Abstract
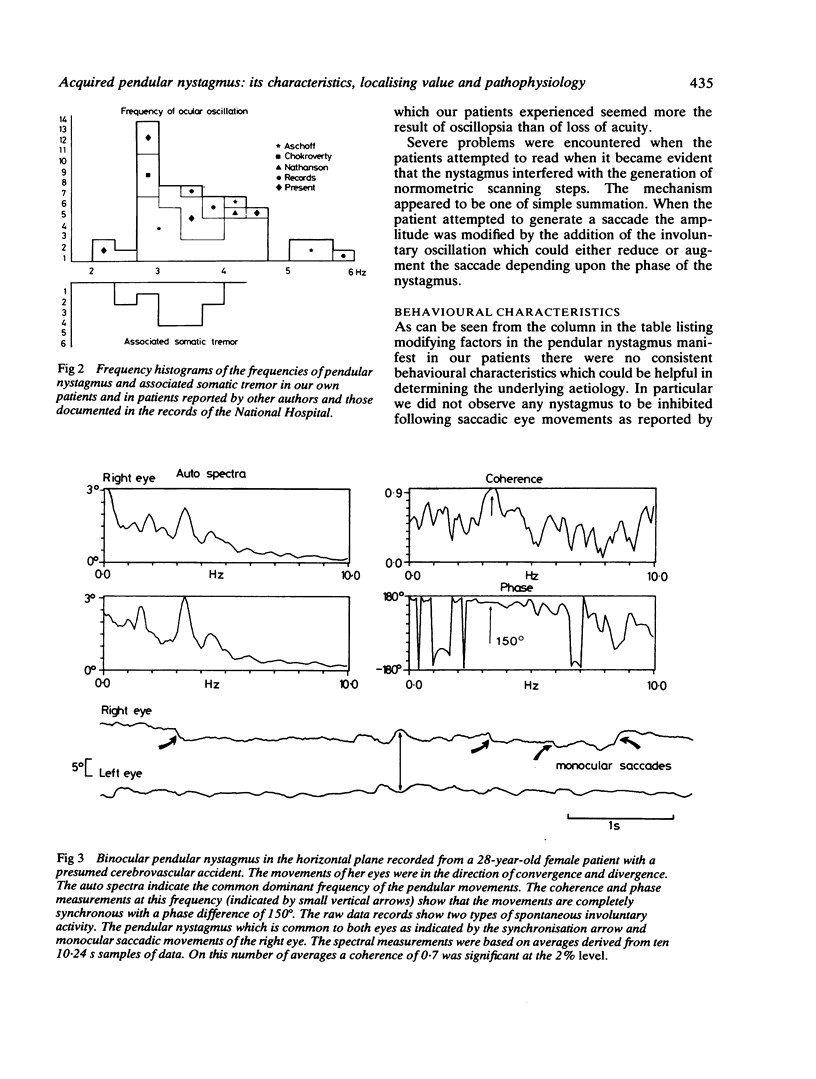
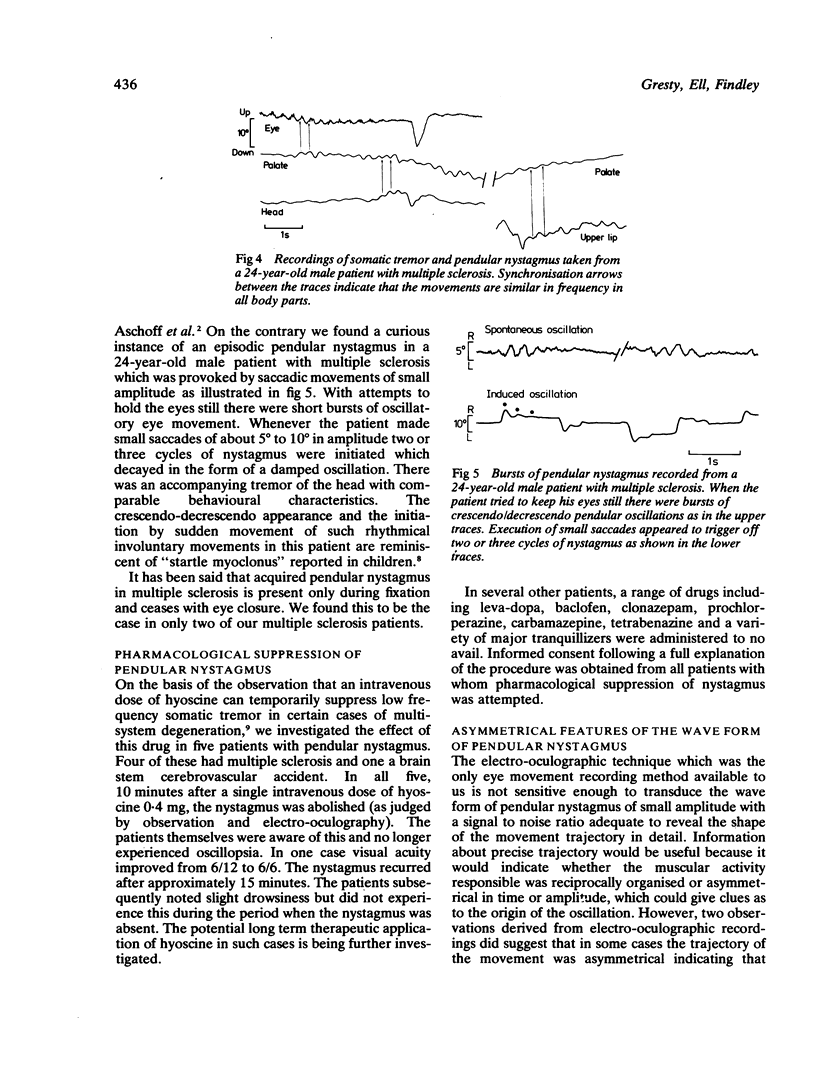
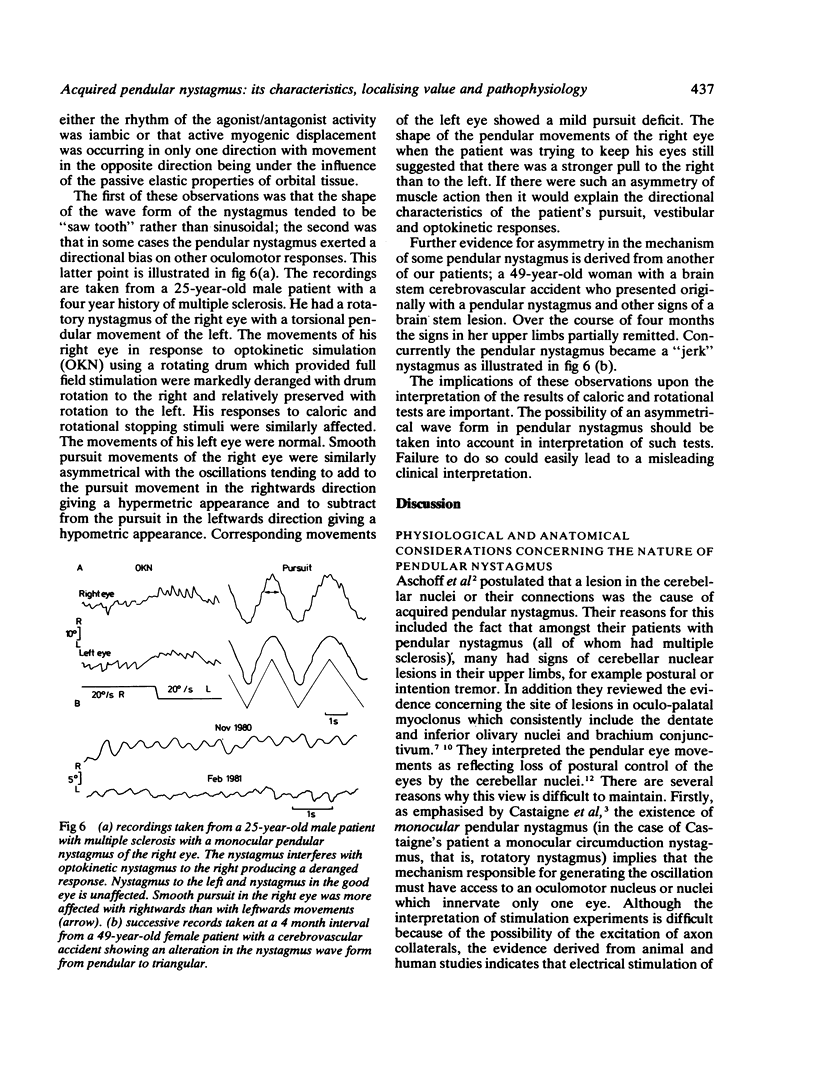
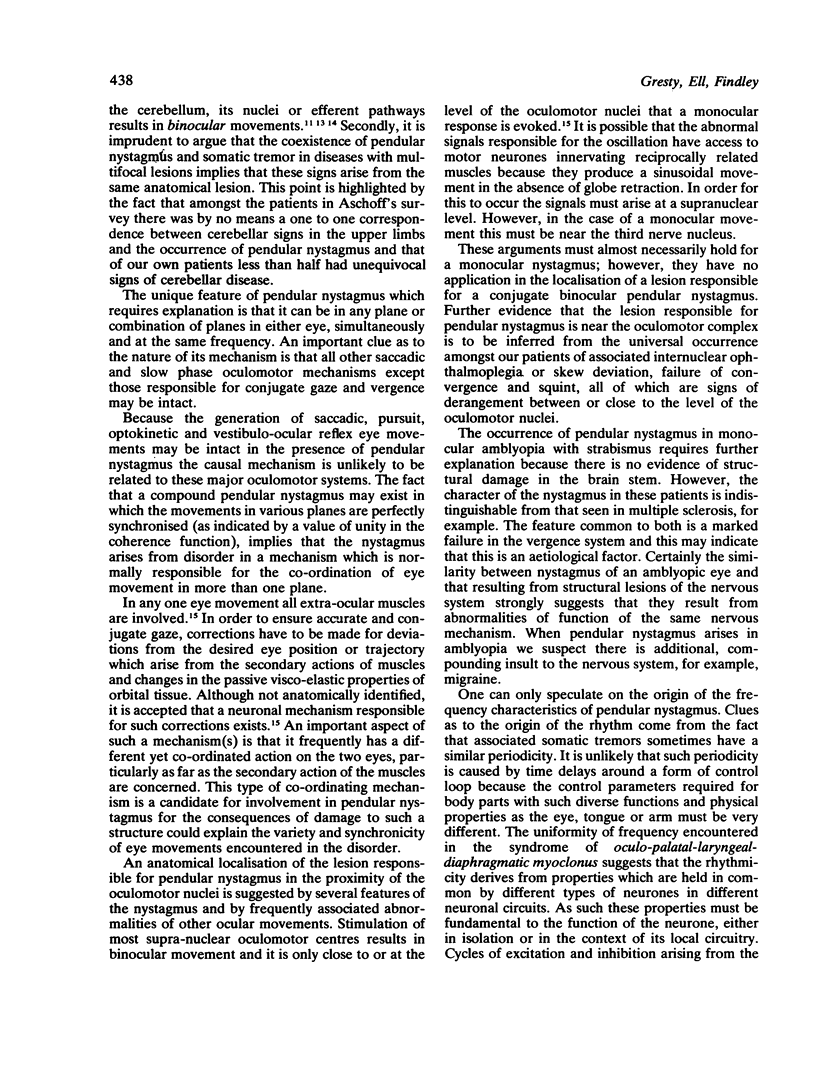
Investigations were made of 16 patients with acquired pendular nystagmus and a further 32 cases reported in the literature were reviewed. Amongst our own patients two thirds had multiple sclerosis, almost one third a cerebrovascular accident or angioma and two had optic atrophy with squint. The nystagmus took forms which could be monocular or binocular, conjugate or disconjugate and could involve movements about single or multiple axes. Spectral analysis was used to characterise the amplitude and frequency of the movements and to estimate the degree of relationship (coherence) between movements of the two eyes or between movements of one eye about several axes. The oscillations ranged in frequency from 2·5 Hz to 6 Hz, with typical amplitudes between 3° and 5°. In a given patient all oscillations, regardless of plane, were highly synchronised. Somatic tremors of the upper limb, face and palate associated with the nystagmus were often at similar frequencies to the eye movement. The other ocular signs common to all our patients were the presence of