Abstract
Despite significant advances in the understanding and delivery of osteosynthesis, fracture non-union remains a challenging clinical problem in orthopaedic surgery. To bridge the gap, basic science characterization of fracture healing provides a platform to identify and target biological strategies to enhance fracture healing. Of immense interest, Platelet-rich plasma (PRP) is a point of care orthobiologic that has been extensively studied in bone and soft tissue healing given its relative ease of translation from the benchtop to the clinic. The aim of this narrative review is to describe and relate pre-clinical in-vitro and in-vivo findings to clinical observations investigating the efficacy of PRP to enhance bone healing for primary fracture management and non-union treatment. A particular emphasis is placed on the heterogeneity of PRP preparation techniques, composition, activation strategies, and delivery. In the context of existing data, the routine use of PRP to enhance primary fracture healing and non-union management cannot be supported. However, it is acknowledged that extensive heterogeneity of PRP treatments in clinical studies adds obscurity; ultimately, refinement (and consensus) of PRP treatments for specific clinical indications, including repetition studies are warranted.
Keywords: platelet rich plasma, bone regeneration, fracture healing, fractures, ununited
Introduction
Bone healing stands as a complex and pivotal process within the realm of orthopedics, carrying with it substantial clinical and financial burdens. In 2019, the global incidence of bony fractures stood at a staggering 178 million cases, underscoring the pervasive nature of this often-debilitating health concern.1 While the majority of fractures heal successfully, approximately 5–10% of patients encounter a formidable obstacle: non-union.2 The Food and Drug Administration (FDA)3 has defined a non-union as a fracture that persists at 9 months post-injury, exhibiting insufficient signs of healing over three consecutive months. This condition manifests in two distinct forms—hypertrophic non-union, due to inadequate stability at the fracture site, and atrophic non-union, attributed to a deficiency of fracture biology and bone healing.4 The management of fracture non-union is considered on an individualized basis and involves surgical strategies to optimize stability (and strain) at the fracture site while identifying and addressing any deficits in fracture biology manifested in the bone healing response [183]. The costs associated with non-union treatment can be staggering, with tibial non-unions, for example, incurring an approximate cost of $25,556 USD compared to $11,686 USD for tibial fractures without non-union complications.5
The physiological process of bone healing is intrinsically sophisticated, typically progressing through three stages: the inflammatory phase, where hematoma forms and inflammatory cells infiltrate the site; the reparative phase, which involves the formation of a soft callus that gradually mineralizes; and the remodeling phase, where the callus is replaced by mature bone tissue.6 Each of these stages is marked by a distinct cascade of cellular and molecular events, underscoring the potential for therapeutic interventions that can modulate these processes.
Historically, the treatment of bone injuries has evolved from rudimentary splinting techniques to advanced surgical interventions, reflecting a deepening understanding of bone biology and healing processes. In the quest to enhance bone healing, regenerative medicine has introduced several innovative therapies, of which platelet-rich plasma (PRP) therapy has emerged as a significant contender. PRP therapy, in comparison to other regenerative approaches like stem cell therapy or bone morphogenetic proteins (BMPs), offers a unique blend of autologous growth factors and cytokines, potentially reducing the risk of immune rejection and other complications associated with allogeneic or synthetic materials.7 Initially recognized for its role in tissue sealing as fibrin tissue adhesives, PRP subsequently garnered attention for its potential to emulate the initiation of the natural healing cascade.8 The rationale behind PRP therapy lies in its ability to release biologically active factors and adhesion proteins, offering the potential to stimulate the resolution of chronic pathological processes.9 Specifically, PRP is replete with growth factors such as Platelet-Derived Growth Factor (PDGF), Transforming Growth Factor-beta (TGF-β), and Insulin-Like Growth Factor-1 (IGF-1), which are critical mediators in the bone healing process.10 These growth factors and cytokines play key roles in regulating inflammation, angiogenesis, and osteoblastic activity, making them vital to the various phases of bone repair.11–13
Despite promising pre-clinical data supporting the potential of PRP, clinical trials have yet to unequivocally demonstrate its benefits in bone healing. Moreover, the absence of a standardized PRP injection protocol(s) hinders efforts to generalize findings or collate the data of individual studies. Dosage and timing intervals remain uncertain, and the composition of PRP varies widely in terms of leukocyte and platelet count, growth factor concentration, and red blood cell contamination due to patient characteristics and the preparation kit used.8,14 This heterogeneity in PRP formulations further complicates its clinical application to date, given the current absence of a universally accepted PRP injection protocol. Therefore, the aim of this narrative review is to provide a comprehensive platform to evaluate the evidence regarding the use of PRP for bone healing.
Biological Activity of PRP: Influence on the Bone Regeneration Process
The pursuit of optimal strategies for bone healing has driven the exploration of PRP therapy due to its ability to serve as a concentrated source of autologous growth factors and cytokines. Our current understanding of PRP’s biological activity in bone healing has been predominantly centered on three key aspects: inflammatory cytokines, growth factors, and angiogenic factors (Table 1). These factors orchestrate the intricate process of cell signaling, tissue regeneration, and angiogenesis during the bone healing process.
Table 1.
Function of the Growth Factors and Cytokines Found in PRP on Bone Regeneration
| Category | Factors | Roles and Function |
|---|---|---|
| Inflammatory Cytokines | Interleukin-1 (IL-1) | Initiates inflammation, recruits immune cells, and triggers cellular responses. |
| Interleukin-6 (IL-6) | Involved in callus remodeling and mineralization, recruit’s osteoblasts. | |
| Tumor Necrosis Factor-alpha (TNF-a) | Recruit’s osteoblasts and plays a pivotal role in bone formation. | |
| Growth Factors | Platelet-Derived Growth Factor (PDGF) | Stimulates revascularization, collagen synthesis, and bone regeneration. |
| Transforming Growth Factor-beta (TGF-B) | Initiates signaling pathways in osteoprogenitor cells and supports long-term healing, bone regeneration, and remodeling. | |
| Insulin-Like Growth Factor-1 (IGF-1) | Influences osteoblasts and pre-osteoblasts, inhibits apoptosis, and enhances collagen synthesis and osteogenesis. | |
| Angiogenic Factors | Vascular Endothelial Growth Factor (VEGF) | Stimulates angiogenesis, recruits endothelial cells, and supports oxygen and nutrient delivery. |
| Angiogenin | Contributes to the development of collateral circulation, enhancing blood supply redundancy. | |
| Other Bioactive Factors | Serotonin, Histamine, and Dopamine | Increases capillary permeability, facilitating the influx of inflammatory cells. |
| Calcium | Promotes the formation of a stable fibrin clot. | |
| Adenosine | Mitigates excessive inflammation and tissue damage. |
Inflammatory Cytokines
The initial phase of bone healing is characterized by inflammation, a crucial process that dictates the subsequent stages of repair, and platelets in PRP have been shown to successfully modulate this inflammatory response.10,15 Once activated, the platelets in PRP release a spectrum of inflammatory cytokines from their alpha-granules such as Interleukin-1 (IL-1), Interleukin-6 (IL-6), and Tumor Necrosis Factor-alpha (TNF- α).13,16 These cytokines play pivotal roles in the initiation of fracture repair by recruiting immune cells and initiating a cascade of biochemical and cellular alterations that set the stage for subsequent stages of bone repair. IL-1 stands out as a main regulator of the initial inflammatory responses in bone healing. Its release at the fracture site follows a biphasic pattern, characterized by an initial peak during the onset of the fracture healing process, succeeded by a subsequent peak during the shift from chondrogenesis to osteogenesis in the phase of endochondral maturation.17,18 This cytokine plays a multifaceted role, influencing the recruitment of immune cells to the injury site and initiating a multitude of cellular responses necessary to the bone healing process.19–21 Additionally, TNF-alpha also follows a biphasic pattern in its expression during the healing process and plays a pivotal role in recruiting osteoblasts to the injury site.17,18 These bone-forming cells are crucial for the synthesis of new bone tissue and studies20–22 have indicated that both TNF-α and IL-1β recruit osteoblasts, highlighting their collaborative role in bone regeneration. Furthermore, IL-6 is a multifunctional cytokine involved in bone repair. Studies using IL-6 knockout mice23 have shown that this cytokine plays a role in callus remodeling and mineralization, indicating its significance in the later stages of bone healing. Additionally, IL-6 has been implicated in recruiting osteoblasts, further contributing to bone formation.24,25 Thus, the orchestrated release of inflammatory cytokines in the early phases of bone healing is crucial for initiating the repair process and may be able to be amplified through the application and activation of PRP.
Growth Factors
PRP’s effectiveness in bone healing can be attributed significantly to the rich assortment of growth factors contained in the alpha-granules of platelets. Of the numerous growth factors that have been defined in the literature,26–29 the three that appear to play the most prominent role in bone healing include PDGF, TGF-β, and IGF-1.10 PDGF is a critical growth factor in PRP that plays a pivotal role in the early phases of bone healing by initiating several essential processes upon release from activated platelets. It stimulates revascularization, an essential step in bone repair, by promoting the growth of new blood vessels.11,30 This improved blood supply may facilitate the delivery of oxygen and nutrients to the injury site, accelerating the healing process. PDGF also has a profound impact on collagen synthesis, a key component of bone tissue. It encourages the production of collagen, enhancing the formation of a robust extracellular matrix (ECM) essential for bone regeneration.11,31,32 Moreover, PDGF can directly influence mesenchymal stem cells (MSCs), inducing their migration and osteogenic differentiation.33,34 These MSCs are crucial for generating new bone tissue, making PDGF a potent stimulator of bone formation.
TGF-β is also abundantly present in PRP and holds a multifaceted role in bone healing. It functions by exerting both paracrine and autocrine effects, influencing various cell types involved in long-term healing, bone regeneration, and bone modeling.29 One of TGF-β’s most crucial functions is its ability to initiate the signaling pathway of osteoprogenitor cells, which synthesize BMPs.12 These BMPs have demonstrated the potential to play a pivotal role in regulating the expression of growth factors in bone and cartilage tissue, further promoting bone healing and regeneration.35,36 TGF-β’s influence also extends to fibroblasts and pre-osteoblasts, stimulating the biosynthesis of type I collagen and fibronectin, supporting the formation of a robust ECM.37–39 Additionally, TGF-β promotes the deposition of bone matrix, contributing to the early stages of bone repair.40 Furthermore, it inhibits osteoclast formation and bone resorption, tilting the balance toward bone formation over resorption.41
IGF-1 is another significant component of PRP that plays a vital role in bone regeneration. This growth factor is deposited in bone matrix, endothelial cells, and chondrocytes and is released during the bone regeneration process.42 IGF-1 is responsible for orchestrating the complex interaction between bone formation and bone resorption. IGF-1’s presence in platelets influences osteoblasts and pre-osteoblasts, initiating osteogenesis and inhibiting the apoptosis of bone cells.43 Additionally, IGF-1 affects the expression of mesenchymal collagen enzymes, decreasing their degradation and enhancing collagen synthesis within the ECM. This leads to improved structural integrity and strength in the newly formed bone tissue.43 The growth factors found in PRP, including PDGF, TGF-β, and IGF-1, work synergistically to enhance bone healing. They promote angiogenesis, collagen synthesis, ECM formation, and osteogenesis, contributing to the regeneration and repair of bone tissue. These growth factors play distinct but interconnected roles, collectively facilitating the intricate process of bone healing and regeneration.
Angiogenic Factors
Angiogenesis plays a sustained role in delivering oxygen, nutrients, and precursor cells to the site of injury.44–46 PRP has demonstrated the ability to serve as a potent facilitator of angiogenesis, promoting the formation of new blood vessels that are crucial for supporting the regenerative processes in bone repair. Among the angiogenic factors found within PRP, Vascular Endothelial Growth Factor (VEGF) stands out as a principal driver of neovascularization. VEGF is a signal protein and its primary function is to stimulate angiogenesis.47 Upon the application of PRP to the bone defect site, the release of VEGF from platelets sets in motion a cascade of events. VEGF initiates a signaling cascade, acting as a potent mitogen and chemoattractant for endothelial cells, promoting their proliferation and migration to the area surrounding the bone defect.48–50 Once recruited, endothelial cells start to organize into primitive vascular structures, sprouting and elongating to form capillaries that infiltrate the damaged tissue.48,51 This neovascularization process serves two essential purposes in bone healing. Firstly, it ensures a continuous supply of oxygen and nutrients to the healing site, facilitating the metabolic demands of reparative cells. Secondly, it provides a conduit for the migration of osteoprogenitor cells and mesenchymal stem cells, which are crucial for the formation of new bone tissue.10,52,53
While VEGF primarily influences the growth of new vessels, angiogenin, another angiogenic factor found in PRP, contributes to the development of collateral circulation, which can be particularly relevant in cases where the primary blood supply to a bone defect may be compromised.10 Enhanced blood supply increases the resilience of the healing process, ensuring that adequate resources are available to support the regenerative demands of the damaged bone tissue. In the intricate orchestration of bone healing, angiogenesis is a fundamental process that ensures the delivery of essential resources to the site of injury. PRP therapy, enriched with angiogenic factors such as VEGF and angiogenin, plays a central role in promoting neovascularization and collateral circulation. By stimulating the formation of new blood vessels and alternate circulation pathways, PRP creates an environment conducive to optimal bone regeneration.
Other Bioactive Factors
In addition to growth factors, PRP contains a diverse array of bioactive factors stored within the dense granules of platelets, including serotonin, histamine, dopamine, calcium, and adenosine.54,55 These factors exert fundamental effects on the biologic aspects of wound healing, influencing inflammation modulation and cell function. In the context of PRP therapy, serotonin, histamine, and dopamine contribute to wound healing by increasing capillary permeability. This effect facilitates the influx of inflammatory cells to the site of injury, promoting an initial immune response and the activation of macrophages.56,57 Furthermore, calcium is essential for blood clotting, and its release from platelet granules upon activation is crucial for the formation of a stable fibrin clot at the site of injury.58 The clot not only prevents excessive bleeding but also provides a scaffold for cells involved in tissue repair to attach and proliferate. Additionally, adenosine receptor activation has been shown to modulate inflammation during wound healing, promoting an anti-inflammatory environment.59 Attenuation of local inflammation may be beneficial in the early stages of bone repair, as it may help mitigate excessive inflammation and tissue damage.10,59
PRP Separation: Optimizing Platelet Concentration
Over the past decade, substantial efforts have been devoted to refining PRP preparation techniques, with the aim of optimizing platelet concentration—a critical factor influencing its therapeutic effectiveness in bone healing. While numerous studies have demonstrated PRP’s positive effects on the differentiation and proliferation of human osteoblasts, at present, there exists no unanimous agreement on the ideal PRP dosage. Marx et al initially defined PRP as containing a minimum platelet concentration of 1,000,000 platelets/µL, however, the US Food and Drug Administration (FDA) mandates that PRP products must possess a minimum platelet concentration of 250 × 103/mL.60 Several additional investigators61–63 have also reported that a platelet concentration approximately two times greater than that found in peripheral blood positively affects osteoblast proliferation in vitro and significantly reduces bone healing time. However, Jovani-Sancho et al64 reported that an optimal platelet concentration of four times that of peripheral blood was necessary for optimal results. Other studies65–67 have indicated that concentrations below approximately 0.85 × 109/mL had no significant effect on osteogenesis. In contrast, however, Choi et al68 found that lower PRP concentrations, ranging from 1% to 5% of peripheral blood levels, stimulated the viability and proliferation of osteoblasts. Furthermore, it is crucial to exercise caution when considering platelet concentration, as adverse events have been observed at higher dosages.69–71 Fernandez-Medina et al72 indicated that cell viability and migration assays demonstrated detrimental effects on human osteoblasts when the PRP concentration exceeded 60%. Similarly, Al-Hamed et al61 reported that platelet concentrations greater than 8.21 ± 0.4 × 109/mL inhibited osteogenic proliferation and Graziani et al65 observed that a platelet concentration approximately 3.5 times greater than that of native blood led to a reduction in cell proliferation. These findings underscore the complexity of determining the precise platelet concentration required for optimal bone healing, as different concentrations of PRP may produce varying effects.
