Abstract
During the late 19th and early 20th century, several states mandated midwifery licensing requirements to improve midwives’ knowledge, education, and quality. Previous studies point to the health benefits of midwifery quality improvements for maternal and infant health outcomes. This paper exploits the staggered adoption of midwifery laws across states using event-study and difference-in-difference frameworks. We use the universe of death records in the US over the years 1979–2020 and find that exposure to a midwifery licensing law at birth is associated with a 2.5 percent reduction in cumulative mortality rates and an increase of 0.6 months in longevity during adulthood and old age. The effects are concentrated on deaths due to infectious diseases, neoplasm diseases, and suicide mortality. We also show that the impacts are confined among blacks and are slightly larger among males. Additional analyses using alternative data sources suggest small but significant increases in educational attainments, income, measures of socioeconomic status, employment, and measures of height as potential mechanism channels. We provide a discussion on the economic magnitude and policy implication of the results.
Keywords: H75, I18, K23, N31, N32, Health, Mortality, Longevity, Occupational Licensing, Midwifery, Historical Data
1. Introduction
Several growing strands of research highlight the importance of early-life conditions and childhood experiences for later-life mortality outcomes (Almond et al., 2018; Almond & Currie, 2011a, 2011b). The early-life exposures influence short-run health and human capital, which change the trajectory of outcomes throughout the life cycle and appear in old-age health and mortality. For instance, exposure to disease environment, medical innovations, access to healthcare, and general economic conditions are among the early-life factors that are associated with later-life mortality (Aizer et al., 2016; Finch & Crimmins, 2004; Goodman-Bacon, 2021b; Hayward & Gorman, 2004; Moore et al., 2006; Van Den Berg et al., 2006). These exposures may operate through several mediatory channels to affect mortality, including cognitive development, education, income, marital status, and measures of physical and mental health (Bleakley, 2007; Currie et al., 2010; Smith, 2009; Van Den Berg et al., 2015).
This paper examines the role of state-level adoption of midwifery laws during the early decades of the 20th century on long-run health outcomes. Specifically, we explore the effects on mortality outcomes of infants born in states that implemented midwifery policies versus those with no licensing restrictions. These laws required midwives to obtain a license in order to be permitted to offer their services.1 The licensing process for midwives often required them to complete a set of specific educational and training programs, pass exams, and fulfill additional requirements established by regulatory bodies. This process aims to ensure that midwives possess the necessary knowledge, skills, and expertise to offer secure and competent care to women and their families throughout pregnancy, childbirth, and postpartum. In addition, licensing requirements could force low-quality providers to exit the market. Occupational licensing could benefit consumers and protect their health and safety through quality improvement (Kleiner, 2000; Shapiro, 1986).
Although the basic argument for professional licensing is securing quality service, there are concerns about increases in service prices for those granted licensure. This potential rise in prices may limit access to midwifery services, especially among the disadvantaged population, and lead them to move to inferior alternatives (Frank et al., 2003; Kleiner, Discussants, et al., 2016; Shepard, 1978). This channel could mitigate or even reverse the health benefits of licensing. Therefore, the net effects of professional licensing, specifically midwifery licensing requirements, on health outcomes are theoretically ambiguous. However, a narrow strand of literature that evaluates the health effects of midwifery laws usually finds positive net benefits (Högberg, 2011; Miller, 2006; Van Lerberghe et al., 2014). For instance, Anderson et al. (2020) show that midwifery law adoptions across US states between the years 1900–1940 were associated with reductions in maternal and infant mortality. Lazuka (2018) uses data from rural Sweden during the late 19th and early 20th century and finds that receiving treatment from a qualified midwife during birth and postnatal period is associated with lower neonatal mortality. The author explores the effects throughout the life-cycle and shows that those treated by qualified midwives rather than traditional attendants reveal lower mortality rates from cardiovascular and diabetes at ages 40–80. The current study extends this literature by exploring the effects of exposure to midwifery licensing adoption at birth on long-run old-age mortality and longevity.
We employ the universe of death records in the US over the years 1979–2020 and cohorts born between 1900–1940. We find that conditional on fixed effects and covariates, exposure to midwifery law is associated with a 2.5 percent reduction in cumulative mortality rate and roughly 0.6 months of additional life. These effects are larger for tuberculosis, syphilis, other infectious diseases, and suicide. Moreover, the effects are concentrated among nonwhites and males.
The causal interpretation of these results stems from the assumption that the mortality outcomes of treated and control states would have had a similar path in the absence of law changes. We provide two pieces of evidence to support this. First, we show that exposure to midwifery laws does not change the sample’s demographic composition, which could result from differential selection into the sample. We also explore the dynamic changes in states’ sociodemographic characteristics several years before and after the law change. The event-study results fail to provide significant and robust evidence for the endogeneity of midwifery adoption with respect to states’ sociodemographic features. Second, we implement a series of event study analyses and show no discernible difference in mortality and longevity for several years prior to the policy change in treated and control states. Therefore, we rule out the concern over preexisting trends in mortality and argue that the parallel trend assumption holds.
In search of mechanism channels, we use Social Security Administration Death Master Files (DMF). The DMF can be linked to the full-count 1940 census and also World War II enlistment data at the individual level. Using DMF-1940-census-linked data, we observe small increases in socioeconomic status and slight improvements in educational outcomes. In addition, the DMF-enlistment-linked data shows increases in height and height-for-age at the time of WWII enlistment. As an alternative data source, we also use the 1980 census and explore the impacts on other measures of socioeconomic status. We find small but statistically significant effects on the likelihood of employment, higher income, lower likelihood of being low-educated, and slightly lower probability of having a work disability.
This study makes several important contributions to the literature. First, this is the first study to explore the long-run health effects of midwifery laws in the US. While studies suggest potential health gains of improvements in care delivery under midwifery law changes in the early 20th century, fewer studies explore their long-run effects (Anderson et al., 2020; Ten Hoope-Bender et al., 2014).2 The results of this study also relate to midwifery policies and regulations in developing countries where the level of professional care, birth attendance, and prenatal and postnatal environment resembles the early decades of the 20th century in the US.3 Furthermore, since midwifery laws generally improved prenatal and postnatal conditions, this study also relates to current policies regarding expanding healthcare access for pregnant mothers and improving prenatal and postnatal care services (Corman et al., 2019). The second contribution of this paper is to the ongoing policy debates regarding professional and occupational licensing (Kleiner, 2000, 2017; Kleiner, Discussants, et al., 2016; Law & Kim, 2005; Peterson et al., 2014; Timmons & Mills, 2018). The main controversy of this literature is regarding the net benefits of occupational licensing in the healthcare industry. Licensure requirements may improve the quality of providers while increasing the prices due to entry barriers. The magnitude of benefits and costs as well as the net effects, are a priori unknown. Further, it is essential to understand and evaluate the full benefits and costs, including the long-run effects. This study adds to the benefits side of licensing by exploring its effects on an overlooked, understudied outcome, i.e., later-life mortality. The third contribution of the paper is to the ongoing literature that examines the relevance of early-life shocks on later-life mortality (Almond et al., 2018; Almond & Currie, 2011a, 2011b; Barker, 1994, 1995, 1997; Cunha & Heckman, 2007; Hayward & Gorman, 2004; Heckman et al., 2013; Montez & Hayward, 2011). Improvements in midwifery quality due to the change in licensing regime may have direct benefits for infants and reduce pregnancy complications, hence providing better initial health for newborns. Midwifery laws could also mitigate the incidence of maternal mortality with potentially long-lasting effects on individuals, specifically if experienced early in life (Berg et al., 2014; Kes et al., 2015; Thaddeus & Maine, 1994). Therefore, midwifery law change provides a unique and distinguished early-life shock in contrast to other studies that examine adversities and early-life health shocks on later-life outcomes, including mortality (Ding & He, 2021; Fletcher, 2011, 2018a, 2018b; Fletcher et al., 2010; Hayward & Gorman, 2004; Lee & Ryff, 2019; Lei et al., 2020; Lindeboom et al., 2010; Noghanibehambari & Noghani, 2023; Scholte et al., 2015; Steine et al., 2020; Van Den Berg et al., 2006).
The rest of the paper is organized as follows. Section 2 provides a short background on midwifery laws. Section 3 reviews the literature. Section 4 introduces data sources. Section 5 discusses the empirical strategy. We go over the results in section 6. Finally, we conclude the paper in section 7.
2. Background on Midwifery Laws
In the early 20th century, the majority of births were delivered at home with the help of traditional attendants and midwives. The market for midwives in the US was largely unregulated and practiced by women who had learned through traditional apprenticeship rather than formal education. However, this began to change in the 1920s and 1930s as the medical profession began to assert greater control over childbirth and midwifery care. As a result, many states passed laws requiring midwives to be licensed or registered, and some began to require that midwives work under the supervision of a physician. These laws were often motivated by concerns about infant mortality rates and the perceived need for greater standardization and professionalization of midwifery practice.
The Illinois Medical Practice Act of 1877 was one of the earliest examples of state-level medical licensing and regulation in the United States. This act established a framework for the regulation of midwifery in the state. The act required midwives to be licensed by the state board of health and to pass an examination demonstrating their knowledge of anatomy, physiology, and hygiene. It also required midwives to report cases of infectious disease to the board of health (Goebel, 1994). This act set a precedent for similar laws in other states and helped establish modern medical licensure system and regulation systems. By 1900, seven other states passed similar laws in an attempt to solve the “midwife problems,” including Connecticut, Indiana, Louisiana, Minnesota, New Jersey, Ohio, and Wyoming (Rude, 1923). As public health concerns regarding midwifery practices grew, there was mounting pressure on authorities to regulate the market of midwifery professionals. Consequently, 22 more states joined the movement between 1900 and 1940.4
Fig. 1 shows states and years of midwifery law adoption.
Fig. 1.
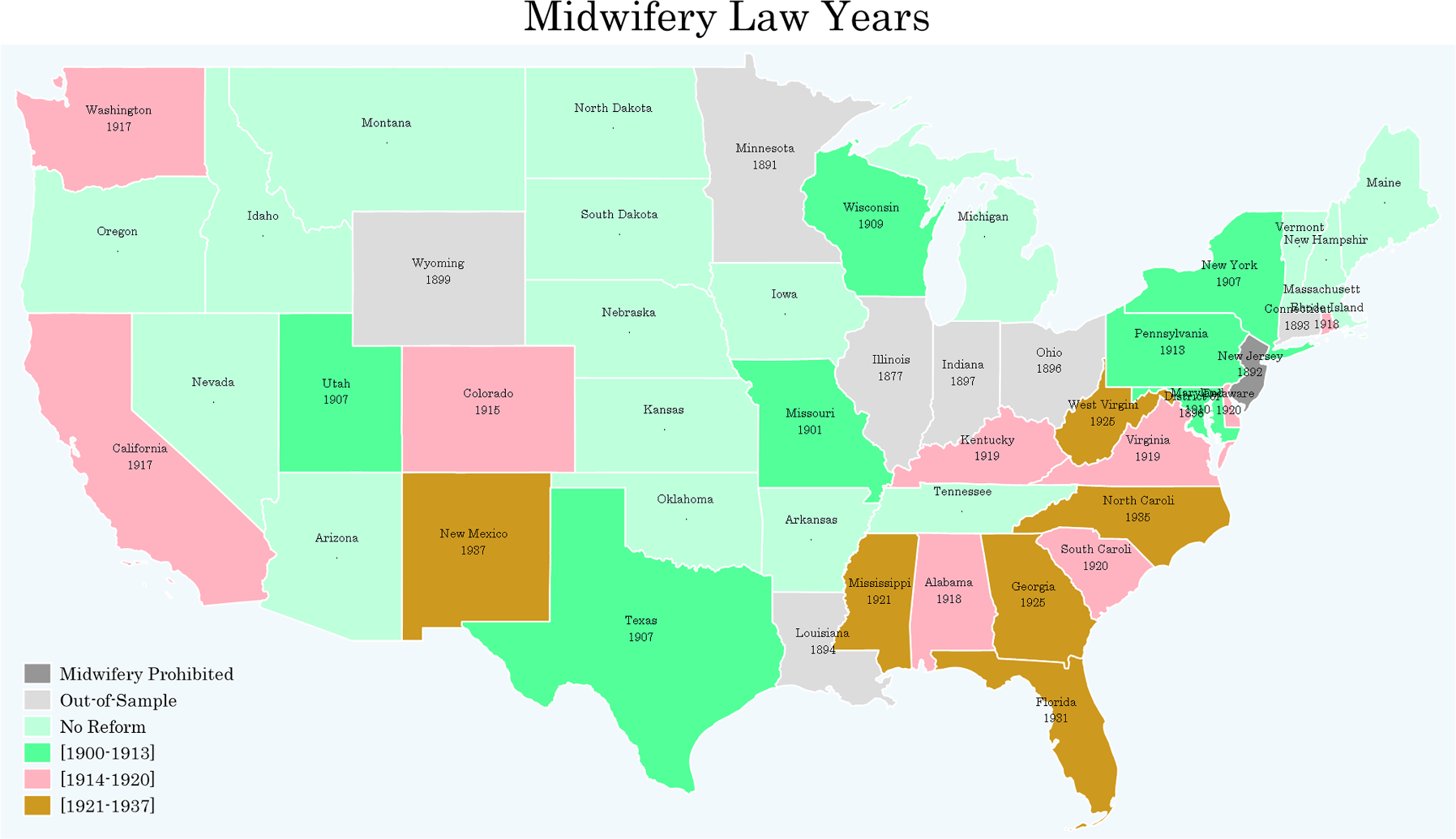
Midwifery Law Year across States.
The regulation of midwives was not uniform across states. For instance, under the California Midwifery Act of 1917, midwives were required to complete a training program covering anatomy, physiology, obstetrics, and hygiene topics. They were also required to pass an examination demonstrating their knowledge and skills in these areas. The 1907 midwifery law of New York established minimum age requirements for midwifery licensure applicants. In addition, it mandated that midwives attend a minimum of 20 supervised deliveries before they could be granted a license. While the law in Washington (1917) required applicants to attend 14 months of training from a state-recognized midwifery school, the Mississippi law did not require formal training or passing an exam. In spite of these discrepancies, licensing requirements changed over time, and additional provisions to the baseline midwifery laws made several aspects of these laws more universal, including formal education, training, and knowledge.
