective agent against MPTP-induced neurotoxicity [130].
4.3. Da-Bu-Yin-Wan (DBYW)
DBYW is composed of Amur corktree bark (Phellodendron chinense Cortex; Huang-Bai) 12 g, common Anemarrhena rhizome (Anemarrhenae Rhizoma; Zhi-Mu) 12 g, prepared rehmannia root (Radix Rehmanniae Praeparata; Shu-Di-Huang) 18 g, and tortoise shell (Carapax et Plastrum Testudinis; Gui-Jia) 18 g, as described in a prior study [131]. This study has shown that DBYW can elevate the expression of tyrosine hydroxylase (TH), enhance levels of monoamine neurotransmitters, and minimize mitochondrial DNA damage. The study demonstrates that DJ-1 overexpression increases Akt phosphorylation, leading to improved mitochondrial function and cell survival in a cellular model of Parkinson’s disease. Furthermore, DBYW was found to augment this process by enhancing the effects of DJ-1 on mitochondrial function through Akt phosphorylation. Additionally, DBYW enhances mitochondrial protection in PD by elevating cellular ATP content and decreasing the expression of ATP-sensitive potassium channel subunits [132].
4.4. Bee Venom Phospholipase A2 (BvPLa2)
BvPLa2 is an enzyme present in bee venom. This enzyme breaks down membrane phospholipids, producing free fatty acids and lysophospholipids. BvPla2 is known for its varied pharmacological effects, including anti-HIV activity, myotoxicity, and the promotion of neurite growth [133,134]. As a significant component of bee venom, BvPla2 stimulates regulatory T cells, mitigating neuroinflammatory reactions. This leads to the improvement of movement disorders and a reduction in α-Syn levels [135].
4.5. Hesperetin
Hesperetin is a flavonoid found in citrus fruits. It has shown protective effects against 6-hydroxydopamine (6-OHDA) lesions in rat striatum. Hesperetin treatment in 6-OHDA lesioned rats resulted in a reduction in apomorphine-induced rotational asymmetry, indicating an improvement in motor function. Additionally, hesperetin decreased the latency to initiate and the total time on the narrow beam task, suggesting an enhancement in motor coordination and balance. These effects indicate that hesperetin has the potential to improve motor function and coordination in rats with 6-hydroxydopamine-induced damage, possibly through its protective effects on the dopaminergic system and related motor pathways. It was found to provide protective effects in early models of PD by reducing behavioral disorders, alleviating oxidative stress, and reducing astrogliosis. Furthermore, hesperetin can be considered a potential adjunct therapy for PD management by preventing cell death and loss of dopaminergic neurons in the substantia nigra [136].
4.6. Paeonol
Paeonol is a major phenol compound from the Chinese herb Cortex Moutan, known for its antioxidant, anti-inflammatory, and anticancer properties [137]. This study showed that paeonol treatment significantly restored the activity of superoxide dismutase (SOD), catalase (CAT), and glutathione (GSH) in the midbrain, thereby alleviating oxidative stress induced by 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine/probenecid (MPTP/p). Additionally, Paeonol treatment decreased the levels of microglia and interleukin-1β (IL-1β), indicating a reduction in neuroinflammation, and increased the levels of brain-derived neurotrophic factor (BDNF), indicating neurotrophic effects on dopaminergic neurons. It has shown therapeutic effects against MPTP-induced PD in mice by improving behavioral tests, enhancing TH expression, reducing oxidative stress, and inhibiting microglial activation. Paeonol’s capability to promote neuronal survival and delay PD progression suggests its possibility as a treatment for PD [138].
4.7. Gastrodin
The Chinese herb Rhizoma Gastrodiae contains Gastrodin, a phenol glycoside known for its neuroprotective, antidepressant, and antiepileptic properties [139]. Gastrodin protects dopaminergic neurons, reduces the accumulation of α-Syn protein, and inhibits amyloid-β production and aggregation. In this study, Gastrodin rescued the climbing ability of Pink1 mutant flies, indicating an improvement in their motor function. Moreover, Gastrodin delayed the progressive loss of a cluster of dopaminergic neurons in the protocerebral posterial lateral 1 region of Pink1 mutant flies, and increased the dopamine content in the brain of Pink1 mutant flies. In other words, Gastrodin demonstrated potential anti-aging effects by extending lifespan, enhancing antioxidant capacity, and delaying PD-like phenotypes [140].
4.8. Trehalose
Trehalose is a natural disaccharide found in invertebrates, fungi, and many plants. It has value in various potential applications; has anti-inflammatory, antioxidant stress, and anti-cell death effects; and is a non-toxic compound [141,142]. In an AAV α-synuclein rat model of PD, animals that received unilateral AAV1/2 A53T α-synuclein showed a deficit in the use of their paw contralateral to the site of vector injection 3 weeks post-surgery, compared with empty vector controls. Neurochemical analysis demonstrated a significant attenuation in α-synuclein-mediated deficits in motor asymmetry and DA neurodegeneration, including impaired DA neuronal survival and DA turnover, as well as α-synuclein accumulation and aggregation in the nigrostriatal system, by commencing 5 and 2% trehalose at the same time as delivery of AAV. Trehalose protects against α-synuclein-mediated DA degeneration by enhancing autophagy in the striatum, which leads to the reduction of α-synuclein aggregates, improved DA neuronal survival, and prevention of behavioral asymmetry. Trehalose stimulates autophagy in an mTOR-independent manner, which helps in the clearance of α-synuclein aggregates [143].
4.9. Bu-Shen-Jie-Du-Fang (BSJDF)
BSJDF is a composite traditional Chinese medicine made up of Rehmannia glutinosa, Cistanche deserticola, Paeonia lactiflora Pall, Radix Angelica sinensis, Puerariae Radix, Rhizoma Coptidis, Radix Scutellariae, Antelope Horn Powder, and Glycyrrhizae Radix in a weight ratio of 5:5:4:4:5:4:4:1:2 [144,145]. BSJDF was found to protect PC12 cells by inducing autophagy in an MPP+-induced cell model of Parkinson’s Disease. The BSJDF group had the greatest surviving cell counts compared with all other treated cell groups except the normal group. Autophagy was observed in the BSJDF group by transmission electron microscopy (TEM), and protein expression of Atg12 and LC3 in the BSJDF group was upregulated compared to the PD model group. BSJDF was found to improve cell survival in an MPP+-induced cell model of Parkinson’s Disease by inducing autophagy, as evidenced by increased protein expression of Atg12 and LC3, and upregulated Atg12 mRNA expression. The study suggests that autophagy plays an important role in cell fate and maintaining cellular metabolic balance in Parkinson’s disease. These findings highlight the potential role of BSJDF in modulating autophagy and its implications for the development of treatments for Parkinson’s disease [146].
4.10. Nerolidol (NRD)
NRD is a sesquiterpene alcohol found in the essential oils of Baccharis dracunculifolia, Amaranthus retroflexus, and Canarium schweinfurthii. It exhibits various biological properties, including antioxidant and anti-inflammatory effects. NRD’s ability to easily cross the BBB enhances its potential as a treatment for neurodegenerative diseases like PD [147]. This study does not explicitly address whether NRD can be used as a standalone treatment for PD or if it needs to be combined with other medications. However, it is important to note that the neuroprotective effects of NRD against neuroinflammation and oxidative stress were demonstrated in an experimental model of PD induced by rotenone. NRD exerts its neuroprotective effects by reducing oxidative stress and neuroinflammation. It has been reported to increase the activities of antioxidant enzymes such as SOD and CAT, and to decrease the level of the antioxidant tripeptide GSH. Additionally, NRD inhibits the release of proinflammatory cytokines and inflammatory mediators, and prevents the activation of glial cells, ultimately attenuating neurodegeneration induced by rotenone. Furthermore, NRD has been shown to reduce the level of lipid peroxidation and nitrite content in the hippocampus, protecting against oxidative stress. NRD supplementation demonstrates promising neuroprotective effects by attenuating dopaminergic neurodegeneration, enhancing antioxidant enzyme activity, and inhibiting brain inflammatory mediators and lipid peroxidation [148].
4.11. Vanillic Acid (VA)
Vanillic acid, 4-hydroxy-3-methoxybenzoic acid, is the oxidized form of vanillin, and can be isolated from Gastrodia [149]. Co-treatment with VA and Levodopa–Carbidopa in a rotenone-induced Parkinson’s disease rat model showed significant effects on various Parkinson’s symptoms [150]. The co-treatment led to a significant reduction in muscle rigidity and catalepsy, along with a significant increase in body weight, rearing behavior, locomotion, and muscle activity in a dose-dependent manner, with the maximum effect observed at the 50 mg/kg dose of VA. Additionally, the co-treatment resulted in a significant increase in the level of dopamine in the VA plus standard drug-treated animals compared to the rotenone-treated group. Furthermore, histopathological evaluation showed a reduction in the number of eosinophilic lesions in the VA co-treated group compared to the rotenone group, indicating protection against neuronal damage due to oxidative stress and attenuation of motor defects. Furthermore, the study indicates a reduction in various oxidative stress markers in the brain, including increased lipid peroxidation and decreased GSH and catalase [149].