squint with failure of convergence. Most patients also had skew deviation or internuclear ophthalmoplegia or both. The major oculomotor systems, that is, saccades, pursuit, optokinetic and vestibulo-ocular reflexes could be intact. It is inferred that the mechanism responsible for the pendular nystagmus lies at a level which is close to the oculomotor nuclei so that it can have monocular effects but is not part of the primary motor pathways. It is possible that this mechanism normally subserves maintenance of conjugate movement and posture of the eyes. The periodicity of the nystagmus is likely to arise from instability in a certain type(s) of neurone, for the associated somatic tremors have similar characteristics and yet involve very different neuronal muscular circuitry. Prognosis for cessation of the nystagmus is poor. In five patients with multiple sclerosis it was suppressed by intravenous hyoscine with, however, unacceptable subsequent side effects.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aschoff J. C., Conrad B., Kornhuber H. H. Acquired pendular nystagmus with oscillopsia in multiple sclerosis: a sign of cerebellar nuclei disease. J Neurol Neurosurg Psychiatry. 1974 May;37(5):570–577. doi: 10.1136/jnnp.37.5.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BENDER M. B., NATHANSON M., GORDON G. G. Myoclonus of muscles of the eye, face, and throat. AMA Arch Neurol Psychiatry. 1952 Jan;67(1):44–58. doi: 10.1001/archneurpsyc.1952.02320130050004. [DOI] [PubMed] [Google Scholar]
- Bender M. B. Brain control of conjugate horizontal and vertical eye movements: a survey of the structural and functional correlates. Brain. 1980 Mar;103(1):23–69. doi: 10.1093/brain/103.1.23. [DOI] [PubMed] [Google Scholar]
- Chokroverty S., Barron K. D. Palatal myoclonus and rhythmic ocular movements: a polygraphic study. Neurology. 1969 Oct;19(10):975–982. doi: 10.1212/wnl.19.10.975. [DOI] [PubMed] [Google Scholar]
- Findley L. J., Gresty M. A., Halmagyi M. G. A novel method of recording arm movements. A survey of common abnormalities. Arch Neurol. 1981 Jan;38(1):38–42. doi: 10.1001/archneur.1981.00510010064011. [DOI] [PubMed] [Google Scholar]
- Gresty M. A., Halmagyi G. M. Abnormal head movements. J Neurol Neurosurg Psychiatry. 1979 Aug;42(8):705–714. doi: 10.1136/jnnp.42.8.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guillain G. The Syndrome of Synchronous and Rhythmic Palato-Pharyngo-Laryngo-Oculo-Diaphragmatic Myoclonus: (Section of Neurology). Proc R Soc Med. 1938 Jul;31(9):1031–1038. [PMC free article] [PubMed] [Google Scholar]