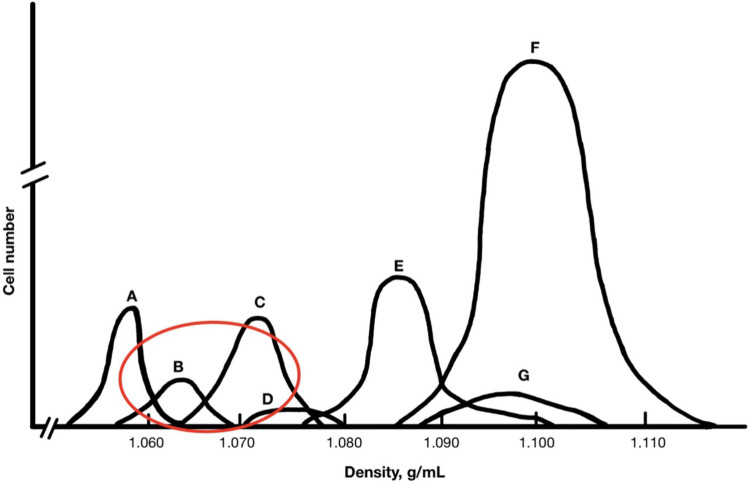
Centrifugation separates individual cells within blood based on their individual density gradients, thus the overlaps and proximity of the density of platelets and leukocytes present the possibility of contamination (Figure 1). Similar to other indications, the optimal concentration of leukocytes within PRP for bone healing remains not fully understood. Proponents of incorporating leukocytes argue that the antimicrobial properties of WBCs could mitigate the risk of infection, particularly when PRP is utilized intraoperatively.73–76 Moreover, studies by Zimmermann et al77 have revealed that leukocytes in leukocyte-rich PRP (LR-PRP) contribute significantly to the increased variability of growth factors, such as PDGF-αβ, PDGF-β1, and VEGF, in comparison to leukocyte-poor PRP (LP-PRP). This suggests that the concentration of white blood cells can be manipulated to optimize growth factor levels, potentially influencing the healing process positively. However, critics of leukocyte incorporation argue that the existence of WBCs can result in immediate pain and discomfort post-injection, while their catabolic and proinflammatory attributes may adversely impact the process of articular cartilage recovery as a result of the increased release of proinflammatory cytokines.78–80 Clinical investigations have further validated concerns regarding increased acute swelling and pain after intra-articular LR-PRP injection.81,82 Nevertheless, it is noteworthy that both LR-PRP and LP-PRP have demonstrated statistically significant improvements in clinical outcomes. Recent research, however, has added to this debate by highlighting the importance of matching the type of PRP with the specific clinical context. The prevailing evidence suggests that the choice of leukocyte concentration should be guided by the injection site.73,83 For intra-articular applications, LP-PRP appears to be more beneficial, as indicated in the treatment of knee osteoarthritis. LR-PRP has shown adverse effects on synovial cells, resulting in cell death and proinflammatory mediator production.81,84 In contrast, for the treatment of chronic tendinopathy, leukocyte-rich PRP has demonstrated superiority over leukocyte-poor PRP.85
Figure 1.
Density Gradients of Cells Contained within Blood Aspirate.
Notes: (A) Platelets, (B) Monocytes, (C) Lymphocytes, (D) Basophils, (E) Neutrophils, (F) Erythrocytes, (G) Eosinophils.
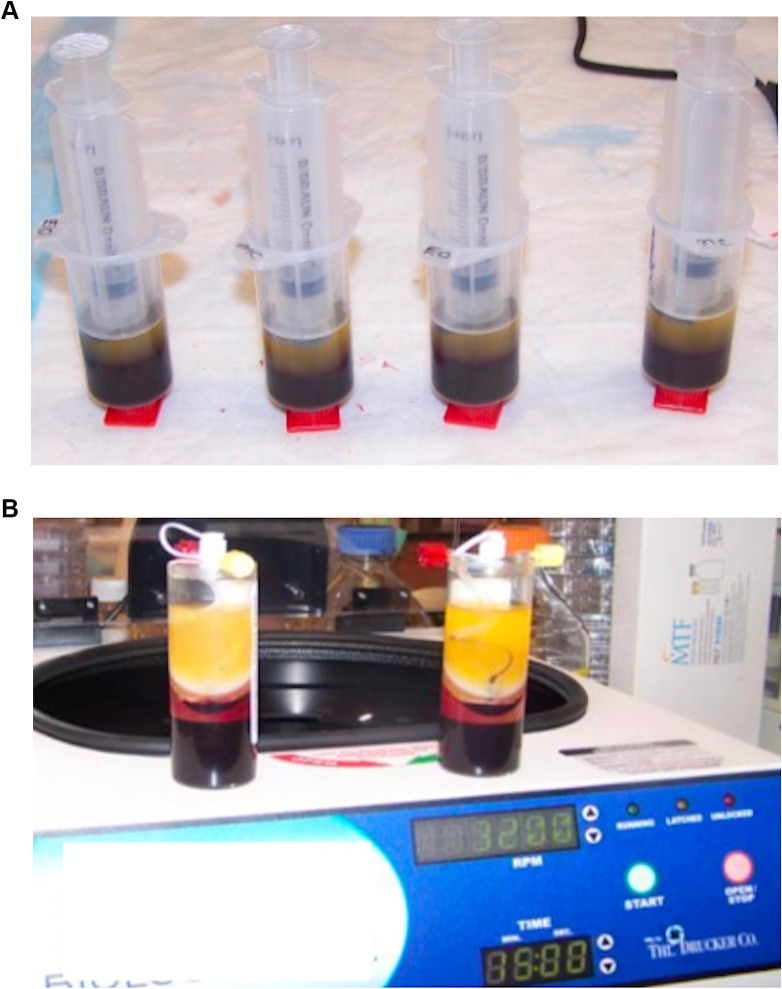
Unfortunately, a lack of universal preparation standardization and compositional reporting hampers our ability to collate data from individual studies and to gain consensus on findings. In most cases, blood is drawn from a patient, treated with an anticoagulant, and then centrifuged within an hour of collection. The methods then employed for isolating platelets and growth factors from whole blood can be broadly categorized based on two different distinctions: plasma vs buffy coat-based systems and single-spin vs double-spin processes. Plasma-based systems utilize a slower, shorter spin to isolate plasma and remove WBCs, resulting in platelet 2–3x’s baseline levels (Figure 2A). 69 Contrary, buffy coat-based systems utilize a longer, double spin to isolate a platelet-poor layer (Figure 2B). This allows for an obtained platelet concentration of 3–8x that of baseline levels, however, because of the density it also keeps a concentration of WBCs.69 Furthermore, single-spin processes, represented by many clinically used commercial devices, encompass variations such as low-platelet PRP (PRPLP) and high-platelet PRP (PRPHP). These one-step methods offer a more straightforward and less resource-intensive approach to PRP preparation. Conversely, double-spin processes (PRPDS) have historically been favored in basic science investigations due to their ability to produce PRP with higher platelet concentrations.86 These methods often involve two sequential centrifugation steps, allowing for the separation of platelets from other blood components more effectively. However, recent studies have provided conflicting insights into the strengths and limitations of single-spin and double-spin processes. Notably, Mazzocca et al87 demonstrated that PRPHP produced significantly higher platelet and white blood cell concentrations compared to both the single-step PRPLP and two-step PRPDS procedures. However, no significant differences were observed between PRPLP and PRPDS. Conversely, Saqlian et al88 and Nagata et al89 reported a greater platelet and WBC quantity following PRPDS compared to single-spin techniques. Additionally, when considering specific growth factors, Han Oh et al88 demonstrated that PRPDS resulted in a significantly greater concentration of PDGF and VEGF whereas single-spin methods produced a significantly greater concentration of TGF and FGF. While findings by Mazzocca et al underscore the potential efficacy of one-step procedures and suggest that the increased time required for two-step procedures may not necessarily be advantageous for producing therapeutic PRP preparations, other studies still provide support to the historical superiority of PRPDS.
Figure 2.
(A) Plasma-Based PRP Preparation. (B) Buffy Coat-Based PRP Preparation.
With the clinical advent of PRP use for bone and soft tissue indications, numerous commercial PRP preparation kits have entered the market. These devices offer the convenience of pre-packaged, standardized protocols, which can be especially beneficial for clinical applications. However, while designed to serve a common purpose, these kits exhibit noteworthy differences in multiple aspects of PRP preparation which manifests as variations in platelet, WBC, and RBC concentrations in the final PRP product. Numerous comprehensive reviews of currently available devices reveal substantial variability in their methodologies and the resultant PRP compositions. Dejnek et al89 extensively evaluated four commonly used commercial PRP systems: Arthrex Autologous Conditioned Plasma (ACP), Mini GPS III, Xerthra, and Dr. PRP. Among the systems evaluated, Mini GPS III notably stood out, yielding significantly higher concentrations of platelets, WBCs, and RBCs compared to the other three systems. Additionally, in a systematic review of the 10 most referenced commercially available PRP systems, Oudelaar et al83 found significant variations in platelet and leukocyte concentrations. The highest concentration of platelets was produced by the Cascade system, while the lowest concentration of platelets was generated by the ACP system. Notably, the GPS III system exhibited a significantly higher concentration of leukocytes compared to other systems. Furthermore, the study reported that the GPS III and SmartPrep systems had the highest platelet enrichment factors, while the ACP, RegenPRP, and Cascade systems showed lower platelet enrichment factors. Furthermore, when analyzing 33 different commercial systems, Fadadu et al73 found a significantly positive correlation between maximum centrifuge spin force, platelet concentration, and PDGF concentration, however, spin time demonstrated no significant relationships. Additionally, 3 of the 33 systems resulted in a platelet count less than that of whole blood. A review by Magalon et al90 also demonstrated that of the 36 PRP preparation systems analyzed, 11 resulted in a final product made up of more RBCs than platelets. These findings emphasize immense variability in commercially available PRP preparation systems. Thus, the choice of a specific commercial device plays a substantial role in determining PRP composition and underscores the importance of selecting the most suitable system based on the intended clinical application. Despite the profound importance of optimizing PRP’s platelet concentration, the challenge of defining a singular optimal value is exacerbated by the variability in research methods employed by past studies.87,91 Consequently, tailoring PRP to individual clinical contexts remains a dynamic process that considers the nature of the injury, the patient’s unique characteristics, and the desired treatment outcomes.
Activation of PRP: Unleashing the Healing Potential
The activation of PRP is an important phase in its therapeutic application, as it serves to transform concentrated platelets into a biologically active state, primed to effectively stimulate the regenerative process. This activation process encompasses two key elements. Firstly, it involves the degranulation of platelets, liberating GFs from α-granules. Secondly, it triggers the cleavage of fibrinogen, initiating matrix formation—a clotting process that facilitates the development of a platelet gel, effectively constraining the secretion of molecules to the designated site.92,93 Consequently, the choice of activator during PRP preparation becomes a critical determinant of its efficacy, influencing both the quantity and release kinetics of GFs from platelets within PRP. Research on the activation of PRP has unveiled a complex interplay of factors that significantly influence its clinical efficacy and therapeutic potential and activation methods have undergone significant development, with multiple techniques devised to unlock the potential of growth factors and other bioactive molecules.
One traditional method of activation involves the addition of bovine thrombin to PRP. Thrombin serves as a rapid activator of platelets, promoting degranulation and facilitating the conversion of fibrinogen into fibrin, resulting in the formation of a stable clot that effectively traps platelets at the target location.94 This entrapment promotes immediate degranulation and the release of growth factors and cytokines. Prior studies have demonstrated that the rapid action of thrombin resulted in an immediate release pattern of approximately 70% of stored growth factors within 10 minutes and nearly 100% released within 1 hour.29,95 While this method offers swift and substantial growth factor activation, it comes with a challenge—released growth factors are swiftly cleared, precluding their long-term stimulatory effects on cells. This concept has been supported by studies that have found that the rapid activation triggered by bovine thrombin results in a reduction in the overall quantity of growth factors accessible at the tissue location over time.69,93 If not promptly utilized upon release, GFs risk degradation before additional tissue receptors become available.95,96 Additionally, bovine thrombin has been shown to carry the potential for complications arising from the generation of antibodies that may result in immune-mediated coagulopathy.86
An alternative approach utilizes calcium chloride to convert autologous prothrombin to thrombin, resulting in platelets being trapped in a fibrin matrix. Numerous studies97,98 have demonstrated that using calcium chloride as an activator can lead to higher concentrations of specific GFs, such as TGF-β(1) and PDGF-AB. Additionally, calcium-based activators have been shown to induce a gradual and extended process of platelet activation, leading to the progressive release of platelet content.93,95 This sustained activation results in the gradual accumulation of endogenous thrombin, facilitating a slower and more extended release of growth factors spanning several days.99 Consequently, this extended-release pattern addresses the need for sustained growth factor delivery necessary for the prolonged nature of bone regeneration.100–102 Additionally, calcium chloride activation was observed to have advantages beyond its release kinetics. Zhuang et al97 demonstrated that calcium chloride can avoid the complications related to antibody formation and immune-mediated coagulopathy associated with bovine thrombin due to the autologous formation of thrombin from prothrombin. However, calcium chloride activation is not without potential shortfalls as well. An excess of calcium has been shown to trigger the swift activation of the clotting cascade, inducing rapid degranulation.102 Additionally, elevated calcium levels may enhance the activity of protein C, protein S, and antithrombin III, potentially destabilizing the fibrin clot and consequently shortening the therapeutic window for platelets.102,103
Fufa et al104 initially proposed the concept of Type-1 collagen as a safe and effective alternative to bovine thrombin for clot activation in PRP. Their initial findings supported this notion by demonstrating a reduction in clot retraction and comparable levels of PDGF-AB and VEGF release. However, recent research has cast some uncertainty on its efficacy. While numerous studies8,95 have observed a more sustained cytokine release pattern with Type-1 collagen compared to bovine thrombin, a contrasting perspective emerged from Cavallo et al,93 indicating that collagen’s platelet-activating capabilities were relatively weak, leading to a lack of clot formation and notably lower GF release compared to bovine thrombin and calcium chloride. While this approach holds promise, further investigations are imperative to elucidate the genuine activation potential of Type-1 collagen in PRP applications.
In some cases, PRP may be applied without exogenous activators. During local infusion, the presence of the natural clotting factor, thrombin, often suffices to activate platelets effectively.105,106 This simplified activation process, however, may lead to variations in growth factor release contingent upon the specific clinical context. Additionally, in a recent meta-analysis99 comparing activated and non-activated PRP, it was observed that non-activated PRP did not yield any substantial clinical improvements in terms of pain relief or functional scores when compared to a placebo. The choice of activator, whether it be calcium chloride, thrombin, collagen, or others, has a profound impact on clot formation, release kinetics, and the therapeutic potential of PRP. Understanding these factors is essential for tailoring PRP preparations to specific clinical needs and optimizing their effectiveness in various medical applications. In the context of bone healing, achieving sustained and controlled release of growth factors is often desirable as this aligns with the gradual and intricate nature of bone regeneration. Ongoing research continues to shed light on this dynamic field, enhancing our ability to harness the therapeutic potential of PRP for improved patient outcomes.
Delivery: Tailoring Application Methods
The manner in which PRP is delivered to the target site also plays a role in optimizing PRP’s therapeutic potential for bone healing. Clinically, PRP is often given through direct injection, topical application, or in combination with a surgical procedure and remains a widely employed and versatile clinical delivery method for bone healing. By injecting PRP directly into the affected site, clinicians can promote a concentrated release of growth factors precisely where they are needed most. Thus, this method expedites the regenerative process by providing a high concentration of growth factors directly to the injury site. Precision of delivery to the targeted tissue using ultrasound may also enhance clinically efficacy.107–109 Additionally, topical application of PRP has gained recognition as an effective clinical approach for surgical or wound site(s), promoting tissue repair, reducing inflammation, and accelerating the healing process.110–112 Furthermore, in addition to standalone PRP delivery, clinicians frequently combine PRP with surgical procedures involving bone grafts. This approach aims to optimize the integration of graft materials and enhance the overall success of the surgical intervention. For instance, PRP may be mixed with bone graft materials such as autografts, allografts, or synthetic grafts before implantation. However, this combination has shown contradicting effects on the enhancement of the graft’s osteogenic potential and ability to accelerate bone healing and reduce the risk of graft rejection.113–116
To address the need for sustained growth factor release, researchers have employed scaffolds as delivery vehicles for PRP. In the context of bone healing, scaffolds can play a critical role in maintaining the integrity of the injury site, preventing migration of PRP, and enabling controlled and sustained release of growth factors.117 Scaffolds such as hydrogels, sponges, and nanofiber-based structures offer the ability to tailor the release kinetics of PRP-derived growth factors.118 Thus, the choice of scaffold material can influence factors like degradation rate, which, in turn, affects the release profile of PRP components. Hydrogels and sponges, composed of materials such as alginate and gelatin, have demonstrated their efficacy as delivery systems for PRP in bone regeneration. These systems offer the advantage of tailorable scaffold degradation, which affects the release of incorporated factors, making them ideal for sustained delivery and enhanced bioavailability of growth factors at the injury site.119 In support of this, Lin et al120 incorporated PRP into an alginate hydrogel, demonstrating that the growth factors released from the hydrogel stimulated the osteogenic differentiation of human MSCs in vitro. Lu et al121 further investigated the growth factor release kinetics of PRP-incorporated alginate hydrogels, showcasing the varying release profiles based on carrier type and the potential of these factors to promote osteoblast-like cell proliferation and activity. In addition to alginate, gelatin, a denatured collagen derivative, has gained attention as a base material for scaffolds in bone healing. Gelatin shares functional groups with collagen, the primary organic component of bone, yet is easier to obtain and less expensive making it an attractive option.119,122 Animal studies by Hokugo et al123,124 have demonstrated that PRP growth factors can be immobilized within gelatin hydrogels, leading to growth factor release correlating with hydrogel degradation. Such studies highlight the potential of hydrogels and sponges to offer controlled and sustained delivery of PRP-derived growth factors, contributing to enhanced bone healing both in vitro and in vivo. Incorporation of bioactive inorganic calcium phosphates, such as carbonated hydroxyapatite (CHA), into PRP-based scaffolds holds significant promise for bone healing and regeneration. Kaur et al125 conducted a study in which they explored the combination of PRP and CHA, finding that this hybrid scaffold yielded significantly enhanced histological bone formation. This suggests that the integration of CHA into PRP delivery systems can enhance the osteogenic potential, potentially accelerating bone healing. Additionally, a study by Liu et al,126 focusing on the inclusion of platelets in calcium phosphate cement, indicated promising outcomes for angiogenesis and osteogenesis. Furthermore, an animal study by Qiu et al127 adds to the growing body of evidence supporting the positive impact of PRP in combination with calcium phosphate cement on bone regeneration by demonstrating favorable results in minipigs. These studies underline the versatile applications of PRP, especially when combined with calcium-based materials, in promoting both vascularization and bone tissue formation. PRP has also been covalently or ionically bonded onto plasma polymers, showcasing enhanced scaffold properties.128 Specifically, it has been reported that the application of poly-ε-caprolactone (PCL) nanofibers coated with PRP substantially enhances the survival and growth of human MSCs.128 These findings emphasize the diverse strategies available for optimizing PRP delivery systems and their potential to enhance bone healing through various approaches, including surface modifications and the development of novel biomaterials.