4.12. Vanillin
Vanillin, 4-hydroxy-3-methoxybenzaldehyde, an aromatic organic phenol molecule that can be extracted from Gastrodia, is widely used as a fragrance in the food, beverage, cosmetics, and pharmaceutical industries. This study demonstrated that Vanillin administration significantly increased striatal tissue dopamine content in 6-OHDA lesioned animals, which is a key indicator of nigrostriatal neurodegeneration. Additionally, Vanillin administration showed that attenuated 6-OHDA-induced rotations during apomorphine challenge, indicating its potential efficacy in reducing the phenotypic behavior associated with 6-OHDA lesion [151].
Table 1.
Effect of natural products for PD.
| Origin of Extraction | Mechanism | Cell or Animal Model | Inducer | Mode of Action and Target Signal | Site of Action (Figure 1) | Ref. |
|---|---|---|---|---|---|---|
| Duzhong Fang | Inflammation | C57bl/6 mice | MPTP | ↓ locomotor dysfunction, inflammation, Iba1, microglia reactivity state ↑ striatal dopamine content, dopaminergic neurons, TH |
3 | [128] |
| KOK | Inflammation | C57BL/6 mice | MPTP ML385 | ↓ neurological dysfunction and motor impairments, the loss of dopaminergic neurons and fibers, Iba1, the upregulation of inflammatory mediators (IL-6, TNF-α, COX-2, and iNOS), neurotoxicity (microglial activation and inflammatory response ↓), BBB disruption markers (PECAM-1 and GFAP), neurotoxicity and inflammation (phosphorylated forms of ERK, JNK, and p38 & IκB and NF-κB ↓), ROS, MAPKs and NF-κB signaling pathways ↑ Nrf2 signaling (decreases the expression levels of Keap1 (a repressor protein that binds to Nrf2), and increases the expression levels of Nrf2 transcription factor, Nrf2 targeting genes HO-1 and NQO-1) |
3 | [130] |
| DBYW | Mitochondrial dysfunction | Rat PC-12 cells | pDJ-1 transfection MPP+ |
↓ DJ-1, mitochondrial dysfunction ↑ mitochondrial mass, total ATP content, the Akt phosphorylation |
2 | [132] |
| BvPLA2 | Inflammation | Human A53T α-Syn Transgenic mice | A53T Transgenes | ↓ motor dysfunction, α-Syn, the activation and numbers of microglia, and the ratio of M1/M2 | 3 | [135] |
| Hesperetin | Inflammation | Wistar rats | 6-OHDA | ↓ astrogliosis (GFAP ↓), apoptosis (nigral DNA fragmentation ↓), the loss of SNC dopaminergic neurons ↑ striatal catalase activity and GSH content, Bcl2 |
3 | [136] |
| Paeonol | Inflammation | C57BL/6 mice | MPTP | ↓ motor dysfunction, oxidative stress (the activity levels of SOD, CAT, and GSH ↑), neuroinflammation(the number of Iba1-positive and IL-1β-positive cells ↓), ↑ TH-positive neurons, BDNF, dopaminergic neurons protection |
3 | [138] |
| Gastrodin | Mitochondrial dysfunction | Drosophila melanogaster | PINK1 gene mutant | ↓ the loss of dopaminergic neurons, the onset of Parkinson-like phenotypes ↑ lifespan, climbing ability, resistance to oxidative stress, enzyme activities of superoxide dismutase (SOD) and catalase (CAT), the expression of anti-oxidative genes |
2 | [140] |
| Trehalose | Lysosomal Disorders | Human A53T α-Syn Transgenic mice | A53T Transgenes | ↓ α-Synuclein-Induced Behavioral Impairment, α-Synuclein Accumulation ↑ DA Neuronal Survival, protection against the reduction of TH protein expression, autophagosome formation, LC3-II levels |
1 | [143] |
| BSJDF | Lysosomal Disorders | Pheochromocytoma12 (PC12) | MPP+ (MPTP) |
improved cell survival in the PC12 cell PD model activated the autophagic process in PC12 cells. increased expression of Atg12 and LC3 proteins and upregulated Atg12 mRNA. |
1 | [146] |
| NRD | inflammation | Wistar rats |
Rotenone | ↑ level of superoxide dismutase, catalase, and glutathione ↓ level of malondialdehyde inhibited the release of proinflammatory cytokines and inflammatory mediators prevented ROT-induced glial cell activation and the loss of dopaminergic neurons and nerve fibers attenuated rotenone-induced dopaminergic neurodegeneration. |
3 | [148] |
| Vanillic acid | Mitochondrial dysfunction | Sprague Dawley rats | Rotenone | ↓ Weight gain, Catalepsy, Rearing TBARS level (at 25 mg/kg and 50 mg/kg) SAG(superoxide anion generation) ↑ behaviour, CAT |
2 | [149] |
| Vanillin | Inflammation | Male Wistar rats | 6-OHDA | ↓ apomorphine-induced rotations, free radical release, expression of pro-inflammatory cytokines, lipid peroxidation ↑ striatal dopamine content, glutathione and superoxide dismutase enzyme protection of dopaminergic neurons |
3 | [151] |
5. Evidence of Natural Products from Clinical Trials
Recently, clinical trials utilizing various natural substances for the improvement of PD symptoms have been conducted. These studies collectively suggest that natural products can potentially reduce neurotoxicity caused by oxidative stress and improve various symptoms associated with Parkinson’s disease.
Natural substances applied in the clinical trials include Licorice root, Origanum majorana L., and Pingchan. The trial results suggested that these natural substances are effective in reducing neurotoxicity caused by oxidative stress and improving motor symptoms. We, hereby, hypothesize that natural substances can be utilized in PD treatment [152].
According to Persian traditional literature [153], Licorice root was used for neurological conditions like headaches as a neuroprotective agent. In Persian folk medicine, formulations including Licorice extracts were used as neuroprotective herbal treatments for preventing disabilities associated with strokes or PD. In modern medicine, Licorice has shown various biological activities, such as anti-inflammatory, antioxidant [154], anti-tumor [155], antidepressant [156], memory-enhancing [157], neuroprotective [158], and anti-apoptotic effects. In a clinical trial involving 39 PD patients, patients were randomly divided into two groups and given either Licorice or a placebo syrup twice daily for six months. The results showed that adding Licorice extract as an adjunctive therapy can improve the overall Unified Parkinson’s Disease Rating Scale score of PD patients, improving daily activities, tremor and motor ability tests, and rigidity scores [152].
Origanum majorana L, known as sweet marjoram or simply marjoram, is an evergreen plant that belongs to the Lauraceae family. It is believed to have originated in the Mediterranean, North Africa, Egypt, and Asia and is widely used for culinary or medicinal purposes. In a clinical trial with 51 PD patients, patients who consumed Origanum majorana tea showed significant improvement in non-motor symptoms such as depression, anxiety, gastrointestinal and urinary symptoms, restlessness, and fatigue compared to the placebo group. Furthermore, consuming Origanum majorana tea daily for a month did not have adverse effects on liver and kidney functions. Notably, Origanum majorana L is rich in antioxidants like polyphenols and monoterpenes. Hence, this plant can neutralize reactive oxygen species and delay neurodegeneration [159].
Pingchan granule, a traditional Chinese herbal formulation, is composed of nine widely recognized herbs. These include Lycium barbarum L., Taxillus chinensis (DC.) Danser, Gastrodia elata Blume, Paeonia lactiflora Pall., Arisaema erubescens (Wall.) Schott, and Curcuma phaeocaulis Valeton. Additionally, it incorporates Bombyx mori Linnaeus, Buthus martensii Karsch, and Scolopendra subspinipes mutilans L. Koch. Each of these herbs has been carefully selected for their unique medicinal properties and synergistic effects in this composite herbal remedy. A randomized double-blind placebo-controlled trial was conducted on a cohort of 292 mild-to-moderate PD patients across multiple centers. This trial demonstrated the superiority of Pingchan granule over the placebo in managing both motor and non-motor symptoms of PD over a treatment period of 24 weeks. This effect persisted during the 12-week follow-up period. The Pingchan granule group showed better improvements in motor outcomes at timepoints 1, 2, and 3 compared to the placebo group, and demonstrated efficacy across a range of both motor and non-motor symptoms, suggesting the long-term beneficial effects of Pingchan granule on both motor and non-motor symptoms [160] of PD. The results of these trials can provide as strong evidence that the development of natural product-based medicines would be expected to have a very positive effect on PD treatment. However, further research with larger sample sizes and longer study durations is necessary to fully understand their long-term effects and potential in PD treatment.
