Highlights
-
•
The Promoting Physical Activity in Regional and Remote Cancer Survivors (PPARCS) intervention produced a significant net increase of 50 min/week of moderate-to-vigorous physical activity (MVPA) favoring the intervention.
-
•
PPARCS is the first trial to demonstrate preliminary effectiveness of a low-intensity, distance-based intervention for increasing MVPA in non-metropolitan breast and colorectal cancer survivors (standardized mean difference = 0.56).
-
•
The intervention demonstrates feasibility in terms of reach and acceptability in terms of high levels of engagement.
-
•
Given the low-intensity nature of the intervention and limited resources required (i.e., wearable tracker and phone support), PPARCS would appear to be scalable and could potentially be scaled up and delivered through existing infrastructure such as Cancer Councils nationwide.
Keywords: Behavior change, Exercise, Health disparities, Oncology, Wearable technology
Abstract
Background
Physical activity (PA) is important for cancer survivors. Trials of remotely delivered interventions are needed to assist in reaching under-served non-metropolitan cancer survivors. The objective of this study was to ascertain whether wearable technology, coupled with health coaching was effective in increasing PA in breast and colorectal cancer survivors living in regional and remote areas in Australia.
Methods
Cancer survivors from 5 states were randomized to intervention and control arms. Intervention participants were given a Fitbit Charge 2TM and received up to 6 telephone health coaching sessions. Control participants received PA print materials. Accelerometer assessments at baseline and 12 weeks measured moderate-to-vigorous PA (MVPA), light PA, and sedentary behavior.
Results
Eighty-seven participants were recruited (age = 63 ± 11 years; 74 (85%) female). There was a significant net improvement in MVPA of 49.8 min/week, favoring the intervention group (95% confidence interval (95%CI): 13.6–86.1, p = 0.007). There was also a net increase in MVPA bouts of 39.5 min/week (95%CI: 11.9–67.1, p = 0.005), favoring the intervention group. Both groups improved light PA and sedentary behavior, but there were no between-group differences.
Conclusion
This is the first study to demonstrate that, when compared to standard practice (i.e., PA education), a wearable technology intervention coupled with distance-based health coaching, improves MVPA in non-metropolitan cancer survivors. The results display promise for the use of scalable interventions using smart wearable technology in conjunction with phone-based health coaching to foster increased PA in geographically disadvantaged cancer survivors.
Graphical Abstract
1. Introduction
There were approximately 19.3 million newly diagnosed cancer cases globally in 2020.1 Despite a trend of increasing survival, cancer survivors are at an increased risk of secondary cancers, cardiovascular disease (CVD), and functional decline compared to the general population.2,3 Physical activity (PA) reduces the risk of CVD,4 cancer-related death, and all-cause mortality,5 and it may reduce the risk of recurrence in cancer survivors.5 Sedentary behavior has also been associated with increased mortality in survivors of breast cancer and colorectal cancer (CRC)6 and across mixed cancer types.7 Despite the recognized health benefits of PA, many cancer survivors fail to meet the guidelines of engaging in at least 150 min of aerobic moderate-intensity PA per week and resistance or strength training at least twice a week.8 As a result, insufficiently physically active survivors who fail to make lifestyle changes following treatment are likely to have a substantially higher risk of functional decline, CVD, cancer-related death, and all-cause mortality.
In Australia, breast cancers (29%) and CRC (11%) are the most common cancers in women. In men, prostate (25%) and CRC (12%) are the most commonly diagnosed cancers.9 Pooled data from 8 studies across 4 countries (Australia, Canada, the Netherlands, and the USA) have identified high levels of sedentary behavior in cancer survivors,10 which is consistent with findings specific to Australian breast cancer and CRC survivors.11,12 Breast cancer and CRC survivors account for a significant proportion of the cancer survivor cohort globally.13 Hence they are an important target group for the implementation of PA interventions.
There are also substantial geographic inequalities related to cancer survival.14 Survival rates for Australians who live in non-metropolitan areas are poorer than for those living in major cities.14 Mortality rates for all cancers combined are 1.4 times higher in remote areas when compared to major cities.15 Those living in rural and remote Australia are often disadvantaged in their access to services, education, and income. Furthermore, they are more likely to engage in health behaviors associated with poorer health, including insufficient PA.14,16 Rural cancer survivors are more likely to be obese and physically inactive compared to their urban counterparts.17 Given these disparities, the promotion of PA in non-metropolitan cancer survivors is an important endeavor. However, existing PA programs for survivors tend to be facility-based and in major cities. Previous work with survivors has identified cost along with availability of and access to exercise programs to be significant barriers to participation.18, 19, 20 Effective, distance-based PA interventions have the potential to reduce inequalities in health for non-metropolitan cancer survivors by reducing inequality in PA engagement.
Even internationally there have been very few distance-based PA interventions to recruit rural cancer survivors specifically.21 These interventions have tended to be intensive, with 16–24 telephone sessions over 6 months,22,23 and have produced mixed findings. Eakin et al.22 conducted a trial involving 16 telephone calls over 8 months and found no effect on moderate-to-vigorous PA (MVPA) in rural breast cancer survivors at follow up (approximately 2 months post intervention). In contrast, Fazzino et al.23 reported on a weight management intervention which showed a significant increase in MVPA of 46.9 min/week following 6 months of weekly group phone sessions exploring effectiveness and maintenance. Following the 6 month intensive phase, participants either engaged in biweekly group phone sessions for a further 12 months or received a biweekly newsletter. MVPA at 18 months reduced but remained significantly higher than baseline (18.4 min/week vs. 38.1 min/week). Further, only 1 study to date in rural cancer survivors has used a device-based assessment of PA, but it did not include a control group.23 Overall, there is a gap in the current literature on the effectiveness of scalable, less intensive distance-based interventions that can be delivered to cancer survivors living in non-metropolitan areas.
Wearable activity trackers (wearables) hold potential as a low-cost self-monitoring tool, and their associated applications (Apps) offer several evidence-based behavior change techniques (BCTs), including self-monitoring, goal-setting, and feedback.24,25 Research using “smart” wearables in conjunction with health coaching (The ACTIVity and Technology (ACTIVATE) Trial) or group sessions (Wearable Activity Technology And Action-Planning (WATAAP)) have shown promise in increasing MVPA, albeit in metropolitan cancer survivors.26, 27, 28 To our knowledge, the present trial is the first to combine “smart” wearables with telephone health coaching in an entirely distance-based intervention to improve PA and reduce sedentary behavior in non-metropolitan cancer survivors. It is also the first national study to promote PA to regional and remote cancer survivors in Australia.
