Abstract
Background:
Labor neuraxial analgesia may reduce the odds of postpartum hemorrhage, the leading indication for maternal blood transfusion during childbirth. This study tested the hypothesis that labor neuraxial analgesia is associated with reduced odds of maternal blood transfusion overall.
Methods:
US birth certificate data in Natality File of the National Vital Statistics System for all 50 states from 2015 to 2018 for vaginal and intrapartum cesarean deliveries were analyzed. The exposure was labor neuraxial analgesia. The primary outcome was maternal blood transfusion, recorded on the birth certificate, which has low sensitivity for this outcome. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) of blood transfusion associated with neuraxial analgesia were estimated using propensity-score matching. The aORs were estimated overall and according to delivery mode, and treatment effect compared between vaginal and intrapartum cesarean deliveries using an interaction term. Sensitivity analyses were performed using inverse propensity-score weighting and quantitative bias analysis for outcome misclassification.
Results:
Of the 12,503,042 deliveries analyzed, 9,479,291 (75.82%) were with neuraxial analgesia and 42,485 (0.34%) involved maternal blood transfusion. After propensity-score matching, the incidence of blood transfusion was 0.30% in women without neuraxial analgesia (7907 of 2,589,493) and 0.20% in women with neuraxial analgesia (5225 of 2,589,493), yielding an aOR of 0.87 (95% CI: 0.82, 0.91) overall. For intrapartum cesarean deliveries, the aOR was 0.55 (95% CI: 0.48, 0.64), and for vaginal deliveries 0.93 (95% CI: 0.88, 0.98; P-value for the interaction term <0.001). Results were consistent in the sensitivity analyses, although the quantitative bias analysis demonstrated wide variation in potential effect size point estimates.
Conclusions:
Labor neuraxial analgesia may be associated with reduced odds of maternal blood transfusion in intrapartum cesarean deliveries and, to a lesser extent, vaginal deliveries. The specific effect size varies widely by delivery mode and is unclear given the poor sensitivity of the dataset for the maternal transfusion primary outcome.
INTRODUCTION
Labor neuraxial analgesia (i.e., epidural, or combined spinal epidural analgesia) is the most effective technique to alleviate pain during labor and is used in approximately 70% of US births.1,2 Furthermore, labor neuraxial analgesia is suggested to be associated with reduced odds of severe maternal morbidity. Severe maternal morbidity refers to unintended adverse outcomes during childbirth, resulting in significant short- or long-term consequences to a mother’s health.3
At least two pathways have been suggested for explaining the reduced odds of severe maternal morbidity associated with labor neuraxial analgesia. First, for women who gave birth vaginally, prior research reports that labor neuraxial analgesia is associated with reduced odds of postpartum hemorrhage.4,5 As of 2022, postpartum hemorrhage is the leading cause of preventable severe maternal morbidity and preventable maternal mortality.6–8 Furthermore, postpartum hemorrhage is one of the leading indications for blood product transfusion during childbirth and the postpartum.9 Of concern, blood transfusion in postpartum women is reported to be associated with increased odds of transfusion reactions (e.g., transfusion related acute lung injury) compared to non-pregnant women.10 Second, labor neuraxial analgesia may prevent the use of general anesthesia if an intrapartum cesarean delivery is required; general anesthesia is associated with increased odds of postpartum hemorrhage and maternal morbidity.11–13 The reported reduction in odds of postpartum hemorrhage associated with labor neuraxial analgesia makes it plausible to hypothesize that labor neuraxial analgesia is associated with reduced odds of blood transfusion during childbirth. Using birth certificate data for vaginal and intrapartum cesarean deliveries in the 50 states and the District of Columbia between 2015 and 2018, we conducted this study to assess the association of labor neuraxial analgesia with maternal blood transfusion.
MATERIALS AND METHODS
The study protocol was deemed exempt by the Institutional Review Board of the Columbia University Irving Medical Center. A data analysis and statistical plan was written and shared before data were accessed with the funding agency (National Institute on Minority Health and Health Disparities). The study follows the STROBE reporting guidelines. The currently presented analysis was based on the initial analysis combined with changes made during the peer review process.
Data system
We analyzed US birth certificate data contained in the restricted access Natality File of the National Vital Statistics System (National Center for Health Statistics, Centers for Diseases Control and Prevention). The Natality File is based on the 2003 revised US Standard Certificate of Live Birth.14 As of January 2015, the 2003 revised US Standard Certificate of Live Birth was implemented in the 50 US states and the District of Columbia. The Natality File is a census of all live births in the U.S. and contains comprehensive information on the mother, pregnancy, labor, and delivery. Residence and hospital county characteristics were abstracted from the Area Health Resource File.15
Study sample
The study sample included birth certificates for vaginal and intrapartum cesarean deliveries from January 2015 to December 2018. Non-intrapartum cesarean deliveries were excluded. We identified vaginal and cesarean deliveries using a specific checkbox on the birth certificate. Since the checkbox did not indicate whether a cesarean delivery was intrapartum or not, we defined a cesarean delivery as intrapartum if associated with at least one of the following characteristics indicating labor: 1) trial of labor attempted if previous cesarean delivery; 2) induction of labor; 3) augmentation of labor; 4) antibiotics received by the mother during labor; 5) and clinical chorioamnionitis diagnosed during labor or maternal temperature >38°C during labor (Supplemental Digital Content Table 1). Exclusion criteria were (Figure 1): 1) missing information on labor neuraxial analgesia; 2) missing information on maternal outcome; 3) missing information on maternal race and ethnicity; 4) birth not occurring in the state of residence; 5) birth not occurring in a hospital; 6) mother not residing in the US; and 7) missing information on residence or hospital county.