3. Literature Review
Empirical research on occupational licensing focus primarily on the supply-side factors and consequences of licensing for the providers and market equilibrium outcomes (Fillmore et al., 2020; Kleiner, 2000, 2017; Kleiner, Discussants, et al., 2016; Kleiner & Krueger, 2010, 2013; Kleiner & Kudrle, 2000; Law & Kim, 2005; Maurizi, 1974; McMichael, 2017; Timmons & Mills, 2018). A narrow strand of research explores the short-run and long-run health impacts of professional medical licensing. For instance, Kleiner & Kudrle (2000) use dental records of Air Force enlistees to examine the effects of licensing stringency on dental health and dental service prices. They find increases in prices and practitioners’ earnings while no effects on dental health outcomes. In a similar study, Kleiner, Marier, et al. (2016) show that more rigid occupational regulations among nurse practitioners increase the price of visits while having no effect on outcomes related to the quality of services.
Several studies suggest that improvements in midwifery training and skills have positive effects on maternal and infant health outcomes. For instance, Homer et al. (2014) estimate that improving midwifery access and quality is associated with reductions in maternal, neonatal, and fetal deaths. They estimate that improving midwifery could save up to 60 percent of maternal and neonatal deaths in countries with the lowest Human Development Index. Anderson et al. (2020) exploit the rollout of midwifery laws across US states over the years 1900–1940 and show that midwifery licensing significantly reduced maternal and infant mortality. Lazuka (2018) employ data from rural Sweden and show that individuals receiving treatment from qualified midwives during birth have lower mortality from cardiovascular diseases and diabetes during adulthood and old age. However, the improvements in health outcomes following a ban on unlicensed practice requires additional elements such as a better quality of healthcare services post laws. Godlonton & Okeke (2016) examine the effects of a ban on informal health providers in Malawi on infants’ health outcomes. They find that the ban reduced the use of informal care and increased the use of formal care services but had no effects on infants’ health. They argue that the quality of formal care services is the main barrier to improving health outcomes.
Midwifery provider quality improvements under state-level licensing regulations could improve life-cycle health outcomes, including mortality and longevity, through several channels. First, the midwives’ role is not limited to birth attendance. They also provide a series of prenatal care to support a healthy pregnancy, including regular check-ups, monitoring the health of the pregnant person and their developing fetus, providing advice on nutrition and exercise, and offering emotional and psychological support (Weisband et al., 2018; Rooks, 1999). Several studies point to the benefits of prenatal care and professional visits during pregnancy on birth outcomes and infants’ health (Camacho & Conover, 2013; Corman et al., 2019; Joyce, 1999). A better health endowment at birth, in turn, affects life-cycle outcomes (Behrman & Rosenzweig, 2004; Black et al., 2007; Cook & Fletcher, 2015; Fletcher, 2011; Maruyama & Heinesen, 2020; Royer, 2009). For instance, Black et al. (2007) employ sibling fixed effects and show that birth weight significantly affects adult height, earnings, and IQ. Fletcher (2011) uses Add Health data and shows that individuals with low birth weight are more likely to have reported learning disabilities and grade repetition. Royer (2009) provides evidence that birth weight is associated with higher years of schooling during adulthood. These early adulthood effects of birth endowment can influence old-age health and longevity. Several strands of research point to the influence of income, education, health, height, and adulthood socioeconomic status on old-age mortality outcomes (Chetty et al., 2016; Crimmins & Finch, 2006; Fletcher et al., 2021; Fletcher, 2015; Lleras-Muney, 2005; Lleras-Muney et al., 2020; Mazumder, 2008; Meghir et al., 2018; Salm, 2011).
The second channel relates the provider quality to a healthy birth delivery and to improvements in postnatal care. Healthier delivery and better early-life care can reduce the likelihood of diseases and improve the health of newborns and their neurocognitive development (McCauley et al., 2022; I. Yang et al., 2016). A growing strand of the literature suggests that early-life disease and general health environment are associated with later-life disease and other health outcomes (Blackwell et al., 2001; Currie et al., 2010; Gluckman et al., 2007; Smith, 2009). For instance, Gensollen et al. (2016) explore the impact of early-life disruptions in microbiota colonization on immune function and the potential long-term health consequences of such disruptions. They highlight the role of microbiota colonization during early life in shaping the development and function of the immune system. They argue that the interaction between the immune system and microbiota plays a crucial role in the establishment of immune tolerance and in protecting against pathogenic infections later in life.
The third channel of impact is through potential gains from reductions in maternal mortality through midwifery quality improvements (Anderson et al., 2020). Maternal death during early-life has short-run and long-run consequences for cognitive development, emotional development, and later-life outcomes of children (Berg et al., 2014; Case & Ardington, 2006; Kes et al., 2015; Rostila & Saarela, 2011; Shenk & Scelza, 2012; Thaddeus & Maine, 1994). Smith & Smith (2010) show that psychological conditions during early-life and childhood are associated with lower educational attainments and labor market earnings during adulthood. Rostila & Saarela (2011) show that parental death, and specifically maternal death, during childhood is associated with higher mortality risks at ages 10–59.
4. Data and Sample Selection
The primary source of data is the death records of the National Center for Health Statistics (NCHS). The NCHS data covers the universe of death records in the US. It reports age at death, cause of death, location of death, and limited demographic information. Starting from 1979, the NCHS also reports the birth-state, an important variable in our analysis. Therefore, we use NCHS death data between the years 1979–2020.5 We remove individuals born in Hawaii and Alaska from the final sample as they entered into the registration area in later years and we do not observe earlier cohorts in these states. We focus on birth cohorts of 1900–1940, so that the oldest and youngest cohorts in our sample are 79 and 39 years old, respectively. This selection avoids the inclusion of very old and very young individuals in our sample. It also allows for considerable cross-state and across-cohort variation in our sample.6
The state-level midwifery law database is extracted from Anderson et al. (2020). Fig. 1 illustrates the timing of midwifery law adoption across states. Several states initiated midwifery laws prior to 1900. These states include Connecticut (1893), Illinois (1877), Indiana (1897), Louisiana (1894), Minnesota (1891), New Jersey (1892), Ohio (1896), and Wyoming (1899). Since our sample starts at cohorts born in 1900, these states are always treated over the sample period. Therefore, a comparison of later-treated cohorts and these already-treated states may bias the OLS estimations (Goodman-Bacon, 2021a). To avoid this issue, we remove those individuals born in these states.7
As covariates in our regressions, we use historical censuses (1900–1940) to extract state-level characteristics in decennial censuses and interpolate linearly for inter-decennial years. The historical census data is extracted from Ruggles et al. (2020).
To explore the effects on cumulative mortality rates, we collapse the NCHS data at the birth-state, birth-year, gender (female/male), and race (white/nonwhite) level. We then calculate the mortality rate using the following formula:
Where indexes gender, race, birth-state, and birth-year. The numerator counts total death to each gender-race-state-year level. The ideal denominator in this equation is the number of alive individuals in 1979 (start of the sample) for each gender-birth-state-birth-cohort group. One potential solution is to use random samples of the decennial censuses, e.g., the 1980 census (Goodman-Bacon, 2021b; Snyder & Evans, 2006). However, using a random sample of individuals could add noise to our population estimates. To address this problem, we use the full-count 1940 census as the baseline estimate of the number of alive people in 1940 at each cell level (i.e., gender-birth-state-birth-cohort group). To account for those who died between 1940 and 1980, we use cohort-level estimates of total people alive in 1980 and 1940. We then calculate the share of each cohort who died from 1940 to 1980.8 We deflate the cell-level population estimates of the 1940 census by this number to obtain an estimate of population for the denominator .9 Finally, we use the log of this ratio as the primary outcome in our analyses.
Summary statistics of the final samples are reported in two panels of Table 1. The full NCHS sample covers roughly 48M death records. Using the 1980 census, we estimate that those born between 1900–1940 in states covered in the final sample who survived to 1980 (around the start of NCHS coverage) to be about 56.3M persons. Therefore, our sample covers about 86 percent of the original population. In the final sample, about 21M (43.5%) were born in states and years that had established a midwifery licensing law. Among exposed (unexposed) people, 49 (54) percent are females, and 88 (88) percent are whites. The average age at death among exposed and unexposed cohorts is 76.3 and 79.9 years, respectively.10 Exposed cohorts have lower longevity since they are more likely to belong to later birth cohorts and be underrepresented in the death window of 1979–2020. However, the cumulative mortality rates of both subsamples are more similar (bottom panel of Table 1). The rates for exposed and unexposed cohorts are 60K and 66K per 100K of the original population.
Table 1.
Summary Statistics.
| Exposed to Midwifery Laws | Non-Exposed to Midwifery Laws | |||
|---|---|---|---|---|
|
|
|
|||
| Mean | SD | Mean | SD | |
|
| ||||
| Female | .49 | .5 | .54 | .5 |
| White | .88 | .32 | .88 | .33 |
| Black | .11 | .31 | .12 | .32 |
| Other Races | 0 | .07 | .01 | .08 |
| Birth Year | 1926.29 | 7.99 | 1917.14 | 10.18 |
| Death Year | 2002.57 | 11.11 | 1997.08 | 11.03 |
| Death Age | 76.27 | 11.16 | 79.94 | 10.07 |
| Observations | 21036529 | 27215338 | ||
| NCHS Collapsed at Birth-State-Year and Race-Gender Level (Death Years 1979–2020): | ||||
| Female | .5 | .5 | .5 | .5 |
| White | .5 | .5 | .51 | .5 |
| Black | .39 | .45 | .31 | .42 |
| Other Race | .11 | .26 | .18 | .33 |
| Birth Year | 1930.86 | 6.75 | 1917.48 | 11.26 |
| Log Mortality Rate | 10.97 | .32 | 11.1 | .43 |
| Mortality Rate (per 100,000) | 59949.12 | 17545.31 | 66975.34 | 21873.41 |
| Birth-State-Year Covariates: | ||||
| Population (1,000) | 3649.49 | 3307.98 | 1679.43 | 1561.25 |
| Share of Homeowners | .47 | .1 | .5 | .1 |
| Share of Children less than 5 | .37 | .09 | .47 | .12 |
| Share of Immigrants | .1 | .08 | .12 | .09 |
| Share of White-Collar Occupations | .04 | .01 | .03 | .01 |
| Share of Farmers | .17 | .11 | .27 | .15 |
| Share of Other Occupations | .78 | .11 | .7 | .14 |
| Share of Literate | .64 | .34 | .84 | .22 |
| Share of Married | .61 | .02 | .59 | .03 |
| Female Labor Force Participation Rate | .26 | .05 | .21 | .09 |
| Socioeconomic Index | 27.53 | 3.69 | 23.59 | 3.98 |
| Observations | 1,284 | 5,131 | ||
Fig. 2 shows the geographic distribution of mortality and longevity across states.
Fig. 2.
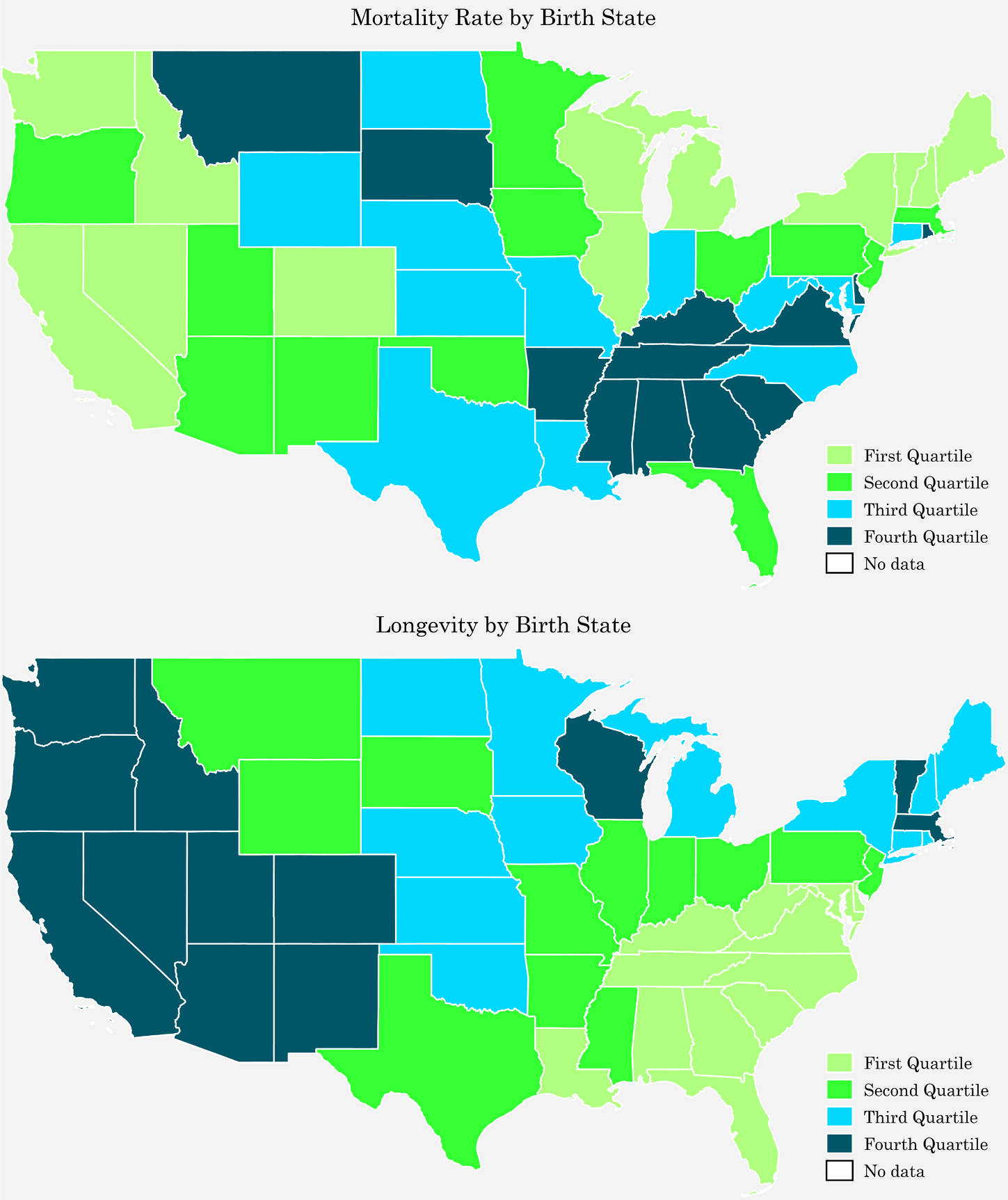
Geographic Distribution of Mortality and Longevity by Birth States in the NCHS Mortality Data (Death Years 1979–2020).