The primary aim of the Promoting Physical Activity in Regional and Remote Cancer Survivors (PPARCS) trial was to ascertain whether smart wearable technology, in conjunction with health coaching, is effective for increasing MVPA in breast cancer and CRC survivors residing in regional and remote Australia. A secondary aim was to assess the effectiveness of the PPARCS intervention for reducing sedentary behavior.
2. Methods
The trial was a 2-arm multicenter randomized controlled trial (RCT) conducted across 5 Australian states (New South Wales, Victoria, Western Australia, South Australia, and Tasmania). The study was approved by the St. John of God Human Research Ethics Committee (Reference #1201) and registered (ACTRN12618001743257). Written informed consent was obtained from participants prior to enrollment.
2.1. Participants
Participants included adult breast cancer and CRC survivors who had completed active cancer treatment in the 5 years prior to recruitment. Full eligibility criteria have been published previously.29 In brief, participants were recruited based on (a) remoteness and (b) low levels of PA. Remoteness was measured according to the accessibility/remoteness index of Australia and the Australian Statistical Geography Standard, which define 5 statistical areas: major cities, inner regional, outer regional, remote, and very remote.30 For international comparison, approximately 28% of Australians reside in regional and remote areas. Approximately 4,608,000 (17.9%) and 2,067,000 (8%) reside in inner and outer regional areas, respectively. A further 291,000 (1.1%) and 201,000 (0.8%) reside in remote and very remote areas, respectively.31 Eligible participants resided in either a regional or remote area, were insufficiently physically active (i.e., engaging in <150 min of moderate-intensity or 75 min of vigorous-intensity PA per week), and had access to the internet via a computer or smartphone.8 Insufficient PA was determined according to the older guidelines (i.e., accumulating <150 min of MVPA per week in bouts of at least 10 min), which were assessed during phone screening using the Active Australia Survey.32 One individual who expressed interest in participating was deemed ineligible due to having no internet access. Another participant had internet access but no smartphone. In this case, the participant was mailed a second-hand smartphone to enable access to the Fitbit App (Fitbit LLC, San Francisco, CA, USA). All other individuals screened on internet and phone access met the inclusion criteria.
2.2. Recruitment
Eligible participants were identified from oncologists’ medical records and were mailed a participant information sheet and invitation letter from their treating surgical, medical, or radiation oncologist. Individuals who expressed interest were screened by telephone to ensure eligibility prior to recruitment. On receipt of written consent, participants were telephoned and an initial screening questionnaire (which included the Active Australia Survey32 to assess PA status) was administered to determine eligibility.
2.3. Randomization
Following baseline assessments, an independent statistician, who was blinded to the assessments and intervention, randomized participants using consecutive randomization codes (STATA Version15; StataCorp., College Station, TX, USA) with a 1:1 allocation in block sizes of 4 and 6 to support allocation concealment. Participant allocation was implemented using sequentially numbered envelopes that were opaque and sealed. Following consent and baseline assessment, the trial coordinator opened the next envelope in the sequence and wrote the participant study number onto it prior to allocating the participant to that group. Carbon paper inside the envelope transferred the number onto the card containing the details of allocation. If the participant was allocated to the intervention group, the trial coordinator mailed out a Fitbit Charge 2TM (Fitbit LLC) along with detailed instructions on tracker set-up and functions. Further, the name and contact details of the participant were emailed to the health coach to arrange the first health-coaching session.
2.4. Design
2.4.1. Intervention arm
The 12-week intervention consisted of 2 components, which have been described previously.29
-
1.
Smart tracker: The Fitbit Charge 2TM (Fitbit LLC) is a wrist-worn device that displays steps, distance, heart rate, and active minutes while providing automated prompts to nudge participants to accumulate at least 250 step/h. The Fitbit Charge 2TM was chosen because previous work has demonstrated its usefulness and acceptance among survivors33 and older adults (>70 years).34 Data from the device is uploaded to the Fitbit App via Bluetooth.
-
2.
Health coaching: The purpose of the telephone health coaching was to motivate increased PA and reduced sedentary behavior by supporting participants’ self-efficacy, action planning, and problem solving. The first session (Week 1; up to 60 min) covered technical issues and features of the Fitbit. The first session sought to foster positive outcome expectancies and confidence towards PA by emphasizing the importance of MVPA and providing information on the risks of inactivity, and by guiding participants to create action plans for self-monitoring their PA over the following 3 weeks. Three follow-up sessions (Weeks 2, 4, and 8; approximate 30 min each) provided feedback on PA behavior, assistance with problem solving, and support with updating goals and action plans as they progressed. A patient-centered and stepped-care approach was adopted by providing additional health-coaching sessions (i.e., at Weeks 6 and 10) to those who may need them to achieve meaningful sustained PA change. The weekly exercise target was at least 180 min of moderate-intensity PA, based on research demonstrating better long-term survival in cancer survivors who engaged in 3–5 h of moderate activity per week.35,36
2.4.2. Control arm
This group received a mailed booklet (which was also given to the intervention group) designed to educate and motivate improvements in PA. The booklet provided was called “Exercise for People Living with Cancer” (2016 edition, reprinted 2017 (https://www.cancer.org.au)). It is freely available from Cancer Council Australia, widely distributed, and as such, represents usual care.
2.4.3. Assessments
Data collection was conducted remotely at baseline (T1) and Week 12 (T2). Once eligibility was confirmed, participants were mailed the study questionnaire, an ActiGraph GTX9 accelerometer (ActiGraph, Pensacola, FL, USA), written accelerometer instructions, and a reply-paid satchel.
2.5. Outcome measures
2.5.1. PA
The ActiGraph GT9X accelerometer (ActiGraph) was used to ascertain min/week of MVPA. Participants wore the accelerometer on their right hip for all waking hours across 7 consecutive days at each assessment time point. Wear-time had to exceed 10 h/day and contain no excessive counts (>20,000) to be considered valid, with non-wear-time defined as at least 60 consecutive min of 0 counts.37 Data were processed using 60-s epochs. Daily accelerometer logs were completed by participants to allow for cross-checking of data. Freedson cut-points38 were adopted as follows: sedentary (<100 counts per minute (cpm)), light (100 to <1952 cpm), moderate (1952–5724 cpm), vigorous (5725+ cpm), and MVPA (1952+ cpm). Total duration of MVPA was examined as both weekly time accumulated (min/week) and time in bouts of at least 10 consecutive minutes (MV10; min/week) using a modified 10+ min bouts/week minus 2 min hesitation.