6. Discussion
PD is a neurodegenerative disorder resulting from the progressive degeneration of dopamine-producing neurons in a brain region called the substantia nigra [161]. A primary pathology of PD is the widespread distribution of abnormal aggregates of the protein α-Syn. [162] This abnormal protein accumulation induces mitochondrial dysfunction, lysosomal disorders, and neuroinflammation, accelerating the death of dopamine-producing neurons [163,164,165]. Currently, medications such as Levodopa, COMT inhibitors, MAO-B inhibitors, and dopamine agonists are used to treat patients with this condition. However, these drugs only slow down the progression of the disease and do not cure it. They fail to fully address various non-motor symptoms like depression and sleep disorders and, thus, can cause various side effects [166,167]. However, various natural products such as curcumin, epigallocatechin gallate (EGCG), resveratrol, and quercetin have demonstrated minimal or negligible side effects, even at higher oral doses, in both animal and human studies [168]. These safety profiles are a primary reason that natural products are increasingly utilized in drug development. These products exhibit considerable advantages in terms of safety, underlining their potential as therapeutic agents in various medical applications.
Currently, due to the inefficacy, resistance issues, and side effects of single synthetic drugs, there is a shift from chemical monotherapy to multi-drug therapy. Multiple mechanisms and genes can be involved in a single disease, requiring multi-drug strategies [169]. Plant extracts contain various bioactive compounds that can interact with multiple targets in the body to produce therapeutic effects. When the multiple compounds in plant extracts interact with different targets, a synergistic effect can occur, enhancing the overall pharmacological impact [170]. Herbal medicine works in a similar manner, with complex interactions among various bioactive ingredients in herbs and herbal formulations leading to synergistic therapeutic effects. Moreover, synergistic interactions between herbal medicine and pharmaceuticals can enhance therapeutic effects or reduce side effects [171]. Therefore, using plant extracts and herbal medicines as therapeutic agents can complement the limitations of current treatments (e.g., levodopa) by acting on pathways not targeted by them.
Clinical trials utilizing herbal medicines and natural products to alleviate PD symptoms demonstrate that these materials exhibit various biological activities and can be extensively applied to target both motor and non-motor symptoms of PD. This suggests that herbal medicines and natural products can be employed in PD treatment, reducing neurotoxicity and improving both motor and non-motor symptoms [152,159,160].
There are limitations when developing drugs based on natural products. Due to the lack of standardized procedures for producing natural products, the quality and composition of natural products intended for medicinal use can vary greatly. Likewise, there is a scarcity of clinical trials conducted under standardized criteria, which subsequently results in insufficient scientific evidence for the therapeutic use of natural products. Thus, more clinical trials and research are required to verify the safety of these natural-product-based treatments in the human body under standardized criteria. Furthermore, because natural products contain a mix of various chemicals acting simultaneously, it is challenging to identify and isolate the active ingredients responsible for specific therapeutic effects. Moreover, research on the biological mechanisms through which these individual components act in the body is limited, calling for further investigation [172].
Author Contributions
Conceptualization, G.Y., J.-H.L. and J.-U.K.; writing—original draft preparation, Y.-J.S., J.-U.L. and G.-S.Y.; writing—review and editing, S.-W.K., G.Y. and J.-H.L.; visualization, Y.-J.S., J.-U.L. and G.-S.Y.; supervision, J.-H.L. and J.-U.K.; funding acquisition, J.-H.L. and J.-U.K. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
Author Jun-Ho Lee was employed by the company Da CaPo Co. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding Statement
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIP) (No. 2021R1A2C1012846), and by the Basic Science Research Program through the NRF, funded by the Ministry of Education (NRF-2021R1I1A1A01059706).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Cho K.h. Korean Medicine Clinical Practice Guideline for Parkinson’s Disease. National Institute for Korean Medicine Development; Seoul, Republic of Korea: 2021. [Google Scholar]
- 2.Hirsch L., Jette N., Frolkis A., Steeves T., Pringsheim T. The Incidence of Parkinson’s Disease: A Systematic Review and Meta-Analysis. Neuroepidemiology. 2016;46:292–300. doi: 10.1159/000445751. [DOI] [PubMed] [Google Scholar]
- 3.Abbas M.M., Xu Z., Tan L.C.S. Epidemiology of Parkinson’s Disease—East Versus. West. Mov. Disord. Clin. Pract. 2018;5:14–28. doi: 10.1002/mdc3.12568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jerry M., Arcona S., McMorrow D., Schwartz H., Princic N., Sasane R. Work Loss and Direct and Indirect Costs Associated with Parkinson’s Disease. Clin. Outcomes Res. 2023;15:309–319. doi: 10.2147/CEOR.S398509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simon D.K., Tanner C.M., Brundin P. Parkinson Disease Epidemiology, Pathology, Genetics, and Pathophysiology. Clin. Geriatr. Med. 2020;36:1–12. doi: 10.1016/j.cger.2019.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Church F.C. Treatment Options for Motor and Non-Motor Symptoms of Parkinson’s Disease. Biomolecules. 2021;11:612. doi: 10.3390/biom11040612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kempster P.A., Williams D.R., Selikhova M., Holton J., Revesz T., Lees A.J. Patterns of levodopa response in Parkinson’s disease: A clinico-pathological study. Brain. 2007;130:2123–2128. doi: 10.1093/brain/awm142. [DOI] [PubMed] [Google Scholar]
- 8.Bäckström D., Granåsen G., Domellöf M.E., Linder J., Jakobson Mo S., Riklund K., Zetterberg H., Blennow K., Forsgren L. Early predictors of mortality in parkinsonism and Parkinson disease: A population-based study. Neurology. 2018;91:e2045–e2056. doi: 10.1212/WNL.0000000000006576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Choi H.G., Lim J.S., Lee Y.K., Sim S., Kim M. Mortality and cause of death in South Korean patients with Parkinson’s disease: A longitudinal follow-up study using a national sample cohort. BMJ Open. 2019;9:e029776. doi: 10.1136/bmjopen-2019-029776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rong S., Xu G., Liu B., Sun Y., Snetselaar L.G., Wallace R.B., Li B., Liao J., Bao W. Trends in Mortality From Parkinson Disease in the United States, 1999–2019. Neurology. 2021;97:e1986–e1993. doi: 10.1212/WNL.0000000000012826. [DOI] [PubMed] [Google Scholar]
- 11.Macleod A.D., Taylor K.S., Counsell C.E. Mortality in Parkinson’s disease: A systematic review and meta-analysis. Mov. Disord. 2014;29:1615–1622. doi: 10.1002/mds.25898. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhuri K.R., Healy D.G., Schapira A.H. Non-motor symptoms of Parkinson’s disease: Diagnosis and management. Lancet Neurol. 2006;5:235–245. doi: 10.1016/S1474-4422(06)70373-8. [DOI] [PubMed] [Google Scholar]
- 13.Schapira A.H.V., Chaudhuri K.R., Jenner P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 2017;18:435–450. doi: 10.1038/nrn.2017.62. [DOI] [PubMed] [Google Scholar]
- 14.Sveinbjornsdottir S. The clinical symptoms of Parkinson’s disease. J. Neurochem. 2016;139((Suppl. S1)):318–324. doi: 10.1111/jnc.13691. [DOI] [PubMed] [Google Scholar]
- 15.Schaeffer E., Postuma R.B., Berg D. Prodromal PD: A new nosological entity. Prog. Brain Res. 2020;252:331–356. doi: 10.1016/bs.pbr.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 16.Crouse J.J., Phillips J.R., Jahanshahi M., Moustafa A.A. Postural instability and falls in Parkinson’s disease. Rev. Neurosci. 2016;27:549–555. doi: 10.1515/revneuro-2016-0002. [DOI] [PubMed] [Google Scholar]