Fig. 3 shows the density distribution of longevity and cumulative mortality rate in the top and bottom panels, respectively.
Fig. 3.
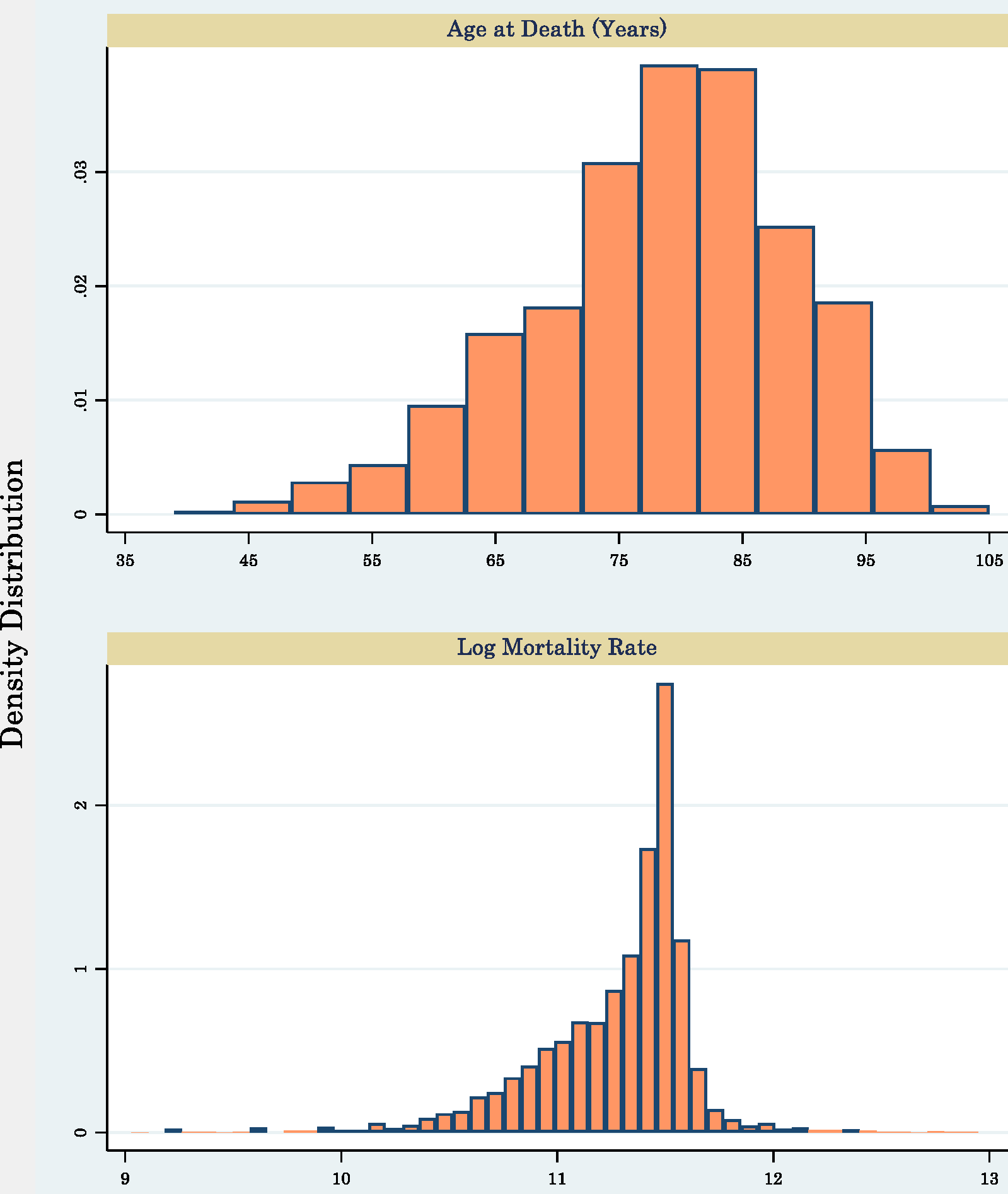
Density Distribution of Mortality and Longevity in the NCHS Mortality Data (Death Years 1979–2020).
For the analyses of mechanism channels, we use an alternative mortality database. We employ Death Master Files (DMF) data extracted from Goldstein et al. (2021). The DMF is the Social Security Administration death records covering the years 1975–2005. The advantage of the DMF data is its link to the full-count 1940 census at the individual level. Therefore, we are able to observe individual and family characteristics for a portion of cohorts in our main analysis, which we use to examine the potential effects of midwifery laws on educational and other socioeconomic outcomes. Moreover, a subsample of the DMF data is linked to the World War II enlistment data. The enlistment data reports limited anthropometric outcomes. We use height and height-for-age as mediatory outcomes to explain the impacts of midwifery on early-adulthood health. For further exploring the mechanisms, we employ the 1980 census and examine the effects on education, income, and disability. Table 2 reports summary statistics of the DMF and 1980 census. The DMF data overrepresents whites (93%) and underrepresents blacks (7%) relative to the original population and relative to the NCHS death population. However, Breen & Osborne (2022) show that despite this differential representation, each subpopulation fairly represents its original demographic population (of 1940 census) regarding socioeconomic characteristics. The average age at death among exposed and unexposed cohorts have 69.5 and 75.1 years, respectively. While both cohorts of WWII enlistees have similar height, the average height-for-age is slightly larger among exposed cohorts. Based on 1980 census data, work disability among exposed (unexposed) cohorts is 14 (24) percent.
Table 2.
Summary Statistics for Mechanism Analysis.
| Exposed to Midwifery Laws | Non-Exposed to Midwifery Laws | |||
|---|---|---|---|---|
|
|
|
|||
| Mean | SD | Mean | SD | |
|
| ||||
| White | .93 | .26 | .92 | .26 |
| Black | .07 | .25 | .07 | .26 |
| Birth Year | 1922.75 | 8.33 | 1914.16 | 9.51 |
| Death Year | 1992.76 | 8.56 | 1989.78 | 8.57 |
| Death Age | 69.5 | 10.45 | 75.09 | 10.09 |
| Socioeconomic Index | 26.35 | 20.22 | 26.99 | 21.5 |
| Years of Schooling | 9.87 | 2.87 | 9.47 | 3.29 |
| Education < High School | .34 | .47 | .44 | .5 |
| Education < 12 | .66 | .47 | .67 | .47 |
| Education College-More | .11 | .31 | .12 | .33 |
| Migrant (Birth-State Different than 1940-State) | .16 | .37 | .27 | .45 |
| Observations | 2045047 | 2827817 | ||
| Birth Year | 1917.97 | 3.77 | 1914.39 | 5.87 |
| Age | 22.03 | 3.77 | 25.61 | 5.87 |
| Height | 68.01 | 2.32 | 68.03 | 2.32 |
| Log Height | 4.22 | .03 | 4.22 | .03 |
| Height-for-Age | 3.17 | .53 | 2.8 | .63 |
| Log Height-for-Age | 1.11 | .18 | .96 | .24 |
| Observations | 219833 | 253792 | ||
| Employed | .65 | .48 | .46 | .5 |
| Log Total Personal Income | 9.13 | 1.12 | 8.9 | 1.09 |
| Log Household Income | 9.88 | .81 | 9.65 | .88 |
| Log House Value | 10.76 | .73 | 10.67 | .74 |
| Education < High School | .15 | .36 | .25 | .43 |
| Work Disability | .14 | .35 | .24 | .43 |
| Observations | 1765130 | 2644312 | ||
5. Empirical Method
The identification strategy exploits the staggered adoption of midwifery laws across states and over the years. We implement a difference-in-difference method to compare the cumulative mortality rate of cohorts born in different years relative to the state-specific year of the midwifery law change. Specifically, we operationalize this comparison using the following event-study formulation:
| (1) |
The outcome is the natural logarithm of cumulative mortality rate over the years 1979–2020 for cohorts born in state year in census region who belong to gender group and race group . The function equals one if the argument is one and zero otherwise. The parameters and represent negative and positive event time dummies which measure the distance between birth year and state-specific midwifery law establishment. In , we include birth state-year covariates using historical decennial censuses 1900–1940 and linearly interpolate for inter-decennial years.11 These covariates include the share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. The parameters and represent gender and race dummies. The matrix represents birth-year by region-of-birth fixed effects to control for cross-cohort differences in mortality across census regions. We control for all unobserved time-invariant characteristics of birth-states by adding state fixed effects . We also include a state-specific trend in birth cohorts in our preferred specifications to account for linear evolution in states’ unobserved characteristics. is a disturbance term. We use the birth-state population to weight the regressions. We cluster standard errors at the birth-state level to account for serial correlation in error terms and at the birth-year level to account for spatial correlations.12
In addition to the event-study, we report the difference-in-difference estimates in which the main independent variable measures the exposure to midwifery law at birth year, as follows:
| (2) |
The parameter is a dummy that equals one if the state had an established midwifery law in year-of-birth . All other parameters are as in equation 1. Therefore, in these models, the main parameter of interest is which shows the association between being born under a midwifery licensing regime (versus being born in state-years without any licensing regime) and mortality rates.
To explore the effects on longevity, we use individual-level NCHS data and implement similar difference-in-difference and event-study analyses to compare the longevity of individuals who were born in different years relative to the state-specific year of midwifery law change. These regressions include the same set of covariates, fixed effects, and trends as in equations 1 and 2.
6. Results
6.1. Event-Study Results
We start the results by showing the event study results of equation 1. The advantage of the event-study is its transparency in showing the evolution of coefficients in different years relative to midwifery reforms. It also allows us to examine whether the results are an artifact of preexisting trends in mortality and longevity. The event study results for log cumulative mortality rate are reported in the top panel of Fig. 4. The small and insignificant pre-event coefficients rule out the concerns over preexisting trends in mortality rates. Post-midwifery laws, the coefficients rise (in magnitude). The point estimates become statistically different from zero for the subset of cohorts born 7-and-more years after the law change.
Fig. 4.
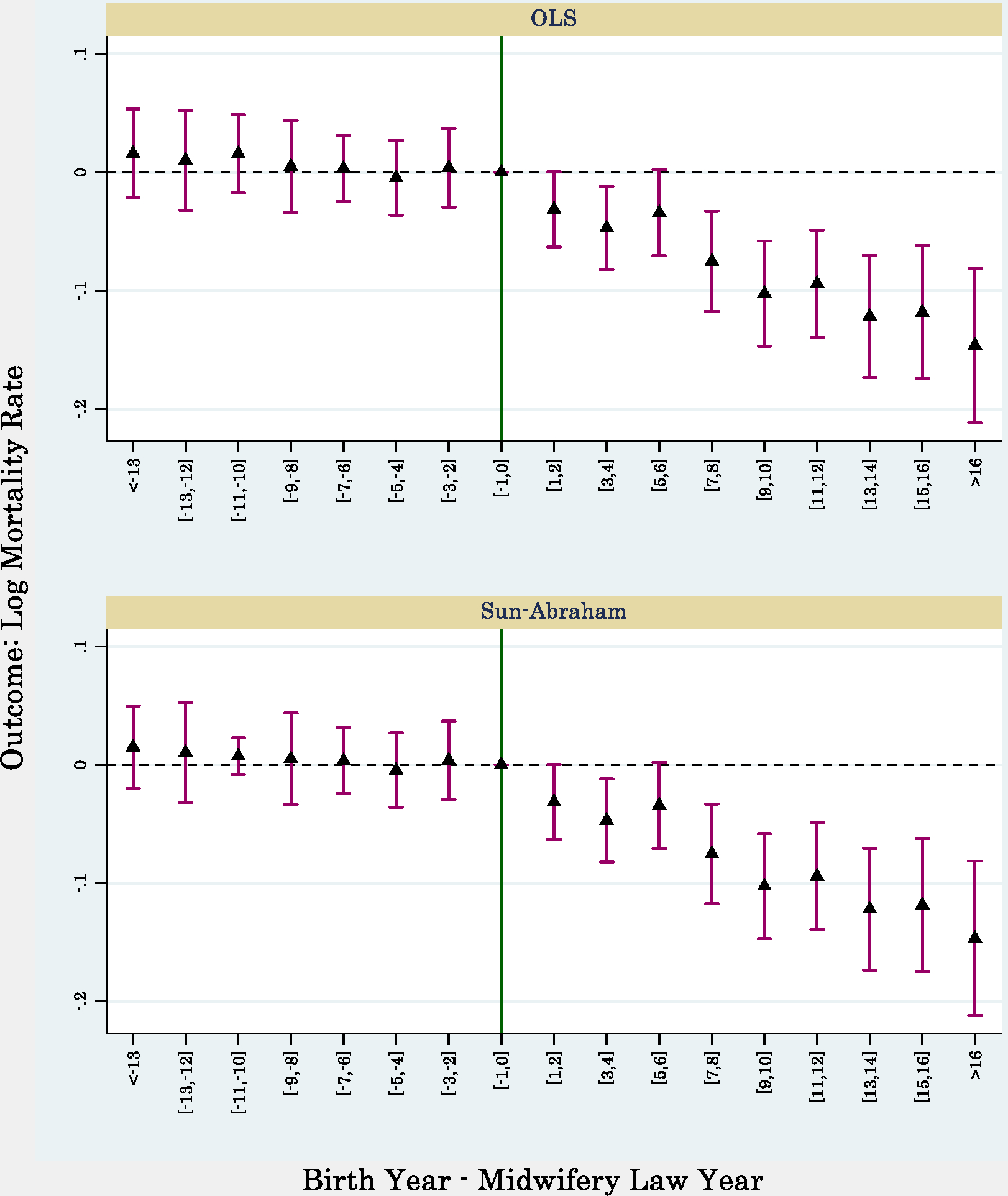
Event-Study to Explore the Effects of Midwifery Law Enactment on Mortality Rate.