2.5.2. Sedentary behavior
Sedentary behavior was defined by accelerometer activity counts of <100 cpm for 20 consecutive minutes or more, which corresponds to clinical changes in cardiometabolic biomarkers.39 The accelerometer log assisted in differentiating sedentary time from non-wear time.
2.6. Covariates
Sociodemographic information and comorbidities were self-reported. The following variables were collected: gender, age, ethnicity, marital status, educational attainment, gross household income, cancer treatment. Comorbidity was assessed using the Self-administered Comorbidity Questionnaire.40 The Self-administered Comorbidity Questionnaire includes 12 medical conditions, and participants have the option of indicating 3 additional conditions. Up to 3 points are allocated to each condition (i.e., one for the condition, one for the treatment, and an additional point if the condition causes a limitation in functioning).
2.7. Sample size
The primary outcome variable was total minutes of MVPA. A sample size of 86 participants was required to achieve 80% power to detect an arm by time interaction at the 0.05 level. Our calculations are based on the covariance matrix from a previous trial in survivors that used accelerometers to assess MVPA27 assuming a 70 min/week increase in MVPA at T2 in the intervention group but no change in the control arm.
2.8. Statistical methods
Demographic characteristics at baseline are reported for both groups (Table 1). MVPA and secondary outcome variables were analyzed using linear mixed models with arm, time, and their interaction included as fixed effects, and participant as a random effect. All available data were included based on the random allocation to group.
Table 1.
Baseline characteristics of participants.
| Overall (n = 87) | Intervention (n = 43) | Control (n = 44) | |
|---|---|---|---|
| Age (year) | 63.1 ± 11.1 | 63.7 ± 10.1 | 62.6 ± 11.8 |
| Gender (female) | 74 (85.1) | 38 (88.4) | 36 (81.8) |
| Marital status | |||
| Married/in a relationship | 64 (73.6) | 32 (74.4) | 32 (72.7) |
| Divorced/separated | 9 (10.4) | 6 (13.9) | 3 (6.8) |
| Single | 7 (8.0) | 0 (0.0) | 7 (15.9) |
| Widowed | 7 (8.0) | 5 (5.7) | 2 (5.6) |
| Education | |||
| University degree | 26 (30) | 14 (33) | 12 (27) |
| Post-school training | 29 (33) | 13 (30) | 16 (36) |
| High school | 28 (32) | 13 (30) | 15 (34) |
| Other/no qualifications | 4 (5) | 3 (7) | 1 (3) |
| Household income (AUD) | |||
| ≤30,000 | 19 (22) | 12 (28) | 7 (16) |
| 30,001–52,000 | 20 (23) | 5 (12) | 15 (34) |
| 52,001–104,000 | 23 (26) | 11 (26) | 12 (27) |
| 104,001–156,000 | 11 (13) | 6 (14) | 5 (11) |
| >156,000 | 8 (19) | 4 (9) | 5 (9) |
| Missing | 6 (7) | 5 (11) | 1 (3) |
| Australian state | |||
| New South Wales | 53 (61.0) | 28 (65.1) | 25 (56.8) |
| Victoria | 17 (19.5) | 8 (18.6) | 9 (20.4) |
| Western Australia | 14 (16.1) | 6 (14.0) | 8 (18.2) |
| South Australia | 2 (2.3) | 1 (2.3) | 1 (2.3) |
| Tasmania | 1 (1.1) | 0 (0.0) | 1 (2.3) |
| Cancer type | |||
| Breast | 66 (75.9) | 34 (79.1) | 32 (72.7) |
| Colorectal | 21 (24.1) | 9 (20.9) | 12 (27.3) |
| Comorbidity score | 6.5 ± 5.1 | 6.5 ± 4.9 | 6.5 ± 5.4 |
| Months since diagnosisa | 24.8 ± 12.7 | 25.1 ± 12.4 | 24.5 ± 13.1 |
| Treatment | |||
| Surgery only | 13 (15.0) | 8 (19.0) | 5 (11.0) |
| Surgery with chemotherapy | 47 (54.0) | 19 (44.0) | 28 (64.0) |
| Surgery with radiation therapy | 53 (60.9) | 26 (59.1) | 27 (62.8) |
| Hormone therapy | 31 (35.6) | 17 (38.6) | 14 (32.6) |
| Remoteness classification | |||
| Inner regional | 32 (36.9) | 16 (37.2) | 16 (36.4) |
| Outer regional | 51 (58.6) | 25 (58.2) | 26 (59.1) |
| Remote | 3 (3.4) | 1 (2.3) | 2 (4.5) |
| Very remote | 1 (1.1) | 1 (2.3) | 0 (0.0) |
Note: Data are presented as mean ± SD or n (%).
Abbreviation: AUD = Australian dollar.
Months since diagnosis (mean ± SD) was available for Control (n = 30) and Intervention (n = 29) participants.
Sensitivity analyses included refitting the models to exclude participants who recorded T1 MVPA of ≥150 min/week (Supplementary Table 1). This was a post hoc decision given the unanticipated finding that these participants were more active than reported at screening. Further planned sensitivity analyses involved refitting the above models by (a) adjusting them for accelerometer wear-time, age, gender, cancer type, comorbidity index, and remoteness (inner regional vs. other) (Supplementary Table 2); and (b) excluding participants from the intervention group who did not attend 4 or more health-coaching sessions (Supplementary Table 1). These results were consistent with the initial analyses.
All models were assessed for goodness of fit via inspection of residuals. Standard errors for the MV10 outcome were bootstrapped (1000 repetitions) using cluster resampling due to deviations from this. All analyses were conducted in STATA Version17 (StataCorp) and p < 0.05 was considered evidence to infer an effect.
