Abstract
Dual-mobility (DM) implants have been used in total hip arthroplasty since 1974. Modular DM implants have seen an increase in use in primary and revision total hip arthroplasties given the theoretical decreased dislocation rate. DM constructs have 2 articulation sites, one between the acetabular shell and a polyethylene liner, as well as one between the liner and the femoral head component. However, dislocations with modular DM implant dislocations can still occur. These dislocations occur via an extraprosthetic or intraprosthetic mechanism. Intraprosthetic dislocation is a phenomenon in which the smaller femoral head dissociates from the polyethylene liner. We present a case of intraprosthetic dislocation in an 81-year-old female with migration of the polyethylene liner into her gluteal muscles after 2 attempted closed reductions.
Keywords: Intraprosthetic dislocation, Dual-mobility implant, Hip arthroplasty
Introduction
In 1974, the use of dual-mobility (DM) implants in total hip arthroplasty (THA) was introduced in France by Bousquet resulting in increased implant longevity and joint stability following THA [1]. DM provides dual articular surfaces, increased range of motion (ROM), and an increased jump distance, which allows for increased stability [2]. Hip dislocation is a significant concern in THA patients with a recent meta-analysis reporting an incidence of 2.1% [3]. In an effort to remedy the problem of dislocation seen in THA, there has been an overall increase in the use of DM.
While the use of DM implants has shown a significant decrease in the overall risk of hip dislocation [4,5], intraprosthetic dislocation (IPD) remains a rare and potentially serious complication. IPD is unique to DM implants and refers to the failure of articulation of the femoral head with the polyethylene (PE) liner. This rare complication can be missed following a closed reduction of the metal femoral head into the acetabular cup that now lacks the PE liner. Once recognized, this requires open reduction with component revision. We present a case of IPD of a DM implant in an 81-year-old woman with a history of repeat hip dislocation with migration of the PE liner into the gluteal musculature.
Case history
An 81-year-old female presented to our clinic for evaluation 1 month following 2 dislocations and subsequent relocations of her right hip arthroplasty within a 30-day period at an outside facility. The index procedure was done at an outside facility 8 years prior for primary osteoarthritis of her hip with an overall unremarkable recovery leading up to her initial dislocation event. Two months prior to presenting to our facility, the patient bent over at the waist to pick up an item from the floor, felt her hip give out, and heard a clunk. She was unable to range her hip or bear weight and was taken to an outside emergency department where she was found to have a periprosthetic hip dislocation. The hip was reduced, and the patient was sent home with hip flexion precautions. The patient sustained a similar event less than 1 month later while bending at the waist. She was again taken to an outside facility where she was diagnosed with a presumed periprosthetic hip dislocation and underwent closed reduction. She was sent home with a wheelchair, knee immobilizer, and instructions to follow up with a hip revision specialist for presumed wear of the PE liner.
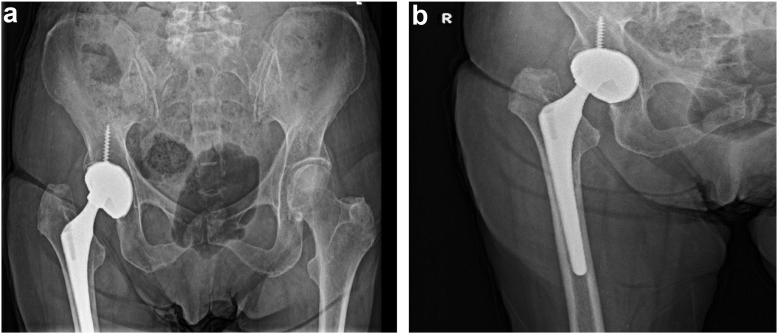
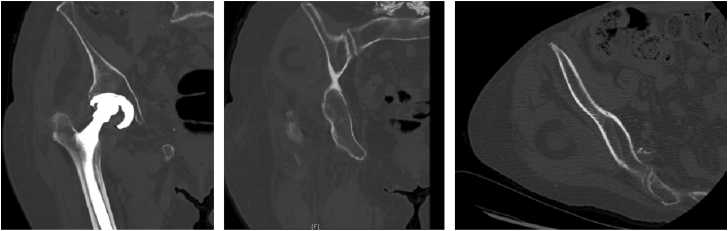
The patient presented to our clinic using a wheelchair for ambulation and her knee in an immobilizer. Radiographs obtained showed the femoral component to be eccentrically located in the acetabular cup, suggestive of IPD (Fig. 1). Computerized tomography confirmed a dislocation of the PE liner with the liner located superior and posterior to the joint, embedded within the patient’s right gluteus medius muscle (Fig. 2). Infectious workup with erythrocyte sedimentation rate, C-reactive protein, and complete blood count with differential was performed and found to be benign. Expedited revision surgery was planned.