- 17.Palakurthi B., Burugupally S.P. Postural Instability in Parkinson’s Disease: A Review. Brain Sci. 2019;9:239. doi: 10.3390/brainsci9090239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schrag A., Ben-Shlomo Y., Quinn N. How common are complications of Parkinson’s disease? J. Neurol. 2002;249:419–423. doi: 10.1007/s004150200032. [DOI] [PubMed] [Google Scholar]
- 19.Van Den Eeden S.K., Tanner C.M., Bernstein A.L., Fross R.D., Leimpeter A., Bloch D.A., Nelson L.M. Incidence of Parkinson’s disease: Variation by age, gender, and race/ethnicity. Am. J. Epidemiol. 2003;157:1015–1022. doi: 10.1093/aje/kwg068. [DOI] [PubMed] [Google Scholar]
- 20.Armstrong M.J., Okun M.S. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA. 2020;323:548–560. doi: 10.1001/jama.2019.22360. [DOI] [PubMed] [Google Scholar]
- 21.Marino B.L.B., de Souza L.R., Sousa K.P.A., Ferreira J.V., Padilha E.C., da Silva C., Taft C.A., Hage-Melim L.I.S. Parkinson’s Disease: A Review from Pathophysiology to Treatment. Mini Rev. Med. Chem. 2020;20:754–767. doi: 10.2174/1389557519666191104110908. [DOI] [PubMed] [Google Scholar]
- 22.Weintraub D., Aarsland D., Biundo R., Dobkin R., Goldman J., Lewis S. Management of psychiatric and cognitive complications in Parkinson’s disease. BMJ. 2022;379:e068718. doi: 10.1136/bmj-2021-068718. [DOI] [PubMed] [Google Scholar]
- 23.Yang J.Y., Jin C., Lee J., Lee H.G., Cho S.Y., Park S.U., Jung W.S., Moon S.K., Park J.M., Ko C.N., et al. Patients with Parkinson Disease in a Traditional Korean Medicine Hospital: A Five-Year Audit. Evid. Based Complement. Altern. Med. 2021;2021:6842863. doi: 10.1155/2021/6842863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jun P., Zhao H., Kwon O., Jang J.H. Efficacy of Traditional Herbal Medicine Treatment Based on Pattern Identification for Idiopathic Parkinson’s Disease: A Protocol for Systematic Review and Meta-Analysis. Evid. Based Complement. Altern. Med. 2022;2022:4777849. doi: 10.1155/2022/4777849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bae N., Chung S., Kim H.J., Cha J.W., Oh H., Gu M.Y., Oh M.S., Yang H.O. Neuroprotective effect of modified Chungsimyeolda-tang, a traditional Korean herbal formula, via autophagy induction in models of Parkinson’s disease. J. Ethnopharmacol. 2015;159:93–101. doi: 10.1016/j.jep.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Calabresi P., Mechelli A., Natale G., Volpicelli-Daley L., Di Lazzaro G., Ghiglieri V. Alpha-synuclein in Parkinson’s disease and other synucleinopathies: From overt neurodegeneration back to early synaptic dysfunction. Cell Death Dis. 2023;14:176. doi: 10.1038/s41419-023-05672-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dagra A., Miller D.R., Lin M., Gopinath A., Shaerzadeh F., Harris S., Sorrentino Z.A., Støier J.F., Velasco S., Azar J., et al. α-Synuclein-induced dysregulation of neuronal activity contributes to murine dopamine neuron vulnerability. NPJ Park. Dis. 2021;7:76. doi: 10.1038/s41531-021-00210-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Srinivasan E., Chandrasekhar G., Chandrasekar P., Anbarasu K., Vickram A.S., Karunakaran R., Rajasekaran R., Srikumar P.S. Alpha-Synuclein Aggregation in Parkinson’s Disease. Front. Med. 2021;8:736978. doi: 10.3389/fmed.2021.736978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spillantini M.G., Schmidt M.L., Lee V.M., Trojanowski J.Q., Jakes R., Goedert M. Alpha-synuclein in Lewy bodies. Nature. 1997;388:839–840. doi: 10.1038/42166. [DOI] [PubMed] [Google Scholar]
- 30.Breydo L., Wu J.W., Uversky V.N. A-synuclein misfolding and Parkinson’s disease. Biochim. Biophys. Acta. 2012;1822:261–885. doi: 10.1016/j.bbadis.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 31.Vekrellis K., Xilouri M., Emmanouilidou E., Rideout H.J., Stefanis L. Pathological roles of α-synuclein in neurological disorders. Lancet Neurol. 2011;10:1015–1025. doi: 10.1016/S1474-4422(11)70213-7. [DOI] [PubMed] [Google Scholar]
- 32.Cookson M.R. Alpha-Synuclein and neuronal cell death. Mol. Neurodegener. 2009;4:9. doi: 10.1186/1750-1326-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Volpicelli-Daley L.A., Luk K.C., Patel T.P., Tanik S.A., Riddle D.M., Stieber A., Meaney D.F., Trojanowski J.Q., Lee V.M. Exogenous α-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron. 2011;72:57–71. doi: 10.1016/j.neuron.2011.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Luk K.C., Kehm V., Carroll J., Zhang B., O’Brien P., Trojanowski J.Q., Lee V.M. Pathological α-synuclein transmission initiates Parkinson-like neurodegeneration in nontransgenic mice. Science. 2012;338:949–953. doi: 10.1126/science.1227157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olanow C.W., Perl D.P., DeMartino G.N., McNaught K.S. Lewy-body formation is an aggresome-related process: A hypothesis. Lancet Neurol. 2004;3:496–503. doi: 10.1016/S1474-4422(04)00827-0. [DOI] [PubMed] [Google Scholar]
- 36.Lee H.-J., Ricarte D., Ortiz D., Lee S.-J. Models of multiple system atrophy. Exp. Mol. Med. 2019;51:1–10. doi: 10.1038/s12276-019-0346-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee H.-J., Bae E.-J., Lee S.-J. Extracellular α-synuclein—A novel and crucial factor in Lewy body diseases. Nat. Rev. Neurol. 2014;10:92–98. doi: 10.1038/nrneurol.2013.275. [DOI] [PubMed] [Google Scholar]
- 38.McCann H., Cartwright H., Halliday G.M. Neuropathology of α-synuclein propagation and braak hypothesis. Mov. Disord. 2016;31:152–160. doi: 10.1002/mds.26421. [DOI] [PubMed] [Google Scholar]
- 39.Schulz-Schaeffer W.J. The synaptic pathology of alpha-synuclein aggregation in dementia with Lewy bodies, Parkinson’s disease and Parkinson’s disease dementia. Acta Neuropathol. 2010;120:131–143. doi: 10.1007/s00401-010-0711-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kefalopoulou Z., Politis M., Piccini P., Mencacci N., Bhatia K., Jahanshahi M., Widner H., Rehncrona S., Brundin P., Björklund A., et al. Long-term clinical outcome of fetal cell transplantation for Parkinson disease: Two case reports. JAMA Neurol. 2014;71:83–87. doi: 10.1001/jamaneurol.2013.4749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Braak H., Del Tredici K., Rüb U., de Vos R.A., Steur E.N.J., Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol. Aging. 2003;24:197–211. doi: 10.1016/S0197-4580(02)00065-9. [DOI] [PubMed] [Google Scholar]
- 42.Burke R.E., Dauer W.T., Vonsattel J.P. A critical evaluation of the Braak staging scheme for Parkinson’s disease. Ann. Neurol. 2008;64:485–491. doi: 10.1002/ana.21541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ye H., Robak L.A., Yu M., Cykowski M., Shulman J.M. Genetics and Pathogenesis of Parkinson’s Syndrome. Annu. Rev. Pathol. 2023;18:95–121. doi: 10.1146/annurev-pathmechdis-031521-034145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tolosa E., Santamaria J., Gaig C., Compta Y. Chapter 14—Nonmotor Aspects of Parkinson’s Disease. In: Schapira A.H.V., Lang A.E.T., Fahn S., editors. Blue Books of Neurology. Butterworth-Heinemann; Oxford, UK: 2010. pp. 229–251. [Google Scholar]
- 45.Jellinger K.A. Is Braak staging valid for all types of Parkinson’s disease? J. Neural. Transm. 2019;126:423–431. doi: 10.1007/s00702-018-1898-9. [DOI] [PubMed] [Google Scholar]
- 46.Horsager J., Andersen K.B., Knudsen K., Skjærbæk C., Fedorova T.D., Okkels N., Schaeffer E., Bonkat S.K., Geday J., Otto M., et al. Brain-first versus body-first Parkinson’s disease: A multimodal imaging case-control study. Brain. 2020;143:3077–3088. doi: 10.1093/brain/awaa238. [DOI] [PubMed] [Google Scholar]