A Review of Pre-Clinical and Clinical Studies
Vitro Pre-Clinical Studies
This comprehensive review identified 24 in vitro studies that investigated the effects of PRP or a related derivative, on various cell types.31,32,61,67,72,129–147 The diverse spectrum of cell types included osteoblasts, fibroblasts, osteocytes, myocytes, tenocytes, human umbilical vein endothelial cells, bone marrow mesenchymal stem cells, marrow stromal cells, and human osteosarcoma cell lines. Among these studies, 14 (58%)32,61,67,129,136–140,142–144,146,147 of the 24 studies reported PRP increased cell proliferation, 7 studies (29%)67,132,134,135,139,141 reported PRP increased expression of bone-related genes and growth factors, and 5 studies (21%)31,132,143,146,147 reported PRP increased cell migration. Notably, several of these investigations highlighted the effects of PRP were dose-dependent with differing cell responses at different concentrations.61,67,72,142,144,146 In addition, 2 studies (8%)140,141 provided evidence suggesting that PRP has the potential to facilitate osteogenic differentiation of pluripotent stem cells. Furthermore, 1 study (4%)137 reported PRP’s ability to induce tubular formation in human umbilical vein endothelial cells (HUVECs). Another study (4%)145 indicated an increase in osteoblast viability and adhesion following PRP exposure. Conversely, 2 studies (8%)130,131 did not discern any notable impact of PRP on cell behavior. Lastly, 1 study (4%)72 found that concentrations of PRP exceeding 60% decreased cell viability and migration. A summary of the main details of all in-vitro pre-clinical studies can be found in Table 2.
Table 2.
Effects of PRP on Cell Behavior in vitro
| Author (Year) | Cell Type(s) Used | Control Group(s) | PRP Effect on Cells |
|---|---|---|---|
| Kinoshita et al (2020)31 | Human osteoblasts | Cell media only | Fresh and freeze-dried PRP increased osteoblast proliferation |
| Kanno et al (2004)129 | Human osteosarcoma cell lines HOS and SaOS-2 | Cell media only | PRP increases HOS and SaOS-2 proliferation in dose-dependent manner |
| Fernandez-Medina et al (2019)72 | Human osteoblasts | Thrombus (clot) | Reduced cell viability and migration above concentrations of 60% |
| Ferreira et al (2005)142 | Human osteoblasts | None | PRP increases osteoblast proliferation in dose-dependent manner up to 50% concentration |
| Steller et al (2019)143 | Osteoblasts and oral fibroblasts | Cell media only | PRP and PRF increased proliferation and migration of osteoblasts and fibroblasts, counteracting the negative effects of zoledronic acid |
| Ogino et al (2016)144 | Human osteosarcoma cell line SaOS-2 | Platelet poor plasma (PPP) | PRP increases cell proliferation in dose-dependent manner |
| Vahabi et al (2019)45 | MG-63 osteoblast-like cells and human fibroblasts | Cell media only | PRP increases viability and adhesion of osteoblast like cells and fibroblasts |
| Celotti et al (2015)146 | Human osteosarcoma cell line SaOS-2 | Cell media only | PRP increases cell proliferation and migration in dose-dependent manner |
| Wang et al (2018)147 | Human osteoblasts | Cell media only | iPRF more so than PRP, promoted osteoblast proliferation and migration |
| Graziani et al (2006)61 | Human osteoblasts and fibroblasts | Cell media only | PRP increases cell proliferation of both osteoblasts and fibroblasts in dose dependent manner up to 50% concentration above which caused reduced cell proliferation |
| Vahabi et al (2017)130 | MG-63 osteoblast-like cells and human fibroblasts | Cell media only | PRP did not show significant increase in cell proliferation |
| Casati et al (2015)30 | Human osteosarcoma cell line SaOS-2 | Cell media only | PRP stimulates cell migration |
| Slapnicka et al (2008)131 | Human osteoblasts | Cell media only | PRP did not significantly increase cell proliferation |
| Martinotti et al (2014)132 | Human osteosarcoma cell line SaOS-2 | Cell media only | PRP promotes cell migration and induces a mixed osteoclastic/osteogenic gene expression |
| Gaßling et al (2009)133 | Human osteosarcoma cell line SaOS-2, human osteoblasts, and human fibroblasts | Cell media only | PRP led to increased growth factor secretion compared to PRF |
| Herrera et al (2012)134 | Human osteosarcoma cell line SaOS-2 | Cell media only | PRP increases osteoblast activity and cytokine release |
| He et al (2009)135 | Rat osteoblasts | Cell media only | PRF led to gradual and sustained release of cytokines compared to PRP |
| Mazzocca et al (2012)136 | Human osteocytes, myocytes, and tenocytes | Cell media only | All forms of PRP increased cell proliferation of all cell types |
| Mooren et al (2010)137 | Rat osteoblast-like cells and human umbilical vein endothelial cells (HUVECs) | Cell media only | PRP promotes proliferation of osteoblast-like cells and promotes tubular formation in endothelial cells in a dose-dependent manner |
| Garcia-Martinez et al (2012)138 | Human osteoblasts | Cell media only | PRP increases cell proliferation and altered expression of cell-surface markers |
| Zou et al (2014)140 | Rabbit bone marrow mesenchymal stem cells (BMSCs) | Cell media only | PRP can promote proliferation and osteogenic differentiation of BMSCs |
| Bi et al (2010)139 | Goat marrow stromal cells (MSCs) | Cell media only | Cell growth and alkaline phosphatase activity greater on the TCP+PRP composite compared to TCP and cell media alone control. |
| Chen et al (2013)67 | Rate Bone marrow mesenchymal stem cells (BmMSCs) | Cell media only | Greater cell proliferation in high and medium concentration PRP. Higher alkaline phosphatase activity in low and medium concentration PRP, but inhibited activity in high concentration PRP. |
| Qi et al (2015)141 | Bone marrow mesenchymal stem cells (BmMSCs) | Cell media only | Increased expression of collagen I, collagen III, tenomodulin, and osteocalcin genes, increased alizarin red staining, and increased alkaline phosphatase activity in PRP group suggestive of ability of PRP to promote osteogenic differentiation |
Vivo Pre-Clinical Studies
A total of sixty pre-clinical in vivo animal studies were identified which investigated the impact of PRP on bone healing.63,67,123,139,141,148–202 The animal models employed in these studies exhibited a notable variation in usage, with rabbits being the most commonly utilized model in 25 studies (42%), followed by rats in 12 studies (20%) and sheep in 8 studies (13%). Conversely, the less frequently employed animal models included goats in 2 studies (3%), pigs in 2 studies (3%), and mice in 1 study (2%). Regarding the bones studied, the tibia was the most frequently examined bone in 23 studies (38%), followed by the femur in 18 studies (30%) and the radius in 11 studies (18%). In contrast, the skull/forehead was among the least studied bone in 3 studies (5%), along with the fibula and metatarsal, each studied in 2 studies (3%).
Out of the 43 in vivo animal studies that incorporated scaffolds-based delivery methods, a variety of scaffold types were employed. Examples included calcium phosphate, bone autograft, bone allograft, gelatin hydrogels, titanium mesh, collagen, ceramic-coated hydroxyapatite, and coral. In several instances, studies compared the effectiveness of PRP delivery with and without a scaffold, with the most favorable outcomes generally observed when PRP was administered alongside a scaffold.123,150,154,161,168,175,176,178 Notably, the dose-dependent response of PRP observed in in vitro studies was also echoed in some of the in vivo experiments.67,190
Of the 45 pre-clinical animal studies that evaluated radiographic bone healing, 36 studies (80%) reported improvements when PRP was employed, whereas 7 studies (16%) did not reveal any radiographic improvement, and 2 studies (4%) even indicated reduced radiographic bone healing. Similarly, out of the 58 pre-clinical animal studies assessing histopathologic bone healing, 43 studies (74%) reported positive outcomes when PRP was applied. Conversely, 13 studies (22%) did not detect any histopathologic improvement, and 2 studies (3%) reported reduced histopathologic bone healing in association with PRP. Biomechanical properties also displayed favorable trends, with 11 out of 13 pre-clinical animal studies (85%) reporting improvements in bone healing when PRP was employed. Only 2 studies (15%) did not observe any biomechanical improvement, and none indicated a reduction in biomechanical properties when PRP was used.
In summary, pre-clinical in vivo animal studies generally demonstrate overall positive effects of PRP on bone healing. However, the substantial variability in study designs and protocols makes direct comparisons challenging. Moreover, several studies combined PRP with other factors like stem cells or scaffolds, complicating the isolation of PRP’s specific effects. Additionally, many studies compared interventions to untreated negative controls, which may not be ideal, and a few studies lacked control groups entirely. Furthermore, subjective evaluations and a lack of statistical comparisons were observed in several studies.152,154,155,158,167,171,198 Lastly, the use of blinded analysis of specimens was inconsistent, with only 20 studies (33%) reporting its implementation. Table 3 presents a concise overview of the key information pertaining to all in-vivo pre-clinical studies.
Table 3.
Effects of PRP on Bone Healing in Pre-Clinical in vivo Animal Models
| Author (Year) | Animal Model (Bone) | Scaffold Used | PRP Group(s) | Control Group(s) | Endpoint | Blinded Evaluation? | Radiographic Outcome | Histopathologic Outcome | Biomechanical Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Rai et al (2007)164 | Rat (femur) | Polycaprolactone tricalcium phosphate (PCL-TCP) | PCL-TCP + PRP | PCL-TCP | 12 weeks | X-rays | Increased bone formation in PRP group by x-ray and micro-CT | Similar qualitative outcomes between PRP group and control group | PRP group stiffer but no difference in yield and maximum torque |
| Cho et al (2013)177 | Dog (tibia) | None | PRP | Untreated | 16 weeks | None | Bone activity index on nuclear scan greater at 4 weeks in PRP group, but less in PRP group at weeks 8, 12, and 16 | Bone-to-implant contact (BIC) was higher for the PRP group | None |
| Dallari et al (2006)178 | Rabbit (femur) | Freeze-dried bone allograft (FDBA) | PRP Bone marrow stromal cells (BMSCs)+PRP FDBA+PRP BMSCs+FDBA+PRP |
Untreated | 12 weeks | Histology | None | Increased bone healing in all experimental groups compared to control. Increased bone healing in FDBA+PRP, and BMSCs+FDBA+PRP compared to PRP alone |
None |
| Guzel et al (2015)196 | Rat (femur) | None | PRP | Untreated | 9 weeks | Histology and biomechanics | None | Increased bone healing in the PRP group | Higher ultimate failure load in PRP group |
| Hakimi et al (2010)197 | Mini pig (tibia) | Autologous bone graft | Autologous bone graft+PRP | Autologous bone graft | 6 weeks | None | Similar rates of osseous bridging on x-rays | Superior bone formation in central and cortical defect zone in PRP group | None |
| Hokugo et al (2005)123 | Rabbit (ulnar) | Gelatin hydrogel | Gelatin Hydrogel+PRP Fibrin+PRP PRP |
Gelatin hydrogel Untreated |
4 weeks | None | Greatest rate of bone healing in Gelatin hydrogel+PRP group followed by the Fibrin+PRP group | Greatest rate of bone healing in Gelatin hydrogel+PRP group followed by the Fibrin+PRP group | None |
| Jungbluth et al (2010)198 | Mini pig (tibia) | Calcium phosphate granules (CPG) | CPG+PRP | CPG | 6 weeks | X-rays | Semi-quantitative analysis showed slightly more osseous bridging in PRP group | Greater new bone formation in PRP group in central and cortical defect zones | None |
| Kanthan et al (2011)150 | Rabbit (tibia) | Artificial bone graft (ABG) | ABG+PRP PRP |
ABG Untreated |
11 weeks | X-rays | Greatest healing in ABG+PRP group compared to all other groups. PRP alone better than untreated control but no different to ABG alone | Greatest healing in ABG+PRP group. ABG better healing than control. PRP did NOT have better histologic healing than untreated control. | None |
| Kasten et al (2008)151 | Rabbit (radius) | Calcium-deficient hydroxyapatite ceramic scaffold (CDHA) | CDHA+PRP CDHA+PRP+mesenchymal stem cells (MSCs) |
CDHA Untreated |
16 weeks | None | Bone formation greater in CDHA+PRP and CDHA+PRP+MSC groups compared to CDHA alone, as measured by micro-CT | Bone formation greater in CDHA+PRP and CDHA+PRP+MSC groups compared to CDHA alone | All test groups were stiffer than untreated control. No difference in stiffness between test groups |
| Kroese-Deutamn et al (2008)152 | Rabbit (radius) | Titanium fiber mesh (TFM) | TFM+autologous bone+PRP TFM autologous bone |
TFM | 12 weeks | None | Bone healing seen in all test groups but not in all control groups | Greater bone formation in TFM+autologous bone+PRP than all other groups | None |
| Kurikchy et al (2013)153 | Rabbit (femur) | Xenogeneic bone graft (XBG) | XBG+PRP | XFG Untreated |
4 weeks | None | None | Increased number of osteocytes, osteon diameter, and lamellar thickness in XBG+PRP groups compared to all other groups | None |
| Lin et al (2013)154 | Rabbit (femur) | Nanohydroxyapatite-type I collagen beads (CIB) | CIB+BMSCs+PRP CIB+PRP PRP+BMSCs PRP |
Untreated | 8 weeks | Histology | Greater bone healing in all experimental groups compared to untreated control as assessed on micro-CT | Increased bone formation in CIB+BMSCs+PRP and PRP+BMSCs groups | None |
| Lysiak et al (2008)155 | Rabbit (femur) | Collagen | Collagen+PRP | Untreated | 12 weeks | None | None | Greater bone formation in experimental groups compared to control group | None |
| Malhotra et al (2014)156 | Sheep (tibia) | Biphasic calcium phosphate (BCP) | BCP+PRP | BCP Untreated |
4 weeks | X-ray and histology | Greater bone healing in BCP+PRP compared to all other groups via micro-CT Greater bone healing in BCP+PRP group compared to untreated but no different to BCP alone on x-ray. |
Greater bone formation in BCP+PRP compared to BCP alone and untreated control. | None |
| Manitha et al (2009)158 | Goat (femur) | Tri-phasic ceramic-coated hydroxyapatite (HASi) | HASi+BMSCs+PRP | HASi | 8 weeks | None | Greater bone formation in the experimental group compared to HASi alone | No significant difference in bone formation between all groups | None |
| Niemeyer et al (2010)160 | Sheep (tibia) | Collagen sponges (CS) | CS+Adipose-tissue derived stems cells (ASCs)+PRP | CS | 26 weeks | None | No significant difference in bone formation between test group and control assessed on x-ray | No significant difference in bone formation between test group and control assessed on histology | None |
| Parizi et al (2012)162 | Rabbit (radius) | Coral | Coral+PRP | Coral Untreated |
8 weeks | Gross evaluation | Improved bone healing in the coral and coral+PRP groups compared to untreated control | Improved bone healing in the coral and coral+PRP groups compared to untreated control | PRP with coral group had higher ultimate load than the negative control group, whereas coral group alone did not |
| Simman et al (2008)166 | Rat (femur) | None | PRP | Untreated | 4 weeks | Fully blinded analysis | Higher callus to cortex width ratio in PRP group | No difference in BMP2 or total TGF-B expression between the groups | Increased strength in PRP group |
| Souza et al (2012)167 | Dog (radius) | None | PRP | Untreated | 8 weeks | Fully blinded analysis | Greater healing in the PRP group | PRP group showed new bone formation superior to control group | None |
| Sugimori et al (2006)168 | Rat (tibia) | Apatite foam (AF) | AF+PRP PRP |
AF Untreated |
12 weeks | None | None | AF+PRP has more bone formation than all other groups | None |
| Zhang et al (2013)169 | Rabbit (radius) | Deproteinized bone matrix (DBM) | DBM+PR DBM+PRP+MSCs |
DBM | 12 weeks | None | Greater bone formation in all experimental groups compared to control, and greater bone formation in DBM+PRP+MSC compared to DBM+PRP | Greater bone formation in all experimental groups compared to control, and greater bone formation in DBM+PRP+MSC compared to DBM+PRP | None |
| Chaput et al (2007)148 | Rabbit (femur) | Beaded metal implant (BMI) | BMI+PRP | BMI | 5 weeks | None | None | No difference in bone growth between groups | None |
| Hernandez-Fernandez et al (2013)149 | Sheep (femur) | None | PRP | Untreated | 6 weeks | Fully blinded analysis | No difference in bone growth between groups | No difference in bone growth between groups | None |
| Molina-Minano et al (2009)157 | Rabbit (tibia) | Autologous bone graft (ABG) | ABG+PRP PRP |
ABG Untreated |
8 weeks | Fully blinded analysis | No difference in bone growth between groups | No difference in bone growth between groups | None |
| Nather et al (2012)159 | Rabbit (tibia) | Autologous bone graft Allograft |
Allograft+PRP | Allograft | 24 weeks | None | None | Allograft+PRP had more osteocytes than allograft alone. The greatest new bone formation, callus encasement index, and osteocyte count was seen in autograft compared to all other groups |
None |
| Rabillard et al (2009)163 | Dog (ulnar) | Calcium phosphate ceramic granules (CaP) | CaP+PRP | CaP | 16 weeks | None | None | No difference in bone growth between groups | None |
| Sarkar et al (2006)165 | Sheep (tibia) | Collagen matrix (CM) | CM+PRP | CM | 12 weeks | None | No difference between groups on x-ray or CT | No difference between groups | No difference between groups |
| Lopez et al (2019)63 | Dog (radius/ulnar and tibia/fibula) | None | PRP | Untreated | 24 weeks | Fully blinded analysis | Faster rate of bone healing in the PRP group | None | None |