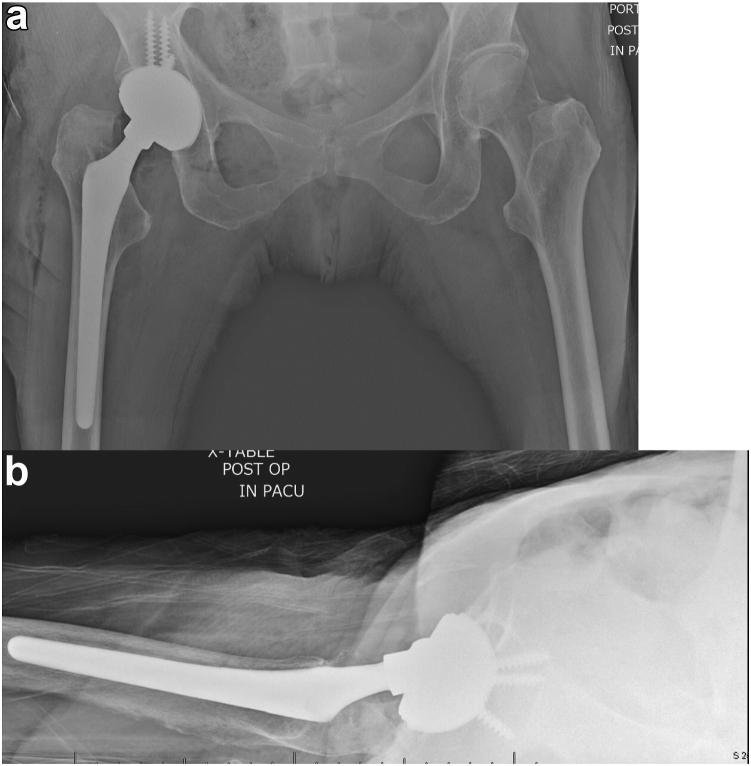
Figure 1.
Anteroposterior (AP) pelvis (a) and AP right hip (b) of a patient demonstrating eccentric nature of femoral component within the acetabular shell. No obvious radiographic signs of femoral or acetabular shell loosening or osteolysis.
Figure 2.
Representative CT cuts redemonstrating the eccentric position of the femoral component within the acetabular shell. The polyethylene liner location is demonstrated on both the coronal and axial cuts posterior and superior to the hip joint in the gluteus medius musculature.