- 47.Ahn E.H., Kang S.S., Liu X., Chen G., Zhang Z., Chandrasekharan B., Alam A.M., Neish A.S., Cao X., Ye K. Initiation of Parkinson’s disease from gut to brain by δ-secretase. Cell Res. 2020;30:70–87. doi: 10.1038/s41422-019-0241-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Klann E.M., Dissanayake U., Gurrala A., Farrer M., Shukla A.W., Ramirez-Zamora A., Mai V., Vedam-Mai V. The Gut-Brain Axis and Its Relation to Parkinson’s Disease: A Review. Front. Aging Neurosci. 2021;13:782082. doi: 10.3389/fnagi.2021.782082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deng J.H., Zhang H.W., Liu X.L., Deng H.Z., Lin F. Morphological changes in Parkinson’s disease based on magnetic resonance imaging: A mini-review of subcortical structures segmentation and shape analysis. World J. Psychiatry. 2022;12:1356–1366. doi: 10.5498/wjp.v12.i12.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Painous C., Pascual-Diaz S., Muñoz-Moreno E., Sánchez V., Pariente J.C., Prats-Galino A., Soto M., Fernández M., Pérez-Soriano A., Camara A., et al. Midbrain and pons MRI shape analysis and its clinical and CSF correlates in degenerative parkinsonisms: A pilot study. Eur. Radiol. 2023;33:4540–4551. doi: 10.1007/s00330-023-09435-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuzkina A., Rößle J., Seger A., Panzer C., Kohl A., Maltese V., Musacchio T., Blaschke S.J., Tamgüney G., Kaulitz S., et al. Combining skin and olfactory α-synuclein seed amplification assays (SAA)-towards biomarker-driven phenotyping in synucleinopathies. NPJ Park. Dis. 2023;9:79. doi: 10.1038/s41531-023-00519-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kuzkina A., Bargar C., Schmitt D., Rößle J., Wang W., Schubert A.L., Tatsuoka C., Gunzler S.A., Zou W.Q., Volkmann J., et al. Diagnostic value of skin RT-QuIC in Parkinson’s disease: A two-laboratory study. NPJ Park. Dis. 2021;7:99. doi: 10.1038/s41531-021-00242-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fricova D., Harsanyiova J., Trancikova A.K. Alpha-Synuclein in the Gastrointestinal Tract as a Potential Biomarker for Early Detection of Parkinson’s Disease. Int. J. Mol. Sci. 2020;21:8666. doi: 10.3390/ijms21228666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ruffmann C., Bengoa-Vergniory N., Poggiolini I., Ritchie D., Hu M.T., Alegre-Abarrategui J., Parkkinen L. Detection of alpha-synuclein conformational variants from gastro-intestinal biopsy tissue as a potential biomarker for Parkinson’s disease. Neuropathol. Appl. Neurobiol. 2018;44:722–736. doi: 10.1111/nan.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu W., Lim K.L., Tan E.K. Intestine-derived α-synuclein initiates and aggravates pathogenesis of Parkinson’s disease in Drosophila. Transl. Neurodegener. 2022;11:44. doi: 10.1186/s40035-022-00318-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Horsager J., Knudsen K., Sommerauer M. Clinical and imaging evidence of brain-first and body-first Parkinson’s disease. Neurobiol. Dis. 2022;164:105626. doi: 10.1016/j.nbd.2022.105626. [DOI] [PubMed] [Google Scholar]
- 57.Macdonald R., Barnes K., Hastings C., Mortiboys H. Mitochondrial abnormalities in Parkinson’s disease and Alzheimer’s disease: Can mitochondria be targeted therapeutically? Biochem Soc. Trans. 2018;46:891–909. doi: 10.1042/BST20170501. [DOI] [PubMed] [Google Scholar]
- 58.Malpartida A.B., Williamson M., Narendra D.P., Wade-Martins R., Ryan B.J. Mitochondrial Dysfunction and Mitophagy in Parkinson’s Disease: From Mechanism to Therapy. Trends Biochem. Sci. 2021;46:329–343. doi: 10.1016/j.tibs.2020.11.007. [DOI] [PubMed] [Google Scholar]
- 59.Kaur R., Mehan S., Singh S. Understanding multifactorial architecture of Parkinson’s disease: Pathophysiology to management. Neurol. Sci. 2019;40:13–23. doi: 10.1007/s10072-018-3585-x. [DOI] [PubMed] [Google Scholar]
- 60.Charan R.A., Johnson B.N., Zaganelli S., Nardozzi J.D., LaVoie M.J. Inhibition of apoptotic Bax translocation to the mitochondria is a central function of parkin. Cell Death Dis. 2014;5:e1313. doi: 10.1038/cddis.2014.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Drouin-Ouellet J. Mitochondrial complex I deficiency and Parkinson disease. Nat. Rev. Neurosci. 2023;24:193. doi: 10.1038/s41583-023-00676-y. [DOI] [PubMed] [Google Scholar]
- 62.Chen C., McDonald D., Blain A., Mossman E., Atkin K., Marusich M.F., Capaldi R., Bone L., Smith A., Filby A., et al. Parkinson’s disease neurons exhibit alterations in mitochondrial quality control proteins. NPJ Park. Dis. 2023;9:120. doi: 10.1038/s41531-023-00564-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rocha E.M., De Miranda B., Sanders L.H. Alpha-synuclein: Pathology, mitochondrial dysfunction and neuroinflammation in Parkinson’s disease. Neurobiol. Dis. 2018;109:249–257. doi: 10.1016/j.nbd.2017.04.004. [DOI] [PubMed] [Google Scholar]
- 64.O’Hara D.M., Pawar G., Kalia S.K., Kalia L.V. LRRK2 and α-Synuclein: Distinct or Synergistic Players in Parkinson’s Disease? Front. Neurosci. 2020;14:577. doi: 10.3389/fnins.2020.00577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zanon A., Pramstaller P.P., Hicks A.A., Pichler I. Environmental and Genetic Variables Influencing Mitochondrial Health and Parkinson’s Disease Penetrance. Park. Dis. 2018;2018:8684906. doi: 10.1155/2018/8684906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Borsche M., Pereira S.L., Klein C., Grünewald A. Mitochondria and Parkinson’s Disease: Clinical, Molecular, and Translational Aspects. J. Park. Dis. 2021;11:45–60. doi: 10.3233/JPD-201981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Park J.S., Davis R.L., Sue C.M. Mitochondrial Dysfunction in Parkinson’s Disease: New Mechanistic Insights and Therapeutic Perspectives. Curr. Neurol. Neurosci. Rep. 2018;18:21. doi: 10.1007/s11910-018-0829-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Monzio Compagnoni G., Di Fonzo A., Corti S., Comi G.P., Bresolin N., Masliah E. The Role of Mitochondria in Neurodegenerative Diseases: The Lesson from Alzheimer’s Disease and Parkinson’s Disease. Mol. Neurobiol. 2020;57:2959–2980. doi: 10.1007/s12035-020-01926-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Madsen D.A., Schmidt S.I., Blaabjerg M., Meyer M. Interaction between Parkin and α-Synuclein in PARK2-Mediated Parkinson’s Disease. Cells. 2021;10:283. doi: 10.3390/cells10020283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Matheoud D., Sugiura A., Bellemare-Pelletier A., Laplante A., Rondeau C., Chemali M., Fazel A., Bergeron J.J., Trudeau L.E., Burelle Y., et al. Parkinson’s Disease-Related Proteins PINK1 and Parkin Repress Mitochondrial Antigen Presentation. Cell. 2016;166:314–327. doi: 10.1016/j.cell.2016.05.039. [DOI] [PubMed] [Google Scholar]
- 71.Mencke P., Boussaad I., Romano C.D., Kitami T., Linster C.L., Krüger R. The Role of DJ-1 in Cellular Metabolism and Pathophysiological Implications for Parkinson’s Disease. Cells. 2021;10:347. doi: 10.3390/cells10020347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Imberechts D., Kinnart I., Wauters F., Terbeek J., Manders L., Wierda K., Eggermont K., Madeiro R.F., Sue C., Verfaillie C., et al. DJ-1 is an essential downstream mediator in PINK1/parkin-dependent mitophagy. Brain. 2022;145:4368–4384. doi: 10.1093/brain/awac313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ammal Kaidery N., Thomas B. Current perspective of mitochondrial biology in Parkinson’s disease. Neurochem. Int. 2018;117:91–113. doi: 10.1016/j.neuint.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pan T., Kondo S., Le W., Jankovic J. The role of autophagy-lysosome pathway in neurodegeneration associated with Parkinson’s disease. Brain. 2008;131:1969–1978. doi: 10.1093/brain/awm318. [DOI] [PubMed] [Google Scholar]
- 75.Navarro-Romero A., Montpeyó M., Martinez-Vicente M. The Emerging Role of the Lysosome in Parkinson’s Disease. Cells. 2020;9:2399. doi: 10.3390/cells9112399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abe T., Kuwahara T. Targeting of Lysosomal Pathway Genes for Parkinson’s Disease Modification: Insights From Cellular and Animal Models. Front. Neurol. 2021;12:681369. doi: 10.3389/fneur.2021.681369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lehtonen Š., Sonninen T.M., Wojciechowski S., Goldsteins G., Koistinaho J. Dysfunction of Cellular Proteostasis in Parkinson’s Disease. Front. Neurosci. 2019;13:457. doi: 10.3389/fnins.2019.00457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Jackson M.P., Hewitt E.W. Cellular proteostasis: Degradation of misfolded proteins by lysosomes. Essays Biochem. 2016;60:173–180. doi: 10.1042/EBC20160005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Senkevich K., Gan-Or Z. Autophagy lysosomal pathway dysfunction in Parkinson’s disease; evidence from human genetics. Park. Relat. Disord. 2020;73:60–71. doi: 10.1016/j.parkreldis.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 80.Gan-Or Z., Dion P.A., Rouleau G.A. Genetic perspective on the role of the autophagy-lysosome pathway in Parkinson disease. Autophagy. 