Notes. Point estimates and 95 percent confidence intervals are depicted. Standard errors are clustered at birth-state-year level. Regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, and birth-state covariates. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population. The data comes from NCHS death records collapsed at birth-state-year and gender-race level for death years of 1979–2020.
N=6,415
Since the adoption of laws across states has a staggered adoption, it raises concerns regarding the bias produced by ordinary least square regressions as a result of comparing states that received the treatment at different points of time (Callaway & Sant’Anna, 2021; Goodman-Bacon, 2021a; Sun & Abraham, 2021). To show the robustness to alternative estimators, we use the methodology developed by Sun & Abraham (2021) and replicate the event-study analysis. The results, reported in the bottom panel of Fig. 4, provide the same pattern of effects as those produced by OLS.13
In Fig. 5, we replicate the event-study using longevity as the outcome and employing the individual-level NCHS data. While the results do not point to discernible evidence of preexisting longevity trends, the coefficients rise and become significant for post-reform cohorts.
Fig. 5.
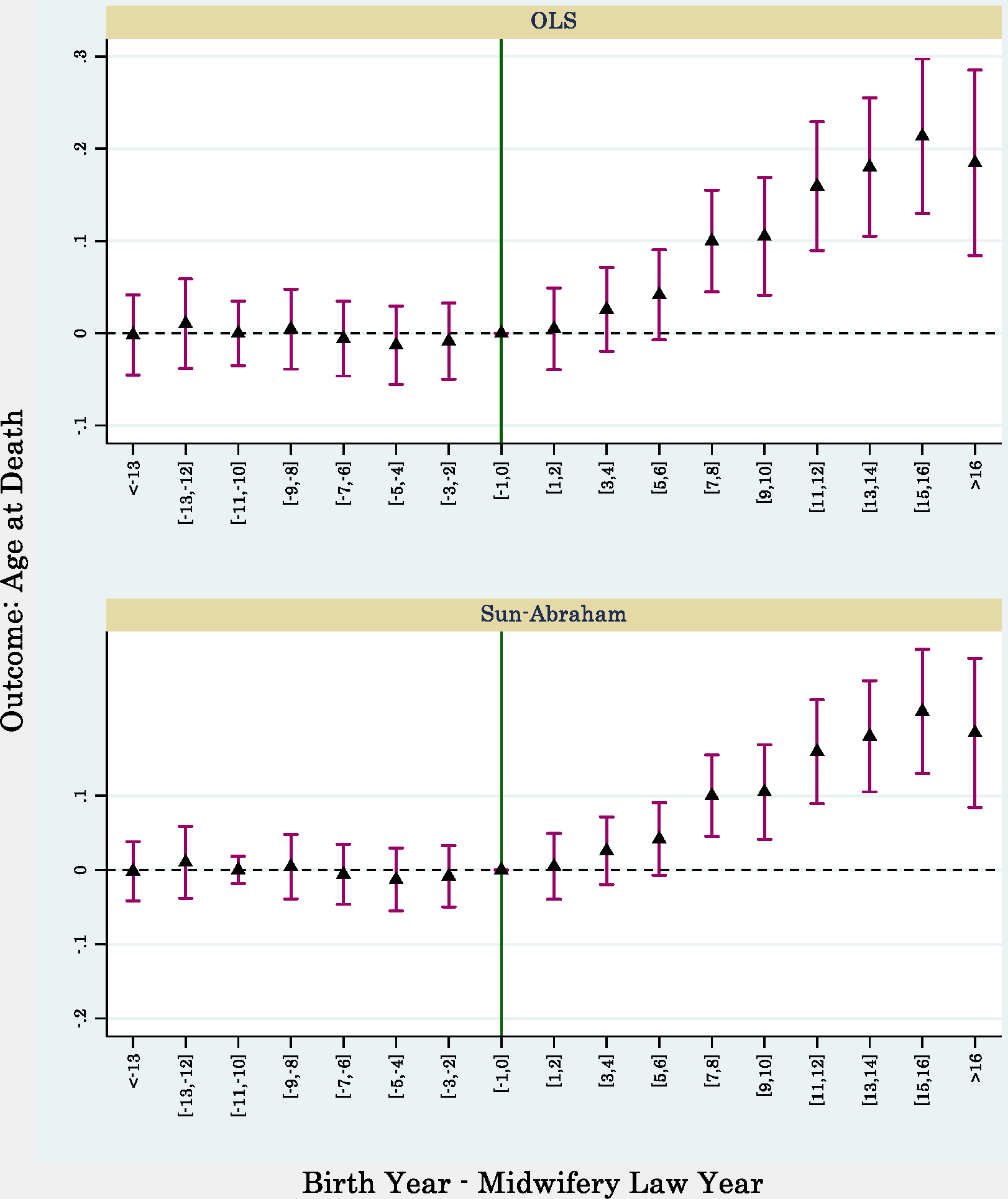
Event-Study to Explore the Effects of Midwifery Law Enactment on Longevity.
Notes. Point estimates and 95 percent confidence intervals are depicted. Standard errors are clustered at birth-state-year level. Regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, and birth-state covariates. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population. The data comes from NCHS death records at the individual level for death years of 1979–2020.
N=48,251,867
These event studies are in-line with the results of Anderson et al. (2020) that explore the effects of midwifery laws on contemporaneous maternal and infant mortality rates. One conspicuous difference is that the event-study of maternal mortality reported by Anderson et al. (2020) suggests relatively stable and flat post-trend coefficients for maternal mortality while both event studies of Fig. 4 and Fig. 5 provide post-trend point estimates that grow in size as we move further from the law change year. We should note that reductions in maternal mortality are only one possible channel of impact as we discuss further in section 6.6. General improvements in health-related knowledge of midwives which leads to improvements in prenatal and postnatal care are other channels that arguably grow over time and lends to the observed reduced-form estimates in our event studies.
6.2. Difference-in-Difference Results of Mortality Rates
The results of difference-in-difference regressions introduced in equation 2 are reported in Table 3. We add more covariates to the model across consecutive columns. The fully parametrized model of column 3 suggests that being born under the midwifery licensing regime is associated with a 2.5 percent reduction in cumulative mortality rates during adulthood and old age.14 This is in line with the findings of Lazuka (2018) that shows about 7 percent lower risks of mortality for those who received treatment from qualified midwives at birth.
Table 3.
Exposure to Midwifery Laws at Birth and Later-Life Old-Age Mortality.
| Outcome: Log Mortality Rate | |||
|---|---|---|---|
|
|
|||
| (1) | (2) | (3) | |
|
| |||
| Exposed to Midwifery Law at Birth | −.0256*** (.0094) | −.0348*** (.0104) | −.0246** (.0099) |
| Observations | 6415 | 6415 | 6415 |
| R-squared | .5687 | .5782 | .598 |
| Mean DV | 11.076 | 11.076 | 11.076 |
| Birth-State FE | ✓ | ✓ | ✓ |
| Birth-Year FE | ✓ | ✓ | ✓ |
| Birth-State Controls | ✓ | ✓ | ✓ |
| Individual Controls | ✓ | ✓ | ✓ |
| Region-of-Birth by Birth-Year FE | ✓ | ✓ | |
| Birth-State Trend | ✓ | ||
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
To have an understanding of the magnitude of the effects, we can compare them with other studies in similar settings and data. Goodman-Bacon (2021b) explores the later-life mortality effects of Medicaid introduction during the 1960s using the NCHS death records. He finds that Medicaid eligibility during early-life is associated with 10–14 percent lower cumulative mortality rates. The introduction of Medicaid was a large social program that provided insurance access to a largely uninsured population. The fact that the effects of midwifery licensing are about 18–25 percent of the later-life effect of Medicaid points to the economically meaningful impacts of these laws.
6.3. Heterogeneity Analysis
Table 4 reports the results by cause of death.15 We find significant and relatively larger effects for mortality due to tuberculosis, syphilis, other infectious diseases, neoplasm diseases, and all other diseases. Nonetheless, the impacts are negative across all non-external causes. We find very small and insignificant effects on deaths due to external causes. These are primarily injury-based with undetermined intent events which lead to death. Therefore, the coefficient of column 7 can be interpreted as a placebo test, which shows no effect on deaths that should not have been impacted by midwifery interventions.
Table 4.
Exposure to Midwifery Laws at Birth and Later-Life Old-Age Mortality by Cause-of-Death
| Outcome: Log Mortality Rate, Cause: | ||||||||
|---|---|---|---|---|---|---|---|---|
|
|
||||||||
| TB, Syphilis Other Infectious Diseases | Neoplasm Diseases | Diabetes | Cardiovascular Diseases | Influenza, Pneumonia, Peptic Ulcer, Nephritis | All other Diseases | External Causes | Suicide | |
|
| ||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | |
| Exposed to Midwifery Law at Birth | −.03618** (.01809) | −.02341* (.01292) | .01099 (.01601) | −.00486 (.01245) | −.00973 (.01386) | −.02427* (.01429) | .00889 (.01993) | −.06313* (.03646) |
| Observations | 5744 | 6370 | 6224 | 6402 | 6344 | 6358 | 6074 | 4836 |
| R-squared | .7178 | .61754 | .70348 | .73287 | .58864 | .56227 | .55252 | .82741 |
| Mean DV | 6.217 | 9.605 | 8.042 | 10.173 | 8.841 | 9.158 | 7.333 | 5.276 |
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. All regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, and birth-state covariates. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
These effects are expected based on studies that point to the relevance of hygiene and early-life disease environment to improve the immune system of newborns, which helps them against diseases in later life (Arrieta et al., 2014; Case & Paxson, 2009; Gensollen et al., 2016; Gluckman et al., 2008). Moreover, Anderson et al. (2020) document a larger effect of midwifery laws on infant mortality rates due to diarrhea diseases. Contraction of diarrhea during childhood may weaken the overall immune system which leaves individuals vulnerable to other infectious diseases later in life, as we observe in column 1 (Ochoa et al., 2004).
Interestingly, we observe the largest effect on suicide mortality. One possible explanation is that midwifery licensing resulted in reductions in maternal mortality. Parental loss during early life could influence mental health across the life-cycle. This evidence is also in-line with several studies in sociology and psychology that parental death during childhood is associated with adverse mental health during adulthood (Luecken & Roubinov, 2012; Stikkelbroek et al., 2012).16
In Table 5, we explore the heterogeneity by race and gender as studies document the heterogenous effects of occupational licensing across different sociodemographic populations (Blair & Chung, 2019, 2022; Law & Marks, 2009).17 We observe a positive coefficient among whites. However, the effect is small in magnitude, representing a 0.3 percent change and statistically insignificant. We observe a large, negative, and statistically significant effect among nonwhites, suggesting a drop of about 4.5 percent. This heterogeneity is also in-line with the larger effects of midwifery on maternal and infant death among blacks found by Anderson et al. (2020).18 Another reason for this observed heterogeneity is the difference in the share of births that are delivered by midwives. For instance, Jacobson (1956) shows that in 1940 about 64 percent of births among nonwhites were delivered by midwives while this number is roughly 5 percent among whites. Therefore, the dosage of treatment is much larger among nonwhites and there is no surprise to observe larger effects of midwifery laws. Moreover, the larger effects on males are in line with studies that suggest larger effects of early-life exposures on later-life outcomes among males (Lindeboom et al., 2010; Noghanibehambari & Engelman, 2022; Scholte et al., 2015).
Table 5.
Heterogeneity in the Effects of Exposure to Midwifery Laws at Birth and Later-Life Old-Age Mortality
| Outcome: Log Mortality Rate, Subsamples | ||||
|---|---|---|---|---|
|
|
||||
| Whites (1) |
Nonwhites (2) |
Females (3) |
Males (4) |
|
|
| ||||
| Exposed to Midwifery Law at Birth | .00358 (.0048) | −.04472** (.02032) | −.00016 (.01345) | −.04695*** (.01447) |
| Observations | 3280 | 3135 | 3216 | 3199 |
| R-squared | .9438 | .67888 | .6852 | .54252 |
| Mean DV | 11.136 | 11.015 | 11.013 | 11.139 |
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. All regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, and birth-state covariates. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
Moreover, the effects are significant only among males. In addition, in Appendix E., we show that the effects are more pronounced for individuals who were born in states with higher per capita midwives. This evidence also supports the claim that the impacts are driven by changes in midwifery quality rather than alternative explanations.
6.4. Results of Longevity
To complement the analysis of cumulative mortality rates, we use individual-level NCHS data and look at an alternative outcome, longevity. We report the difference-in-difference results in Table 6. In column 1, we report the results with birth-state fixed effects, birth-year fixed effects, and individual and state controls. In column 2, we add region-by-birth-year fixed effects. In column 3, we add a birth-state linear trend in birth-year. The results of the full model suggest an increase of about 0.06 years, equivalent to 0.7 months, higher longevity due to exposure to midwifery laws at birth. In Appendix H., we use two alternative difference-in-difference estimator to re-evaluate thiseffect. The results of De Chaisemartin & D’haultfoeuille (2020) suggest quite comparable effect of 0.6 months and the Callaway & Sant’Anna (2021) estimate points to a considerably larger effceect of 1.3 months.
Table 6.