Figure 1:
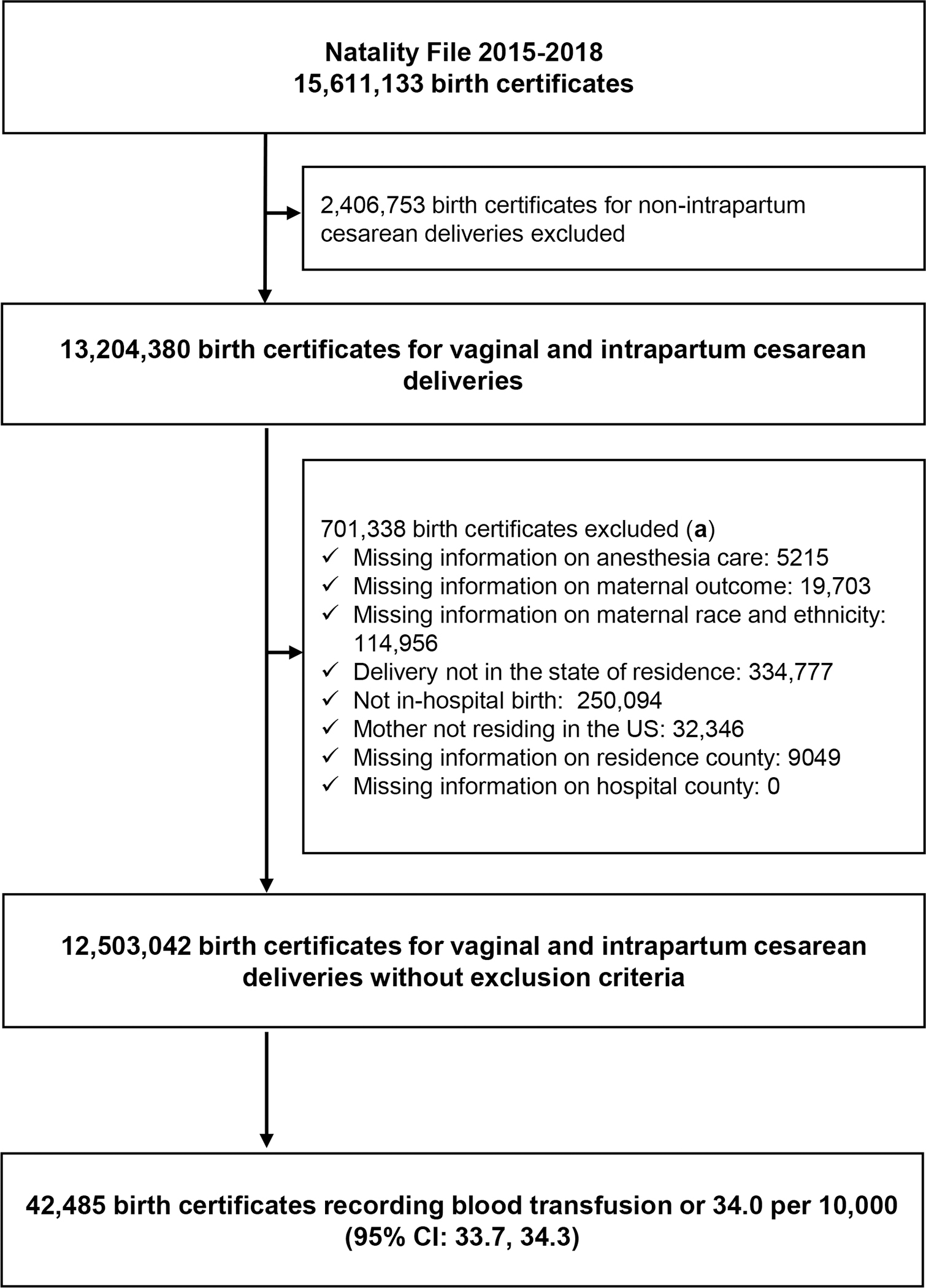
Flowchart of the study.
(a) Reasons for exclusion are not mutually exclusive.
Exposure
The exposure of interest was labor neuraxial analgesia. In the birth certificate, it is reported in a specific checkbox (“Epidural or spinal anesthesia during labor”) and defined as the “administration to the mother of a regional anesthetic for control of the pain of labor (i.e., delivery of the agent into a limited space with the distribution of the analgesic effect limited to the lower body)”.16 The reported sensitivity of labor neuraxial analgesia in birth certificate data in a study conducted in two states in 2009–2011 and in a study conducted in New York City in 2013 was greater than 85%.17,18 The Natality File does not contain detailed information on the type of labor neuraxial analgesia precluding the analysis of the effect of neuraxial techniques (epidural or combined spinal epidural).
Outcome measure
The outcome measure of interest was maternal blood transfusion, reported in a specific checkbox, and defined as “infusion of whole blood or packed red blood cells associated with labor and delivery”.16 The reported sensitivity and positive predictive value of blood transfusion in birth certificate data in the state of Massachusetts in 2011–2013 were 12% and 73% respectively.19 In a recent study analyzing birth certificate data from 2014 to 2016 in the United States, the reported incidence of blood transfusion was 0.3%.20 Birth certificates do not contain codes of the International Classification of Diseases, precluding the assessment of severe maternal morbidity as defined by the US Centers for Disease Control and Prevention (CDC).21
Maternal and hospital characteristics
We selected maternal and hospital characteristics for this study based on their plausible association with labor neuraxial analgesia use or with maternal blood transfusion.
Maternal characteristics and comorbidities from the birth certificate data included: age (≤ 19, 20–29, 30–39, or ≥ 40 years); race and ethnicity; education level (less than high school, high-school with no diploma, high school graduate or general educational diploma, and college or higher); health insurance (Medicaid, private, self-pay, or other); body mass index (≤ 18.4, 18.5–24.9, 25.0–29.9, 30.0–34.9, or ≥ 35 kg/m2); and preexisting or gestational diabetes or hypertension. Maternal race and ethnicity included six mutually exclusive groups: 1) non-Hispanic White (hereafter referred to as White); 2) non-Hispanic Black (Black); 3) Hispanic; 4) non-Hispanic Asian, Native Hawaiian, and Other Pacific Islander (Asian and Pacific Islander); 5) non-Hispanic American Indian and Alaskan Native (Native American); 6) and more than one race. We acknowledge that race is a social construct, these data have inherent limitations, and include the data given evidence of inequities and racism in maternal and infant outcomes.22
We abstracted the following residence county characteristics from the Area Health Resource File: location (urban, suburban, or rural); proportion of persons in poverty; and proportion of persons unemployed.15 Area Health Resource File data for the year 2015 were used for births in 2015 and 2016, and Area Health Resource File data for the year 2017 were used for births in 2017 and 2018.
Obstetrical characteristics from the birth certificate data included: previous cesarean section; month of gestation prenatal care began (1st –3rd, 4th –6th, ≥ 7th, or no prenatal care); number of prenatal visits; delivery during a weekend; mother transferred in (i.e., transfer from another facility for maternal medical or fetal indications for delivery); nulliparous; gestational age at delivery (≤ 33 weeks, 34–38 weeks, or ≥ 39 weeks); multiple gestation; non-cephalic presentation; induction of labor; augmentation of labor; antibiotics during labor; chorioamnionitis; attendant at birth (doctor of Medicine, doctor of Osteopathy, midwife, or other); and birth weight (≤ 2499 grams, 2500–4000 grams, or > 4000 grams).
We abstracted the following hospital county characteristics form the Area Health Resource File file: location (urban, suburban, or rural); number of in-hospital births; number of physician anesthesiologists (per 1000 in-hospital births); number of certified registered nurse anesthetists (per 1000 in-hospital births); and number of obstetricians and gynecologists (per 1000 in-hospital births). Area Health Resource File data for the year 2015 were used for births in 2015 and 2016, and Area Health Resource File data for the year 2017 were used for births in 2017 and 2018.
Statistical analysis
We performed the statistical analysis using R software version 3.6.2 (R Foundation for Statistical Computing, Vienna, Austria) and specific packages (‘Matching’ for matching, ‘survival’ for conditional logistic regression, and ‘episensr’ for probabilistic sensitivity analysis).23
Descriptive statistics
We calculated the labor neuraxial analgesia rate overall, and according to delivery mode (vaginal or intrapartum cesarean delivery) and maternal race and ethnicity (White, Black, Hispanic, Asian and Pacific Islander, Native American, and more than one race). We compared characteristics between women with and without labor neuraxial analgesia using the absolute standardized difference, with a value greater than 10% used to define a clinically important imbalance.24
Crude analysis
We calculated the incidence of blood transfusion in women with and without labor neuraxial analgesia, overall and according to delivery mode. The crude risk difference was calculated as the difference in blood transfusion incidence between women with and without labor neuraxial analgesia. Crude odds ratios (OR) of blood transfusion associated with labor neuraxial analgesia were estimated using univariate logistic regression models overall, and according to delivery mode.