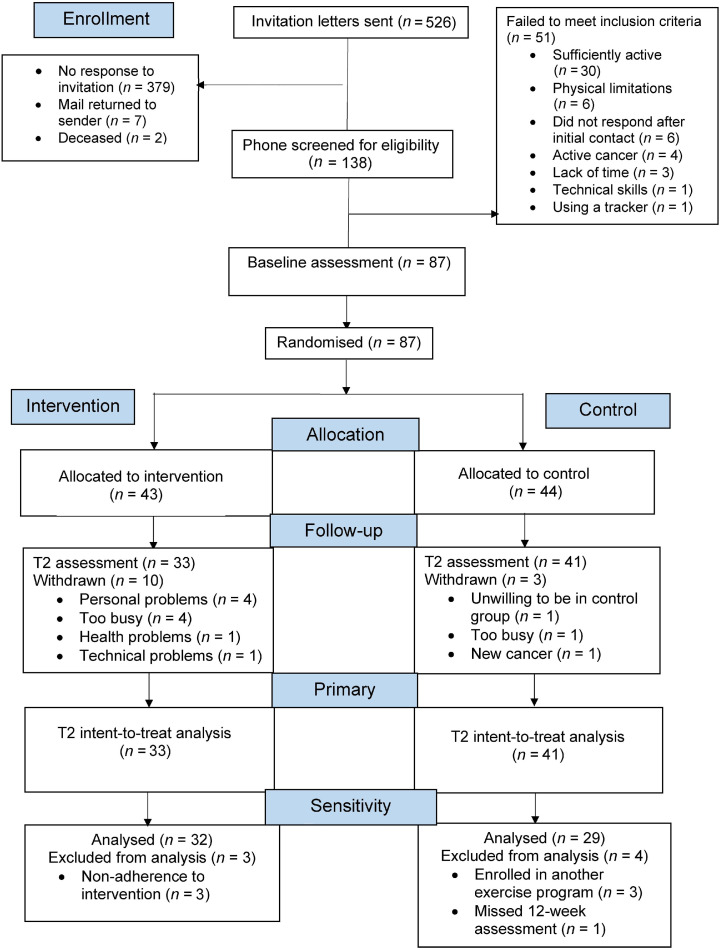
3. Results
Fig. 1 displays the flow of randomized participants to intervention (n = 43) and control (n = 44) groups. Compared to those who did not respond to the initial invitation, responders were similar in geographical remoteness (inner regional vs. outer regional/remote/very remote, p = 0.085) and more likely to be women (p = 0.020).
Fig. 1.
CONSORT diagram of trial. CONSORT = Consolidated Standards of Reporting Trials; T2 = 12-weeks following baseline.
Demographic characteristics were similar across groups at baseline (Table 1). Seventy-four participants (85%) remained in the trial at T2. Those who remained at T2 did not differ from those who did not by age (64.0 ± 12.7 vs. 61.0 ± 10.7, mean ± SD; t (16.7) = –0.63, p = 0.537), gender (100% vs. 82% women, Fisher's exact test p = 0.116), months since diagnosis (24.1 ± 12.4 vs. 29.1 ± 14.4, t (8.7) = 0.98, p = 0.352), or cancer type (CRC 24.7% vs. 21.4%, breast cancer 75.3% vs. 78.6%, Fisher's exact test p = 1.0). However, the proportion of participants who did not complete T2 differed between study arms, with 74% in the intervention arm completing T2, compared to 93% in the control arm (Fisher's exact test p = 0.021). Intervention completers had higher T1 MVPA levels (150.3 ± 108.3 min/week vs. 62.9 ± 65.8 min/week, t (22.6) = –3.1, p = 0.004), whereas control completers had lower T1 MVPA, albeit with no statistical evidence for this difference (126.1 ± 119.5 min/week vs. 178.7 ± 112.4 min/week, t (2.3) = 0.78, p = 0.507) (Supplementary Table 1).
Health-coaching session attendance was high, with a mean attendance of (4.7 ±1.7) sessions and (138 ± 63) min of health coaching. Fitbit engagement was high, with 94.6% of valid wear-days over 12 weeks for those with T2 data (n = 32) (Supplementary Table 1). A step count of ≥1000 step/day was considered a valid wear-day. Fitbit data was missing for 9 participants; 7 of these participants dropped out of the trial, and 2 experienced syncing errors. Despite all participants reporting as insufficiently active during phone screening, 32 participants (37%) completed ≥150 min/week of MVPA at baseline, although few (9%) were achieving higher levels of MVPA (i.e., ≥ 300 min/week of MVPA).
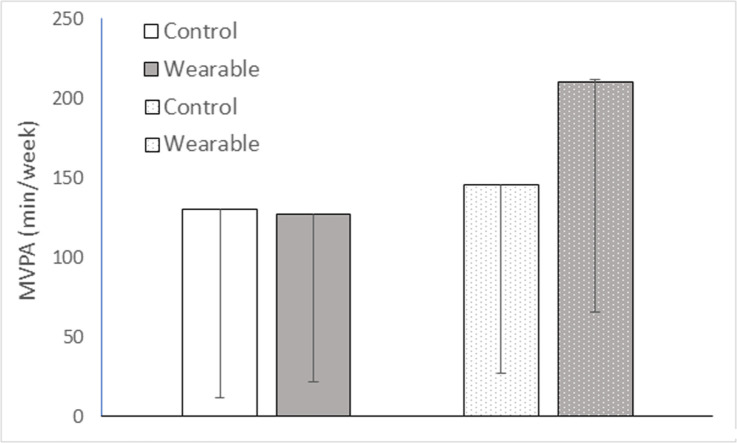
The mean (SD) for all variables in each arm at T1 and T2 are shown in Table 2. Compared with controls, the intervention group had a significant net mean increase in MVPA of 49.8 min/week (95% confidence interval (95%CI): 13.6–86.1, p = 0.007) (Table 3). There was also a net increase in MVPA bouts (i.e., MVPA performed in bouts of ≥10 min) of 39.5 min/week (95%CI: 11.9–67.1, p = 0.005) favoring the intervention group (Table 3).
Table 2.
Observed means and SD for ActiGraph measures at T1 (Baseline) and T2 (Week 12) for Control and Intervention groups.
| T1 |
T2 |
|||
|---|---|---|---|---|
| Outcome | Control (n = 44) | Intervention (n = 42) | Control (n = 41) | Intervention (n = 32) |
| MVPA (min/week) | 129.7 ± 118.5 | 127.4 ± 105.6 | 145.9 ± 119.2 | 210.6 ±145.1 |
| MV10 (min/week) | 28.5 ± 45.4 | 17.4 ± 38.0 | 39.0 ± 63.6 | 68.6 ± 68.8 |
| Moderate PA (min/week) | 128.9 ± 117.1 | 125.6 ± 101.2 | 141.6 ± 115.0 | 204.3 ±142.6 |
| Light PA (min/week) | 2165.9 ± 631.0 | 2160.9 ± 610.0 | 2267.7 ± 649.2 | 2433.9 ± 658.7 |
| Sedentary time (min/week) | 3604.1 ± 624.7 | 3633.8 ± 589.5 | 3493.0 ± 707.9 | 3422.6 ± 688.1 |
| Sedentary time (≥20-min bouts) (min/week) | 1513.4 ± 663.4 | 1578.5 ± 713.5 | 1527.6 ± 678.0 | 1484.4 ± 714.0 |
| Valid wear-days (day) | 6.7 ± 0.6 | 6.8 ± 0.6 | 6.6 ± 0.9 | 6.9 ± 0.6 |
| Wear-time (min/day) | 842.8 ± 66.7 | 846.0± 61.7 | 843.8 ± 76.1 | 865.1 ± 63.1 |
Data are presented as mean ± SD.