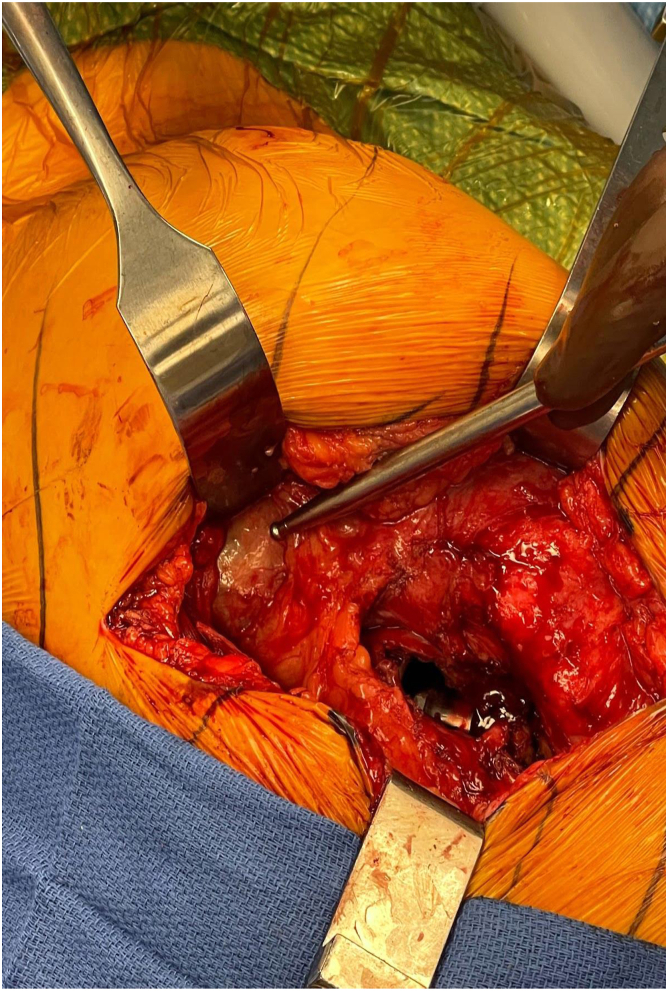
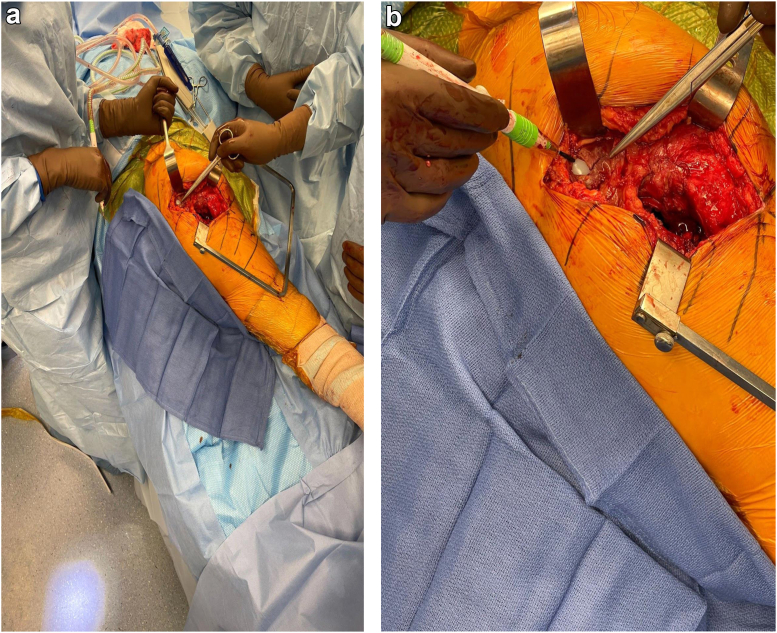
The patient was brought to the operating room and placed under general anesthesia. She was positioned in a lateral decubitus position using a peg board. The surgery began with utilization of the patient’s previous incision through a standard posterolateral approach to the hip. The dissection was taken down through the fascia where disruption of the capsule with corresponding hematoma was noted. There was no purulence or other signs of infection as well as no signs of metal debris within the joint. The short external rotators were taken down revealing the metal femoral head within the metal acetabular liner with a missing PE insert. Next, we began tracking the incision proximally in search of the patient’s PE liner, which was palpable in the patient’s muscle mass of the gluteus musculature. It was found to be surrounded by a pseudomembrane (Fig. 3). A small incision was made in the pseudomembrane, and the component was removed (Figure 4, Figure 5a and b).
Figure 3.
Intraoperative image showing the pseudomembrane surrounding the polyethylene component lodged within the gluteus medius musculature.
Figure 4.
Intraoperative images (a and b) demonstrating the location of the polyethylene component within the gluteus medius musculature with pseudomembrane excised.
Figure 5.
AP pelvis (a) and cross-table lateral hip (b) postoperative radiographs obtained in recovery.