Adjusted analysis
We estimated the adjusted differences and adjusted ORs using the propensity-score matching method, with the propensity score estimating the individual probability of receiving labor neuraxial analgesia. We calculated the propensity score using a fixed-effect logistic regression model, with labor neuraxial analgesia as the dependent variable and 33 patient- and hospital-level characteristics as the independent variables (Supplemental Digital Content Table 2). The propensity score was computed independently for each of the four years of the study period. We performed a complete case analysis with 968,635 discharges excluded (7.7%). The matching procedure used the nearest neighbor approach with a caliper of 0.001, one case matched to one control, and stratification according to delivery mode and year of delivery. We assessed the balance after matching using the absolute standardized difference. In propensity-score matched data, we estimated adjusted ORs using conditional logistic regression models, overall and according to delivery mode. We compared the odds of blood transfusion associated with labor neuraxial analgesia between women who had a vaginal delivery and women who had an intrapartum cesarean delivery using the regression coefficient of an interaction term between labor neuraxial analgesia and delivery mode. We added to the models variables with a persistent imbalance after matching (absolute standardized difference >10%). In a pre-planned sensitivity analysis, we re-estimated the adjusted ORs of blood transfusion associated with labor neuraxial analgesia using the inverse propensity-score weighting method. Weights were stabilized and truncated at 1% and 99%.
To assess potential bias due to unmeasured confounder, we calculated the E-value associated with the adjusted OR of blood transfusion. The E-value estimates how strong an unmeasured confounder (i.e., an unknown factor associated with both labor neuraxial analgesia and blood transfusion) would need to be to explain away the observed association between labor neuraxial analgesia and blood transfusion.25 The lowest possible E-value is 1 and indicates that no unmeasured confounding is needed to explain away the observed association. The higher the E-value, the stronger the confounder must be to explain away the observed association.
Subgroup analyses
To assess the robustness of our findings, we estimated the adjusted ORs of blood transfusion associated with labor neuraxial analgesia in three subgroups of women: 1) women at low risk of cesarean delivery defined as women with singleton, head-first, term (37, 38, 49, 40, or 41 completed weeks) first births; 2) women at low infectious risk defined as women who did not receive antibiotics during labor, had no clinical chorioamnionitis diagnosed during labor, and had no temperature >38°C during labor; and 3) women without comorbidities defined as women with no pre-existing or gestational diabetes, no pre-existing or gestational hypertension, no pre-eclampsia, and no eclampsia.
Sample size and study power
Since the study sample size was fixed, we estimated the minimum detectable effect using this study sample. We expected to include about 10 million birth certificates for vaginal or intrapartum cesarean deliveries, including 7 million with labor neuraxial analgesia (70%). We expected to propensity score match 2.1 million birth certificates with labor neuraxial analgesia (30%) to 2.1 million birth certificates without labor neuraxial analgesia. With an incidence of blood transfusion of 30 per 10,000 in certificates without labor neuraxial analgesia,20 a two-sided test at a significance level of 0.05, our data would have 90% power to detect a minimum OR of blood transfusion associated with labor neuraxial analgesia of 0.94 (or lower).26
Post hoc analyses
We performed two post hoc analyses suggested by the reviewers to assess the degree of underreporting of blood transfusion in birth certificate data and its impact on the adjusted odds ratio of maternal blood transfusion associated with labor neuraxial analgesia. First, we estimated the incidence of blood transfusion using the National Inpatient Sample from October 2015 to December 2018. The National Inpatient Sample is a stratified 20% sample of all discharge records from community hospitals in the United States,27 and blood product transfusion was identified using the CDC algorithm based on ICD-10-CM codes.21 Second, we performed a probabilistic sensitivity analysis to correct for outcome misclassification and the odds ratios of blood transfusion associated with labor neuraxial analgesia.28 We performed this analysis in crude data and in data weighted using the inverse propensity score weighting method using the following assumptions: sensitivity of blood transfusion between 10 and 50% (uniform distribution), specificity between 75 and 100% (uniform distribution), and non-differential misclassification of blood transfusion between women who received labor neuraxial analgesia and women who did not. Corrected median odds ratio (2.5–97.5th percentile) of blood transfusion associated with labor neuraxial analgesia were estimated using 100,000 iterations.
RESULTS
Of the 12,503,042 birth certificates meeting inclusion and exclusion criteria for analysis, 2,532,011 (20.2%) were for intrapartum cesarean deliveries (Figure 1). The number of births certificates with labor neuraxial analgesia was 9,479,291, yielding an overall labor neuraxial analgesia rate of 75.82% (95% CI: 75.79, 75.84). Labor neuraxial analgesia rate was higher for intrapartum cesarean deliveries (90.77%; 95% CI: 90.73, 90.81) than for vaginal deliveries (72.02%; 95% CI: 71.99, 72.05). Among the six racial and ethnic groups, Hispanic and Native American women had the lowest labor neuraxial analgesia rate (Table 1).
Table 1:
Labor neuraxial analgesia rate according to maternal race and ethnicity (United States 2015–2018).
| Number of women | Number of women with labor neuraxial analgesia | Labor neuraxial analgesia rate (95% CI) | |
|---|---|---|---|
|
| |||
| All women | 12,503,042 | 9,479,291 | 75.82% (75.79, 75.84) |
| Non-Hispanic White | 6,506,786 | 5,128,373 | 78.82% (78.78, 78.85) |
| More than 1 race | 271,959 | 209,126 | 76.90% (76.74, 77.05) |
| Asian and Pacific Islander | 851,063 | 650,659 | 76.45% (76.36, 76.54) |
| Non-Hispanic Black | 1,801,365 | 1,354,148 | 75.17% (75.11, 75.24) |
| Hispanic | 2,971,883 | 2,074,383 | 69.80% (69.75, 69.85) |
| Native American | 99,986 | 62,602 | 62.61% (62.31, 62.91) |
Abbreviations: CI: confidence interval.
Compared to women delivering without labor neuraxial analgesia (Table 2), women delivering with labor neuraxial analgesia had a higher education level, or private health insurance, or lived in a county with lower unemployment rate. They had more often gestational hypertension. They received an earlier initiation of prenatal care or had a higher number of prenatal visits. They were more often nulliparous or with a previous cesarean section, had an induction or augmentation of labor, and delivered more often in an urban setting, or with a Doctor of Medicine as an attendant at birth.