Abbreviations: MV10 = minutes of moderate-to-vigorous physical activity completed in bouts of at least 10 min; MVPA = moderate-to-vigorous physical activity; PA = physical activity; T1= baseline; T2 = 12-weeks following baseline.
Table 3.
Estimated between arm (Intervention change–Control change at T2) and within arm (T2–T1) mean differences (95%CI) for MVPA and secondary ActiGraph outcomes.
| ActiGraph outcomes | Intervention change–Control change T2 |
Arm × Time interactiona |
Intervention change (T2–T1) |
Control change (T2–T1) |
||||
|---|---|---|---|---|---|---|---|---|
| Net mean difference | 95%CI | χ2(1)b | p | Mean difference | 95%CI | Mean difference | 95%CI | |
| MVPA (min/week) | 49.8 | 13.6 to 86.1 | 7.27 | 0.007 | 68.7 | 41.5 to 95.9 | 18.9 | –5.1 to 42.8 |
| MV10 (min/week) | 39.5 | 11.9 to 67.1 | 7.88 | 0.005 | 49.8 | 27.7 to 72.0 | 10.3 | –5.4 to 26.1 |
| Moderate PA (min/week) | 49.5 | 13.0 to 85.9 | 7.09 | 0.008 | 64.8 | 37.5 to 92.1 | 15.3 | –8.8 to 39.4 |
| Light PA (min/week) | 30.5 | 143.7 to 204.8 | 0.12 | 0.731 | 158.7 | 27.8 to 289.6 | 128.2 | 13.1 to 243.2 |
| Sedentary time (min/week) | –65.2 | –2707 to 140.4 | 0.39 | 0.534 | –194.5 | –348.7 to –40.4 | –129.4 | –265.4 to 6.6 |
| Sedentary time (≥20-min bouts) (min/week) | –55.6 | –271.8 to 160.7 | 0.25 | 0.615 | –65.2 | –227.4 to 96.9 | –9.7 | –152.7 to 133.4 |
Abbreviations: 95%CI = 95% confidence interval; MV10 = minutes of moderate-to-vigorous physical activity completed in bouts of at least 10 min; MVPA = moderate-to-vigorous physical activity; PA = physical activity; T1= baseline; T2 = 12-weeks following baseline.
Bold font denotes a statistically significant result. Mean differences are estimated from the mixed model; they will be slightly different from those calculated from observed means (Table 2) due to the estimation process.
Wald χ2 test for the Arm × Time interaction.
As shown in Supplementary Table 1, 64% (n = 28) of control participants and 62% (n = 26) of the intervention group were insufficiently active at T1. Limiting the sample to only those insufficiently active, the net intervention effect was reduced to 30.4 min/week MVPA (95%CI: –4.2 to 65.0, p = 0.085). The increase in the intervention group was still 61 min/week (95%CI: 34.3–87.6); however, the control group increased by 30.6 (95%CI: 8.5–52.7) min/week.
4. Discussion
Our trial is the first to utilize “smart” wearables in combination with health coaching in a distance-based intervention to increase PA in under-served, non-metropolitan breast cancer and CRC survivors. Intention-to-treat analyses revealed a significant between-group net difference of 50 min/week of MVPA favoring the intervention group (a 69-min/week increase in the intervention group). The net improvement generated by the PPARCS intervention is promising given that more intensive face-to-face PA counseling interventions in survivors have yielded a similar improvement, equivalent to approximate 47 min/week of MVPA.41 Sedentary behavior improved in both groups, although there were no significant differences between the groups.
Recruitment to PPARCS was modest, with a 26.7% response rate, but comparable with other trials in cancer survivors that have used direct mailing approaches.42,43 For example, Befort et al.43 achieved a response rate of 13.6% in their study recruiting rural breast cancer survivors. In a similar smart wearable intervention, WATAAP achieved a comparable response rate of 23% through direct mailing of endometrial cancer and CRC survivors in Australia.27 Retention (85%) was comparable to previous PA interventions that included rural cancer survivors, with an average retention rate of 82%.41 Given that only 1 individual was deemed ineligible to participate due to having no internet access, the present study supports the feasibility of smart wearable interventions in non-metropolitan cancer survivors.
Even following rigorous screening, over one-third of the sample reported achieving the minimal PA guidelines at baseline, perhaps stimulated by study recruitment. However, very few (8%) were achieving high levels of MVPA (more than 300 min/week), providing scope for improvement. The largest reductions in CVD risk and mortality are obtained when MVPA exceeds recommended guidelines by 3–5 times.44,45 The recruitment of more physically active survivors in this study may be related to greater levels of occupational and domestic PA in rural areas, due to physically demanding jobs (e.g., farming) and larger properties/yards to maintain. Vaughan et al.46 found that from a sample of 490 men living in rural Australia, 45% were involved in agriculture, forestry, or fishing occupations and 66% reported high levels of occupational PA. It should be noted that while occupational MVPA counts towards achieving the recommended PA guidelines, research has observed that it is negatively related to quality of life in breast cancer survivors.47
There have been very few PA interventions that have specifically recruited rural cancer survivors. Of the 5 RCTs included in Mama et al.’s review,21 none reported improvements in MVPA compared to controls. Limitations of previous studies in rural cancer survivors include intensive high-contact interventions (e.g., median intervention contact time was 467 min21), the inclusion of metropolitan cancer survivors,48 self-reported PA, and interventions focused on multiple health behaviors rather than PA alone.23 This is an area in which scalable interventions are greatly needed to increase PA in under-served regional and remote cancer survivors.