- Kornhuber H. H. Motor functions of cerebellum and basal ganglia: the cerebellocortical saccadic (ballistic) clock, the cerebellonuclear hold regulator, and the basal ganglia ramp (voluntary speed smooth movement) generator. Kybernetik. 1971 Apr;8(4):157–162. doi: 10.1007/BF00290561. [DOI] [PubMed] [Google Scholar]
- NATHANSON M. Palatal myoclonus; further clinical and pathophysiological observations. AMA Arch Neurol Psychiatry. 1956 Mar;75(3):285–296. [PubMed] [Google Scholar]
- Nashold B. S., Jr, Gills J. P., Jr Ocular signs from brain stimulation and lesions. Arch Ophthalmol. 1967 May;77(5):609–618. doi: 10.1001/archopht.1967.00980020611009. [DOI] [PubMed] [Google Scholar]
- Nashold B. S., Jr, Slaughter D. G., Gills J. P. Ocular reactions in man from deep cerebellar stimulation and lesions. Arch Ophthalmol. 1969 Apr;81(4):538–543. doi: 10.1001/archopht.1969.00990010540013. [DOI] [PubMed] [Google Scholar]
- Ron S., Robinson D. A. Eye movements evoked by cerebellar stimulation in the alert monkey. J Neurophysiol. 1973 Nov;36(6):1004–1022. doi: 10.1152/jn.1973.36.6.1004. [DOI] [PubMed] [Google Scholar]