Table 2:
Comparison of women who received and women who did not receive labor neuraxial analgesia, before and after propensity-score matching (United States, 2015–2018).
| Before matching | After matching | ||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Missing | No neuraxial analgesia n = 3,023,751 | Neuraxial Analgesia n = 9,479,291 | Absolute standardized difference | No neuraxial analgesia n = 2,589,493 | Neuraxial Analgesia n = 2,589,493 | Absolute standardized difference | |
|
| |||||||
| General characteristics | |||||||
|
| |||||||
| Age (year) | 0 | 3.4% | 1.4% | ||||
| ≤ 19 | 165,113 (5.5%) | 579,733 (6.1%) | 142,515 (5.5%) | 149,270 (5.8%) | |||
| 20–29 | 1,525,142 (50.4%) | 4,834,847 (51.0%) | 1,309,179 (50.6%) | 1,315,947 (50.8%) | |||
| 30–39 | 1,246,573 (41.2%) | 3,808,509 (40.2%) | 1,065,176 (41.1%) | 1,053,403 (40.7%) | |||
| ≥ 40 | 86,923 (2.9%) | 256,202 (2.7%) | 72,623 (2.8%) | 70,873 (2.7%) | |||
|
| |||||||
| Race or ethnicity | 0 | 20.6% | 8.8% | ||||
| White | 1,378,413 (45.6%) | 5,128,373 (54.1%) | 1,223,371 (47.2%) | 1,140,878 (44.1%) | |||
| Black | 447,217 (14.8%) | 1,354,148 (14.3%) | 374,198 (14.5%) | 352,879 (13.6%) | |||
| Hispanic | 897,500 (29.7%) | 2,074,383 (21.9%) | 736,730 (28.5%) | 799,462 (30.9%) | |||
| Asian and Pacific Islander | 200,404 (6.6%) | 650,659 (6.9%) | 174,297 (6.7%) | 212,354 (8.2%) | |||
| Native American | 37,384 (1.2%) | 62,602 (0.7%) | 26,050 (1.0%) | 25,492 (1.0%) | |||
| More than one race | 62,833 (2.1%) | 209,126 (2.2%) | 54,847 (2.1%) | 58,428 (2.3%) | |||
|
| |||||||
| Education level | 101,439 | 23.8% | 4.3% | ||||
| Less than high school | 177,715 (5.9%) | 216,920 (2.3%) | 120,321 (4.6%) | 103,086 (4.0%) | |||
| High school with no diploma | 383,634 (12.8%) | 916,568 (9.7%) | 319,113 (12.3%) | 299,949 (11.6%) | |||
| High school graduate or general educational diploma | 817,835 (27.3%) | 2,374,954 (25.2%) | 704,446 (27.2%) | 704,666 (27.2%) | |||
| College and higher | 1,611,188 (53.9%) | 5,902,789 (62.7%) | 1,445,613 (55.8%) | 1,481,792 (57.2%) | |||
|
| |||||||
| Health insurance | 71,467 | 20.8% | 2.9% | ||||
| Medicaid | 1,462,514 (48.7%) | 3,946,677 (41.9%) | 1,232,868 (47.6%) | 1,209,547 (46.7%) | |||
| Private | 1,263,737 (42.1%) | 4,854,450 (51.5%) | 1,134,994 (43.8%) | 1,164,748 (45.0%) | |||
| Self-pay (uninsured) | 154,252 (5.1%) | 267,327 (2.8%) | 116,708 (4.5%) | 106,977 (4.1%) | |||
| Other | 121,681 (4.1%) | 360,937 (3.8%) | 104,923 (4.1%) | 108,221 (4.2%) | |||
|
| |||||||
| Body mass index (kg/m2) | 315,036 | 7.8% | 2.2% | ||||
| ≤ 18.4 | 112,902 (3.9%) | 325,944 (3.5%) | 99,565 (3.8%) | 105,694 (4.1%) | |||
| 18.5–24.9 | 1,361,675 (46.5%) | 4,109,496 (44.4%) | 1,204,356 (46.5%) | 1,219,632 (47.1%) | |||
| 25.0–29.9 | 773,205 (26.4%) | 2,416,486 (26.1%) | 680,743 (26.3%) | 676,149 (26.1%) | |||
| 30.0–34.9 | 396,969 (13.6%) | 1,323,496 (14.3%) | 351,543 (13.6%) | 346,453 (13.4%) | |||
| ≥ 35 | 280,976 (9.6%) | 1,086,857 (11.7%) | 253,286 (9.8%) | 241,565 (9.3%) | |||
|
| |||||||
| County of residence | |||||||
|
| |||||||
| Core base statistical area classification (a) | 1888 | 9.2% | 8.1% | ||||
| Metropolitan | 2,556,456 (84.6%) | 8,315,894 (87.7%) | 2,197,727 (84.9%) | 2,269,526 (87.6%) | |||
| Micropolitan | 287,815 (9.5%) | 731,251 (7.7%) | 246,079 (9.5%) | 198,102 (7.7%) | |||
| Non-metropolitan and non-micropolitan | 178,173 (5.9%) | 431,565 (4.6%) | 145,687 (5.6%) | 121,865 (4.7%) | |||
|
| |||||||
| Percent persons in poverty (a) | 1888 | 14.6 (1 sd, 5.2) | 14.3 (1 sd, 5.1) | 5.8% | 14.5 (1 sd, 5.1) | 14.7 (1 sd, 4.7) | 4.4% |
|
| |||||||
| Percent unemployed (a) | 1888 | 5.1 (1 sd, 1.7) | 4.8 (1 sd, 1.4) | 14.0% | 5.0 (1 sd, 1.6) | 5.1 (1 sd, 1.8) | 8.3% |
|
| |||||||
| Comorbidites | |||||||
|
| |||||||
| Preexisting diabetes | 0 | 17,297 (0.6%) | 78,234 (0.8%) | 3.0% | 15,226 (0.6%) | 13,901 (0.5%) | <0.1% |
|
| |||||||
| Gestational diabetes | 0 | 155,631 (5.1%) | 589,522 (6.2%) | 4.6% | 137,347 (5.3%) | 135,262 (5.2%) | <0.1% |
|
| |||||||
| Preexisting hypertension | 0 | 35620 (1.2%) | 175,708 (1.9%) | 5.5% | 31,700 (1.2%) | 27,454 (1.1%) | 1.5% |
|
| |||||||
| Gestational hypertension | 0 | 118727 (3.9%) | 661,735 (7.0%) | 13.5% | 107,820 (4.2%) | 107,024 (4.1%) | <0.1% |
|
| |||||||
| Pregnancy, labor, and delivery | |||||||
|
| |||||||
| Previous cesarean section | 0 | 139,116 (4.6%) | 909,325 (9.6%) | 19.5% | 125,335 (4.8%) | 102,036 (3.9%) | 4.4% |
|
| |||||||
| Month prenatal care began | 341,841 | 13.7% | 5.4% | ||||
| 1st –3rd | 2,150,999 (73.6%) | 7,259,086 (78.6%) | 1,940,526 (74.9%) | 1,997,490 (77.1%) | |||
| 4th –6th | 543,708 (18.6%) | 1,470,546 (15.9%) | 471,303 (18.2%) | 433,225 (16.7%) | |||
| ≥ 7th | 148,467 (5.1%) | 394,142 (4.3%) | 125,540 (4.8%) | 116,698 (4.5%) | |||
| No prenatal care | 77,462 (2.7%) | 116,791 (1.3%) | 52,124 (2.0%) | 42,080 (1.6%) | |||
|
| |||||||