The PPARCS trial represents a low-cost and low-intensity intervention that may be scalable. Scalability requires consideration of a range of dimensions, including feasibility, acceptability, effectiveness, cost, fidelity/intervention adaptability (i.e., an intervention that is sufficiently flexible to meet the needs of the context in which it is to be scaled-up), implementation infrastructure, and sustainability.49 In recognition of these dimensions, Milat and colleagues50 have developed the Intervention Scalability Assessment Tool to support policy makers and practitioners as they make a comprehensive assessment of the suitability of an intervention for scale-up. In relation to the scale-up of PPARCS, further research (including a larger definitive trial of PPARCS with a longer follow up) is required to demonstrate effectiveness. However, the present study provides preliminary evidence of the potential for scale-up of this intervention in terms of its feasibility, acceptability, initial effectiveness, and cost. For example, the intervention demonstrates feasibility in reaching non-metropolitan cancer survivors with an entirely distance-based intervention and acceptability in terms of its high levels of engagement. The present study also provides evidence of the initial effectiveness of the intervention for increasing MVPA. Given the low-intensity nature of the intervention and the limited resources required (i.e., wearable tracker and phone support), PPARCS would appear to be scalable in terms of cost. Its delivery to non-metropolitan cancer survivors could potentially be scaled up within the existing infrastructure, such as through Cancer Council nurses nationwide or through outpatient oncology services. The PPARCS intervention is the first to demonstrate a significant between-group increase of 50 min/week in MVPA from baseline to follow up in rural cancer survivors. Notwithstanding the obvious advantages of remotely delivered interventions, a review51 revealed only a small effect of 0.21 (standardized mean difference (SMD)) for distance-based PA interventions compared to the moderate effect of 0.56 (SMD) observed in the PPARCS trial. Most interventions included in the review utilized print and telephone modes of delivery,51 but few used electronic health platforms or smart technology such as wearables.
Recent reviews suggest that wearables are an effective tool for increasing PA in cancer survivors.52, 53, 54 The most recent meta-analysis on wearables in cancer survivors provides strong support for wearable interventions. Across interventions of between 4 weeks and 1 year (median = 12 weeks), wearables had moderate-to-large effects on moderate-intensity PA (SMD = 0.87) and MVPA (SMD = 0.61) in cancer survivors.53 Wearable interventions in cancer survivors show promise, with significant increases in MVPA of 99 min/week, 66 min/week, and 45 min/week between baseline and 12 weeks compared to controls in the Memory and Motion, ACTIVATE, and WATAAP interventions, respectively.26,27,55 Increased MVPA was maintained at 6 months in the WATAAP trial.28
Interventions that utilize smart wearables may be particularly helpful for increasing PA in geographically disadvantaged cancer survivors since interventions can be delivered, and participant wearable data monitored, remotely. Further, evidence-based BCTs such as self-monitoring and feedback on performance are now incorporated into smart-tracker technology. Therefore, the impact of these BCTs should theoretically continue following cessation of an intervention, provided the participant continues to engage with the tracker. As such, wearables could represent cost-effective and scalable tools suited to reaching under-served cancer survivors who reside in rural areas. In relation to the “active ingredients” in PPARCS, self-monitoring in conjunction with goal setting and feedback on performance appear, from a cursory examination of the process evaluation data, to be the most utilized BCTs among participants. Reviews also support the role of self-monitoring of behavior41,56,57 and goal setting56,57 for PA behavior change in cancer survivors.
Limitations include a relatively brief intervention period and low recruitment of participants residing in remote or very remote areas. Our sample may be subject to a participation bias, as it is likely we have recruited a more motivated cohort. Further, the ActiGraph, worn on the hip, may have overestimated sedentary behavior (i.e., by classifying time spent standing as sedentary time). However, this would not have affected our primary outcome, which was MVPA. Given the short-term follow up, the efficacy of the intervention for sustained PA behavior change is undetermined.
5. Conclusion
PPARCS was the first trial to demonstrate the preliminary effectiveness of a low-intensity, distance-based intervention for increasing MVPA in regional and remote cancer survivors. We found a between-group net difference in MVPA of 50 min/week favoring the intervention group. The findings show great promise in a group that is geographically and socially disadvantaged and difficult to reach, and where scalable interventions are greatly needed. Remotely delivered interventions such as PPARCS can make a difference.
The PPARCS intervention yielded a significant and clinically meaningful increase in MVPA compared to controls, displaying promise for the use of low-intensity and purely distance-based interventions using smart wearables. Further examination of the extended-term efficacy of wearables for PA maintenance is essential.
Acknowledgments
Acknowledgments
This work was sponsored by a grant from the Tonkinson Colorectal Cancer Research Fund (#57838). The authors also acknowledge the Ministry of Education, Culture and Sports of Spain for the financing of the José Castillejo scholarship (CAS19/00043) to MLR.
Authors’ contributions
SJH conceived the study, was the principal investigator, and took the lead role in producing the manuscript; CMS and MLR contributed to data collection; VC and TB contributed to study design and data curation; DH and MB contributed to data analysis and interpretation; CP, ML, CS, FS, SN, JM, CL, and PAC contributed to data collection. All authors contributed to manuscript writing. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
Supplementary materials associated with this article can be found in the online version at doi:10.1016/j.jshs.2023.01.003.