Exposure to Midwifery Laws at Birth and Later-Life Old-Age Longevity
| Outcome: Age at Death (Years) | |||
|---|---|---|---|
|
|
|||
| (1) | (2) | (3) | |
|
| |||
| Exposed to Midwifery Law at Birth | .11096*** (.01639) | .10393*** (.01627) | .06026*** (.01453) |
| Observations | 48251867 | 48251867 | 48251867 |
| R-squared | .18379 | .21182 | .21184 |
| Mean DV | 78.344 | 78.344 | 78.344 |
| Birth-State FE | ✓ | ✓ | ✓ |
| Birth-Year FE | ✓ | ✓ | ✓ |
| Individual Controls | ✓ | ✓ | ✓ |
| Birth-State Controls | ✓ | ✓ | ✓ |
| Region-of-Birth by Birth-Year FE | ✓ | ✓ | |
| Birth-State Trend | ✓ | ||
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
To understand the magnitude of this intent-to-treat effect, we can compare it with other studies and early-life exposures. For instance, Noghanibehambari & Fletcher (2022) explore the early-life exposure to the Dust Bowl of the 1930s as an environmental disaster that resulted in a large and long-lasting drop in agricultural production and find intent-to-treat effects of about 1-month reductions in longevity. Therefore, the positive impact of midwifery quality improvements under the licensing requirements is about 60 percent of the negative effects of the Dust Bowl. Aizer et al. (2016) examine the effects of the Mothers’ Pension (MP) program, a cash transfer initiative for single mothers that was administered by the government from 1911 to 1935, on longevity in later life. The program typically lasted for three years and provided single mothers with approximately 29–39% of their income. By comparing the outcomes of children whose mothers were accepted into the program with those who were rejected, they find that children whose mothers were accepted into the program experienced an increase in old-age longevity of approximately 11.6 months. Therefore, the intent-to-treat effect of midwifery laws is about 6 percent of treatment-on-treated effects of a relatively large increase in single-poor mothers’ income due to the MP.
6.5. Concerns over Endogenous Licensing Adoption
The main argument regarding the exogeneity of our method is that the licensing reforms are orthogonal to other determinants of infants’ and mothers’ health outcomes. This assumption could be violated in several ways, which we discuss below. The midwifery policy change could be a provision of a series of other reforms that occur before or after the law change and could confound the longevity equations. Moreover, there could be contemporaneous changes in state-level characteristics prior to or following law changes and the results might pick up on those characteristics rather than midwifery laws. In Appendix I., we empirically investigate these sources of endogeneity using decennial full-count censuses 1900–1940 and a series of other state-level policy data. We fail to find consistent and significant effects for a wide array of state-level outcomes.
Another concern to consider is the effects of midwifery laws on the number of nursing and selection into nursing (Bae & Timmons, 2022; Markowitz et al., 2017; Shakya et al., 2022; Yang et al., 2016).19 Similarly, midwifery laws could only reflect recent state-level changes in the number of nurses and other related professionals and be a response to this secular trend. Therefore, our results may pick up on the effects of those secular changes rather than the policy reforms. In Appendix Figure L2, we show that there is no clear pattern of changes in County Health Departments openings, physicians per capita, and nurses per capita. However, there is a small reduction (about 0.2 midwives per 10,000 women aged 15–45, off a mean of 2.8).
Another concern regarding the endogeneity of the results is nonrandom changes in the sociodemographic composition of the final sample. This endogenous change could result from migration before and after the reforms in response to the reforms. It also could stem from differential fertility or survival during adulthood.20 For instance, if the benefits of midwifery are specific to blacks, and the higher survival of black people into old age and to the final sample results in an overrepresentation of blacks, the results of midwifery-longevity may underestimate the true effects as the longevity of blacks falls below non-black population for many unobservable reasons. We test for this source of concern using an event-study design similar to equation 1, except that the outcome is individual characteristics, such as race and gender dummies, rather than mortality rate. These regressions include birth-state fixed effects, region-by-birth-year fixed effects, and a birth-state trend. We report the results in Fig. 6. We do not observe significant pre-event or post-event changes in individual characteristics. The point estimates are small in magnitude and statistically insignificant.
Fig. 6.
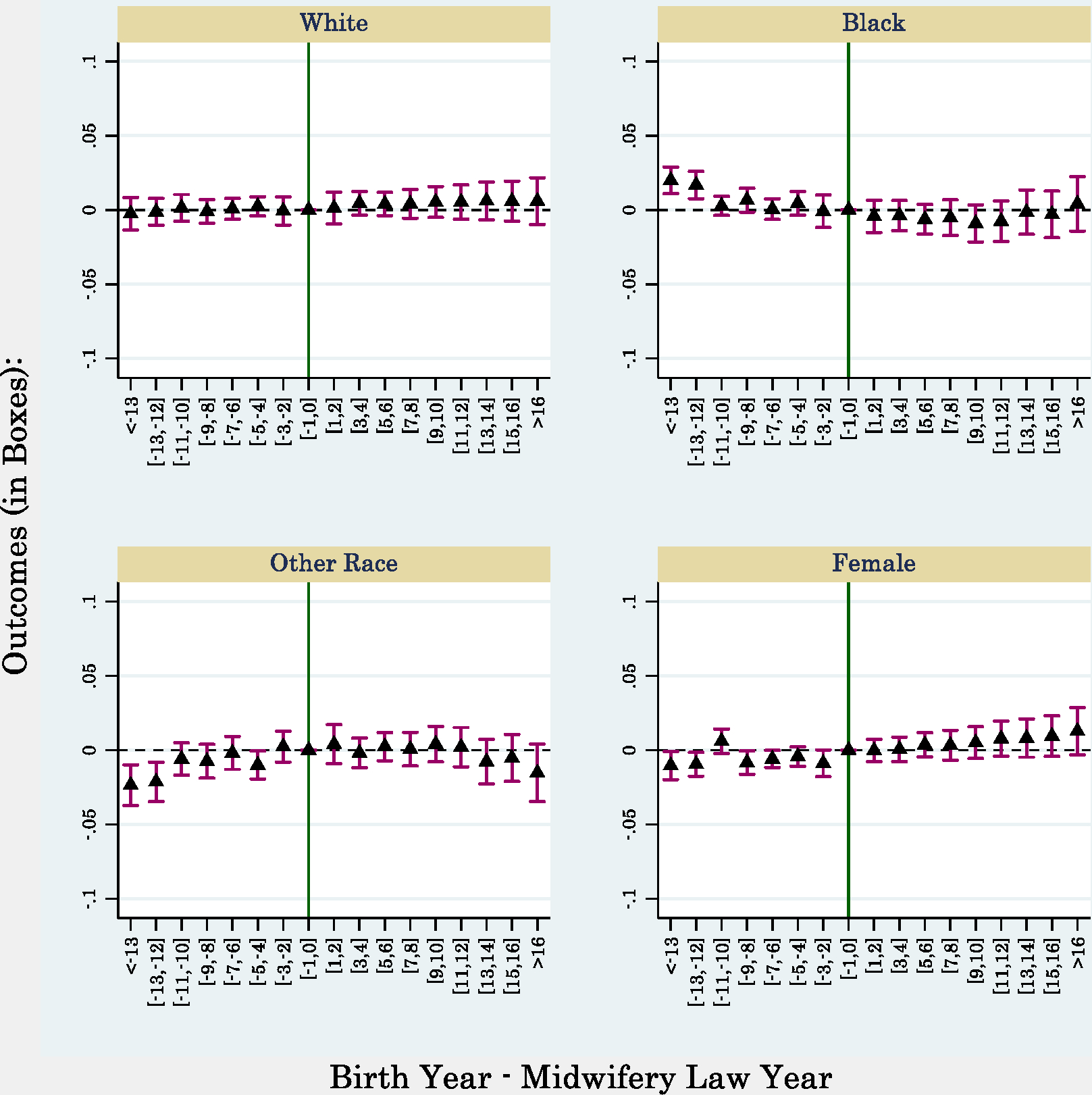
Balancing Test Event-Study to Explore Changes in the Sample Demographic Composition before and after Midwifery Law Enactment.
Notes. Point estimates and 95 percent confidence intervals are depicted. Regressions include state fixed effects, year-by-region fixed effects, and a state-specific trend. Regressions are weighted using state-level population. The data comes from NCHS death records collapsed at birth-state-year and gender-race level for death years of 1979–2020.
N=6,415
6.6. Potential Mechanisms
We use several alternative data sources to explore the mechanism channels. First, we use DMF data linked to the 1940 full-count census to explore several early-adulthood outcomes.21 We implement the full specification of equation 2 and report the results in columns 1–7 of Table 7.22 We should note that the analysis sample of these columns is restricted to cohorts at least 17 years old in 1940. In column 1, we explore the effect on age-at-death and find increases of about 0.11 years. This effect is larger than that of NCHS death records. This could partly be the result of a different death window of DMF (1975–2005) compared with the NCHS data (1979–2020). Column 2 suggests an increase of 0.48 units in the socioeconomic status score, off a mean of 26.8. To exploit the information on family characteristics in 1940 available in the DMF, we explore the heterogeneity by race and maternal education. We report and discuss these results in Appendix D. We find marginal effects on longevity that are 2.8 times larger among children of low-educated mothers compared with those of high-educated mothers. We also observe an effect on nonwhites that is 5.5 times larger than the coefficient we find in the whites sample.
Table 7.
Exploring Mechanism Channels Using DMF Data
| DMF Data (Death Years 1975–2005), Outcomes: | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Age at Death (Years) | Socioeconomic Index | Years of Schooling | Education < High School | Education < 12 Years | Education: College-More | Migrant (Birth-State different than 1940-State) | Being in the WWII Enlistment Data | Height (inch) | Log Height-for-Age | |
|
| ||||||||||
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) | (9) | (10) | |
| Exposed to Midwifery Law at Birth | .10575*** (.01911) | .48052*** (.09524) | .04777*** (.01431) | −.00382 (.0024) | −.00754*** (.0026) | .00523*** (.00157) | −.00327* (.00191) | .00587*** (.00149) | .02331* (.01408) | .00037* (.00022) |
| Observations | 4870650 | 2887115 | 3492378 | 3564529 | 3564529 | 3564529 | 3564529 | 4870650 | 364620 | 364620 |
| R-squared | .42083 | .11969 | .19073 | .13307 | .12774 | .06944 | .09172 | .11234 | .01878 | .98861 |
| Mean DV | 72.743 | 26.800 | 9.607 | 0.405 | 0.667 | 0.116 | 0.237 | 0.097 | 67.786 | 1.027 |
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. All regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, family controls, and birth-state covariates. Individual controls include dummies for race and ethnicity. Family controls include dummies for maternal education and paternal socioeconomic status. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
Column 3 reports the results of years of schooling. Midwifery law exposure at birth raises schooling by about 0.05 years, off a baseline of 9.6 years. Lleras-Muney (2005) examines the education-mortality relationship using state-level compulsory schooling laws as instruments for education. She finds that an additional year of schooling decreases the 10-year cumulative mortality rate by about 3.6 percentage-points, off a mean of 0.11. Based on her findings and the effects of column 3, one can expect a roughly 1.6 percent reduction in mortality rate if one assumes that education is the sole mechanism. This is equivalent to 63 percent of the effects of Table 3.23 Columns 4–5 show reductions in the share of low-educated individuals due to midwifery exposure at birth. We also find 52 basis-points increases in the likelihood of college education, equivalent to a 4.5 percent rise from the mean. Fletcher & Noghanibehambari (2021) investigate the effects of college openings on education and longevity. They estimate treatment-on-treated impacts of college education on old-age longevity of about 1 year. Therefore, the portion of midwifery effects that can be explained by increases in college education is about 8.6 percent.24
Another outcome of interest is migration considering the studies that point to the influence of migration on health and mortality and their interaction with childhood exposures (Aaronson et al., 2021; Black et al., 2015). We define the outcome as the change in state-of-birth versus state-of-residence in 1940. We find a negative and significant effect on migration (column 7). The estimated coefficient suggests a change of about 1.3 percent.
The second data source is World War II enlistment data linked to the 1940 census and DMF death records. This data is gathered by enlistment enumerators and contain an important measure of the health of enlistees, height.25 Height can be linked to early-life environments, socioeconomic factors, and later-life health outcomes (Bozzoli et al., 2009; Crimmins & Finch, 2006; Deaton, 2007; Deaton & Arora, 2009; Sunder, 2005). In column 8, we find that individuals are more likely to be among the enlistees (compared to other records in DMF-census data) if they were exposed to midwifery laws. In columns 9–10, we find increases in height (in inches) and log of height-for-age. Although the magnitudes of effects are small, they are statistically significant at 10 percent level.26
In Table 8, we explore additional outcomes based on the 5% 1980 census. We focus on 1980 rather than later years as it measures outcomes at the beginning of the NCHS death sample and limits the influence of mortality on selection into the sample. We find evidence of increases in the probability of being employed (column 1), personal income (column 2), and household income (column 3). Although these effects are statistically significant, they point to relatively small changes. Chetty et al. (2016) investigate the relationship between income and longevity using tax and death records from 1999–2014. They find that for every 5 percentiles increase in income, there is a corresponding increase in longevity of around 0.8 years. To use their estimations and calculate the potential longevity gains from the observed rises in income, we also use the household income percentile and use it as the outcome. We find that midwifery exposure at birth is associated with about a 0.25-percentiles increase in household income. Using Chetty et al. (2016)’s estimations, we expect to observe 0.04 years higher longevity. This is about 66 percent of the reduced form effect we find in Table 6.
Table 8.