2015;11:1443–1457. doi: 10.1080/15548627.2015.1067364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Riboldi G.M., Di Fonzo A.B. GBA, Gaucher Disease, and Parkinson’s Disease: From Genetic to Clinic to New Therapeutic Approaches. Cells. 2019;8:364. doi: 10.3390/cells8040364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lwin A., Orvisky E., Goker-Alpan O., LaMarca M.E., Sidransky E. Glucocerebrosidase mutations in subjects with parkinsonism. Mol. Genet. Metab. 2004;81:70–73. doi: 10.1016/j.ymgme.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 83.Steger M., Tonelli F., Ito G., Davies P., Trost M., Vetter M., Wachter S., Lorentzen E., Duddy G., Wilson S., et al. Phosphoproteomics reveals that Parkinson’s disease kinase LRRK2 regulates a subset of Rab GTPases. Elife. 2016;5:e12813. doi: 10.7554/eLife.12813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Orenstein S.J., Kuo S.H., Tasset I., Arias E., Koga H., Fernandez-Carasa I., Cortes E., Honig L.S., Dauer W., Consiglio A., et al. Interplay of LRRK2 with chaperone-mediated autophagy. Nat. Neurosci. 2013;16:394–406. doi: 10.1038/nn.3350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Gómez-Suaga P., Fdez E., Ramírez M.B., Hilfiker S. A Link between Autophagy and the Pathophysiology of LRRK2 in Parkinson’s Disease. Park. Dis. 2012;2012:324521. doi: 10.1155/2012/324521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Teixeira M., Sheta R., Idi W., Oueslati A. Alpha-Synuclein and the Endolysosomal System in Parkinson’s Disease: Guilty by Association. Biomolecules. 2021;11:1333. doi: 10.3390/biom11091333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Vivekanantham S., Shah S., Dewji R., Dewji A., Khatri C., Ologunde R. Neuroinflammation in Parkinson’s disease: Role in neurodegeneration and tissue repair. Int. J. Neurosci. 2015;125:717–725. doi: 10.3109/00207454.2014.982795. [DOI] [PubMed] [Google Scholar]
- 88.Tansey M.G., Wallings R.L., Houser M.C., Herrick M.K., Keating C.E., Joers V. Inflammation and immune dysfunction in Parkinson disease. Nat. Rev. Immunol. 2022;22:657–673. doi: 10.1038/s41577-022-00684-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Qian L., Flood P.M. Microglial cells and Parkinson’s disease. Immunol. Res. 2008;41:155–164. doi: 10.1007/s12026-008-8018-0. [DOI] [PubMed] [Google Scholar]
- 90.Block M.L., Hong J.S. Microglia and inflammation-mediated neurodegeneration: Multiple triggers with a common mechanism. Prog. Neurobiol. 2005;76:77–98. doi: 10.1016/j.pneurobio.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 91.Nakagawa Y., Chiba K. Role of microglial m1/m2 polarization in relapse and remission of psychiatric disorders and diseases. Pharmaceuticals. 2014;7:1028–1048. doi: 10.3390/ph7121028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Butovsky O., Talpalar A.E., Ben-Yaakov K., Schwartz M. Activation of microglia by aggregated beta-amyloid or lipopolysaccharide impairs MHC-II expression and renders them cytotoxic whereas IFN-gamma and IL-4 render them protective. Mol. Cell. Neurosci. 2005;29:381–393. doi: 10.1016/j.mcn.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 93.Zhou X., Spittau B., Krieglstein K. TGFβ signalling plays an important role in IL4-induced alternative activation of microglia. J. Neuroinflammation. 2012;9:210. doi: 10.1186/1742-2094-9-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Guo S., Wang H., Yin Y. Microglia Polarization From M1 to M2 in Neurodegenerative Diseases. Front. Aging Neurosci. 2022;14:815347. doi: 10.3389/fnagi.2022.815347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Isik S., Kiyak B.Y., Akbayir R., Seyhali R., Arpaci T. Microglia Mediated Neuroinflammation in Parkinson’s Disease. Cells. 2023;12:1012. doi: 10.3390/cells12071012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Tang Y., Le W. Differential Roles of M1 and M2 Microglia in Neurodegenerative Diseases. Mol. Neurobiol. 2016;53:1181–1194. doi: 10.1007/s12035-014-9070-5. [DOI] [PubMed] [Google Scholar]
- 97.Jung U.J., Kim S.R. Beneficial Effects of Flavonoids Against Parkinson’s Disease. J. Med. Food. 2018;21:421–432. doi: 10.1089/jmf.2017.4078. [DOI] [PubMed] [Google Scholar]
- 98.Khazdair M.R., Kianmehr M., Anaeigoudari A. Effects of Medicinal Plants and Flavonoids on Parkinson’s Disease: A Review on Basic and Clinical Evidences. Adv. Pharm. Bull. 2021;11:224–232. doi: 10.34172/apb.2021.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Magalingam K.B., Radhakrishnan A.K., Haleagrahara N. Protective Mechanisms of Flavonoids in Parkinson’s Disease. Oxid. Med. Cell. Longev. 2015;2015:314560. doi: 10.1155/2015/314560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chen Y., Peng F., Xing Z., Chen J., Peng C., Li D. Beneficial effects of natural flavonoids on neuroinflammation. Front. Immunol. 2022;13:1006434. doi: 10.3389/fimmu.2022.1006434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lu J., Wang J., Yu L., Cui R., Zhang Y., Ding H., Yan G. Shaoyao-Gancao Decoction Promoted Microglia M2 Polarization via the IL-13-Mediated JAK2/STAT6 Pathway to Alleviate Cerebral Ischemia-Reperfusion Injury. Mediat. Inflamm. 2022;2022:1707122. doi: 10.1155/2022/1707122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wang T., Yin Y., Jiang X., Ruan Y., Xu J., Hu X., Li T., Chu L., Li L. Exploring the mechanism of luteolin by regulating microglia polarization based on network pharmacology and in vitro experiments. Sci. Rep. 2023;13:13767. doi: 10.1038/s41598-023-41101-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zhang T.T., Xue R., Fan S.Y., Fan Q.Y., An L., Li J., Zhu L., Ran Y.H., Zhang L.M., Zhong B.H., et al. Ammoxetine attenuates diabetic neuropathic pain through inhibiting microglial activation and neuroinflammation in the spinal cord. J. Neuroinflammation. 2018;15:176. doi: 10.1186/s12974-018-1216-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Heidari A., Yazdanpanah N., Rezaei N. The role of Toll-like receptors and neuroinflammation in Parkinson’s disease. J. Neuroinflammation. 2022;19:135. doi: 10.1186/s12974-022-02496-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yun S.P., Kam T.I., Panicker N., Kim S., Oh Y., Park J.S., Kwon S.H., Park Y.J., Karuppagounder S.S., Park H., et al. Block of A1 astrocyte conversion by microglia is neuroprotective in models of Parkinson’s disease. Nat. Med. 2018;24:931–938. doi: 10.1038/s41591-018-0051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Yang C., Mo Y., Xu E., Wen H., Wei R., Li S., Zheng J., Li W., Le B., Chen Y., et al. Astragaloside IV ameliorates motor deficits and dopaminergic neuron degeneration via inhibiting neuroinflammation and oxidative stress in a Parkinson’s disease mouse model. Int. Immunopharmacol. 2019;75:105651. doi: 10.1016/j.intimp.2019.05.036. [DOI] [PubMed] [Google Scholar]
- 107.Maciel-Barón L., Moreno-Blas D., Morales-Rosales S.L., González-Puertos V.Y., López-Díazguerrero N.E., Torres C., Castro-Obregón S., Königsberg M. Cellular Senescence, Neurological Function, and Redox State. Antioxid. Redox Signal. 2018;28:1704–1723. doi: 10.1089/ars.2017.7112. [DOI] [PubMed] [Google Scholar]
- 108.Santoro A., Spinelli C.C., Martucciello S., Nori S.L., Capunzo M., Puca A.A., Ciaglia E. Innate immunity and cellular senescence: The good and the bad in the developmental and aged brain. J. Leukoc. Biol. 2018;103:509–524. doi: 10.1002/JLB.3MR0118-003R. [DOI] [PubMed] [Google Scholar]
- 109.Xia M.L., Xie X.H., Ding J.H., Du R.H., Hu G. Astragaloside IV inhibits astrocyte senescence: Implication in Parkinson’s disease. J. Neuroinflammation. 2020;17:105. doi: 10.1186/s12974-020-01791-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Dutta D., Jana M., Majumder M., Mondal S., Roy A., Pahan K. Selective targeting of the TLR2/MyD88/NF-κB pathway reduces α-synuclein spreading in vitro and in vivo. Nat. Commun. 2021;12:5382. doi: 10.1038/s41467-021-25767-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ramirez A.I., de Hoz R., Salobrar-Garcia E., Salazar J.J., Rojas B., Ajoy D., López-Cuenca I., Rojas P., Triviño A., Ramírez J.M. The Role of Microglia in Retinal Neurodegeneration: Alzheimer’s Disease, Parkinson, and Glaucoma. Front. Aging Neurosci. 2017;9:214. doi: 10.3389/fnagi.2017.00214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Qu Y., Li J., Qin Q., Wang D., Zhao J., An K., Mao Z., Min Z., Xiong Y., Li J., et al. A systematic review and meta-analysis of inflammatory biomarkers in Parkinson’s disease. NPJ Park. Dis. 2023;9:18. doi: 10.1038/s41531-023-00449-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Gundersen V. Parkinson’s Disease: Can Targeting Inflammation Be an Effective Neuroprotective Strategy? Front. Neurosci. 2020;14:580311. doi: 10.3389/fnins.2020.580311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nagatsu T., Sawada M. Inflammatory process in Parkinson’s disease: Role for cytokines. Curr. Pharm. Des. 2005;11:999–1016. doi: 10.2174/1381612053381620. [DOI] [PubMed] [Google Scholar]