Supplementary materials
References
- 1.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Baade PD, Frischi L, Eakin EG. Non-cancer mortality among people diagnosed with cancer. Cancer Causes Control. 2006;17:287–297. doi: 10.1007/s10552-005-0530-0. [DOI] [PubMed] [Google Scholar]
- 3.Keats MR, Cui Y, Grandy SA, Parker L. Cardiovascular disease and physical activity in adult cancer survivors: A nested, retrospective study from the Atlantic PATH cohort. J Cancer Surviv. 2017;11:264–273. doi: 10.1007/s11764-016-0584-x. [DOI] [PubMed] [Google Scholar]
- 4.Stewart J, Manmathan G, Wilkinson P. Primary prevention of cardiovascular disease: A review of contemporary guidance and literature. JRSM Cardiovasc Dis. 2017;6 doi: 10.1177/2048004016687211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hamer J, Warner E. Lifestyle modifications for patients with breast cancer to improve prognosis and optimize overall health. CMAJ. 2017;189:e268–e274. doi: 10.1503/cmaj.160464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swain CT, Nguyen NH, Eagles T, et al. Postdiagnosis sedentary behavior and health outcomes in cancer survivors: A systematic review and meta-analysis. Cancer. 2020;126:861–869. doi: 10.1002/cncr.32578. [DOI] [PubMed] [Google Scholar]
- 7.Cao C, Friedenreich CM, Yang L. Association of daily sitting time and leisure-time physical activity with survival among US cancer survivors. JAMA Oncol. 2022;8:395–403. doi: 10.1001/jamaoncol.2021.6590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:242–274. doi: 10.3322/caac.21142. [DOI] [PubMed] [Google Scholar]
- 9.Australian Institute for Health and Welfare . Australian Institute for Health and Welfare; Canberra, Australian Capital Territory: 2019. Cancer in Australia 2019. Cancer Series no. 119. Cat. No. CAN 123. [Google Scholar]
- 10.Sweegers MG, Boyle T, Vallance JK, et al. Which cancer survivors are at risk for a physically inactive and sedentary lifestyle? Results from pooled accelerometer data of 1447 cancer survivors. Int J Behav Nutr Phys Act. 2019;16:66. doi: 10.1186/s12966-019-0820-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lynch BM, Dunstan DW, Healy GN, Winkler E, Eakin E, Owen N. Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: Findings from NHANES (2003–2006) Cancer Causes Control. 2010;21:283–288. doi: 10.1007/s10552-009-9460-6. [DOI] [PubMed] [Google Scholar]
- 12.Vallance JK, Boyle T, Courneya KS, Lynch BM. Accelerometer-assessed physical activity and sedentary time among colon cancer survivors: Associations with psychological health outcomes. J Cancer Surviv. 2015;9:404–411. doi: 10.1007/s11764-014-0409-8. [DOI] [PubMed] [Google Scholar]
- 13.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 26 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 14.Australian Institute of Health and Welfare . Australian Institute for Health and Welfare; Canberra, Australian Capital Territory: 2019. Alcohol and other drug use in regional and remote Australia; Consumption, Harms, and Access to treatment 2016–2017. [Google Scholar]
- 15.Australian Institute of Health and Welfare . Australian Institute for Health and Welfare; Canberra, Australian Capital Territory: 2014. Australians’ health. [Google Scholar]
- 16.Goodwin BC, Rowe AK, Crawford-Williams F, et al. Geographical disparities in screening and cancer-related health behaviour. Int J Environ Res Public Health. 2020;17:1246. doi: 10.3390/ijerph17041246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gunn KM, Berry NM, Meng XQ, et al. Differences in the health, mental health and health-promoting behaviours of rural versus urban cancer survivors in Australia. Support Care Cancer. 2020;28:633–643. doi: 10.1007/s00520-019-04822-0. [DOI] [PubMed] [Google Scholar]
- 18.Olson JL, March S, Brownlow C, Biddle SJH, Ireland M. Inactive lifestyles in peri-urban Australia: A qualitative examination of social and physical environmental determinants. Health Promot J Austr. 2019;30:153–162. doi: 10.1002/hpja.199. [DOI] [PubMed] [Google Scholar]
- 19.Hardcastle SJ, Maxwell-Smith C, Kamarova S, Lamb S, Millar L, Cohen PA. Factors influencing non-participation in an exercise program and attitudes towards physical activity amongst cancer survivors. Support Care Cancer. 2018;26:1289–1295. doi: 10.1007/s00520-017-3952-9. [DOI] [PubMed] [Google Scholar]
- 20.Hardcastle SJ, Galliott M, Lynch BM, et al. “If I had someone looking over my shoulder…”: Exploration of advice received and factors influencing physical activity among non-metropolitan cancer survivors. Int J Behav Med. 2019;26:551–561. doi: 10.1007/s12529-019-09808-0. [DOI] [PubMed] [Google Scholar]
- 21.Mama SK, Lopez-Olivob MA, Bhuiyanc N, Leach HJ. Effectiveness of physical activity interventions among rural cancer survivors: A systematic review and meta-analysis. Cancer Epidemiol Biomarkers Prev. 2021;30:2143–2153. doi: 10.1158/1055-9965.EPI-21-0871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eakin EG, Lawler SP, Winkler EAH, Hayes SC. A randomised trial of a telephone-delivered exercise intervention for non-urban dwelling women newly diagnosed with breast cancer: Exercise for health. Ann Beh Med. 2012;43:229–238. doi: 10.1007/s12160-011-9324-7. [DOI] [PubMed] [Google Scholar]
- 23.Fazzino TL, Fabian C, Befort CA. Change in physical activity during a weight management intervention for breast cancer survivors: Association with weight outcomes. Obesity (Silver Spring) 2017;25(Suppl. 2):S109–S115. doi: 10.1002/oby.22007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lyons EJ, Lewis ZH, Mayrsohn BG, Rowland JL. Behavior change techniques implemented in electronic lifestyle activity monitors: A systematic content analysis. J Med Internet Res. 2014;16:e192–e206. doi: 10.2196/jmir.3469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mercer K, Li M, Giangregorio L, Burns C, Grindrod K. Behavior change techniques present in wearable activity trackers: A critical analysis. JMIR Mhealth Uhealth. 2016;4:e40. doi: 10.2196/mhealth.4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lynch BM, Nguyen NH, Moore MM, et al. A randomized controlled trial of a wearable technology-based intervention for increasing moderate to vigorous physical activity and reducing sedentary behavior in breast cancer survivors: The ACTIVATE Trial. Cancer. 2019;125:2845–2855. doi: 10.1002/cncr.32143. [DOI] [PubMed] [Google Scholar]
- 27.Maxwell-Smith C, Hince D, Cohen PA, et al. A randomized controlled trial of WATAAP to promote physical activity in colorectal and endometrial cancer survivors. Psychooncology. 2019;28:1420–1429. doi: 10.1002/pon.5090. [DOI] [PubMed] [Google Scholar]
- 28.Hardcastle SJ, Maxwell-Smith C, Hince D, et al. The wearable activity technology and action-planning trial in cancer survivors: Physical activity maintenance post-intervention. J Sci Med Sport. 2021;24:902–907. doi: 10.1016/j.jsams.2021.04.004. [DOI] [PubMed] [Google Scholar]