Exploring Mechanism Channels Using 1980 Census Data
| Outcomes: | |||||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Employed | Log Total Personal Income | Log Household Income | Household Income Percentile | Log House Value | Education < High School | Work Disability | |
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|
| |||||||
| Exposed to Midwifery Law at Birth | .00355** (.00155) | .0059* (.00303) | .00826*** (.00271) | .25593*** (.0926) | .00304 (.00248) | −.00784*** (.00201) | −.00188 (.00135) |
| Observations | 3768281 | 3298054 | 3647761 | 3679768 | 2255675 | 3768281 | 3768281 |
| R-squared | .33826 | .27377 | .21938 | .23327 | .26854 | .17049 | .11711 |
| Mean DV | 0.496 | 8.955 | 9.710 | 48.919 | 10.672 | 0.238 | 0.226 |
Notes. Standard errors, clustered at birth-state-year level, are in parentheses. All regressions include birth-state fixed effects, birth-year by region-of-birth fixed effects, birth-state trend, individual controls, and birth-state covariates. Individual controls include dummies for gender and race. Birth-state controls include share of homeowners, share of children, share of immigrants, share of different occupations, literacy rate, share of married people, female labor force participation rate, and average socioeconomic index. Regressions are weighted using average birth-state population.
p<0.01
p<0.05
p<0.1
We also find positive but insignificant increases in house value (column 5). Consistent with the DMF results of Table 7, we find reductions in the probability of being low-educated (column 6). Finally, we observe small and insignificant reductions in work disability (column 7).
Overall, the results of Table 7 and Table 8 suggest increases in educational attainments and socioeconomic measures as potential pathways. We should acknowledge that these estimates are relatively small in magnitude and economically trivial although large sample sizes result in statistically significant effects. However, it is also the case that these estimates are intent-to-treat effects with potentially larger influence among the treated population and more affected subpopulations as evidence reported in Appendix D. suggests.
6.7. Discussion on the Magnitudes
Our results suggest significant reductions in mortality rate and improvements in longevity as a result of early-life exposure to midwifery licensing regulations. Based on the 1980 census, about 56.2 million people who satisfied our sample selection survived till 1980. On the other end, a reduction of 2.5 percent in cumulative mortality over a 42-year window is equivalent to a 0.059 percent reduction in the annual mortality rate of this population. Therefore, this effect is equivalent to an annual reduction of about 33,158 deaths in the nation.
Jacobson (1956) documents that before World War I about 40 percent of births are delivered by midwives. Assuming the same rate post-WWI, we can do a back-of-an-envelop calculation to reach a treatment-on-treated effect of 1.8 months increase due to exposure to midwifery law change. Across cohorts of the final sample (1900–1940), the life expectancy at age 40 (the minimum age-at-death in the final sample of NCHS data) increased from around 65.5 to 78 years. Therefore, the effect of midwifery law changes can explain about 1.2 percent of overall longevity improvements (conditional on survival up to age 40) during this period.27
Further, we can also use the results on longevity (Table 6) to calculate life-years saved due to the policy reforms. In the final sample, the population of exposed cohorts counts to about 35.7 million persons. Based on this sample and the longevity effects we found, we can estimate 1.8 million life-years saved due to midwifery law changes.
Another way to understand the magnitude of these results is to use Value of Statistical Life (VSL) estimates. Given the difference of about 1.2 years in average age-at-death in the final sample of exposed people and the average longevity of all cohorts born 1900–1940 who died between 1979–2020, and assuming a discount rate of 3 percent, we reach a Value of Statistical Life at age 77 (VSL77) of about $1.8M (Colmer, 2020; Kniesner & Viscusi, 2019; Viscusi, 2018). Using our back-of-the-envelope calculation on life-years saved, we reach a total saving of about $3.24 trillion.
7. Conclusion
During the late 19th and early 20th century, the majority of American women gave birth using traditional birth attendants or midwives’ assistants. Several states initiated licensing requirement regimes for midwives to improve the skills, knowledge, and quality of midwifery services and regulate the market. Under these reforms, midwives were required to attain formal training, education, and experience and comply with a series of hygiene procedures to obtain a midwifery license and be able to practice midwifery legally. Several studies point to the short-run and long-run health benefits of midwifery quality improvements (Anderson et al., 2020; Lazuka, 2018). In this paper, we extended this literature by providing evidence of midwifery reforms’ long-run effects on mortality outcomes.
We exploited the staggered adoption of midwifery laws using event-study and difference-in-difference frameworks. We used the universe of death records in the US over the years 1979–2020 and found that exposure to midwifery licensing law at birth is associated with a 2.5 percent reduction in cumulative mortality rates and an increase of 0.6 months in longevity.
The effects are concentrated on deaths due to infectious diseases, neoplasm diseases, and suicide mortality. We also found that the impacts are confined among blacks and are slightly larger among males. We employed alternative data sources to explore the mechanism channels. We found increases in educational attainments, income, measures of socioeconomic status, employment, and measures of height as mediatory channels. Finally, we discussed the economic significance of the results and the life years saved due to exposure to midwifery laws in early life.
Supplementary Material
Footnotes
The authors claim no conflict of interest. The authors would like to acknowledge financial support from NIA grant R01AG060109 and the Center for Demography of Health and Aging (CDHA) at the University of Wisconsin-Madison under NIA core grant P30 AG17266.
Declaration of Competing Interest
The author claims no conflict of interest.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jhealeco.2023.102807.
In the absence of modern-day hospitals and specialized physicians, midwives were the primary healthcare providers for women during pregnancy and childbirth. Moreover, midwives also provided prenatal care, including advice on nutrition and exercise, as well as postpartum care for both mother and baby. Midwives were trained to detect deviations from normal delivery and provide intervention services in high-risk pregnancies, such as twin births and breech births. The training of midwives was informal and through apprenticeship of new entrants by more experienced midwives. In the late 19th century, midwifery became more regulated. Several states initiated midwifery regulation requiring formal training, education, and experience to obtain a midwifery license.
We should also note that evaluation of adoption of midwifery laws provides a different insight than studies that explore expansions and marginal changes implemented in more recent periods. Going from a completely unregulated regime to a license and training requirement was a big step toward quality improvements. Thus, this policy change is inherently different than many incremental changes in the provisions of license requirements in modern medical services where all professionals have already attained relevant licensing, education, and training. Therefore, studying the effects and consequences of these law changes differs from the literature evaluating modern midwifery laws (Ten Hoope-Bender et al., 2014; Van Lerberghe et al., 2014).
This is more concerning given that in many developing countries, the majority of births are delivered at home with the help of traditional birth attendants and midwives (WHO, 2020). Nonetheless, many midwives lack formal education and training (UNFPA, 2021).
While in the main analysis we include states that passed the law before 1900, we show the robustness of the results to excluding these states in Appendicx B.
In Appendix A, we show the robustness of the results across alternative and more limited death years and death ages.
In the main analysis sample, we do not force a balanced sample. However, in Appendix J, we show that the results are robust if we focus on states with available information in all 41 years of the sample (1900–1940).
In Appendix B, we show the robustness of the results to including those born pre-1900 and these excluded states.
One argument is the noise in alive cohort estimates of the 1980 census. This is the same issue as the cell-level noise concern. However, at more aggregated levels, such as cohort level aggregation, the measurement errors are considerably mitigated.
In Appenix R, we show that the results are robust if we replace the denominator with 1980 population.
Although this difference seems large, it is mainly driven by cross-cohort secular trends in longevity. To show this, we regress age-at-death on an exposure dummy (born in a state with an established midwifery law) and birth-year fixed effects. The coefficient of exposure dummy is 0.093 (se=0.003). Exposed cohorts’ longevity is 0.1 years larger than non-exposed cohorts).
One concern is that within each decade these interpolated covariates are collinear with state trends. Another related concern is the issues that are raised regarding the inclusion of trends and the concern that they induce artificial variation in midwifery law exposures (Chou et al., 2006; Gruber & Frakes, 2006; Meer & West, 2016). In Appendix F, we show that, in the absence of state trends, pre-event coefficients of event studies are slightly larger. Therefore, the combination of covariates and trends absorb the pre-treatment evolution in outcomes and better isolate the treatment effects.
In Appendix C, we show the results of difference-in-difference and event-study for mortality and longevity in regressions that cluster the standard errors at the birth-state level.
In Appendix H, we also show the event-study results based on the estimation strategy proposed by Callaway & Sant’Anna (2021). We find quite similar pattern as the event studies reported in the paper.
In Appendix H, we show the results using alternative difference-in-difference estimates. The results of De Chaisemartin & D’haultfoeuille (2020) suggest quite comparable effect while Callaway & Sant’Anna (2021) estimate suggest much larger impacts. These alternative estimates suggest that the OLS-produced estimates might underestimate the effects and provide a lower bound for the true effects. However, the results of longevity (discussed in section 6.4) are quite robust and similar for alternative estimators compared with the OLS-produced estimates.
In Appendix Q, we illustrate the event studies associated with the mortality results by cause of death reported in this section.
The suicide sample of Table 4 is roughly 75 percent of the full sample. In Appendix I, we show that the mortality effects are smaller when we exclude cells with missing suicide deaths. We also show that the effects in suicide is larger in states with a higher share of urban population, a fact that is consistent with findings of Anderson et al. (2020) for maternal mortality. Moreover, we replicate the event study for suicide death rate and find relatively stable and flat post-trend coefficients, which are again consistent with the event study of Anderson et al. (2020) for maternal mortality.
In Appendix M, we show the event studies of Table 5.
In Appendix E, we also explore the heterogeneity based on the strictness of midwifery laws and share of urban areas in states as Anderson et al. (2020) show higher maternal mortality in urban areas and states with more strict laws. We find relatively larger effects in states with higher share of urban population but do not find a difference between states with more/less strict laws.
For instance, Markowitz et al. (2017) examine the effects of “Scope of Practice” restrictions (regulatory limits for healthcare professionals which defines the scope of their permitted activities as a function of their training, qualifications, and licensure.) for certified nurse midwives on their employment and on maternal and infants’ health. They find small reductions in births delivered by nurse midwives and increases in rates of induced labor. Moreover, policy changes may induce migration which we discuss in Appendix I. For instance, Shakya et al. (2022) explore the impact of Nurse Licensure Compact (NLC) (a policy that allows licensed nurses to practice in the so-called registered compact states) on mobility. They find that relaxing state-specific licensure requirement and allowing to practice in compact states resulted in increases in mobility of registered nurses.
Although the tests in this section is a combination of fertility and survival, we implement more direct tests of fertility in Appendix P. We find no evidence of the effects on birth rate and birth rate to whites and blacks.
The advantage of DMF over NCHS data is that it allows up to observe a wide array of education-socioeconomic measures that are useful for our mechanism section. However, it reports deaths for a much more limited death window (1975–2005) compared with wider death window of NCHS (1979–2020). Moreover, since the NCHS data covers the universe of deaths, we can use the combined death counts to build cumulative mortality rate. The DMF data, on the other hand, does not report all deaths. Not all people who are not in the DMF are alive. This fact limits our scope and we cannot calculate mortality rates based on DMF death counts.
In Appendicx G, we implement event-study-type balancing tests and argue that differential fertility does not affect the sociodemographic composition of the final DMF sample based. Further, in Appendix N, we show the event studies for primary outcomes of DMF analysis of Table 7.
This is calculated using the marginal effect of 3.6 percentage-points and the average mortality rate of 0.11 in (Lleras-Muney, 2005), marginal effect of column 3 of Table 7 (0.047), and marginal effect of column 3 of Table 3 (0.06), as follows: This is calculated as the product of 0.0052 (marginal effect of column 6 of Table 7) and 1 year (Fletcher & Noghanibehambari (2021)’s results) divided by 0.06 (marginal effect of column 3 of Table 6).
In Appendix O, we evaluate the association between successful linking between DMF-Enlistment data and observable individual and family characteristics. We find that relatively advantaged people are more likely to be in the Enlistment data. We should note that that enlistment could also grant better access to health care but we cannot test for these effects directly with the data we have. However, state and cohort fixed effects can account for a significant portion of these confounders and rule out the interpretation that places with midwifery laws also have other health-related influences such as being better at obtaining birth records and recruiting and providing health care. Our econometric setting focuses on cohort specific changes in health as induced by the midwifery laws that control for time invariant place effects.
Another concern about the results of height measures is that the sample of DMF-Enlistment is considerably smaller than that of DMF in columns 1–7. In Appendix K, we replicate columns 1–7 of Table 7 for the DMF-Enlistment sample and find effects that are much smaller in magnitude and statistically insignificant. Therefore, we acknowledge that since we do not observe the general pattern of effects for the DMF-Enlistment sample, we should exercise caution in generalizing the effects on height in Table 7.
We obtain a similar number when we focus on life expectancy at birth. Across cohorts of the final sample (1900–1940), the life expectancy at birth increased from 48.2 years to 62.1 years. Therefore, the effect of midwifery can explain about 1 percent of overall longevity improvements during this period.
We obtain a similar number when we focus on life expectancy at birth. Across cohorts of the final sample (1900–1940), the life expectancy at birth increased from 48.2 years to 62.1 years. Therefore, the effect of midwifery can explain about 1 percent of overall longevity improvements during this period.