| Number of prenatal visits | 330,752 | 10.8 (1 sd, 4.2) | 11.5 (1 sd, 4.0) | 16.5% | 11.0 (1 sd, 4.1) | 11.1 (1 sd, 4.0) | 3.9% |
|
| |||||||
| Delivery during a weekend | 0 | 842,057 (27.8%) | 2,570,093 (27.1%) | 1.6% | 717,088 (27.7%) | 720,128 (27.8%) | <0.1% |
|
| |||||||
| Mother transferred in | 3739 | 16,897 (0.6%) | 40,378 (0.4%) | 1.9% | 12,257 (0.5%) | 9329 (0.4%) | 1.8% |
|
| |||||||
| Nulliparous | 52,875 | 770,847 (25.6%) | 3,442,982 (36.5%) | 23.6% | 687,032 (26.5%) | 770,255 (29.7%) | 7.2% |
|
| |||||||
| Gestational age at delivery | 5688 | 7.0% | 4.1% | ||||
| ≤ 33 weeks | 111,692 (3.7%) | 241,749 (2.6%) | 84,048 (3.2%) | 67,128 (2.6%) | |||
| 34–38 weeks | 996,916 (33.0%) | 3,067,886 (32.4%) | 849,632 (32.8%) | 840,907 (32.5%) | |||
| ≥ 39 weeks | 1,911,272 (63.3%) | 6,167,839 (65.1%) | 1,655,813 (63.9%) | 1,681,458 (64.9%) | |||
|
| |||||||
| Multiple gestation | 0 | 42,214 (1.4%) | 251,783 (2.7%) | 9.0% | 36,427 (1.4%) | 32,030 (1.2%) | 1.5% |
|
| |||||||
| Non-cephalic presentation | 67,874 | 66,883 (2.2%) | 320,835 (3.4%) | 7.1% | 58,173 (2.2%) | 40,981 (1.6%) | 4.8% |
|
| |||||||
| Induction of labor | 2138 | 582,867 (19.3%) | 3,202,372 (33.8%) | 33.3% | 537,713 (20.8%) | 568,982 (22.0%) | 2.9% |
|
| |||||||
| Augmentation of labor | 0 | 510,137 (16.9%) | 2,653,965 (28.0%) | 26.9% | 466,345 (18.0%) | 519,812 (20.1%) | 5.3% |
|
| |||||||
| Antibiotics during labor | 0 | 576,007 (19.0%) | 3,124,974 (33.0%) | 32.1% | 521,158 (20.1%) | 510,673 (19.7%) | 1.0% |
|
| |||||||
| Chorioamnionitis | 0 | 16,516 (0.5%) | 214,771 (2.3%) | 14.6% | 14,567 (0.6%) | 20,994 (0.8%) | 3.0% |
|
| |||||||
| Attendant at birth | 4179 | 26.5% | 3.5% | ||||
| Doctor of Medicine | 2,271,294 (75.2%) | 7,925,032 (83.6%) | 1,977,589 (76.4%) | 1,981,557 (76.5%) | |||
| Doctor of Osteopathy | 221,820 (7.3%) | 732,536 (7.7%) | 196,473 (7.6%) | 175,631 (6.8%) | |||
| Midwife | 500,559 (16.6%) | 776,342 (8.2%) | 393,911 (15.2%) | 411,715 (15.9%) | |||
| Other | 28,378 (0.9%) | 42,902 (0.5%) | 21,520 (0.8%) | 20,590 (0.8%) | |||
|
| |||||||
| Intrapartum cesarean delivery | 0 | 233,701 (7.7%) | 2,298,310 (24.2%) | 46.3% | 211,027 (8.1%) | 211,027 (8.1%) | <0.1% (b) |
|
| |||||||
| Birth weight (grams) | 8648 | 4.2% | 3.9% | ||||
| ≤ 2499 grams | 234,206 (7.8%) | 658,217 (6.9%) | 189,589 (7.3%) | 165,608 (6.4%) | |||
| 2500–4000 grams | 2,578,578 (85.4%) | 8,091,180 (85.4%) | 2,219,784 (85.7%) | 2,250,973 (86.9%) | |||
| > 4000 grams | 206,682 (6.8%) | 725,531 (7.7%) | 180,120 (7.0%) | 172,912 (6.7%) | |||
|
| |||||||
| Hospital county characteristics | |||||||
|
| |||||||
| Core base statistical area classification (a) | 897 | 13.0% | 7.3% | ||||
| Metropolitan | 2,656,304 (87.9%) | 8,680,751 (91.6%) | 2,283,973 (88.2%) | 2,342,283 (90.5%) | |||
| Micropolitan | 281,223 (9.3%) | 657,840 (6.9%) | 240,250 (9.3%) | 194,144 (7.5%) | |||
| Non-metropolitan and non-micropolitan | 85,636 (2.8%) | 140,391 (1.5%) | 65,270 (2.5%) | 53,066 (2.0%) | |||
|
| |||||||
| Number of in-hospital births (a) | 897 | 17,069 (1 sd, 26,520) | 16,832 (1 sd, 23,429) | 1.0% | 17,264 (1 sd, 26,604) | 24,151 (1 sd, 33,367) | 22.8% |
|
| |||||||
| Number of physician anesthesiologists (per 1000 hospital births) (a) | 68,099 | 12.7 (1 sd, 14.9) | 13.5 (1 sd, 15.0) | 5.5% | 12.5 (1 sd, 12.7) | 12.4 (1 sd, 7.9) | 1.2% |
|
| |||||||
| Number of certified registered nurse anesthetists (per 1000 hospital births) (a) | 68,099 | 13.6 (1 sd, 29.0) | 14.8 (1 sd, 33.0) | 3.7% | 13.1 (1 sd, 25.6) | 10.9 (1 sd, 12.6) | 10.9% |
|
| |||||||
| Number of obstetricians and gynecologists (per 1000 hospital births) (a) | 68,099 | 11.5 (1 sd, 24.4) | 12.3 (1 sd, 28.5) | 3.0% | 11.1 (1 sd, 20.9) | 10.5 (1 sd, 7.9) | 3.9% |
|
| |||||||
| State characteristics | |||||||
|
| |||||||
| Hospital state identifier | 0 | (c) | (c) | 34.0% | (c) | (c) | 103.2% |
|
| |||||||
| Other | |||||||
|
| |||||||
| Year of delivery | 0 | 5.5% | <0.1% (b) | ||||
| 2015 | 802,715 (26.5%) | 2,347,947 (24.8%) | 665,476 (25.7%) | 665,476 (25.7%) | |||
| 2016 | 783,620 (25.9%) | 2,394,708 (25.3%) | 668,878 (25.8%) | 668,878 (25.8%) | |||
| 2017 | 739,860 (24.5%) | 2,371,217 (25.0%) | 642,534 (24.8%) | 642,534 (24.8%) | |||
| 2018 | 697,556 (23.1%) | 2,365,419 (25.0%) | 612,605 (23.7%) | 612,605 (23.7%) | |||
Abbreviations: sd: standard deviation.
Results are presented as count (%) or mean (1 standard deviation). An absolute standardized difference greater than 10% indicates a clinically relevant imbalance between groups.
Abstracted from the county-level Area Health Resource File for the year 2015 for births in 2015 and 2016, and for the year 2017 for births in 2017 and 2018.
The matching procedure was stratified according to the delivery mode and to the year of delivery.
Results for the 51 state identifiers are not presented in this Table for clarity purpose. They are presented in Supplemental Table 3.