- 29.Hardcastle SJ, Hince D, Jiménez-Castuera R, et al. Promoting physical activity in regional and remote cancer survivors (PPARCS) using wearables and health coaching: Randomised controlled trial protocol. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-028369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Australian Statistical Geography Standard . Australian Bureau of Statistics; Canberra, Australian Capital Territory: 2016. Volume 5- Remoteness structure. [Google Scholar]
- 31.Australian Institute of Health and Welfare . Australian Institute for Health and Welfare; Canberra, Australian Capital Territory: 2022. Profile of Australia's population. [Google Scholar]
- 32.Brown WJ, Burton NW, Marshall AL, Miller YD. Reliability and validity of a modified self-administered version of the Active Australia physical activity survey in a sample of mid-age women. Aust N Z J Public Health. 2008;32:535–541. doi: 10.1111/j.1753-6405.2008.00305.x. [DOI] [PubMed] [Google Scholar]
- 33.Hardcastle SJ, Galliott M, Lynch BM, et al. Acceptability and utility of, and preference for wearable activity trackers amongst non-metropolitan cancer survivors. PLoS One. 2018;13 doi: 10.1371/journal.pone.0210039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McMahon SK, Lewis B, Oakes M, Guan W, Wyman JF, Rothman AJ. Older adults’ experiences using a commercially available monitor to self-track their physical activity. JMIR Mhealth Uhealth. 2016;4:e35. doi: 10.2196/mhealth.5120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li T, Wei S, Shi Y, et al. The dose–response effect of physical activity on cancer mortality: Findings from 71 prospective cohort studies. Br J Sports Med. 2016;50:339–345. doi: 10.1136/bjsports-2015-094927. [DOI] [PubMed] [Google Scholar]
- 36.Lahart IM, Metsios GS, Nevill AM, Carmichael AR. Physical activity, risk of death and recurrence in breast cancer survivors: A systematic review and meta-analysis of epidemiological studies. Acta Oncol. 2015;54:635–654. doi: 10.3109/0284186X.2014.998275. [DOI] [PubMed] [Google Scholar]
- 37.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167:875–881. doi: 10.1093/aje/kwm390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 39.Lynch BM, Boyle T, Winkler E, Occleston J, Courneya KS, Vallance JK. Patterns and correlates of accelerometer-assessed physical activity and sedentary time among colon cancer survivors. Cancer Causes Control. 2016;27:59–68. doi: 10.1007/s10552-015-0683-4. [DOI] [PubMed] [Google Scholar]
- 40.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 41.Meyer-Schwickerath C, Morawietz C, Baumann FT, Huber G, Wiskemann J. Efficacy of face-to-face behavior change counseling interventions on physical activity behavior in cancer survivors—A systematic review and meta-analysis. Disabil Rehabil. 2021;14:5386–5401. doi: 10.1080/09638288.2021.1938247. [DOI] [PubMed] [Google Scholar]
- 42.Cadmus LA, Salovey P, Yu H, Chung G, Kasl S, Irwin ML. Exercise and quality of life during and after treatment for breast cancer: Results of two randomized controlled trials. Psychooncology. 2009;18:343–352. doi: 10.1002/pon.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Befort CA, Bennett L, Christifano D, Klemp JR, Krebill H. Effective recruitment of rural breast cancer survivors into a lifestyle intervention. Psychooncology. 2015;24:487–490. doi: 10.1002/pon.3614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu Q, Liu FC, Huang KY, et al. Beneficial effects of moderate to vigorous physical activity on cardiovascular disease among Chinese adults. J Geriatr Cardiol. 2020;17:85–95. doi: 10.11909/j.issn.1671-5411.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arem H, Moore SC, Patel A, et al. Leisure time physical activity and mortality: A detailed pooled analysis of the dose-response relationship. JAMA Intern Med. 2015;175:959–967. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vaughan C, Kilkkinen A, Philpot B, et al. Physical activity behaviours of adults in the Greater Green Triangle region of rural Australia. Aust J Rural Health. 2008;16:92–99. doi: 10.1111/j.1440-1584.2008.00957.x. [DOI] [PubMed] [Google Scholar]
- 47.Ribeiro FE, Tebar WR, Vanderlei LCM, et al. Physical activity domains are differently related with quality of life in breast cancer survivors: A cross-sectional study. Menopause. 2021;28:1233–1238. doi: 10.1097/GME.0000000000001837. [DOI] [PubMed] [Google Scholar]
- 48.Frensham LJ, Parfitt G, Dollman J. Predicting engagement with online walking promotion among metropolitan and rural cancer survivors. Cancer Nurs. 2020;43:52–59. doi: 10.1097/NCC.0000000000000649. [DOI] [PubMed] [Google Scholar]
- 49.Milat AJ, King L, Bauman AE, Redman S. The concept of scalability: Increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promot Int. 2013;28:285–298. doi: 10.1093/heapro/dar097. [DOI] [PubMed] [Google Scholar]
- 50.Milat AJ, Lee K, Conte K., et al. Intervention scalability assessment tool: A decision support tool for health policy makers and implementers. Health Res. Policy Syst. 2020;18:1. doi: 10.1186/s12961-019-0494-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Groen WG, van Harten WH, Vallance JK. Systematic review and meta-analysis of distance-based physical activity interventions for cancer survivors (2013–2018): We still haven't found what we're looking for. Cancer Treat Rev. 2018;69:188–203. doi: 10.1016/j.ctrv.2018.07.012. [DOI] [PubMed] [Google Scholar]
- 52.Khoo S, Mohbin N, Ansari P, Al-Kitani M, Müller AM. mHealth interventions to address physical activity and sedentary behavior in cancer survivors: A systematic review. Int J Environ Res Public Health. 2021;18:5798. doi: 10.3390/ijerph18115798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Singh B, Zopf EM, Howden EJ. Effect and feasibility of wearable physical activity trackers and pedometers for increasing physical activity and improving health outcomes in cancer survivors: A systematic review and meta-analysis. J Sport Health Sci. 2022;11:184–193. doi: 10.1016/j.jshs.2021.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coughlin SS, Caplan LS, Stone R. Use of consumer wearable devices to promote physical activity among breast, prostate, and colorectal cancer survivors: A review of health intervention studies. J Cancer Surviv. 2020;14:386–392. doi: 10.1007/s11764-020-00855-1. [DOI] [PubMed] [Google Scholar]
- 55.Hartman SJ, Nelson SH, Myers E, et al. Randomized controlled trial of increasing physical activity on objectively measured and self-reported cognitive functioning among breast cancer survivors: The memory & motion study. Cancer. 2018;124:192–202. doi: 10.1002/cncr.30987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mbous YP, Patel J, Kelly KM. A systematic review and meta-analysis of physical activity interventions among colorectal cancer survivors. Transl Behav Med. 2020;10:1134–1143. doi: 10.1093/tbm/ibz176. [DOI] [PubMed] [Google Scholar]
- 57.Hailey V, Rojas-Garcia A, Kassianos AP. A systematic review of behaviour change techniques used in interventions to increase physical activity among breast cancer survivors. Breast Cancer. 2022;29:193–208. doi: 10.1007/s12282-021-01323-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.