References
- Aaronson D, Mazumder B, Sanders SG, Taylor EJ, 2021. Estimating the effect of school quality on mortality in the presence of migration: Evidence from the jim crow south. Journal of Labor Economics 39 (2), 527–558. 10.1086/709783/SUPPL_FILE/17462DATA.ZIP. [DOI] [Google Scholar]
- Aizer A, Eli S, Ferrie J, Muney AL, 2016. The Long-Run Impact of Cash Transfers to Poor Families. American Economic Review 106 (4), 935–971. 10.1257/AER.20140529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almond D, Currie J, 2011a. Human capital development before age five. In: HANDBOOK OF LABOR ECONOMICS, 4. Elsevier. 10.1016/S0169-7218(11)02413-0. [DOI] [Google Scholar]
- Almond D, Currie J, 2011b. Killing Me Softly: The Fetal Origins Hypothesis. Journal of Economic Perspectives 25 (3), 153–172. 10.1257/JEP.25.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Almond D, Currie J, Duque V, 2018. Childhood circumstances and adult outcomes: Act II. Journal of Economic Literature 56 (4), 1360–1446. [Google Scholar]
- Anderson DM, Brown R, Charles KK, Rees DI, 2020. Occupational Licensing and Maternal Health: Evidence from Early Midwifery Laws. Journal of Political Economy 128 (11), 4337–4383. 10.1086/710555. [DOI] [Google Scholar]
- Arrieta MC, Stiemsma LT, Amenyogbe N, Brown E, Finlay B, 2014. The intestinal microbiome in early life: Health and disease. Frontiers in Immunology 5 (AUG), 427. 10.3389/FIMMU.2014.00427/BIBTEX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bae K, Timmons E, 2022. Restrictions on Health Care Profession Scope of Practice: Do They Help or Harm Patients? Upjohn Press Book Chapters; 97–122. 10.17848/9780880996877.Ch6. [DOI] [Google Scholar]
- Barker DJP, 1994. MOTHERS, BABIES, AND DISEASE IN LATER LIFE. BMJ publishing group London. [Google Scholar]
- Barker DJP, 1995. Fetal origins of coronary heart disease. BMJ 311 (6998), 171–174. 10.1136/BMJ.311.6998.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJP, 1997. Maternal nutrition, fetal nutrition, and disease in later life. Nutrition 13 (9), 807–813. 10.1016/S0899-9007(97)00193-7. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Rosenzweig MR, 2004. Returns to birthweight. Review of Economics and Statistics 86 (2), 586–601. 10.1162/003465304323031139. [DOI] [Google Scholar]
- Berg L, Rostila M, Saarela J, Hjern A, 2014. Parental Death During Childhood and Subsequent School Performance. Pediatrics 133 (4), 682–689. 10.1542/PEDS.2013-2771. [DOI] [PubMed] [Google Scholar]
- Black DA, Sanders SG, Taylor EJ, Taylor LJ, 2015. The Impact of the Great Migration on Mortality of African Americans: Evidence from the Deep South. American Economic Review 105 (2), 477–503. 10.1257/AER.20120642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black SE, Devereux PJ, Salvanes KG, 2007. From the cradle to the labor market? The effect of birth weight on adult outcomes. The Quarterly Journal of Economics 122 (1), 409–439. 10.1162/qjec.122.1.409. [DOI] [Google Scholar]
- Blackwell DL, Hayward MD, Crimmins EM, 2001. Does childhood health affect chronic morbidity in later life? Social Science & Medicine 52 (8), 1269–1284. 10.1016/S0277-9536(00)00230-6. [DOI] [PubMed] [Google Scholar]
- Blair PQ, Chung BW, 2019. How Much of Barrier to Entry is Occupational Licensing? British Journal of Industrial Relations 57 (4), 919–943. 10.1111/BJIR.12470. [DOI] [Google Scholar]
- Bleakley H, 2007. Disease and Development: Evidence from Hookworm Eradication in the American South. The Quarterly Journal of Economics 122 (1), 73–117. 10.1162/QJEC.121.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozzoli C, Deaton A, Quintana-Domeque C, 2009. Adult height and childhood disease. Demography 46 (4), 647–669. 10.1353/DEM.0.0079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breen CF, Osborne M, 2022. An Assessment of CenSoc Match Quality. 10.31235/OSF.IO/BJ5MD. [DOI] [Google Scholar]
- Callaway B, Sant’Anna PHC, 2021. Difference-in-Differences with multiple time periods. Journal of Econometrics 225 (2), 200–230. 10.1016/J.JECONOM.2020.12.001. [DOI] [Google Scholar]
- Camacho A, Conover E, 2013. Effects of subsidized health insurance on newborn health in a developing country. Economic Development and Cultural Change 61 (3), 633–658. 10.1086/669263/ASSET/IMAGES/LARGE/FG4.JPEG. [DOI] [Google Scholar]
- Case A, Ardington C, 2006. The impact of parental death on school outcomes: Longitudinal evidence from South Africa. Demography 43 (3), 401–420. 10.1353/DEM.2006.0022. [DOI] [PubMed] [Google Scholar]
- Case A, Paxson C, 2009. Early Life Health and Cognitive Function in Old Age. American Economic Review 99 (2), 104–109. 10.1257/AER.99.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chetty R, Stepner M, Abraham S, Lin S, Scuderi B, Turner N, Bergeron A, Cutler D, 2016. The Association Between Income and Life Expectancy in the United States, 2001–2014. JAMA 315 (16), 1750–1766. 10.1001/JAMA.2016.4226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou SY, Grossman M, Saffer H, 2006. Reply to Jonathan Gruber and Michael Frakes. Journal of Health Economics 25 (2), 389–393. 10.1016/J.JHEALECO.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Colmer J, 2020. What is the meaning of (statistical) life? Benefit–cost analysis in the time of COVID-19. Oxford Review of Economic Policy 36 (Supplement_1), S56–S63. 10.1093/OXREP/GRAA022. [DOI] [Google Scholar]
- Cook CJ, Fletcher JM, 2015. Understanding heterogeneity in the effects of birth weight on adult cognition and wages. Journal of Health Economics 41, 107–116. 10.1016/j.jhealeco.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman H, Dave D, Reichman NE, Corman H, Dave D, Reichman NE, 2019. The Effects of Prenatal Care on Birth Outcomes: Reconciling a Messy Literature. OXFORD RESEARCH ENCYCLOPEDIA OF ECONOMICS AND FINANCE. Oxford University Press. 10.1093/acrefore/9780190625979.013.375. [DOI] [Google Scholar]
- Crimmins EM, Finch CE, 2006. Infection, inflammation, height, and longevity. Proceedings of the National Academy of Sciences of the United States of America 103 (2), 498–503. 10.1073/PNAS.0501470103/SUPPL_FILE/01470FIG4.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha F, Heckman J, 2007. The Technology of Skill Formation. American Economic Review 97 (2), 31–47. 10.1257/AER.97.2.31. [DOI] [Google Scholar]
- Currie J, Stabile M, Manivong P, Roos LL, 2010. Child Health and Young Adult Outcomes. Journal of Human Resources 45 (3), 517–548. 10.3368/JHR.45.3.517. [DOI] [Google Scholar]
- De Chaisemartin C, D’haultfoeuille X, 2020. Two-Way Fixed Effects Estimators with Heterogeneous Treatment Effects. American Economic Review 110 (9), 2964–2996. 10.1257/AER.20181169. [DOI] [Google Scholar]
- Deaton A, 2007. Height, health, and development. Proceedings of the National Academy of Sciences 104 (33), 13232–13237. 10.1073/PNAS.0611500104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deaton A, Arora R, 2009. Life at the top: The benefits of height. Economics and Human Biology 7 (2), 133–136. 10.1016/j.ehb.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding R, He P, 2021. Associations between childhood adversities and late-life cognitive function: Potential mechanisms. Social Science & Medicine 291, 114478. 10.1016/J.SOCSCIMED.2021.114478. [DOI] [PubMed] [Google Scholar]
- Fillmore I, Ham H, Kerwin J, Marks M, Mas A, Rothstein J, Schulhofer-Wohl S, Slutsky D, Stevenson B, Sojourner A, We AW, Cai J, Furdek R, Lehninger R, Wang W, Zawila S, Johnson JE, Kleiner MM, 2020. Is Occupational Licensing a Barrier to Interstate Migration? American Economic Journal: Economic Policy 12 (3), 347–373. 10.1257/POL.20170704. [DOI] [Google Scholar]
- Finch CE, Crimmins EM, 2004. Inflammatory exposure and historical changes in human life-spans. Science 305 (5691), 1736–1739. 10.1126/SCIENCE.1092556/ASSET/02F255E8-C8D1-46C1-B84F-0E0CD47778A7/ASSETS/GRAPHIC/ZSE0360428410001.JPEG. [DOI] [PubMed] [Google Scholar]
- Fletcher JM, 2011. The medium term schooling and health effects of low birth weight: Evidence from siblings. Economics of Education Review 30 (3), 517–527. 10.1016/j.econedurev.2010.12.012. [DOI] [Google Scholar]
- Fletcher JM, 2015. New evidence of the effects of education on health in the US: Compulsory schooling laws revisited. Social Science & Medicine 127, 101–107. 10.1016/J.SOCSCIMED.2014.09.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, 2018a. New evidence on the impacts of early exposure to the 1918 influenza pandemic on old-age mortality. Biodemography and Social Biology 64 (2), 123–126. 10.1080/19485565.2018.1501267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, 2018b. Examining the long-term mortality effects of early health shocks. Applied Economics Letters 26 (11), 902–908. 10.1080/13504851.2018.1520960. [DOI] [Google Scholar]
- Fletcher JM, Green JC, Neidell MJ, 2010. Long term effects of childhood asthma on adult health. Journal of Health Economics 29 (3), 377–387. 10.1016/J.JHEALECO.2010.03.007. [DOI] [PubMed] [Google Scholar]
- Fletcher JM, & Noghanibehambari H (2021). The Effects of Education on Mortality: Evidence Using College Expansions. doi: 10.3386/W29423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher J, Topping M, Zheng F, Lu Q, 2021. The effects of education on cognition in older age: Evidence from genotyped Siblings. Social Science & Medicine 280, 114044. 10.1016/J.SOCSCIMED.2021.114044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank, A. A Iii, Ekelund RB, Jacksonj JD, 2003. Occupational Licensing of a Credence Good: The Regulation of Midwifery. Southern Economic Journal 69 (3), 659–675. 10.1002/J.2325-8012.2003.TB00519.X. [DOI] [Google Scholar]
- Gensollen T, Iyer SS, Kasper DL, Blumberg RS, 2016. How colonization by microbiota in early life shapes the immune system. Science 352 (6285), 539–544. 10.1126/SCIENCE.AAD9378/ASSET/2F91909F-0DF5-4161-88BB-078F2A92D227/ASSETS/GRAPHIC/352_539_F3.JPEG. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA, Beedle AS, 2007. Early life events and their consequences for later disease: A life history and evolutionary perspective. American Journal of Human Biology 19 (1), 1–19. 10.1002/AJHB.20590. [DOI] [PubMed] [Google Scholar]
- Gluckman PD, Hanson MA, Cooper C, Thornburg KL, 2008. Effect of In Utero and Early-Life Conditions on Adult Health and Disease. New England Journal of Medicine 359 (1), 61–73. 10.1056/NEJMRA0708473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godlonton S, Okeke EN, 2016. Does a ban on informal health providers save lives? Evidence from Malawi. Journal of Development Economics 118, 112–132. 10.1016/J.JDEVECO.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goebel T, 1994. Professionalization and State Building: The State and the Professions in Illinois, 1870–1920. Social Science History 18 (2), 309–337. 10.1017/S0145553200017028. [DOI] [Google Scholar]
- Goldstein JR, Alexander M, Breen C, Miranda González A, Menares F, Osborne M, Snyder M, Yildirim U, 2021. Censoc Project. CENSOC MORTALITY FILE: VERSION 2.0. University of California, Berkeley. https://censoc.berkeley.edu/data/. [Google Scholar]
- Goodman-Bacon A, 2021a. Difference-in-differences with variation in treatment timing. Journal of Econometrics. 10.1016/J.JECONOM.2021.03.014. [DOI] [Google Scholar]
- Goodman-Bacon A, 2021b. The Long-Run Effects of Childhood Insurance Coverage: Medicaid Implementation, Adult Health, and Labor Market Outcomes. American Economic Review 111 (8), 2550–2593. 10.1257/AER.20171671. [DOI] [Google Scholar]
- Gruber J, Frakes M, 2006. Does falling smoking lead to rising obesity? Journal of Health Economics 25 (2), 183–197. 10.1016/J.JHEALECO.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Gorman BK, 2004. The long arm of childhood: The influence of early-life social conditions on men’s mortality. Demography 41 (1), 87–107. 10.1353/DEM.2004.0005. 2004 41:1. [DOI] [PubMed] [Google Scholar]
- Heckman J, Pinto R, Savelyev P, 2013. Understanding the Mechanisms through Which an Influential Early Childhood Program Boosted Adult Outcomes. American Economic Review 103 (6), 2052–2086. 10.1257/AER.103.6.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Högberg U, 2011. The Decline in Maternal Mortality in Sweden: The Role of Community Midwifery. American Journal of Public Health 94 (8), 1312–1320. 10.2105/AJPH.94.8.1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Homer CSE, Friberg IK, Dias MAB, Ten Hoope-Bender P, Sandall J, Speciale AM, Bartlett LA, 2014. The projected effect of scaling up midwifery. The Lancet 384 (9948), 1146–1157. 10.1016/S0140-6736(14)60790-X. [DOI] [PubMed] [Google Scholar]
- Jacobson PH, 1956. Hospital care and the vanishing midwife. The Milbank Memorial Fund Quarterly 34 (3), 253–261. 10.2307/3348527. [DOI] [PubMed] [Google Scholar]
- Joyce T, 1999. Impact of augmented prenatal care on birth outcomes of Medicaid recipients in New York City. Journal of Health Economics 18 (1), 31–67. 10.1016/S0167-6296(98)00027-7. [DOI] [PubMed] [Google Scholar]
- Kes A, Ogwang S, Pande RP, Douglas Z, Karuga R, Odhiambo FO, Laserson K, Schaffer K, 2015. The economic burden of maternal mortality on households: Evidence from three sub-counties in rural western Kenya. Reproductive Health 12 (1), 1–10. 10.1186/1742-4755-12-S1-S3/TABLES/9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiner MM, 2000. Occupational Licensing. Journal of Economic Perspectives 14 (4), 189–202. 10.1257/JEP.14.4.189. [DOI] [Google Scholar]