The hip was then dislocated to evaluate the remaining components. The acetabular cup metal insert was in a relatively good condition, but given the evidence of metal grinding from the femoral head component, the bearing surfaces were replaced. The acetabular shell was in acceptable condition and well ingrown to the bony pelvis. However, more screws were placed for added stability given the possibility of transitioning to a constrained liner. Trials were used to evaluate different constructs for stability. The clinical assessment and close visual evaluation gave us confidence to proceed with the same DM construct instead of a constrained option. The final implants consisted of a metal acetabular insert with an internal diameter of 38 mm, a PE liner with an outer diameter 38 mm and inner diameter of 22.2 mm (size 38D), and a 22 + 10 mm c-taper low friction ion treatment head with a low flexion femoral head. The final implants were stable to 80-90 degrees of flexion on the table, adduction of 20 degrees, and internal rotation of 25 degrees. The hip was brought in 10-15 degrees of extension and 25-30 degrees of external rotation and was felt to be stable. There was no impingement noted. The hip was also stable with shuck testing with appropriate tension of abductors for stability. The hip was irrigated copiously with saline and closed in normal fashion with repair of the short external rotators and capsule. Postoperative radiographs obtained in the recovery room are shown in Figure 5.
The patient has experienced an uncomplicated postoperative course with radiographs at 12 months showing appropriate position of all DM components (Fig. 6). She is ambulating without pain, and her hip remains stable on exam. The patient provided informed, written consent for the use of her case in this publication.
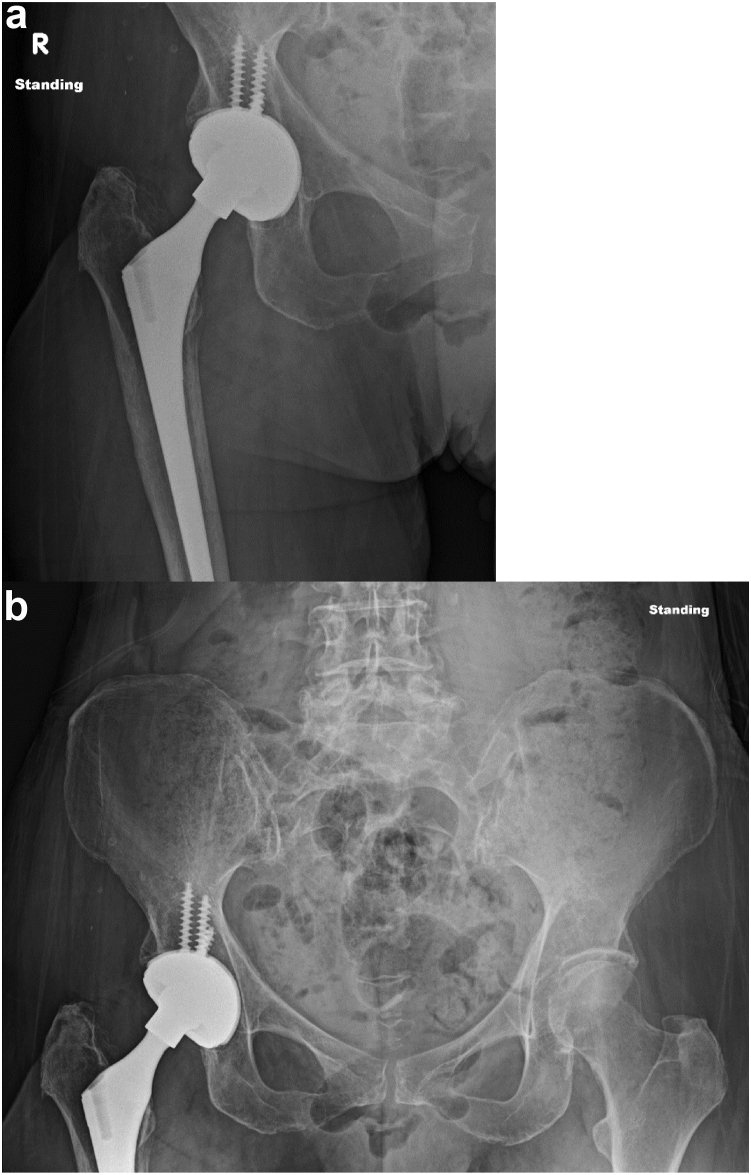
Figure 6.
AP (a) right hip and (b) pelvis at 1-year follow-up appointment.