| Orth et al (2018)161 | Mouse (femur) | Microcalcite (MCA) | MCP+PRP PRP |
Untreated | 5 weeks | None | Bone volume higher in MCRP+PRP group compared to controls | Smaller callus formation in MCP+PRP group compared to control | Polar moment of inertia (PMOI—used as surrogate for mechanical stability) higher in MCRP+PRP group compared to controls |
| Szponder et al (2018)173 | Rabbit (tibia) | Tri-calcium phosphate (TCP) | External fixator or intramedullary nail with TCP+PRP | None | 12 weeks | None | Bone formation observed in both ex-fix and IMN group | Bone formation observed in both ex-fix and IMN group | None |
| Canbeyli et al (2018)170 | Rabbit (femur) | None | PRP | Untreated | 12 weeks | X-rays | Increased union rate in PRP group | Greater cortical callus formation, woven bone percentage area, fibroblast proliferation, and mature bone formation in PRP group | None |
| Kim et al (2014)172 | Rat (ulna) | Gelatin hydrogel | PRP+SEW2871 (macrophage recruiter) PRP |
Untreated | 6 weeks | None | Greater bony healing and bone density observed in the PRP+SEW and PRP groups compared to controls as assessed by micro-CT | Greater bony healing observed in the PRP+SEW and PRP groups compared to controls | None |
| He et al (2015)171 | Rabbit (radius) | Poly (lactic-co-glycolic acid) with calcium phosphate cement (PLGA-CPC) | PLGA-CPC+PRP | PLGA-CPC | 12 weeks | None | No difference in healing at 12 weeks between groups. However, micro-CT showed more bone healing in PRP group compared to control | More bone formation in PRP group compared to control | None |
| Shafiei-Sarvestani et al (2015)174 | Rabbit (radius) | None | PRP | Untreated | 8 weeks | Histology | More bone growth and union in PRP group | Greater bony healing in PRP group | Greater ultimate strength in PRP group |
| Weibrich et al (2004)189 | Rabbit (femur) | None | PRP | Untreated | 4 weeks | None | None | Higher platelet concentration in PRP group but no difference in bone healing | None |
| Wiltfang et al (2004)190 | Mini pig (forehead) | Autologous bone graft Tricalcium-phosphate granules (Cerasorb) Bovine spongious blocks (BioOss) Bovine bone-inducing collagenous sponge (Colloss) |
4 different scaffolds (listed left) with PRP (2 different concentrations) | 4 scaffolds without PRP | 12 weeks | None | PRP increased bone healing in the autologous bone group but not the other bone scaffold groups | PRP did not change bone healing | None |
| Thorwarth et al (2006)188 | Pig (skull) | Autologous bone graft Deproteinized bovine bone matrix (DBBM) |
2 scaffolds with PRP (2 different concentrations) | Autologous bone alone DBBM alone |
26 weeks | None | No significant difference in bone mineralization | No difference in expression of bone-related gene expression | None |
| Bi et al (2010)139 | Goat (tibia) | Tricalcium phosphate/chitosan composite (TCP) | TCP+PRP | Untreated | 16 weeks | None | Improved bone healing in the TCP+PRP group | Higher rate of newly formed bone in the TCP+PRP group | TCP+PRP biomechanically equivalent to TCP alone |
| Kon et al (2010)184 | Sheep (femur) | Hydroxyapatite-collagen nanocomposite scaffold | Hydroxyapatite-collagen nanocomposite scaffold+PRP | Untreated | 24 weeks | Histology | Scaffold+PRP had worse bone regeneration than scaffold alone | Scaffold+PRP had worse bone regeneration than scaffold alone | None |
| Oryan et al (2012)186 | Rabbit (radius) | Hydroxyapatite scaffold | Hydroxyapatite+PRP | Untreated | 8 weeks | N/A | Scaffold+PRP and scaffold without PRP had equal bone formation but better than negative control | Scaffold+PRP and scaffold without PRP had equal bone formation but better than negative control | Ultimate strength greater in scaffold+PRP group compared to untreated defect control |
| Neves et al (2013)185 | Rabbit (fibula) | None | PRP Hyperbaric oxygen + PRP |
Untreated | 8 weeks | None | None | Hyperbaric oxygen and PRP together or alone showed increased bone formation | None |
| Kasten et al (2012)183 | Rabbit (radius) | Calcium-deficient hydroxyapatite (CDHA) | CDHA+PRP | CDHA alone | 16 weeks | None | CDHA+PRP had greater bone formation | CDHA+PRP had greater bone formation | None |
| Chen et al (2013)67 | Rat (femur) | None | PRP clot with low, medium, and high PRP concentrations | Untreated | 8 weeks | Histology and radiology | Medium concentration PRP has increased bone healing | Medium concentration PRP has increased bone healing | Ultimate strength higher in medium concentration PRP |
| Gumieiro et al (2010)181 | Rat (tibia) | None | PRP | Untreated | 12 weeks | None | None | Increased bone formation in the PRP group | None |
| Filardo et al (2014)180 | Sheep (metatarsal) | Biomorphic silicon carbide (BioSiC) scaffold | BioSiC+PRP | BioSiC alone | 16 weeks | None | No radiographic difference in the PRP group | Increased bone formation in the PRP group | None |
| Velev et al (2015)179 | Rabbit (tibia) | Calcium phosphate cement (CPC) | CPC+PRP | CPC alone | 4 weeks | None | None | Increased bone formation in the PRP group | None |
| Zhong et al (2014)192 | Dog (tibia) | Tricalcium phosphate (TCP) | TCP+PRP | TCP alone | 12 weeks | None | Increased bone formation in the PRP group | Increased bone formation in the PRP group | Ultimate strength higher in TCP+PRP group |
| Qi et al (2015)141 | Rat (femur) | Calcium phosphate particles (CPP) | CPP+PRP | CPP alone | 4 weeks | None | Increased bone formation in the PRP group | Increased bone formation in the PRP group | None |
| Yilmaz et al (2014)191 | Pig (tibia) | Tricalcium phosphate (TCP) | TCP+PRP | TCP alone | 12 weeks | None | None | Increased bone formation in the PRP group | None |
| Hakimi et al (2014)182 | Mini pig (tibia) | Calcium phosphate granules (CPG) | CPG+PRP+bone marrow concentrate (BMC) | CPG alone | 6 weeks | None | Increased bone formation in the CPG+PRP+BMC group | Increased bone formation in the CPG+PRP+BMC group | None |
| Chen et al (2016)176 | Rabbit (radius) | Calcium sulfate (CS) | CS+PRP PRP alone |
CS alone | 10 weeks | None | Increased bone formation in the CP+PRP group | Increased bone formation in the CP+PRP group | None |
| Bölükbaşı et al (2013)175 | Sheep (tibia) | Biphasic calcium phosphate (BCP) | BCP+PRF PRF alone |
Untreated | 6 weeks | None | Increased bone formation in the BCP+PRF group | None | None |
| Schneppendahl et al (2015)187 | Rabbit (tibia) | Autologous bone graft | Autograft+PRP | Autograft | 6 weeks | N/A | Increased bone formation in the Autograft+PRP group | Increased bone formation in the Autograft+PRP group | None |
| Batista et al (2011)194 | Rabbit (tibia) | Tricalcium phosphate (TCP) | TCP+PRP | TCP+bone marrow concentrate | 4 weeks | None | Similar bone formation in the TCP+PRP group on x-ray but increased bone formation in the TCP+PRP group on micro-CT | Increased bone formation in the TCP+PRP group | |
| Park et al (2016)200 | Dog (femur) | None | PRF | Untreated | 4 weeks | None | None | Increased bone formation in PRF group | None |
| Sindel et al (2017)202 | Rat (skull) | None | PRF | Untreated | 3 weeks | None | None | Increased bone formation in PRF group | None |
| Dulgeroglu et al73 (2017)195 | Rat (femur) | None | PRF | Untreated | 4 weeks | Histology | Increased bone formation in PRF group | Increased bone formation in PRF group | None |
| Akyildiz et al (2018)193 | Rat (tibia) | None | PRF | Untreated | 6 weeks | Radiology and histology | Reduced bone formation in PRF group | Reduced bone formation in PRF group | None |
| Raafat et al (2018)201 | Rat (tibia) | None | PRF Simvastatin+PRF |
Untreated | 8 weeks | None | Increased bone formation in simvastatin+PRF group | Increased bone formation in simvastatin+PRF group | None |
| Lucarelli et al (2005)199 | Sheep (metatarsal) | Allograft | Allograft+bone-marrow-derived stromal stem cells (BmMSCs)+PRP+collagen | Allograft alone | 16 weeks | Histology | Increased bone formation in PRP group | Increased bone formation in PRP group | Higher extraction torque values in the PRP group |
Vivo Clinical Studies
There were 24 clinical studies that evaluated PRP to treat fractures in human patients (Table 4). 203–226 Among these studies, 11 were prospective randomized control trials, 8 were prospective case series, and 5 were retrospective case series. The bones predominantly examined were the tibia in 9 studies (38%) and the femur in 5 studies (21%). In terms of PRP delivery methods, 11 studies (46%) utilized PRP injection alone at the injury site, while 9 studies (38%) incorporated PRP with a scaffold, such as bone graft. Four studies (17%) involved the injection of PRP in combination with other substances like bone marrow aspirate or stem cells. The average number of patients per study was 52±52, with a range of 10 to 200 patients, and an average follow-up period of approximately 16±15 months (range 2–72 months). Of the clinical studies, 19 (79%) reported favorable clinical outcomes associated with the use of PRP to improve bone healing. Three studies (13%) demonstrated equivocal outcomes, while two studies (8%) indicated negative effects of PRP on bone healing. As with the pre-clinical studies, there is considerable variability among clinical studies, making it challenging to draw direct comparisons between outcomes. Notably, 9 studies (38%) lacked a control group, rendering it impossible to draw definitive conclusions due to the absence of a comparative baseline. Additionally, 14 studies (58%) did not employ any form of randomization in patient assignment to different treatment types within the study. It is worth noting that, to the best of our knowledge, there are no published double-blinded randomized control trials of PRP in the context of bone healing. Considering the existing body of research, which encompasses a reasonable number of patients and follow-up periods, future clinical investigations should prioritize the use of double-blinded randomized control trials to ascertain the true efficacy of PRP in promoting bone healing.
Table 4.
Effects of PRP on Bone Healing in Clinical Studies
| Author (Year) | Study Design | PRP Delivery | Bone(s) Studied | PRP Group (s) | Control Group(s) | Sorting Method | Number of Patients | Follow-Up | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Namazi et al (2016)217 | Prospective randomized control trial | Intra-articular PRP injection | Radius | CRPP+PRP injection | CRPP | Non-blinded randomization | 30 | 6m | PRP group shows decreased pain and increased function |
| Wei et al (2012)225 | Prospective randomized control trial | Allograft bone+PRP | Calcaneus | ORIF+allograft+PRP | ORIF+allograft Autograft |
Non-blinded randomization | 175 | 72m | Better radiographic outcomes for allograft+PRP and autograft groups compared to allograft alone |
| Namazi et al (2016)218 | Prospective randomized control trial | Intra-articular PRP injection | Scaphoid | Casting+PRP injection | Casting | Non-blinded randomization | 14 | 6m | PRP group had decreased pain at rest and increased total function |
| Griffin et al (2013)210 | Prospective randomized control trial | Fracture site PRP injection | Femur | CRPP+PRP injection | CRPP | Participant blinded randomization | 200 | 12m | PRP reduced length of hospital stay, but risk of revision and clinical outcomes were equivalent |
| Rodriguez-Collazo et al (2015)226 | Retrospective case series | Demineralized bone matrix (DBM)+PRP | Tibia/fibula | Ilizarov fixator+DBM+PRP Ilizarov fixator+DBM+concentrate bone marrow aspirate (cBMA) |
Ilizarov fixator+DBM | None | 20 | 18m | Faster radiographic healing with PRP and cBMA compared to control |
| Samy et al (2016)220 | Prospective randomized control trial | Fracture site PRP injection | Femur | CRPP+PRP injection | CRPP | Non-blinded randomization | 60 | 12–48m | Faster radiographic healing with PRP group, no difference in functional outcomes |
| Chiang et al (2007)206 | Prospective case series | Bone graft and autologous platelet gel at fracture site | Femur and tibia | Internal or external fixation, ± soft tissue reconstruction | None | None | 12 | 24–40m | Possible benefit of using PRP to treat non-unions |
| Lee et al (2014)213 | Prospective randomized control trial | Bone marrow aspirate concentrate (BMAC)+PRP at fracture site | Tibia | External fixator (limb lengthening) | External fixator alone | Non-blinded randomization | 20 | 24m | Significant improvement in bone formation in PRP+BMAC group |
| Calori et al (2008)205 | Prospective randomized control trial | PRP injection at fracture site | Various | Surgical fixation + PRP | BMP-7 injection at fracture site | None | 120 | 9–25m | Lower rate of clinical and radiographic union in PRP group compared to BMP-7 group |
| Liebergall et al (2013)214 | Prospective randomized control trial | Demineralized bone matrix (DBM), mesenchymal stem cells (MSCs), and PRP injected into fracture site | Tibia | Surgical fixation + DBM+MSCs+PRP | Surgical fixation alone | Non-blinded randomization | 24 | 12m | The PRP group decreased time to union |
| Bielecki et al (2008)204 | Prospective case series | Platelet-leukocyte rich gel (PLRG) injection at fracture site | Tibia/fibula | PLRG injection to fracture site | None | None | 32 | 9m | Possible benefit of using PRP to treat non-unions |
| Peerbooms et al (2012)219 | Prospective randomized control trial | PRP and bone chips at fracture site | Tibia | PRP and bone chips | Bone chips alone | Non-blinded randomization | 41 | 3m | PRP group had lower bone density |
| Mariconda et al (2008)216 | Prospective case series (compared to historical control group) | PRP injection at fracture site | Various | PRP and external fixator | External fixator alone | None | 20 | 9m | PRP showed equal union rates compared to controls |
| Dallari et al (2007)207 | Prospective randomized control trial | PRP and bone chips at fracture site | Tibia | PRP and bone chips PRP+bone chips+bone marrow stromal cells |
Bone chips alone | Non-blinded randomization | 33 | 12m | Higher rates of osseointegration in both PRP groups compared to control |
| Sanchez et al (2009)221 | Retrospective case series | PRP and bone graft at fracture site at time of surgery, then repeated PRP injections into fracture site post-operatively | Various | PRP and bone graft | None | None | 15 | 8m | Possible benefit of using PRP to treat non-unions |
| Malhotra et al (2015)215 | Prospective case series | PRP injection at fracture site | Various | PRP injection | None | None | 94 | 4m | Possible benefit of using PRP to treat non-unions |
| Galasso et al (2008)208 | Prospective case series | PRP injection at fracture site | Various | Intra-medullary nail and PRP at fracture site | None | None | 22 | 13m | Possible benefit of using PRP to treat non-unions |
| Say et al (2014)222 | Prospective case series | PRP injection at fracture site | Various | PRP injection at fracture site | None | None | 20 | 12m | Possible benefit of using PRP to treat non-unions |
| Tarallo et al (2012)224 | Retrospective case series | Bone graft+PRP | Ulna | Surgical fixation with bone graft+PRP | None | None | 10 | 3–36m | Possible benefit of using PRP to treat non-unions |
| Golos et al (2014)209 | Prospective case series | PRP injection at fracture site | Various | PRP injection | None | None | 132 | 4m | Possible benefit of using PRP to treat non-unions |
| Bibbo et al (2005)203 | Prospective case series | Autologous platelet concentrate (APC) | Various | APC+autograft APC alone |
None | None | 62 | 2m | Possible benefit of using PRP to treat high risk fractures |
| Kitoh et al (2007a)211 | Retrospective case series | Bone marrow cells (BMCs)+PRP at distraction osteotomy site | Femur/tibia | Distraction osteogenesis BMC+PRP | Distraction osteogenesis alone | None | 20 | N/A | Faster union rate in BMC+PRP group |
| Kitoh et al (2007b)212 | Retrospective case series | Bone marrow cells (BMCs)+PRP at distraction osteotomy site | Femur/tibia | Distraction osteogenesis BMC+PRP | Distraction osteogenesis alone | None | 46 | N/A | Faster union rate in BMC+PRP group |
| Sys et al (2011)223 | Prospective randomized control trial | Autograft+PRP to posterior lumbar interbody fusion site | Lumbar spine | Autograft+PRP | Autograft alone | Non-blinded randomization, Radiologists were blinded | 38 | 24m | No improvement in autograft+PRP compared to autograft alone |
Conclusion
Recent evidence gathered in this extensive review of in vitro pre-clinical, in vivo pre-clinical, and clinical studies underscores the growing significance of PRP as a valuable adjunct in the domain of bone healing. In vitro investigations have demonstrated PRP’s potential to stimulate various cell types, promoting proliferation, gene expression, and migration, thereby substantiating its regenerative potential at the cellular level. Pre-clinical animal investigations, despite the inherent diversity in experimental models and methodologies, affirm the positive impact of PRP on radiographic, histopathologic, and biomechanical aspects of bone regeneration. However, the landscape of pre-clinical research reveals the complexity of direct comparisons due to the variable inclusion of adjunctive factors. In the clinical arena, a majority of studies extend support for the beneficial role of PRP in bone healing yet emphasize the demand for more rigorous methodologies to delineate its precise therapeutic potential. Furthermore, investigations delving into dose-dependent PRP effects and the differentiation between PRP formulations concerning platelet concentration and leukocyte content also represent areas meriting further exploration.