Crude analysis
Before matching (Table 3), the incidence of blood transfusion was 30.6 per 10,000 in women delivering without labor neuraxial analgesia and 35.1 per 10,000 in women delivering with labor neuraxial analgesia, yielding a risk difference of +4.5 per 10,000 (95% CI: 3.7, 5.2) and a crude OR of 1.15 (95% CI:1.12, 1.17). The risk difference was −52.7 per 10,000 (95% CI: −57.4, −48.1) and a crude OR of 0.58 (95% CI: 0.55, 0.60) for intrapartum cesarean deliveries and +0.3 per 10,000 (95% CI: −0.3, 1.0) and a crude OR of 1.01 (0.99, 1.04) for vaginal deliveries.
Table 3:
Crude odds ratios of blood transfusion associated with labor neuraxial analgesia (United States 2015–2018).
| No labor neuraxial analgesia | Labor neuraxial analgesia | ||||||
|---|---|---|---|---|---|---|---|
| No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | Difference (Per 10,000) | Crude OR (95% CI) |
| Vaginal and intrapartum cesarean deliveries | |||||||
| 3,023,751 | 9256 | 30.6 (30.0, 31.2) | 9,479,291 | 33,229 | 35.1 (34.7, 35.4) | +4.5 | 1.15 (1.12, 1.17) |
| Vaginal deliveries | |||||||
| 2,790,050 | 6325 | 22.7 (22.1, 23.2) | 7,180,981 | 16,528 | 23.0 (22.7, 23.4) | +0.3 | 1.01 (0.99, 1.04) |
| Intrapartum cesarean deliveries | |||||||
| 233,701 | 2931 | 125.4 (120.9, 130.0) | 2,298,310 | 16,701 | 72.7 (71.6, 73.8) | −52.7 | 0.58 (0.55, 0.60) |
Abbreviations: CI: confidence interval; No.: number; OR: odds ratio.
Adjusted analysis
After propensity-score matching, 2,589,493 women delivering without labor neuraxial analgesia were matched to 2,589,493 women delivering with labor neuraxial analgesia. Among the 33 variables included in the propensity score, three had an absolute standardized difference greater than 10% after matching (hospital county number of in-hospital births, hospital county number of certified registered nurse anesthetists, and hospital state), and were added to the conditional logistic regression model used to estimate the adjusted ORs (Table 2 and Supplemental Digital Content Table 2).
After matching, the incidence of blood transfusion was 30.5 per 10,000 in women delivering without labor neuraxial analgesia and 20.2 per 10,000 in women delivering with labor neuraxial analgesia, yielding a risk difference of −10.4 per 10,000 (95% CI: −11.2, −9.5) (Table 4). The adjusted OR of blood transfusion was 0.87 for women receiving labor neuraxial analgesia (95% CI: 0.82, 0.91) compared to women without neuraxial analgesia, with an associated E-value of 1.56. In the subgroup of women with intrapartum cesarean deliveries, the risk difference was −68.2 per 10,000 (95% CI: −73.9, −62.5), the adjusted OR was 0.55 (95% CI: 0.48, 0.64), and the associated E-value 3.04. In the subgroup of women with vaginal deliveries, the risk difference was −5.2 per 10,000 (95% CI: −6.0, −4.4,), the adjusted OR was 0.93 (95% CI: 0.88, 0.98), and the associated E-value 1.36. The regression coefficient of the interaction term between labor neuraxial analgesia and delivery mode was −0.40 (95% CI: −0.48, −0.31), indicating lower odds of blood transfusion associated with labor neuraxial analgesia in women who had an intrapartum cesarean delivery compared to women who had a vaginal delivery.
Table 4:
Adjusted odds ratios of blood transfusion associated with labor neuraxial analgesia using the propensity-score matching method (United States 2015–2018).
| No labor neuraxial analgesia | Labor neuraxial analgesia | |||||||
|---|---|---|---|---|---|---|---|---|
| No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | Difference (Per 10,000) | Adjusted OR (95% CI) (a) | E-value (b) |
| Vaginal and intrapartum cesarean deliveries | ||||||||
| 2,589,493 | 7907 | 30.5 (29.9, 31.2) | 2,589,493 | 5225 | 20.2 (19.6, 20.7) | −10.4 | 0.87 (0.82, 0.91) | 1.56 |
| Vaginal deliveries | ||||||||
| 2,378,466 | 5282 | 22.2 (21.6, 22.8) | 2,378,466 | 4039 | 17.0 (16.5, 17.5) | −5.2 | 0.93 (0.88, 0.98) | 1.36 |
| Intrapartum cesarean deliveries | ||||||||
| 211,027 | 2625 | 124.4 (119.7, 129.2) | 211,027 | 1186 | 56.2 (53.1, 59.5) | −68.2 | 0.55 (0.48, 0.64) | 3.04 |
Abbreviations: CI: confidence interval; No.: number; OR: odds ratio.
Estimated in propensity score matched data using a conditional logistic regression and further adjustment for 3 variables with a persistent imbalance after matching: 1) Hospital county number of in-hospital births, 2) Hospital county number of certified registered nurse anesthetists, and 3) Hospital state.
The E-value estimates how strong an unmeasured confounder would need to be to explain away the observed association between labor neuraxial analgesia and blood transfusion, conditional of the measured covariates. The lowest possible E-value is 1 and indicates that no unmeasured confounding is needed to explain away the observed association. The higher the E-value, the stronger the confounder association must be to explain away the observed association.
Results were consistent when using the inverse propensity-score weighting method (Table 5 and Supplemental Digital Content Table 4). Using the weighting method, the regression coefficient of the interaction term between labor neuraxial analgesia and delivery mode was −0.31 (95% CI: −0.36, −0.26), indicating lower odds of blood transfusion associated with labor neuraxial analgesia in women who had an intrapartum cesarean delivery compared to women who had a vaginal delivery.
Table 5:
Sensitivity analysis with adjusted odds ratios of blood transfusion associated with labor neuraxial analgesia estimated using the inverse propensity-score weighting method. Weights were stabilized and truncated at 1% and 99%.
| No labor neuraxial analgesia | Labor neuraxial analgesia | ||||||
|---|---|---|---|---|---|---|---|
| No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | No. of women | No. of blood transfusion | Incidence (Per 10,000; 95% CI) | Difference (Per 10,000) | Adjusted OR (95% CI) (a) |
| Vaginal and intrapartum cesarean deliveries | |||||||
| 2,626,611 | 9584 | 36.5 (35.6, 37.4) | 8,796,641 | 29,262 | 33.3 (32.9, 33.6) | −3.2 | 0.91 (0.89, 0.93) |
| Vaginal deliveries | |||||||
| 2,307,382 | 5916 | 25.6 (24.8, 26.4) | 6,866,356 | 15,194 | 22.1 (21.8, 22.5) | −3.5 | 0.86 (0.84, 0.89) |
| Intrapartum cesarean deliveries | |||||||
| 319,229 | 3668 | 114.9 (110.0, 119.9) | 1,930,285 | 14,068 | 72.9 (71.7, 74.1) | −42.0 | 0.63 (0.61, 0.65) |
Abbreviations: CI: confidence interval; No.: number; OR: odds ratio.
Estimated using weighted logistic regression models. No imbalance was observed after weighting.
Subgroup analyses
In the three subgroup analyses (Supplemental Table 5), labor neuraxial analgesia was associated with a significantly decreased odds of blood transfusion in women who had an intrapartum cesarean delivery and, to a lesser extent, in women who had a vaginal delivery.