Discussion
DM implants have been used in THA since 1974, with 2 common systems: anatomic and modular DM systems [1]. The anatomic system consists of a press-fit cup that articulates with a nonconstrained mobile liner surrounding a 28-mm femoral head. Whereas the modular system contains a press-fit cup with a separate cobalt-chromium liner. The cobalt-chromium liner is the surface of articulation with a PE liner containing a smaller femoral head. An advantage to the modular system is the various options it provides surgeons in primary and revision surgery secondary to the presence of screw holes in the cup with the liner removed. Neither system appears to be superior to the other in regards to dislocation rates [6].
There are multiple proposed mechanisms of IPD, but traditionally it was often linked to PE wear resulting in direct, metal-on-metal articulation of the metallic bearing with the femoral cup [4,7]. Advances have been made in DM design to decrease forces of stress, improve PE longevity, and increase stability [2]. In a 5-year prospective study involving 321 patients, Epinette et al. [8] reported no IPD at 5 years with the modern DM design with hyper-cross-linked PE liners. As presented in a recent systematic review on DM [7], several studies with greater than 10 years of follow-up have detailed no IPD of modern DMs, indicating design changes to the DM system have been positive improvements in THA.
Even with steps forward in design of the DM system, IPD continues to be a cause for concern. As PE improvements have led to a decreased rate of wear, early IPD has become more iatrogenic in nature. In a recent systematic review, De Martino et al [2] found many early IPD cases to be secondary to attempted closed reduction. The proposed mechanism involves the outer PE liner levering against the rim of the acetabular cup or on pelvic bone during an attempted closed reduction resulting in what has been termed the “bottle opener effect” [9]. Concern for iatrogenic IPD should be considered when radiographs show what appears to be a reduced hip, while clinically the hip remains unstable on examination [10]. Addona et al. reported a 71% incidence of IPD following closed reduction of a dislocated DM hip [11]. Delayed recognition can lead to increased damage to the cup with potentially significant soft-tissue metallosis and elevated levels of cobalt and chromium [12,13].
In our case, it is difficult to determine the cause of IPD, but with a history of repeat dislocation followed by closed reduction, it is reasonable to consider manipulation of the hip contributed to the IPD. As continued effort is given to the prevention of THA dislocation, including IPD, it is important to consider the physician’s role in preventing iatrogenic causes. The incidence of IPD with closed reduction of DM implants facilitates a need for determination of an ideal closed-reduction technique, maneuvers, and guidelines in pursuit of decreasing IPD secondary to iatrogenic causes [14]. Current suggestions for prevention of IPD on closed reduction include sedation with adequate muscle relaxation, fluoroscopic guidance, and gentle maneuvers [10,11]. Future cadaveric studies aimed at reduction maneuvers and technique may prove a beneficial start in improving closed reduction of DM implants. Furthermore, it may be of value to enhance education, both for patients and providers, surrounding the increasing prevalence of DM implants in THA and the important differences in dislocation between DM and standard implants. Beyond education, recently suggested inclusion of a radiolucent ring on PE liners may lead to better identification of a displaced liner in radiographs without a clear “bubble sign” and/or eccentric position of the femoral head [15,16].
Summary
The use of DM systems for THA is increasing in popularity secondary to associations with decreased dislocation rates. A complication unique to DM systems is IPD. Traditionally associated with wear of the PE liner, recent reports have increased regarding iatrogenic IPD following closed reduction. Given the seriousness of the situation, it is important to consider the presence of a DM system in a dislocated THA hip with early recognition on radiograph and care taken during reduction via full sedation and gentle reduction maneuvers. This case also highlights the role of computerized tomography scan in the identification of the dislodged PE component and its location in the soft tissues surrounding the hip. Further clinical studies are warranted for determination of best practice in the management of a dislocated DM hip.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101290.
Informed patient consent
The author(s) confirm that written informed consent has been obtained from the involved patient(s) or if appropriate from the parent, guardian, power of attorney of the involved patient(s); and, they have given approval for this information to be published in this case report (series).