Overall, PRP has emerged as a promising adjunctive tool in the context of bone healing, offering multifaceted advantages that encompass augmented cellular responses, accelerated tissue restoration, and potential expedited rehabilitation. However, advancing its integration into evidence-based medical practice necessitates meticulous and standardized clinical investigations, encompassing larger and more diverse patient cohorts, and employing well-defined outcome measures. These endeavors are poised to deepen our comprehension of PRP’s therapeutic implications, particularly in the dynamic field of regenerative medicine, offering renewed optimism for individuals seeking enhanced musculoskeletal recovery.
Abbreviations
PRP, Platelet-Rich Plasma; LR-PRP, Leukocyte-Rich PRP; LP-PRP, Leukocyte-Poor PRP; PRPLP, Low-Platelet PRP; PRPHP, High-Platelet PRP; PRPDS, Double-Spin PRP; FDA, Food and Drug Administration; GF, Growth Factor; IL-1, Interleukin-1; IL-6, Interleukin-6; TNF-α, Tumor Necrosis Factor-alpha; PDGF, Platelet-Derived Growth Factor; TGF-β, Transforming Growth Factor-beta; IGF-1, Insulin-Like Growth Factor-1; ECM, Extracellular Matrix; MSCs, Mesenchymal Stem Cells; BMPs, Bone Morphogenetic Proteins; VEGF, Vascular Endothelial Growth Factor; WBC, White Blood Cell; ACP, Autologous Conditioned Plasma; CHA, Carbonated Hydroxyapatite; PCL, Poly-ε-Caprolactone; HUVEC, Human Umbilical Vein Endothelial Cell.
Disclosure
ADM disclosures include research support and consulting with Arthrex Inc., Naples, FL, as well as consulting and stock interests in Restor3d. All other authors report no conflicts of interest in this work.
References
- 1.Wu A-M, Bisignano C, James S, et al. Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Long. 2021;2(9):e580–e592. doi: 10.1016/S2666-7568(21)00172-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Calori GM, Mazza E, Colombo M, Ripamonti C, Tagliabue L. Treatment of long bone non-unions with polytherapy: indications and clinical results. Injury. 2011;42(6):587–590. doi: 10.1016/j.injury.2011.03.046 [DOI] [PubMed] [Google Scholar]
- 3.Cunningham BP, Brazina S, Morshed S, Miclau T. Fracture healing: a review of clinical, imaging and laboratory diagnostic options. Injury. 2017;48(Suppl 1):S69–s75. doi: 10.1016/j.injury.2017.04.020 [DOI] [PubMed] [Google Scholar]
- 4.Bell A, Templeman D, Weinlein JC. Nonunion of the Femur and Tibia: an Update. Orthop Clin North Am. 2016;47(2):365–375. doi: 10.1016/j.ocl.2015.09.010 [DOI] [PubMed] [Google Scholar]
- 5.Antonova E, Le TK, Burge R, Mershon J. Tibia shaft fractures: costly burden of nonunions. BMC Musculoskelet Disord. 2013;14:42. doi: 10.1186/1471-2474-14-42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cruess RL, Dumont J. Fracture healing. Can J Surg. 1975;18(5):403–413. [PubMed] [Google Scholar]
- 7.Cole BJ, Seroyer ST, Filardo G, Bajaj S, Fortier LA. Platelet-rich plasma: where are we now and where are we going? Sports Health. 2010;2(3):203–210. doi: 10.1177/1941738110366385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Everts P, Onishi K, Jayaram P, Lana JF, Mautner K. Platelet-Rich Plasma: new Performance Understandings and Therapeutic Considerations in 2020. Int J Mol Sci. 2020;21(20). doi: 10.3390/ijms21207794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Collins T, Alexander D, Barkatali B. Platelet-rich plasma: a narrative review. EFORT Open Rev. 2021;6(4):225–235. doi: 10.1302/2058-5241.6.200017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang N, Wu Y-P, Qian S-J, Teng C, Chen S, Li H. Research Progress in the Mechanism of Effect of PRP in Bone Deficiency Healing. Sci World J. 2013;2013:134582. doi: 10.1155/2013/134582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Chen J, Zhong ZM, Yang D, Zhu Q. Is platelet-derived growth factor-BB expression proportional to fibrosis in the hypertrophied lumber ligamentum flavum? Spine. 2010;35(25):E1479–86. doi: 10.1097/BRS.0b013e3181f3d2df [DOI] [PubMed] [Google Scholar]
- 12.Panseri S, Russo A, Cunha C, et al. Osteochondral tissue engineering approaches for articular cartilage and subchondral bone regeneration. Knee Surg Sports Traumatol Arthrosc. 2012;20(6):1182–1191. doi: 10.1007/s00167-011-1655-1 [DOI] [PubMed] [Google Scholar]
- 13.Cachaço AS, Carvalho T, Santos AC, et al. TNF-alpha regulates the effects of irradiation in the mouse bone marrow microenvironment. PLoS One. 2010;5(2):e8980. doi: 10.1371/journal.pone.0008980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jamal MS, Hurley ET, Asad H, Asad A, Taneja T. The role of Platelet Rich Plasma and other orthobiologics in bone healing and fracture management: a systematic review. J Clin Orthop Trauma. 2022;25:101759. doi: 10.1016/j.jcot.2021.101759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Glass GE, Chan JK, Freidin A, Feldmann M, Horwood NJ, Nanchahal J. TNF-alpha promotes fracture repair by augmenting the recruitment and differentiation of muscle-derived stromal cells. Proc Natl Acad Sci U S A. 2011;108(4):1585–1590. doi: 10.1073/pnas.1018501108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.David JP, Schett G. TNF and bone. Curr Dir Autoimmun. 2010;11:135–144. doi: 10.1159/000289202 [DOI] [PubMed] [Google Scholar]
- 17.Lyras DN, Kazakos K, Verettas D, et al. The effect of platelet-rich plasma gel in the early phase of patellar tendon healing. Arch Orthop Trauma Surg. 2009;129(11):1577–1582. doi: 10.1007/s00402-009-0935-4 [DOI] [PubMed] [Google Scholar]
- 18.Lyras DN, Kazakos K, Verettas D, et al. The influence of platelet-rich plasma on angiogenesis during the early phase of tendon healing. Foot Ankle Int. 2009;30(11):1101–1106. doi: 10.3113/fai.2009.1101 [DOI] [PubMed] [Google Scholar]
- 19.Lange J, Sapozhnikova A, Lu C, et al. Action of IL-1beta during fracture healing. J Orthop Res. 2010;28(6):778–784. doi: 10.1002/jor.21061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee Y-M, Fujikado N, Manaka H, Yasuda H, Iwakura Y. IL-1 plays an important role in the bone metabolism under physiological conditions. Int Immunol. 2010;22(10):805–816. doi: 10.1093/intimm/dxq431 [DOI] [PubMed] [Google Scholar]
- 21.Lange J, Sapozhnikova A, Lu C, et al. Action of IL-1 beta during Fracture Healing. J Orthop Res. 2009;28:778–784. doi: 10.1002/jor.21061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spindler KP, Murray MM, Carey JL, Zurakowski D, Fleming BC. The use of platelets to affect functional healing of an anterior cruciate ligament (ACL) autograft in a caprine ACL reconstruction model. J Orthop Res. 2009;27(5):631–638. doi: 10.1002/jor.20785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray MM, Spindler KP, Abreu E, et al. Collagen-platelet rich plasma hydrogel enhances primary repair of the porcine anterior cruciate ligament. J Orthop Res. 2007;25(1):81–91. doi: 10.1002/jor.20282 [DOI] [PubMed] [Google Scholar]
- 24.Coates BA, McKenzie JA, Yoneda S, Silva MJ. Interleukin-6 (IL-6) deficiency enhances intramembranous osteogenesis following stress fracture in mice. Bone. 2021;143:115737. doi: 10.1016/j.bone.2020.115737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmisano B, Riminucci M, Karsenty G. Interleukin-6 signaling in osteoblasts regulates bone remodeling during exercise. Bone. 2023;176:116870. doi: 10.1016/j.bone.2023.116870 [DOI] [PubMed] [Google Scholar]
- 26.Alves R, Grimalt R. A Review of Platelet-Rich Plasma: history, Biology, Mechanism of Action, and Classification. Skin Appendage Disord. 2018;4(1):18–24. doi: 10.1159/000477353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taschieri S, Lolato A, Ofer M, Testori T, Francetti L, Del Fabbro M. Immediate post-extraction implants with or without pure platelet-rich plasma: a 5-year follow-up study. Oral Maxillofac Surg. 2017;21(2):147–157. doi: 10.1007/s10006-017-0609-2 [DOI] [PubMed] [Google Scholar]
- 28.Georgakopoulos I, Tsantis S, Georgakopoulos P, et al. The impact of Platelet Rich Plasma (PRP) in osseointegration of oral implants in dental panoramic radiography: texture based evaluation. Clin Cases Miner Bone Metab. 2014;11(1):59–66. [PMC free article] [PubMed] [Google Scholar]
- 29.Marx RE. Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 2004;62(4):489–496. doi: 10.1016/j.joms.2003.12.003 [DOI] [PubMed] [Google Scholar]
- 30.Kao HK, Chen B, Murphy GF, Li Q, Orgill DP, Guo L. Peripheral blood fibrocytes: enhancement of wound healing by cell proliferation, re-epithelialization, contraction, and angiogenesis. Ann Surg. 2011;254(6):1066–1074. doi: 10.1097/SLA.0b013e3182251559 [DOI] [PubMed] [Google Scholar]
- 31.Casati L, Celotti F, Negri-Cesi P, Sacchi MC, Castano P, Colciago A. Platelet derived growth factor (PDGF) contained in Platelet Rich Plasma (PRP) stimulates migration of osteoblasts by reorganizing actin cytoskeleton. Cell Adh Migr. 2014;8(6):595–602. doi: 10.4161/19336918.2014.972785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kinoshita H, Orita S, Inage K, et al. Freeze-Dried Platelet-Rich Plasma Induces Osteoblast Proliferation via Platelet-Derived Growth Factor Receptor-Mediated Signal Transduction. Asian Spine J. 2020;14(1):1–8. doi: 10.31616/asj.2019.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ng F, Boucher S, Koh S, et al. PDGF, TGF-beta, and FGF signaling is important for differentiation and growth of mesenchymal stem cells (MSCs): transcriptional profiling can identify markers and signaling pathways important in differentiation of MSCs into adipogenic, chondrogenic, and osteogenic lineages. Blood. 2008;112(2):295–307. doi: 10.1182/blood-2007-07-103697 [DOI] [PubMed] [Google Scholar]
- 34.Kreja L, Brenner RE, Tautzenberger A, et al. Non-resorbing osteoclasts induce migration and osteogenic differentiation of mesenchymal stem cells. J Cell Biochem. 2010;109(2):347–355. doi: 10.1002/jcb.22406 [DOI] [PubMed] [Google Scholar]
- 35.Dumic-Cule I, Peric M, Kucko L, Grgurevic L, Pecina M, Vukicevic S. Bone morphogenetic proteins in fracture repair. Int Orthop. 2018;42(11):2619–2626. doi: 10.1007/s00264-018-4153-y [DOI] [PubMed] [Google Scholar]
- 36.Lademann F, Hofbauer LC, Rauner M. The Bone Morphogenetic Protein Pathway: the Osteoclastic Perspective. Front Cell Dev Biol. 2020;8:586031. doi: 10.3389/fcell.2020.586031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wrana JL, Maeno M, Hawrylyshyn B, Yao KL, Domenicucci C, Sodek J. Differential effects of transforming growth factor-beta on the synthesis of extracellular matrix proteins by normal fetal rat calvarial bone cell populations. J Cell Biol. 1988;106(3):915–924. doi: 10.1083/jcb.106.3.915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bonewald LF, Mundy GR. Role of transforming growth factor-beta in bone remodeling. Clin Orthop Relat Res. 1990. [PubMed] [Google Scholar]
- 39.Jain NK, Gulati M. Platelet-rich plasma: a healing virtuoso. Blood Res. 2016;51(1):3–5. doi: 10.5045/br.2016.51.1.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Beck LS, DeGuzman L, Lee WP, Xu Y, Siegel MW, Amento EP. One systemic administration of transforming growth factor-beta 1 reverses age- or glucocorticoid-impaired wound healing. J Clin Invest. 1993;92(6):2841–2849. doi: 10.1172/jci116904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wrotniak M, Bielecki T, Gaździk TS. Current opinion about using the platelet-rich gel in orthopaedics and trauma surgery. Ortop Traumatol Rehabil. 2007;9(3):227–238. [PubMed] [Google Scholar]
- 42.Mohan S, Baylink DJ. IGF-binding proteins are multifunctional and act via IGF-dependent and -independent mechanisms. J Endocrinol. 2002;175(1):19–31. doi: 10.1677/joe.0.1750019 [DOI] [PubMed] [Google Scholar]
- 43.Joseph BK, Savage NW, Daley TJ, Young WG. In situ hybridization evidence for a paracrine/autocrine role for insulin-like growth factor-I in tooth development. Growth Factors. 1996;13(1–2):11–17. doi: 10.3109/08977199609034563 [DOI] [PubMed] [Google Scholar]
- 44.Noh KC, Park SH, Yang CJ, Lee GW, Kim MK, Kang YH. Involvement of synovial matrix degradation and angiogenesis in oxidative stress-exposed degenerative rotator cuff tears with osteoarthritis. J Shoulder Elbow Surg. 2018;27(1):141–150. doi: 10.1016/j.jse.2017.08.007 [DOI] [PubMed] [Google Scholar]
- 45.van der Bijl I, Vlig M, Middelkoop E, de Korte D. Allogeneic platelet-rich plasma (PRP) is superior to platelets or plasma alone in stimulating fibroblast proliferation and migration, angiogenesis, and chemotaxis as relevant processes for wound healing. Transfusion. 2019;59(11):3492–3500. doi: 10.1111/trf.15535 [DOI] [PubMed] [Google Scholar]
- 46.Zhang L, Qiu H, Wang D, et al. Enhanced vascularization and biocompatibility of rat pancreatic decellularized scaffolds loaded with platelet-rich plasma. J Biomater Appl. 2020;35(3):313–330. doi: 10.1177/0885328220933890 [DOI] [PubMed] [Google Scholar]
- 47.Shibuya M. Vascular Endothelial Growth Factor (VEGF) and Its Receptor (VEGFR) Signaling in Angiogenesis: a Crucial Target for Anti- and Pro-Angiogenic Therapies. Genes Cancer. 2011;2(12):1097–1105. doi: 10.1177/1947601911423031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Behr B, Tang C, Germann G, Longaker MT, Quarto N. Locally applied vascular endothelial growth factor A increases the osteogenic healing capacity of human adipose-derived stem cells by promoting osteogenic and endothelial differentiation. Stem Cells. 2011;29(2):286–296. doi: 10.1002/stem.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hu K, Olsen BR. The roles of vascular endothelial growth factor in bone repair and regeneration. Bone. 2016;91:30–38. doi: 10.1016/j.bone.2016.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Yang Y-Q, Tan -Y-Y, Wong R, Wenden A, Zhang L-K, Rabie ABM. The role of vascular endothelial growth factor in ossification. Int J Oral Sci. 2012;4(2):64–68. doi: 10.1038/ijos.2012.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kim ES, Kim JJ, Park EJ. Angiogenic factor-enriched platelet-rich plasma enhances in vivo bone formation around alloplastic graft material. J Adv Prosthodont. 2010;2(1):7–13. doi: 10.4047/jap.2010.2.1.7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ball SG, Shuttleworth CA, Kielty CM. Mesenchymal stem cells and neovascularization: role of platelet-derived growth factor receptors. J Cell Mol Med. 2007;11(5):1012–1030. doi: 10.1111/j.1582-4934.2007.00120.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Massberg S, Konrad I, Schürzinger K, et al. Platelets secrete stromal cell-derived factor 1alpha and recruit bone marrow-derived progenitor cells to arterial thrombi in vivo. J Exp Med. 2006;203(5):1221–1233. doi: 10.1084/jem.20051772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chesney CM, Pifer DD, Byers LW, Muirhead EE. Effect of platelet-activating factor (PAF) on human platelets. Blood. 1982;59(3):582–585. [PubMed] [Google Scholar]
- 55.Mehta SK, Tucci MA, Benghuzzi HA. Effect of platelet dense granule contents upon osteoblast viability. Biomed Sci Instrum. 2012;48:288–295. [PubMed] [Google Scholar]
- 56.McManus LM, Pinckard RN. PAF, a putative mediator of oral inflammation. Crit Rev Oral Biol Med. 2000;11(2):240–258. doi: 10.1177/10454411000110020701 [DOI] [PubMed] [Google Scholar]