Post hoc analyses
The incidence of blood product transfusion during delivery hospitalizations estimated using the National Inpatient Sample was 1.1% (0.7% for vaginal deliveries and 2.1% for cesarean deliveries), which is 3.7 times the incidence of blood transfusion in birth certificate data. Results of the probabilistic sensitivity analysis for outcome misclassification (Table 6) were consistent with results of the main analysis. Although the 2.5th to 97.5th percentile point estimates varied widely, the range consistently demonstrated that labor neuraxial analgesia was associated a lower adjusted odds of maternal transfusion.
Table 6:
Probabilistic sensitivity analysis to correct for outcome misclassification and the odds ratios of maternal blood transfusion associated with labor neuraxial analgesia.
| Observed OR (95% CI) | Median corrected OR (2.5–97.5th percentile) (a) | |
|---|---|---|
|
| ||
| Crude data | ||
| Vaginal and intrapartum cesarean deliveries | 1.15 (1.12, 1.17) | 1.29 (1.14, 6.79) |
| Vaginal deliveries | 1.01 (0.99, 1.04) | 1.04 (0.99, 1.61) |
| Intrapartum cesarean deliveries | 0.58 (0.55, 0.60) | 0.39 (0.03, 0.56) |
|
| ||
| Inverse propensity score weighted data | ||
| Vaginal and intrapartum cesarean deliveries | 0.91 (0.89, 0.93) | 0.84 (0.21, 0.91) |
| Vaginal deliveries | 0.86 (0.84, 0.89) | 0.76 (0.14, 0.87) |
| Intrapartum cesarean deliveries | 0.63 (0.61, 0.65) | 0.46 (0.04, 0.62) |
Abbreviations: CI: confidence interval; OR: odds ratio.
The following assumptions were used: sensitivity of blood transfusion between 10 and 50% (uniform distribution), specificity between 75 and 100% (uniform distribution), and non-differential misclassification of the outcome blood transfusion between women who received labor neuraxial analgesia and women who did not. Corrected median odds ratio (2.5–97.5th percentile) of blood transfusion associated with labor neuraxial analgesia were estimated using 100,000 iterations.
DISCUSSION
In this national study of vaginal and intrapartum cesarean deliveries, labor neuraxial analgesia was associated with reduced odds of maternal blood transfusion, although the clinical significance and effect size of this observation varied by delivery mode. Results were consistent in the sensitivity analyses.
Reduction in the odds of maternal blood transfusion was more pronounced in intrapartum cesarean deliveries than in vaginal deliveries (45% vs. 7%). This difference between delivery modes was consistent in the subgroups of women at low cesarean delivery risk, low infectious risk, or without comorbidities (Supplemental Table 5). The small effect size for vaginal deliveries raises legitimate concern about its clinical relevance and reproducibility. Nevertheless, the reported effect size for maternal outcomes associated with labor neuraxial analgesia for vaginal delivery varies with the outcome examined. For example, in a study analyzing French data between 2004 and 2006, Driessen et al. reported 47% decreased odds of severe postpartum hemorrhage, defined as a decrease in postpartum hemoglobin concentration greater than 4g/dL, associated with labor neuraxial analgesia.4 This marked decrease contrast with another study analyzing New York State data between 2010 and 2017, reporting a 14% decrease in the odds of severe maternal morbidity, as defined by the CDC, and a 9% reduction in the odds of postpartum hemorrhage associated with labor neuraxial analgesia.5 In other words, the relatively small effect size for maternal blood transfusion observed in vaginal deliveries does not preclude a greater effect size for other maternal health outcomes.29 Similarly, we observed some differences in the odds of blood transfusion between the main analysis using the propensity score matching method and the sensitivity analysis using the inverse propensity score weighting method. For example, for intrapartum cesarean deliveries, the reduction was 45% (95% CI: 36, 52) using matching (Table 4) and 37% (95% CI: 35, 39) using weighting (Table 5). While the matching procedure tends to favor internal validity, the weighting procedure tends to favor external validity. In other words, reproducing our study using another data system may yield an estimate close to the one we obtained using the weighting method.
We cannot rule out with certainty other mechanisms rather than labor neuraxial analgesia per se that are responsible for the observed reduced odds of maternal blood transfusion. Indeed, in a previous study from our group limited to vaginal deliveries, we reported that labor neuraxial analgesia per se accounted for a small fraction of the reduced odds of severe maternal morbidity observed in women who received labor neuraxial analgesia.5 Other possible mechanisms may include sustained monitoring of women with labor neuraxial analgesia, enhancing early detection of blood loss immediately after childbirth; adequate intravenous access and fluid resuscitation; and continuous anesthesia provider availability and oversight of the process of labor and delivery and preparedness for acute events.30,31 In other words, use of labor neuraxial analgesia could be a proxy for provision of high-quality obstetric anesthesia care.
Limitations
Our findings should be interpreted in the context of the significant limitations related birth certificates data. First, these data provide no information on strong risk factors for blood transfusion (e.g., anemia prior to pregnancy) or conditions associated with a markedly increased risk of obstetric hemorrhage (e.g., placenta accreta disorders) exposing the analysis to the risk of residual confounding. Second, the sensitivity of birth certificate data to detect blood transfusion is low, as reflected by a transfusion rate of 0.3% in our study contrasting with 1.1% in a nationally representative sample.19 Although our quantitative bias analysis suggests that this underreporting did not affect the directionality of the associations, we there is some uncertainty around the point estimate of the reduction of blood transfusion associated with labor neuraxial analgesia. Third, because birth certificate data do not provide a hospital identifier, we estimated hospital characteristics (e.g., number of anesthesia providers) at the hospital-county level. While this approach may be accurate for counties with only one hospital, it may not be accurate for counties with more than one hospital. Last, because birth certificate data do not provide a patient identifier, the analysis could not account for women who had more than one childbirth during the study period.
Conclusion
Labor neuraxial analgesia may be associated with reduced odds of maternal blood transfusion in intrapartum cesarean deliveries and, to a lesser extent, in vaginal deliveries. The specific effect size varies widely by delivery type and is unclear given the poor sensitivity of the dataset for the maternal transfusion primary outcome.
Supplementary Material
Table 1: Definition of intrapartum cesarean deliveries
Table 2: Variables included in the propensity score
Table 3: Hospital state of delivery
Table 4: Balance after inverse propensity-score weighting
Table 5: Subgroups analyses
Funding Statement:
This study was funded by grant R21 MD016414 from the National Institute on Minority Health and Health Disparities, National Institutes of Health.
Footnotes
Conflicts of Interest:
- Jean Guglielminotti is supported by grants from the National Institute on Minority Health and Health Disparities (R01 MD018410, R21 MD016414) and from the National Institute of Mental Health (R21 MH126096), National Institutes of Health.
- Alexander Friedman is supported by grant from the National Institute of Child Health and Human Development (R01 HD104943) not related to the study and has served on an advisory board for Sage and Biogen.
- Ruth Landau was a consultant for Pacira Pharmaceuticals Incorporated and serves on the editorial board of the journal Regional Anesthesia and Pain Medicine.
Prior presentations:
This work was presented in part at the Virtual 53rd Meeting of the Society of Obstetric Anesthesia and Perinatology (May 13–16, 2021).