- 115.Koprich J.B., Reske-Nielsen C., Mithal P., Isacson O. Neuroinflammation mediated by IL-1beta increases susceptibility of dopamine neurons to degeneration in an animal model of Parkinson’s disease. J. Neuroinflammation. 2008;5:8. doi: 10.1186/1742-2094-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.de Bie R.M.A., Clarke C.E., Espay A.J., Fox S.H., Lang A.E. Initiation of pharmacological therapy in Parkinson’s disease: When, why, and how. Lancet Neurol. 2020;19:452–461. doi: 10.1016/S1474-4422(20)30036-3. [DOI] [PubMed] [Google Scholar]
- 117.Ntetsika T., Papathoma P.E., Markaki I. Novel targeted therapies for Parkinson’s disease. Mol. Med. 2021;27:17. doi: 10.1186/s10020-021-00279-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Carrarini C., Russo M., Dono F., Di Pietro M., Rispoli M.G., Di Stefano V., Ferri L., Barbone F., Vitale M., Thomas A., et al. A Stage-Based Approach to Therapy in Parkinson’s Disease. Biomolecules. 2019;9:388. doi: 10.3390/biom9080388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kim S.W., Lee J.H., Kim B., Yang G., Kim J.U. Natural Products as the Potential to Improve Alzheimer’s and Parkinson’s Disease. Int. J. Mol. Sci. 2023;24:8827. doi: 10.3390/ijms24108827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Kwon D.K., Kwatra M., Wang J., Ko H.S. Levodopa-Induced Dyskinesia in Parkinson’s Disease: Pathogenesis and Emerging Treatment Strategies. Cells. 2022;11:3736. doi: 10.3390/cells11233736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Elsworth J.D. Parkinson’s disease treatment: Past, present, and future. J. Neural. Transm. 2020;127:785–791. doi: 10.1007/s00702-020-02167-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kaakkola S. Problems with the present inhibitors and a relevance of new and improved COMT inhibitors in Parkinson’s disease. Int. Rev. Neurobiol. 2010;95:207–225. doi: 10.1016/B978-0-12-381326-8.00009-0. [DOI] [PubMed] [Google Scholar]
- 123.Tan Y.Y., Jenner P., Chen S.D. Monoamine Oxidase-B Inhibitors for the Treatment of Parkinson’s Disease: Past, Present, and Future. J. Park. Dis. 2022;12:477–493. doi: 10.3233/JPD-212976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Malek N.M., Grosset D.G. Investigational agents in the treatment of Parkinson’s disease: Focus on safinamide. J. Exp. Pharmacol. 2012;4:85–90. doi: 10.2147/JEP.S34343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jost W.H. A critical appraisal of MAO-B inhibitors in the treatment of Parkinson’s disease. J. Neural. Transm. 2022;129:723–736. doi: 10.1007/s00702-022-02465-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Borovac J.A. Side effects of a dopamine agonist therapy for Parkinson’s disease: A mini-review of clinical pharmacology. Yale J. Biol. Med. 2016;89:37–47. [PMC free article] [PubMed] [Google Scholar]
- 127.Fan S., Yin Q., Li D., Ma J., Li L., Chai S., Guo H., Yang Z. Anti-neuroinflammatory effects of Eucommia ulmoides Oliv. In a Parkinson’s mouse model through the regulation of p38/JNK-Fosl2 gene expression. J. Ethnopharmacol. 2020;260:113016. doi: 10.1016/j.jep.2020.113016. [DOI] [PubMed] [Google Scholar]
- 128.Li L., Fan S., Zhang W., Li D., Yang Z., Zhuang P., Han J., Guo H., Zhang Y. Duzhong Fang Attenuates the POMC-Derived Neuroinflammation in Parkinsonian Mice. J. Inflamm. Res. 2021;14:3261–3276. doi: 10.2147/JIR.S316314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Jang M., Lee M.J., Lee J.M., Bae C.S., Kim S.H., Ryu J.H., Cho I.H. Oriental medicine Kyung-Ok-Ko prevents and alleviates dehydroepiandrosterone-induced polycystic ovarian syndrome in rats. PLoS ONE. 2014;9:e87623. doi: 10.1371/journal.pone.0087623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Choi J.H., Jang M., Lee J.I., Chung W.S., Cho I.H. Neuroprotective Effects of a Traditional Multi-Herbal Medicine Kyung-Ok-Ko in an Animal Model of Parkinson’s Disease: Inhibition of MAPKs and NF-κB Pathways and Activation of Keap1-Nrf2 Pathway. Front. Pharmacol. 2018;9:1444. doi: 10.3389/fphar.2018.01444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhang Y., Sun H.M., He X., Wang Y.Y., Gao Y.S., Wu H.X., Xu H., Gong X.G., Guo Z.Y. Da-Bu-Yin-Wan and Qian-Zheng-San, two traditional Chinese herbal formulas, up-regulate the expression of mitochondrial subunit NADH dehydrogenase 1 synergistically in the mice model of Parkinson’s disease. J. Ethnopharmacol. 2013;146:363–371. doi: 10.1016/j.jep.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 132.Zhang Y., XGong G., Sun H.M., Guo Z.Y., Hu J.H., Wang Y.Y., Feng W.D., Li L., Li P., Wang Z.Z., et al. Da-Bu-Yin-Wan Improves the Ameliorative Effect of DJ-1 on Mitochondrial Dysfunction Through Augmenting the Akt Phosphorylation in a Cellular Model of Parkinson’s Disease. Front. Pharmacol. 2018;9:1206. doi: 10.3389/fphar.2018.01206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Fenard D., Lambeau G., Maurin T., Lefebvre J.C., Doglio A. A peptide derived from bee venom-secreted phospholipase A2 inhibits replication of T-cell tropic HIV-1 strains via interaction with the CXCR4 chemokine receptor. Mol. Pharmacol. 2001;60:341–347. doi: 10.1124/mol.60.2.341. [DOI] [PubMed] [Google Scholar]
- 134.Nakashima S., Kitamoto K., Arioka M. The catalytic activity, but not receptor binding, of sPLA2s plays a critical role for neurite outgrowth induction in PC12 cells. Brain Res. 2004;1015:207–211. doi: 10.1016/j.brainres.2004.04.069. [DOI] [PubMed] [Google Scholar]
- 135.Ye M., Chung H.S., Lee C., Song J.H., Shim I., Kim Y.S., Bae H. Bee venom phospholipase A2 ameliorates motor dysfunction and modulates microglia activation in Parkinson’s disease alpha-synuclein transgenic mice. Exp. Mol. Med. 2016;48:e244. doi: 10.1038/emm.2016.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kiasalari Z., Khalili M., Baluchnejadmojarad T., Roghani M. Protective Effect of Oral Hesperetin Against Unilateral Striatal 6-Hydroxydopamine Damage in the Rat. Neurochem. Res. 2016;41:1065–1072. doi: 10.1007/s11064-015-1796-6. [DOI] [PubMed] [Google Scholar]
- 137.Zhang B., Yu D., Luo N., Yang C., Zhu Y. Four active monomers from Moutan Cortex exert inhibitory effects against oxidative stress by activating Nrf2/Keap1 signaling pathway. Korean J. Physiol. Pharmacol. 2020;24:373–384. doi: 10.4196/kjpp.2020.24.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Shi X., Chen Y.H., Liu H., Qu H.D. Therapeutic effects of paeonol on methyl-4-phenyl-1,2,3,6-tetrahydropyridine/probenecid-induced Parkinson’s disease in mice. Mol. Med. Rep. 2016;14:2397–2404. doi: 10.3892/mmr.2016.5573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Liu Y., Gao J., Peng M., Meng H., Ma H., Cai P., Xu Y., Zhao Q., Si G. A Review on Central Nervous System Effects of Gastrodin. Front. Pharmacol. 2018;9:24. doi: 10.3389/fphar.2018.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.He J., Li X., Yang S., Li Y., Lin X., Xiu M., Li X., Liu Y. Gastrodin extends the lifespan and protects against neurodegeneration in the Drosophila PINK1 model of Parkinson’s disease. Food Funct. 2021;12:7816–7824. doi: 10.1039/D1FO00847A. [DOI] [PubMed] [Google Scholar]
- 141.Pupyshev A.B., Klyushnik T.P., Akopyan A.A., Singh S.K., Tikhonova M.A. Disaccharide trehalose in experimental therapies for neurodegenerative disorders: Molecular targets and translational potential. Pharmacol. Res. 2022;183:106373. doi: 10.1016/j.phrs.2022.106373. [DOI] [PubMed] [Google Scholar]