- 57.Mishra A, Woodall J, Vieira A. Treatment of tendon and muscle using platelet-rich plasma. Clin Sports Med. 2009;28(1):113–125. doi: 10.1016/j.csm.2008.08.007 [DOI] [PubMed] [Google Scholar]
- 58.Golebiewska EM, Poole AW. Platelet secretion: from haemostasis to wound healing and beyond. Blood Rev. 2015;29(3):153–162. doi: 10.1016/j.blre.2014.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hashikawa T, Takedachi M, Terakura M, et al. Involvement of CD73 (ecto-5’-nucleotidase) in adenosine generation by human gingival fibroblasts. J Dent Res. 2003;82(11):888–892. doi: 10.1177/154405910308201108 [DOI] [PubMed] [Google Scholar]
- 60.Marx RE. Platelet-rich plasma (PRP): what is PRP and what is not PRP? Implant Dent. 2001;10(4):225–228. doi: 10.1097/00008505-200110000-00002 [DOI] [PubMed] [Google Scholar]
- 61.Graziani F, Ivanovski S, Cei S, Ducci F, Tonetti M, Gabriele M. The in vitro effect of different PRP concentrations on osteoblasts and fibroblasts. Clin Oral Implants Res. 2006;17(2):212–219. doi: 10.1111/j.1600-0501.2005.01203.x [DOI] [PubMed] [Google Scholar]
- 62.Mazzucco L, Balbo V, Cattana E, Guaschino R, Borzini P. Not every PRP-gel is born equal Evaluation of growth factor availability for tissues through four PRP-gel preparations: fibrinet®, RegenPRP-Kit®, Plateltex® and one manual procedure. Vox Sanguinis. 2009;97(2):110–118. doi: 10.1111/j.1423-0410.2009.01188.x [DOI] [PubMed] [Google Scholar]
- 63.López S, Vilar JM, Sopena JJ, et al. Assessment of the Efficacy of Platelet-Rich Plasma in the Treatment of Traumatic Canine Fractures. Int J Mol Sci. 2019;20(5). doi: 10.3390/ijms20051075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jovani-Sancho M, Sheth CC, Marqués-Mateo M, Puche-Torres M. Platelet-Rich Plasma: a Study of the Variables that May Influence Its Effect on Bone Regeneration. Clin Implant Dentistry Relat Res. 2016;18(5):1051–1064. doi: 10.1111/cid.12361 [DOI] [PubMed] [Google Scholar]
- 65.Al-Hamed FS, Abu-Nada L, Rodan R, et al. Differences in platelet-rich plasma composition influence bone healing. J Clin Periodontol. 2021;48(12):1613–1623. doi: 10.1111/jcpe.13546 [DOI] [PubMed] [Google Scholar]
- 66.Kawasumi M, Kitoh H, Siwicka KA, Ishiguro N. The effect of the platelet concentration in platelet-rich plasma gel on the regeneration of bone. J Bone Joint Surg Br. 2008;90(7):966–972. doi: 10.1302/0301-620x.90b7.20235 [DOI] [PubMed] [Google Scholar]
- 67.Chen L, Yang X, Huang G, et al. Platelet-rich plasma promotes healing of osteoporotic fractures. Orthopedics. 2013;36(6):e687–94. doi: 10.3928/01477447-20130523-10 [DOI] [PubMed] [Google Scholar]
- 68.Choi BH, Zhu SJ, Kim BY, Huh JY, Lee SH, Jung JH. Effect of platelet-rich plasma (PRP) concentration on the viability and proliferation of alveolar bone cells: an in vitro study. Int J Oral Maxillofac Surg. 2005;34(4):420–424. doi: 10.1016/j.ijom.2004.10.018 [DOI] [PubMed] [Google Scholar]
- 69.DeLong JM, Russell RP, Mazzocca AD. Platelet-rich plasma: the PAW classification system. Arthroscopy. 2012;28(7):998–1009. doi: 10.1016/j.arthro.2012.04.148 [DOI] [PubMed] [Google Scholar]
- 70.Yamaguchi R, Terashima H, Yoneyama S, Tadano S, Ohkohchi N. Effects of platelet-rich plasma on intestinal anastomotic healing in rats: PRP concentration is a key factor. J Surg Res. 2012;173(2):258–266. doi: 10.1016/j.jss.2010.10.001 [DOI] [PubMed] [Google Scholar]
- 71.Laver L, Marom N, Dnyanesh L, Mei-Dan O, Espregueira-Mendes J, Gobbi A. PRP for Degenerative Cartilage Disease: a Systematic Review of Clinical Studies. Cartilage. 2017;8(4):341–364. doi: 10.1177/1947603516670709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fernández-Medina T, Vaquette C, Ivanovski S. Systematic Comparison of the Effect of Four Clinical-Grade Platelet Rich Hemoderivatives on Osteoblast Behaviour. Int J Mol Sci. 2019;20(24). doi: 10.3390/ijms20246243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fadadu PP, Mazzola AJ, Hunter CW, Davis TT. Review of concentration yields in commercially available platelet-rich plasma (PRP) systems: a call for PRP standardization. Reg Anesth Pain Med. 2019. doi: 10.1136/rapm-2018-100356 [DOI] [PubMed] [Google Scholar]
- 74.Mariani E, Canella V, Cattini L, et al. Leukocyte-Rich Platelet-Rich Plasma Injections Do Not Up-Modulate Intra-Articular Pro-Inflammatory Cytokines in the Osteoarthritic Knee. PLoS One. 2016;11(6):e0156137. doi: 10.1371/journal.pone.0156137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Anitua E. Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants. 1999;14(4):529–535. [PubMed] [Google Scholar]
- 76.Kobayashi Y, Saita Y, Nishio H, et al. Leukocyte concentration and composition in platelet-rich plasma (PRP) influences the growth factor and protease concentrations. J Orthop Sci. 2016;21(5):683–689. doi: 10.1016/j.jos.2016.07.009 [DOI] [PubMed] [Google Scholar]
- 77.Zimmermann R, Jakubietz R, Jakubietz M, et al. Different preparation methods to obtain platelet components as a source of growth factors for local application. Transfusion. 2001;41(10):1217–1224. doi: 10.1046/j.1537-2995.2001.41101217.x [DOI] [PubMed] [Google Scholar]
- 78.Xu Z, Yin W, Zhang Y, et al. Comparative evaluation of leukocyte- and platelet-rich plasma and pure platelet-rich plasma for cartilage regeneration. Sci Rep. 2017;7:43301. doi: 10.1038/srep43301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yin WJ, Xu HT, Sheng JG, et al. Advantages of Pure Platelet-Rich Plasma Compared with Leukocyte- and Platelet-Rich Plasma in Treating Rabbit Knee Osteoarthritis. Med Sci Monit. 2016;22:1280–1290. doi: 10.12659/msm.898218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Yin W, Qi X, Zhang Y, et al. Advantages of pure platelet-rich plasma compared with leukocyte- and platelet-rich plasma in promoting repair of bone defects. J Transl Med. 2016;14(1):73. doi: 10.1186/s12967-016-0825-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Riboh JC, Saltzman BM, Yanke AB, Fortier L, Cole BJ. Effect of Leukocyte Concentration on the Efficacy of Platelet-Rich Plasma in the Treatment of Knee Osteoarthritis. Am J Sports Med. 2016;44(3):792–800. doi: 10.1177/0363546515580787 [DOI] [PubMed] [Google Scholar]
- 82.Filardo G, Kon E, Pereira Ruiz MT, et al. Platelet-rich plasma intra-articular injections for cartilage degeneration and osteoarthritis: single- versus double-spinning approach. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2082–2091. doi: 10.1007/s00167-011-1837-x [DOI] [PubMed] [Google Scholar]
- 83.Oudelaar BW, Peerbooms JC, Huis In ‘t Veld R, Vochteloo AJH. Concentrations of Blood Components in Commercial Platelet-Rich Plasma Separation Systems: a Review of the Literature. Am J Sports Med. 2019;47(2):479–487. doi: 10.1177/0363546517746112 [DOI] [PubMed] [Google Scholar]
- 84.Braun HJ, Kim HJ, Chu CR, Dragoo JL. The effect of platelet-rich plasma formulations and blood products on human synoviocytes: implications for intra-articular injury and therapy. Am J Sports Med. 2014;42(5):1204–1210. doi: 10.1177/0363546514525593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fitzpatrick J, Bulsara M, Zheng MH. The Effectiveness of Platelet-Rich Plasma in the Treatment of Tendinopathy: a Meta-analysis of Randomized Controlled Clinical Trials. Am J Sports Med. 2017;45(1):226–233. doi: 10.1177/0363546516643716 [DOI] [PubMed] [Google Scholar]
- 86.Foster TE, Puskas BL, Mandelbaum BR, Gerhardt MB, Rodeo SA. Platelet-rich plasma: from basic science to clinical applications. Am J Sports Med. 2009;37(11):2259–2272. doi: 10.1177/0363546509349921 [DOI] [PubMed] [Google Scholar]
- 87.Mazzocca AD, McCarthy MB, Chowaniec DM, et al. Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am. 2012;94(4):308–316. doi: 10.2106/jbjs.K.00430 [DOI] [PubMed] [Google Scholar]
- 88.Oh JH, Kim W, Park KU, Roh YH. Comparison of the Cellular Composition and Cytokine-Release Kinetics of Various Platelet-Rich Plasma Preparations. Am J Sports Med. 2015;43(12):3062–3070. doi: 10.1177/0363546515608481 [DOI] [PubMed] [Google Scholar]
- 89.Dejnek M, Witkowski J, Moreira H, et al. Content of blood cell components, inflammatory cytokines and growth factors in autologous platelet-rich plasma obtained by various methods. World J Orthop. 2022;13(6):587–602. doi: 10.5312/wjo.v13.i6.587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Magalon J, Brandin T, Francois P, et al. Technical and biological review of authorized medical devices for platelets-rich plasma preparation in the field of regenerative medicine. Platelets. 2021;32(2):200–208. doi: 10.1080/09537104.2020.1832653 [DOI] [PubMed] [Google Scholar]
- 91.Straum OK. The optimal platelet concentration in platelet-rich plasma for proliferation of human cells in vitro-diversity, biases, and possible basic experimental principles for further research in the field: a review. PeerJ. 2020;8:e10303. doi: 10.7717/peerj.10303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wasterlain A, Braun H, Dragoo J. Contents and Formulations of Platelet-Rich Plasma. Operat Tech Orthop. 2012;22:33–42. doi: 10.1053/j.oto.2011.11.001 [DOI] [Google Scholar]
- 93.Cavallo C, Roffi A, Grigolo B, et al. Platelet-Rich Plasma: the Choice of Activation Method Affects the Release of Bioactive Molecules. Biomed Res Int. 2016;2016:6591717. doi: 10.1155/2016/6591717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Smith OJ, Talaat S, Tomouk T, Jell G, Mosahebi A. An Evaluation of the Effect of Activation Methods on the Release of Growth Factors from Platelet-Rich Plasma. Plast Reconstr Surg. 2022;149(2):404–411. doi: 10.1097/prs.0000000000008772 [DOI] [PubMed] [Google Scholar]
- 95.Harrison S, Vavken P, Kevy S, Jacobson M, Zurakowski D, Murray MM. Platelet activation by collagen provides sustained release of anabolic cytokines. Am J Sports Med. 2011;39(4):729–734. doi: 10.1177/0363546511401576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Bir SC, Esaki J, Marui A, et al. Angiogenic properties of sustained release platelet-rich plasma: characterization in-vitro and in the ischemic hind limb of the mouse. J Vasc Surg. 2009;50(4):870–879.e2. doi: 10.1016/j.jvs.2009.06.016 [DOI] [PubMed] [Google Scholar]
- 97.Zhuang YW, Zeng YM, Chen YF, et al. 不同激活剂对人富血小板血浆释放曲线的影响 [The effects of different activators on the release curve of human platelet-rich plasma]. Zhonghua Jie He He Hu Xi Za Zhi. 2018;41(11):868–872. doi: 10.3760/cma.j.issn.1001-0939.2018.11.008. Chinese. [DOI] [PubMed] [Google Scholar]
- 98.Toyoda T, Isobe K, Tsujino T, et al. Direct activation of platelets by addition of CaCl2 leads coagulation of platelet-rich plasma. Int J Implant Dentist. 2018;4(1):23. doi: 10.1186/s40729-018-0134-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Simental-Mendía M, Ortega-Mata D, Tamez-Mata Y, Olivo CAA, Vilchez-Cavazos F. Comparison of the clinical effectiveness of activated and non-activated platelet-rich plasma in the treatment of knee osteoarthritis: a systematic review and meta-analysis. Clin Rheumatol. 2023;42(5):1397–1408. doi: 10.1007/s10067-022-06463-x [DOI] [PubMed] [Google Scholar]
- 100.Sheen JR, Mabrouk A, Garla VV. Fracture Healing Overview. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.; 2023. [PubMed] [Google Scholar]
- 101.Ghiasi MS, Chen J, Vaziri A, Rodriguez EK, Nazarian A. Bone fracture healing in mechanobiological modeling: a review of principles and methods. Bone Reports. 2017;6:87–100. doi: 10.1016/j.bonr.2017.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Marsell R, Einhorn TA. The biology of fracture healing. Injury. 2011;42(6):551–555. doi: 10.1016/j.injury.2011.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Kumar V, Madsen T, Zhu H, Semple E. Stability of human thrombin produced from 11 mL of plasma using the thrombin processing device. J Extra Corpor Technol. 2005;37(4):390–395. [PMC free article] [PubMed] [Google Scholar]
- 104.Fufa D, Shealy B, Jacobson M, Kevy S, Murray MM. Activation of platelet-rich plasma using soluble type I collagen. J Oral Maxillofac Surg. 2008;66(4):684–690. doi: 10.1016/j.joms.2007.06.635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Mikel S, Maider B, Orlando P, et al. Isolation, Activation, and Mechanism of Action of Platelet-Rich Plasma and Its Applications for Joint Repair. In: Mahmood SC, editor. Regenerative Medicine. IntechOpen; 2019:Ch.3. [Google Scholar]
- 106.Kikuchi N, Yoshioka T, Taniguchi Y, et al. Optimization of leukocyte-poor platelet-rich plasma preparation: a validation study of leukocyte-poor platelet-rich plasma obtained using different preparer, storage, and activation methods. J Exper Orthop. 2019;6(1):24. doi: 10.1186/s40634-019-0190-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Ali M, Mohamed A, Ahmed HE, Malviya A, Atchia I. The use of ultrasound-guided platelet-rich plasma injections in the treatment of Hip osteoarthritis: a systematic review of the literature. J Ultrason. 2018;18(75):332–337. doi: 10.15557/JoU.2018.0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Lam KHS, Hung CY, Hung A. Ultrasound-Assisted Intraosseous Injection of Platelet-Rich Plasma for a Patient With Tibial Plateau Subchondral Bone Marrow Lesion: a Case Presentation and Technical Illustration. Cureus. 2020;12(12):e12312. doi: 10.7759/cureus.12312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sağlam G, Çetinkaya Alişar D. Ultrasound-guided versus palpation-guided platelet-rich plasma injection for the treatment of chronic lateral epicondylitis: a prospective, randomized study. Arch Rheumatol. 2023;38(1):67–74. doi: 10.46497/ArchRheumatol.2023.9196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Carter MJ, Fylling CP, Parnell LK. Use of platelet rich plasma gel on wound healing: a systematic review and meta-analysis. Eplasty. 2011;11:e38. [PMC free article] [PubMed] [Google Scholar]
- 111.Abdullah BJ, Atasoy N, Omer AK. Evaluate the effects of platelet rich plasma (PRP) and zinc oxide ointment on skin wound healing. Ann Med Surg. 2019;37:30–37. doi: 10.1016/j.amsu.2018.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bolton L. Platelet-Rich Plasma: optimal Use in Surgical Wounds. Wounds. 2021;33(8):219–221. [PubMed] [Google Scholar]
- 113.Galanis V, Fiska A, Kapetanakis S, Kazakos K, Demetriou T. Effect of platelet-rich plasma combined with demineralised bone matrix on bone healing in rabbit ulnar defects. Singapore Med J. 2017;58(9):551–556. doi: 10.11622/smedj.2016095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jensen TB, Rahbek O, Overgaard S, Søballe K. Platelet rich plasma and fresh frozen bone allograft as enhancement of implant fixation. An experimental study in dogs. J Orthop Res. 2004;22(3):653–658. doi: 10.1016/j.orthres.2003.10.006 [DOI] [PubMed] [Google Scholar]
- 115.Consolo U, Bertoldi C, Zaffe D. Intermittent loading improves results in mandibular alveolar distraction osteogenesis. Clin Oral Implants Res. 2006;17(2):179–187. doi: 10.1111/j.1600-0501.2005.01213.x [DOI] [PubMed] [Google Scholar]
- 116.Badr M, Coulthard P, Alissa R, Oliver R. The efficacy of platelet-rich plasma in grafted maxillae. A randomised clinical trial. Eur J Oral Implantol. 2010;3(3):233–244. [PubMed] [Google Scholar]