REFERENCES
- 1.Anim-Somuah M, Smyth RM, Cyna AM, Cuthbert A: Epidural versus non-epidural or no analgesia for pain management in labour. Cochrane Database Syst Rev 2018; 5: CD000331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Butwick AJ, Bentley J, Wong CA, Snowden JM, Sun E, Guo N: United States state-level variation in the use of neuraxial analgesia during labor for pregnant women. JAMA Netw Open 2018; 1: e186567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American College of Obstetricians and Gynecologists, the Society for Maternal-Fetal Medicine, Kilpatrick SK, Ecker JL: Severe maternal morbidity: screening and review. Am J Obstet Gynecol 2016; 215: B17–22 [DOI] [PubMed] [Google Scholar]
- 4.Driessen M, Bouvier-Colle MH, Dupont C, Khoshnood B, Rudigoz RC, Deneux-Tharaux C, Pithagore G: Postpartum hemorrhage resulting from uterine atony after vaginal delivery: factors associated with severity. Obstet Gynecol 2011; 117: 21–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guglielminotti J, Landau R, Daw J, Friedman AM, Chihuri S, Li G: Use of labor neuraxial analgesia for vaginal delivery and severe maternal morbidity. JAMA Netw Open 2022; 5: e220137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maternal Mortality Review Committees. Building U.S. capacity to review and prevent maternal deaths. Report from nine maternal mortality review committee. Available at: https://stacks.cdc.gov/view/cdc/51660. Last accessed: February 17, 2023. [Google Scholar]
- 7.Trost S, Beauregard J, Chandra G, Njie F, Berry J, Harvey A, Goodman DA. Pregnancy-related deaths: data from Maternal Mortality Review Committees in 36 US states, 2017–2019. Available at: https://www.cdc.gov/reproductivehealth/maternal-mortality/docs/pdf/Pregnancy-Related-Deaths-Data-MMRCs-2017-2019-H.pdf. Last accessed: February 17, 2023.
- 8.Bienstock JL, Eke AC, Hueppchen NA: Postpartum hemorrhage. N Engl J Med 2021; 384: 1635–1645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Corbetta-Rastelli CM, Friedman AM, Sobhani NC, Arditi B, Goffman D, Wen T: Postpartum hemorrhage trends and outcomes in the United States, 2000–2019. Obstet Gynecol 2023; 141: 152–161 [DOI] [PubMed] [Google Scholar]
- 10.Thurn L, Wikman A, Westgren M, Lindqvist PG: Incidence and risk factors of transfusion reactions in postpartum blood transfusions. Blood Adv 2019; 3: 2298–2306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang CC, Wang IT, Chen YH, Lin HC: Anesthetic management as a risk factor for postpartum hemorrhage after cesarean deliveries. Am J Obstet Gynecol 2011; 205: 462 e1–7 [DOI] [PubMed] [Google Scholar]
- 12.Butwick AJ, Ramachandran B, Hegde P, Riley ET, El-Sayed YY, Nelson LM: Risk factors for severe postpartum hemorrhage after cesarean delivery: case-control studies. Anesth Analg 2017; 125: 523–532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guglielminotti J, Landau R, Li G: Adverse events and factors associated with potentially avoidable use of general anesthesia in cesarean deliveries. Anesthesiology 2019; 130: 912–922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention. U.S. standard certificate of live birth. Available at: https://www.cdc.gov/nchs/data/dvs/birth11-03final-ACC.pdf. Last accessed: February 17, 2023.
- 15.Health Resources and Services Administration. Area Health Resources Files (AHRF). 2018–2019. Available at: https://data.hrsa.gov/topics/health-workforce/ahrf. Last accessed: February 17, 2023. [Google Scholar]
- 16.National Center for Health Statistics. Guide to completing the facility worksheets for the certificate of live birth and report of fetal death. Available at: https://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. Last accessed: February 17, 2023.
- 17.Martin JA, Wilson EC, Osterman MJ, Saadi EW, Sutton SR, Hamilton BE: Assessing the quality of medical and health data from the 2003 birth certificate revision: results from two states. Natl Vital Stat Rep 2013; 62: 1–19 [PubMed] [Google Scholar]
- 18.Gregory ECW, Martin JA, Argov EL, Osterman MJK: Assessing the quality of medical and health data from the 2003 birth certificate revision: results from New York City. Natl Vital Stat Rep 2019; 68: 1–20 [PubMed] [Google Scholar]
- 19.Luke B, Brown MB, Liu CL, Diop H, Stern JE: Validation of severe maternal morbidity on the US certificate of live birth. Epidemiology 2018; 29: e31–e32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hartenbach EM, Kuo HD, Greene MZ, Shrider EA, Antony KM, Ehrenthal DB: Peripartum blood transfusion among rural women in the United States. Obstet Gynecol 2020; 135: 685–695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. How does CDC identify severe maternal morbidity? Available at: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.htm. Last accessed: January 4, 2023.
- 22.Society for Maternal-Fetal Medicine, Wheeler SM, Bryant AS, Bonney EA, Howell EA: Society for Maternal-Fetal Medicine special statement: race in maternal-fetal medicine research- Dispelling myths and taking an accurate, antiracist approach. Am J Obstet Gynecol 2022; 226: B13–B22 [DOI] [PubMed] [Google Scholar]
- 23.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. Available at: https://www.R-project.org/. Last accessed: February 17, 2023. [Google Scholar]
- 24.Austin P: Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Communications in Statistics - Simulation and Computation 2009; 38: 1228–1234 [Google Scholar]
- 25.VanderWeele TJ, Ding P: Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med 2017; 167: 268–274 [DOI] [PubMed] [Google Scholar]
- 26.Demidenko E: Sample size determination for logistic regression revisited. Stat Med 2007; 26: 3385–97 [DOI] [PubMed] [Google Scholar]
- 27.Agency for Healthcare Research and Quality. HCUP databases. Healthcare Cost and Utilization Project (HCUP). Available at: https://www.hcup-us.ahrq.gov/sidoverview.jsp. Last accessed: January 4, 2023. [PubMed]
- 28.Fox MP, MacLehose RF, Lash TL: Applying quantitative bias analysis to epidemiologic data, second edition, Springer Nature; Switzerland AG, 2021 [Google Scholar]
- 29.Pankiv E, Yang A, Aoyama K: Neuraxial labor analgesia for vaginal delivery and severe maternal morbidity. JAMA Netw Open 2022; 5: e220142. [DOI] [PubMed] [Google Scholar]
- 30.Mhyre JM, D’Oria R, Hameed AB, Lappen JR, Holley SL, Hunter SK, Jones RL, King JC, D’Alton ME: The maternal early warning criteria: a proposal from the National Partnership for Maternal Safety. Obstet Gynecol 2014; 124: 782–6 [DOI] [PubMed] [Google Scholar]
- 31.Association of Women’s Health Obstetric Neonatal Nurses: Role of the registered nurse in the care of the pregnant woman receiving analgesia and anesthesia by catheter techniques. Nurs Womens Health 2020; 24: 149–151 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1: Definition of intrapartum cesarean deliveries
Table 2: Variables included in the propensity score
Table 3: Hospital state of delivery
Table 4: Balance after inverse propensity-score weighting
Table 5: Subgroups analyses