CRediT authorship contribution statement
Austin J. Cantrell: Conceptualization, Writing – original draft, Writing – review & editing. D. Alex Forrester: Conceptualization, Writing – review & editing. Alexander W. Crawford: Conceptualization, Writing – original draft. Cade Morris: Writing – original draft, Writing – review & editing. Rishi Thakral: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
Appendix A. Supplementary data
References
- 1.Philippot R., Neri T., Boyer B., Viard B., Farizon F. Bousquet dual mobility socket for patient under fifty years old. More than twenty year follow-up of one hundred and thirty one hips. Int Orthop. 2017;41:589–594. doi: 10.1007/s00264-016-3385-y. [DOI] [PubMed] [Google Scholar]
- 2.De Martino I., Triantafyllopoulos G.K., Sculco P.K., Sculco T.P. Dual mobility cups in total hip arthroplasty. World J Orthop. 2014;5:180–187. doi: 10.5312/wjo.v5.i3.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kunutsor S.K., Barrett M.C., Beswick A.D., Judge A., Blom A.W., Wylde V., et al. Risk factors for dislocation after primary total hip replacement: meta-analysis of 125 studies involving approximately five million hip replacements. Lancet Rheumatol. 2019;1:e111–e121. doi: 10.1016/s2665-9913(19)30045-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boyer B., Philippot R., Geringer J., Farizon F. Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop. 2012;36:511–518. doi: 10.1007/s00264-011-1289-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philippot R., Camilleri J.P., Boyer B., Adam P., Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dubin J.A., Westrich G.H. Anatomic dual mobility compared to modular dual mobility in primary total hip arthroplasty: a matched cohort study. Arthroplast Today. 2019;5:509–514. doi: 10.1016/j.artd.2019.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Batailler C., Fary C., Verdier R., Aslanian T., Caton J., Lustig S. The evolution of outcomes and indications for the dual-mobility cup: a systematic review. Int Orthop. 2017;41:645–659. doi: 10.1007/s00264-016-3377-y. [DOI] [PubMed] [Google Scholar]
- 8.Epinette J.A., Harwin S.F., Rowan F.E., Tracol P., Mont M.A., Chughtai M., et al. Early experience with dual mobility acetabular systems featuring highly cross-linked polyethylene liners for primary hip arthroplasty in patients under fifty five years of age: an international multi-centre preliminary study. Int Orthop. 2017;41:543–550. doi: 10.1007/s00264-016-3367-0. [DOI] [PubMed] [Google Scholar]
- 9.Loubignac F., Boissier F. [Cup dissociation after reduction of a dislocated hip hemiarthroplasty] Rev Chir Orthop Reparatrice Appar Mot. 1997;83:469–472. [PubMed] [Google Scholar]
- 10.Piette N., Guyen O., Moerenhout K. Intra-prosthetic dislocation of dual mobility hip prosthesis: an original and unusual complication. J Radiol Case Rep. 2019;13:15–23. doi: 10.3941/jrcr.v13i5.3465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Addona J.L., Gu A., De Martino I., Malahias M.A., Sculco T.P., Sculco P.K. High rate of early intraprosthetic dislocations of dual mobility implants: a single surgeon series of primary and revision total hip replacements. J Arthroplasty. 2019;34:2793–2798. doi: 10.1016/j.arth.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Hermena S., Tawfeek W., Latimer P. Intraprosthetic dislocation of dual-mobility total hip arthroplasty: the unforeseen complication. Cureus. 2021;13 doi: 10.7759/cureus.19858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schirmers M.D.J., Horazdovsky M.D.R., Marston M.D.S. Early intraprosthetic dislocation of dual-mobility total hip arthroplasty implant following attempted closed reduction: a case report. Reconstr Rev. 2014;5:47–50. [Google Scholar]
- 14.Waddell B.S., De Martino I., Sculco T., Sculco P. Total hip arthroplasty dislocations are more complex than they appear: a case report of intraprosthetic dislocation of an anatomic dual-mobility implant after closed reduction. Ochsner J. 2016;16:185–190. [PMC free article] [PubMed] [Google Scholar]
- 15.Endo Y., Geannette C., Chang W.T. Imaging evaluation of polyethylene liner dissociation in total hip arthroplasty. Skeletal Radiol. 2019;48:1933–1939. doi: 10.1007/s00256-019-03232-x. [DOI] [PubMed] [Google Scholar]
- 16.Fox O.J.K., Cairns S.L., Jarman P.G. Recurrent and radiographically unrecognized iatrogenic intra-prosthesis hip dislocations. J Am Coll Emerg Physicians Open. 2020;1:419–422. doi: 10.1002/emp2.12050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.