- Kleiner MM, 2017. The influence of occupational licensing and regulation. IZA World of Labor. 10.15185/IZAWOL.392. [DOI] [Google Scholar]
- Kleiner MM, Discussants Joskow P, 2016. Battling over Jobs: Occupational Licensing in Health Care. American Economic Review 106 (5), 165–170. 10.1257/AER.P20161000. [DOI] [PubMed] [Google Scholar]
- Kleiner MM, Krueger AB, 2010. The Prevalence and Effects of Occupational Licensing. British Journal of Industrial Relations 48 (4), 676–687. 10.1111/J.1467-8543.2010.00807.X. [DOI] [Google Scholar]
- Kleiner MM, Krueger AB, 2013. Analyzing the extent and influence of occupational licensing on the labor market. Journal of Labor Economics 31 (2 PART2). 10.1086/669060/ASSET/IMAGES/LARGE/FG1_ONLINE.JPEG. [DOI] [Google Scholar]
- Kleiner MM, Kudrle RT, 2000. Does Regulation Affect Economic Outcomes? the Case of Dentistry*. The Journal of Law and Economics 43 (2), 547–582. 10.1086/467465. [DOI] [Google Scholar]
- Kleiner MM, Marier A, Park KW, Wing C, 2016. Relaxing occupational licensing requirements: Analyzing wages and prices for a medical service. Journal of Law and Economics 59 (2), 261–291. 10.1086/688093/ASSET/IMAGES/LARGE/FGA1.JPEG. [DOI] [Google Scholar]
- Kniesner TJ, Viscusi WK, 2019. The Value of a Statistical Life. Oxford Research Encyclopedia of Economics and Finance. 10.1093/ACREFORE/9780190625979.013.138. [DOI] [Google Scholar]
- Law MT, Kim S, 2005. Specialization and Regulation: The Rise of Professionals and the Emergence of Occupational Licensing Regulation. The Journal of Economic History 65 (3), 723–756. 10.1017/S0022050705000264. [DOI] [Google Scholar]
- Law MT, Marks MS, 2009. Effects of occupational licensing laws on minorities: Evidence from the progressive era. Journal of Law and Economics 52 (2), 351–366. 10.1086/596714/ASSET/IMAGES/LARGE/FG1.JPEG. [DOI] [Google Scholar]
- Lazuka V, 2018. The long-term health benefits of receiving treatment from qualified midwives at birth. Journal of Development Economics 133, 415–433. 10.1016/j.jdeveco.2018.03.007. [DOI] [Google Scholar]
- Lee C, Ryff CD, 2019. Pathways linking combinations of early-life adversities to adult mortality: Tales that vary by gender. Social Science & Medicine 240, 112566. 10.1016/J.SOCSCIMED.2019.112566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei MK, Berg MT, Simons RL, Simons LG, Beach SRH, 2020. Childhood adversity and cardiovascular disease risk: An appraisal of recall methods with a focus on stress-buffering processes in childhood and adulthood. Social Science & Medicine 246, 112794. 10.1016/J.SOCSCIMED.2020.112794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindeboom M, Portrait F, Van Den Berg GJ, 2010. Long-run effects on longevity of a nutritional shock early in life: The Dutch Potato famine of 1846–1847. Journal of Health Economics 29 (5), 617–629. 10.1016/J.JHEALECO.2010.06.001. [DOI] [PubMed] [Google Scholar]
- Lleras-Muney A, 2005. The Relationship Between Education and Adult Mortality in the United States. The Review of Economic Studies 72 (1), 189–221. 10.1111/0034-6527.00329. [DOI] [Google Scholar]
- Lleras-Muney A, Price J, & Yue D (2020). The Association Between Educational Attainment and Longevity using Individual Level Data from the 1940 Census. doi: 10.3386/W27514. [DOI] [PubMed] [Google Scholar]
- Luecken LJ, Roubinov DS, 2012. Pathways to Lifespan Health Following Childhood Parental Death. Social and Personality Psychology Compass 6 (3), 243–257. 10.1111/J.1751-9004.2011.00422.X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz S, Adams EK, Lewitt MJ, Dunlop AL, 2017. Competitive effects of scope of practice restrictions: Public health or public harm? Journal of Health Economics 55, 201–218. 10.1016/J.JHEALECO.2017.07.004. [DOI] [PubMed] [Google Scholar]
- Maruyama S, Heinesen E, 2020. Another look at returns to birthweight. Journal of Health Economics 70, 102269. 10.1016/j.jhealeco.2019.102269. [DOI] [PubMed] [Google Scholar]
- Maurizi A, 1974. Occupational Licensing and the Public Interest. Journal of Political Economy 82 (2), 399–413. 10.1086/260199. Part 1. [DOI] [Google Scholar]
- Mazumder B, 2008. Does education improve health? A reexamination of the evidence from compulsory schooling laws. Economic Perspectives 32 (Q II), 2–16. [Google Scholar]
- McCauley H, Lowe K, Furtado N, Mangiaterra V, van den Broek N, 2022. Essential components of postnatal care – a systematic literature review and development of signal functions to guide monitoring and evaluation. BMC Pregnancy and Childbirth 22 (1), 1–16. 10.1186/S12884-022-04752-6/TABLES/2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael BJ, 2017. The Demand for Healthcare Regulation: The Effect of Political Spending on Occupational Licensing Laws. Southern Economic Journal 84 (1), 297–316. 10.1002/SOEJ.12211. [DOI] [Google Scholar]
- Meer J, West J, 2016. Effects of the Minimum Wage on Employment Dynamics. Journal of Human Resources 51 (2), 500–522. 10.3368/JHR.51.2.0414-6298R1. [DOI] [Google Scholar]
- Meghir C, Palme M, Simeonova E, 2018. Education and Mortality: Evidence from a Social Experiment. American Economic Journal: Applied Economics 10 (2), 234–256. 10.1257/APP.20150365. [DOI] [Google Scholar]
- Miller AR, 2006. The Impact of Midwifery-Promoting Public Policies on Medical Interventions and Health Outcomes. Advances in Economic Analysis & Policy 6 (1). 10.2202/1538-0637.1589. [DOI] [Google Scholar]
- Montez J, Hayward MD, 2011. Early Life Conditions and Later Life Mortality. International Handbook of Adult Mortality; 187–206. 10.1007/978-90-481-9996-9_9. [DOI] [Google Scholar]
- Moore SE, Collinson AC, N’Gom PT, Aspinall R, Prentice AM, 2006. Early immunological development and mortality from infectious disease in later life. Proceedings of the Nutrition Society 65 (3), 311–318. 10.1079/PNS2006503. [DOI] [PubMed] [Google Scholar]
- Noghanibehambari H, Engelman M, 2022. Social insurance programs and later-life mortality: Evidence from new deal relief spending. Journal of Health Economics 86. 10.1016/J.JHEALECO.2022.102690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noghanibehambari H, & Fletcher JM (2022). Dust to Feed, Dust to Grey: The Effect of In-Utero Exposure to the Dust Bowl on Old-Age Longevity. doi: 10.3386/W30531. [DOI] [PubMed] [Google Scholar]
- Noghanibehambari H, Noghani F, 2023. Long-run intergenerational health benefits of women empowerment: Evidence from suffrage movements in the US. Health Economics. 10.1002/HEC.4744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochoa TJ, Salazar-Lindo E, Cleary TG, 2004. Management of children with infection-associated persistent diarrhea. Seminars in Pediatric Infectious Diseases 15 (4), 229–236. 10.1053/J.SPID.2004.07.003. [DOI] [PubMed] [Google Scholar]
- Peterson BD, Pandya SS, Leblang D, 2014. Doctors with borders: Occupational licensing as an implicit barrier to high skill migration. Public Choice 160 (1–2), 45–63. 10.1007/S11127-014-0152-8/TABLES/3. [DOI] [Google Scholar]
- Rooks JP, 1999. The midwifery model of care. Journal of Nurse-Midwifery 44 (4), 370–374. 10.1016/S0091-2182(99)00060-9. [DOI] [PubMed] [Google Scholar]
- Rostila M, Saarela JM, 2011. Time Does Not Heal All Wounds: Mortality Following the Death of a Parent. Journal of Marriage and Family 73 (1), 236–249. 10.1111/J.1741-3737.2010.00801.X. [DOI] [Google Scholar]
- Royer H, 2009. Separated at girth: US twin estimates of the effects of birth weight. American Economic Journal: Applied Economics 1 (1), 49–85. 10.1257/app.1.1.49. [DOI] [Google Scholar]
- Rude AE, 1923. The midwife problem in the United States. Journal of the American Medical Association 81 (12), 987–992. 10.1001/JAMA.1923.02650120019006. [DOI] [Google Scholar]
- Ruggles S, Flood S, Goeken R, Grover J, Meyer E, 2020. IPUMS USA: Version 10.0. IPUMS, Minneapolis, MN, 10.18128/D010.V10.0. [DOI] [Google Scholar]
- Salm M, 2011. The Effect of Pensions on Longevity: Evidence from Union Army Veterans. The Economic Journal 121 (552), 595–619. 10.1111/J.1468-0297.2011.02427.X. [DOI] [Google Scholar]
- Scholte RS, Van Den Berg GJ, Lindeboom M, 2015. Long-run effects of gestation during the Dutch Hunger Winter famine on labor market and hospitalization outcomes. Journal of Health Economics 39, 17–30. 10.1016/J.JHEALECO.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Shakya S, Ghosh S, Norris C, 2022. Nurse Licensure Compact and Mobility. Journal of Labor Research 43 (2), 260–274. 10.1007/S12122-022-09333-2/FIGURES/2. [DOI] [Google Scholar]
- Shapiro C, 1986. Investment, Moral Hazard, and Occupational Licensing. The Review of Economic Studies 53 (5), 843–862. 10.2307/2297722. [DOI] [Google Scholar]
- Shenk MK, Scelza BA, 2012. Paternal investment and status-related child outcomes: timing of father’s death affects offspring success. Journal of Biosocial Science 44 (5), 549–569. 10.1017/S0021932012000053. [DOI] [PubMed] [Google Scholar]
- Shepard L, 1978. Licensing Restrictions and the Cost of Dental Care. The Journal of Law and Economics 21 (1), 187–201. 10.1086/466916. [DOI] [Google Scholar]
- Smith JP, 2009. The Impact of Childhood Health on Adult Labor Market Outcomes. The Review of Economics and Statistics 91 (3), 478–489. 10.1162/REST.91.3.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JP, Smith GC, 2010. Long-term economic costs of psychological problems during childhood. Social Science & Medicine 71 (1), 110–115. 10.1016/J.SOCSCIMED.2010.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder SE, Evans WN, 2006. The effect of income on mortality: Evidence from the social security Notch. Review of Economics and Statistics 88 (3), 482–495. 10.1162/rest.88.3.482. [DOI] [Google Scholar]
- Steine IM, LeWinn KZ, Lisha N, Tylavsky F, Smith R, Bowman M, Sathyanarayana S, Karr CJ, Smith AK, Kobor M, Bush NR, 2020. Maternal exposure to childhood traumatic events, but not multi-domain psychosocial stressors, predict placental corticotrophin releasing hormone across pregnancy. Social Science & Medicine 266, 113461. 10.1016/J.SOCSCIMED.2020.113461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stikkelbroek Y, Prinzie P, de Graaf R, ten Have M, Cuijpers P, 2012. Parental death during childhood and psychopathology in adulthood. Psychiatry Research 198 (3), 516–520. 10.1016/J.PSYCHRES.2011.10.024. [DOI] [PubMed] [Google Scholar]
- Sun L, Abraham S, 2021. Estimating dynamic treatment effects in event studies with heterogeneous treatment effects. Journal of Econometrics 225 (2), 175–199. 10.1016/J.JECONOM.2020.09.006. [DOI] [Google Scholar]
- Sunder M, 2005. Toward generation XL: Anthropometrics of longevity in late 20th-century United States. Economics & Human Biology 3 (2), 271–295. 10.1016/J.EHB.2005.04.006. [DOI] [PubMed] [Google Scholar]
- Ten Hoope-Bender P, De Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, Homer CSE, Kennedy HP, Matthews Z, McFadden A, Renfrew MJ, Van Lerberghe W, 2014. Improvement of maternal and newborn health through midwifery. The Lancet 384 (9949), 1226–1235. 10.1016/S0140-6736(14)60930-2. [DOI] [PubMed] [Google Scholar]
- Thaddeus S, Maine D, 1994. Too far to walk: Maternal mortality in context. Social Science & Medicine 38 (8), 1091–1110. 10.1016/0277-9536(94)90226-7. [DOI] [PubMed] [Google Scholar]
- Timmons EJ, Mills A, 2018. Bringing the Effects of Occupational Licensing into Focus: Optician Licensing in the United States. Eastern Economic Journal 44 (1), 69–83. 10.1057/EEJ.2016.4/TABLES/8. [DOI] [Google Scholar]
- UNFPA. (2021). The State of the World’s Midwifery 2021 | United Nations Population Fund. https://www.unfpa.org/sowmy.
- Van Den Berg GJ, Gupta S, van den Berg GJ, Gupta S, 2015. The role of marriage in the causal pathway from economic conditions early in life to mortality. Journal of Health Economics 40, 141–158. 10.1016/j.jhealeco.2014.02.004. [DOI] [PubMed] [Google Scholar]
- Van Den Berg GJ, Lindeboom M, Portrait F, Berg G.J.Van Den, Lindeboom M, Portrait F, den Berg GJ, Lindeboom M, Portrait F, 2006. Economic Conditions Early in Life and Individual Mortality. American Economic Review 96 (1), 290–302. 10.1257/000282806776157740. [DOI] [PubMed] [Google Scholar]
- Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, De Bernis L, De Brouwere V, Fauveau V, Fogstad H, Koblinsky M, Liljestrand J, Mechbal A, Murray SF, Rathavay T, Rehr H, Richard F, Ten Hoope-Bender P, Turkmani S, 2014. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. The Lancet 384 (9949), 1215–1225. 10.1016/S0140-6736(14)60919-3. [DOI] [PubMed] [Google Scholar]
- Viscusi WK, 2018. Best Estimate Selection Bias in the Value of a Statistical Life. Journal of Benefit-Cost Analysis 9 (2), 205–246. 10.1017/BCA.2017.21. [DOI] [Google Scholar]
- WHO, 2020. World Health Organization Reports. Global Health Observatory data repository: Institutional births - Data by country. WHO. https://apps.who.int/gho/data/view.main.SRHIBv. [Google Scholar]
- Yang I, Corwin EJ, Brennan PA, Jordan S, Murphy JR, Dunlop A, 2016. The Infant Microbiome: Implications for Infant Health and Neurocognitive Development. Nursing Research 65 (1), 76. 10.1097/NNR.0000000000000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