- 117.Sittinger M, Hutmacher DW, Risbud MV. Current strategies for cell delivery in cartilage and bone regeneration. Curr Opin Biotechnol. 2004;15(5):411–418. doi: 10.1016/j.copbio.2004.08.010 [DOI] [PubMed] [Google Scholar]
- 118.Shakoor S, Kibble E, El-Jawhari JJ. Bioengineering Approaches for Delivering Growth Factors: a Focus on Bone and Cartilage Regeneration. Bioengineering. 2022;9(5):223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Rodriguez IA, Growney Kalaf EA, Bowlin GL, Sell SA. Platelet-rich plasma in bone regeneration: engineering the delivery for improved clinical efficacy. Biomed Res Int. 2014;2014:392398. doi: 10.1155/2014/392398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lin SS, Landesberg R, Chin HS, Lin J, Eisig SB, Lu HH. Controlled release of PRP-derived growth factors promotes osteogenic differentiation of human mesenchymal stem cells. Conf Proc IEEE Eng Med Biol Soc. 2006;2006:4358–4361. doi: 10.1109/iembs.2006.260847 [DOI] [PubMed] [Google Scholar]
- 121.Lu HH, Vo JM, Chin HS, et al. Controlled delivery of platelet-rich plasma-derived growth factors for bone formation. J Biomed Mater Res A. 2008;86(4):1128–1136. doi: 10.1002/jbm.a.31740 [DOI] [PubMed] [Google Scholar]
- 122.Neffe AT, Loebus A, Zaupa A, Stoetzel C, Müller FA, Lendlein A. Gelatin functionalization with tyrosine derived moieties to increase the interaction with hydroxyapatite fillers. Acta Biomater. 2011;7(4):1693–1701. doi: 10.1016/j.actbio.2010.11.025 [DOI] [PubMed] [Google Scholar]
- 123.Hokugo A, Ozeki M, Kawakami O, et al. Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. Tissue Eng. 2005;11(7–8):1224–1233. doi: 10.1089/ten.2005.11.1224 [DOI] [PubMed] [Google Scholar]
- 124.Hokugo A, Sawada Y, Hokugo R, et al. Controlled release of platelet growth factors enhances bone regeneration at rabbit calvaria. Oral Surg, Oral Med Oral Pathol Oral Radiol Endod. 2007;104(1):44–48. doi: 10.1016/j.tripleo.2006.11.032 [DOI] [PubMed] [Google Scholar]
- 125.Kaur P, Maria A. Efficacy of platelet rich plasma and hydroxyapatite crystals in bone regeneration after surgical removal of mandibular third molars. J Maxillofac Oral Surg. 2013;12(1):51–59. doi: 10.1007/s12663-012-0382-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Liu X, Wang P, Chen W, Weir MD, Bao C, Xu HH. Human embryonic stem cells and macroporous calcium phosphate construct for bone regeneration in cranial defects in rats. Acta Biomater. 2014;10(10):4484–4493. doi: 10.1016/j.actbio.2014.06.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Qiu G, Shi Z, Hhk X, et al. Bone regeneration in minipigs via calcium phosphate cement scaffold delivering autologous bone marrow mesenchymal stem cells and platelet-rich plasma. J Tissue Eng Regen Med. 2018;12(2):e937–e948. doi: 10.1002/term.2416 [DOI] [PubMed] [Google Scholar]
- 128.Solovieva A, Miroshnichenko S, Kovalskii A, et al. Immobilization of Platelet-Rich Plasma onto COOH Plasma-Coated PCL Nanofibers Boost Viability and Proliferation of Human Mesenchymal Stem Cells. Polymers. 2017;9(12). doi: 10.3390/polym9120736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kanno T, Takahashi T, Tsujisawa T, Ariyoshi W, Nishihara T. Platelet-rich plasma enhances human osteoblast-like cell proliferation and differentiation. J Oral Maxillofac Surg. 2005;63(3):362–369. doi: 10.1016/j.joms.2004.07.016 [DOI] [PubMed] [Google Scholar]
- 130.Vahabi S, Yadegari Z, Mohammad-Rahimi H. Comparison of the effect of activated or non-activated PRP in various concentrations on osteoblast and fibroblast cell line proliferation. Cell Tissue Bank. 2017;18(3):347–353. doi: 10.1007/s10561-017-9640-7 [DOI] [PubMed] [Google Scholar]
- 131.Slapnicka J, Fassmann A, Strasak L, Augustin P, Vanek J. Effects of activated and nonactivated platelet-rich plasma on proliferation of human osteoblasts in vitro. J Oral Maxillofac Surg. 2008;66(2):297–301. doi: 10.1016/j.joms.2007.05.022 [DOI] [PubMed] [Google Scholar]
- 132.Martinotti S, Mazzucco L, Balbo V, et al. Platelet-rich plasma induces mixed osteogenic/osteoclastogenic phenotype in osteosarcoma SaOS-2 cells: role of TGF-beta. Curr Pharm Biotechnol. 2014;15(2):120–126. doi: 10.2174/1389201015666140604121407 [DOI] [PubMed] [Google Scholar]
- 133.Gassling VL, Açil Y, Springer IN, Hubert N, Wiltfang J. Platelet-rich plasma and platelet-rich fibrin in human cell culture. Oral Surg, Oral Med Oral Pathol Oral Radiol Endod. 2009;108(1):48–55. doi: 10.1016/j.tripleo.2009.02.007 [DOI] [PubMed] [Google Scholar]
- 134.Herrera BS, Coimbra LS, Bastos AS, et al. Platelet-rich plasma stimulates cytokine expression and alkaline phosphatase activity in osteoblast-derived osteosarcoma cells. Arch Oral Biol. 2012;57(9):1282–1289. doi: 10.1016/j.archoralbio.2012.03.004 [DOI] [PubMed] [Google Scholar]
- 135.He L, Lin Y, Hu X, Zhang Y, Wu H. A comparative study of platelet-rich fibrin (PRF) and platelet-rich plasma (PRP) on the effect of proliferation and differentiation of rat osteoblasts in vitro. Oral Surg, Oral Med Oral Pathol Oral Radiol Endod. 2009;108(5):707–713. doi: 10.1016/j.tripleo.2009.06.044 [DOI] [PubMed] [Google Scholar]
- 136.Mazzocca AD, McCarthy MB, Chowaniec DM, et al. The positive effects of different platelet-rich plasma methods on human muscle, bone, and tendon cells. Am J Sports Med. 2012;40(8):1742–1749. doi: 10.1177/0363546512452713 [DOI] [PubMed] [Google Scholar]
- 137.Mooren RE, Hendriks EJ, van den Beucken JJ, et al. The effect of platelet-rich plasma in vitro on primary cells: rat osteoblast-like cells and human endothelial cells. Tissue Eng Part A. 2010;16(10):3159–3172. doi: 10.1089/ten.tea.2009.0832 [DOI] [PubMed] [Google Scholar]
- 138.García-Martínez O, Reyes-Botella C, Díaz-Rodríguez L, et al. Effect of platelet-rich plasma on growth and antigenic profile of human osteoblasts and its clinical impact. J Oral Maxillofac Surg. 2012;70(7):1558–1564. doi: 10.1016/j.joms.2011.06.199 [DOI] [PubMed] [Google Scholar]
- 139.Bi L, Cheng W, Fan H, Pei G. Reconstruction of goat tibial defects using an injectable tricalcium phosphate/chitosan in combination with autologous platelet-rich plasma. Biomaterials. 2010;31(12):3201–3211. doi: 10.1016/j.biomaterials.2010.01.038 [DOI] [PubMed] [Google Scholar]
- 140.Zou J, Yuan C, Wu C, Cao C, Yang H. The effects of platelet-rich plasma on the osteogenic induction of bone marrow mesenchymal stem cells. Connect Tissue Res. 2014;55(4):304–309. doi: 10.3109/03008207.2014.930140 [DOI] [PubMed] [Google Scholar]
- 141.Qi Y, Niu L, Zhao T, et al. Combining mesenchymal stem cell sheets with platelet-rich plasma gel/calcium phosphate particles: a novel strategy to promote bone regeneration. Stem Cell Res Ther. 2015;6(1):256. doi: 10.1186/s13287-015-0256-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Ferreira CF, Carriel Gomes MC, Filho JS, Granjeiro JM, Oliveira Simões CM, Magini Rde S. Platelet-rich plasma influence on human osteoblasts growth. Clin Oral Implants Res. 2005;16(4):456–460. doi: 10.1111/j.1600-0501.2005.01145.x [DOI] [PubMed] [Google Scholar]
- 143.Steller D, Herbst N, Pries R, Juhl D, Hakim SG. Positive impact of Platelet-rich plasma and Platelet-rich fibrin on viability, migration and proliferation of osteoblasts and fibroblasts treated with zoledronic acid. Sci Rep. 2019;9(1):8310. doi: 10.1038/s41598-019-43798-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ogino Y, Ayukawa Y, Kukita T, Koyano K. The contribution of platelet-derived growth factor, transforming growth factor-beta1, and insulin-like growth factor-I in platelet-rich plasma to the proliferation of osteoblast-like cells. Oral Surg, Oral Med Oral Pathol Oral Radiol Endod. 2006;101(6):724–729. doi: 10.1016/j.tripleo.2005.08.016 [DOI] [PubMed] [Google Scholar]
- 145.Vahabi S, Yadegary Z, Karamshahi M. Evaluating the adhesion of human gingival fibroblasts and MG-63 osteoblast-like cells to activated PRP-coated membranes. Cell Tissue Bank. 2019;20(3):339–349. doi: 10.1007/s10561-019-09772-9 [DOI] [PubMed] [Google Scholar]
- 146.Celotti F, Colciago A, Negri-Cesi P, Pravettoni A, Zaninetti R, Sacchi MC. Effect of platelet-rich plasma on migration and proliferation of SaOS-2 osteoblasts: role of platelet-derived growth factor and transforming growth factor-beta. Wound Repair Regen. 2006;14(2):195–202. doi: 10.1111/j.1743-6109.2006.00110.x [DOI] [PubMed] [Google Scholar]
- 147.Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron RJ. Effects of an injectable platelet-rich fibrin on osteoblast behavior and bone tissue formation in comparison to platelet-rich plasma. Platelets. 2018;29(1):48–55. doi: 10.1080/09537104.2017.1293807 [DOI] [PubMed] [Google Scholar]
- 148.Chaput CD, Patel KV, Brindley GW, et al. Influence of a platelet concentrate on prosthetic bone ingrowth in a rabbit model. J Surg Orthop Adv. 2007;16(4):159–163. [PubMed] [Google Scholar]
- 149.Hernandez-Fernandez A, Vélez R, Soldado F, Saenz-Ríos JC, Barber I, Aguirre-Canyadell M. Effect of administration of platelet-rich plasma in early phases of distraction osteogenesis: an experimental study in an ovine femur model. Injury. 2013;44(7):901–907. doi: 10.1016/j.injury.2012.10.018 [DOI] [PubMed] [Google Scholar]
- 150.Kanthan SR, Kavitha G, Addi S, Choon DS, Kamarul T. Platelet-rich plasma (PRP) enhances bone healing in non-united critical-sized defects: a preliminary study involving rabbit models. Injury. 2011;42(8):782–789. doi: 10.1016/j.injury.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 151.Kasten P, Vogel J, Geiger F, Niemeyer P, Luginbühl R, Szalay K. The effect of platelet-rich plasma on healing in critical-size long-bone defects. Biomaterials. 2008;29(29):3983–3992. doi: 10.1016/j.biomaterials.2008.06.014 [DOI] [PubMed] [Google Scholar]
- 152.Kroese-Deutman HC, Vehof JW, Spauwen PH, Stoelinga PJ, Jansen JA. Orthotopic bone formation in titanium fiber mesh loaded with platelet-rich plasma and placed in segmental defects. Int J Oral Maxillofac Surg. 2008;37(6):542–549. doi: 10.1016/j.ijom.2008.01.009 [DOI] [PubMed] [Google Scholar]
- 153.Kurikchy MQ, Al-Rawi NH, Ayoub RS, Mohammed SS. Histological evaluation of bone healing using organic bovine bone in combination with platelet-rich plasma (an experimental study on rabbits). Clin Oral Investig. 2013;17(3):897–904. doi: 10.1007/s00784-012-0751-z [DOI] [PubMed] [Google Scholar]
- 154.Lin BN, Whu SW, Chen CH, et al. Bone marrow mesenchymal stem cells, platelet-rich plasma and nanohydroxyapatite-type I collagen beads were integral parts of biomimetic bone substitutes for bone regeneration. J Tissue Eng Regen Med. 2013;7(11):841–854. doi: 10.1002/term.1472 [DOI] [PubMed] [Google Scholar]
- 155.Lysiak-Drwal K, Dominiak M, Solski L, et al. Early histological evaluation of bone defect healing with and without guided bone regeneration techniques: experimental animal studies. Postepy Hig Med Dosw. 2008;62:282–288. [PubMed] [Google Scholar]
- 156.Malhotra A, Pelletier M, Oliver R, Christou C, Walsh WR. Platelet-rich plasma and bone defect healing. Tissue Eng Part A. 2014;20(19–20):2614–2633. doi: 10.1089/ten.TEA.2013.0737 [DOI] [PubMed] [Google Scholar]
- 157.Molina-Miñano F, López-Jornet P, Camacho-Alonso F, Vicente-Ortega V. Plasma rich in growth factors and bone formation: a radiological and histomorphometric study in New Zealand rabbits. Braz Oral Res. 2009;23(3):275–280. doi: 10.1590/s1806-83242009000300009 [DOI] [PubMed] [Google Scholar]
- 158.Nair MB, Varma HK, Menon KV, Shenoy SJ, John A. Reconstruction of goat femur segmental defects using triphasic ceramic-coated hydroxyapatite in combination with autologous cells and platelet-rich plasma. Acta Biomater. 2009;5(5):1742–1755. doi: 10.1016/j.actbio.2009.01.009 [DOI] [PubMed] [Google Scholar]
- 159.Nather A, Wong KL, David V, Pereira BP. Allografts with autogenous platelet-rich plasma for tibial defect reconstruction: a rabbit study. J Orthop Surg. 2012;20(3):375–380. doi: 10.1177/230949901202000324 [DOI] [PubMed] [Google Scholar]
- 160.Niemeyer P, Fechner K, Milz S, et al. Comparison of mesenchymal stem cells from bone marrow and adipose tissue for bone regeneration in a critical size defect of the sheep tibia and the influence of platelet-rich plasma. Biomaterials. 2010;31(13):3572–3579. doi: 10.1016/j.biomaterials.2010.01.085 [DOI] [PubMed] [Google Scholar]
- 161.Orth M, Shadmanov T, Scheuer C, et al. Marble-derived microcalcite improves bone healing in mice osteotomy. Biomed Mater. 2018;14(2):025001. doi: 10.1088/1748-605X/aaee54 [DOI] [PubMed] [Google Scholar]
- 162.Parizi AM, Oryan A, Shafiei-Sarvestani Z, Bigham AS. Human platelet rich plasma plus Persian Gulf coral effects on experimental bone healing in rabbit model: radiological, histological, macroscopical and biomechanical evaluation. J Mater Sci Mater Med. 2012;23(2):473–483. doi: 10.1007/s10856-011-4478-1 [DOI] [PubMed] [Google Scholar]
- 163.Rabillard M, Grand JG, Dalibert E, Fellah B, Gauthier O, Niebauer GW. Effects of autologous platelet rich plasma gel and calcium phosphate biomaterials on bone healing in an ulnar ostectomy model in dogs. Vet Comp Orthop Traumatol. 2009;22(6):460–466. doi: 10.3415/vcot-09-04-0048 [DOI] [PubMed] [Google Scholar]
- 164.Rai B, Oest ME, Dupont KM, Ho KH, Teoh SH, Guldberg RE. Combination of platelet-rich plasma with polycaprolactone-tricalcium phosphate scaffolds for segmental bone defect repair. J Biomed Mater Res A. 2007;81(4):888–899. doi: 10.1002/jbm.a.31142 [DOI] [PubMed] [Google Scholar]
- 165.Sarkar MR, Augat P, Shefelbine SJ, et al. Bone formation in a long bone defect model using a platelet-rich plasma-loaded collagen scaffold. Biomaterials. 2006;27(9):1817–1823. doi: 10.1016/j.biomaterials.2005.10.039 [DOI] [PubMed] [Google Scholar]
- 166.Simman R, Hoffmann A, Bohinc RJ, Peterson WC, Russ AJ. Role of platelet-rich plasma in acceleration of bone fracture healing. Ann Plast Surg. 2008;61(3):337–344. doi: 10.1097/SAP.0b013e318157a185 [DOI] [PubMed] [Google Scholar]
- 167.Souza TF, Andrade AL, Ferreira GT, et al. Healing and expression of growth factors (TGF-β and PDGF) in canine radial ostectomy gap containing platelet-rich plasma. Vet Comp Orthop Traumatol. 2012;25(6):445–452. doi: 10.3415/vcot-10-10-0146 [DOI] [PubMed] [Google Scholar]
- 168.Sugimori E, Shintani S, Ishikawa K, Hamakawa H. Effects of apatite foam combined with platelet-rich plasma on regeneration of bone defects. Dent Mater J. 2006;25(3):591–596. doi: 10.4012/dmj.25.591 [DOI] [PubMed] [Google Scholar]
- 169.Zhang ZY, Huang AW, Fan JJ, et al. The potential use of allogeneic platelet-rich plasma for large bone defect treatment: immunogenicity and defect healing efficacy. Cell Transplant. 2013;22(1):175–187. doi: 10.3727/096368912x653183 [DOI] [PubMed] [Google Scholar]
- 170.Canbeyli İD, Akgun RC, Sahin O, Terzi A, Tuncay İC. Platelet-rich plasma decreases fibroblastic activity and woven bone formation with no significant immunohistochemical effect on long-bone healing: an experimental animal study with radiological outcomes. J Orthop Surg. 2018;26(3):2309499018802491. doi: 10.1177/2309499018802491 [DOI] [PubMed] [Google Scholar]
- 171.He F, Chen Y, Li J, et al. Improving bone repair of femoral and radial defects in rabbit by incorporating PRP into PLGA/CPC composite scaffold with unidirectional pore structure. J Biomed Mater Res A. 2015;103(4):1312–1324. doi: 10.1002/jbm.a.35248 [DOI] [PubMed] [Google Scholar]