- 142.Bastin A.R., Nazari-Robati M., Sadeghi H., Doustimotlagh A.H., Sadeghi A. Trehalose and N-Acetyl Cysteine Alleviate Inflammatory Cytokine Production and Oxidative Stress in LPS-Stimulated Human Peripheral Blood Mononuclear Cells. Immunol. Investig. 2022;51:963–979. doi: 10.1080/08820139.2021.1891095. [DOI] [PubMed] [Google Scholar]
- 143.He Q., Koprich J.B., Wang Y., Yu W.B., Xiao B.G., Brotchie J.M., Wang J. Treatment with Trehalose Prevents Behavioral and Neurochemical Deficits Produced in an AAV α-Synuclein Rat Model of Parkinson’s Disease. Mol. Neurobiol. 2016;53:2258–2268. doi: 10.1007/s12035-015-9173-7. [DOI] [PubMed] [Google Scholar]
- 144.Law B.Y., Mok S.W., Wu A.G., Lam C.W., Yu M.X., Wong V.K. New Potential Pharmacological Functions of Chinese Herbal Medicines via Regulation of Autophagy. Molecules. 2016;21:359. doi: 10.3390/molecules21030359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Chang W.H., Chen C.H., Lu F.J. Different effects of baicalein, baicalin and wogonin on mitochondrial function, glutathione content and cell cycle progression in human hepatoma cell lines. Planta Med. 2002;68:128–132. doi: 10.1055/s-2002-20246. [DOI] [PubMed] [Google Scholar]
- 146.Liu C., Huang X., Qiu S., Chen W., Li W., Zhang H., Wang T., Wang X., Wu X. Chinese Herbal Complex ‘Bu Shen Jie Du Fang’ (BSJDF) Modulated Autophagy in an MPP(+)-Induced Cell Model of Parkinson’s Disease. Evid. Based Complement Altern. Med. 2019;2019:8920813. doi: 10.1155/2019/8920813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Nogueira Neto J.D., de Almeida A.A., da Silva Oliveira J., Santos P.S.D., de Sousa D.P., de Freitas R.M. Antioxidant effects of nerolidol in mice hippocampus after open field test. Neurochem. Res. 2013;38:1861–1870. doi: 10.1007/s11064-013-1092-2. [DOI] [PubMed] [Google Scholar]
- 148.Javed H., Azimullah S., Khair S.B.A., Ojha S., Haque M.E. Neuroprotective effect of nerolidol against neuroinflammation and oxidative stress induced by rotenone. BMC Neurosci. 2016;17:58. doi: 10.1186/s12868-016-0293-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ingole A., Kadam M.P., Dalu A.P., Kute S.M., Mange P.R., Theng V.D., Lahane O.R., Nikas A.P., Kawal Y.V., Nagrik S.U., et al. A review of the pharmacological characteristics of vanillic acid. J. Drug Deliv. Ther. 2021;11:200–204. doi: 10.22270/jddt.v11i2-S.4823. [DOI] [Google Scholar]
- 150.Lu C., Qu S., Zhong Z., Luo H., Lei S.S., Zhong H.J., Su H., Wang Y., Chong C.M. The effects of bioactive components from the rhizome of gastrodia elata blume (Tianma) on the characteristics of Parkinson’s disease. Front. Pharmacol. 2022;13:963327. doi: 10.3389/fphar.2022.963327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Abuthawabeh R., Abuirmeileh A.N., Alzoubi K.H. The beneficial effect of vanillin on 6-hydroxydopamine rat model of Parkinson’s disease. Restor. Neurol. Neurosci. 2020;38:369–373. doi: 10.3233/RNN-201028. [DOI] [PubMed] [Google Scholar]
- 152.Petramfar P., Hajari F., Yousefi G., Azadi S., Hamedi A. Efficacy of oral administration of licorice as an adjunct therapy on improving the symptoms of patients with Parkinson’s disease, A randomized double blinded clinical trial. J. Ethnopharmacol. 2020;247:112226. doi: 10.1016/j.jep.2019.112226. [DOI] [PubMed] [Google Scholar]
- 153.Zargaran A., Zarshenas M.M., Mehdizadeh A., Mohagheghzadeh A. Management of tremor in medieval Persia. J. Hist Neurosci. 2013;22:53–61. doi: 10.1080/0964704X.2012.670475. [DOI] [PubMed] [Google Scholar]
- 154.Chin Y.W., Jung H.A., Liu Y., Su B.N., Castoro J.A., Keller W.J., Pereira M.A., Kinghorn A.D. Anti-oxidant constituents of the roots and stolons of licorice (Glycyrrhiza glabra) J. Agric. Food Chem. 2007;55:4691–4697. doi: 10.1021/jf0703553. [DOI] [PubMed] [Google Scholar]
- 155.Sheela M.L., Ramakrishna M.K., Salimath B.P. Angiogenic and proliferative effects of the cytokine VEGF in Ehrlich ascites tumor cells is inhibited by Glycyrrhiza glabra. Int. Immunopharmacol. 2006;6:494–498. doi: 10.1016/j.intimp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 156.Dhingra D., Sharma A. Antidepressant-like activity of Glycyrrhiza glabra L. in mouse models of immobility tests. Prog. Neuropsychopharmacol. Biol. Psychiatry. 2006;30:449–454. doi: 10.1016/j.pnpbp.2005.11.019. [DOI] [PubMed] [Google Scholar]
- 157.Dhingra D., Parle M., Kulkarni S.K. Memory enhancing activity of Glycyrrhiza glabra in mice. J. Ethnopharmacol. 2004;91:361–365. doi: 10.1016/j.jep.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 158.Yu X.Q., Xue C.C., Zhou Z.W., Li C.G., Du Y.M., Liang J., Zhou S.F. In vitro and in vivo neuroprotective effect and mechanisms of glabridin, a major active isoflavan from Glycyrrhiza glabra (licorice) Life Sci. 2008;82:68–78. doi: 10.1016/j.lfs.2007.10.019. [DOI] [PubMed] [Google Scholar]
- 159.Chahra C., Anis H., Bissene D., Mejda S., Jihène M., Salma N., Manel N., Sana B.A., Hedi K., Maha B.F. The effect of Origanum majorana tea on motor and non-motor symptoms in patients with idiopathic Parkinson’s disease: A randomized controlled pilot study. Park. Relat. Disord. 2021;91:23–27. doi: 10.1016/j.parkreldis.2021.08.013. [DOI] [PubMed] [Google Scholar]
- 160.Gu S.C., Ye Q., Wang C.D., Zhao S.R., Zhou J., Gao C., Zhang Y., Liu Z.G., Yuan C.X. Pingchan Granule for Motor Symptoms and Non-Motor Symptoms of Parkinson’s Disease: A Randomized, Double-Blind, Placebo-Controlled Study. Front. Pharmacol. 2022;13:739194. doi: 10.3389/fphar.2022.739194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Beitz J.M. Parkinson’s disease: A review. Front. Biosci. (Schol. Ed.) 2014;6:65–74. doi: 10.2741/S415. [DOI] [PubMed] [Google Scholar]
- 162.Radhakrishnan D.M., Goyal V. Parkinson’s disease: A review. Neurol. India. 2018;66:S26–S35. doi: 10.4103/0028-3886.226451. [DOI] [PubMed] [Google Scholar]
- 163.Mullin S., Schapira A. α-Synuclein and mitochondrial dysfunction in Parkinson’s disease. Mol. Neurobiol. 2013;47:587–597. doi: 10.1007/s12035-013-8394-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Mazzulli J.R., Zunke F., Isacson O., Studer L., Krainc D. α-Synuclein-induced lysosomal dysfunction occurs through disruptions in protein trafficking in human midbrain synucleinopathy models. Proc. Natl. Acad. Sci. USA. 2016;113:1931–1936. doi: 10.1073/pnas.1520335113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.La Vitola P., Balducci C., Baroni M., Artioli L., Santamaria G., Castiglioni M., Cerovic M., Colombo L., Caldinelli L., Pollegioni L., et al. Peripheral inflammation exacerbates α-synuclein toxicity and neuropathology in Parkinson’s models. Neuropathol. Appl. Neurobiol. 2021;47:43–60. doi: 10.1111/nan.12644. [DOI] [PubMed] [Google Scholar]
- 166.Jankovic J., Aguilar L.G. Current approaches to the treatment of Parkinson’s disease. Neuropsychiatr. Dis. Treat. 2008;4:743–757. doi: 10.2147/NDT.S2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Jankovic J., Tan E.K. Parkinson’s disease: Etiopathogenesis and treatment. J. Neurol. Neurosurg. Psychiatry. 2020;91:795–808. doi: 10.1136/jnnp-2019-322338. [DOI] [PubMed] [Google Scholar]
- 168.Koeberle A., Werz O. Multi-target approach for natural products in inflammation. Drug Discov. Today. 2014;19:1871–1882. doi: 10.1016/j.drudis.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 169.Yang Y., Zhang Z., Li S., Ye X., Li X., He K. Synergy effects of herb extracts: Pharmacokinetics and pharmacodynamic basis. Fitoterapia. 2014;92:133–147. doi: 10.1016/j.fitote.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 170.David B., Wolfender J.-L., Dias D.A. The pharmaceutical industry and natural products: Historical status and new trends. Phytochem. Rev. 2015;14:299–315. doi: 10.1007/s11101-014-9367-z. [DOI] [Google Scholar]
- 171.Zhou X., Seto S.W., Chang D., Kiat H., Razmovski-Naumovski V., Chan K., Bensoussan A. Synergistic Effects of Chinese Herbal Medicine: A Comprehensive Review of Methodology and Current Research. Front. Pharmacol. 2016;7:201. doi: 10.3389/fphar.2016.00201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Thomford N.E., Senthebane D.A., Rowe A., Munro D., Seele P., Maroyi A., Dzobo K. Natural Products for Drug Discovery in the 21st Century: Innovations for Novel Drug Discovery. Int. J. Mol. Sci. 2018;19:1578. doi: 10.3390/ijms19061578. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.