- 172.Kim YH, Furuya H, Tabata Y. Enhancement of bone regeneration by dual release of a macrophage recruitment agent and platelet-rich plasma from gelatin hydrogels. Biomaterials. 2014;35(1):214–224. doi: 10.1016/j.biomaterials.2013.09.103 [DOI] [PubMed] [Google Scholar]
- 173.Szponder T, Wessely-Szponder J, Sobczyńska-Rak A, Żylińska B, Radzki RP, Polkowska I. Application of Platelet-rich Plasma and Tricalcium Phosphate in the Treatment of Comminuted Fractures in Animals. Vivo. 2018;32(6):1449–1455. doi: 10.21873/invivo.11398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Shafiei-Sarvestani Z, Oryan A, Maimandi-Parizi A, Bigham Sadegh A. Histological, Biomechanical and Radiological Evaluation of Bone Repair with Human Platelet Rich Plasma in Rabbit Model. Zahedan J Res Med Sci. 2013;17. [Google Scholar]
- 175.Bölükbaşı N, Yeniyol S, Tekkesin MS, Altunatmaz K. The use of platelet-rich fibrin in combination with biphasic calcium phosphate in the treatment of bone defects: a histologic and histomorphometric study. Curr Ther Res Clin Exp. 2013;75:15–21. doi: 10.1016/j.curtheres.2013.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Chen H, Ji XR, Zhang Q, Tian XZ, Zhang BX, Tang PF. Effects of Calcium Sulfate Combined with Platelet-rich Plasma on Restoration of Long Bone Defect in Rabbits. Chin Med J. 2016;129(5):557–561. doi: 10.4103/0366-6999.176981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Cho K, Kim JM, Kim MH, Kang SS, Kim G, Choi SH. Scintigraphic evaluation of osseointegrative response around calcium phosphate-coated titanium implants in tibia bone: effect of platelet-rich plasma on bone healing in dogs. Eur Surg Res. 2013;51(3–4):138–145. doi: 10.1159/000357197 [DOI] [PubMed] [Google Scholar]
- 178.Dallari D, Fini M, Stagni C, et al. In vivo study on the healing of bone defects treated with bone marrow stromal cells, platelet-rich plasma, and freeze-dried bone allografts, alone and in combination. J Orthop Res. 2006;24(5):877–888. doi: 10.1002/jor.20112 [DOI] [PubMed] [Google Scholar]
- 179.Emilov-Velev K, Clemente-de-Arriba C, Alobera-García M, Moreno-Sansalvador EM, Campo-Loarte J. Bone regeneration in experimental animals using calcium phosphate cement combined with platelet growth factors and human growth hormone. Rev Esp Cir Ortop Traumatol. 2015;59(3):200–210. doi: 10.1016/j.recot.2014.07.011 [DOI] [PubMed] [Google Scholar]
- 180.Filardo G, Kon E, Tampieri A, et al. New bio-ceramization processes applied to vegetable hierarchical structures for bone regeneration: an experimental model in sheep. Tissue Eng Part A. 2014;20(3–4):763–773. doi: 10.1089/ten.TEA.2013.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Gumieiro EH, Abrahão M, Jahn RS, et al. Platelet-rich plasma in bone repair of irradiated tibiae of Wistar rats. Acta Cir Bras. 2010;25(3):257–263. doi: 10.1590/s0102-86502010000300007 [DOI] [PubMed] [Google Scholar]
- 182.Hakimi M, Grassmann JP, Betsch M, et al. The composite of bone marrow concentrate and PRP as an alternative to autologous bone grafting. PLoS One. 2014;9(6):e100143. doi: 10.1371/journal.pone.0100143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kasten P, Beverungen M, Lorenz H, Wieland J, Fehr M, Geiger F. Comparison of platelet-rich plasma and VEGF-transfected mesenchymal stem cells on vascularization and bone formation in a critical-size bone defect. Cells Tissues Organs. 2012;196(6):523–533. doi: 10.1159/000337490 [DOI] [PubMed] [Google Scholar]
- 184.Kon E, Filardo G, Delcogliano M, et al. Platelet autologous growth factors decrease the osteochondral regeneration capability of a collagen-hydroxyapatite scaffold in a sheep model. BMC Musculoskelet Disord. 2010;11:220. doi: 10.1186/1471-2474-11-220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Neves PC, Abib Sde C, Neves RF, et al. Effect of hyperbaric oxygen therapy combined with autologous platelet concentrate applied in rabbit fibula fraction healing. Clinics. 2013;68(9):1239–1246. doi: 10.6061/clinics/2013(09)11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Oryan A, Meimandi Parizi A, Shafiei-Sarvestani Z, Bigham AS. Effects of combined hydroxyapatite and human platelet rich plasma on bone healing in rabbit model: radiological, macroscopical, hidtopathological and biomechanical evaluation. Cell Tissue Bank. 2012;13(4):639–651. doi: 10.1007/s10561-011-9285-x [DOI] [PubMed] [Google Scholar]
- 187.Schneppendahl J, Jungbluth P, Lögters TT, et al. Treatment of a diaphyseal long-bone defect with autologous bone grafts and platelet-rich plasma in a rabbit model. Vet Comp Orthop Traumatol. 2015;28(3):164–171. doi: 10.3415/vcot-14-05-0079 [DOI] [PubMed] [Google Scholar]
- 188.Thorwarth M, Wehrhan F, Schultze-Mosgau S, Wiltfang J, Schlegel KA. PRP modulates expression of bone matrix proteins in vivo without long-term effects on bone formation. Bone. 2006;38(1):30–40. doi: 10.1016/j.bone.2005.06.020 [DOI] [PubMed] [Google Scholar]
- 189.Weibrich G, Hansen T, Kleis W, Buch R, Hitzler WE. Effect of platelet concentration in platelet-rich plasma on peri-implant bone regeneration. Bone. 2004;34(4):665–671. doi: 10.1016/j.bone.2003.12.010 [DOI] [PubMed] [Google Scholar]
- 190.Wiltfang J, Kloss FR, Kessler P, et al. Effects of platelet-rich plasma on bone healing in combination with autogenous bone and bone substitutes in critical-size defects. An animal experiment. Clin Oral Implants Res. 2004;15(2):187–193. doi: 10.1111/j.1600-0501.2004.00980.x [DOI] [PubMed] [Google Scholar]
- 191.Yilmaz D, Dogan N, Ozkan A, Sencimen M, Ora BE, Mutlu I. Effect of platelet rich fibrin and beta tricalcium phosphate on bone healing. A histological study in pigs. Acta Cir Bras. 2014;29(1):59–65. doi: 10.1590/s0102-86502014000100009 [DOI] [PubMed] [Google Scholar]
- 192.Zhong D, Wang CG, Yin K, et al. In vivo ossification of a scaffold combining β-tricalcium phosphate and platelet-rich plasma. Exp Ther Med. 2014;8(5):1381–1388. doi: 10.3892/etm.2014.1969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Akyildiz S, Soluk-Tekkesin M, Keskin-Yalcin B, et al. Acceleration of Fracture Healing in Experimental Model: platelet-Rich Fibrin or Hyaluronic Acid? J Craniofac Surg. 2018;29(7):1794–1798. doi: 10.1097/scs.0000000000004934 [DOI] [PubMed] [Google Scholar]
- 194.Batista MA, Leivas TP, Rodrigues CJ, Arenas GC, Belitardo DR, Guarniero R. Comparison between the effects of platelet-rich plasma and bone marrow concentrate on defect consolidation in the rabbit tibia. Clinics. 2011;66(10):1787–1792. doi: 10.1590/s1807-593220110007000018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Dülgeroglu TC, Metineren H. Evaluation of the Effect of Platelet-Rich Fibrin on Long Bone Healing: an Experimental Rat Model. Orthopedics. 2017;40(3):e479–e484. doi: 10.3928/01477447-20170308-02 [DOI] [PubMed] [Google Scholar]
- 196.Guzel Y, Karalezli N, Bilge O, et al. The biomechanical and histological effects of platelet-rich plasma on fracture healing. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1378–1383. doi: 10.1007/s00167-013-2734-2 [DOI] [PubMed] [Google Scholar]
- 197.Hakimi M, Jungbluth P, Sager M, et al. Combined use of platelet-rich plasma and autologous bone grafts in the treatment of long bone defects in mini-pigs. Injury. 2010;41(7):717–723. doi: 10.1016/j.injury.2009.12.005 [DOI] [PubMed] [Google Scholar]
- 198.Jungbluth P, Wild M, Grassmann JP, et al. Platelet-rich plasma on calcium phosphate granules promotes metaphyseal bone healing in mini-pigs. J Orthop Res. 2010;28(11):1448–1455. doi: 10.1002/jor.21152 [DOI] [PubMed] [Google Scholar]
- 199.Lucarelli E, Fini M, Beccheroni A, et al. Stromal stem cells and platelet-rich plasma improve bone allograft integration. Clin Orthop Relat Res. 2005;435:62–68. doi: 10.1097/01.blo.0000165736.87628.12 [DOI] [PubMed] [Google Scholar]
- 200.Park HC, Kim SG, Oh JS, et al. Early Bone Formation at a Femur Defect Using CGF and PRF Grafts in Adult Dogs: a Comparative Study. Implant Dent. 2016;25(3):387–393. doi: 10.1097/id.0000000000000423 [DOI] [PubMed] [Google Scholar]
- 201.Raafat SN, Amin RM, Elmazar MM, Khattab MM, El-Khatib AS. The sole and combined effect of simvastatin and platelet rich fibrin as a filling material in induced bone defect in tibia of albino rats. Bone. 2018;117:60–69. doi: 10.1016/j.bone.2018.09.003 [DOI] [PubMed] [Google Scholar]
- 202.Sindel A, Dereci Ö, Toru HS, Tozoğlu S. Histomorphometric Comparison of Bone Regeneration in Critical-Sized Bone Defects Using Demineralized Bone Matrix, Platelet-Rich Fibrin, and Hyaluronic Acid as Bone Substitutes. J Craniofac Surg. 2017;28(7):1865–1868. doi: 10.1097/scs.0000000000003588 [DOI] [PubMed] [Google Scholar]
- 203.Bibbo C, Bono CM, Lin SS. Union rates using autologous platelet concentrate alone and with bone graft in high-risk foot and ankle surgery patients. J Surg Orthop Adv. 2005;14(1):17–22. [PubMed] [Google Scholar]
- 204.Bielecki T, Gazdzik TS, Szczepanski T. Benefit of percutaneous injection of autologous platelet-leukocyte-rich gel in patients with delayed union and nonunion. Eur Surg Res. 2008;40(3):289–296. doi: 10.1159/000114967 [DOI] [PubMed] [Google Scholar]
- 205.Calori GM, Tagliabue L, Gala L, d’Imporzano M, Peretti G, Albisetti W. Application of rhBMP-7 and platelet-rich plasma in the treatment of long bone non-unions: a prospective randomised clinical study on 120 patients. Injury. 2008;39(12):1391–1402. doi: 10.1016/j.injury.2008.08.011 [DOI] [PubMed] [Google Scholar]
- 206.Chiang CC, Su CY, Huang CK, Chen WM, Chen TH, Tzeng YH. Early experience and results of bone graft enriched with autologous platelet gel for recalcitrant nonunions of lower extremity. J Trauma. 2007;63(3):655–661. doi: 10.1097/01.ta.0000219937.51190.37 [DOI] [PubMed] [Google Scholar]
- 207.Dallari D, Savarino L, Stagni C, et al. Enhanced tibial osteotomy healing with use of bone grafts supplemented with platelet gel or platelet gel and bone marrow stromal cells. J Bone Joint Surg Am. 2007;89(11):2413–2420. doi: 10.2106/jbjs.F.01026 [DOI] [PubMed] [Google Scholar]
- 208.Galasso O, Mariconda M, Romano G, et al. Expandable intramedullary nailing and platelet rich plasma to treat long bone non-unions. J Orthop Traumatol. 2008;9(3):129–134. doi: 10.1007/s10195-008-0021-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gołos J, Waliński T, Piekarczyk P, Kwiatkowski K. Results of the use of platelet rich plasma in the treatment of delayed union of long bones. Ortop Traumatol Rehabil. 2014;16(4):397–406. doi: 10.5604/15093492.1119617 [DOI] [PubMed] [Google Scholar]
- 210.Griffin XL, Achten J, Parsons N, Costa ML. Platelet-rich therapy in the treatment of patients with Hip fractures: a single centre, parallel group, participant-blinded, randomised controlled trial. BMJ Open. 2013;3(6). doi: 10.1136/bmjopen-2013-002583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kitoh H, Kitakoji T, Tsuchiya H, Katoh M, Ishiguro N. Distraction osteogenesis of the lower extremity in patients with achondroplasia/hypochondroplasia treated with transplantation of culture-expanded bone marrow cells and platelet-rich plasma. J Pediatr Orthop. 2007;27(6):629–634. doi: 10.1097/BPO.0b013e318093f523 [DOI] [PubMed] [Google Scholar]
- 212.Kitoh H, Kitakoji T, Tsuchiya H, Katoh M, Ishiguro N. Transplantation of culture expanded bone marrow cells and platelet rich plasma in distraction osteogenesis of the long bones. Bone. 2007;40(2):522–528. doi: 10.1016/j.bone.2006.09.019 [DOI] [PubMed] [Google Scholar]
- 213.Lee DH, Ryu KJ, Kim JW, Kang KC, Choi YR. Bone marrow aspirate concentrate and platelet-rich plasma enhanced bone healing in distraction osteogenesis of the tibia. Clin Orthop Relat Res. 2014;472(12):3789–3797. doi: 10.1007/s11999-014-3548-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Liebergall M, Schroeder J, Mosheiff R, et al. Stem cell-based therapy for prevention of delayed fracture union: a randomized and prospective preliminary study. Mol Ther. 2013;21(8):1631–1638. doi: 10.1038/mt.2013.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Malhotra R, Kumar V, Garg B, et al. Role of autologous platelet-rich plasma in treatment of long-bone nonunions: a prospective study. Musculoskelet Surg. 2015;99(3):243–248. doi: 10.1007/s12306-015-0378-8 [DOI] [PubMed] [Google Scholar]
- 216.Mariconda M, Cozzolino F, Cozzolino A, D’Agostino E, Bove A, Milano C. Platelet gel supplementation in long bone nonunions treated by external fixation. J Orthop Trauma. 2008;22(5):342–345. doi: 10.1097/BOT.0b013e318172cea5 [DOI] [PubMed] [Google Scholar]
- 217.Namazi H, Kayedi T. Investigating the Effect of Intra-articular Platelet-Rich Plasma Injection on Union: pain and Function Improvement in Patients with Scaphoid Fracture. J Hand Microsurg. 2016;8(3):140–144. doi: 10.1055/s-0036-1597088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Namazi H, Mehbudi A. Investigating the effect of intra-articular PRP injection on pain and function improvement in patients with distal radius fracture. Orthop Traumatol Surg Res. 2016;102(1):47–52. doi: 10.1016/j.otsr.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 219.Peerbooms JC, Colaris JW, Hakkert AA, et al. No positive bone healing after using platelet rich plasma in a skeletal defect. An observational prospective cohort study. Int Orthop. 2012;36(10):2113–2119. doi: 10.1007/s00264-012-1603-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Samy AM. The role of platelet rich plasma in management of fracture neck femur: new insights. Int Orthop. 2016;40(5):1019–1024. doi: 10.1007/s00264-015-2844-1 [DOI] [PubMed] [Google Scholar]
- 221.Sanchez M, Anitua E, Cugat R, et al. Nonunions treated with autologous preparation rich in growth factors. J Orthop Trauma. 2009;23(1):52–59. doi: 10.1097/BOT.0b013e31818faded [DOI] [PubMed] [Google Scholar]
- 222.Say F, Türkeli E, Bülbül M. Is platelet-rich plasma injection an effective choice in cases of non-union? Acta Chir Orthop Traumatol Cech. 2014;81(5):340–345. [PubMed] [Google Scholar]
- 223.Sys J, Weyler J, Van Der Zijden T, Parizel P, Michielsen J. Platelet-rich plasma in mono-segmental posterior lumbar interbody fusion. Eur Spine J. 2011;20(10):1650–1657. doi: 10.1007/s00586-011-1897-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Tarallo L, Mugnai R, Adani R, Catani F. Treatment of the ulna non-unions using dynamic compression plate fixation, iliac bone grafting and autologous platelet concentrate. Eur J Orthop Surg Traumatol. 2012;22(8):681–687. doi: 10.1007/s00590-011-0902-y [DOI] [PubMed] [Google Scholar]
- 225.Wei LC, Lei GH, Sheng PY, et al. Efficacy of platelet-rich plasma combined with allograft bone in the management of displaced intra-articular calcaneal fractures: a prospective cohort study. J Orthop Res. 2012;30(10):1570–1576. doi: 10.1002/jor.22118 [DOI] [PubMed] [Google Scholar]
- 226.Rodriguez-Collazo ER, Urso ML. Combined use of the Ilizarov method, concentrated bone marrow aspirate (cBMA), and platelet-rich plasma (PRP) to expedite healing of bimalleolar fractures. Strategies Trauma Limb Reconstr. 2015;10(3):161–166. doi: 10.1007/s11751-015-0239-x [DOI] [PMC free article] [PubMed] [Google Scholar]